Revision arthroplasty around the hip and the knee


- Slides: 27
Revision arthroplasty around the hip and the knee Plenary – case-based Periprosthetic Fractures Periprosthetic Fracture Management
Learning objectives for the cases • • Classify the fracture Describe the options and indications for nonoperative, fixation, and revision treatment Select an appropriate treatment Identify and address potential complications
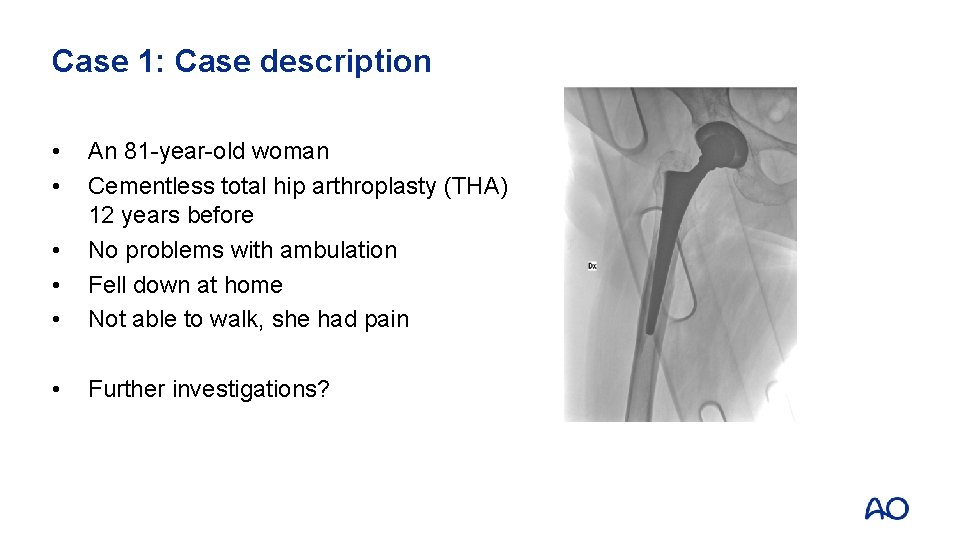
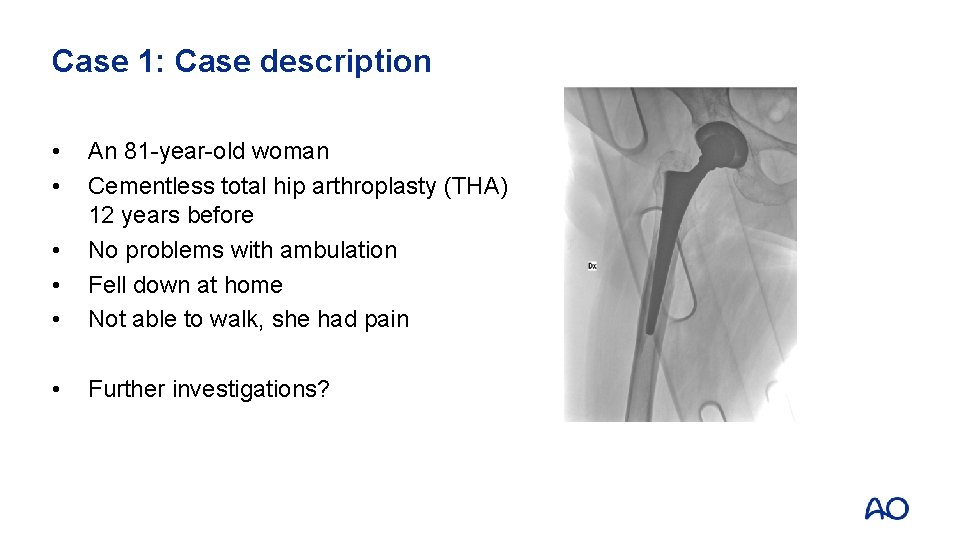
Case 1: Case description • • • An 81 -year-old woman Cementless total hip arthroplasty (THA) 12 years before No problems with ambulation Fell down at home Not able to walk, she had pain • Further investigations?
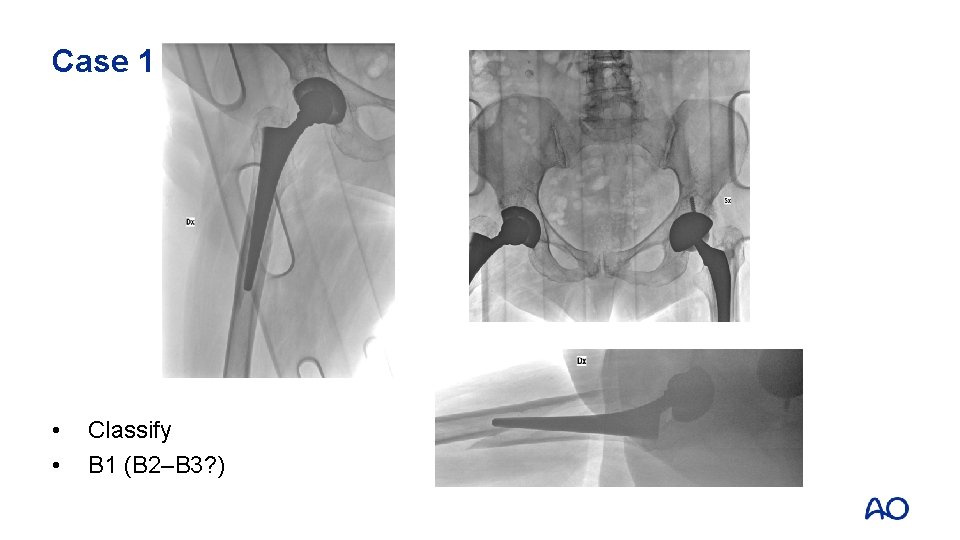
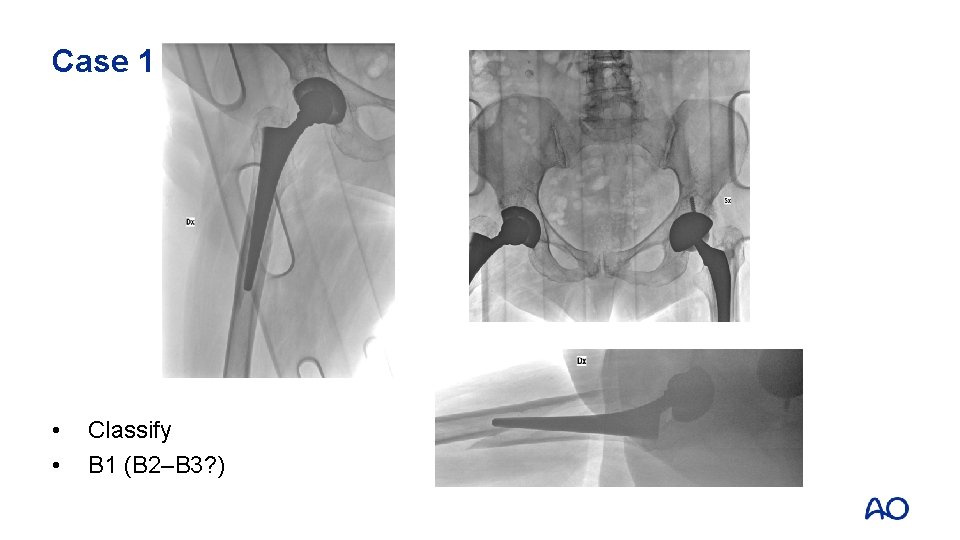
Case 1 • • Classify B 1 (B 2–B 3? )
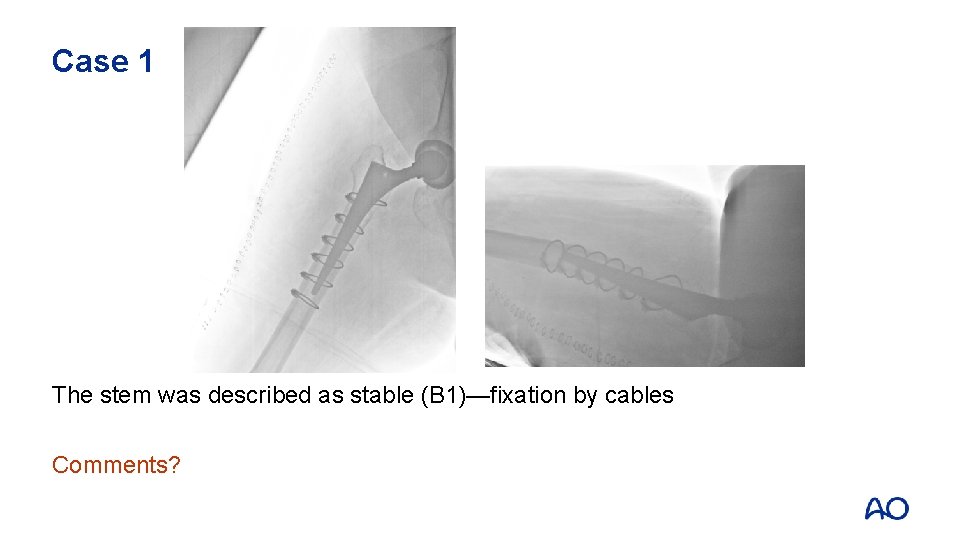
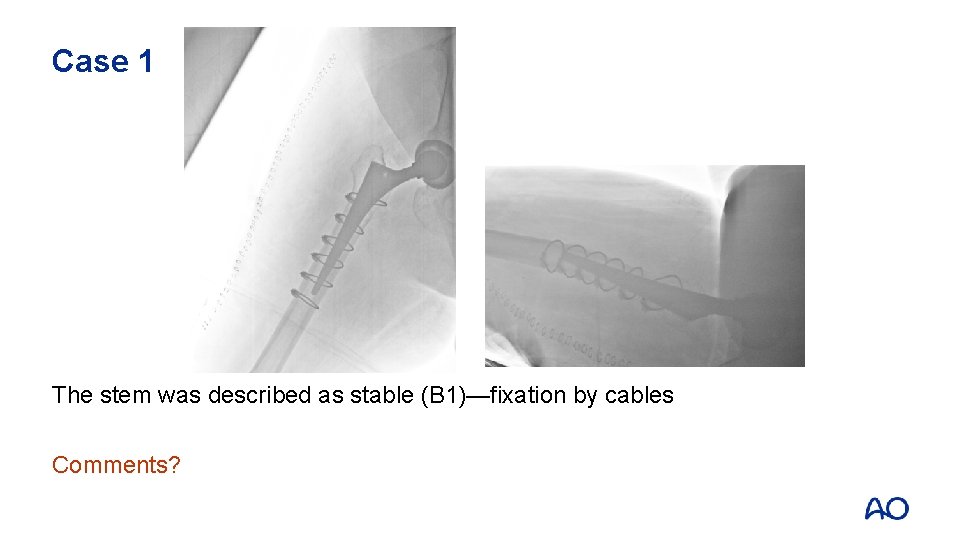
Case 1 The stem was described as stable (B 1)—fixation by cables Comments?
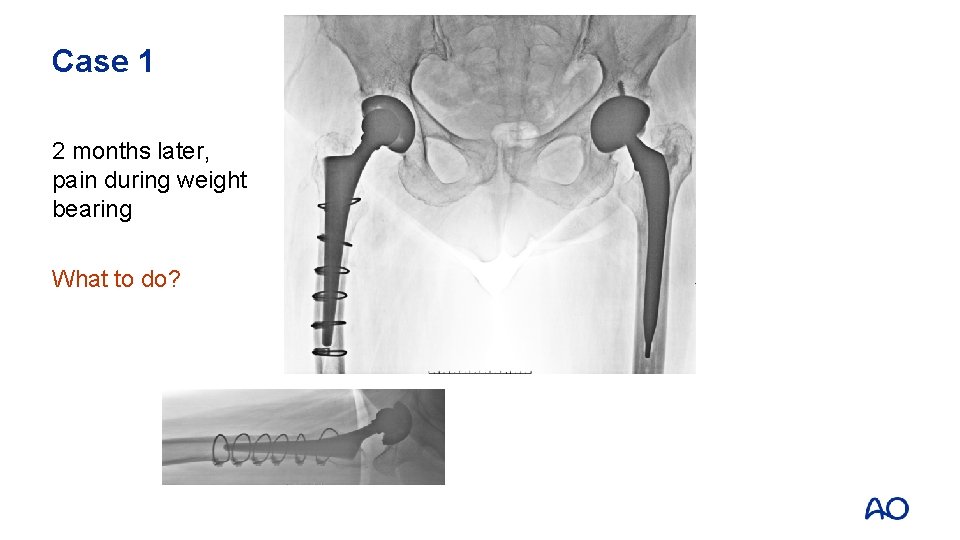
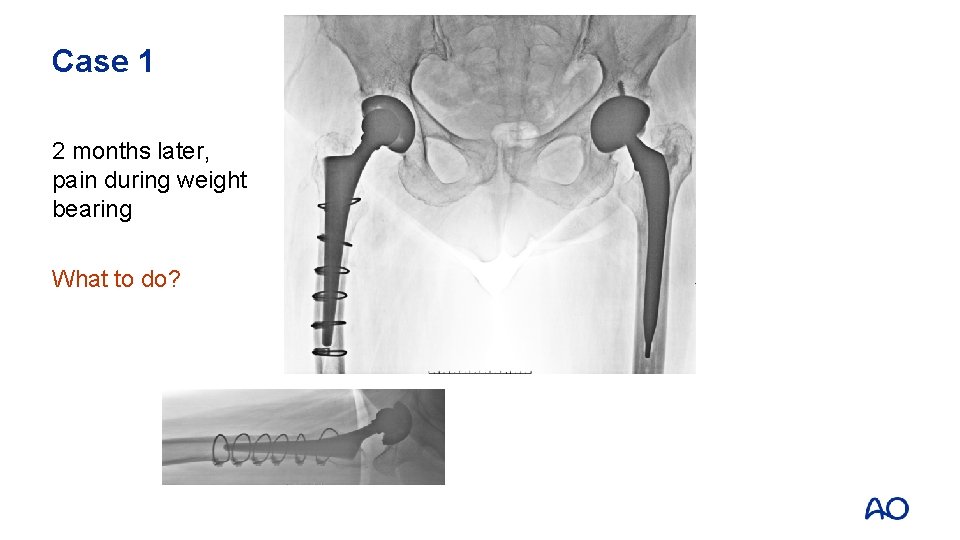
Case 1 2 months later, pain during weight bearing What to do?
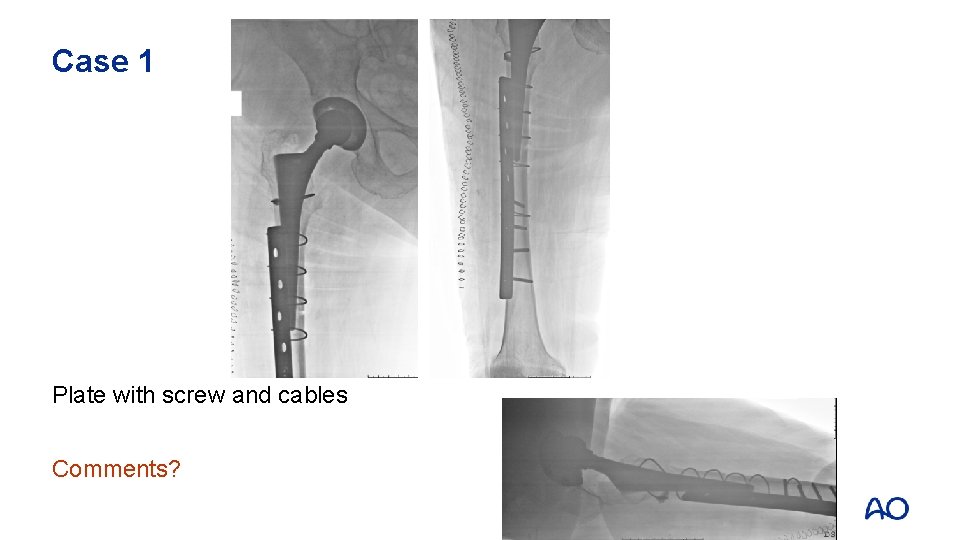
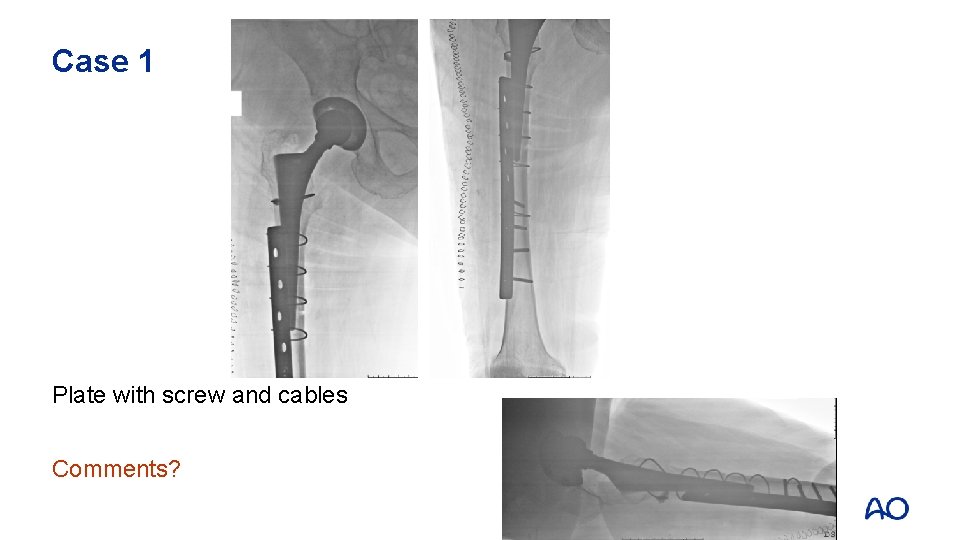
Case 1 Plate with screw and cables Comments?
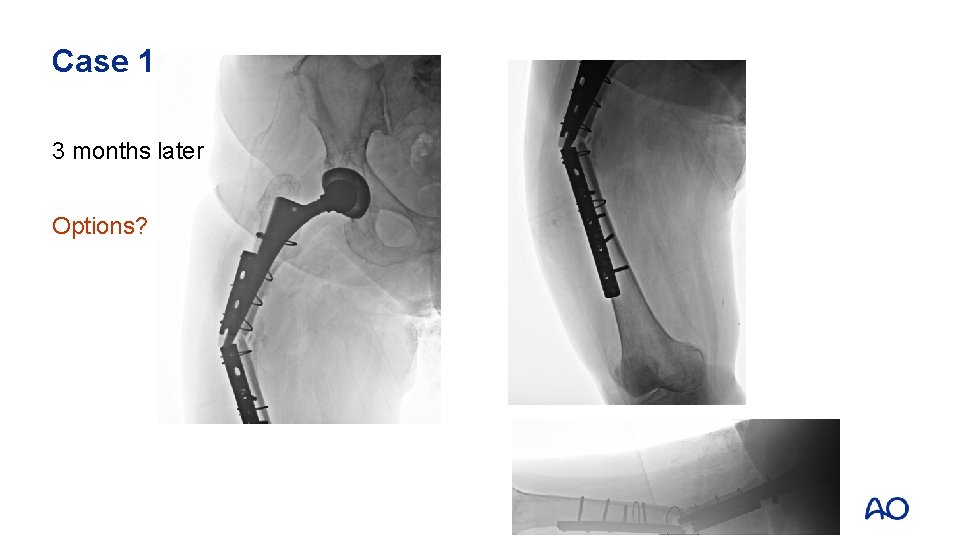
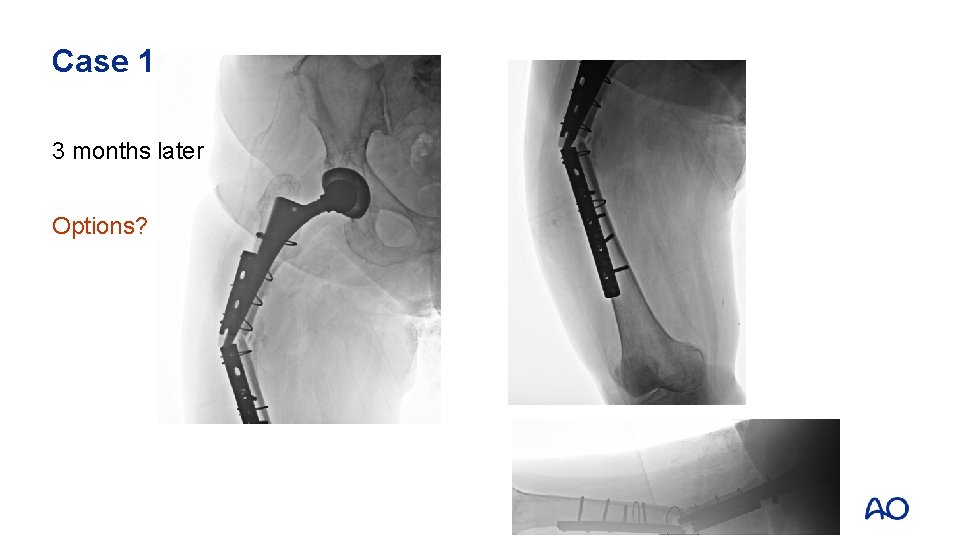
Case 1 3 months later Options?

Case 1 Revision stem, preventive cable
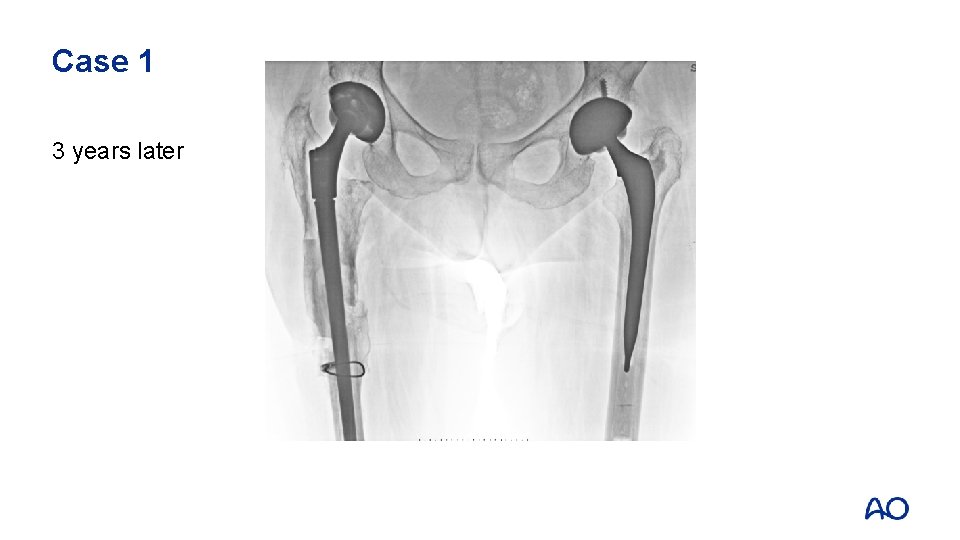
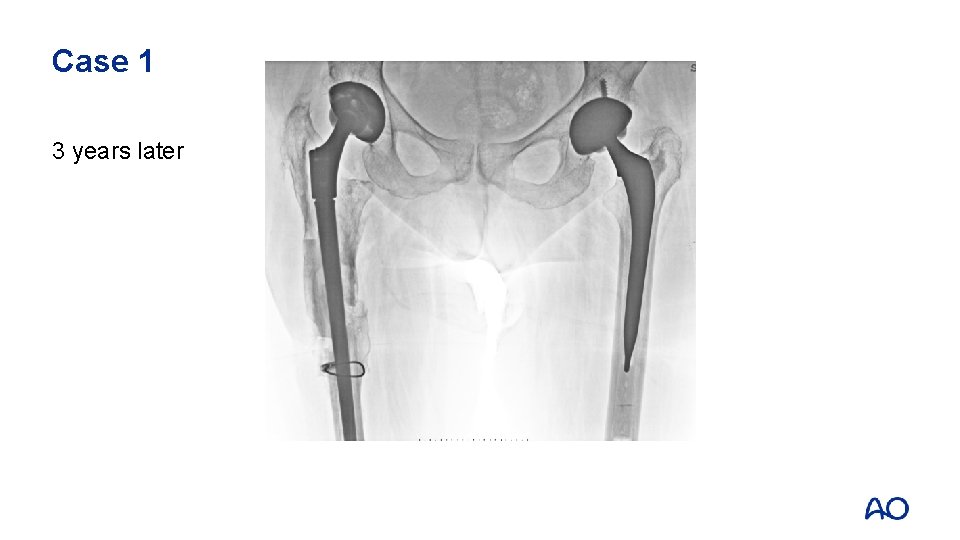
Case 1 3 years later
Case 1: Take-home messages • • • Complete imaging is essential Use stable and correct fixation techniques Be careful when evaluating B 1 fractures
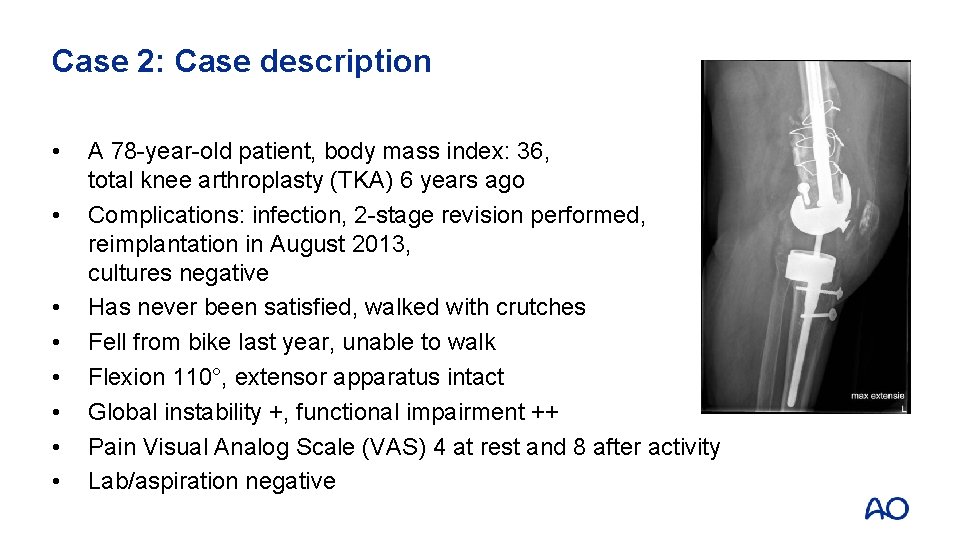
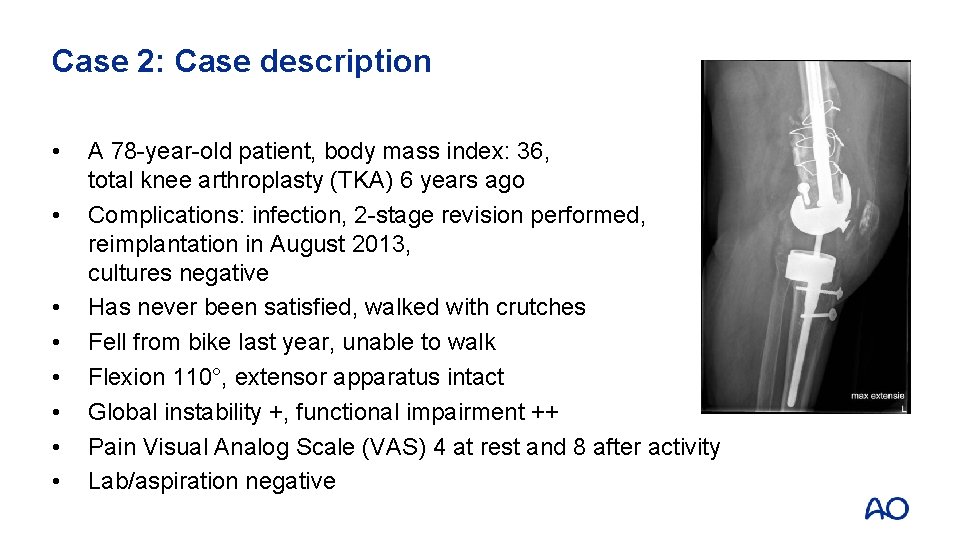
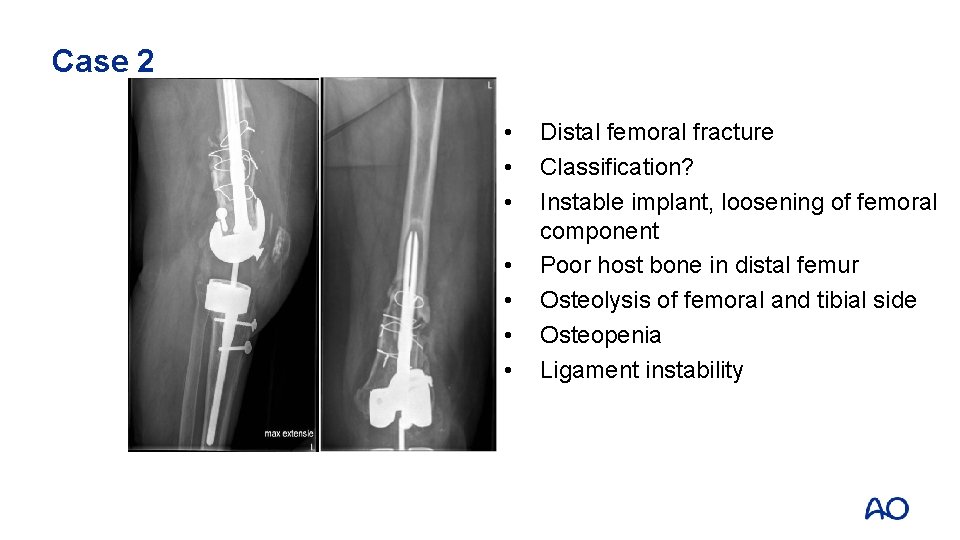
Case 2: Case description • • A 78 -year-old patient, body mass index: 36, total knee arthroplasty (TKA) 6 years ago Complications: infection, 2 -stage revision performed, reimplantation in August 2013, cultures negative Has never been satisfied, walked with crutches Fell from bike last year, unable to walk Flexion 110°, extensor apparatus intact Global instability +, functional impairment ++ Pain Visual Analog Scale (VAS) 4 at rest and 8 after activity Lab/aspiration negative

Case 2
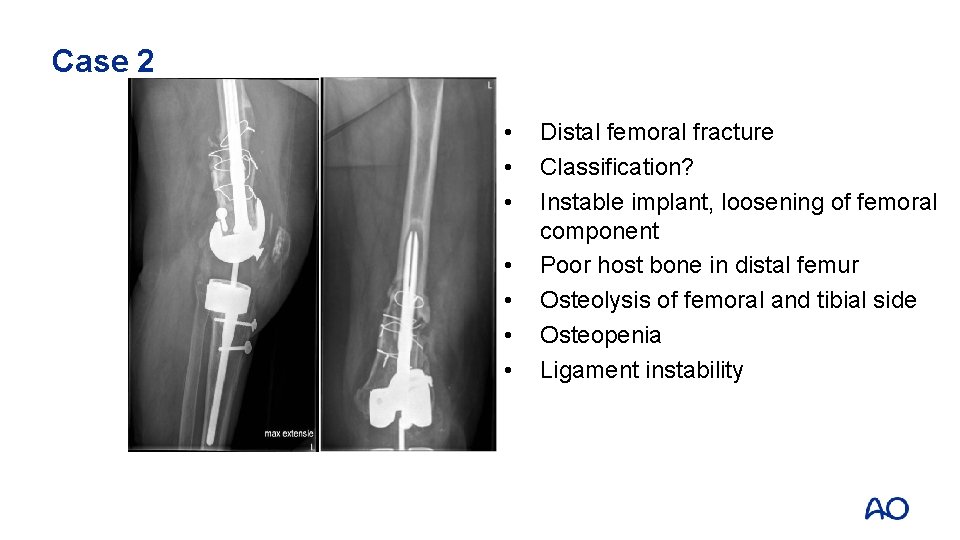
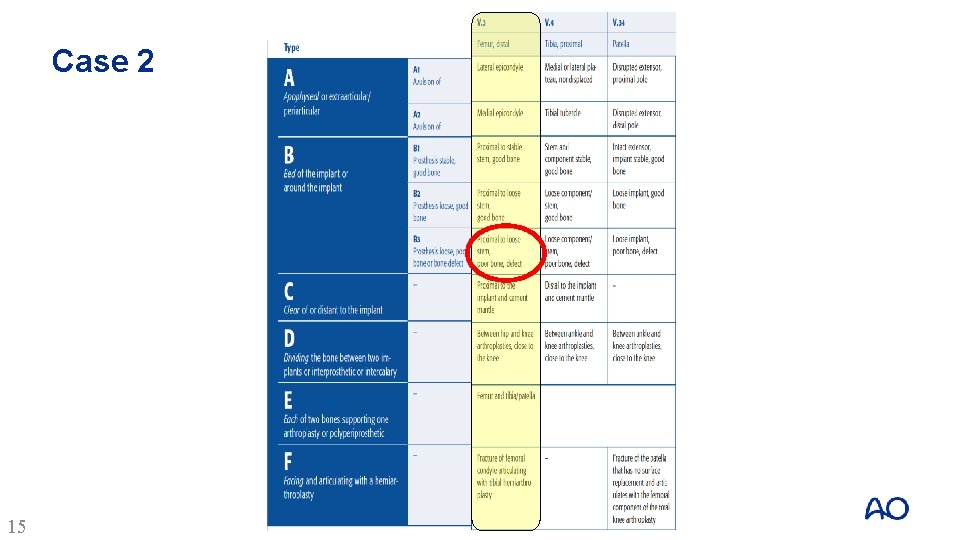
Case 2 • • Distal femoral fracture Classification? Instable implant, loosening of femoral component Poor host bone in distal femur Osteolysis of femoral and tibial side Osteopenia Ligament instability
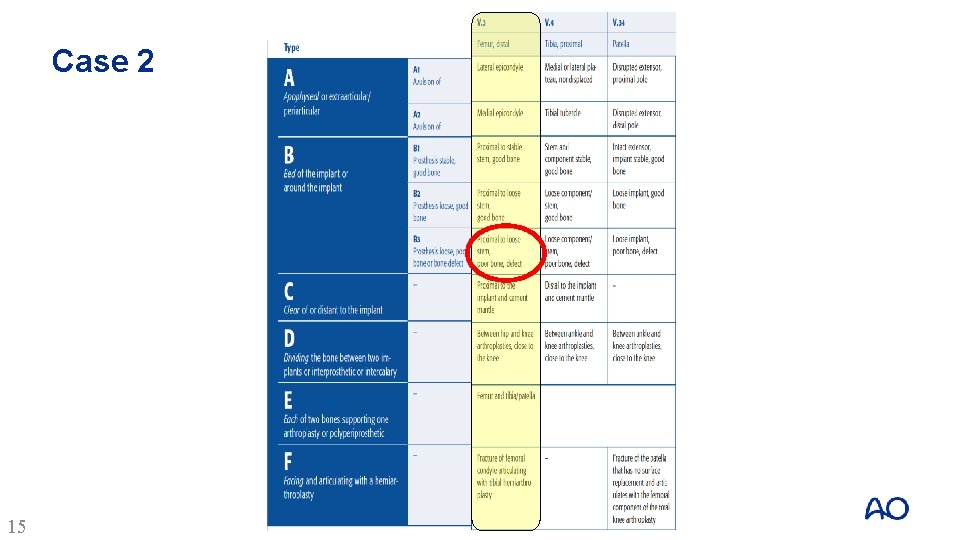
Case 2 15
Case 2 Management options: • Revision TKA? • Distal femoral replacement? • Fracture stabilization? • Other considerations?
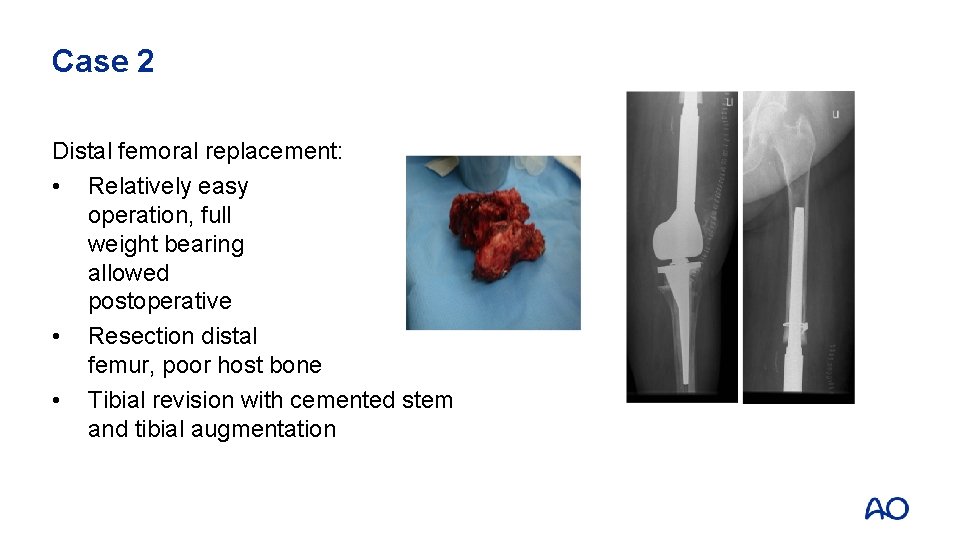
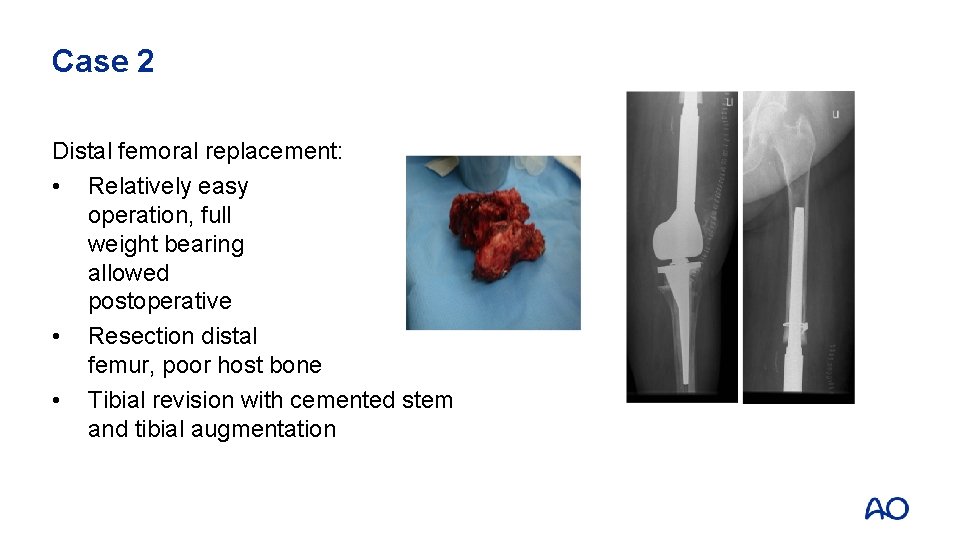
Case 2 Distal femoral replacement: • Relatively easy operation, full weight bearing allowed postoperative • Resection distal femur, poor host bone • Tibial revision with cemented stem and tibial augmentation
Case 2: Take-home messages • Difficult periprosthetic fractures can be managed by excision of the fracture fragments and replacement with tumor-type prostheses • Although providing more rapid recovery, the next operation should be considered
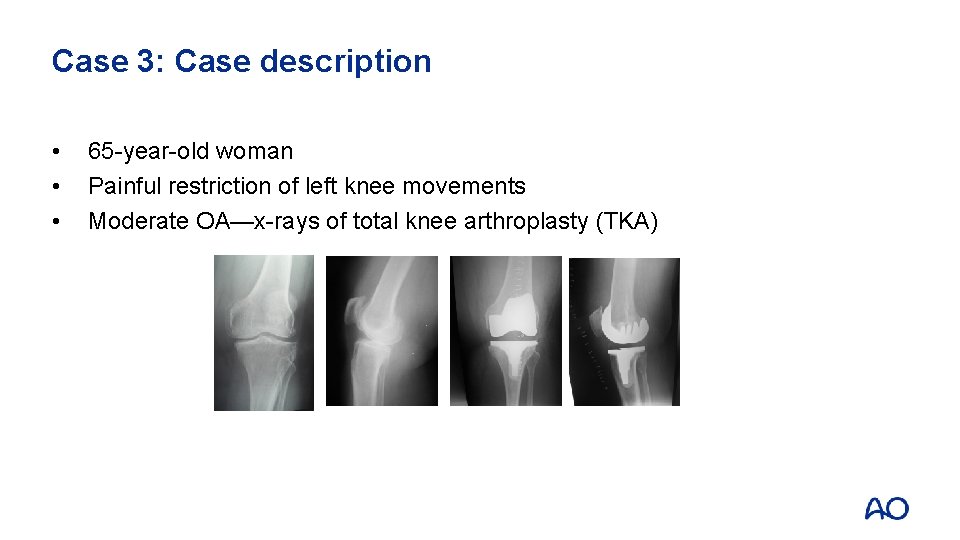
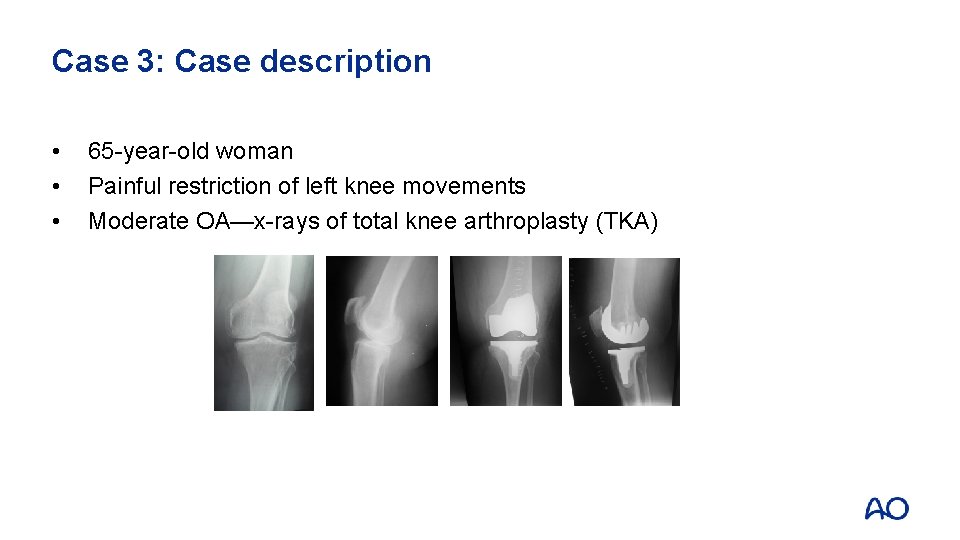
Case 3: Case description • • • 65 -year-old woman Painful restriction of left knee movements Moderate OA—x-rays of total knee arthroplasty (TKA)
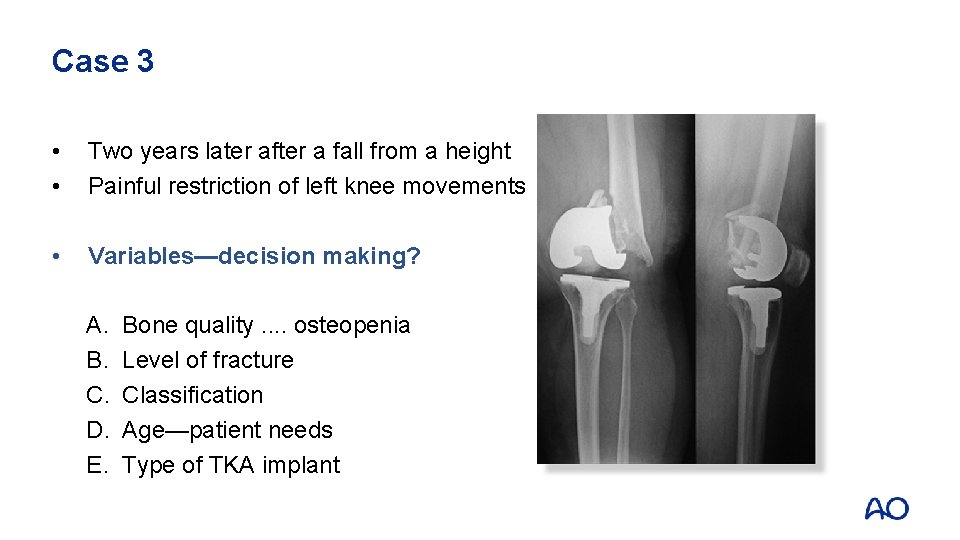
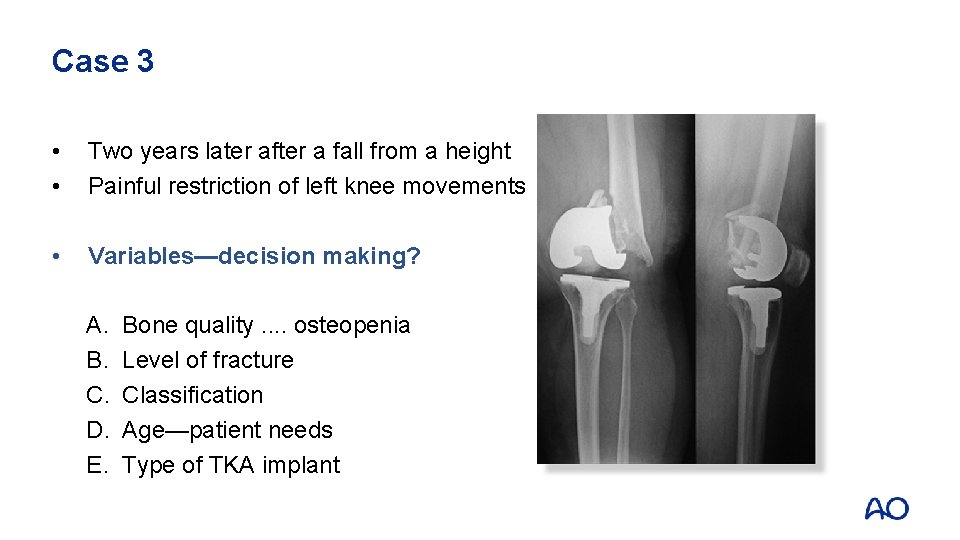
Case 3 • • Two years later after a fall from a height Painful restriction of left knee movements • Variables—decision making? A. B. C. D. E. Bone quality. . osteopenia Level of fracture Classification Age—patient needs Type of TKA implant
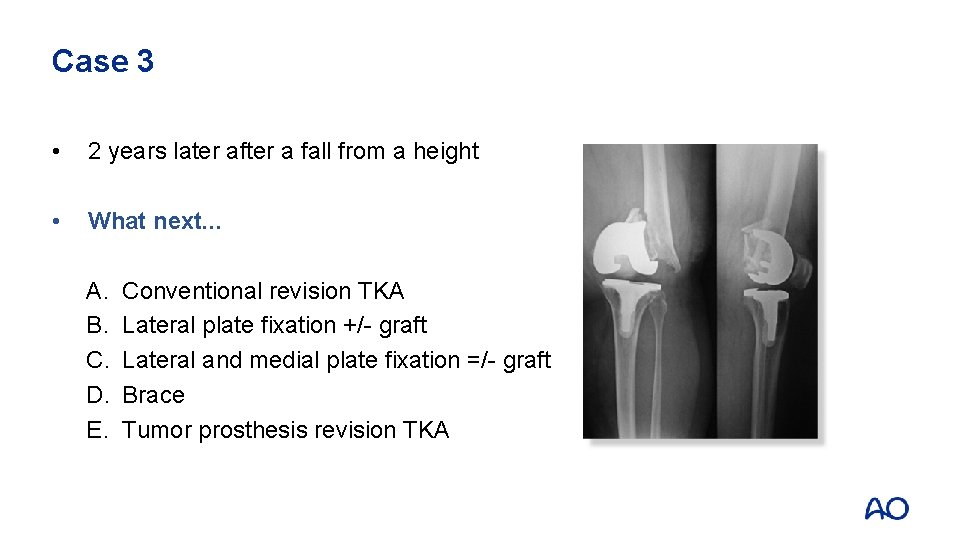
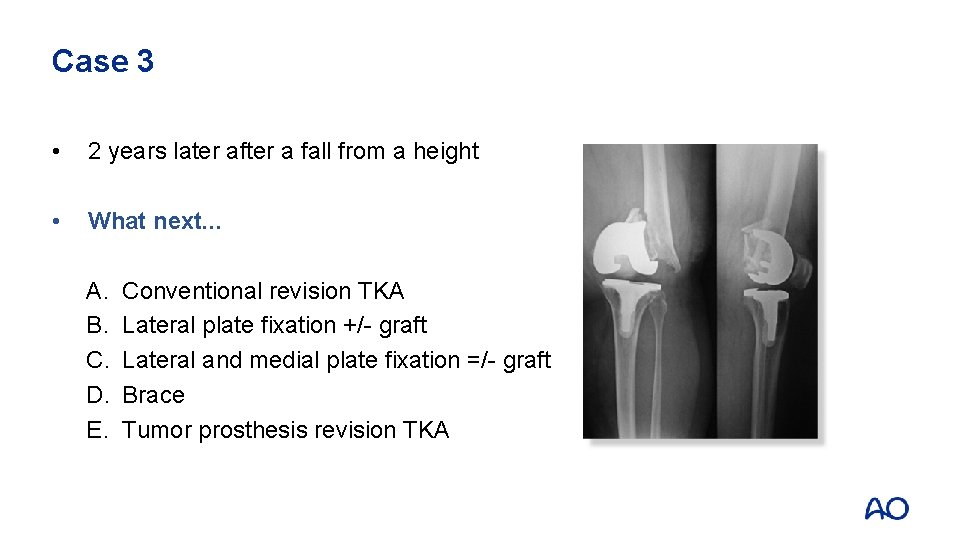
Case 3 • 2 years later after a fall from a height • What next. . . A. B. C. D. E. Conventional revision TKA Lateral plate fixation +/- graft Lateral and medial plate fixation =/- graft Brace Tumor prosthesis revision TKA
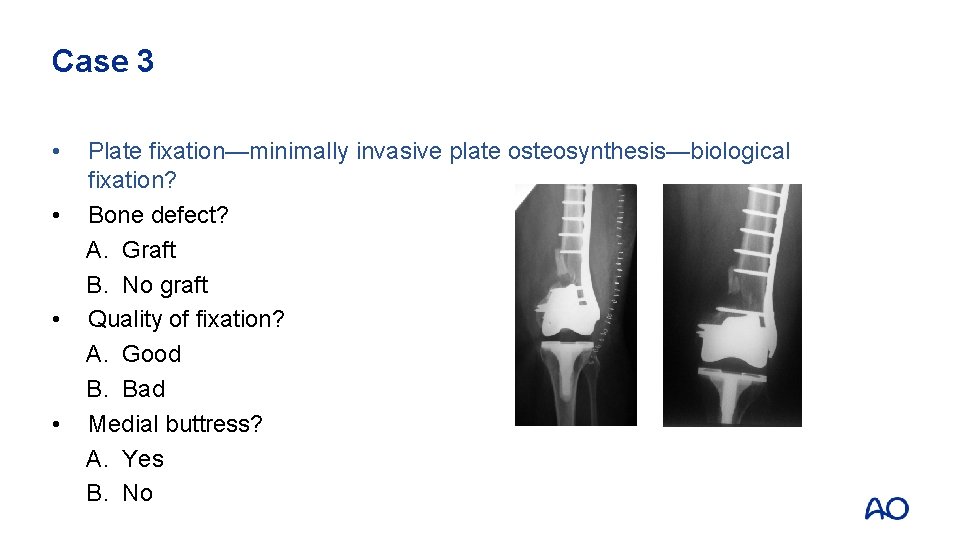
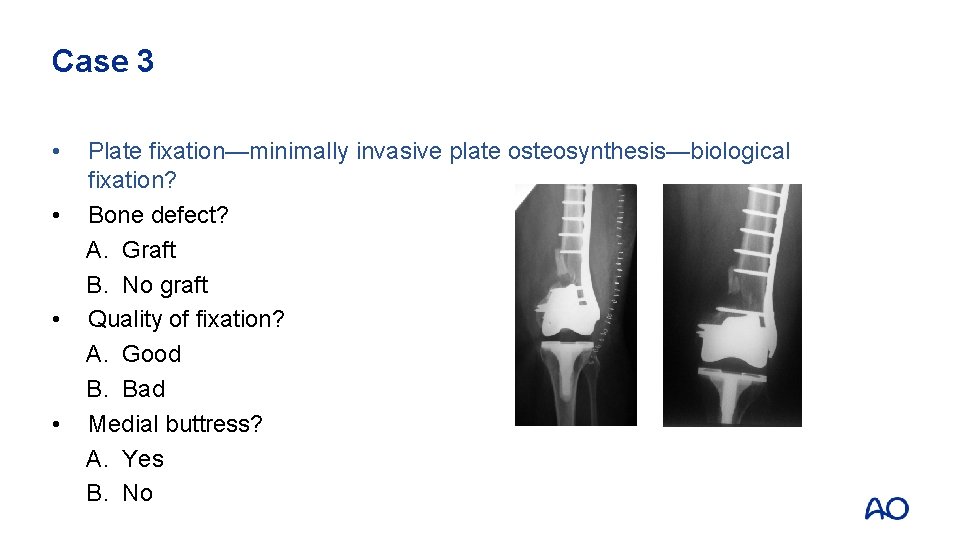
Case 3 • • Plate fixation—minimally invasive plate osteosynthesis—biological fixation? Bone defect? A. Graft B. No graft Quality of fixation? A. Good B. Bad Medial buttress? A. Yes B. No
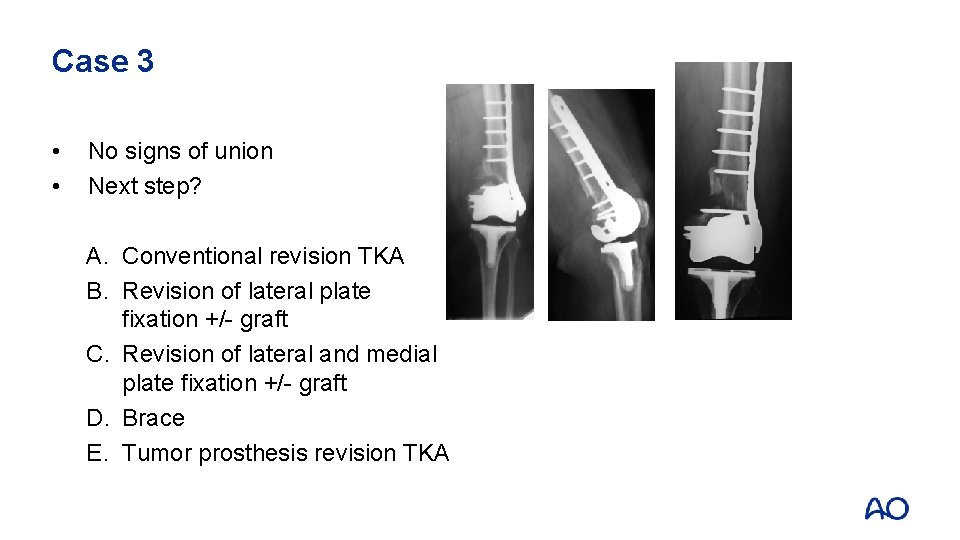
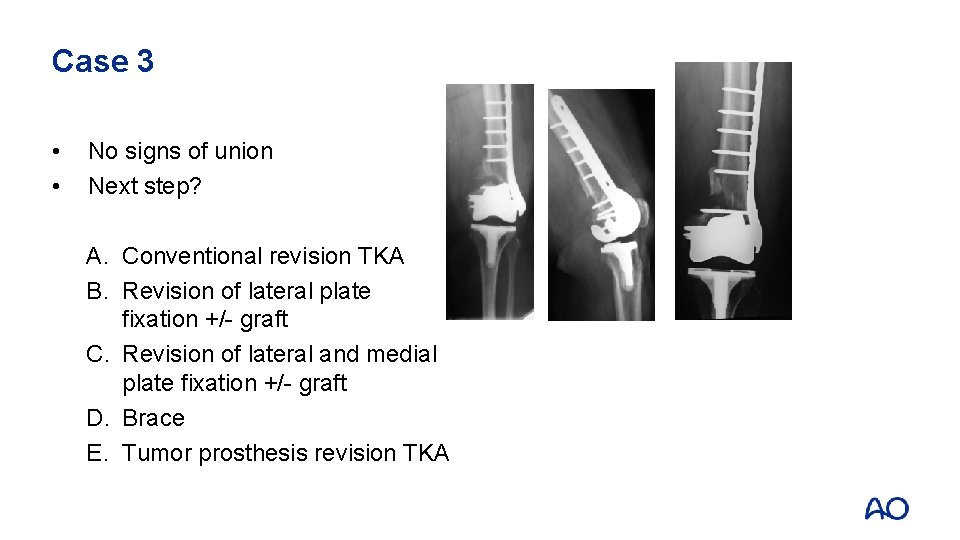
Case 3 • • No signs of union Next step? A. Conventional revision TKA B. Revision of lateral plate fixation +/- graft C. Revision of lateral and medial plate fixation +/- graft D. Brace E. Tumor prosthesis revision TKA
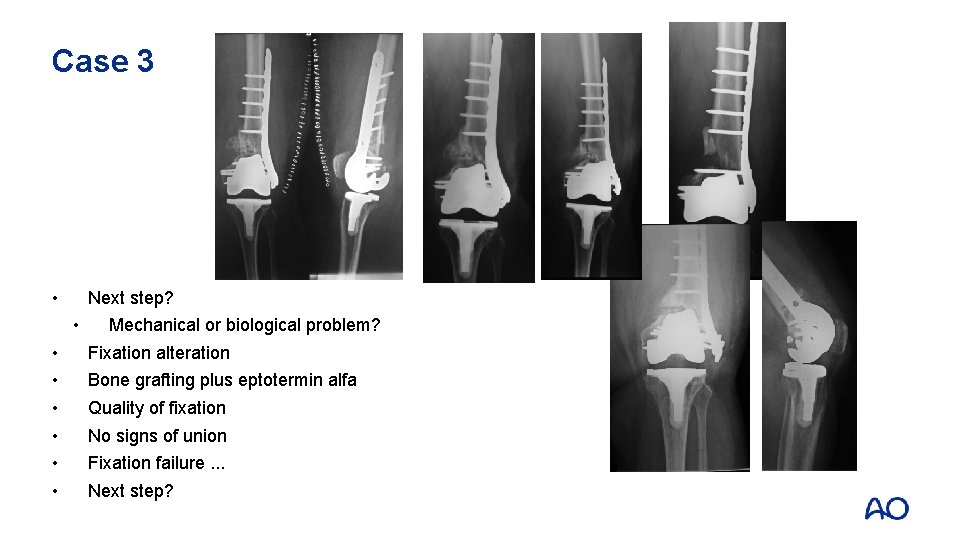
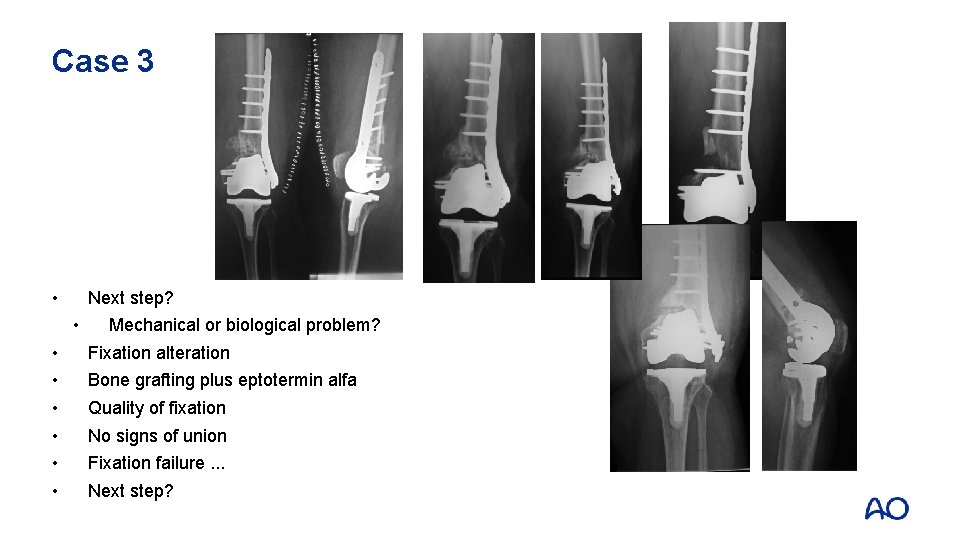
Case 3 • Next step? • • Mechanical or biological problem? Fixation alteration Bone grafting plus eptotermin alfa Quality of fixation No signs of union Fixation failure. . . Next step?
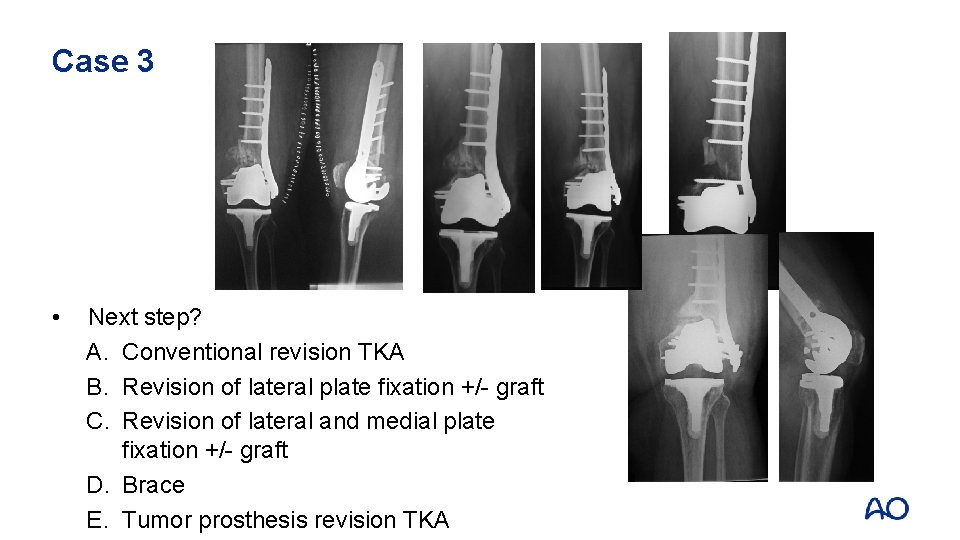
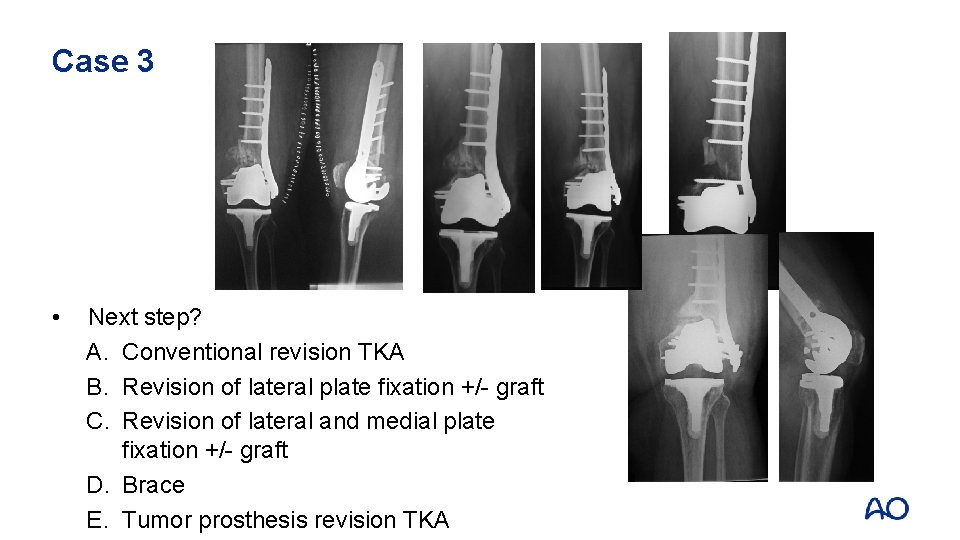
Case 3 • Next step? A. Conventional revision TKA B. Revision of lateral plate fixation +/- graft C. Revision of lateral and medial plate fixation +/- graft D. Brace E. Tumor prosthesis revision TKA
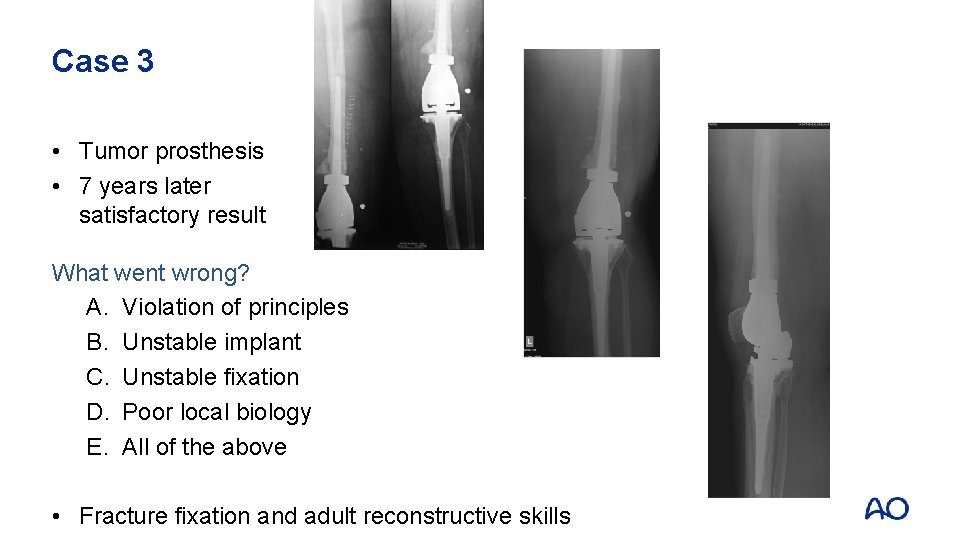
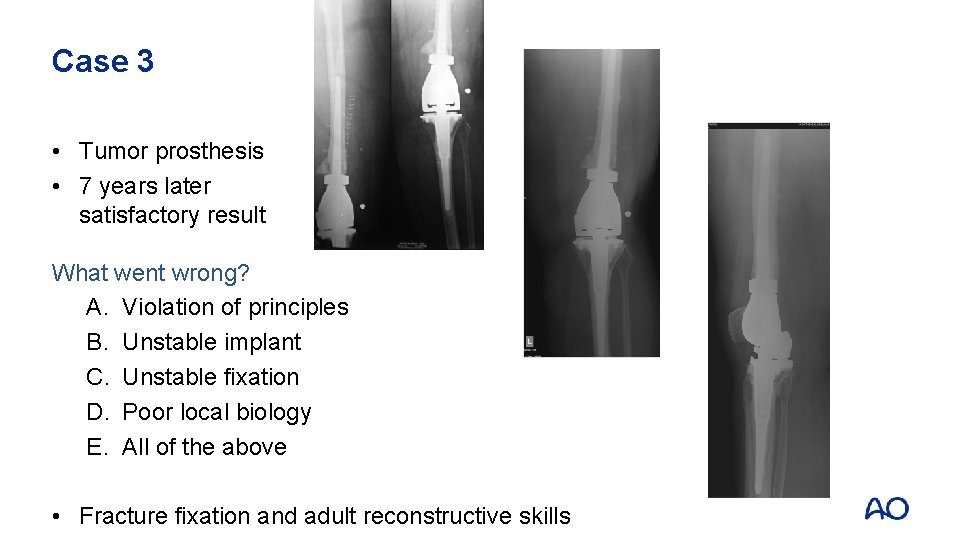
Case 3 • Tumor prosthesis • 7 years later satisfactory result What went wrong? A. Violation of principles B. Unstable implant C. Unstable fixation D. Poor local biology E. All of the above • Fracture fixation and adult reconstructive skills
Case 3: Take-home messages • Be aware of the unexpected and be prepared to react
 Occupational therapy intervention plan for hip arthroplasty
Occupational therapy intervention plan for hip arthroplasty Muscles that cross hip and knee
Muscles that cross hip and knee Hip hop hip to the hippity
Hip hop hip to the hippity Hip hippity hop
Hip hippity hop Arthroplasty practitioner
Arthroplasty practitioner Muscle around knee
Muscle around knee Passive sentence
Passive sentence What goes around comes around examples
What goes around comes around examples Martin luther king of hinduism
Martin luther king of hinduism A spill at parsenn bowl: knee injury and recovery
A spill at parsenn bowl: knee injury and recovery Chapter 16 worksheet the knee and related structures
Chapter 16 worksheet the knee and related structures Chapter 16 worksheet the knee and related structures
Chapter 16 worksheet the knee and related structures Knee joint origin and insertion
Knee joint origin and insertion Crib net restraint
Crib net restraint Locking muscle
Locking muscle Total knee replacement
Total knee replacement Locking and unlocking of knee joint
Locking and unlocking of knee joint Gastroncnemius
Gastroncnemius Hip and shoulder support water rescue
Hip and shoulder support water rescue Chapter 17 the thigh hip groin and pelvis
Chapter 17 the thigh hip groin and pelvis Rom of hip abduction
Rom of hip abduction Hip joint labelled
Hip joint labelled Chapter 17 the thigh hip groin and pelvis
Chapter 17 the thigh hip groin and pelvis Anatomy of the thigh hip groin and pelvis
Anatomy of the thigh hip groin and pelvis Hip and elbow dysplasia
Hip and elbow dysplasia Types of roof plan
Types of roof plan Waist and hip difference
Waist and hip difference Tweedesk
Tweedesk