Family Medicine Gait Analysis Knee Injuries FootAnkle Injuries































- Slides: 95
Family Medicine: Gait Analysis, Knee Injuries, Foot/Ankle Injuries and Overuse Injuries Selina Silva, MD Associate Professor, Pediatric Orthopaedics Medical Director, UNM Carrie Tingley Hospital

Outline • • Gait Analysis Knee injuries Foot/Ankle injuries Pediatric overuse injuries
Gait Analysis • Can be informal with clinical evaluation of gait during a routine visit • Tip: have child walk in hallway if they are older. Easier to see abnormalities. • Can also get formal gait analysis in a gait laboratory.
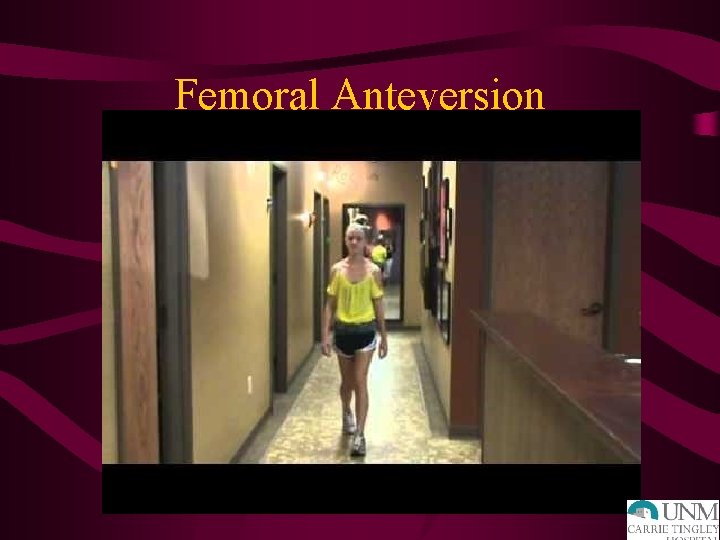
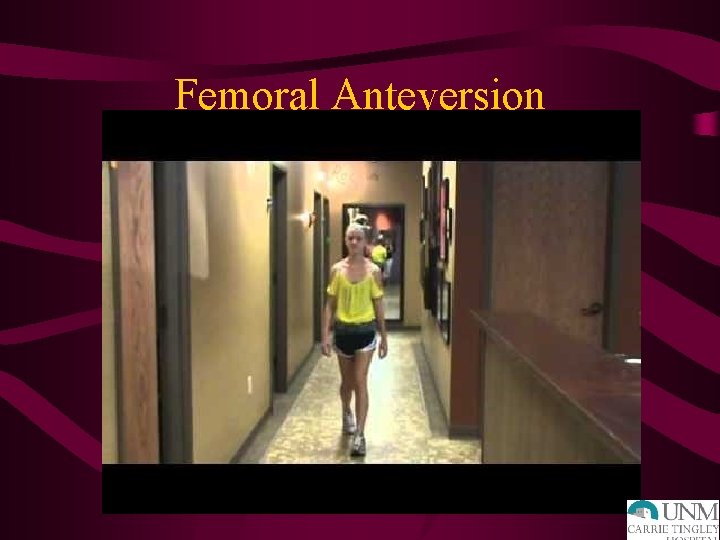
Femoral Anteversion
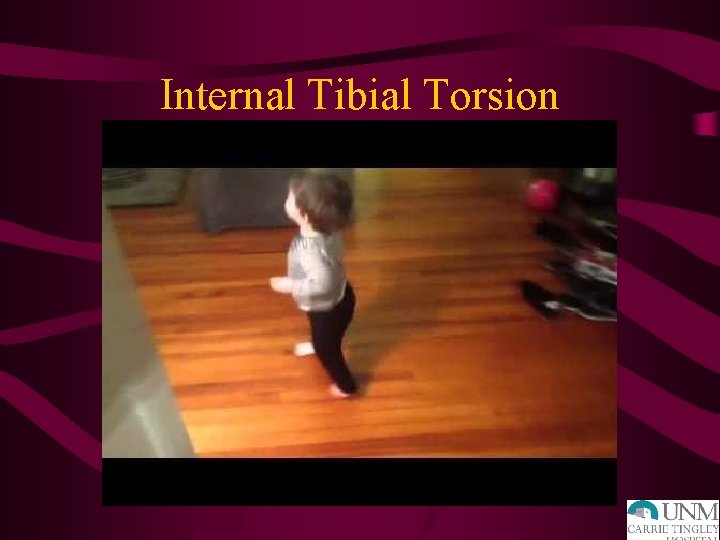
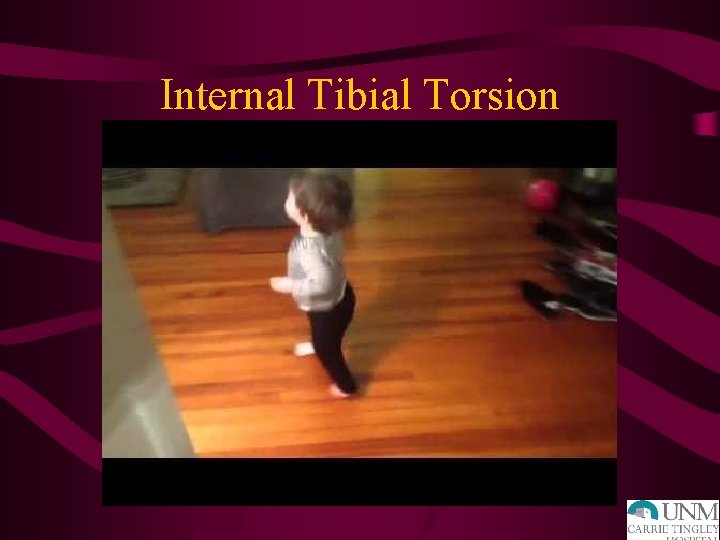
Internal Tibial Torsion
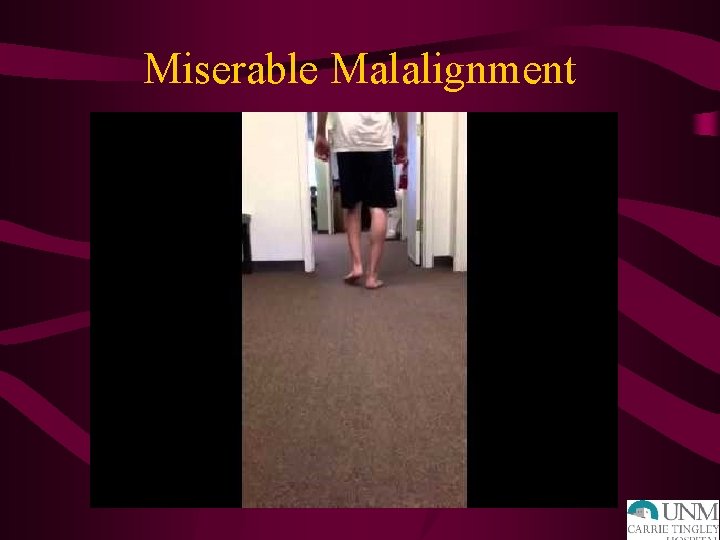
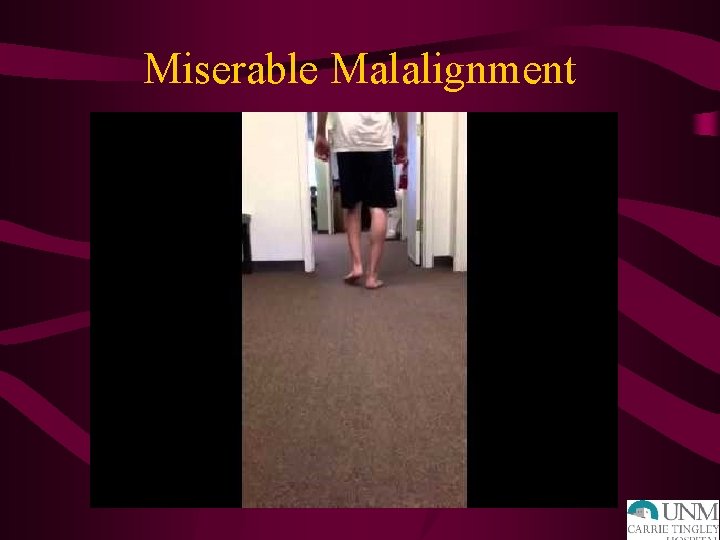
Miserable Malalignment

Miserable Malalignment
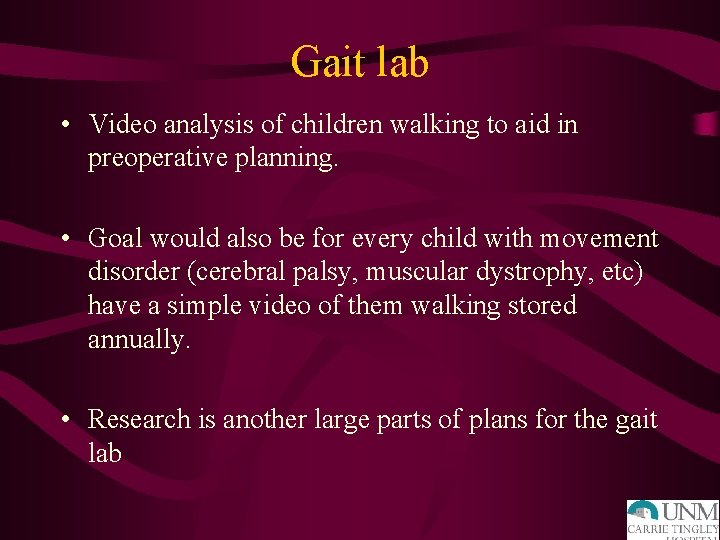
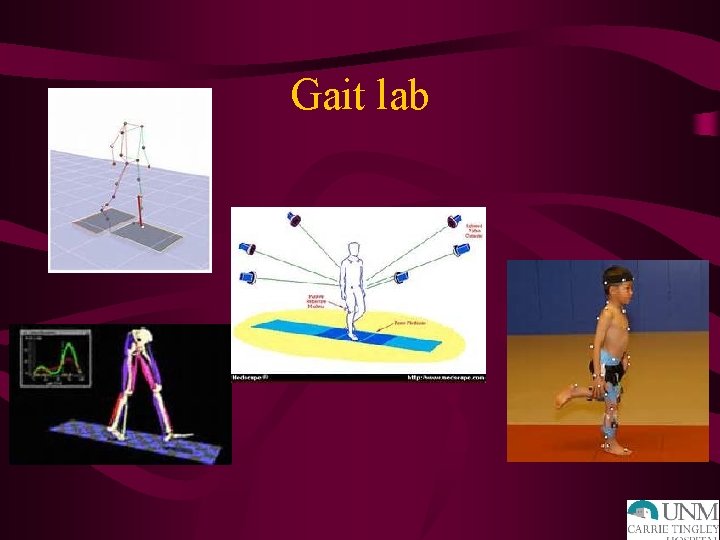
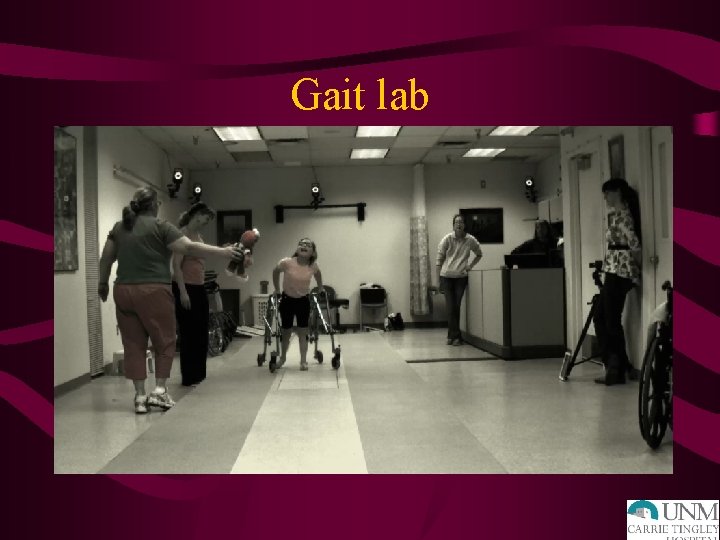
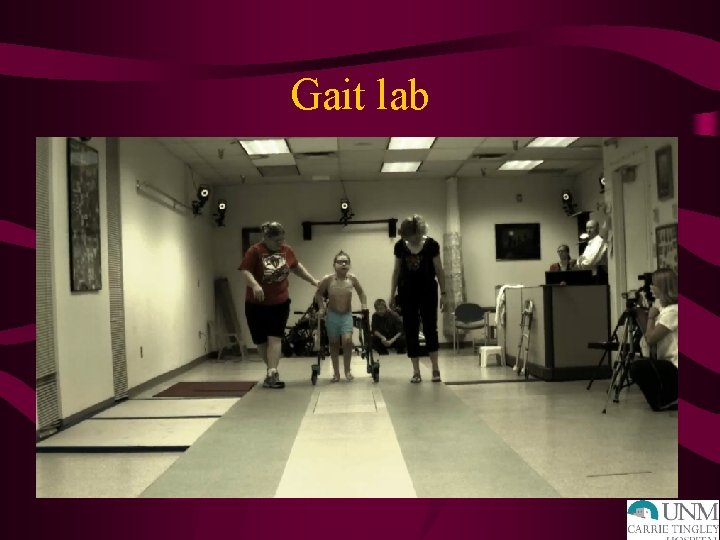
Gait lab • Video analysis of children walking to aid in preoperative planning. • Goal would also be for every child with movement disorder (cerebral palsy, muscular dystrophy, etc) have a simple video of them walking stored annually. • Research is another large parts of plans for the gait lab
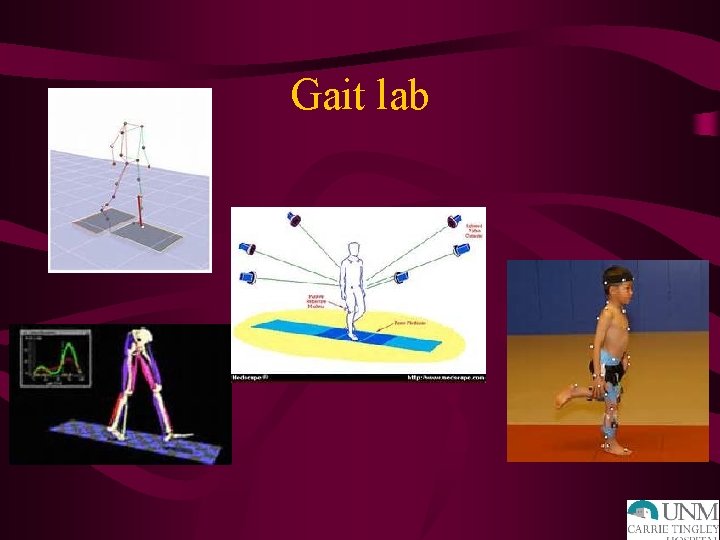
Gait lab
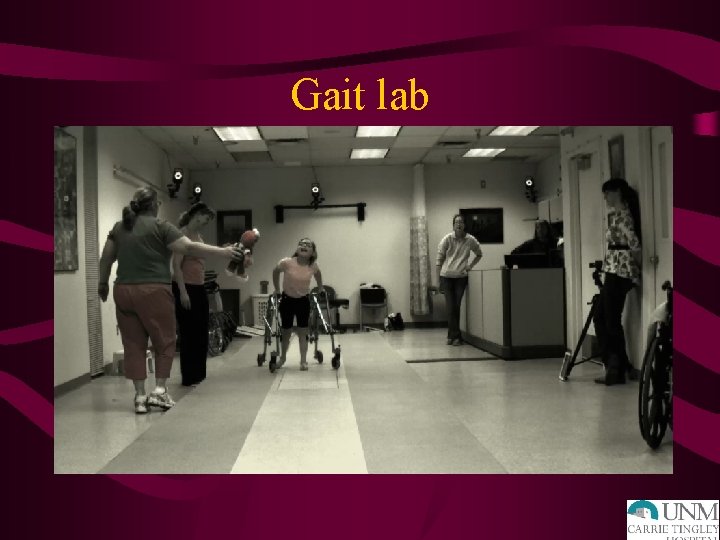
Gait lab

Gait lab
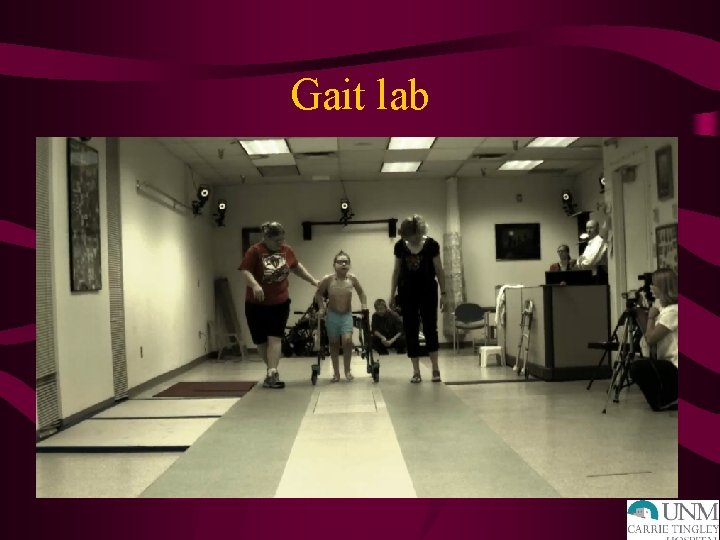
Gait lab
Gait lab

Knee Injuries • • • Anatomy and Physical Exam ACL MCL Patella Dislocations
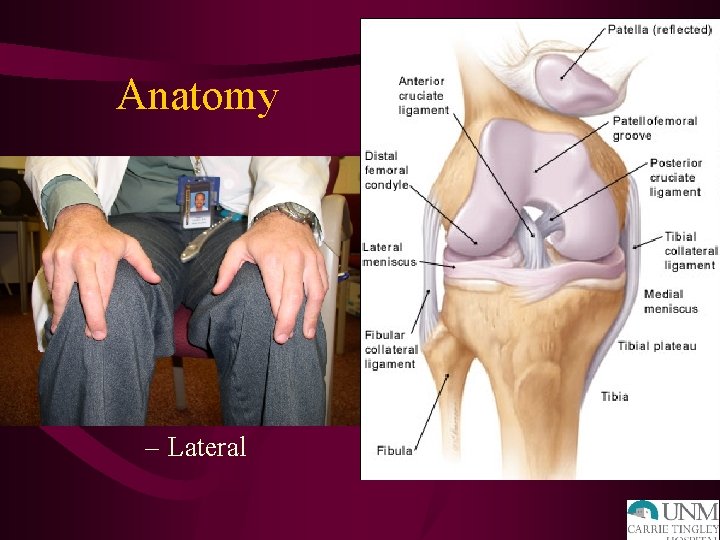
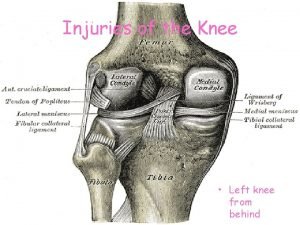
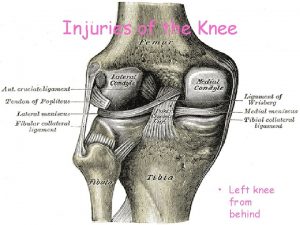
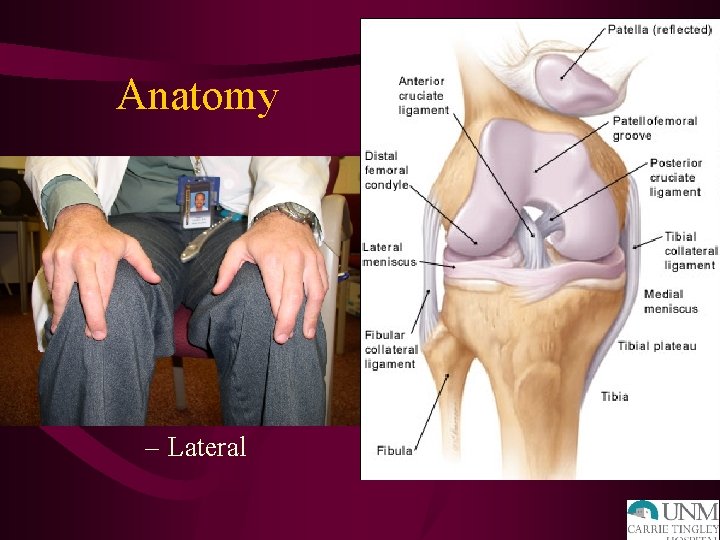
Anatomy • • • ACL PCL MCL LCL Meniscus – Medial – Lateral
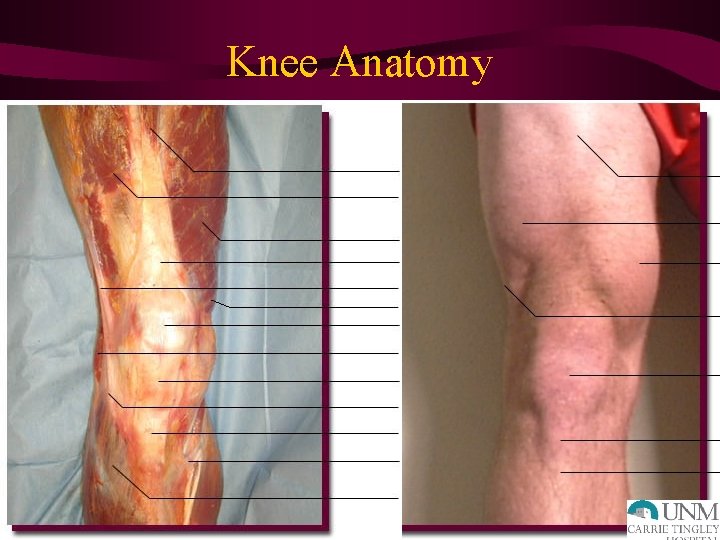
Knee Anatomy
Physical Exam of the Knee • Inspection • Palpation • Range of Motion • Special tests • Neurovascular assessment
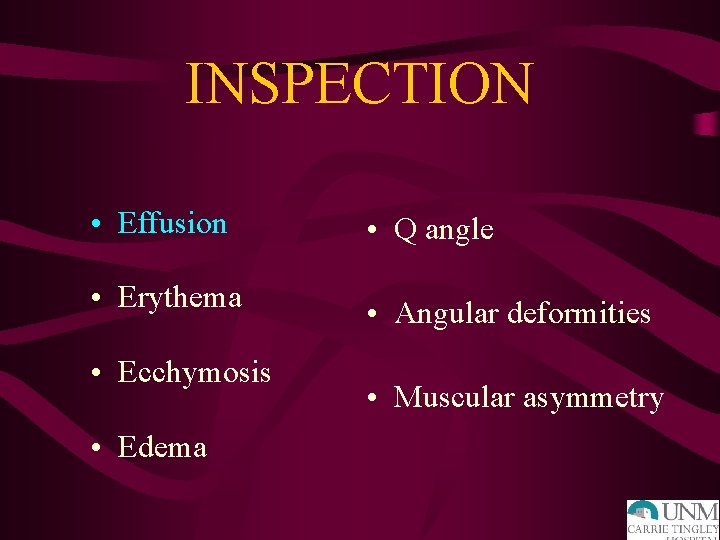
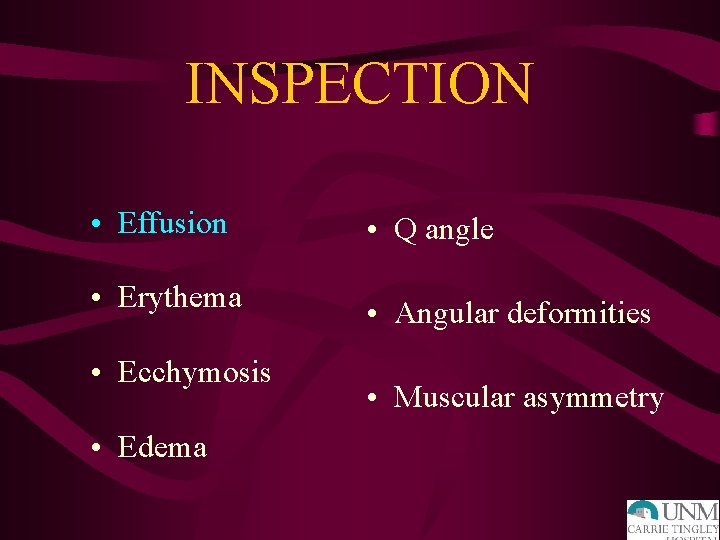
INSPECTION • Effusion • Q angle • Erythema • Angular deformities • Ecchymosis • Edema • Muscular asymmetry

PALPATION ANTERIOR MEDIAL • Tibial tubercle • MCL • Infrapatellar tendon • Meniscus • Quad insertion • Pes anserine insertion • Patellar facets • Tibial plateau • Crepitus ? • Femoral condyle
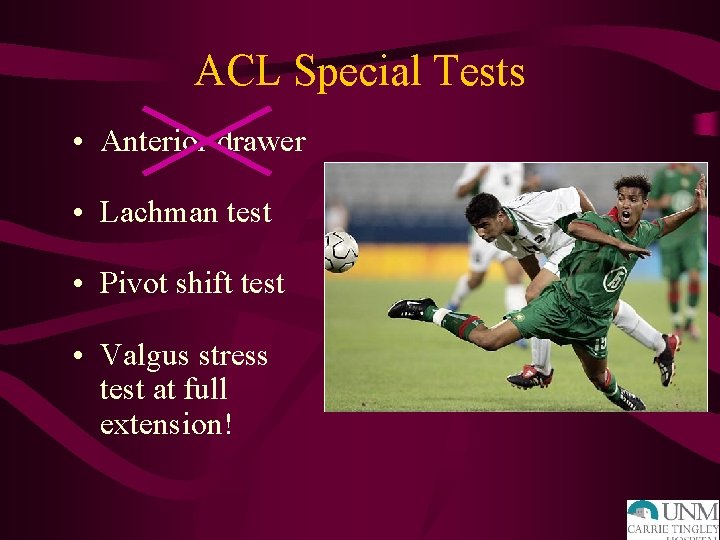
ACL Special Tests • Anterior drawer • Lachman test • Pivot shift test • Valgus stress test at full extension!

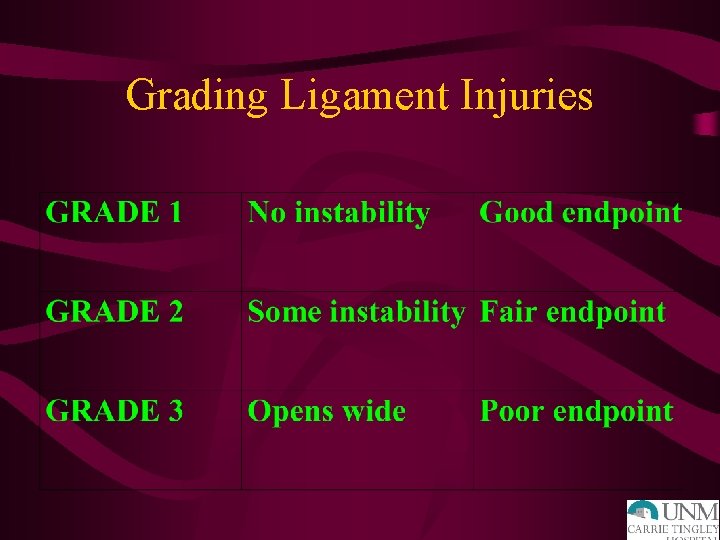
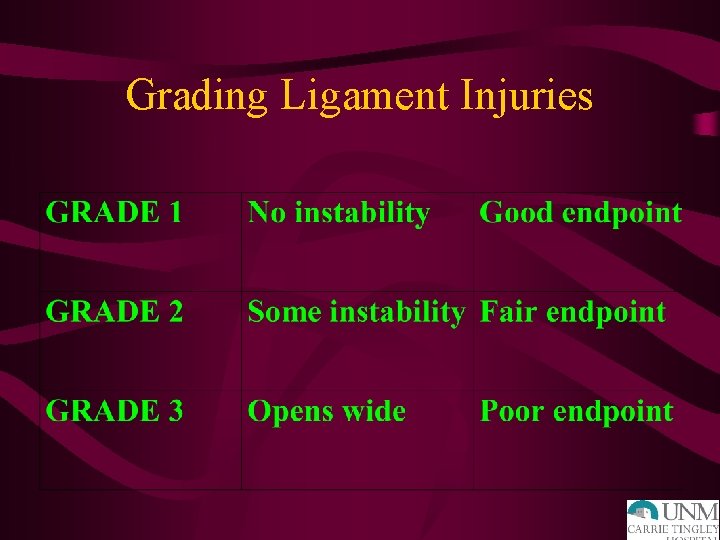
Grading Ligament Injuries

ACL: PHYSICAL EXAM • Decreased ROM • Effusion-hemarthrosis, immediate • + Instability tests – Lachman: most accurate – Pivot shift – Anterior drawer • + MCL and meniscus tests

LIGAMENT INJURIES: XRAY • AP – Lateral capsular sign: Segond fx – Tibial spine avulsion fx – Physeal injuries • Lateral – Lateral condyle divot – Obliques ? • Tangential (Merchant)

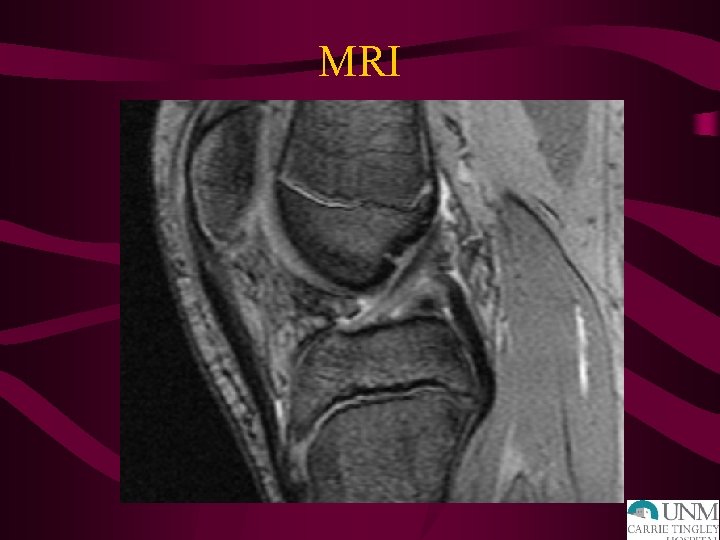
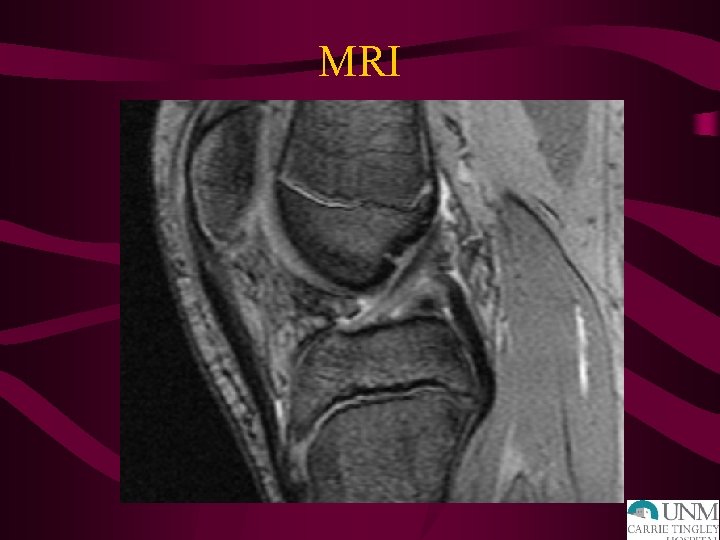
MRI
ACL TREATMENT • Grade 3 Injuries- Surgery • Indications – Most active people will require surgery to restore adequate function and decrease instability – Recurrent instability – Inability to modify activity – Associated injuries: meniscus – Age? • Wait three weeks due to arthrofibrosis risk • 100% @ 6 -12 months
MCL INJURIES HISTORY • Mechanism = valgus stress • Medial joint line pain • Lack of large effusion • Difficulty weight-bearing
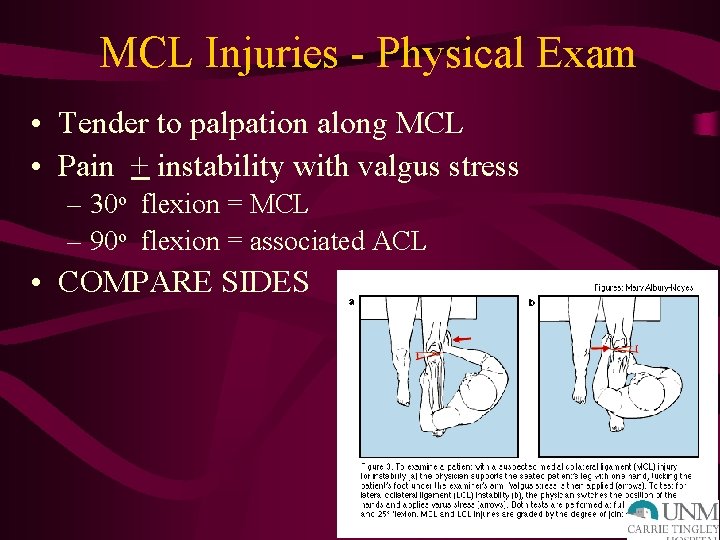
MCL Injuries - Physical Exam • Tender to palpation along MCL • Pain + instability with valgus stress – 30 o flexion = MCL – 90 o flexion = associated ACL • COMPARE SIDES

MCL Injuries – Treatment Grade 1, 2 • Early mobilization • Weight-bearing as tolerated • Hinged knee brace • Recovery 4 -6 weeks
MCL Injuries – Treatment Grade 3 • Isolated = nonsurgical management • Combined = surgery consistent with associated injuries • Natural Hx = lack of long-term degenerative changes seen with ACL, meniscus
PCL INJURIES • Mechanism – Sports = fall on flexed knee with foot plantarflexed, hyperextension, pivot – MVA = dashboard injury • Effusion (less than with ACL) • Shifting/instability (chronic) • Less distinctive

PCL Injuries – Physical Exam • + Effusion • + Posterior drawer test • + Posterior sag sign • False positive Lachman test • Common to have isolated injuries
PCL Injuries - Treatment • Functional bracing (early) • Rehab • Surgery if continued instability, effusions • Note- 2% of NFL preseason exam with incidental isolated PCL tear
PATELLAR INSTABILITY • Acute patellar dislocation • Acute patellar subluxation • Patellar tracking dysfunction
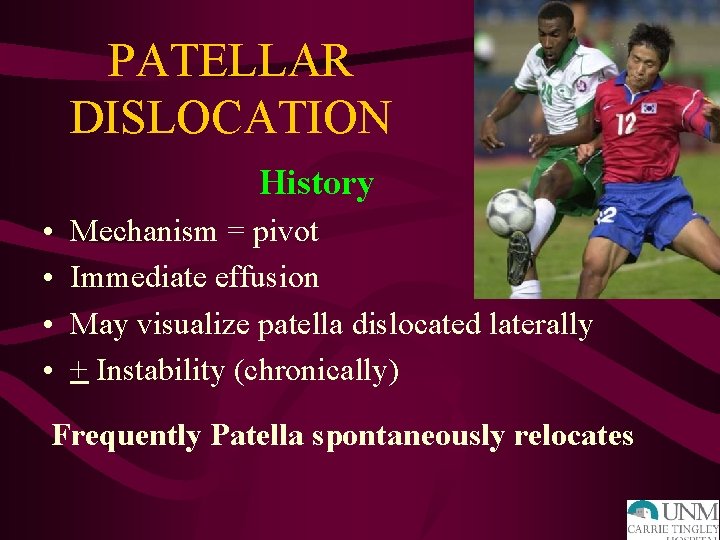
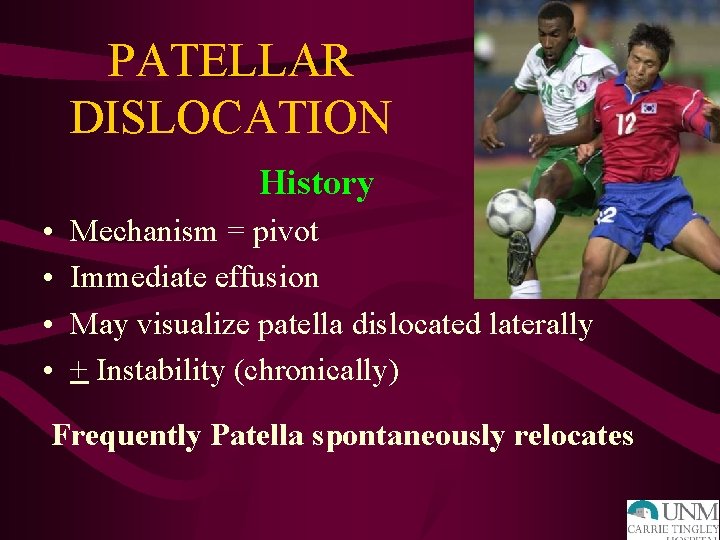
PATELLAR DISLOCATION History • • Mechanism = pivot Immediate effusion May visualize patella dislocated laterally + Instability (chronically) Frequently Patella spontaneously relocates
Patellar Dislocation – Physical Exam • Tender peripatellar structures – Medial retinaculum – Lateral femoral condyle • Effusion • ? Patella dislocated laterally X-rays- osteochondral fracture, effusion

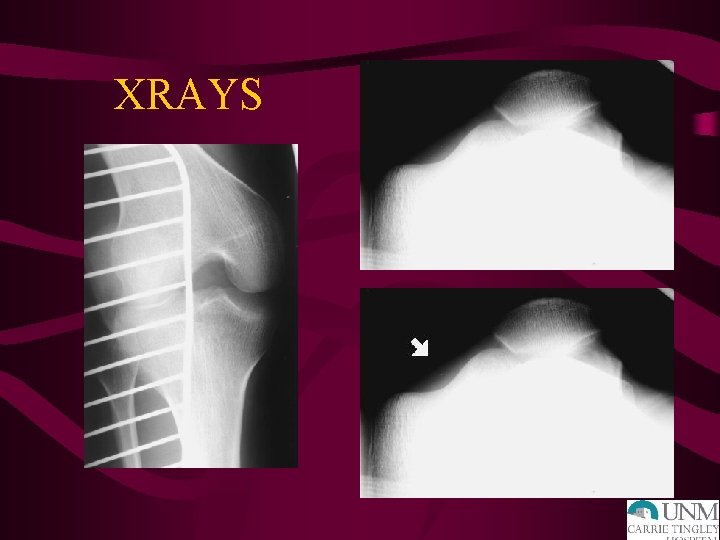
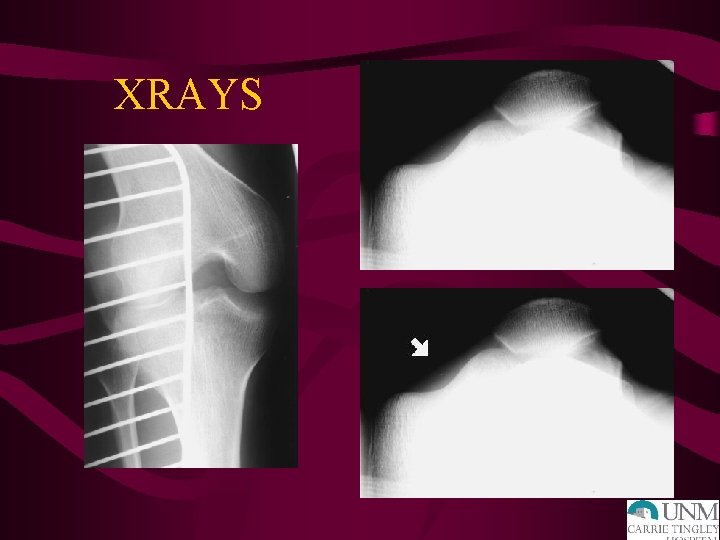
XRAYS

PATELLAR DISLOCATION • • Treatment Knee extension immobilizer in ER Early quad setting exercises Change to Shield’s Brace Return to sport – Full, painless ROM – Normal strength – Adequate aerobic fitness
Fractures and Dislocations about the Knee in Pediatric Patients

Anatomy • Distal femoral physis- large, undulatingirregular • Proximal tibial physis- contiguous with tibial tubercle apophysis • Ligament and muscular attachments may lead to avulsion injuries, fracture angulation
Anatomy- Neurologic and Vascular Structures • Popliteal artery tethered above and below knee • Common peroneal nerve vulnerable at fibular neck/head
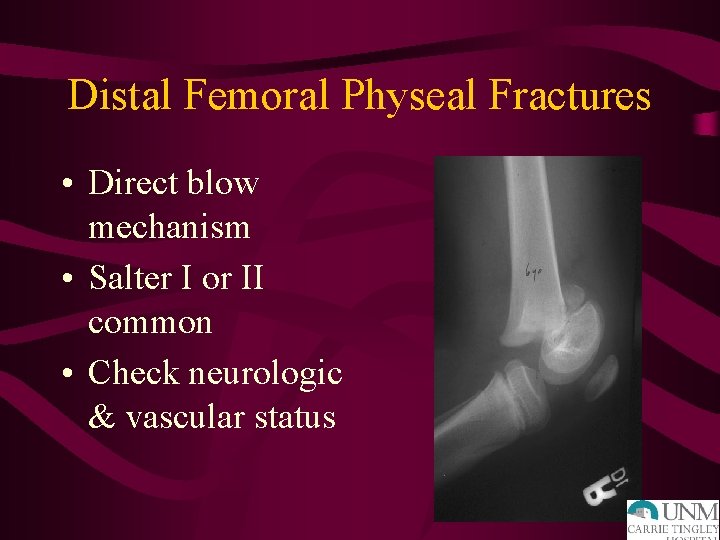
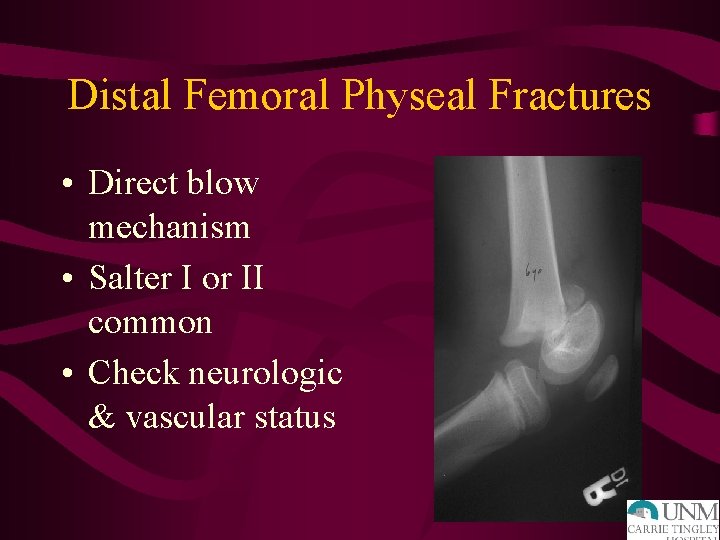
Distal Femoral Physeal Fractures • Direct blow mechanism • Salter I or II common • Check neurologic & vascular status

Distal Femoral Physeal Fractures • Closed reduction and pinning for displaced fractures • Long leg cast
Distal Femoral Physeal Fractures • High rate of premature growth arrest – rare < 2 yo – 80% 2 - 11 yo – 50% > 11 yo • Angular deformity • Leg length discrepancy
Patella Fractures in Children • Largest sesamoid bone, gives extensor mechanism improved lever arm • Uncommon fracture in skeletally immature patients • May have bipartite (superolateral) patella- avoid misdiagnosis
Patellar Sleeve Fracture • 8 -12 year old • Inferior pole sleeve of cartilage may displace • May have small ossified portion • <2 mm displaced, intact extensor mechanism- treat non-operatively
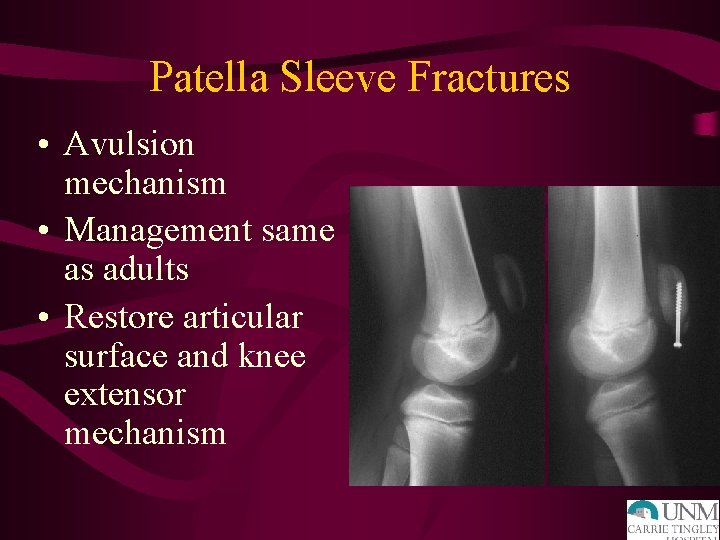
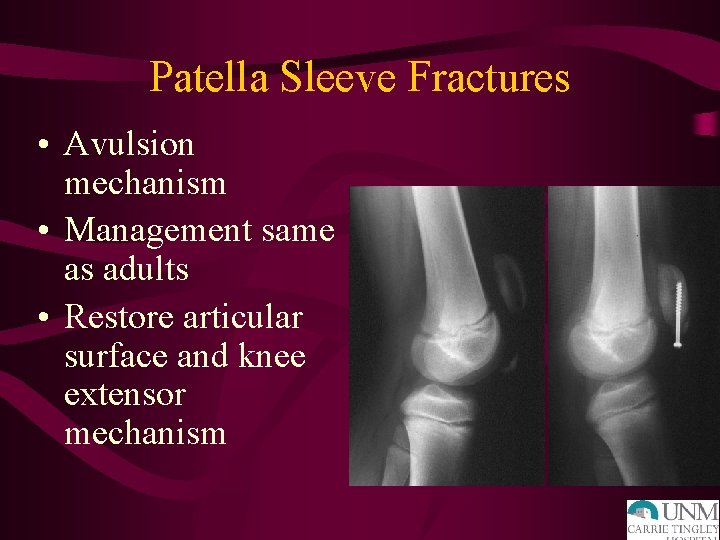
Patella Sleeve Fractures • Avulsion mechanism • Management same as adults • Restore articular surface and knee extensor mechanism
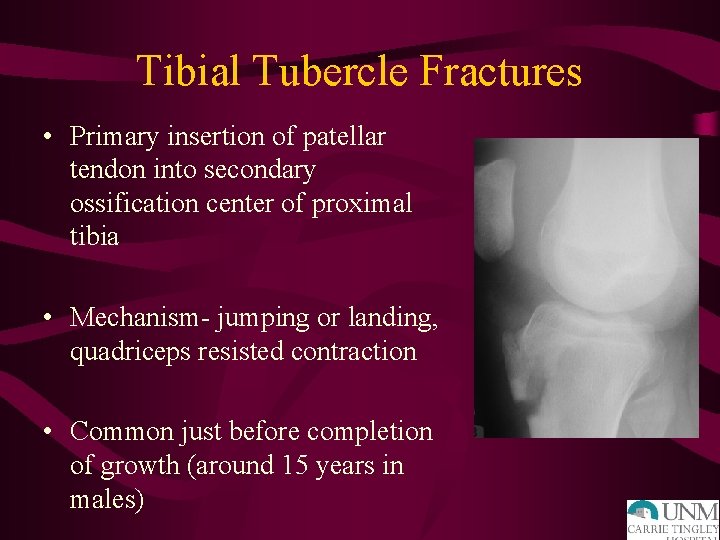
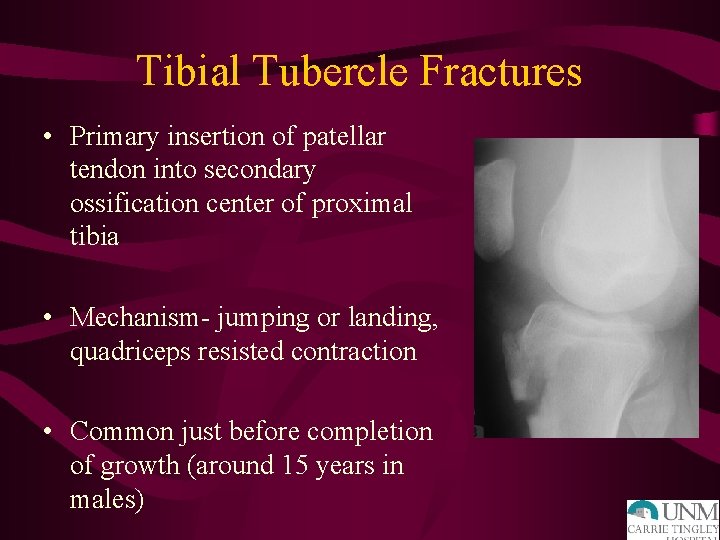
Tibial Tubercle Fractures • Primary insertion of patellar tendon into secondary ossification center of proximal tibia • Mechanism- jumping or landing, quadriceps resisted contraction • Common just before completion of growth (around 15 years in males)

Tibial Tubercle Fractures. Treatment • Nondisplaced, intact extensor mechanism- above knee immobilization for 6 weeks in extension • Displaced, loss of extensor mechanism integrityoperative fixation

Tibial Tubercle Fracture • 10 - 14 year old • Often during basketball • Surgery for displaced fractures, inability to extend knee
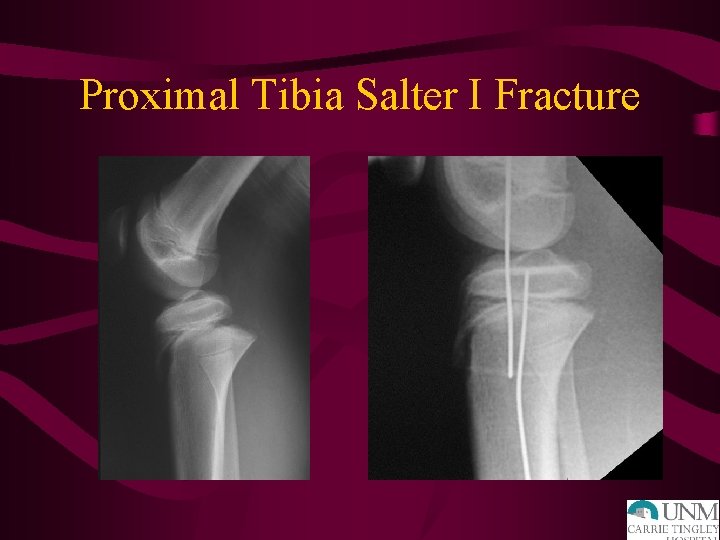
Proximal Tibial Physeal Fractures • Usually Salter II fractures. • Occasionally Salter I or IV • Posterior displacement of epiphysis or metaphysis can cause vascular compromise

Proximal Tibia Fracture
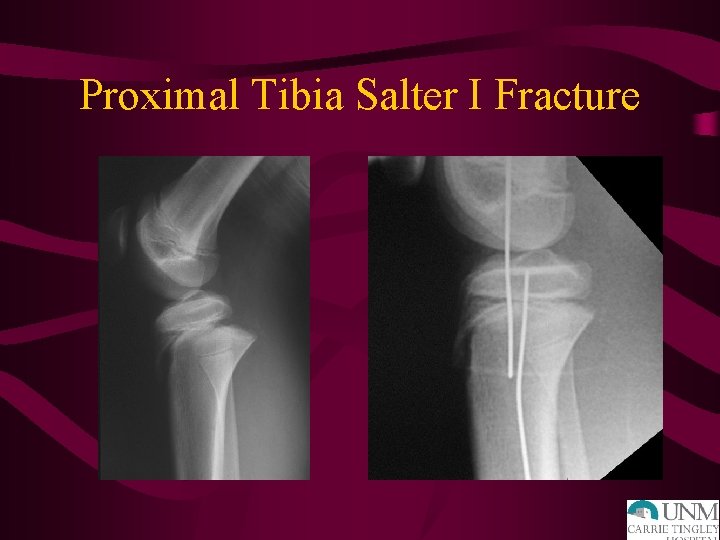
Proximal Tibia Salter I Fracture
Proximal Tibia Physeal Fractures • Open reduction for irreducible Salter I and II, displaced Salter IV • Observe closely for vascular compromise or compartment syndrome in first 24 hours • Follow for growth disturbance, angular deformity

Complications • • Angular deformity Malunion Physeal bar Leg length discrepancy
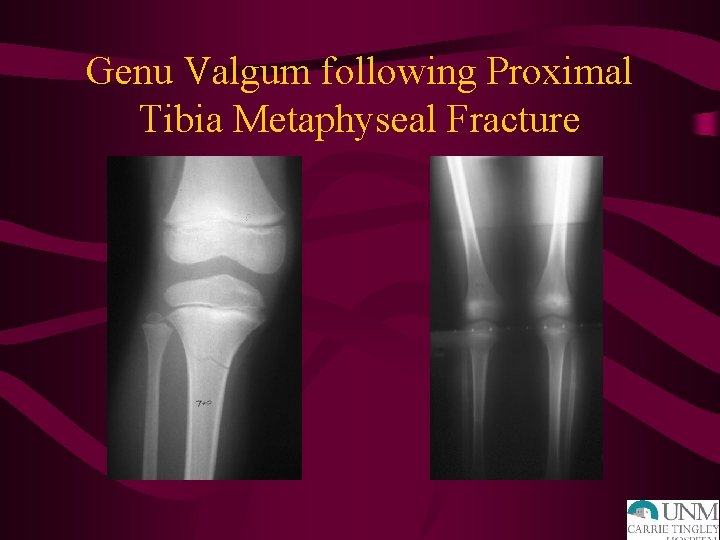
Proximal Tibial Metaphyseal Fractures • Younger patients, less than 6 years • Often nondisplaced, nonangulated • Later progressive valgus deformity can result from medial tibial overgrowth (Cozen Phenomenon)
Proximal Tibial Metaphyseal Fractures • Initial treatment- try to mold into varus to close any medial fracture gap • Notify parents initially of possible valgus deformity development • Follow 2 -4 years
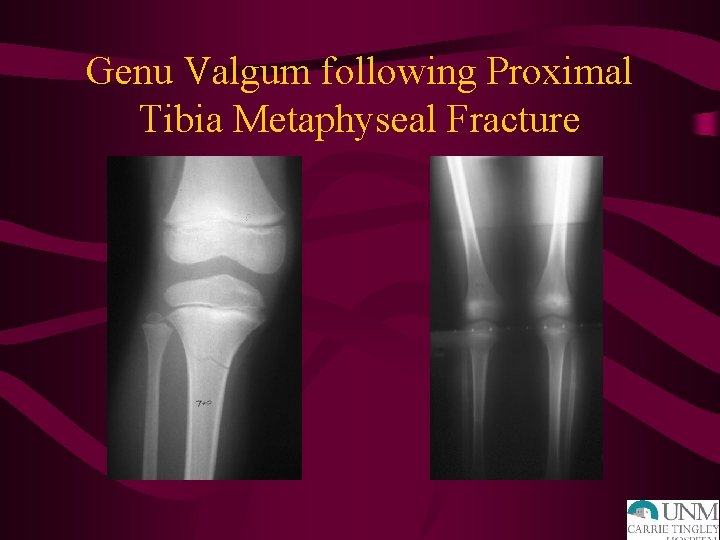
Genu Valgum following Proximal Tibia Metaphyseal Fracture
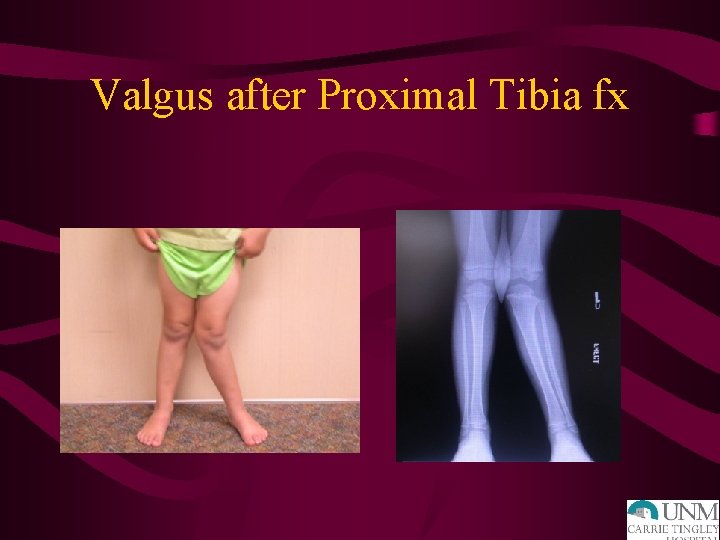
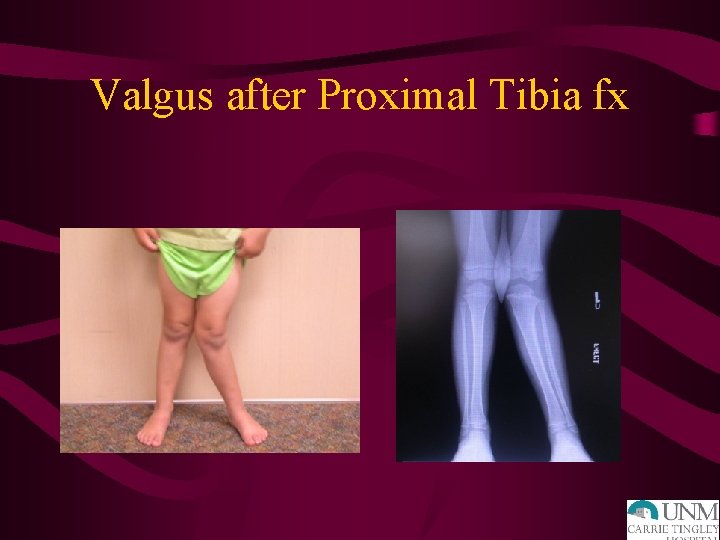
Valgus after Proximal Tibia fx
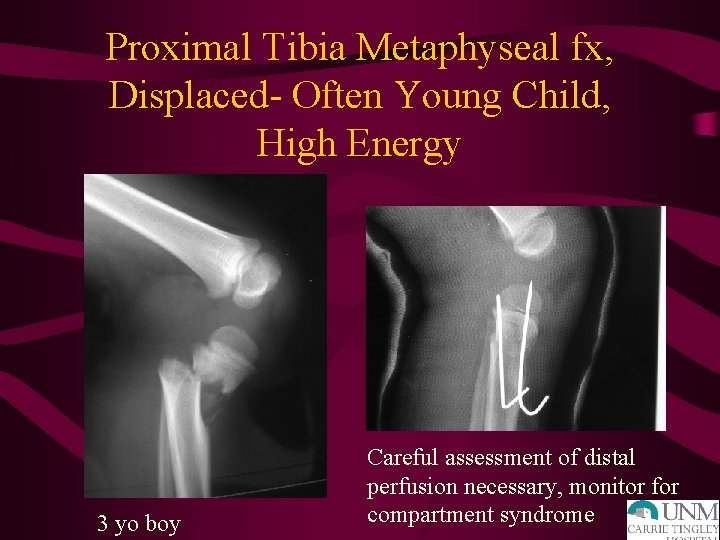
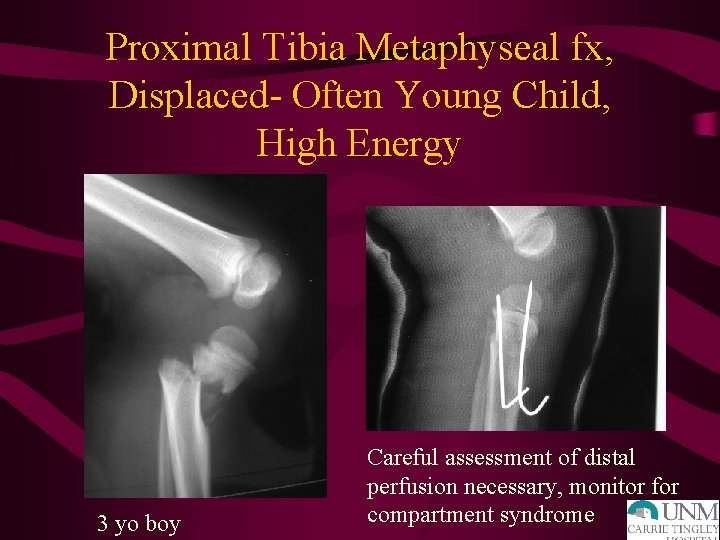
Proximal Tibia Metaphyseal fx, Displaced- Often Young Child, High Energy 3 yo boy Careful assessment of distal perfusion necessary, monitor for compartment syndrome
Foot and Ankle Injuries
Pediatric Ankle Fractures • 2 nd most common site of physeal fractures in children • Most occur between ages 10 - 15 y. o. • Boys > girls • Direct and indirect mechanisms
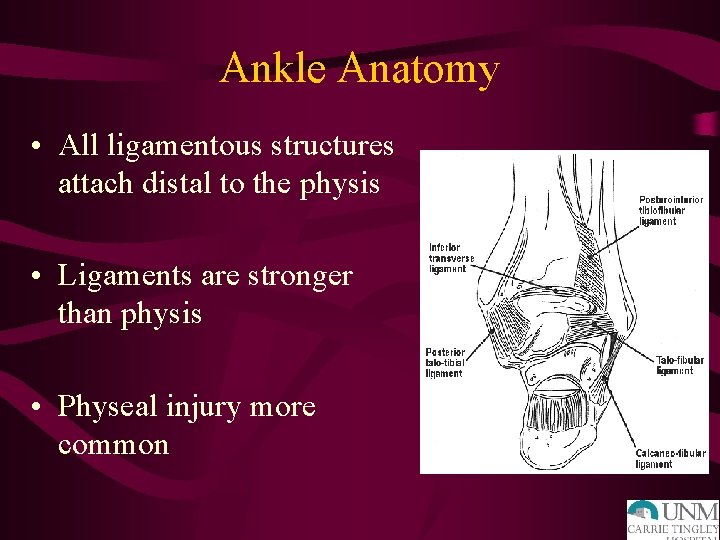
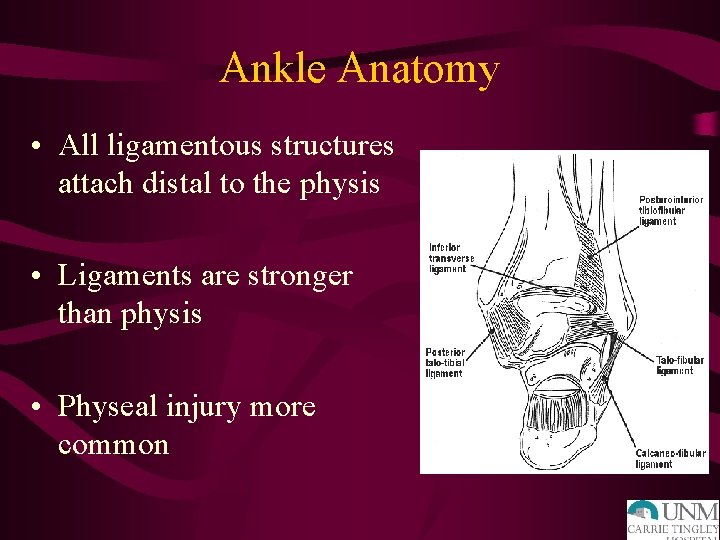
Ankle Anatomy • All ligamentous structures attach distal to the physis • Ligaments are stronger than physis • Physeal injury more common

Distal Tibial Physeal Closure
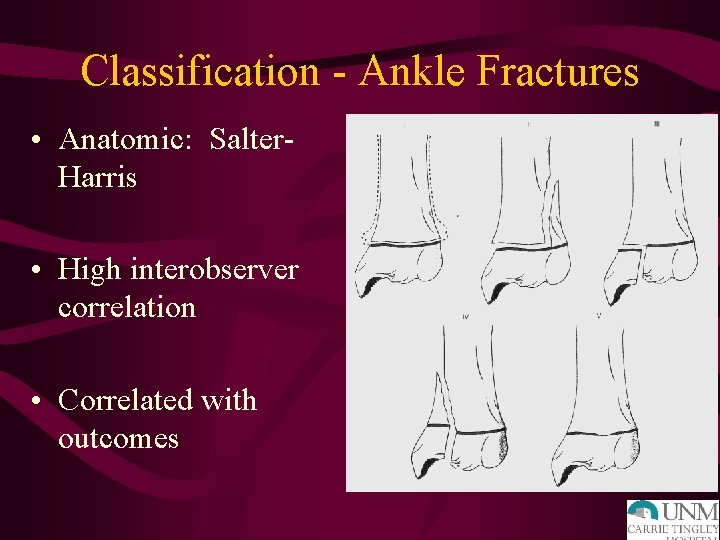
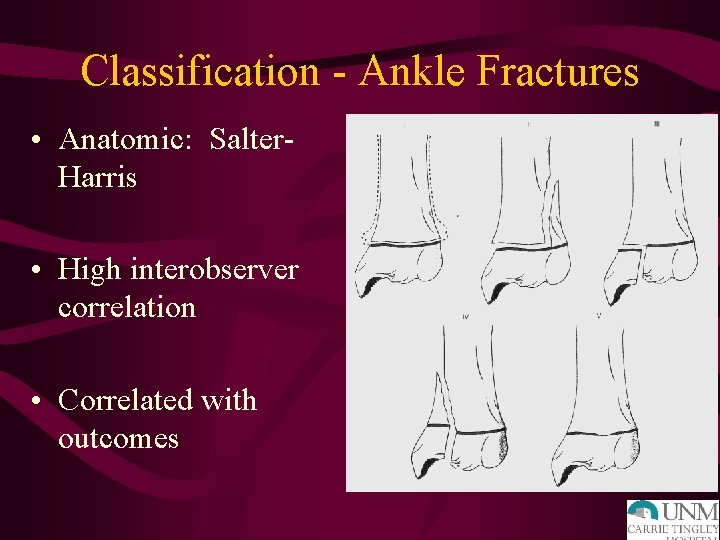
Classification - Ankle Fractures • Anatomic: Salter. Harris • High interobserver correlation • Correlated with outcomes
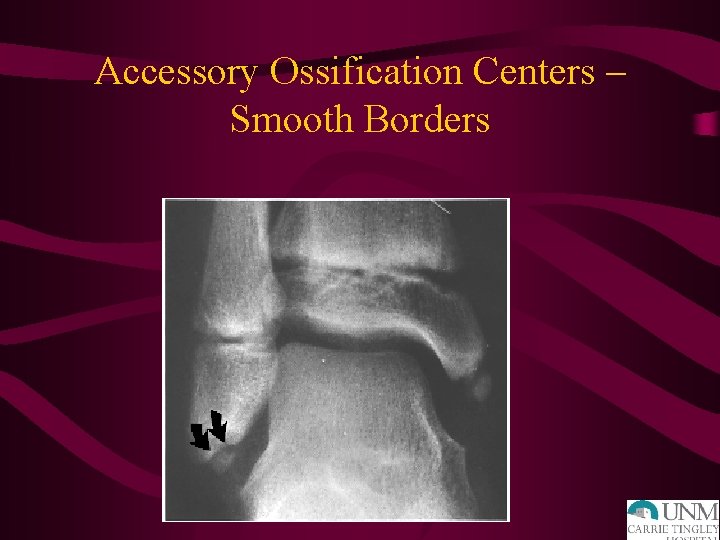
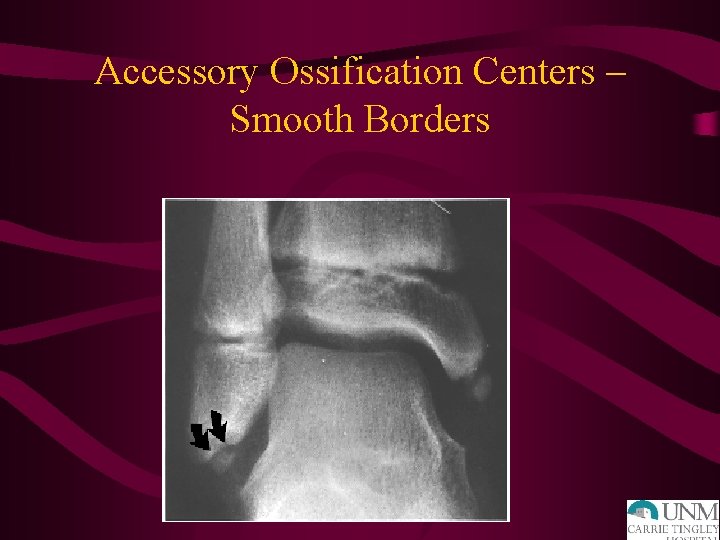
Accessory Ossification Centers – Smooth Borders
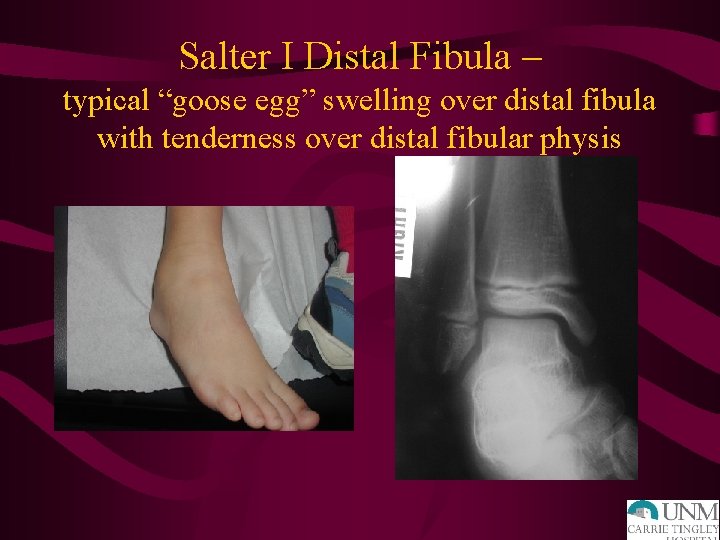
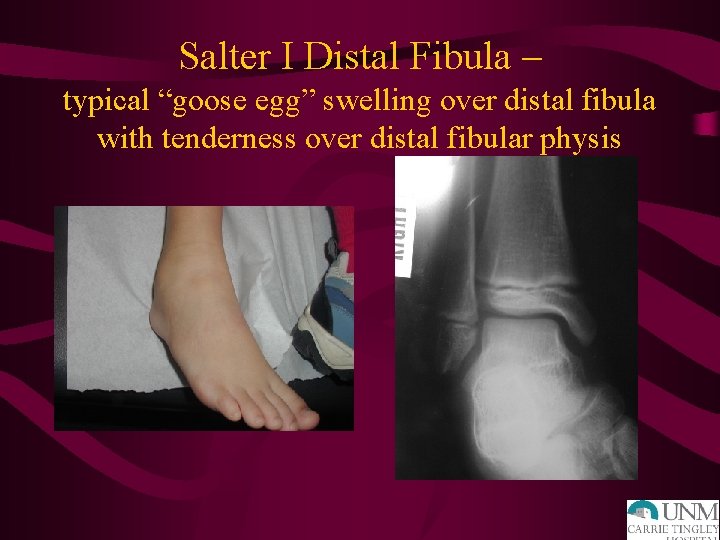
Salter I Distal Fibula – typical “goose egg” swelling over distal fibula with tenderness over distal fibular physis
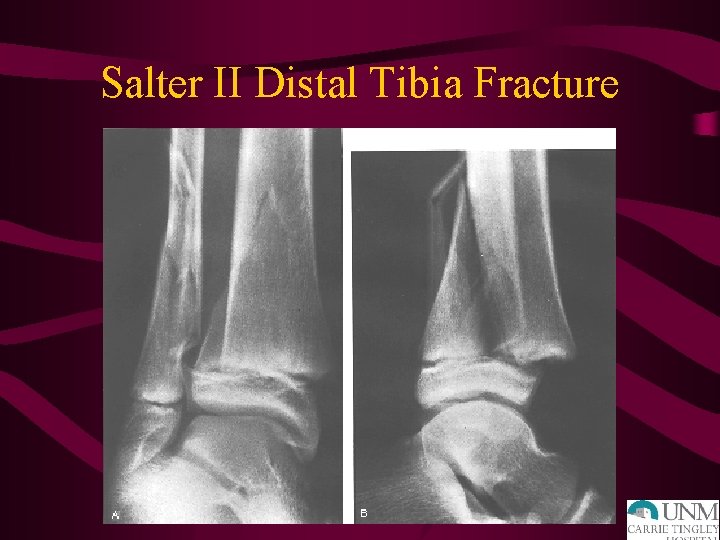
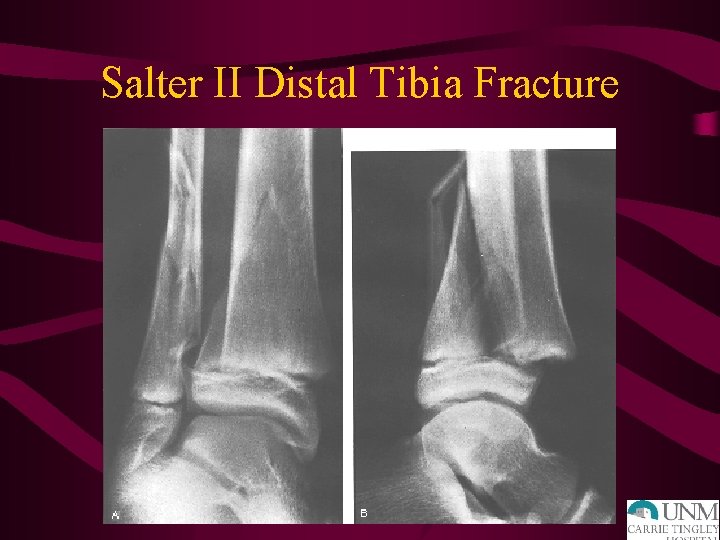
Salter II Distal Tibia Fracture
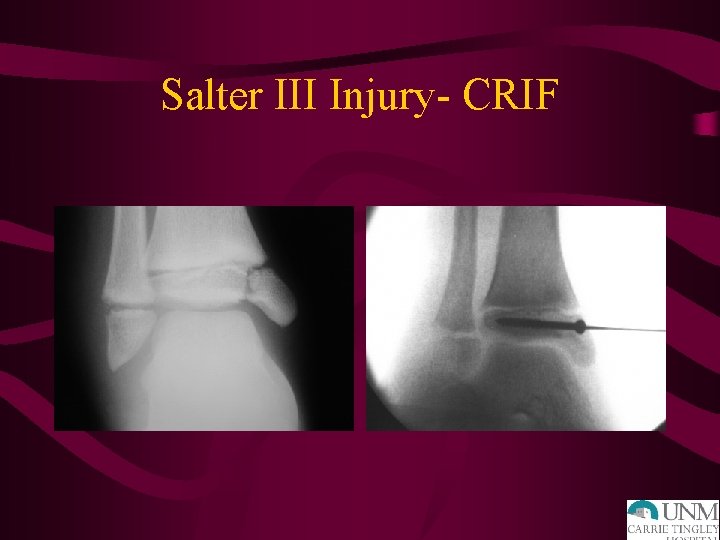
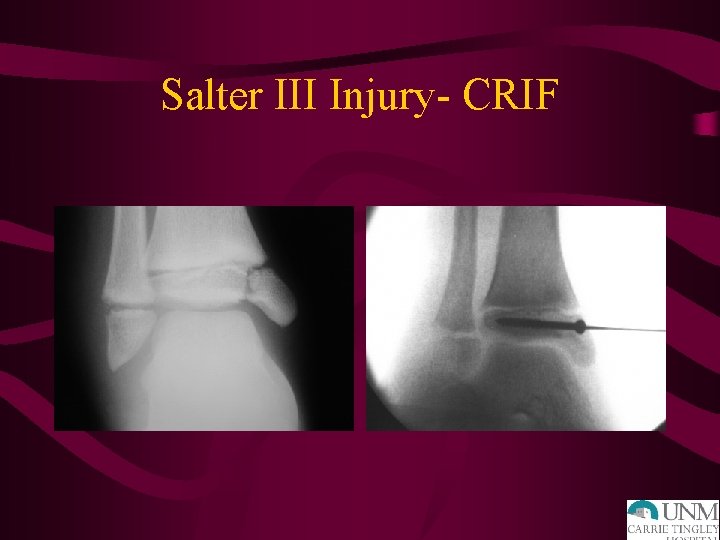
Salter III Injury- CRIF
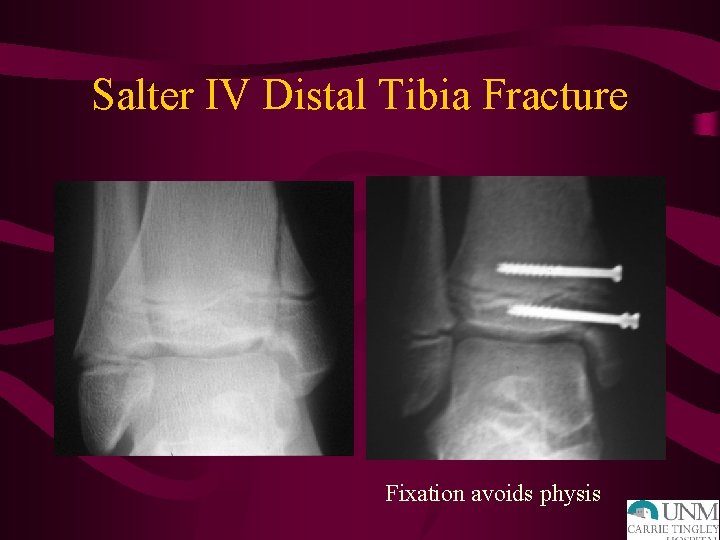
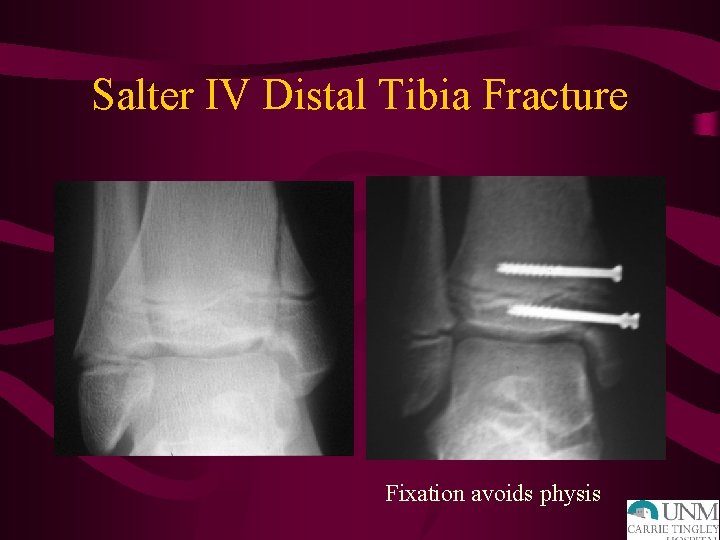
Salter IV Distal Tibia Fracture Fixation avoids physis

Salter-Harris Type V fxs • Crush injury to physis • No associated displacement • Diagnosis made with follow-up xrays revealing premature physeal closure • treatment directed primarily at sequelae of growth arrest

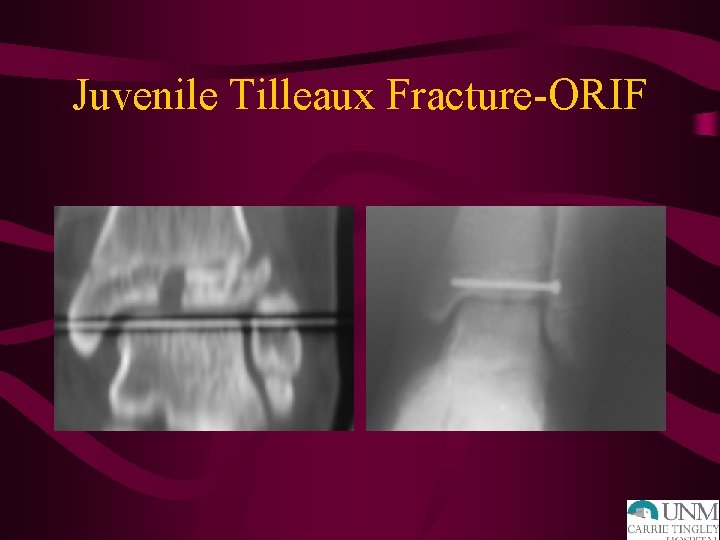
“Transitional” Fractures • Fxs occurring during asymmetric closure of distal tibial physis – Triplane fx • 2, 3 or 4 -part fxs • lateral more common – Juvenile Tillaux fx

“Transitional” Fractures • Triplane fx – tend to be seen in younger pts than pts with Juvenile Tillaux fx – more displacement/swelling more severe – Treatment decisions usually based on articular displacement
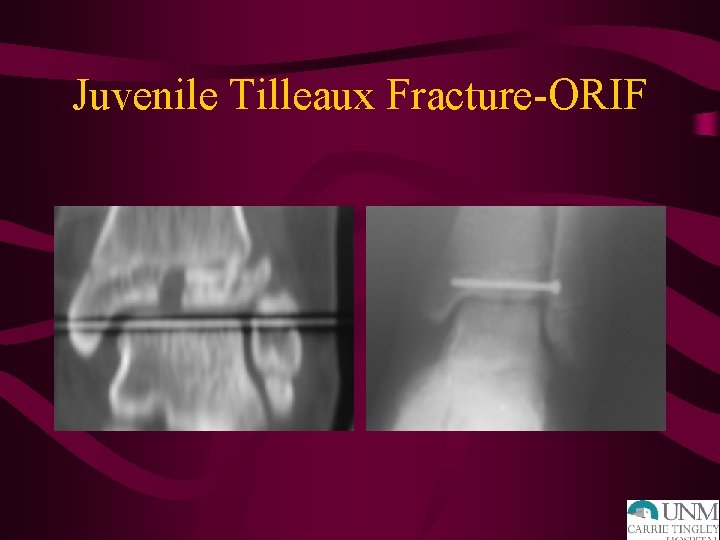
Juvenile Tilleaux Fracture-ORIF
Pediatric Ankle Sprains • Should be diagnosis of exclusion • Where is tenderness – over bone/physis or ankle ligaments? • Often represent missed Salter I ankle fractures, non-displaced calcaneal fractures • Follow-up persistent pain
Pediatric Foot Fractures • Often missed diagnosis • Reductions of fractures important – less remodeling potential – reach 50% of mature length of foot bones by 18 mo. (compared to femur/tibia - do not reach until 3 y. o. )
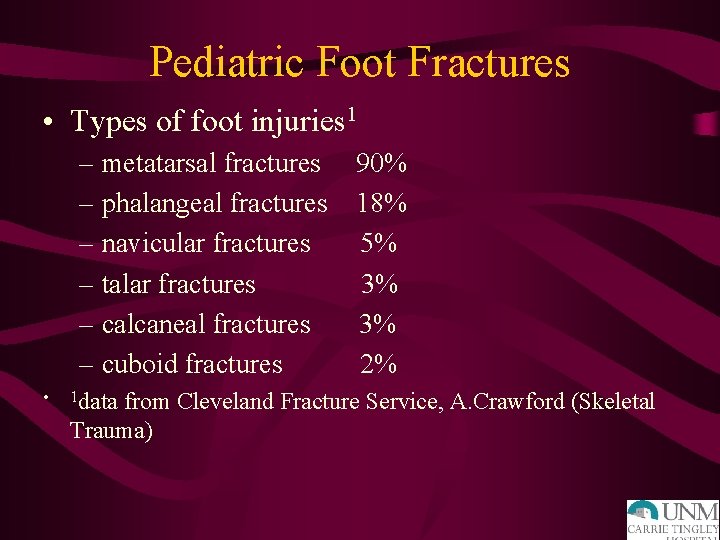
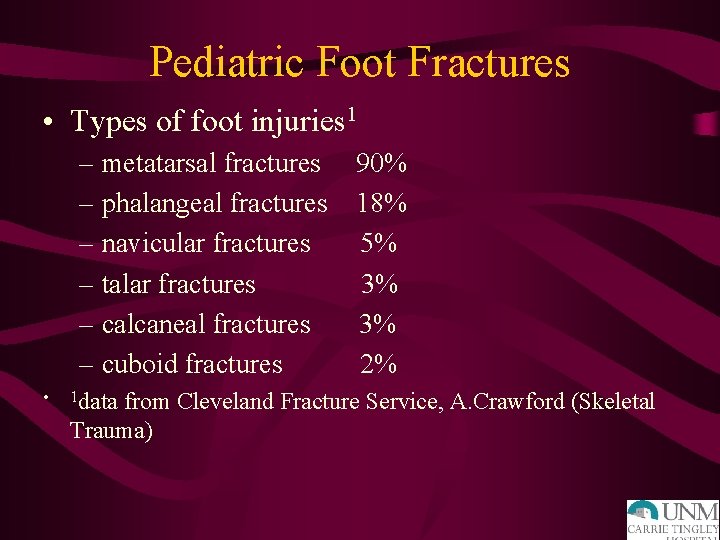
Pediatric Foot Fractures • Types of foot injuries 1 – metatarsal fractures 90% – phalangeal fractures 18% – navicular fractures 5% – talar fractures 3% – calcaneal fractures 3% – cuboid fractures 2% • 1 data from Cleveland Fracture Service, A. Crawford (Skeletal Trauma)
Pediatric Overuse Injuries
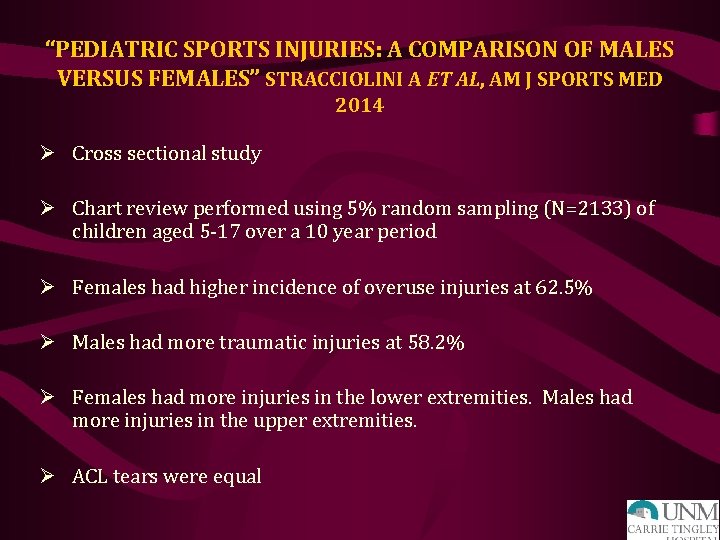
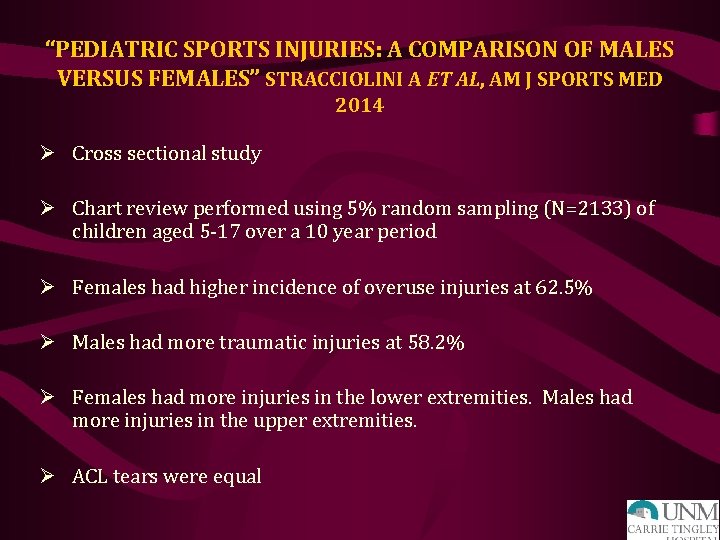
“PEDIATRIC SPORTS INJURIES: A COMPARISON OF MALES VERSUS FEMALES” STRACCIOLINI A ET AL, AM J SPORTS MED 2014 Ø Cross sectional study Ø Chart review performed using 5% random sampling (N=2133) of children aged 5 -17 over a 10 year period Ø Females had higher incidence of overuse injuries at 62. 5% Ø Males had more traumatic injuries at 58. 2% Ø Females had more injuries in the lower extremities. Males had more injuries in the upper extremities. Ø ACL tears were equal

“SPORTS-SPECIALIZED INTENSIVE TRAINING AND THE RISK OF INJURY IN YOUNG ATHLETES: A CLINICAL CASECONTROL STUDY” JAYANTHI NA ET AL, AM J SPORTS MED, 2015 Ø Case Control Study to determine if sports specialization, weekly training volumes, or growth rates are associated with increased risk for serious overuse injuries Ø Injured athletes aged 7 -18, years 2010 -2013 Ø 1214 athletes enrolled, 822 were injured and 368 uninjured Ø Injured athletes were older (14. 1 vs 12. 9) and more total active hours (19. 6 vs 17. 6) Ø Sports specialization was an independent risk of serious overuse injury with odds ratio of 1. 27 and 95% CI Ø Also at significant risk are children that spend more hours/wk in sports than their age. This is different from “free play”


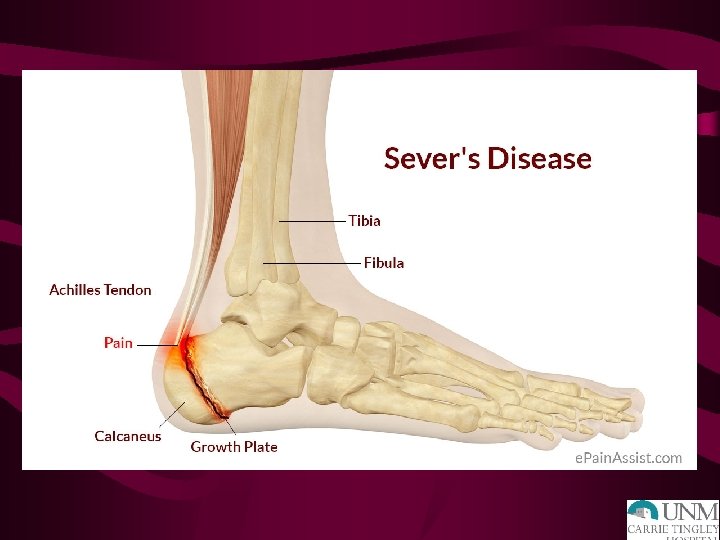
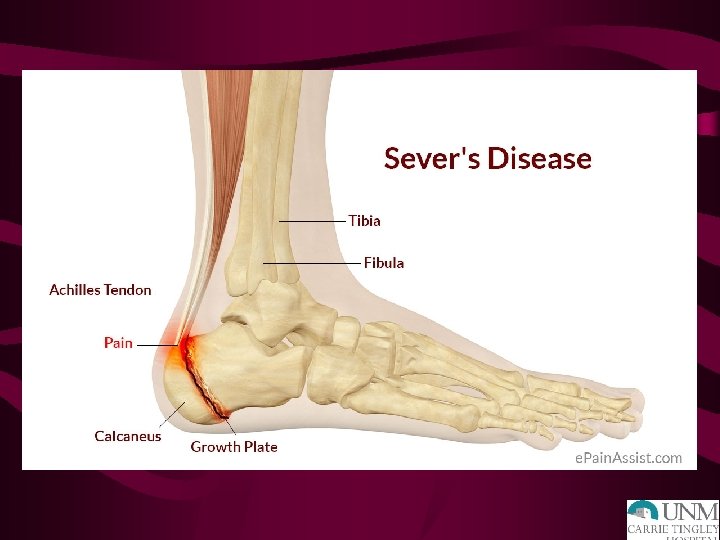
“SPORTS-RELATED OVERUSE INJURIES IN CHILDREN” LAUNAY F, ORTHOP TRAUMATOL SURG RES, 2015 Ø Overuse injuries are better known as “osteochondrosis” Ø This refers to the inflammatory conditions of bone and cartilage Ø Most overuse injuries affect the lower extremities and most common types are Sever’s and Osgood-Schlatter Ø In both of these conditions: the tendon remains relatively short during the pubescent growth spurt which may contribute to their increased incidence Ø Seems to be correlation with not just increased sports activity, but concurrent decreased “free play” or activity out of sports
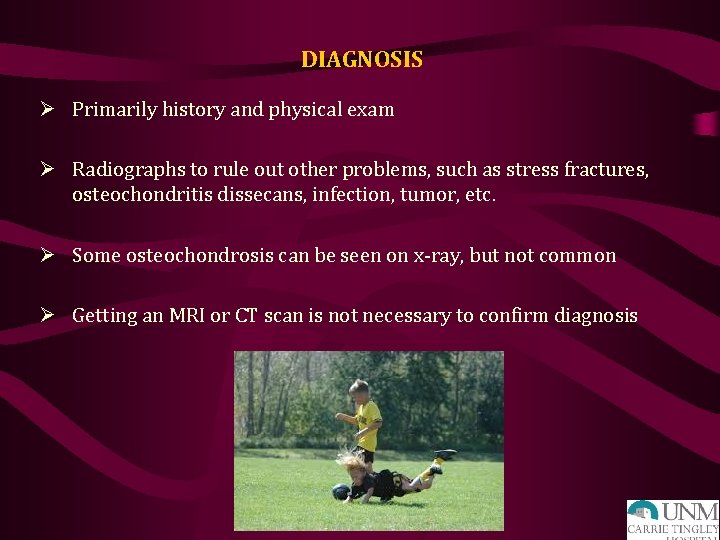
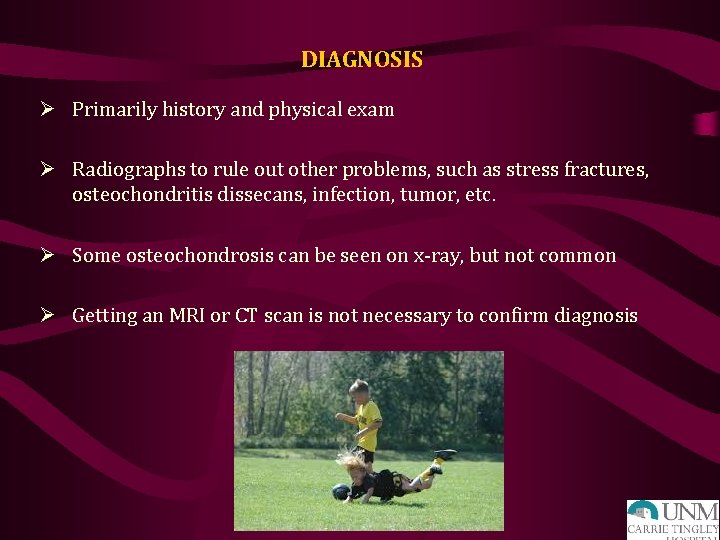
DIAGNOSIS Ø Primarily history and physical exam Ø Radiographs to rule out other problems, such as stress fractures, osteochondritis dissecans, infection, tumor, etc. Ø Some osteochondrosis can be seen on x-ray, but not common Ø Getting an MRI or CT scan is not necessary to confirm diagnosis

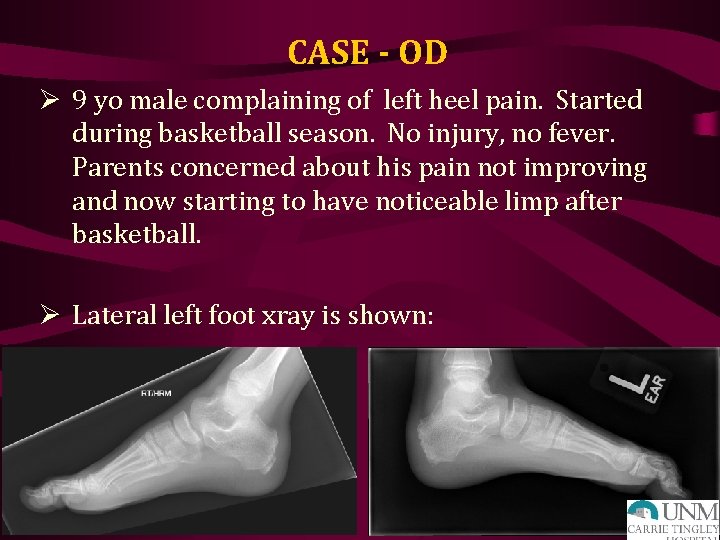
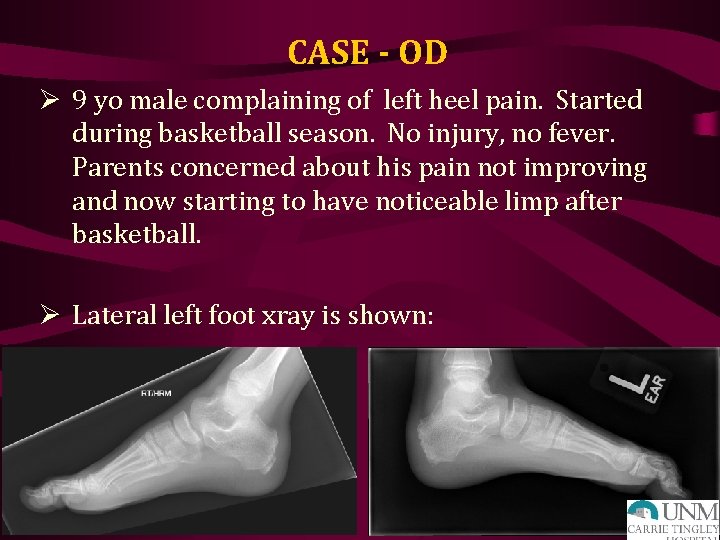
CASE - OD Ø 9 yo male complaining of left heel pain. Started during basketball season. No injury, no fever. Parents concerned about his pain not improving and now starting to have noticeable limp after basketball. Ø Lateral left foot xray is shown:

TREATMENT Ø Break from sport Ø Anti-inflammatories Ø Ice/heat compresses Ø Then stretching program and slow return to sport Ø Really need to speak with the family why their child is in pain and get them on board with prevention of this happening again Ø Unfortunately, commonly a rollercoaster until the child is done growing

“A HEEL CUP IMPROVES THE FUNCTION OF THE HEEL PAD IN SEVER’S INJURY: EFFECTS ON HEEL PAD THICKNESS, PEAK PRESSURE AND PAIN” PERHAMRE S ET AL, SCAND J MED SCI SPORTS, 2012 Ø Apophysitis calcanei is a common cause of heel pain in children 815 years old. Ø Purpose was to assess the effect of a heel cup on heel pad thickness and heel peak pressure Ø 50 subjects evaluated Ø The heel pad thickness improved and heel peak pressure was significantly reduced with use of the heel cups Ø This translated to significant reduction in pain when using a heel cup in a sports shoe versus not using one

“THE EFFECTIVENESS OF EXERCISE INTERVENTIONS TO PREVENT SPORTS INJURIES: A SYSTEMATIC REVIEW AND META-ANALYSIS OF RANDOMIZED CONTROLLED TRIALS” LAUERSEN JB ET AL, BR J SPORTS MED, 2014 Ø To determine if physical activity exercises can reduce sports injuries Ø 3462 studies, 25 trials ultimately selected for total of 26, 610 participants with 3, 464 injuries Ø Favorable estimates were obtained for all injury prevention measures except for stretching. Ø Strength training reduced sports injuries to less than 1/3 and overuse injuries can be reduced by almost 50%
SUMMARY Ø There is more awareness of overuse injuries and there is increased risk in females, older children (teenagers), kids that participate in the same sport year-round, and kids that have sports: free play ratio of 2: 1 Ø Treatment is still rest, ice, anti-inflammatories, and strengthening/stretching program Ø Prevention is the key: Ø More cross training Ø Kids being more active in “free play” Ø Not pushing kids into excessive hours of sport training

THANK YOU!
 Types of family in community medicine
Types of family in community medicine Principles of family medicine
Principles of family medicine Halifax family medicine residency
Halifax family medicine residency Meritus family practice
Meritus family practice Family medicine procedures
Family medicine procedures Milestones family medicine
Milestones family medicine Board review family medicine
Board review family medicine Principles of primary health care
Principles of primary health care Wonca definition of family medicine
Wonca definition of family medicine Surgery nbme percentiles
Surgery nbme percentiles Function of family
Function of family St cloud family medicine
St cloud family medicine Af williams clinic
Af williams clinic Kaiser san diego family medicine residency
Kaiser san diego family medicine residency Family medicine in ethiopia
Family medicine in ethiopia Cabarrus family medicine concord
Cabarrus family medicine concord Uthscsa family medicine residency
Uthscsa family medicine residency St louis family medicine residency
St louis family medicine residency Screem family assessment questionnaire
Screem family assessment questionnaire 10 principles of family medicine
10 principles of family medicine Isu family medicine
Isu family medicine Somatic dysfunction in osteopathic family medicine
Somatic dysfunction in osteopathic family medicine Family medicine meaning
Family medicine meaning Duke family medicine and community health
Duke family medicine and community health Margaret wiedmann
Margaret wiedmann Screem res scoring
Screem res scoring Principle of family medicine
Principle of family medicine Challenges facing family medicine
Challenges facing family medicine Primer family medicine
Primer family medicine 06022007 color
06022007 color Gait iia
Gait iia Patient movement
Patient movement Muscle activity during gait cycle ppt
Muscle activity during gait cycle ppt Medical term for normal gait
Medical term for normal gait Propulsive gait
Propulsive gait Trendelenburg gait treatment
Trendelenburg gait treatment Transfemoral gait deviations
Transfemoral gait deviations Indication of crutches
Indication of crutches Quadriceps gait
Quadriceps gait The lateral displacement of cog exceeds one inch with:
The lateral displacement of cog exceeds one inch with: Scissor gait
Scissor gait Difference between cerebellar ataxia and sensory ataxia
Difference between cerebellar ataxia and sensory ataxia Hiking gait
Hiking gait Medical term for normal gait
Medical term for normal gait Prerequisites of gait
Prerequisites of gait Reeling gait
Reeling gait Bentropin
Bentropin Reeling gait
Reeling gait Dysdiadochokinesia test
Dysdiadochokinesia test Reeling gait
Reeling gait Reeling gait
Reeling gait Figlu
Figlu Gait ataxia spokane
Gait ataxia spokane Duchene gait adalah
Duchene gait adalah Hiatus saphenus
Hiatus saphenus Ascending tracts
Ascending tracts Greater sciatic foramen
Greater sciatic foramen Quadriceps gait
Quadriceps gait Gait aid
Gait aid Ou-isir gait database
Ou-isir gait database Gait trainer gt1
Gait trainer gt1 Conjugal family
Conjugal family Varies from family to family on the periodic table.
Varies from family to family on the periodic table. Binuclear family vs blended family
Binuclear family vs blended family Beck weathers
Beck weathers Unit 15:1 providing first aid
Unit 15:1 providing first aid Chapter 22 hunger games questions
Chapter 22 hunger games questions Strickler spine and sport
Strickler spine and sport Westfield sports injuries
Westfield sports injuries Stobhill miu
Stobhill miu Hammock carry procedure
Hammock carry procedure A short backboard or vest-style immobilization
A short backboard or vest-style immobilization Chapter 21 caring for head and spine injuries
Chapter 21 caring for head and spine injuries 17:5 providing first aid for poisoning
17:5 providing first aid for poisoning Emr chapter 15 injuries to muscles and bones
Emr chapter 15 injuries to muscles and bones Chapter 14:1 using body mechanics
Chapter 14:1 using body mechanics Jones and bartlett learning
Jones and bartlett learning Chapter 13:2 preventing accidents and injuries
Chapter 13:2 preventing accidents and injuries Chapter 11 injuries to the shoulder region
Chapter 11 injuries to the shoulder region Chapter 11 assessment and evaluation of sports injuries
Chapter 11 assessment and evaluation of sports injuries Kristen wilson injuries
Kristen wilson injuries Pallet jack injuries
Pallet jack injuries An epidemiologic survey of roller skating injuries
An epidemiologic survey of roller skating injuries Climatic injury
Climatic injury Jsp539
Jsp539 Chapter 12 lesson 1 benefits of physical activity
Chapter 12 lesson 1 benefits of physical activity Chapter 4 preventing injuries through fitness
Chapter 4 preventing injuries through fitness Chapter 13 worksheet recognizing different sports injuries
Chapter 13 worksheet recognizing different sports injuries Chapter 4 basics of tissue injuries
Chapter 4 basics of tissue injuries Bo taoshi injuries
Bo taoshi injuries Miniscus replacement
Miniscus replacement Preventing hand injuries
Preventing hand injuries How to protect yourself from intentional injuries
How to protect yourself from intentional injuries Glycerin and gelatin fake skin
Glycerin and gelatin fake skin Definition of intentional fallacy
Definition of intentional fallacy Injuries first aid
Injuries first aid