THYROID DISORDERS Dr mirzarahimi HYPOTHYROIDISMEPIDEMIOLOGY Neonatal screening reveals


- Slides: 39
THYROID DISORDERS Dr. mirzarahimi
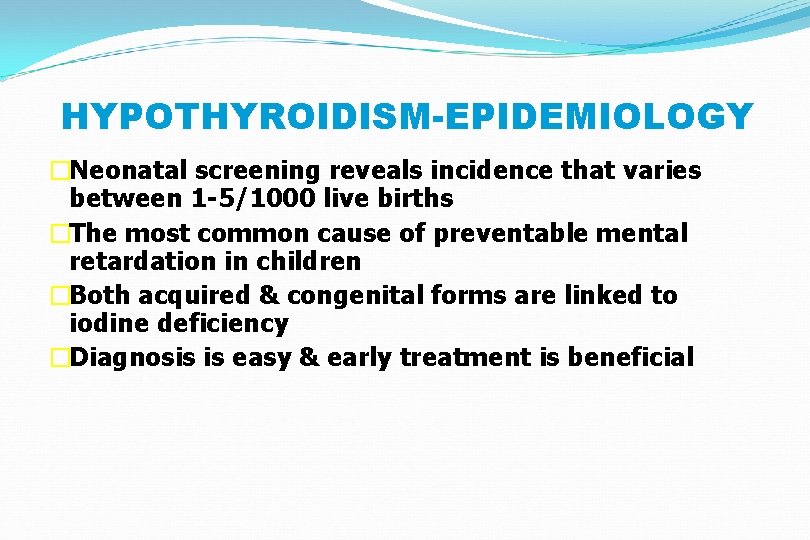
HYPOTHYROIDISM-EPIDEMIOLOGY �Neonatal screening reveals incidence that varies between 1 -5/1000 live births �The most common cause of preventable mental retardation in children �Both acquired & congenital forms are linked to iodine deficiency �Diagnosis is easy & early treatment is beneficial
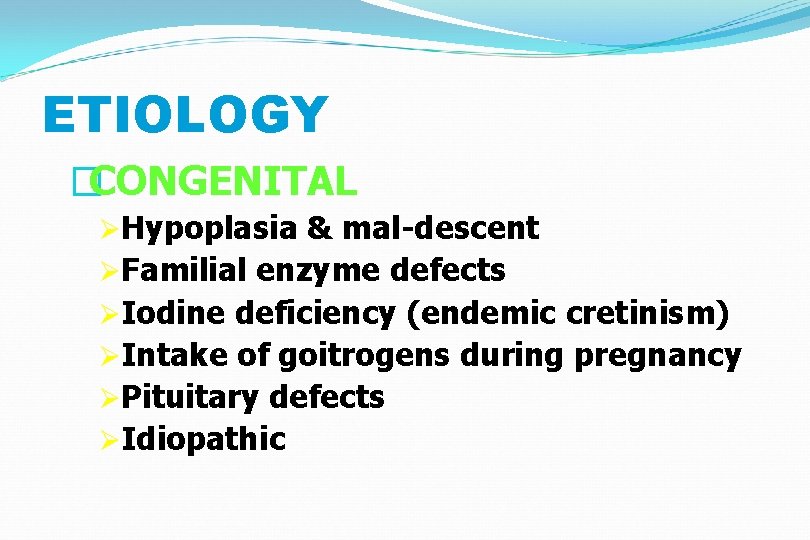
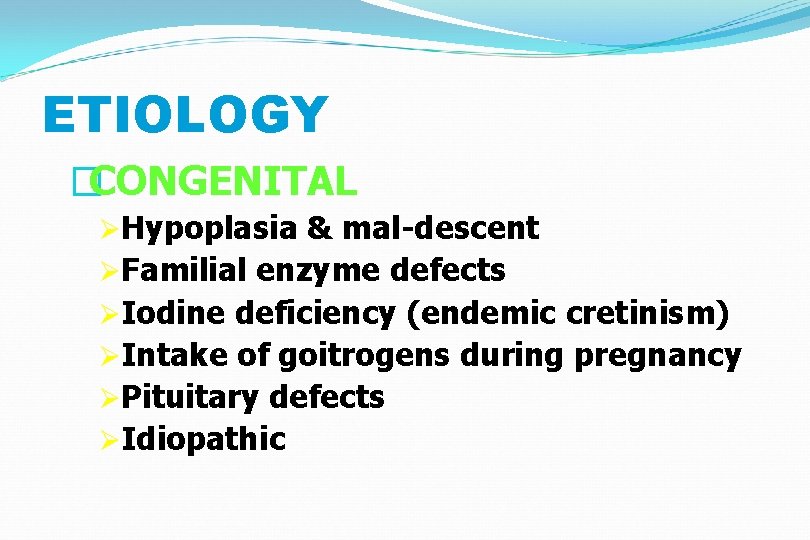
ETIOLOGY �CONGENITAL ØHypoplasia & mal-descent ØFamilial enzyme defects ØIodine deficiency (endemic cretinism) ØIntake of goitrogens during pregnancy ØPituitary defects ØIdiopathic
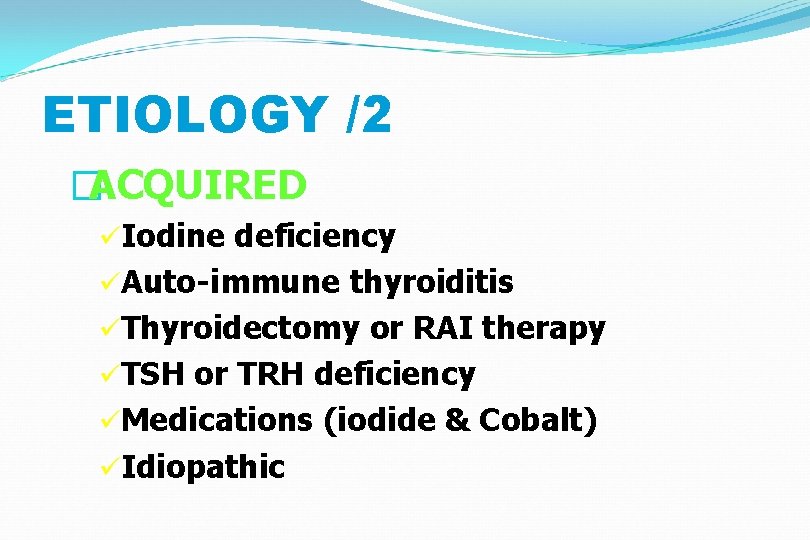
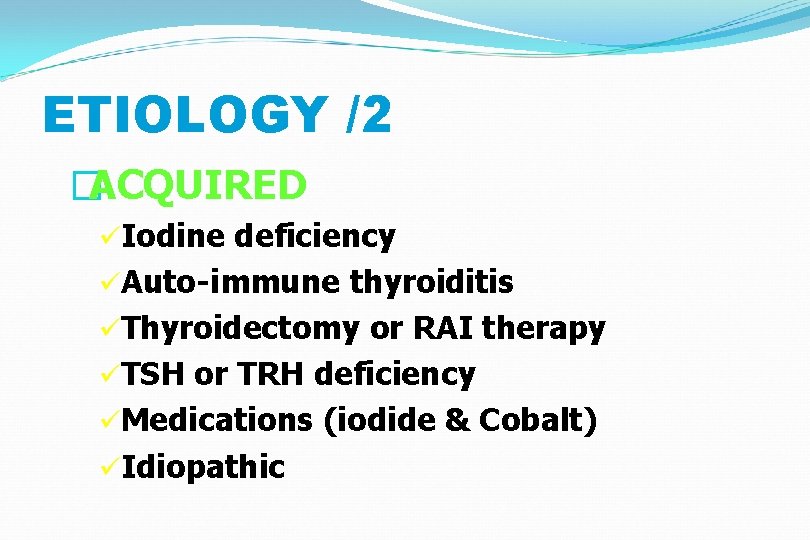
ETIOLOGY /2 �ACQUIRED üIodine deficiency üAuto-immune thyroiditis üThyroidectomy or RAI therapy üTSH or TRH deficiency üMedications (iodide & Cobalt) üIdiopathic
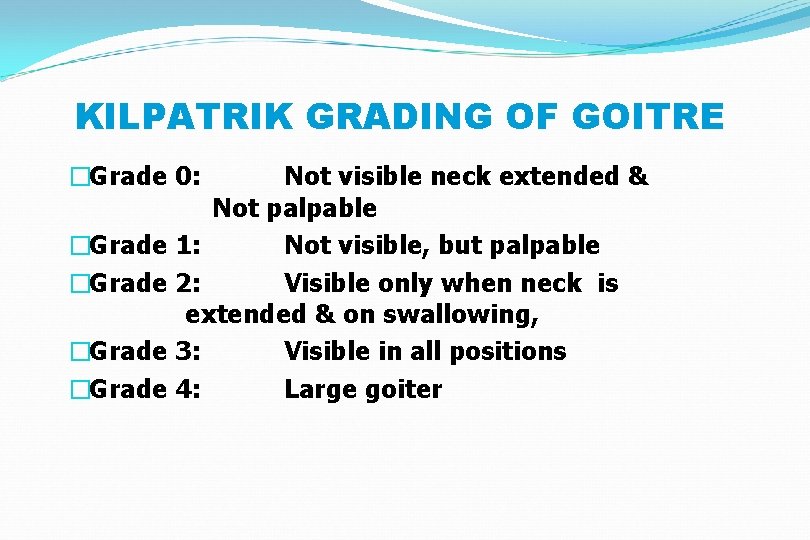
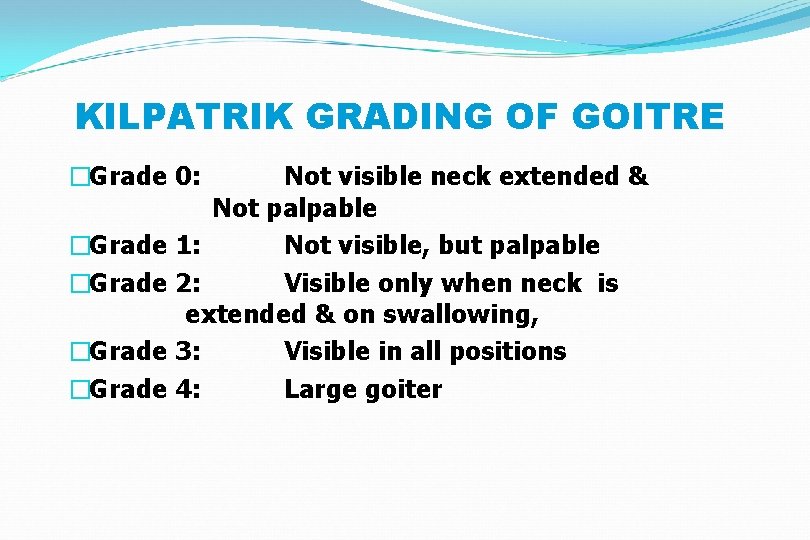
KILPATRIK GRADING OF GOITRE �Grade 0: Not visible neck extended & Not palpable �Grade 1: Not visible, but palpable �Grade 2: Visible only when neck is extended & on swallowing, �Grade 3: Visible in all positions �Grade 4: Large goiter
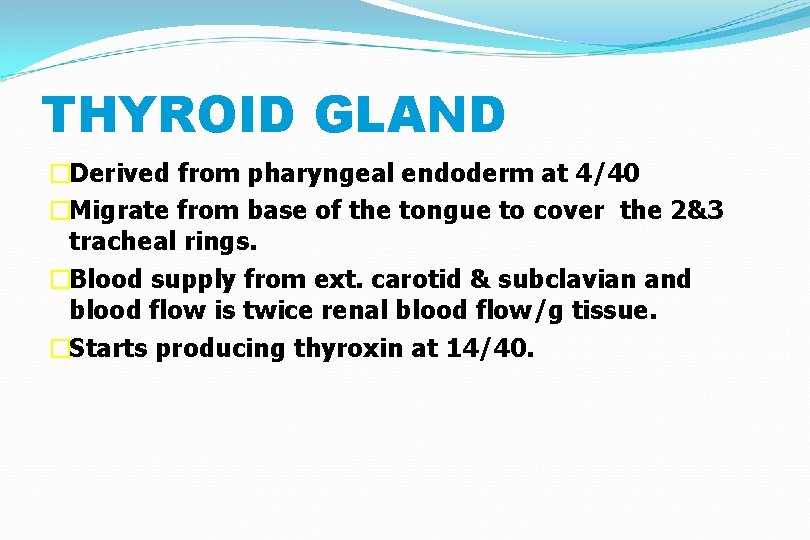
THYROID GLAND �Derived from pharyngeal endoderm at 4/40 �Migrate from base of the tongue to cover the 2&3 tracheal rings. �Blood supply from ext. carotid & subclavian and blood flow is twice renal blood flow/g tissue. �Starts producing thyroxin at 14/40.
OVERVIEW (2) �Maternal & fetal glands are independent with little transplacental transfer of T 4. �TSH doesn’t cross the placenta. �Fetal brain converts T 4 to T 3 efficiently. �Average intake of iodine is 500 mg/day. 70% of this is trapped by the gland against a concentration gradient up to 600: 1
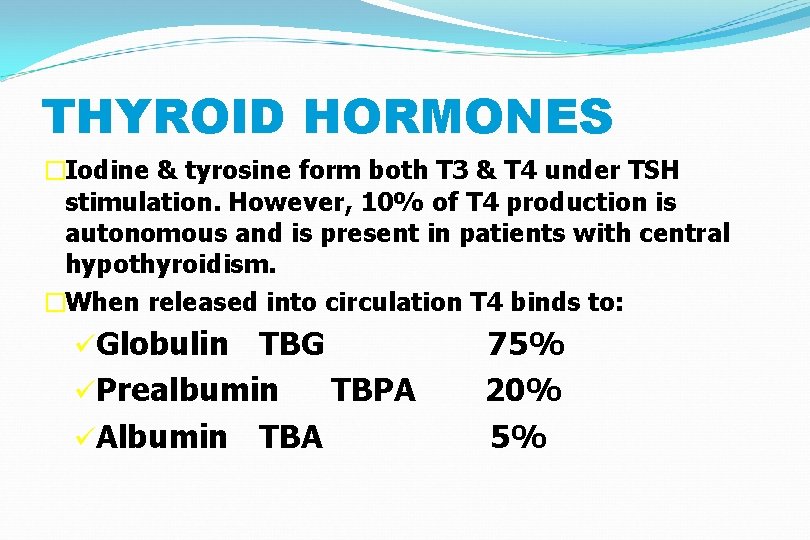
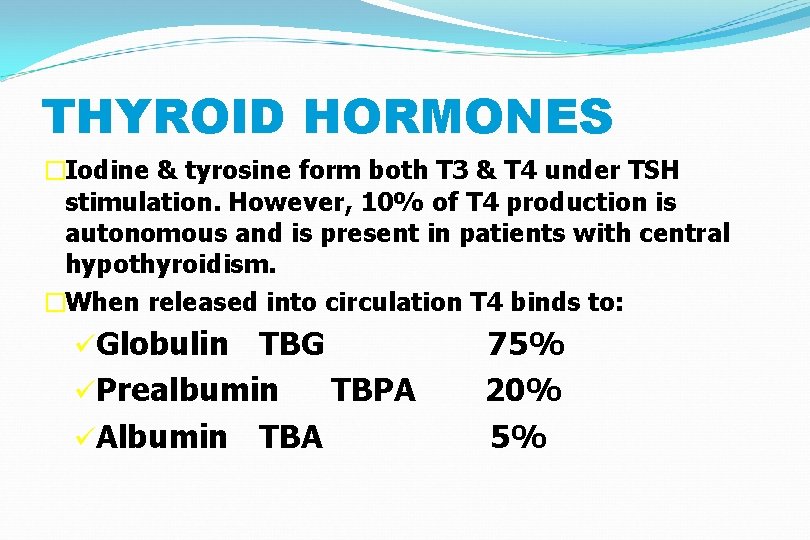
THYROID HORMONES �Iodine & tyrosine form both T 3 & T 4 under TSH stimulation. However, 10% of T 4 production is autonomous and is present in patients with central hypothyroidism. �When released into circulation T 4 binds to: üGlobulin TBG üPrealbumin TBPA üAlbumin TBA 75% 20% 5%
THYROID HORMONES (2) �Less than 1% of T 4 & T 3 is free in plasma. �T 4 is deiodinated in the tissues to either T 3 (active) or reverse T 3 (inactive). �At birth T 4 level approximates maternal level but increases rapidly during the first week of life. �High TSH in the first 5 days of life can give false positive neonatal screening
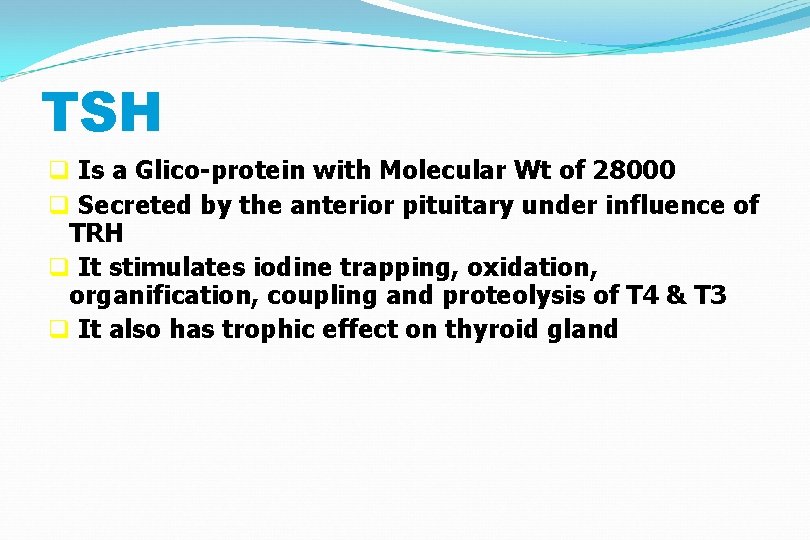
TSH q Is a Glico-protein with Molecular Wt of 28000 q Secreted by the anterior pituitary under influence of TRH q It stimulates iodine trapping, oxidation, organification, coupling and proteolysis of T 4 & T 3 q It also has trophic effect on thyroid gland
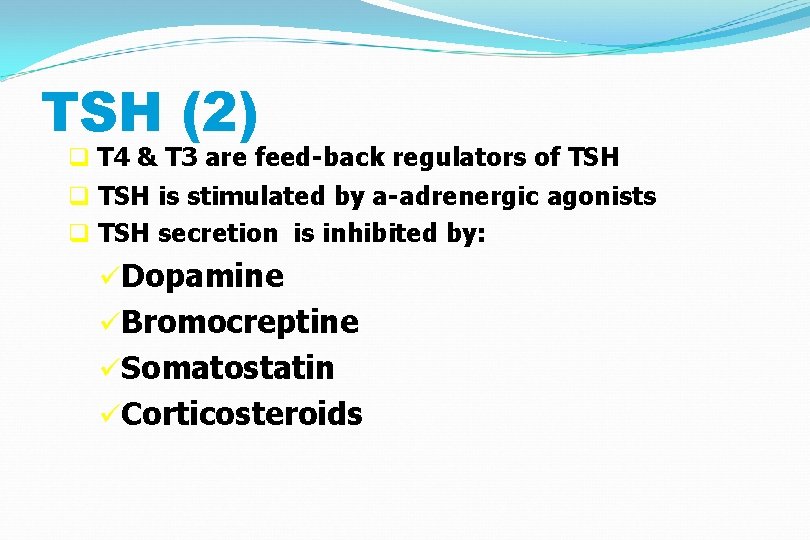
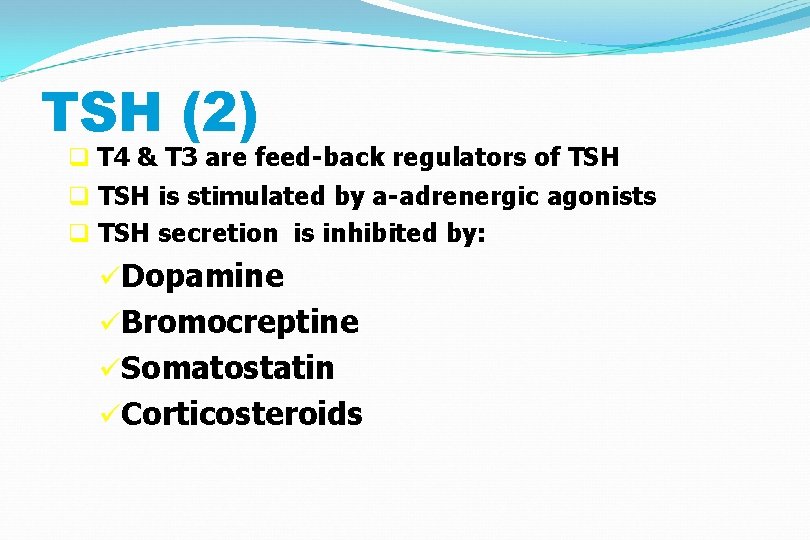
TSH (2) q T 4 & T 3 are feed-back regulators of TSH q TSH is stimulated by a-adrenergic agonists q TSH secretion is inhibited by: üDopamine üBromocreptine üSomatostatin üCorticosteroids
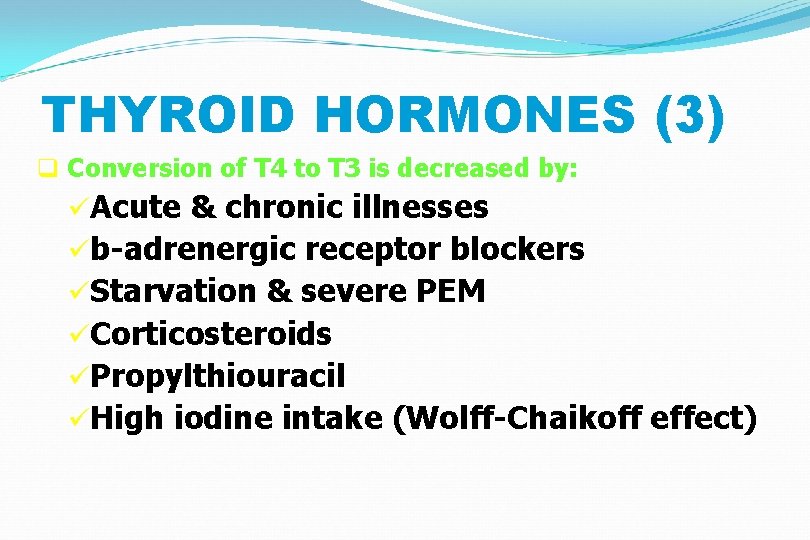
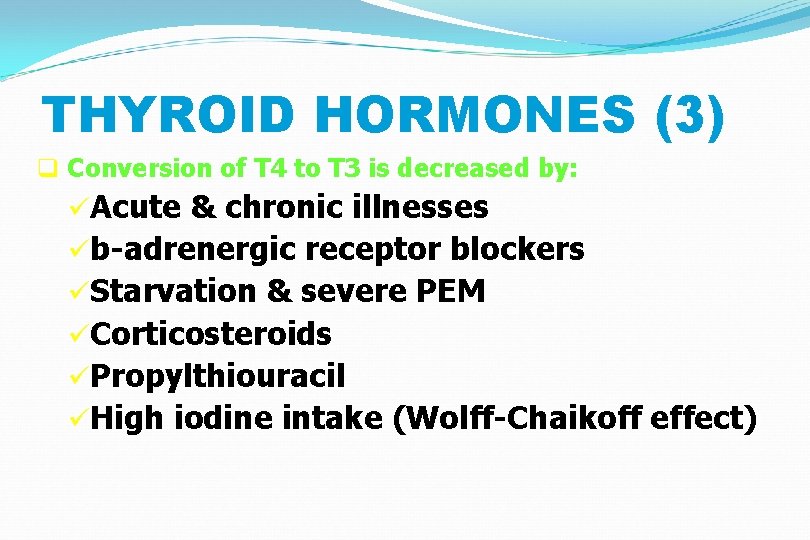
THYROID HORMONES (3) q Conversion of T 4 to T 3 is decreased by: üAcute & chronic illnesses üb-adrenergic receptor blockers üStarvation & severe PEM üCorticosteroids üPropylthiouracil üHigh iodine intake (Wolff-Chaikoff effect)
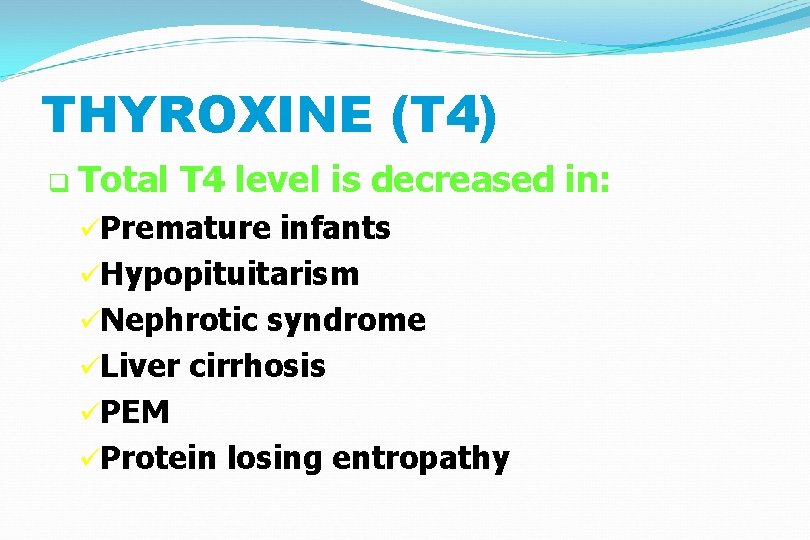
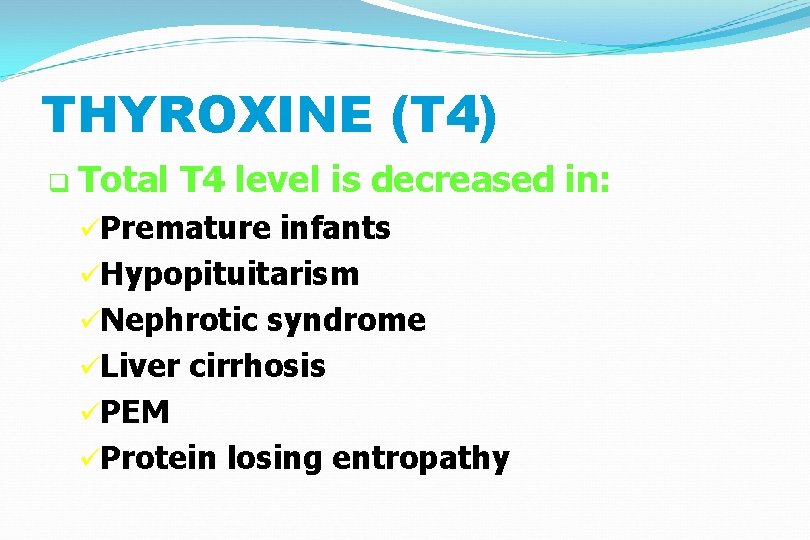
THYROXINE (T 4) q Total T 4 level is decreased in: üPremature infants üHypopituitarism üNephrotic syndrome üLiver cirrhosis üPEM üProtein losing entropathy
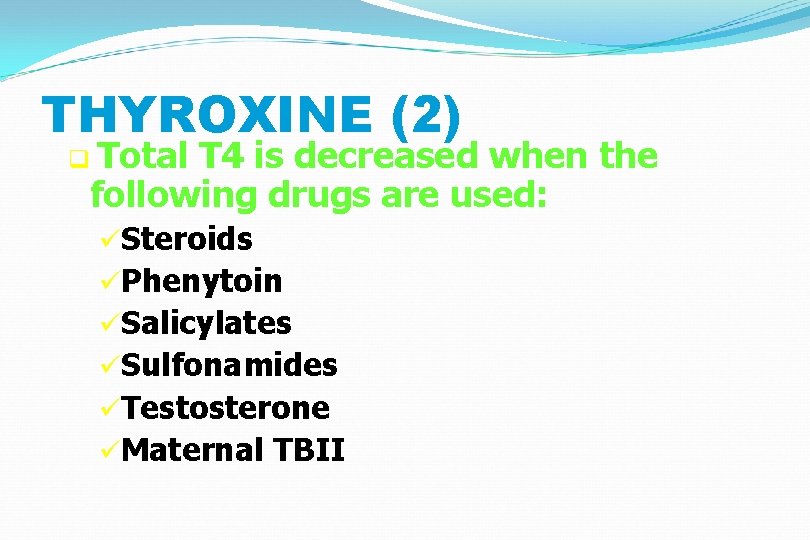
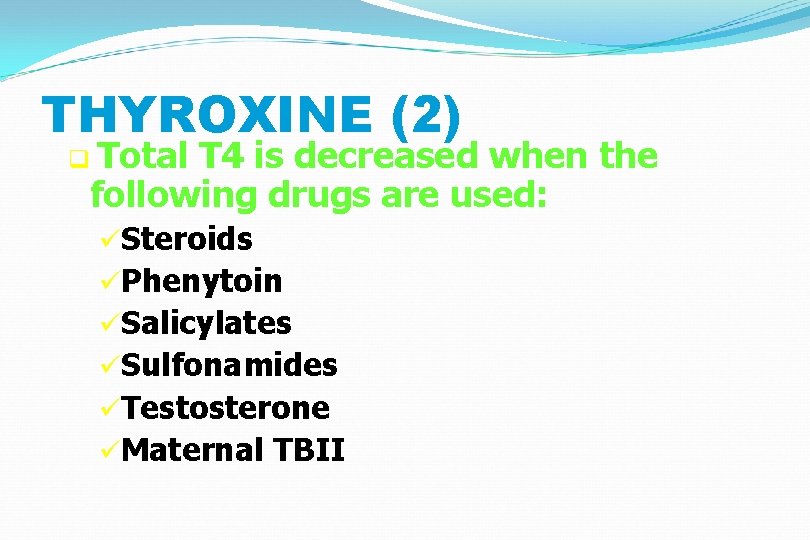
THYROXINE (2) q Total T 4 is decreased when the following drugs are used: üSteroids üPhenytoin üSalicylates üSulfonamides üTestosterone üMaternal TBII
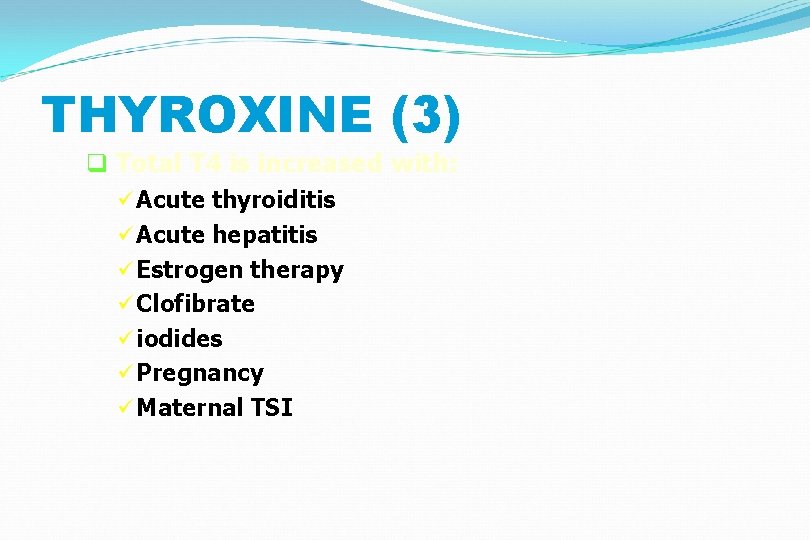
THYROXINE (3) q Total T 4 is increased with: ü Acute thyroiditis ü Acute hepatitis ü Estrogen therapy ü Clofibrate ü iodides ü Pregnancy ü Maternal TSI
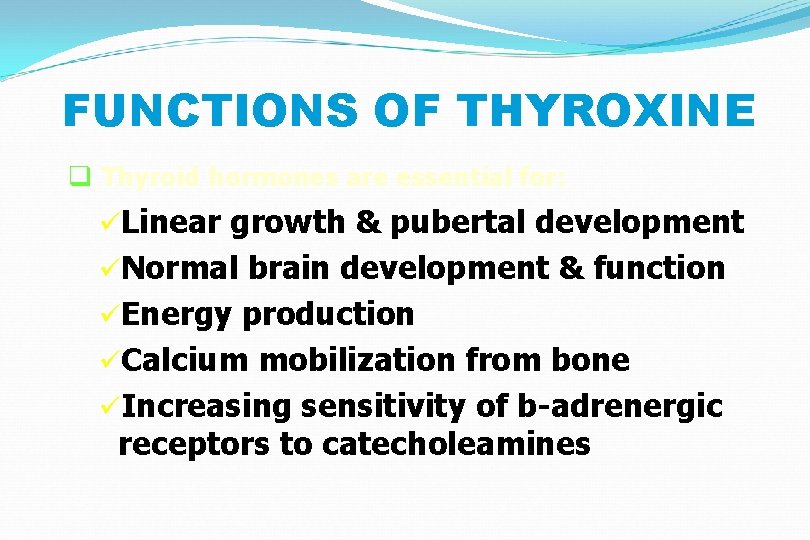
FUNCTIONS OF THYROXINE q Thyroid hormones are essential for: üLinear growth & pubertal development üNormal brain development & function üEnergy production üCalcium mobilization from bone üIncreasing sensitivity of b-adrenergic receptors to catecholeamines
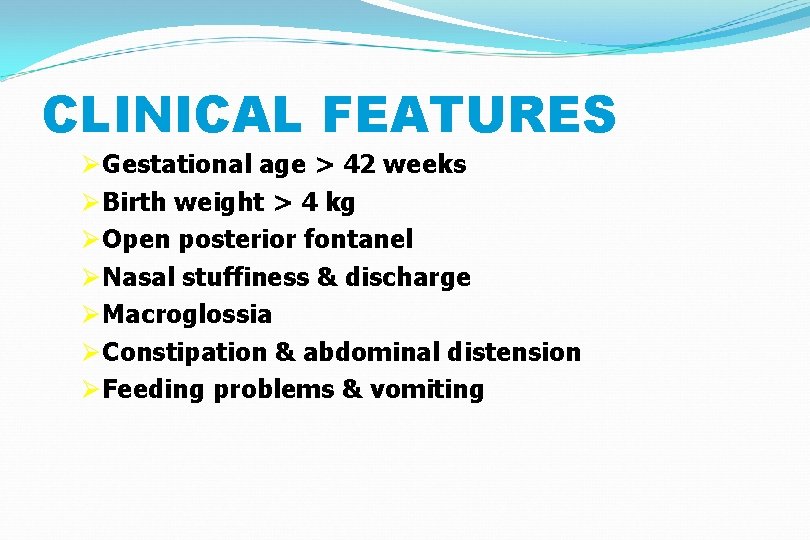
CLINICAL FEATURES Ø Gestational age > 42 weeks Ø Birth weight > 4 kg Ø Open posterior fontanel Ø Nasal stuffiness & discharge Ø Macroglossia Ø Constipation & abdominal distension Ø Feeding problems & vomiting
CLINICAL FEATURES (2) �Non pitting edema of lower limbs & feet �Coarse features �Umbilical hernia �Hoarseness of voice �Anemia �Decreased physical activity �Prolonged (>2/52) neonatal jaundice
CLINICAL FEATURES (3) �Dry, pale & mottled skin �Low hair line & dry, scanty hair �Hypothermia & peripheral cyanosis �Hypercarotenemia �Growth failure �Retarded bone age �Stumpy fingers & broad hands
CLINICAL FEATURES (5) �Skeletal abnormalities: üInfantile proportions üHip & knee flexion üExaggerated lumbar lordosis üDelayed teeth eruption üUnder developed mandible üDelayed closure of anterior fontanel
OCCASIONAL FEATURES �Overt obesity �Myopathy & rheumatic pains �Speech disorder �Impaired night vision �Sleep apnea (central & obstructive) �Anasarca �Achlorhydria & low intrinsic factor
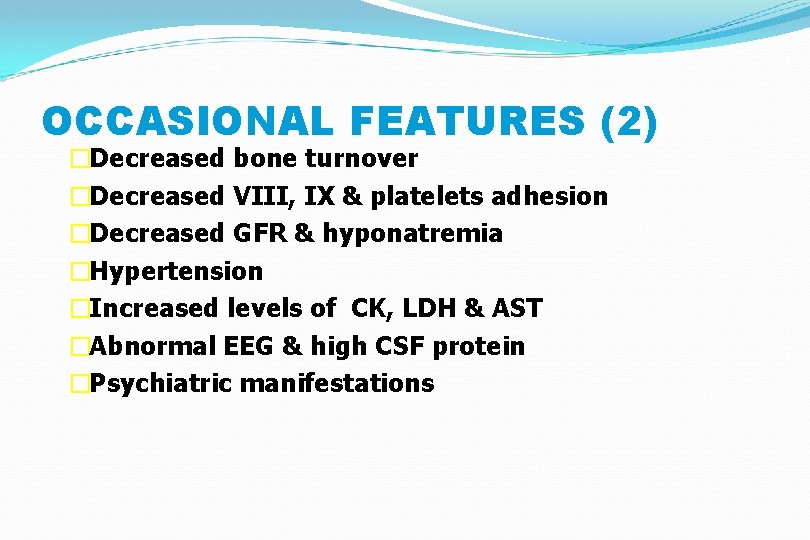
OCCASIONAL FEATURES (2) �Decreased bone turnover �Decreased VIII, IX & platelets adhesion �Decreased GFR & hyponatremia �Hypertension �Increased levels of CK, LDH & AST �Abnormal EEG & high CSF protein �Psychiatric manifestations
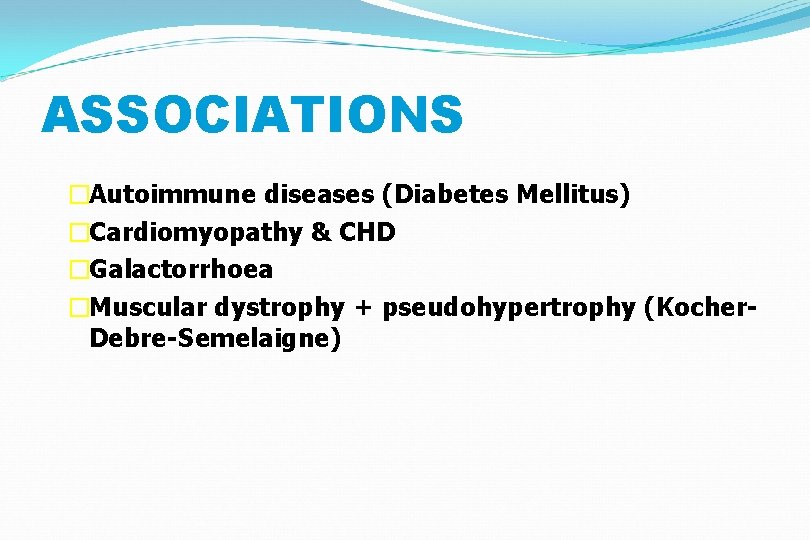
ASSOCIATIONS �Autoimmune diseases (Diabetes Mellitus) �Cardiomyopathy & CHD �Galactorrhoea �Muscular dystrophy + pseudohypertrophy (Kocher. Debre-Semelaigne)
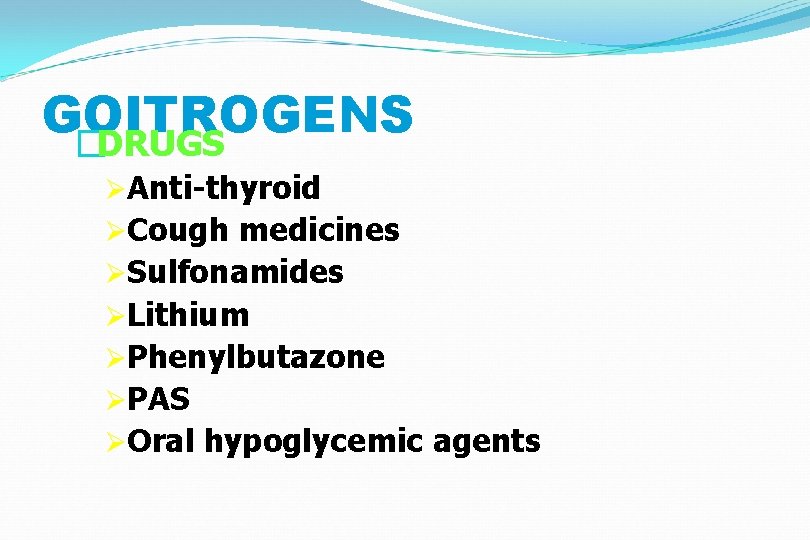
GOITROGENS �DRUGS ØAnti-thyroid ØCough medicines ØSulfonamides ØLithium ØPhenylbutazone ØPAS ØOral hypoglycemic agents

GOITROGENS q FOOD üSoybeans üMillet üCassava üCabbage
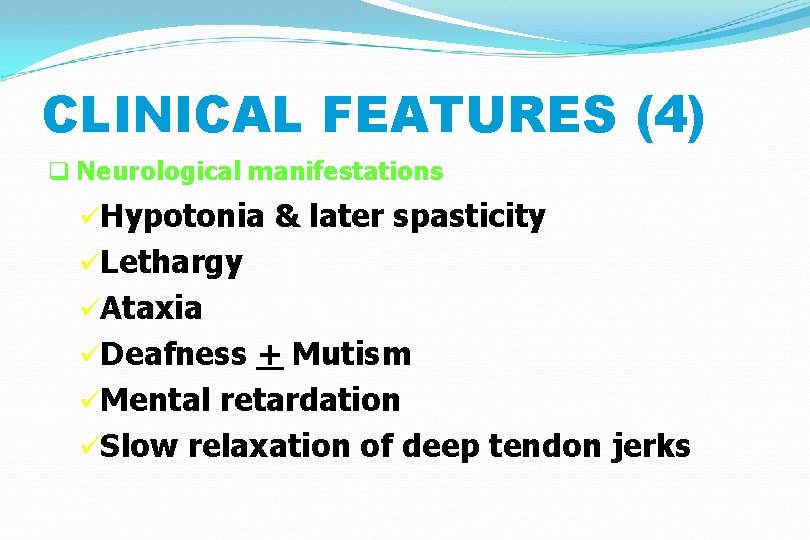
CLINICAL FEATURES (4) q Neurological manifestations üHypotonia & later spasticity üLethargy üAtaxia üDeafness + Mutism üMental retardation üSlow relaxation of deep tendon jerks
CONGENITAL HYPOTHYRODISM �Primary thyroid defect: usually associated with goiter. �Secondary to hypothalamic or pituitary lesions: not associated with goiter. � 2 distinct types of presentation: ü Neurological with MR-deafness & ataxia ü Myxodematous with dwarfism & dysmorphism
DIAGNOSIS �Early detection by neonatal screening �High index of suspicion in all infants with increased risk �Overt clinical presentation �Confirm diagnosis by appropriate lab and radiological tests

LABROTARY FINDINGS �Low (T 4, RI uptake & T 3 resin uptake) �High TSH in primary hypothyroidism �High serum cholesterol & carotene levels �Anaemia (normo, micro or macrocytic) �High urinary creatinine/hydroxyproline ratio �CXR: cardiomegaly �ECG: low voltage & bradycardia
IMAGING TESTS q X-ray films can show: ü Delayed bone age or epiphyseal dysgenesis ü Anterior peaking of vertebrae ü Coxavara & coxa plana q Thyroid radio-isotope scan q Thyroid ultrasound q CT or MRI
TREATMENT (2) �L-Thyroxin is the drug of choice. Start with small dose to avoid cardiac strain. �Dose is 10 mg/kg/day in infancy. In older children start with 25 mg/day and increase by 25 mg every 2 weeks till required dose. �Monitor clinical progress & hormones level
TREATMENT q Life-long replacement therapy q 5 types of preparations are available: ü L-thyroxin (T 4) ü Triiodothyronine (T 3) ü Synthetic mixture T 4/T 3 in 4: 1 ratio ü Desiccated thyroid (38 mg T 4 & 9 mg T 3/grain) ü Thyroglobulin (36 mg T 4 & 12 mg T 3/grain)
THYROID FUNCTION TESTS 1. Peripheral effects: ü BMR ü Deep Tendon Reflex ü Cardiovascular indices (pulse, BP, LV function tests) ü Serum parameters (high cholesterol, CK, AST, LDH & carcino-embryonic antigen)
THYROID FUNCTION TESTS (2) 2. Thyroid gland economy: Ø Radio iodine uptake Ø Perchlorate discharge test (+ve in Pendred syndrome & autoimmune thyroiditis) Ø TSH level Ø TRH stimulation tests Ø Thyroid scan
THYROID FUNCTION TESTS (3) 3. Tests for thyroid hormone: Ø Total & free T 4 & T 3 Ø Reverse T 3 level Ø T 3 Resin Uptake Ø T 3 RU x total T 4= Thyroid Hormone Binding Index (formerly Free Thyroxin Index)
THYROID FUNCTION TESTS (4) q Special Tests: Ø Thyroglobulin level Ø Thyroid Stimulating Immunoglobulin Ø Thyroid antibodies Ø Thyroid radio-isotope scan Ø Thyroid ultrasound Ø CT & MRI Ø Thyroid biopsy
PROGNOSIS q. Depends on: ØEarly diagnosis ØProper diabetes education ØStrict diabetic control ØCareful monitoring ØCompliance
MYXOEDMATOUS COMA q Impaired sensorium, hypoventilation bradycardia, hypotension & hypothermia q Precipitated by: üInfections üTrauma (including surgery) üExposure to cold üCardio-vascular problems üDrugs
PROGNOSIS q Is good for linear growth & physical features even if treatment is delayed, but for mental and intellectual development early treatment is crucial. q Sometimes early treatment may fail to prevent mental subnormality due to severe intra-uterine deficiency of thyroid hormones
 Act 4 hamlet summary
Act 4 hamlet summary One way an author uses direct characterization
One way an author uses direct characterization Whats a controlling idea
Whats a controlling idea What is central idea
What is central idea Characterization is the way an author
Characterization is the way an author The soldier poem meaning
The soldier poem meaning Which narration reveals a character with a shy personality?
Which narration reveals a character with a shy personality? Art reveals society
Art reveals society The theme is the central idea or truth in the story
The theme is the central idea or truth in the story Reveals that his supporters will be made earls
Reveals that his supporters will be made earls Mark twain reveals stage fright
Mark twain reveals stage fright A sustainability report reveals a firm's
A sustainability report reveals a firm's Nipedipina
Nipedipina Emv score
Emv score Hipoglicemia neonatal
Hipoglicemia neonatal Introduction of nursing process
Introduction of nursing process L
L Cuarro
Cuarro Infant mortality rate equation
Infant mortality rate equation Vasculopatia lenticulo estriada
Vasculopatia lenticulo estriada Circulação neonatal
Circulação neonatal Nelson nec
Nelson nec Circulação fetal
Circulação fetal Portal hypertension definition
Portal hypertension definition Neonatal resuscitation definition
Neonatal resuscitation definition Organization of neonatal unit
Organization of neonatal unit Neonatal mortality rate formula
Neonatal mortality rate formula Circulação fetal
Circulação fetal Neonatal energy triangle
Neonatal energy triangle Parâmetros iniciais ventilação mecânica neonatal
Parâmetros iniciais ventilação mecânica neonatal Definición de ictericia
Definición de ictericia Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Nanda hipertension
Nanda hipertension Gig neonatal
Gig neonatal Dope reanimacion neonatal
Dope reanimacion neonatal Curva bilirrubina fototerapia
Curva bilirrubina fototerapia Site:slidetodoc.com
Site:slidetodoc.com Moro reflex
Moro reflex Poliglobulia
Poliglobulia Reflejos en el período neonatal
Reflejos en el período neonatal