MEDICARE AND SKILLED NURSING FACILITIES JIMMO AND APPEALS



- Slides: 70
MEDICARE AND SKILLED NURSING FACILITIES: JIMMO AND APPEALS CONSUMER VOICE Toby S. Edelman Senior Policy Attorney CENTER FOR MEDICARE ADVOCACY November 3, 2015 www. medicareadvocacy. orgwww. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc.
INTRODUCTION § This session is about Medicare coverage of care in a skilled nursing facility (SNF). • Medicare coverage rules • An obstacle: the myth of improvement • Jimmo, ending the myth of “medical improvement” • Medicare appeals www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 2
MEDICARE RESOURCES § Medicare statute, 42 U. S. C. § 1395 § Medicare regulations, 42 C. F. R. Part 409 § Medicare Benefit Policy Manual (MBPM), CMS Pub. 100 -02, Chapter 8, http: //www. cms. hhs. gov/manuals/Downloa ds/bp 102 c 08. pdf www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 3
MEDICARE COVERAGE OF SNFs UNDER PART A § Basic Requirements • • • 3 -day qualifying hospital stay, 42 C. F. R. § 409. 30 Admission within 30 days of hospital discharge Physician certification of beneficiary’s need for SNF care Beneficiary’s requiring daily skilled nursing or daily rehabilitation services Medicare-certified facility; Medicare-certified bed Practical matter: inpatient care needed, 42 C. F. R. § 409. 32 www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 4
MEDICARE COVERAGE OF SNFs UNDER PART A (cont’d) § Care must be reasonable and necessary, 42 U. S. C. § 1395 y(a)(1)(A). § Care must require the skills of technical or professional personnel, such as registered nurses, physical therapists, occupational therapists, and speech pathologists, 42 C. F. R. § 409. 31. § Care must be provided daily, 42 C. F. R. § 409. 34. • Nursing 7 days a week, or • Rehabilitation 5 days a week, or • Combination of nursing and rehabilitation 7 days a week, or • Some per se (automatic) coverage (e. g. , feeding tubes; extensive decubitus ulcers [Manual says stage 3 or worse]), MBPM, Ch. 8, § 30. 3. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 5
MEDICARE COVERAGE OF SNFs UNDER PART A (cont’d) § Up to 100 days in a benefit period (but often, SNFs stop coverage on day 21, when large copayment [$161/day in 2016] begins). § Part A provides all-inclusive coverage (room and board, nursing care, medications, therapy, etc. ). § Medicare Advantage plans also provide all- inclusive coverage, but may have different costsharing obligations. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 6

MEDICARE COVERAGE OF THERAPY IN SNFs UNDER PART B § A Medicare beneficiary who is NOT IN A PART A STAY may qualify for therapy under Part B. • Called outpatient therapy. • No limit on the number of available days, but • subject to therapy caps. May be appropriate for resident who needs therapy fewer than 5 days/week. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 7
PART B THERAPY CAPS § Balanced Budget Act of 1997 imposed caps on outpatient therapy • • $1920 cap for physical therapy and speech therapy (combined) $1920 cap for occupational therapy § Deficit Reduction Act of 2005 created exceptions process (to get therapy above caps) § Automatic exceptions when therapists attest therapy is reasonable and necessary § Beginning 2012, Medicare Contractors conduct mandatory medical review for therapy over $3700 www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 8
PART B THERAPY CAPS (cont’d) § H. R. 2, Medicare Access and CHIP Reauthorization Act (Pub. L. 114 -10, signed by President Obama on April 16, 2015) • Extends the exceptions process until Jan. 2018. • Senator Ben Cardin’s (D, MD) amendment to repeal and replace the exceptions process (with prior authorization process) was defeated. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 9
IDENTICAL STANDARD FOR THERAPY UNDER PARTS A AND B § Therapy is covered if it must be provided by a professional therapist and is necessary to improve or (maintenance standard) to maintain a resident’s functioning or prevent or slow decline or deterioration. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 10
RESTORATION POTENTIAL § Restoration potential of resident is not the deciding factor in determining whether skilled services are needed. 42 C. F. R. § 409. 32(c) • • Statute refers to improvement only as to “malformed body member, ” 42 U. S. C. § 1395 y(a)(1)(A). Coverage must be … “reasonable and necessary for diagnosis, treatment, or rehabilitation of illness or injury or to improve a malformed body member. ” www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 11
MEDICARE MYTHS § Medicare coverage is not available unless the beneficiary shows continued improvement. § Medicare will not cover physical therapy if it is “only maintenance. ” § Medicare coverage is not available if patient has “plateaued. ” § Medicare will not cover care for people with certain diagnoses, chronic conditions (i. e. , they won’t get better). www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 12
MEDICARE TRUTHS § Individualized assessment required. § Restoration potential is not the deciding factor. § Medicare should not be denied because the beneficiary has a chronic condition or needs services to maintain his/her condition. § Rather ask: • • Are the Medicare coverage criteria met? Is the care medically necessary and must it be provided by/under supervision of skilled personnel? www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 13
THE MYTH OF IMPROVEMENT § Pervasive belief among health care professionals, providers, Medicare reviewers, and contractors that Medicare pays only if beneficiary is expected to improve. § Not true and has never been true. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 14
THE MYTH OF IMPROVEMENT § Restoration potential is not a valid reason for denial of coverage. • “Even if full recovery or medical improvement is not possible, a resident may need skilled services to prevent further deterioration or preserve current capabilities. ” 42 C. F. R. § 409. 32(c) www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 15

MAINTENANCE-LEVEL REHABILITATION § Maintenance rehabilitation therapy is a covered service “… when the specialized knowledge of a qualified therapist is required to design and establish a maintenance program based on an initial evaluation and periodic assessment of a resident’s needs…” 42 C. F. R § 409. 33(c)(5) www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 16
CMS MANUALS § CMS revised the Manuals as a result of Jimmo. We’ll discuss them later. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 17
CASES PRE-JIMMO § Individual administrative appeals of denial of coverage. § Individual cases • E. g. , Papciak v. Sebelius, 742 F. Supp. 2 d 765 (W. D. Pa. 2010) www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 18
JIMMO v. SEBELIUS, Civ. No. 5: 11 -CV-17 (D. VT. 1/18/2011) § Federal class action lawsuit to eliminate use of improvement standard in SNFs, home health, outpatient therapy (PT, OT, speech). § § Filed Jan. 18, 2011 in federal District Court in Vermont. Settled Oct. 16, 2012. Court approved settlement Jan. 24, 2013. Plaintiffs: 5 individuals and 6 organizations • • • Alzheimer’s Association National Multiple Sclerosis Society National Committee to Preserve Social Security & Medicare Paralyzed Veterans of America Parkinson’s Action Network United Cerebral Palsy www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 19
WHAT JIMMO SETTLEMENT MEANS: NO DENIALS BASED ON IMPROVEMENT STANDARD § Medicare coverage is improperly denied for skilled nursing or rehabilitation services when the denial is based on: • Individual’s stable or chronic condition. • No expectation of improvement in a reasonable period of time. § Services can be skilled and covered even when: • Individual has “plateaued” • Services are “maintenance only” www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 20
JIMMO CLARIFIES PROPER STANDARD § Is a skilled health care professional (nurse or therapist) needed to ensure that nursing or therapy is safe and effective? § Is a qualified nurse or therapist needed to provide or supervise the care? § If yes, Medicare covers care, regardless of whether the skilled care is needed to improve, maintain function, or slow decline or deterioration. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 21
INDIVIDUALIZED ASSESSMENTS REQUIRED § What does this individual need? § Not, what do people with similar disease or condition need in general? § Not, overall rule based on diagnosis or treatment norm. • E. g. : People who can walk 50 feet without assistance do not need physical therapy. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 22
EXAMPLES OF PROHIBITED RULES OF THUMB • Individual or condition is “stable” or “chronic. ” • Condition will not improve • Lack of “restoration potential. ” • Care is needed for long period of time • Unless a legal limit: e. g. , SNF, 100 days in a Part A benefit period. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 23
WHAT JIMMO SETTLEMENT MEANS: REVISION OF CMS MANUALS § CMS revised Medicare Benefit Policy Manual for SNF, home health, outpatient therapy, and inpatient rehabilitation facility. § CMS clarifies skilled maintenance therapy and skilled maintenance nursing are covered by Medicare; eliminates conflicting provisions in Medicare Manuals. Transmittal 179 (Jan. 14, 2014), http: //www. cms. gov/Regulations-and. Guidance/Transmittals/Downloads/R 179 BP. pdf (replacing Transmittal 176 (Dec. 13, 2013)), http: //www. cms. gov/Regulations-and. Guidance/Transmittals/Downloads/R 176 BP. pdf. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 24
MANUAL GUIDANCE FOR SNFs § “If the inherent complexity of a service prescribed for a patient is such that it can be performed safely and/or effectively only by or under the general supervision of skilled nursing or skilled rehabilitation personnel, the service is a skilled service; e. g. , the administration of intravenous feedings and intramuscular injections; the insertion of suprapubic catheters; and ultrasound, shortwave, and microwave therapy treatments. . While a patient’s particular medical condition is a valid factor in deciding if skilled services are needed, a patient’s diagnosis or prognosis should never be the sole factor in deciding that a service is not skilled. ” Medicare Benefit Policy Manual, Pub. No. 100 -02, Chapter 8, § 30. 2. 2 (scroll down to p. 23). www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 25
MANUAL GUIDANCE FOR SNFs § “A service that is ordinarily considered nonskilled could be considered a skilled service in cases in which, because of special medical complications, skilled nursing or skilled rehabilitation personnel are required to perform or supervise it or to observe the patient. In these cases, the complications and special services involved must be documented by physicians' orders and notes as well as nursing or therapy notes. ” Medicare Benefit Policy Manual, Pub. No. 100 -02, Chapter 8, § 30. 2. 2 (scroll down to p. 23). • Example: “Whirlpool baths do not ordinarily require the skills of a qualified physical therapist. However, the skills, knowledge, and judgment of a qualified physical therapist might be required where the patient’s condition is complicated by circulatory deficiency, areas of desensitization, or open wounds. ” (p. 23) www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 26
MANUAL GUIDANCE FOR SNFs § Example: “An 81 -year-old woman who is aphasic and confused, suffers from hemiplegia, congestive heart failure, and atrial fibrillation, has suffered a cerebrovascular accident, is incontinent, has a Stage 1 decubitus ulcer, and is unable to communicate and make her needs known. Even though no specific service provided is skilled, the patient’s condition requires daily skilled nursing involvement to manage a plan for the total care needed, to observe the patient’s progress, and to evaluate the need for changes in the treatment plan. ” Medicare Benefit Policy Manual, Pub. No. 100 -02, Chapter 8, § 30. 2. 2 (scroll down to p. 24). www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 27
MANUAL GUIDANCE FOR SNFs § Example: “The possibility of adverse effects from the improper performance of an otherwise unskilled service does not make it a skilled service unless there is documentation to support the need for skilled nursing or skilled rehabilitation personnel. Although the act of turning a patient normally is not a skilled service, for some patients the skills of a nurse may be necessary to assure proper body alignment in order to avoid contractures and deformities. In all such cases, the reasons why skilled nursing or skilled rehabilitation personnel are essential must be documented in the patient’s record. ” Medicare Benefit Policy Manual, Pub. No. 100 -02, Chapter 8, § 30. 2. 2 (scroll down to p. 24). www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 28
WHAT DOES THE MANUAL REQUIRE? § Specific, detailed description of resident and detailed explanation of why a skilled person is needed to provide care. § CMS emphasizes documentation (documentation requirements were added to Manuals, although they are not required by Jimmo court decision and settlement). § In practice, the care plan needs to describe maintenance level of care (cannot just assume that after improvement ends, the resident automatically transitions to maintenance coverage). www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 29
WHATJIMMO SETTLEMENT MEANS: EDUCATIONAL CAMPAIGN § CMS conducted nationwide Educational Campaign (one call). § CMS explained Settlement and new Manuals to providers, Medicare Contractors, Medicare adjudicators (one call). www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 30
WHAT JIMMO MEANS: ACCOUNTABILITY AND REVIEW § CMS had to • review random samples of Qualified • • Independent Contractor (QIC) decisions; address errors raised in reviews; meet regularly with Plaintiffs’ counsel to correct errors in individuals’ cases (up to 100). • First in-person meeting, Jan. 6, 2014; with additional e-mails and telephone calls. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 31
WHAT JIMMO SETTLEMENT MEANS: RE-REVIEW § Individuals had opportunity to request Re-review of Medicare’s decisions made after Jan. 18, 2011. § Re-review no longer available. § Assumption is that providers and adjudicators are now using the correct standards for coverage. § Beneficiaries need to use standard appeals process. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 32
WE RETURNED TO COURT § Motion for Resolution of Noncompliance with Settlement Agreement (filed Mar. 1, 2016) § Court granted Motion in part (Aug. 17, 2016); found educational activities insufficient and inaccurate; ordered Government to come up with a plan. § We’re talking. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 33
BIGGEST OBSTACLES TO IMPLEMENTATION SINCE COURT APPROVAL OF SETTLEMENT § Continuing belief among providers and adjudicators that beneficiary must be improving before Medicare will pay. (We still get calls about patient who has “plateaued”). § SNFs refusing to provide therapy, regardless of what surgeon or other physician says. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 34
WHAT WE TELL PEOPLE TO DO IF MEDICARE COVERAGE IS DENIED § Physician is best, most important ally to order care and keep services in place (but new Requirements of Participation may be problem if physician delegates “task of writing therapy orders” to therapist, § 483. 30(e)(3)). www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 35
WHAT WE TELL PEOPLE TO DO IF MEDICARE COVERAGE IS DENIED § Do whatever you can to get covered-services ordered and provided. § Use Jimmo Settlement, regulations, Manual, CMS Jimmo materials, and CMA self-help packets to educate Medicare contractor/ adjudicator and ask provider to continue services. § Use the appeals process. But if services are not provided, resident cannot win appeal. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 36
PHYSICIAN SUPPORT § Ask primary care physician (PCP) or other relevant physician to talk with SNF’s Medical Director, explain why skilled care is necessary. § Ask PCP or other physician to write specific, detailed letter why resident needs skilled care • • • Explain relationship to patient List all medical conditions and medical history Explain which specific services are needed and why. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 37
MEDICARE APPEALS § Appeal from Notice of Medicare Non. Coverage or Medicare Summary Notice • Redetermination • Reconsideration • Administrative Law Judge • Medicare Appeals Council • Federal District Court • Federal Court of Appeals www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 38
KEY BARRIER FOR MEDICARE APPEALS § Beneficiary must have actually received a Medicare-covered level of care (eitherapy 5 days/week or skilled nursing care 7 days/week or a combination of the 2) to appeal. • • Essentially, pay-and-chase situation. If beneficiary does not receive Medicare-covered care, cannot win appeal. • Therapy 5 days/week: good case to appeal • Skilled nursing 7 days/week: more difficult to win www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 39
KEY BARRIER FOR MEDICARE APPEALS (cont’d) § When SNF decides that Medicare won’t pay, it stops providing Medicare-covered services. • Discontinues therapy • Stops doing Medicare-related MDS assessments www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 40
TRANSFER/DISCHARGE RIGHTS § Denial of Medicare coverage is not the same as discharge from SNF. § Resident also has rights under the Nursing Home Reform Law • • • Limited permissible reasons for transfer/discharge Notice Opportunity for administrative hearing 42 U. S. C. § 1395 i-3(c)(2) 42 U. S. C. § 483. 12, effective Nov. 28, 2016, § 483. 15(c) www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 41
TRANSFER/DISCHARGE RIGHTS § Center for Medicare Advocacy, “‘Discharge from a Skilled Nursing Facility: What Does It Mean and What Rights Does a Resident Have? ” (Alert, Jan. 13, 2016), http: //www. medicareadvocacy. org/discharg e-from-a-skilled-nursing-facility-what-doesit-mean-and-what-rights-does-a-residenthave/. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 42
APPEALS § Different ways to get into appeals process, depending on whether SNF denied coverage or whether SNF submitted claim for Part A reimbursement, which was denied by Medicare. § Need formal denial by CMS to get into appeals system. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 43
APPEALS OF SNF DETERMIINATIONS OF NON-COVERAGE § If SNF determines Medicare Part A will not pay, appeal. • Expedited Appeal • Standard Appeal § Different Notices and purposes of these two appeals. Beneficiaries are entitled to, and must do, both. CMS, “Survey and Certification Issues Related to Liability Notices and Beneficiary Appeal Rights in Nursing Homes, ” S&C-09 -20 (Jan. 9, 2009), http: //www. cms. gov/Medicare/Provider-Enrollment-and. Certification/Survey. Certification. Gen. Info/Downloads/SCL etter 09 -20. pdf. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 44
EXPEDITED APPEAL 42 CFR § 405. 1202 § Purpose: to keep services in place. § SNF gives notice at least 2 days prior to discharge from Medicare (i. e. , termination of all Part A services), Notice of Medicare Provider Non-Coverage, Form CMS-10123. § Resident/family must call Quality Improvement Organization (QIO) (now called Beneficiary and Family Centered QIO) by no later than noon the following day. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 45
EXPEDITED APPEAL (cont’d) § Medicare-covered care continues until day of discharge identified in SNF notice, unless QIO reverses decision. § If SNF does not provide timely information to QIO, it may be financially responsible for providing covered care. § If QIO finds SNF’s notice was not valid, coverage continues until at least 2 days after valid notice is provided. 42 C. F. R. § 405. 1202(c) § Burden of proof on SNF to prove termination of services was correct. 42 C. F. R. § 405. 1202(d) www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 46
EXPEDITED APPEAL (cont’d) § QIO procedures • • • Determining whether SNF notice was valid. Examining records submitted by SNF. Soliciting views of beneficiary who requested expedited hearing. Providing opportunity for provider/practitioner to explain why termination of services was appropriate. Within 72 hours, notifying beneficiary, beneficiary’s physician, and SNF of its determination. 42 C. F. R. § 405. 1202(e) www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 47
EXPEDITED APPEAL (cont’d) § SNF responsibilities • When QIO notifies SNF of expedited appeal, SNF must send detailed notice to beneficiary by close of business day, including • “A specific and detailed explanation why services are either no longer reasonable and necessary or are no longer covered. ” • Description of applicable Medicare policy. • “Facts specific to the beneficiary and relevant to the coverage determination. . ” 42 C. F. R. § 405. 1202(f)(1)(i)-(iv) www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 48
EXPEDITED APPEAL (cont’d) § SNF responsibilities • Providing QIO with information it needs. • At beneficiary’s request, providing beneficiary with copy of, or access to, information it provided to QIO. 42 C. F. R. § 405. 1202(f)(2), (3) www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 49
QIO DECISION IN EXPEDITED APPEAL § Initial notification (may be by telephone, followed by written notice) that describes • • • Rationale for decision Explanation of Medicare payment consequences Information about how to request Reconsideration (next level of appeal). 42 C. F. R. § 405. 1202(e)(8)(i)-(iii) www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 50
EXPEDITED APPEAL (cont’d) § Stress again: Unlikely to win without physician support. • Try to get physician letter that is detailed, • specific, and personal about resident’s needs and why, for example, therapy is medically necessary. Physician letter saying care is medically necessary is insufficient. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 51
EXPEDITED RECONSIDERATION 42 C. F. R. § 405. 1204 § Expedited reconsideration by appropriate Qualified Independent Contractor (QIC). • Procedures similar to those required for expedited appeal. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 52
STANDARD APPEAL § As result of Sarrassat v. Sullivan, No. C 88 -20161 (N. D. Cal. 1989), SNF must give beneficiary written notice if it believes Medicare Part A will not pay for care as reasonable and necessary. • • • Either SNF Advance Beneficiary Notice (SNF ABN), Form CMS-10055, or one of five uniform denial letters, http: //www. cms. gov/Medicare-General. Information/BNI/FFSSNFABNand. SNFDenial. Letters. html. These notices inform beneficiary that he/she can require SNF to submit a demand bill to Medicare (to get initial determination by Medicare). SNF may not bill beneficiary until Medicare makes initial determination. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 53
LATER LEVELS OF APPEAL § Possible, but worthwhile only if resident continued to receive Medicare-covered level of care at SNF. § Resident/family will likely be required to pay out-of-pocket for continued care (e. g. , therapy covered by Medicare Part B) and try to win on appeal. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 54
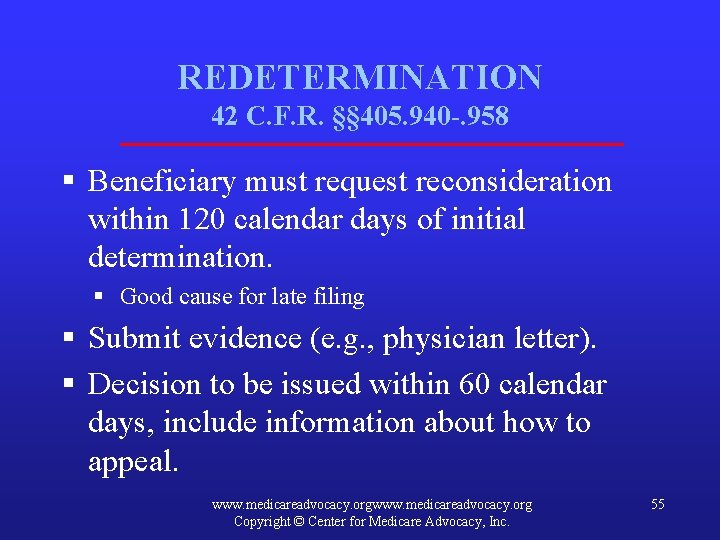
REDETERMINATION 42 C. F. R. §§ 405. 940 -. 958 § Beneficiary must request reconsideration within 120 calendar days of initial determination. § Good cause for late filing § Submit evidence (e. g. , physician letter). § Decision to be issued within 60 calendar days, include information about how to appeal. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 55
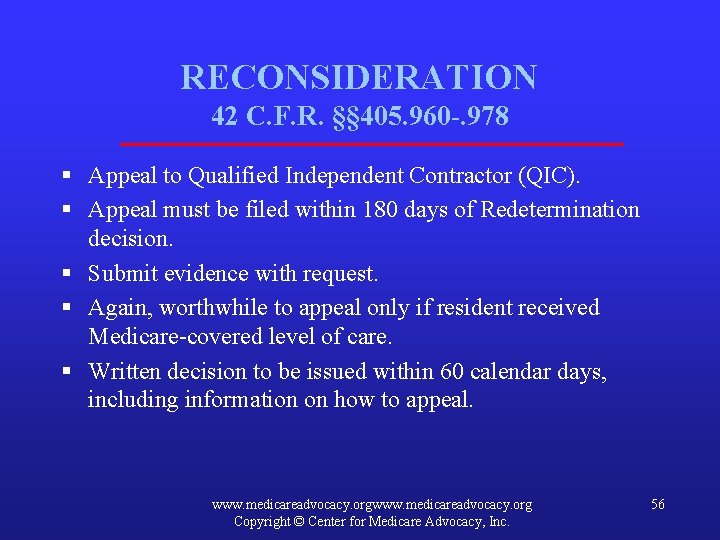
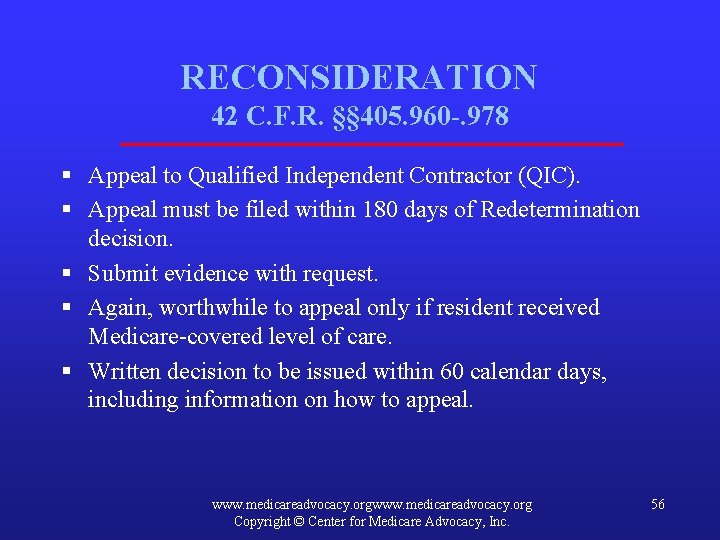
RECONSIDERATION 42 C. F. R. §§ 405. 960 -. 978 § Appeal to Qualified Independent Contractor (QIC). § Appeal must be filed within 180 days of Redetermination decision. § Submit evidence with request. § Again, worthwhile to appeal only if resident received Medicare-covered level of care. § Written decision to be issued within 60 calendar days, including information on how to appeal. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 56
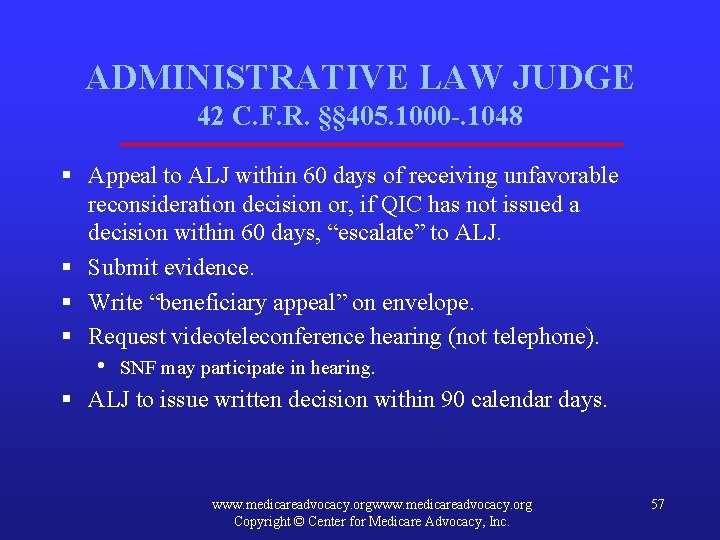
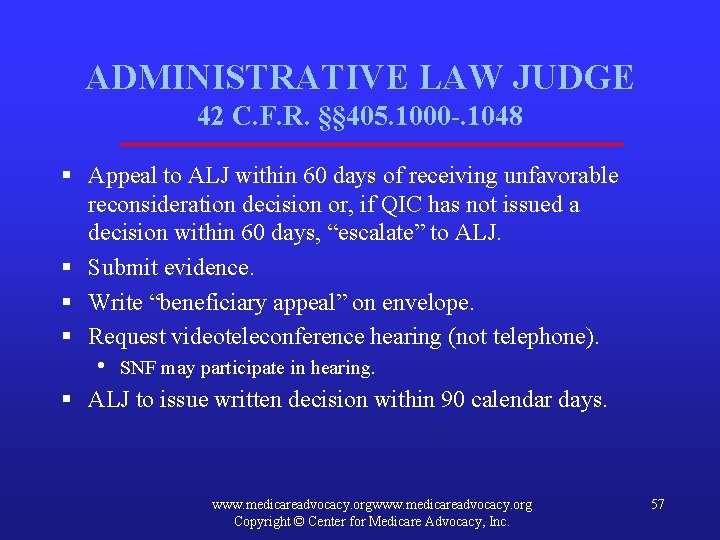
ADMINISTRATIVE LAW JUDGE 42 C. F. R. §§ 405. 1000 -. 1048 § Appeal to ALJ within 60 days of receiving unfavorable reconsideration decision or, if QIC has not issued a decision within 60 days, “escalate” to ALJ. § Submit evidence. § Write “beneficiary appeal” on envelope. § Request videoteleconference hearing (not telephone). • SNF may participate in hearing. § ALJ to issue written decision within 90 calendar days. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 57
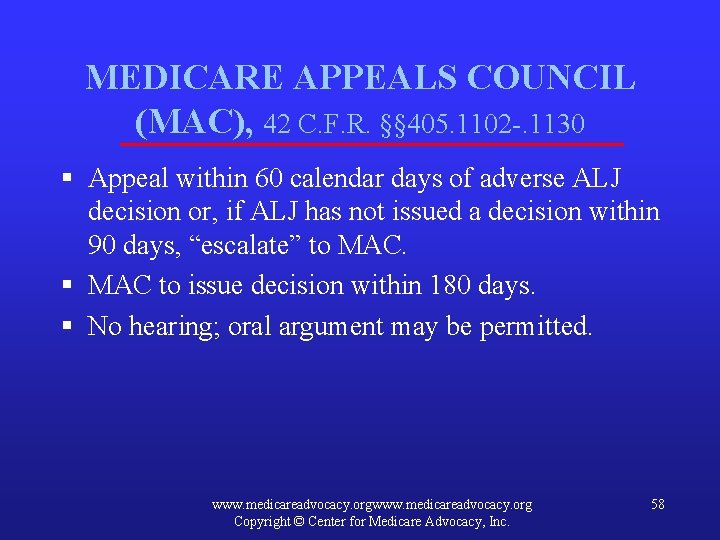
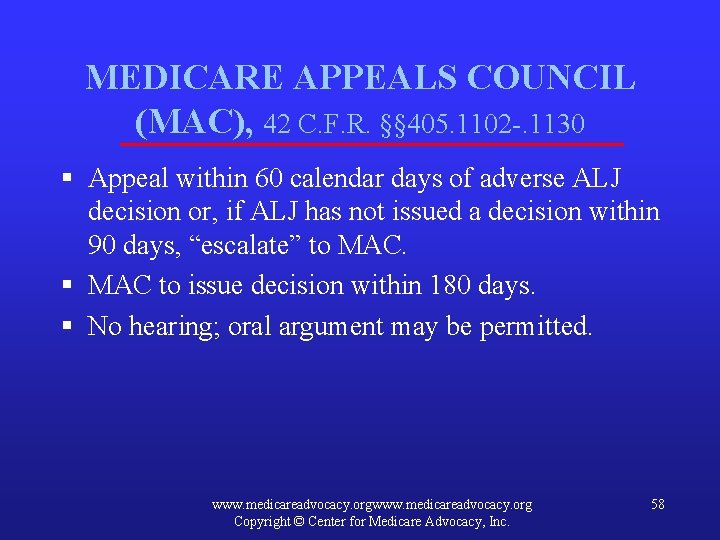
MEDICARE APPEALS COUNCIL (MAC), 42 C. F. R. §§ 405. 1102 -. 1130 § Appeal within 60 calendar days of adverse ALJ decision or, if ALJ has not issued a decision within 90 days, “escalate” to MAC. § MAC to issue decision within 180 days. § No hearing; oral argument may be permitted. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 58
JUDICIAL REVIEW § File in federal District Court. 42 C. F. R. § 405. 1136 www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 59
APPEALS OF MEDICARE DENIALS OF PART A COVERAGE § SNF’s bill to Medicare for Part A payment may be denied. § Beneficiary receives Medicare Summary Notice (MSN) from CMS as initial determination. § Beneficiary appeals from MSN for redetermination. § Then reconsideration, ALJ, Medicare Appeals Council, federal court. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 60
ADDITIONAL CHALLENGES IN MEDICARE APPEALS § Lower levels (redetermination and reconsideration) seem to “rubber stamp” noncoverage decisions. § Long delays in administrative appeals process. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 61
HULL v. SEBELIUS, No. 3: 14 -cv-801 (JAM) (D. Conn. Filed June 4, 2014) § Challenged high denial rates (98%) at redetermination and reconsideration levels for home health care in Connecticut. § Judge dismissed case, 66 F. Supp. 3 d 278 (D. CT 2014) (holding dual-eligible beneficiaries did not have an injury when Medicaid paid for their home health care). § Case dismissed June 7, 2016. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 62
EXLEY v. BURWELL, No. 3: 14 -cv-01230 (JAM) (D. Conn. Filed Aug. 26, 2014) § Complaint alleges failure of ALJs to issue decisions within 90 days (average delay now about 500 days) violates Medicare statute and Due Process. § Court denied government’s Motion to Dismiss (Jan. 27, 2015). www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 63

EXLEY § Settlement approved (May 24, 2016) § Write “Beneficiary Mail Stop” on appeal and envelop to get appeal heard quickly. § Office of Medicare Hearings & Appeals Beneficiary Help Line, (844) 419 -3358 (8: 00 a. m. – 4: 30 p. m. , ET) § More information will be available at Medicare. Advocacy. org. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 64
SENATE FINANCE COMMITTEE HEARING § “Creating an Efficient and More Level Playing Field: Audit and Appeals Issues in Medicare” (Apr. 28, 2015), http: //www. finance. senate. gov/hearings/hearing/? i d=d 29 af 43 d-5056 -a 032 -526 a-1 de 427 f 91 aeb. • • Chairman Hatch: 2009, appeals at ALJ level resolved in 94 days, in 2012, 547 days. FY 2010, high reversal rate at ALJ level (60% of 41, 000 provider appeals were reversed). www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 65
SENATE FINANCE COMMITTEE HEARING (cont’d) § Nancy J. Griswold, chief ALJ, testified • • Beneficiaries file 1% of appeals; 99% of appeals are filed by providers and state Medicaid agencies. FY 2013, received 384, 000 appeals; FY 2014, 474, 000 appeals. http: //www. finance. senate. gov/imo/media/doc/SFC%20 Griswold. OMHA%20 updated%20 testimony%20%204%2028%2015. pdf. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 66
UPDATES ON JIMMO See CMA website: Improvement: http: //www. medicareadvocacy. org/? s=improvement&op. x=0 &op. y=0 § Jimmo: http: //www. medicareadvocacy. org/? s=Jimmo&op. x=0&op. y=0 www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 67
CMA SELF-HELP PACKET FOR SNF APPEALS § Available at http: //www. medicareadvocacy. org/self-help -packet-for-expedited-skilled-nursingfacility-appeals-including-improvementstandard-denials/ www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 68
MORE INFORMATION FROM CMA § Weekly Alerts, e-mailed on Thursdays, free, covering variety of Medicare issues. Sign up at https: //org. salsalabs. com/o/777/p/salsa/web/common/publi c/signup? signup_page_KEY=1411. § Enforcement, monthly mailing on nursing home enforcement issues, available by subscription ($250/year). Subscribe at https: //org. salsalabs. com/o/777/t/13870/shop. jsp? stor efront_KEY=1052. www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 69
CMA Toby S. Edelman Senior Policy Attorney Center for Medicare Advocacy 1025 Connecticut Avenue, NW Washington, DC 20036 (202) 293 -5760 tedelman@Medicare. Advocacy. org www. medicareadvocacy. org Copyright © Center for Medicare Advocacy, Inc. 70
 How to win a medicare appeal for skilled nursing
How to win a medicare appeal for skilled nursing Skilled nursing facility value based purchasing program
Skilled nursing facility value based purchasing program Cause and effect nonfiction
Cause and effect nonfiction Critical thinking in society
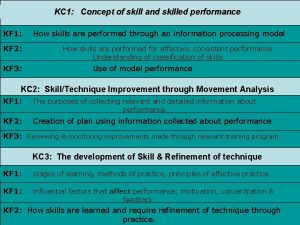
Critical thinking in society Characteristics of skilled performers
Characteristics of skilled performers Asvab average scores
Asvab average scores Skilled staffing jean
Skilled staffing jean Semi skilled labor
Semi skilled labor Skilled performance
Skilled performance Skilled performer
Skilled performer Skilled trades 1201
Skilled trades 1201 Define skilled human resources
Define skilled human resources Become skilled at
Become skilled at Defense office of hearings and appeals
Defense office of hearings and appeals Appeal to logic
Appeal to logic Rhetorical devices kahoot
Rhetorical devices kahoot Apostrophe poetic device
Apostrophe poetic device Persuasive essay strategies
Persuasive essay strategies Persuasive appeals
Persuasive appeals Appeals persuasive technique
Appeals persuasive technique Persuasive appeals
Persuasive appeals Persuasive speech structures
Persuasive speech structures Appeals logos
Appeals logos Ethos pathos logos
Ethos pathos logos Persuasive appeals
Persuasive appeals Context space cat
Context space cat Appeals ethos pathos logos
Appeals ethos pathos logos Appeal to ethos
Appeal to ethos Persuasive appeals
Persuasive appeals Appeal to ethics
Appeal to ethics Persuasive appeals
Persuasive appeals Appeals of persuasion
Appeals of persuasion Execution styles in advertising
Execution styles in advertising Examples of argument from authority
Examples of argument from authority Logical appeals
Logical appeals Rhetorical appeals
Rhetorical appeals Rhetorical triangle example
Rhetorical triangle example Aristotelian appeals
Aristotelian appeals Rhetorical appeals
Rhetorical appeals Rhetorical devices in a modest proposal
Rhetorical devices in a modest proposal Ethos, pathos, logos, kairos examples
Ethos, pathos, logos, kairos examples S48 ndis
S48 ndis Space cat ap lang
Space cat ap lang Contemporary persuasive appeals
Contemporary persuasive appeals 3 persuasive appeals
3 persuasive appeals Kredibilitas adalah
Kredibilitas adalah Rhetorical devices ppt
Rhetorical devices ppt Jeopardy logos
Jeopardy logos Persuasive message strategy body
Persuasive message strategy body Which word most strongly appeals to pathos?
Which word most strongly appeals to pathos? Ethos, pathos and logos
Ethos, pathos and logos Rhetorical appeals
Rhetorical appeals Efile massachusetts appeals court
Efile massachusetts appeals court Sentimental appeal fallacy
Sentimental appeal fallacy Authority fallacy
Authority fallacy Illogical argument examples
Illogical argument examples Superhero ethos
Superhero ethos Imagery appeals to which of these
Imagery appeals to which of these Servsafe cutting board colors
Servsafe cutting board colors Medicare parts c and d general compliance training answers
Medicare parts c and d general compliance training answers Medicare sales certification and recertification
Medicare sales certification and recertification Medicare parts c and d sponsors are not required
Medicare parts c and d sponsors are not required Mmsea act of 2007
Mmsea act of 2007 Medicare improvements for patients and providers act
Medicare improvements for patients and providers act Types of nursing care delivery models
Types of nursing care delivery models Clean public areas facilities and equipment
Clean public areas facilities and equipment Procedures in receiving and storing tools and materials
Procedures in receiving and storing tools and materials Hotel sizes classifications
Hotel sizes classifications Iso 17025 environmental conditions
Iso 17025 environmental conditions Retail storage with customer pickup
Retail storage with customer pickup Cross connection servsafe
Cross connection servsafe