Reproductive Systems 2 Types Male Female Male Reproductive





- Slides: 25
Reproductive Systems 2 Types: Male Female

Male Reproductive System Functions: • Sperm Production • Sperm Nourishment • Sperm Transportation
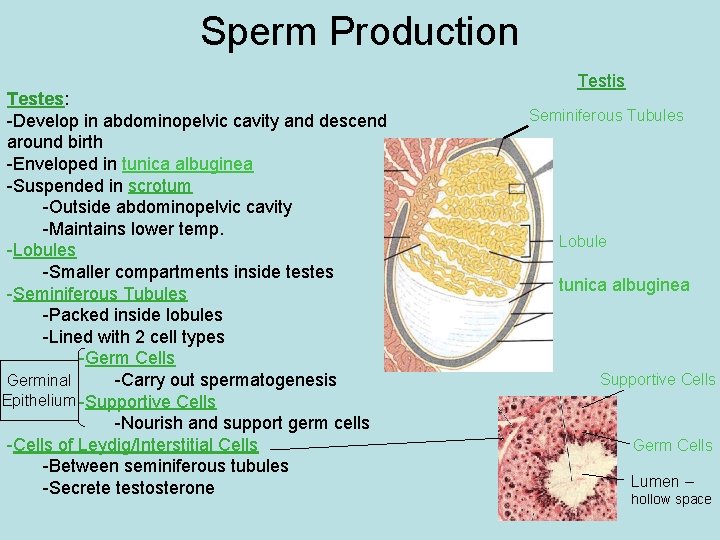
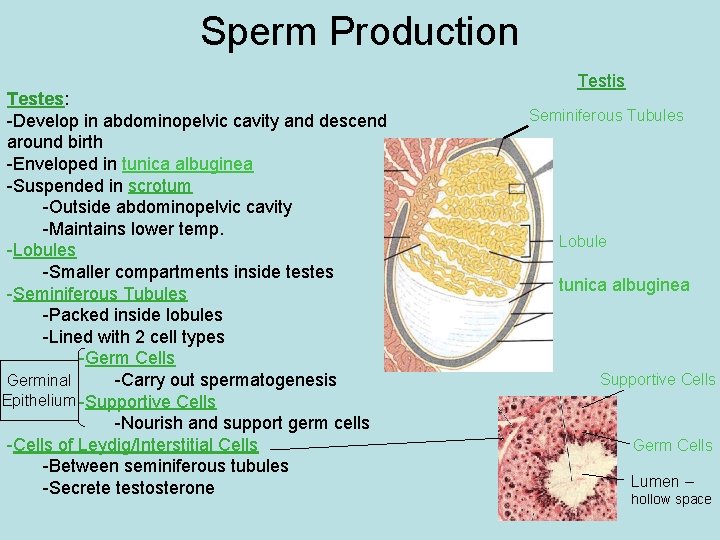
Sperm Production Testes: -Develop in abdominopelvic cavity and descend around birth -Enveloped in tunica albuginea -Suspended in scrotum -Outside abdominopelvic cavity -Maintains lower temp. -Lobules -Smaller compartments inside testes -Seminiferous Tubules -Packed inside lobules -Lined with 2 cell types -Germ Cells -Carry out spermatogenesis Germinal Epithelium -Supportive Cells -Nourish and support germ cells -Cells of Leydig/Interstitial Cells -Between seminiferous tubules -Secrete testosterone Testis Seminiferous Tubules Lobule tunica albuginea Supportive Cells Germ Cells Lumen – hollow space
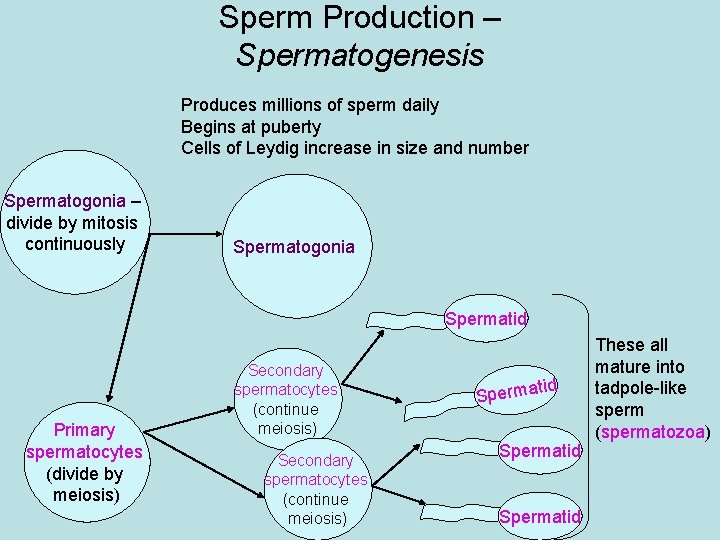
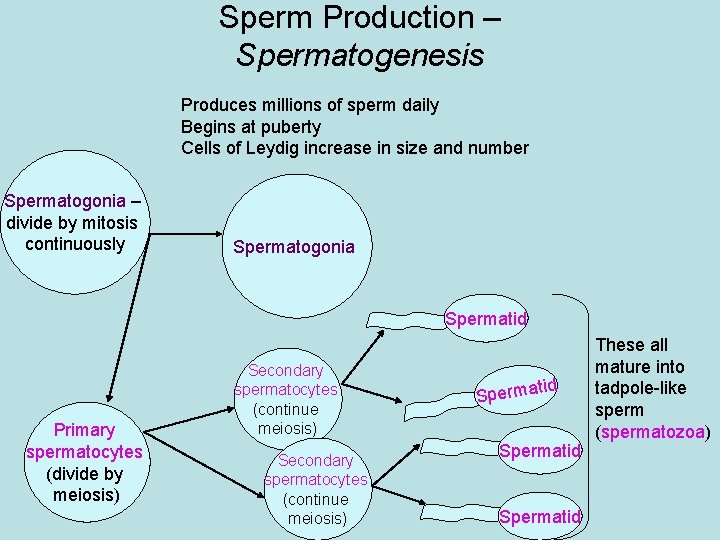
Sperm Production – Spermatogenesis Produces millions of sperm daily Begins at puberty Cells of Leydig increase in size and number Spermatogonia – divide by mitosis continuously Spermatogonia Spermatid Primary spermatocytes (divide by meiosis) Secondary spermatocytes (continue meiosis) tid Spermatid These all mature into tadpole-like sperm (spermatozoa)
Quick Quiz: What process does a cell go through to create sperm? 1. Mitosis 2. Meiosis 1 2 3 4 5 6 7 8 9 10 11 12 21 22 23 24 25 26 27 28 29 30 31 32 13 14 15 16 17 18 19 20
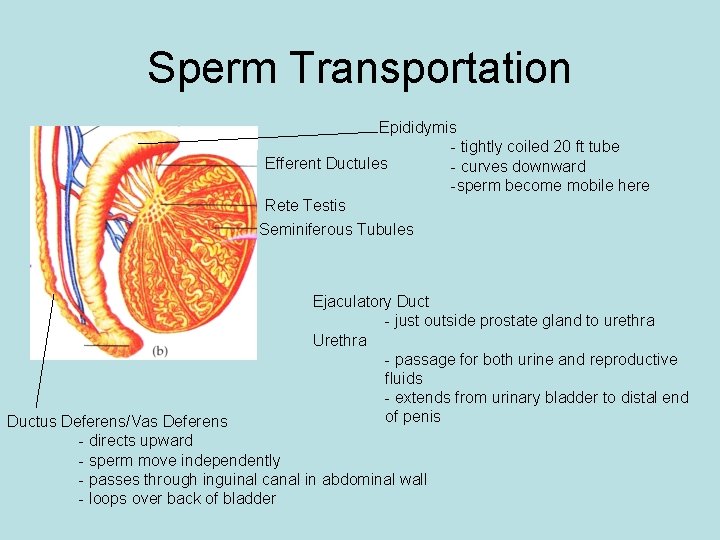
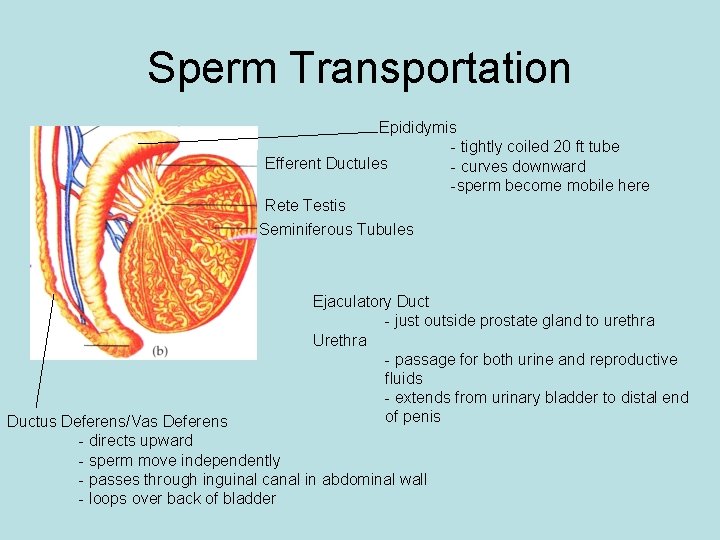
Sperm Transportation Epididymis - tightly coiled 20 ft tube Efferent Ductules - curves downward -sperm become mobile here Rete Testis Seminiferous Tubules Ejaculatory Duct - just outside prostate gland to urethra Urethra - passage for both urine and reproductive fluids - extends from urinary bladder to distal end of penis Ductus Deferens/Vas Deferens - directs upward - sperm move independently - passes through inguinal canal in abdominal wall - loops over back of bladder
Quick Quiz: Where does sperm travel to after it exits the epididymis? 1. 2. 3. 4. 5. Rete Testes Urethra Bladder Vas Deferens Efferent Tubules 1 2 3 4 5 6 7 8 9 10 11 12 21 22 23 24 25 26 27 28 29 30 31 32 13 14 15 16 17 18 19 20
Sperm Nourishment Seminal Vesicles: - located at base of bladder - secretions rich in fructose - contribute 60% of fluid volume Prostate Gland: - walnut sized - located at base of bladder - thick, milky, alkaline secretions - neutralize acidic vaginal fluid Bulbourethral Glands: - pea-sized, paired - located below prostate gland - thick, clear mucus secretions - clear urethra before semen passage, lubricates
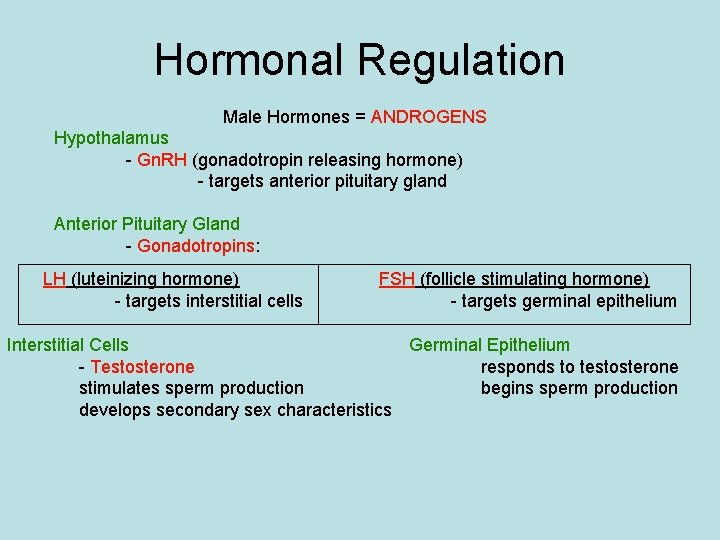
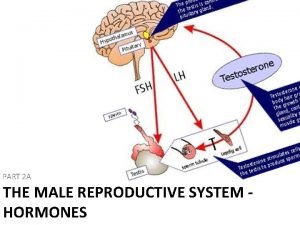
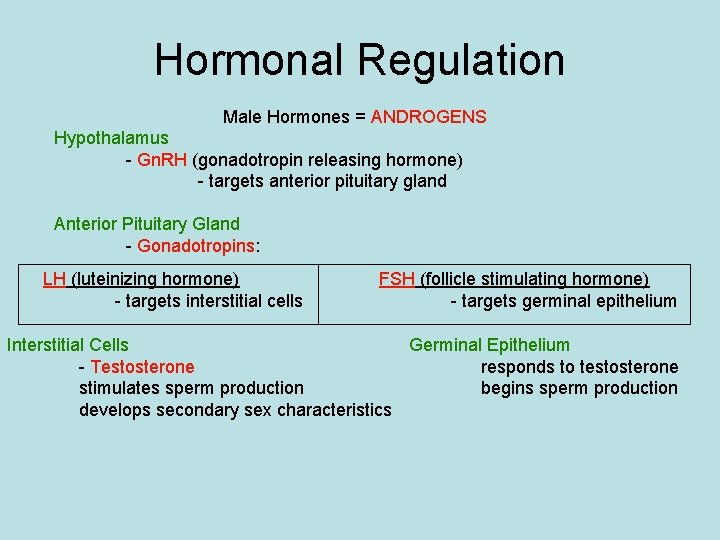
Hormonal Regulation Male Hormones = ANDROGENS Hypothalamus - Gn. RH (gonadotropin releasing hormone) - targets anterior pituitary gland Anterior Pituitary Gland - Gonadotropins: LH (luteinizing hormone) - targets interstitial cells FSH (follicle stimulating hormone) - targets germinal epithelium Interstitial Cells Germinal Epithelium - Testosterone responds to testosterone stimulates sperm production begins sperm production develops secondary sex characteristics
Quick Quiz: What molecule stimulates the secretion of gonadotropins? 1. 2. 3. 4. LH FSH Testosterone Gn. RH 1 2 3 4 5 6 7 8 9 10 11 12 21 22 23 24 25 26 27 28 29 30 31 32 13 14 15 16 17 18 19 20
Quick Quiz: Where is testosterone produced? 1. Brain 2. Pituitary Gland 3. Germinal Epithelium 4. Hypothalamus 5. Interstitial Cells 6. Seminiferous Tubules 1 2 3 4 5 6 7 8 9 10 11 12 21 22 23 24 25 26 27 28 29 30 31 32 13 14 15 16 17 18 19 20
Female Reproductive System Functions: • • Oocyte Production Receive Sperm Develop Offspring Deliver Offspring
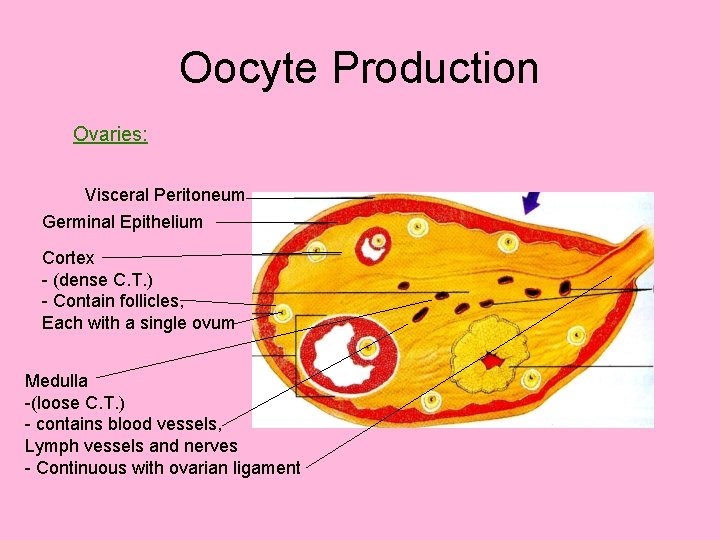
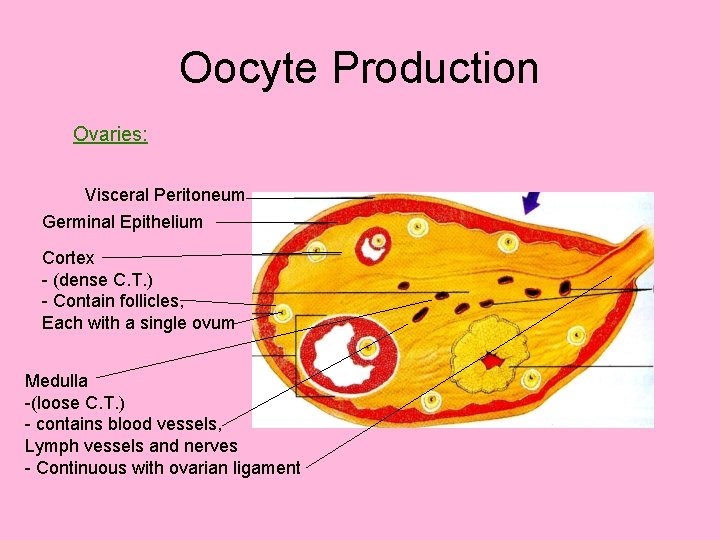
Oocyte Production Ovaries: Visceral Peritoneum Germinal Epithelium Cortex - (dense C. T. ) - Contain follicles, Each with a single ovum Medulla -(loose C. T. ) - contains blood vessels, Lymph vessels and nerves - Continuous with ovarian ligament
Quick Quiz: What function does the germinal epithelium serve in adult females? 1. None 2. Creates new follicles 3. Creates new oocytes 4. Creates new ovaries 5. Brings in blood 1 2 3 4 5 6 7 8 9 10 11 12 21 22 23 24 25 26 27 28 29 30 31 32 13 14 15 16 17 18 19 20
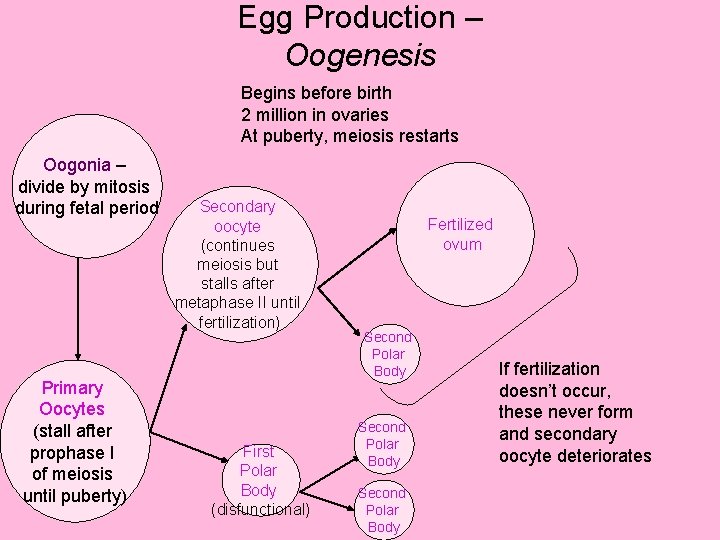
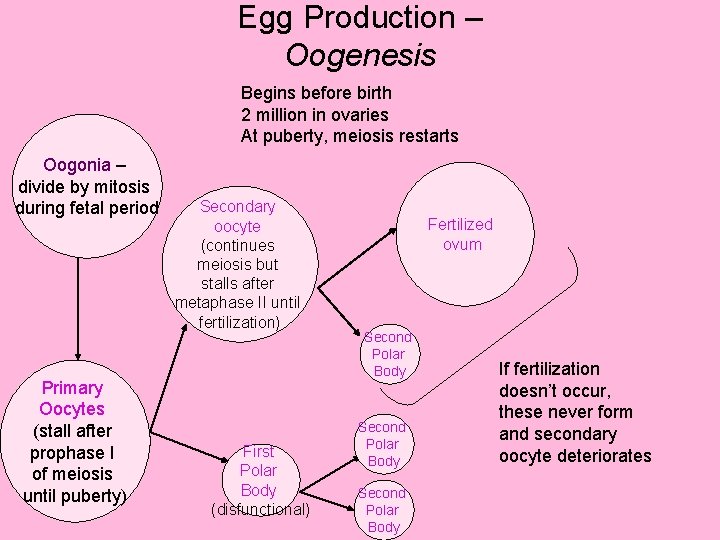
Egg Production – Oogenesis Begins before birth 2 million in ovaries At puberty, meiosis restarts Oogonia – divide by mitosis during fetal period Primary Oocytes (stall after prophase I of meiosis until puberty) Secondary oocyte (continues meiosis but stalls after metaphase II until fertilization) First Polar Body (disfunctional) Fertilized ovum Second Polar Body If fertilization doesn’t occur, these never form and secondary oocyte deteriorates

Quick Quiz: When does the secondary oocyte finish meiosis? 1. Immediately after meiosis I to create a polar body and an ovum 2. Only after fertilization to create a polar body and a fertilized ovum 3. Never, it always deteriorates 1 2 3 4 5 6 7 8 9 10 11 12 21 22 23 24 25 26 27 28 29 30 31 32 13 14 15 16 17 18 19 20
Quick Quiz: What is the function of the polar bodies? 1. Remove excess DNA 2. Become fertilized 3. Supply energy
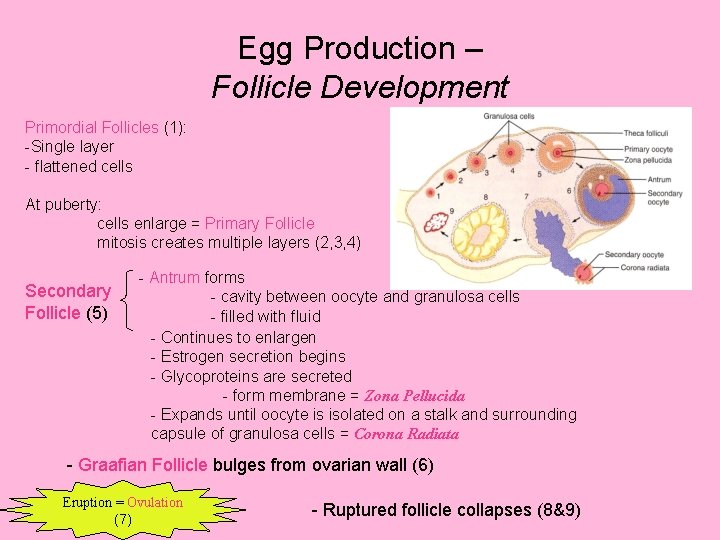
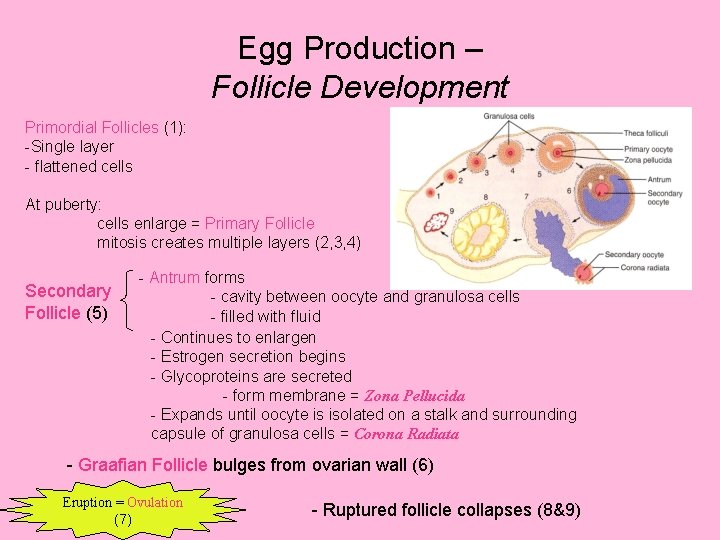
Egg Production – Follicle Development Primordial Follicles (1): -Single layer - flattened cells At puberty: cells enlarge = Primary Follicle mitosis creates multiple layers (2, 3, 4) Secondary Follicle (5) - Antrum forms - cavity between oocyte and granulosa cells - filled with fluid - Continues to enlargen - Estrogen secretion begins - Glycoproteins are secreted - form membrane = Zona Pellucida - Expands until oocyte is isolated on a stalk and surrounding capsule of granulosa cells = Corona Radiata - Graafian Follicle bulges from ovarian wall (6) Eruption = Ovulation (7) - Ruptured follicle collapses (8&9)
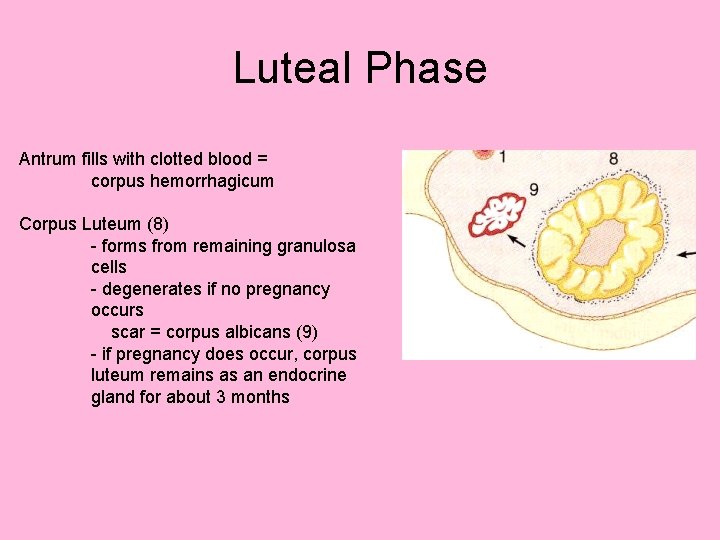
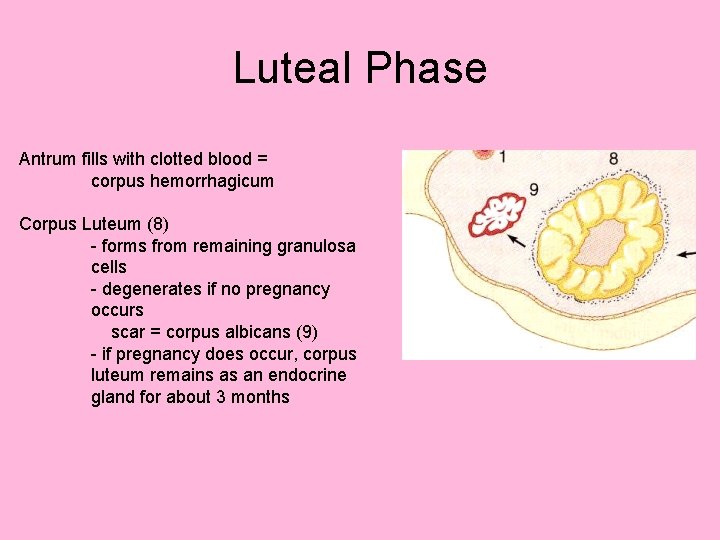
Luteal Phase Antrum fills with clotted blood = corpus hemorrhagicum Corpus Luteum (8) - forms from remaining granulosa cells - degenerates if no pregnancy occurs scar = corpus albicans (9) - if pregnancy does occur, corpus luteum remains as an endocrine gland for about 3 months

Hormonal Regulation Follows an approximately 28 day cycle Day 1 Hypothalamus - Gn. RH (gonadotropin releasing hormone) - targets anterior pituitary gland Anterior Pituitary Gland - Gonadotropins: LH (luteinizing hormone) - targets thecal cells outside follicle Thecal cells secrete androgens FSH (follicle stimulating hormone) - targets follicle cells Follicle cells convert androgens to estrogens Estrogens - target endometrial cells

Hormonal Regulation Estrogens Negative feedback on hypothalamus Positive feedback on follicle cells Day 14 Estrogens reach critical threshold Positive feedback on hypothalamus LH and FSH spike – triggers ovulation - damages follicle Corpus luteum forms Estrogen levels decline Progesterone and estrogen are produced - Supports endometrium Negative feedback on hypothalamus - inhibits new follicle development LH declines as corpus luteum degenerates estrogen and progesterone drop sharply Day 28 Cycle restarts!
FSH Estrogen LH Progesterone
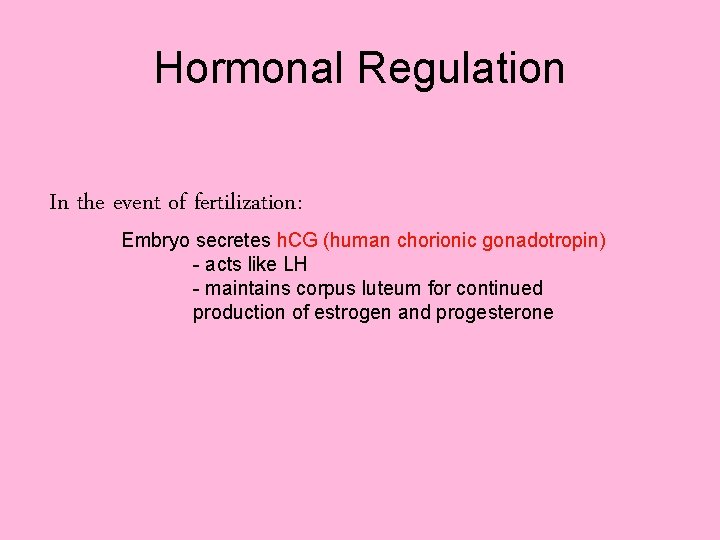
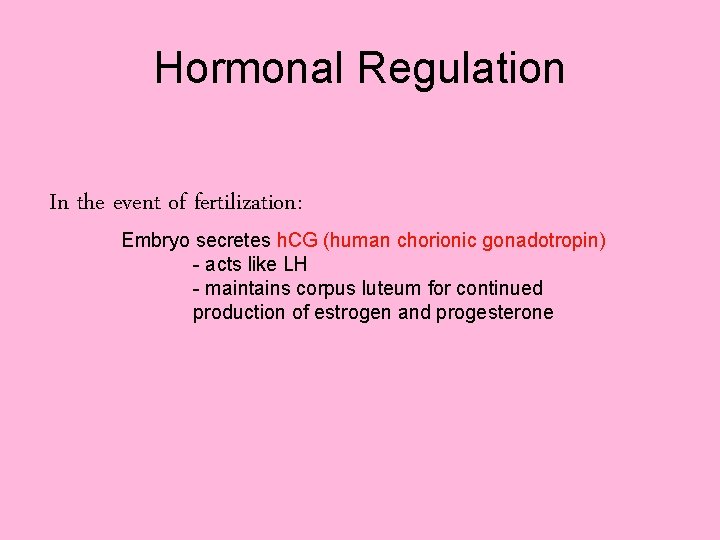
Hormonal Regulation In the event of fertilization: Embryo secretes h. CG (human chorionic gonadotropin) - acts like LH - maintains corpus luteum for continued production of estrogen and progesterone

Offspring Development Ovulation Oocyte and corona radiata are expelled Swept into infundibulum of fallopian tube by fimbriae Fertilization may or may not occur Passes into uterus 2 Regions: Body Cervix - opens into vagina by external os - cervical glands secrete mucus that blocks external os 3 layers: Perimetrium - secretes serous fluid Myometrium - muscular layer Endometrium - epithelial and vascular layer
Remaining Anatomical Structures: Vaginal Structures: Fornix: pockets around external os Vaginal Orifice: external opening Vestibular Glands: - secrete mucus for lubrication
 Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Male fallopian tube
Male fallopian tube Similarities between male and female reproductive system
Similarities between male and female reproductive system Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Erected
Erected Is croaker a cartilaginous fish
Is croaker a cartilaginous fish Structure of female
Structure of female Fetus reproductive system
Fetus reproductive system Ovary structures
Ovary structures Female reproductive system pregnancy
Female reproductive system pregnancy Inguinal
Inguinal Unit 5 lesson 3 the female reproductive system
Unit 5 lesson 3 the female reproductive system Ovary diagram
Ovary diagram Main function of female reproductive system
Main function of female reproductive system Uterus is the part of which system in pila
Uterus is the part of which system in pila Fetal pig urinary system labeled
Fetal pig urinary system labeled Definition of reproductive system
Definition of reproductive system Figure 28-2 the female reproductive system
Figure 28-2 the female reproductive system Sagittal female reproductive system
Sagittal female reproductive system Chapter 16 lesson 3 the female reproductive system
Chapter 16 lesson 3 the female reproductive system Female cow reproductive system
Female cow reproductive system Cows reproductive system
Cows reproductive system Oviduct funnel
Oviduct funnel Male reproductive system diagram
Male reproductive system diagram Oogenesis and follicular development
Oogenesis and follicular development What are primary sexual characteristics
What are primary sexual characteristics