STROKE 101 Elisheva Coleman MD Assistant Professor of



- Slides: 32
STROKE 101 Elisheva Coleman, MD Assistant Professor of Neurology UC Stroke Team February 9, 2018
Case 1 An 88 -year-old woman is evaluated in the emergency department 1 hour after the acute onset of language disturbance and right-sided weakness. The family members who witnessed the onset say that the symptoms progressed over a few minutes and they describe the patient holding her head as if in pain. She has a 20 -year history of hypertension but no other medical problems; her only medication is lisinopril. During the examination, the patient becomes increasingly difficult to arouse and vomits repeatedly. She is afebrile, blood pressure is 220/110 mm Hg, pulse rate is 110/min, and respiration rate is 20/min. There is no nuchal rigidity. Carotid upstrokes are normal; there are no bruits and no jugular venous distention. Other than tachycardia, the cardiopulmonary examination is unremarkable. Global aphasia and right hemiplegia are noted. On the basis of her preliminary clinical evaluation, which of the following is the most likely diagnosis? A. A. Intracerebral hemorrhage B. B. Ischemic stroke C. C. Meningitis D. D. Transient ischemic attack
Stroke • Definition: Focal neurologic deficit caused by cerebrovascular event lasting at least 24 hours, usually of sudden onset • Ischemic (85%) • Hemorrhagic • ICH (10%) • SAH (5%) • TIA: same as above, except resolving completely within 24 hours
Epidemiology • Annual incidence in US: 795, 000 • 610, 000 are first-ever strokes • 185, 000 are recurrent strokes • Fifth leading cause of death • Leading cause of long-term disability • Higher incidence and mortality in southeastern United States ("stroke belt") c 0 mpared to rest of the country • Blacks and Hispanics have an increased risk of stroke compared with whites • The risk of first-ever stroke for blacks is almost twice that of whites
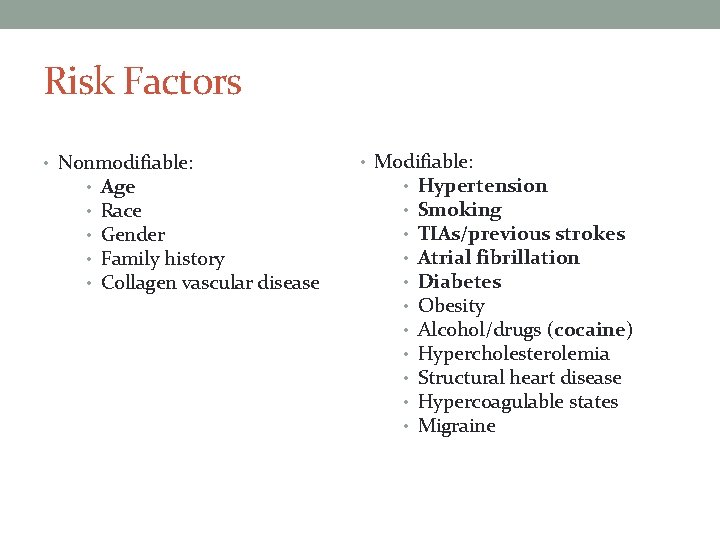
Risk Factors • Nonmodifiable: • • • Age Race Gender Family history Collagen vascular disease • Modifiable: • • • Hypertension Smoking TIAs/previous strokes Atrial fibrillation Diabetes Obesity Alcohol/drugs (cocaine) Hypercholesterolemia Structural heart disease Hypercoagulable states Migraine
Case 2 An 82 -year-old man is evaluated in the office for an episode of hesitancy in speech, word-finding difficulty, right facial droop, and weakness and awkwardness of the right hand arm. The episode occurred early yesterday, lasted 20 minutes, and was witnessed by his wife. The patient has a history of coronary artery disease, hypertension, and hyperlipidemia. Current medications are metoprolol, aspirin, hydrochlorothiazide, and lovastatin. On physical examination, temperature is normal, blood pressure is 148/88 mm Hg, pulse rate is 70/min, and respiration rate is 12/min. Neurologic examination reveals no abnormalities. Which of the following is the most appropriate next step in management? A. Add clopidogrel B. Admit to the hospital C. Order outpatient diagnostic studies D. Schedule a follow-up visit in 1 week
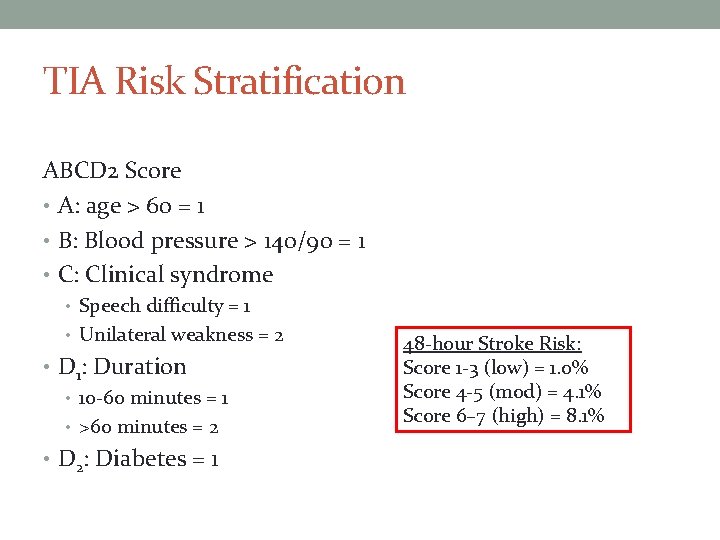
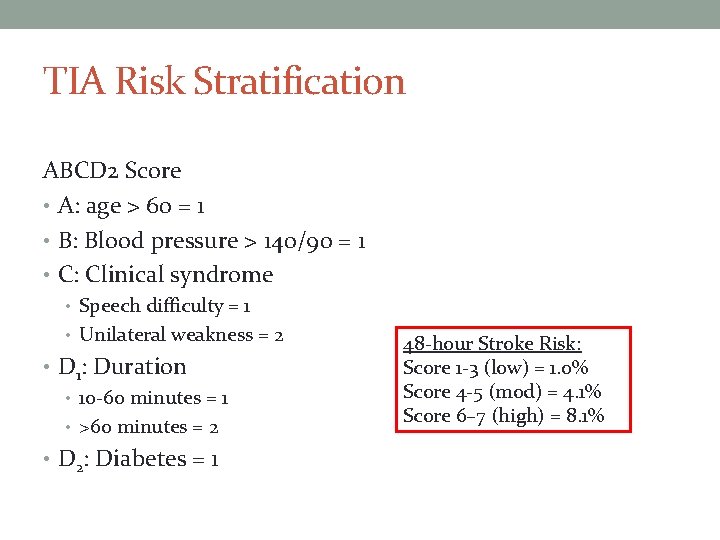
TIA Risk Stratification ABCD 2 Score • A: age > 60 = 1 • B: Blood pressure > 140/90 = 1 • C: Clinical syndrome • Speech difficulty = 1 • Unilateral weakness = 2 • D 1: Duration • 10 -60 minutes = 1 • >60 minutes = 2 • D 2: Diabetes = 1 48 -hour Stroke Risk: Score 1 -3 (low) = 1. 0% Score 4 -5 (mod) = 4. 1% Score 6– 7 (high) = 8. 1%
Case 3 A 74 -year-old man is brought to the emergency department by ambulance 1 hour after acute witnessed onset of aphasia and right hemiparesis. He has a history of hypertension and atrial fibrillation. His current medications are hydrochlorothiazide, metoprolol, and warfarin. On physical examination, blood pressure is 178/94 mm Hg and pulse rate is 80/min and irregular. Neurologic examination confirms nonfluent aphasia, a right pronator drift, a right leg drift, and an extensor plantar response on the right. Results of laboratory studies performed within 1 hour of his arrival at the emergency department show an INR of 1. 5. An electrocardiogram obtained on the patient’s arrival at the emergency department confirms atrial fibrillation. A CT scan of head obtained within 1 hour of his arrival reveals no early ischemic changes. Which of the following is the best treatment? Aspirin B. Continuous intravenous heparin C. Intra-arterial recombinant tissue plasminogen activator (rt. PA) D. Intravenous labetalol E. Intravenous rt. PA A.
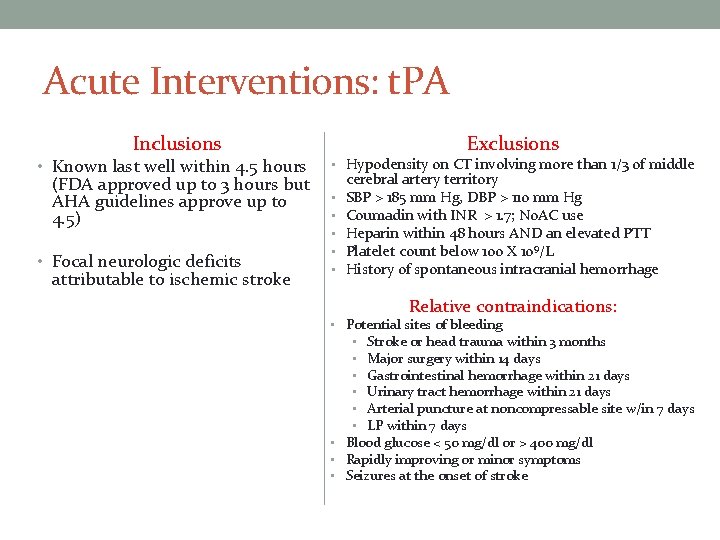
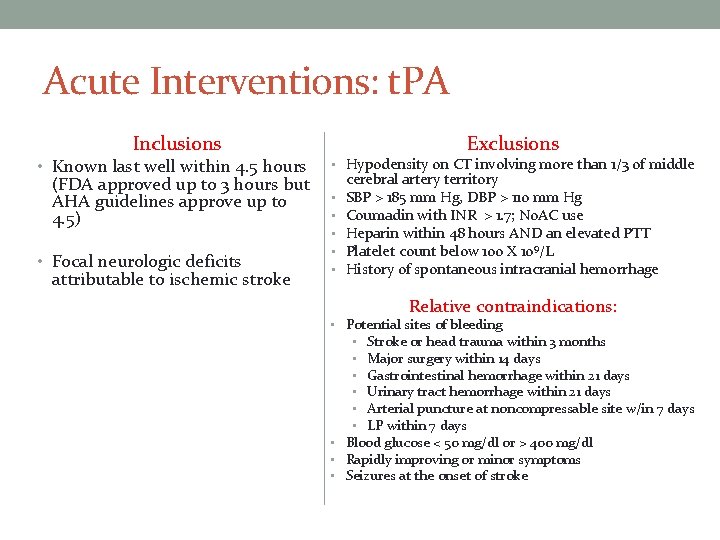
Acute Interventions: t. PA Inclusions Exclusions • Known last well within 4. 5 hours • Hypodensity on CT involving more than 1/3 of middle • Focal neurologic deficits • • • (FDA approved up to 3 hours but AHA guidelines approve up to 4. 5) attributable to ischemic stroke cerebral artery territory SBP > 185 mm Hg, DBP > 110 mm Hg Coumadin with INR > 1. 7; No. AC use Heparin within 48 hours AND an elevated PTT Platelet count below 100 X 109/L History of spontaneous intracranial hemorrhage Relative contraindications: • Potential sites of bleeding • Stroke or head trauma within 3 months • Major surgery within 14 days • Gastrointestinal hemorrhage within 21 days • Urinary tract hemorrhage within 21 days • Arterial puncture at noncompressable site w/in 7 days • LP within 7 days • Blood glucose < 50 mg/dl or > 400 mg/dl • Rapidly improving or minor symptoms • Seizures at the onset of stroke
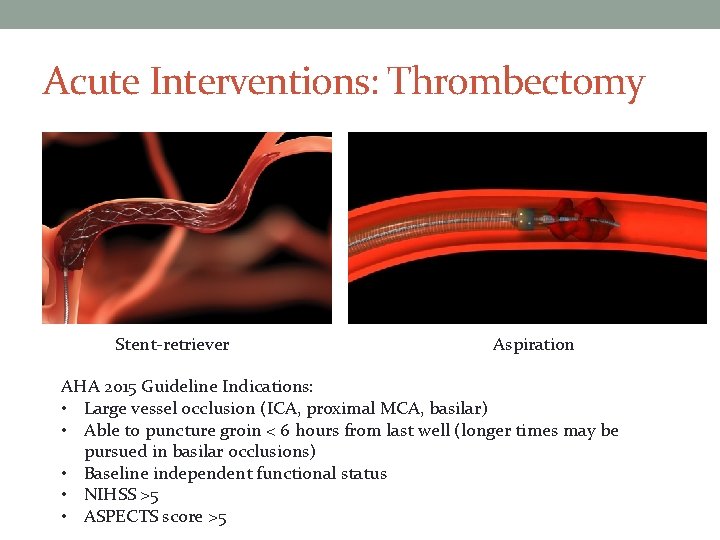
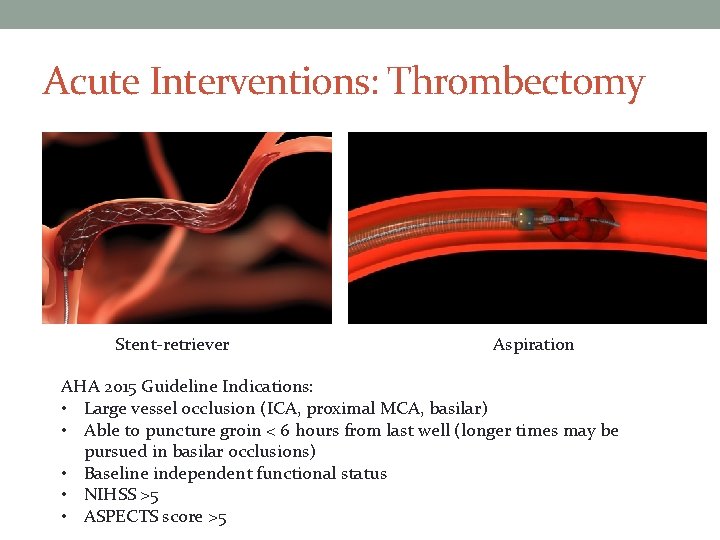
Acute Interventions: Thrombectomy Stent-retriever Aspiration AHA 2015 Guideline Indications: • Large vessel occlusion (ICA, proximal MCA, basilar) • Able to puncture groin < 6 hours from last well (longer times may be pursued in basilar occlusions) • Baseline independent functional status • NIHSS >5 • ASPECTS score >5
Extended-window thrombectomy Two new trials established benefit of thrombectomy in selected patients beyond 6 hours • Must have large vessel occlusion (ICA or M 1) • Selection based upon perfusion imaging (CT or MRI) • Mismatch between ischemic core and clinical symptoms/NIHSS (DAWN) or perfusion defect (DEFUSE 3)
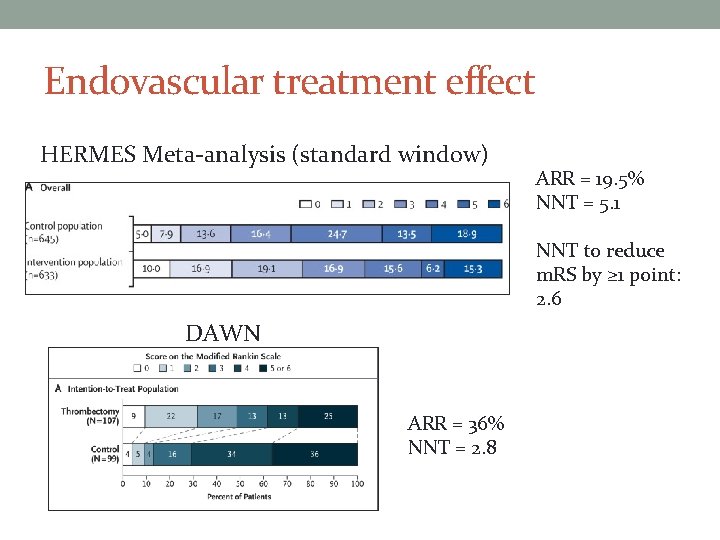
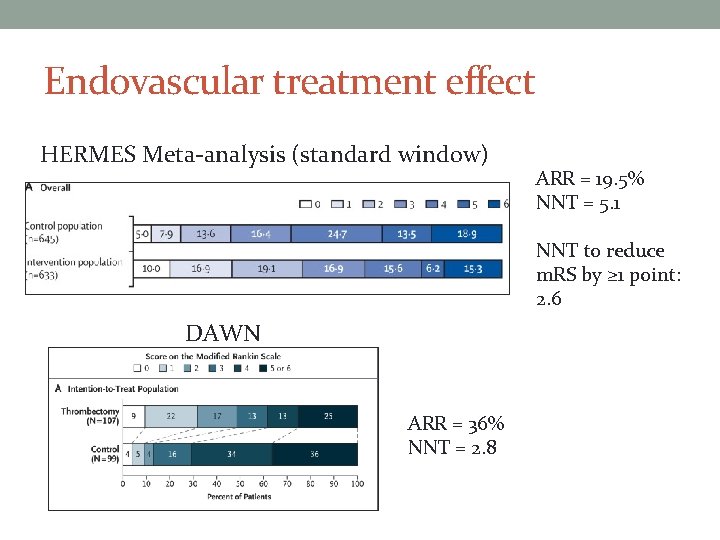
Endovascular treatment effect HERMES Meta-analysis (standard window) ARR = 19. 5% NNT = 5. 1 NNT to reduce m. RS by ≥ 1 point: 2. 6 DAWN ARR = 36% NNT = 2. 8
Diagnosis • Based on history and physical exam • Symptoms/signs localizing to a vascular distribution • Lab tests may exclude mimics (e. g. hypoglycemia) • Non-contrast head CT: hemorrhage vs. ischemia • CT can be normal acutely • Other imaging modalities: CT angiography, MRI with diffusion weighted imaging, perfusion CT/MR
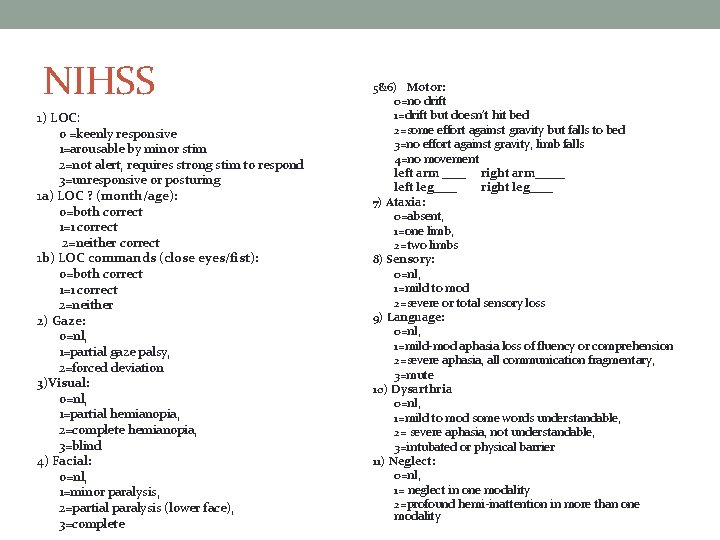
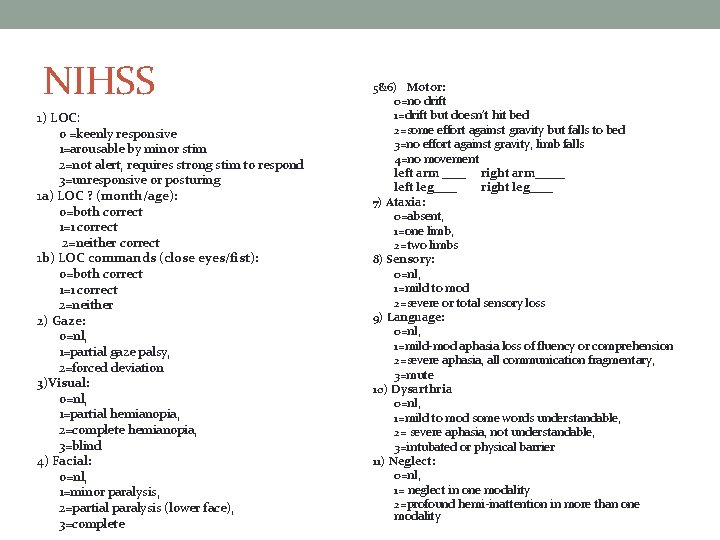
NIHSS 1) LOC: 0 =keenly responsive 1=arousable by minor stim 2=not alert, requires strong stim to respond 3=unresponsive or posturing 1 a) LOC ? (month/age): 0=both correct 1=1 correct 2=neither correct 1 b) LOC commands (close eyes/fist): 0=both correct 1=1 correct 2=neither 2) Gaze: 0=nl, 1=partial gaze palsy, 2=forced deviation 3)Visual: 0=nl, 1=partial hemianopia, 2=complete hemianopia, 3=blind 4) Facial: 0=nl, 1=minor paralysis, 2=partial paralysis (lower face), 3=complete 5&6) Motor: 0=no drift 1=drift but doesn’t hit bed 2=some effort against gravity but falls to bed 3=no effort against gravity, limb falls 4=no movement left arm ____ right arm_____ left leg____ right leg____ 7) Ataxia: 0=absent, 1=one limb, 2=two limbs 8) Sensory: 0=nl, 1=mild to mod 2=severe or total sensory loss 9) Language: 0=nl, 1=mild-mod aphasia loss of fluency or comprehension 2=severe aphasia, all communication fragmentary, 3=mute 10) Dysarthria 0=nl, 1=mild to mod some words understandable, 2= severe aphasia, not understandable, 3=intubated or physical barrier 11) Neglect: 0=nl, 1= neglect in one modality 2=profound hemi-inattention in more than one modality
Stroke Mimics • Seizure with Todd’s paralysis or non-convulsive status • Hypo- or hyper-glycemia • Complicated migraine • Mass lesion • Recrudesence: worsening or emergence of previous deficit due to infection, toxic/metabolic process • Conversion disorder
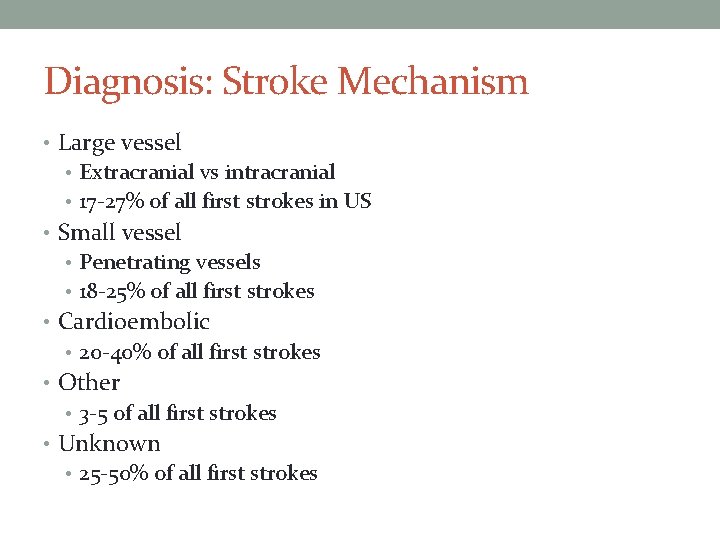
Diagnosis: Stroke Mechanism • Large vessel • Extracranial vs intracranial • 17 -27% of all first strokes in US • Small vessel • Penetrating vessels • 18 -25% of all first strokes • Cardioembolic • 20 -40% of all first strokes • Other • 3 -5 of all first strokes • Unknown • 25 -50% of all first strokes
Case 4 A previously healthy 50 -year-old woman is admitted to the hospital after three recent, transient episodes of nonfluent aphasia and right-hand numbness and weakness. One week before onset of these focal neurologic symptoms, she developed aching left jaw pain, which has persisted. She has no other medical problems and takes no medications. On physical examination, vital signs are normal. A left carotid bruit is heard on auscultation. Left miosis and left ptosis are noted. Results of laboratory studies and a CT scan of the head are normal. Which of the following is the most likely diagnosis? A. A. Cluster headache B. B. Giant cell arteritis C. C. Spontaneous left internal carotid artery dissection D. D. Spontaneous left vertebral artery occlusion
Stroke Mechanism--Other • Dissection • Hypoperfusion/watershed • Hypercoagulable state • Hematologic disorders (sickle cell, polycythemia) • Drug use (cocaine) • Inflammatory (vasculitis) • Autoregulatory disorders (PRES)
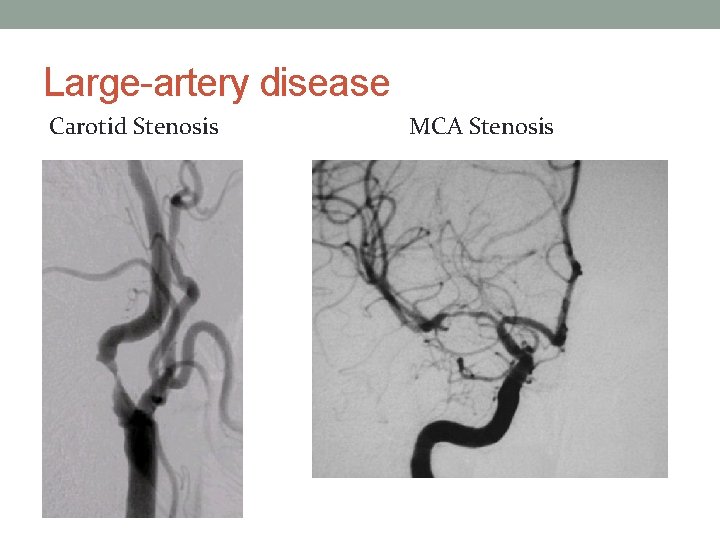
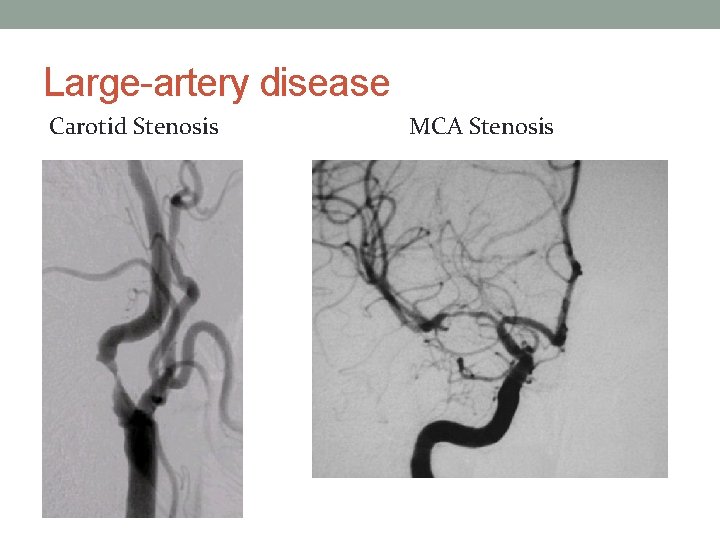
Large-artery disease Carotid Stenosis MCA Stenosis
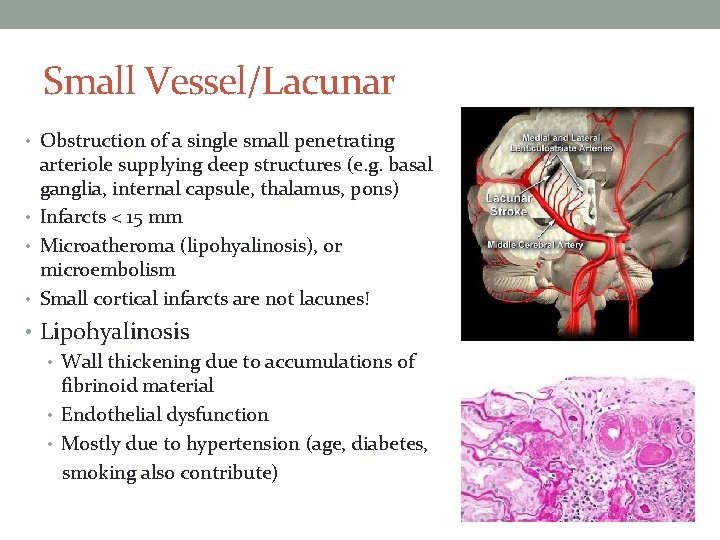
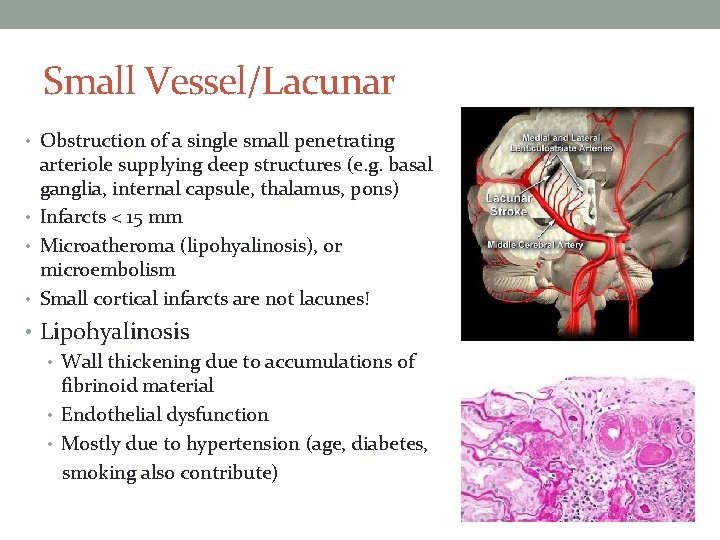
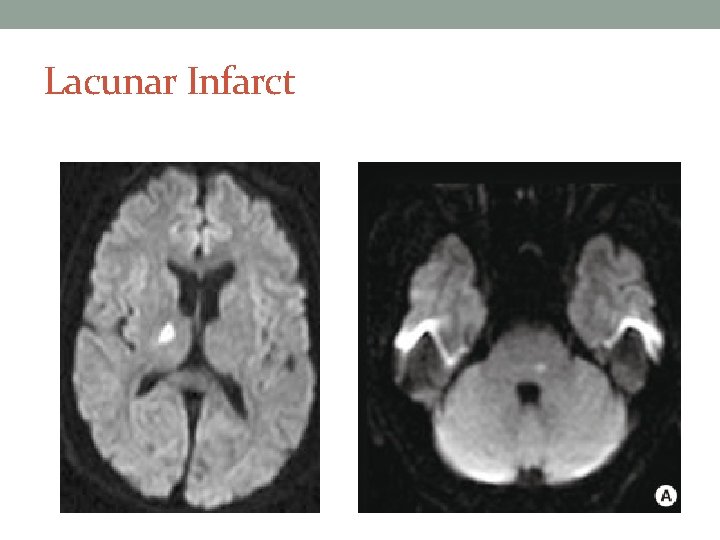
Small Vessel/Lacunar • Obstruction of a single small penetrating arteriole supplying deep structures (e. g. basal ganglia, internal capsule, thalamus, pons) • Infarcts < 15 mm • Microatheroma (lipohyalinosis), or microembolism • Small cortical infarcts are not lacunes! • Lipohyalinosis • Wall thickening due to accumulations of fibrinoid material • Endothelial dysfunction • Mostly due to hypertension (age, diabetes, smoking also contribute)

Lacunar syndromes • Pure motor stroke/hemiparesis • Pure sensory stroke • Mixed sensorimotor stroke • Ataxic hemiparesis • Dysarthria/clumsy hand
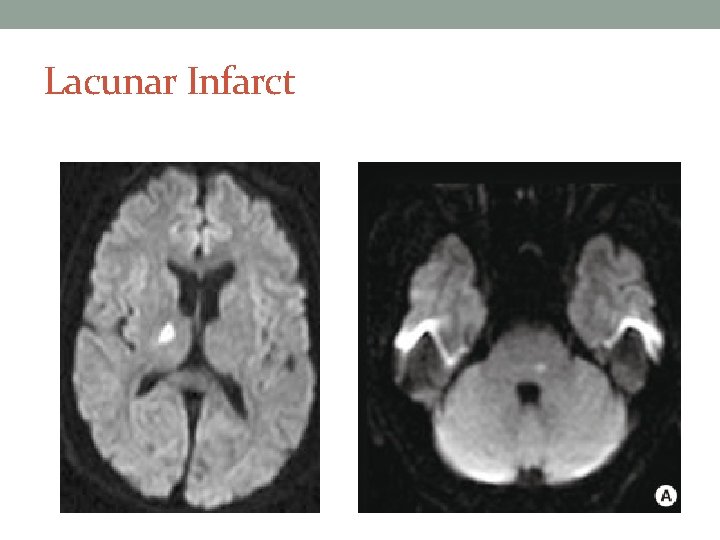
Lacunar Infarct

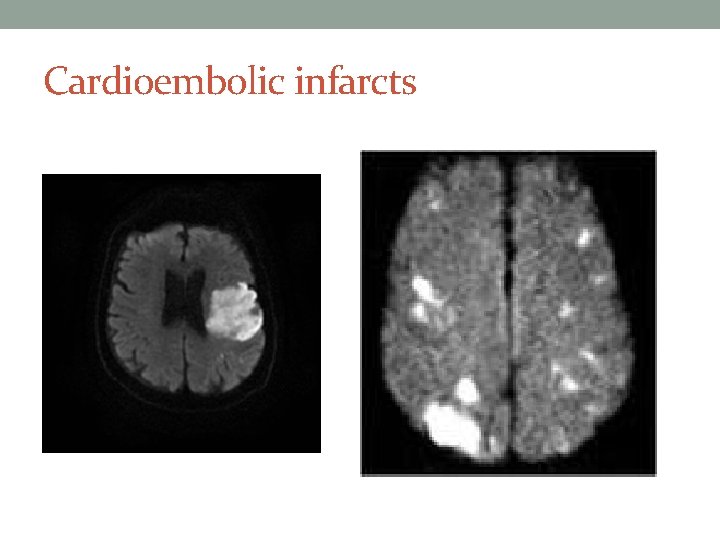
Cardioembolic High Risk • • Atrial fibrillation/flutter Rheumatic mitral or aortic valve disease Bioprosthetic and mechanical heart valves Atrial or ventricular thrombus Endocarditis (Infective, Marantic) Symptomatic congestive heart failure with ejection fraction <30 percent Recent myocardial infarction (within one month) Potential Risk • Patent foramen ovale (paradoxical embolism) • Mitral annular calcification • Atrial septal aneurysm • Left ventricular aneurysm without thrombus • Isolated left atrial “smoke” on echocardiography • Complex atheroma in the ascending aorta or proximal arch
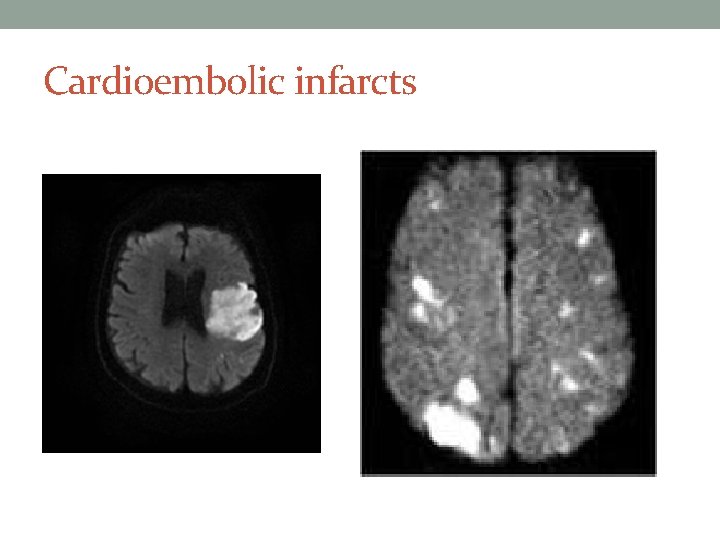
Cardioembolic infarcts
Management • Limiting cellular injury • Reperfusion – salvage penumbra (oligemic but potentially salvageable tissue • Prevent secondary injury • Neurologic Complications Systemic Complications • Rehabilitation

Secondary injury • Maintain cerebral perfusion • Impaired cerebral autoregulation • Large vessel occlusion/stenosis relying on collateral flow Permissive hypertension, don’t lower precipitously • Maintain cerebral oxygenation • Hypoxia is bad for injured brain, but there is no evidence for supplemental O 2 in patients without hypoxia • Maintain normothermia • Fever increased oxygen metabolism/demand • Maintain euglycemia • Hyperglycemia exacerbates ischemic damage
Neurologic complications • Progressive infarction or recurrent cerebral ischemia • Increased intracranial pressure – hemorrhagic transformation – cytotoxic edema (+/- vasogenic edema) • Edema maximal at 36 -72 hours, usually manifests as decline in level of consciousness • Hemicraniectomy is only treatment proven to improve outcomes • Reduces disability-free survival in patients <60 years old • Reduces morbidity in >60 • Seizures • Early seizures occur in about 5% of patients • Recurrence rate for early seizures is 30% • Prophylactic anticonvulsants are not recommended
Case 5 A 79 -year-old woman is to be transferred from the emergency department to a hospital ward for ongoing care. She awoke at home 5 hours ago with slurred speech, difficulty swallowing food and drink, and left hemiparesis. A right hemispheric ischemic stroke was diagnosed in the emergency department after a CT scan of the head confirmed a right hemispheric infarction. Because the time of stroke onset could not be determined, no recombinant tissue plasminogen activator was administered. The patient has no other medical problems and takes no medications. On physical examination, blood pressure is 168/86 mm Hg, pulse rate is 80/min, and respiration rate is 18/min. Neurologic assessment reveals dysarthria, dysphagia, left facial droop, and left hemiparesis. Laboratory studies show a plasma LDL cholesterol level of 158 mg/d. L (4. 09 mmol/L) but no other abnormalities. Which of the following is the most appropriate first step in management after transfer is completed? A. Bedside screening for dysphagia B. Oral administration of an angiotensin-converting enzyme inhibitor C. Oral administration of a statin D. Physical therapy and rehabilitation consultation
Systemic complications • Aspiration NPO, early dysphagia screen, feeding tubes if needed • DVT sub. Q Heparin, SCDs Early mobilization • Infection (leading cause of late death) Remove foleys ASAP Incentive spirometry Early mobilization • Skin Breakdown Early mobilization
Secondary Prevention • Risk factor modification – – – Anti-hypertensive Lipid management DM management Smoking cessation Diet and exercise • Appropriate medical or surgical therapy – Guided by mechanism of stroke – Echo to look for cardiac source Anticoagulation – Imaging to look for carotid source Endarterectomy or stenting – Anti-platelet
Questions?
Selected References 1. 2. 3. 4. 5. 6. 7. 8. Jauch EC , et, al. “Guidelines for the Early Management of Patients with Acute Ischemic Stroke: A Guideline for Healthcare Professionals from the American Heart Associ. . . - Pub. Med - NCBI. ” Accessed March 31, 2017. https: //www. ncbi. nlm. nih. gov/pubmed/23370205. Kolominsky-Rabas, Peter L. , Margarete Weber, Olaf Gefeller, Bernhard Neundoerfer, and Peter U. Heuschmann. “Epidemiology of Ischemic Stroke Subtypes According to TOAST Criteria. ” Stroke 32, no. 12 (December 1, 2001): 2735 – 40. doi: 10. 1161/hs 1201. 100209. Petty, George W. , Robert D. Brown, Jack P. Whisnant, Jo. Rean D. Sicks, W. Michael O’Fallon, and David O. Wiebers. “Ischemic Stroke Subtypes. ” Stroke 30, no. 12 (December 1, 1999): 2513– 16. doi: 10. 1161/01. STR. 30. 12. 2513. Schneider, Alexander T. , Brett Kissela, Daniel Woo, Dawn Kleindorfer, Kathleen Alwell, Rosemary Miller, Jerzy Szaflarski, et al. “Ischemic Stroke Subtypes. ” Stroke 35, no. 7 (July 1, 2004): 1552– 56. doi: 10. 1161/01. STR. 0000129335. 28301. f 5. Goyal, M. , B. K. Menon, W. H. van Zwam, D. W. Dippel, P. J. Mitchell, A. M. Demchuk, A. Davalos, C. B. Majoie, A. van der Lugt, M. A. de Miquel, G. A. Donnan, Y. B. Roos, A. Bonafe, R. Jahan, H. C. Diener, L. A. van den Berg, E. I. Levy, O. A. Berkhemer, V. M. Pereira, J. Rempel, M. Millan, S. M. Davis, D. Roy, J. Thornton, L. S. Roman, M. Ribo, D. Beumer, B. Stouch, S. Brown, B. C. Campbell, R. J. van Oostenbrugge, J. L. Saver, M. D. Hill, T. G. Jovin and H. collaborators (2016). "Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. " Lancet 387(10029): 1723 -1731. Nogueira, R. G, T. G. Jovin and D. T. Investigators (2018). "Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. " N Engl J Med 378(1): 11 -21. Alberti, Andrea, Maurizio Paciaroni, Valeria Caso, Michele Venti, Francesco Palmerini, and Giancarlo Agnelli. “Early Seizures in Patients with Acute Stroke: Frequency, Predictive Factors, and Effect on Clinical Outcome. ” Vascular Health and Risk Management 4, no. 3 (June 2008): 715. Camilo, Osvaldo, and Larry B. Goldstein. “Seizures and Epilepsy After Ischemic Stroke. ” Stroke 35, no. 7 (July 1, 2004): 1769– 75. doi: 10. 1161/01. STR. 0000130989. 17100. 96.