THE HIP AND KNEE Anatomy Injuries THE HIP
















- Slides: 55

THE HIP AND KNEE Anatomy & Injuries
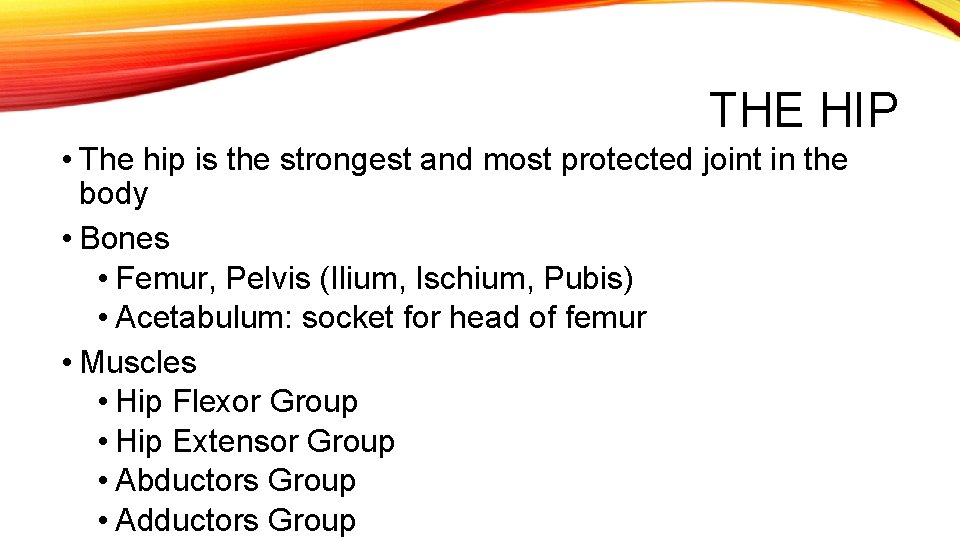
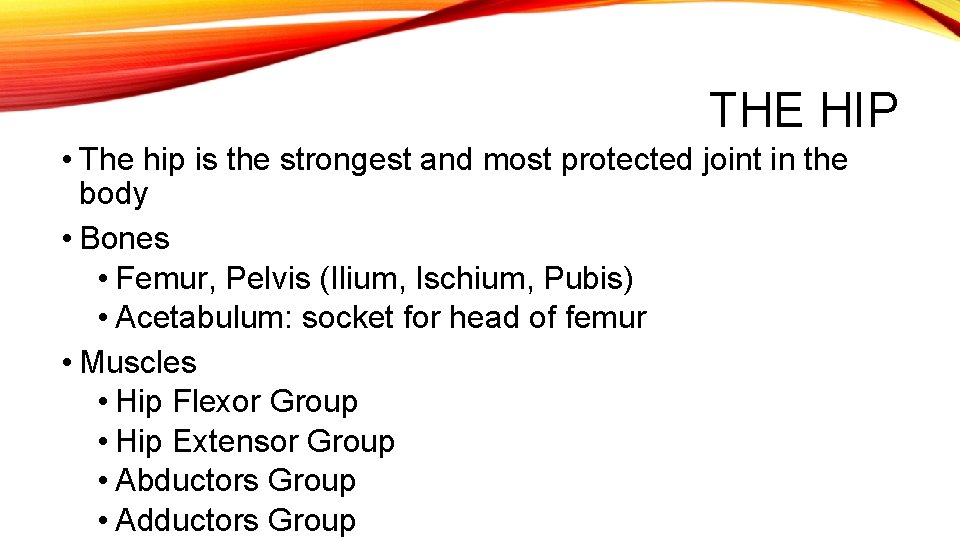
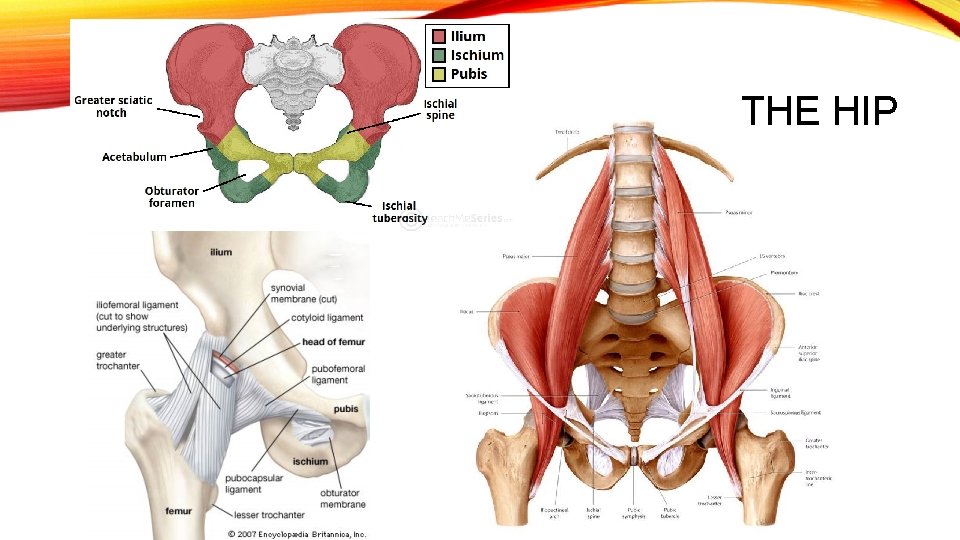
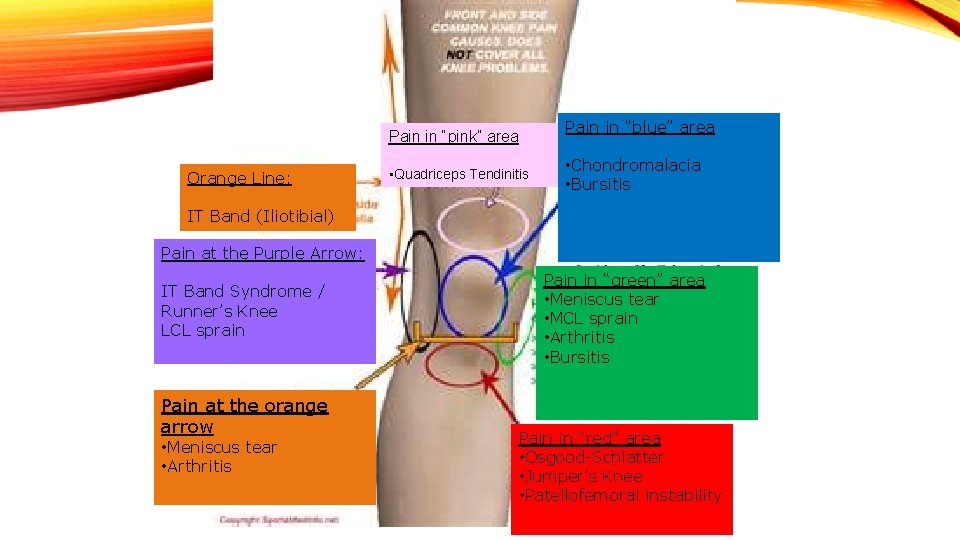
THE HIP • The hip is the strongest and most protected joint in the body • Bones • Femur, Pelvis (Ilium, Ischium, Pubis) • Acetabulum: socket for head of femur • Muscles • Hip Flexor Group • Hip Extensor Group • Abductors Group • Adductors Group
THE HIP
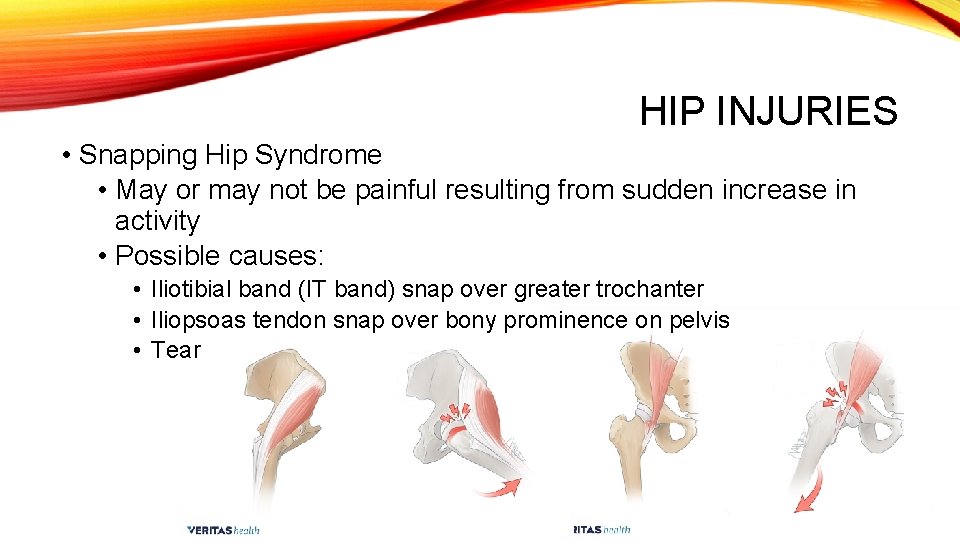
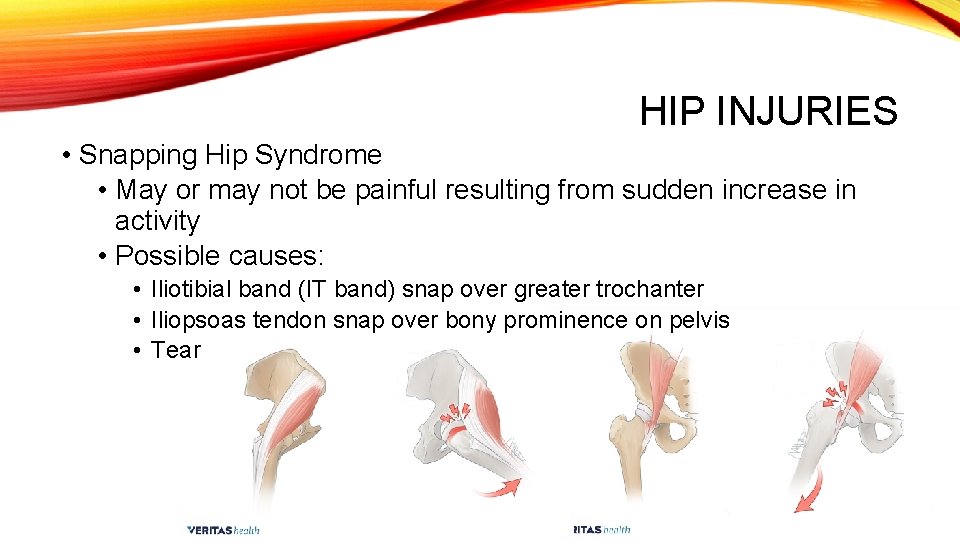
HIP INJURIES • Snapping Hip Syndrome • May or may not be painful resulting from sudden increase in activity • Possible causes: • Iliotibial band (IT band) snap over greater trochanter • Iliopsoas tendon snap over bony prominence on pelvis • Tear
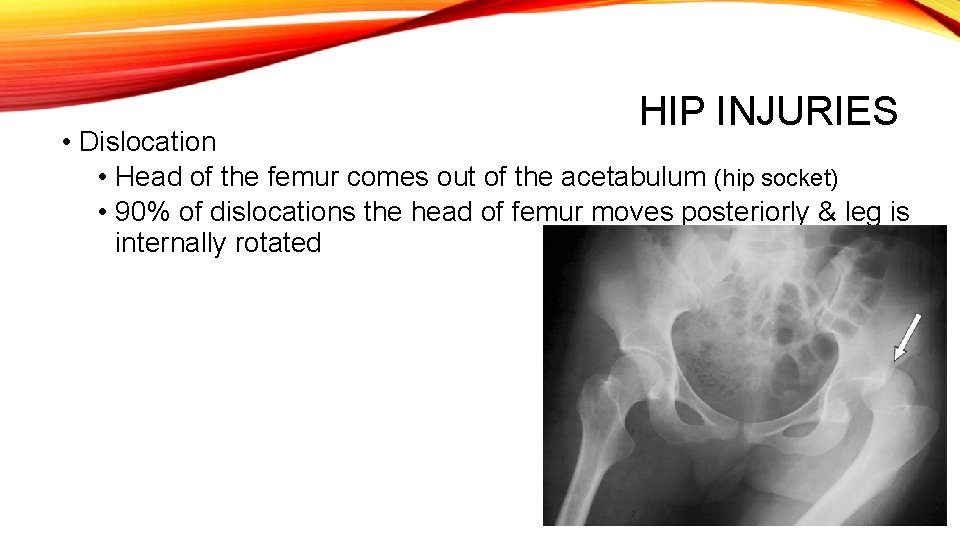
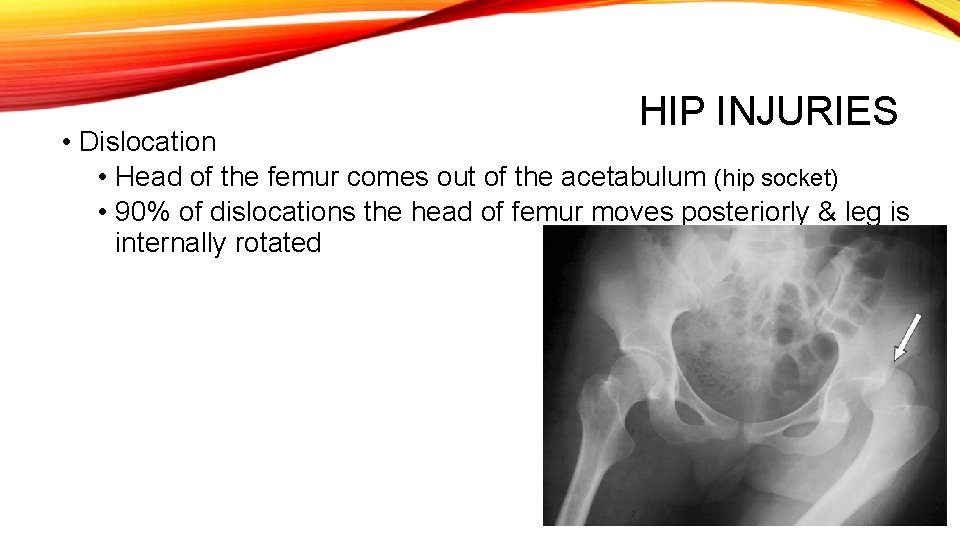
HIP INJURIES • Dislocation • Head of the femur comes out of the acetabulum (hip socket) • 90% of dislocations the head of femur moves posteriorly & leg is internally rotated
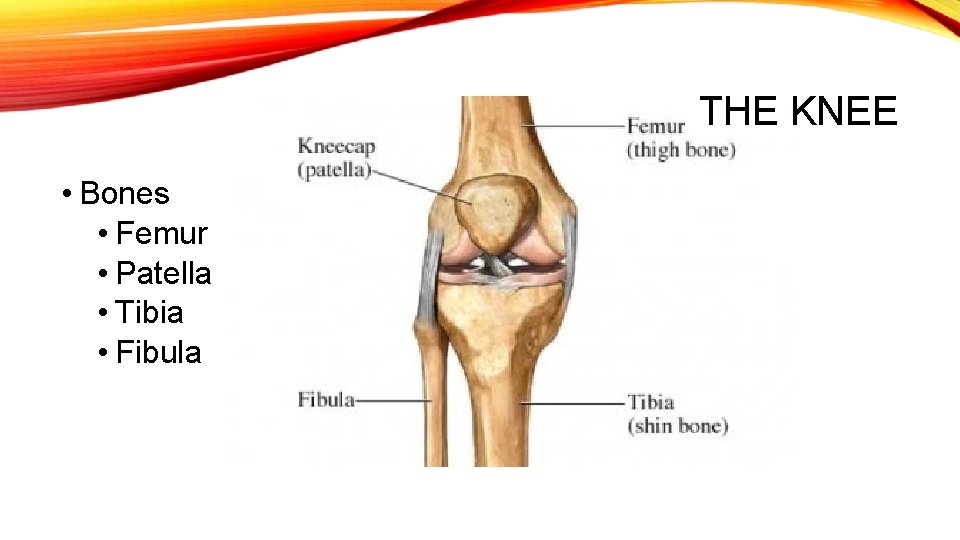
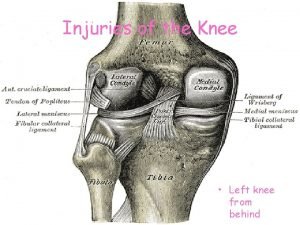
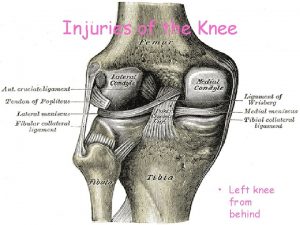
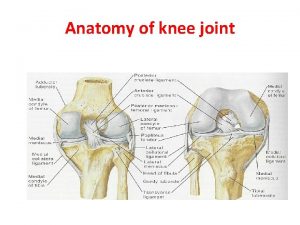
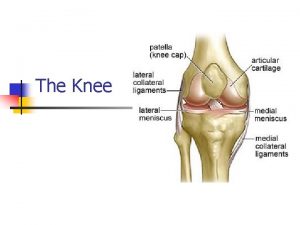
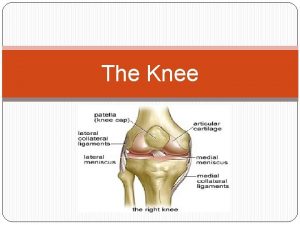
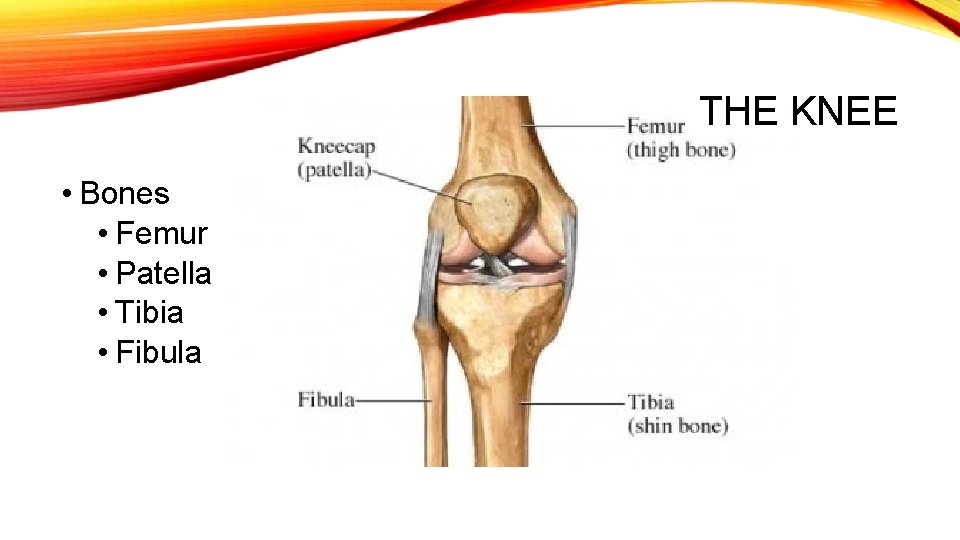
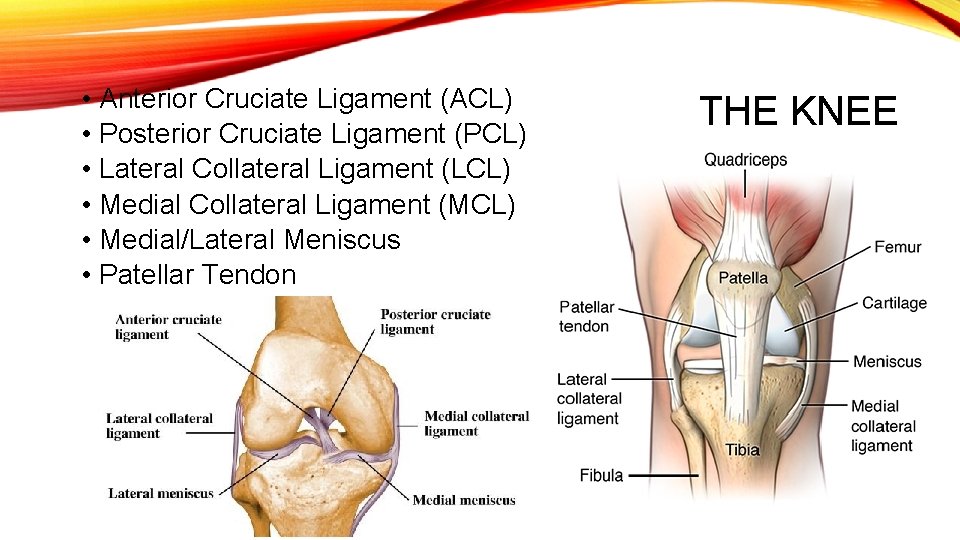
THE KNEE • Bones • Femur • Patella • Tibia • Fibula
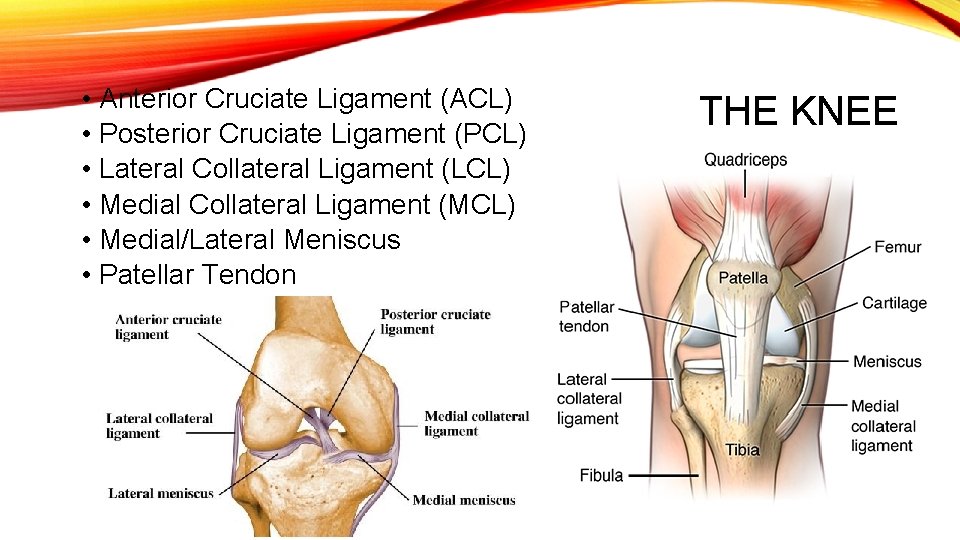
• Anterior Cruciate Ligament (ACL) • Posterior Cruciate Ligament (PCL) • Lateral Collateral Ligament (LCL) • Medial Collateral Ligament (MCL) • Medial/Lateral Meniscus • Patellar Tendon THE KNEE

KNEE INJURIES Acute and Chronic
LIGAMENTS: ACUTE INJURIES! • MCL: Contact • LCL : Contact • ACL: Contact/Noncontact • PCL: Contact

Grade Stretching of ligament; pain but minimal laxity and solid endpoint 1 LIGAMENT INJURIES Grade Partial Tear; laxity with solid endpoint; pain 2 Grade Total Tear; instability; no endpoint; pain; 911 call 3
PREVENTION OF ACUTE INJURIES • Strengthen all muscles surrounding hip/knee • Increase core stability • Check playing field for divots, slick spots, debris • Check length of cleats for turf and grass • Knee braces for lineman and previous injuries

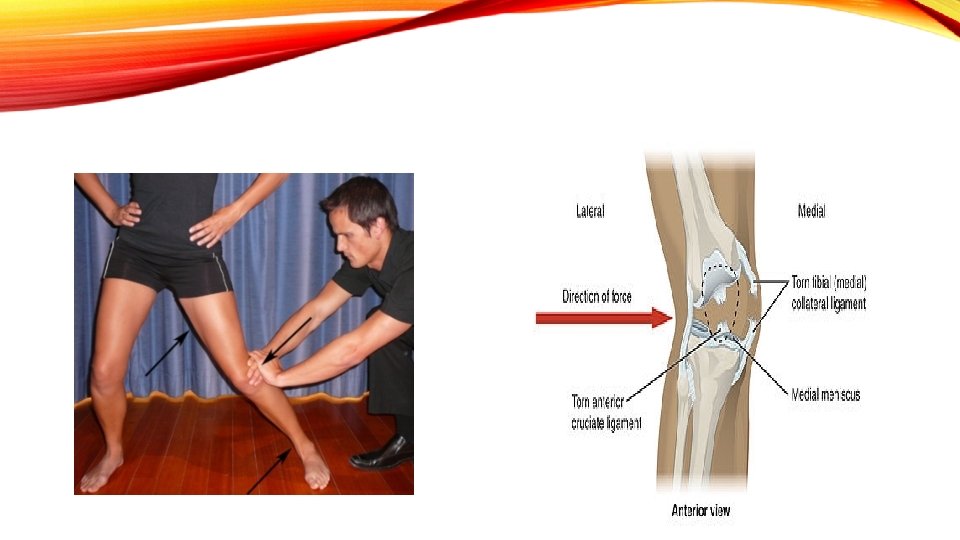
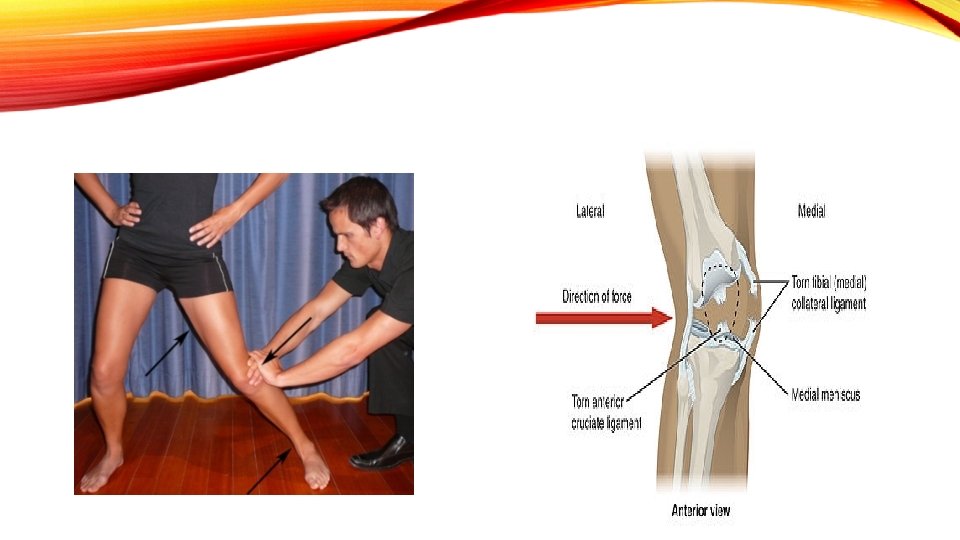
MCL INJURY Mechanism: Valgus Stress to outside of knee; direct contact Signs/Symptoms: Pain, swelling of medial knee Special Test: Valgus Stress Test https: //www. youtube. com/watch? v=j_Ke 0 bms. JXE Braced and Rehab: nonsurgical unless other structures are damaged


MCL INJURY INCREASES RISK OF INJURY AND ACL!

MCL VIDEOS • https: //www. youtube. com/watch? v=Iwaw. Zytom. OI • https: //www. youtube. com/watch? v=h 32 v 3 Ih. Dw. CA
https: //www. youtube. com/watch? v=etjao_65 Kp 0 Positive Valgus Stress test for MCL Tear
LCL INJURY • Mechanism: Varus Stress to Outside of knee • Signs and Symptoms: Pain, swelling over LCL near fibular head; positive stress test ; rule out a fibular fracture with an x-ray • Special Test: Varus Stress Test

Varus Stress Test
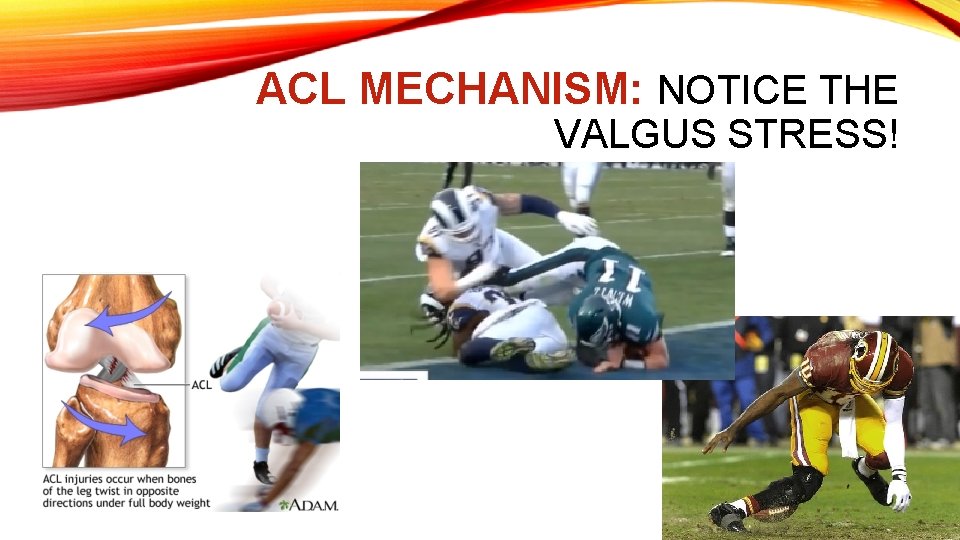
ANTERIOR CRUCIATE INJURY • Mechanism: • Noncontact: attempted deceleration and direction change • Contact: Valgus force to outside of knee • Signs/Symptoms: Hear a loud “POP”; sensation of the knee giving way or shifting; massive swelling in joint • Special Tests: Positive Anterior Drawer, Lachman’s Pivot Shift (Pivot Shift is best done under anesthesia)
ACL • Can never be repaired on its own!! A new ligament must be surgically inserted between Tibia and Femur • Allograft: Cadaver • Autograft: Patient’s own patella or hamstring tendon • Noncontact ACL Injury is greater in women
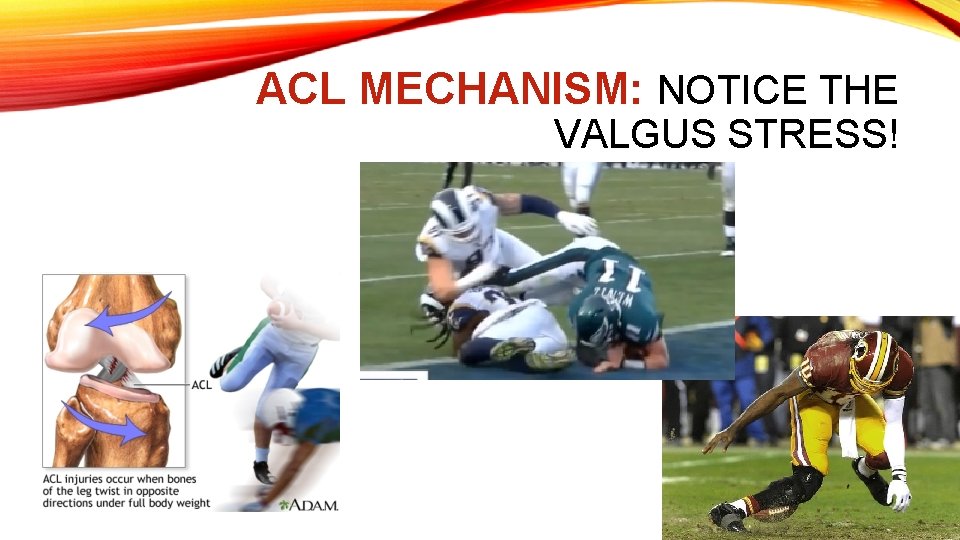
ACL MECHANISM: NOTICE THE VALGUS STRESS!
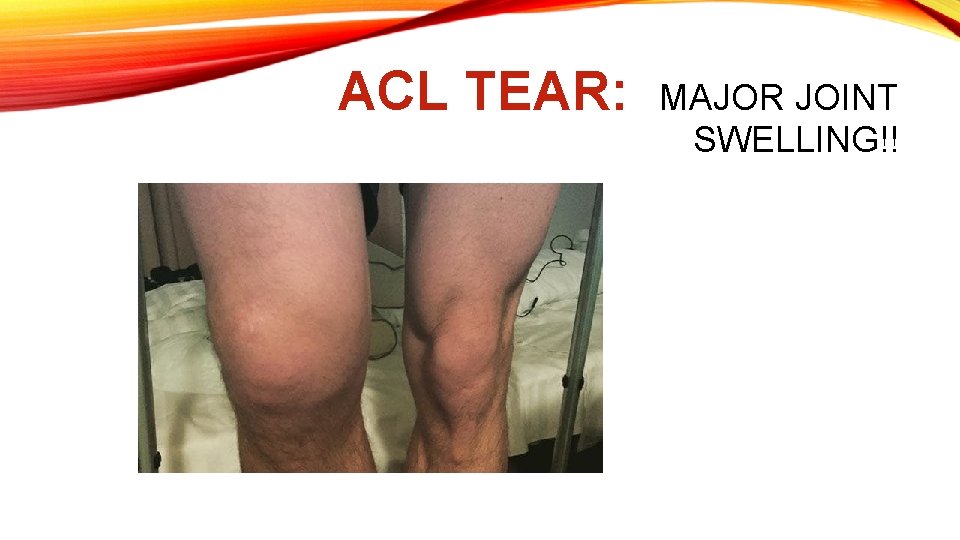
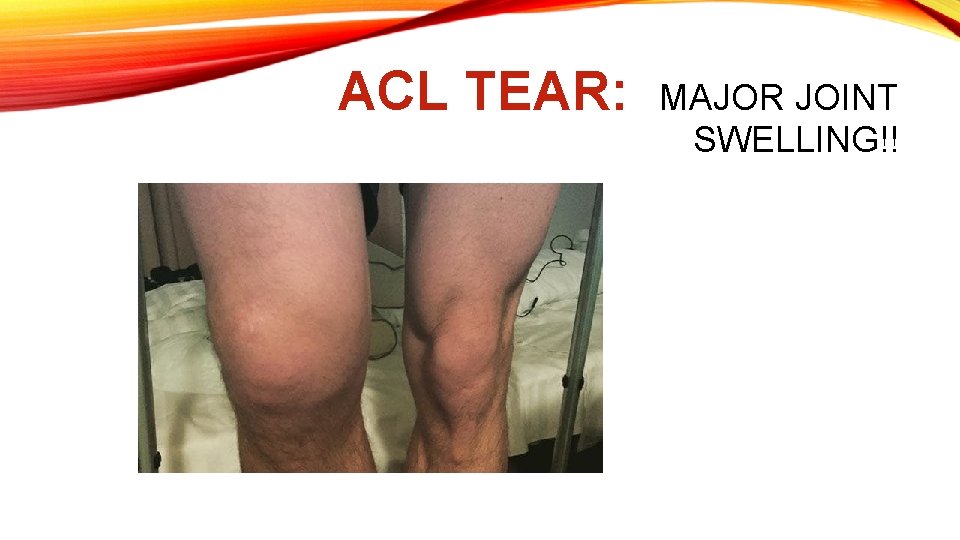
ACL TEAR: MAJOR JOINT SWELLING!!
ACL PREVENTION AND MECHANISM • https: //www. youtube. com/watch? v=Pls 9 Gn. ANx. Wc • https: //www. youtube. com/watch? v=O 0 Kegyyvf. FM • https: //www. youtube. com/watch? v=d. LXo. A 9 d 07 WI • https: //www. youtube. com/watch? v=7 Lag 8 u. NU 6 AQ
• https: //www. youtube. com/watch? v=26 v. Vvyz. AGL 4&index=10&list=PLd. Iv. SPXS 3 UEP oy. SV 5 fx_kobx 18 gwrq. Q 15 • Autograft vs allograft • https: //www. youtube. com/watch? v=gmg 1 id. YLt. Hk&index=9&list=PLd. Iv. SPXS 3 UEPo y. SV 5 fx_kobx 18 gwrq. Q 15 • What if I do not want surgery?
• Positive Lachmans test • https: //www. youtube. com/watch? v=o. FWjwx. JJmm. Q • Positive Anterior Drawer Test • https: //www. youtube. com/watch? v=TX 1 cm 8 jzh. HQ
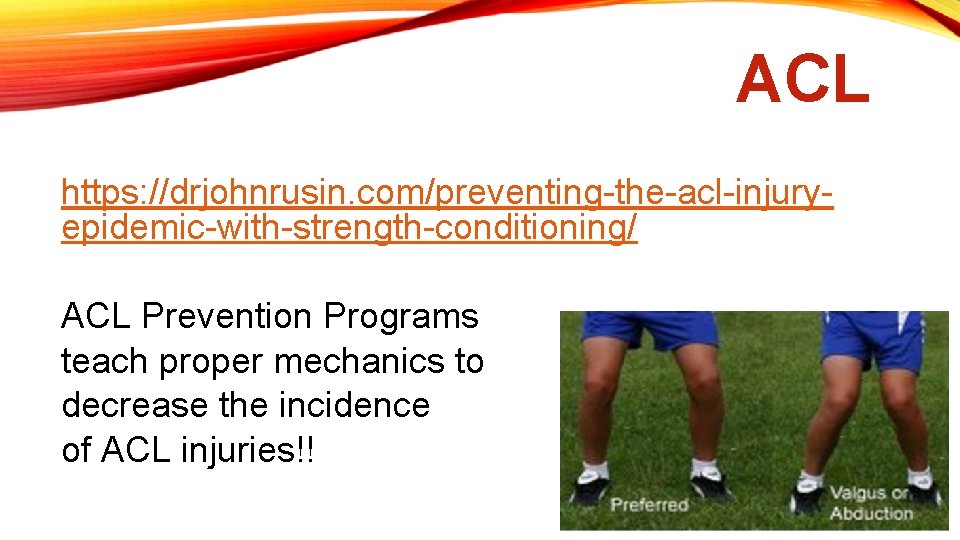
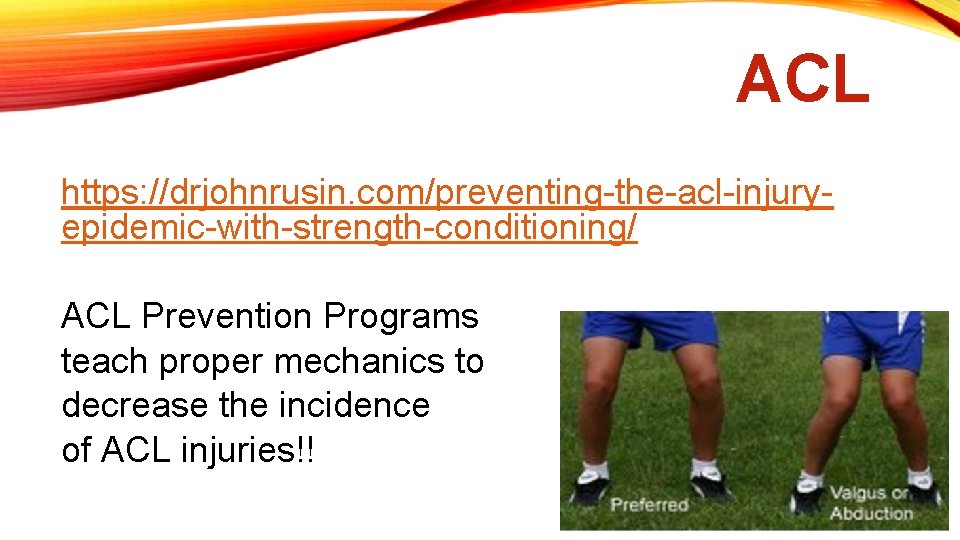
ACL https: //drjohnrusin. com/preventing-the-acl-injuryepidemic-with-strength-conditioning/ ACL Prevention Programs teach proper mechanics to decrease the incidence of ACL injuries!!
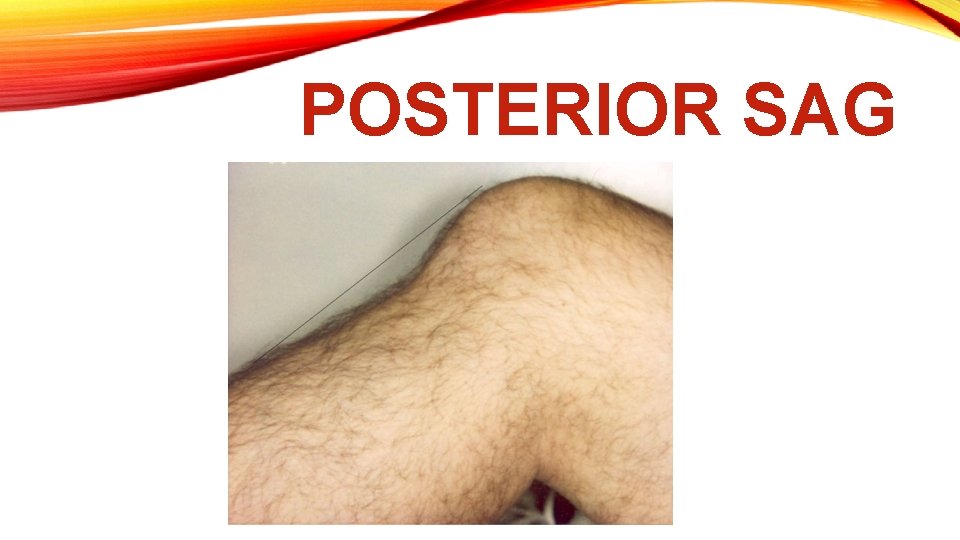
POSTERIOR CRUCIATE LIGAMENT • Mechanism: Fall or hit on Anterior Aspect of bent knee • Signs/Symptoms: Tenderness and swelling within popliteal fossa (knee pit/back of knee); pop • Special Tests: Positive Posterior Drawer/Lachmans • Signs: Posterior Sag/Godfrey’s Sign • Replace or rehab? Not as crucial to stability as ACL
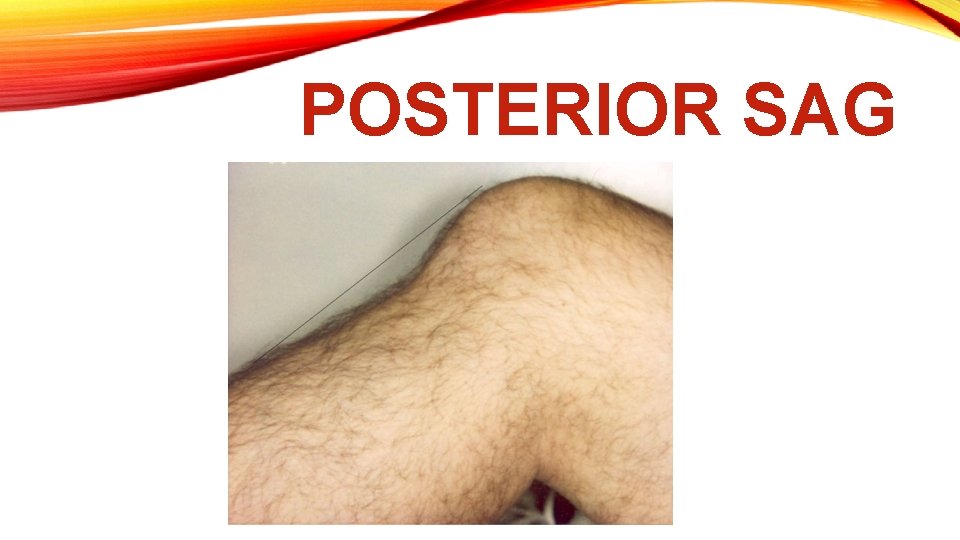
POSTERIOR SAG

MY TORN PCL MRI
• https: //www. youtube. com/watch? v =28 m. JFy. HMXHo • Positive Posterior Drawer test
MENISCUS INJURY • https: //www. youtube. com/watch? v=Rm. Wg. PP 4 Y 7 QY • Info! • https: //www. youtube. com/watch? v=8 Ks. G 3 Mtm. SFA • Surgery or not? • Repair or trim?
MENISCUS • Mechanism: Acute cutting; rotational force; or degeneration - overuse • Signs/Symptoms: Tenderness, swelling in joint line; swelling in popliteal fossa for posterior tear; knee feels as if it gets “locked”; lacks full extension/flexion; pain with squatting, positive stress tests • Special Tests: Mc. Murray’s; Apley’s Compression/Distraction and Duck Walk • Medial Meniscus is torn more often than lateral – prone to valgus stress and not very mobile; attached to deep part of MCL;
SPECIAL TESTS • Mc. Murray’s • • Apley’s Compression/Distraction • • Duck Walk •
CAN MENISCAL TEARS BE REPAIRED? • Outside edge of each meniscus: red/red zone – repairable • Inner portion is the avascular edge; unrepairable; white/white zone • Outside to inside: red/white zone – usually not repairable • Age consideration, location of tear – factors on whether to repair or remove. • Removal will be as little as possible to maintain function

DISLOCATIONS: TIBIAL FEMORAL AND PATELLAR • Tibial Femoral: Multiple Ligaments are torn! Could be combined with a fracture; massive pain, swelling, deformity call 911! • Rare in sports • Follow-up with orthopedic specialist
PATELLA FEMORAL DISLOCATION • Medially directed valgus force similar to mechanism for ACL • i. e athlete plants, decelerates and cuts in opposite direction • End result: Vastus lateralis pulls patella laterally – patella rests on lateral femoral condyle • Special Test: Patella Apprehension • 911 call! Reduction of dislocation must take place ASAP by a physican


PATELLAR TENDON RUPTURE • Mechanism: Eccentric( muscle is lengthening as it is contracting; landing after jumping) Contraction of Quads; violent motion • Also forceful blow and degeneration of tendon with age/injury and corticosteroid injections • Signs/Symptoms: Pain, swelling, deformity, loss of motion, athlete can’t extend lower leg or stand • Special Test: Can the athlete extend his/her lower leg? • Suture repair for total rupture; immobilization; rehab

QUAD TENDON/PATELLA TENDON RUPTURE
ACUTE INJURIES OF LIGAMENTS, MENISCUS, JOINT, PATELLAR TENDON • Must be evaluated by a physician • X-rays, MRI • Initial Rehabilitation by a physical therapist • Repairs, Immobilization, increase ROM, strength, proprioception, function • IMPRESS!!
CHRONIC INJURIES: DEVELOP OVER TIME • Patellar Tendinitis • Pes Anserine Tendinitis • Bursitis(although a fall can be acute – most commonly chronic) • Osgood Schlatter • Chondromalacia Patella (Patella Femoral Syndrome) • Iliotibial Band Syndrome
PATELLAR TENDINITIS • Jumper’s Knee: Inflammation of Patellar Tendon • Mechanism: Repetitive jumping, kicking, running (especially downhill) • Signs/Symptoms: Pain and tenderness over tendon near inferior border of patella; increased pain on deceleration and knee extensions against resistance. • Care: Rest, ice massage, strap/sleeve to alleviate stress, activity modification, gradual stretching, strengthening: be sure exercises are pain free
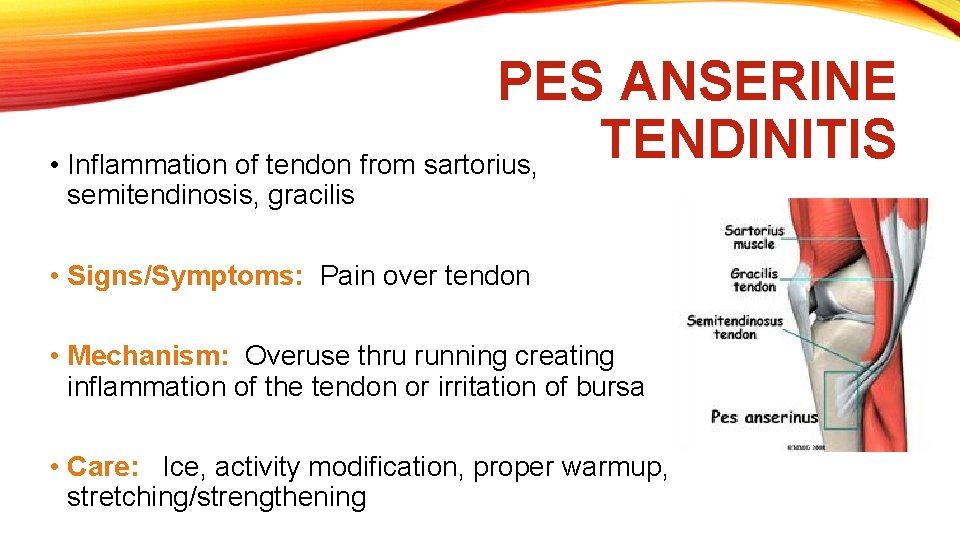
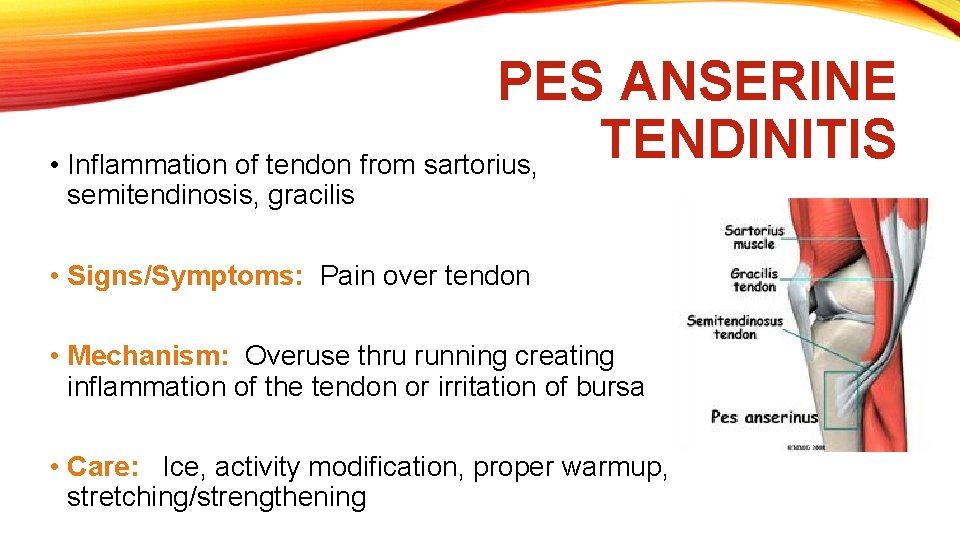
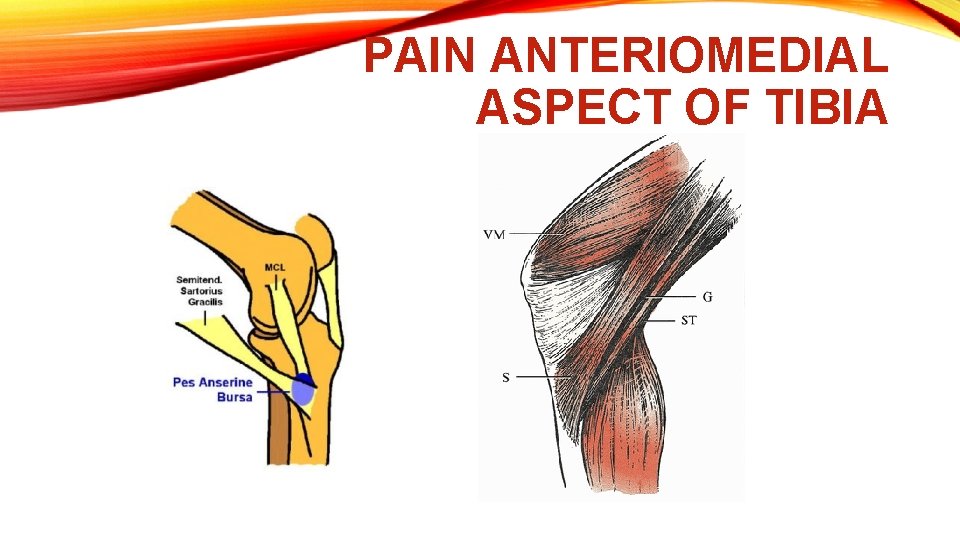
PES ANSERINE TENDINITIS • Inflammation of tendon from sartorius, semitendinosis, gracilis • Signs/Symptoms: Pain over tendon • Mechanism: Overuse thru running creating inflammation of the tendon or irritation of bursa • Care: Ice, activity modification, proper warmup, stretching/strengthening
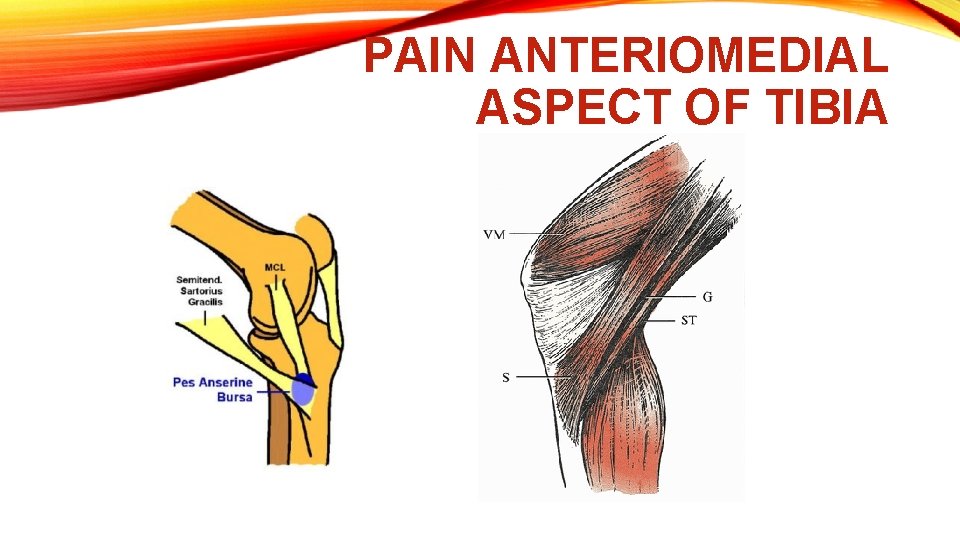
PAIN ANTERIOMEDIAL ASPECT OF TIBIA

BURSITIS: PREPATELLAR/INFRAPATELLAR • Mechanism: Continued kneeling(chronic); Fall – acute; infection • Signs/Symptoms: Localized swelling and pain outside of knee joint • Care: Activity modification, knee pads; may need to be aspirated by a physician • Prevention: Knee pads
OSGOOD-SCHLATTER • Mechanism: Overuse – Repeated pulls of the patella tendon at the tibial tuberosity during activities that require a lot of running, jumping, bending • Occurs during adolescence – 11 -15 yr olds; quads are stronger than bony insertion point; growth spurts • Signs/Symptoms: Pain on kneeling, jumping, running, and on contact swelling, point tenderness at tibial tuberosity; enlarged tuberosity • Care: Ice, rest , strap, c-shaped pad to disperse pressure activity modification – avoid kneeling, crawling, quick stops, starts, downhill running, direct contact • Stretching and strengthening as directed by PT

CHONDROMALACIA PATELLA (PATELLA FEMORAL SYNDROME) • Gradual degenerative change that occurs to the cartilage under patella and femur • Mechanism: Overuse; lateral patellar tracking – Increased quadriceps angle and weak vastus medialis muscle • Signs and Symptoms: Pain surrounding knee cap while walking, running, squatting, going up and down stairs, or sitting for long periods of time; swelling around knee cap; grating sensation; positive grind test • Care: Activity Modification; taping or sleeve to center knee cap, ice straight leg raises, mini squats to strengthen vastus medialis, increase quad and hamstring flexibility, raise bike seat to avoid deep knee flexion
ILIOTIBIAL BAND SYNDROME • Runner’s Knee • Iliotibial band creates friction as it slides over lateral femoral condyle • Mechanism: Overuse, poor footwear and uneven surfaces, anatomical abnormalities in foot and knee • Signs/Symptoms: Tenderness, mild swelling over lateral femoral condyle; pain increases during running and cycling • Care: Correction of alignment with shoe inserts(orthotics), proper warmup, stretching, avoid running on inclines (activity modification), ice massage

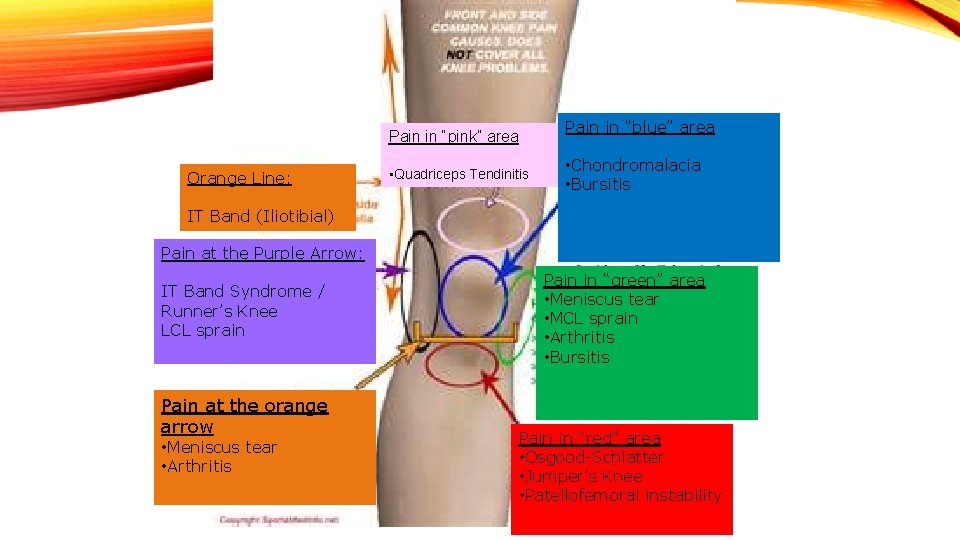
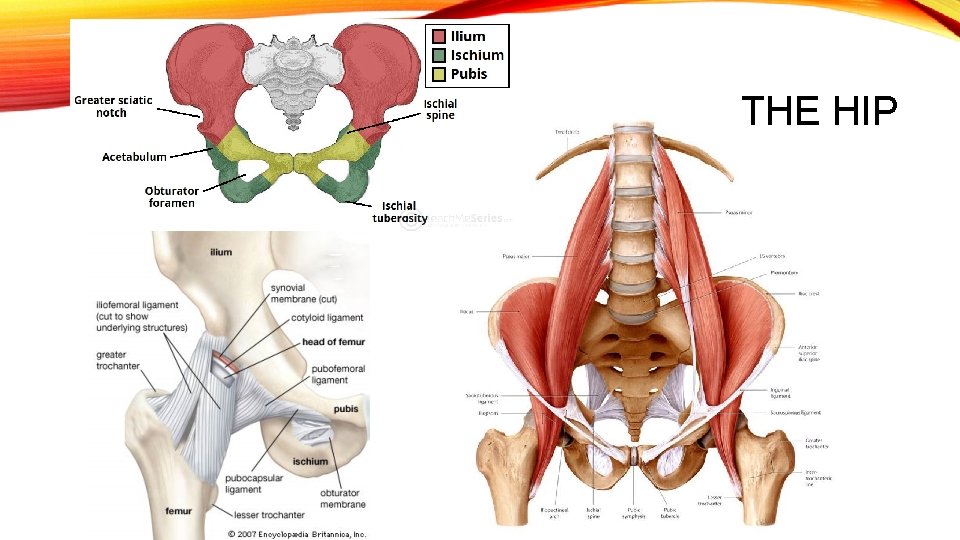
Pain in “blue” area Pain in “pink” area Orange Line: • Quadriceps Tendinitis • Chondromalacia • Bursitis IT Band (Iliotibial) Pain at the Purple Arrow: IT Band Syndrome / Runner’s Knee LCL sprain Pain at the orange arrow • Meniscus tear • Arthritis Pain in “green” area • Meniscus tear • MCL sprain • Arthritis • Bursitis Pain in “red” area • Osgood-Schlatter • Jumper’s Knee • Patellofemoral instability
SUMMARY: CHRONIC INJURIES • If condition doesn’t resolve in 7 -10 days, see a physician, physical therapist, athletic trainer • If condition worsens, seek medical help as well. • Ice after • Stretch and heat before workout • Activity modification – pain free • Rest • Rehab exercises for Hip, knee as directed by medical professional
 Muscles that cross hip and knee
Muscles that cross hip and knee Poem about hip hop
Poem about hip hop The hip to the hop to the hippity hop
The hip to the hop to the hippity hop Makenzie milton injury
Makenzie milton injury Knee anatomy chapter 16 worksheet 1
Knee anatomy chapter 16 worksheet 1 Knee surface anatomy palpation
Knee surface anatomy palpation Knee muscle anatomy
Knee muscle anatomy Femoral anteversion
Femoral anteversion Bryant üçgeni
Bryant üçgeni Unit 15:3 providing first aid for bleeding and wounds
Unit 15:3 providing first aid for bleeding and wounds Chapter 28 head and spine injuries
Chapter 28 head and spine injuries Chapter 21 caring for head and spine injuries
Chapter 21 caring for head and spine injuries Chapter 15 injuries to muscles and bones
Chapter 15 injuries to muscles and bones Chapter 14:1 using body mechanics
Chapter 14:1 using body mechanics Jones and bartlett learning
Jones and bartlett learning Chapter 13:2 preventing accidents and injuries
Chapter 13:2 preventing accidents and injuries Chapter 11 assessment and evaluation of sports injuries
Chapter 11 assessment and evaluation of sports injuries Chapter 12 lesson 4 fitness safety and avoiding injuries
Chapter 12 lesson 4 fitness safety and avoiding injuries Common track and field injuries
Common track and field injuries How are sports injuries classified and managed
How are sports injuries classified and managed Tim madsen everest
Tim madsen everest How is katniss in peeta’s debt again?
How is katniss in peeta’s debt again? Sentinel injuries
Sentinel injuries Westfield sports injuries
Westfield sports injuries Minor injuries unit stobhill
Minor injuries unit stobhill This needed three or more rescuers to form a hammock
This needed three or more rescuers to form a hammock 17:3 providing first aid for bleeding and wounds
17:3 providing first aid for bleeding and wounds Chapter 11 injuries to the shoulder region
Chapter 11 injuries to the shoulder region Tnt swimming
Tnt swimming Uc davis web scheduler
Uc davis web scheduler An epidemiologic survey of roller skating injuries
An epidemiologic survey of roller skating injuries Jsp 539
Jsp 539 Climatic injuries
Climatic injuries Chapter 4 preventing injuries through fitness
Chapter 4 preventing injuries through fitness Chapter 13 worksheet recognizing different sports injuries
Chapter 13 worksheet recognizing different sports injuries Chapter 4 basics of tissue injuries
Chapter 4 basics of tissue injuries Bo taoshi injuries
Bo taoshi injuries Torn lateral miniscus
Torn lateral miniscus Preventing hand injuries
Preventing hand injuries Battering intentional or unintentional
Battering intentional or unintentional How to make fake skin with vaseline and cornstarch
How to make fake skin with vaseline and cornstarch Intentional fallacy example
Intentional fallacy example Injury prevention, safety and first aid
Injury prevention, safety and first aid Emergency care and first aid ppt
Emergency care and first aid ppt Injuries first aid
Injuries first aid Characters of firearm injuries
Characters of firearm injuries Which osha document summarizes occupational injuries
Which osha document summarizes occupational injuries Sports injuries angus, on
Sports injuries angus, on Fundamentals of throwing a football
Fundamentals of throwing a football What does jem realize when he pounds the rail
What does jem realize when he pounds the rail How is dehydration affecting katniss
How is dehydration affecting katniss Chop saw injuries
Chop saw injuries Deadly dozen itls
Deadly dozen itls Clinton achilles tendonitis
Clinton achilles tendonitis A spill at parsenn bowl: knee injury and recovery
A spill at parsenn bowl: knee injury and recovery Chapter 16 worksheet the knee and related structures
Chapter 16 worksheet the knee and related structures