Revision arthroplasty around the hip and the knee
















- Slides: 57
Revision arthroplasty around the hip and the knee Small group discussion 2 Hip and knee cases Periprosthetic Fracture Management Curriculum events 2020
Learning objectives for the cases • • Classify the fracture Describe the options and indications for nonoperative, fixation, and revision treatment Select an appropriate treatment Identify and address potential complications
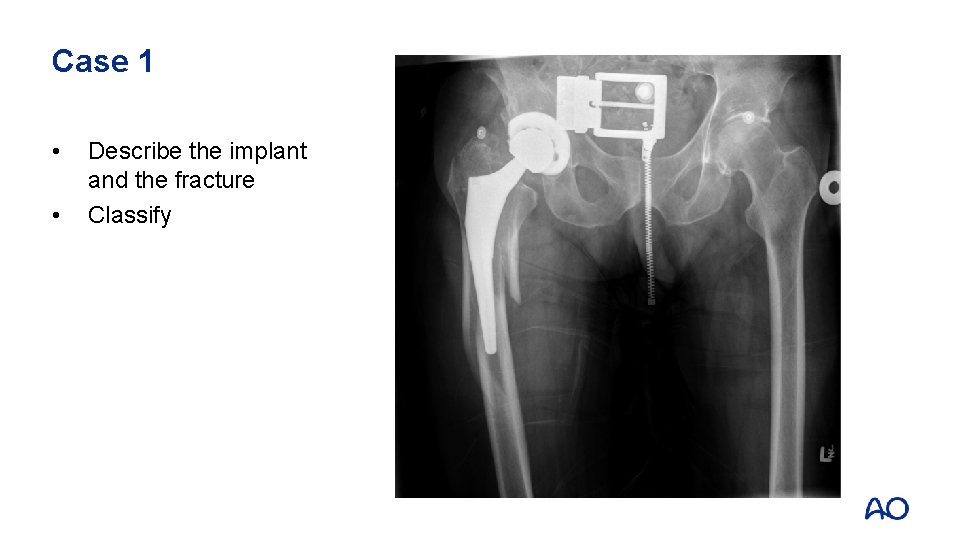
Case 1: Case description • • 78 -year-old Cementless total hip replacement 6 weeks ago Fell at home Severe pain—was unable to get it up
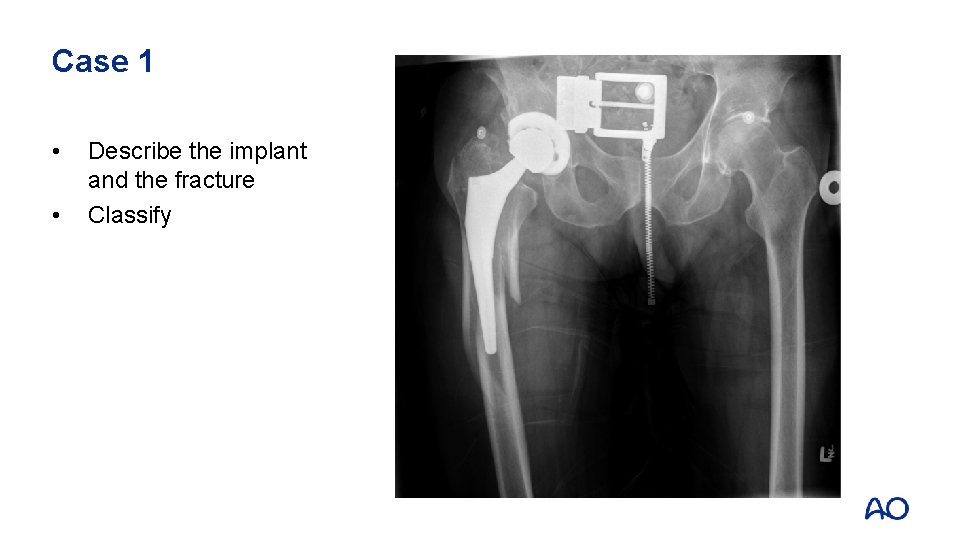
Case 1 • • Describe the implant and the fracture Classify

Case 1 • • Cup is well fixed Stem is loose Fracture extends into greater trochanter (B 2) Distal diaphysis intact
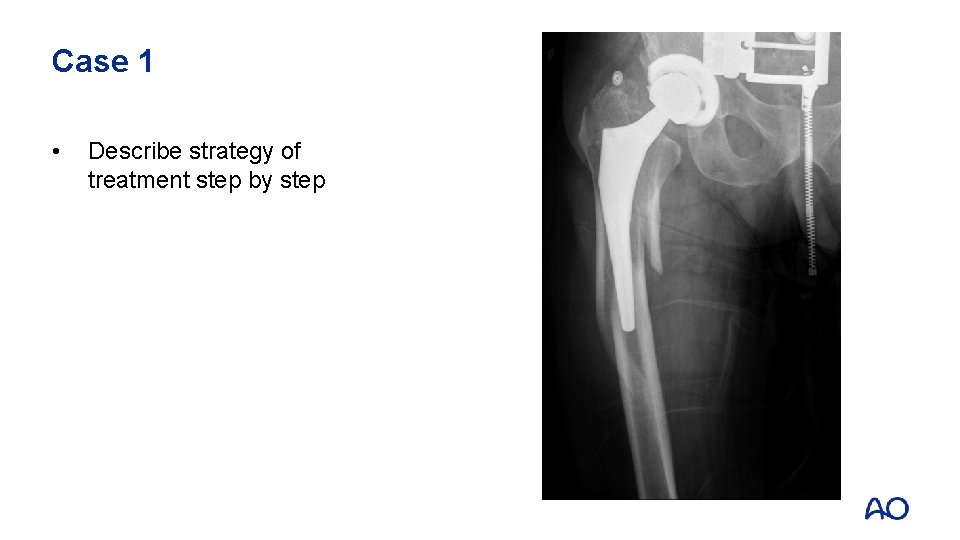
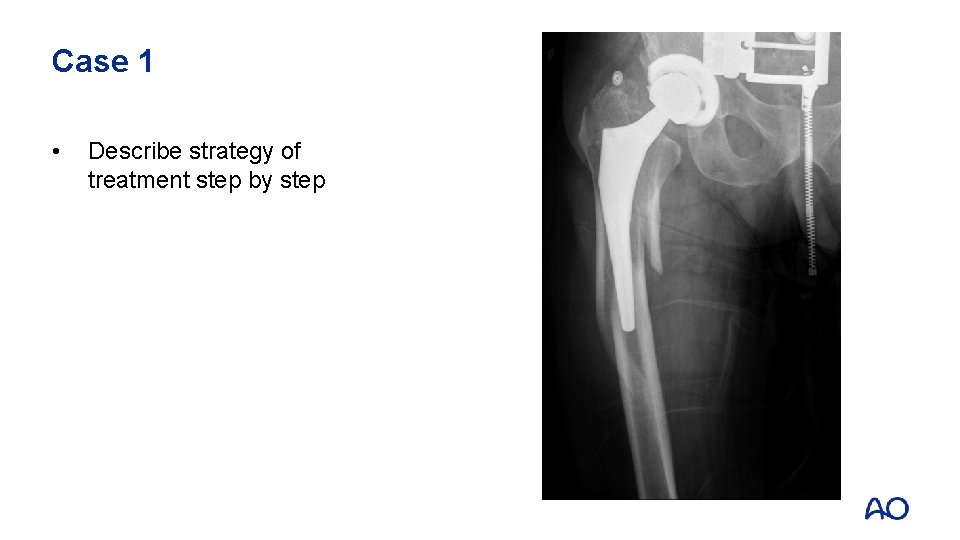
Case 1 • Describe strategy of treatment step by step
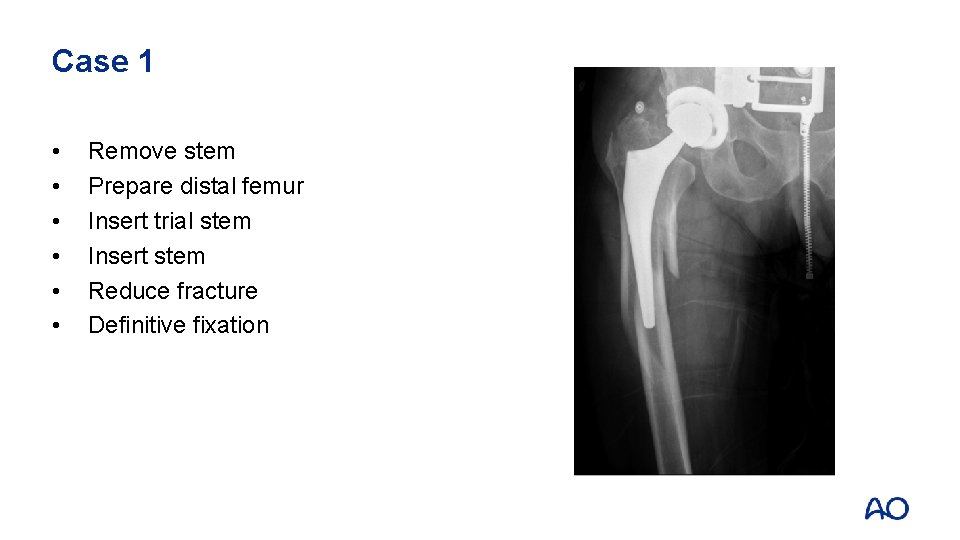
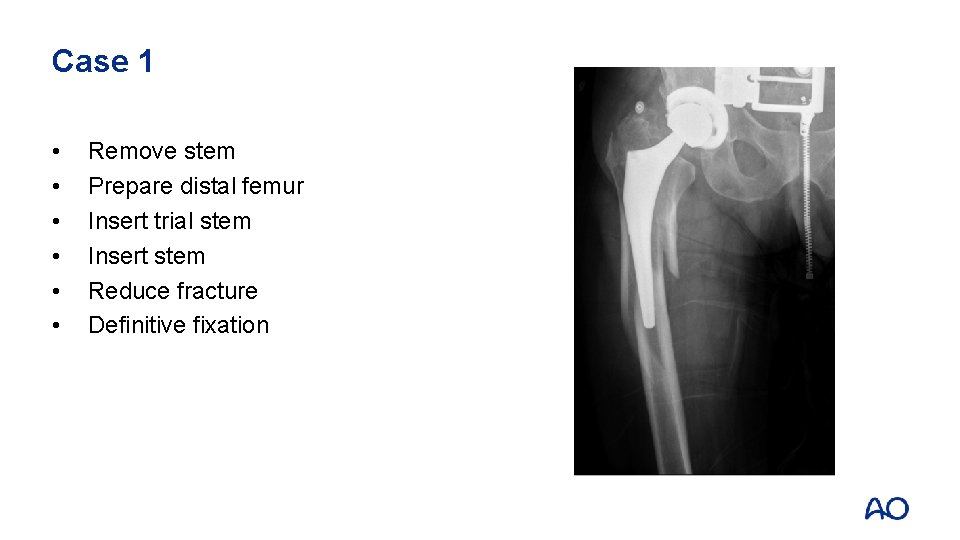
Case 1 • • • Remove stem Prepare distal femur Insert trial stem Insert stem Reduce fracture Definitive fixation
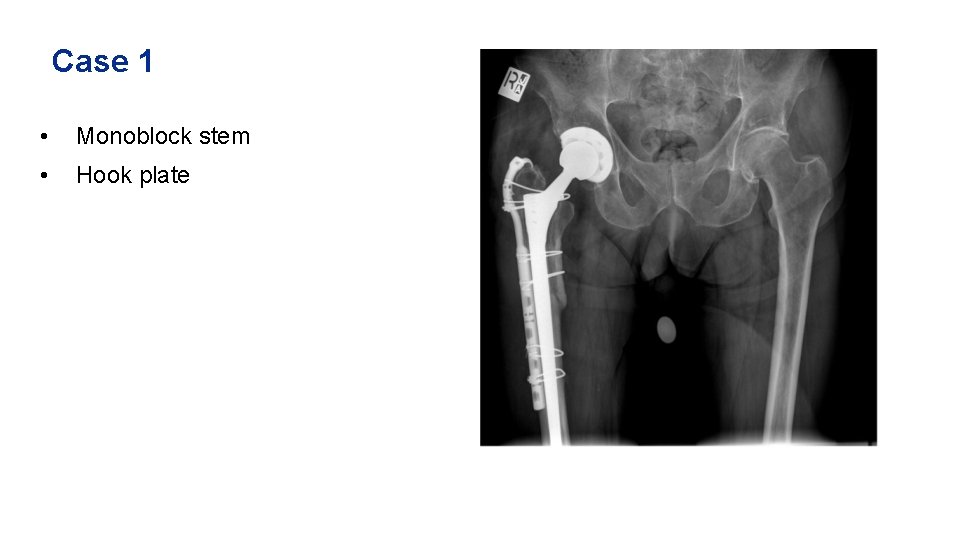
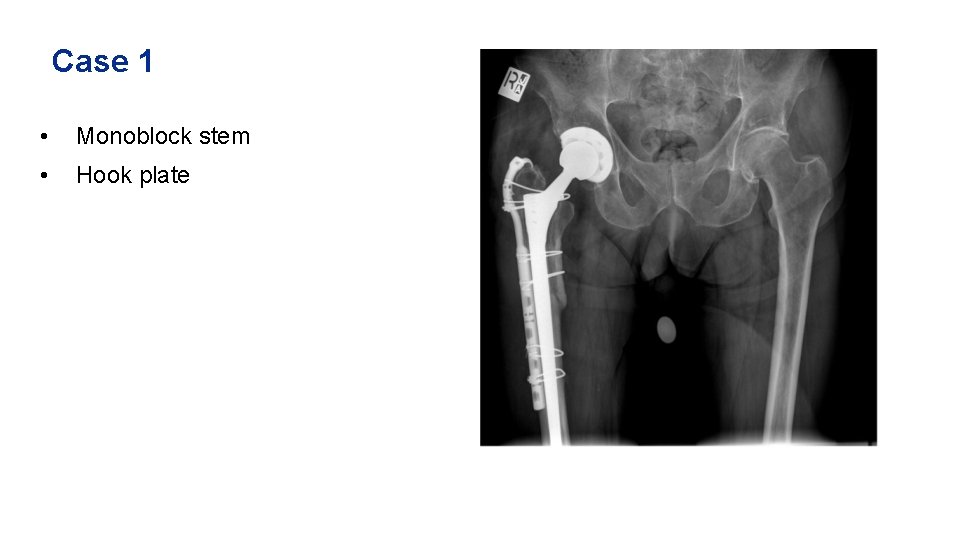
Case 1 • Monoblock stem • Hook plate
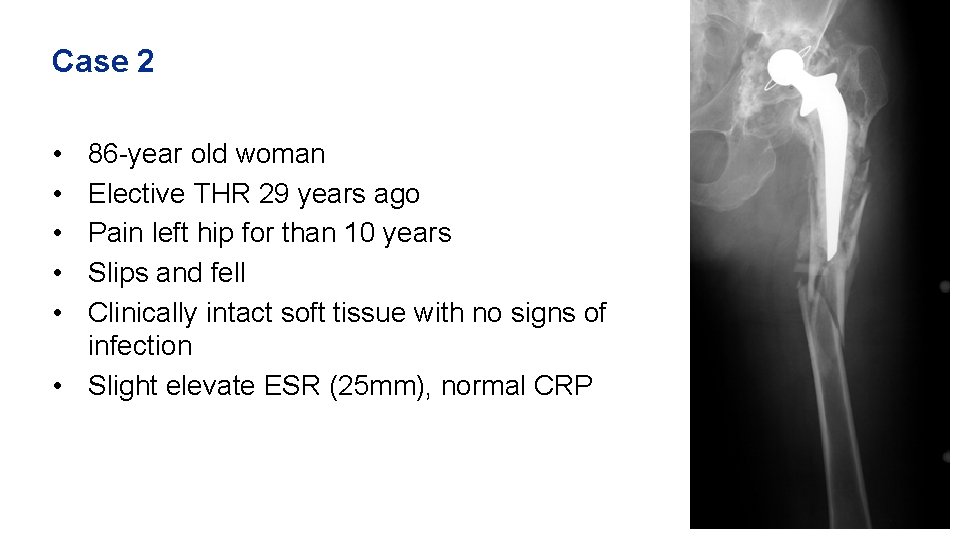
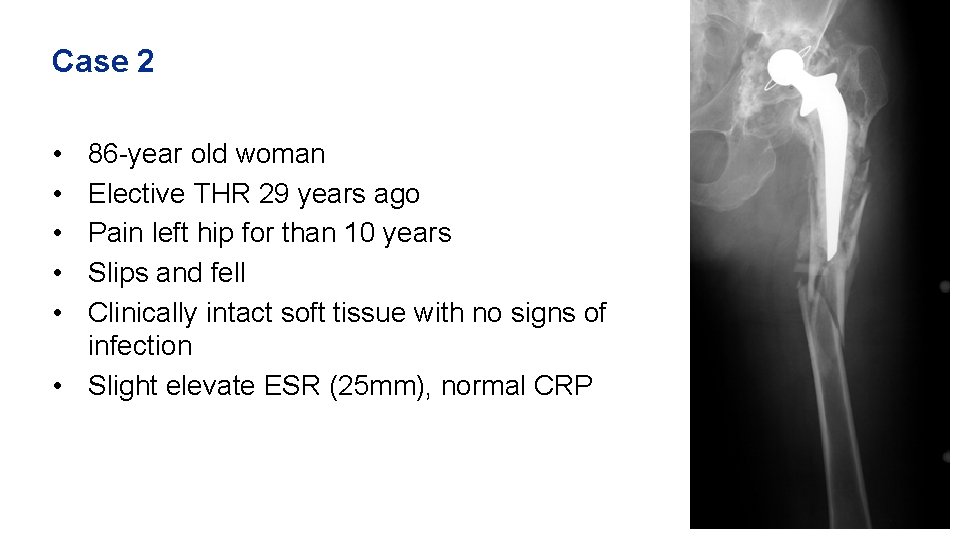
Case 2 • • • 86 -year old woman Elective THR 29 years ago Pain left hip for than 10 years Slips and fell Clinically intact soft tissue with no signs of infection • Slight elevate ESR (25 mm), normal CRP
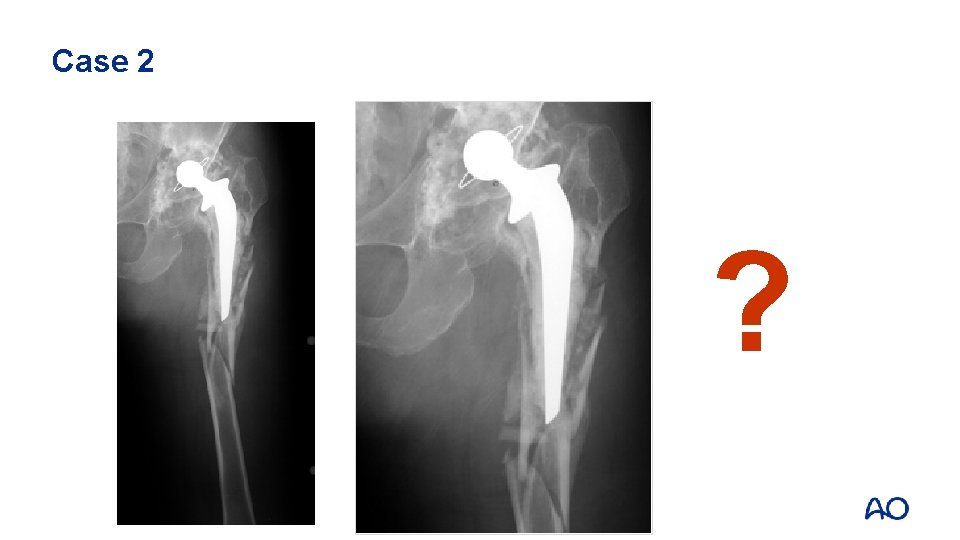
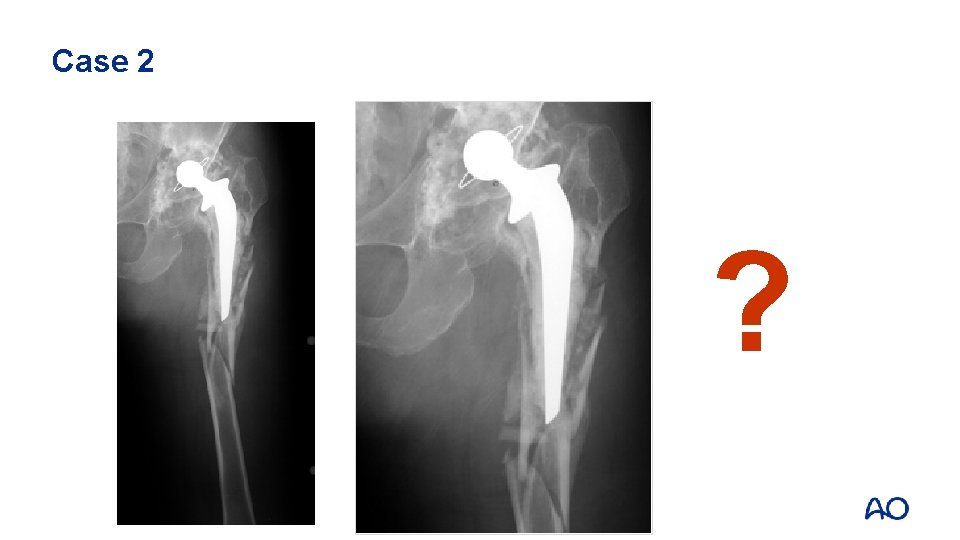
Fracturepatternfx fxof ofshaftfixationand anddesign Case 62 months post # fixation Case 10 5 4 2 ?
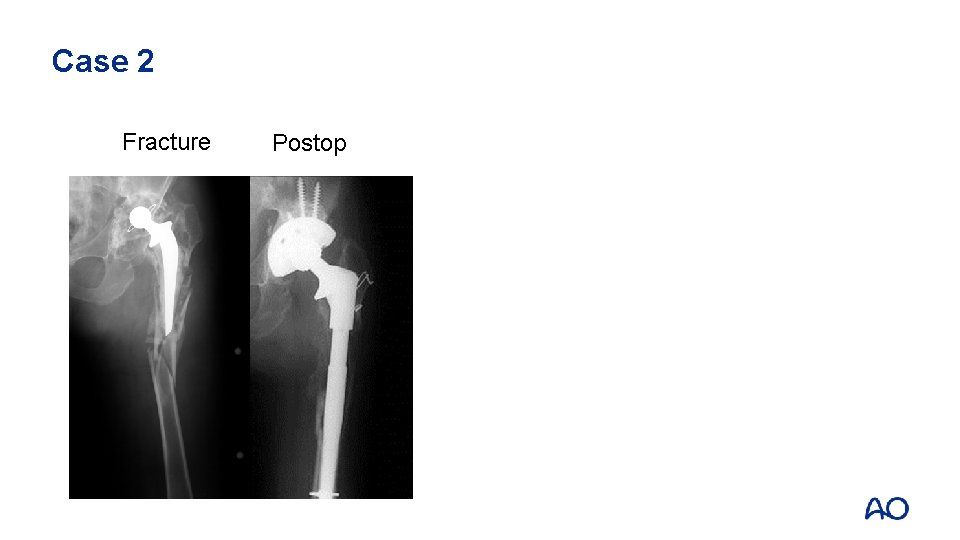
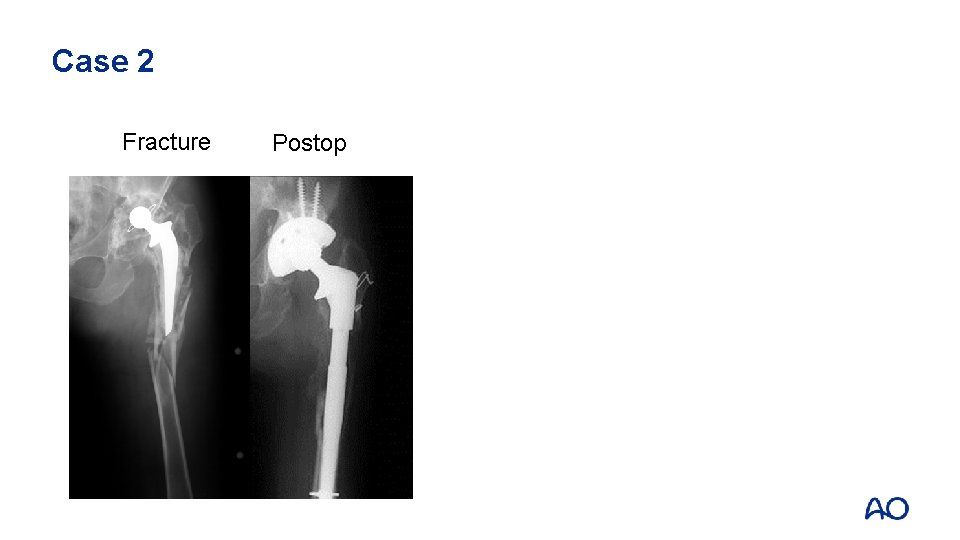
Fracturepatternfx fxof ofshaftfixationand anddesign Case 2 Fracture Case 10 5 4 2 Postop
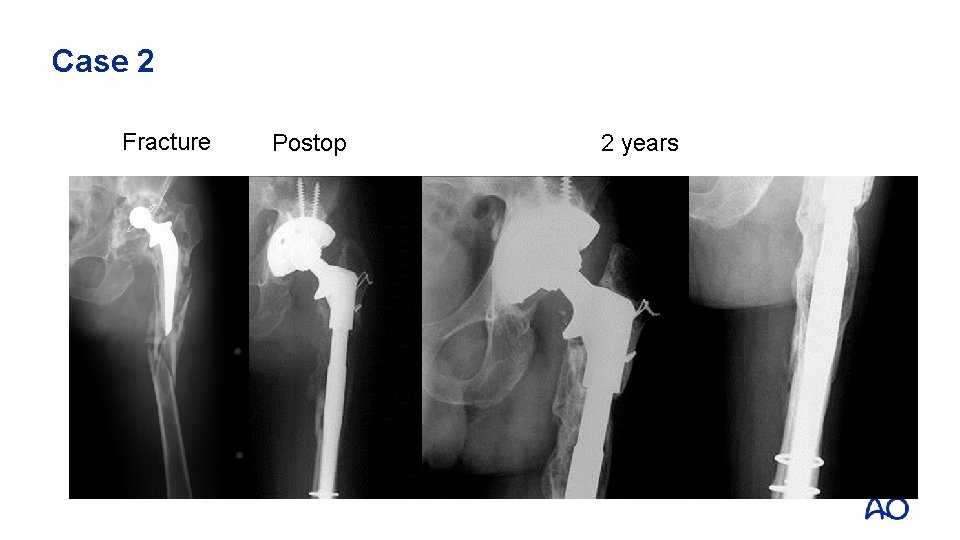
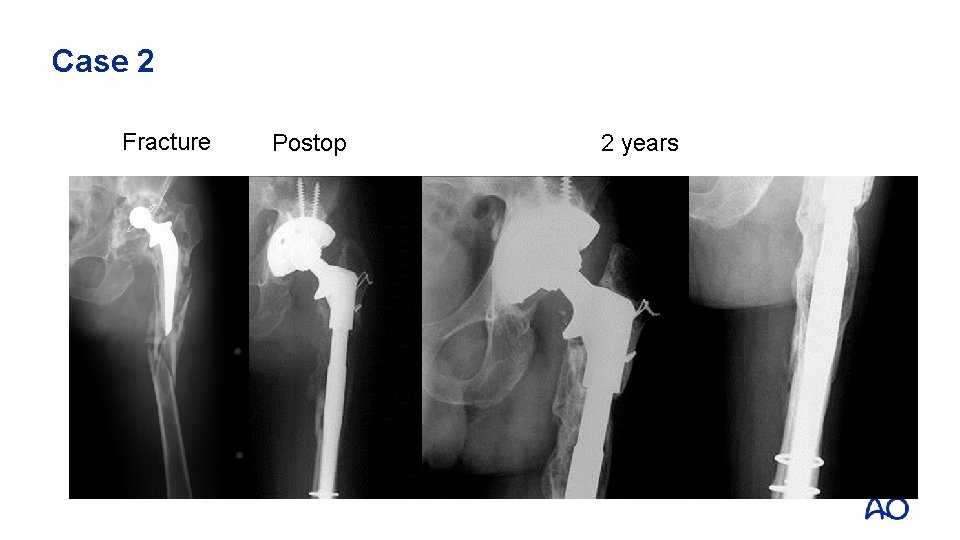
Fracturepatternfx fxof ofshaftfixationand anddesign Case 2 Fracture Case 10 5 4 2 Postop 2 years
Case 2: Take-home messages • • • Remove all the cement Complex fracture can heal (bone formation) Be ready to revise the cup when necessary
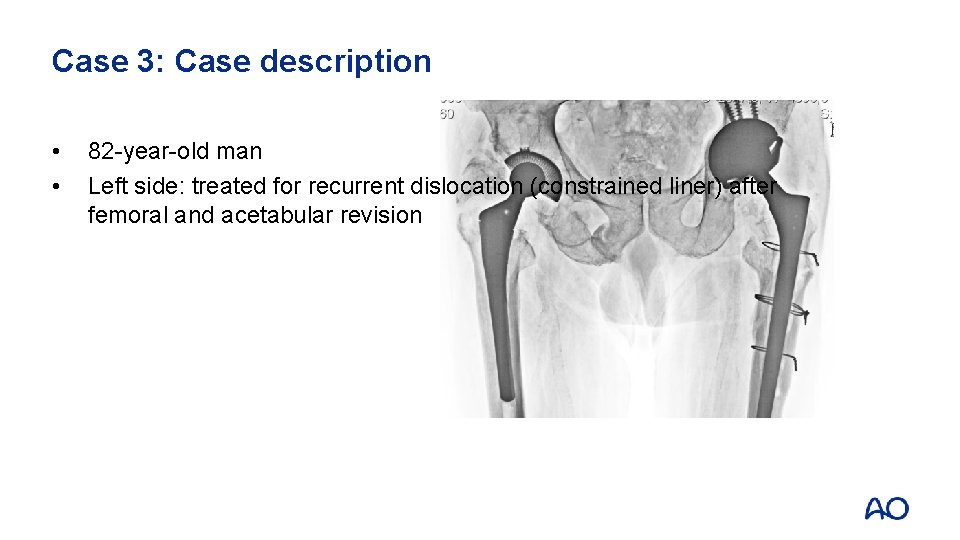
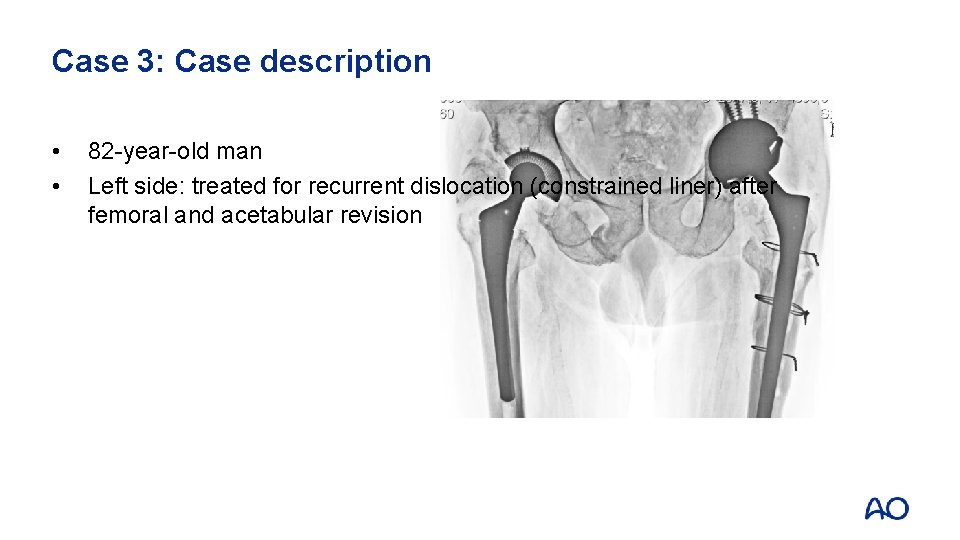
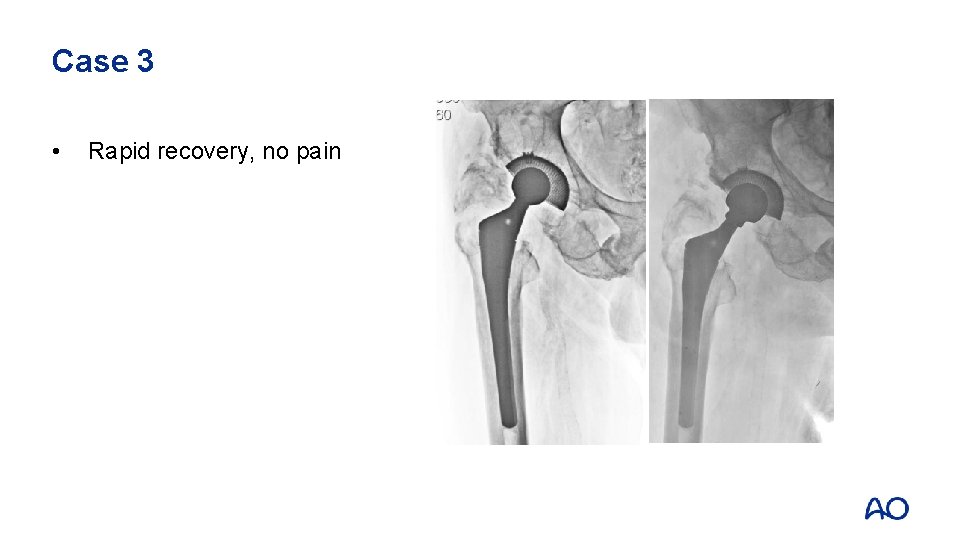
Case 3: Case description • • 82 -year-old man Left side: treated for recurrent dislocation (constrained liner) after femoral and acetabular revision
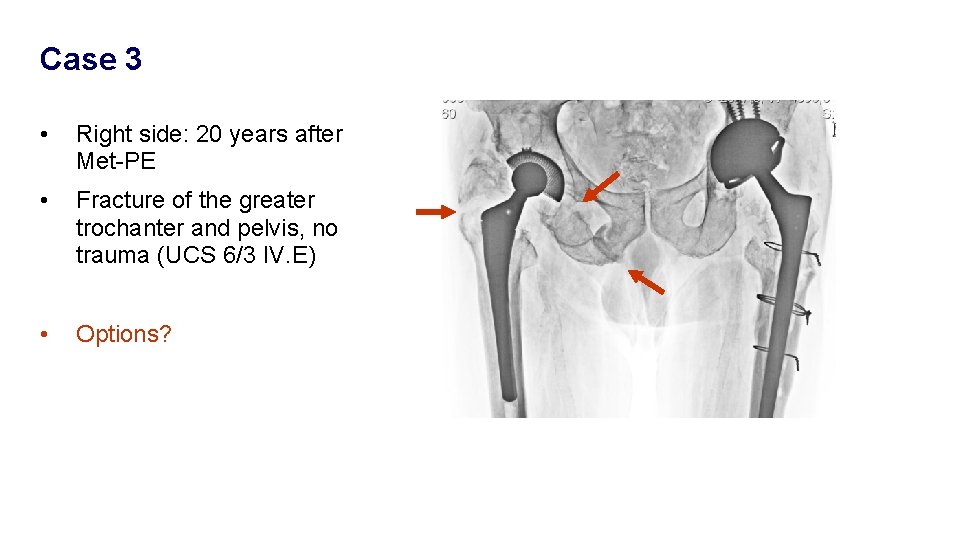
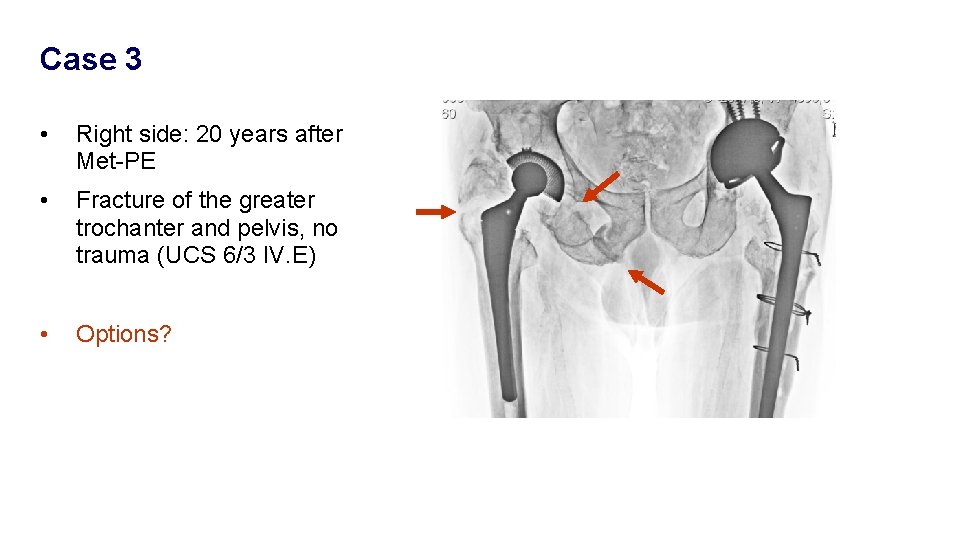
Case 3 • Right side: 20 years after Met-PE • Fracture of the greater trochanter and pelvis, no trauma (UCS 6/3 IV. E) • Options?
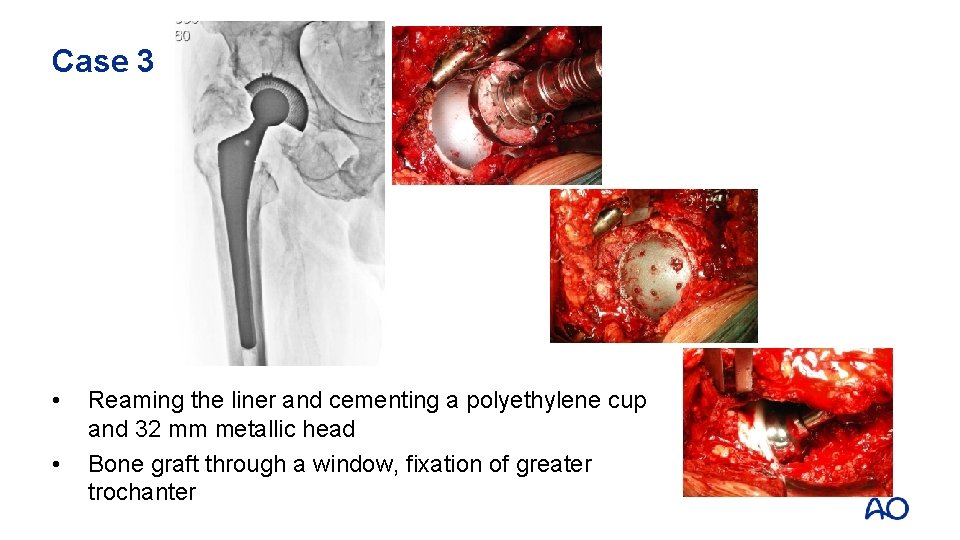
Case 3 • • Reaming the liner and cementing a polyethylene cup and 32 mm metallic head Bone graft through a window, fixation of greater trochanter
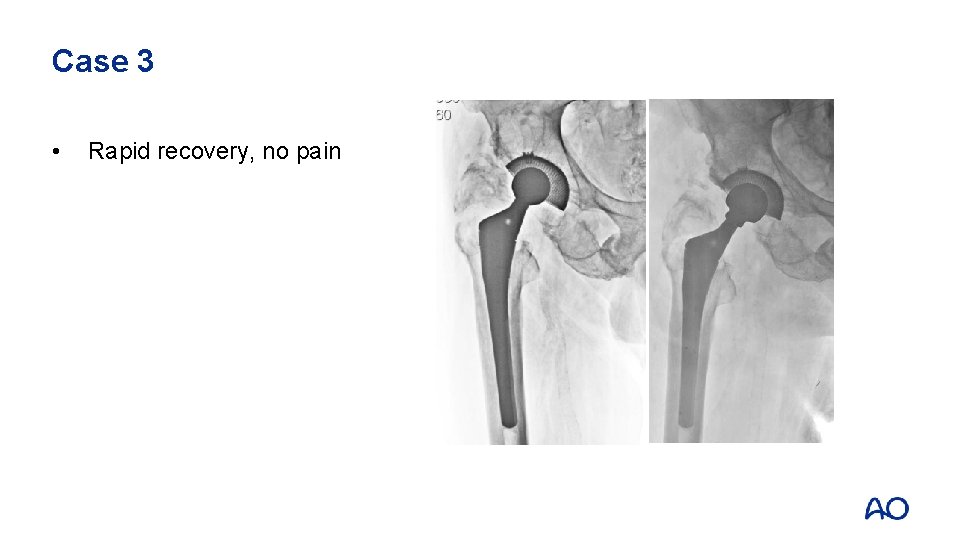
Case 3 • Rapid recovery, no pain
Case 3: Take-home messages • • • Be careful with complications in older population Avoid major surgery if not necessary Improve tribology and materials according to functional requests of the patient
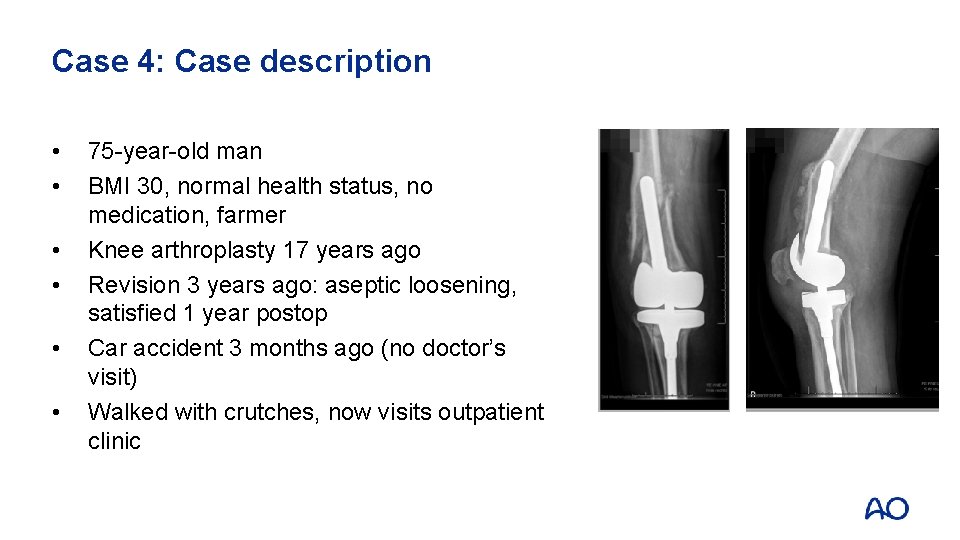
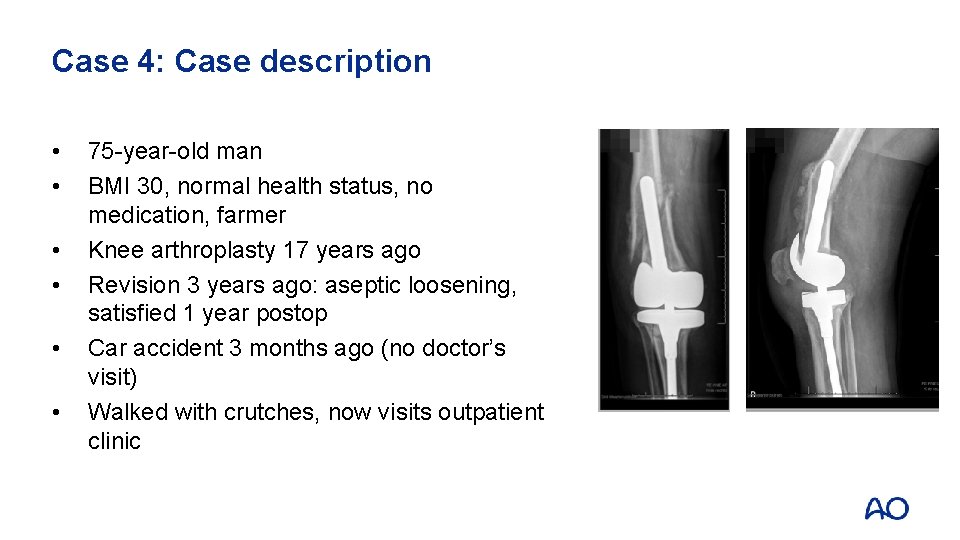
Case 4: Case description • • • 75 -year-old man BMI 30, normal health status, no medication, farmer Knee arthroplasty 17 years ago Revision 3 years ago: aseptic loosening, satisfied 1 year postop Car accident 3 months ago (no doctor’s visit) Walked with crutches, now visits outpatient clinic

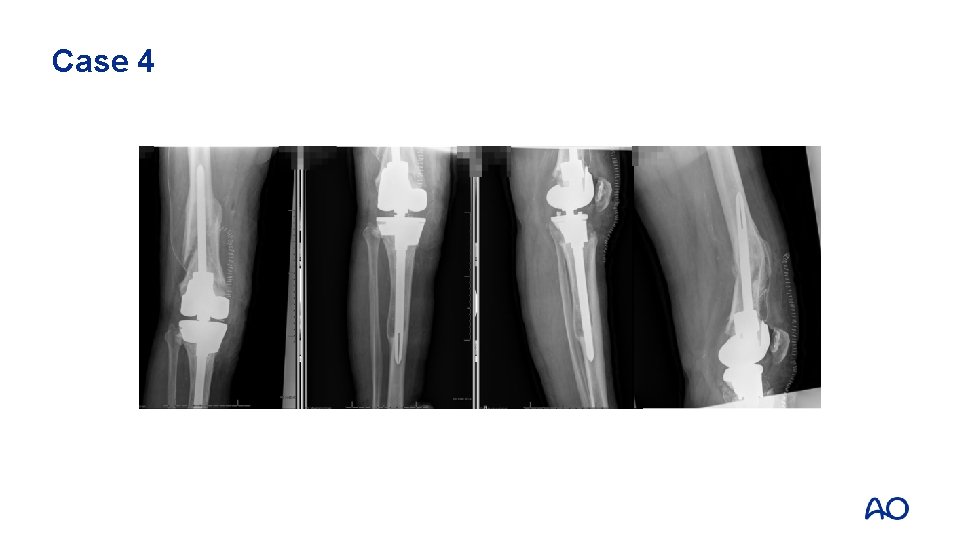
Case 4
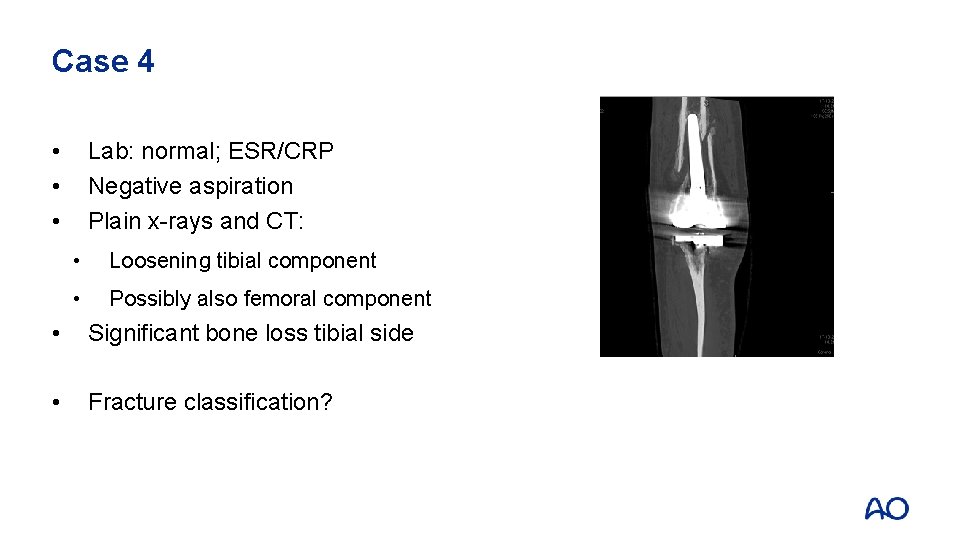
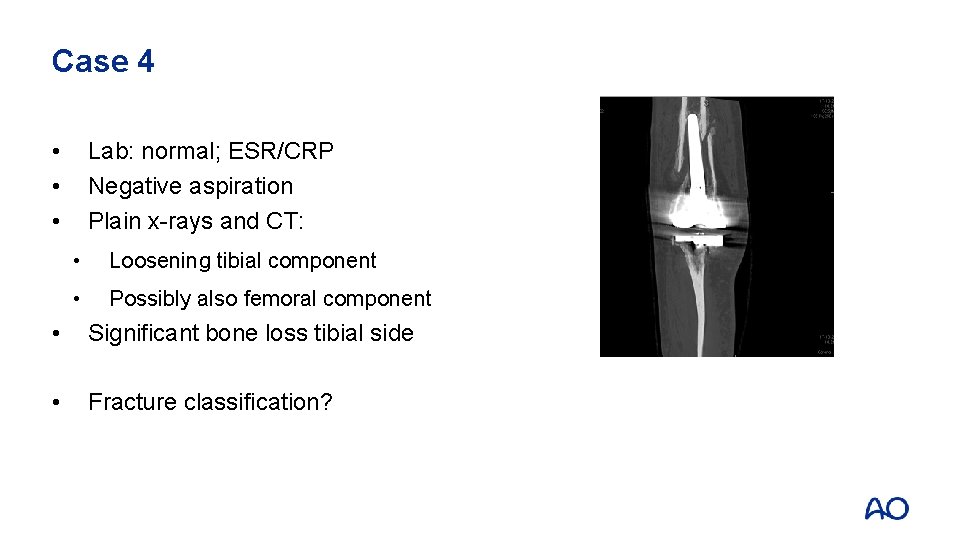
Case 4 • • • Lab: normal; ESR/CRP Negative aspiration Plain x-rays and CT: • Loosening tibial component • Possibly also femoral component • Significant bone loss tibial side • Fracture classification?

Management options • • • Nonoperative until fracture healing? Revision TKA? Treatment of the femoral periprosthetic fracture 3 months after trauma Reduction of fracture possible? Treatment of bone loss on tibial side Other considerations?
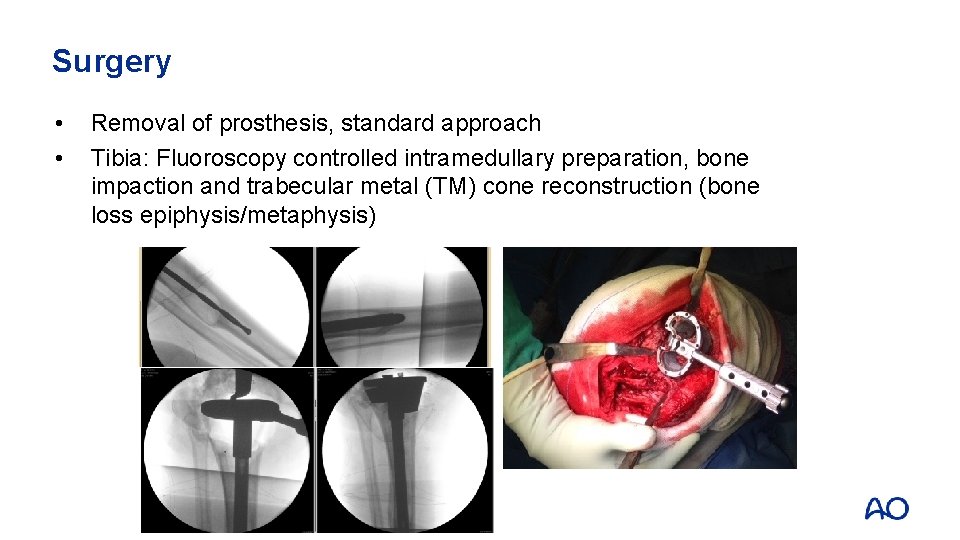
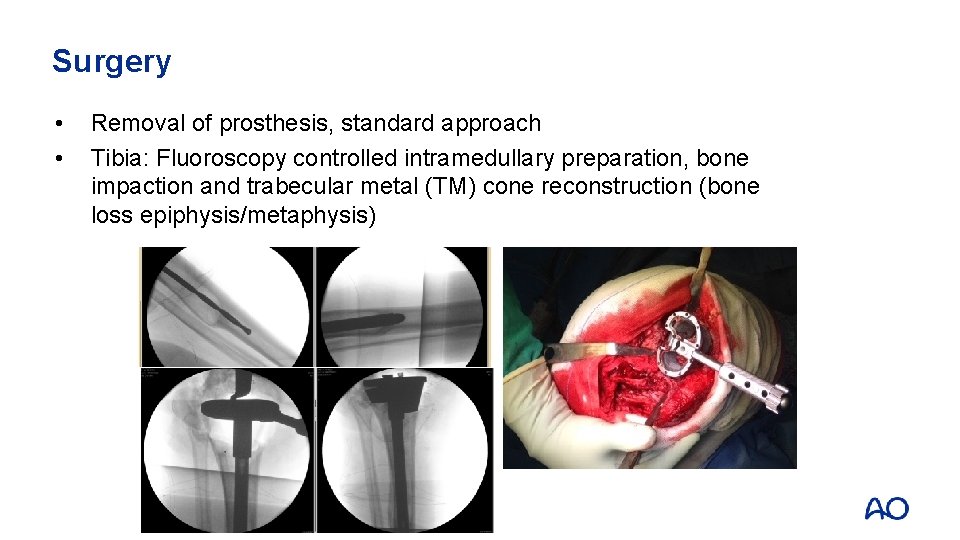
Surgery • • Removal of prosthesis, standard approach Tibia: Fluoroscopy controlled intramedullary preparation, bone impaction and trabecular metal (TM) cone reconstruction (bone loss epiphysis/metaphysis)
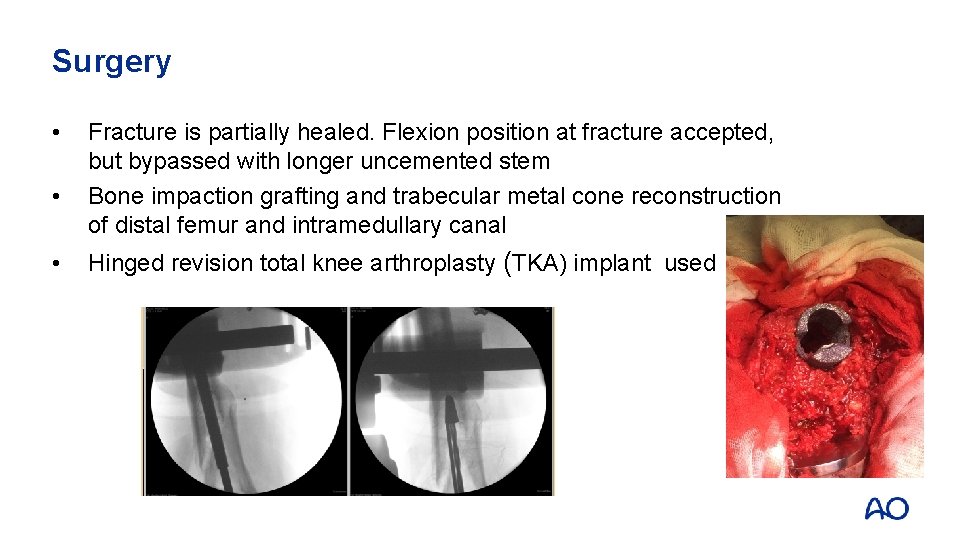
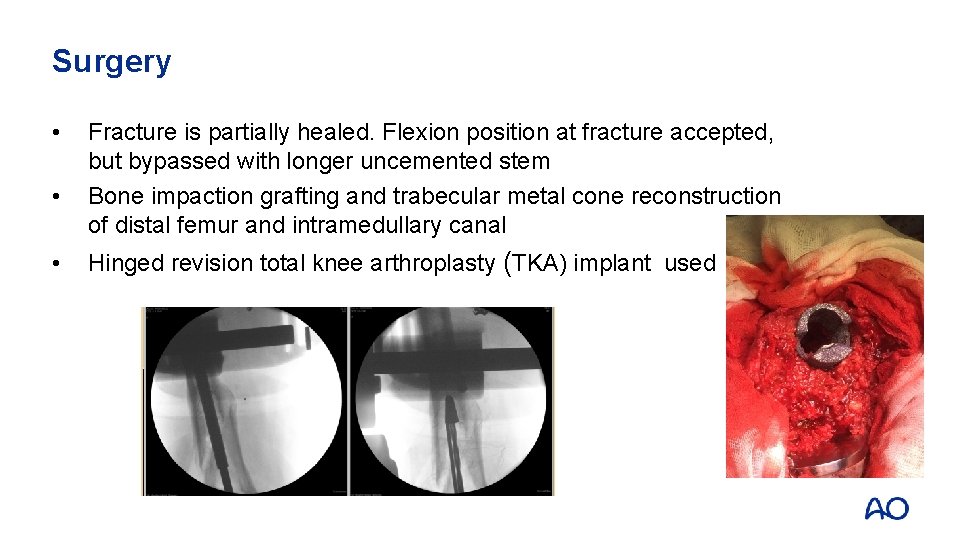
Surgery • • • Fracture is partially healed. Flexion position at fracture accepted, but bypassed with longer uncemented stem Bone impaction grafting and trabecular metal cone reconstruction of distal femur and intramedullary canal Hinged revision total knee arthroplasty (TKA) implant used
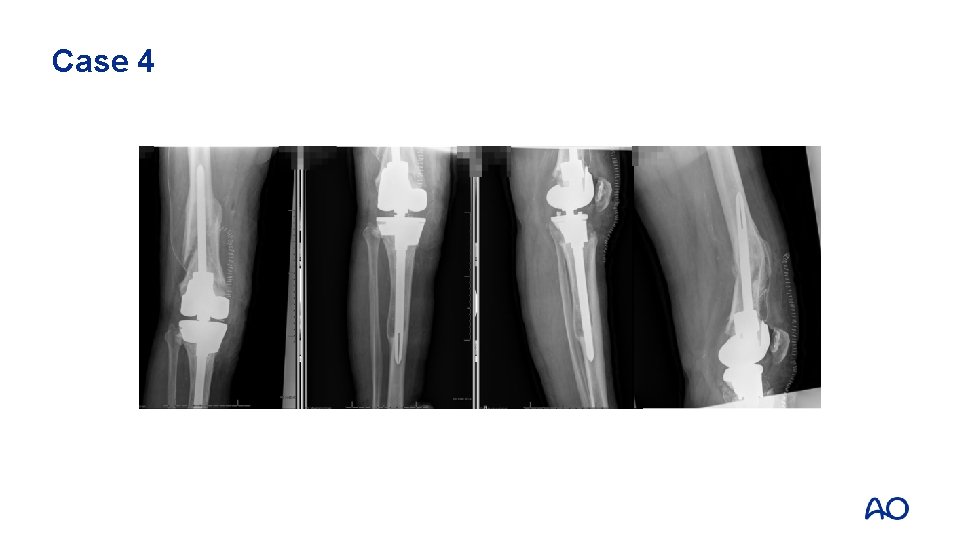
Case 4

Case 4: 6 weeks postop • • No pain Function 120/0/0
Case 4: Take-home messages • • Fractures can be stabilized or excised during revision surgery Biology needs to be respected if strong, durable fixation is to be achieved
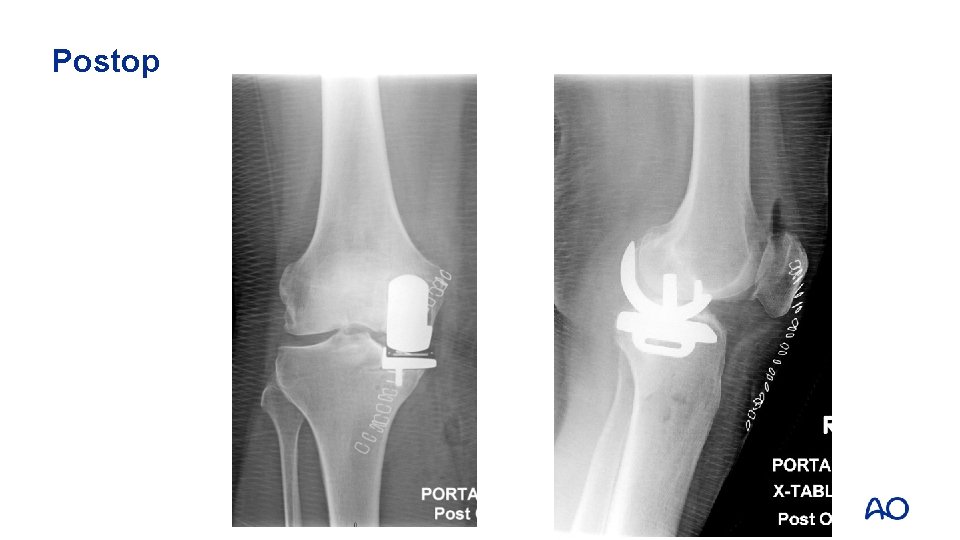
Case 5: Case description • • 64 -year-old woman Medial cementless unicompartmental replacement Always severe pain with weight bearing since operation Presents at two months with worsening varus deformity
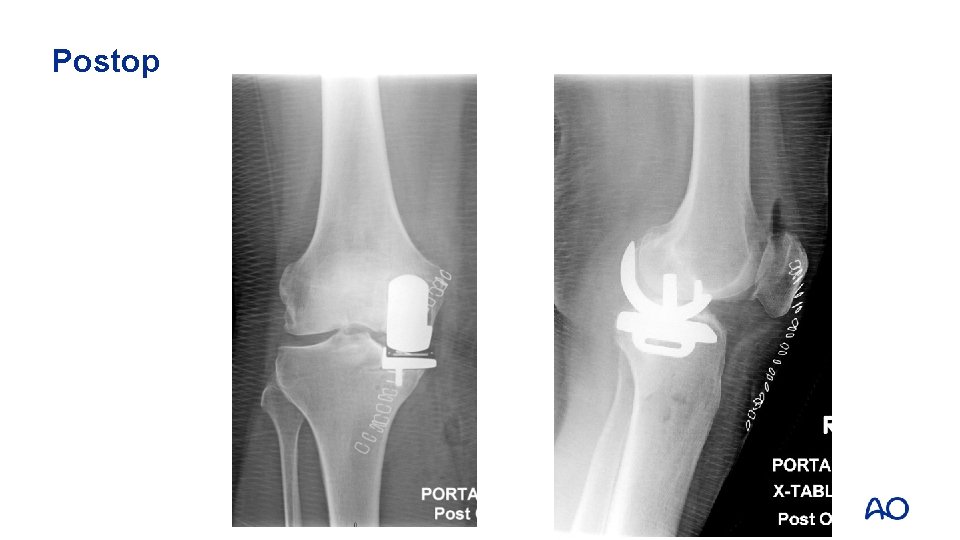
Postop

8 weeks postop

Case 5 • • • What went wrong? Why the fracture? How to treat?
Management options • Tibial component is ingrown to proximal tibia fragment • ORIF vs revision total knee replacement (TKR)?

Proximal tibial allograft
Case 5: Take-home messages • • Periprosthetic fractures require consideration of both the bony injury and the loose prosthesis Revision to a TKA offers a durable solution
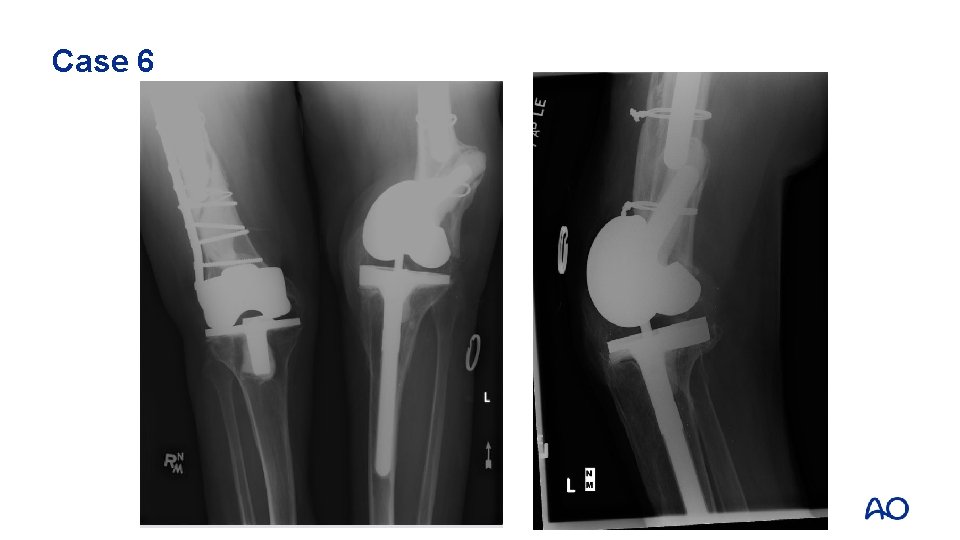
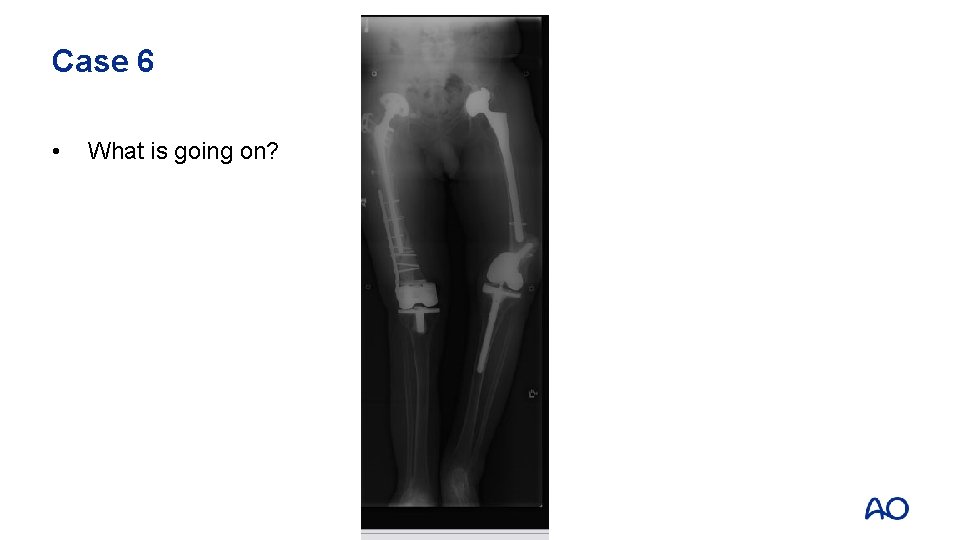
Case 6 • • • 39 -year-old with severe juvenile rheumatoid arthritis (JRA) THR and revision THR many years prior, no issues Revision TKR 4 years prior Minor fall Severe pain left knee
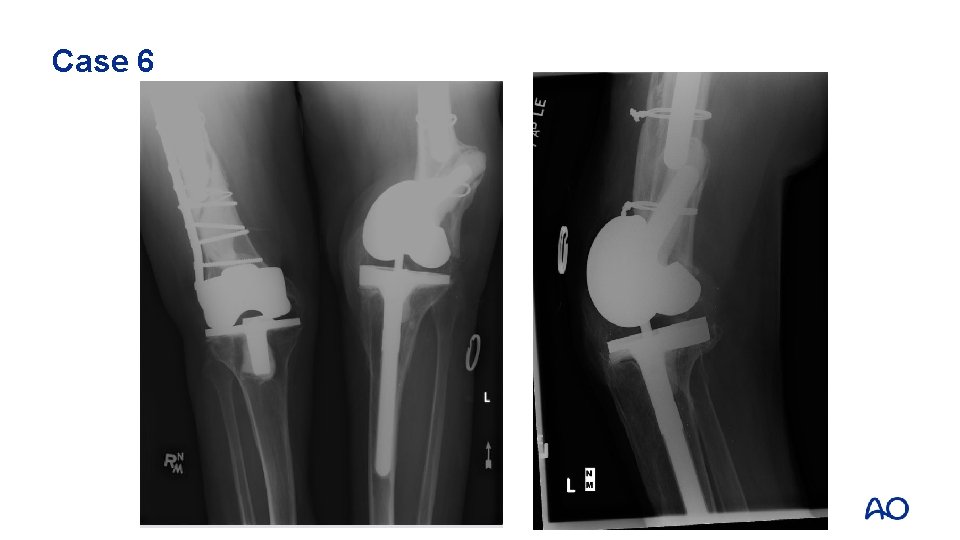
Case 6
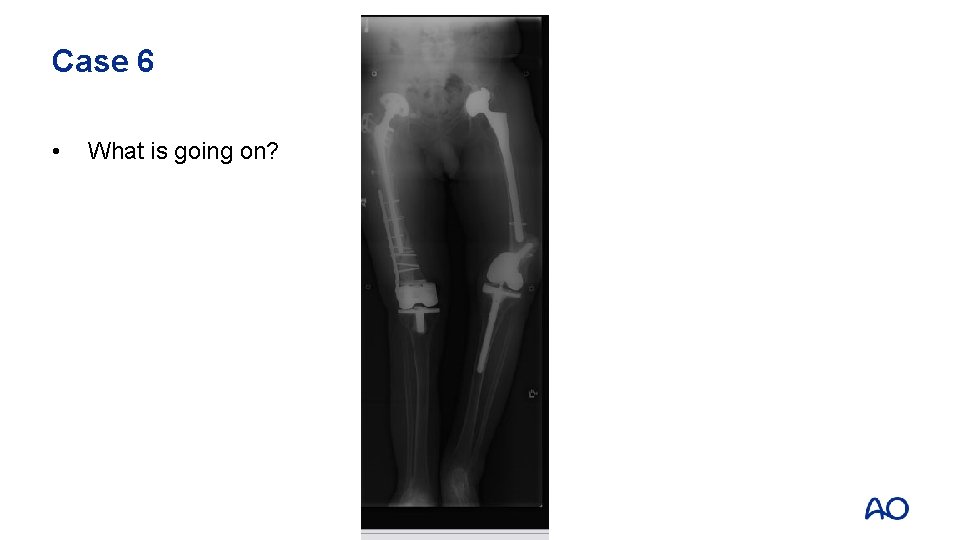
Case 6 • What is going on?

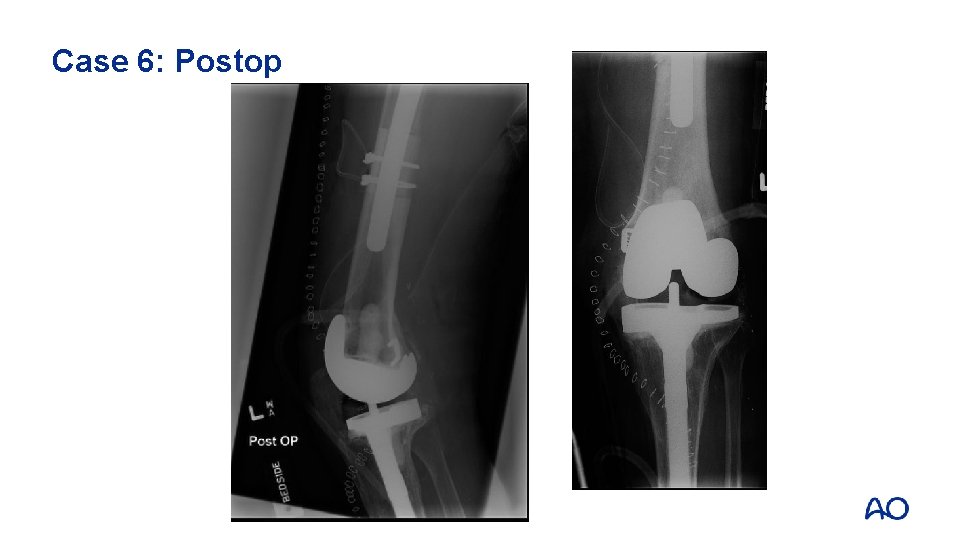
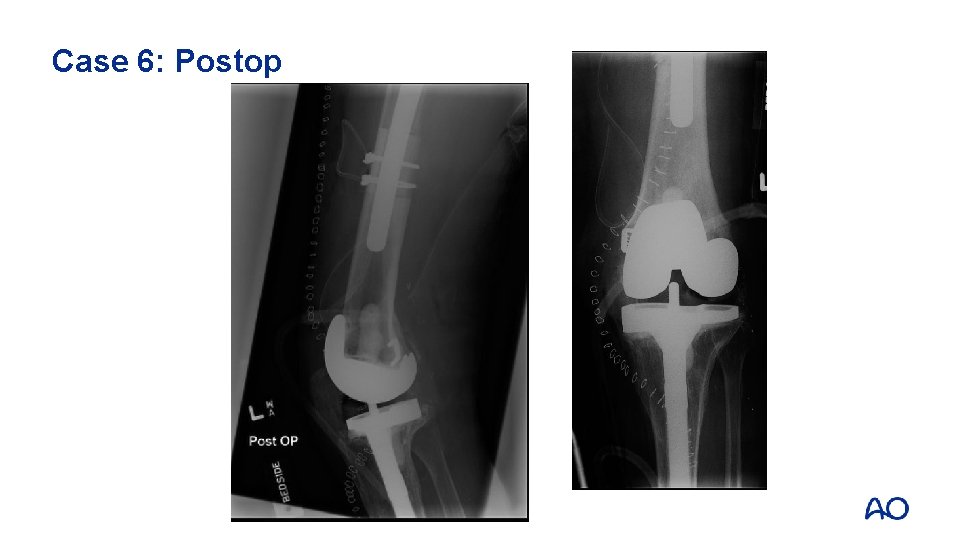
Case 6: Postop

Case 6: Postop
Case 6: Take-home messages • • Composite structural bone graft/prosthetic replacement solutions are an option in cases where the native bone stock is severely depleted Consider tumor prosthesis with diaphyseal replacement as an alternative
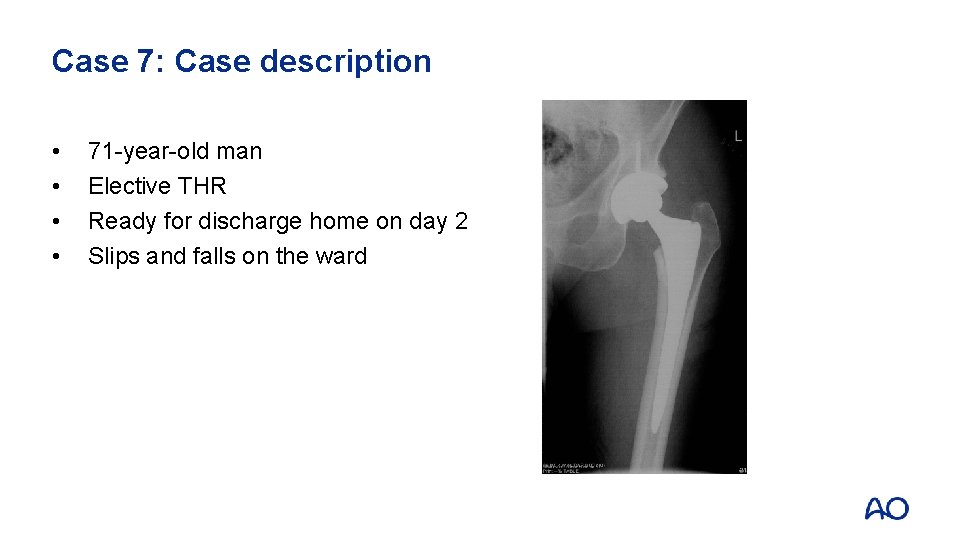
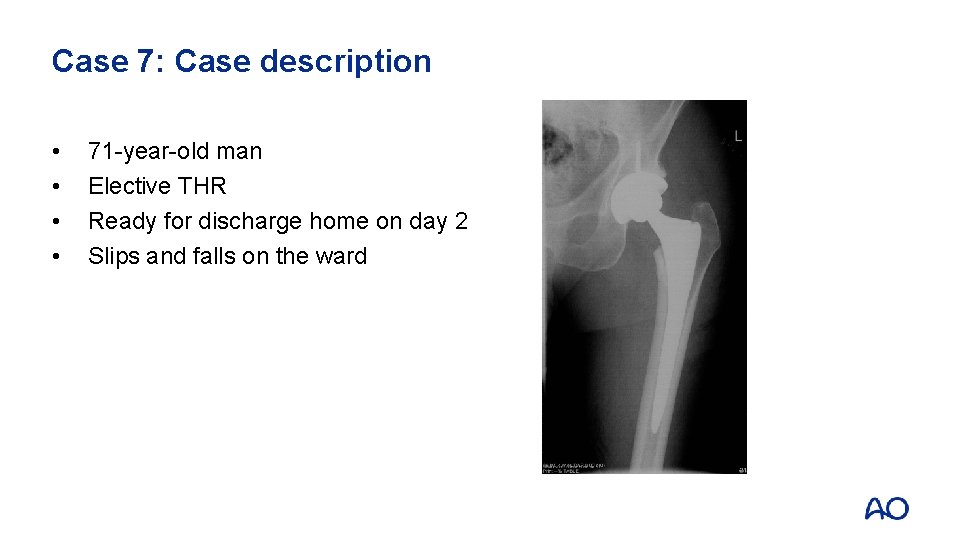
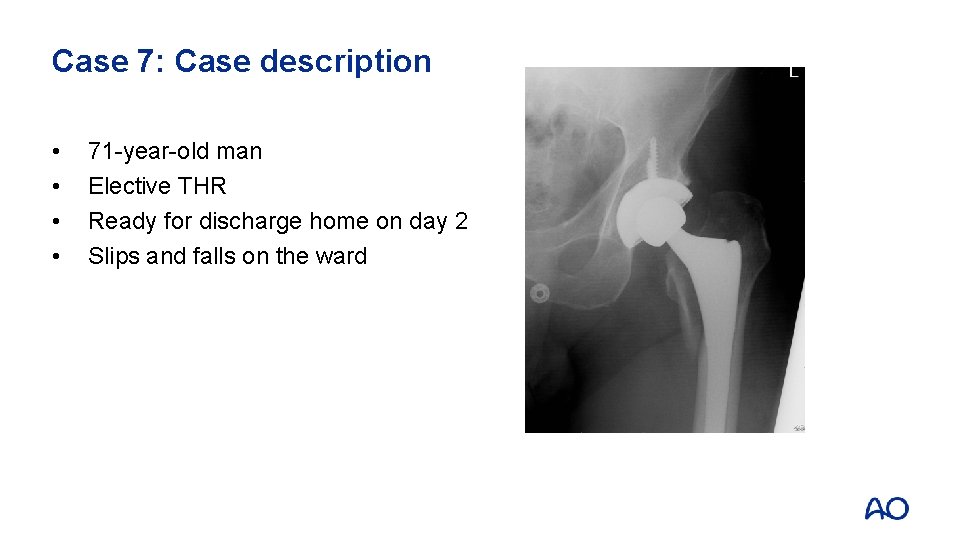
Case 7: Case description • • 71 -year-old man Elective THR Ready for discharge home on day 2 Slips and falls on the ward
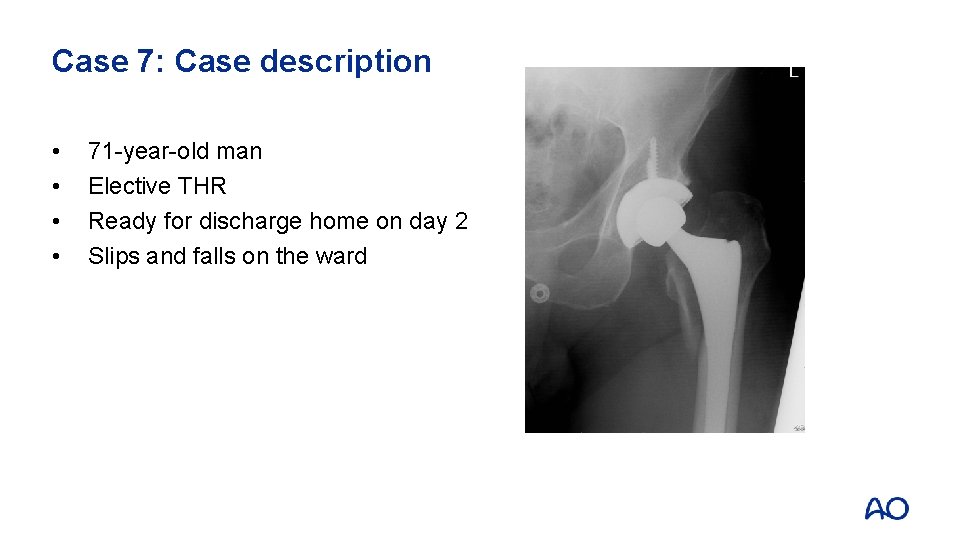
Case 7: Case description • • 71 -year-old man Elective THR Ready for discharge home on day 2 Slips and falls on the ward



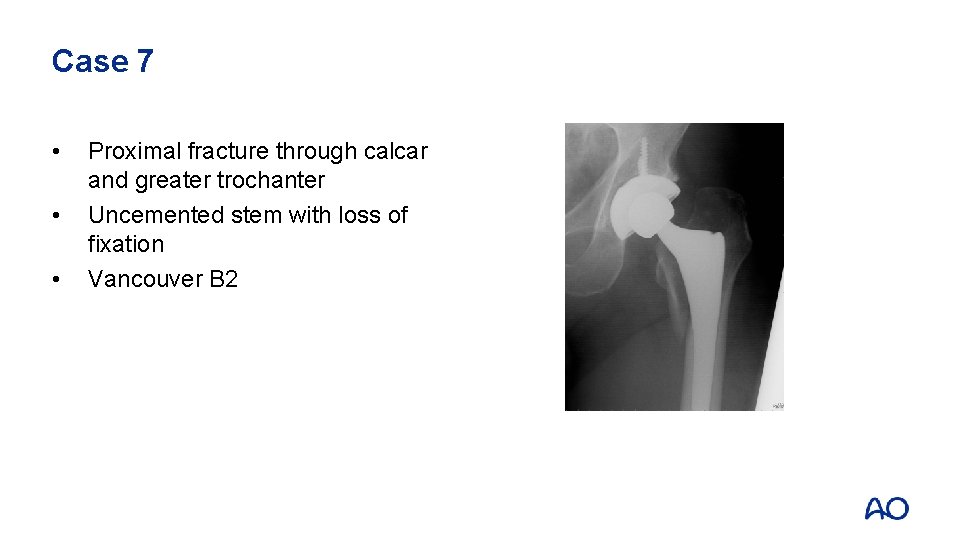
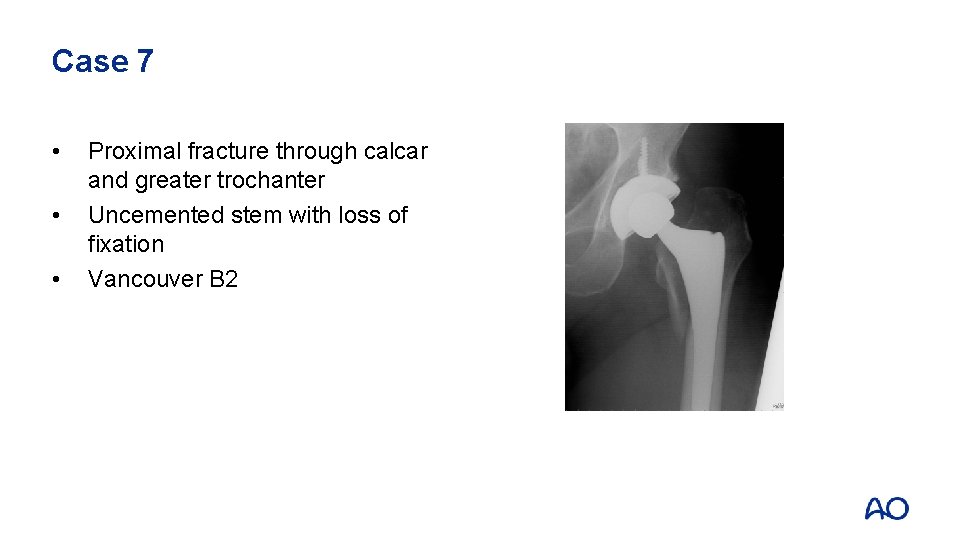
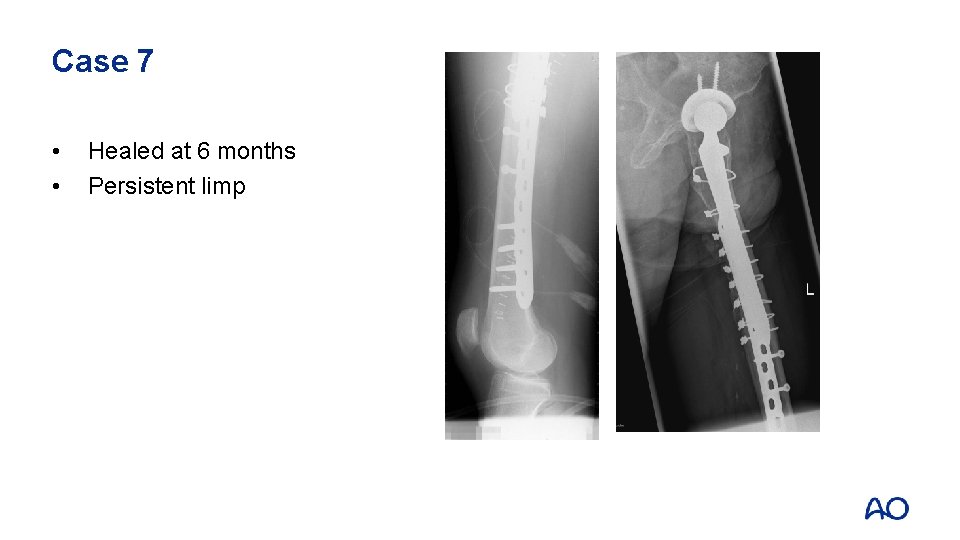
Case 7 • • • Proximal fracture through calcar and greater trochanter Uncemented stem with loss of fixation Vancouver B 2


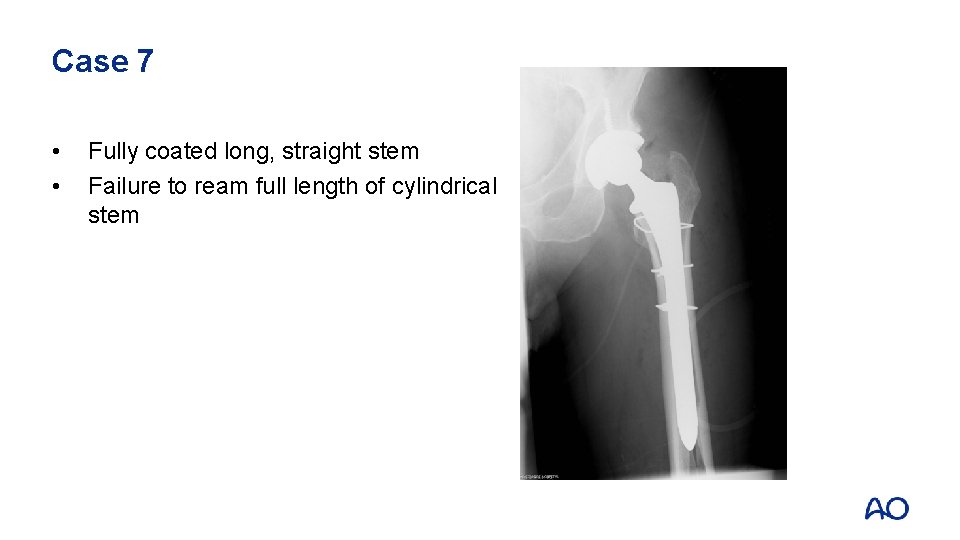
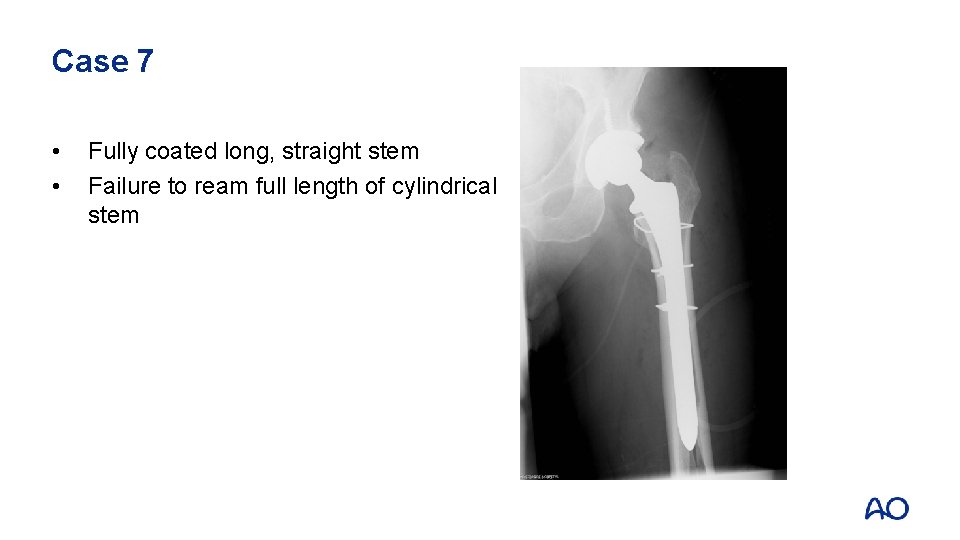
Case 7 • • Fully coated long, straight stem Failure to ream full length of cylindrical stem


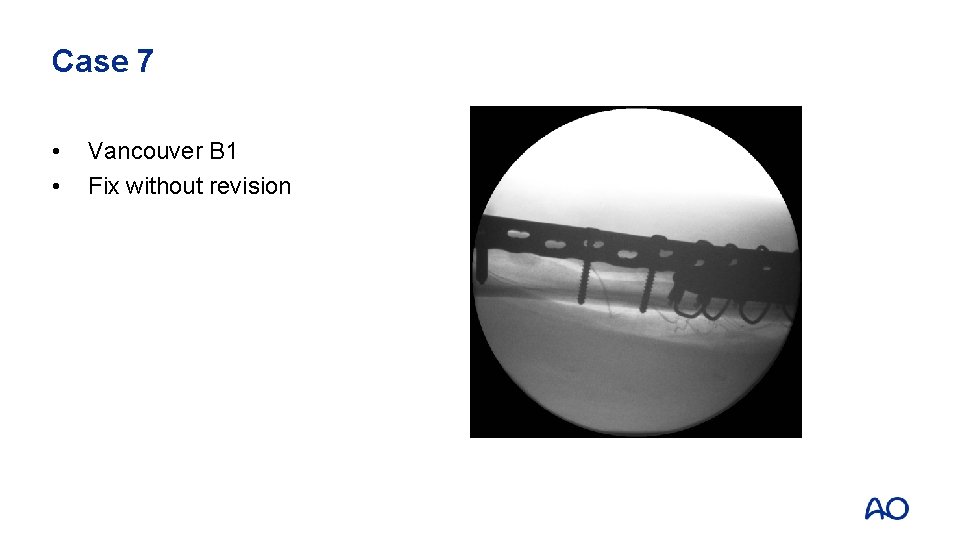
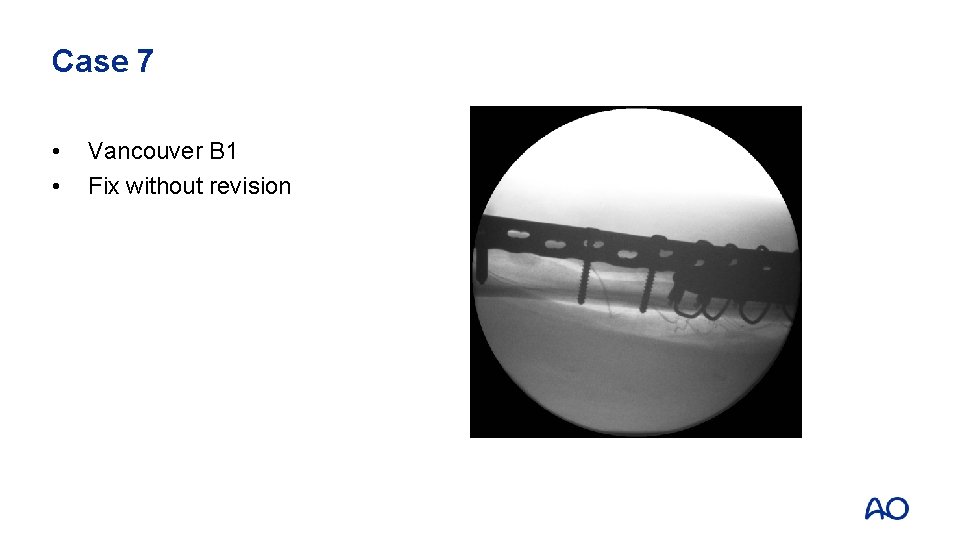
Case 7 • • Vancouver B 1 Fix without revision
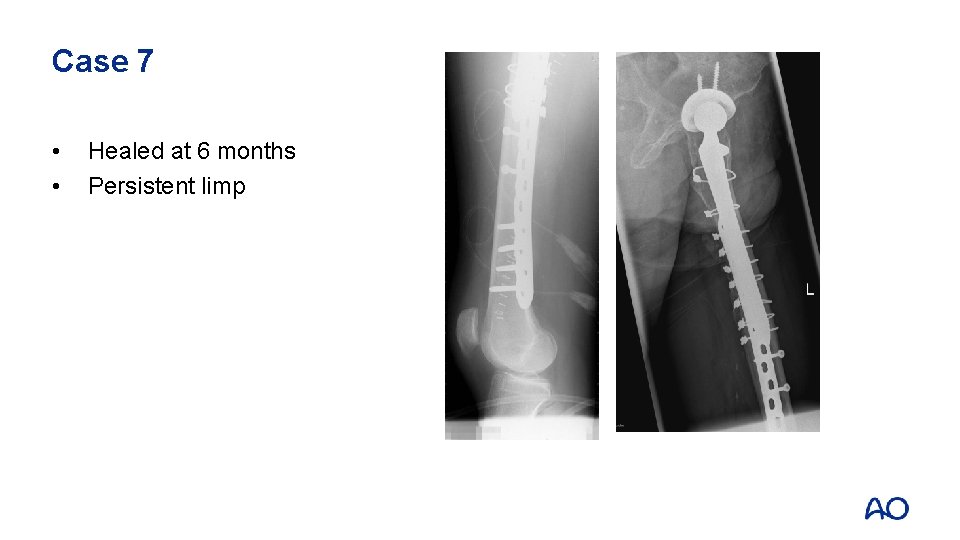
Case 7 • • Healed at 6 months Persistent limp
Case 7: Take-home messages • Be careful with aggressive “designs” and implanting tools
 Occupational therapy hip replacement interventions
Occupational therapy hip replacement interventions Knee flexors
Knee flexors Hip hop hip to the hippity
Hip hop hip to the hippity Hip to the hippity hop
Hip to the hippity hop Arthroplasty practitioner
Arthroplasty practitioner Muscle around knee
Muscle around knee Revision passive voice
Revision passive voice Example of what goes around comes around
Example of what goes around comes around Martin luther king of hinduism
Martin luther king of hinduism A spill at parsenn bowl: knee injury and recovery
A spill at parsenn bowl: knee injury and recovery Makenzie milton injury
Makenzie milton injury Chapter 16 worksheet the knee and related structures
Chapter 16 worksheet the knee and related structures Vastus medialis origin
Vastus medialis origin Elbow restraint definition
Elbow restraint definition Locking muscle
Locking muscle Posterior hip precautions
Posterior hip precautions Locking and unlocking of knee joint
Locking and unlocking of knee joint Quad muscles action
Quad muscles action Types of drowning
Types of drowning Chapter 17 the thigh hip groin and pelvis
Chapter 17 the thigh hip groin and pelvis Internal and external hip rotation
Internal and external hip rotation Pubofemoral ligament
Pubofemoral ligament Chapter 17 the thigh hip groin and pelvis
Chapter 17 the thigh hip groin and pelvis Femoral anteversion
Femoral anteversion Flexor strain elbow
Flexor strain elbow 2 12 pitch angle
2 12 pitch angle Waist hip ratio
Waist hip ratio Beam knee in ship
Beam knee in ship Hip synovial joint
Hip synovial joint Muscular system
Muscular system Trochlea knee
Trochlea knee Patella tilt angle
Patella tilt angle Vertical suspension is used for
Vertical suspension is used for Forearm rom
Forearm rom Postures and gestures at mass
Postures and gestures at mass Bed making articles name
Bed making articles name Horizontal position patient
Horizontal position patient Lateral cutaneous nerve of thigh
Lateral cutaneous nerve of thigh End feel firm adalah
End feel firm adalah Beam knee
Beam knee Lachman test
Lachman test Extensor digitorum longus insertion
Extensor digitorum longus insertion Biomekanik knee joint
Biomekanik knee joint Slocum test for knee
Slocum test for knee Gerakan knee joint
Gerakan knee joint Knee walker rentals of georgia
Knee walker rentals of georgia Peroneus tertius
Peroneus tertius Benign bone island
Benign bone island Knee screw home mechanism
Knee screw home mechanism Resting position of knee
Resting position of knee Jesus at your name we bow the knee lyrics
Jesus at your name we bow the knee lyrics Idk left knee icd 10
Idk left knee icd 10 Posterior capsulotomy knee pcs code
Posterior capsulotomy knee pcs code Comfort devices and their uses
Comfort devices and their uses Pectoralis major agonist
Pectoralis major agonist Bregg knee brace
Bregg knee brace Wilbrand knee
Wilbrand knee Which diode model is the most accurate?
Which diode model is the most accurate?