Total hip arthroplasty Z Rozkydal Hip joint Enarthrosis



















- Slides: 61
Total hip arthroplasty Z. Rozkydal
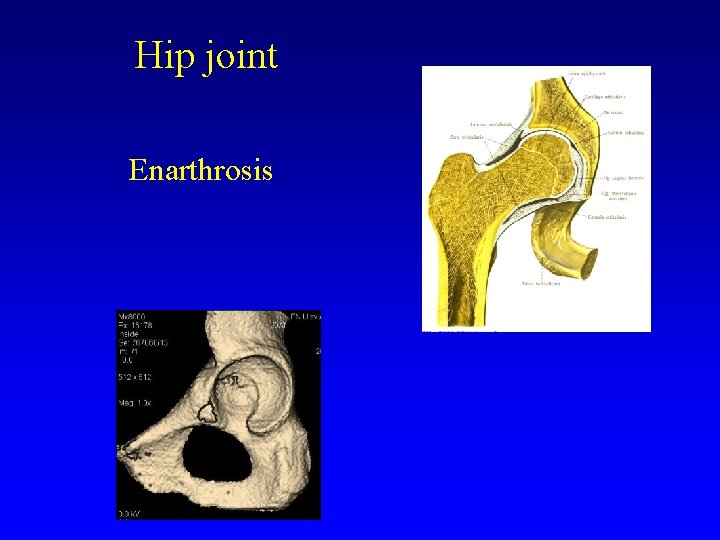
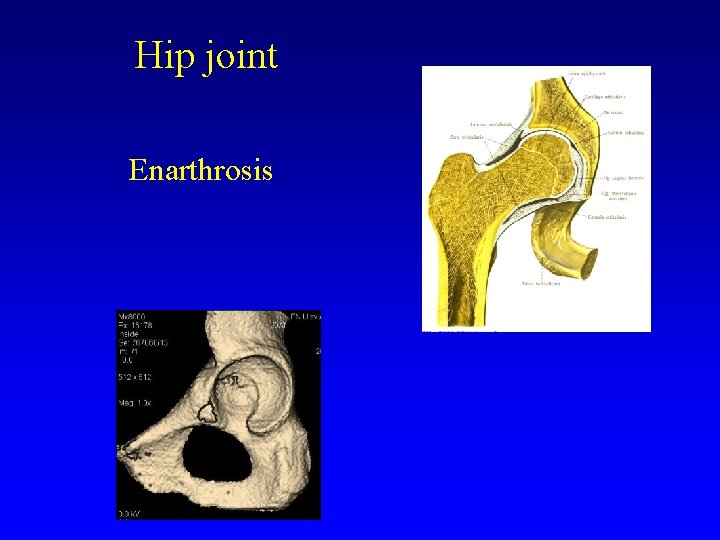
Hip joint Enarthrosis
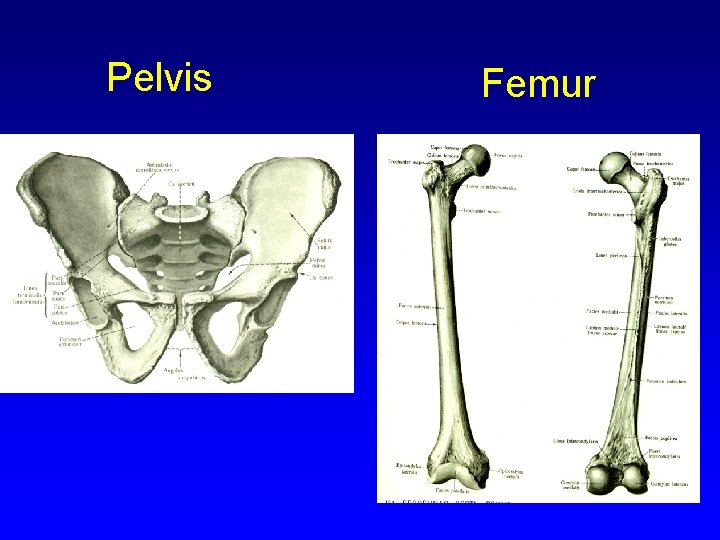
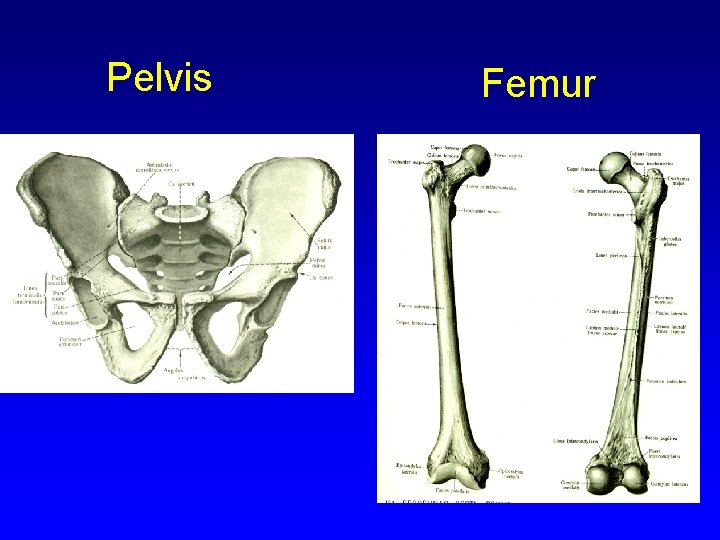
Pelvis Femur
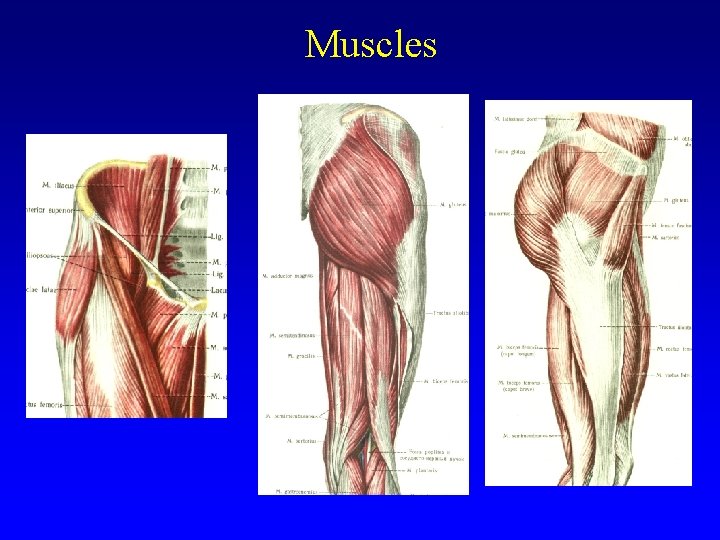
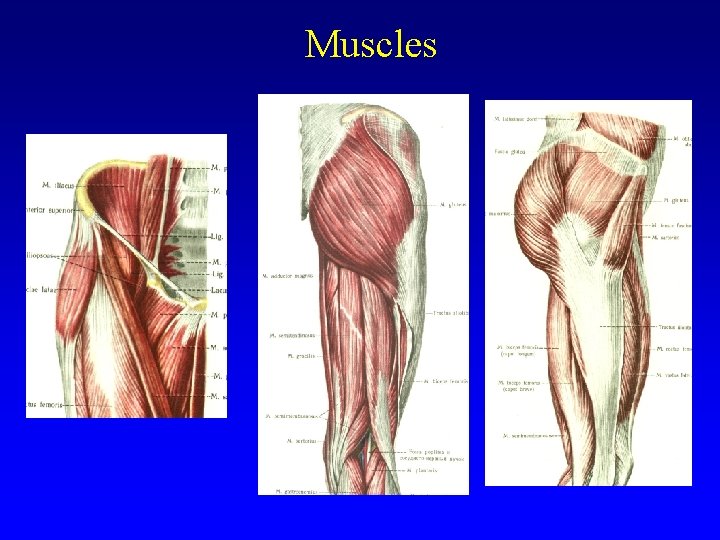
Muscles
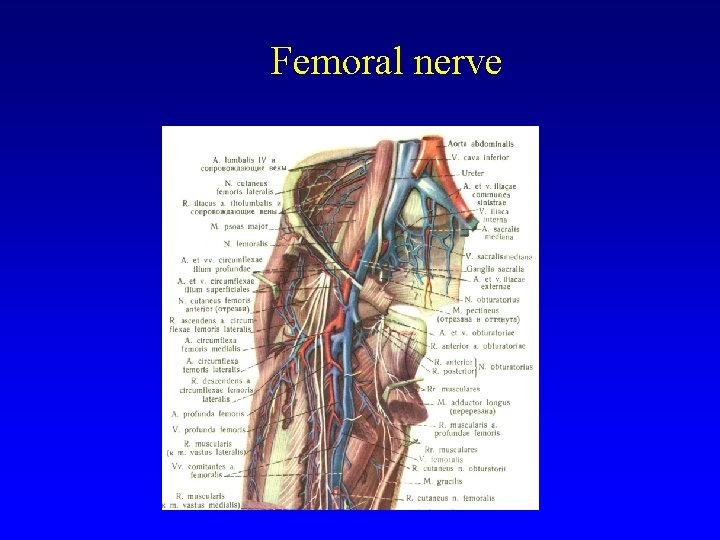
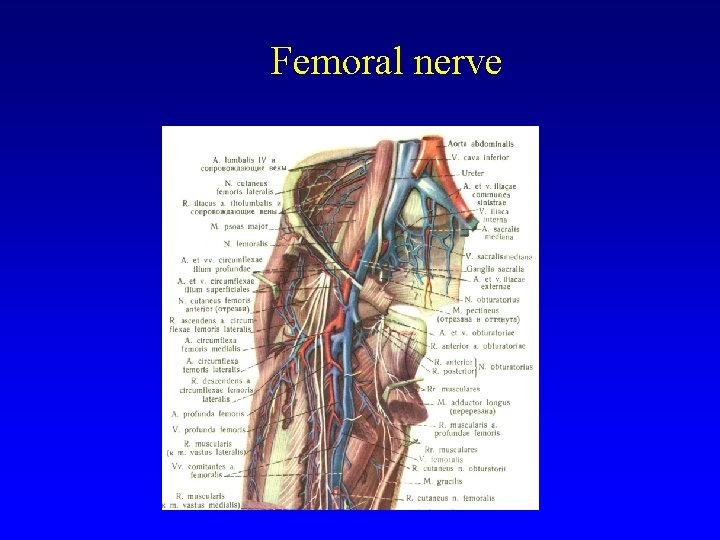
Femoral nerve
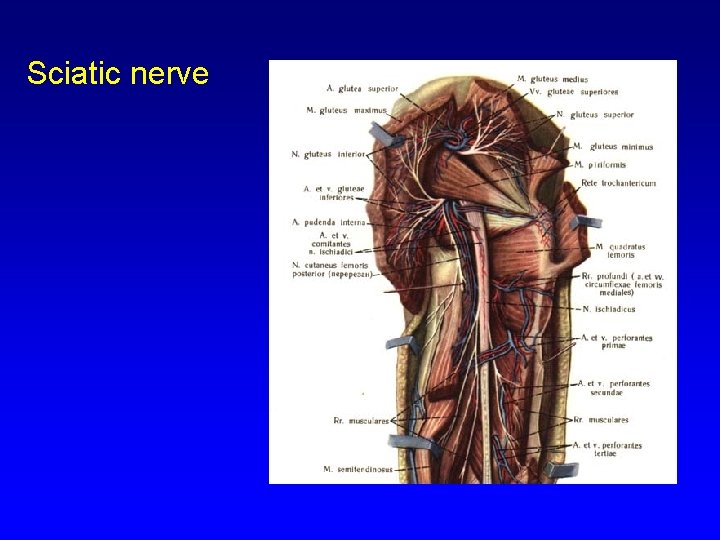
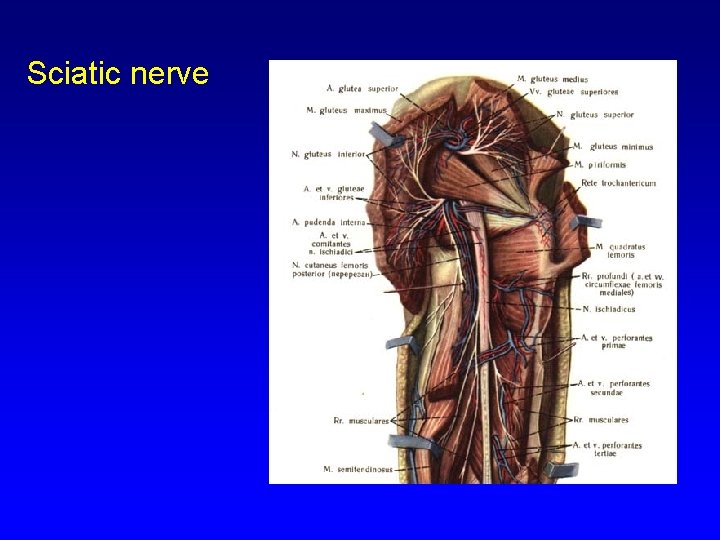
Sciatic nerve
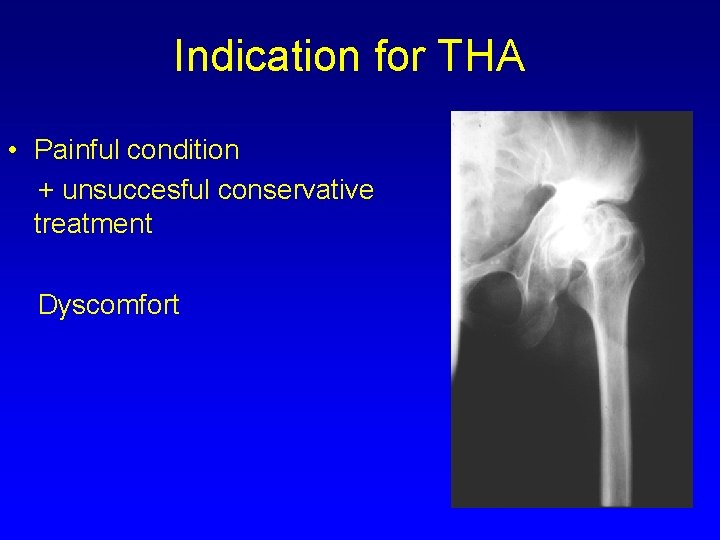
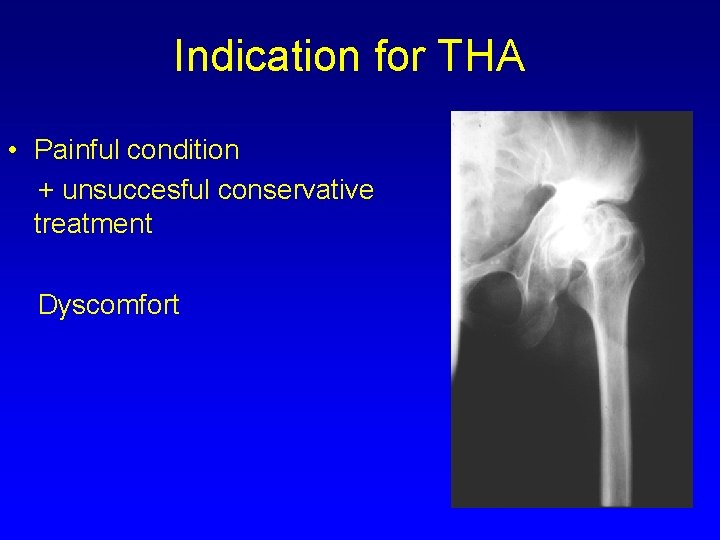
Indication for THA • Painful condition + unsuccesful conservative treatment Dyscomfort

Indications Primary osteoarthrosis Secondary osteoarthrosis: congenital, posttraumatic, after infection Revmatoid arthritis Psoriatic arthropathy Avascular necrosis of the femoral head Primary osteoarthritis
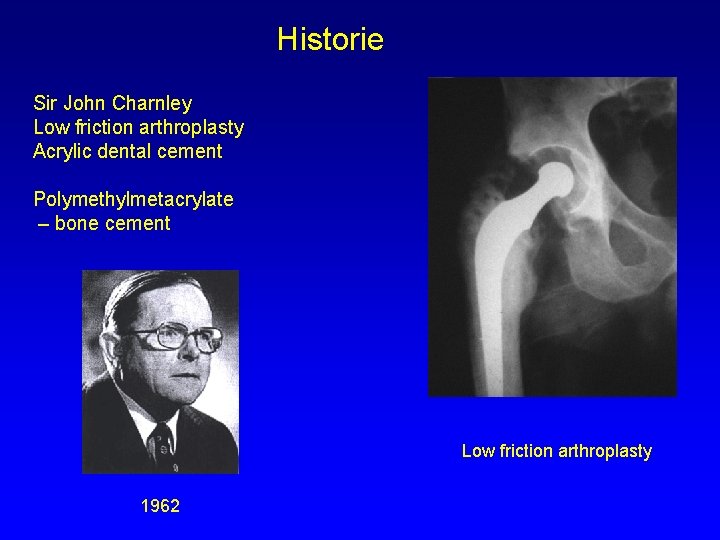
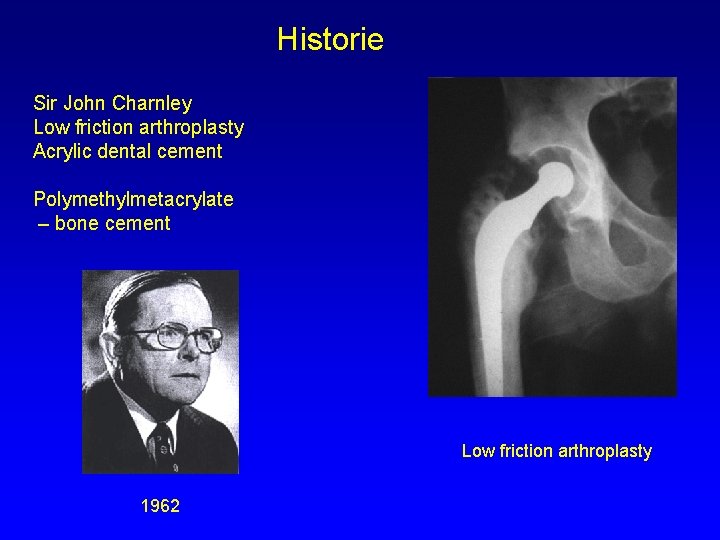
Historie Sir John Charnley Low friction arthroplasty Acrylic dental cement Polymethylmetacrylate – bone cement Low friction arthroplasty 1962
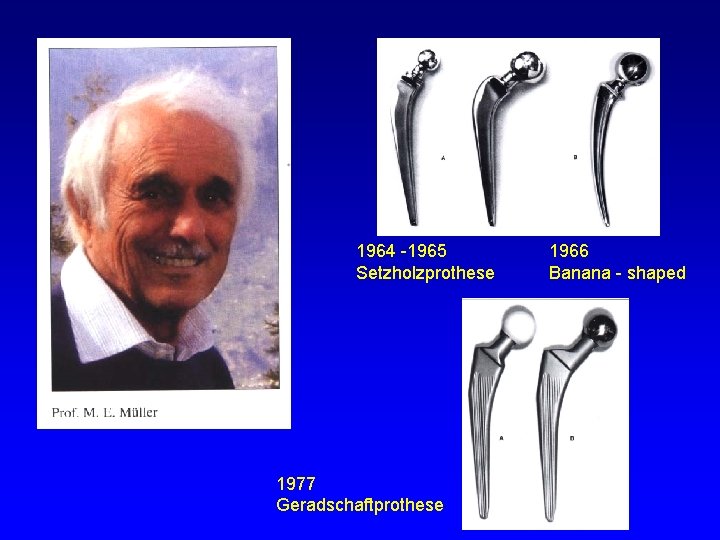
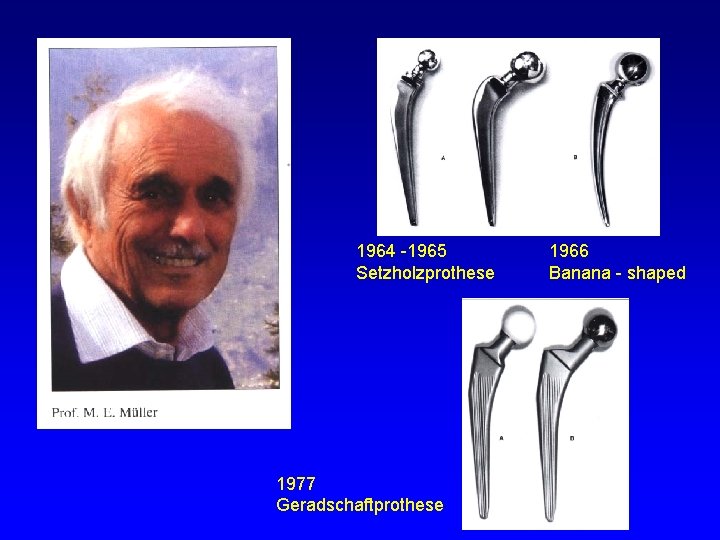
1964 -1965 Setzholzprothese 1977 Geradschaftprothese 1966 Banana - shaped
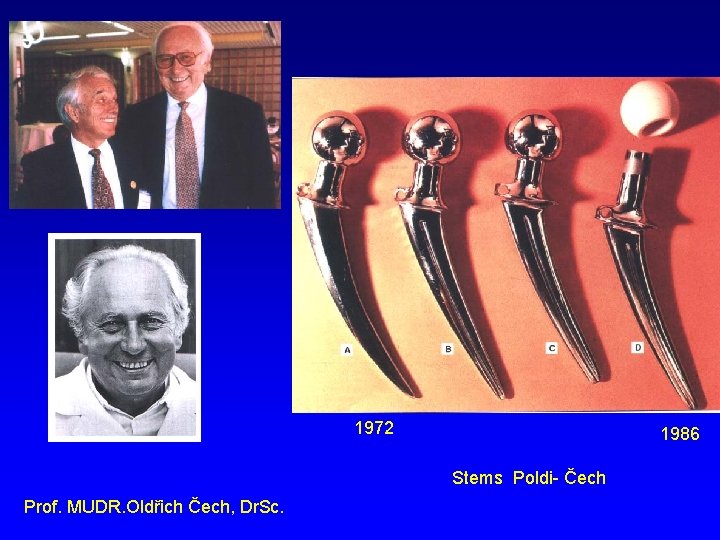
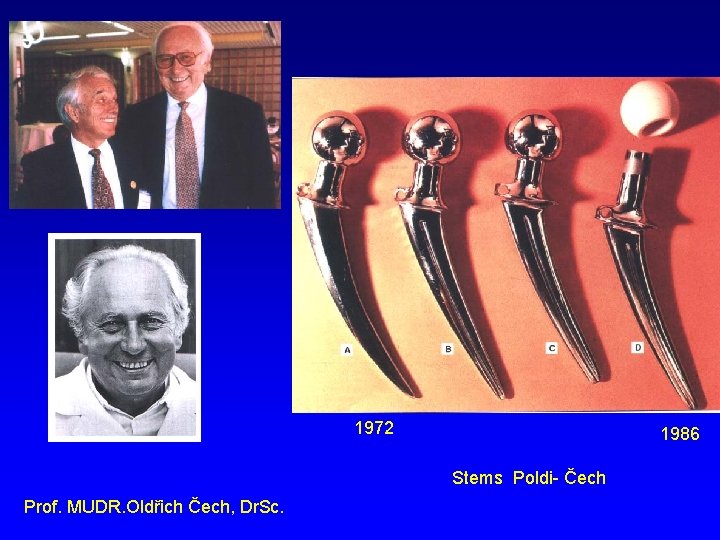
1972 1986 Stems Poldi- Čech Prof. MUDR. Oldřich Čech, Dr. Sc.
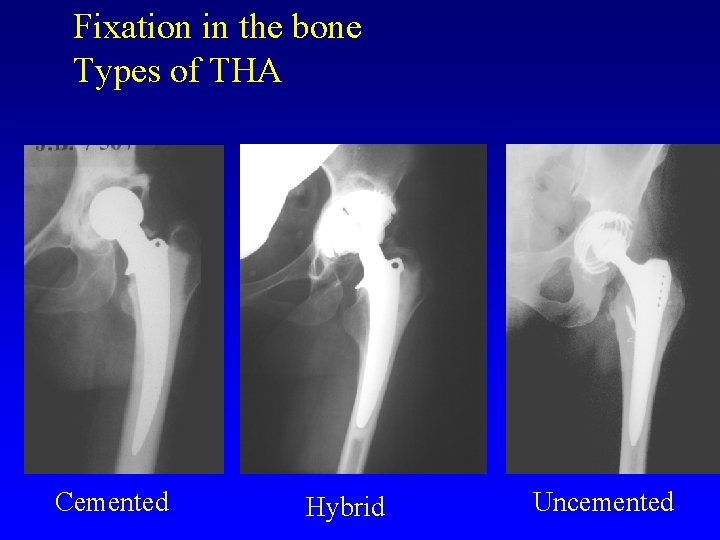
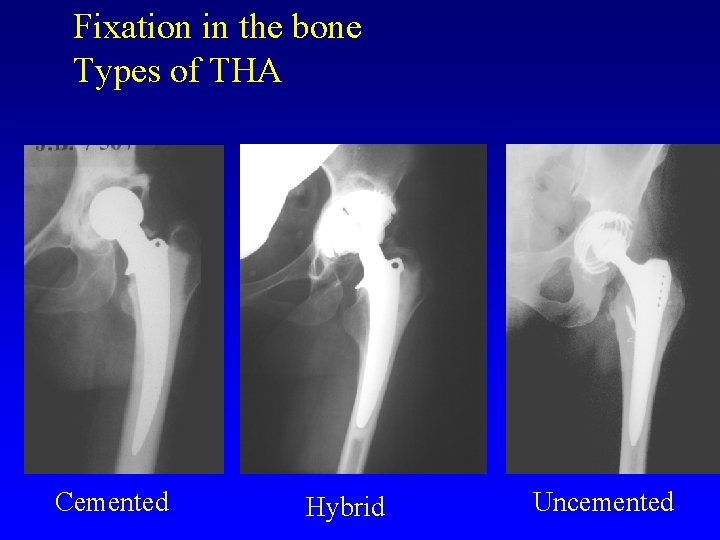
Fixation in the bone Types of THA Cemented Hybrid Uncemented
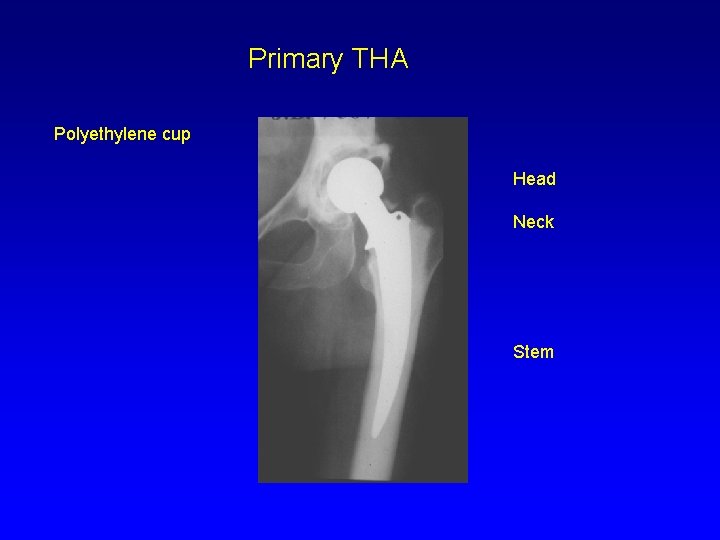
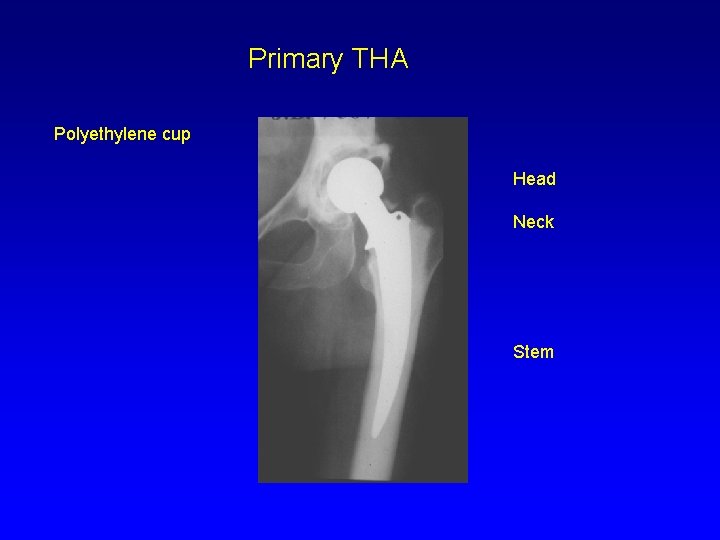
Primary THA Polyethylene cup Head Neck Stem
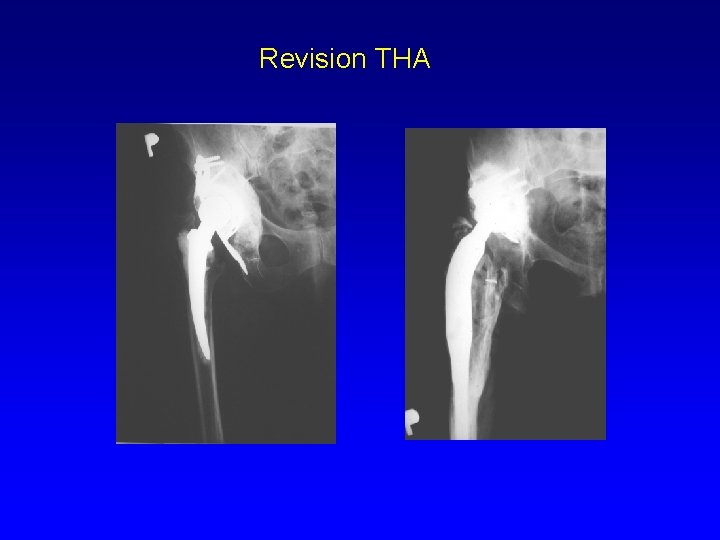
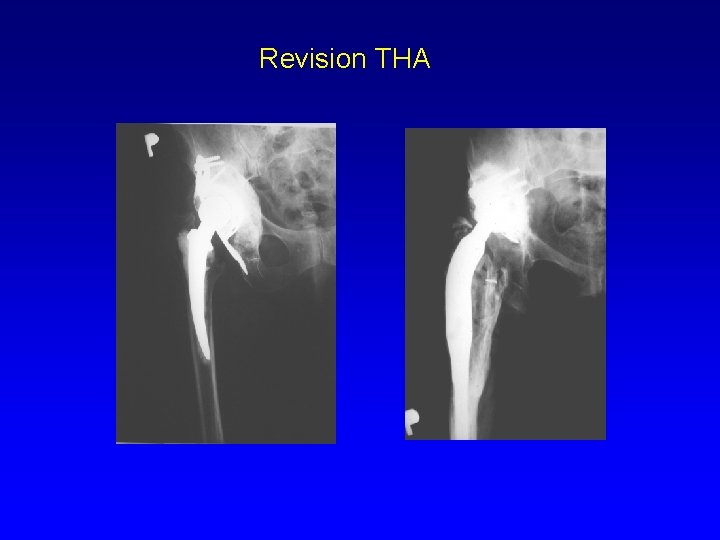
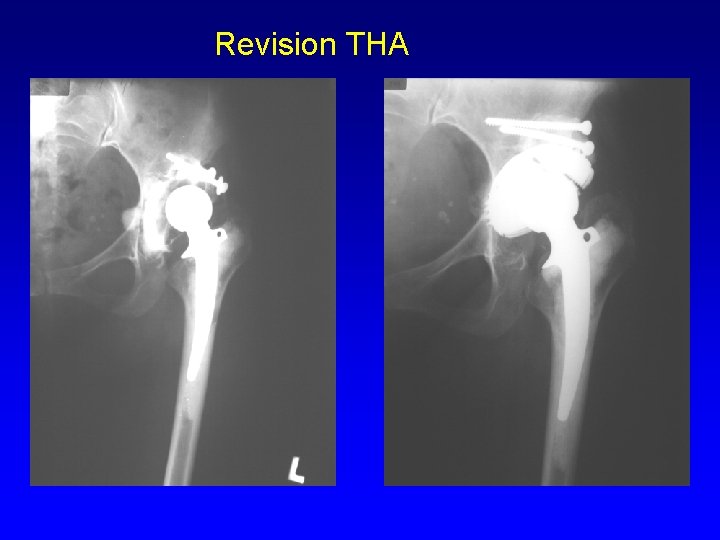
Revision THA
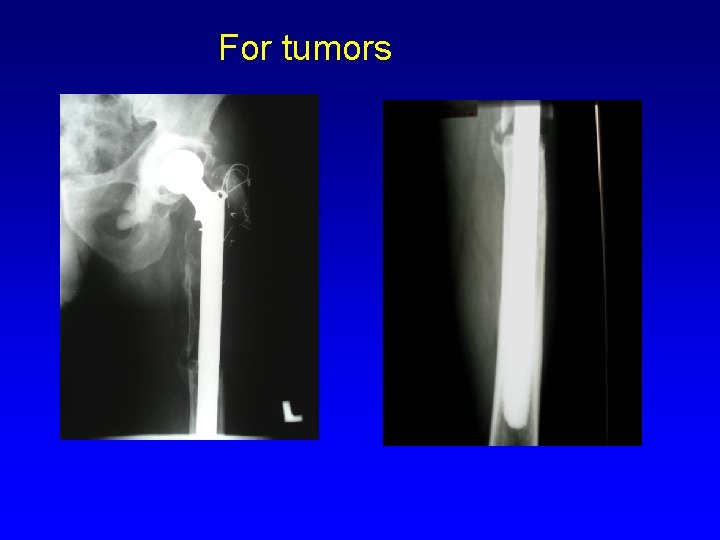
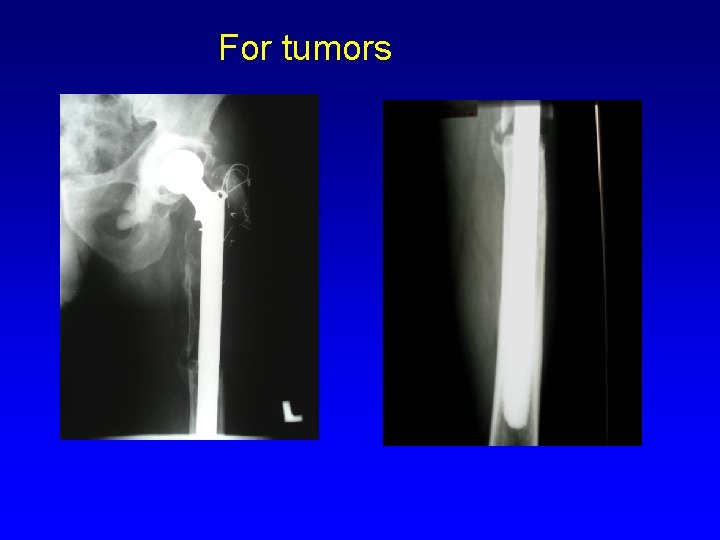
For tumors
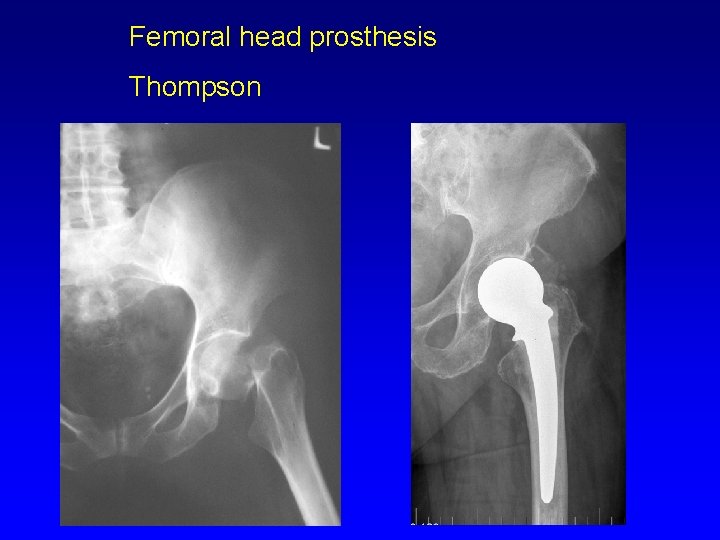
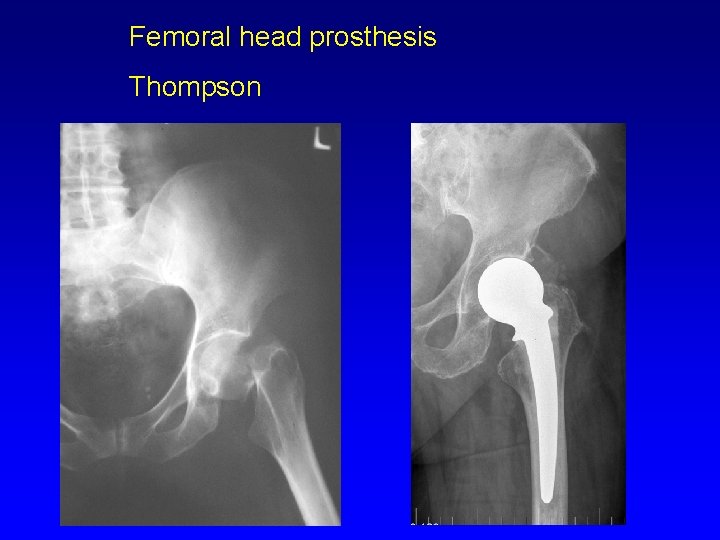
Femoral head prosthesis Thompson

Metal • Steel • Cobalt - chromiummolybdenum alloys • Titanium alloys
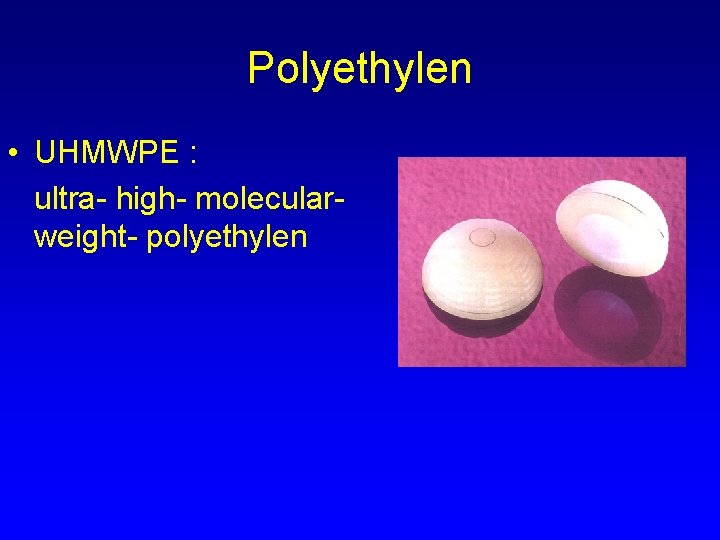
Polyethylen • UHMWPE : ultra- high- molecularweight- polyethylen
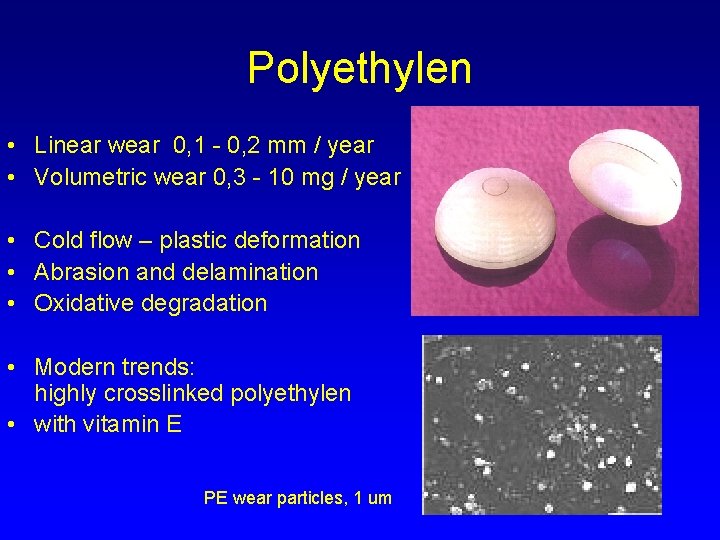
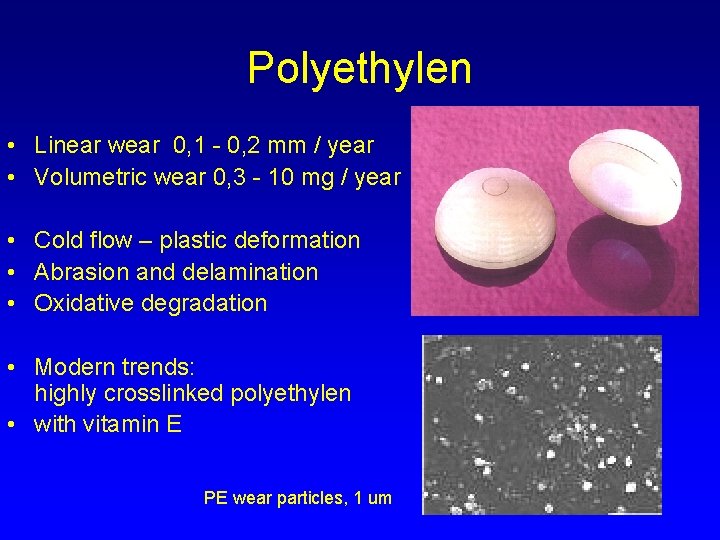
Polyethylen • Linear wear 0, 1 - 0, 2 mm / year • Volumetric wear 0, 3 - 10 mg / year • Cold flow – plastic deformation • Abrasion and delamination • Oxidative degradation • Modern trends: highly crosslinked polyethylen • with vitamin E PE wear particles, 1 um
XPE- highly-cross-linked polyethylen + vitamin E Antioxidant Increases mechanical properties of PE
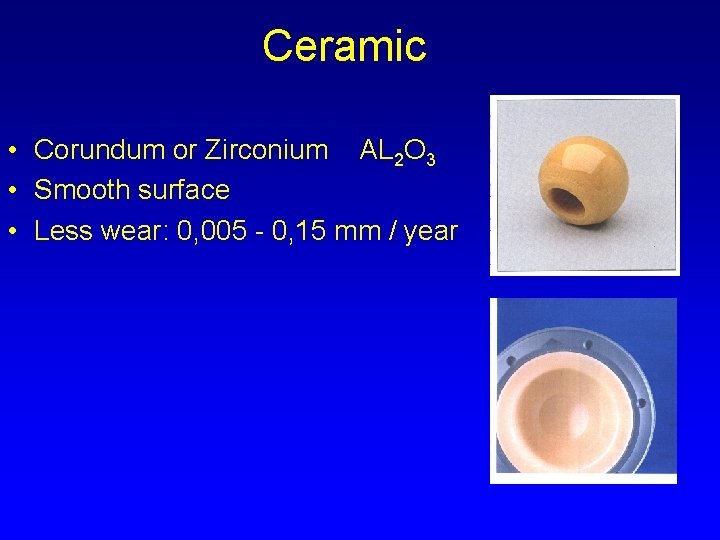
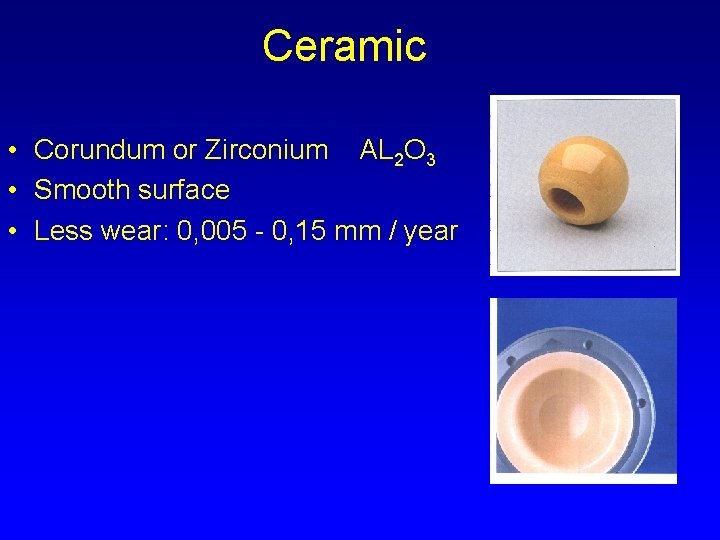
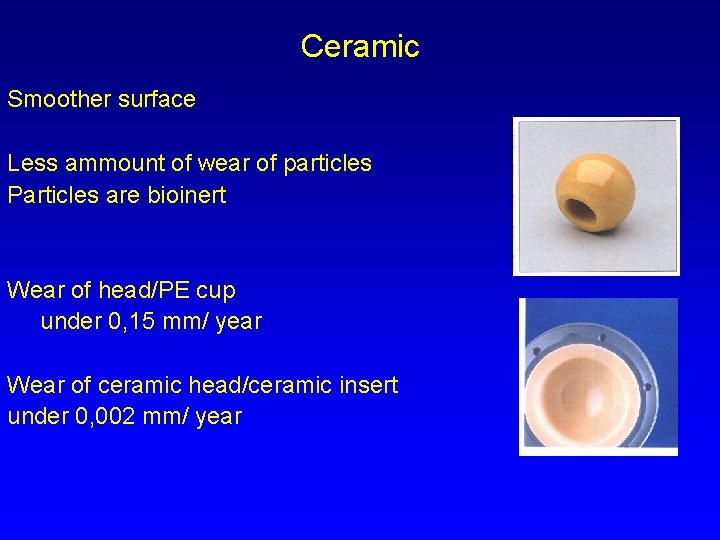
Ceramic • Corundum or Zirconium AL 2 O 3 • Smooth surface • Less wear: 0, 005 - 0, 15 mm / year
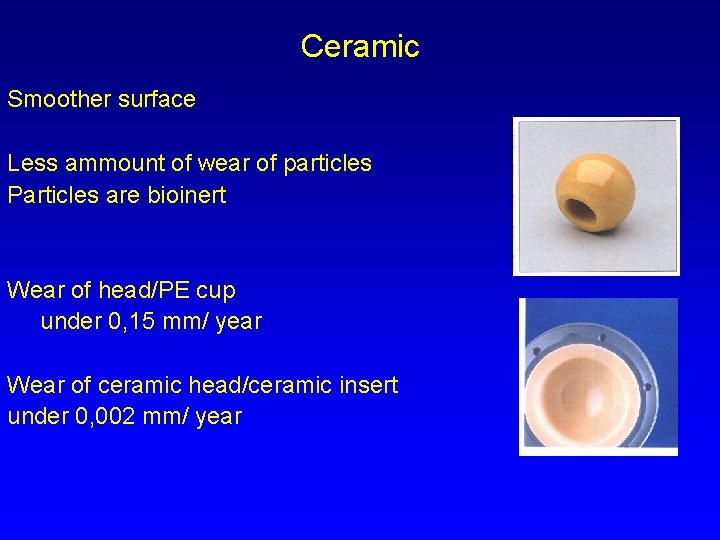
Ceramic Smoother surface Less ammount of wear of particles Particles are bioinert Wear of head/PE cup under 0, 15 mm/ year Wear of ceramic head/ceramic insert under 0, 002 mm/ year

Contact : head - cup • Metal- polyethylen • Ceramic -ceramic
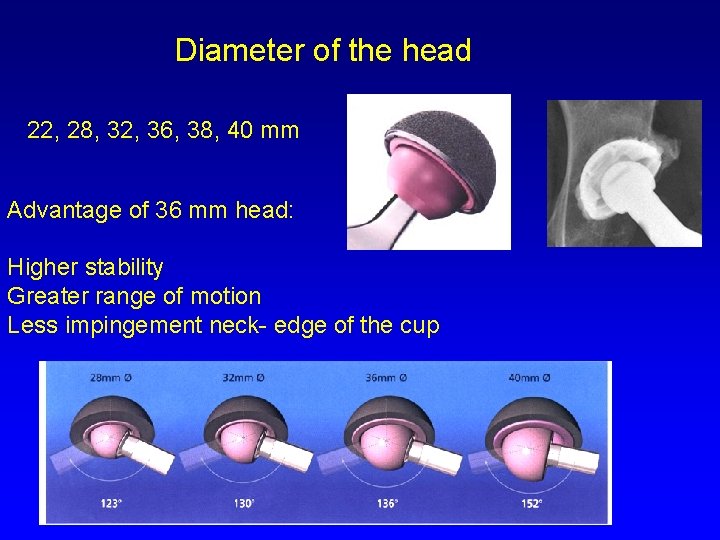
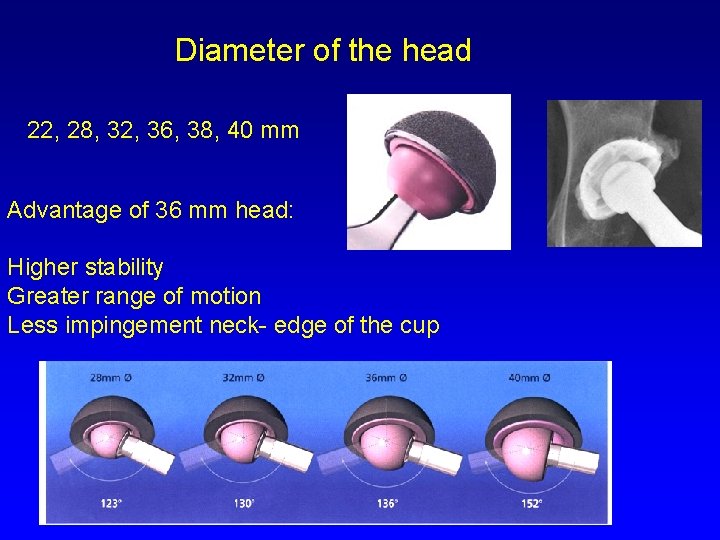
Diameter of the head 22, 28, 32, 36, 38, 40 mm Advantage of 36 mm head: Higher stability Greater range of motion Less impingement neck- edge of the cup

Bone cement • Polymethylmetacrylate • Powder polymer, fluid monomer • Exothermic reaction 83 - 100° C • Hardening in 10 min. • Adverse effects: hypotension, coagulation of proteins, cytotoxicity
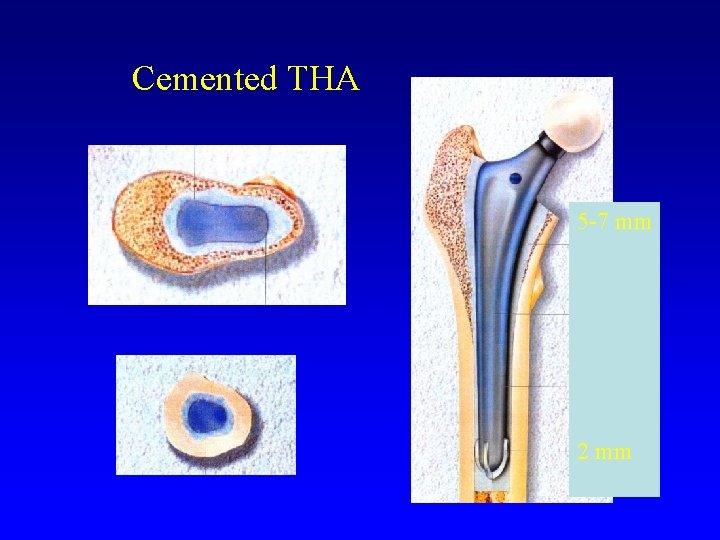
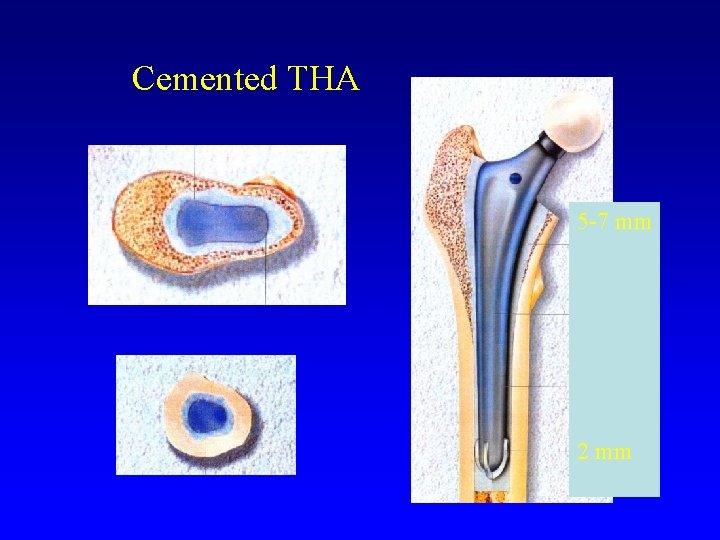
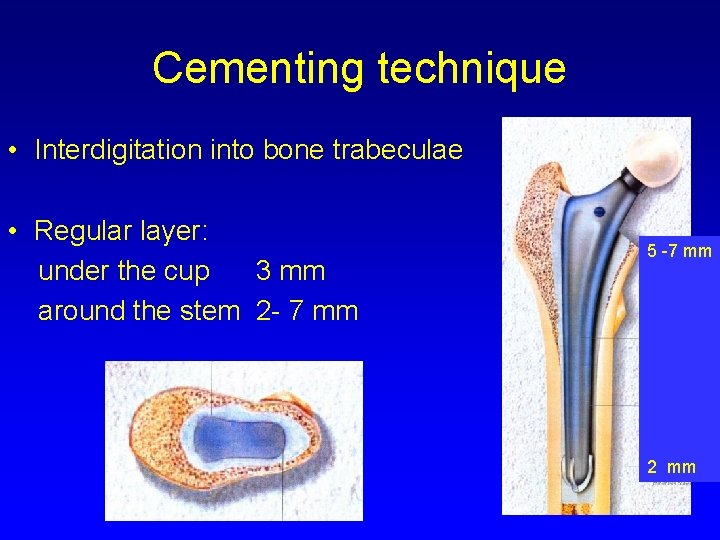
Cemented THA 5 -7 mm 2 mm
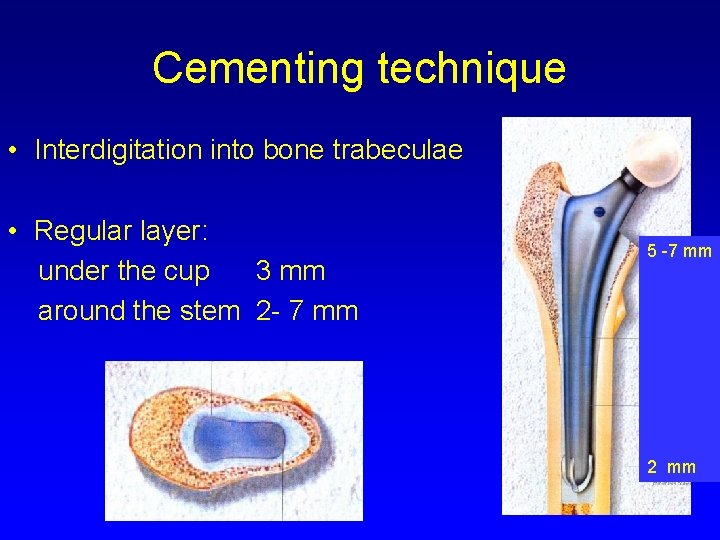
Cementing technique • Interdigitation into bone trabeculae • Regular layer: under the cup 3 mm around the stem 2 - 7 mm 5 -7 mm 2 mm
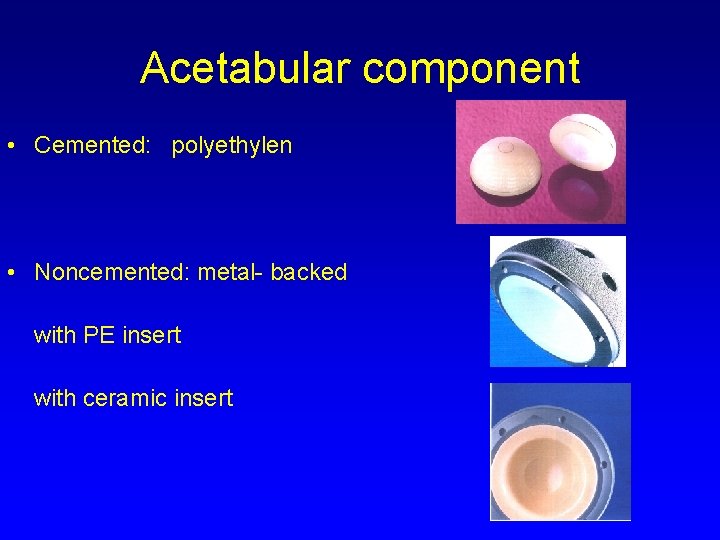
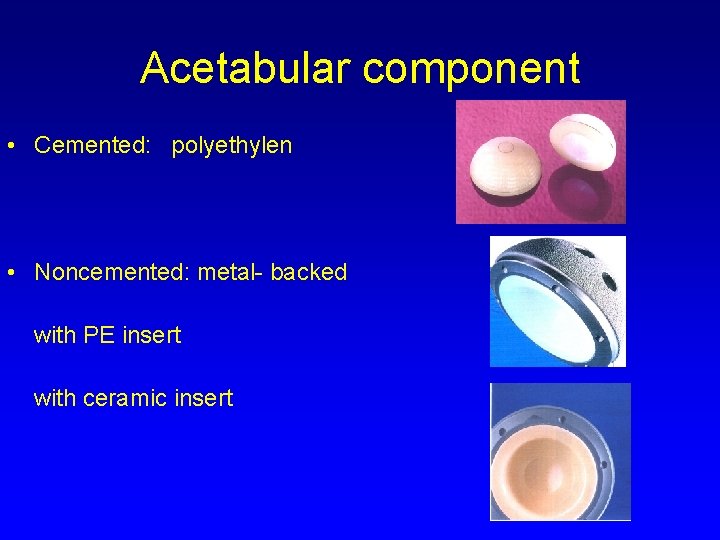
Acetabular component • Cemented: polyethylen • Noncemented: metal- backed with PE insert with ceramic insert
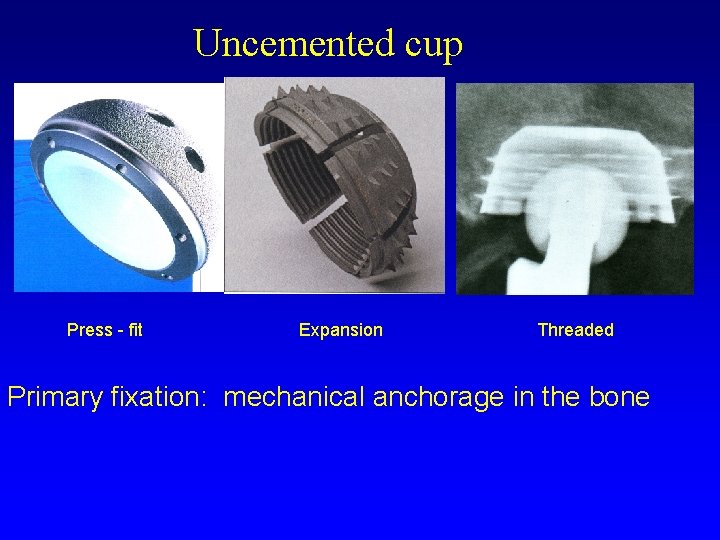
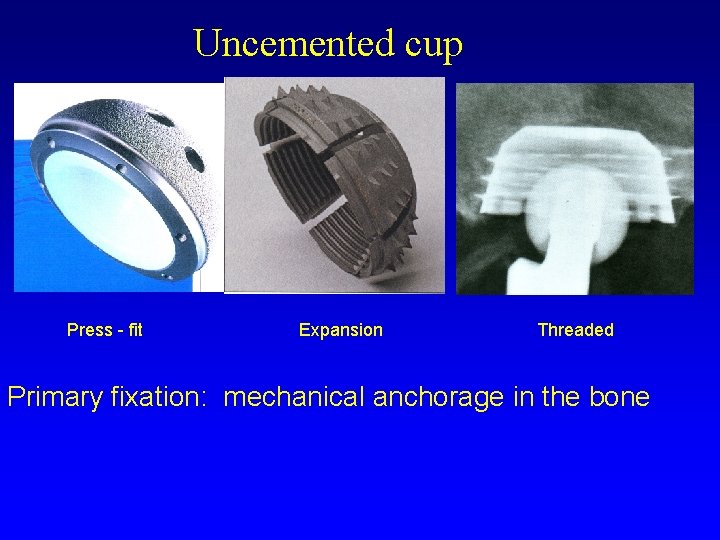
Uncemented cup Press - fit Expansion Threaded Primary fixation: mechanical anchorage in the bone
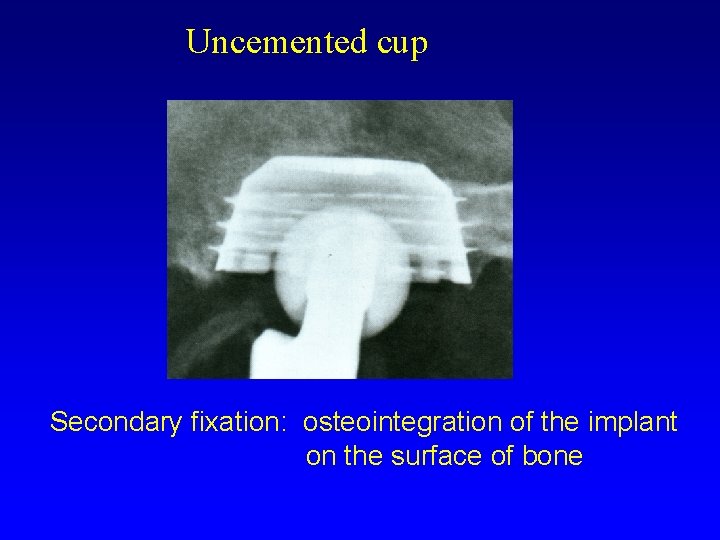
Uncemented cup Secondary fixation: osteointegration of the implant on the surface of bone
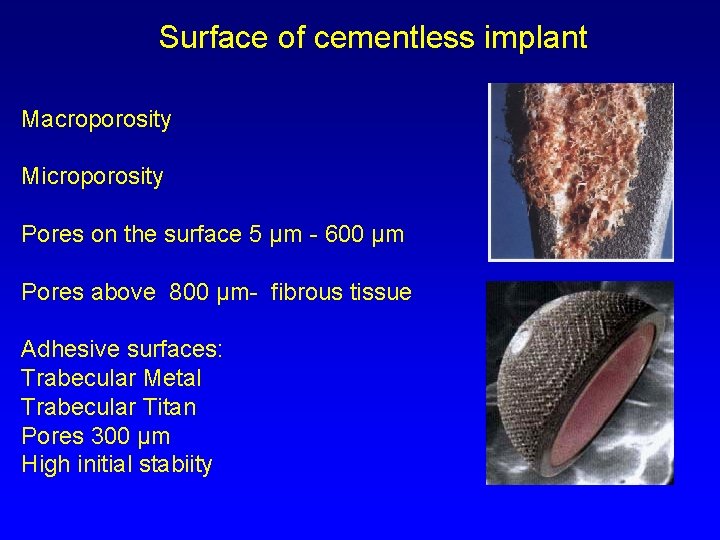
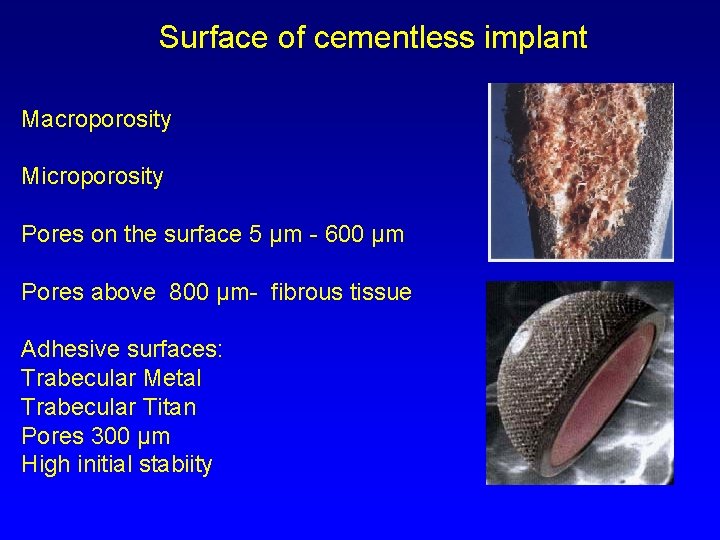
Surface of cementless implant Macroporosity Microporosity Pores on the surface 5 µm - 600 µm Pores above 800 µm- fibrous tissue Adhesive surfaces: Trabecular Metal Trabecular Titan Pores 300 µm High initial stabiity
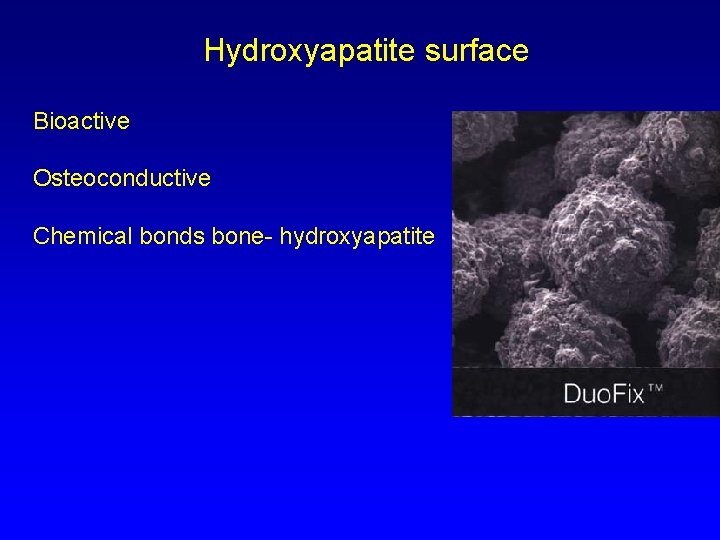
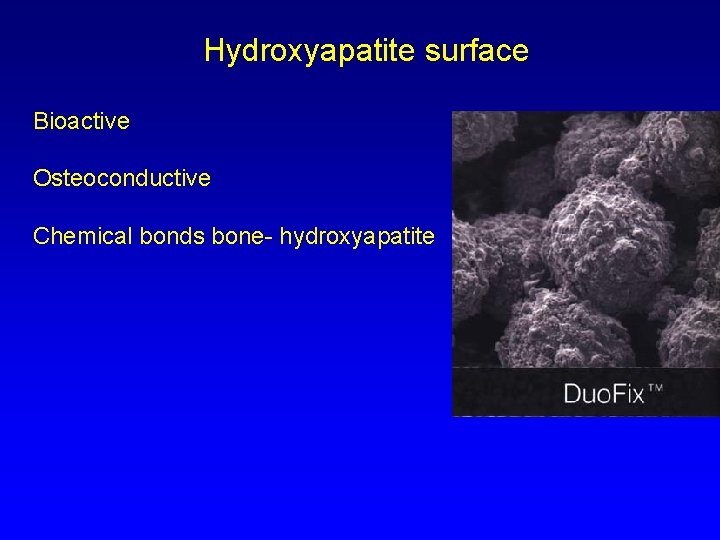
Hydroxyapatite surface Bioactive Osteoconductive Chemical bonds bone- hydroxyapatite

Expansion cup- CLS

Bicon – Zweyműller cup
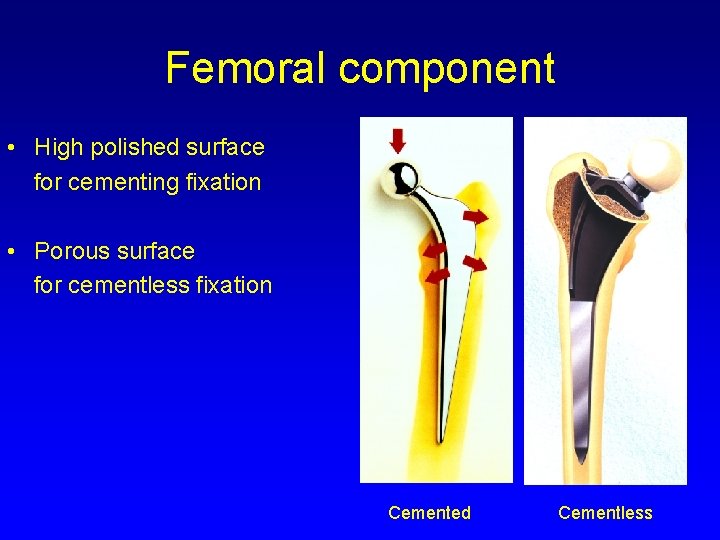
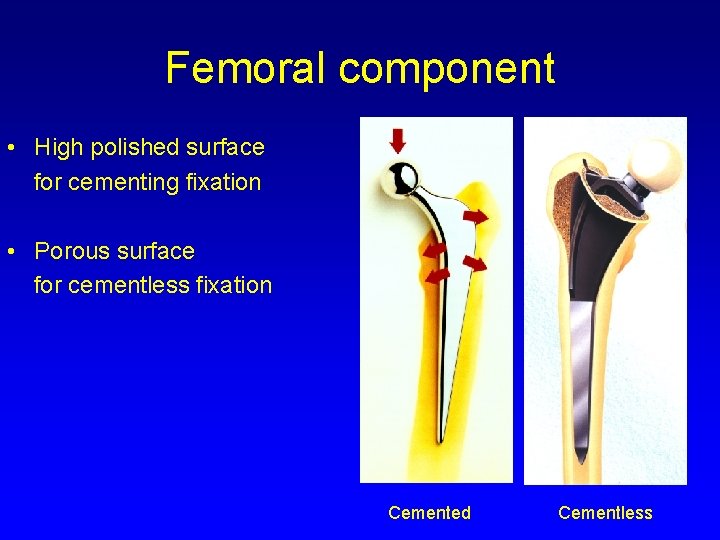
Femoral component • High polished surface for cementing fixation • Porous surface for cementless fixation Cemented Cementless

Morscher, Spotorno MS – 30 stem cemented

Uncemented stems Proximal fixed Distal fixed
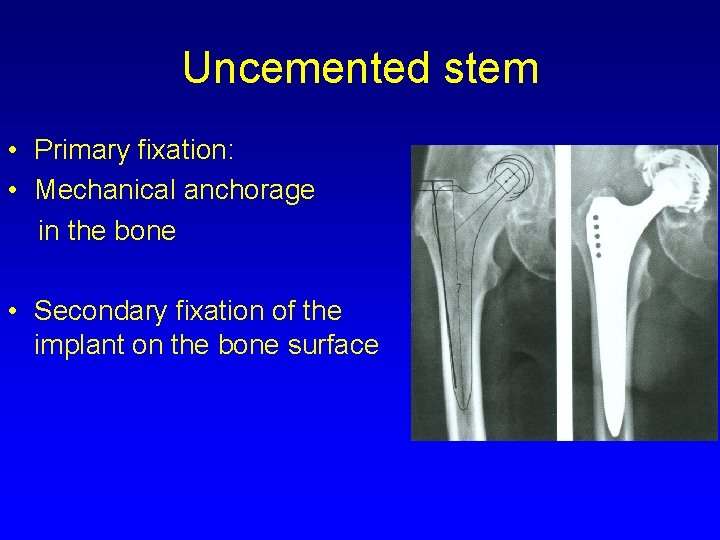
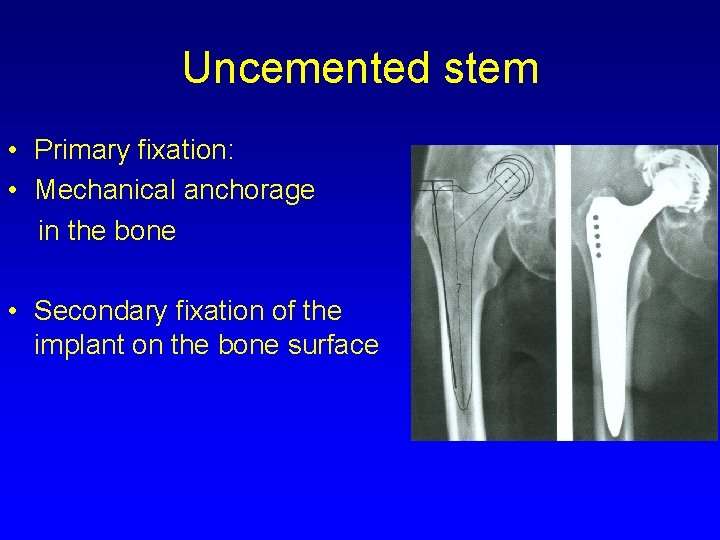
Uncemented stem • Primary fixation: • Mechanical anchorage in the bone • Secondary fixation of the implant on the bone surface
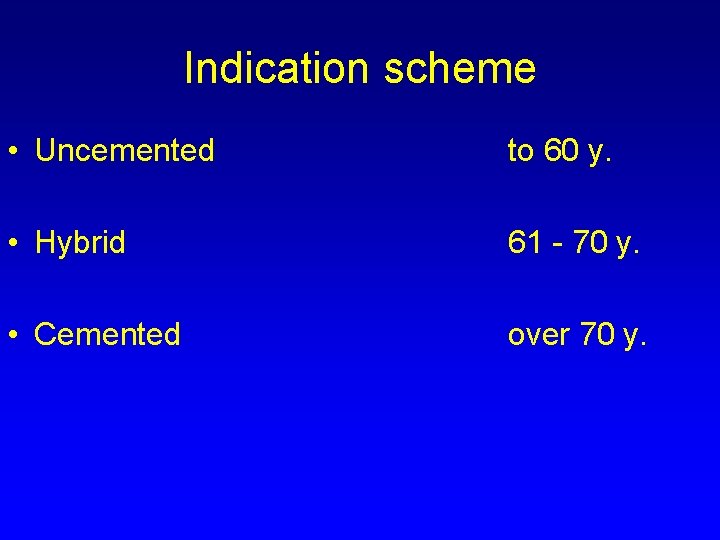
Indication scheme • Uncemented to 60 y. • Hybrid 61 - 70 y. • Cemented over 70 y.
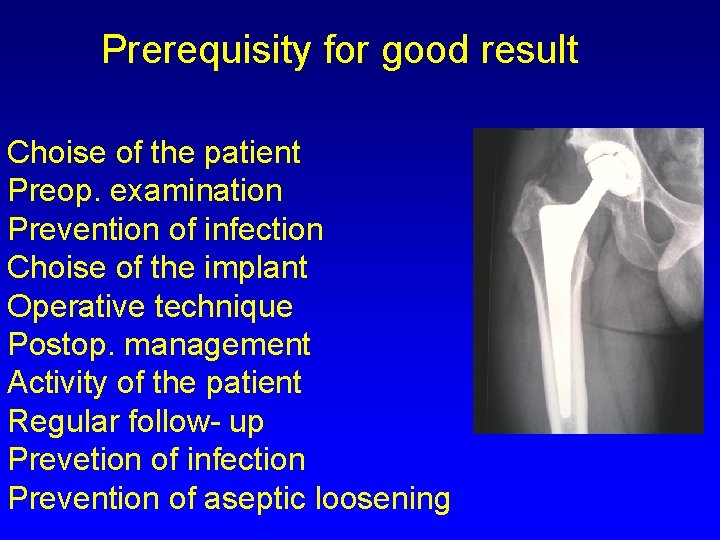
Prerequisity for good result Choise of the patient Preop. examination Prevention of infection Choise of the implant Operative technique Postop. management Activity of the patient Regular follow- up Prevetion of infection Prevention of aseptic loosening
Contraindication • • Active infection of the hip Infection in the body General condition not good Neurogenic arthropathy Extreme low bone quality No cooperation of the patient Relative: age over 80 y. elevated ESR

Approaches

MIS- mini invasive surgery
Operative technique Femur – brush pulsatile lavage sealing of medular cavity prox. - dist. drainage of the femur Vacuum mixing of bone cement Pressurisation of bone cement Timing of insertion of the stem Continuous pressure

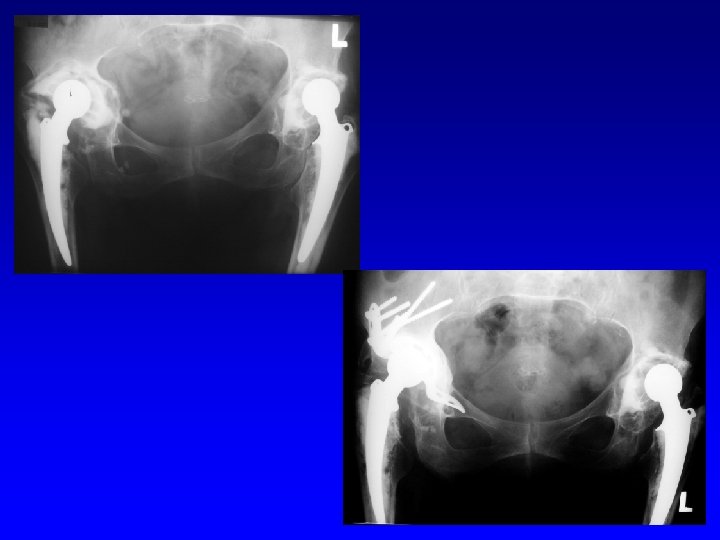
Revision THA


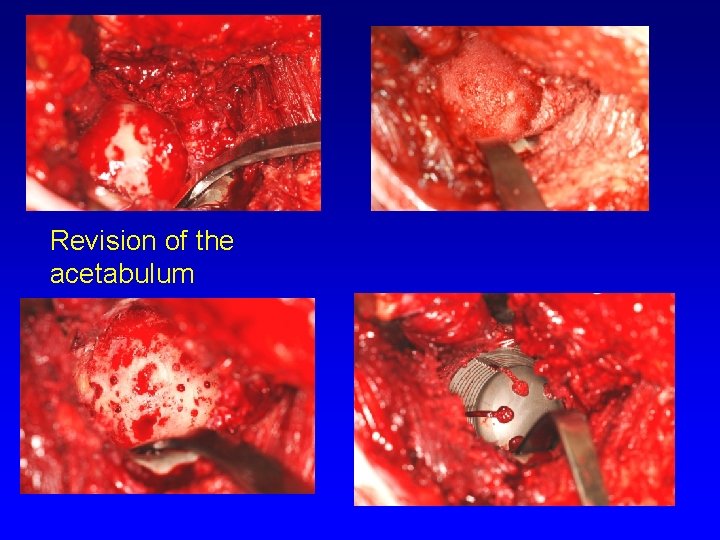
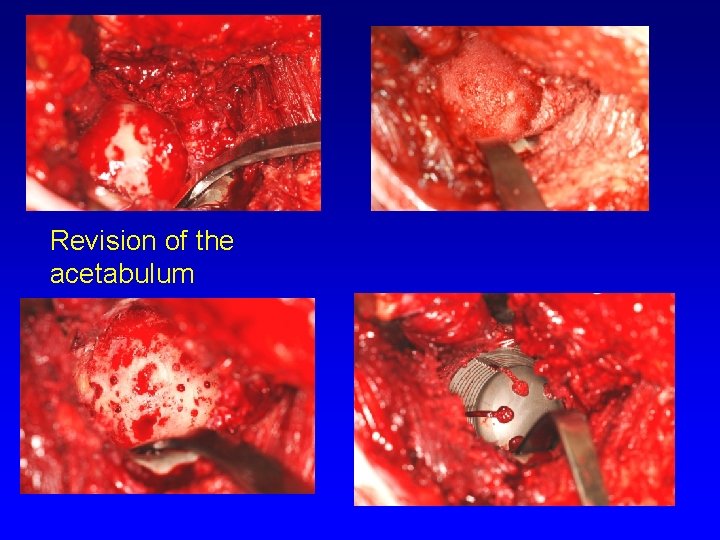
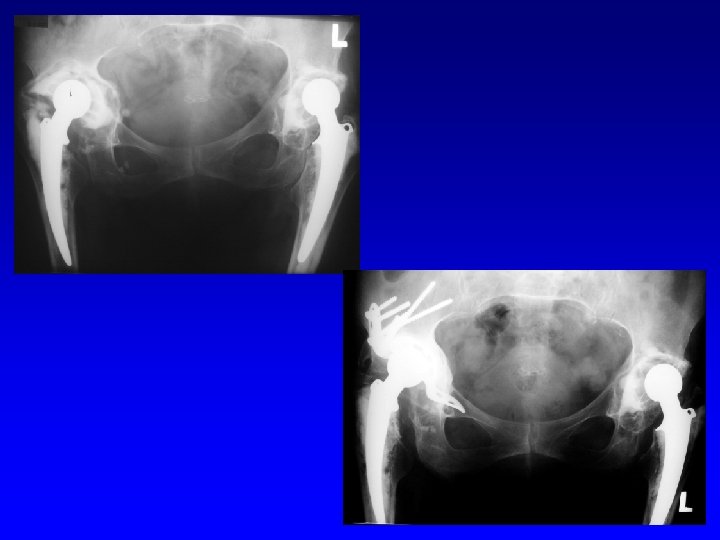
Revision of the acetabulum
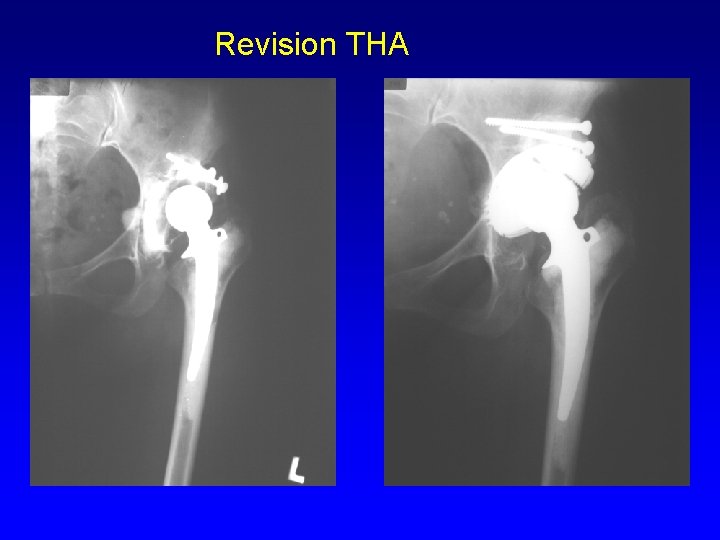
Revision THA


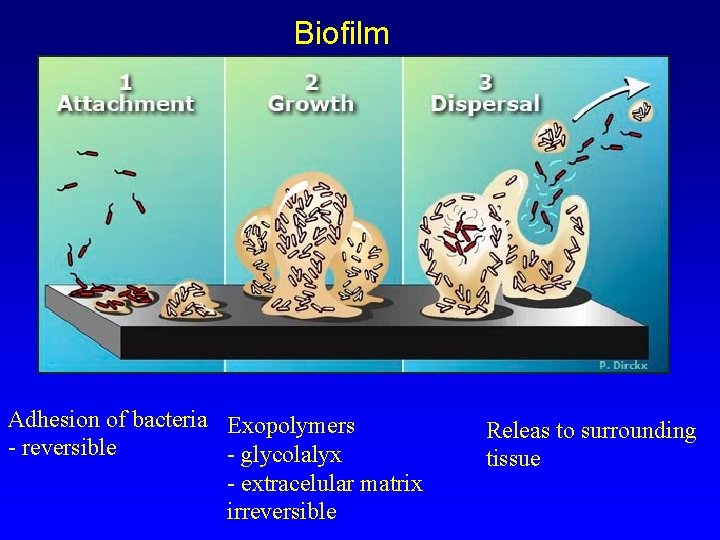
Periprosthetic infection St. aureus St. coagulase negative Streptococci Enterococci, others MRSA, MRSE Polyresistant G- bacteria Sessile form and planctonic Race for surface They produce glycocalyx- mucose substance of glycoproteins It leads to high resistence to antibodies and antibiotics Biofilm
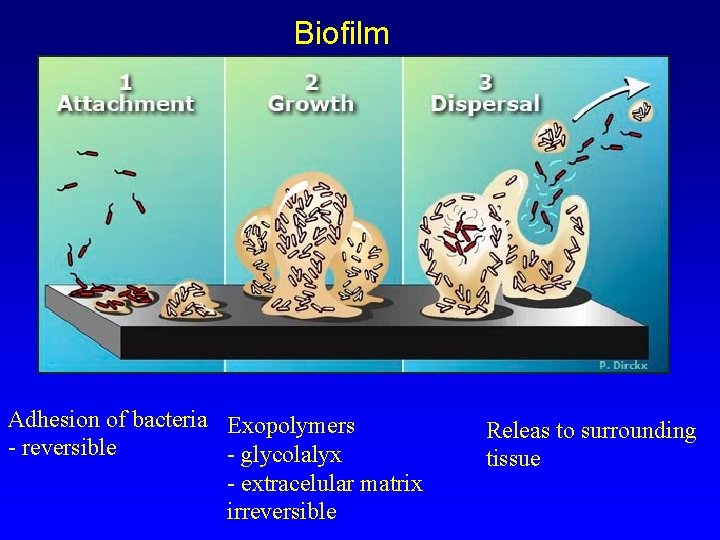
Biofilm Adhesion of bacteria Exopolymers - reversible - glycolalyx - extracelular matrix irreversible Releas to surrounding tissue
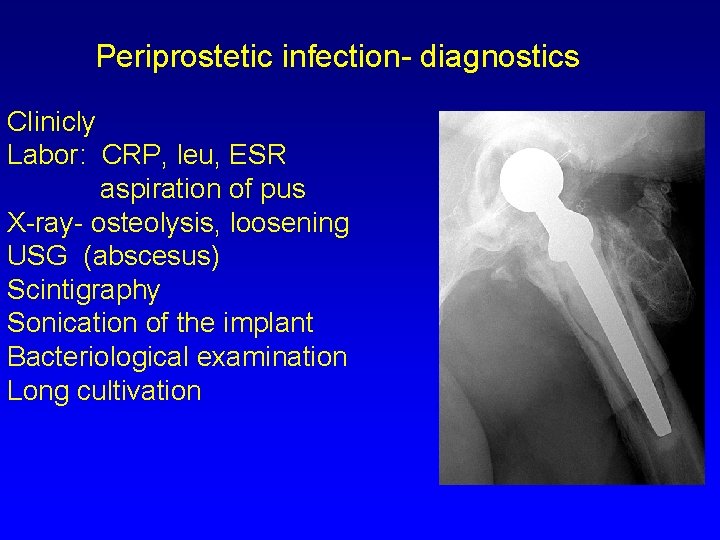
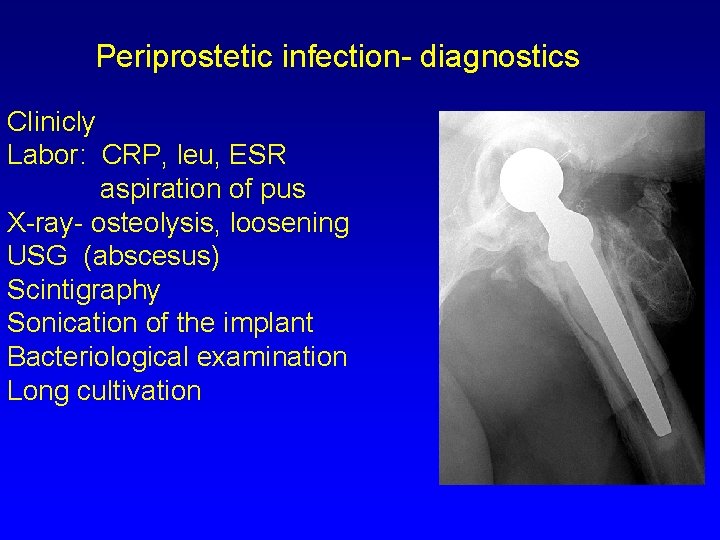
Periprostetic infection- diagnostics Clinicly Labor: CRP, leu, ESR aspiration of pus X-ray- osteolysis, loosening USG (abscesus) Scintigraphy Sonication of the implant Bacteriological examination Long cultivation
Periprostetic infection- PPI Acute PPI Chronic PPI Late haematogenic PPI

Management To start treatment as soon as possible: 10 -14 days from the onset of symptoms Prerequisity: cooperation of the patient informed physician

Periprosthetic infection-treatment Debridement One stage surgery Two stage surgery Resection artroplasty Antibiotic suppresion

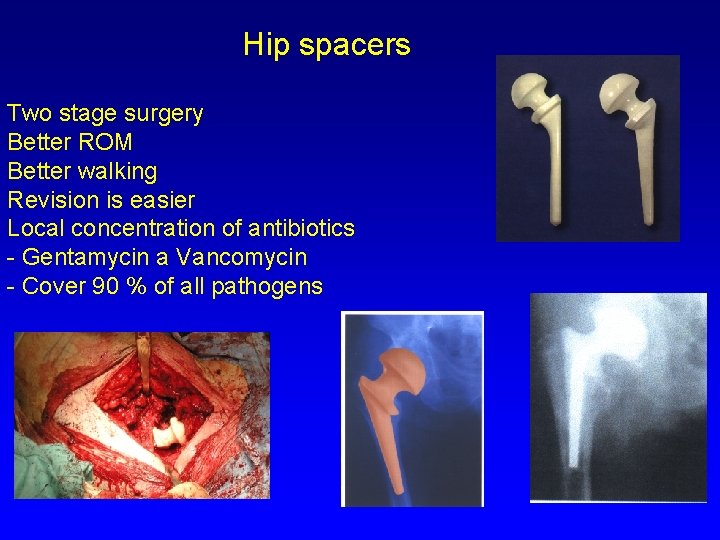
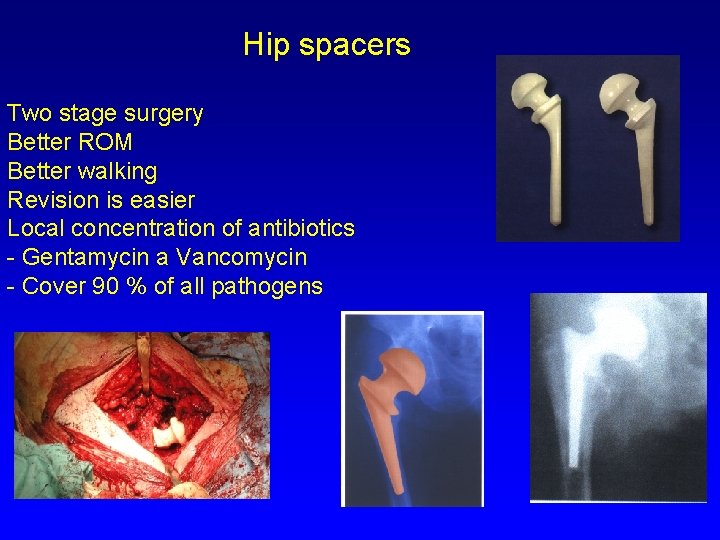
Hip spacers Two stage surgery Better ROM Better walking Revision is easier Local concentration of antibiotics - Gentamycin a Vancomycin - Cover 90 % of all pathogens

Principles Experience of the hospital Long term results National registries Operative technique Reliable implants Activity of the patient Regular follow up
Daily activity after THA No lifting and wearing of heavy objects No strenuous manual labor Limited running and jumping No contact sports Recommened sports: swimming, bicycle, tennis tourism, skiing?
 Occupational therapy intervention plan for hip arthroplasty
Occupational therapy intervention plan for hip arthroplasty Periprostetic
Periprostetic Enarthrosis
Enarthrosis Enarthroses
Enarthroses Arthroplasty practitioner
Arthroplasty practitioner Hip hop hip to the hippity
Hip hop hip to the hippity Hip hop hip the hippity
Hip hop hip the hippity Hip joint ppt
Hip joint ppt Pelvis surface anatomy
Pelvis surface anatomy Coracohumeral ligament
Coracohumeral ligament X-ray hip joint
X-ray hip joint Suspension therapy for hip joint
Suspension therapy for hip joint Fibrous capsule of hip joint
Fibrous capsule of hip joint Biomekanik hip joint
Biomekanik hip joint Pelvic extension
Pelvic extension Hip joint type and subtype
Hip joint type and subtype Joint venture account
Joint venture account Spool joint lamb
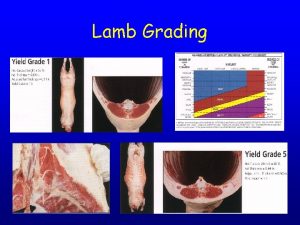
Spool joint lamb Lamb carcass grading
Lamb carcass grading Hyaline cartilage in vertebrae
Hyaline cartilage in vertebrae Ellipsoid joint
Ellipsoid joint Non permanent joint คือ
Non permanent joint คือ Total revenue minus total expenses
Total revenue minus total expenses Total revenues minus total costs equals
Total revenues minus total costs equals Total revenues minus total costs equals
Total revenues minus total costs equals Total revenues minus total costs equals
Total revenues minus total costs equals Activo promedio
Activo promedio Checkrein taping definition
Checkrein taping definition Hip hop publications
Hip hop publications Barlow ortolani
Barlow ortolani Shakespeare is hip-hop flocabulary answer key
Shakespeare is hip-hop flocabulary answer key Bo jackson hip dislocation
Bo jackson hip dislocation Hip international limited
Hip international limited Hip lateral rotation
Hip lateral rotation Protocolo sctp
Protocolo sctp Hands on hips
Hands on hips Hip pointer moi
Hip pointer moi Hyperextension
Hyperextension Weak abductors
Weak abductors Subkultur hip hop
Subkultur hip hop Hip bone
Hip bone Chapter 17 the thigh hip groin and pelvis
Chapter 17 the thigh hip groin and pelvis Bryant traction
Bryant traction Ppt
Ppt Flocabulary shakespeare is hip hop
Flocabulary shakespeare is hip hop Leverage flag in football
Leverage flag in football Hip hop questions to ask
Hip hop questions to ask Bryant triangle
Bryant triangle Hip club
Hip club Hip hop php
Hip hop php Hip usg
Hip usg Chapter 17 the thigh hip groin and pelvis
Chapter 17 the thigh hip groin and pelvis Coxa plana
Coxa plana Copyright
Copyright Pots fracture
Pots fracture Sacroiliac bone
Sacroiliac bone Horizontal
Horizontal Curiosidade do hip hop
Curiosidade do hip hop Hip tiles
Hip tiles Hip international
Hip international Hip hop quiz
Hip hop quiz Hip hughes hinduism
Hip hughes hinduism