Reproductive System Reproductive System Male and female system
- Slides: 46
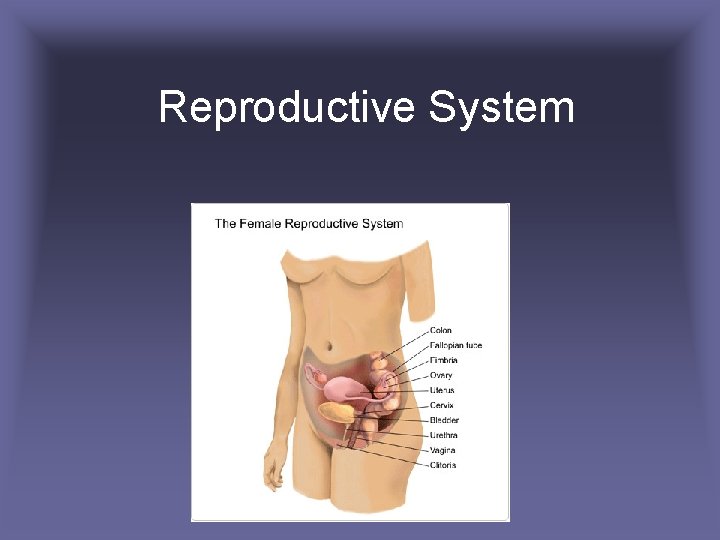
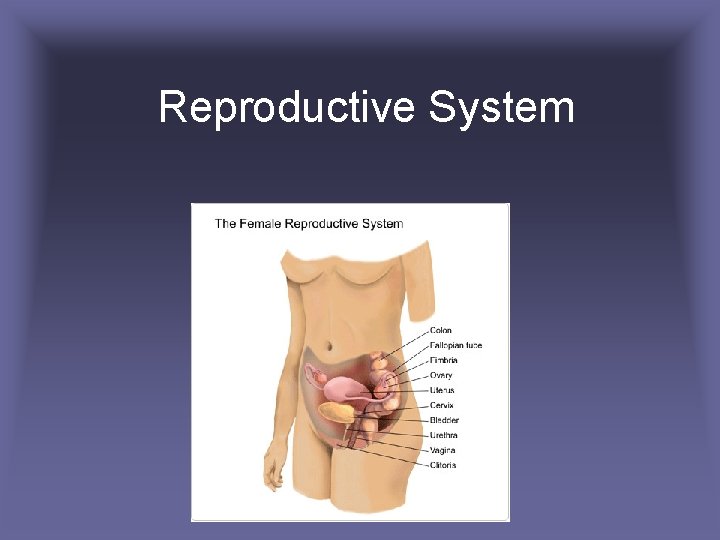
Reproductive System
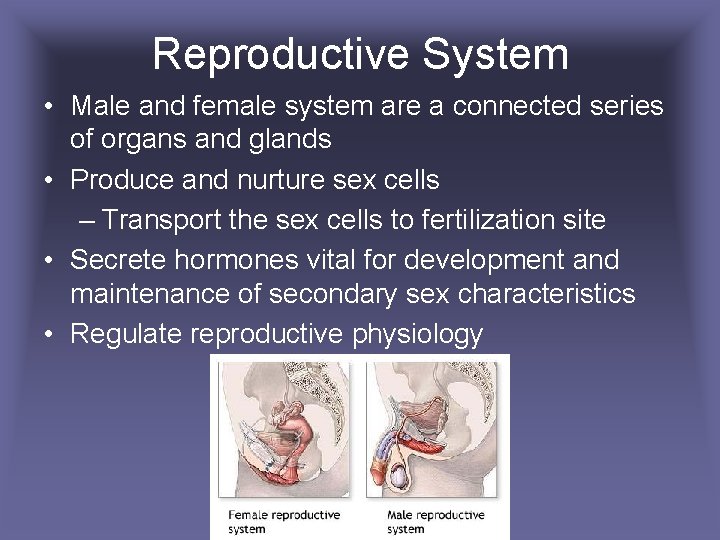
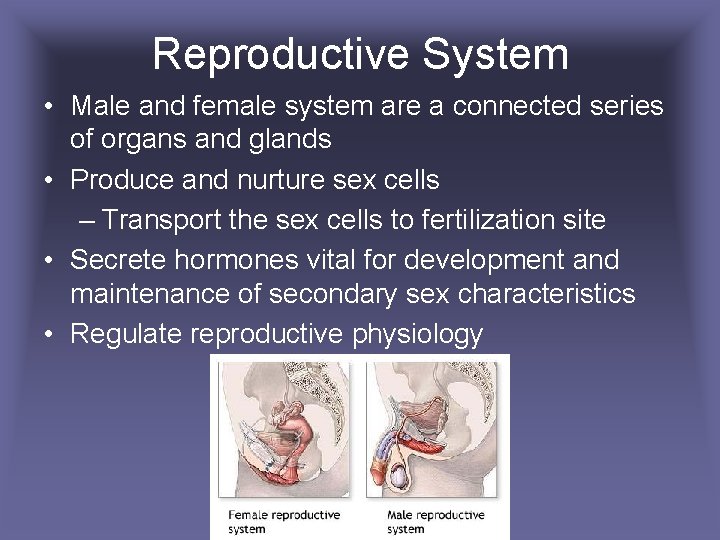
Reproductive System • Male and female system are a connected series of organs and glands • Produce and nurture sex cells – Transport the sex cells to fertilization site • Secrete hormones vital for development and maintenance of secondary sex characteristics • Regulate reproductive physiology
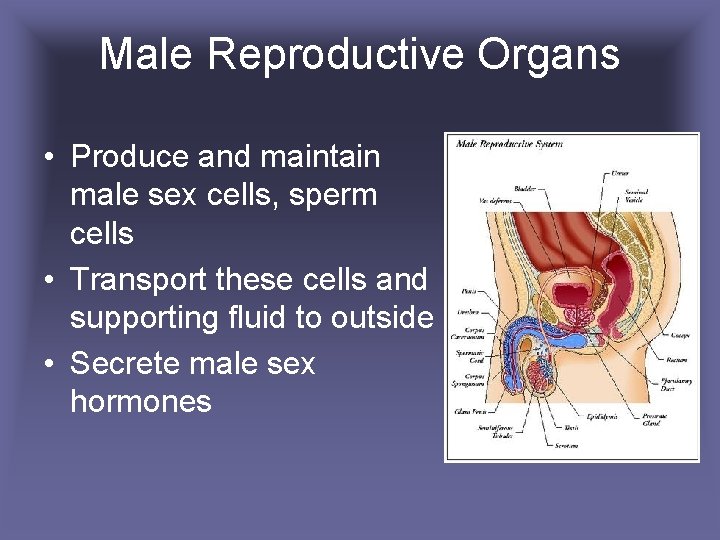
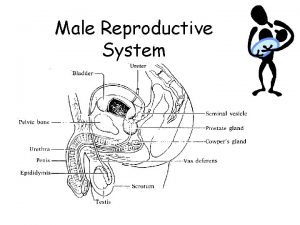
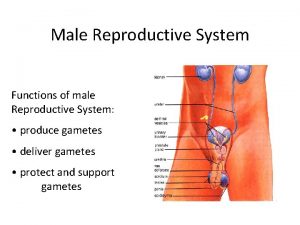
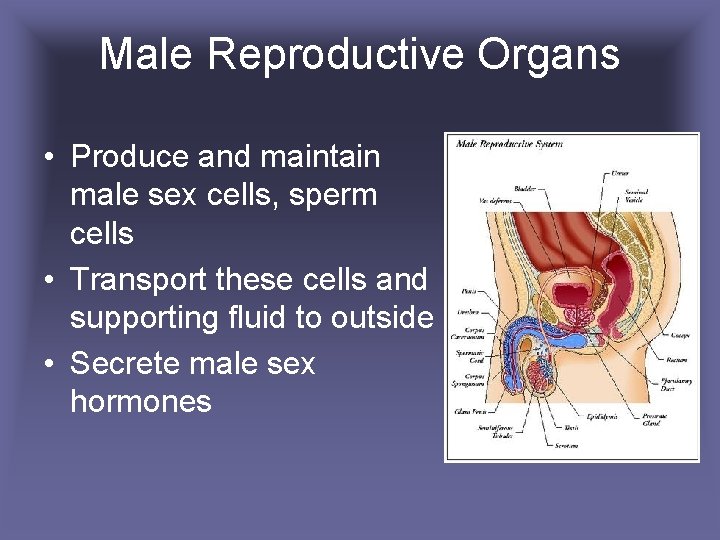
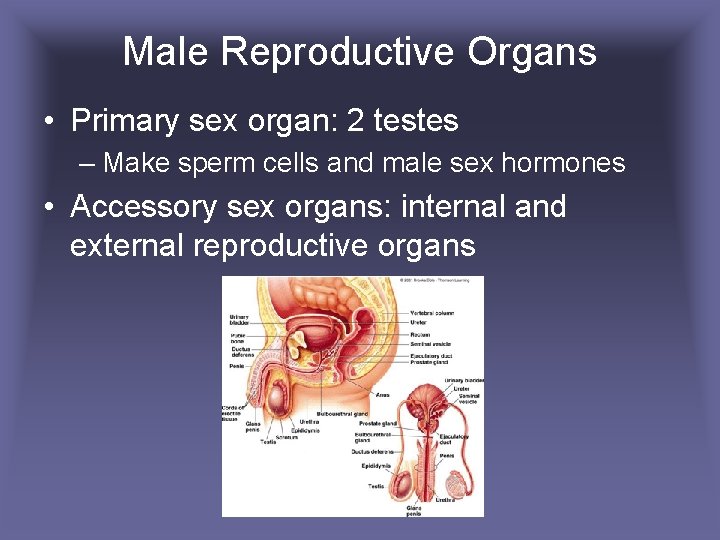
Male Reproductive Organs • Produce and maintain male sex cells, sperm cells • Transport these cells and supporting fluid to outside • Secrete male sex hormones
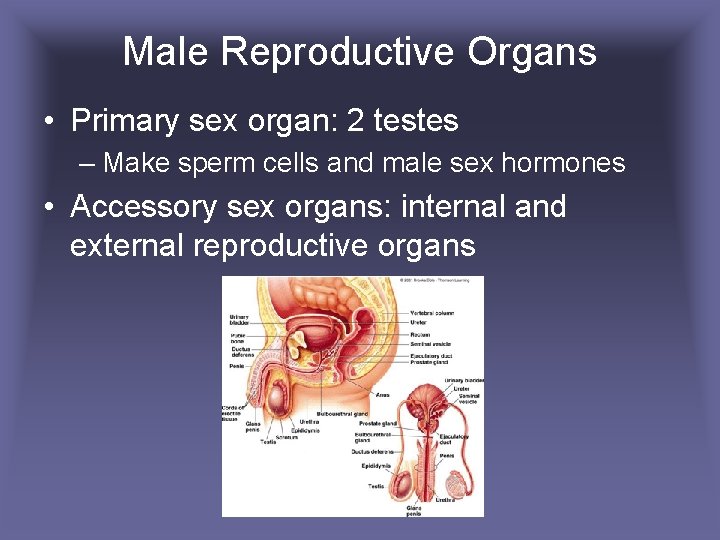
Male Reproductive Organs • Primary sex organ: 2 testes – Make sperm cells and male sex hormones • Accessory sex organs: internal and external reproductive organs
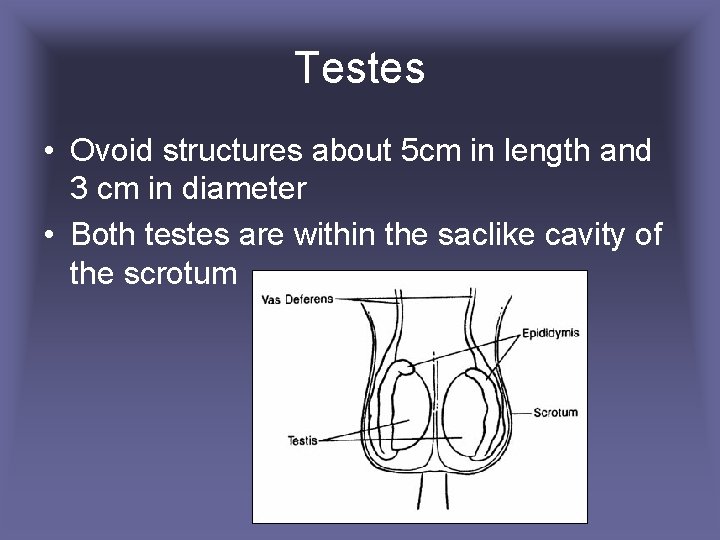
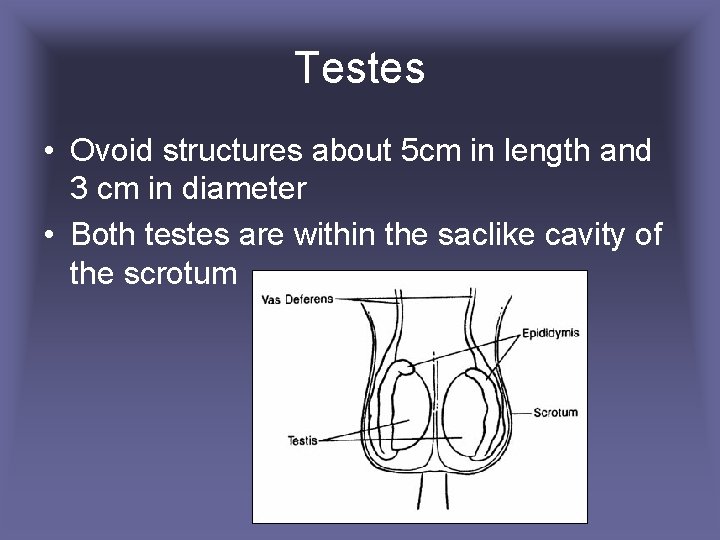
Testes • Ovoid structures about 5 cm in length and 3 cm in diameter • Both testes are within the saclike cavity of the scrotum
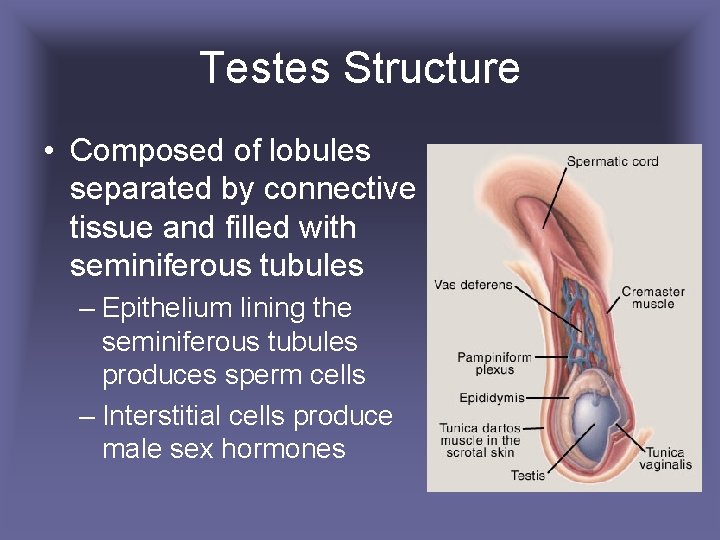
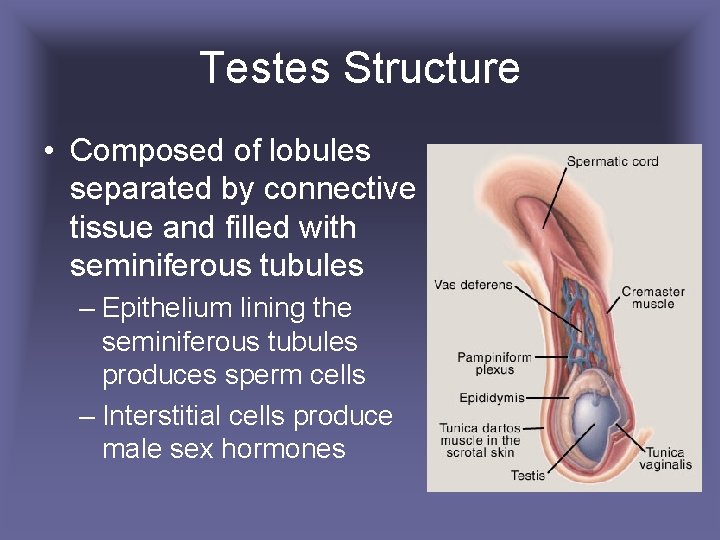
Testes Structure • Composed of lobules separated by connective tissue and filled with seminiferous tubules – Epithelium lining the seminiferous tubules produces sperm cells – Interstitial cells produce male sex hormones
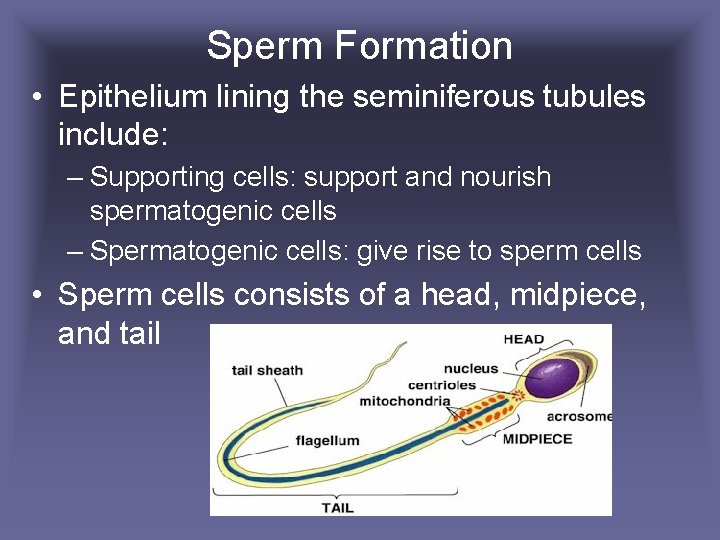
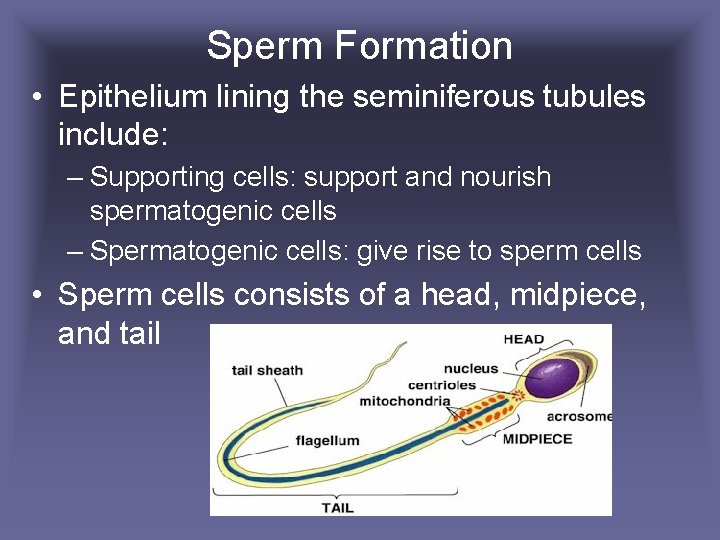
Sperm Formation • Epithelium lining the seminiferous tubules include: – Supporting cells: support and nourish spermatogenic cells – Spermatogenic cells: give rise to sperm cells • Sperm cells consists of a head, midpiece, and tail
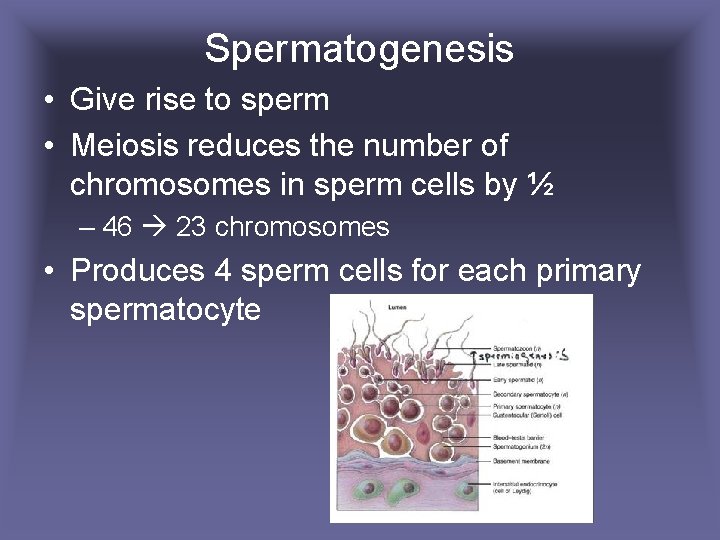
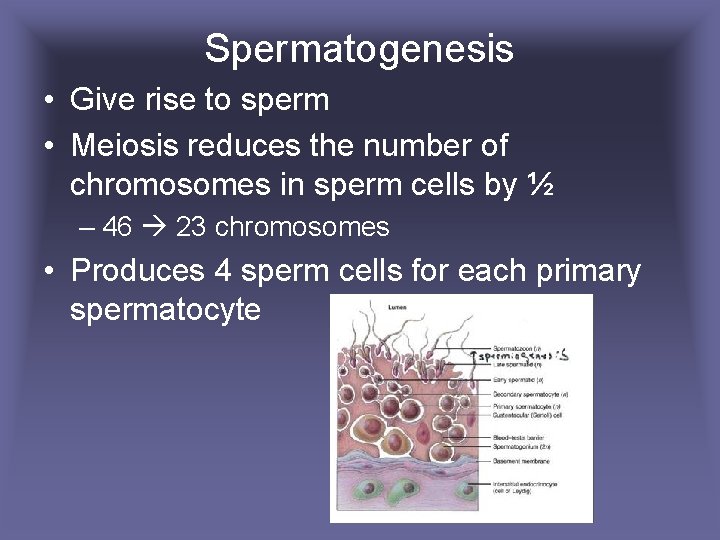
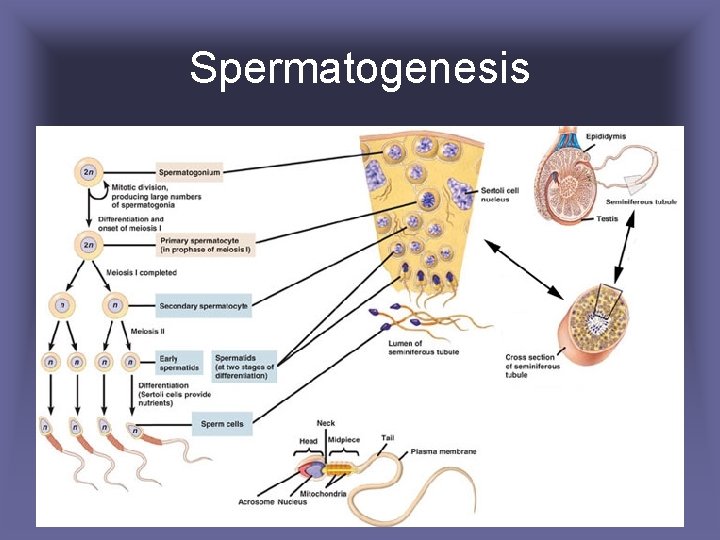
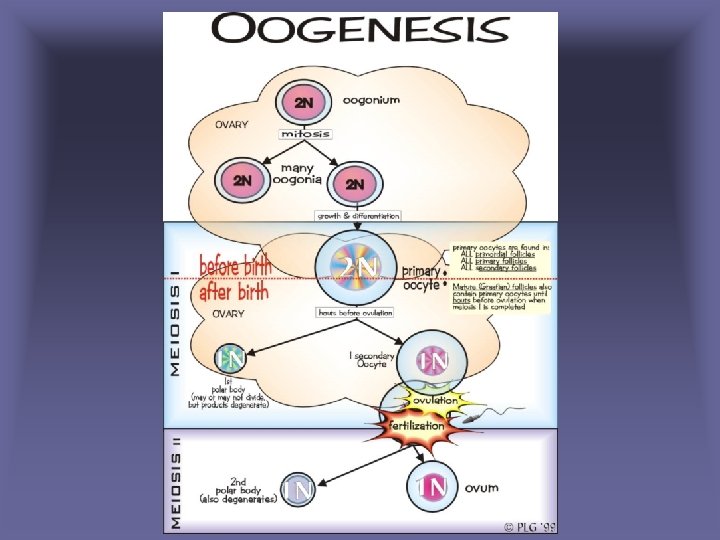
Spermatogenesis • Give rise to sperm • Meiosis reduces the number of chromosomes in sperm cells by ½ – 46 23 chromosomes • Produces 4 sperm cells for each primary spermatocyte
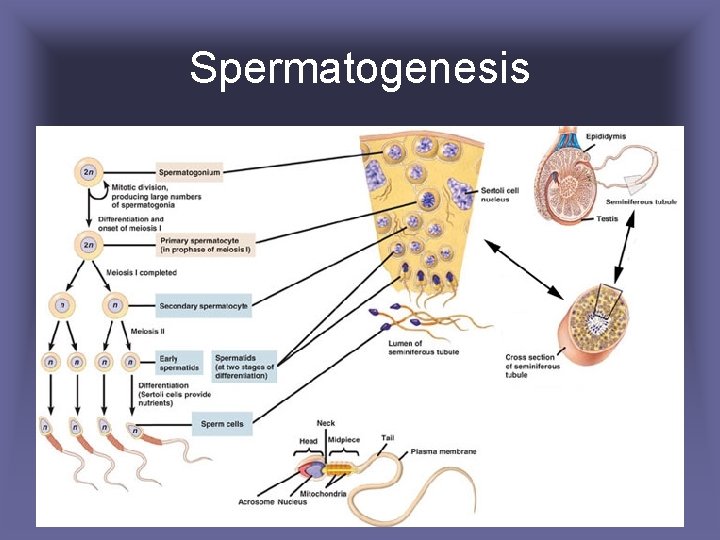
Spermatogenesis
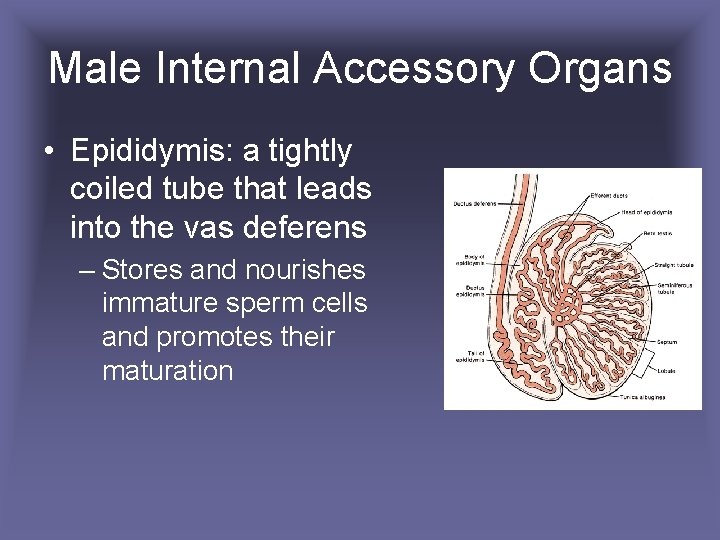
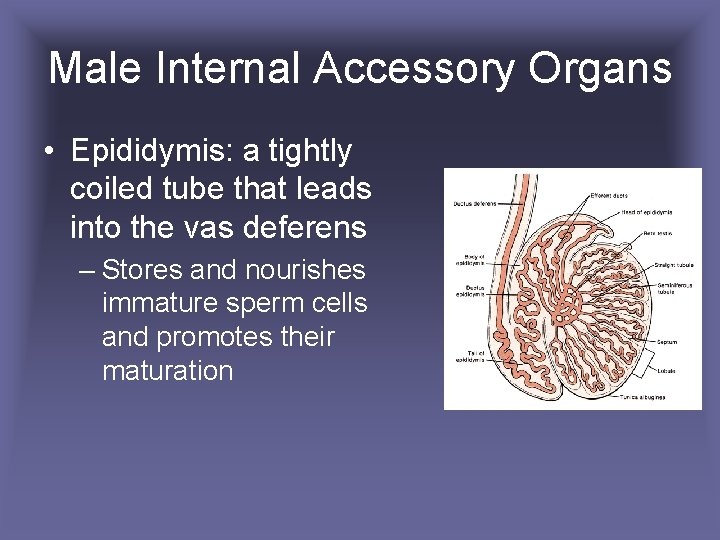
Male Internal Accessory Organs • Epididymis: a tightly coiled tube that leads into the vas deferens – Stores and nourishes immature sperm cells and promotes their maturation
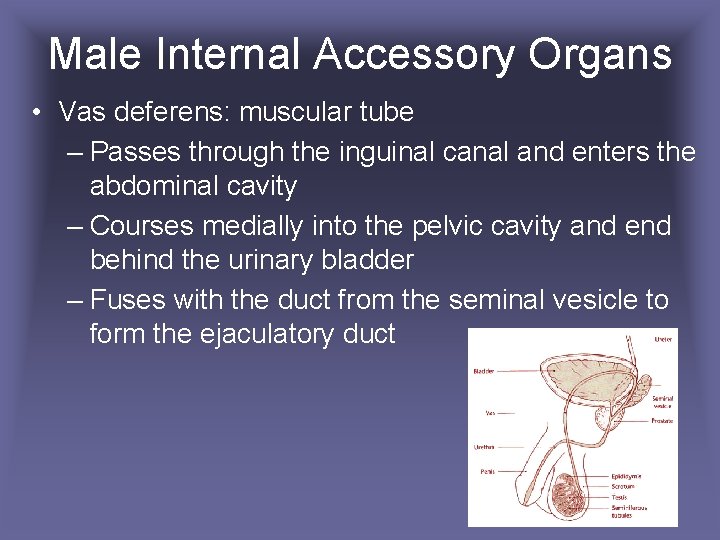
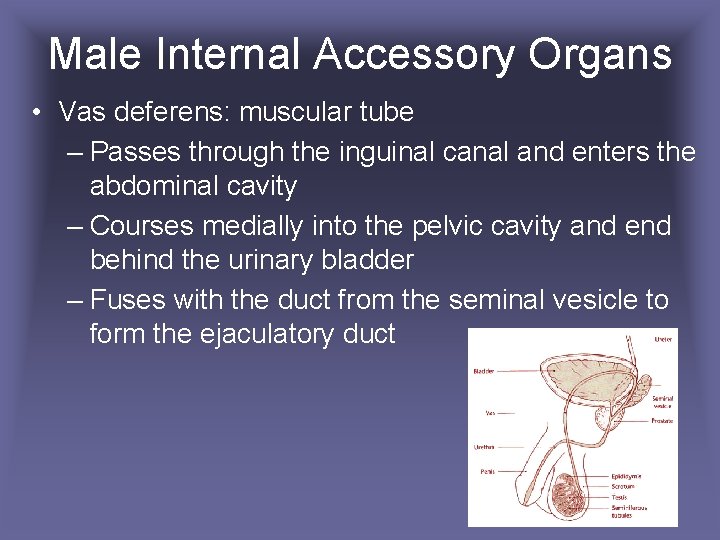
Male Internal Accessory Organs • Vas deferens: muscular tube – Passes through the inguinal canal and enters the abdominal cavity – Courses medially into the pelvic cavity and end behind the urinary bladder – Fuses with the duct from the seminal vesicle to form the ejaculatory duct
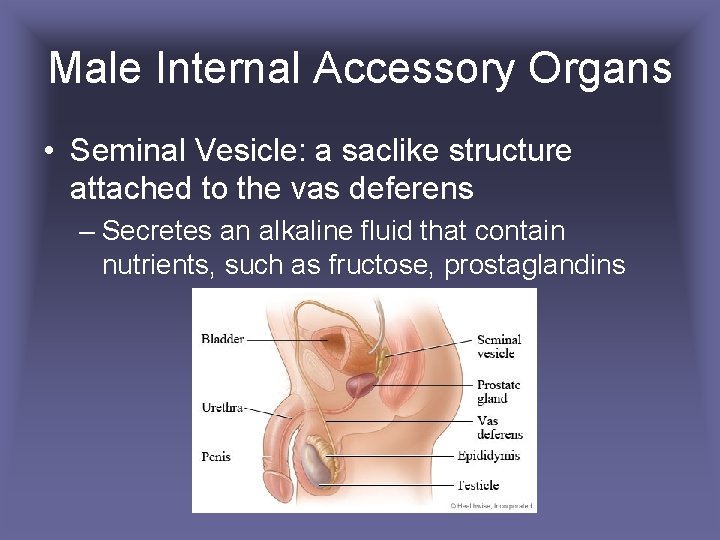
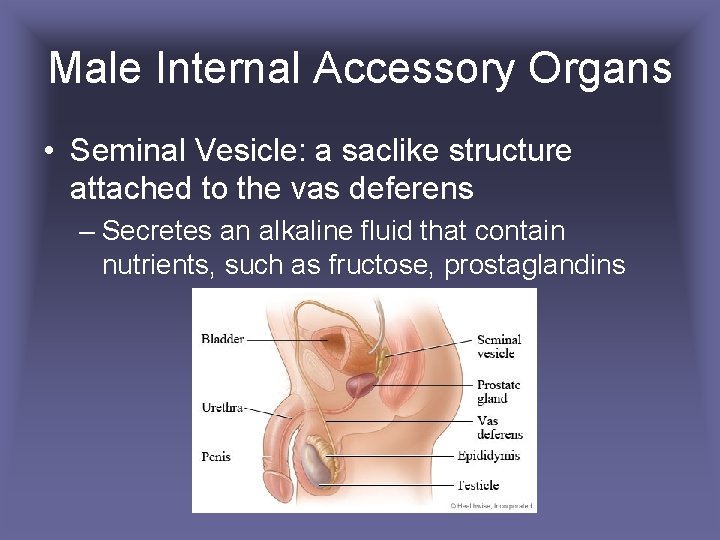
Male Internal Accessory Organs • Seminal Vesicle: a saclike structure attached to the vas deferens – Secretes an alkaline fluid that contain nutrients, such as fructose, prostaglandins
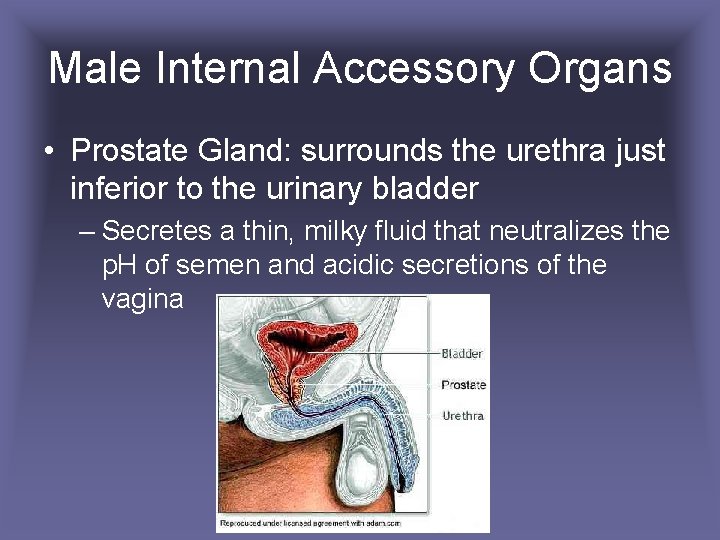
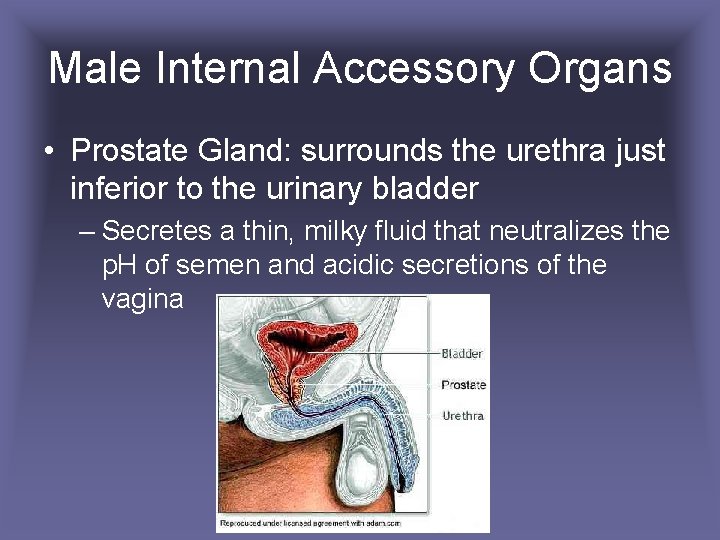
Male Internal Accessory Organs • Prostate Gland: surrounds the urethra just inferior to the urinary bladder – Secretes a thin, milky fluid that neutralizes the p. H of semen and acidic secretions of the vagina
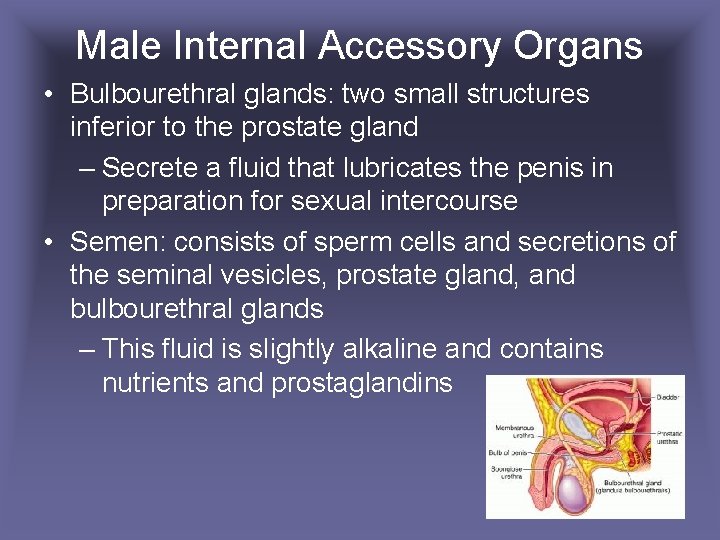
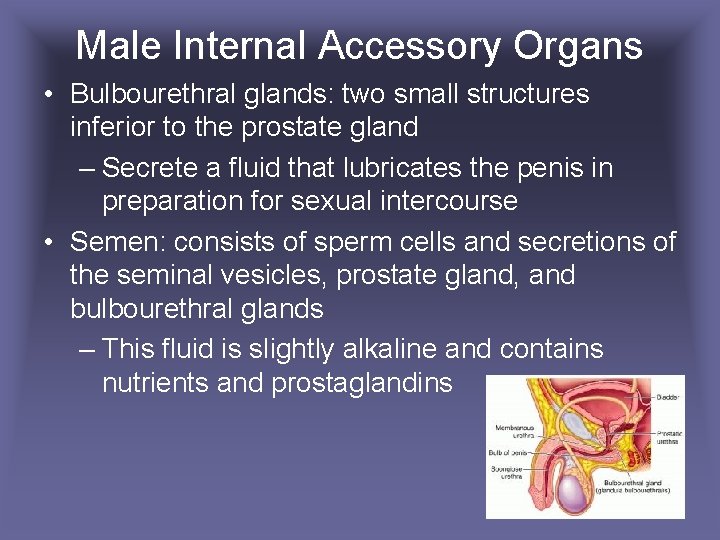
Male Internal Accessory Organs • Bulbourethral glands: two small structures inferior to the prostate gland – Secrete a fluid that lubricates the penis in preparation for sexual intercourse • Semen: consists of sperm cells and secretions of the seminal vesicles, prostate gland, and bulbourethral glands – This fluid is slightly alkaline and contains nutrients and prostaglandins
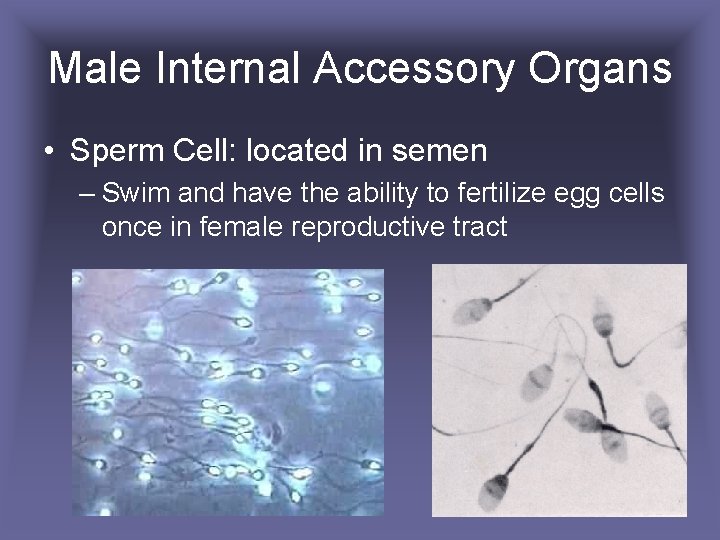
Male Internal Accessory Organs • Sperm Cell: located in semen – Swim and have the ability to fertilize egg cells once in female reproductive tract
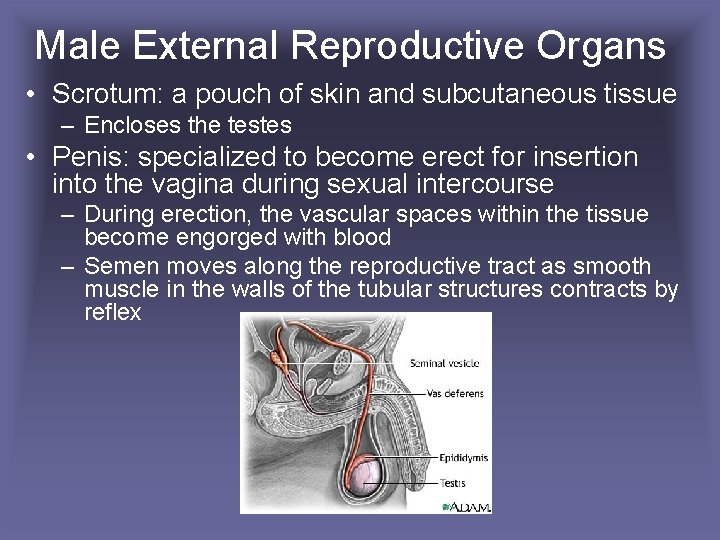
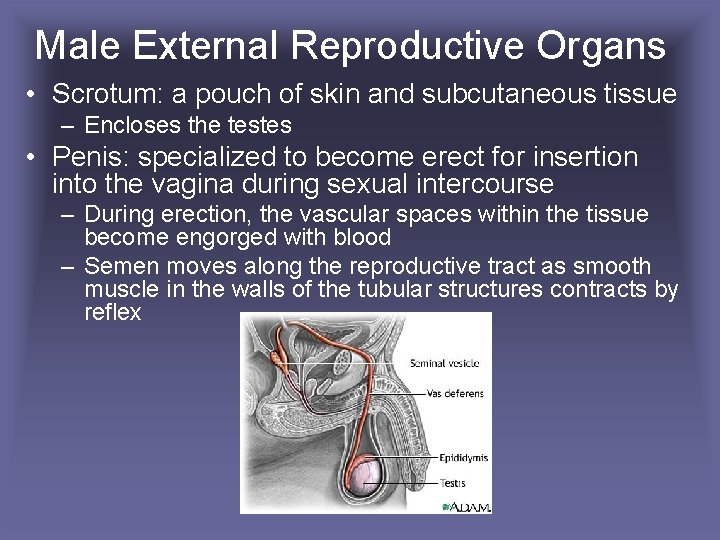
Male External Reproductive Organs • Scrotum: a pouch of skin and subcutaneous tissue – Encloses the testes • Penis: specialized to become erect for insertion into the vagina during sexual intercourse – During erection, the vascular spaces within the tissue become engorged with blood – Semen moves along the reproductive tract as smooth muscle in the walls of the tubular structures contracts by reflex
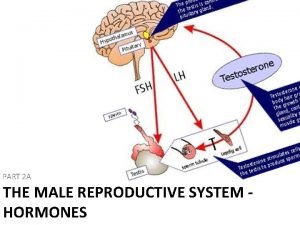
Male Hormones • Hypothalamic and Pituitary Hormones – Male body remains reproductively immature until the hypothalamus releases gonadotropin-releasing hormone (Gn. RH) – Stimulates the anterior pituitary gland to release gonadotropin – Follicle-stimulating hormone (FSH) stimulates spermatogenesis – Luteinizing hormone (LH) stimulates interstitial cells to produce male sex hormones
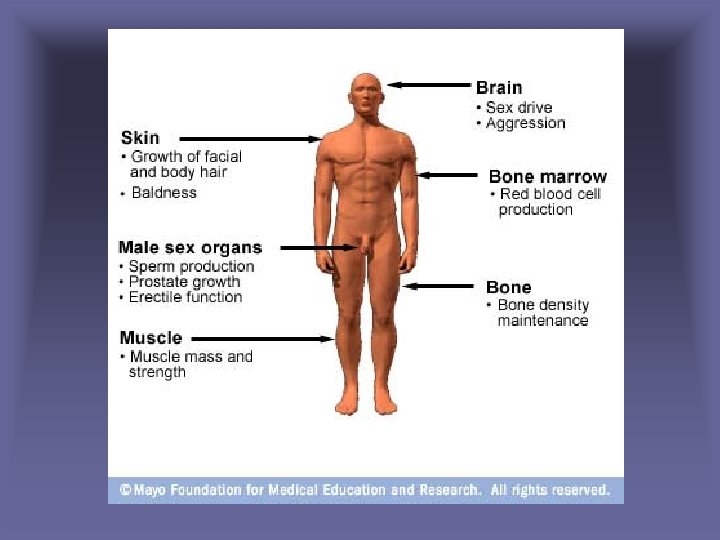
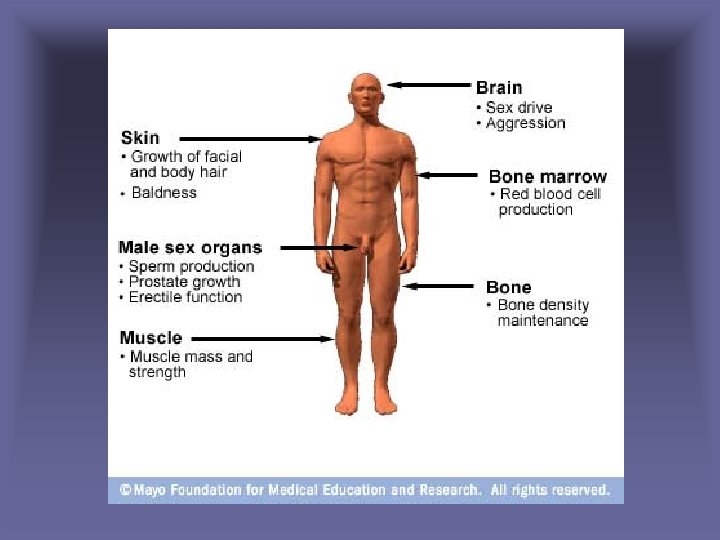
Male Sex Hormones • Androgens – Production increases rapidly at puberty – Testosterone: most important • Stimulates development of male reproductive organs • Male sexual characteristics
Regulation of Male Sex Hormones • A negative feedback mechanism regulates testosterone concentration – Rising testosterone concentration inhibits the hypothalamus and reduces the anterior pituitary’s secretion of gonadotropins – As testosterone concentrations falls, the hypothalamus signals the anterior pituitary to secrete gonadotropins – Testosterone concentrations remain stable from day to day
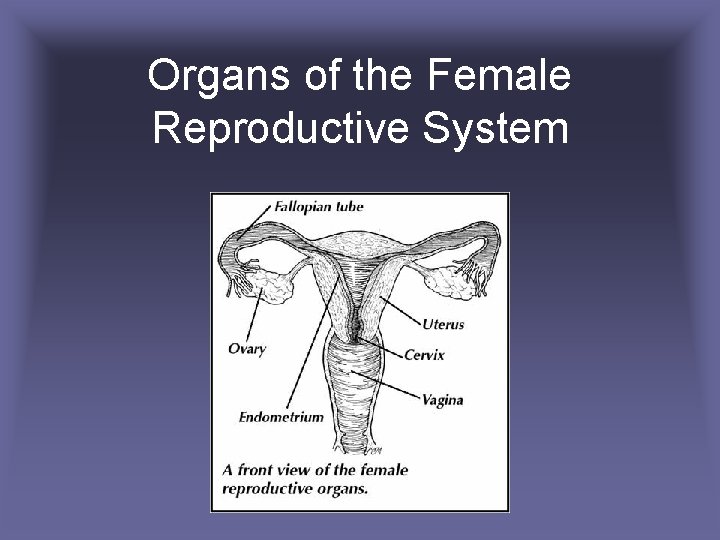
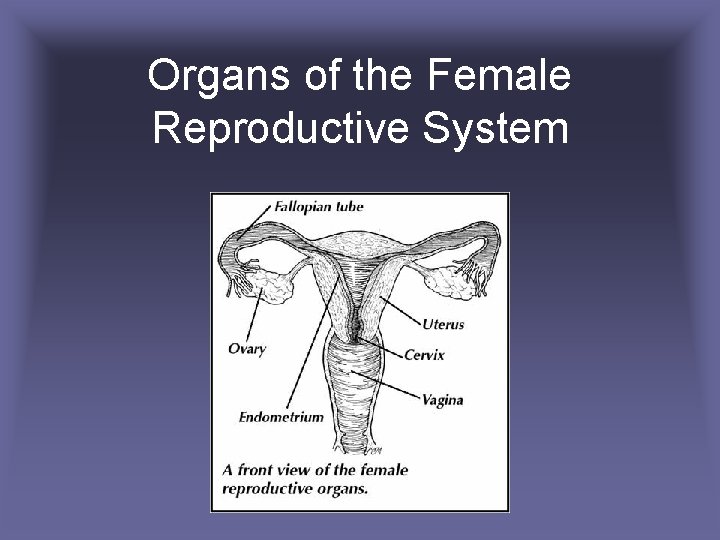
Organs of the Female Reproductive System
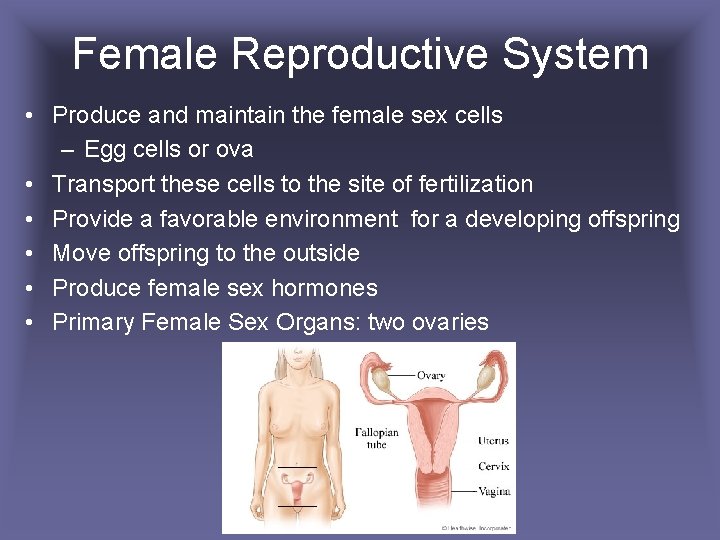
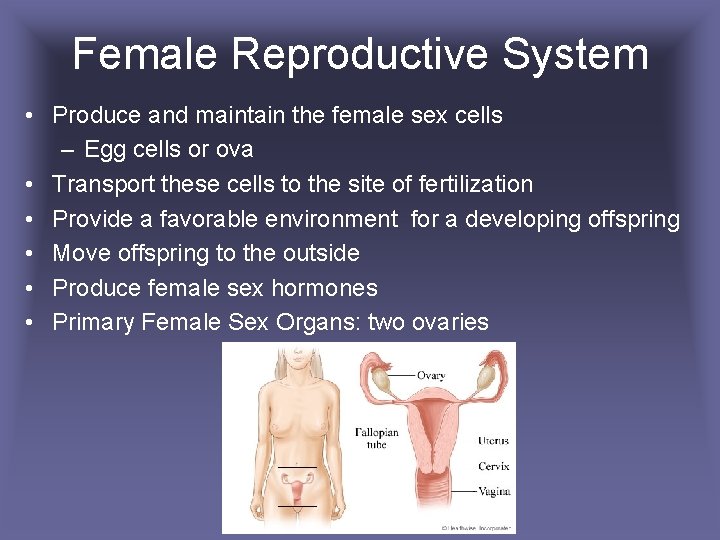
Female Reproductive System • Produce and maintain the female sex cells – Egg cells or ova • Transport these cells to the site of fertilization • Provide a favorable environment for a developing offspring • Move offspring to the outside • Produce female sex hormones • Primary Female Sex Organs: two ovaries
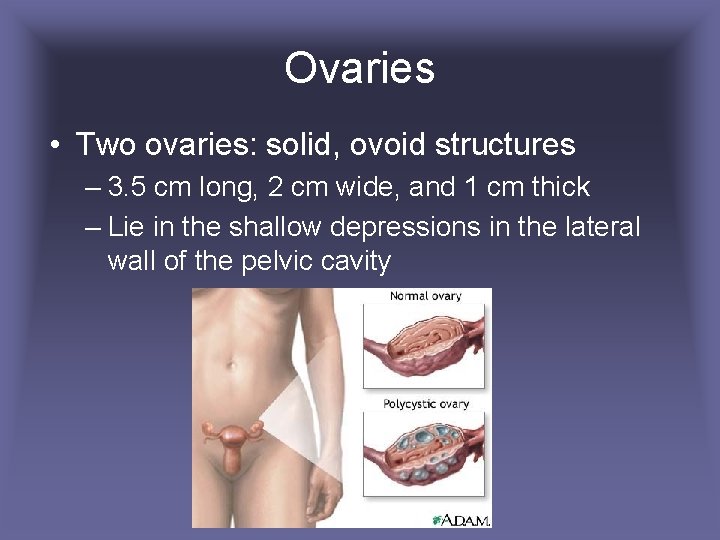
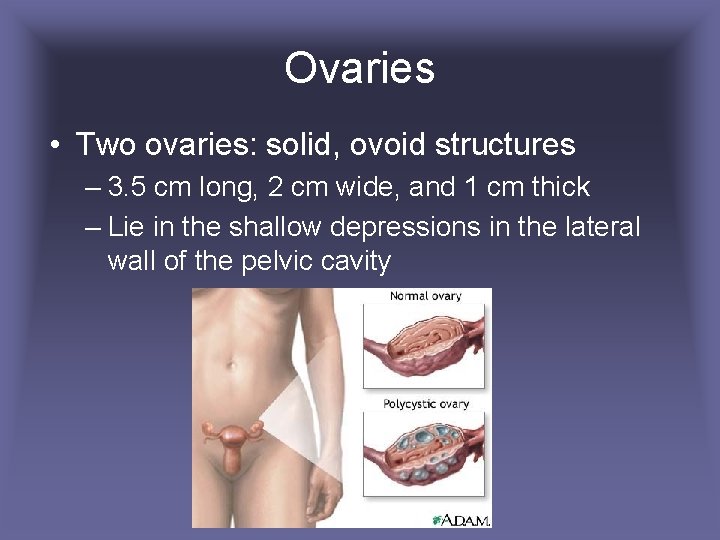
Ovaries • Two ovaries: solid, ovoid structures – 3. 5 cm long, 2 cm wide, and 1 cm thick – Lie in the shallow depressions in the lateral wall of the pelvic cavity
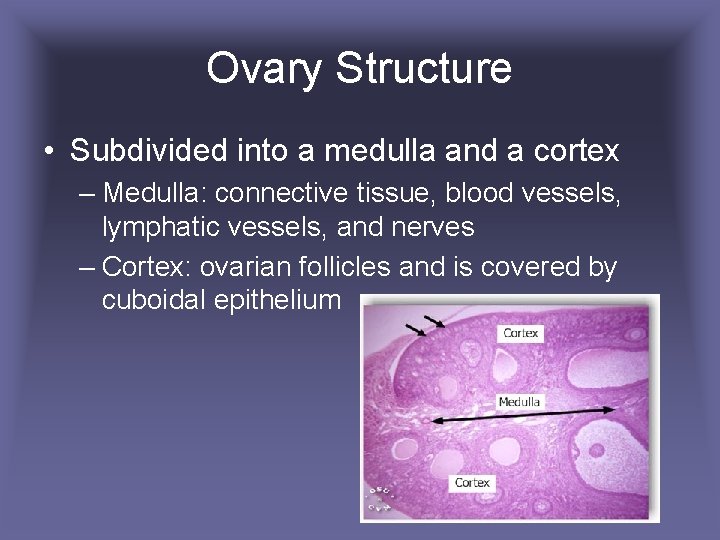
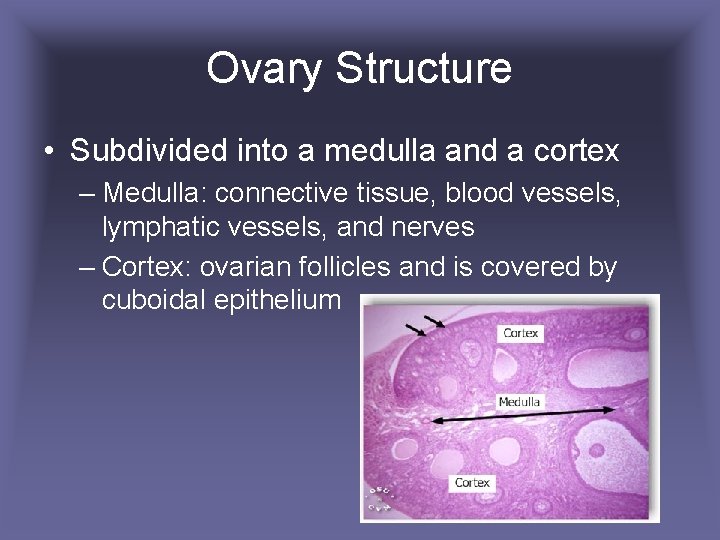
Ovary Structure • Subdivided into a medulla and a cortex – Medulla: connective tissue, blood vessels, lymphatic vessels, and nerves – Cortex: ovarian follicles and is covered by cuboidal epithelium
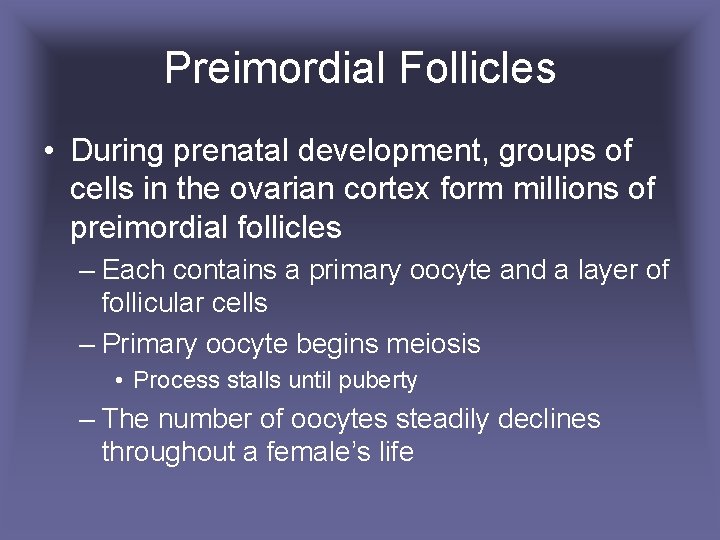
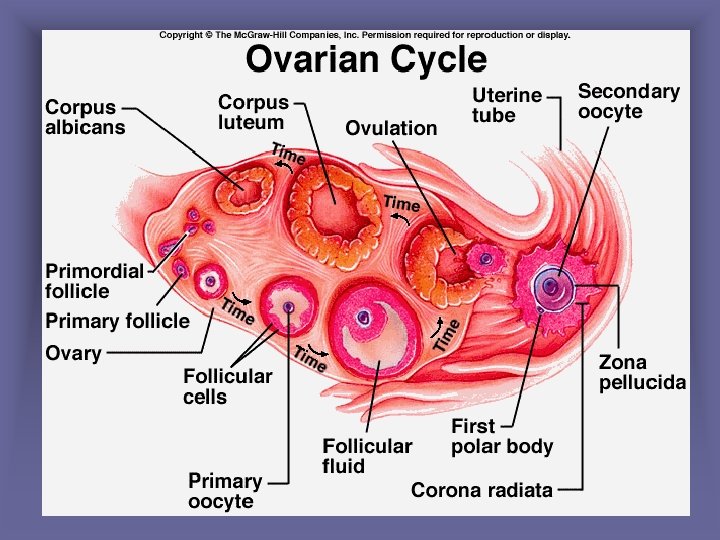
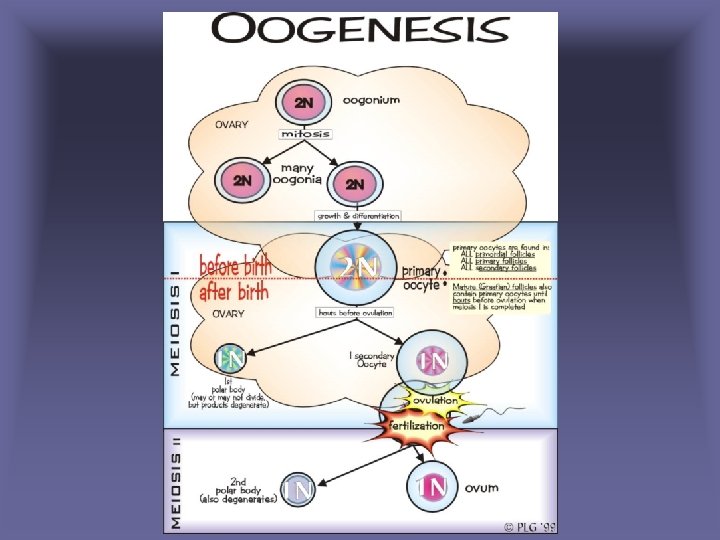
Preimordial Follicles • During prenatal development, groups of cells in the ovarian cortex form millions of preimordial follicles – Each contains a primary oocyte and a layer of follicular cells – Primary oocyte begins meiosis • Process stalls until puberty – The number of oocytes steadily declines throughout a female’s life
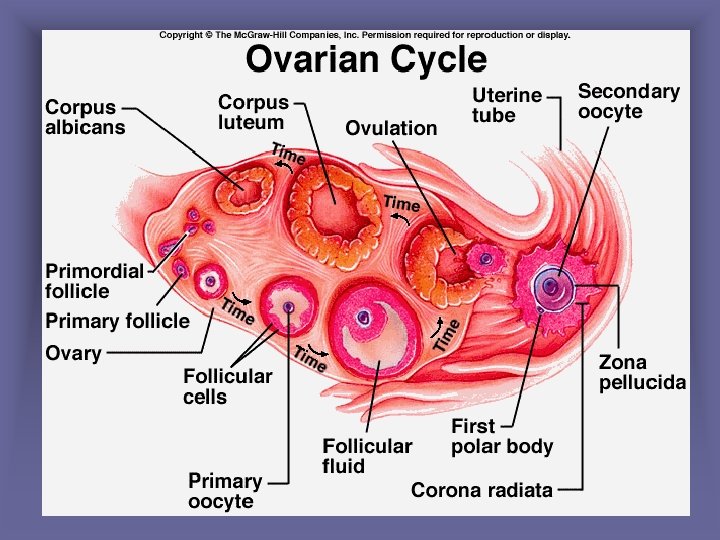
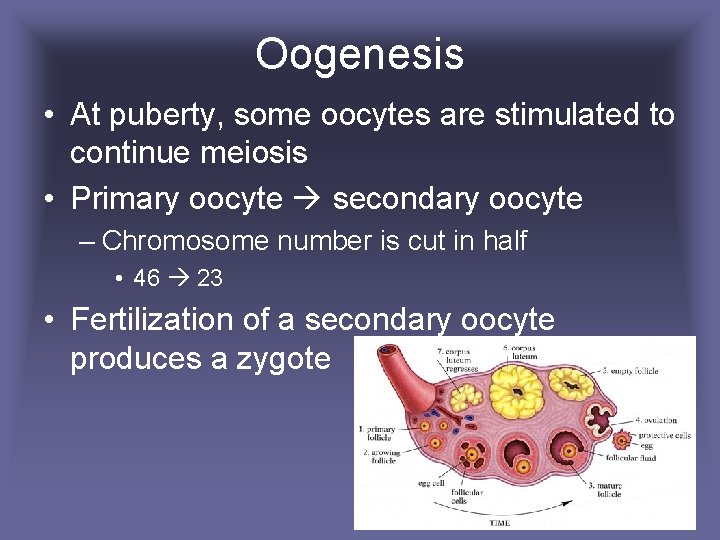
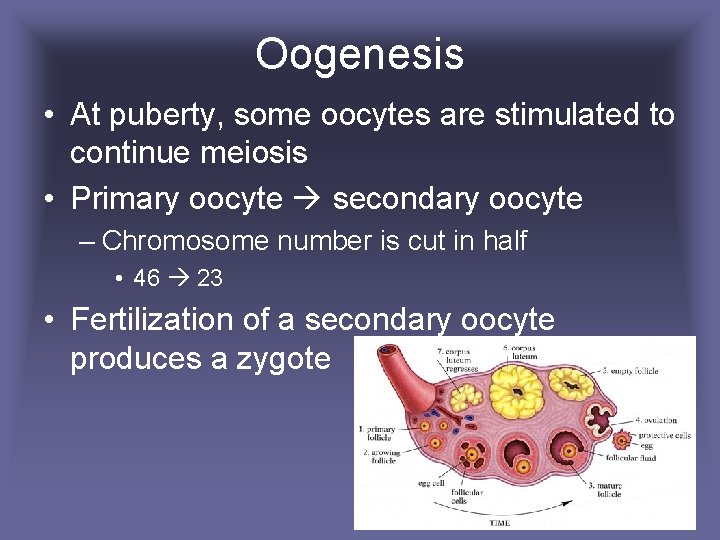
Oogenesis • At puberty, some oocytes are stimulated to continue meiosis • Primary oocyte secondary oocyte – Chromosome number is cut in half • 46 23 • Fertilization of a secondary oocyte produces a zygote
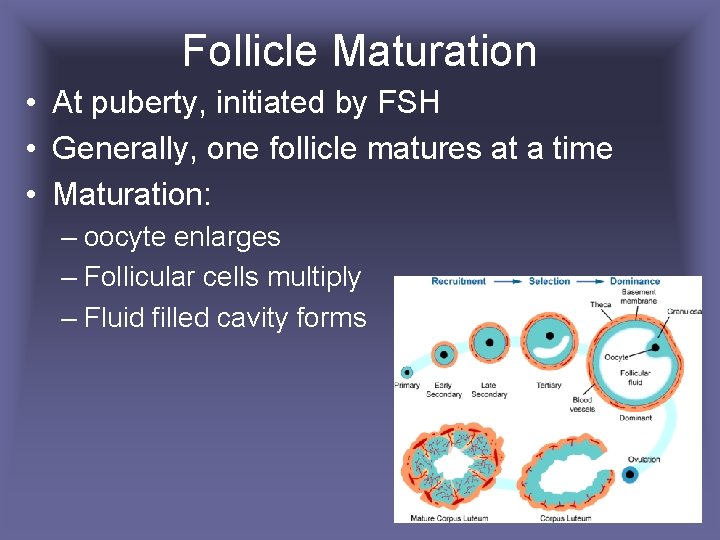
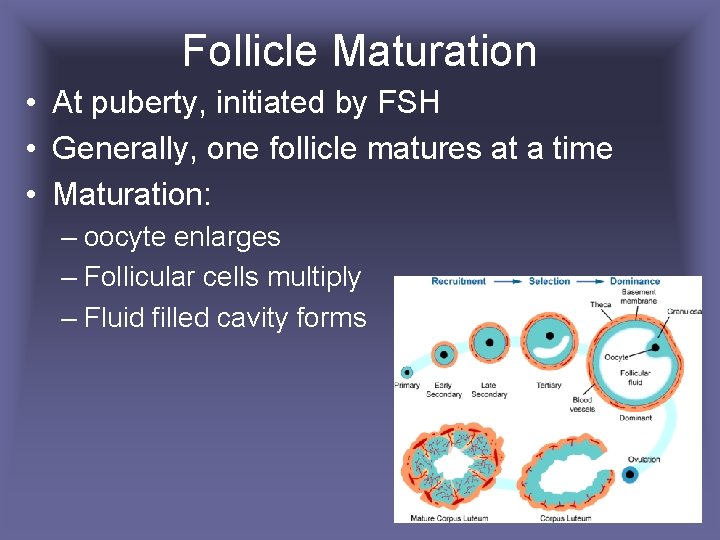
Follicle Maturation • At puberty, initiated by FSH • Generally, one follicle matures at a time • Maturation: – oocyte enlarges – Follicular cells multiply – Fluid filled cavity forms
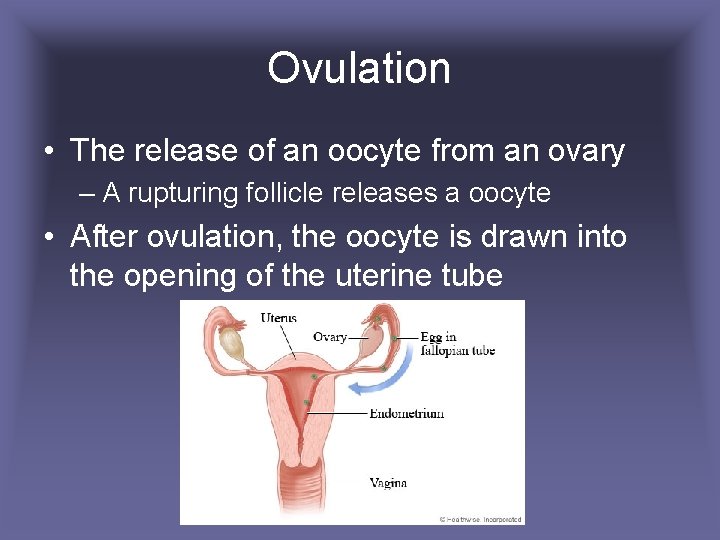
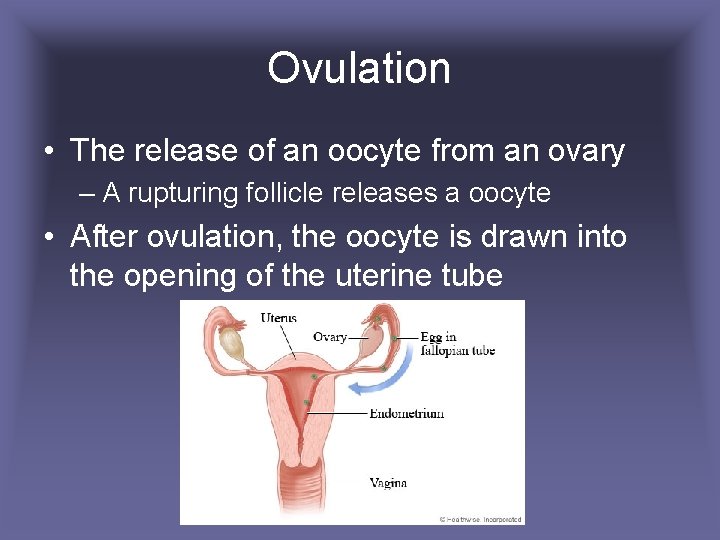
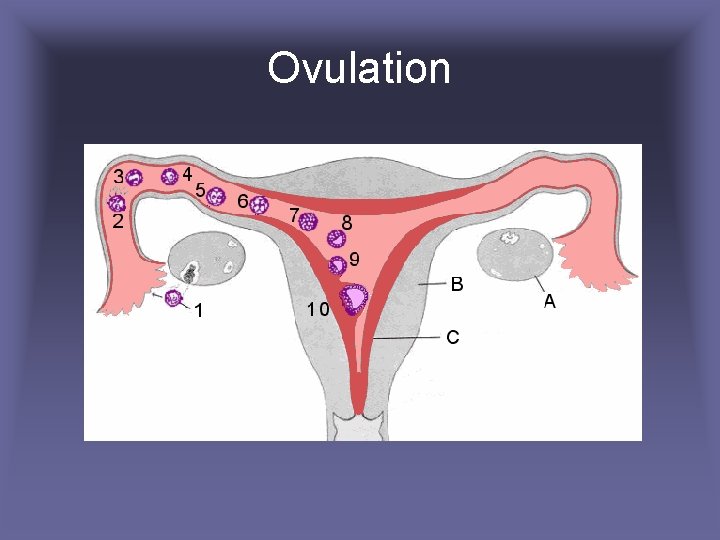
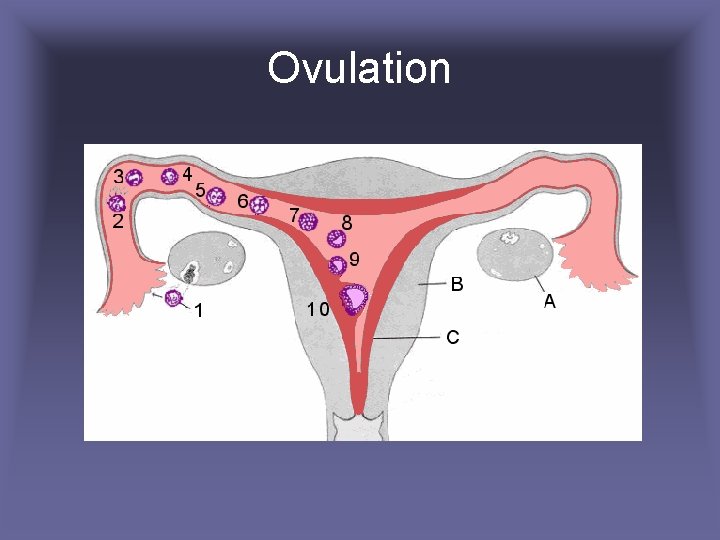
Ovulation • The release of an oocyte from an ovary – A rupturing follicle releases a oocyte • After ovulation, the oocyte is drawn into the opening of the uterine tube
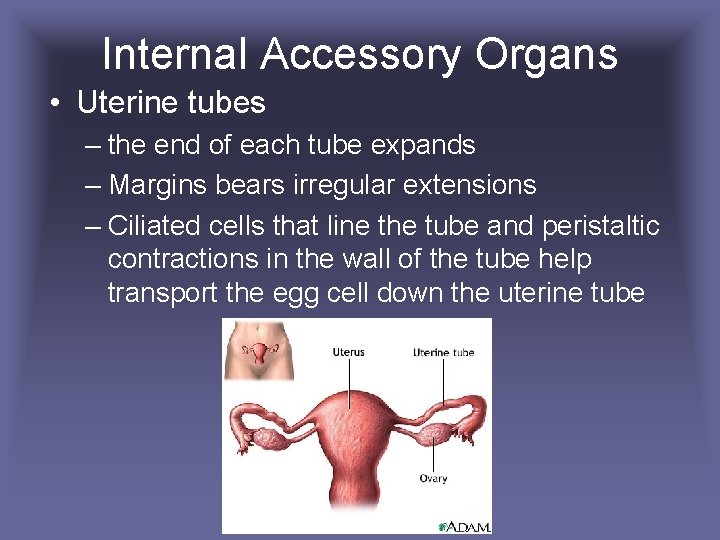
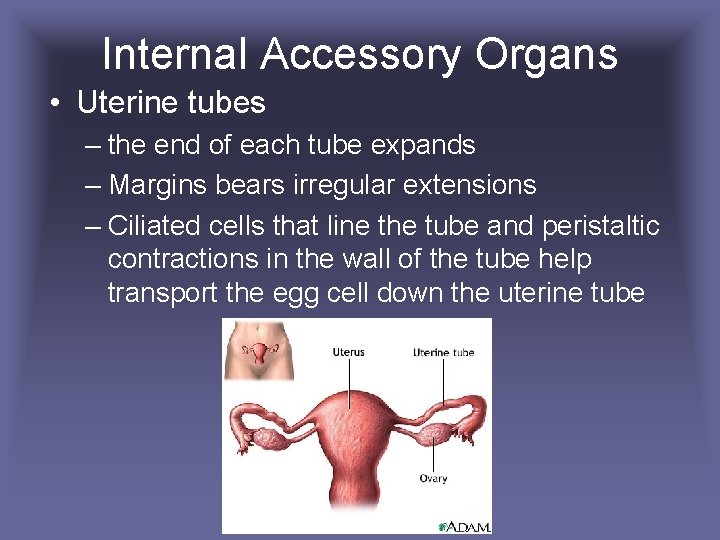
Internal Accessory Organs • Uterine tubes – the end of each tube expands – Margins bears irregular extensions – Ciliated cells that line the tube and peristaltic contractions in the wall of the tube help transport the egg cell down the uterine tube
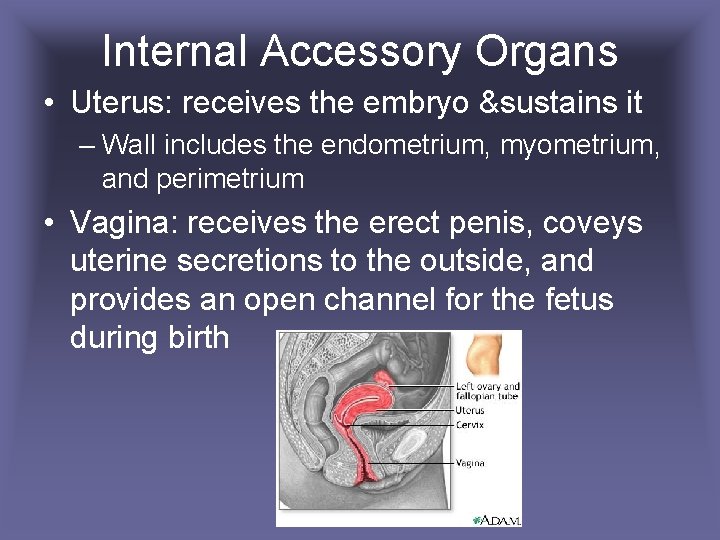
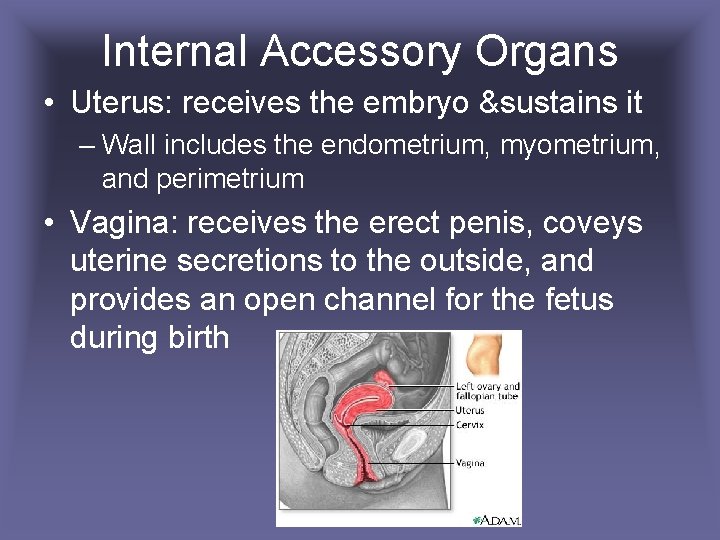
Internal Accessory Organs • Uterus: receives the embryo &sustains it – Wall includes the endometrium, myometrium, and perimetrium • Vagina: receives the erect penis, coveys uterine secretions to the outside, and provides an open channel for the fetus during birth
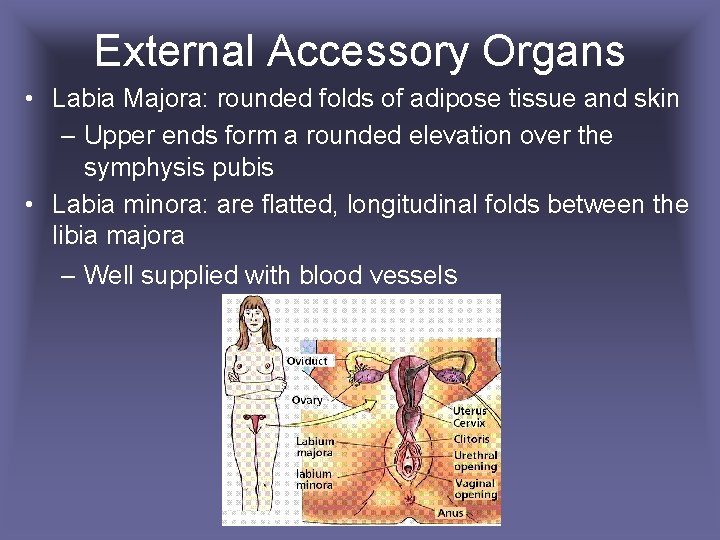
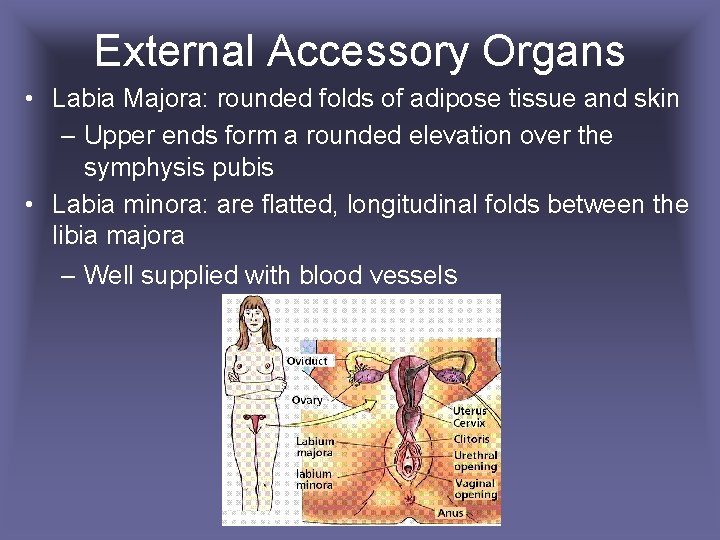
External Accessory Organs • Labia Majora: rounded folds of adipose tissue and skin – Upper ends form a rounded elevation over the symphysis pubis • Labia minora: are flatted, longitudinal folds between the libia majora – Well supplied with blood vessels
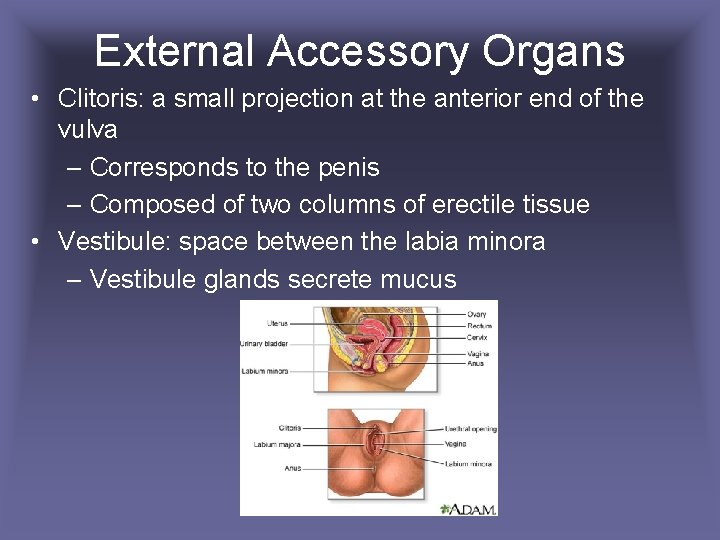
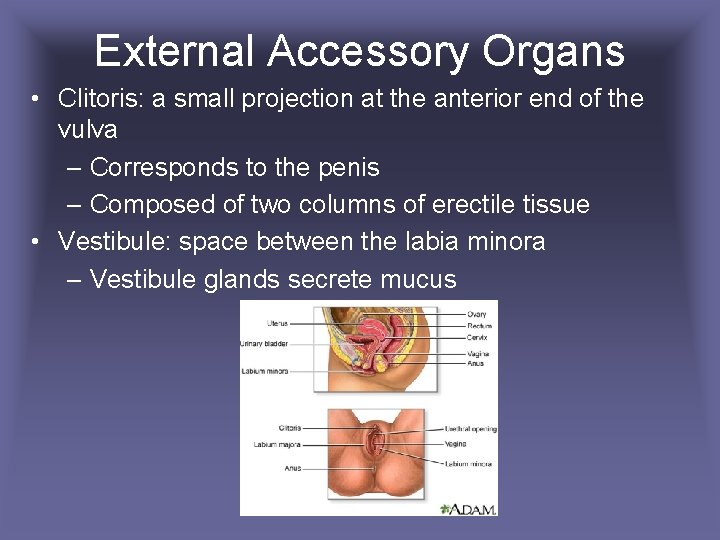
External Accessory Organs • Clitoris: a small projection at the anterior end of the vulva – Corresponds to the penis – Composed of two columns of erectile tissue • Vestibule: space between the labia minora – Vestibule glands secrete mucus
Female Hormones and Mammary Glands
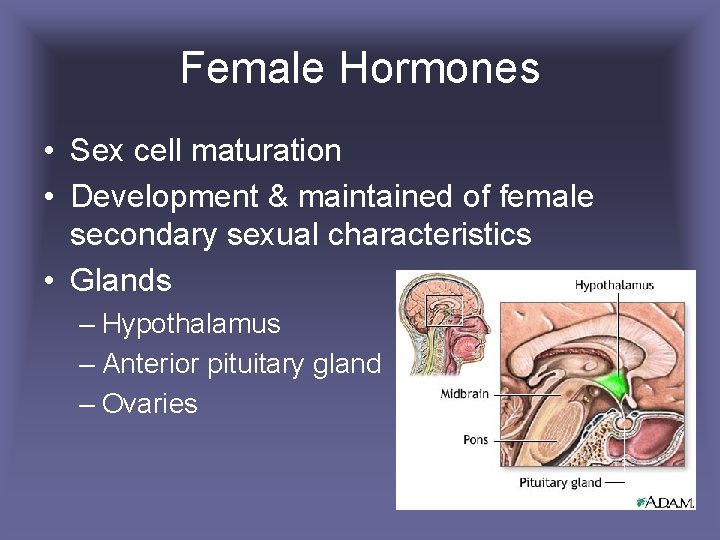
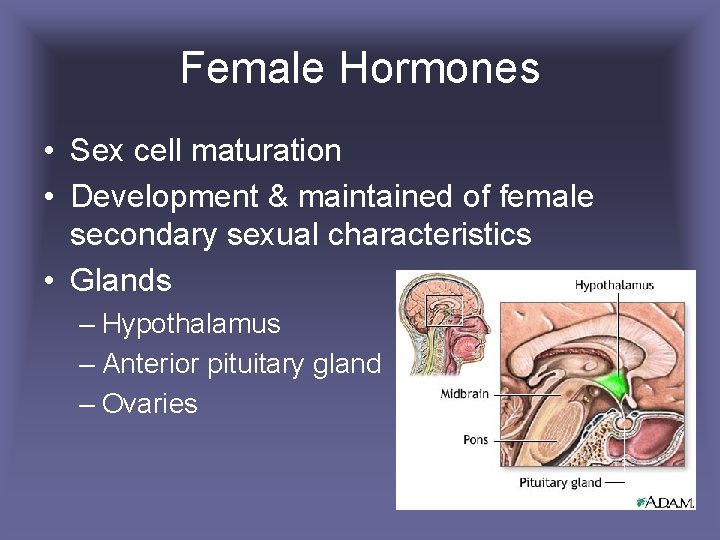
Female Hormones • Sex cell maturation • Development & maintained of female secondary sexual characteristics • Glands – Hypothalamus – Anterior pituitary gland – Ovaries
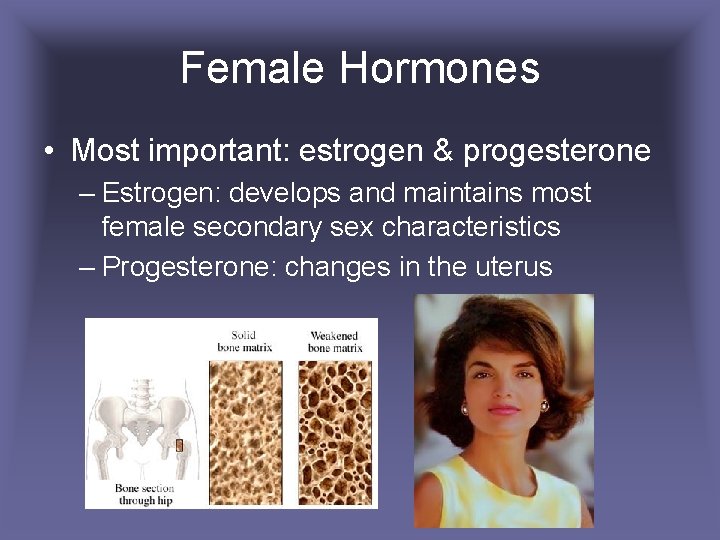
Female Hormones • Most important: estrogen & progesterone – Estrogen: develops and maintains most female secondary sex characteristics – Progesterone: changes in the uterus
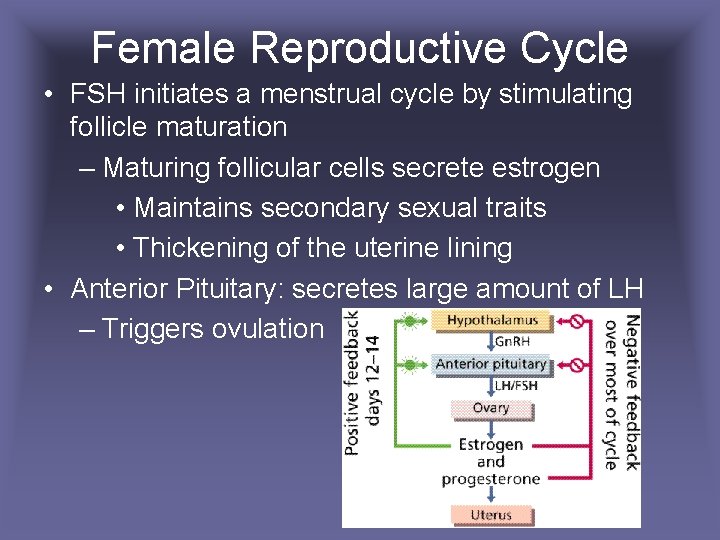
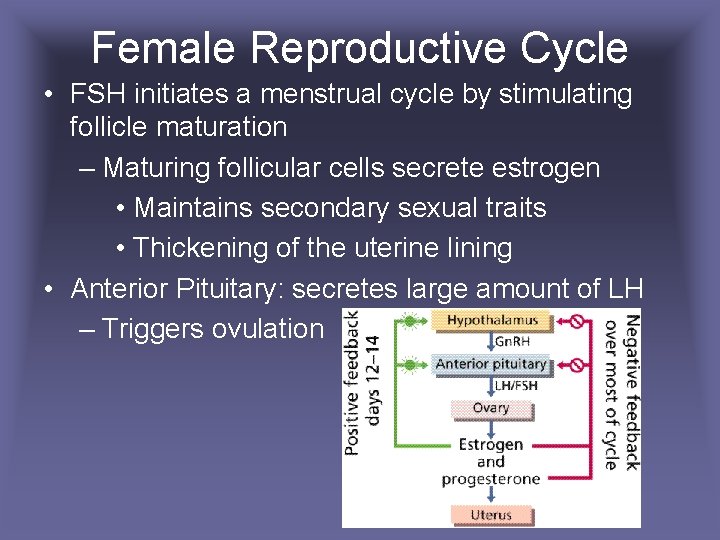
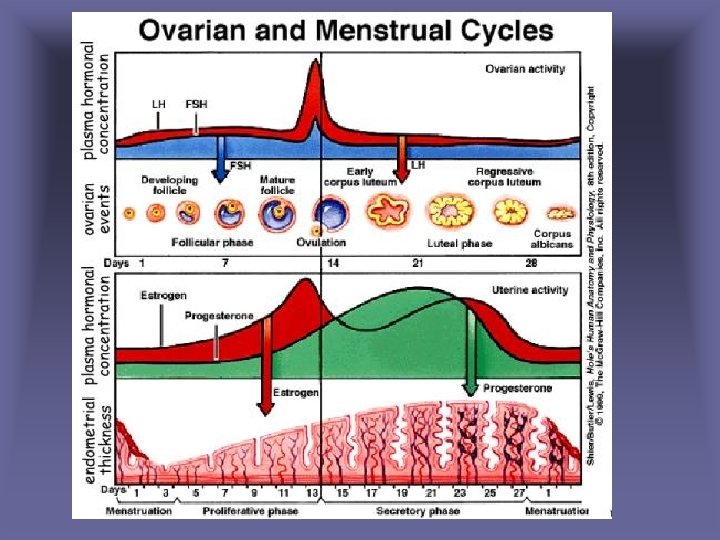
Female Reproductive Cycle • FSH initiates a menstrual cycle by stimulating follicle maturation – Maturing follicular cells secrete estrogen • Maintains secondary sexual traits • Thickening of the uterine lining • Anterior Pituitary: secretes large amount of LH – Triggers ovulation
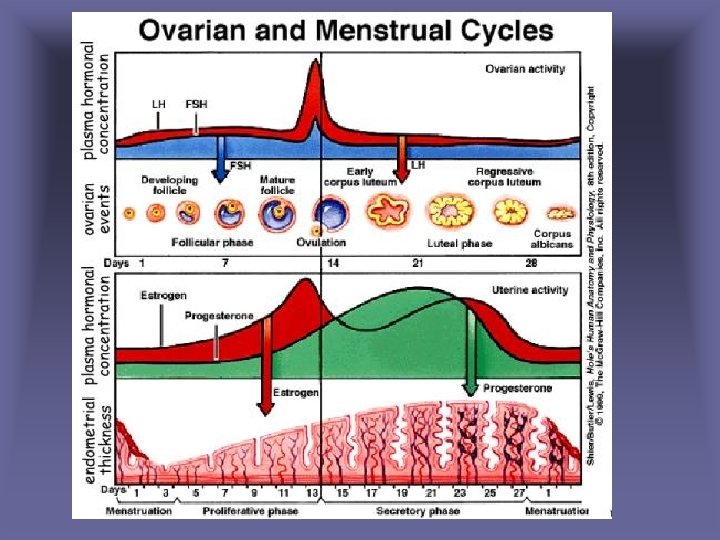
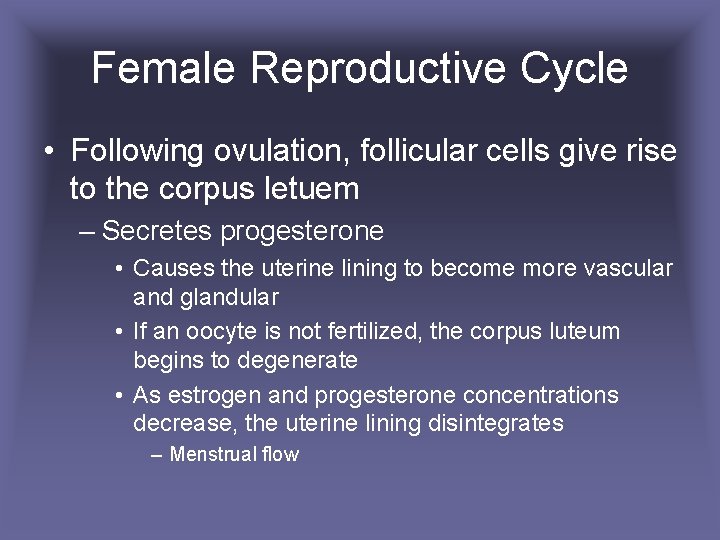
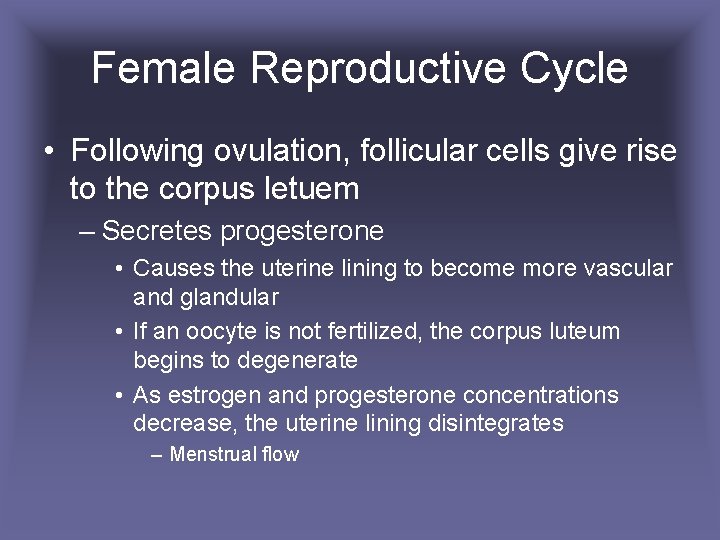
Female Reproductive Cycle • Following ovulation, follicular cells give rise to the corpus letuem – Secretes progesterone • Causes the uterine lining to become more vascular and glandular • If an oocyte is not fertilized, the corpus luteum begins to degenerate • As estrogen and progesterone concentrations decrease, the uterine lining disintegrates – Menstrual flow
Ovulation
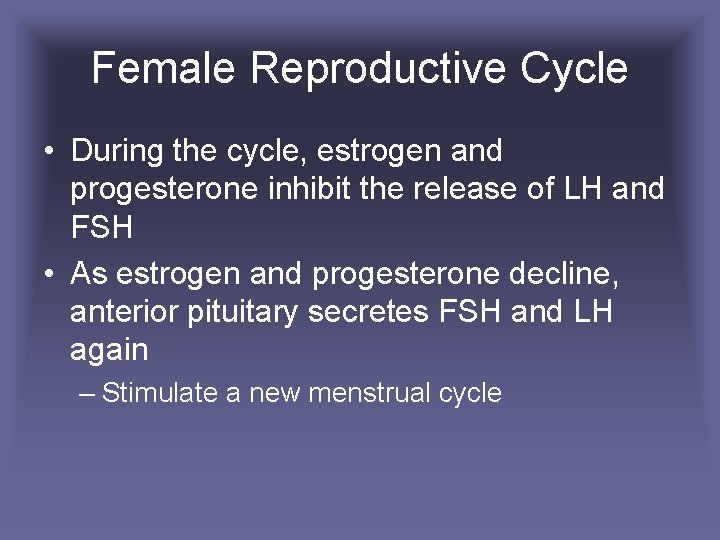
Female Reproductive Cycle • During the cycle, estrogen and progesterone inhibit the release of LH and FSH • As estrogen and progesterone decline, anterior pituitary secretes FSH and LH again – Stimulate a new menstrual cycle
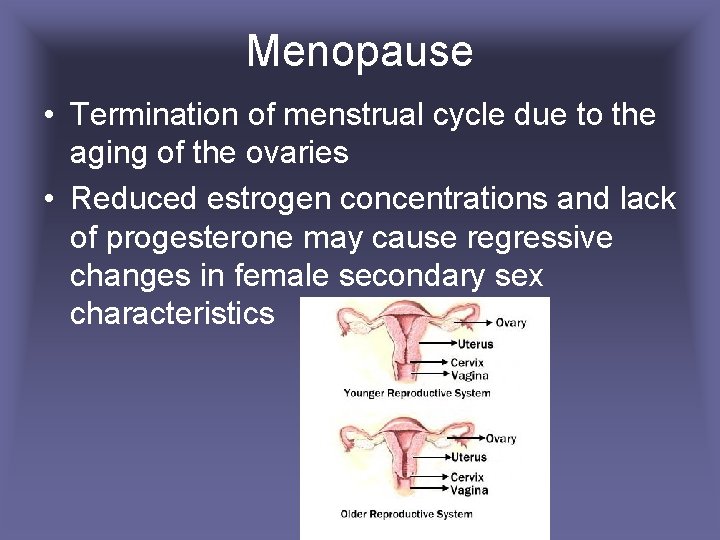
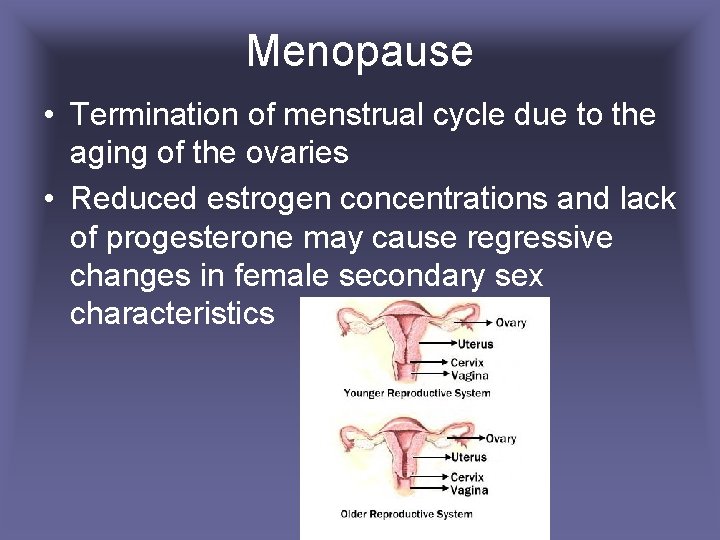
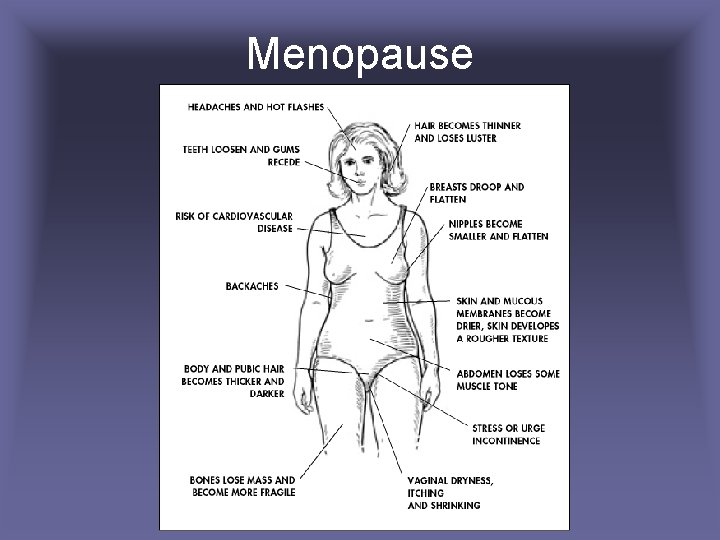
Menopause • Termination of menstrual cycle due to the aging of the ovaries • Reduced estrogen concentrations and lack of progesterone may cause regressive changes in female secondary sex characteristics
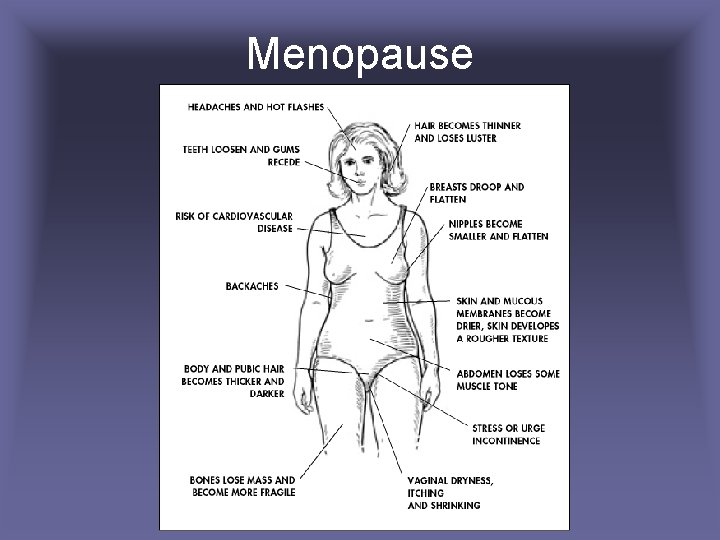
Menopause
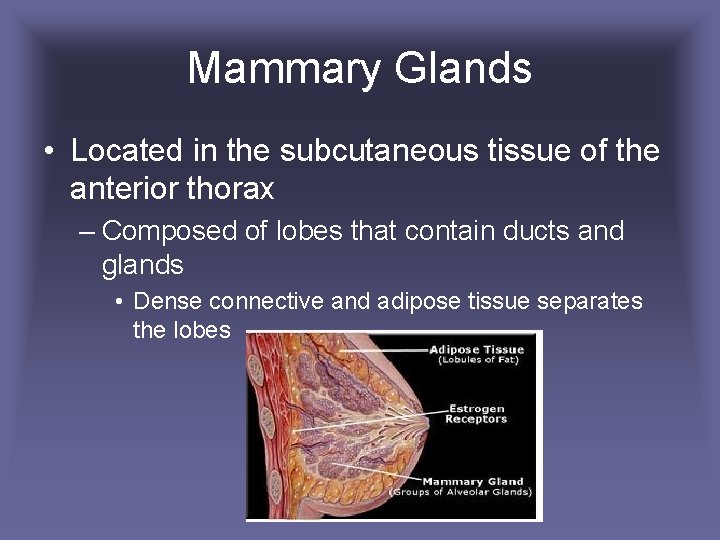
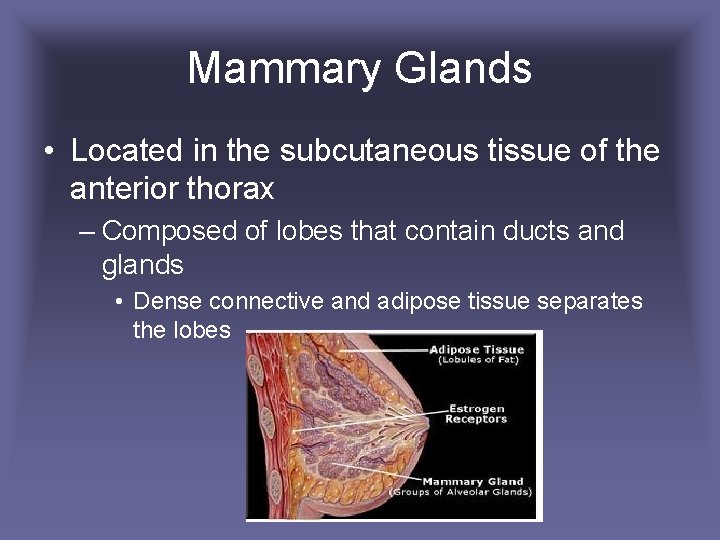
Mammary Glands • Located in the subcutaneous tissue of the anterior thorax – Composed of lobes that contain ducts and glands • Dense connective and adipose tissue separates the lobes
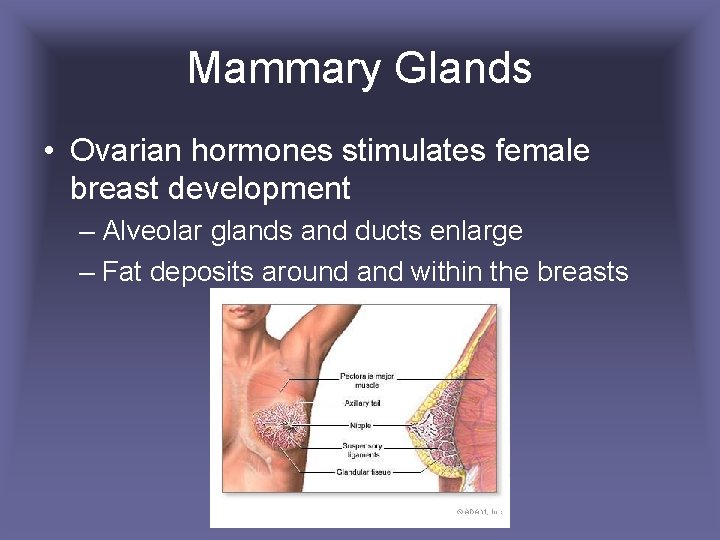
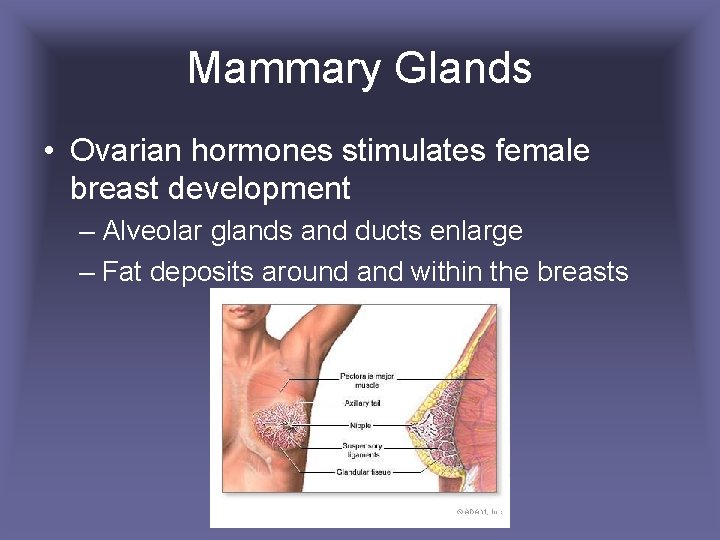
Mammary Glands • Ovarian hormones stimulates female breast development – Alveolar glands and ducts enlarge – Fat deposits around and within the breasts
 Female testes
Female testes Parts of male and female reproductive system
Parts of male and female reproductive system Differences between male and female reproductive organ
Differences between male and female reproductive organ 90/2
90/2 What does the seminal vesicle secrete
What does the seminal vesicle secrete Is croaker a cartilaginous fish
Is croaker a cartilaginous fish Labeled female reproductive system
Labeled female reproductive system Function of male reproductive system
Function of male reproductive system Sperm duct
Sperm duct Chapter 16 reproductive system
Chapter 16 reproductive system Male reproductive system table
Male reproductive system table Major endocrine glands male and female
Major endocrine glands male and female Endocrine system organs
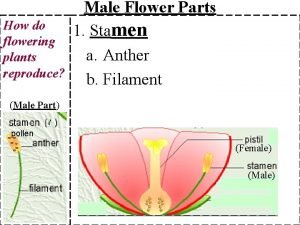
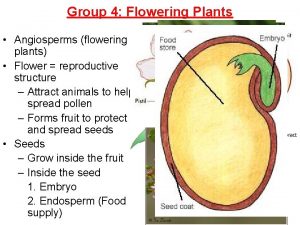
Endocrine system organs Part of flower that produces pollen
Part of flower that produces pollen Chapter 7 extending mendelian genetics answer key
Chapter 7 extending mendelian genetics answer key Male flower
Male flower What part of the flower makes pollen
What part of the flower makes pollen Difference between male and female drosophila
Difference between male and female drosophila Sciatic notch male vs female
Sciatic notch male vs female How many lower teeth
How many lower teeth Female parts of plants
Female parts of plants Bispinous diameter
Bispinous diameter Androgen insensitivity
Androgen insensitivity Bone bonanza a lab on male and female skeletons answer key
Bone bonanza a lab on male and female skeletons answer key Difference between male and female sharks
Difference between male and female sharks All plants have flowers
All plants have flowers Pictures of male and female ladybugs
Pictures of male and female ladybugs Lesson 14.2 male and female urinary structures
Lesson 14.2 male and female urinary structures Female gopher tortoise
Female gopher tortoise Male and female hormones
Male and female hormones Male and female hormones
Male and female hormones Codominance
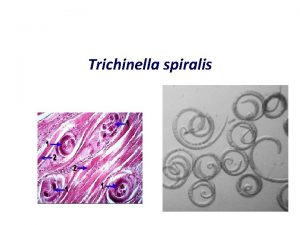
Codominance Trichinella spiralis egg morphology
Trichinella spiralis egg morphology Ap physics 1 momentum equations
Ap physics 1 momentum equations Larva
Larva Copyright
Copyright Venn diagram of plant and animal reproduction
Venn diagram of plant and animal reproduction Human development cycle
Human development cycle Piggender
Piggender Function of vagina
Function of vagina Exercise 42 anatomy of the reproductive system
Exercise 42 anatomy of the reproductive system Oogenesis process
Oogenesis process Round ligament of uterus
Round ligament of uterus Luteinizing hormone in male reproductive system
Luteinizing hormone in male reproductive system Male reproductive system of a plant
Male reproductive system of a plant Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Male reproductive system information
Male reproductive system information