PNEUMOTRIESTE 2016 Ventilatore Meccanico come utilizzarlo nel malato








- Slides: 54
PNEUMOTRIESTE 2016 Ventilatore Meccanico: come utilizzarlo nel malato neuromuscolare A. Vianello S. C. Fisiopatologia Respiratoria Azienda Ospedale-Università di Padova
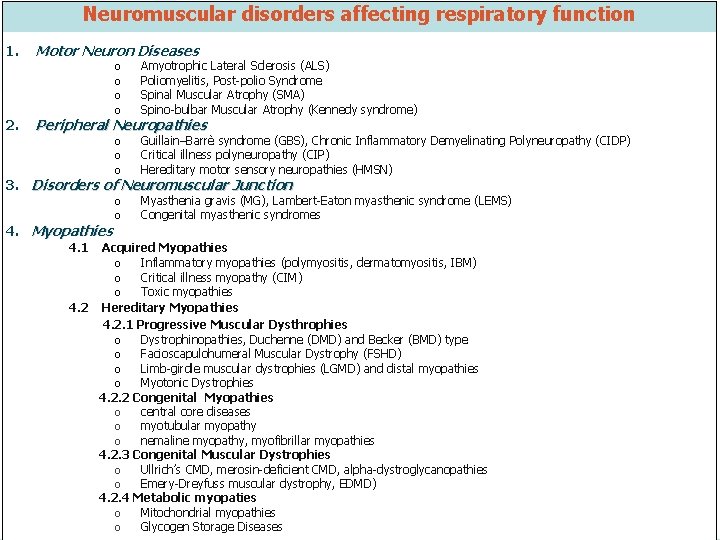
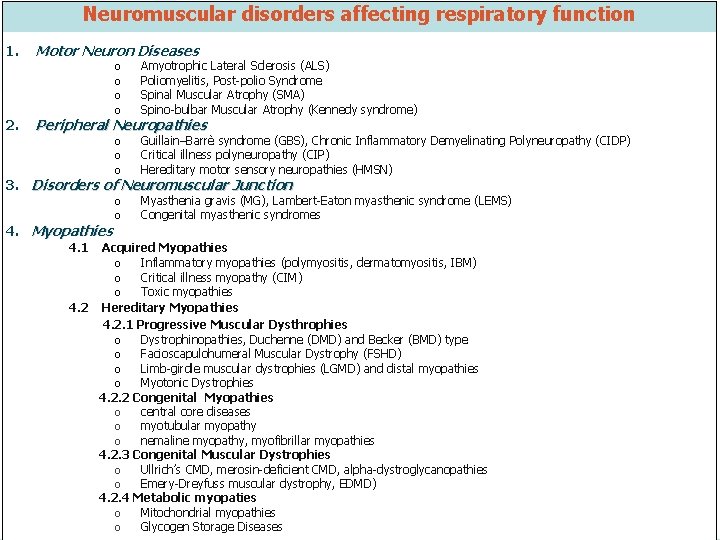
Neuromuscular disorders affecting respiratory function 1. 2| Motor Neuron Diseases o o Amyotrophic Lateral Sclerosis (ALS) Poliomyelitis, Post-polio Syndrome Spinal Muscular Atrophy (SMA) Spino-bulbar Muscular Atrophy (Kennedy syndrome) o o o Guillain–Barrè syndrome (GBS), Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) Critical illness polyneuropathy (CIP) Hereditary motor sensory neuropathies (HMSN) o o Myasthenia gravis (MG), Lambert-Eaton myasthenic syndrome (LEMS) Congenital myasthenic syndromes Peripheral Neuropathies 3. Disorders of Neuromuscular Junction 4. Myopathies 4. 1 Acquired Myopathies o Inflammatory myopathies (polymyositis, dermatomyositis, IBM) o Critical illness myopathy (CIM) o Toxic myopathies 4. 2 Hereditary Myopathies 4. 2. 1 Progressive Muscular Dysthrophies o Dystrophinopathies, Duchenne (DMD) and Becker (BMD) type o Facioscapulohumeral Muscular Dystrophy (FSHD) o Limb-girdle muscular dystrophies (LGMD) and distal myopathies o Myotonic Dystrophies 4. 2. 2 Congenital Myopathies o central core diseases o myotubular myopathy o nemaline myopathy, myofibrillar myopathies 4. 2. 3 Congenital Muscular Dystrophies o Ullrich’s CMD, merosin-deficient CMD, alpha-dystroglycanopathies o Emery-Dreyfuss muscular dystrophy, EDMD) 4. 2. 4 Metabolic myopaties o Mitochondrial myopathies o Glycogen Storage Diseases
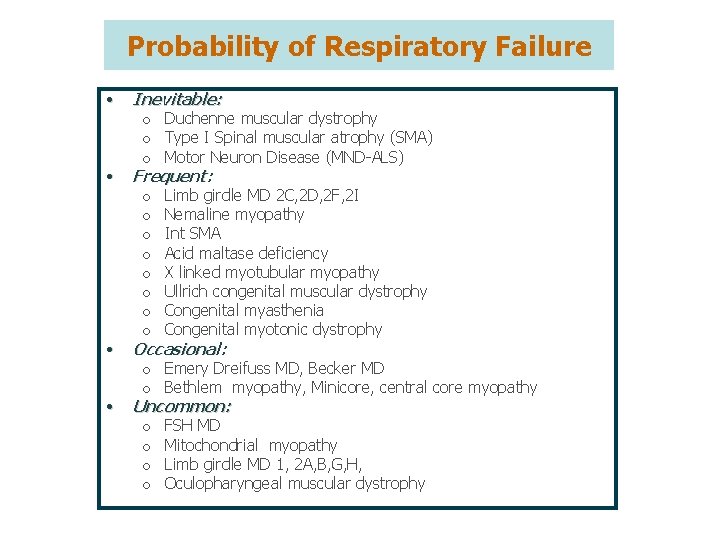
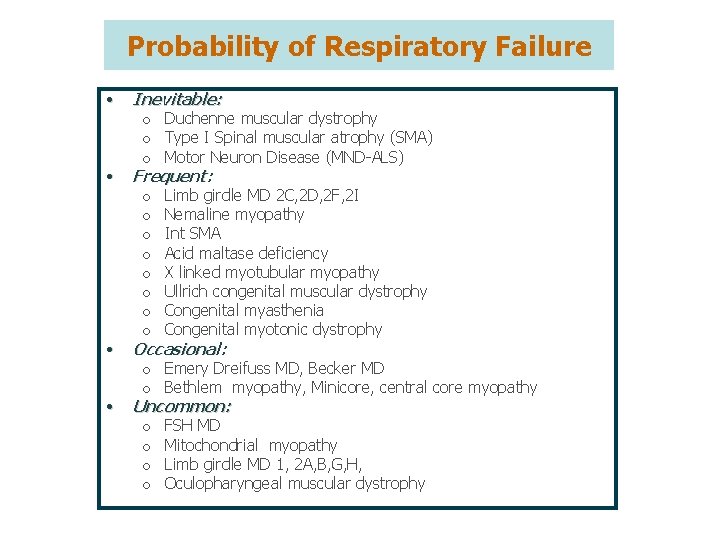
Probability of Respiratory Failure • • Inevitable: o Duchenne muscular dystrophy o Type I Spinal muscular atrophy (SMA) o Motor Neuron Disease (MND-ALS) Frequent: o Limb girdle MD 2 C, 2 D, 2 F, 2 I o Nemaline myopathy o Int SMA o Acid maltase deficiency o X linked myotubular myopathy o Ullrich congenital muscular dystrophy o Congenital myasthenia o Congenital myotonic dystrophy Occasional: o Emery Dreifuss MD, Becker MD o Bethlem myopathy, Minicore, central core myopathy Uncommon: o FSH MD o Mitochondrial myopathy o Limb girdle MD 1, 2 A, B, G, H, o Oculopharyngeal muscular dystrophy
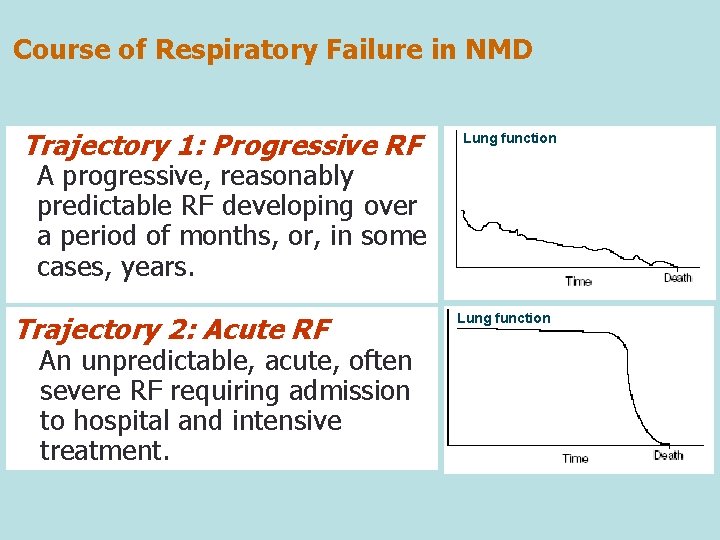
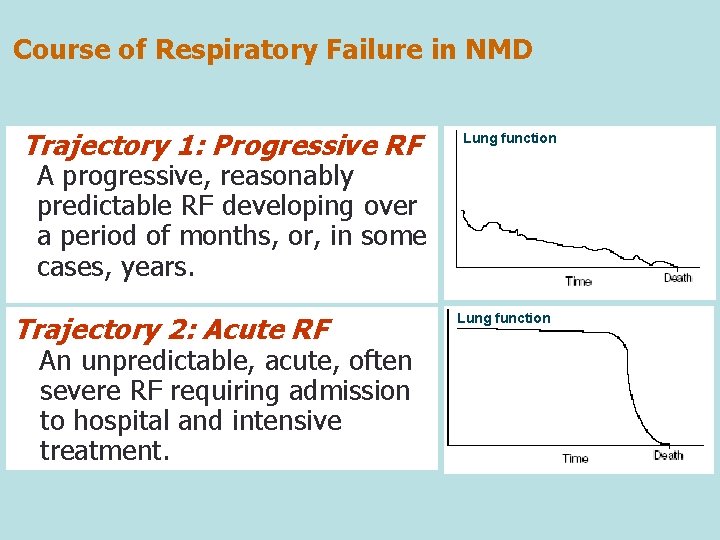
Course of Respiratory Failure in NMD Trajectory 1: Progressive RF Lung function A progressive, reasonably predictable RF developing over a period of months, or, in some cases, years. Trajectory 2: Acute RF An unpredictable, acute, often severe RF requiring admission to hospital and intensive treatment. Lung function
Management of Slowly Progressive RF by Long-Term NIV
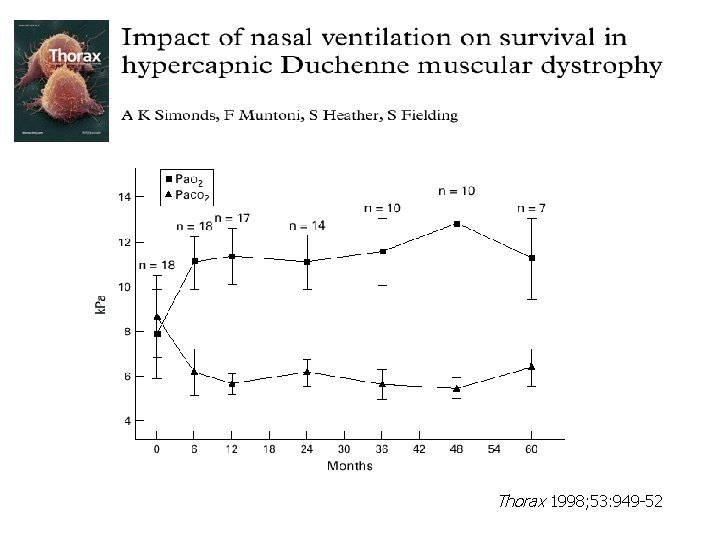
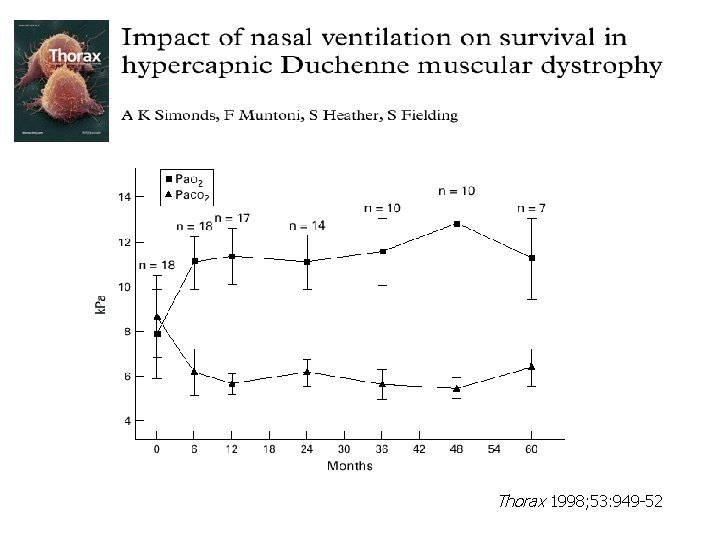
Thorax 1998; 53: 949 -52
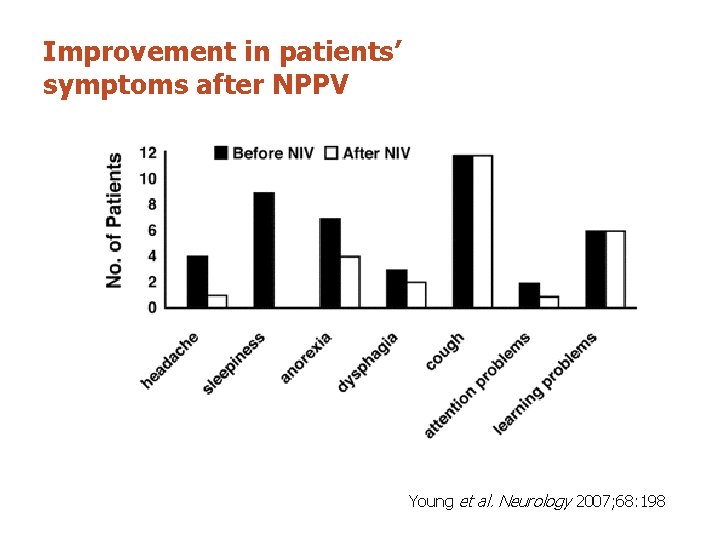
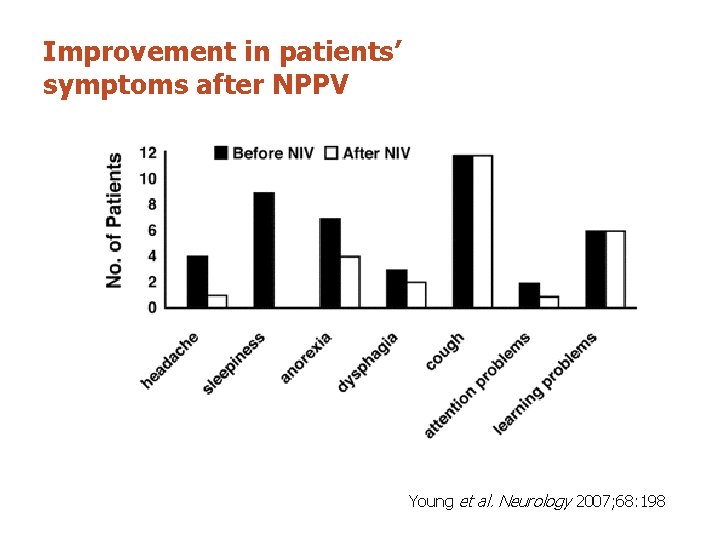
Improvement in patients’ symptoms after NPPV Young et al. Neurology 2007; 68: 198
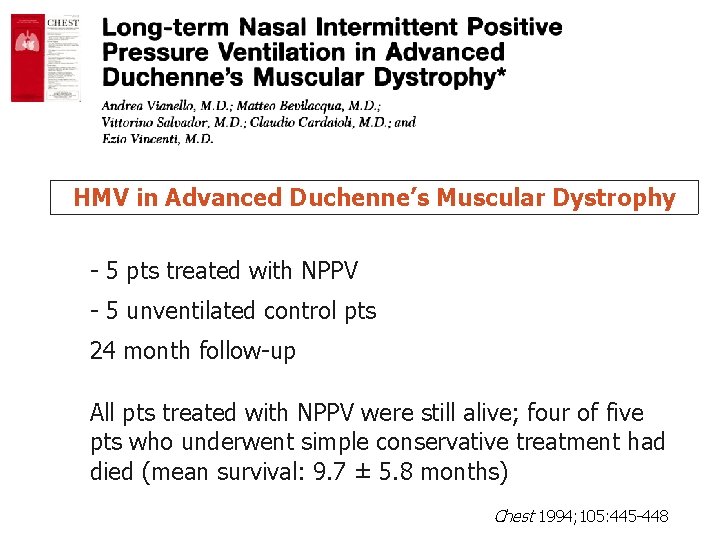
HMV in Advanced Duchenne’s Muscular Dystrophy - 5 pts treated with NPPV - 5 unventilated control pts 24 month follow-up All pts treated with NPPV were still alive; four of five pts who underwent simple conservative treatment had died (mean survival: 9. 7 ± 5. 8 months) Chest 1994; 105: 445 -448
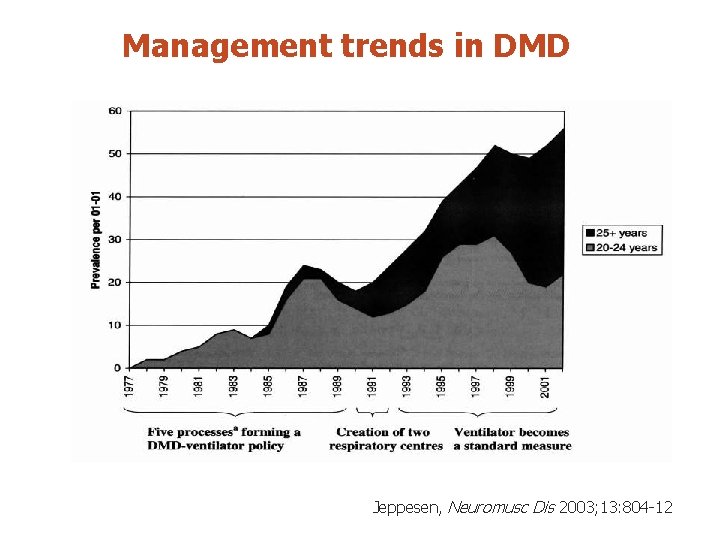
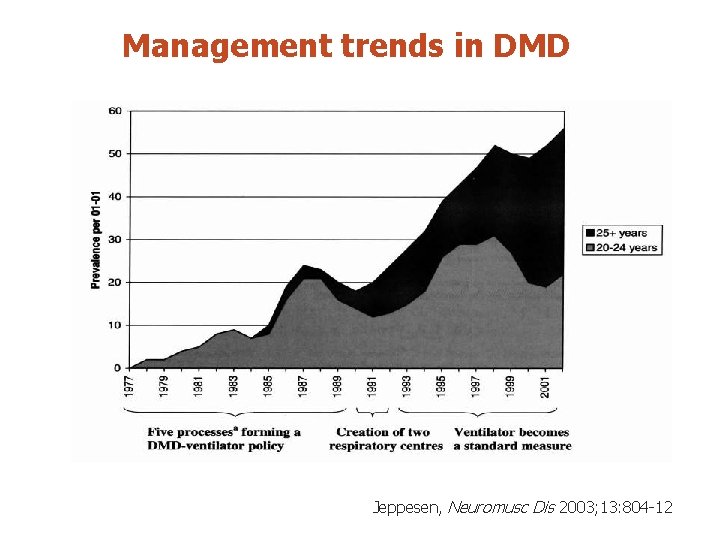
Management trends in DMD Jeppesen, Neuromusc Dis 2003; 13: 804 -12
Nocturnal mechanical ventilation for chronic hypoventilation in patients with neuromuscular and chest wall disorders. Current evidence about therapeutic benefit of mechanical ventilation is weak, but consistent, suggesting alleviation of the symptoms of chronic hypoventilation in the short term, and in two small studies survival was prolonged. Mechanical ventilation should be offered as a therapeutic option to patients with chronic hypoventilation due to neuromuscular diseases. Annane D et al, Cochrane Database of Systematic Reviews 2001
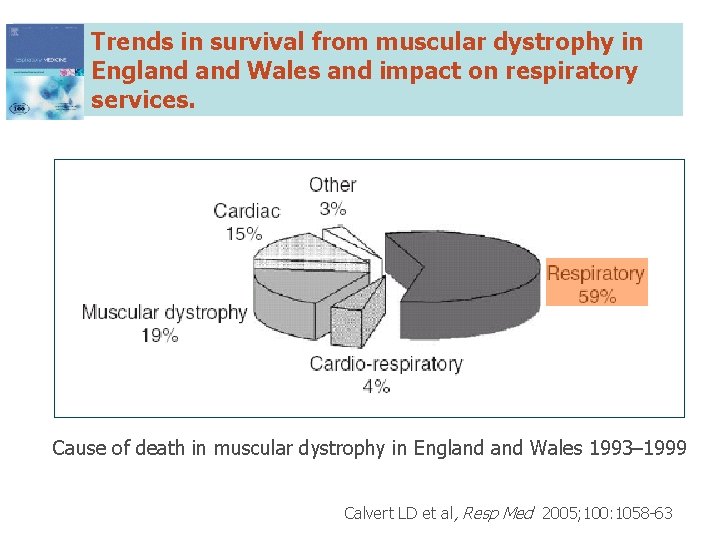
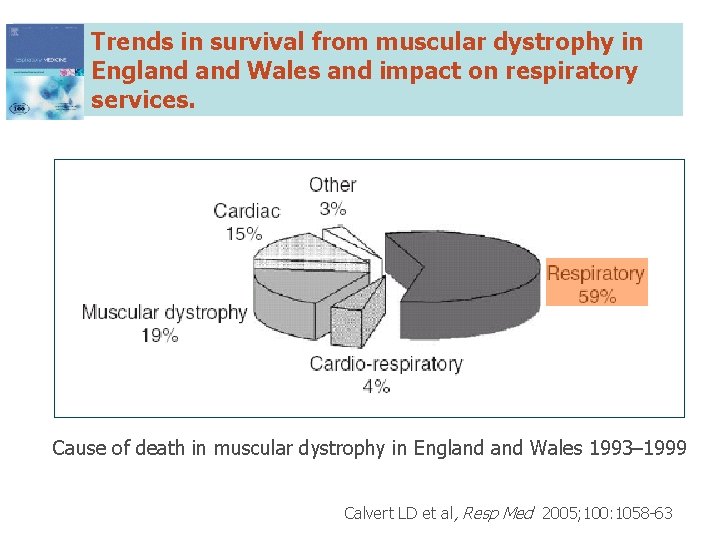
Trends in survival from muscular dystrophy in England Wales and impact on respiratory services. Cause of death in muscular dystrophy in England Wales 1993– 1999 Calvert LD et al, Resp Med 2005; 100: 1058 -63

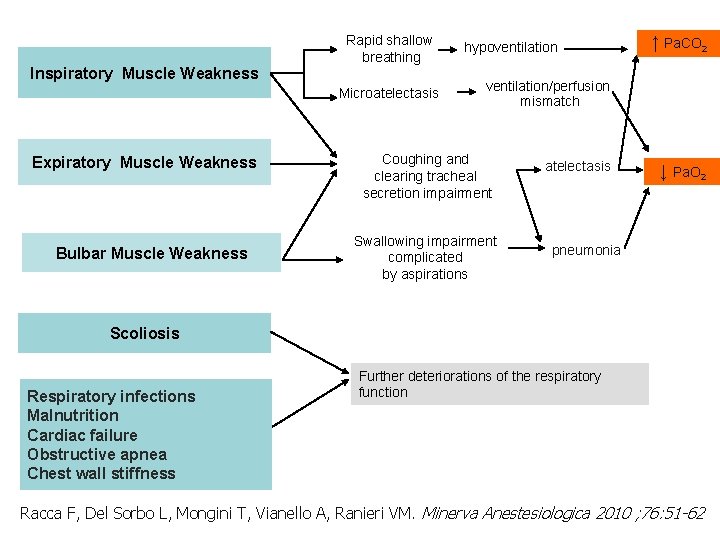
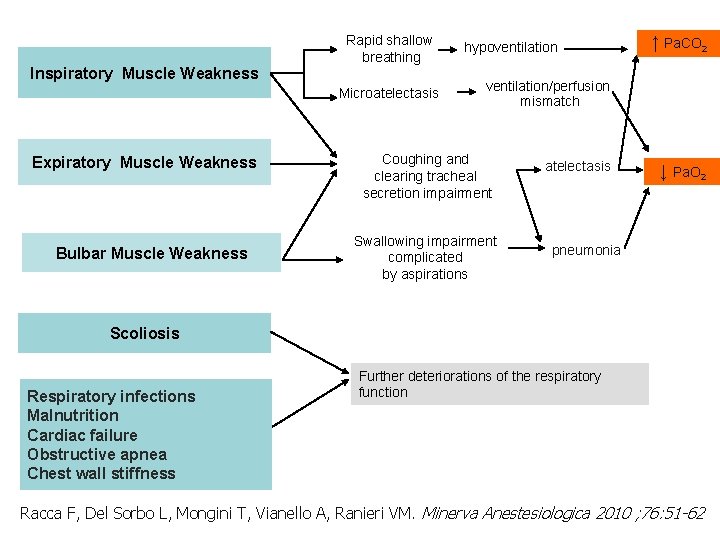
Inspiratory Muscle Weakness Rapid shallow breathing Microatelectasis Expiratory Muscle Weakness Bulbar Muscle Weakness hypoventilation ↑ Pa. CO 2 ventilation/perfusion mismatch Coughing and clearing tracheal secretion impairment Swallowing impairment complicated by aspirations atelectasis ↓ Pa. O 2 pneumonia Scoliosis Respiratory infections Malnutrition Cardiac failure Obstructive apnea Chest wall stiffness Further deteriorations of the respiratory function Racca F, Del Sorbo L, Mongini T, Vianello A, Ranieri VM. Minerva Anestesiologica 2010 ; 76: 51 -62
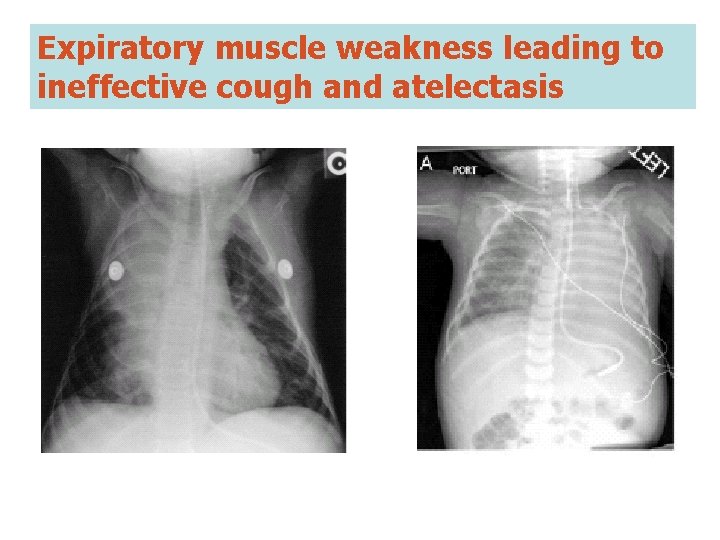
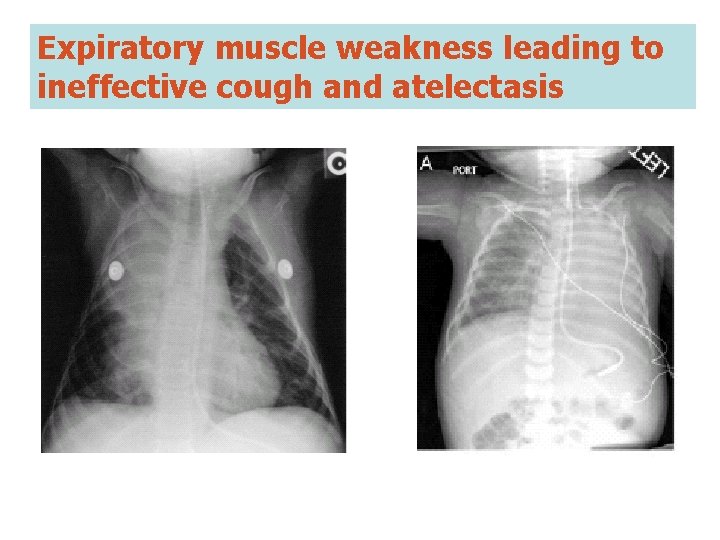
Expiratory muscle weakness leading to ineffective cough and atelectasis
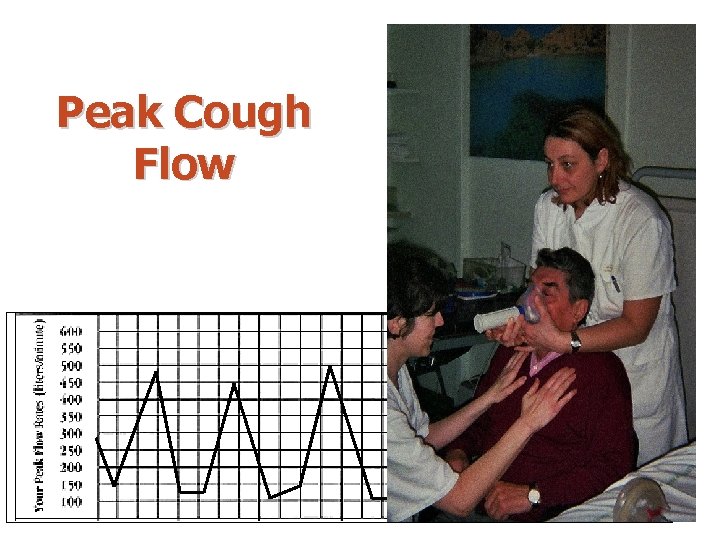
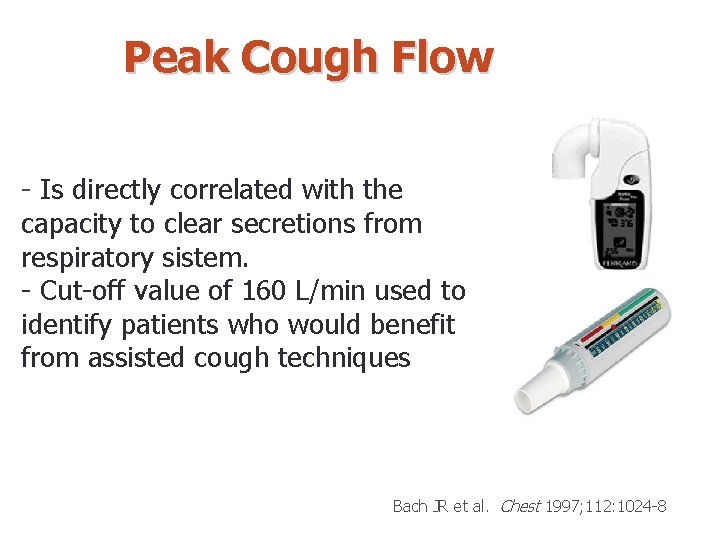
Peak Cough Flow

Ullrich’s Congenital Muscular Dystrophy
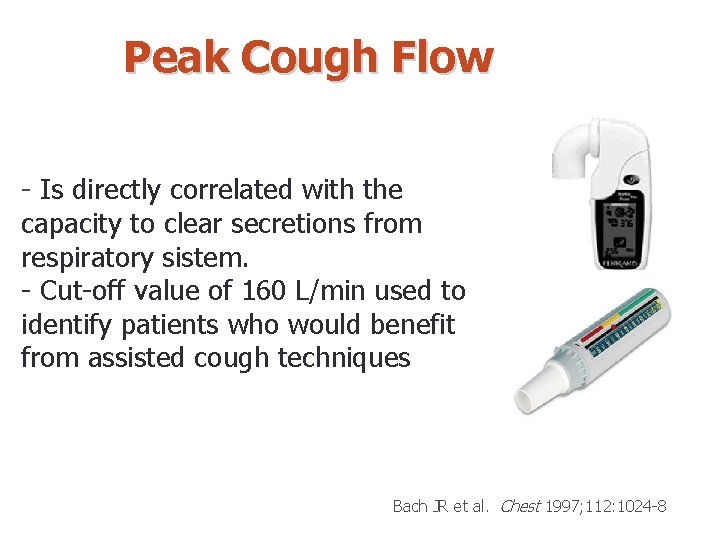
Peak Cough Flow - Is directly correlated with the capacity to clear secretions from respiratory sistem. - Cut-off value of 160 L/min used to identify patients who would benefit from assisted cough techniques Bach JR et al. Chest 1997; 112: 1024 -8
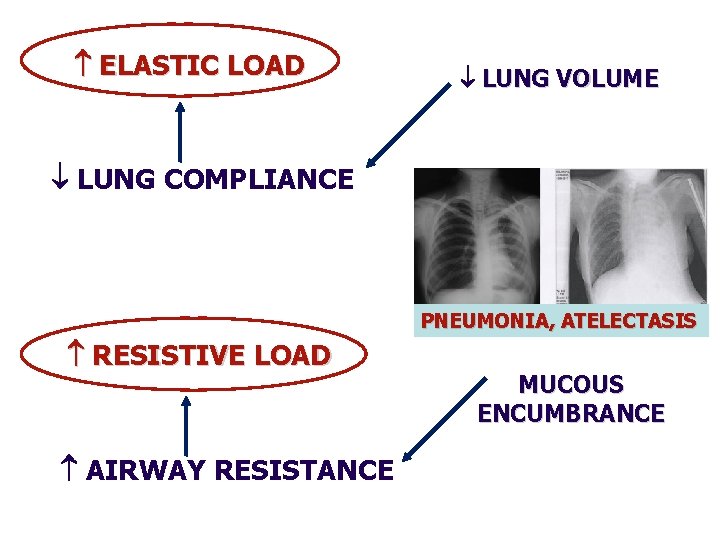
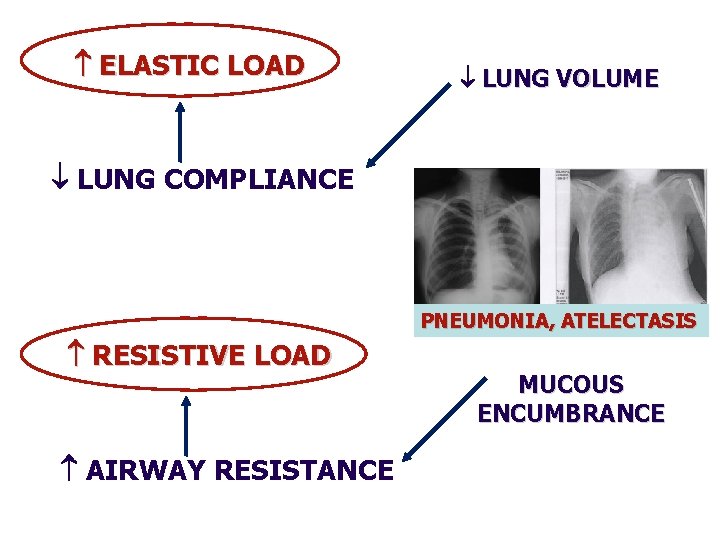
ELASTIC LOAD LUNG VOLUME LUNG COMPLIANCE PNEUMONIA, ATELECTASIS RESISTIVE LOAD AIRWAY RESISTANCE MUCOUS ENCUMBRANCE
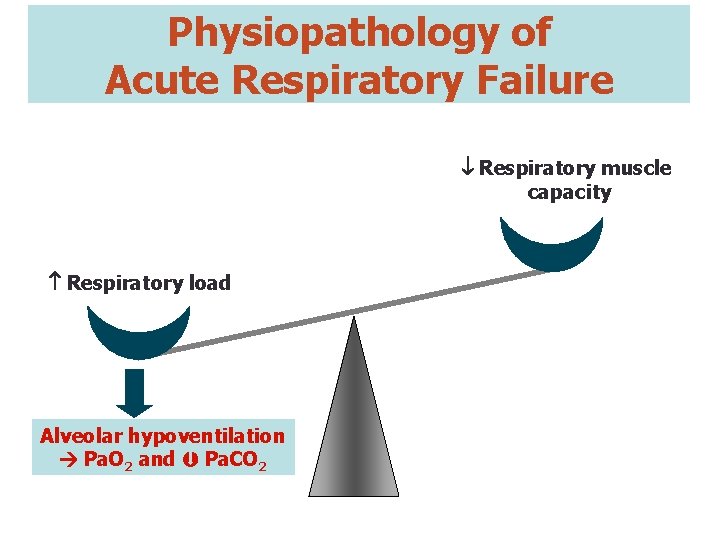
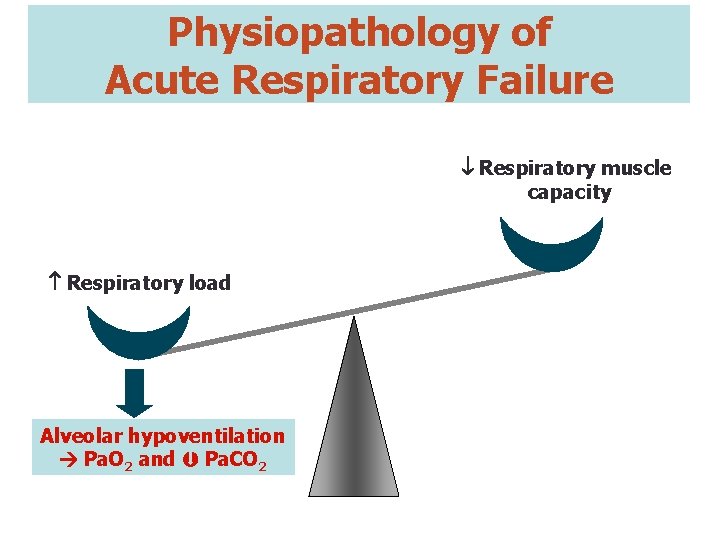
Physiopathology of Acute Respiratory Failure Respiratory muscle capacity Respiratory load Alveolar hypoventilation Pa. O 2 and Pa. CO 2
Conventional Approach to Managing ARF 20 | in Neuromuscular Disorders Facio-Scapulo-Humeral Muscular Dystrophy
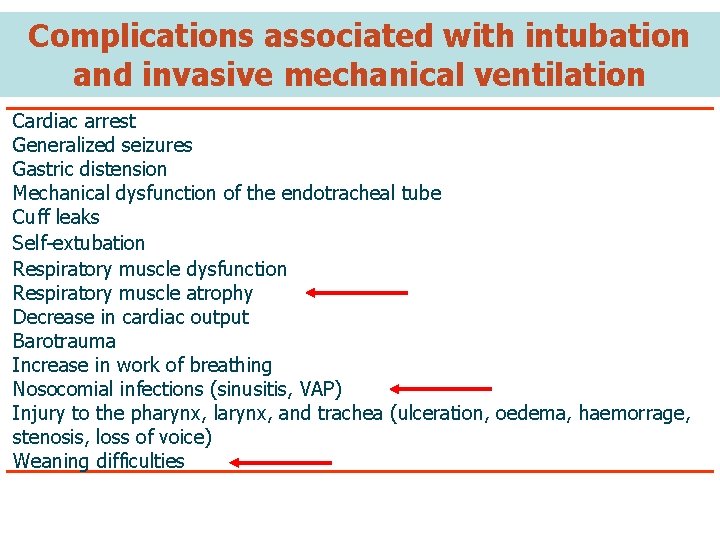
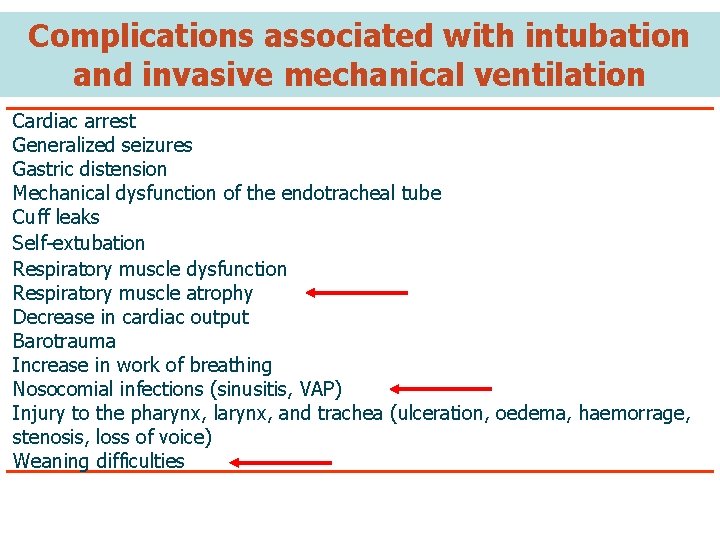
Complications associated with intubation and invasive mechanical ventilation Cardiac arrest Generalized seizures Gastric distension Mechanical dysfunction of the endotracheal tube Cuff leaks Self-extubation Respiratory muscle dysfunction Respiratory muscle atrophy Decrease in cardiac output Barotrauma Increase in work of breathing Nosocomial infections (sinusitis, VAP) Injury to the pharynx, larynx, and trachea (ulceration, oedema, haemorrage, stenosis, loss of voice) Weaning difficulties
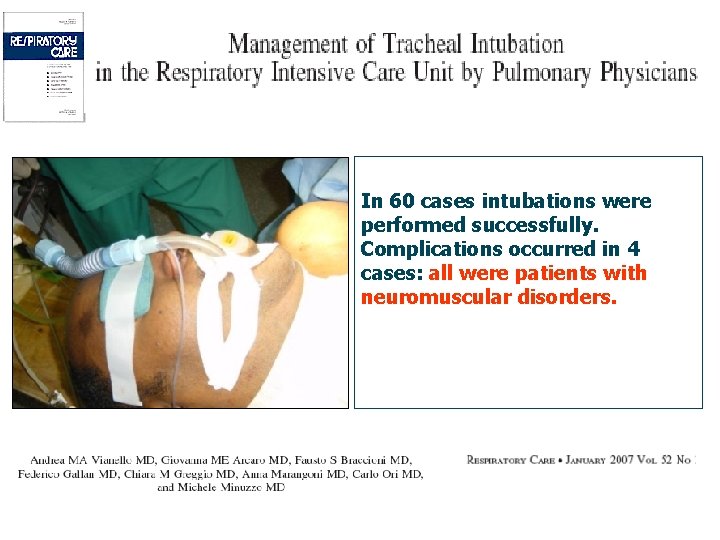
In 60 cases intubations were performed successfully. Complications occurred in 4 cases: all were patients with neuromuscular disorders.
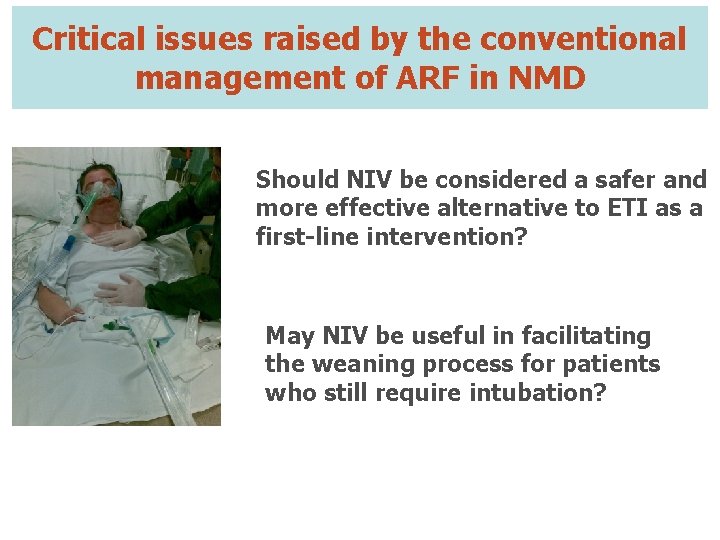
Critical issues raised by the conventional management of ARF in NMD Should NIV be considered a safer and more effective alternative to ETI as a first-line intervention? May NIV be useful in facilitating the weaning process for patients who still require intubation?
NIV as a first-line intervention for Acute Respiratory Failure
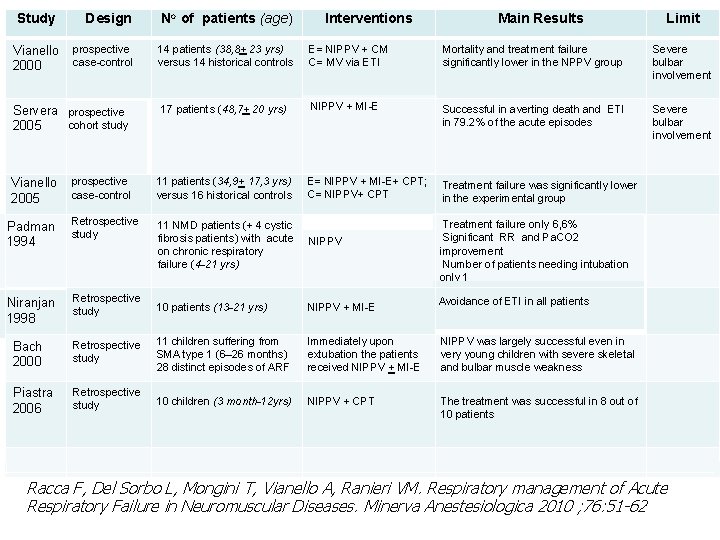
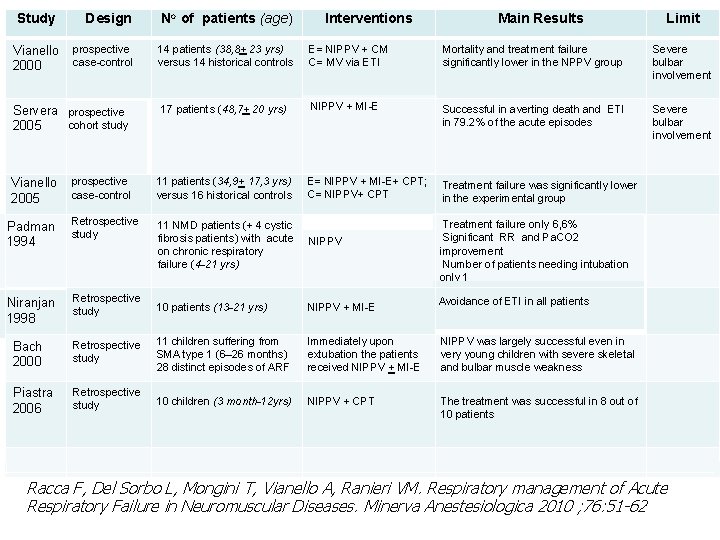
Study Vianello 2000 Design No of patients (age) prospective case-control 14 patients (38, 8+ 23 yrs) versus 14 historical controls E= NIPPV + CM C= MV via ETI Mortality and treatment failure significantly lower in the NPPV group Severe bulbar involvement 17 patients (48, 7+ 20 yrs) NIPPV + MI-E Successful in averting death and ETI in 79. 2% of the acute episodes Severe bulbar involvement E= NIPPV + MI-E+ CPT; C= NIPPV+ CPT Treatment failure was significantly lower in the experimental group Servera prospective cohort study 2005 Interventions Main Results prospective case-control 11 patients (34, 9+ 17, 3 yrs) versus 16 historical controls Padman 1994 Retrospective study 11 NMD patients (+ 4 cystic fibrosis patients) with acute on chronic respiratory failure (4 -21 yrs) NIPPV Niranjan 1998 Retrospective study 10 patients (13 -21 yrs) NIPPV + MI-E Bach 2000 Retrospective study 11 children suffering from SMA type 1 (6– 26 months) 28 distinct episodes of ARF Immediately upon extubation the patients received NIPPV + MI-E NIPPV was largely successful even in very young children with severe skeletal and bulbar muscle weakness Piastra 2006 Retrospective study 10 children (3 month-12 yrs) NIPPV + CPT The treatment was successful in 8 out of 10 patients Vianello 2005 Limit Treatment failure only 6, 6% Significant RR and Pa. CO 2 improvement Number of patients needing intubation only 1 Avoidance of ETI in all patients Racca F, Del Sorbo L, Mongini T, Vianello A, Ranieri VM. Respiratory management of Acute Respiratory Failure in Neuromuscular Diseases. Minerva Anestesiologica 2010 ; 76: 51 -62
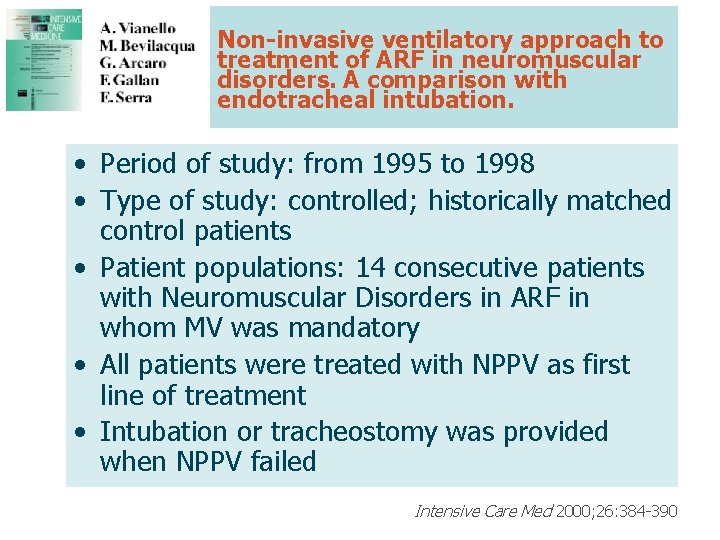
Non-invasive ventilatory approach to treatment of ARF in neuromuscular disorders. A comparison with endotracheal intubation. • Period of study: from 1995 to 1998 • Type of study: controlled; historically matched control patients • Patient populations: 14 consecutive patients with Neuromuscular Disorders in ARF in whom MV was mandatory • All patients were treated with NPPV as first line of treatment • Intubation or tracheostomy was provided when NPPV failed Intensive Care Med 2000; 26: 384 -390
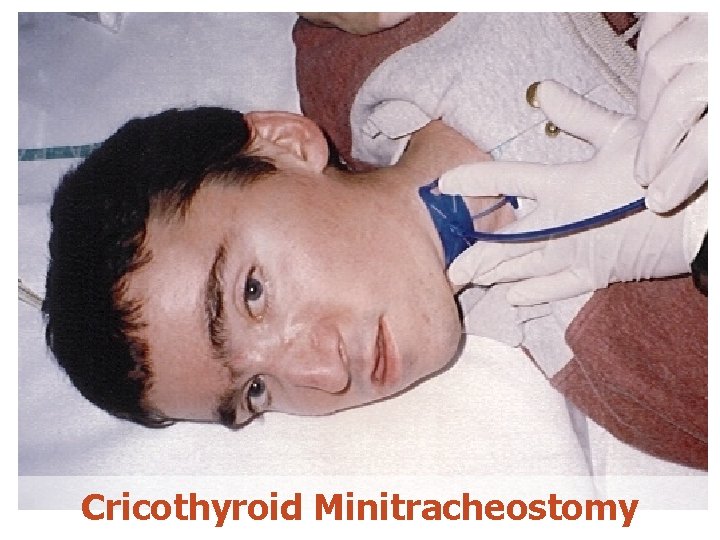
Cricothyroid Minitracheostomy

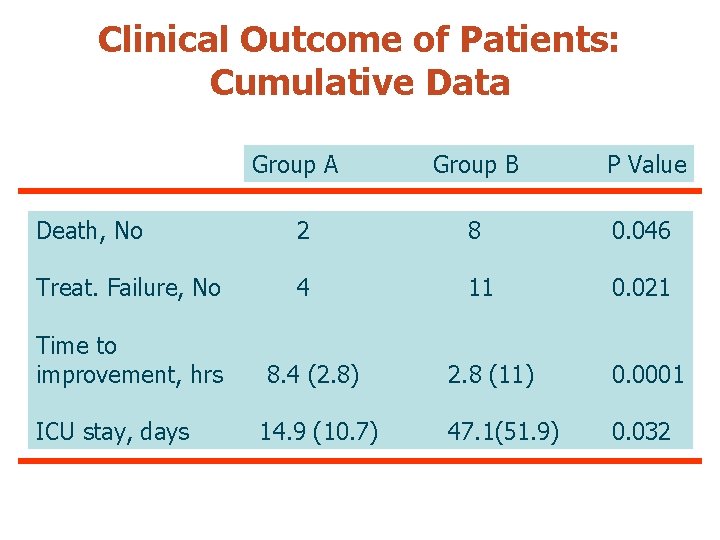
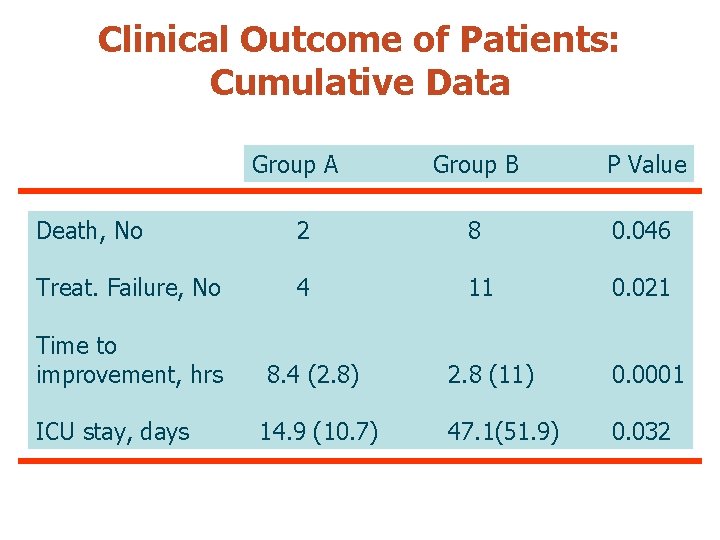
Clinical Outcome of Patients: Cumulative Data Group A Group B P Value Death, No 2 8 0. 046 Treat. Failure, No 4 11 0. 021 Time to improvement, hrs ICU stay, days 8. 4 (2. 8) 14. 9 (10. 7) 2. 8 (11) 0. 0001 47. 1(51. 9) 0. 032
Non-invasive ventilatory approach to treatment of ARF in neuromuscular disorders. A comparison with endotracheal intubation. Conclusions • The application of NIV tends to reduce mortality and treatment failure in comparison with PPV via ETI • The use of NIV combined with cricothyroid "minitracheostomy” in neuromuscular ARF could be extended to patients with ineffective cough • However, the ability to adequately protect the upper airway is crucial to the success and patient selection remains important Intensive Care Med 2000; 26: 384 -390
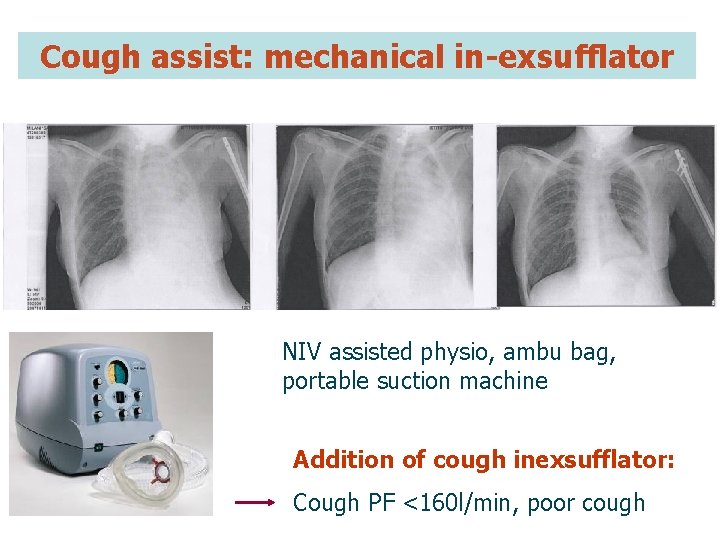
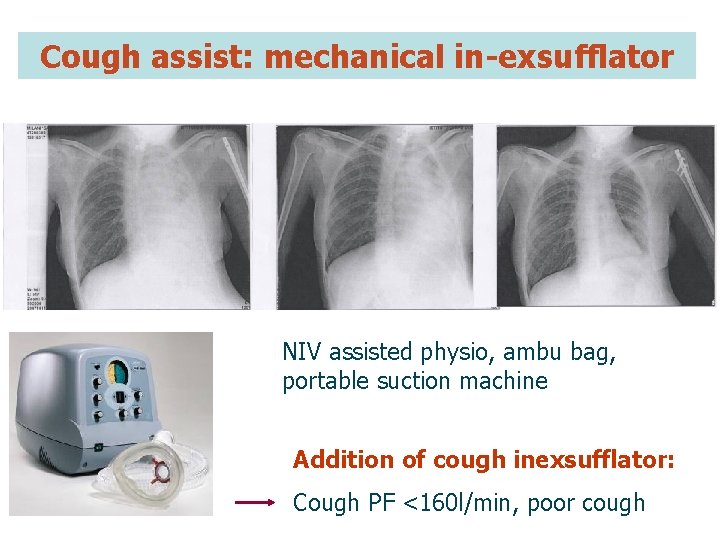
Cough assist: mechanical in-exsufflator NIV assisted physio, ambu bag, portable suction machine Addition of cough inexsufflator: Cough PF <160 l/min, poor cough
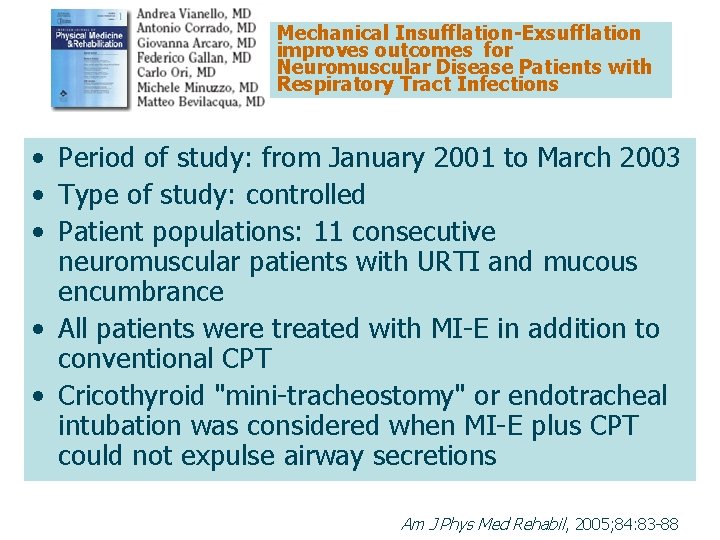
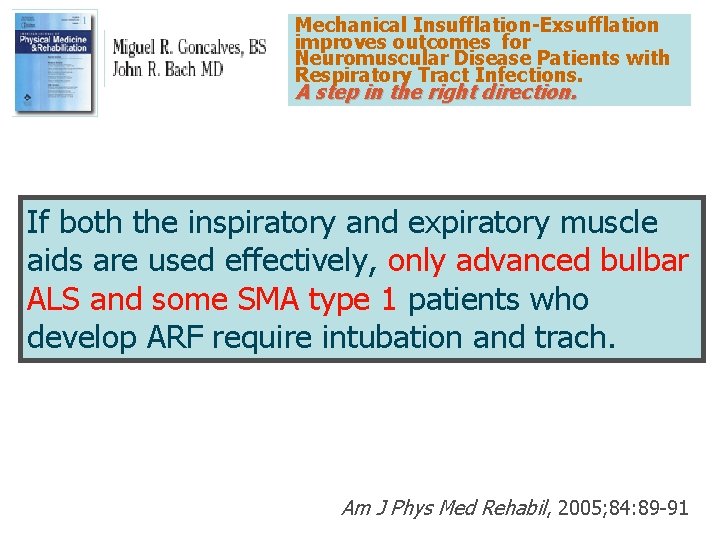
Mechanical Insufflation-Exsufflation improves outcomes for Neuromuscular Disease Patients with Respiratory Tract Infections Am J Phys Med Rehabil, 2005; 84: 83 -88
Mechanical Insufflation-Exsufflation improves outcomes for Neuromuscular Disease Patients with Respiratory Tract Infections • Period of study: from January 2001 to March 2003 • Type of study: controlled • Patient populations: 11 consecutive neuromuscular patients with URTI and mucous encumbrance • All patients were treated with MI-E in addition to conventional CPT • Cricothyroid "mini-tracheostomy" or endotracheal intubation was considered when MI-E plus CPT could not expulse airway secretions Am J Phys Med Rehabil, 2005; 84: 83 -88
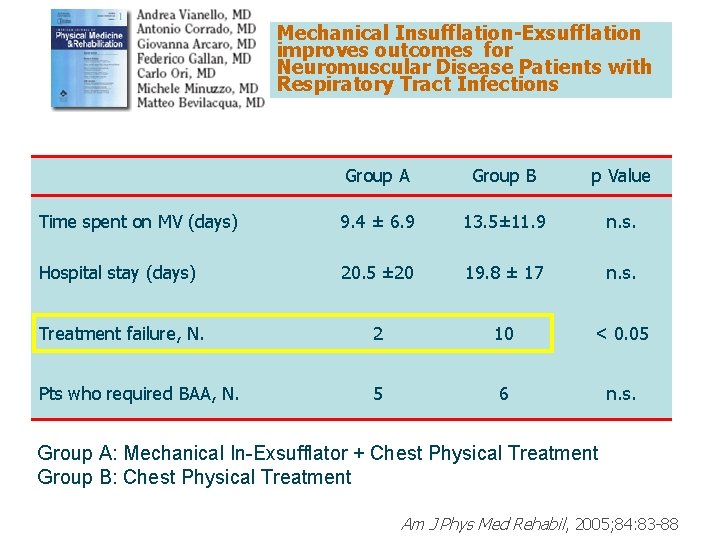
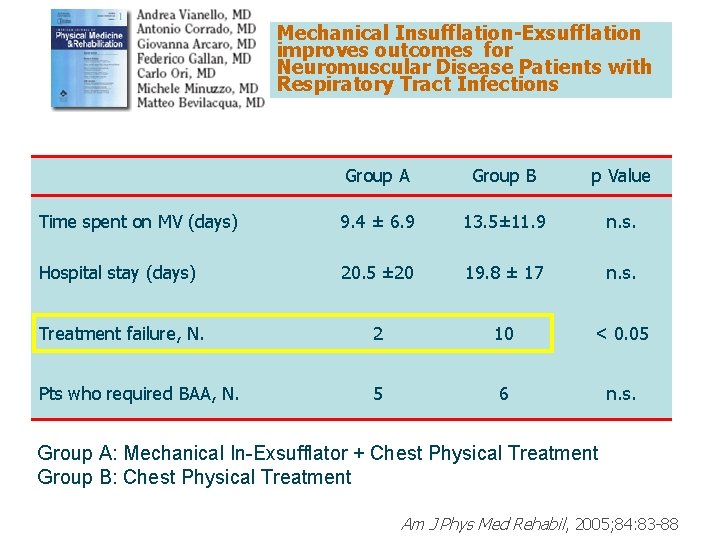
Mechanical Insufflation-Exsufflation improves outcomes for Neuromuscular Disease Patients with Respiratory Tract Infections Group A Group B p Value Time spent on MV (days) 9. 4 ± 6. 9 13. 5± 11. 9 n. s. Hospital stay (days) 20. 5 ± 20 19. 8 ± 17 n. s. Treatment failure, N. 2 10 < 0. 05 Pts who required BAA, N. 5 6 n. s. Group A: Mechanical In-Exsufflator + Chest Physical Treatment Group B: Chest Physical Treatment Am J Phys Med Rehabil, 2005; 84: 83 -88
Mechanical Insufflation-Exsufflation improves outcomes for Neuromuscular Disease Patients with Respiratory Tract Infections. A step in the right direction. If both the inspiratory and expiratory muscle aids are used effectively, only advanced bulbar ALS and some SMA type 1 patients who develop ARF require intubation and trach. Am J Phys Med Rehabil, 2005; 84: 89 -91
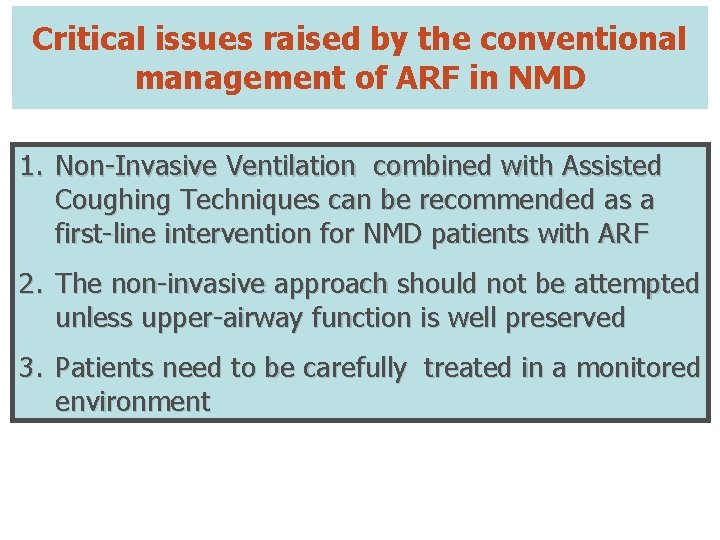
Critical issues raised by the conventional management of ARF in NMD 1. Non-Invasive Ventilation combined with Assisted Coughing Techniques can be recommended as a Should NIV befor considered a with ARF first-line intervention NMD patients safer and more effective 2. The non-invasive should not be attempted alternativeapproach to ETI as a firstunlessline upper-airway function is well preserved intervention? 3. Patients need to be carefully treated in a monitored environment ?
NIV in the Weaning Process

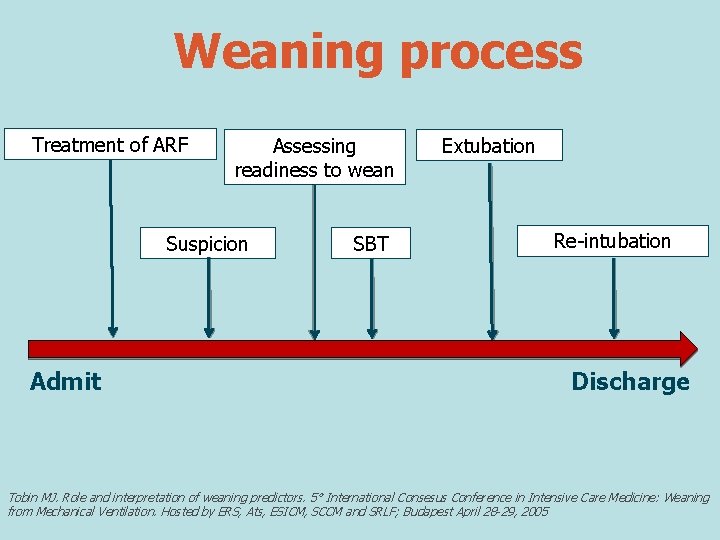
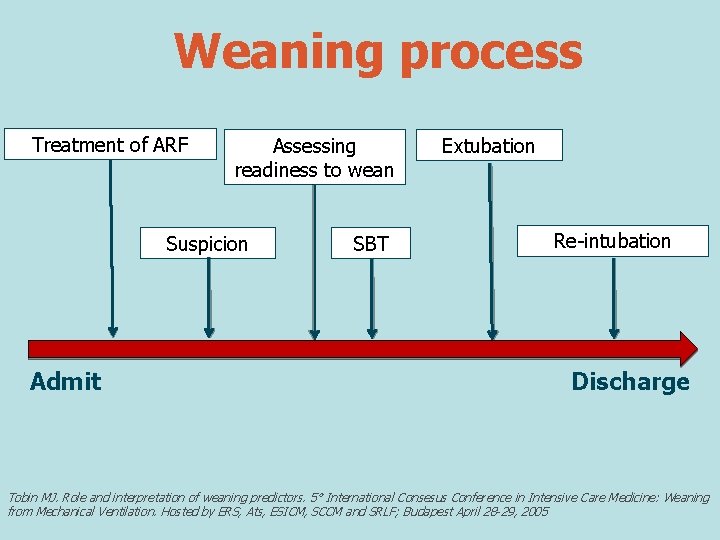
Weaning process Treatment of ARF Assessing readiness to wean Suspicion Admit SBT Extubation Re-intubation Discharge Tobin MJ. Role and interpretation of weaning predictors. 5° International Consesus Conference in Intensive Care Medicine: Weaning from Mechanical Ventilation. Hosted by ERS, Ats, ESICM, SCCM and SRLF; Budapest April 28 -29, 2005
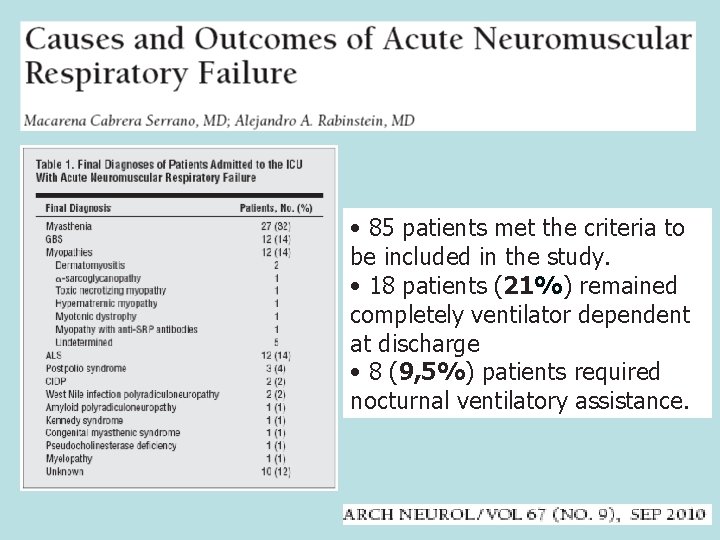
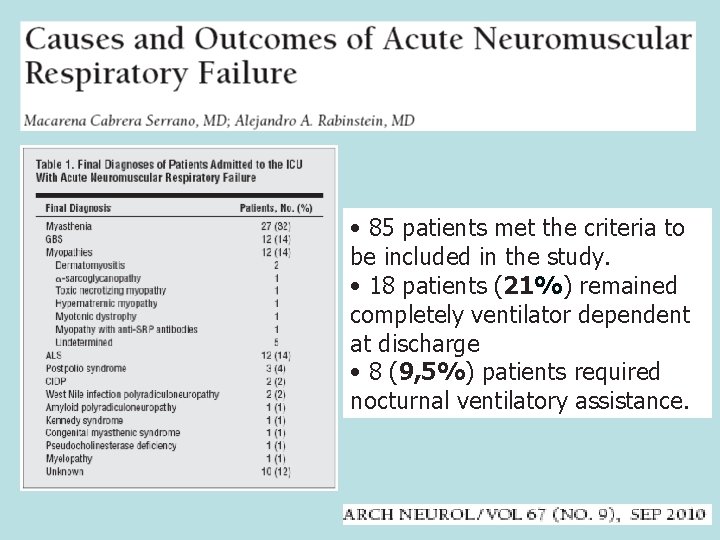
• 85 patients met the criteria to be included in the study. • 18 patients (21%) remained completely ventilator dependent at discharge • 8 (9, 5%) patients required nocturnal ventilatory assistance.
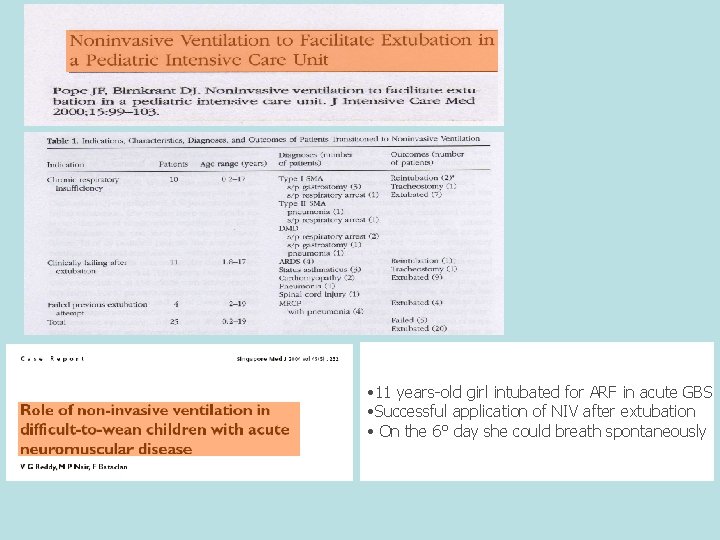
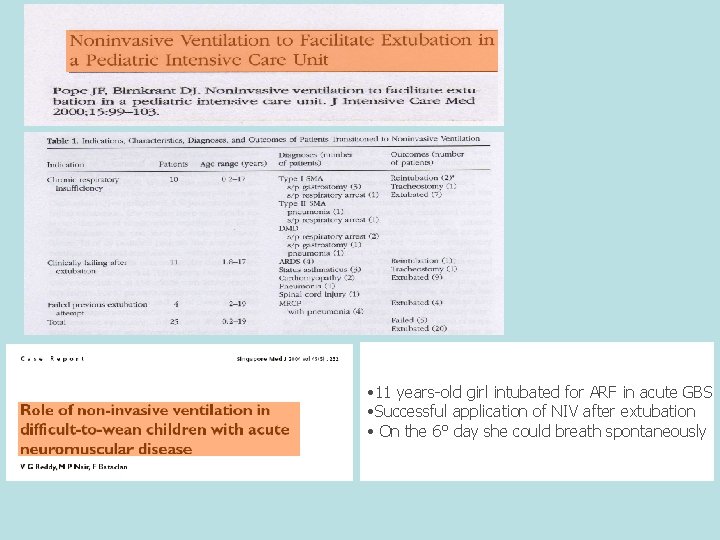
• 11 years-old girl intubated for ARF in acute GBS • Successful application of NIV after extubation • On the 6° day she could breath spontaneously
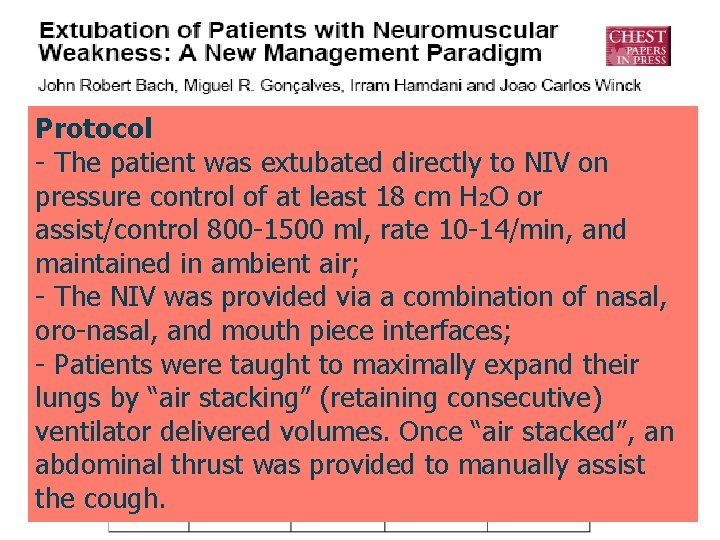
Protocol - The patient was extubated directly to NIV on pressure control of at least 18 cm H 2 O or assist/control 800 -1500 ml, rate 10 -14/min, and maintained in ambient air; - The NIV was provided via a combination of nasal, oro-nasal, and mouth piece interfaces; - Patients were taught to maximally expand their lungs by “air stacking” (retaining consecutive) ventilator delivered volumes. Once “air stacked”, an abdominal thrust was provided to manually assist the cough.
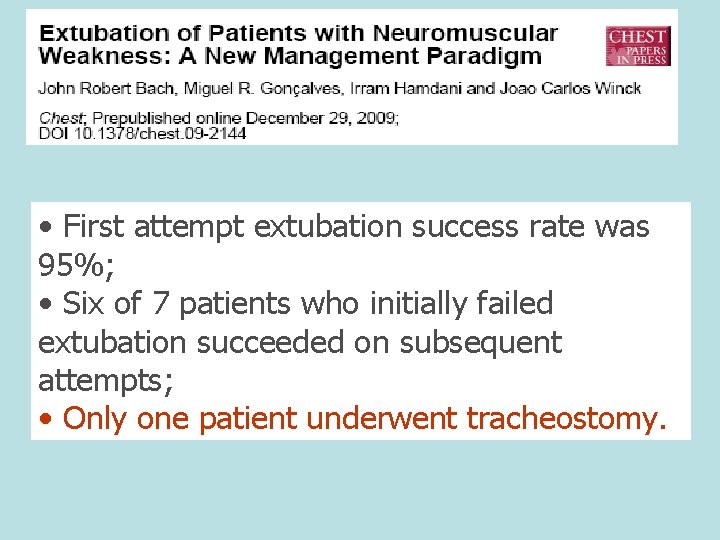
• First attempt extubation success rate was 95%; • Six of 7 patients who initially failed extubation succeeded on subsequent attempts; • Only one patient underwent tracheostomy.
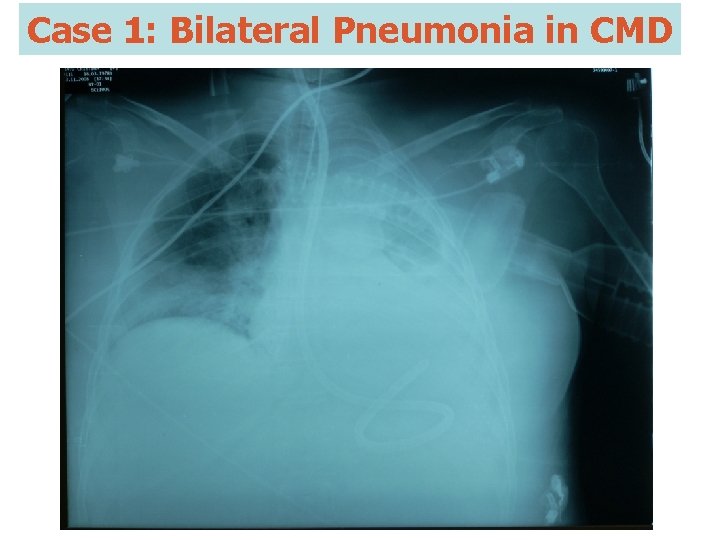
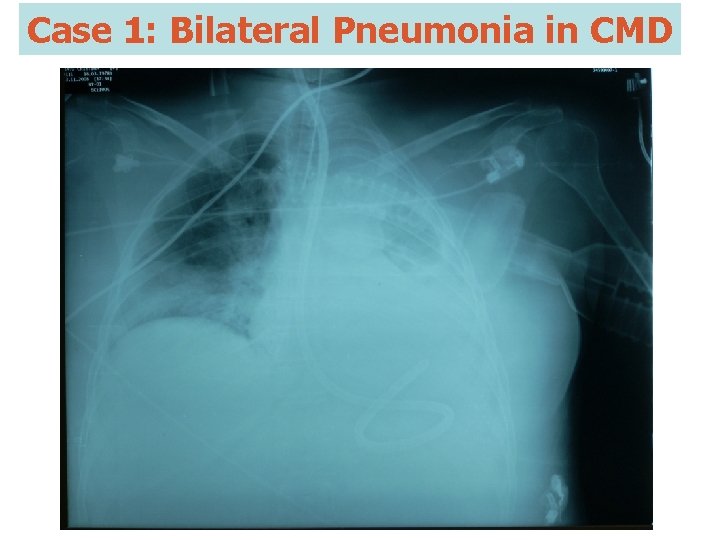
Case 1: Bilateral Pneumonia in CMD

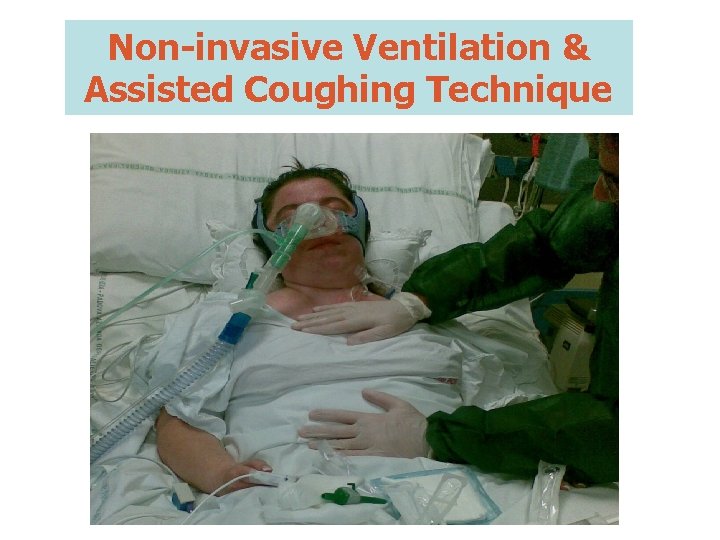
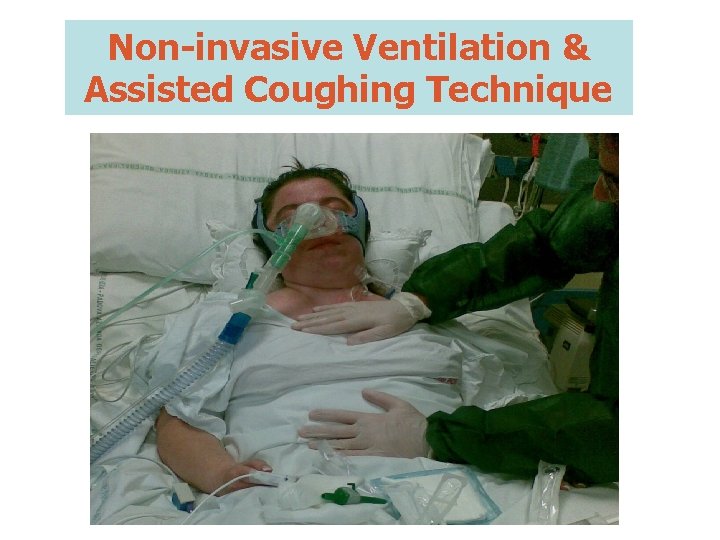
Non-invasive Ventilation & Assisted Coughing Technique
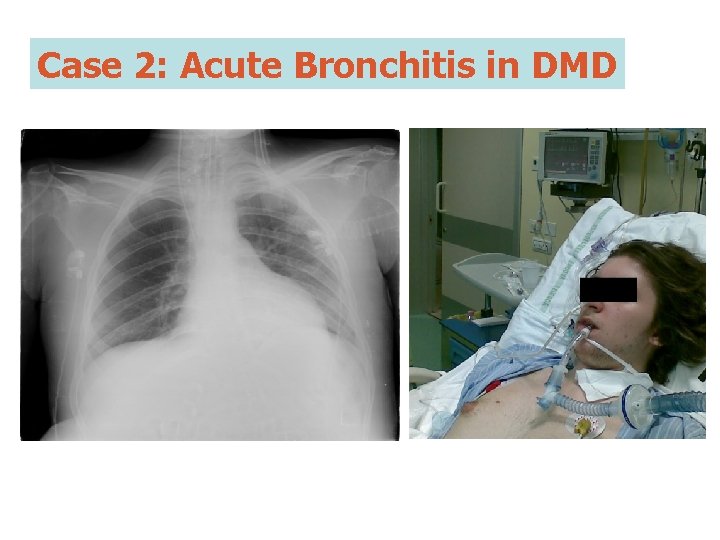
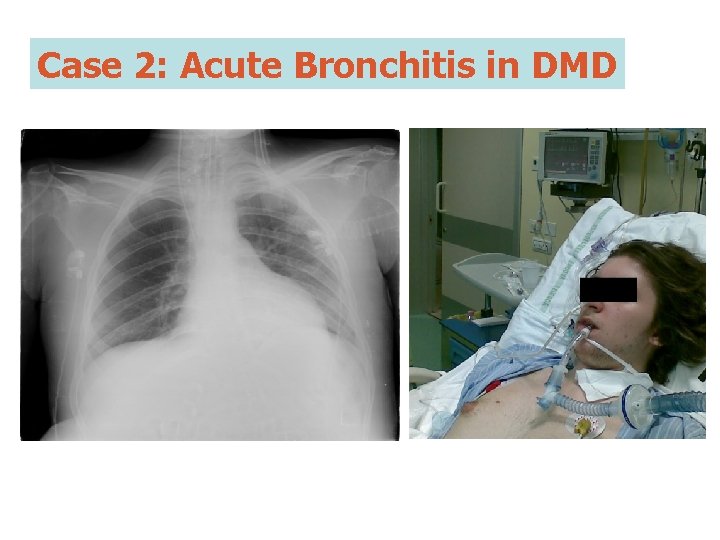
Case 2: Acute Bronchitis in DMD

PCF : 80 L/min MEP: 20 cm. H 2 O MIP: -18 cm. H 2 O


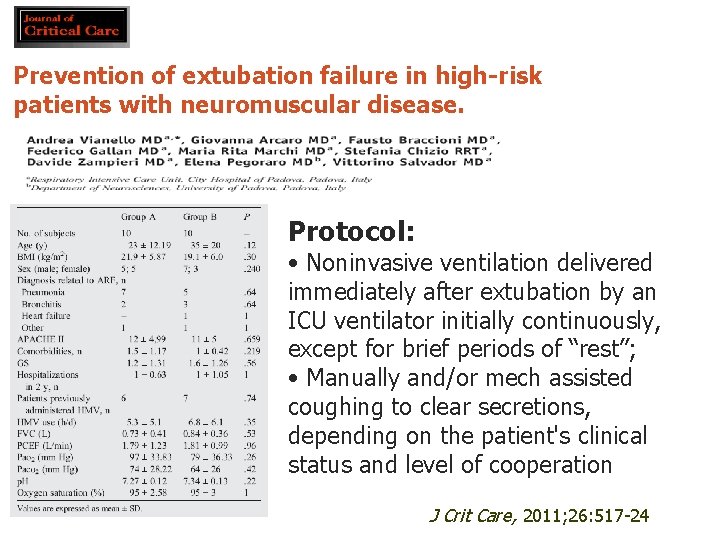
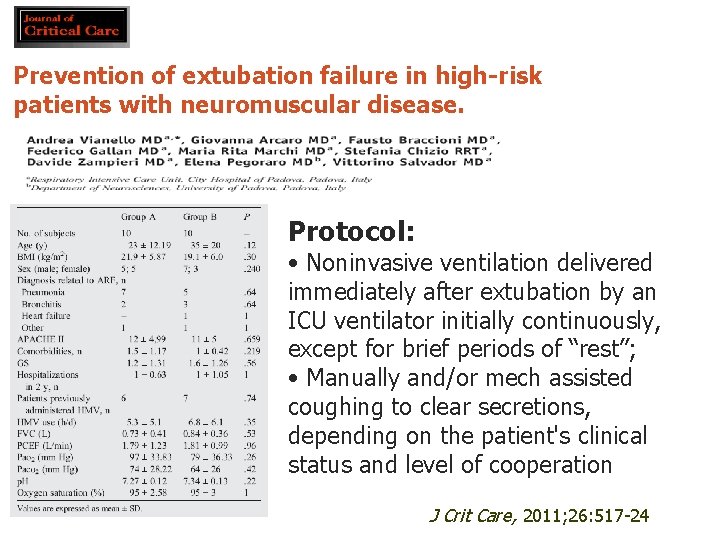
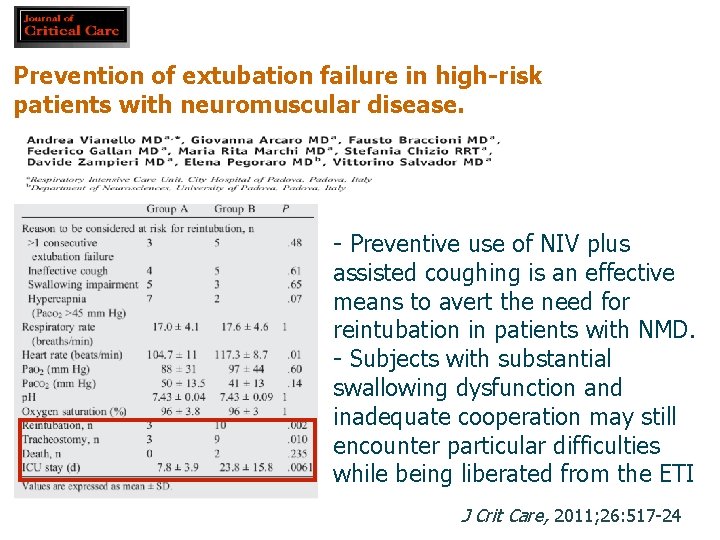
Prevention of extubation failure in high-risk patients with neuromuscular disease. Protocol: • Noninvasive ventilation delivered immediately after extubation by an ICU ventilator initially continuously, except for brief periods of “rest”; • Manually and/or mech assisted coughing to clear secretions, depending on the patient's clinical status and level of cooperation J Crit Care, 2011; 26: 517 -24
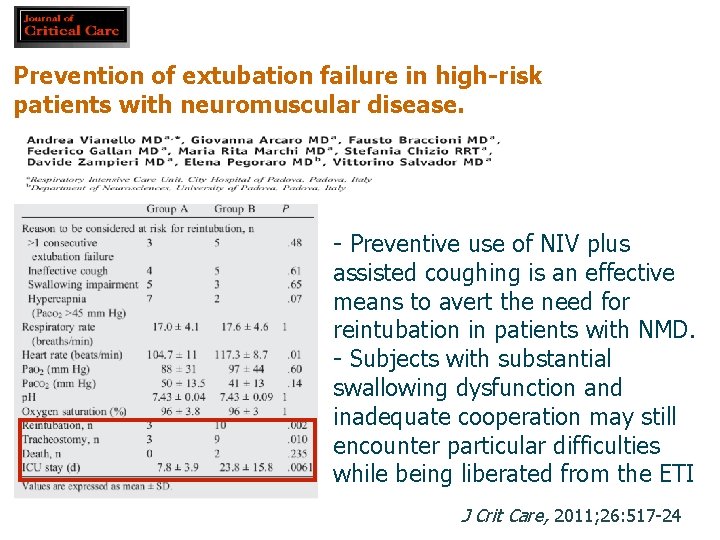
Prevention of extubation failure in high-risk patients with neuromuscular disease. - Preventive use of NIV plus assisted coughing is an effective means to avert the need for reintubation in patients with NMD. - Subjects with substantial swallowing dysfunction and inadequate cooperation may still encounter particular difficulties while being liberated from the ETI J Crit Care, 2011; 26: 517 -24
We believe that the ability to adequately protect the upper airway is crucial to the success and safety of the weaning process and that extubation remains problematic for a significant proportion of patients with neuromyopathic conditions because of the May NIV be useful in facilitating the weaning process for severe risk of aspiration ofintubation? food and saliva. patients who still require
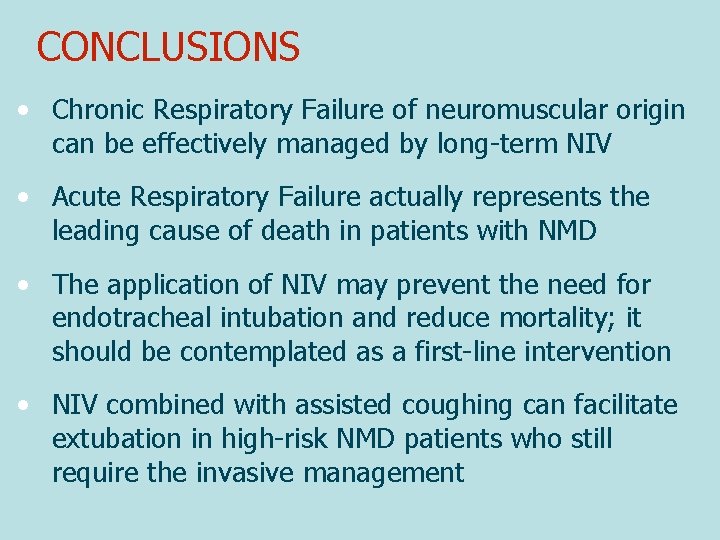
CONCLUSIONS • Chronic Respiratory Failure of neuromuscular origin can be effectively managed by long-term NIV • Acute Respiratory Failure actually represents the leading cause of death in patients with NMD • The application of NIV may prevent the need for endotracheal intubation and reduce mortality; it should be contemplated as a first-line intervention • NIV combined with assisted coughing can facilitate extubation in high-risk NMD patients who still require the invasive management
 Acido sulfridico
Acido sulfridico Dispnea malato terminale
Dispnea malato terminale Pulmonary hypertension
Pulmonary hypertension Pneumotrieste
Pneumotrieste Pneumotrieste
Pneumotrieste Pneumotrieste
Pneumotrieste Pneumotrieste
Pneumotrieste Mogans cevicheria
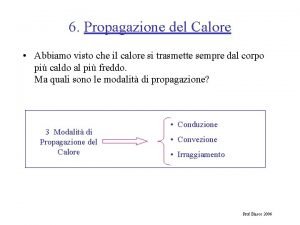
Mogans cevicheria Propagazione per irraggiamento
Propagazione per irraggiamento Trasformare un'equazione in forma esplicita
Trasformare un'equazione in forma esplicita Comandamenti del bullone
Comandamenti del bullone Flessura splenica
Flessura splenica Equivalente meccanico della caloria relazione
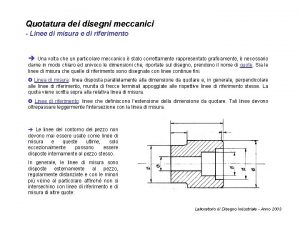
Equivalente meccanico della caloria relazione Disegni meccanici esempi
Disegni meccanici esempi Cerchio parallelo al pv
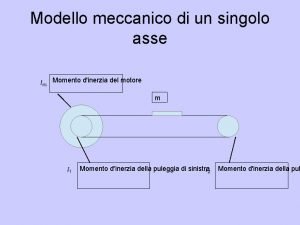
Cerchio parallelo al pv Modello meccanico
Modello meccanico 4 186 joule
4 186 joule Esempi di quotatura
Esempi di quotatura Dispositivi antisvitamento
Dispositivi antisvitamento Disegni pezzi meccanici quotati
Disegni pezzi meccanici quotati Guadagno meccanico leve
Guadagno meccanico leve Come come emmanuel son of god appear
Come come emmanuel son of god appear Forgive past and past participle
Forgive past and past participle Come mi vedo io come mi vedono gli altri
Come mi vedo io come mi vedono gli altri Hey, come on out
Hey, come on out Come mi chiamo?
Come mi chiamo? Come in and sit down
Come in and sit down Come thou fount come thou king lyrics
Come thou fount come thou king lyrics Through all generations everlasting is his mercy
Through all generations everlasting is his mercy Get in touch with god turn your radio on
Get in touch with god turn your radio on Come in come in and sit down
Come in come in and sit down Subject + have/has + verb in past participle + complement
Subject + have/has + verb in past participle + complement Softly and tenderly jesus is calling
Softly and tenderly jesus is calling Come mi chiamo come mi chiamo
Come mi chiamo come mi chiamo Come holy ghost lyrics
Come holy ghost lyrics Struttura divina commedia purgatorio
Struttura divina commedia purgatorio Osmolarità
Osmolarità 10 frasi con il periodo ipotetico della realtà
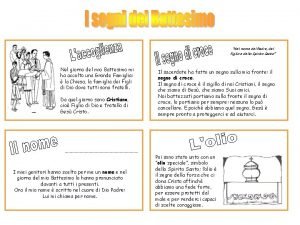
10 frasi con il periodo ipotetico della realtà Nome del padre del figlio e dello spirito santo
Nome del padre del figlio e dello spirito santo Tecniche narrative schema
Tecniche narrative schema La stregoneria nel medioevo
La stregoneria nel medioevo Lo spazio e il tempo nel testo narrativo
Lo spazio e il tempo nel testo narrativo Nato nel 1785
Nato nel 1785 Noddings philosophy of education
Noddings philosophy of education śladami stasia i nel mapa
śladami stasia i nel mapa Correnti convettive nel mantello
Correnti convettive nel mantello Commento ne li occhi porta la mia donna amore
Commento ne li occhi porta la mia donna amore Permeabilità magnetica nel vuoto
Permeabilità magnetica nel vuoto Alice eve measurement
Alice eve measurement Dal selvaggio rosaio scheletrito
Dal selvaggio rosaio scheletrito Eccessiva citolisi nel pap test
Eccessiva citolisi nel pap test Sequenze testo narrativo
Sequenze testo narrativo Teatro nel teatro significato
Teatro nel teatro significato Viaggio nel cosmo
Viaggio nel cosmo Centinaia di milioni
Centinaia di milioni