Module 3 Complex primary total hip arthroplasty Small







- Slides: 33
Module 3: Complex primary total hip arthroplasty Small group discussion AO Recon Course—Complex Total Hip and Knee Arthroplasty
Learning objectives • Assess the patient preoperatively • Classify and manage hip dysplasia requiring total hip arthroplasty (THA) • Plan and perform a THA after previous femoral fracture, acetabular fracture, or femoral osteotomy 2

Case 1 3
Case history • A 36 -year-old woman • Left hip pain, greater than right hip pain • Ambulating without the use of aids • Examination: • No apparent leg-length discrepancy • Range of motion in both hips: abduction 15°, flexion 45° • Gluteus medius strength: 5/5 • No previous surgery 5

Imaging 6
Planning • Special laboratory investigations? • Additional imaging needed? 7
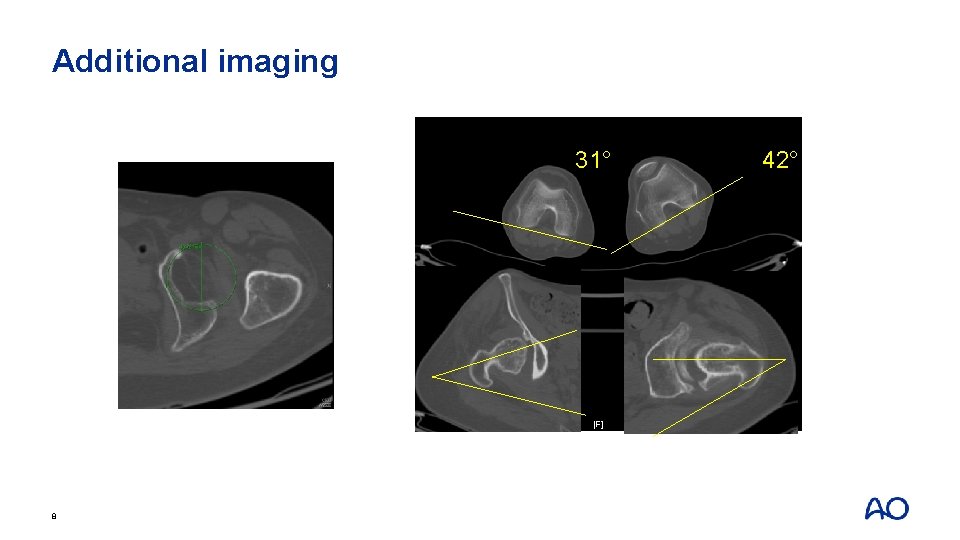
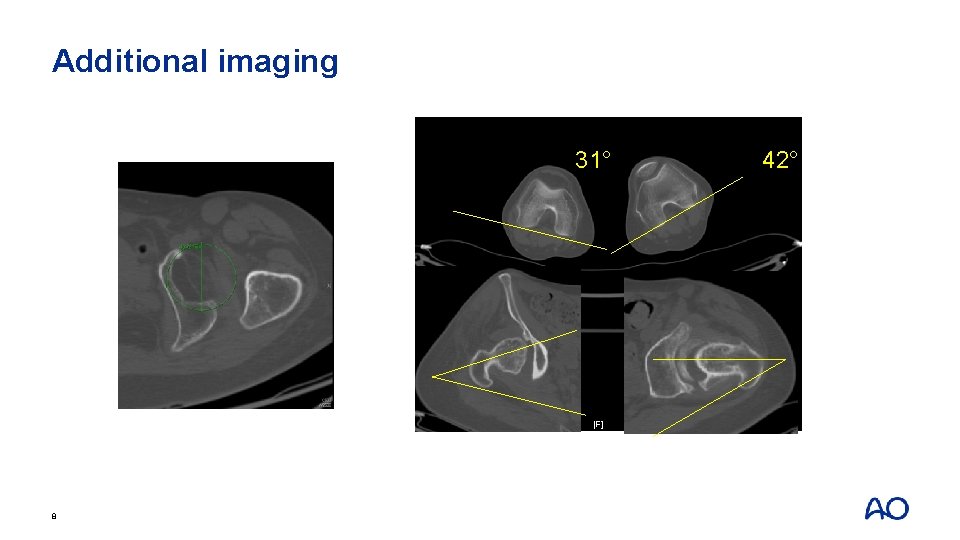
Additional imaging 31° 8 42°
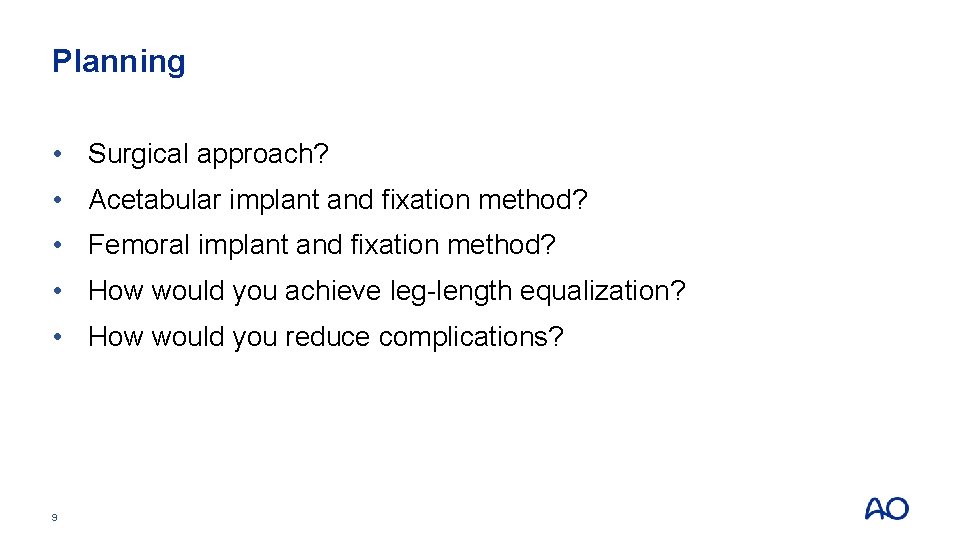
Planning • Surgical approach? • Acetabular implant and fixation method? • Femoral implant and fixation method? • How would you achieve leg-length equalization? • How would you reduce complications? 9
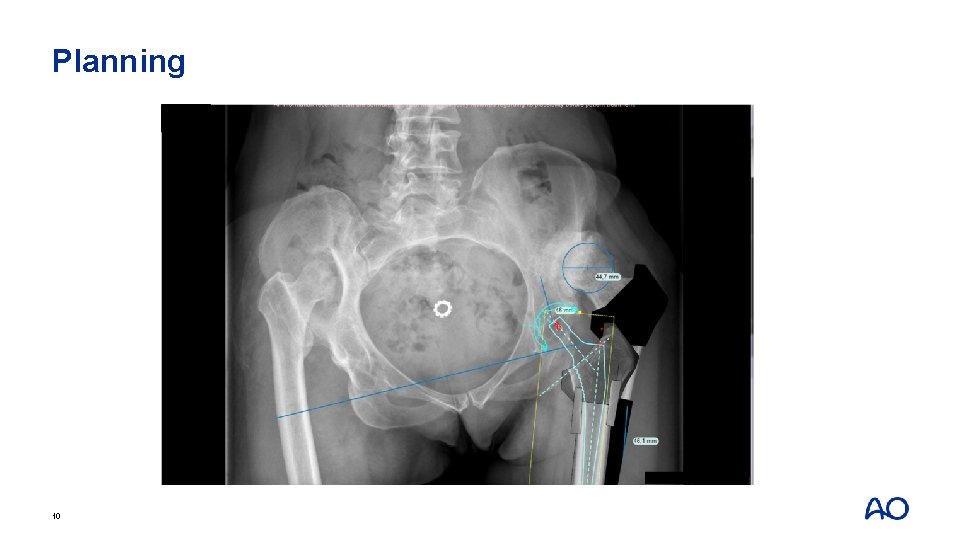
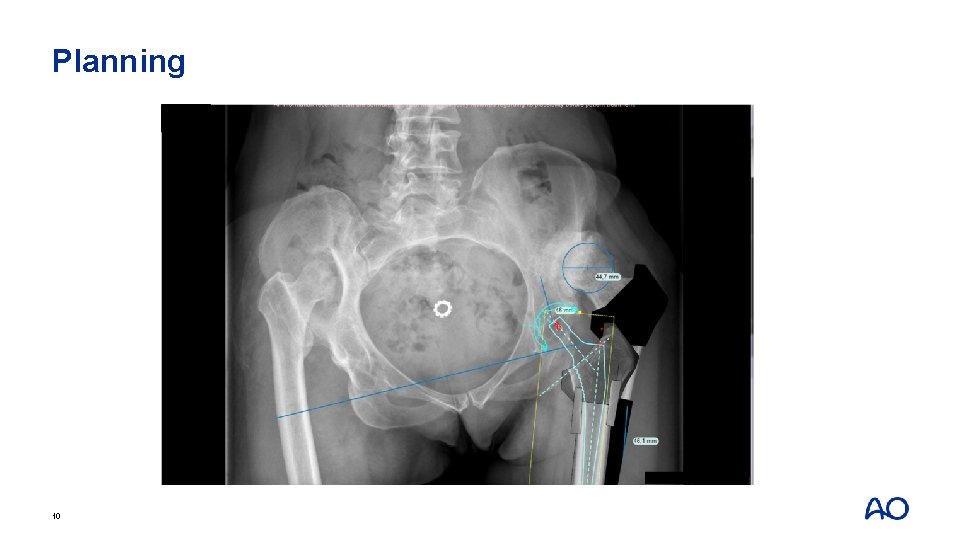
Planning 10
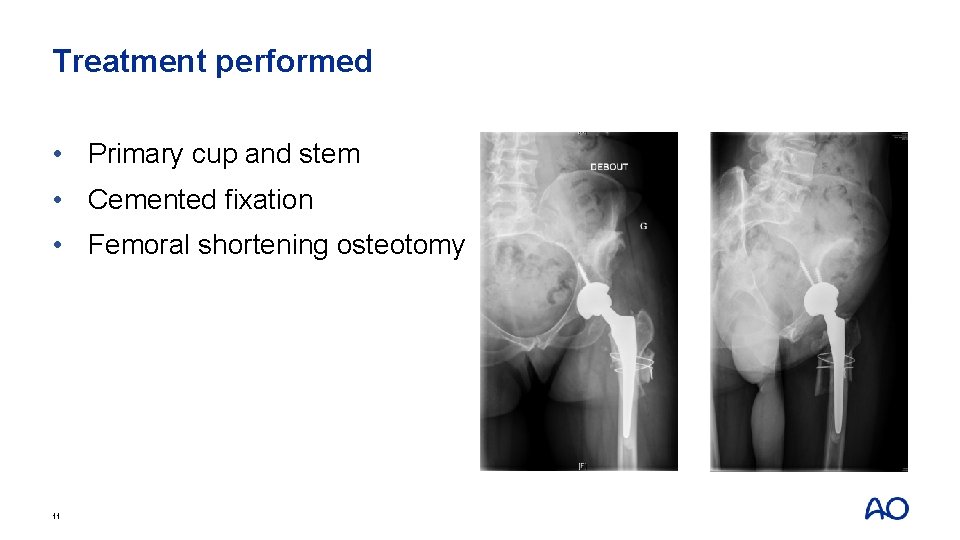
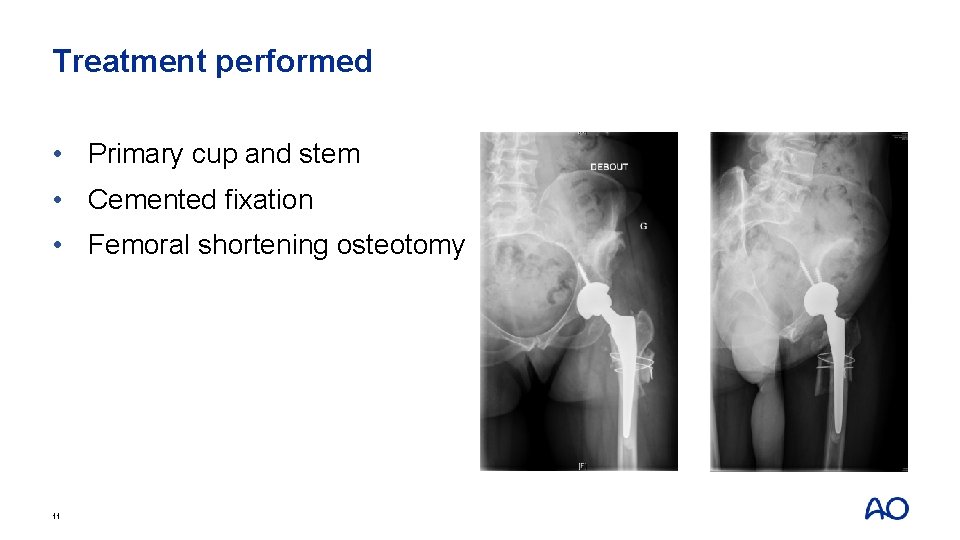
Treatment performed • Primary cup and stem • Cemented fixation • Femoral shortening osteotomy 11
Take-home messages • Should have small-diameter cups and stems in inventory • Consider shortening femoral osteotomy if: • Leg lengthening is greater than 4 cm • Maltorsion (excessive anteversion) • Bilateral high-grade dysplasia 12

Case 2 13
Case history • A 70 -year-old man • Car collision 2 years ago with pelvic-acetabular fracture • Associated injury: none • Percutaneous fixation performed • Increasing pain over past 6 months • Uses a walker now 15

Imaging 16
Planning • What other imaging studies would you order? • What laboratory tests would you order? 17
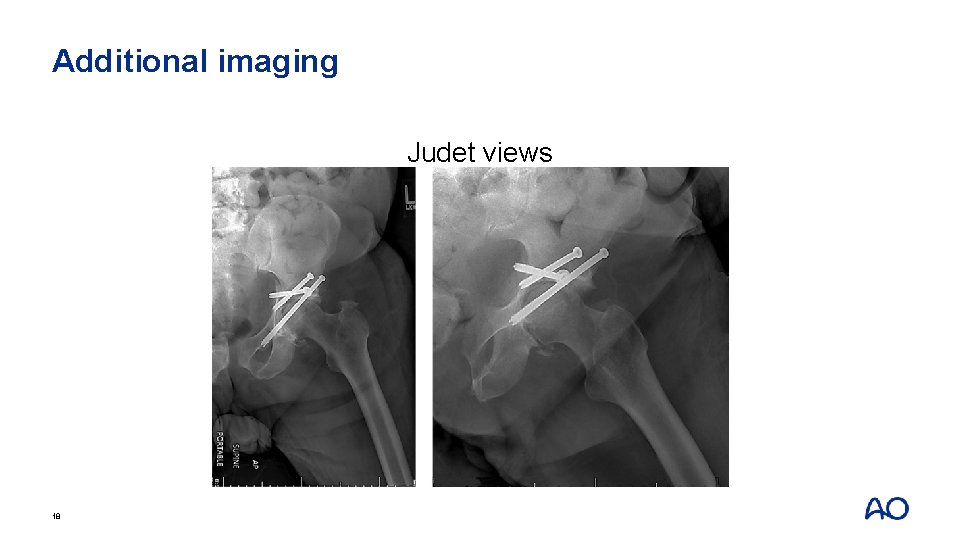
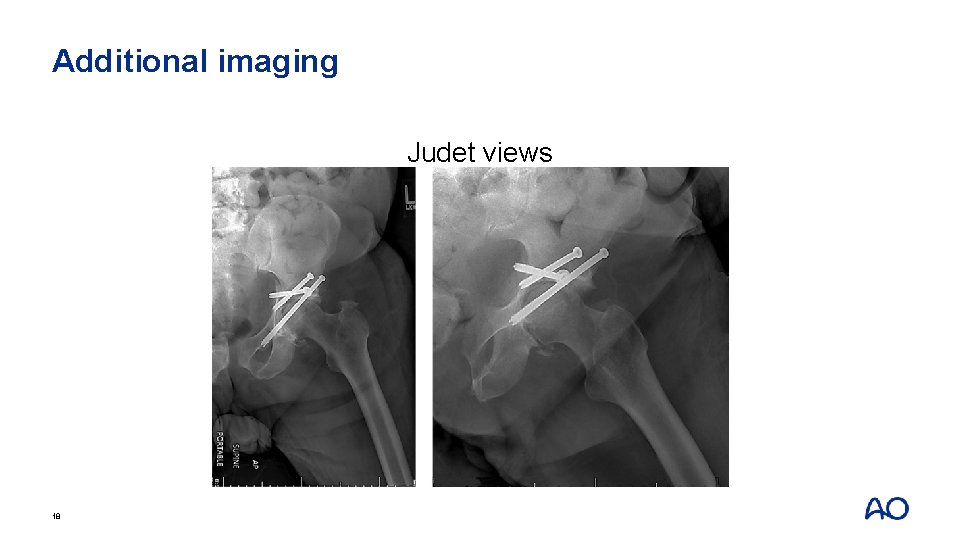
Additional imaging Judet views 18
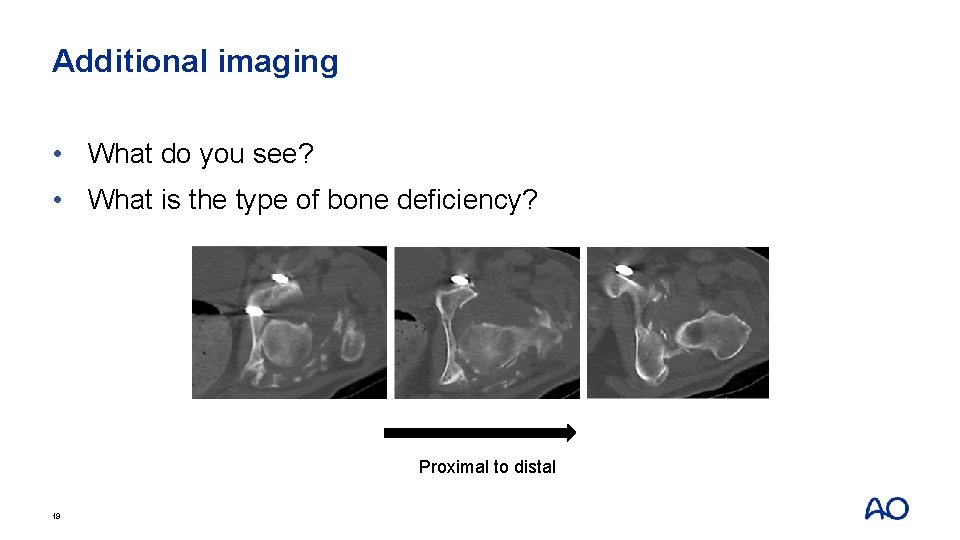
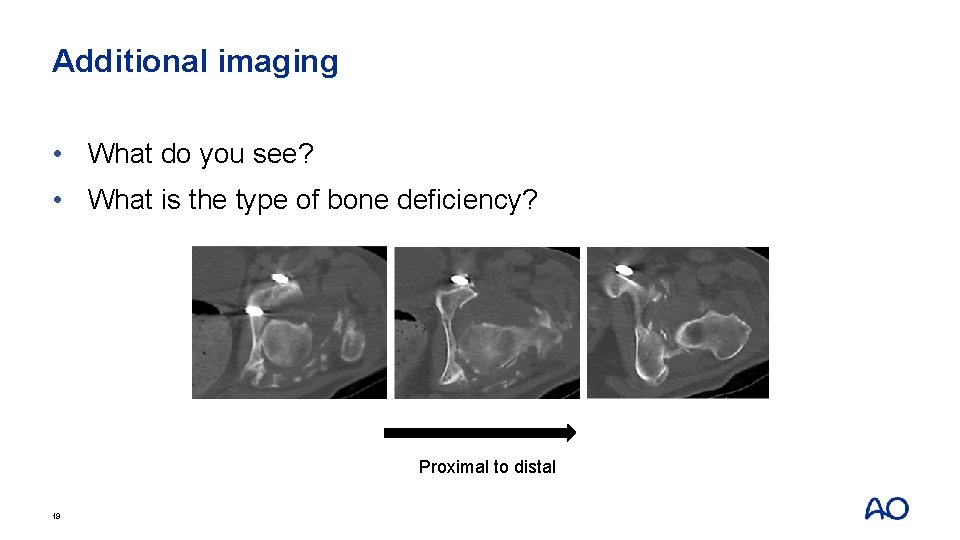
Additional imaging • What do you see? • What is the type of bone deficiency? Proximal to distal 19
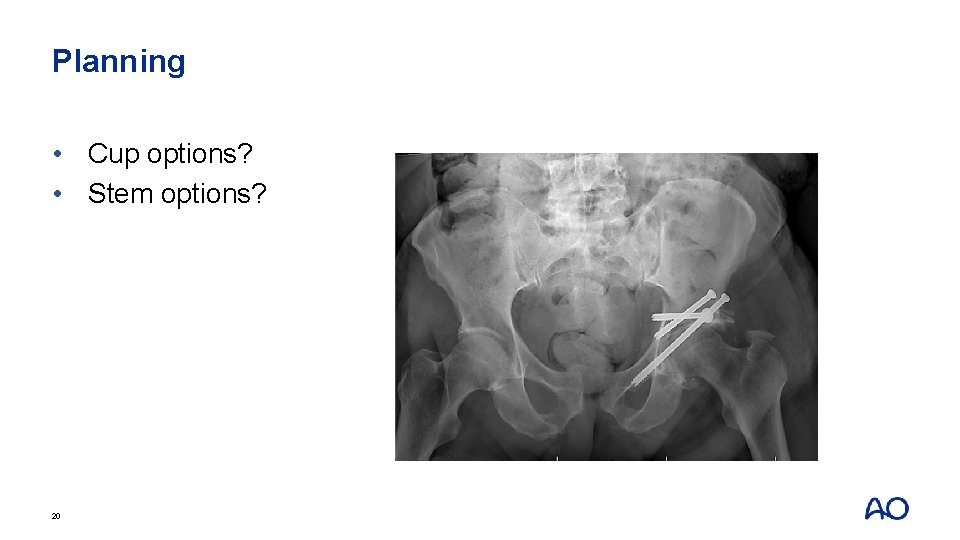
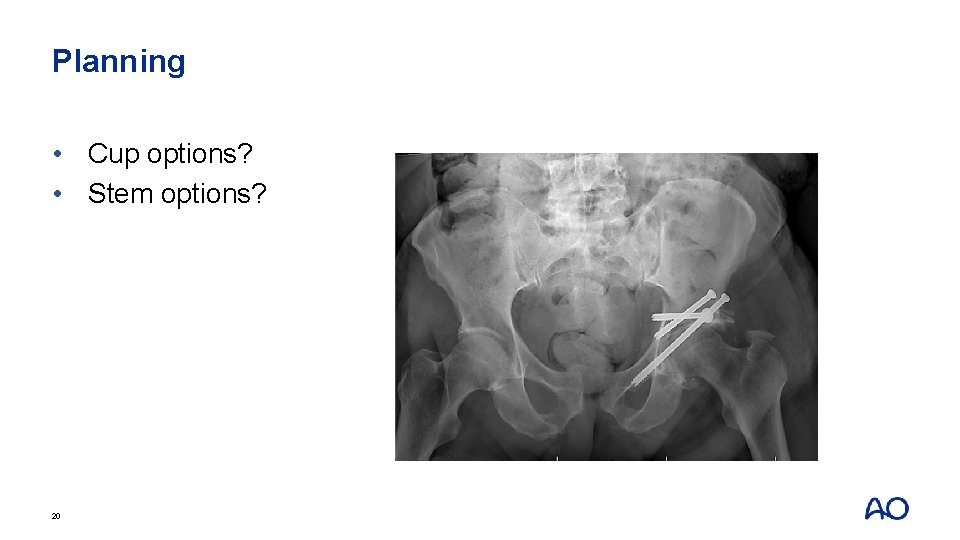
Planning • Cup options? • Stem options? 20
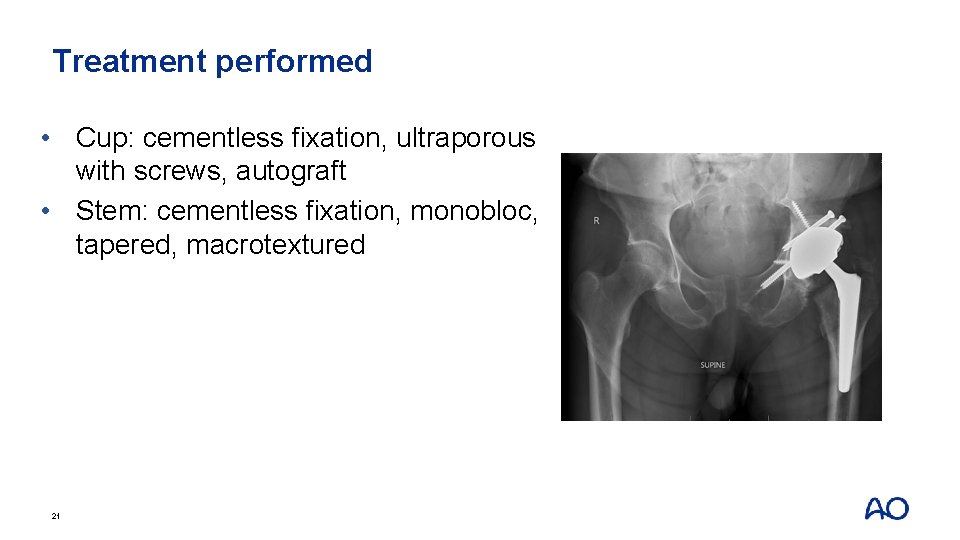
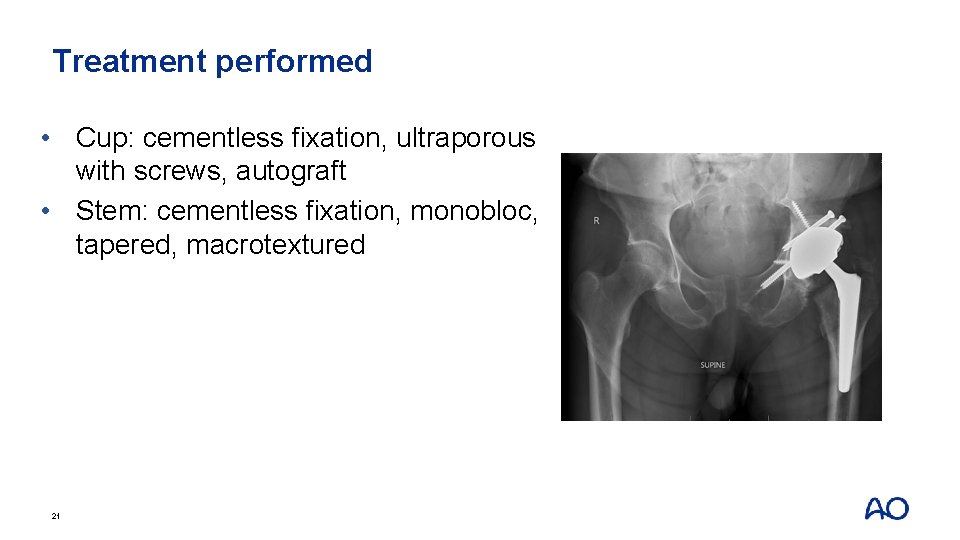
Treatment performed • Cup: cementless fixation, ultraporous with screws, autograft • Stem: cementless fixation, monobloc, tapered, macrotextured 21
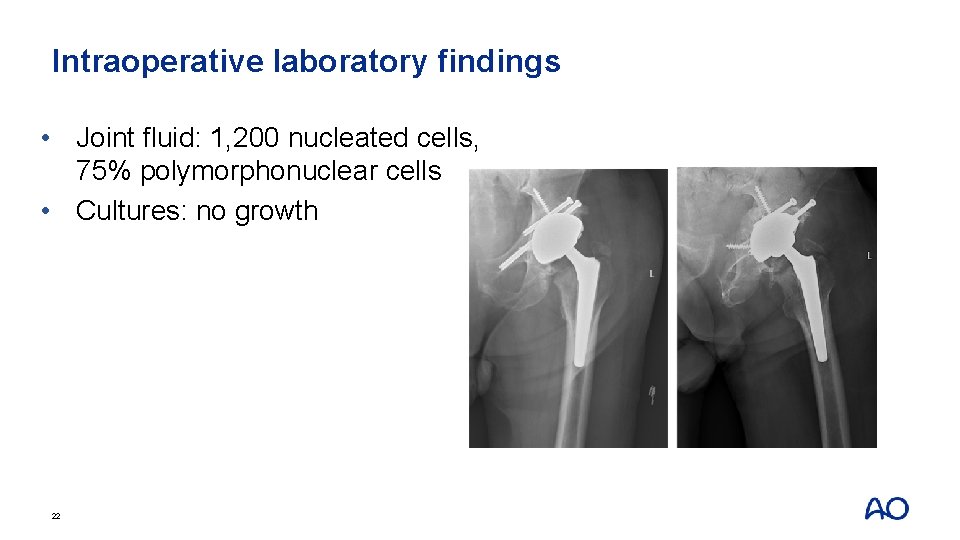
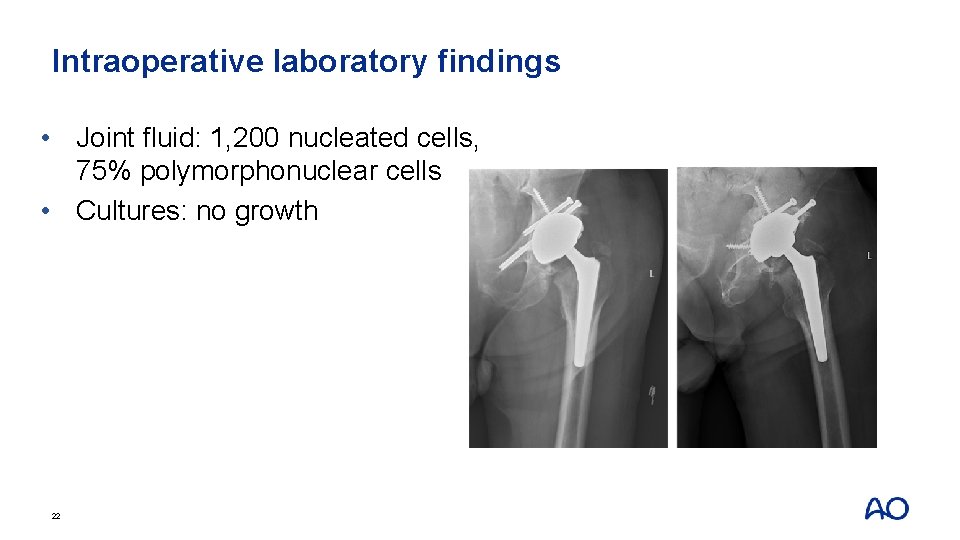
Intraoperative laboratory findings • Joint fluid: 1, 200 nucleated cells, 75% polymorphonuclear cells • Cultures: no growth 22
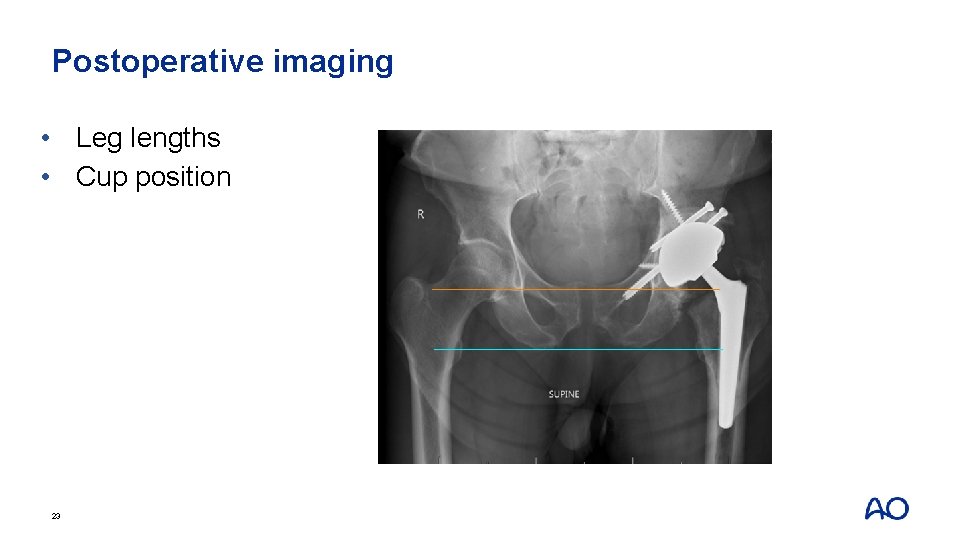
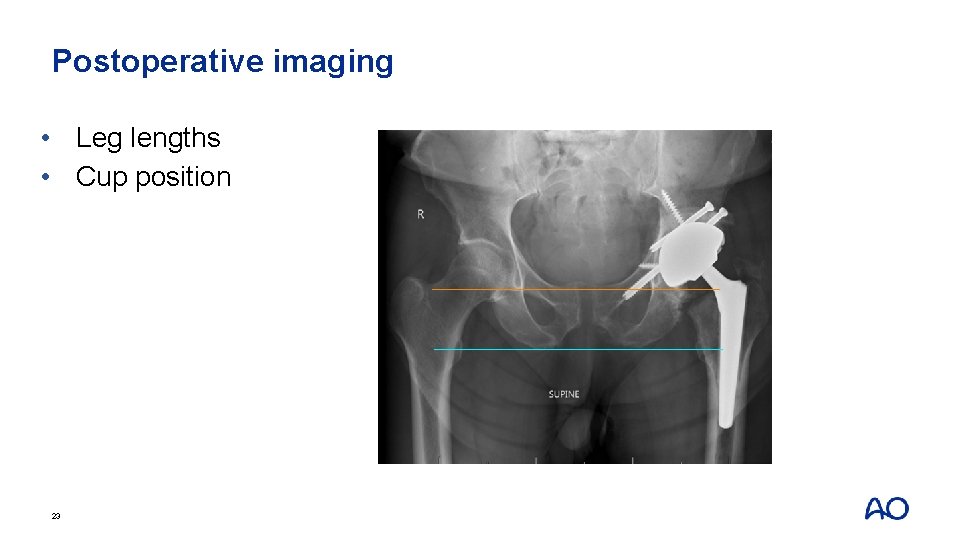
Postoperative imaging • Leg lengths • Cup position 23
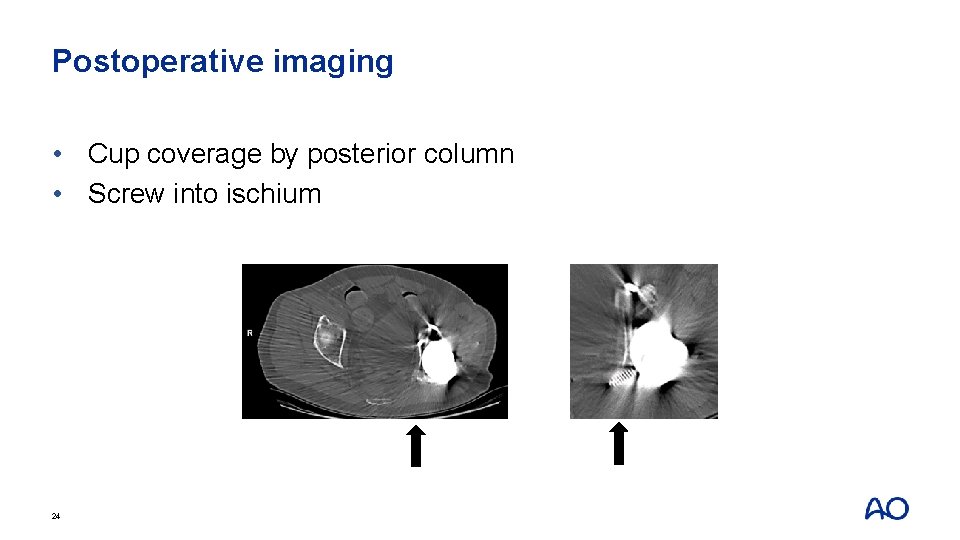
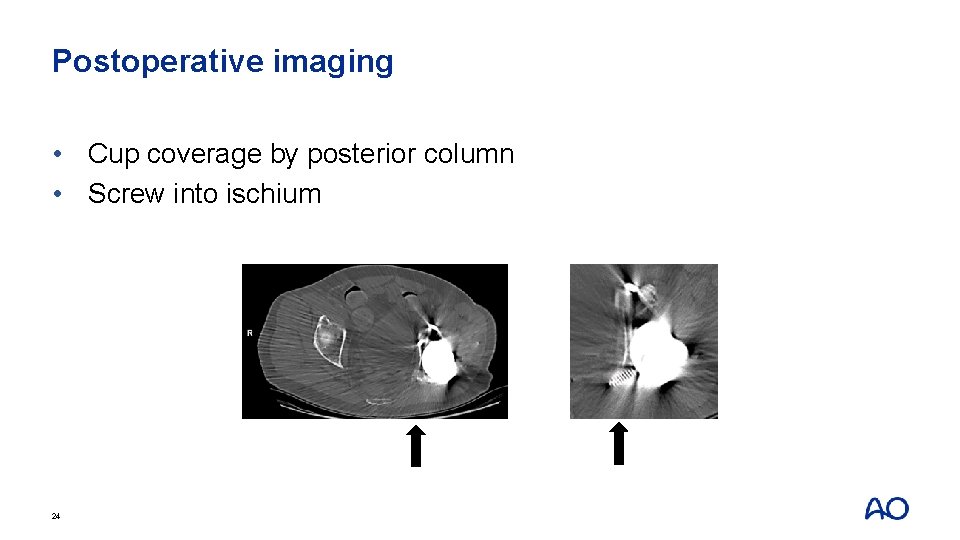
Postoperative imaging • Cup coverage by posterior column • Screw into ischium 24
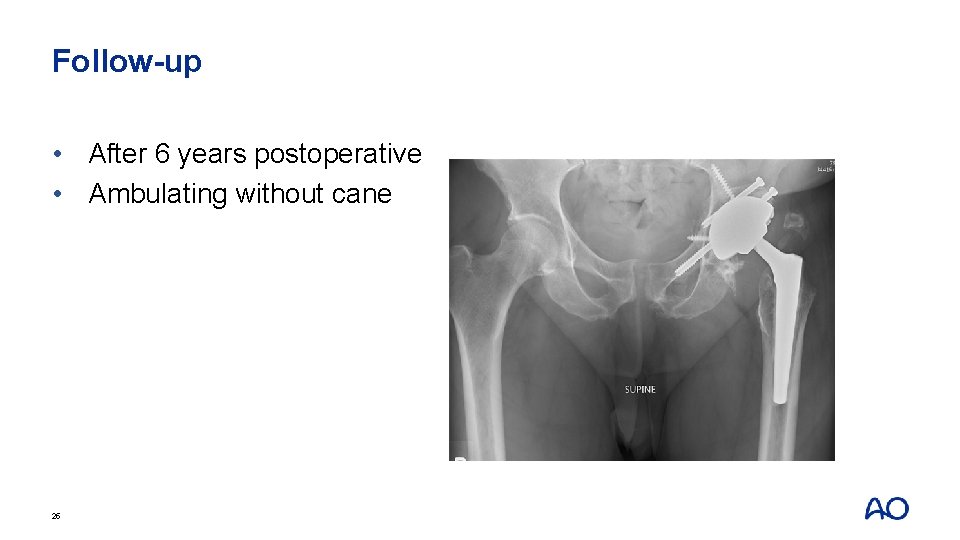
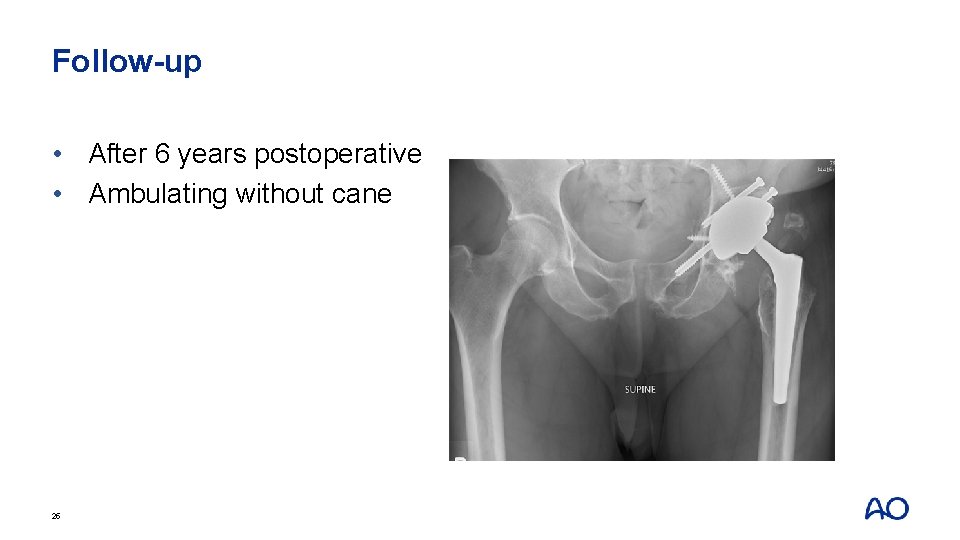
Follow-up • After 6 years postoperative • Ambulating without cane 25
Take-home messages Conversion THA from previous acetabular fracture: • Retained hardware • Possible infection • Acetabular bone deficiency • Prophylaxis against heterotopic ossification 26

Case 3 27
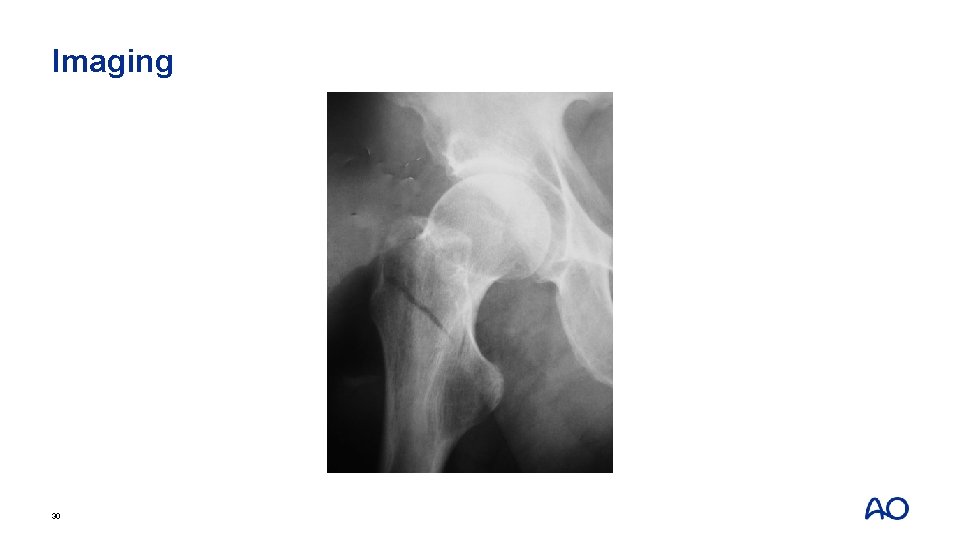
Case history • A 74 -year-old man • Fell from a height of 10 meters • Community ambulator • Lives alone 29
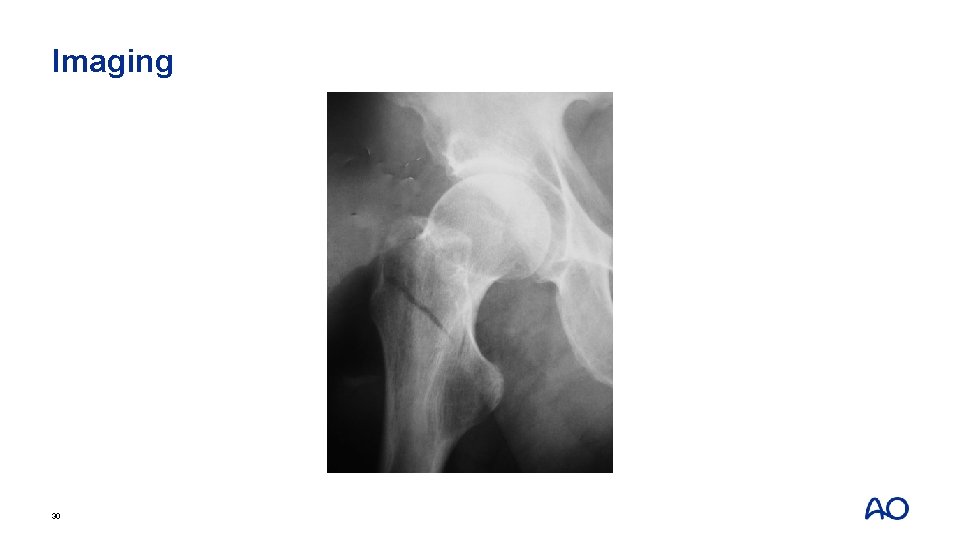
Imaging 30

Initial treatment performed 31

Following initial surgery. . . Fell again at home while going to the bathroom 3 weeks postoperative 32
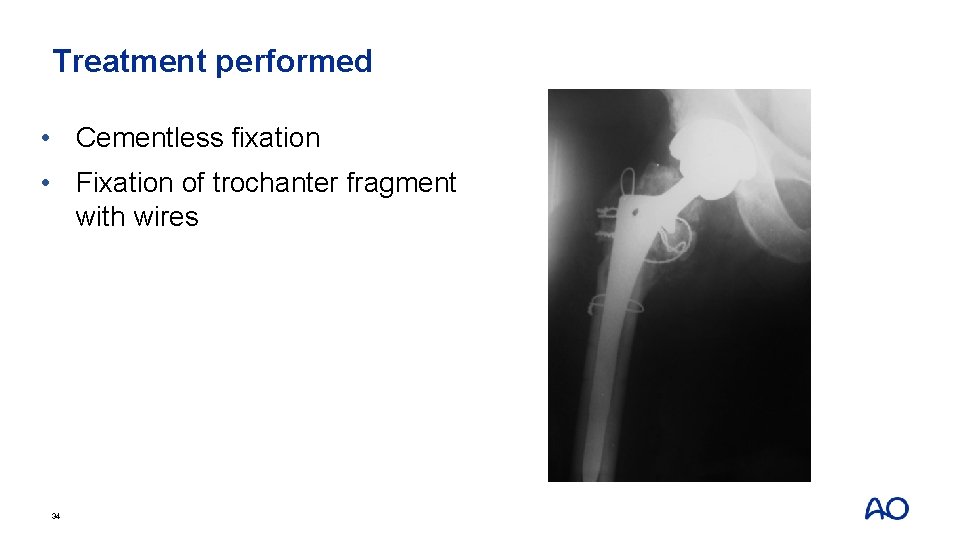
Planning • What treatment options would you consider now? • What implant designs would you select? 33
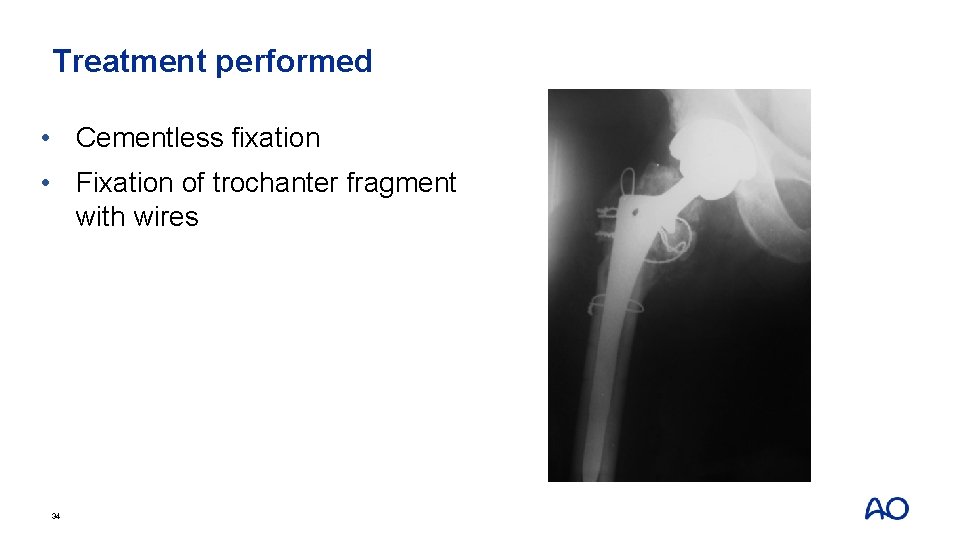
Treatment performed • Cementless fixation • Fixation of trochanter fragment with wires 34
Take-home messages • Removal of retained hardware can create additional fractures • Cementless fixation preferred over cemented to optimize fracture healing • Postoperative weight-bearing restriction may be necessary for trochanter fragment healing 35
Module 3: Complex primary total hip arthroplasty Small group discussion