QIO Office Hours COVID19 Skilled Nursing Facilities and







- Slides: 68
QIO Office Hours COVID-19 Skilled Nursing Facilities �� and Telemedicine Joni Hollister and Becky Sanders April 29. 2020

Agenda • Opening Remarks • Housekeeping • Presentation • Q&A • Closing Remarks 2
On-Demand Learning We also make each Office Hour available for On-Demand Learning to share with peers. Office Hours | COVID-19 Focused Survey for Nursing Homes URL: https: //bit. ly/2 RCWf. Cq Office Hours | How to Safely and Effectively Handle Vendors in Your Facility During COVID-19 URL: https: //bit. ly/2 K 1 o. ZQT 3
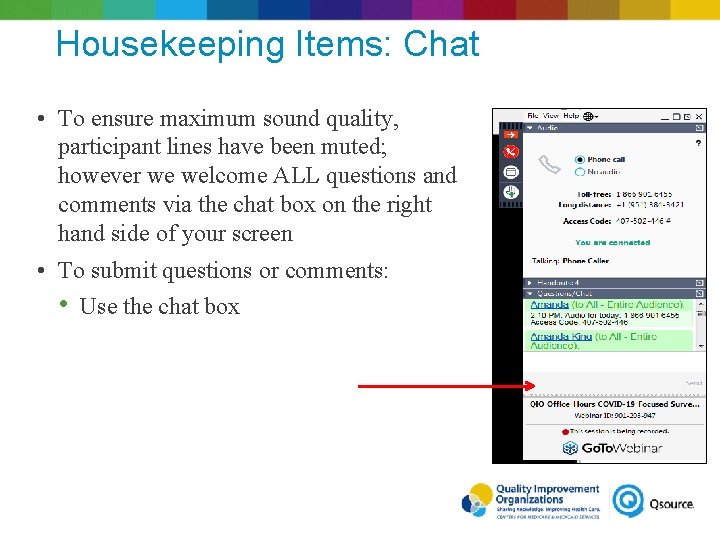
Housekeeping Items: Chat • To ensure maximum sound quality, participant lines have been muted; however we welcome ALL questions and comments via the chat box on the right hand side of your screen • To submit questions or comments: • Use the chat box 4
Polling Question Which of the following sources do you prefer to receive professional development opportunities and information? Select your top 3: Ø Webinars/Webcasts Ø Podcasts/Short audio recordings/On-demand learning sessions Ø Online Journal Articles and/or Blogs Ø Email network/List. Serv with links to online resource Ø Social Media (twitter, facebook, linkedin) 5
Joni Hollister, HFA Health Network Integration Specialist 6
Becky Sanders QIO Office Hours: Skilled Nursing Facilities and Telemedicine April 29, 2020 Please be advised that UMTRC only provides guidance on billing issues based on experience, anecdotal information we have heard in the field, and through research. Following our advice does not guarantee payment. We always recommend you check with the payer (or your Medicare Administrative Contractor) to verify UMTRC’s information. Senior Director, Indiana Rural Health Association Program Director, Upper Midwest Telehealth Resource Center This project is/was supported by the Health Resources and Services Administration (HRSA) of the U. S. Department of Health and Human Services (HHS) under grant number G 22 RH 30351 under the Telehealth Resource Center Grant Program for $325, 000. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U. S. Government. 7
Objectives Know how to access technical assistance if needed Understand the technology needed on both the clinician and patient side to implement telemedicine Be able to begin implementing telemedicine in their facility Understand how state and federal waivers have changed billing requirements for telemedicine services

National Consortium of Telehealth Resource Centers

NCTRC Website https: //www. telehealthresourcecenter. org/
• Virtual Librarians UMTRC Services • • • Individual Consultation Technical Assistance Connections with other programs • Presentations & Trainings • • Project assessments Updates on reimbursement policy and legislative developments
UMTRC Website Facebook Linked. In
Telehealth versus Telemedicine • Definitions and Concepts • Sometimes used interchangeably Two types of distinctions • Telehealth Broader field of distance health activities (CME, etc. ) Clinical remote monitoring (usually at home) Education • • Telemedicine • Billable interactive clinical services
Asynchronous Types of Telemedicine Describes store and forward transmission of medical images or information because the transmission typically occurs in one direction in time Store-and-forward telemedicine Pictures, data Synchronous Describes interactive video connections because the transmission of information in both directions is occurring at exactly the same period Live and Interactive Telemedicine HIPAA Compliant, Secure real-time audio AND video
● Telehealth is a DELIVERY mechanism Telehealth is not a service; but a delivery mechanism for health care services – Live and interactive telehealth services duplicate clinical in-person care – Some services are made better or possible with telehealth when distance is a barrier – Reimbursement should be equal to “in-person” care 15
COVID-19 https: //www. umtrc. org/resources/covid-19/
Medicare and state Medicaid programs have relaxed HIPAA rules COVID-19 HIPAA Rules Relaxed CMS clarified in their Final Interim Rule (released on March 31, 2020) that for telehealth services a “telecommunications system” would mean “multimedia communications equipment that includes, at a minimum, audio and video equipment permitting two-way, real-time interactive communication between the patient and distant site physician or practitioner. ” See CCHP Telehealth Coverage Policies in the time of COVID-19 https: //www. cchpca. org/resources/covid-19 -telehealthcoverage-policies See UMTRC COVID-19 Resource Page https: //www. umtrc. org/resources/covid-19/ UMTRC still recommends HIPAA compliant technology
TTAC Toolkits http: //telehealthtechnology. org/toolkits/

TTAC Toolkits http: //telehealthtechnology. org/toolkits/
Existing Organizational EMR System and Technology Epic Cerner Meditech Cisco Microsoft 20
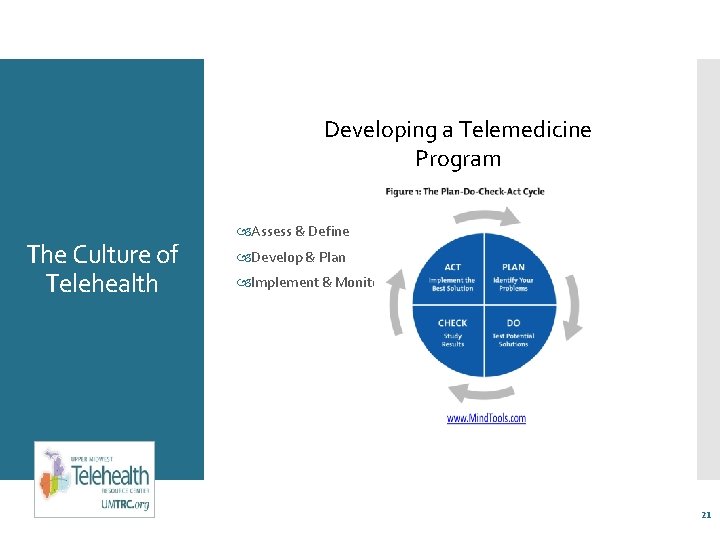
Developing a Telemedicine Program The Culture of Telehealth Assess & Define Develop & Plan Implement & Monitor 21
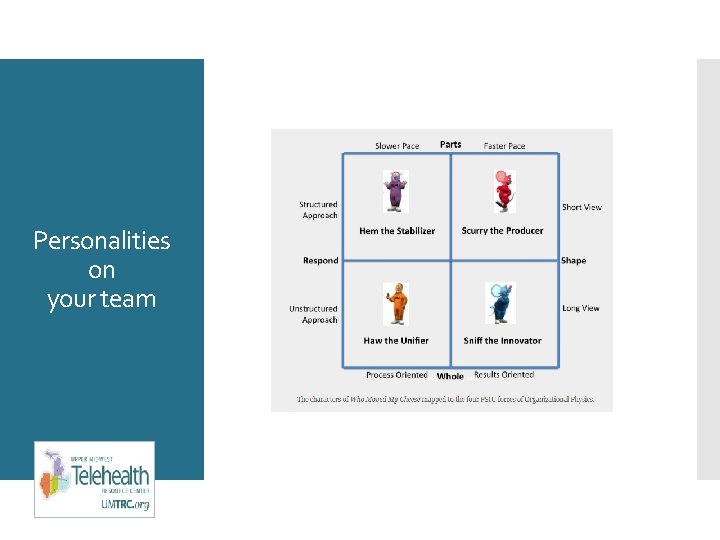
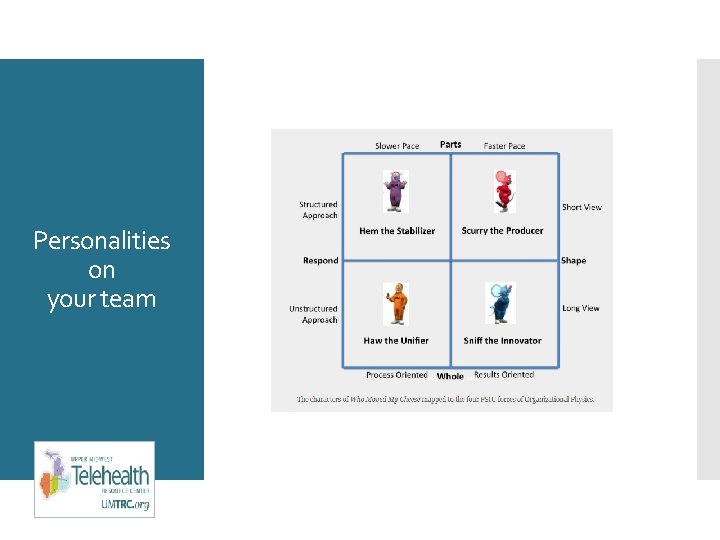
Personalities on your team
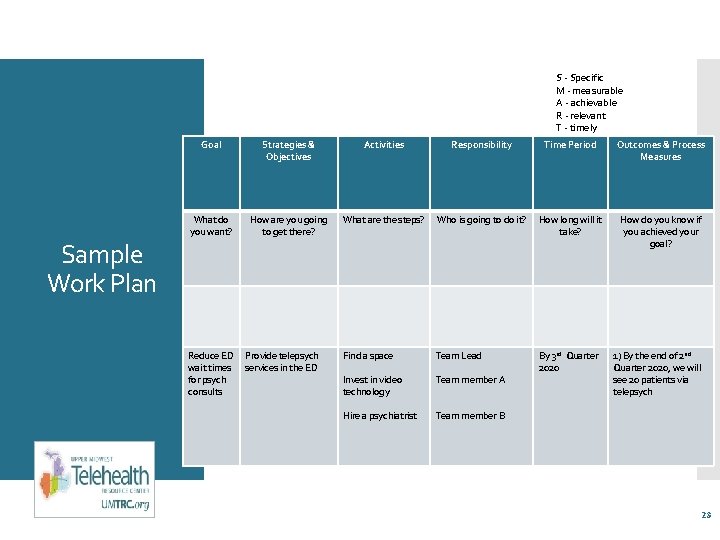
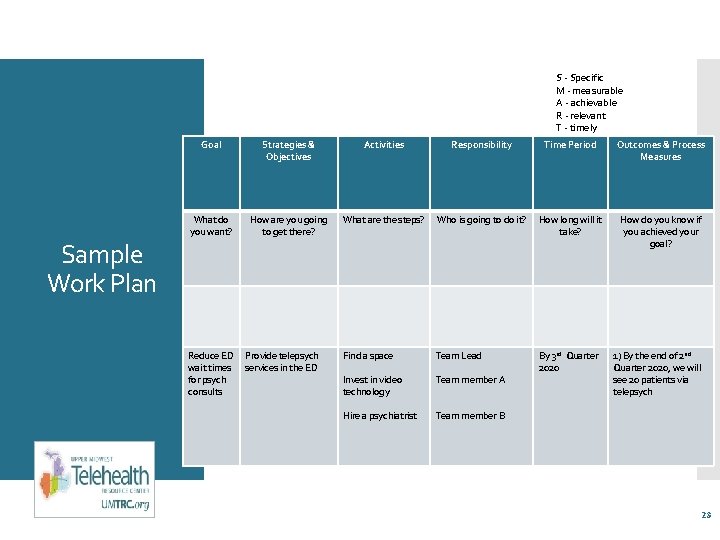
S - Specific M - measurable A - achievable R - relevant T - timely Sample Work Plan Goal Strategies & Objectives Activities Responsibility Time Period Outcomes & Process Measures What do you want? How are you going to get there? What are the steps? Who is going to do it? How long will it take? How do you know if you achieved your goal? Find a space Team Lead Invest in video technology Team member A By 3 rd Quarter 2020 Hire a psychiatrist Team member B Reduce ED wait times for psych consults Provide telepsych services in the ED 1) By the end of 2 nd Quarter 2020, we will see 20 patients via telepsych 23
Not as easy as it sounds! Change management theories Work Plan Implementation Telemedicine room setups The good, bad and the ugly Problem solving solutions 24
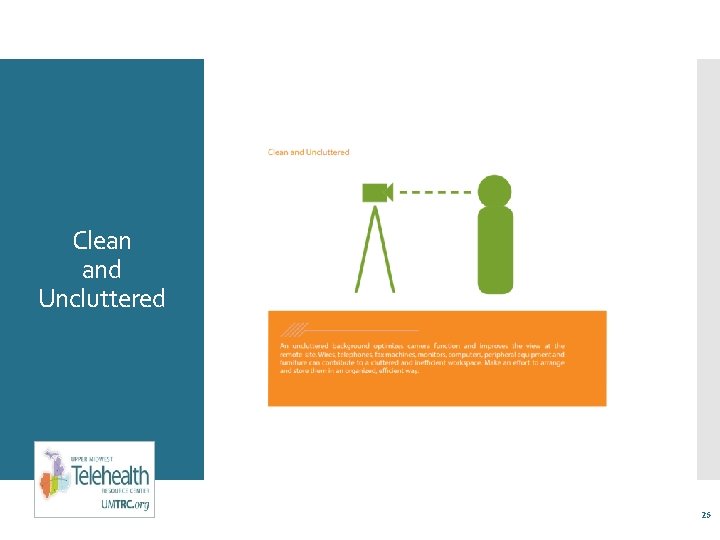
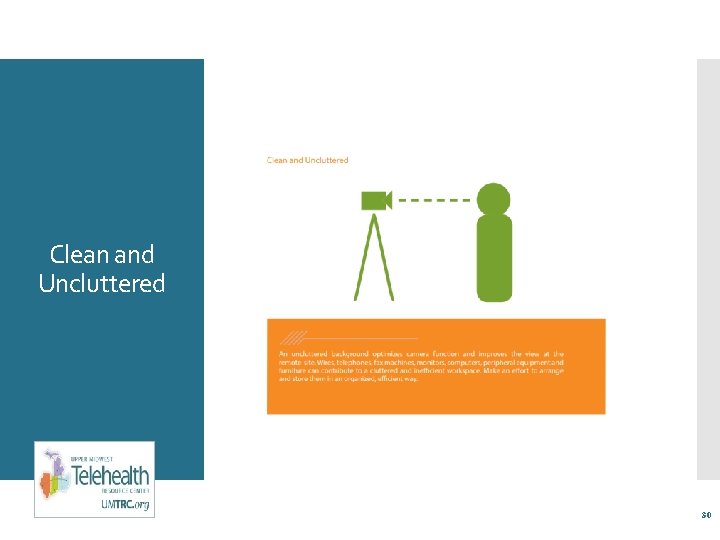
Clean and Uncluttered 25
Existing Patient Room • Large enough to move around comfortably • Exam table • Chairs • Telemedicine equipment • Patient • Telepresenters • Work surface • Phone/computer, etc. 26
Seeing patients from their residential SNF home Privacy Webside Manner Video Etiquette Consent Vital Signs
Technology in a SNF AV Cart for videoconferencing Tablets in patient rooms Patient meals at their doorways

Don’t do this!
Clean and Uncluttered 30
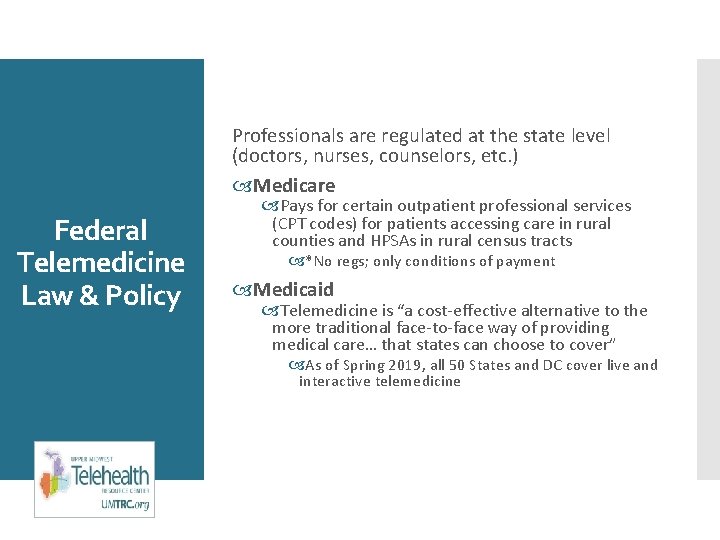
Professionals are regulated at the state level (doctors, nurses, counselors, etc. ) Medicare Federal Telemedicine Law & Policy Pays for certain outpatient professional services (CPT codes) for patients accessing care in rural counties and HPSAs in rural census tracts *No regs; only conditions of payment Medicaid Telemedicine is “a cost-effective alternative to the more traditional face-to-face way of providing medical care… that states can choose to cover” As of Spring 2019, all 50 States and DC cover live and interactive telemedicine
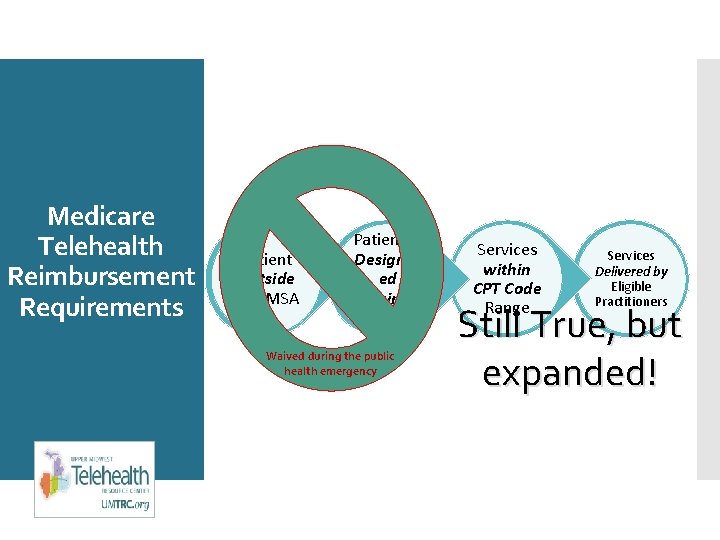
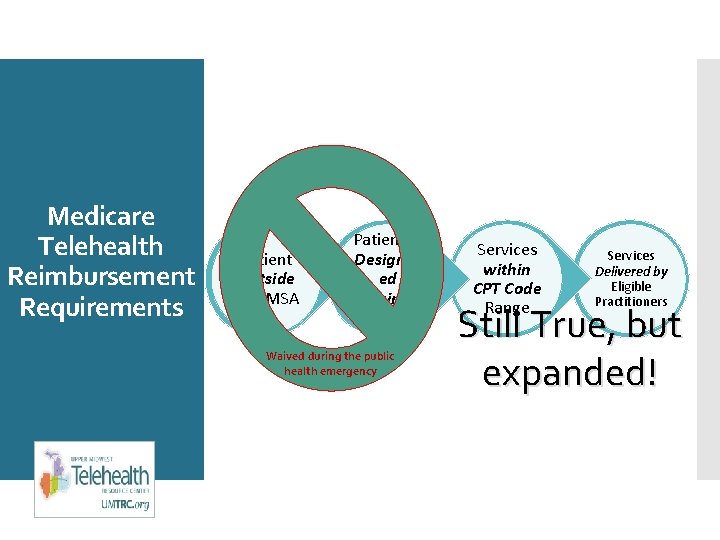
Medicare Telehealth Reimbursement Requirements Patient Outside of a MSA Patient in Designat ed Originati ng Site Waived during the public health emergency Services within CPT Code Range Services Delivered by Eligible Practitioners Still True, but expanded!
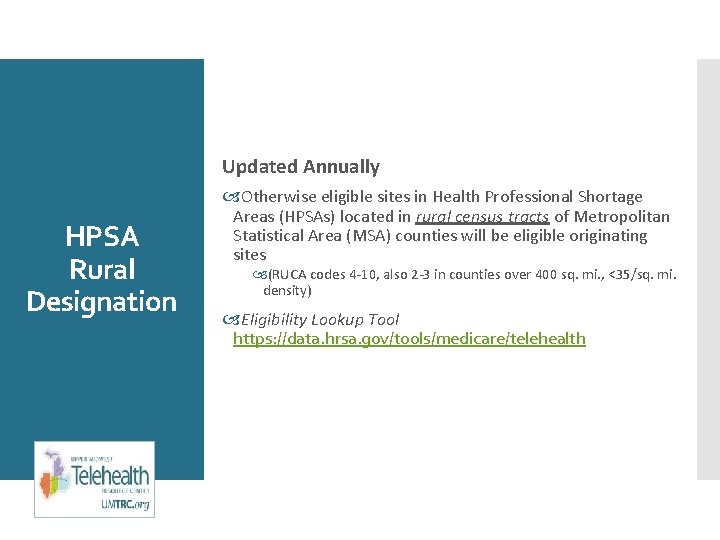
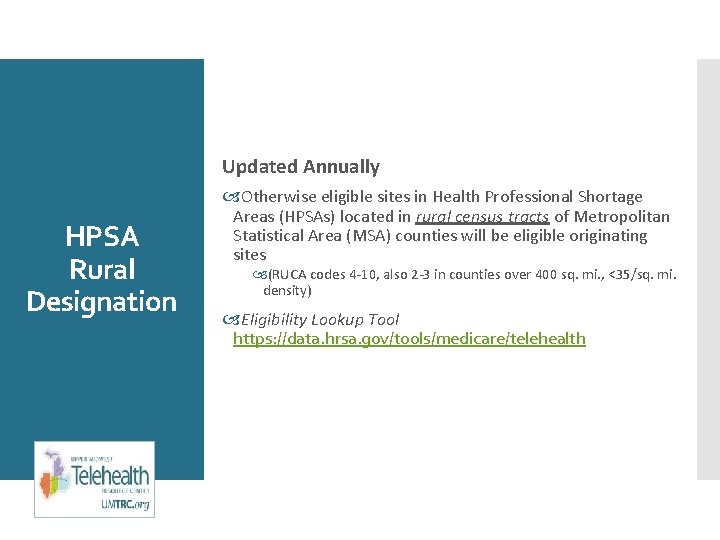
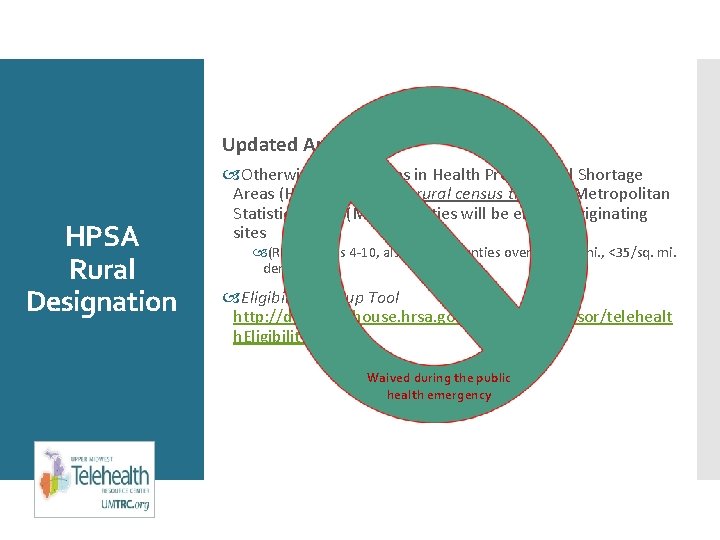
Updated Annually HPSA Rural Designation Otherwise eligible sites in Health Professional Shortage Areas (HPSAs) located in rural census tracts of Metropolitan Statistical Area (MSA) counties will be eligible originating sites (RUCA codes 4 -10, also 2 -3 in counties over 400 sq. mi. , <35/sq. mi. density) Eligibility Lookup Tool https: //data. hrsa. gov/tools/medicare/telehealth
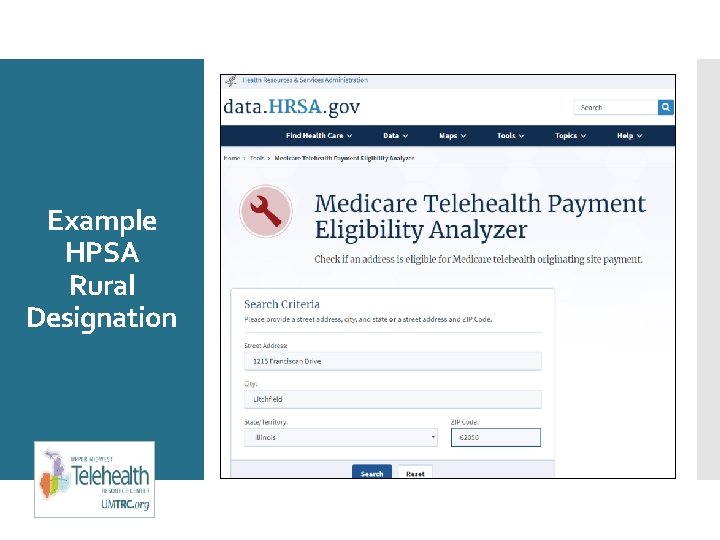
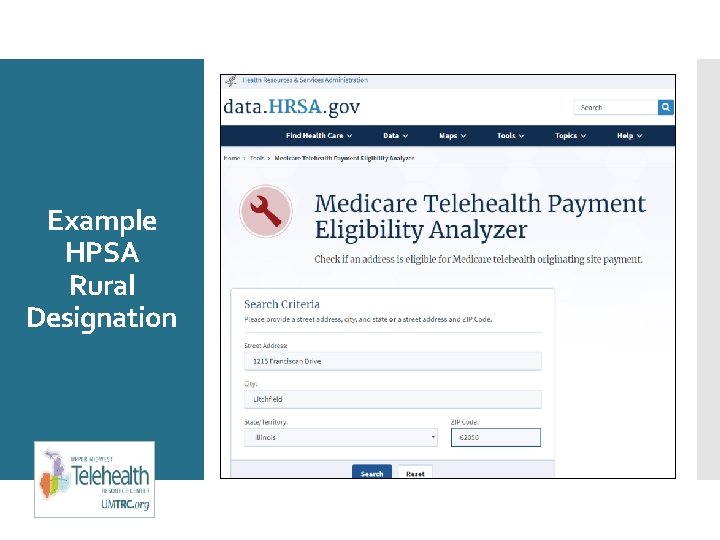
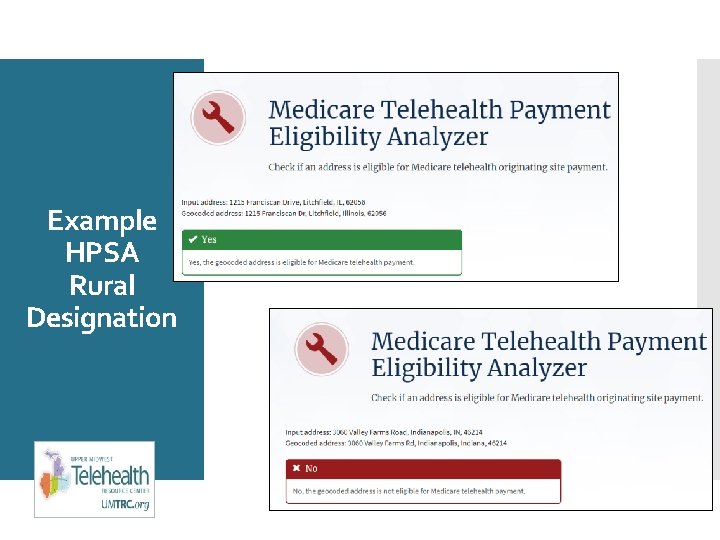
Example HPSA Rural Designation
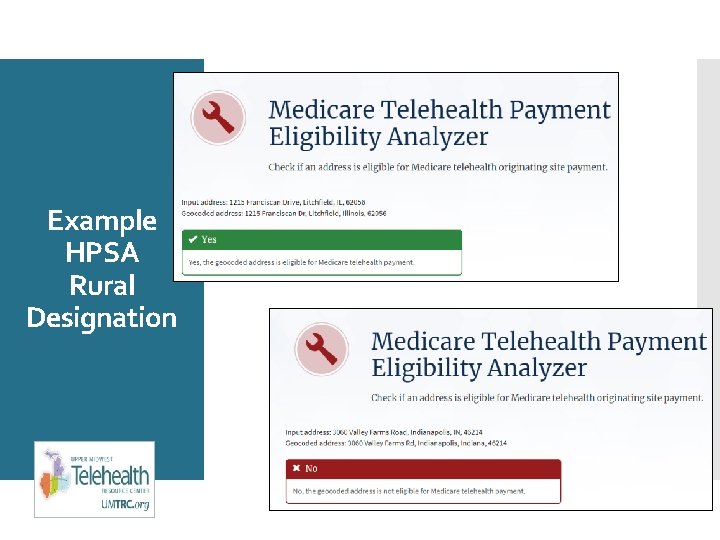
Example HPSA Rural Designation
Updated Annually HPSA Rural Designation Otherwise eligible sites in Health Professional Shortage Areas (HPSAs) located in rural census tracts of Metropolitan Statistical Area (MSA) counties will be eligible originating sites (RUCA codes 4 -10, also 2 -3 in counties over 400 sq. mi. , <35/sq. mi. density) Eligibility Lookup Tool http: //datawarehouse. hrsa. gov/telehealth. Advisor/telehealt h. Eligibility. aspx Waived during the public health emergency
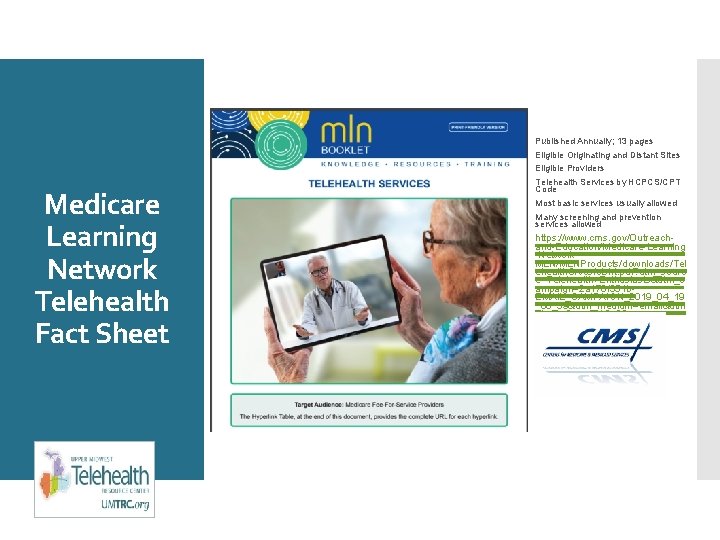
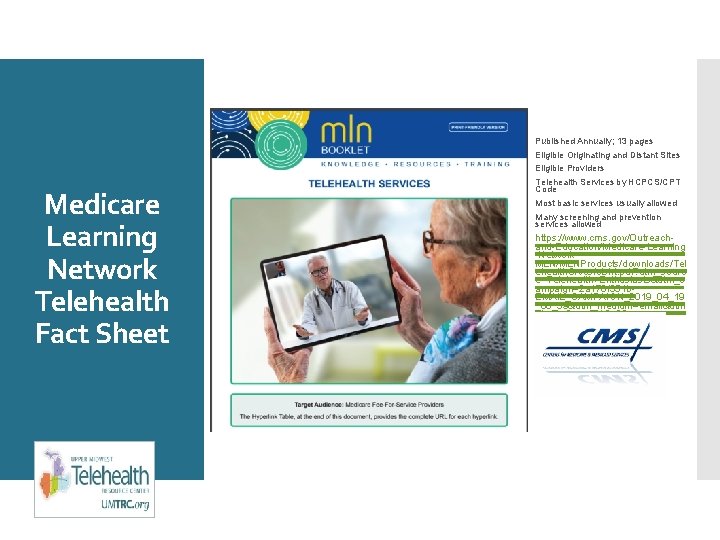
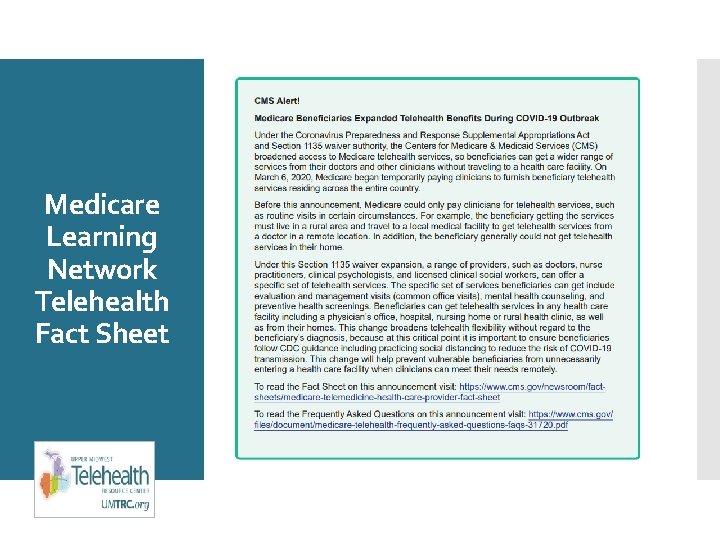
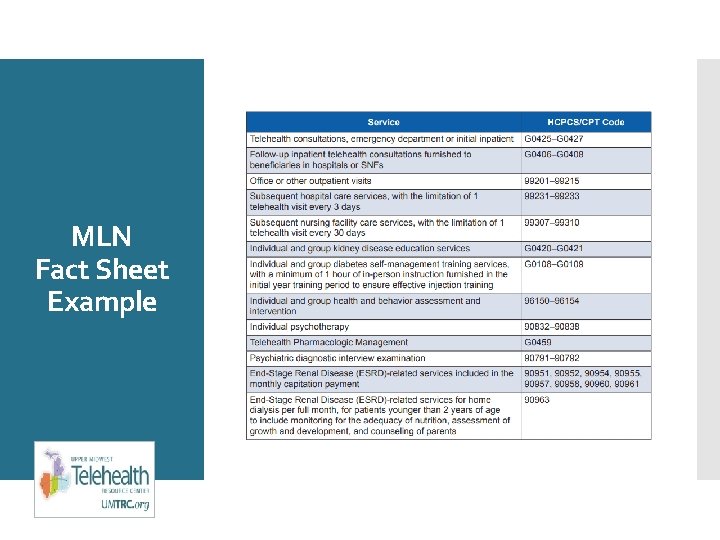
Published Annually; 13 pages Eligible Originating and Distant Sites Eligible Providers Medicare Learning Network Telehealth Fact Sheet Telehealth Services by HCPCS/CPT Code Most basic services usually allowed Many screening and prevention services allowed https: //www. cms. gov/Outreachand-Education/Medicare-Learning -Network. MLN/MLNProducts/downloads/Tel ehealth. Srvcsfctsht. pdf? utm_sourc e=Telehealth+Enthusiasts&utm_c ampaign=2 a 178 f 351 b. EMAIL_CAMPAIGN_2019_04_19 _08_59&utm_medium=email&utm _term=0_ae 00 b 0 e 89 a 2 a 178 f 351 b-353223937
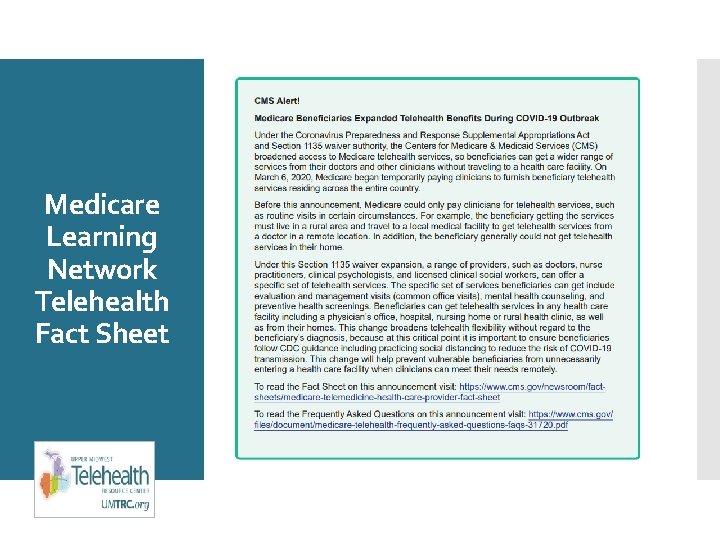
Medicare Learning Network Telehealth Fact Sheet
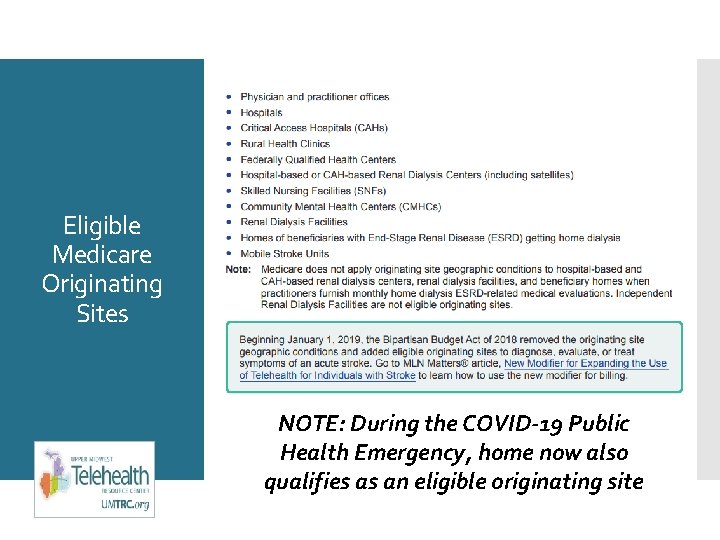
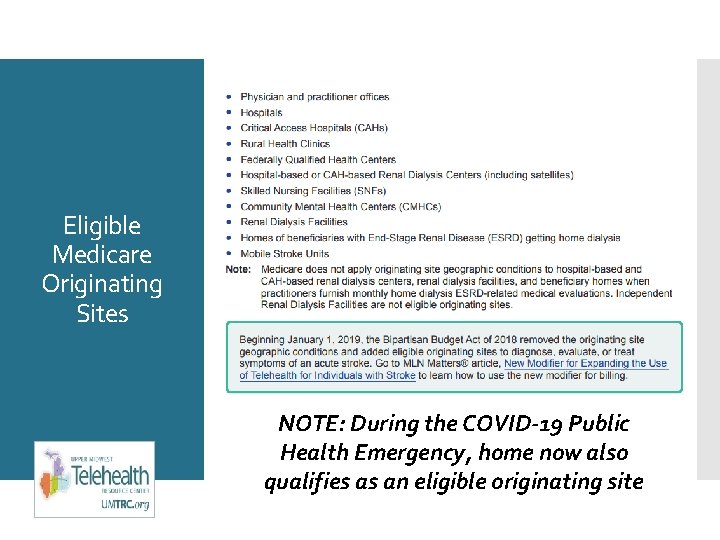
Eligible Medicare Originating Sites NOTE: During the COVID-19 Public Health Emergency, home now also qualifies as an eligible originating site

Distant Site Medicare Practitioners NOTE: During the COVID-19 Public Health Emergency, FQHCs (including lool-alikes) and RHCs can also serve as distant site providers
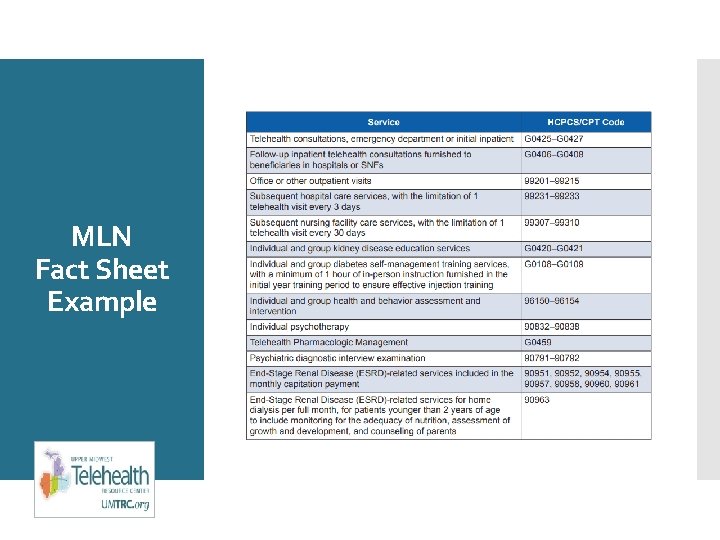
MLN Fact Sheet Example
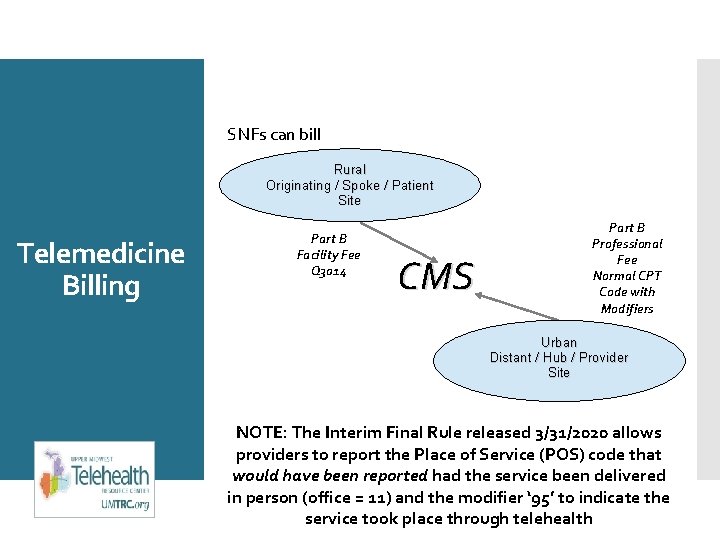
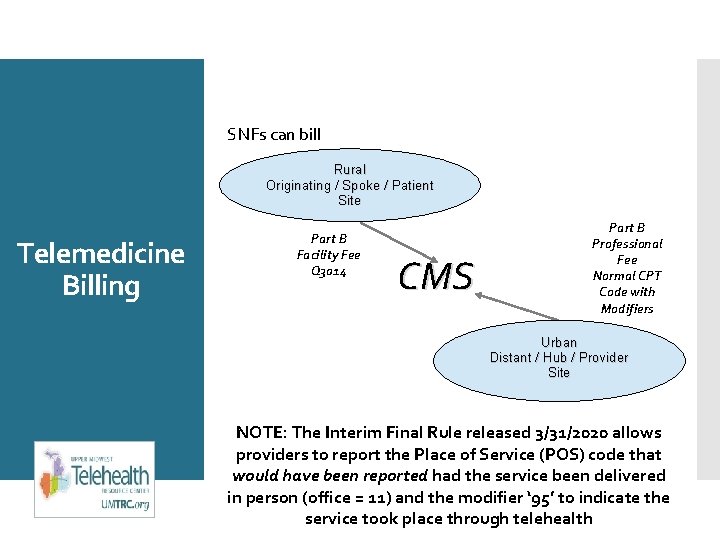
SNFs can bill Rural Originating / Spoke / Patient Site Telemedicine Billing Part B Facility Fee Q 3014 CMS Part B Professional Fee Normal CPT Code with Modifiers Urban Distant / Hub / Provider Site NOTE: The Interim Final Rule released 3/31/2020 allows providers to report the Place of Service (POS) code that would have been reported had the service been delivered in person (office = 11) and the modifier ‘ 95’ to indicate the service took place through telehealth
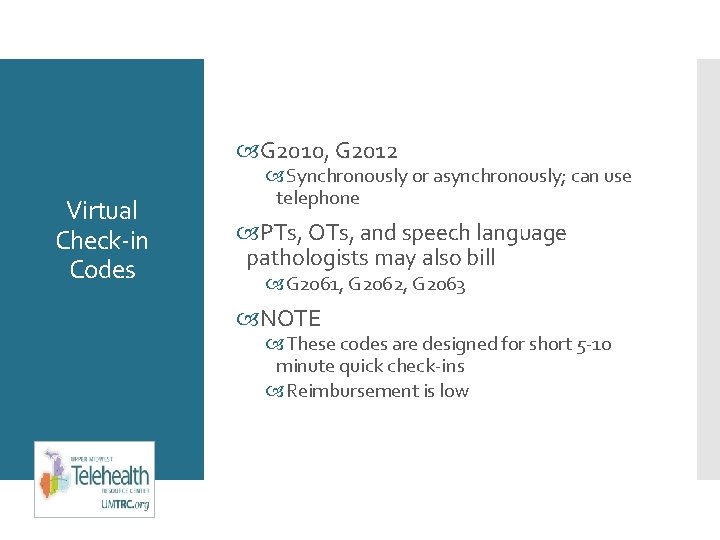
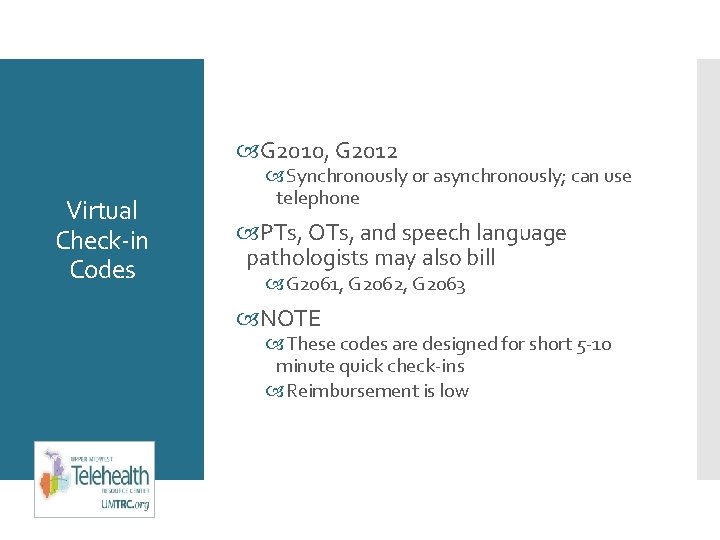
G 2010, G 2012 Virtual Check-in Codes Synchronously or asynchronously; can use telephone PTs, OTs, and speech language pathologists may also bill G 2061, G 2062, G 2063 NOTE These codes are designed for short 5 -10 minute quick check-ins Reimbursement is low
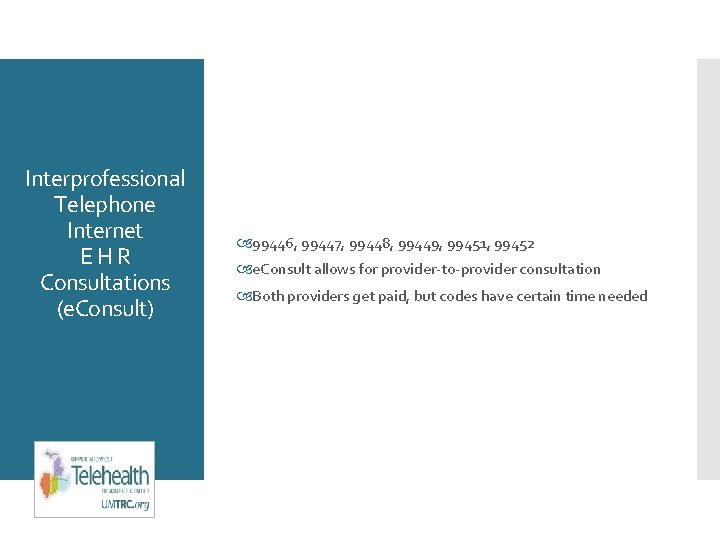
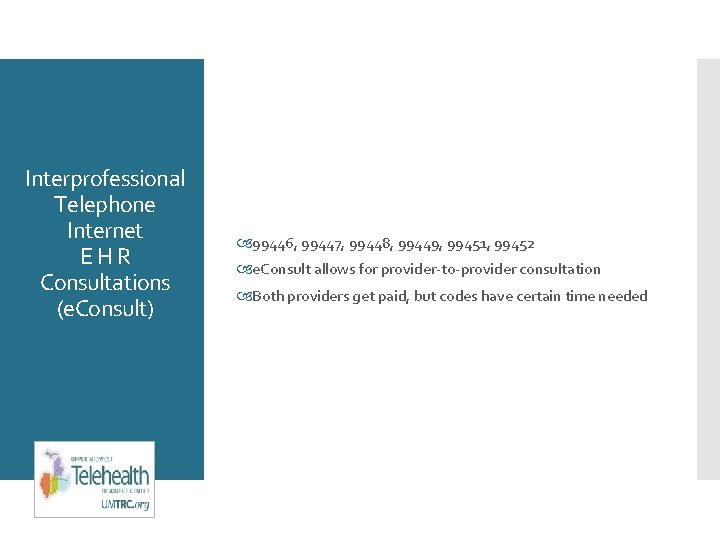
Interprofessional Telephone Internet EHR Consultations (e. Consult) 99446, 99447, 99448, 99449, 99451, 99452 e. Consult allows for provider-to-provider consultation Both providers get paid, but codes have certain time needed
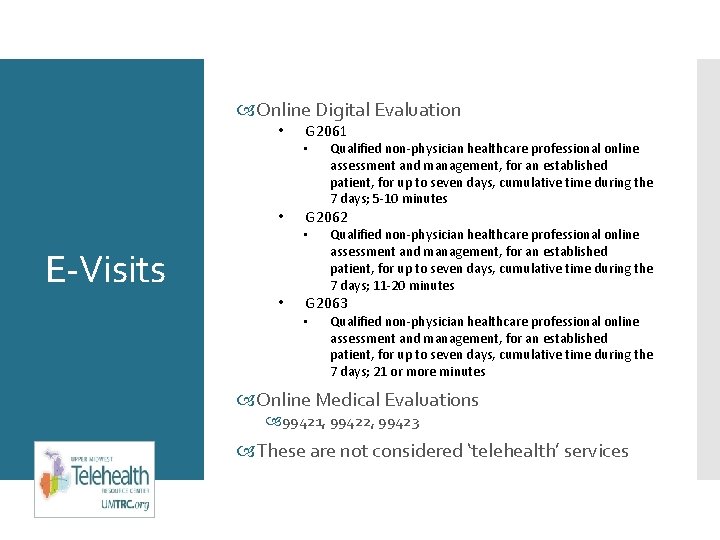
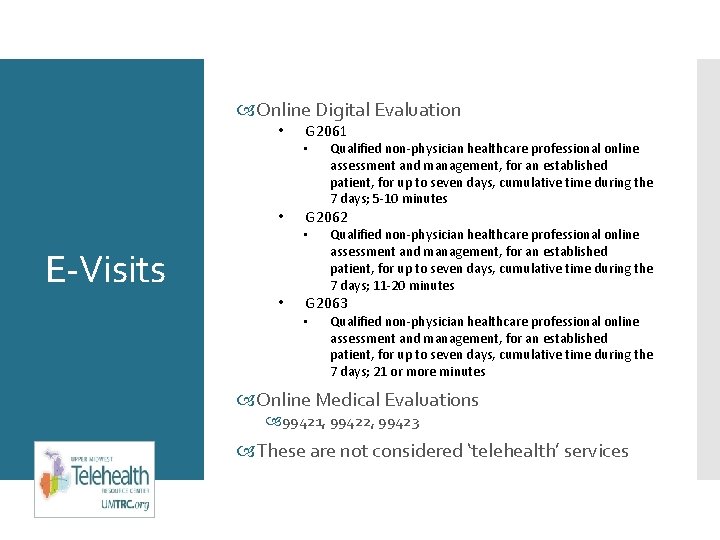
Online Digital Evaluation • G 2061 • • G 2062 • E-Visits • Qualified non-physician healthcare professional online assessment and management, for an established patient, for up to seven days, cumulative time during the 7 days; 5 -10 minutes Qualified non-physician healthcare professional online assessment and management, for an established patient, for up to seven days, cumulative time during the 7 days; 11 -20 minutes G 2063 • Qualified non-physician healthcare professional online assessment and management, for an established patient, for up to seven days, cumulative time during the 7 days; 21 or more minutes Online Medical Evaluations 99421, 99422, 99423 These are not considered ‘telehealth’ services
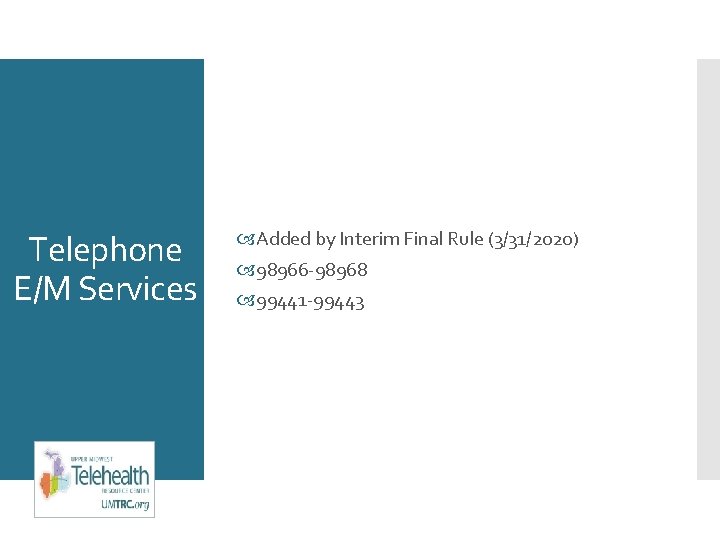
Telephone E/M Services Added by Interim Final Rule (3/31/2020) 98966 -98968 99441 -99443
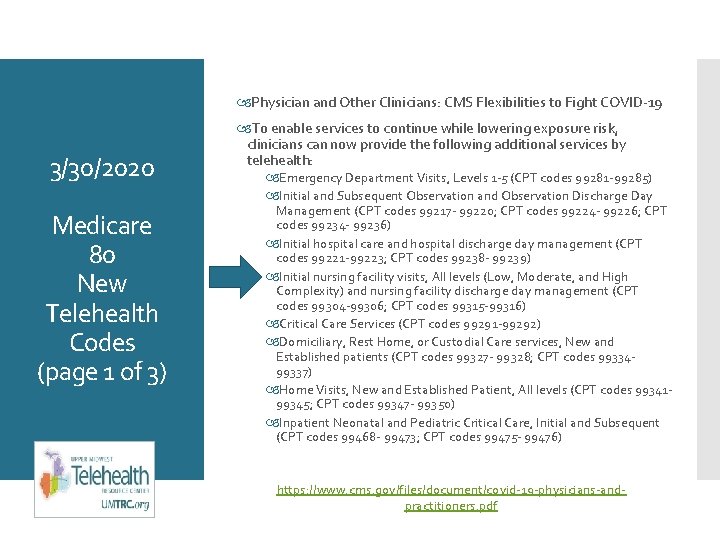
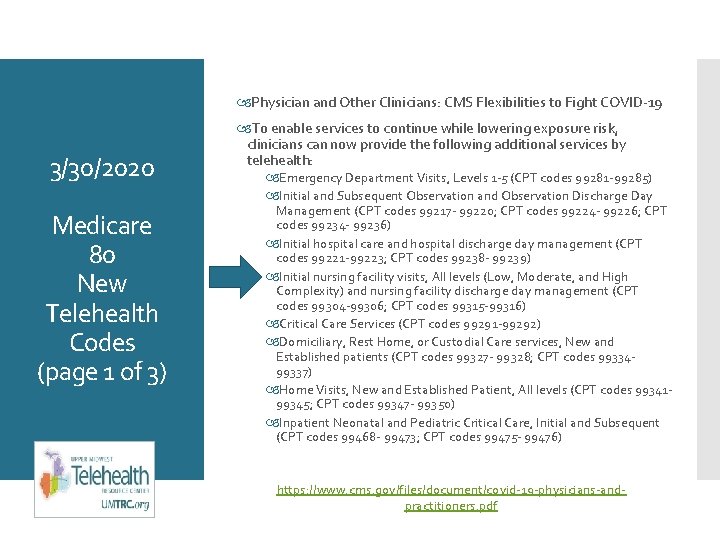
Physician and Other Clinicians: CMS Flexibilities to Fight COVID-19 3/30/2020 Medicare 80 New Telehealth Codes (page 1 of 3) To enable services to continue while lowering exposure risk, clinicians can now provide the following additional services by telehealth: Emergency Department Visits, Levels 1 -5 (CPT codes 99281 -99285) Initial and Subsequent Observation and Observation Discharge Day Management (CPT codes 99217 - 99220; CPT codes 99224 - 99226; CPT codes 99234 - 99236) Initial hospital care and hospital discharge day management (CPT codes 99221 -99223; CPT codes 99238 - 99239) Initial nursing facility visits, All levels (Low, Moderate, and High Complexity) and nursing facility discharge day management (CPT codes 99304 -99306; CPT codes 99315 -99316) Critical Care Services (CPT codes 99291 -99292) Domiciliary, Rest Home, or Custodial Care services, New and Established patients (CPT codes 99327 - 99328; CPT codes 9933499337) Home Visits, New and Established Patient, All levels (CPT codes 9934199345; CPT codes 99347 - 99350) Inpatient Neonatal and Pediatric Critical Care, Initial and Subsequent (CPT codes 99468 - 99473; CPT codes 99475 - 99476) https: //www. cms. gov/files/document/covid-19 -physicians-andpractitioners. pdf
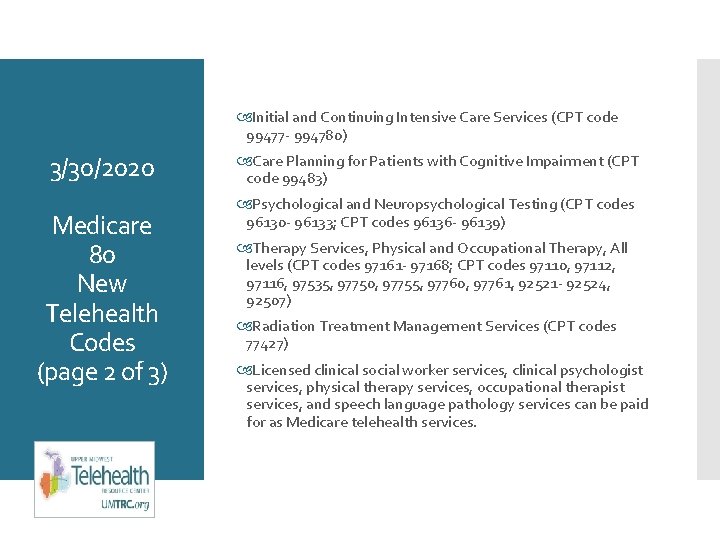
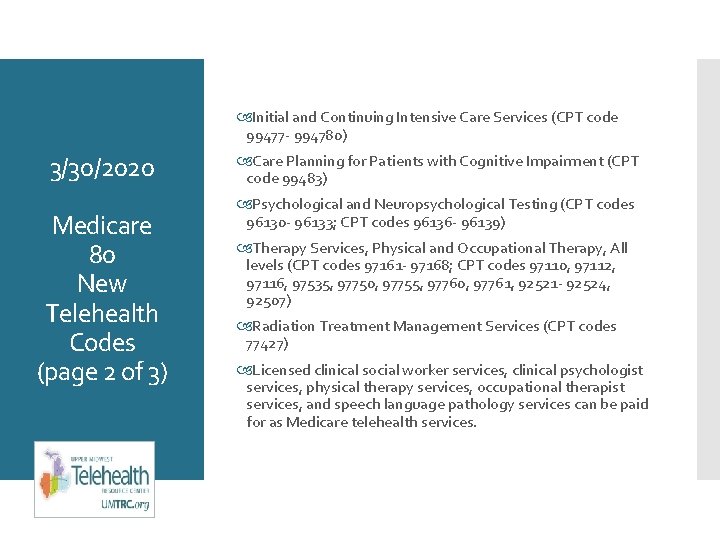
Initial and Continuing Intensive Care Services (CPT code 99477 - 994780) 3/30/2020 Medicare 80 New Telehealth Codes (page 2 of 3) Care Planning for Patients with Cognitive Impairment (CPT code 99483) Psychological and Neuropsychological Testing (CPT codes 96130 - 96133; CPT codes 96136 - 96139) Therapy Services, Physical and Occupational Therapy, All levels (CPT codes 97161 - 97168; CPT codes 97110, 97112, 97116, 97535, 97750, 97755, 97760, 97761, 92521 - 92524, 92507) Radiation Treatment Management Services (CPT codes 77427) Licensed clinical social worker services, clinical psychologist services, physical therapy services, occupational therapist services, and speech language pathology services can be paid for as Medicare telehealth services.
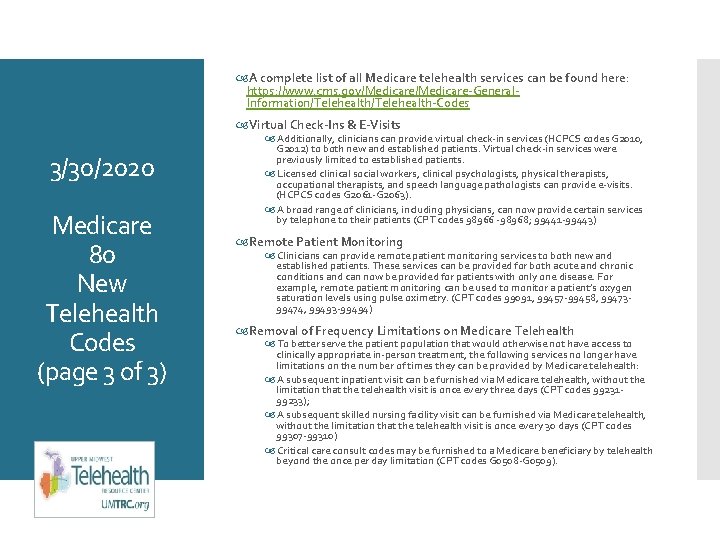
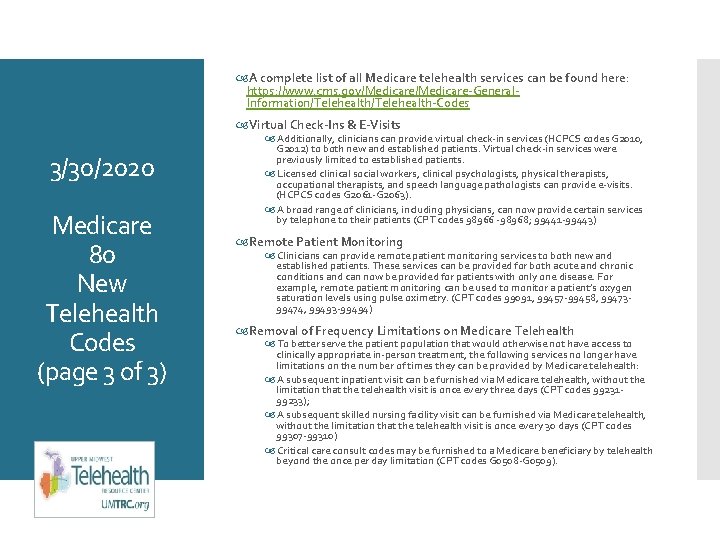
A complete list of all Medicare telehealth services can be found here: https: //www. cms. gov/Medicare-General. Information/Telehealth-Codes Virtual Check-Ins & E-Visits 3/30/2020 Medicare 80 New Telehealth Codes (page 3 of 3) Additionally, clinicians can provide virtual check-in services (HCPCS codes G 2010, G 2012) to both new and established patients. Virtual check-in services were previously limited to established patients. Licensed clinical social workers, clinical psychologists, physical therapists, occupational therapists, and speech language pathologists can provide e-visits. (HCPCS codes G 2061 -G 2063). A broad range of clinicians, including physicians, can now provide certain services by telephone to their patients (CPT codes 98966 -98968; 99441 -99443) Remote Patient Monitoring Clinicians can provide remote patient monitoring services to both new and established patients. These services can be provided for both acute and chronic conditions and can now be provided for patients with only one disease. For example, remote patient monitoring can be used to monitor a patient’s oxygen saturation levels using pulse oximetry. (CPT codes 99091, 99457 -99458, 9947399474, 99493 -99494) Removal of Frequency Limitations on Medicare Telehealth To better serve the patient population that would otherwise not have access to clinically appropriate in-person treatment, the following services no longer have limitations on the number of times they can be provided by Medicare telehealth: A subsequent inpatient visit can be furnished via Medicare telehealth, without the limitation that the telehealth visit is once every three days (CPT codes 9923199233); A subsequent skilled nursing facility visit can be furnished via Medicare telehealth, without the limitation that the telehealth visit is once every 30 days (CPT codes 99307 -99310) Critical care consult codes may be furnished to a Medicare beneficiary by telehealth beyond the once per day limitation (CPT codes G 0508 -G 0509).
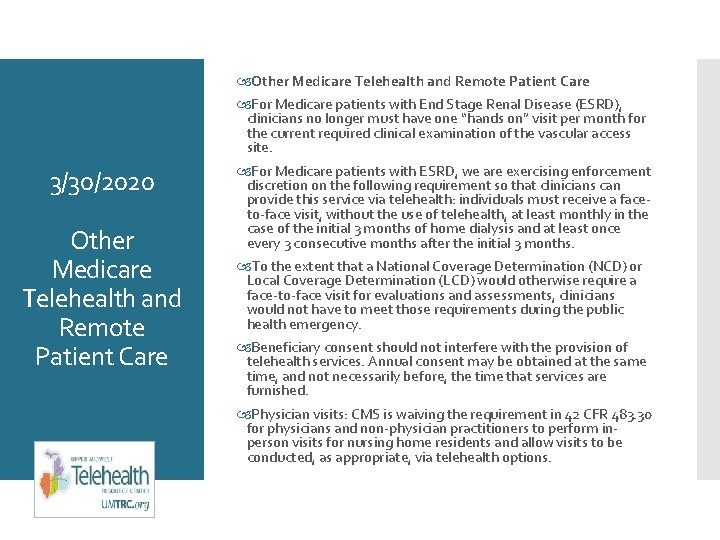
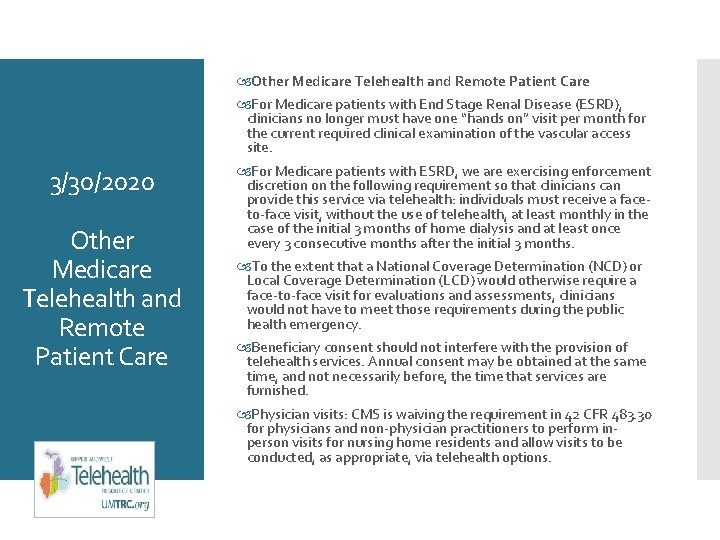
Other Medicare Telehealth and Remote Patient Care For Medicare patients with End Stage Renal Disease (ESRD), clinicians no longer must have one “hands on” visit per month for the current required clinical examination of the vascular access site. 3/30/2020 Other Medicare Telehealth and Remote Patient Care For Medicare patients with ESRD, we are exercising enforcement discretion on the following requirement so that clinicians can provide this service via telehealth: individuals must receive a faceto-face visit, without the use of telehealth, at least monthly in the case of the initial 3 months of home dialysis and at least once every 3 consecutive months after the initial 3 months. To the extent that a National Coverage Determination (NCD) or Local Coverage Determination (LCD) would otherwise require a face-to-face visit for evaluations and assessments, clinicians would not have to meet those requirements during the public health emergency. Beneficiary consent should not interfere with the provision of telehealth services. Annual consent may be obtained at the same time, and not necessarily before, the time that services are furnished. Physician visits: CMS is waiving the requirement in 42 CFR 483. 30 for physicians and non-physician practitioners to perform inperson visits for nursing home residents and allow visits to be conducted, as appropriate, via telehealth options.
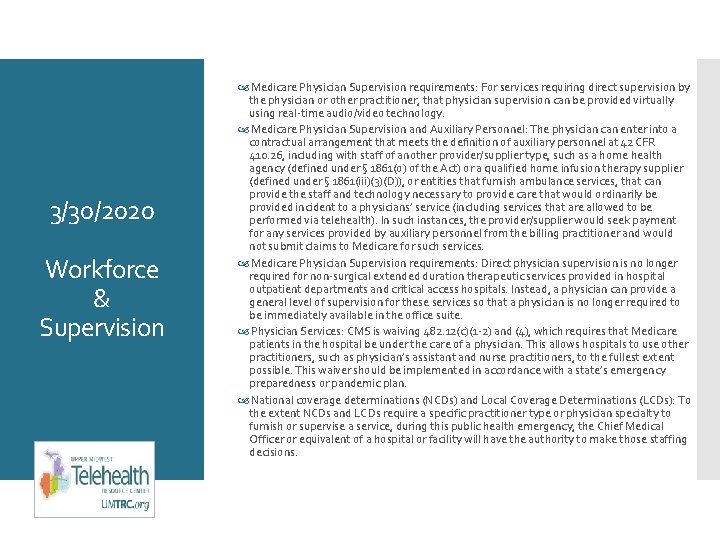
3/30/2020 Workforce & Supervision Medicare Physician Supervision requirements: For services requiring direct supervision by the physician or other practitioner, that physician supervision can be provided virtually using real-time audio/video technology. Medicare Physician Supervision and Auxiliary Personnel: The physician can enter into a contractual arrangement that meets the definition of auxiliary personnel at 42 CFR 410. 26, including with staff of another provider/supplier type, such as a home health agency (defined under § 1861(o) of the Act) or a qualified home infusion therapy supplier (defined under § 1861(iii)(3)(D)), or entities that furnish ambulance services, that can provide the staff and technology necessary to provide care that would ordinarily be provided incident to a physicians’ service (including services that are allowed to be performed via telehealth). In such instances, the provider/supplier would seek payment for any services provided by auxiliary personnel from the billing practitioner and would not submit claims to Medicare for such services. Medicare Physician Supervision requirements: Direct physician supervision is no longer required for non-surgical extended duration therapeutic services provided in hospital outpatient departments and critical access hospitals. Instead, a physician can provide a general level of supervision for these services so that a physician is no longer required to be immediately available in the office suite. Physician Services: CMS is waiving 482. 12(c)(1 -2) and (4), which requires that Medicare patients in the hospital be under the care of a physician. This allows hospitals to use other practitioners, such as physician’s assistant and nurse practitioners, to the fullest extent possible. This waiver should be implemented in accordance with a state’s emergency preparedness or pandemic plan. National coverage determinations (NCDs) and Local Coverage Determinations (LCDs): To the extent NCDs and LCDs require a specific practitioner type or physician specialty to furnish or supervise a service, during this public health emergency, the Chief Medical Officer or equivalent of a hospital or facility will have the authority to make those staffing decisions.
Practitioner Locations: 3/30/2020 Workforce & Supervision Temporarily waive Medicare and Medicaid’s requirements that physicians and non-physician practitioners be licensed in the state where they are providing services. State requirements will still apply. CMS waives the Medicare requirement that a physician or non-physician practitioner must be licensed in the State in which s/he is practicing for individuals for whom the following four conditions are met: 1) must be enrolled as such in the Medicare program, 2) must possess a valid license to practice in the State which relates to his or her Medicare enrollment, 3) is furnishing services – whether in person or via telehealth – in a State in which the emergency is occurring in order to contribute to relief efforts in his or her professional capacity, and 4) is not affirmatively excluded from practice in the State or any other State that is part of the 1135 emergency area. A physician or non-physician practitioner may seek an 1135 -based licensure waiver from CMS by contacting the provider enrollment hotline for the Medicare Administrative Contractor that services their geographic area. This waiver does not have the effect of waiving State or local licensure requirements or any requirement specified by the State or a local government as a condition for waiving its licensure requirements Provider Enrollment: CMS has established toll-free hotlines for physicians, non-physician practitioners and Part A certified providers and suppliers establishing isolation facilities to enroll and receive temporary Medicare billing privileges. CMS is providing the following flexibilities for provider enrollment: Waive certain screening requirements. Postpone all revalidation actions. Allow licensed physicians and other practitioners to bill Medicare for services provided outside of their state of enrollment. Expedite any pending or new applications from providers. Allow practitioners to render telehealth services from their home without reporting their home address on their Medicare enrollment while continuing to bill from your currently enrolled location. Allow opted-out practitioners to terminate their opt-out status early and enroll in Medicare to provide care to more patients.
Stark Law Waivers 3/30/2020 Patients over Paperwork National Coverage Determinations and Local Coverage Determinations on Respiratory Related Devised, Oxygen and Oxygen Equipment, Home Infusion Pumps and Home Anticoagulation Therapy Signature Requirements Changes to MIPS Accelerated/Advance Payments Additional Guidance The Interim Final Rule and waivers can be found at: https: //www. cms. gov/about-cms/emergencypreparednessresponse-operations/current-emergencies/coronavirus-waivers CMS has released guidance to providers related to relaxed reporting requirements for quality reporting programs at: https: //www. cms. gov/newsroom/press-releases/cms-announcesreliefclinicians-providers-hospitals-and-facilities-participatingquality-reporting
COVID-19 https: //www. umtrc. org/resources/covid-19/
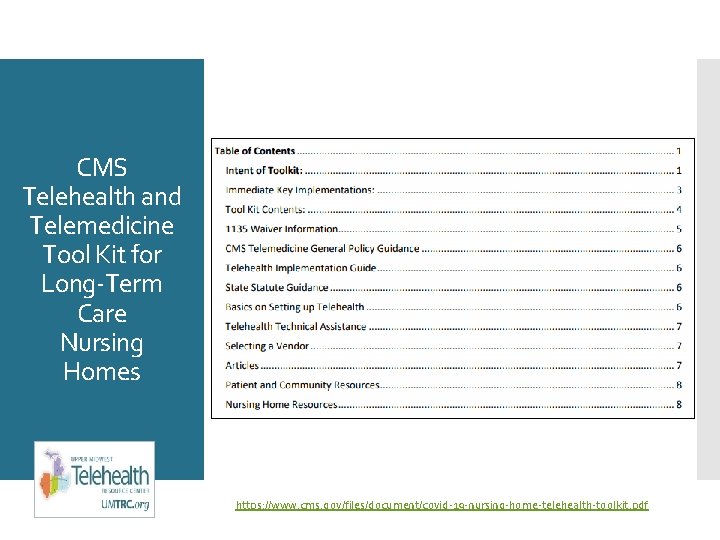
CMS Telehealth and Telemedicine Tool Kit for Long-Term Care Nursing Homes https: //www. cms. gov/files/document/covid-19 -nursing-home-telehealth-toolkit. pdf
Implementing Telehealth in post-acute and long-term care settings https: //www. westhealth. org/wp-content/uploads/2019/04/Tele. Health_Guide_v. 9_PAGES_WEB. pdf
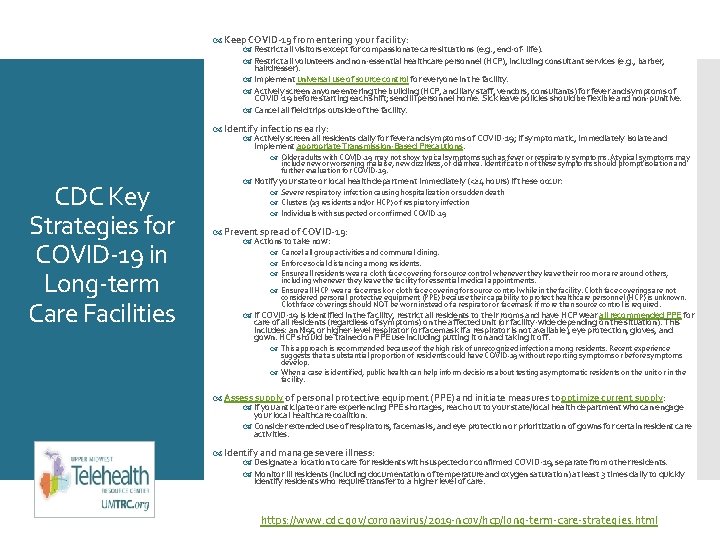
Keep COVID-19 from entering your facility: Restrict all visitors except for compassionate care situations (e. g. , end-of- life). Restrict all volunteers and non-essential healthcare personnel (HCP), including consultant services (e. g. , barber, hairdresser). Implement universal use of source control for everyone in the facility. Actively screen anyone entering the building (HCP, ancillary staff, vendors, consultants) for fever and symptoms of COVID-19 before starting each shift; send ill personnel home. Sick leave policies should be flexible and non-punitive. Cancel all field trips outside of the facility. Identify infections early: Actively screen all residents daily for fever and symptoms of COVID-19; if symptomatic, immediately isolate and implement appropriate Transmission-Based Precautions. Older adults with COVID-19 may not show typical symptoms such as fever or respiratory symptoms. Atypical symptoms may include new or worsening malaise, new dizziness, or diarrhea. Identification of these symptoms should prompt isolation and further evaluation for COVID-19. CDC Key Strategies for COVID-19 in Long-term Care Facilities Notify your state or local health department immediately (<24 hours) if these occur: Severe respiratory infection causing hospitalization or sudden death Clusters (≥ 3 residents and/or HCP) of respiratory infection Individuals with suspected or confirmed COVID-19 Prevent spread of COVID-19: Actions to take now: Cancel all group activities and communal dining. Enforce social distancing among residents. Ensure all residents wear a cloth face covering for source control whenever they leave their room or are around others, including whenever they leave the facility for essential medical appointments. Ensure all HCP wear a facemask or cloth face covering for source control while in the facility. Cloth face coverings are not considered personal protective equipment (PPE) because their capability to protect healthcare personnel (HCP) is unknown. Cloth face coverings should NOT be worn instead of a respirator or facemask if more than source control is required. If COVID-19 is identified in the facility, restrict all residents to their rooms and have HCP wear all recommended PPE for care of all residents (regardless of symptoms) on the affected unit (or facility-wide depending on the situation). This includes: an N 95 or higher-level respirator (or facemask if a respirator is not available), eye protection, gloves, and gown. HCP should be trained on PPE use including putting it on and taking it off. This approach is recommended because of the high risk of unrecognized infection among residents. Recent experience suggests that a substantial proportion of residents could have COVID-19 without reporting symptoms or before symptoms develop. When a case is identified, public health can help inform decisions about testing asymptomatic residents on the unit or in the facility. Assess supply of personal protective equipment (PPE) and initiate measures to optimize current supply: If you anticipate or are experiencing PPE shortages, reach out to your state/local health department who can engage your local healthcare coalition. Consider extended use of respirators, facemasks, and eye protection or prioritization of gowns for certain resident care activities. Identify and manage severe illness: Designate a location to care for residents with suspected or confirmed COVID-19, separate from other residents. Monitor ill residents (including documentation of temperature and oxygen saturation) at least 3 times daily to quickly identify residents who require transfer to a higher level of care. https: //www. cdc. gov/coronavirus/2019 -ncov/hcp/long-term-care-strategies. html
UMTRC Website Facebook Linked. In
CCHP COVID-19 Resources https: //www. cchpca. org/resources/covid-19 -telehealth-coverage-policies
Thank You! Becky Sanders bsanders@indianarha. org
Questions? • To submit questions or comments: • Use the chat box 61
Polling Question What additional resources do you need most right now? Ø Policies/Waivers Ø Activity Ideas for Residents during COVID-19 Ø Surveillance Tools/NHSN Enrollment Assistance Ø Infection Control Education and Training Ø Resident Transfer Resources 62
Q Tips Podcasts for Nursing Homes Get great tips from Qsource as part of our QTips Podcast series. Available each week and sent directly to your email in-box. Podcast 1 | Qsource Assistance Overview URL: https: //bit. ly/2 UV 6 x 2 S Podcast 2 | Dining Assistant Waiver URL: https: //bit. ly/2 wn. F 1 Bq Podcast 3 | Temporary Blanket Waivers for Resident Care Facilities URL: https: //bit. ly/2 Vn. Bcot 63
Q Tips Podcasts for Nursing Homes Get great tips from Qsource as part of our QTips Podcast series. Available each week and sent directly to your email in-box. Podcast 4 | Voluntary Resident Leave of Absence During COVID-19 URL: https: //bit. ly/3 c 9 g. Qp. A Podcast 5 | Caring for Residents and Families Mental Health URL: https: //bit. ly/2 Rzneyt Podcast 6 | MDS and Case Management in the midst of COVID-19 URL: https: //bit. ly/3 a 3 p. Paj 64
Resources Available Resource. Hub. Exchange is our online warehouse of tools, resources, podcast and webinars. 65 New resource to help conduct virtual meetings. Available on Resource. Hub. Exchange.
Hero Stories We want to hear stories of Nursing Home Heroes! Whether a staff member, family member or resident, share with us the stories of those making a difference during this pandemic. From making masks and homemade soap to social distancing bingo and virtual family meetings, tell us how the everyday heroes are impacting you, your residents and the care provided. We will then compile them and share on social media, blogs and e-News to inspire and encourage others during this difficult time. Email your stories to Mitzi Daffron at mdaffron@qsource. org 66
Thank you for joining us! Please complete the survey that will come up as you exit the webinar – we value your feedback in developing future events! Please visit us at www. Qsource. org/qio 67

Connect with Us Reminders Facebook Twitter Linked. In www. facebook. com/Q source. Live. Well www. twitter. com/Qsou rce www. linkedin. com/in/q source-healthcareconsultants This presentation was prepared by Qsource, the Medicare Quality Innovation Network. Quality Improvement Organization (QIN-QIO) for Indiana under a contract with the Centers for Medicare & Medicaid Services (CMS), a federal agency of the U. S. Department of Health 68 and Human Services. Content does not necessarily reflect CMS policy. 20. QIO 3. 04. 020 68
 Livanta qio case lookup
Livanta qio case lookup How to win a medicare appeal for skilled nursing
How to win a medicare appeal for skilled nursing Skilled nursing facility value based purchasing program
Skilled nursing facility value based purchasing program Http//apps.tujuhbukit.com/covid19
Http//apps.tujuhbukit.com/covid19 Do if you covid19
Do if you covid19 Covid19 athome rapid what know
Covid19 athome rapid what know What do if test positive covid19
What do if test positive covid19 Vaksin covid19
Vaksin covid19 Twu fafsa deadline
Twu fafsa deadline Michael schwartz center kent state
Michael schwartz center kent state Csudh fafsa deadline
Csudh fafsa deadline Instructor office hours
Instructor office hours Nonfiction cause and effect
Nonfiction cause and effect Critical thinking in society
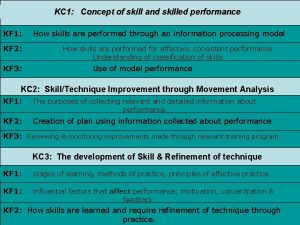
Critical thinking in society 4 characteristics of a skilled performance
4 characteristics of a skilled performance Which post holds up the greater part of the load?
Which post holds up the greater part of the load? Skilled staffing jean
Skilled staffing jean Conclusion of unemployment
Conclusion of unemployment Skilled performance
Skilled performance Characteristics of skilled performance
Characteristics of skilled performance Skilled trades 1201
Skilled trades 1201 Define skilled human resources
Define skilled human resources Operationally attuned
Operationally attuned Sanitary facilities and equipment
Sanitary facilities and equipment Factory office plan
Factory office plan Nursing care delivery models
Nursing care delivery models Public area cleaning equipment
Public area cleaning equipment Purchasing, receiving, storing and issuing
Purchasing, receiving, storing and issuing Hotel classifications
Hotel classifications Facilities and environmental conditions
Facilities and environmental conditions Design options for a distribution network
Design options for a distribution network Sanitary facilities and equipment
Sanitary facilities and equipment Material handling and facilities planning
Material handling and facilities planning Providing support services facilities and other amenities
Providing support services facilities and other amenities Translators and facilities of languages
Translators and facilities of languages Safe facilities and pest management
Safe facilities and pest management Ocd ncp
Ocd ncp Cataract surgery nursing diagnosis
Cataract surgery nursing diagnosis Nursing interventions for neonatal abstinence syndrome
Nursing interventions for neonatal abstinence syndrome Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Cdm welfare facilities
Cdm welfare facilities Shore reception facilities
Shore reception facilities Shopping facilities
Shopping facilities Expansion time variable is declared as
Expansion time variable is declared as Lockheed martin atlanta
Lockheed martin atlanta Article 7 behavioral health residential facilities
Article 7 behavioral health residential facilities Glp
Glp Flowood restitution center
Flowood restitution center Fairfax county public facilities manual
Fairfax county public facilities manual Facility design process
Facility design process Examples of facilities
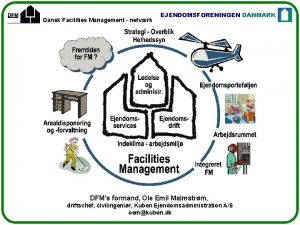
Examples of facilities Facility management history and evolution
Facility management history and evolution Facilities business continuity plan
Facilities business continuity plan Conversation in hotel reservation
Conversation in hotel reservation Gigp 30
Gigp 30 Supporting facility
Supporting facility Framework for structuring drivers
Framework for structuring drivers Johnson's rule
Johnson's rule Vinci facilities maximo
Vinci facilities maximo Define facility planning
Define facility planning Esi hospital kk nagar chennai address
Esi hospital kk nagar chennai address Dansk facilities management
Dansk facilities management Supporting facility
Supporting facility Ada fitness center
Ada fitness center Lesson 2 healthcare facilities
Lesson 2 healthcare facilities Site plan and layout plan
Site plan and layout plan Oom
Oom Une student id
Une student id Reject allowance problem facilities planning
Reject allowance problem facilities planning