Specific Tropical Diseases Cholera Typhoid Schistosomiasis More Preparing









- Slides: 57
Specific Tropical Diseases! Cholera, Typhoid Schistosomiasis & More… Preparing for the unexpected: Epidemics

Birth of an Epidemic!
Responding in crisis! (Cholera as the prototype) First there were two… Then there were twenty two!
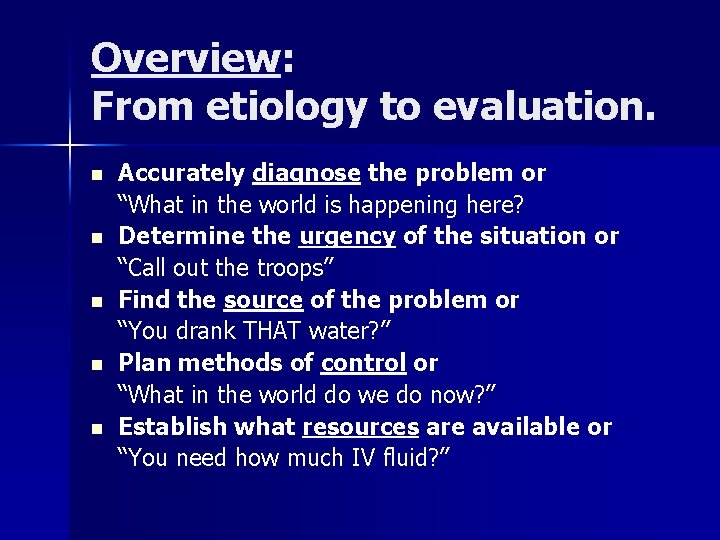
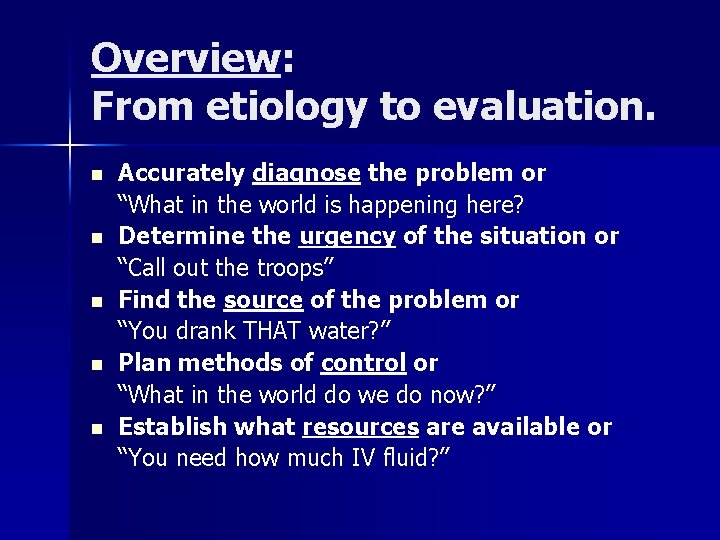
Overview: From etiology to evaluation. n n n Accurately diagnose the problem or “What in the world is happening here? Determine the urgency of the situation or “Call out the troops” Find the source of the problem or “You drank THAT water? ” Plan methods of control or “What in the world do we do now? ” Establish what resources are available or “You need how much IV fluid? ”
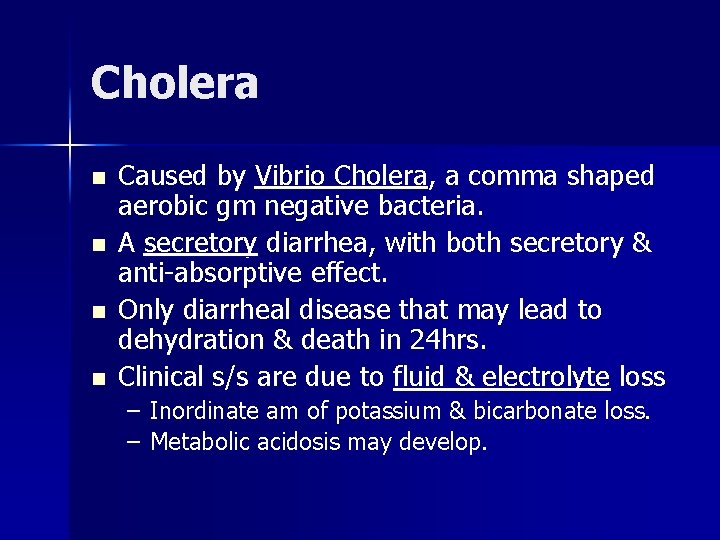
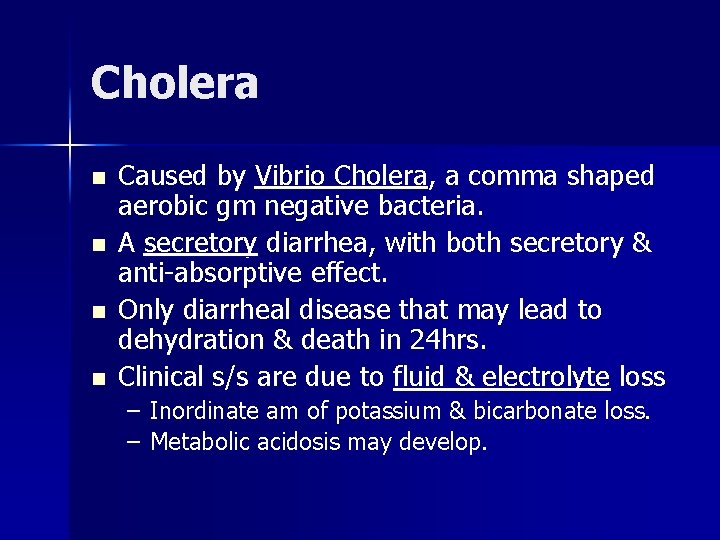
Cholera n n Caused by Vibrio Cholera, a comma shaped aerobic gm negative bacteria. A secretory diarrhea, with both secretory & anti-absorptive effect. Only diarrheal disease that may lead to dehydration & death in 24 hrs. Clinical s/s are due to fluid & electrolyte loss – Inordinate am of potassium & bicarbonate loss. – Metabolic acidosis may develop.
1. Accurately diagnose the problem! n n Is this really cholera? – Laboratory evidence? – Clinical presentation Differential diagnosis for cholera: – Amebic or bacillary Dysentery – HIV/AIDS – Parasitic diarrheal diseases….
2. Determine the urgency of the situation! n n n How many people are being affected or potentially exposed? Causative agent: How is it spread? Is this problem potentially fatal?
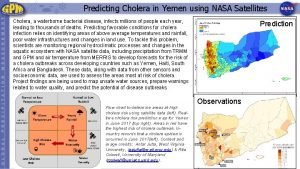
3. Find the source - root cause of the problem? n Water borne: – Ability to purify the water (fecal/oral transmission) n n n Lack of access to clean water & sanitation facilities (poverty) Reservoir: humans (feces & vomitus of sick or carriers) Occurrence of cases(incubation-2 -3 days)
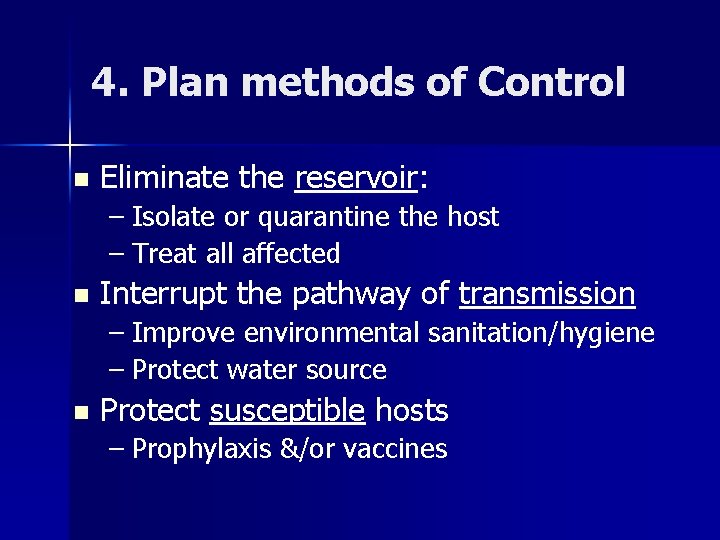
4. Plan methods of Control n Eliminate the reservoir: – Isolate or quarantine the host – Treat all affected n Interrupt the pathway of transmission – Improve environmental sanitation/hygiene – Protect water source n Protect susceptible hosts – Prophylaxis &/or vaccines
5. Establish what resources are available n n n n IV fluids, IV sets, needles, IV poles… Medications: to treat causative agent Personnel: Number of nurses available Laundry facilities Organizations- government or NGOs Vaccines or prophylactic meds Isolation capability Money…
Plan/response to individual case of Cholera. n Signs & Symptoms: – Sudden onset of profuse “ricewater” stools n May be 20 liters/24 hrs n Use a “cholera cot” – Severe dehydration: – Vomiting – Deep rapid respirations: metabolic acidosis – Cir. collapse & shock – Death may result within hours.
Implementing the plan(treatment options) n Rehydration is key – ORS: To 1 L water add; ½ tsp salt, 8 tsp sugar, ½ tsp soda & juice of one orange. – Most can be rehydrated with ORS. – IV Fluids: (type/rate) n n n Lactated ringers Darrows Normal Saline (Nacl)
Treatment-cont’d n Meds-adults – – – n Doxycycline 300 mg stat Cipro 1000 mg stat Bactrim DS 1 q 12 hr x 3 days Meds-peds: – Erythromycin 10 mg/kg q 8 hr for 3 days – Doxycycline 6 mg/kg stat if >7 yrs old
Control-Prevention n n n Proper disposal of waste. Strict hand washing Isolation of cases Restrict public gatherings Proper disposal of dead bodies Boil or treat drinking water. Fly/vector control measures
Control of: contacts/community n n Prophylaxis for close family contacts: (tracing & treating contacts) Sanitation: – Latrines – Chlorination 1. 3 parts/mil n n Proper hygiene Vaccination when appropriate Minimize contacts with infected persons. Health education of the public
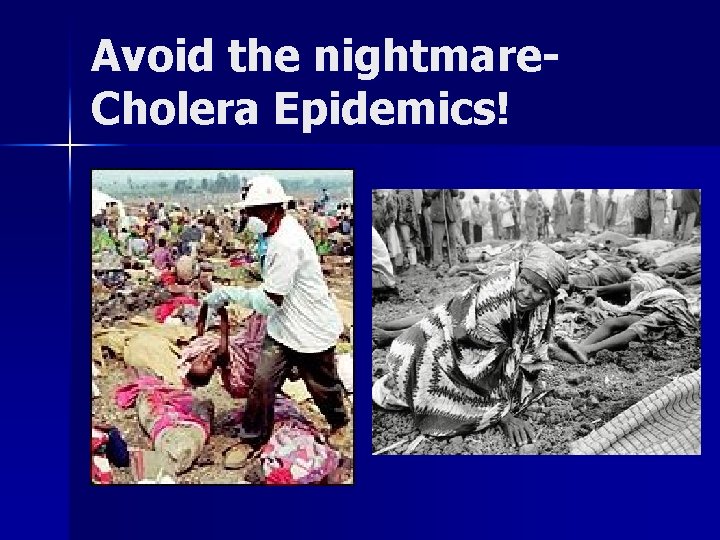
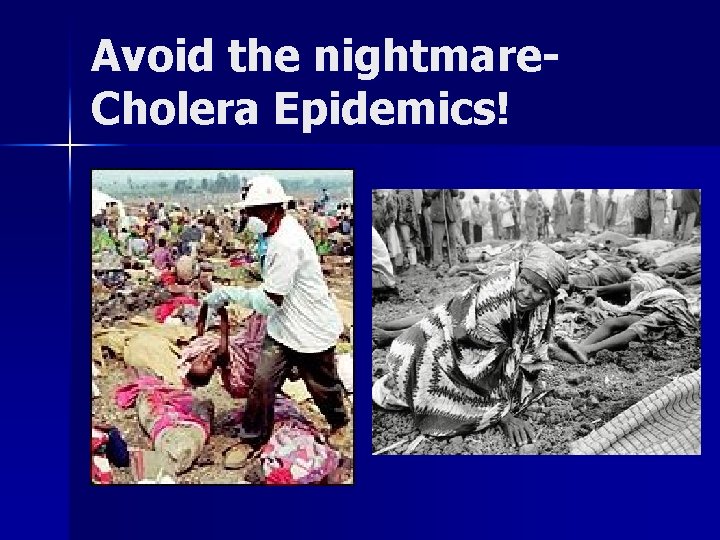
Avoid the nightmare. Cholera Epidemics!

Typhoid Fever The Enteric Fevers!
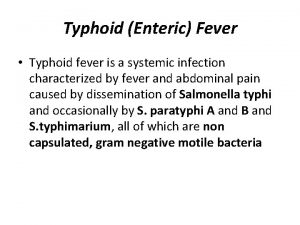
The Scope of the Problem Rare in industrialized nations-70% from international travelers. n In the 3 rd world; 17 million cases annually with >600, 000 deaths. n Without treatment typhoid lasts 3 -4 wks with death rate of 12 -30%. n
Transmission n Caused by bacteria Salmonella typhi – Lives only in bloodstream & GI tract of humans who are ill or chronic carriers. n Spread by: – Drinking & eating fecally contaminated water & food. – Chronic carrier handling food without proper hand washing. – Washing food or bathing in contaminated water
Signs & symptoms: n n n n Fever (103 -104 F) with slow pulse & chills Weak, fatigue, malaise, & headache Stomach pain & loss of appetite Rash with flat, rose-colored spots. Constipation (diarrhea is uncommon) & vomiting usually not severe. Confusion & delirium. Possible intestinal perforation
Treatment n Antibiotics: – Cipro, Chloramphenicol, Amoxicillin or Sulfa Usually feel better in 2 -3 days & death rarely occurs with treatment. n Relapse occurs in 10 -20% of patients. n Observe carefully for GI hemorrhage or perforation (peritonitis). n
Prevention n Avoid risky food & water. – “Boil it, cook it, peel it or forget it” Careful hand washing n Proper sanitation (latrines) n Vaccination: n – Typhoid immunization good for 2 -3 yrs.

Dengue Fever Break-bone fever
Key facts re Dengue is a mosquito borne viral infection. n About ½ the world’s population is at risk; 50 -100 million cases/year. n It is found mostly in tropical & subtropical climates n Often referred to as “Break-bone Fever” n
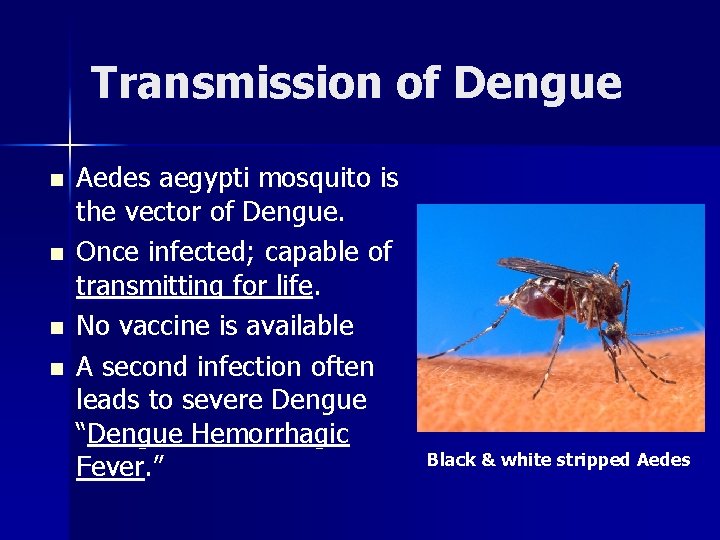
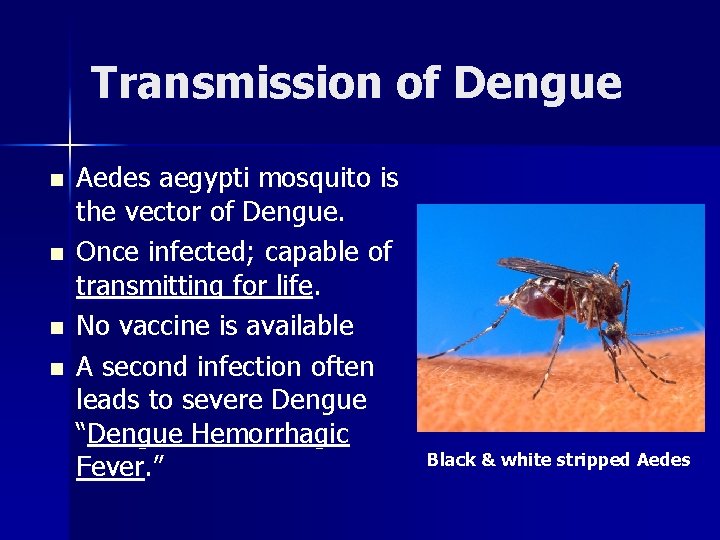
Transmission of Dengue n n Aedes aegypti mosquito is the vector of Dengue. Once infected; capable of transmitting for life. No vaccine is available A second infection often leads to severe Dengue “Dengue Hemorrhagic Fever. ” Black & white stripped Aedes
Signs & Symptoms Abrupt onset of high fever with chills, severe H. A. & pain behind the eyes n Severe muscle & joint pain, N/V & swollen lymph nodes. n Rash on 3 rd to 5 th day starting on trunk and moving to extremities. n May progress to life threatening Dengue Hemorrhagic fever with bleeding. n
Treatment & prevention n There is no specific treatment n Mosquito control measures-daytime bitter – Getting rid of standing water – Use of insect repellants – Use of screens on windows when possible
GUINEA WORM! Still a crippling disease world wide

Areas where Guinea Worm is found:
Guinea Worm! Caused by a nematode n Is crippling but usually not fatal. n Worm does not live in the gut but under the skin. n Worm may grow up to 2 feet long. n

Signs & Symptoms n n Painful swelling develops, usually on lower extremities (worm infl) Painful blister develops due to irritating fluid secreted by worm. May see or feel worm under skin. Can become secondarily infected & occasionally develops tetanus.
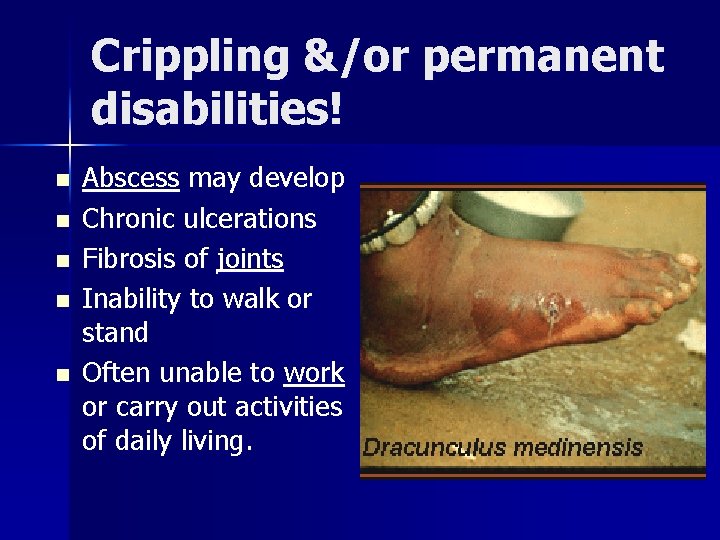
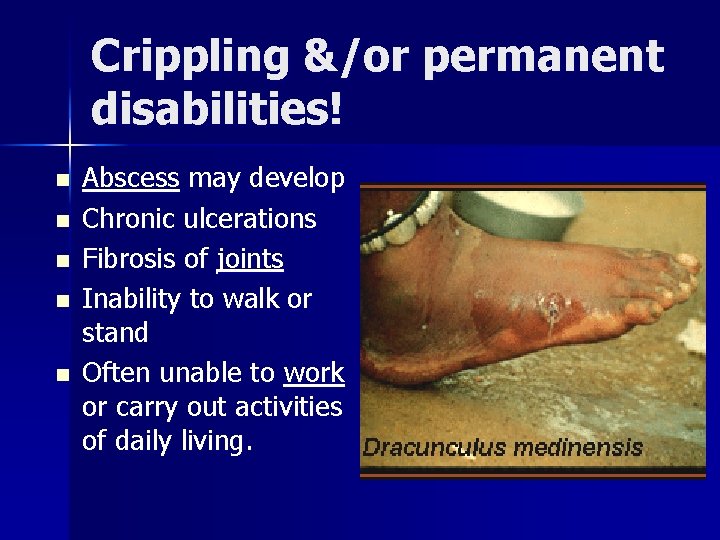
Crippling &/or permanent disabilities! n n n Abscess may develop Chronic ulcerations Fibrosis of joints Inability to walk or stand Often unable to work or carry out activities of daily living.
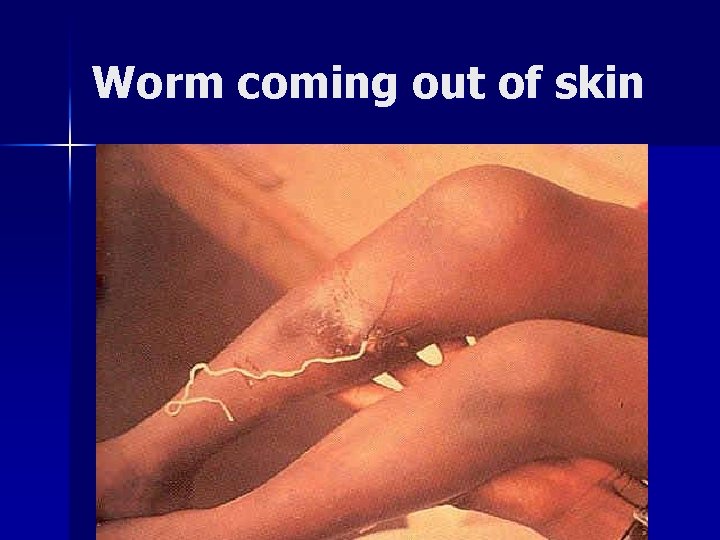
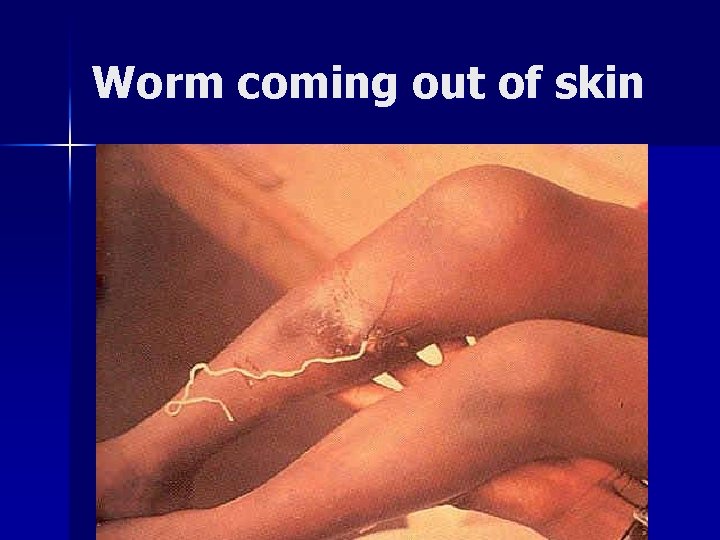
Worm coming out of skin
Transmission n n n Infected person with open sore, wades into water & worm discharges thousands of eggs into water. Tiny “water-fleas”/cyclops (prawns) eat larva. Person drinks water with water flea Stomach acid kills flea & releases larva Eggs slowly develop in connective tissue After 1 yr, worm ready to discharge larva.


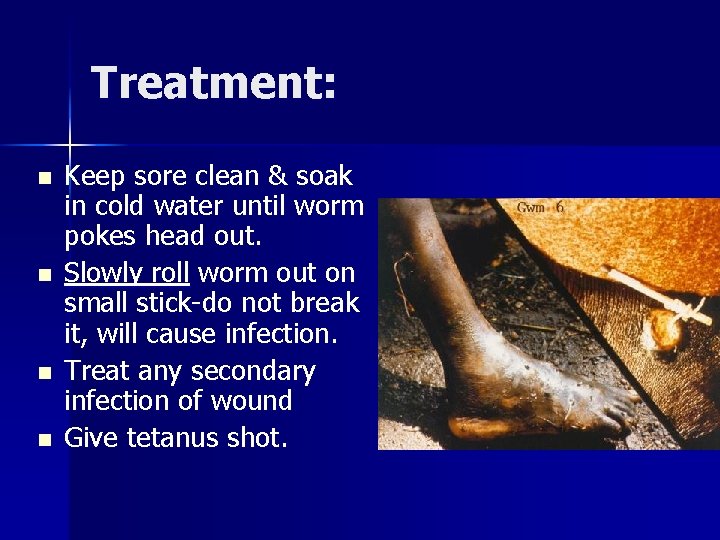
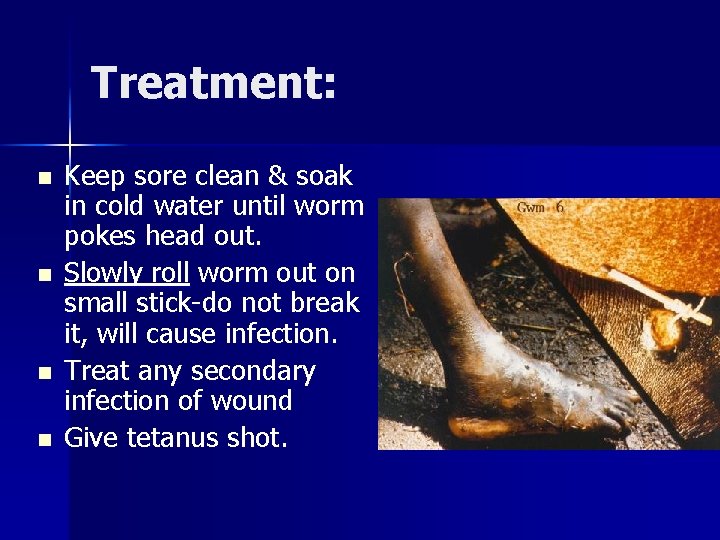
Treatment: n n Keep sore clean & soak in cold water until worm pokes head out. Slowly roll worm out on small stick-do not break it, will cause infection. Treat any secondary infection of wound Give tetanus shot.
Prevention n Filter water thru clean cloth to remove “waterfleas”. Protect water source so people will not have to wade into water. If possible, purify the water
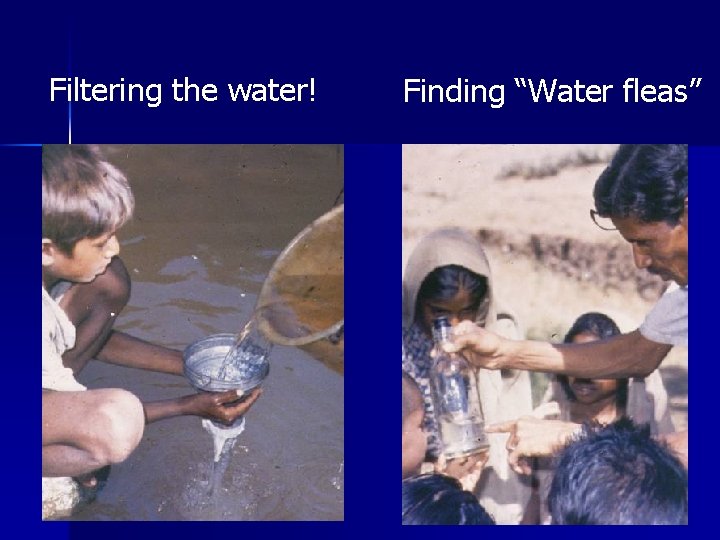
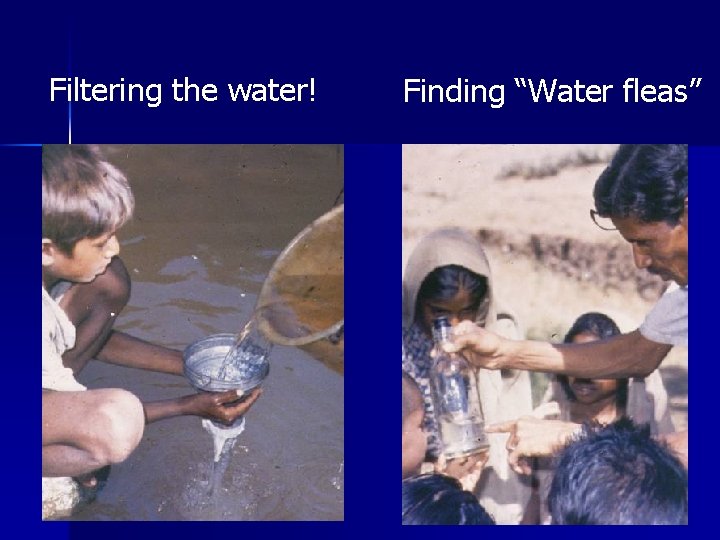
Filtering the water! Finding “Water fleas”

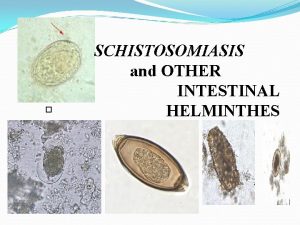
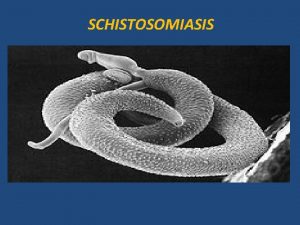
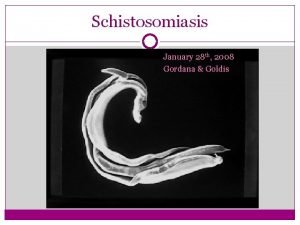
Schistosomiasis Bilharzia Blood Fluke
Schistosomiasis-Bilharzia (Schistosome Hematobium) Next to Malaria, is the most wide spread parasitic infestation of man n ~200 million people are affected n In endemic areas may find egg output of 800 eggs/10 ml of urine. n
Three species n S. hematobium (Urinary Schisto) – Most problematic S. mansoni diarrhea & blood in stools n S. japonicum in orient n
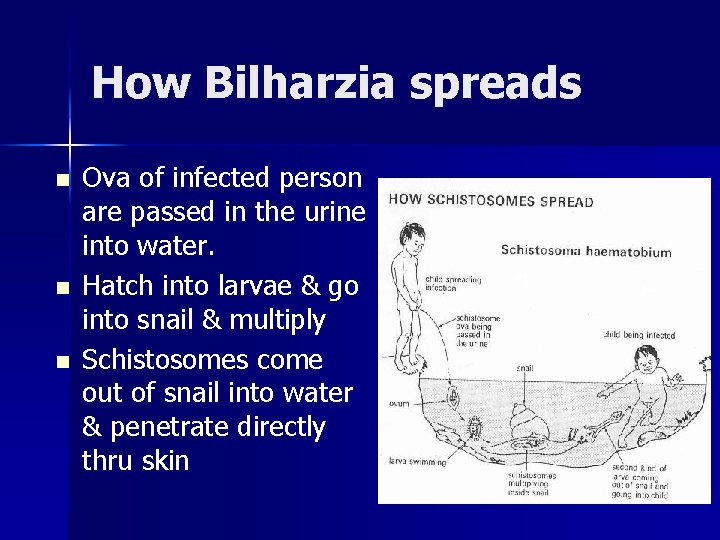
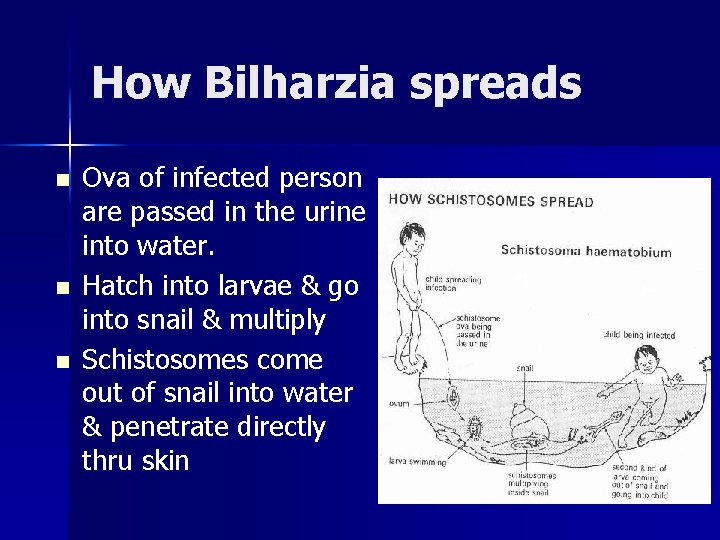
How Bilharzia spreads n n n Ova of infected person are passed in the urine into water. Hatch into larvae & go into snail & multiply Schistosomes come out of snail into water & penetrate directly thru skin
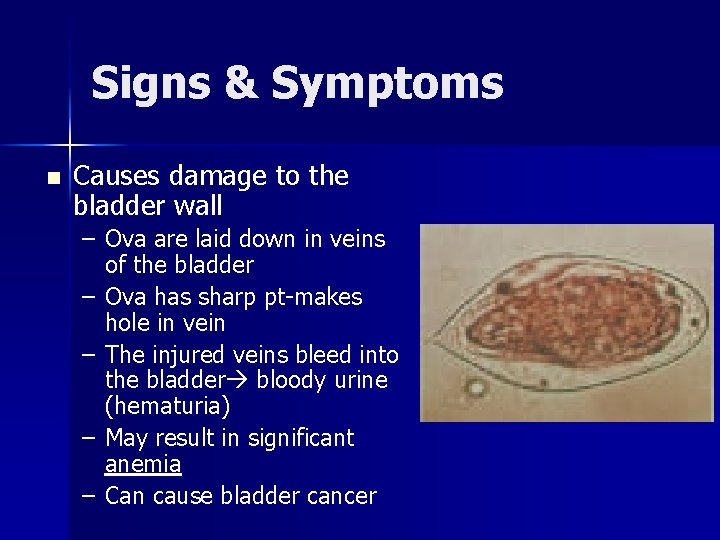
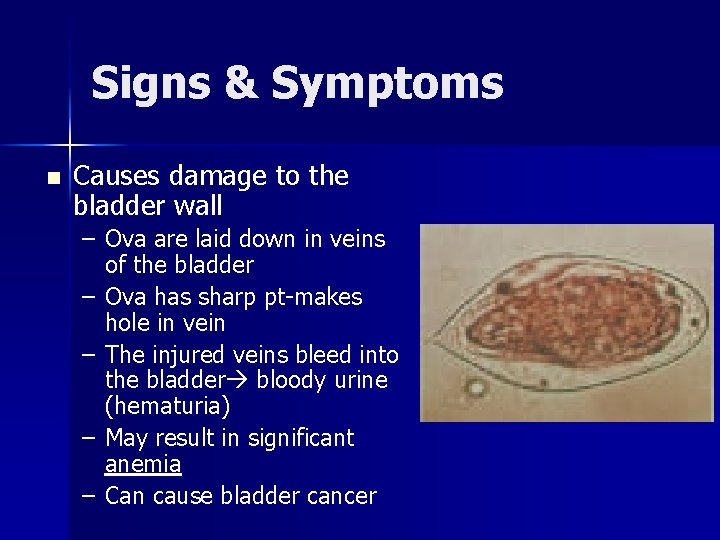
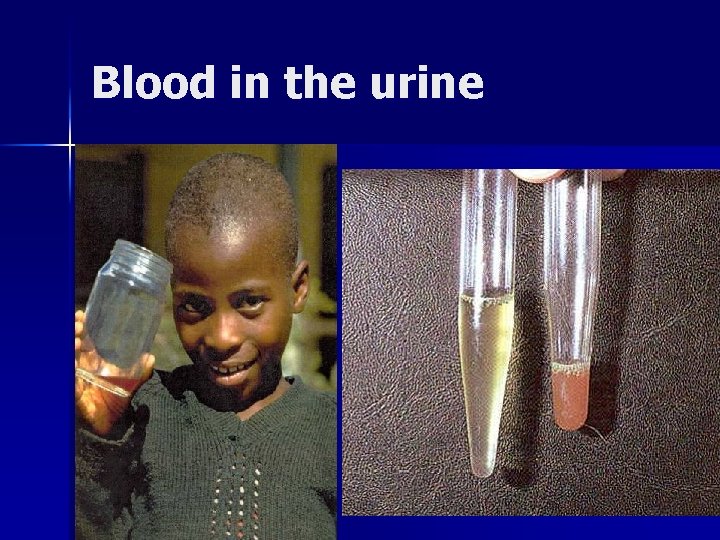
Signs & Symptoms n Causes damage to the bladder wall – Ova are laid down in veins of the bladder – Ova has sharp pt-makes hole in vein – The injured veins bleed into the bladder bloody urine (hematuria) – May result in significant anemia – Can cause bladder cancer

Swimmer’s Itch
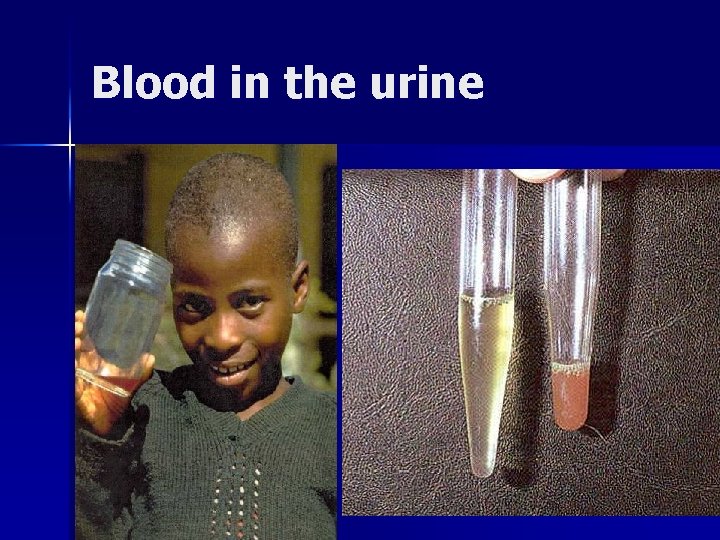
Blood in the urine
Prevention & Treatment Avoid fresh water that may be contaminated (Lake Victoria) n Avoid urinating or defecating near water sources. n Protect the water source n Treatment: n – Praziquantel (40 mg/kg/day in 2 doses)
Loaisis: Loa Only found in equatorial rain forest of Central & West Africa n Caused by filarial worm Loa loa. n Spread by a biting fly n The adult worms cause the symptoms & not the microfilaria. n
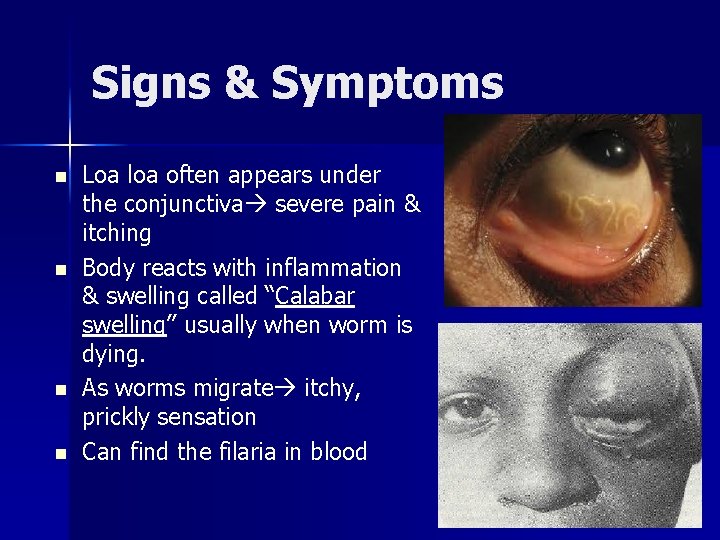
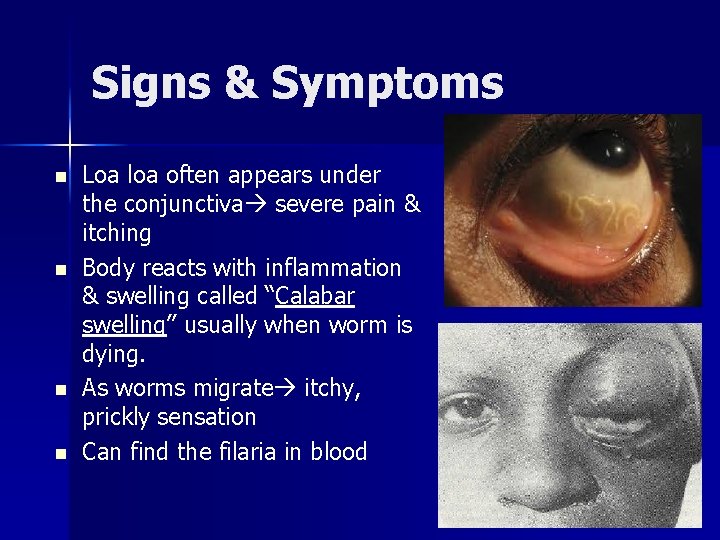
Signs & Symptoms n n Loa loa often appears under the conjunctiva severe pain & itching Body reacts with inflammation & swelling called “Calabar swelling” usually when worm is dying. As worms migrate itchy, prickly sensation Can find the filaria in blood
Ebola Hemorrhagic Fever The “Hot Zone”! (Level 4 virus)
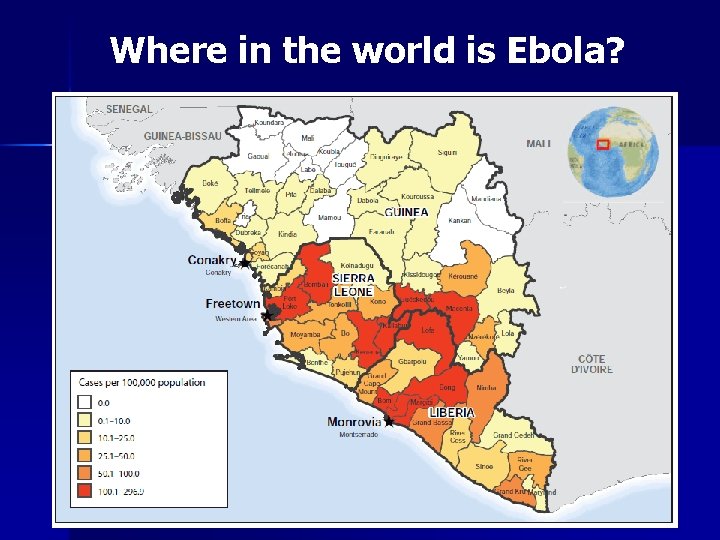
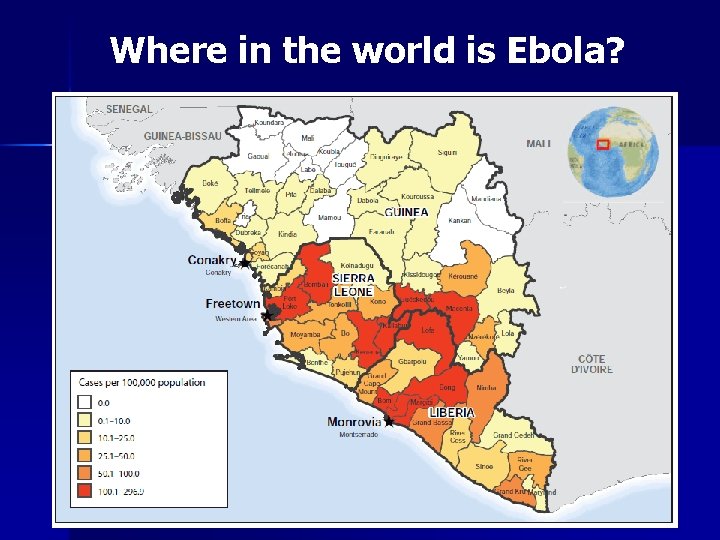
Where in the world is Ebola?
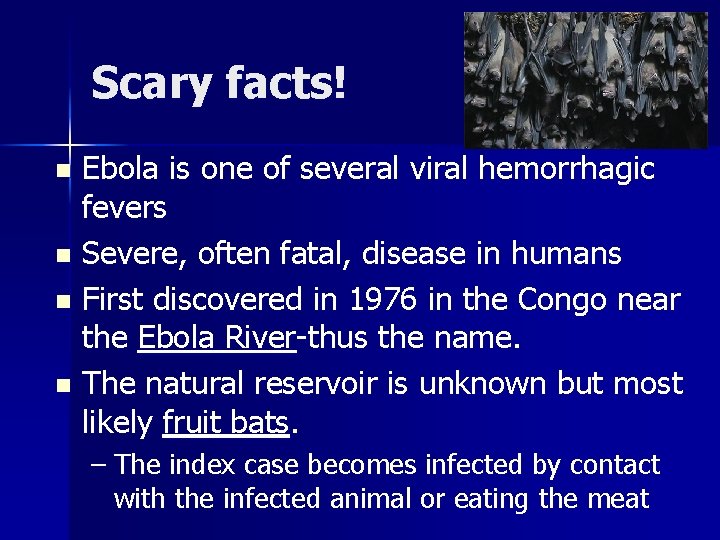
Scary facts! Ebola is one of several viral hemorrhagic fevers n Severe, often fatal, disease in humans n First discovered in 1976 in the Congo near the Ebola River-thus the name. n The natural reservoir is unknown but most likely fruit bats. n – The index case becomes infected by contact with the infected animal or eating the meat
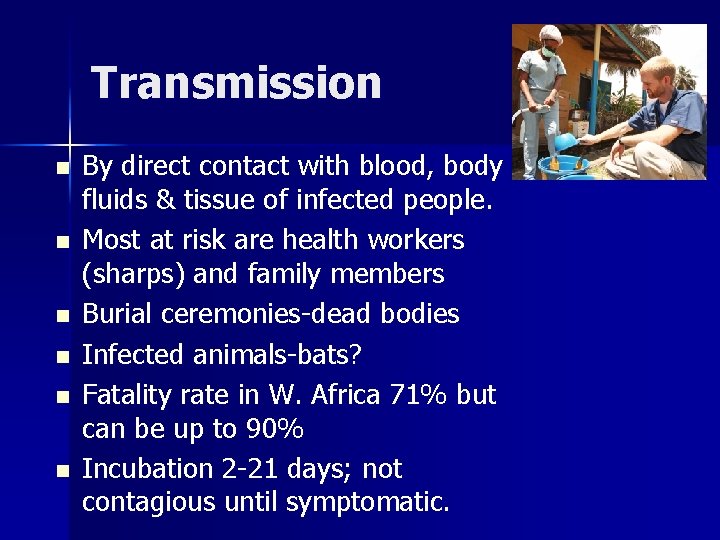
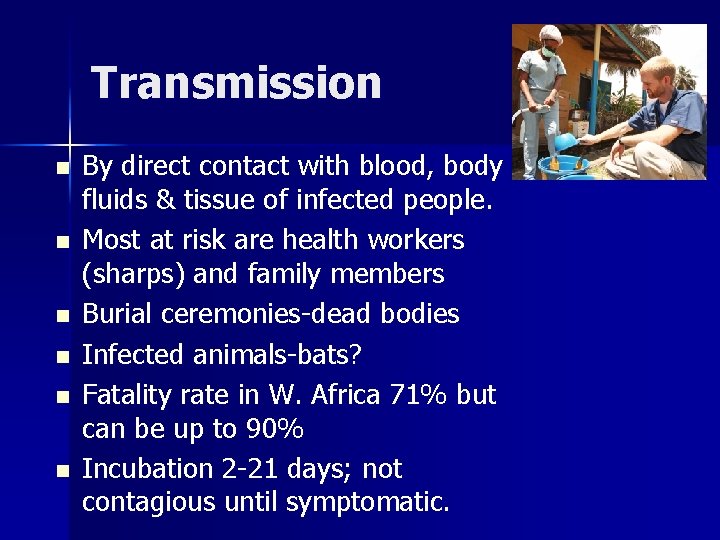
Transmission n n n By direct contact with blood, body fluids & tissue of infected people. Most at risk are health workers (sharps) and family members Burial ceremonies-dead bodies Infected animals-bats? Fatality rate in W. Africa 71% but can be up to 90% Incubation 2 -21 days; not contagious until symptomatic.
Signs & Symptoms Initially non-specific: sudden onset of fever >101, chills, HA & malaise n Progress to GI with severe watery diarrhea with N/V & abdominal pain n Most common reported s/s n – Fever – Fatigue – Vomiting - diarrhea - loss of appetite
Signs & Symptoms Hemorrhage not universally presentpetechiae, bruising or oozing of blood. n Additional s/s: chest pain, SOB, seizures & cerebral edema. n May cause: n – Impaired kidney & liver function – Internal and external bleeding – Multiple organ failure
Treatment: n n n No specific treatment available (experimental vaccine Zmapp) Intensive supportive care with fluid replacement -IV & blood. Treat any complicating bacterial infection Very strict, level 4 isolation Education of the public is key
 More more more i want more more more more we praise you
More more more i want more more more more we praise you More more more i want more more more more we praise you
More more more i want more more more more we praise you Schistosomiasis
Schistosomiasis Schistosomiasis
Schistosomiasis Hematouria
Hematouria Schistosoma eggs
Schistosoma eggs Amal mitra
Amal mitra Cholera outbreak malaysia
Cholera outbreak malaysia Cholera
Cholera Cholera toxin
Cholera toxin Cholera
Cholera Stool analysis
Stool analysis Severe dehydration
Severe dehydration Cholera
Cholera Distribution in epidemiology
Distribution in epidemiology Epidemiological triad of typhoid fever
Epidemiological triad of typhoid fever Cholera classification
Cholera classification Cholera is a greek word that means gutter of roof
Cholera is a greek word that means gutter of roof Solve the baltimore cholera mystery puzzle
Solve the baltimore cholera mystery puzzle Cholera
Cholera Introduction of typhoid fever
Introduction of typhoid fever Epidemiological triad of typhoid fever
Epidemiological triad of typhoid fever Typhoid medicine course
Typhoid medicine course Typhoid fever
Typhoid fever Typhoid
Typhoid Typhoid fever
Typhoid fever Laboratory diagnosis of typhoid fever
Laboratory diagnosis of typhoid fever Typhoid fever
Typhoid fever Salwa touma
Salwa touma Typhosin
Typhosin Intestine
Intestine Nursing care plan for typhoid fever slideshare
Nursing care plan for typhoid fever slideshare Typhoid stages
Typhoid stages Specific volume is an abstract number
Specific volume is an abstract number Calculate weight using specific gravity and volume
Calculate weight using specific gravity and volume I think you should be more specific here in step two
I think you should be more specific here in step two Specific details examples
Specific details examples Knowing more remembering more
Knowing more remembering more The more you study the more you learn
The more you study the more you learn The more i give to thee the more i have
The more i give to thee the more i have Aspire not to
Aspire not to More choices more chances
More choices more chances Examples of newton's first law
Examples of newton's first law Human history becomes more and more a race
Human history becomes more and more a race 5 apples in a basket riddle
5 apples in a basket riddle Minerals sources functions and deficiency chart
Minerals sources functions and deficiency chart 10 diseases of lymphatic system
10 diseases of lymphatic system Non communicable diseases infographic
Non communicable diseases infographic Retention hyperkeratosis dermnet
Retention hyperkeratosis dermnet Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Microbes
Microbes Inflammation of mfa ppt
Inflammation of mfa ppt Sphyx medical term
Sphyx medical term Chapter 23 lesson 1 understanding communicable diseases
Chapter 23 lesson 1 understanding communicable diseases Std
Std Myth and fallacies about non-communicable diseases
Myth and fallacies about non-communicable diseases Nutritional diseases
Nutritional diseases King of diseases
King of diseases