Mood Disorders Chapter 18 Impact of Mood Disorders

















- Slides: 58
Mood Disorders Chapter 18
Impact of Mood Disorders • Depression is number one leading cause of disability worldwide. • Associated with high levels of impairment • Often goes undetected and untreated • Less than 50% receive treatment • One-third of bipolar diagnosed
Key Concepts • Mood: – Pervasive and sustained emotion that colors one’s perception of the world and how one functions in it • Mood Disorder: – Persisting or recurrent disturbances or alterations in mood that continually cause psychological stress and behavioral impairment over the years – Alteration in mood, not thought
Observable Expressions of Mood • Blunted • Flat • Inappropriate • Labile • Restricted or constricted
Primary Mood Disorders • Bipolar – Bipolar or manic depressive – Manic • Depressive (Unipolar) – Unipolar – Depression
Depressive Episode (DSM-IV-TR) • Depressed mood (loss of interest for two weeks) • Somatic complaints rather than sadness • Increased irritability

Depressive Disorders Clinical Course • Dysthymic Disorder – Milder, but more chronic form than MDD • Major Depressive Disorder – Progressive, recurrent illness – Over time, episodes are more frequent, severe and longer in duration. – Mean age of onset is about 40 years of age. – An untreated episode lasts six to 13 months. – Suicide is the most serious complication (10 to 15%).
Depression in Children • Less likely to experience psychosis • More likely to manifest symptoms of anxiety (fear of separation) and somatic symptoms • Mood may be irritable, rather than sad. • Suicide is a real risk, which peaks during midadolescents. • Mortality from suicide increases steadily through the teens (third leading cause of death).

Depression in the Elderly • • Most do not meet criteria for depression 8 to 20% of older adults in community 37% in primary care setting Treatment successful in 60 to 80%, but response slower • Associated with chronic illness • Highest suicide rate, especially over 85 years
Epidemiology • Lifetime risk is 7 to 12% in men, 20 to 25% in women. • Prevalence is unrelated to race. • In some cultures, somatic symptoms predominate rather than sadness.
Risk Factors • • • Prior episode of depression Family history of depressive disorder Lack of social support Stressful life event Current substance use Medical comorbidity
Major Depressive Disorder • 17% of population will have a depressive episode in their lifetime. • Age – 25 -44 years most affected • Other ages increasing, especially in the elderly • More common in women • Expressed in culture differently • Often occur with other disorders
Clinical Course of a Major Depressive Episode • Usually develops over days - weeks • Episode – minimum of two weeks • Untreated lasts six months or more, but then remits in most cases • Recovery – eight weeks of remission

Etiological Factors Biologic – Genetics • 1. 5 to 3 times first-degree relative • Alcoholism in biological parent – Biochemical changes • Serotonin, acetlycholine, norepinephrine, dopamine and GABA • Alterations in HPA, HPT axes
Etiological Factors Psychological – Psychodynamic • Deprivation of love, loss • Guilt – Behavioral • Reduction in pleasant activities – Cognitive • Irrational beliefs • Distorted attitudes – Developmental • Premature loss of parent

Etiological Factors Social – Family interactions – Adverse life event – Sexual, physical abuse

Goals of Interdisciplinary Treatment • Reduce, remove symptoms. • Restore occupational and psychosocial functioning. • Reduce likelihood of relapse. • Safety is a priority. Suicide assessment
Family Response • Affects the whole family • Often has financial hardships
Priority Care Issues • Safety • Risk for suicide
Nursing Management: Biologic Domain Assessment – Systems Review (CNS, endocrine, anemia, chronic pain, etc. ) – Physical exam: palpation of the neck for thyroid abnormalities – Appetite and weight – Sleep disturbance – Decreased energy
Nursing Diagnosis: Biologic Domain • • Disturbed sleep pattern Imbalanced nutrition Fatigue Many other possible – Failure to thrive – Bathing/hygiene deficit – Pain
Nursing Interventions: Biologic Domain • • Sleep hygiene Nutritional intervention Exercise Pharmacologic interventions – Acute – Continuation – Maintenance – Discontinuation
Psychopharmacologic Interventions • Cyclic antidepressants • Selective Serotonin Reuptake Inhibitors (SSRIs) – Fluoxetine, sertraline, fluvoxamine, paroxtine, citalopram, escitalopram • Monoamine Oxidase Inhibitors (MAOIs) – Phenelzine (Nardil), Tranylcypromine (Parnate) • Atypical antidepressants – Trazodone, bupropion, nefazodone, venalfaxine and mirtazapine
Pharmacological Nursing Interventions Monitoring and Administration – Observe taking meds (acute phase) – Vital signs (observe for orthostatic hypotension), lab reports – Diet restrictions as appropriate
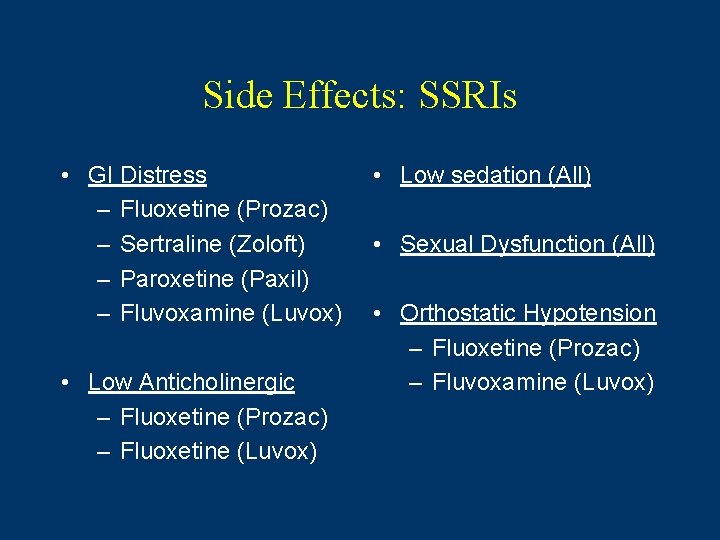
Side Effects: SSRIs • GI Distress – Fluoxetine (Prozac) – Sertraline (Zoloft) – Paroxetine (Paxil) – Fluvoxamine (Luvox) • Low Anticholinergic – Fluoxetine (Prozac) – Fluoxetine (Luvox) • Low sedation (All) • Sexual Dysfunction (All) • Orthostatic Hypotension – Fluoxetine (Prozac) – Fluvoxamine (Luvox)
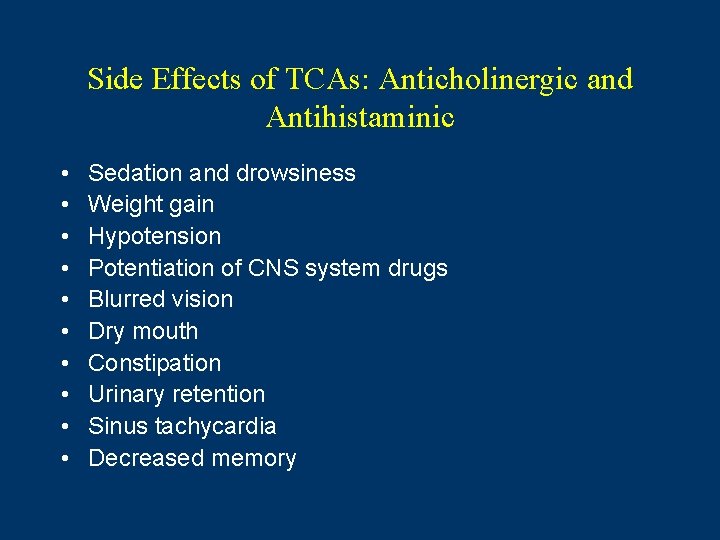
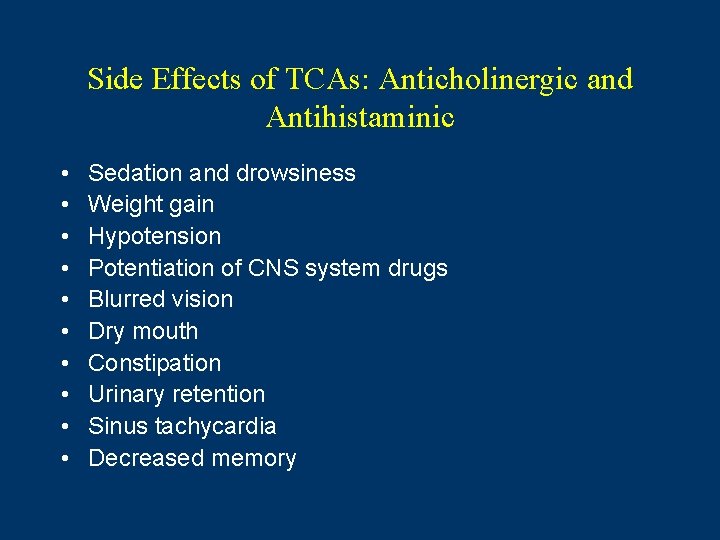
Side Effects of TCAs: Anticholinergic and Antihistaminic • • • Sedation and drowsiness Weight gain Hypotension Potentiation of CNS system drugs Blurred vision Dry mouth Constipation Urinary retention Sinus tachycardia Decreased memory
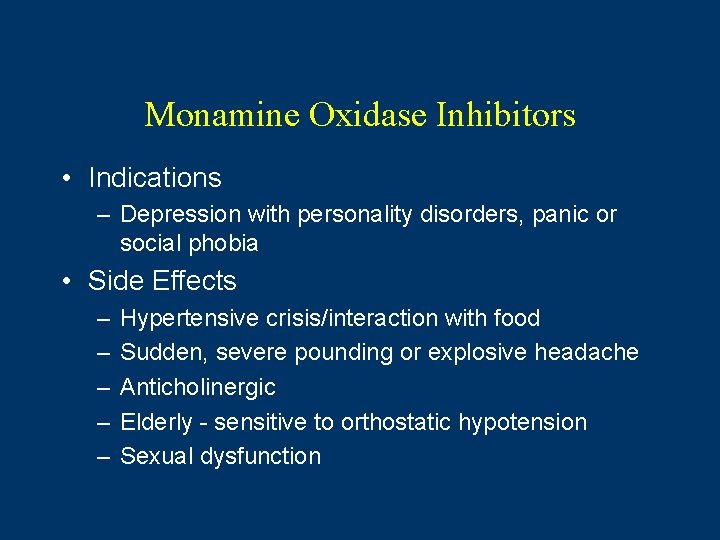
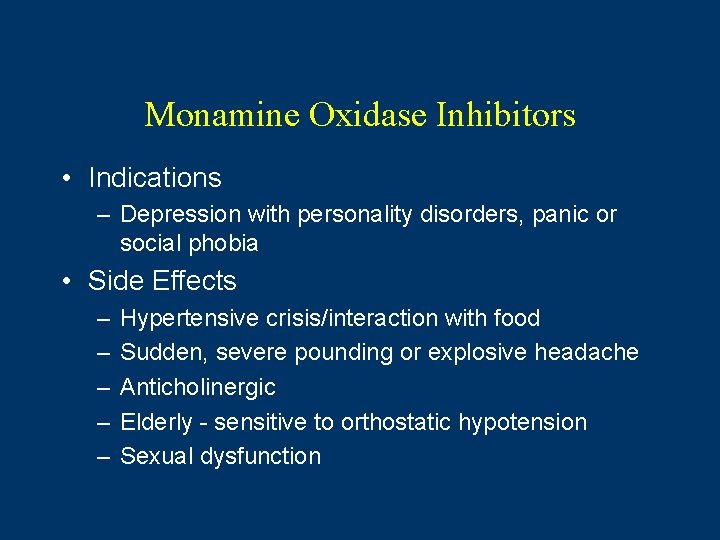
Monamine Oxidase Inhibitors • Indications – Depression with personality disorders, panic or social phobia • Side Effects – – – Hypertensive crisis/interaction with food Sudden, severe pounding or explosive headache Anticholinergic Elderly - sensitive to orthostatic hypotension Sexual dysfunction

Serotonin Syndrome • More likely to be reported in patients taking two or more serotonin antagonists • Usually mild, but can cause death • Rapid onset (compared to NMS) • Symptoms – Mental status, agitation, myoclonus, hyperreflexia, fever, shivering, diaphoresis, ataxia and diarrhea • Treatment – Stop offending drug. – Provide supportive treatment. – Notify physician.
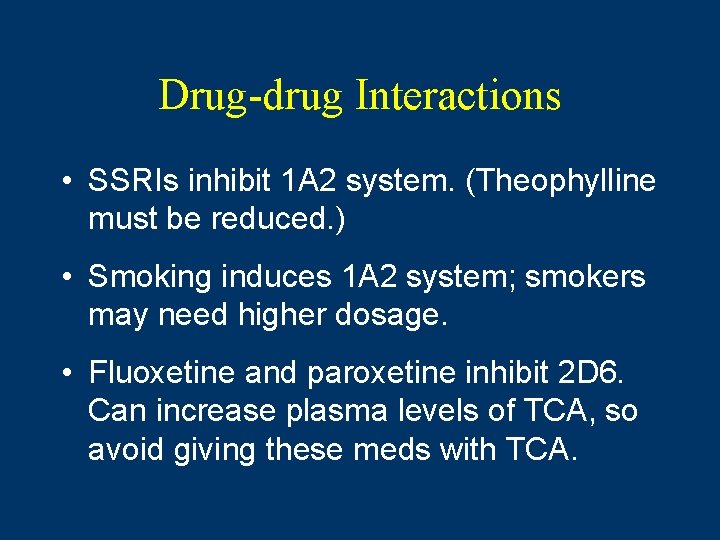
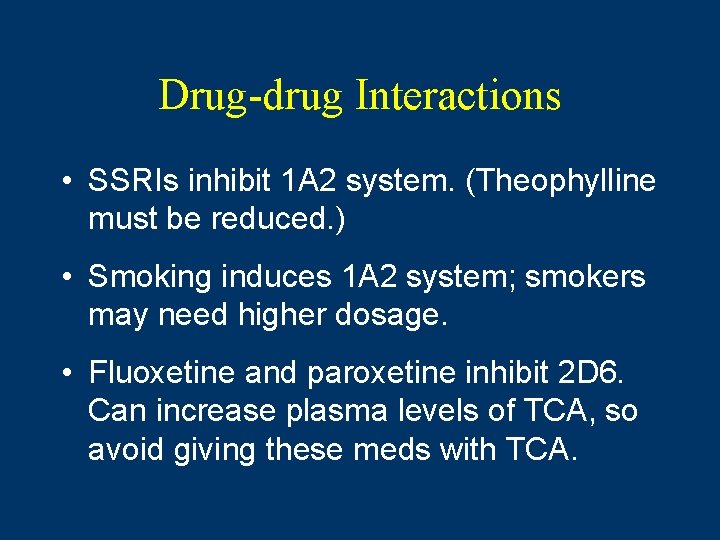
Drug-drug Interactions • SSRIs inhibit 1 A 2 system. (Theophylline must be reduced. ) • Smoking induces 1 A 2 system; smokers may need higher dosage. • Fluoxetine and paroxetine inhibit 2 D 6. Can increase plasma levels of TCA, so avoid giving these meds with TCA.

Teaching Points • If depression goes untreated or is inadequately treated, episodes become more frequent, severe and longer in duration. • Importance of continuing medication • Avoid St. John’s Wort.
Other Somatic Treatments • Electroconvulsive therapy (See Ch. 9) • Light therapy – SAD – Light - very bright, full-spectrum light, usually 2, 500 lux – Immediately upon rising – Exposure as little as 30 minutes and then increase – Full effect after two weeks

Nursing Management: Assessment Psychological – Assessment scales self-report – Mood and affect – Thought content – Suicidal behavior – Cognition and memory
Nursing Diagnoses Psychological Domain • Anxiety • Decisional conflict • Fatigue • Grieving, dysfunctional • Hopelessness • Self-esteem, low • Risk for suicide
Psychological Interventions Nurse-Patient Relationship – Withdrawn patients have difficulty expressing feelings. – Nurse should be warm and empathic, but not a cheerleader. – See Therapeutic Dialogue.
Psychological Interventions • • • Cognitive therapy - psychotherapy Behavior therapy Interpersonal therapy Marital and family therapy Group therapy Patient and family education

Nursing Management: Assessment Social Domain • Developmental history • Family psychiatric history • Quality of support system • Role of substance abuse in relationships • Work history • Physical and sexual abuse

Social Nursing Interventions • • Patient and family education Medication adherence Marital and family therapy Group therapy
Continuum of Care • Non-psychiatric setting • Acute care – hospitalization • Outpatient • See appendices for clinical pathways.
Manic Episode • Feeling unusually “high”, euphoric, irritable for at least one week • Four of the following: – – – Needing little sleep, great amount of energy Talking fast, others can’t follow Racing thoughts Easily distracted Inflated feeling of power, greatness or importance Reckless behavior (money, sex, drugs)

Types of Bipolar • Bipolar I – Combinations of major depression and full manic episode – Mixed episodes: alternating between manic and depressive episodes • Bipolar II – Combination of major depression and hypomania (less severe form of mania)

Specifiers • Mixed episodes – criteria for both manic and depressive episodes met • Hypomanic episode – same as manic but less than four days • Secondary mania – caused by medical disorders or treatment • Rapid cycling – four or more episodes within 12 months
Clinical Course • Chronic cyclic disorder • Later episodes occur more frequently than earlier. • Interpersonal relationships and occupational functioning are affected. • Patient may have rapid cycling.
Bipolar in Special Populations: Children • Recently recognized in children, it is characterized by intense rage episodes for up to two to three hours. • Symptoms of bipolar disorder reflect the developmental level of the child. • First contact with mental health agency is 5 to 10 years old. • Often have other psychiatric disorders
Bipolar Disorder: Elderly People • More neurologic abnormalities and cognitive disturbances • Late-onset bipolar disorder recently recognized • Poorer prognosis because of comorbid medical conditions
Bipolar Disorder: Epidemiology • Prevalence - 0. 4 to 1. 6% of population • Onset: 21 -30 years • Men and women equally • Ten to 15% of adolescents with recurrent depressive episodes develop bipolar I. • Many comorbid disorders (substance abuse, in particular)

Gender and Ethnic/Cultural Differences • No gender difference in incidence • Gender differences reported in phenomenology, course and treatment. – Females at greater risk for depression and rapid cycling

Etiology Biologic • Neurobiologic theories • – – – Neurotransmitter hypotheses Chronobiologic theories Sensitization and kindling theory Genetic factors – Bipolar I – 4 to 24% first-degree relatives – 80% concordance rate in identical twins – Bipolar II – 1 to 5% first-degree relatives • Psychosocial factors – Contribute to the timing of the disorder

Treatment Issues • Complex issues treated by an interdisciplinary team • Priority issues: • Safety from poor judgement and risk-taking behaviors • Risk for suicide during depressive disorders • Devastating to families, especially dealing with the consequences of impulsive behavior
Nursing Management: Biologic Domain • Assessment – – – – Evaluation of mania symptoms Sleep may be nonexistent. Irritability and physical exhaustion Eating habits, weight loss Lab studies - thyroid Hypersexual, risky behaviors Pharmacologic (may be triggered by antidepressant), alcohol use • Nursing diagnosis – Disturbed sleep pattern, sleep deprivation – Imbalanced nutrition, hypothermia, deficit fluid balance

Nursing Interventions: Biologic Domain • Physical care • Pharmacologic – Acute - symptom reduction and stabilization – Continuation – prevention of relapse – Maintenance - sustained remission – Discontinuation - very carefully, if at all • Electroconvulsive therapy
Mood Stabilizers • Lithium Carbonate (Eskalith) – Mechanism of action: unknown – Blood levels 0. 5 -1. 2 – Side effects: GI, weight gain • Divalproex Sodium (Depakote) – Increase inhibitory transmitter, GABA – Sedation, tremor • Carbamazepine
Mood Stabilizers • Lithium Carbonate • Drug profile • Lithium blood levels • Divalproex sodium (Depokote) (Drug Profile) • Carbamazapine (Tegretol) • Baseline liver function tests and complete blood count • Newer anticonvulsants • Lamotrigine (Lamictal) • Gabapentin (Neurontin) • Topiramate (Topamax)
Other Medications Used • Antidepressants – Used during depressed phases – Can trigger manic phase • Antipsychotics – Psychosis – Mania – Dosage usually lower • Benzodiazepines – Short-term for agitation
Other Medication Issues • Monitoring important • Side effect monitoring important because taking more than one medication • Drug-drug interactions – Especially, alcohol, drugs, OTC and herbal supplements • Teaching points – Lithium (Change in salt intake can affect lithium. ) – Most of these medications cause weight gain. – Check before using OTC.
Nursing Management: Psychological Domain Assessment – Mood – Cognitive – Thought Disturbances – Stress and coping factors – Risk assessment Nursing Diagnosis – Disturbed sensory perception – Disturbed thought processes – Defensive coping – Risk for suicide – Risk for violence – Ineffective coping
Nursing Management: Social Domain • Assessment – Social and occupational changes – Cultural views of mental illness • Nursing Diagnosis – – – Ineffective role performance Interrupted family processes Impaired social interaction Impaired parenting Compromised family coping
Nursing Interventions: Social Domain • Protect from over-extending boundaries • Support groups • Family interventions – Marital and family interventions

Continuum of Care • • • Inpatient management – short-term Intensive outpatient programs Frequent office visits Crisis telephone calls Family session or -
 Dsm 5 mood disorder
Dsm 5 mood disorder Chapter 18 psychological disorders
Chapter 18 psychological disorders Concept mapping chapter 11 genetic disorders
Concept mapping chapter 11 genetic disorders Define a primary skin lesion and list three types
Define a primary skin lesion and list three types Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders Chapter 46 digestive and endocrine disorders
Chapter 46 digestive and endocrine disorders Chapter 29 somatic symptom and dissociative disorders
Chapter 29 somatic symptom and dissociative disorders Chapter 29 endocrine and metabolic disorders
Chapter 29 endocrine and metabolic disorders Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 18 psychological disorders
Chapter 18 psychological disorders Chapter 18 eating and feeding disorders
Chapter 18 eating and feeding disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Chapter 15 anxiety and obsessive-compulsive disorders
Chapter 15 anxiety and obsessive-compulsive disorders Chapter 14 psychological disorders
Chapter 14 psychological disorders Chapter 14 depressive disorders
Chapter 14 depressive disorders Chapter 11 childhood and neurodevelopmental disorders
Chapter 11 childhood and neurodevelopmental disorders Chapter 5 mental and emotional problems
Chapter 5 mental and emotional problems Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases Chapter 5 lesson 2 mental disorders
Chapter 5 lesson 2 mental disorders In what situation should a nail service not be performed?
In what situation should a nail service not be performed? Milady nail diseases and disorders
Milady nail diseases and disorders Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Chapter 14 psychological disorders
Chapter 14 psychological disorders Ap psychology chapter 15
Ap psychology chapter 15 Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders Chapter 47 urinary and reproductive disorders
Chapter 47 urinary and reproductive disorders Chapter 17 somatic symptom disorders
Chapter 17 somatic symptom disorders Chapter 12 schizophrenia spectrum disorders
Chapter 12 schizophrenia spectrum disorders Extreme harmful eating behaviors
Extreme harmful eating behaviors Chapter 10 lymphatic system diseases and disorders
Chapter 10 lymphatic system diseases and disorders Is schizophrenia on a spectrum
Is schizophrenia on a spectrum Chapter 27 human impact on earth resources
Chapter 27 human impact on earth resources Chapter 16 the impact of technology
Chapter 16 the impact of technology Chapter 16: human impact on ecosystems answer key
Chapter 16: human impact on ecosystems answer key Chapter 7 lesson 4 the war's impact
Chapter 7 lesson 4 the war's impact Chapter 16 human impact on ecosystems
Chapter 16 human impact on ecosystems Chapter 21 lesson 3 the impact of alcohol abuse
Chapter 21 lesson 3 the impact of alcohol abuse Health and social care unit 14 coursework
Health and social care unit 14 coursework Unit 14 task 1
Unit 14 task 1 Neurocognitive disorder
Neurocognitive disorder Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders The flinders model
The flinders model Assistive technology for behavior
Assistive technology for behavior Somatoform disorder
Somatoform disorder Coprophilic disorder
Coprophilic disorder Types of sensory disorders
Types of sensory disorders Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Puberty and autism spectrum disorders
Puberty and autism spectrum disorders Different personality disorders
Different personality disorders Cluster c
Cluster c Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Avoidant personality traits
Avoidant personality traits Personality disorders dsm 5
Personality disorders dsm 5 Group c personality disorders
Group c personality disorders Cluster c
Cluster c