TOP 10 ARTICLES FROM 2017 CGS Annual Scientific



- Slides: 63

TOP 10 ARTICLES FROM 2017 CGS Annual Scientific Meeting – April 2018 Fadi Massoud MD FRCPC Internist – Geriatrician Centre Hospitalier Charles Le. Moyne and Institut de Gériatrie de Montréal
• I have no conflicts of interest to declare

Bad Year for Professional Sports in Montreal …

But there is hope !!
Introduction / Methods • Challenge ! • Pubmed Search – Elderly or old-age or geriatric or older adults or elders – N = 61 836 citations for 2017 ! • Personnal interests and biases • Review of TOC of general internal medicine journals, geriatric journals, specialized journals • Journal Watch / Medical Letter
Introduction / Methods • • • Two categories Geriatric Giants : 5 papers Medicine in the Elderly : 5 papers Other relevant references Not only research article…
GERIATIC GIANTS • • • New Dx Criteria for DLB SSRI in MCI Prevention of falls Neurophysiology of delirium Fesoterodine in Urinary Incontinence
Diagnostic Criteria for Dementia with Lewy Bodies
Diagnostic Criteria for DLB • Mc. Keith IG et al (DLB consortium); Neurology 2017; 89: 88– 100 • Fourth report – Last updated in 2005 • Multidisciplinary working groups (including patients and caregivers). • Clinical and Pathological criteria • Added value of biomarkers (indicative or supportive) • “Suggestive” clinical features replaced by “Supportive” clinical features
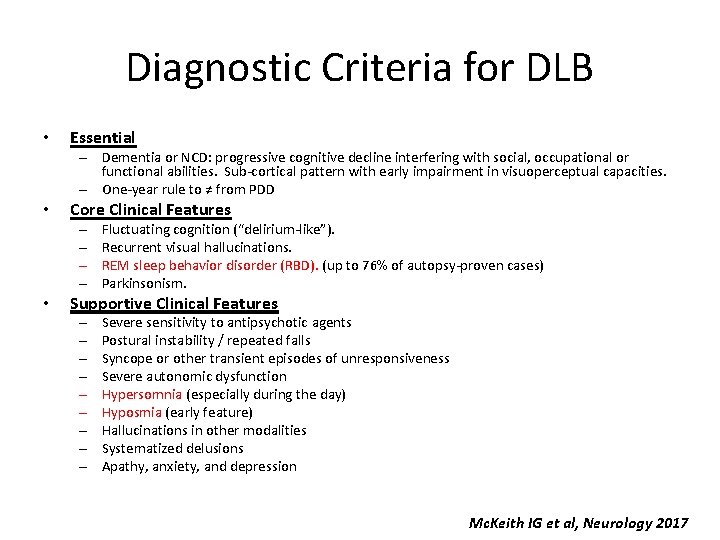
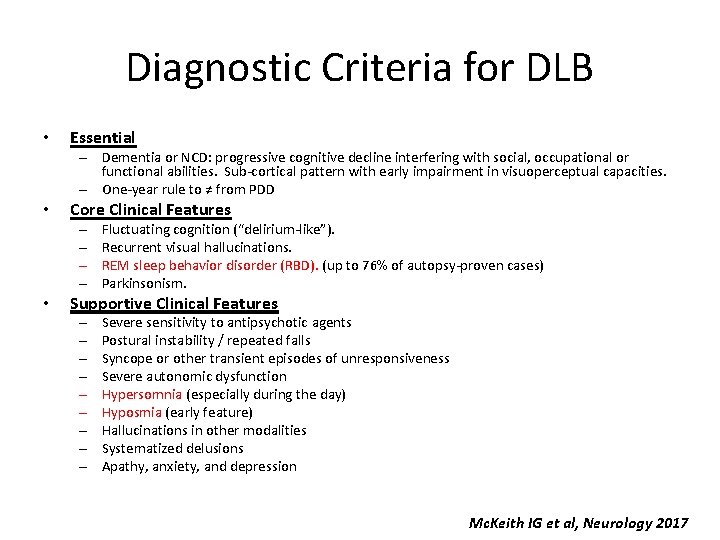
Diagnostic Criteria for DLB • Essential – Dementia or NCD: progressive cognitive decline interfering with social, occupational or functional abilities. Sub-cortical pattern with early impairment in visuoperceptual capacities. – One-year rule to ≠ from PDD • Core Clinical Features – – • Fluctuating cognition (“delirium-like”). Recurrent visual hallucinations. REM sleep behavior disorder (RBD). (up to 76% of autopsy-proven cases) Parkinsonism. Supportive Clinical Features – – – – – Severe sensitivity to antipsychotic agents Postural instability / repeated falls Syncope or other transient episodes of unresponsiveness Severe autonomic dysfunction Hypersomnia (especially during the day) Hyposmia (early feature) Hallucinations in other modalities Systematized delusions Apathy, anxiety, and depression Mc. Keith IG et al, Neurology 2017
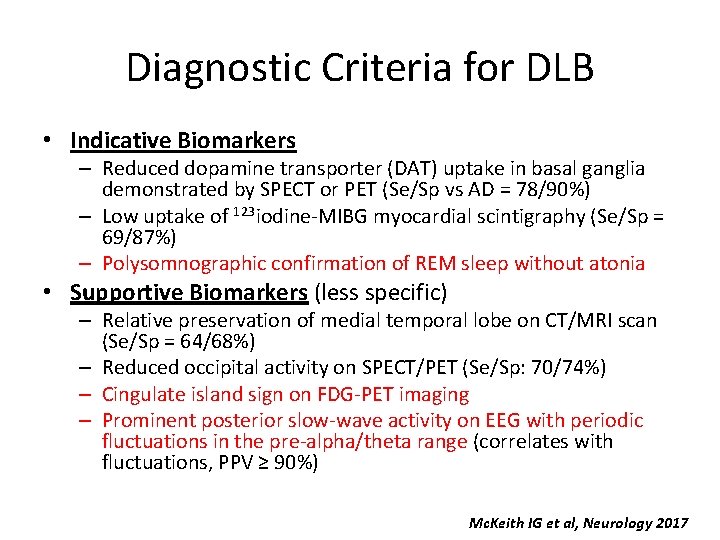
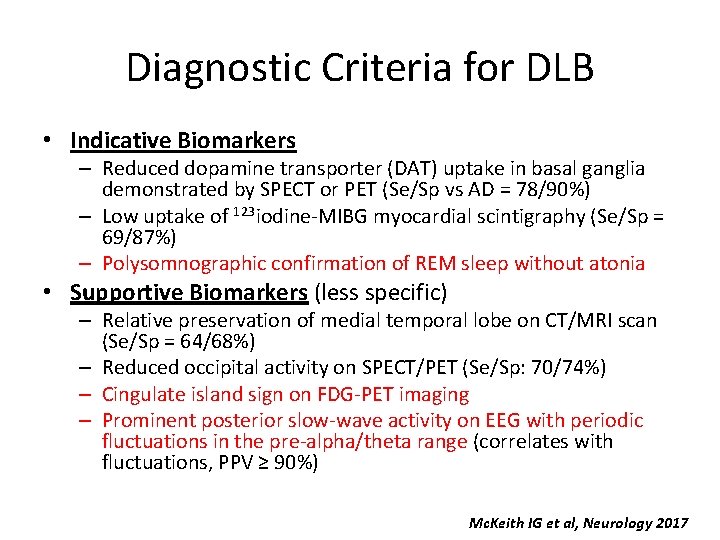
Diagnostic Criteria for DLB • Indicative Biomarkers – Reduced dopamine transporter (DAT) uptake in basal ganglia demonstrated by SPECT or PET (Se/Sp vs AD = 78/90%) – Low uptake of 123 iodine-MIBG myocardial scintigraphy (Se/Sp = 69/87%) – Polysomnographic confirmation of REM sleep without atonia • Supportive Biomarkers (less specific) – Relative preservation of medial temporal lobe on CT/MRI scan (Se/Sp = 64/68%) – Reduced occipital activity on SPECT/PET (Se/Sp: 70/74%) – Cingulate island sign on FDG-PET imaging – Prominent posterior slow-wave activity on EEG with periodic fluctuations in the pre-alpha/theta range (correlates with fluctuations, PPV ≥ 90%) Mc. Keith IG et al, Neurology 2017
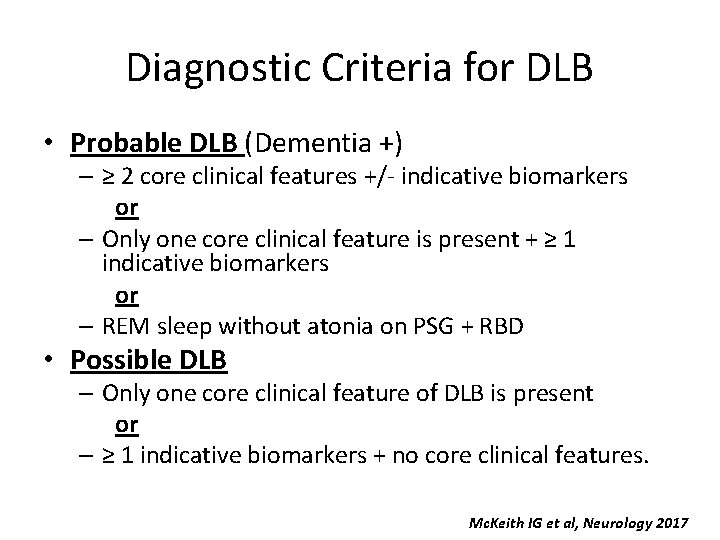
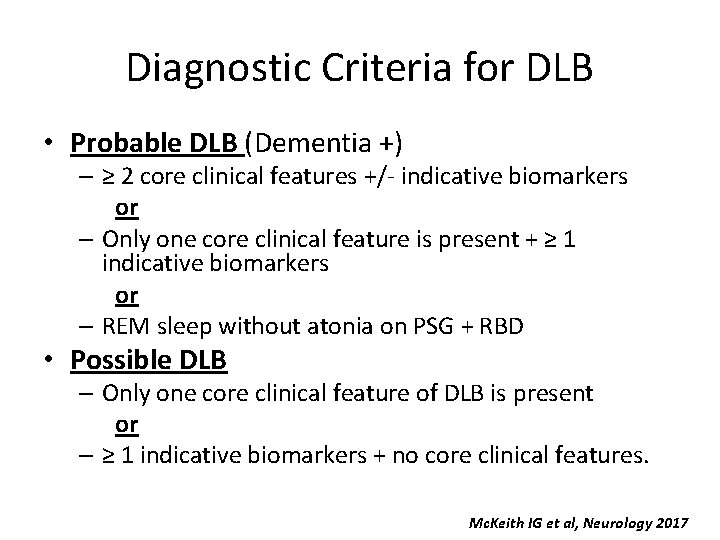
Diagnostic Criteria for DLB • Probable DLB (Dementia +) – ≥ 2 core clinical features +/- indicative biomarkers or – Only one core clinical feature is present + ≥ 1 indicative biomarkers or – REM sleep without atonia on PSG + RBD • Possible DLB – Only one core clinical feature of DLB is present or – ≥ 1 indicative biomarkers + no core clinical features. Mc. Keith IG et al, Neurology 2017
SSRIs in Mild Cognitive Impairment
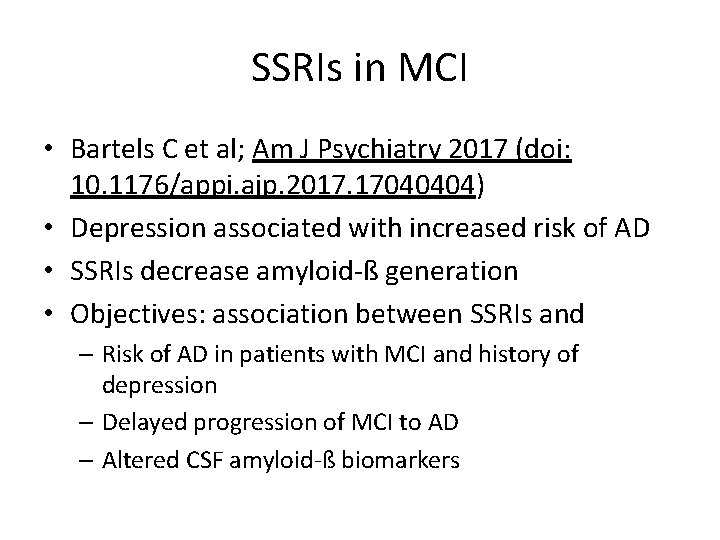
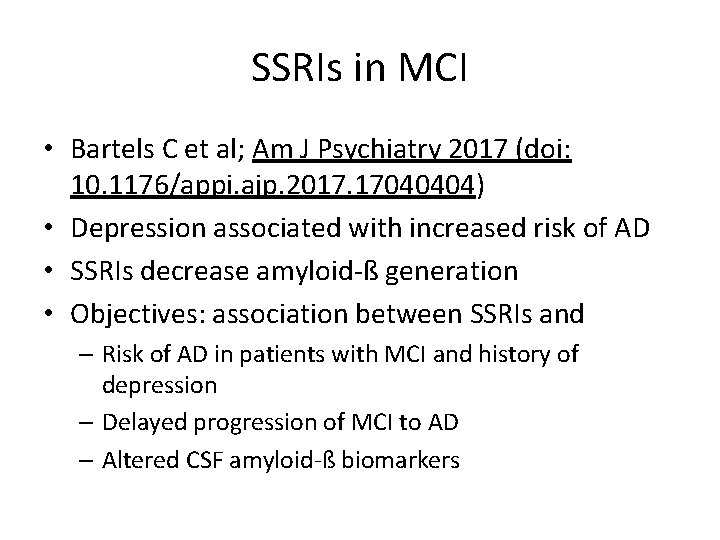
SSRIs in MCI • Bartels C et al; Am J Psychiatry 2017 (doi: 10. 1176/appi. ajp. 2017. 17040404) • Depression associated with increased risk of AD • SSRIs decrease amyloid-ß generation • Objectives: association between SSRIs and – Risk of AD in patients with MCI and history of depression – Delayed progression of MCI to AD – Altered CSF amyloid-ß biomarkers
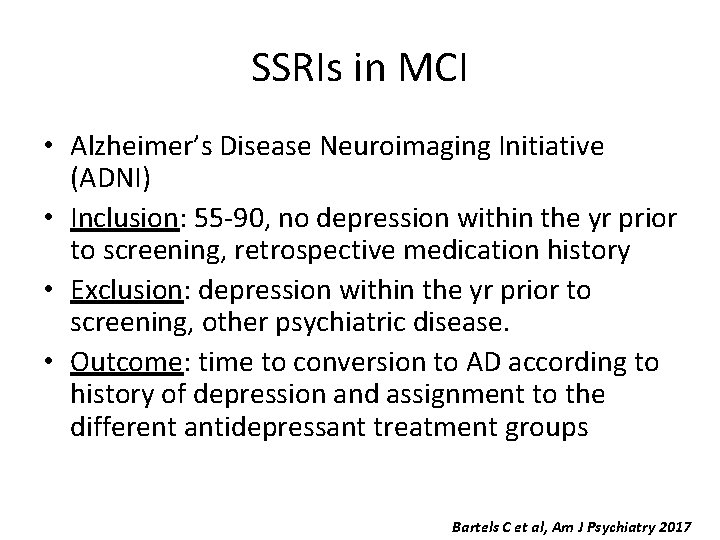
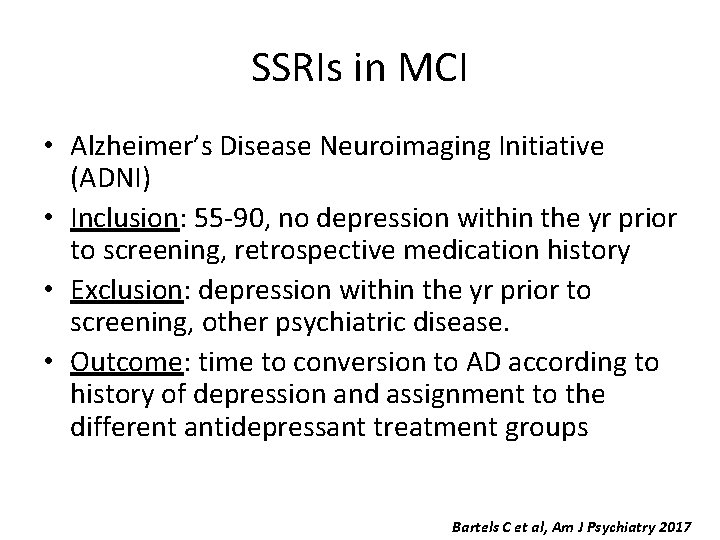
SSRIs in MCI • Alzheimer’s Disease Neuroimaging Initiative (ADNI) • Inclusion: 55 -90, no depression within the yr prior to screening, retrospective medication history • Exclusion: depression within the yr prior to screening, other psychiatric disease. • Outcome: time to conversion to AD according to history of depression and assignment to the different antidepressant treatment groups Bartels C et al, Am J Psychiatry 2017
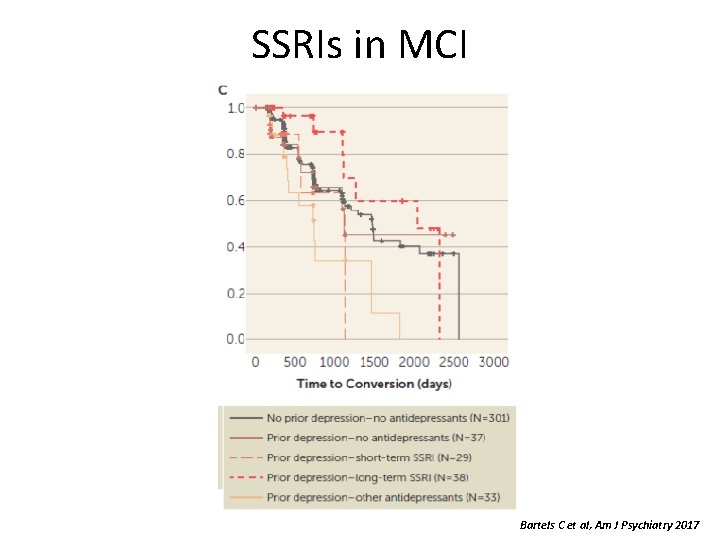
SSRIs in MCI • N = 438 individuals with MCI / Mean age = 72. 6 / Mean MMSE = 27. 7 / ♀: 34% • Mean follow-up period = 691 d • Mean duration of ATD Tx = 2, 256 d • History of depression not associated with rate of conversion • probability of progression in long-term (>1610 d of Tx) SSRI-treated subgroup vs other-antidepressants (and no Tx) subgroup. • Kaplan-Meier analysis: decreased conversion persisted up to 3 years of FU. • No main effect of treatment on Amyloid-ß biomarkers Bartels C et al, Am J Psychiatry 2017
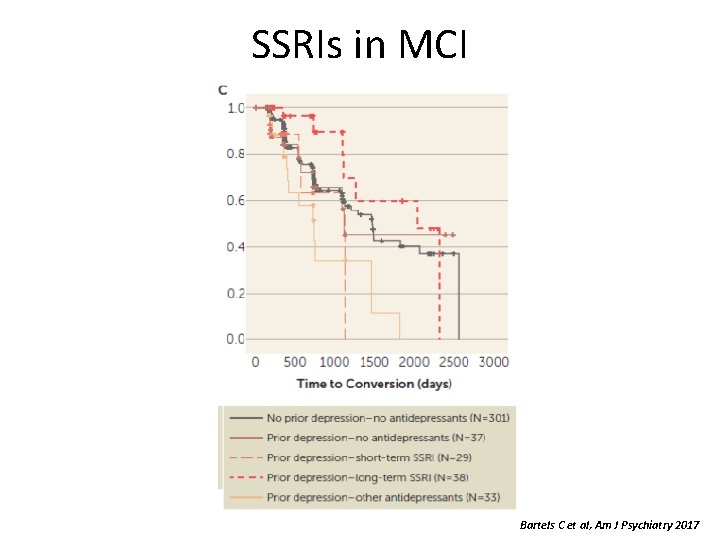
SSRIs in MCI Bartels C et al, Am J Psychiatry 2017
SSRIs in MCI • Strengths – Multicenter, prospective, longitudinal cohort / highly standardized, research-based definitions. – Large number of individuals – Exclusion of depression at baseline • Limitations – Recurrent episodes vs late-life depression? – No information on duration, severity, and treatment of past episodes – Observational: Rx not randomly assigned • Conclusions – Long-term SSRI maintenance treatment may be beneficial in elderly patients with MCI and a history of depression – Three-year delay in conversion of MCI to Alzheimer’s dementia – Recommend a prospective intervention study Bartels C et al, Am J Psychiatry 2017
Prevention of Falls
Prevention of Falls • Tricco AC et al; JAMA 2017: 318(17): 1687 -1699 • Substantial burden for patients and health care systems. • Incidence of falls on the rise • Objective: – Assess effectiveness of interventions for preventing falls
Prevention of Falls • Systematic review / pairwise and network metanalyses – Direct evidence and indirect comparisons (inferred by the results of other comparisons) • Inclusion – RCT of fall prevention interventions – ≥ 65 • Main outcome: – Injurious falls – Fall-related hospitalization Tricco AC et al, JAMA 2017
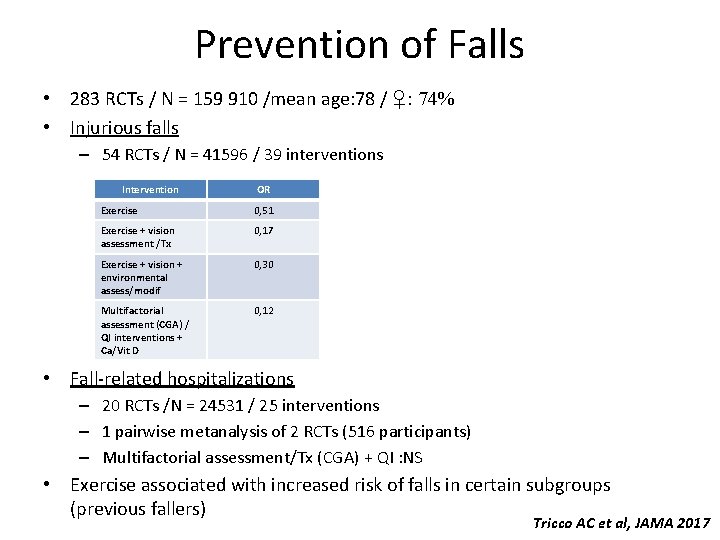
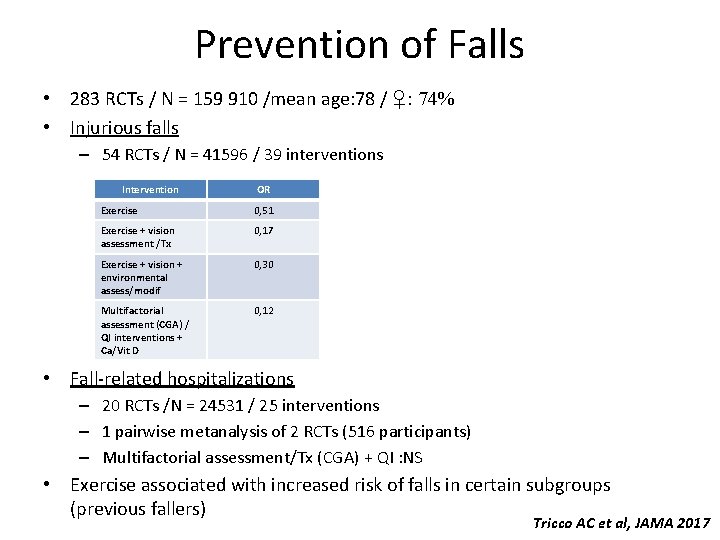
Prevention of Falls • 283 RCTs / N = 159 910 /mean age: 78 / ♀: 74% • Injurious falls – 54 RCTs / N = 41596 / 39 interventions Intervention OR Exercise 0, 51 Exercise + vision assessment /Tx 0, 17 Exercise + vision + environmental assess/modif 0, 30 Multifactorial assessment (CGA) / QI interventions + Ca/Vit D 0, 12 • Fall-related hospitalizations – 20 RCTs /N = 24531 / 25 interventions – 1 pairwise metanalysis of 2 RCTs (516 participants) – Multifactorial assessment/Tx (CGA) + QI : NS • Exercise associated with increased risk of falls in certain subgroups (previous fallers) Tricco AC et al, JAMA 2017
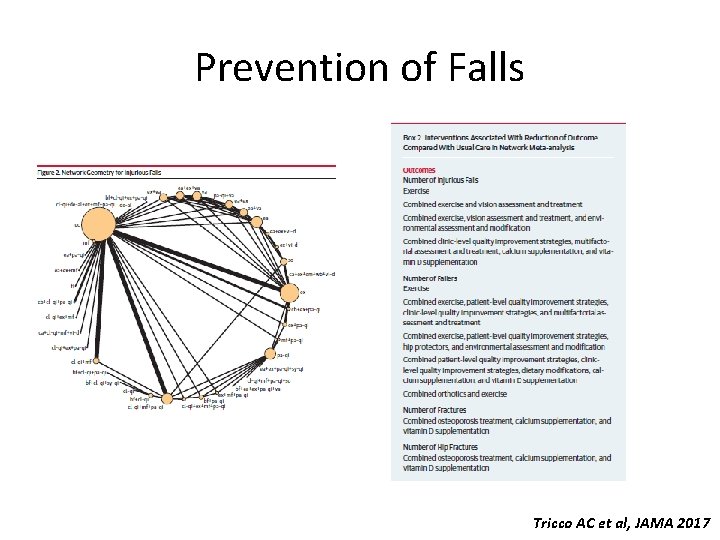
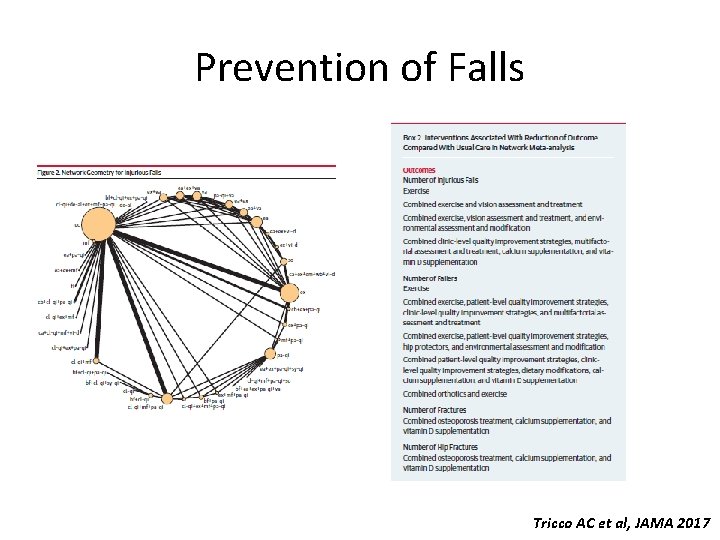
Prevention of Falls Tricco AC et al, JAMA 2017
Prevention of Falls • Limitations – Insufficient data for some secondary outcomes (cost) – Large number of comparisons (Multiplicity) and risk or type I error. • Strengths – Largest metanalysis / review – Reviewers worked in pairs + 3 rd reviewer cleaned data – Standards of the International Society for Pharmacoeconomics and Outcomes Research • Conclusions – Exercise alone and various combined interventions were associated with lower risk of injurious falls compared with usual care – Editorial calls for proactive approach to prevention based on this data Tricco AC et al, JAMA 2017
Neurophysiology of Delirium J Am Geriatr Soc 2017; 65: 1114– 1118
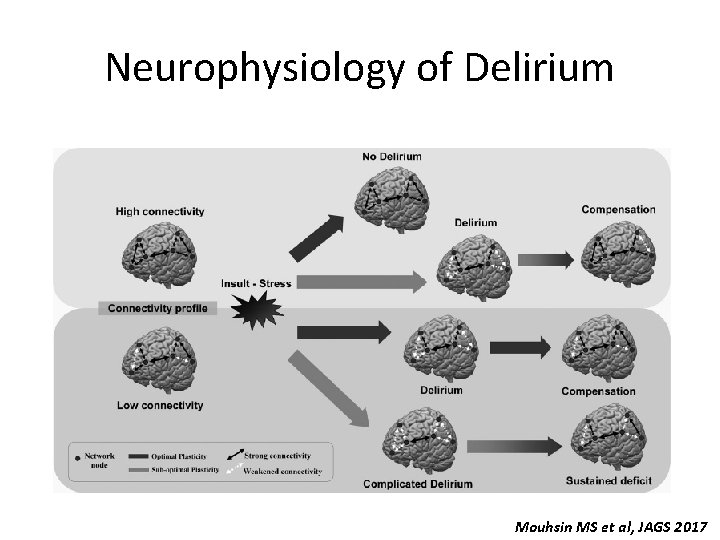
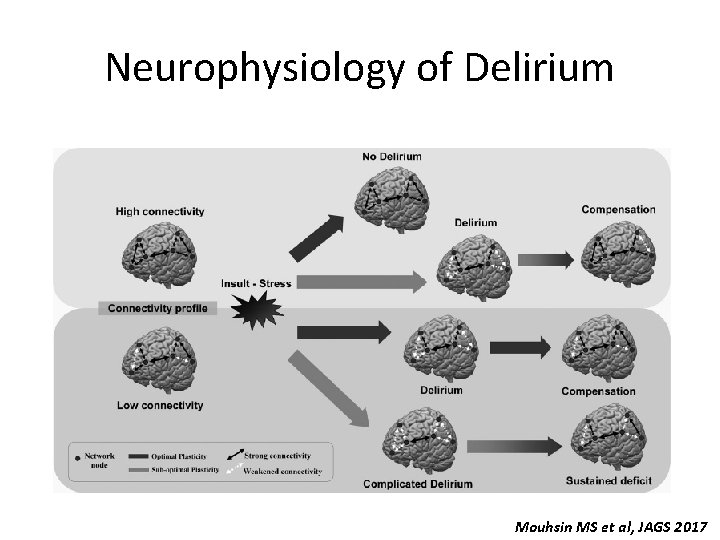
Neurophysiology of Delirium • Common and costly medical complication • Review of neurophysiologic changes in brain function in delirium and dementia • Conceptual model of delirium • Occurrence and prognosis results from impairment in : – Brain connectivity – Brain plasticity • Potential use for prevention and guiding interventions Mouhsin MS et al, JAGS 2017
Neurophysiology of Delirium • Connectivity (functional/effective) – EEG • Changes in Delirium • Differentiate delirium from other conditions (dementia, epilepsy, psychiatric conditions, etc. ) – Resting state f. MRI • Abnormal interactions between brains regions in delirium • Connectivity and plasticity – TMS-EEG: Transcranial Magnetic Stimulation (TMS) – Non-invasive brain stimulation to produce change in activity cerebral response indicative of connectivity and plasticity – Studies in hepatic encephalopathy and AD – Potential for use in delirium
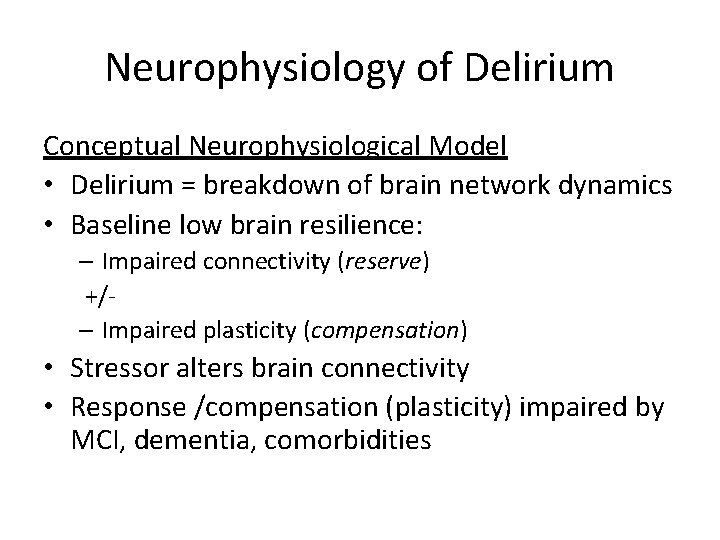
Neurophysiology of Delirium Conceptual Neurophysiological Model • Delirium = breakdown of brain network dynamics • Baseline low brain resilience: – Impaired connectivity (reserve) +/– Impaired plasticity (compensation) • Stressor alters brain connectivity • Response /compensation (plasticity) impaired by MCI, dementia, comorbidities
Neurophysiology of Delirium Mouhsin MS et al, JAGS 2017
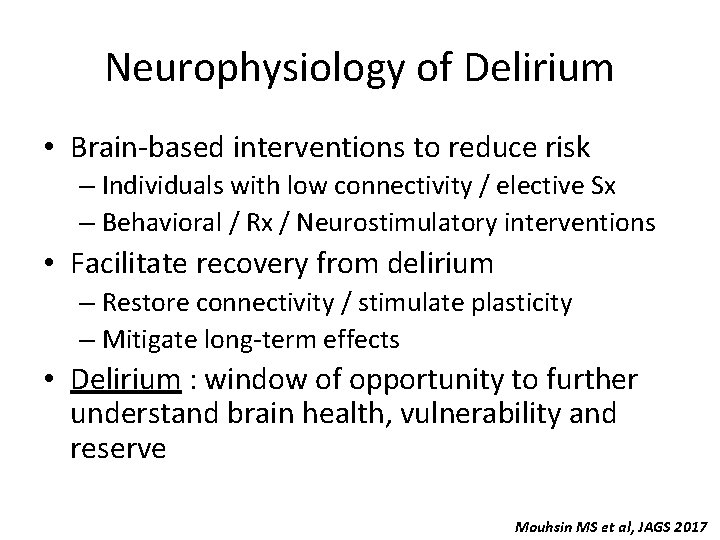
Neurophysiology of Delirium • Brain-based interventions to reduce risk – Individuals with low connectivity / elective Sx – Behavioral / Rx / Neurostimulatory interventions • Facilitate recovery from delirium – Restore connectivity / stimulate plasticity – Mitigate long-term effects • Delirium : window of opportunity to further understand brain health, vulnerability and reserve Mouhsin MS et al, JAGS 2017
Fesoterodine in Urinary Incontinence
Fesoterodine in Urinary Incontinence • Clinicians reluctant to use antimuscarinic agents in OAB • Efficacy and safety from patients ≥ 65 in fesoterodine trials • Attention to coexisting Rx and comorbidities • Data from 10 DBRCT (phase 3 -4) / N = 4040 (2116 ≥ 65) • Treatment-emergent adverse (TEAE) events considering coexisting Rx and comorbidities Wagg A et al, Age & Ageing 2017
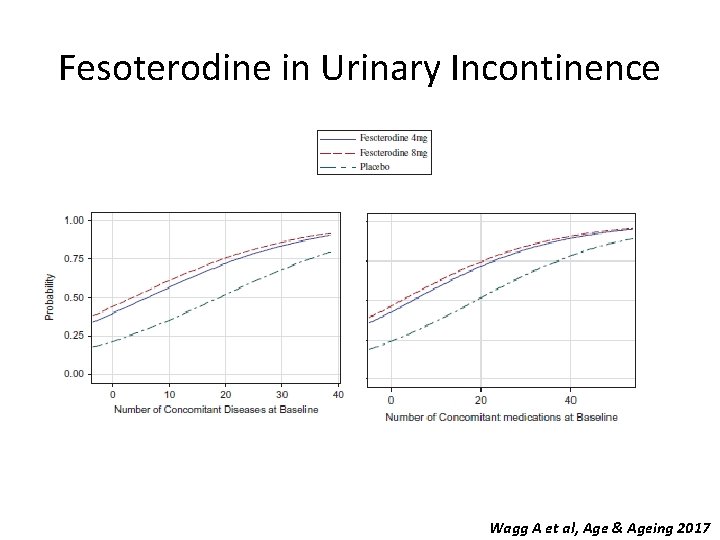
Fesoterodine in Urinary Incontinence • Fesoterodine improved all disease-related and patient-reported outcomes vs Pbo (SS) at 12 wks (both 65 -74 and ≥ 75 subgoups) • TEAE higher in the fesoterodine groups vs pbo • TEAE associated with number of Rx (OR: 1, 028/Rx) and comorbidities (OR: 1, 058/disease) • Few TEAEs of the CNS across entire population – Not associated with fesoterodine dose – No clear cumulative effect with number of coexisting Rx Wagg A et al, Age & Ageing 2017
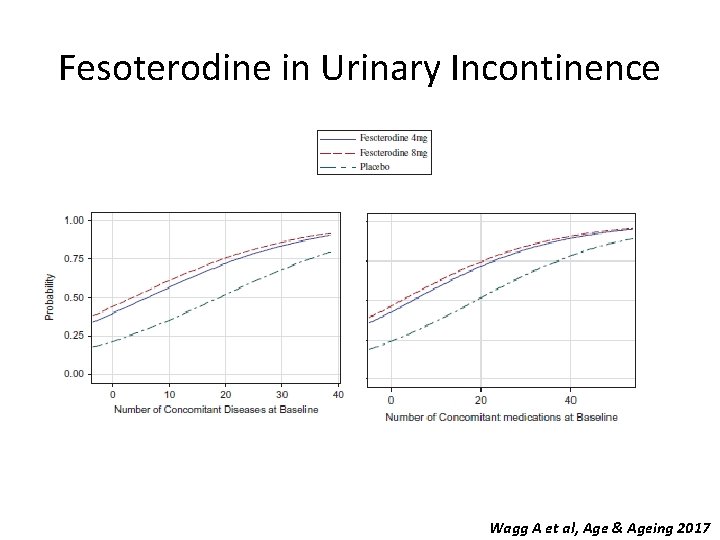
Fesoterodine in Urinary Incontinence Wagg A et al, Age & Ageing 2017
Fesoterodine in Urinary Incontinence • Limitations – Generalizability – Categories of Rx and concomitant disease not evaluated – Short exposure time • Conclusions – Confirms clinical efficacy / safety of fesoterodine for the treatment of OAB in ≥ 65 – Additional impact of polypharmacy and multimorbidity on the likelihood of experiencing TEAE – “Peripheral” anticholinergic side effects ? Wagg A et al, Age & Ageing 2017
MEDICINE IN THE ELDERLY • • • Rumozumab for osteoporosis Levothyroxine in subclinical hypothyroidism New zoster vaccine Probiotics for prevention of C Difficile infection AHA guidelines for HTN
Romosozumab for Postmenopausal Osteoporosis
Romosozumab for Osteoporosis • Use of sequential therapy in OP is the focus of much attention • Bone-forming agents (teriparatide): – Very high fracture risk – Previously exposed to biphosphonate therapy – Clinical benefit might be reduced in previous users of biphosphonates (blunting BMD gains especially at hip) • Romosozumab (AMG 785): inhibits sclerostin – ↑ bone formation and ↓bone resorption – Superior gains in BMD than alendronate or teriparatide (Mc. Clung MR et al, N Engl J Med 2014) Langdahl BL et al, Lancet 2017
Romosozumab for Osteoporosis • Inclusion – ♀55 -90 – postmenoposal osteoporosis – Oral bisphonate for ≥ 3 years (alendronate x 1 yr) – Mean duration: 6, 2 yrs – BMD T score ≤ 2, 5 hip/femoral neck/L spine – History of fracture • Intervention – Romosozomuab 210 mg s/c q 1 month vs Teriparatide 20 μg s/c q day x 12 months • Primary Outcome – Change BMD at months 6 and 12 Langdahl BL et al, Lancet 2017
Romosozumab for Osteoporosis • N = 436 (218 each arm) • Romo: ↑ BMD 2. 6% / Teri: ↓BMD 0, 6% – ≠ 3. 2% (p<0. 001) • Romo – Increased integral/cortical / trabecular bone at hip with (quantitative CT) – Increased hip strength (finite element analysis) – ↑bone-formation BM and ↓ bone-resorption BM • Adverse events balanced between groups – More nasopharyngitis and arthralgia in Romo and more hypocalcemia and serious AE in Teri Langdahl BL et al, Lancet 2017
Romosozumab for Osteoporosis • Limitations – Open-label study (Teri administered by pen) – Not powered to detect ≠ in fracture incidence – Benefit of Teri beyond 12 mos ? (approved up to 24) • Strengths – Complementary imaging modalities – Adjustment for baseline variables • Conclusions – Superiority of Romo on BMD gains thought to be due to dual effect – Unique benefit to patients transitioning from bisphonate Tx (vs decline in sequential exposure to bisphonates and teriparatide) Langdahl BL et al, Lancet 2017
Levothyroxine for Subclinical Hypothyrodism N Engl J Med 2017; 376: 2534 -2544
Levothyroxine for Subclinical Hypothyroidism • The use of levothyroxine in subclinical hypothyroidism is controversial • Objective: benefit of levothyroxine in this condition • Inclusion: ≥ 65 / ↑ TSH (max=20) and N T 4 • DBRCT / N=368 received levothyroxine (25 -50μg) with adjusted titration according to TSH levels / N= 369 Pbo / 1 yr + extended FU • Primary Outcomes – Hypothyroid Symptoms score (0 -100) – Tiredness score (0 -100) – Minimal clinical response on each scale = 9 pts • Secondary Outcomes – QOL measures, handgrip strength, executive function (processing speed), ADL, IADL, BP, cvs events, weight, BMI, waist circumference. Stott DJ et al, N Engl J Med 2017
Levothyroxine for Subclinical Hypothyroidism Mean age 74. 4 / 53. 7% ♀ Mean TSH at baseline: 6. 40 Mean TSH at 1 yr : Pbo= 5. 48 / LT 4 = 3. 63 (P<0. 001) Median dose of LT 4 of 50 μg Mean FU: 17 -18 months No difference on mean changes on 1 ry or 2 ry outcomes at 1 yr (except slight deterioration on QOL in LT 4 group) • Minor improvement on tiredness scale and one scale of QOL on extended FU • No excess SAE of interest • • • Stott DJ et al, N Engl J Med 2017
Levothyroxine for Subclinical Hypothyroidism • Strengths – Adequate power – Validated measures including gip strength and processing speed • Limitations – – Few individuals with TSH levels ≥ 10 Symptom levels at entry low Antiobody levels not measured No adequate power for CVS events and mortality • Conclusions – Tx with LT 4 in elders with subclinical hypothyroidism did not provide symptomatic benefit – In longitudinal studies, TSH reverts to normal in more than half of individuals (3/5 during screening for this study). Stott DJ et al, N Engl J Med 2017
New Herpes Zoster Vaccine
New Herpes Zoster Vaccine • Following primary infection, VZV persists in a latent form in sensory ganglia; • When VZV-specific cell-mediated immunity falls below a critical threshold, VZV reactivates, causing shingles and, occasionally, postherpetic neuralgia (PHN) • Canada: 130, 000 cases of shingles / yr • Since 2005, live attenuated vaccine available (Zostavax)
New Herpes Zoster Vaccine • Live attenuated vaccine (Zostavax) – C-I in immunocompromised individuals – ↓ efficacy overtime (≥ 8 yrs) – ↓ efficacy in ≥ 80 – Must be frozen during transportation /storage • New vaccine (Shingrix) – Approved in Canada and US – Oct 2017 – Recombinant zoster glycoprotein (g. E) + potent adjuvant (AS 01 B) – Clinical trials published in 2015 and 2016 show better and more sustained response than previous vaccine
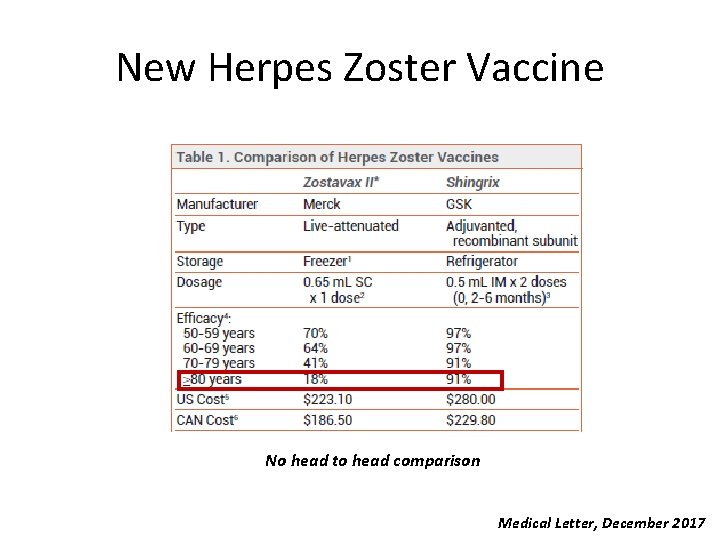
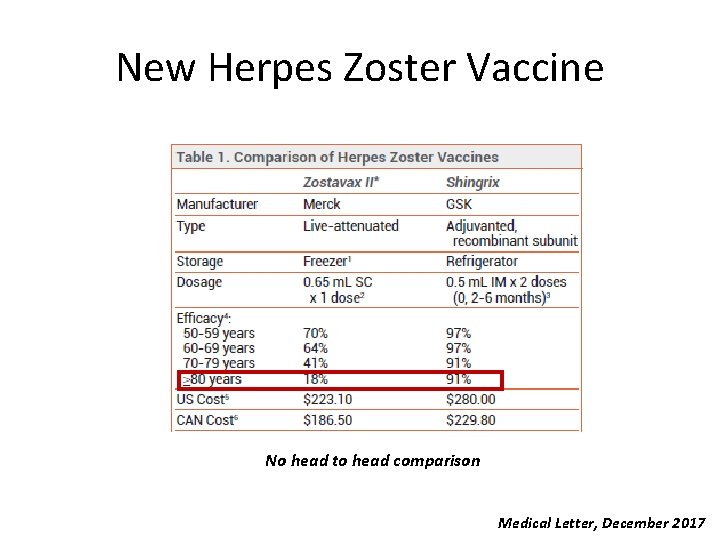
New Herpes Zoster Vaccine No head to head comparison Medical Letter, December 2017
New Herpes Zoster Vaccine • Pros – – – • Cons – – • • • Safe in immunocompromised individuals (studies ongoing) Better and more sustained response in older individuals Effective in those previously vaccinated Easier to store and transport Cost-effective Duration of protection ? Booster dose at 2 months Painful local reaction Uptake ? ? (already a problem with Zostavax: 30% in eligible individuals) In the US, the Advisory Committee on Immunization Practices (ACIP) recommends Shingrix over Zostavax in ≥ 50, even those previously vaccinated. In Canada, the National Advisory Committee on Immunization (NACI) has not published new recommendations yet. Conclusion (Medical Letter): The adjuvanted, recombinant VZV vaccine appears to be considerably more effective than the live-attenuated VZV vaccine
Probiotics for Prevention of Clostridium Difficile
Probiotics for Prevention of C. Difficile • C. difficile infx common and more severe in the elderly • Previous reviews on the efficacy of probiotics in preventing c. diff provide conflicting results • Current guidelines do not recommend their use • Systematic review and metanalysis of probiotic use in hospitalized patients started on Ab to prevent C. difficile Shen NT et al, Gastroenterology 2017
Probiotics for Prevention of C. Difficile • Inclusion: RCTs (no restriction for language, publication)/ inpatient / adult population • Intervention: probiotics in prevention of CDI • Outcome: incidence of CDI • Each study evaluated by 2 -3 reviewers for inclusion criteria and quality (GRADE) • 19 RCT / N = 6261 (3277 probiotic/2984 pbo) • Mean age 68 -69 Shen NT et al, Gastroenterology 2017
Probiotics for Prevention of C. Difficile • Incidence of C. difficile infection was lower in probiotic users 1, 6% vs. 3, 9%; pooled RR: 0, 42) – NNT: 23 -144 • The protective effect of probiotics was lower if started > 2 days after initiation of Ab vs within 2 days (RR: 0, 70 vs 0, 32) • Meta-regression showed an 18% decline in benefit for every day of delay in starting prob. • No increase in side effects • There were nonsignificant trends toward better protection – Lactobacillus + Streptococcus + Bifidobacterium Shen NT et al, Gastroenterology 2017
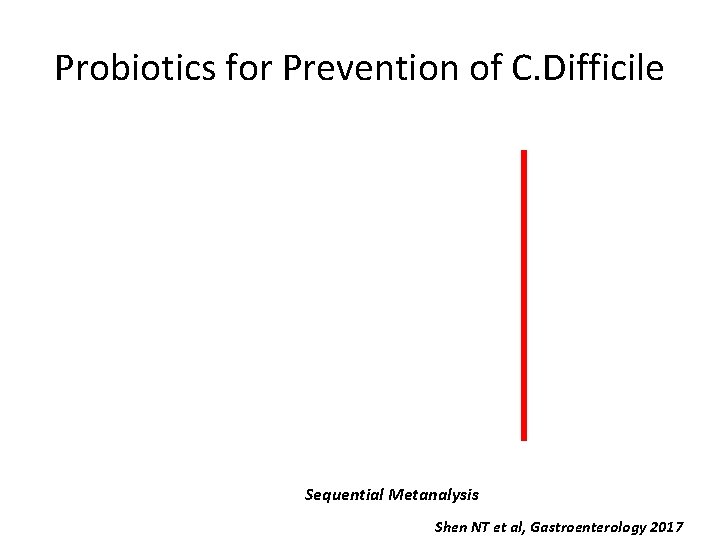
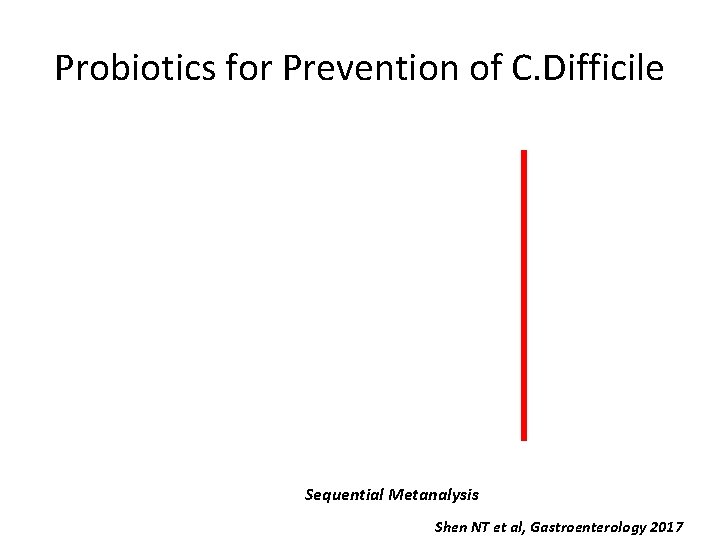
Probiotics for Prevention of C. Difficile Sequential Metanalysis Shen NT et al, Gastroenterology 2017
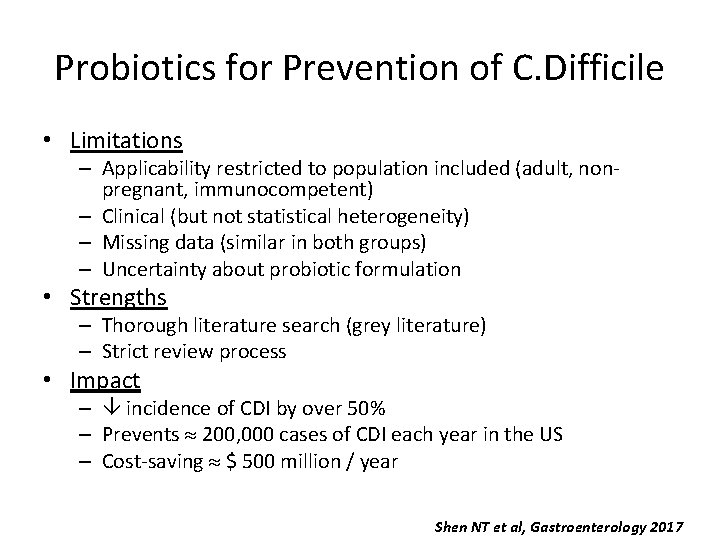
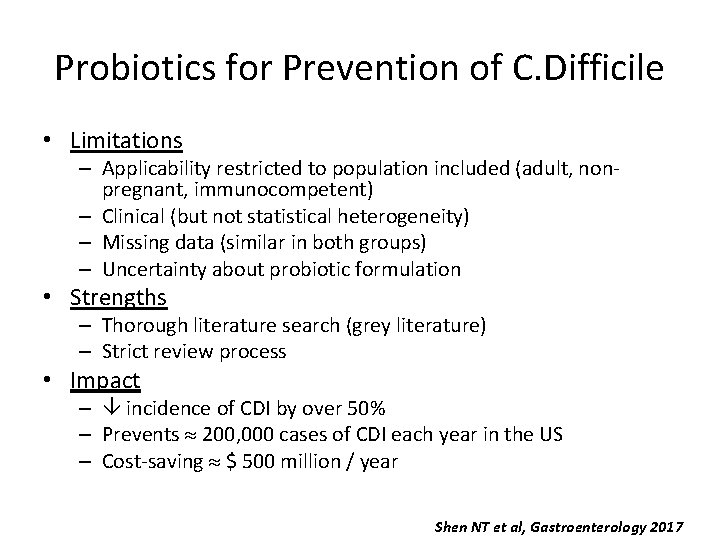
Probiotics for Prevention of C. Difficile • Limitations – Applicability restricted to population included (adult, nonpregnant, immunocompetent) – Clinical (but not statistical heterogeneity) – Missing data (similar in both groups) – Uncertainty about probiotic formulation • Strengths – Thorough literature search (grey literature) – Strict review process • Impact – incidence of CDI by over 50% – Prevents 200, 000 cases of CDI each year in the US – Cost-saving $ 500 million / year Shen NT et al, Gastroenterology 2017
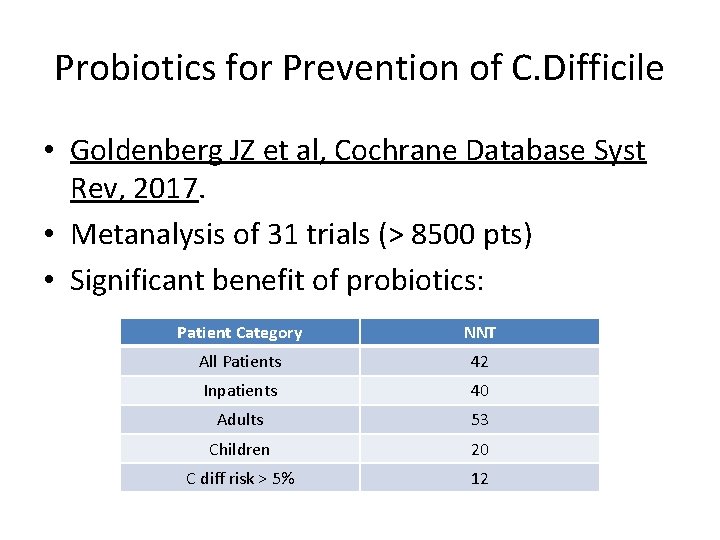
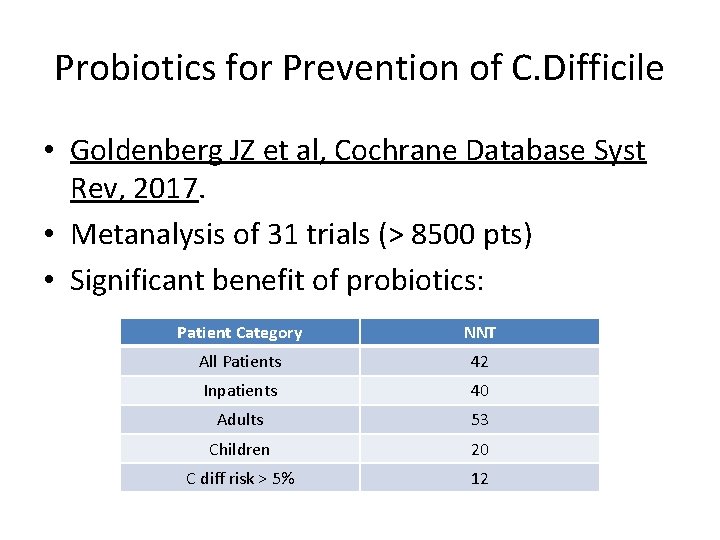
Probiotics for Prevention of C. Difficile • Goldenberg JZ et al, Cochrane Database Syst Rev, 2017. • Metanalysis of 31 trials (> 8500 pts) • Significant benefit of probiotics: Patient Category NNT All Patients 42 Inpatients 40 Adults 53 Children 20 C diff risk > 5% 12
Hypertension Guidelines Hypertension 2017
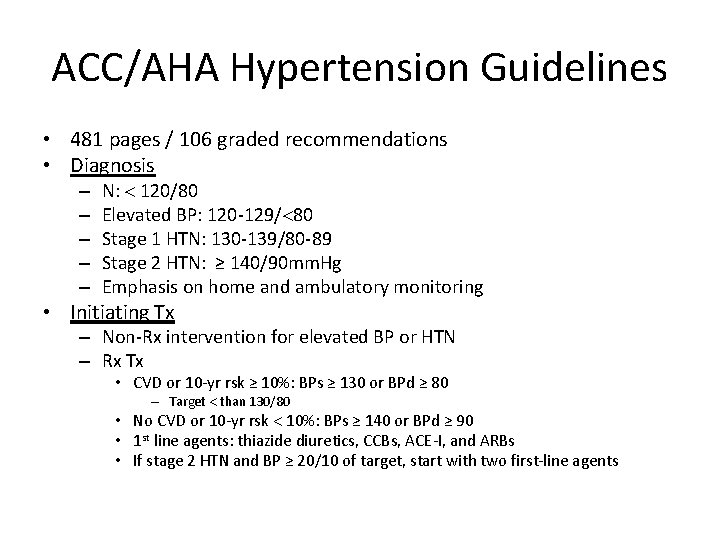
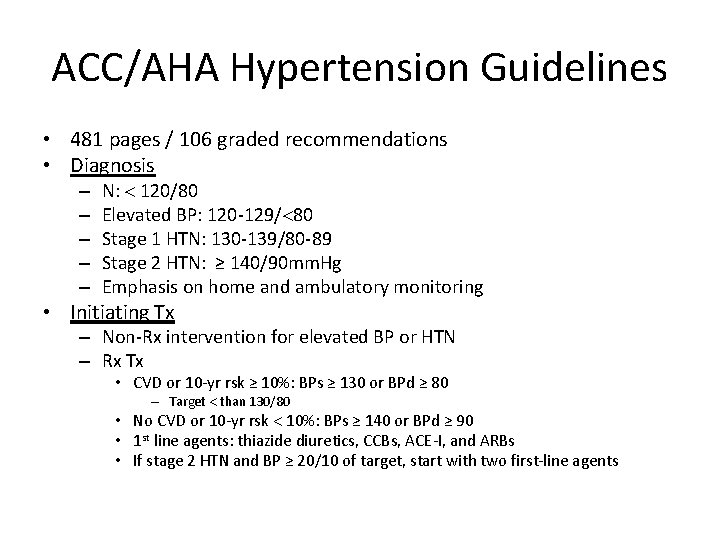
ACC/AHA Hypertension Guidelines • 481 pages / 106 graded recommendations • Diagnosis – – – N: 120/80 Elevated BP: 120 -129/ 80 Stage 1 HTN: 130 -139/80 -89 Stage 2 HTN: ≥ 140/90 mm. Hg Emphasis on home and ambulatory monitoring • Initiating Tx – Non-Rx intervention for elevated BP or HTN – Rx Tx • CVD or 10 -yr rsk ≥ 10%: BPs ≥ 130 or BPd ≥ 80 – Target than 130/80 • No CVD or 10 -yr rsk 10%: BPs ≥ 140 or BPd ≥ 90 • 1 st line agents: thiazide diuretics, CCBs, ACE-I, and ARBs • If stage 2 HTN and BP ≥ 20/10 of target, start with two first-line agents
ACC/AHA Hypertension Guidelines Recommendations in Older Persons: 1. 5 pages /481 ! • Noninstitutionalized ambulatory community dwelling adults: same. • Comorbidity / Limited life expectancy: clinical judgment, patient preference, and a team-based approach to assess risk/benefit for intensity of BP lowering and choice of Rx • Those with prevalent and frequent falls /advanced cognitive impairment/multiple comorbidities may be at risk of adverse outcomes with intensive BP lowering – not represented in RCT • Treatment is challenging because of a high degree of heterogeneity in comorbidity /poly-pharmacy/ frailty/ cognitive impairment /life expectancy • BUT, HYVET and SPRINT included frail but still living independently in the community , and both were stopped early for benefit.
• Pharmacologic Treatment – SBP ≥ 150 (GRADE: strong / high quality evidence) – SBP ≥ 140 if previous TIA/stroke (GRADE: weak / moderate-quality evidence) – SBP ≥ 140 in some at high cardiovascular risk based on individualized assessment (GRADE: weak / low-quality evidence)
• Brings much-needed nuance to the ACC-AHA guidelines • Not appropriate for application in general population of elderly • Clinical trials do not provide consistent benefit on mortality (even in review of the ACC guidelines) – SPRINT weighs +++ • When applied to general population, benefits overestimated and harms underestimated – Run-in periods to randomize most compliant individuals – Time and labor-intensive measurements of BP (feasible ? ) • Risk of overtreating individuals when BP measured in less strict conditions • No evidence from RCTs for benefit of Tx of diastolic BP ≤ 80 • Guidelines inadequately recognize/assess potential harm – No increased risk of cognitive impairment, falls / fractures – BUT, electrolyte abnormalities, hypotension, syncope, AKI Wilt TJ et al, Ann Int Med 2018
Hypertension Guidelines • Hypertension linked to CVS morbidity/mortality and contributes to disability in the elderly • Benefits of treatment clearly demonstrated • Target levels require individualisation according to comorbidity, poly. Rx, frailty, falls, cognitive impairment, life expectancy • Risks of overtreatment underestimated in ACC/AHA guidelines • Careful of basing guidelines almost exclusively on results of single trial • ACP/ACFP more appropriate for frail elderly