The Mood Disorders Dr Kayj Nash Okine The
- Slides: 55
The Mood Disorders Dr. Kayj Nash Okine
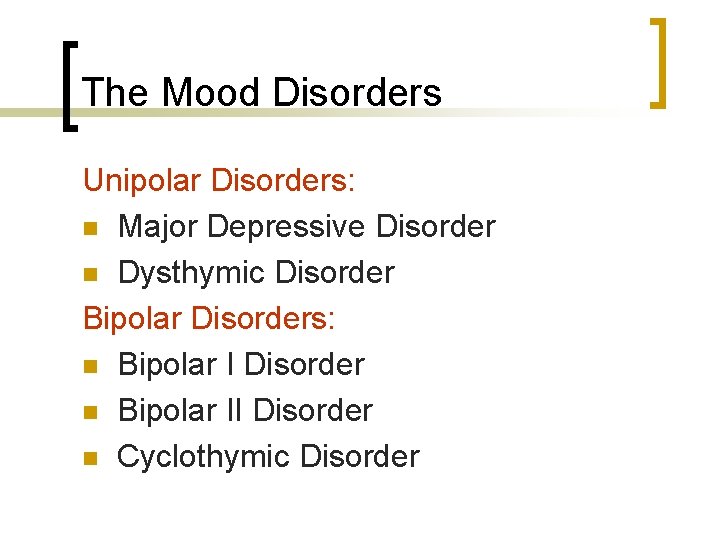
The Mood Disorders Unipolar Disorders: n Major Depressive Disorder n Dysthymic Disorder Bipolar Disorders: n Bipolar I Disorder n Bipolar II Disorder n Cyclothymic Disorder
Major Depression Emotional Symptoms: § § § § Sadness, depressed mood Anhedonia – lack of interest or pleasure Irritability Excessive or inappropriate guilt Hopelessness Feelings of worthlessness Low self-esteem
Major Depression Vegetative Symptoms: n Lack of motivation n Insomnia or hypersomnia n Increased or decreased appetite n Weight loss or gain n Fatigue, loss of energy n Psychomotor retardation or agitation
Major Depression Cognitive Symptoms: § Impaired concentration & attention § Indecisiveness § Suicidal ideation § Delusions § Hallucinations
Major Depression Social Symptoms: n Social withdrawal & isolation n Lack of communication n Lack of social initiation n Relationship problems & conflict n Dependency – clinginess, neediness
Diagnostic Criteria for a Major Depressive Episode 5+ symptoms are present for at least 2 weeks: §Depressed mood* §Loss of interest or pleasure in most activities* §Significant increase or decrease in appetite or weight §Insomnia or hypersomnia §Psychomotor agitation or retardation §Fatigue or loss of energy §Feelings of worthlessness or excessive or inappropriate guilt §Diminished ability to think or concentrate or indecisiveness §Suicidal ideation
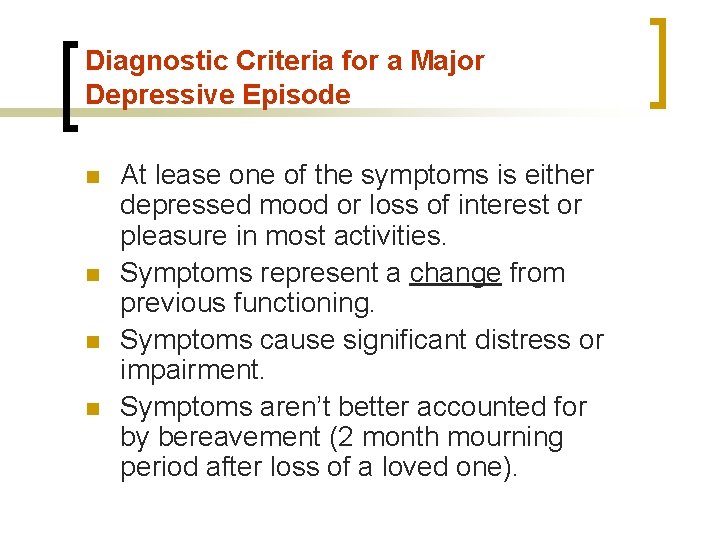
Diagnostic Criteria for a Major Depressive Episode n n At lease one of the symptoms is either depressed mood or loss of interest or pleasure in most activities. Symptoms represent a change from previous functioning. Symptoms cause significant distress or impairment. Symptoms aren’t better accounted for by bereavement (2 month mourning period after loss of a loved one).
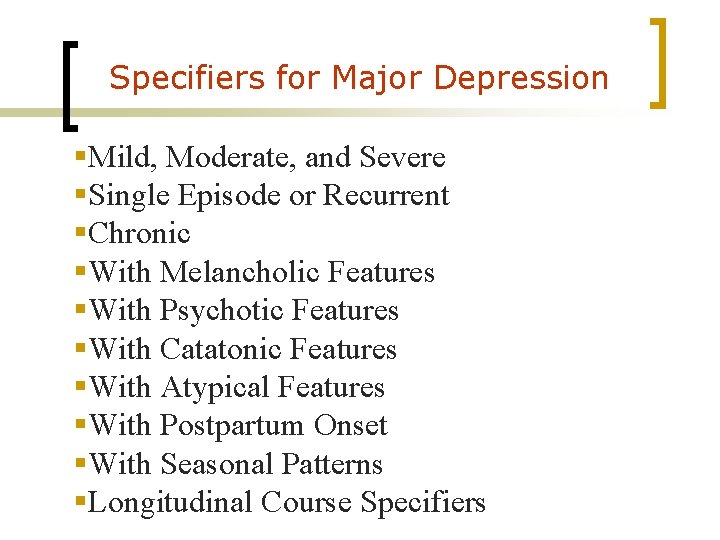
Specifiers for Major Depression §Mild, Moderate, and Severe §Single Episode or Recurrent §Chronic §With Melancholic Features §With Psychotic Features §With Catatonic Features §With Atypical Features §With Postpartum Onset §With Seasonal Patterns §Longitudinal Course Specifiers
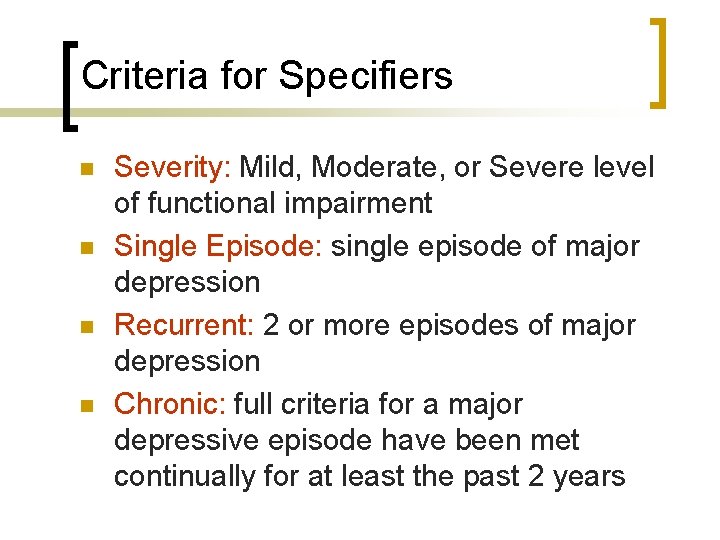
Criteria for Specifiers n n Severity: Mild, Moderate, or Severe level of functional impairment Single Episode: single episode of major depression Recurrent: 2 or more episodes of major depression Chronic: full criteria for a major depressive episode have been met continually for at least the past 2 years
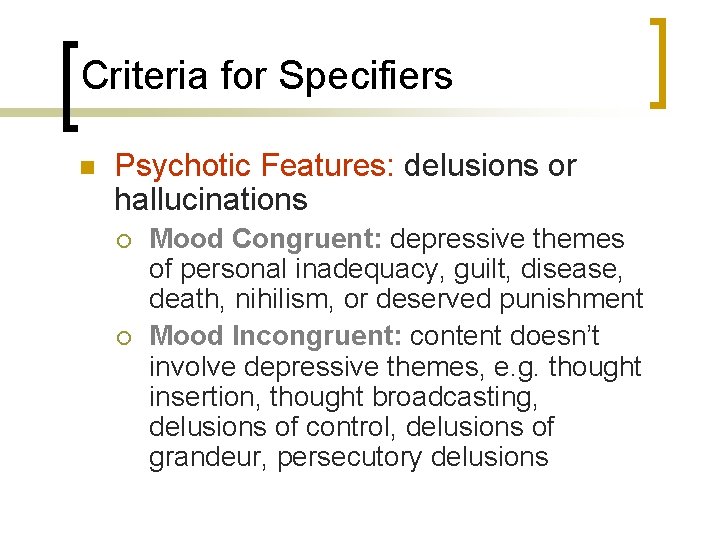
Criteria for Specifiers n Psychotic Features: delusions or hallucinations ¡ ¡ Mood Congruent: depressive themes of personal inadequacy, guilt, disease, death, nihilism, or deserved punishment Mood Incongruent: content doesn’t involve depressive themes, e. g. thought insertion, thought broadcasting, delusions of control, delusions of grandeur, persecutory delusions
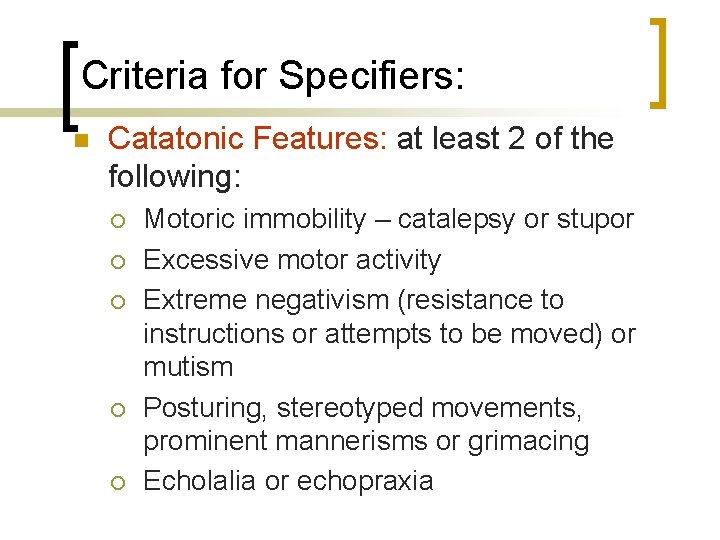
Criteria for Specifiers: n Catatonic Features: at least 2 of the following: ¡ ¡ ¡ Motoric immobility – catalepsy or stupor Excessive motor activity Extreme negativism (resistance to instructions or attempts to be moved) or mutism Posturing, stereotyped movements, prominent mannerisms or grimacing Echolalia or echopraxia
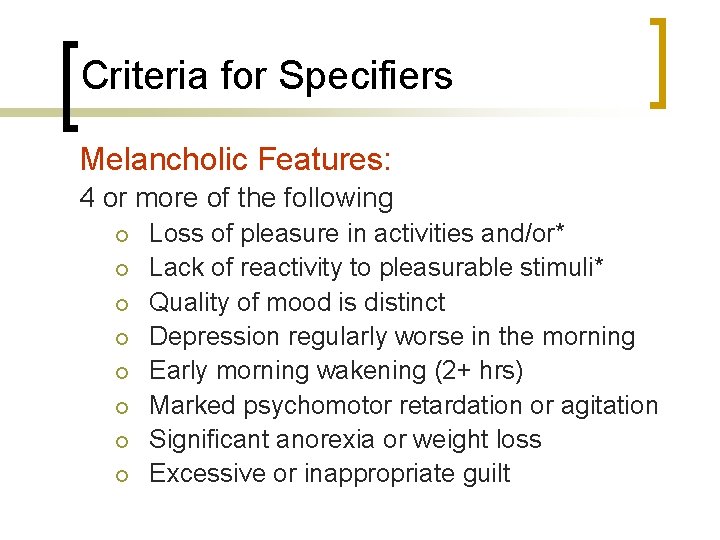
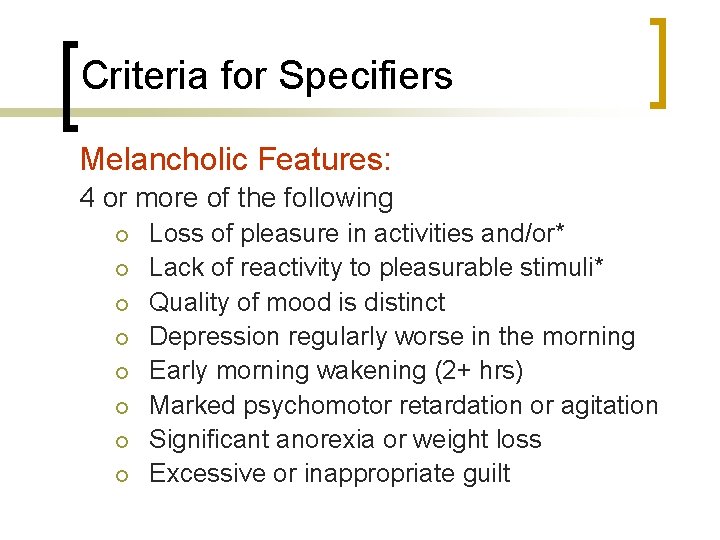
Criteria for Specifiers Melancholic Features: 4 or more of the following ¡ ¡ ¡ ¡ Loss of pleasure in activities and/or* Lack of reactivity to pleasurable stimuli* Quality of mood is distinct Depression regularly worse in the morning Early morning wakening (2+ hrs) Marked psychomotor retardation or agitation Significant anorexia or weight loss Excessive or inappropriate guilt
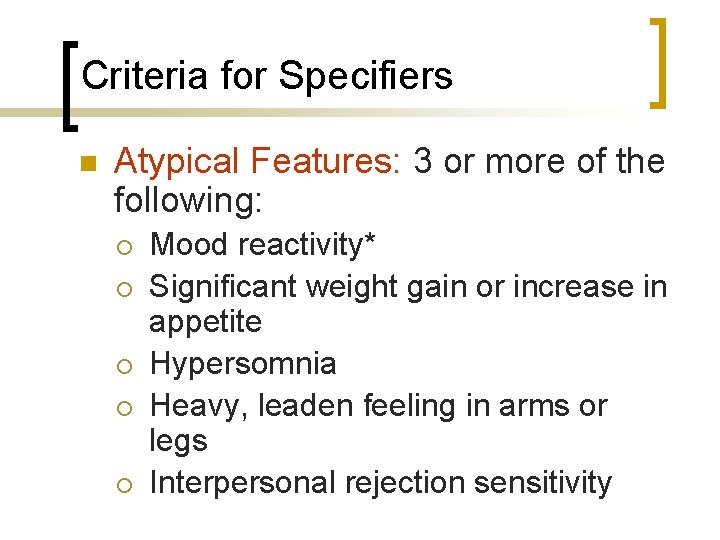
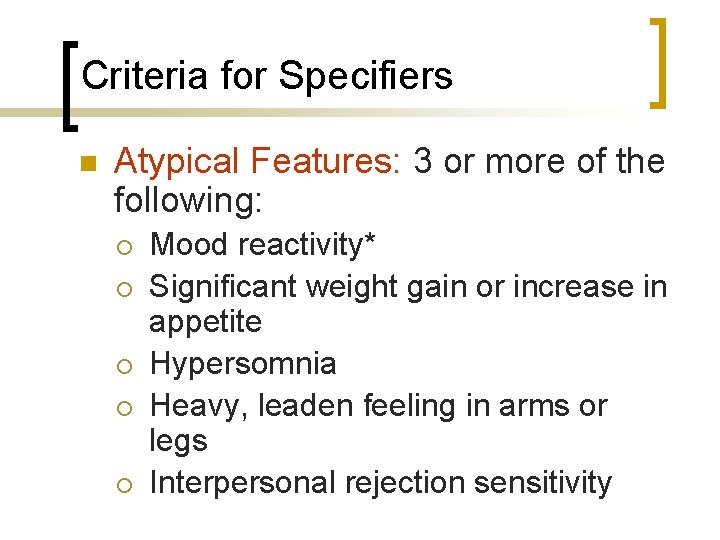
Criteria for Specifiers n Atypical Features: 3 or more of the following: ¡ ¡ ¡ Mood reactivity* Significant weight gain or increase in appetite Hypersomnia Heavy, leaden feeling in arms or legs Interpersonal rejection sensitivity
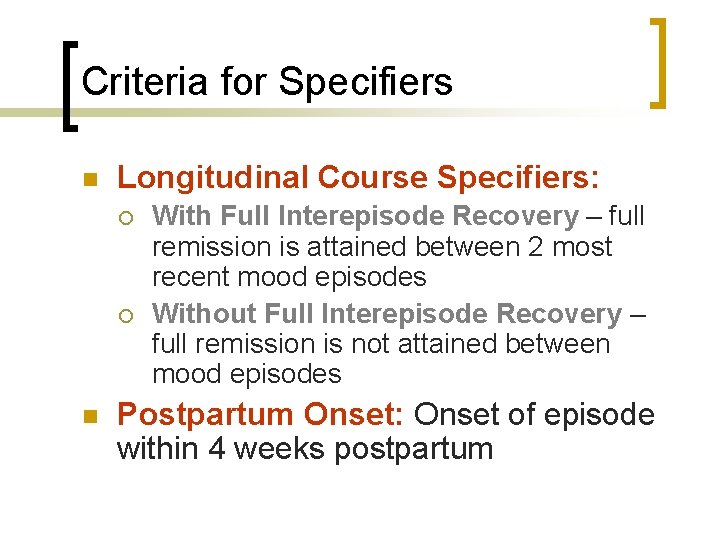
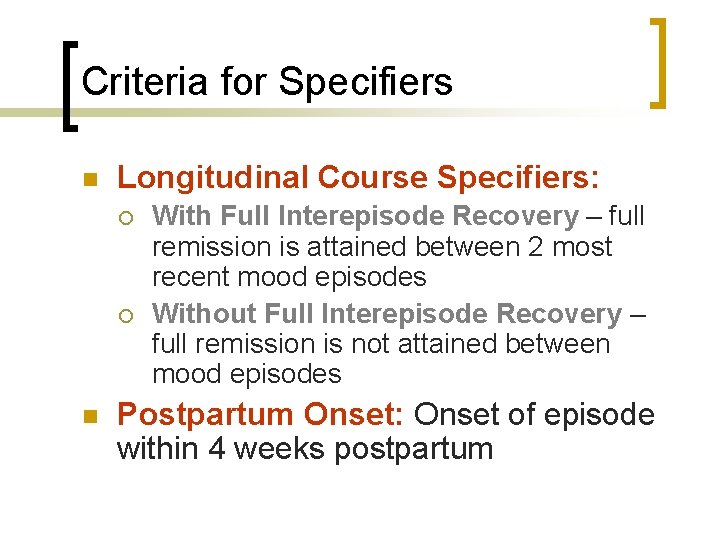
Criteria for Specifiers n Longitudinal Course Specifiers: ¡ ¡ n With Full Interepisode Recovery – full remission is attained between 2 most recent mood episodes Without Full Interepisode Recovery – full remission is not attained between mood episodes Postpartum Onset: Onset of episode within 4 weeks postpartum
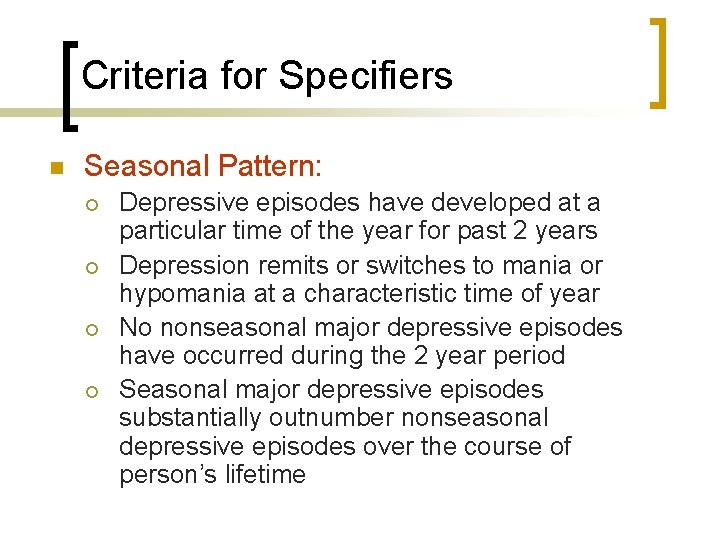
Criteria for Specifiers n Seasonal Pattern: ¡ ¡ Depressive episodes have developed at a particular time of the year for past 2 years Depression remits or switches to mania or hypomania at a characteristic time of year No nonseasonal major depressive episodes have occurred during the 2 year period Seasonal major depressive episodes substantially outnumber nonseasonal depressive episodes over the course of person’s lifetime
Prevalence Rates For Major Depressive Disorder §Lifetime prevalence: 10 -25% for women; 5 -12% for men §Point prevalence: 5 -9% for women; 2 -3% for men §Gender: women have 2 x the rates as men §Age: highest rates among 15 -24 year olds §Onset: early 20’s §Other variables: no consistent differences in rates across levels of ethnicity, education, income, or marital status
Diagnostic Criteria For Dysthymia A. Depressed mood for at least 2 years. For children & adolescents, mood may be irritable and duration may be 1 year. B. Presence of 2 or more of the following: -Poor appetite or over-eating -Insomnia or hypersomnia -Low energy or fatigue -Low self esteem -Poor concentration or difficulty making decisions -Feelings of hopelessness
Diagnostic Criteria For Dysthymia C. During the 2 yr period, the person has not been without symptoms for more than 2 months at a time. D. No major depressive episode has been present during the 1 st 2 yrs of the disturbance. After the initial 2 yrs, there may be superimposed episodes of Major Depressive Disorder, in which case both diagnoses are given.
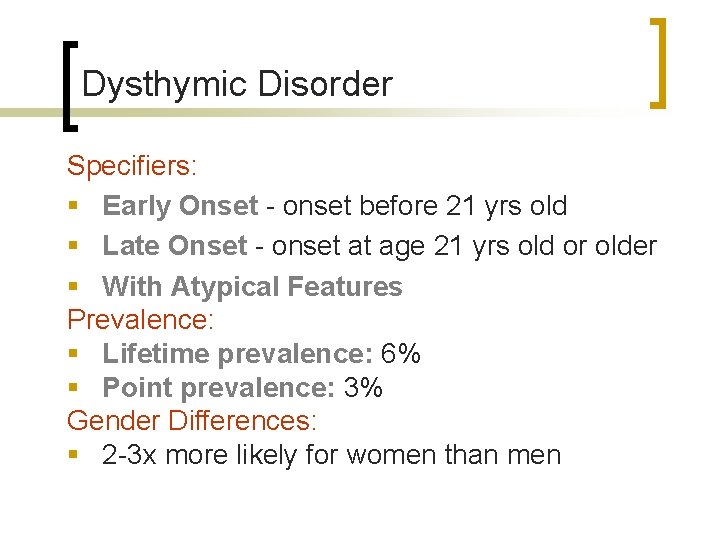
Dysthymic Disorder Specifiers: § Early Onset - onset before 21 yrs old § Late Onset - onset at age 21 yrs old or older § With Atypical Features Prevalence: § Lifetime prevalence: 6% § Point prevalence: 3% Gender Differences: § 2 -3 x more likely for women than men
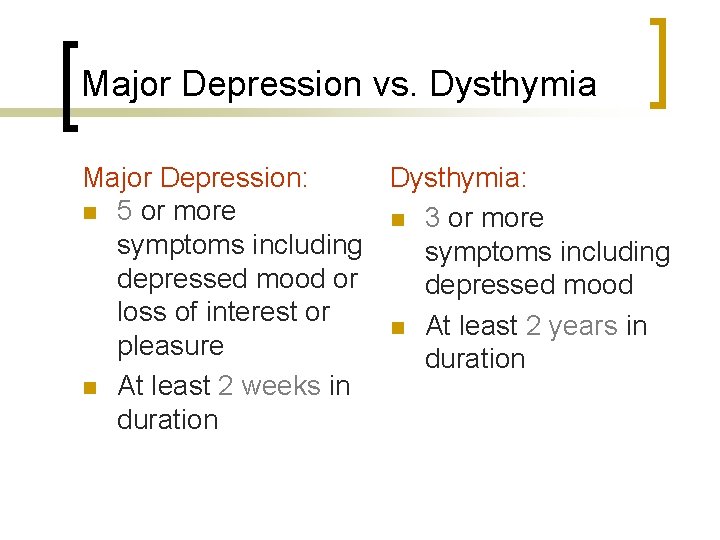
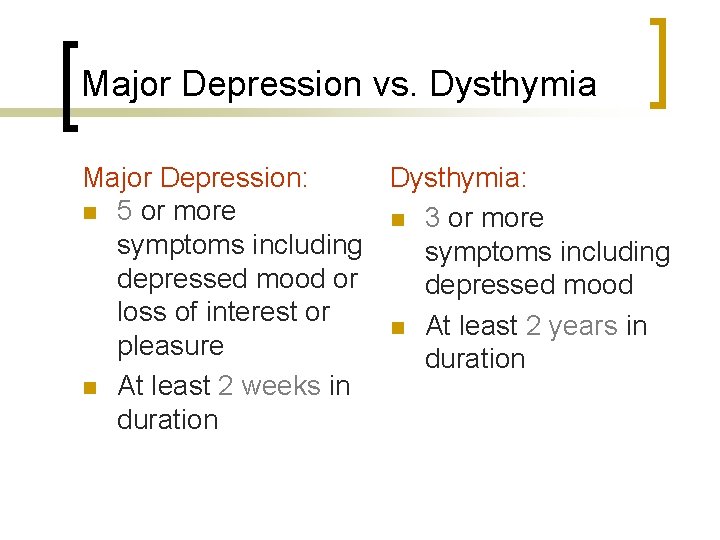
Major Depression vs. Dysthymia Major Depression: Dysthymia: n 5 or more n 3 or more symptoms including depressed mood or depressed mood loss of interest or n At least 2 years in pleasure duration n At least 2 weeks in duration
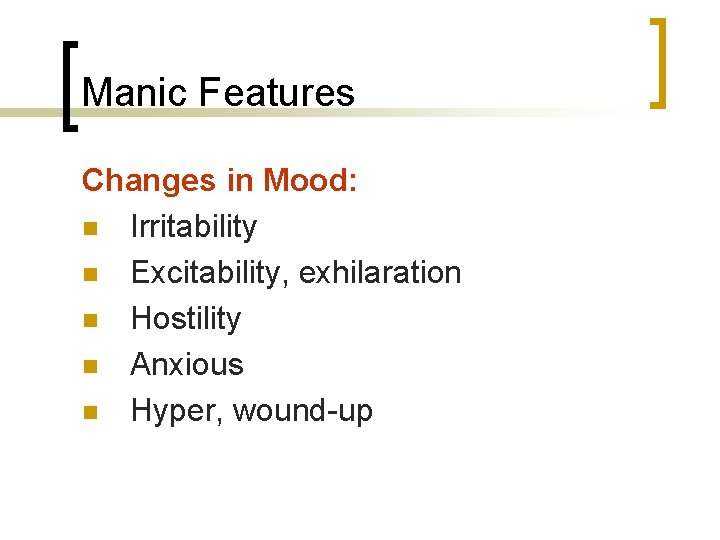
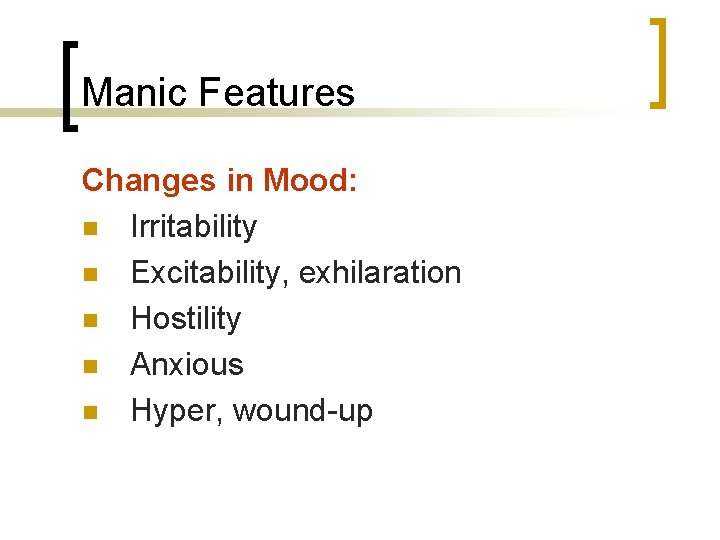
Manic Features Changes in Mood: n Irritability n Excitability, exhilaration n Hostility n Anxious n Hyper, wound-up
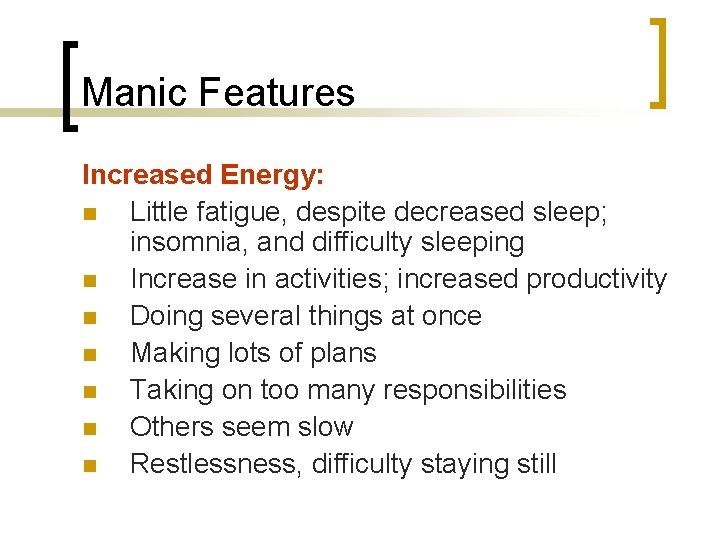
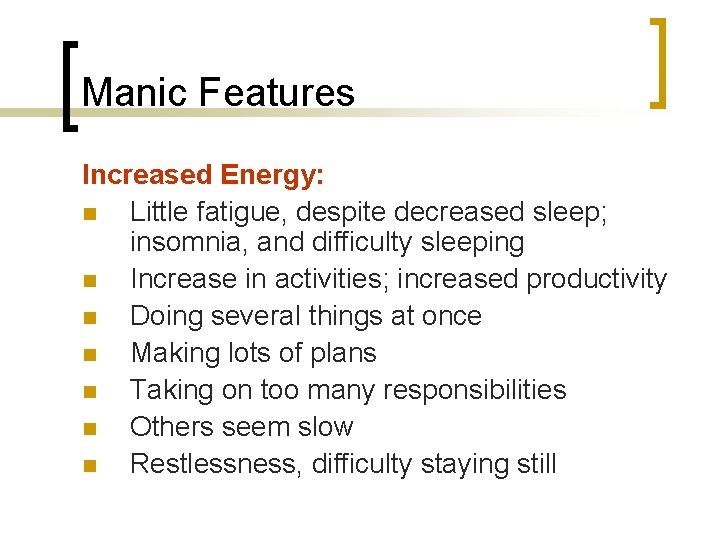
Manic Features Increased Energy: n Little fatigue, despite decreased sleep; insomnia, and difficulty sleeping n Increase in activities; increased productivity n Doing several things at once n Making lots of plans n Taking on too many responsibilities n Others seem slow n Restlessness, difficulty staying still
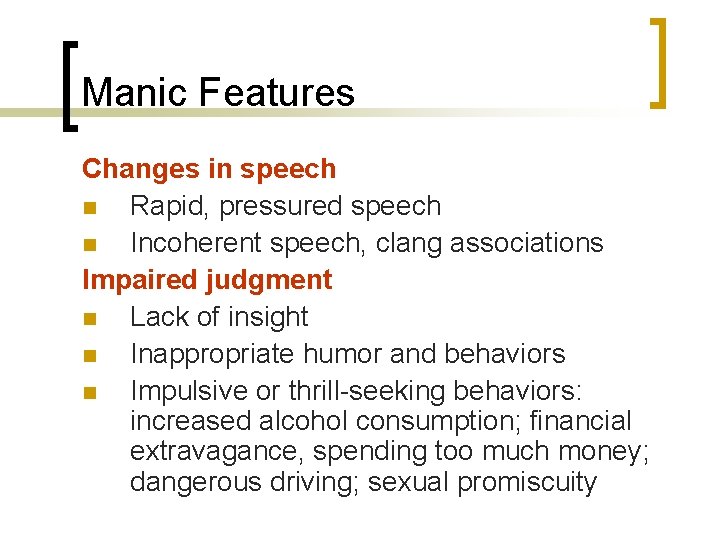
Manic Features Changes in speech n Rapid, pressured speech n Incoherent speech, clang associations Impaired judgment n Lack of insight n Inappropriate humor and behaviors n Impulsive or thrill-seeking behaviors: increased alcohol consumption; financial extravagance, spending too much money; dangerous driving; sexual promiscuity
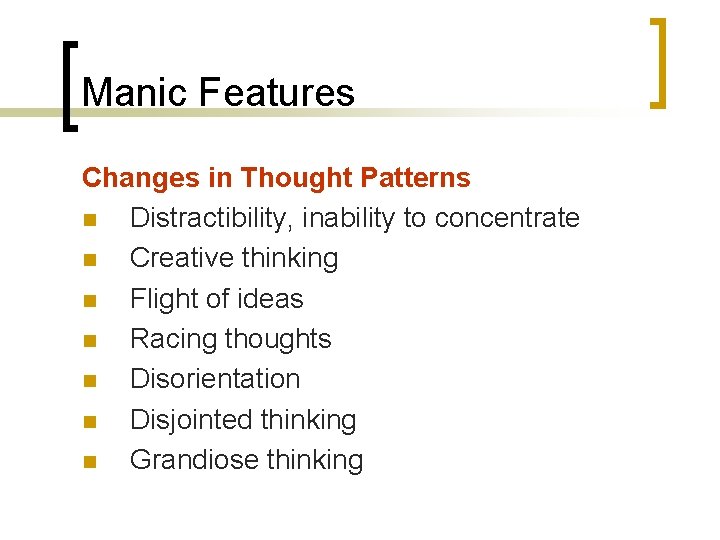
Manic Features Changes in Thought Patterns n Distractibility, inability to concentrate n Creative thinking n Flight of ideas n Racing thoughts n Disorientation n Disjointed thinking n Grandiose thinking
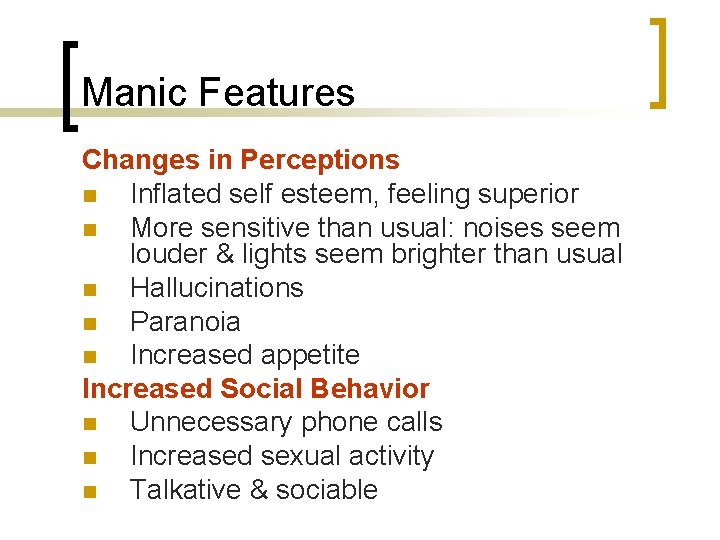
Manic Features Changes in Perceptions n Inflated self esteem, feeling superior n More sensitive than usual: noises seem louder & lights seem brighter than usual n Hallucinations n Paranoia n Increased appetite Increased Social Behavior n Unnecessary phone calls n Increased sexual activity n Talkative & sociable
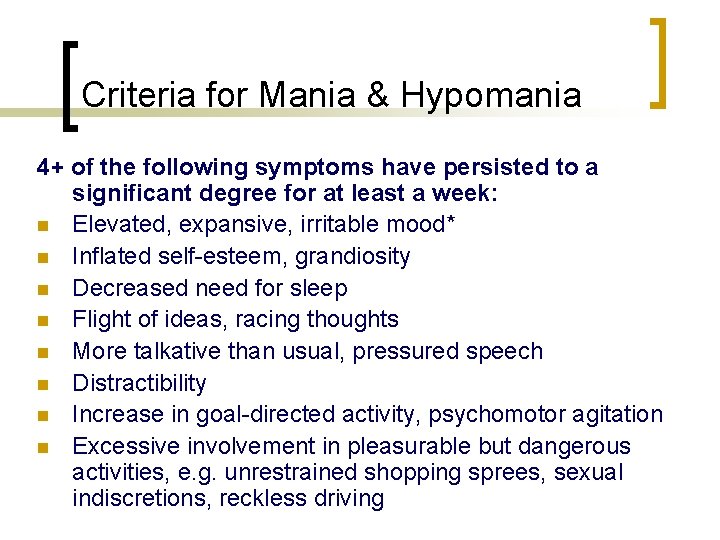
Criteria for Mania & Hypomania 4+ of the following symptoms have persisted to a significant degree for at least a week: n Elevated, expansive, irritable mood* n Inflated self-esteem, grandiosity n Decreased need for sleep n Flight of ideas, racing thoughts n More talkative than usual, pressured speech n Distractibility n Increase in goal-directed activity, psychomotor agitation n Excessive involvement in pleasurable but dangerous activities, e. g. unrestrained shopping sprees, sexual indiscretions, reckless driving
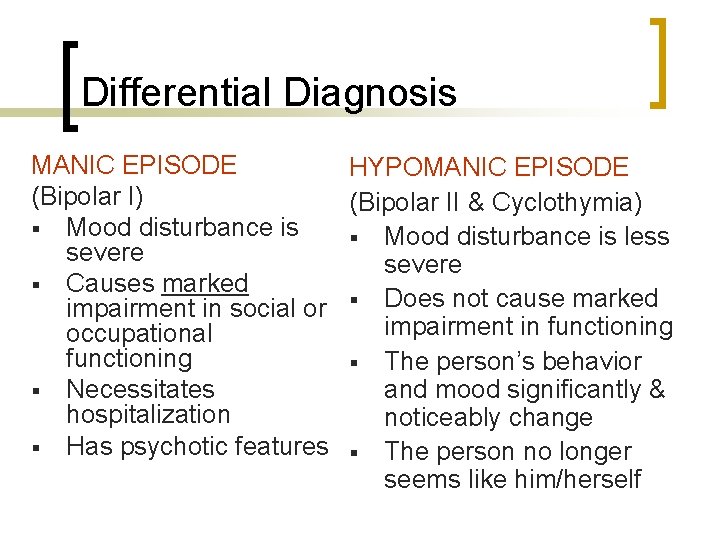
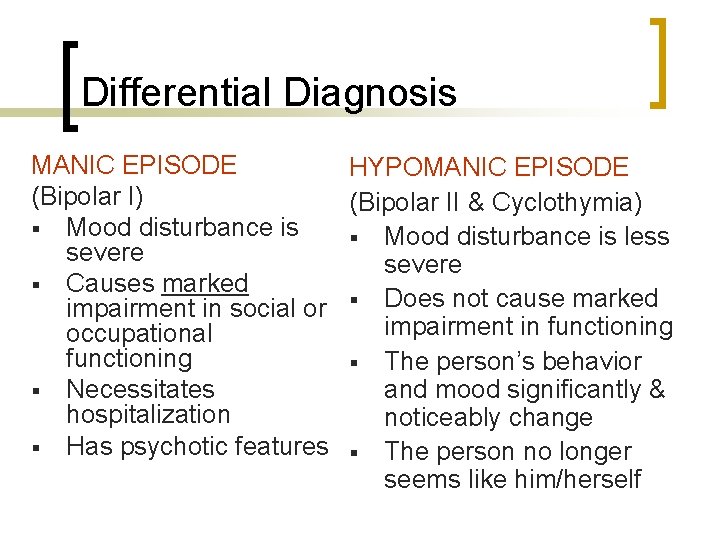
Differential Diagnosis MANIC EPISODE HYPOMANIC EPISODE (Bipolar I) (Bipolar II & Cyclothymia) § Mood disturbance is less severe § Causes marked impairment in social or § Does not cause marked impairment in functioning occupational functioning § The person’s behavior and mood significantly & § Necessitates hospitalization noticeably change § Has psychotic features § The person no longer seems like him/herself
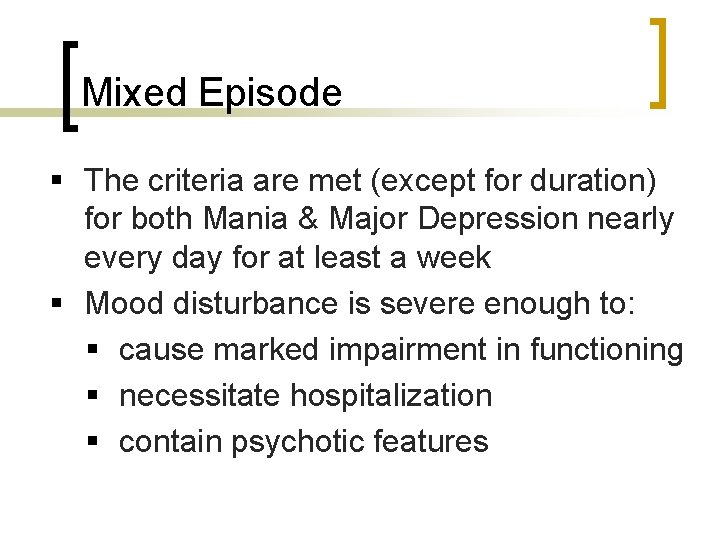
Mixed Episode § The criteria are met (except for duration) for both Mania & Major Depression nearly every day for at least a week § Mood disturbance is severe enough to: § cause marked impairment in functioning § necessitate hospitalization § contain psychotic features
Bipolar I Disorder Characterized by the occurrence of: n 1 or more Manic or Mixed Episodes n (usually) 1 or more Major Depressive Episodes
Bipolar II Disorder Characterized by the occurrence of: n 1 or more Major Depressive Episodes n At least 1 Hypomanic Episode n There has never been a Manic or Mixed Episode
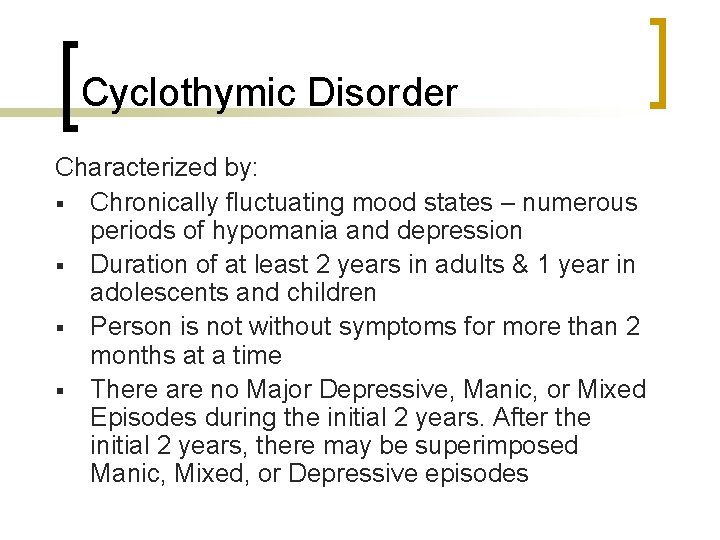
Cyclothymic Disorder Characterized by: § Chronically fluctuating mood states – numerous periods of hypomania and depression § Duration of at least 2 years in adults & 1 year in adolescents and children § Person is not without symptoms for more than 2 months at a time § There are no Major Depressive, Manic, or Mixed Episodes during the initial 2 years. After the initial 2 years, there may be superimposed Manic, Mixed, or Depressive episodes
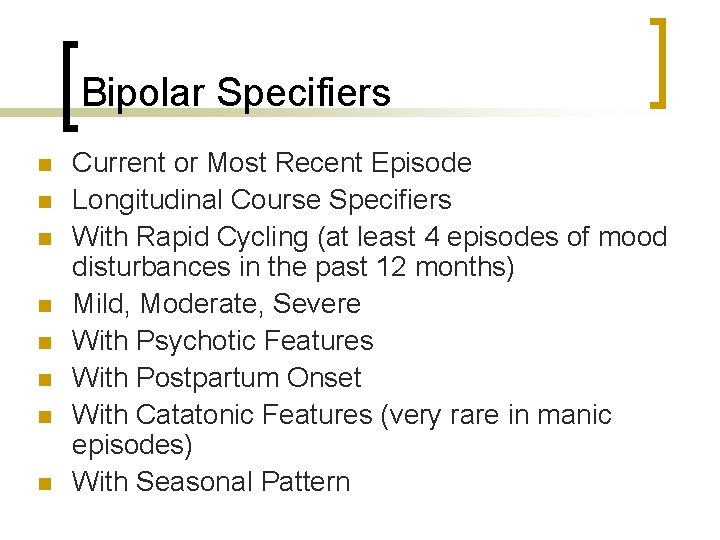
Bipolar Specifiers n n n n Current or Most Recent Episode Longitudinal Course Specifiers With Rapid Cycling (at least 4 episodes of mood disturbances in the past 12 months) Mild, Moderate, Severe With Psychotic Features With Postpartum Onset With Catatonic Features (very rare in manic episodes) With Seasonal Pattern
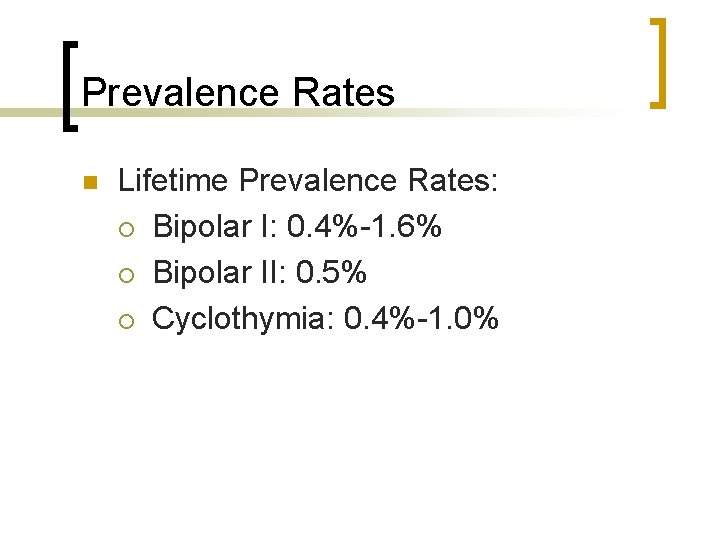
Prevalence Rates n Lifetime Prevalence Rates: ¡ Bipolar I: 0. 4%-1. 6% ¡ Bipolar II: 0. 5% ¡ Cyclothymia: 0. 4%-1. 0%
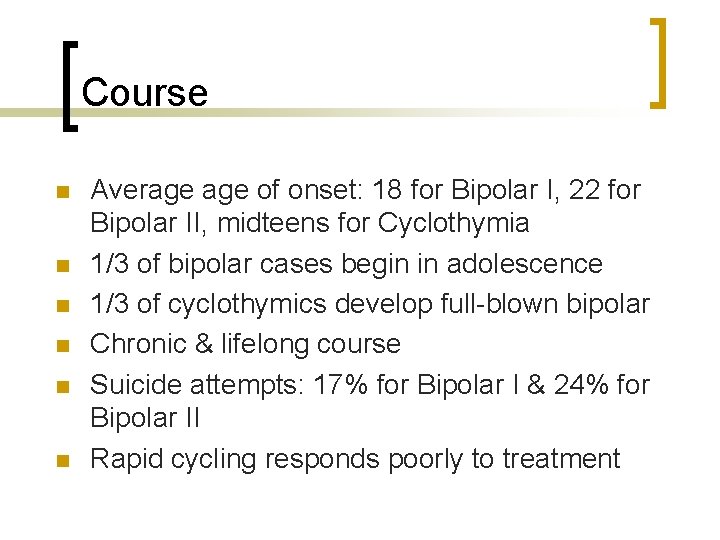
Course n n n Average of onset: 18 for Bipolar I, 22 for Bipolar II, midteens for Cyclothymia 1/3 of bipolar cases begin in adolescence 1/3 of cyclothymics develop full-blown bipolar Chronic & lifelong course Suicide attempts: 17% for Bipolar I & 24% for Bipolar II Rapid cycling responds poorly to treatment
Gender Features n n n Bipolar I and Cyclothymia are equally common in men and women Bipolar II is more common in women. Men tend to have more Manic Episodes Women tend to have more Major Depressive Episodes Women are more likely to be rapid cyclers
Biological Theories for Mood Disorders Genetic Theories: §If an individual has a mood disorder, the rates of mood disorders in his/her relatives is 2 -3 x greater §If one twin has a mood disorder, an identical twin is 2 -3 x more likely than a fraternal twin to have a mood disorder §Severe mood disorders have a stronger genetic contribution §Bipolar disorder has a stronger genetic loading §Women have a stronger genetic contribution for depression than men do
Biological Theories for Mood Disorders Neurotransmitter Theories: n Low levels of serotonin (5 HT) n Permissive hypothesis: when 5 HT levels are low, other neurotransmitters, such as norepinephrine and dopamine, range more widely & become dysregulated, contributing to mood irregularities n Kindling-sensitization model: neurotransmitter systems become more easily dysregulated with each episode of depression or mania n Dopamine may play a role in manic episodes
Biological Theories for Mood Disorders Neurophysiological Abnormalities Sleep EEG abnormalities: § Sleep continuity disturbances – the person takes longer to fall asleep, wakes more throughout the night, & wakes much earlier than usual in the morning § Reduced slow wave sleep § Earlier onset of REM sleep § Increased duration & intensity of REM sleep
Biological Theories for Mood Disorders Neurophysiological Abnormalities Alterations in cerebral blood flow & metabolism: § Increased blood flow to limbic system § Decreased blood flow to prefrontal cortex § Overactivation of nondominant side of brain
Biological Theories for Mood Disorders Hormonal Factors (“The Stress Hypothesis”) § Chronic hyperactivity in the hypothalamic-pituitary -adrenal (HPA) axis § Inability of HPA axis to return to normal following a stressor § Heightened HPA activity produces excess of the stress hormone cortisol, which may inhibit monoamine receptors § Chronic stress poorly regulated neuroendocrine systems
Drug Treatments for Mood Disorders n Drug Treatments for Major Depression – ¡ ¡ ¡ n n n Monoamine Oxidase Inhibitors (MAOI’s) Tricyclic Antidepressants (TCA’s) Selective Serotonin Reuptake Inhibitors (SSRI’s) SNRI’s Dopamine Agonists Drug Treatments for Bipolar Disorder Lithium, anticonvulsants, calcium channel blockers, antipsychotics Electroconvulsive Therapy (ECT) Light Therapy (for SAD)
Biological Treatments n n Electroconvulsive Therapy (ECT): person is anesthetized & given muscle relaxant drugs & then electric shock is administered directly to the brain, producing a seizure and convulsions Transcranial Magnetic Stimulation (TMS): magnetic coil is placed over the indiviuals head to generate a precisely localized electromagnetic pulse
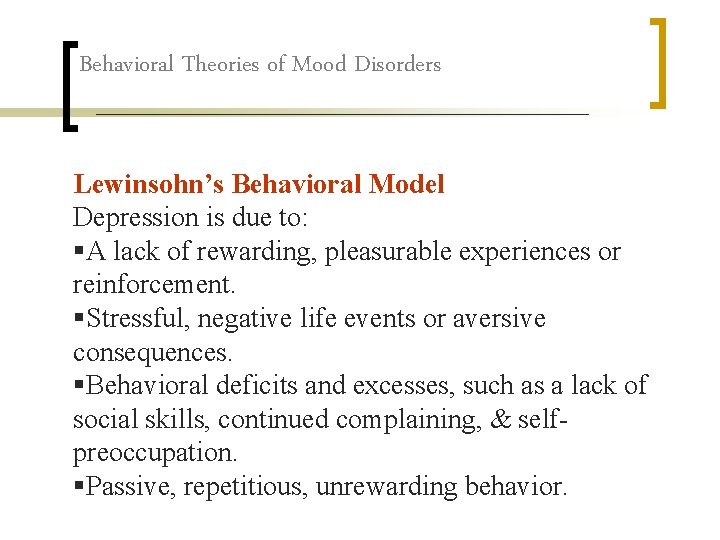
Behavioral Theories of Mood Disorders Lewinsohn’s Behavioral Model Depression is due to: §A lack of rewarding, pleasurable experiences or reinforcement. §Stressful, negative life events or aversive consequences. §Behavioral deficits and excesses, such as a lack of social skills, continued complaining, & selfpreoccupation. §Passive, repetitious, unrewarding behavior.
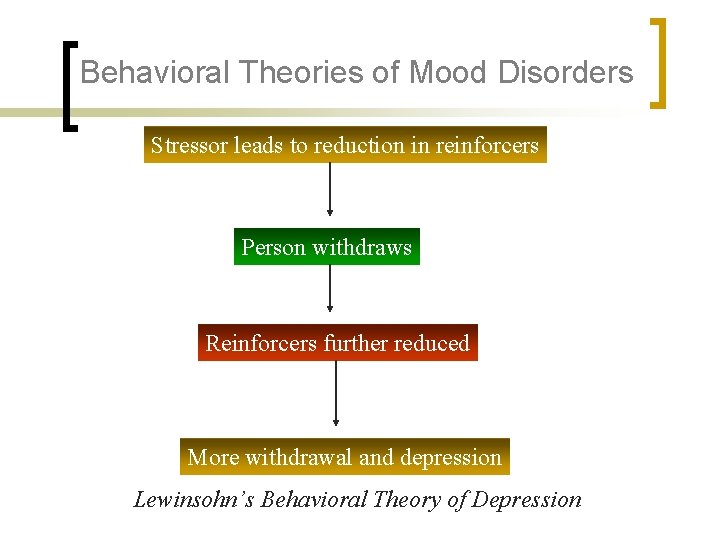
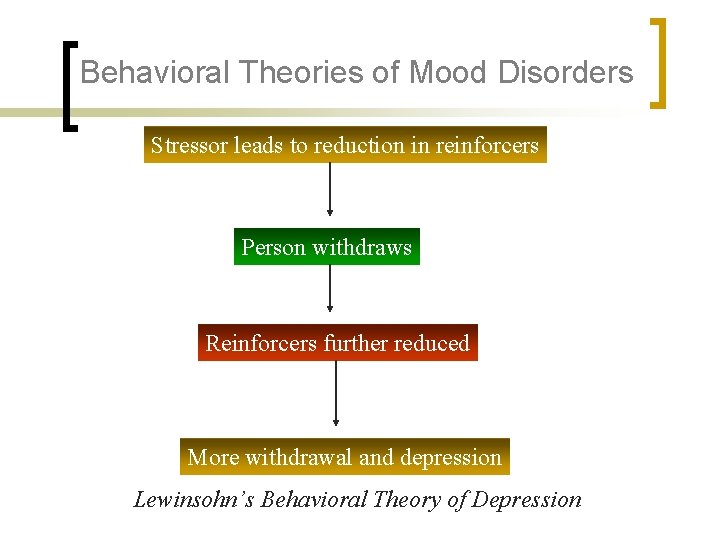
Behavioral Theories of Mood Disorders Stressor leads to reduction in reinforcers Person withdraws Reinforcers further reduced More withdrawal and depression Lewinsohn’s Behavioral Theory of Depression
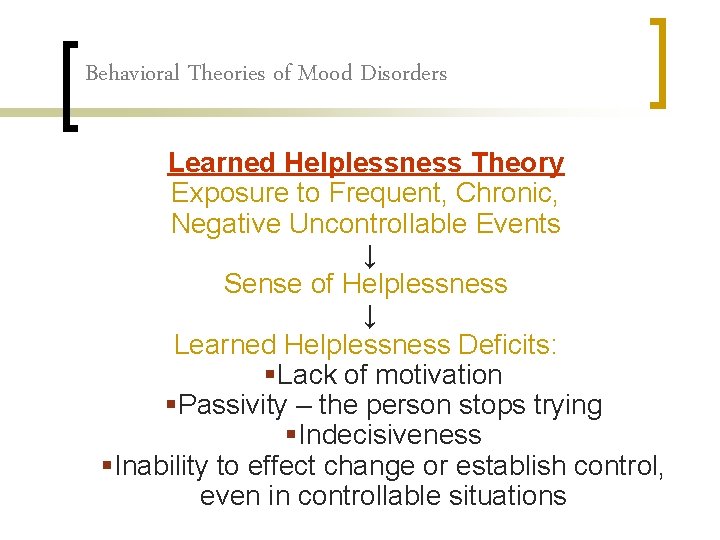
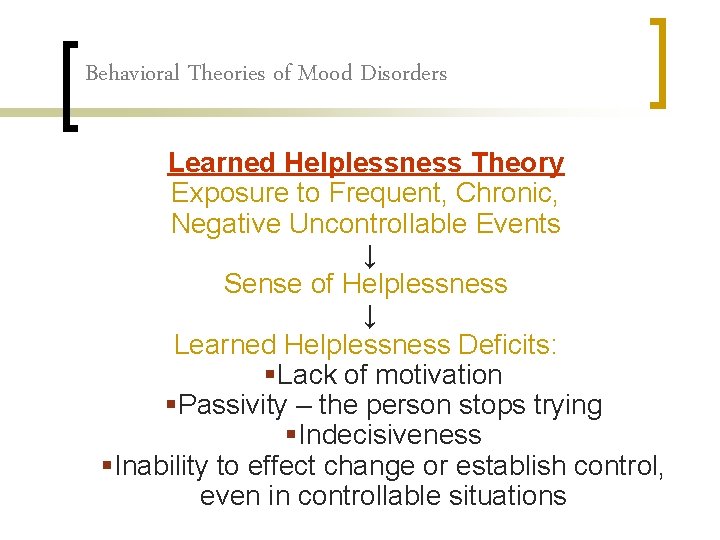
Behavioral Theories of Mood Disorders Learned Helplessness Theory Exposure to Frequent, Chronic, Negative Uncontrollable Events ↓ Sense of Helplessness ↓ Learned Helplessness Deficits: §Lack of motivation §Passivity – the person stops trying §Indecisiveness §Inability to effect change or establish control, even in controllable situations
Behavioral Therapy for Mood Disorders §Increase positive reinforcers & decrease aversive events §Change aspects of the environment related to depression §Teach person skills for addressing negative circumstances and social interactions more effectively §Teach person skills for managing their emotions and moods.
Cognitive Theories Aaron Beck’s Theory The Negative Cognitive Triad: Depressed people tend to have negative views of: (1) themselves; (2) the world; (3) the future. Cognitive distortions cause or maintain depression: §Distorted Automatic Thoughts – pervasive, negative thoughts regarding oneself, one’s experience, and one’s future, e. g. “Nothing I do works out. ” §Maladaptive Assumptions – rigid, punitive, unreasonable rules or guiding principles, e. g. “I don’t deserve to be happy. ” §Negative Schemas – core beliefs about oneself and others, e. g. “I’m such a loser. ”
Cognitive Theories Seligman’s Theory of the Depressive Attributional Style Self-critical depression and helplessness stem from certain patterns of causal attributions for negative events or failure: § Internal (vs. external) – blame self, e. g. lack of effort § Global (vs. specific) – touches many areas of one’s life § Stable – e. g. lack of ability or aptitude
Cognitive-Behavioral Therapy § § § Help person identify and challenge negative, distorted thinking and maladaptive beliefs Help the person learn more adaptive ways of thinking Help clients learn new behavioral skills
Psychodynamic Theory Early childhood experiences § unhealthy relationship patterns § dependence on the approval of others § anxiety about separation and abandonment Introjected hostility – person perceives rejection or abandonment and turns anger in on self, e. g. by blaming or punishing him/herself
Psychodynamic Therapy Insight Oriented Approach: Help the person gain insight into “old wounds” and unconscious conflicts and themes, such as introjected hostility and fears of abandonment stemming from childhood, in order to facilitate change
Interpersonal Theory of Depression (Klerman, Weissman, Rounsaville, & Chevron) §Depression is precipitated or maintained by problematic childhood relationships and current interpersonal difficulties or patterns. §Depression occurs in the interpersonal context of: §Grief over loss of significant relationships §Interpersonal role disputes & conflict §Role transitions §Interpersonal deficits – e. g. lack of social support or intimacy
Interpersonal Therapy Focuses on four types of interpersonal problems: §Grief & loss §Role disputes & conflict §Role transitions §Deficits in interpersonal skills Helps the person to establish more social support and more positive, healthy relationships
Treatments for Bipolar Disorder n n Psychotherapy: supportive, psychoeducational, self-care, family involvement Drug Treatments: ¡ ¡ Lithium Carbonate Anticonvulsants – Depakote, Lamictal Calcium Channel Blockers Antipsychotics
 Dsm 5 mood disorder
Dsm 5 mood disorder équilibre de nash
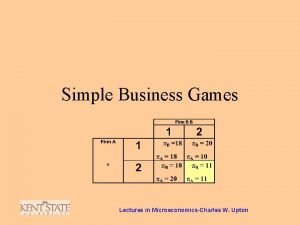
équilibre de nash Game theory microeconomics
Game theory microeconomics Pure strategy nash equilibrium example
Pure strategy nash equilibrium example Nach operating system
Nach operating system Cournot nash equilibrium
Cournot nash equilibrium John nash non cooperative game theory survivor
John nash non cooperative game theory survivor Var
Var John nash roommate
John nash roommate Equilibrio de nash ejemplos resueltos
Equilibrio de nash ejemplos resueltos John charles martin nash şizofreni
John charles martin nash şizofreni Pengertian siyaqul kalam
Pengertian siyaqul kalam Debra engelhardt-nash
Debra engelhardt-nash Brewer and nash model
Brewer and nash model Teorema de folk
Teorema de folk Harvey nash edinburgh
Harvey nash edinburgh Adam nash designer baby
Adam nash designer baby To my valentine by ogden nash summary
To my valentine by ogden nash summary Frank and jellys
Frank and jellys Doyle v white city stadium
Doyle v white city stadium Nash gleichgewicht
Nash gleichgewicht Nash-evenwicht
Nash-evenwicht Roeland van der rijst
Roeland van der rijst Nash's pyramid
Nash's pyramid Nash moe
Nash moe Simultaan en sequentieel spel
Simultaan en sequentieel spel Equilibrio de nash
Equilibrio de nash Stag hunt vs prisoner's dilemma
Stag hunt vs prisoner's dilemma Happiness reloaded meaning
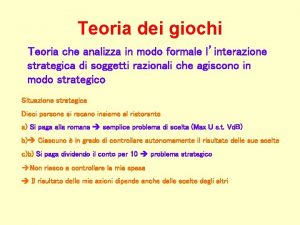
Happiness reloaded meaning Equilibrio di nash
Equilibrio di nash Ehud kalai
Ehud kalai Prisoner's dilemma nash equilibrium
Prisoner's dilemma nash equilibrium Nash-evenwicht
Nash-evenwicht Pure-strategy nash equilibria
Pure-strategy nash equilibria Fossils by ogden nash
Fossils by ogden nash Equilibrio di nash esercizi
Equilibrio di nash esercizi Ogletree, deakins, nash, smoak
Ogletree, deakins, nash, smoak Cystic hygroma
Cystic hygroma Summary of to my valentine
Summary of to my valentine Assamad nash
Assamad nash Brewer-nash model (chinese wall)
Brewer-nash model (chinese wall) Pure strategy nash equilibrium example
Pure strategy nash equilibrium example Joan nash
Joan nash Dominant strategy economics
Dominant strategy economics Extensive games with imperfect information
Extensive games with imperfect information Meeliftersgedrag
Meeliftersgedrag Nashin tasapaino
Nashin tasapaino Dominant strategy
Dominant strategy Nash delirium
Nash delirium Game theory pure strategy
Game theory pure strategy Ogden nash isabel
Ogden nash isabel Neurona motora
Neurona motora Nash equilibrium là gì
Nash equilibrium là gì Nash equilibrium prisoners dilemma
Nash equilibrium prisoners dilemma Nash evenwicht
Nash evenwicht Assamad nash
Assamad nash