Pediatric Procedural Sedation Dr Marc N Francis MD








- Slides: 79

Pediatric Procedural Sedation Dr. Marc N. Francis MD, FRCPC University of Calgary Foothills Medical Centre Alberta Children’s Hospital
Disclosure I do not have an affiliation (financial or otherwise) with any commercial organization that may have a direct or indirect connection to the content of my presentation.
PSA in the ED n n “Painful procedures are unavoidable in emergency medicine” “While anesthesiologists have unique qualifications to provide sedation, their availability is variable and unreliable, and is limited by commitments to the operating room” Procedural Sedation and Analgesia in the Emergency Department. Canadian Consensus Guidelines Journal of Emergency Medicine 1999; 17(1): 145 -156
Learning Objectives n “Tools of the Trade” n n “The Right Tool for the Job” n n Some adjuncts and techniques that will make your job easier Controversies n n Discuss the variable needs for procedural sedation in the ED and pharmaceutical options “Tricks of the Trade” n n Sedation medications that you should know well and be familiar with A look at some of the more controversial aspects of procedural sedation in children The Future n What is coming down the pipe for the future of procedural sedation

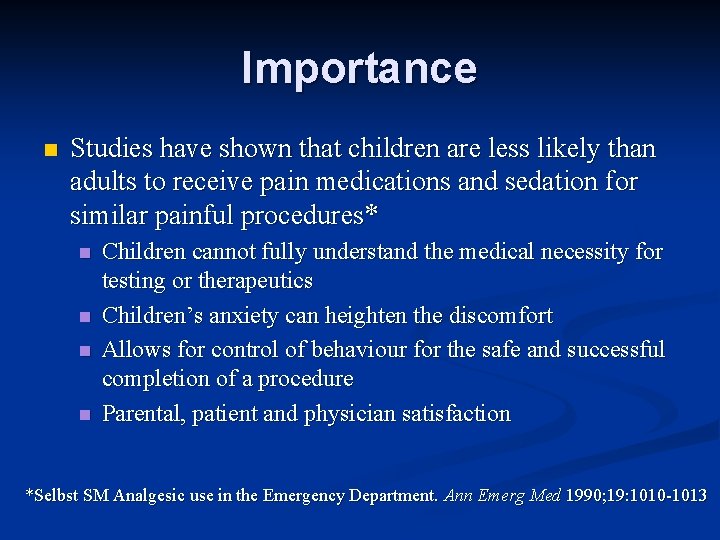
Importance n Studies have shown that children are less likely than adults to receive pain medications and sedation for similar painful procedures* n n Children cannot fully understand the medical necessity for testing or therapeutics Children’s anxiety can heighten the discomfort Allows for control of behaviour for the safe and successful completion of a procedure Parental, patient and physician satisfaction *Selbst SM Analgesic use in the Emergency Department. Ann Emerg Med 1990; 19: 1010 -1013
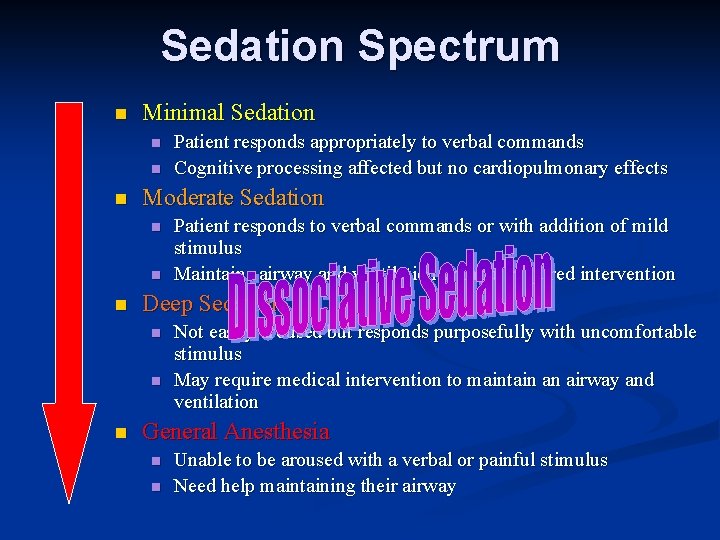
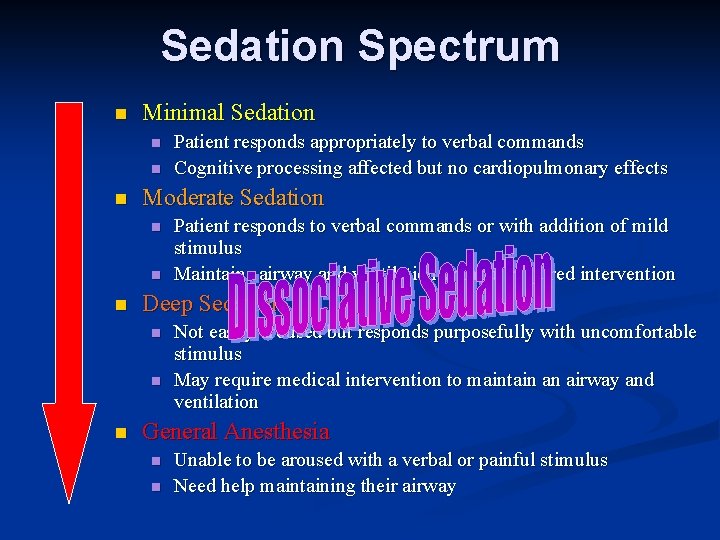
Sedation Spectrum n Minimal Sedation n Moderate Sedation n Patient responds to verbal commands or with addition of mild stimulus Maintains airway and ventilation without required intervention Deep Sedation n Patient responds appropriately to verbal commands Cognitive processing affected but no cardiopulmonary effects Not easily aroused but responds purposefully with uncomfortable stimulus May require medical intervention to maintain an airway and ventilation General Anesthesia n n Unable to be aroused with a verbal or painful stimulus Need help maintaining their airway
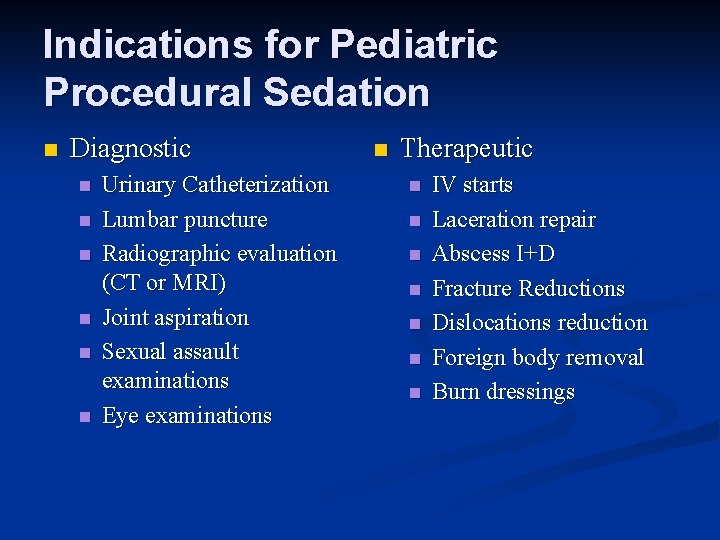
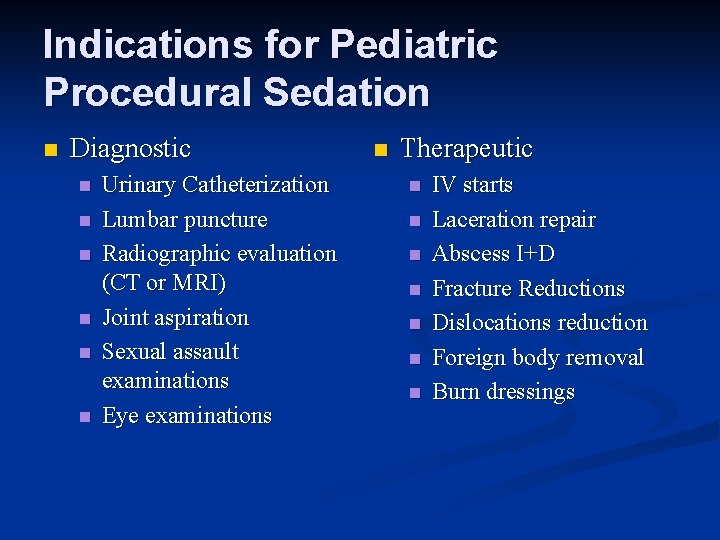
Indications for Pediatric Procedural Sedation n Diagnostic n n n Urinary Catheterization Lumbar puncture Radiographic evaluation (CT or MRI) Joint aspiration Sexual assault examinations Eye examinations n Therapeutic n n n n IV starts Laceration repair Abscess I+D Fracture Reductions Dislocations reduction Foreign body removal Burn dressings
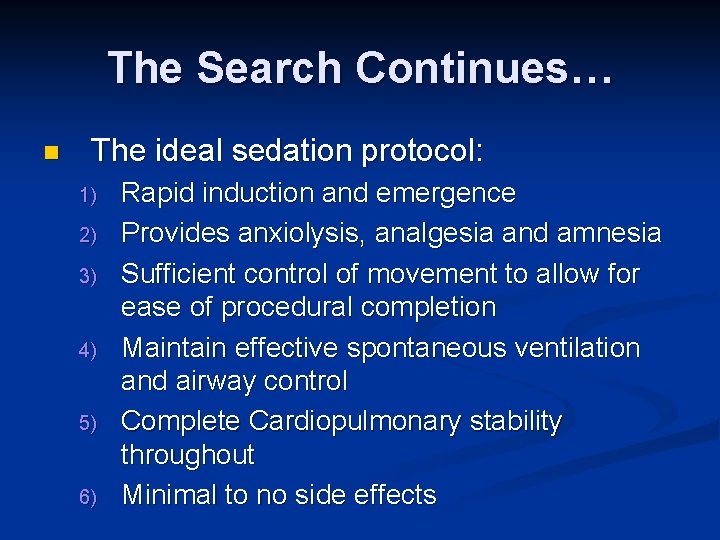
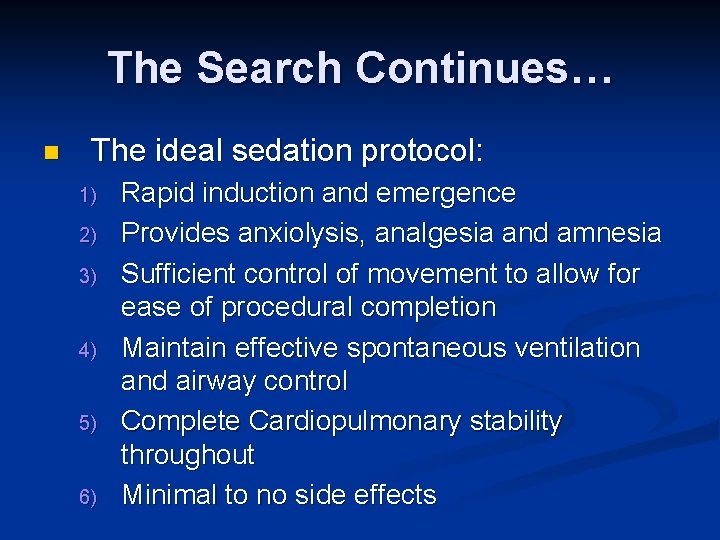
The Search Continues… n The ideal sedation protocol: 1) 2) 3) 4) 5) 6) Rapid induction and emergence Provides anxiolysis, analgesia and amnesia Sufficient control of movement to allow for ease of procedural completion Maintain effective spontaneous ventilation and airway control Complete Cardiopulmonary stability throughout Minimal to no side effects
“Tools of the Trade”
Nitrous Oxide n n n Dissociative gas with mild to moderate procedural anxiolysis, analgesia and amnesia Dosage n n 50% concentration blended with oxygen Ideally self administered Advantages n n n Onset and offset within 5 mins Does not require an IV Disadvantages n n n Requires special delivery device Nausea and Vomiting Well ventilated room with scavenger system
Midazolam n n Short-acting agent with rapid onset of anxiolysis, sedative and amnestic properties n n Interacts with GABA receptors in the brain Dosage n n 0. 2 -0. 6 mg/kg intranasally 0. 05 -0. 2 mg/kg IV 0. 1 -0. 2 mg/kg IM 0. 5 -0. 75 mg/kg PO Advantages n n n Rapid onset Anxiolysis Profound retrograde amnesia No IV required Disadvantages n n n Does not provide analgesia Disturbance in respiratory function +/- hypoxemia Paradoxical reactions
Fentanyl n n n Synthetic opiod which is narcotic of choice in PSA n Rapid onset and short duration make it easy to titrate Does not cause histamine release so minimal CV effects Dosage n n 1 -3 mcg/kg IM or IV 10 -20 mcg/kg oral or Advantages n n n Excellent analgesic Peak effect within 15 -30 mins Reversible with naloxone Disadvantages n n n Nausea and vomiting Respiratory depression Hypotension No amnesia. Minimal sedation Fentanyl Rigid Chest
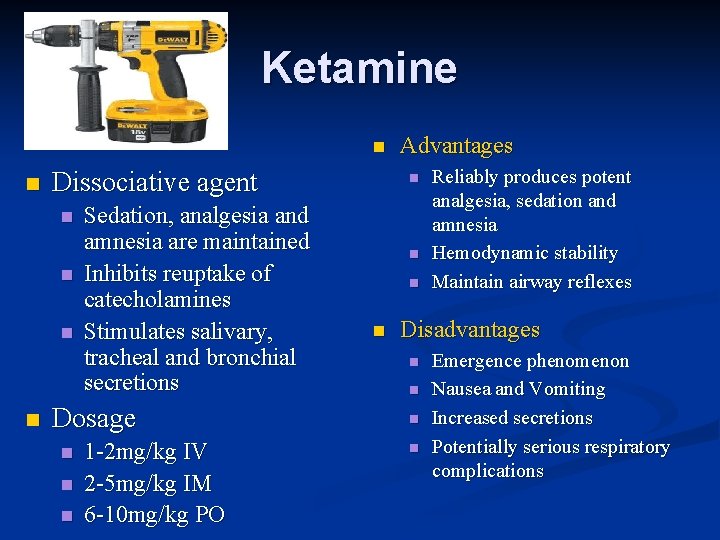
Ketamine n n Dissociative agent n n Sedation, analgesia and amnesia are maintained Inhibits reuptake of catecholamines Stimulates salivary, tracheal and bronchial secretions Dosage n n n 1 -2 mg/kg IV 2 -5 mg/kg IM 6 -10 mg/kg PO Advantages n n Reliably produces potent analgesia, sedation and amnesia Hemodynamic stability Maintain airway reflexes Disadvantages n n Emergence phenomenon Nausea and Vomiting Increased secretions Potentially serious respiratory complications
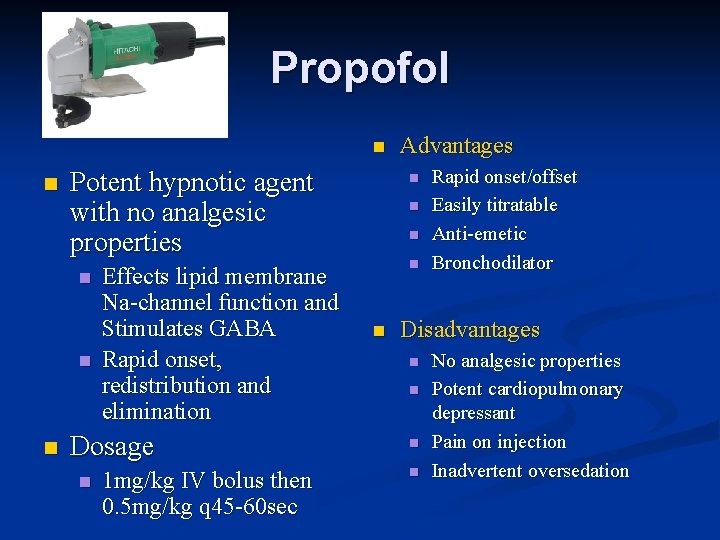
Propofol n n Potent hypnotic agent with no analgesic properties n n n Effects lipid membrane Na-channel function and Stimulates GABA Rapid onset, redistribution and elimination Dosage n 1 mg/kg IV bolus then 0. 5 mg/kg q 45 -60 sec Advantages n n n Rapid onset/offset Easily titratable Anti-emetic Bronchodilator Disadvantages n n No analgesic properties Potent cardiopulmonary depressant Pain on injection Inadvertent oversedation
“The Right Tool for the Job”
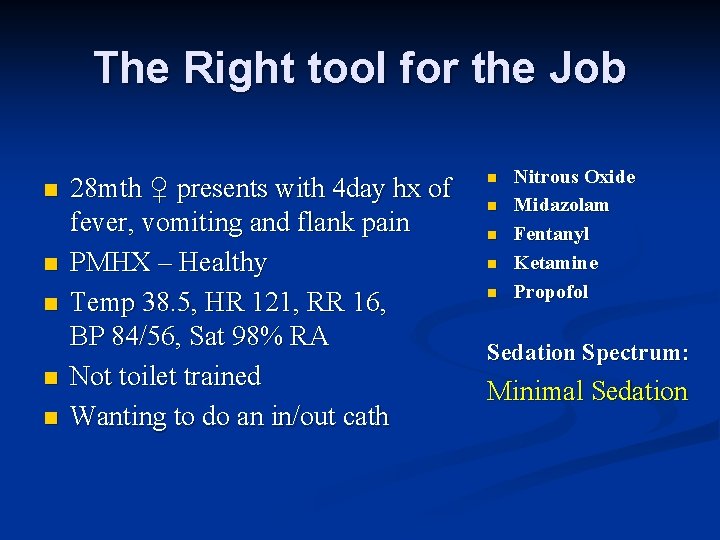
The Right tool for the Job n n n 28 mth ♀ presents with 4 day hx of fever, vomiting and flank pain PMHX – Healthy Temp 38. 5, HR 121, RR 16, BP 84/56, Sat 98% RA Not toilet trained Wanting to do an in/out cath n n n Nitrous Oxide Midazolam Fentanyl Ketamine Propofol Sedation Spectrum: Minimal Sedation
The Right tool for the Job n n 5 yo ♂ fell onto wooden post Extensive and complex facial laceration requiring multilayer closure PMHX – Asthma well controlled VSSA n n n Nitrous Oxide Midazolam Fentanyl Ketamine Propofol Sedation Spectrum: Dissociative Sedation

The Right tool for the Job n n n 15 yo ♂ playing soccer and collided with another player Immediate pain to R shoulder which is clinically consistent with anterior dislocation Very Anxious!!! PMHX – Healthy Normal Vital signs n n n Nitrous Oxide Midazolam Fentanyl Ketamine Propofol Sedation Spectrum: Moderate Sedation
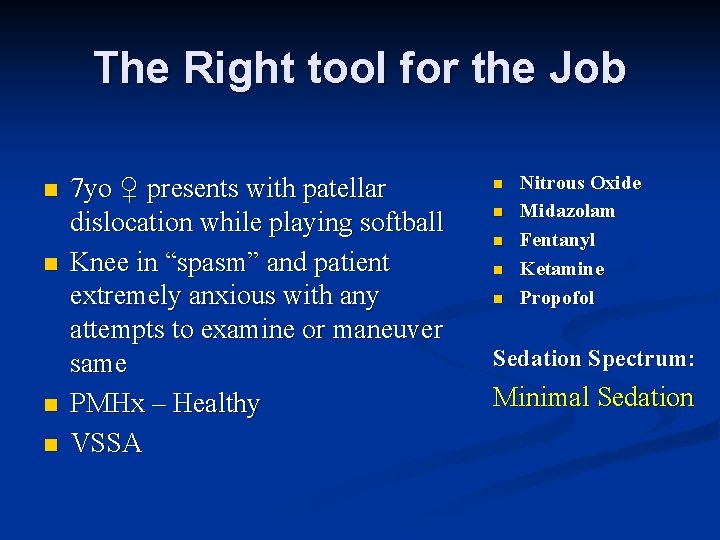
The Right tool for the Job n n 7 yo ♀ presents with patellar dislocation while playing softball Knee in “spasm” and patient extremely anxious with any attempts to examine or maneuver same PMHx – Healthy VSSA n n n Nitrous Oxide Midazolam Fentanyl Ketamine Propofol Sedation Spectrum: Minimal Sedation
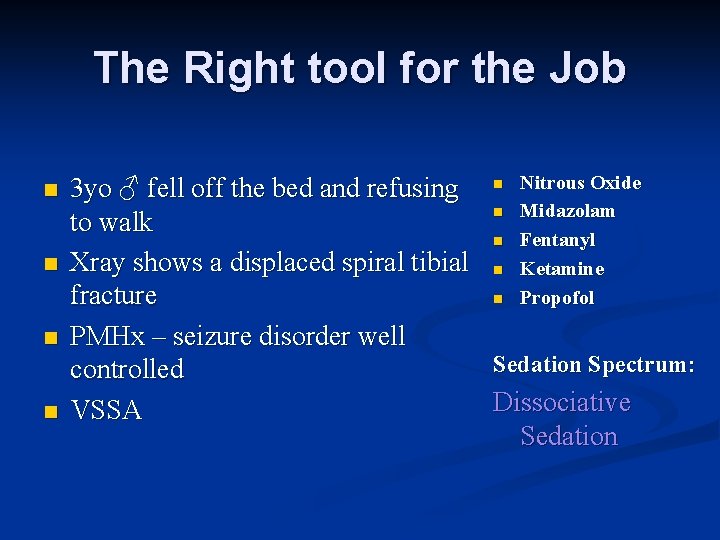
The Right tool for the Job n n 3 yo ♂ fell off the bed and refusing to walk Xray shows a displaced spiral tibial fracture PMHx – seizure disorder well controlled VSSA n n n Nitrous Oxide Midazolam Fentanyl Ketamine Propofol Sedation Spectrum: Dissociative Sedation
“Tricks of the Trade”
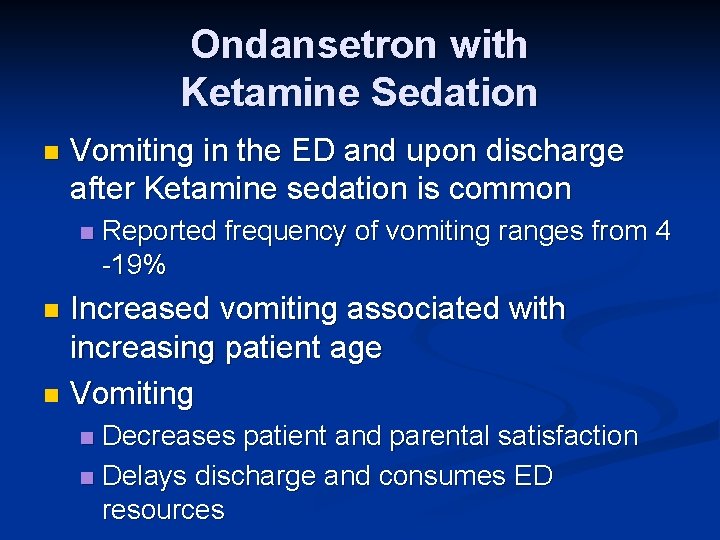
Ondansetron with Ketamine Sedation n Vomiting in the ED and upon discharge after Ketamine sedation is common n Reported frequency of vomiting ranges from 4 -19% Increased vomiting associated with increasing patient age n Vomiting n Decreases patient and parental satisfaction n Delays discharge and consumes ED resources n
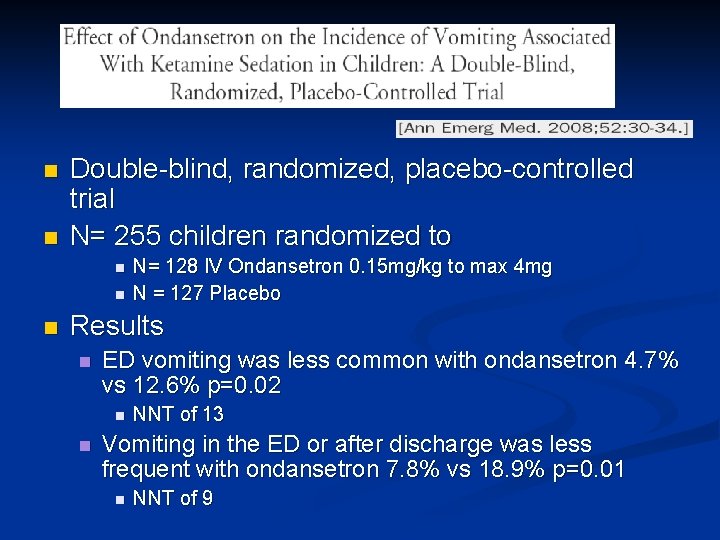
n n Double-blind, randomized, placebo-controlled trial N= 255 children randomized to n n n N= 128 IV Ondansetron 0. 15 mg/kg to max 4 mg N = 127 Placebo Results n ED vomiting was less common with ondansetron 4. 7% vs 12. 6% p=0. 02 n n NNT of 13 Vomiting in the ED or after discharge was less frequent with ondansetron 7. 8% vs 18. 9% p=0. 01 n NNT of 9
Pre-oxygenation with procedural sedation n n Published adverse event rates during pediatric ED procedural sedation vary between 2% and 18% Consistently the most common adverse event is transient hypoxia n n Children’s basal oxygen use/kg is twice that of adults Smaller FRC Shorter “safe apnea” period before desaturation Transient hypoxia is predictably seen with propofol n n Very common with Midazolam and Fentanyl Less likely with Ketamine unless co-administration with other
Adjunctive Atropine with Ketamine Sedation n Ketamine stimulates oral secretions n n In rare circumstances this has been implicated in airway compromise 1 Historically prophylactic anticholinergic agents have been given with ketamine to blunt hypersalivation n Glycopyrrolate 0. 2 mg n Atropine 0. 02 mg/kg
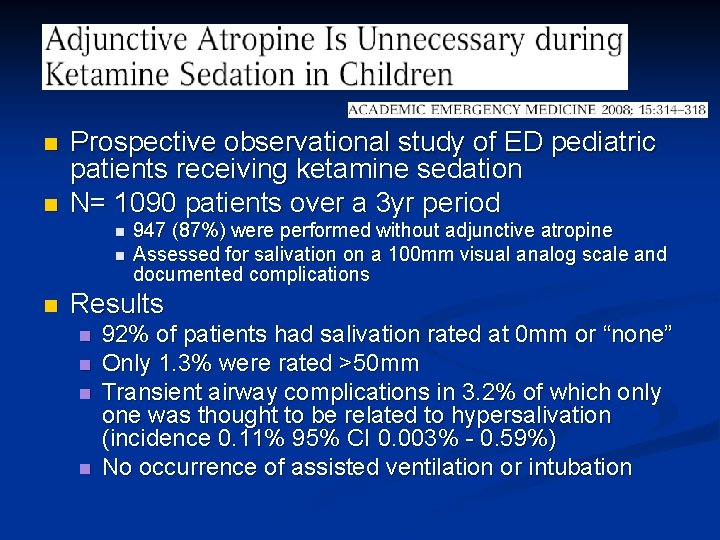
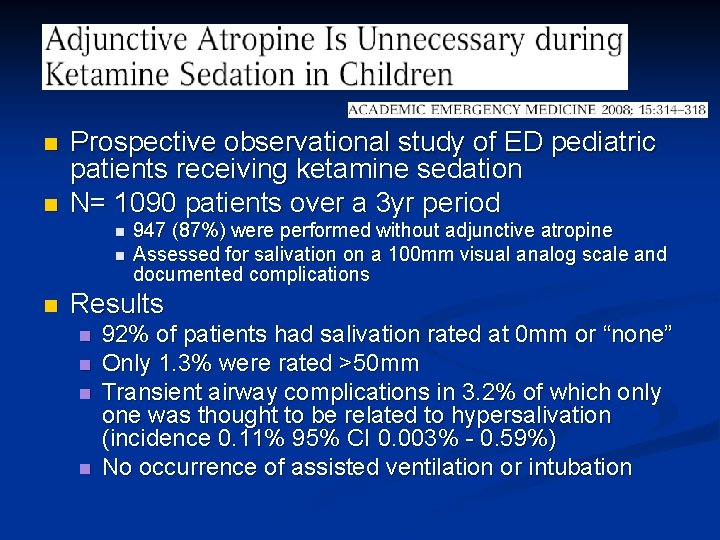
n n Prospective observational study of ED pediatric patients receiving ketamine sedation N= 1090 patients over a 3 yr period n n n 947 (87%) were performed without adjunctive atropine Assessed for salivation on a 100 mm visual analog scale and documented complications Results n n 92% of patients had salivation rated at 0 mm or “none” Only 1. 3% were rated >50 mm Transient airway complications in 3. 2% of which only one was thought to be related to hypersalivation (incidence 0. 11% 95% CI 0. 003% - 0. 59%) No occurrence of assisted ventilation or intubation
Adjunctive Atropine with Ketamine Sedation Omission of atropine is safe n Routine prophylaxis is unnecessary n There is minimal added risk presented with its administration n Possible subsets of patients which may benefit n n Very young children n Those undergoing oropharyngeal procedures
Controversies
In your local ED…. 9 yo M previously healthy with no meds/allergies n Fell mountain biking 40 mins ago and has deformed and partially angulated radius/ulnar # n Neurovascularly intact distally n Wearing helmet and no issues with potential HI n Bag of chips 2 hrs ago with bottle of Gatorade n Survey n
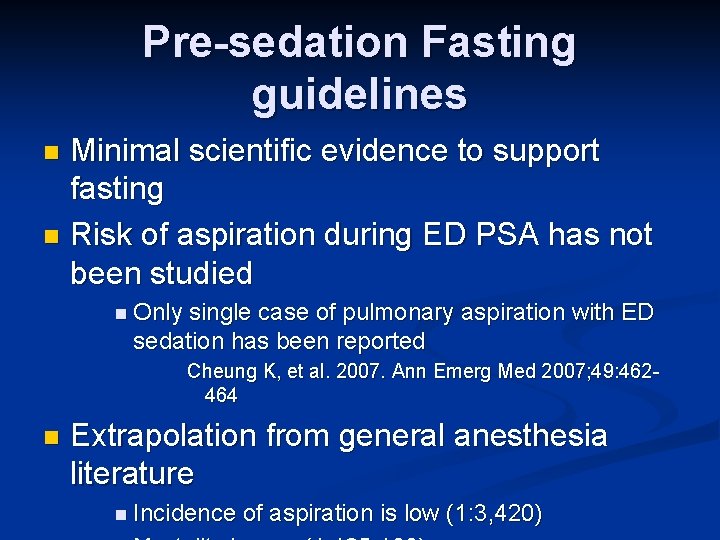
Pre-sedation Fasting guidelines Minimal scientific evidence to support fasting n Risk of aspiration during ED PSA has not been studied n n Only single case of pulmonary aspiration with ED sedation has been reported Cheung K, et al. 2007. Ann Emerg Med 2007; 49: 462464 n Extrapolation from general anesthesia literature n Incidence of aspiration is low (1: 3, 420)
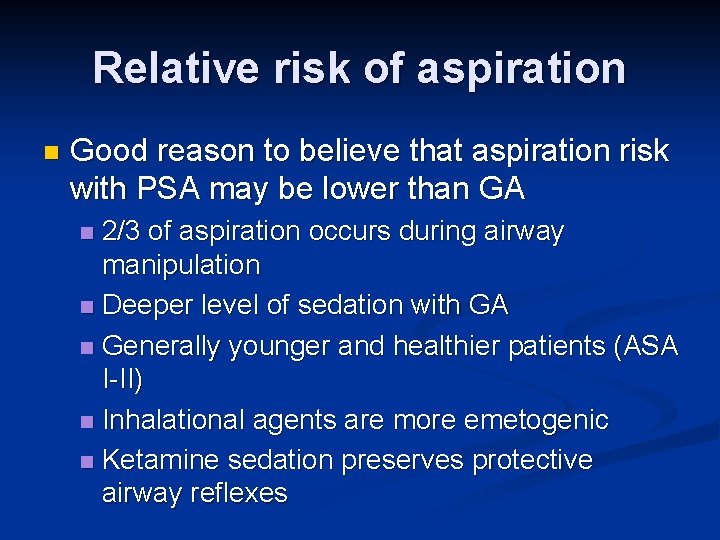
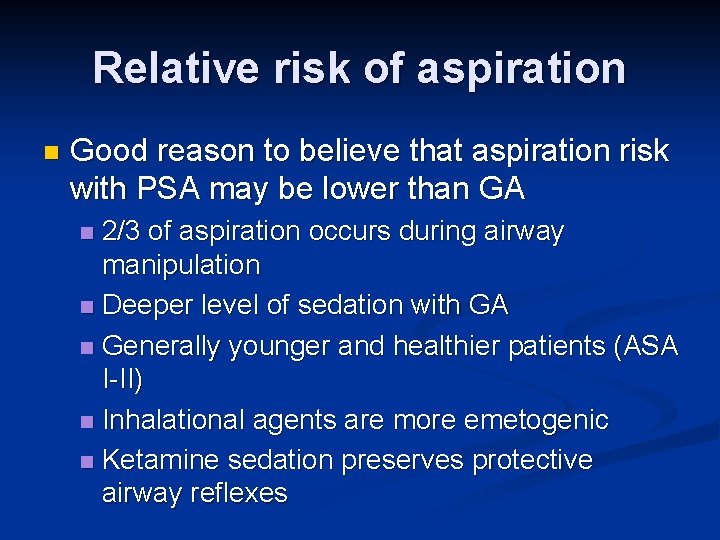
Relative risk of aspiration n Good reason to believe that aspiration risk with PSA may be lower than GA 2/3 of aspiration occurs during airway manipulation n Deeper level of sedation with GA n Generally younger and healthier patients (ASA I-II) n Inhalational agents are more emetogenic n Ketamine sedation preserves protective airway reflexes n
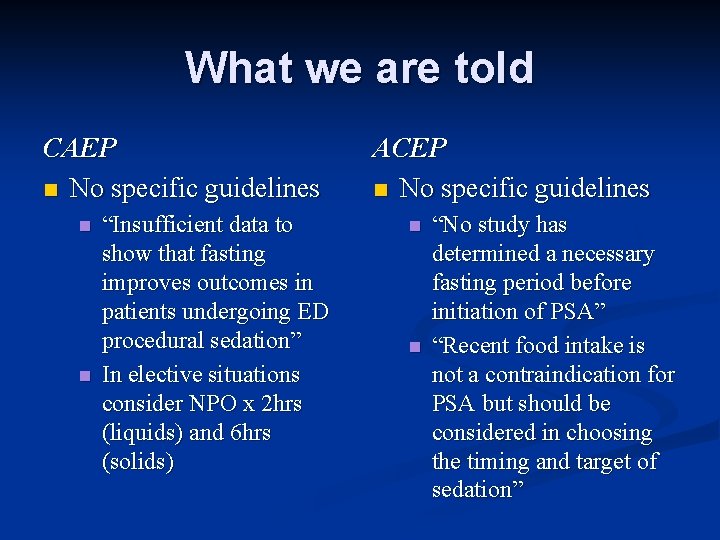
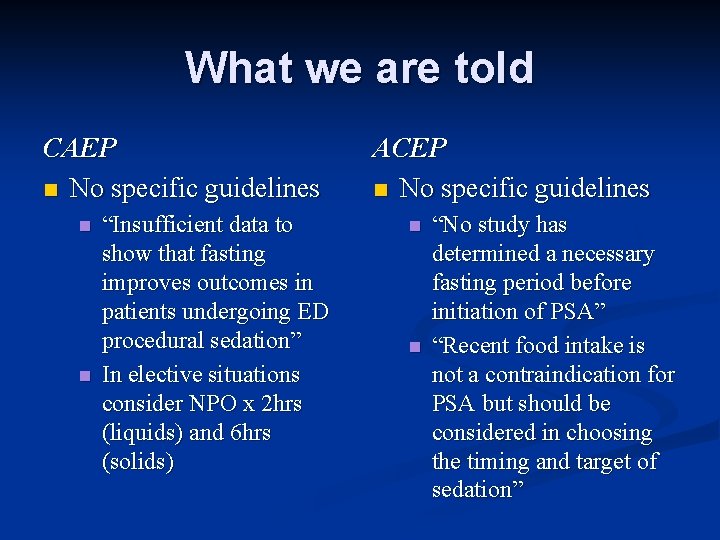
What we are told CAEP n No specific guidelines n n “Insufficient data to show that fasting improves outcomes in patients undergoing ED procedural sedation” In elective situations consider NPO x 2 hrs (liquids) and 6 hrs (solids) ACEP n No specific guidelines n n “No study has determined a necessary fasting period before initiation of PSA” “Recent food intake is not a contraindication for PSA but should be considered in choosing the timing and target of sedation”
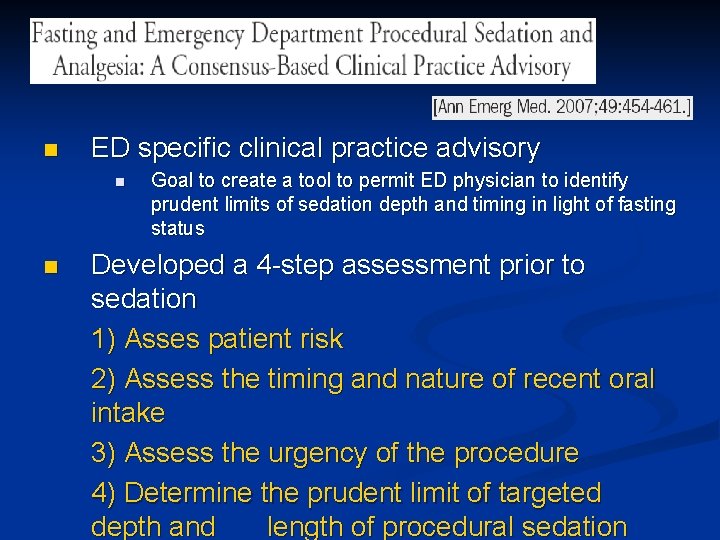
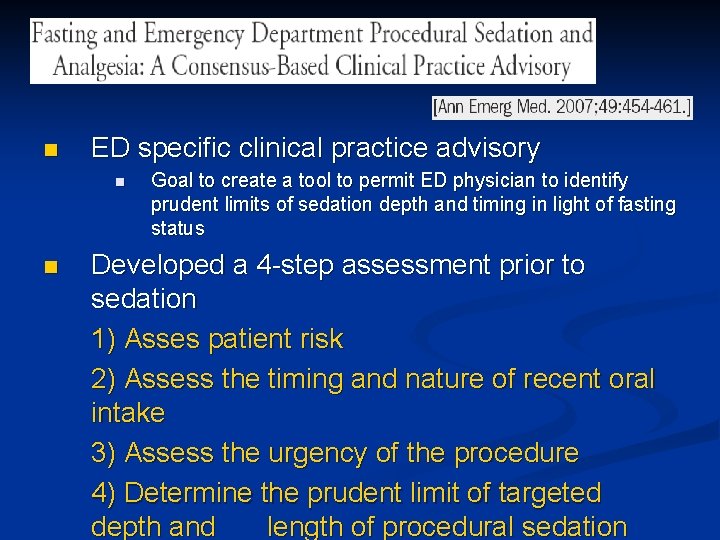
n ED specific clinical practice advisory n n Goal to create a tool to permit ED physician to identify prudent limits of sedation depth and timing in light of fasting status Developed a 4 -step assessment prior to sedation 1) Asses patient risk 2) Assess the timing and nature of recent oral intake 3) Assess the urgency of the procedure 4) Determine the prudent limit of targeted depth and length of procedural sedation
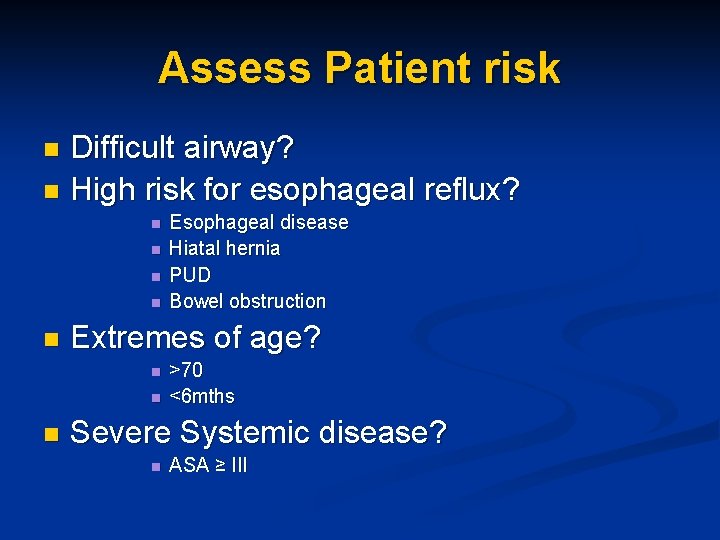
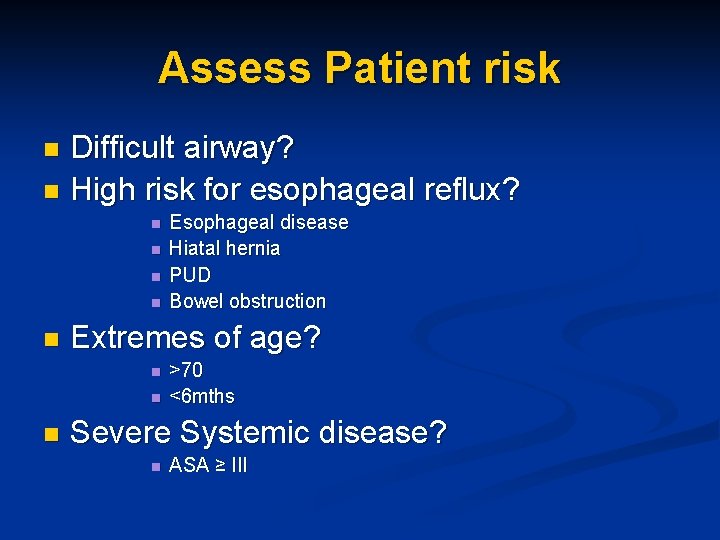
Assess Patient risk Difficult airway? n High risk for esophageal reflux? n n n Extremes of age? n n n Esophageal disease Hiatal hernia PUD Bowel obstruction >70 <6 mths Severe Systemic disease? n ASA ≥ III
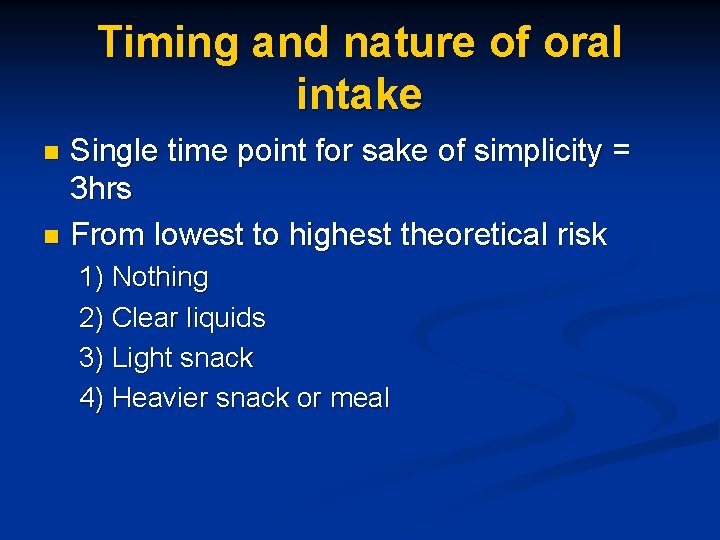
Timing and nature of oral intake Single time point for sake of simplicity = 3 hrs n From lowest to highest theoretical risk n 1) Nothing 2) Clear liquids 3) Light snack 4) Heavier snack or meal
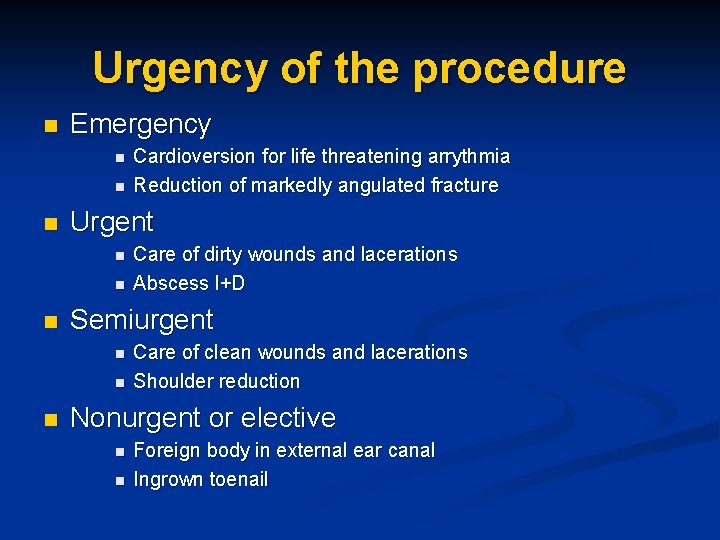
Urgency of the procedure n Emergency n n n Urgent n n n Care of dirty wounds and lacerations Abscess I+D Semiurgent n n n Cardioversion for life threatening arrythmia Reduction of markedly angulated fracture Care of clean wounds and lacerations Shoulder reduction Nonurgent or elective n n Foreign body in external ear canal Ingrown toenail
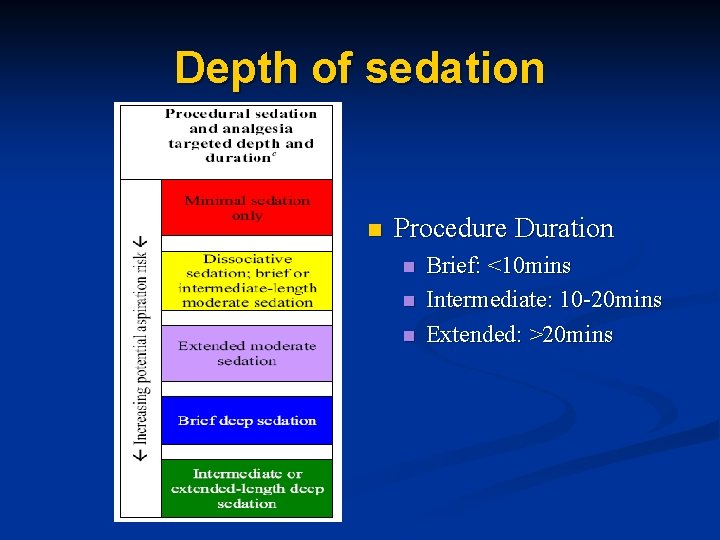
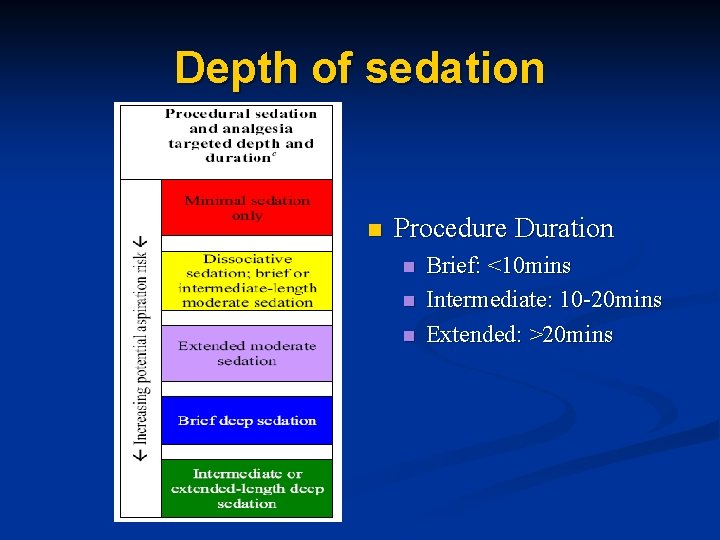
Depth of sedation n Procedure Duration n Brief: <10 mins Intermediate: 10 -20 mins Extended: >20 mins

Standard-risk patient

Higher-risk Patient
Capnography monitoring during procedural sedation n Non-invasive measurement of the partial pressure of CO 2 from the airway during inspiration and expiration
Capnography monitoring n Traditional monitoring n n n Pulse oximetry = oxygenation RR and clinical observation = ventilation Capnography n n More precise and direct assessment of the patient’s ventilatory status Assessment of airway patency and respiratory pattern Early warning system for prehypoxic respiratory depression Assessment of depth of sedation

Show me the evidence!!! n Comparison of oximetry, capnography and clinical observation in the ED 2 n 75% of pediatric patients with respiratory compromise were noted by Et. CO 2 monitoring only n Pediatric RCT comparing capnography to clinical observation in detecting resp events 3 n Clinical assessment identified hypoventilation in 3% and did not identify any patients with apnea n Capnography data showed ventilation was compromised in >50% of cases and nearly 25% fulfilled criteria for apnea
Recommendations n Good evidence that capnography provides a means for early detection of sedationrelated hypoventilation n Clinical significance with regards to improved patient outcomes has not been shown

Future “where we’re going we don’t need roads” – Dr. Emmett Brown
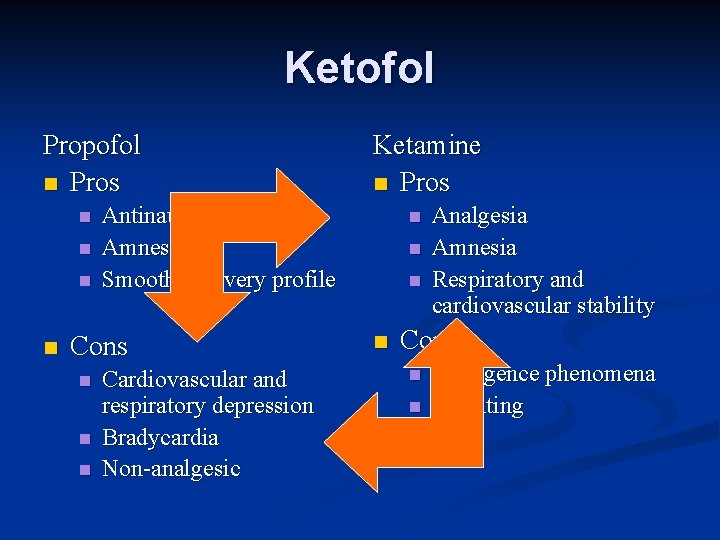
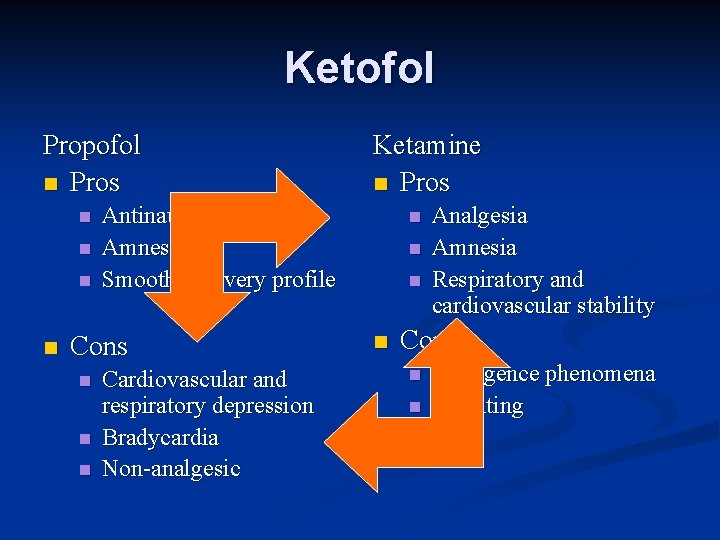
Ketofol Propofol n Pros n n Antinauseant effects Amnestic Smooth recovery profile Cons n n n Ketamine n Pros Cardiovascular and respiratory depression Bradycardia Non-analgesic n n Analgesia Amnesia Respiratory and cardiovascular stability Cons n n Emergence phenomena Vomiting
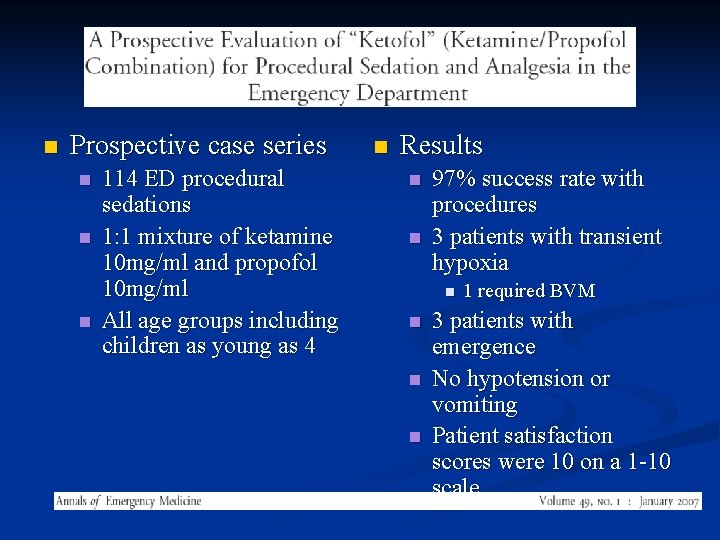
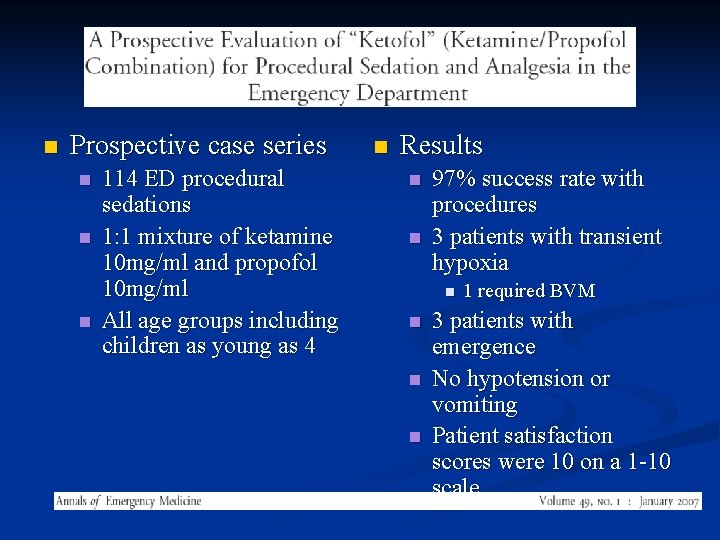
n Prospective case series n n n 114 ED procedural sedations 1: 1 mixture of ketamine 10 mg/ml and propofol 10 mg/ml All age groups including children as young as 4 n Results n n 97% success rate with procedures 3 patients with transient hypoxia n n 1 required BVM 3 patients with emergence No hypotension or vomiting Patient satisfaction scores were 10 on a 1 -10 scale
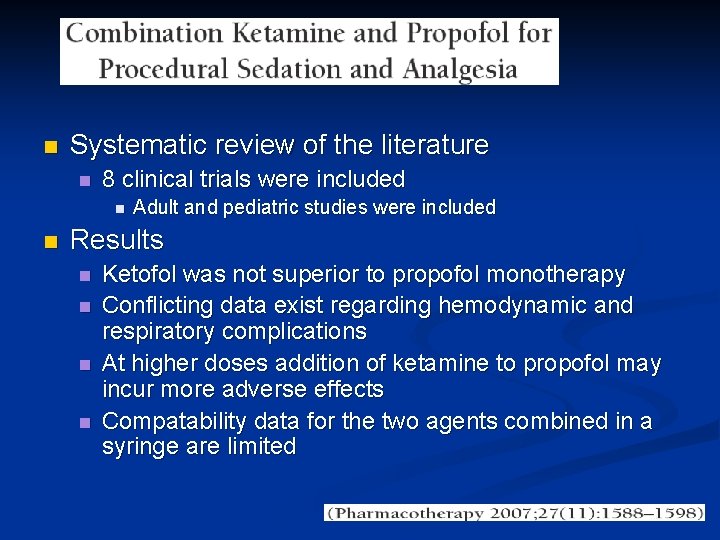
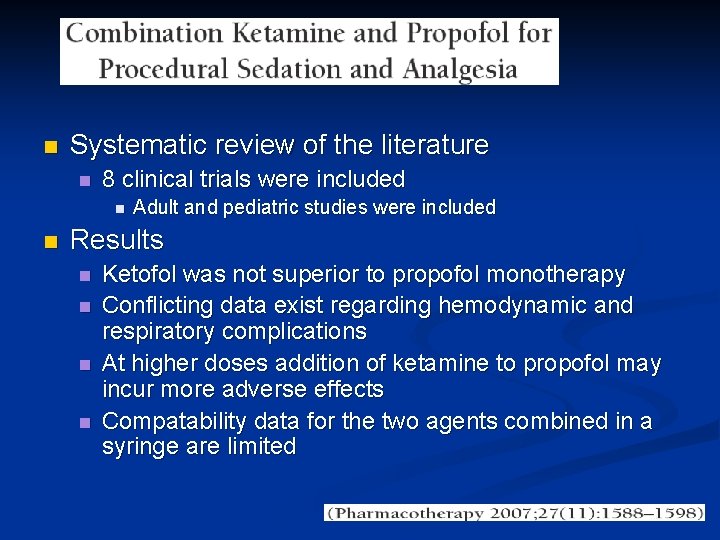
n Systematic review of the literature n 8 clinical trials were included n n Adult and pediatric studies were included Results n n Ketofol was not superior to propofol monotherapy Conflicting data exist regarding hemodynamic and respiratory complications At higher doses addition of ketamine to propofol may incur more adverse effects Compatability data for the two agents combined in a syringe are limited
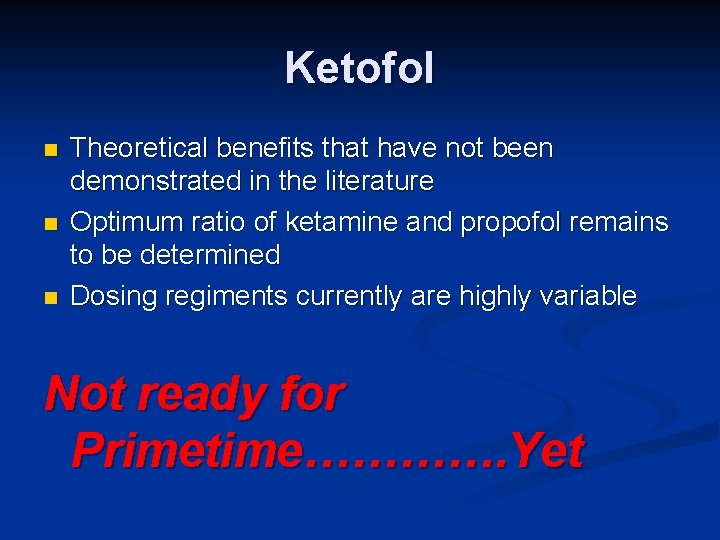
Ketofol n n n Theoretical benefits that have not been demonstrated in the literature Optimum ratio of ketamine and propofol remains to be determined Dosing regiments currently are highly variable Not ready for Primetime…………. Yet
BIS
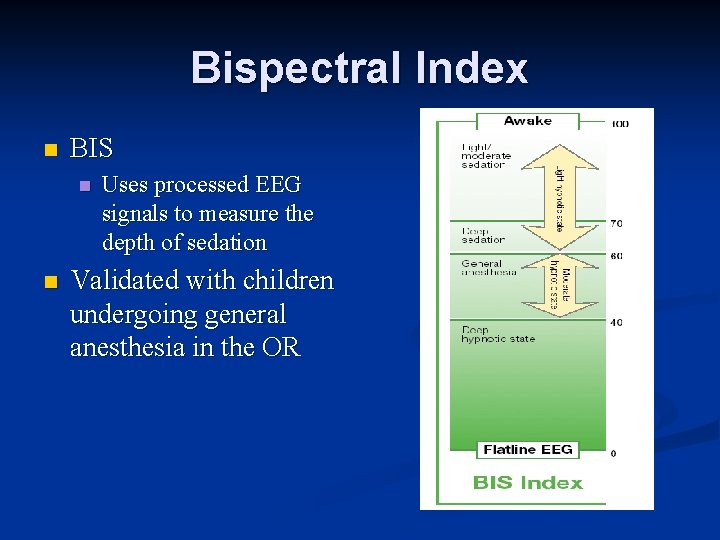
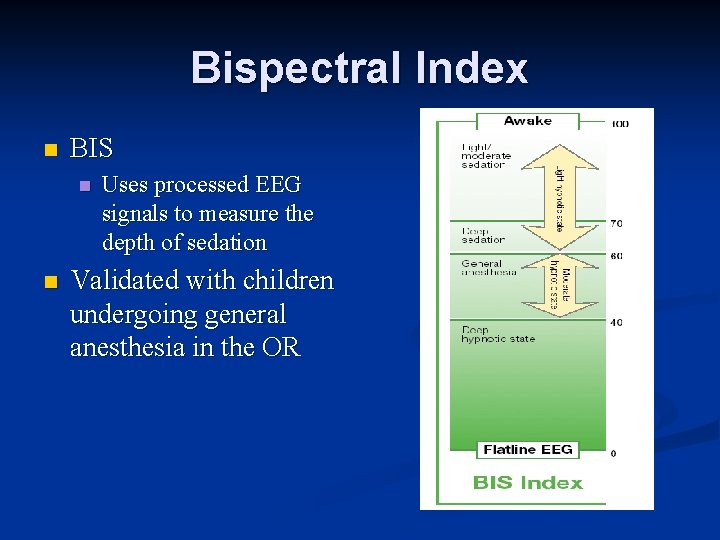
Bispectral Index n BIS n n Uses processed EEG signals to measure the depth of sedation Validated with children undergoing general anesthesia in the OR
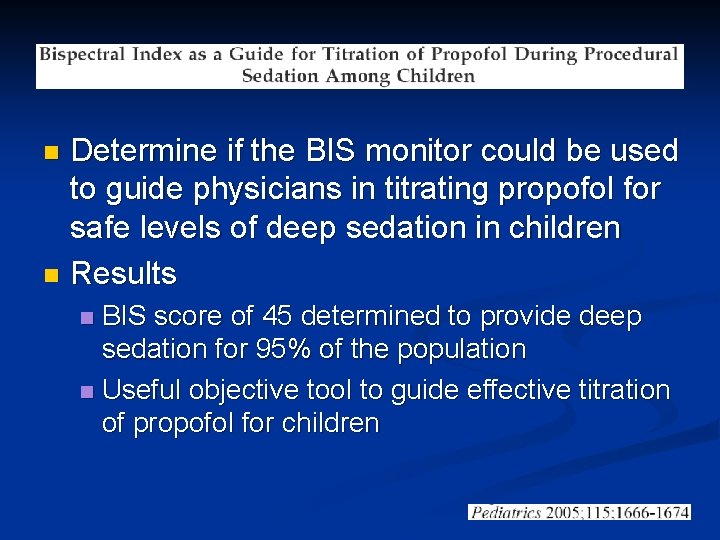
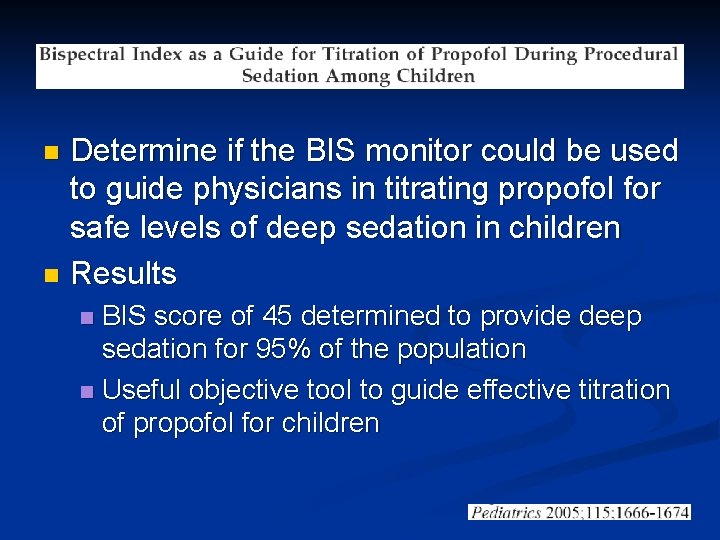
Determine if the BIS monitor could be used to guide physicians in titrating propofol for safe levels of deep sedation in children n Results n BIS score of 45 determined to provide deep sedation for 95% of the population n Useful objective tool to guide effective titration of propofol for children n
Conclusions n n n Familiarize yourself with your pharmaceutical options and “pick the right tool for the job” Pre-oxygenation is your friend Atropine is out and ondansetron is in for routine ketamine sedations Pre-procedural fasting guidelines are not blackand-white and each situation is unique Consider the additional information provided by capnography if it is available to you Ketofol not ready for primetime…. . yet
Questions?
Additional References 1) 2) 3) 4) Green SM et al. Intramuscular ketamine for pediatric sedation in the emergency department: safety profile with 1022 cases. Ann Emerg Med. 1998; 31: 688 -97 Hart LS et al. The value of end-tidal CO 2 monitoring when comparing three methods of conscious sedation in children undergoing painful procedures in the emergency department. Pediatr Emerg Care 1997; 13(3): 189 -93 Lightdale JR et al. Microstream capnography improves patient monitoring during moderate sedation: a randomized, controlled trial. Pediatrics 2006; 117(6): e 1170 -8 Lopez MD et al. Pediatric Procedural Sedation. Emergency Medicine Reports 2008; 13(12): 145 -156
Additional Slides
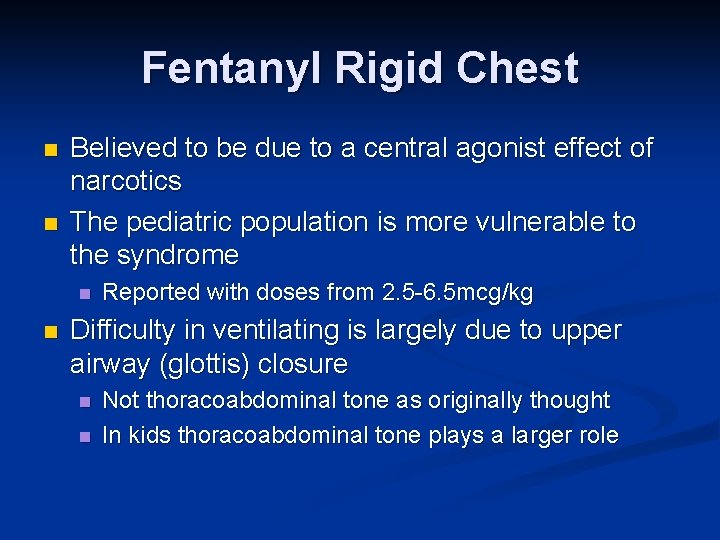
Fentanyl Rigid Chest n n Believed to be due to a central agonist effect of narcotics The pediatric population is more vulnerable to the syndrome n n Reported with doses from 2. 5 -6. 5 mcg/kg Difficulty in ventilating is largely due to upper airway (glottis) closure n n Not thoracoabdominal tone as originally thought In kids thoracoabdominal tone plays a larger role
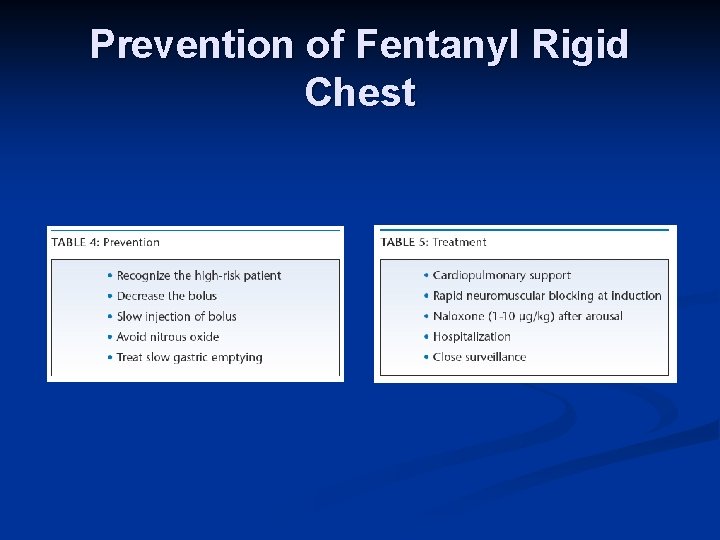
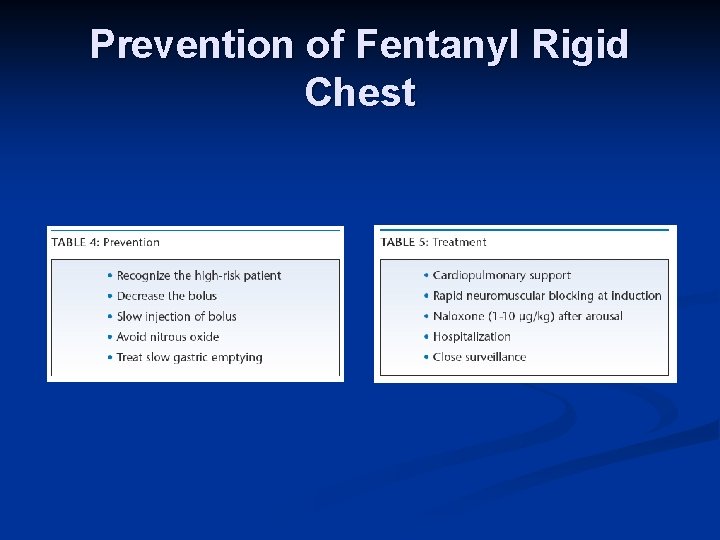
Prevention of Fentanyl Rigid Chest
Propofol epilepsy
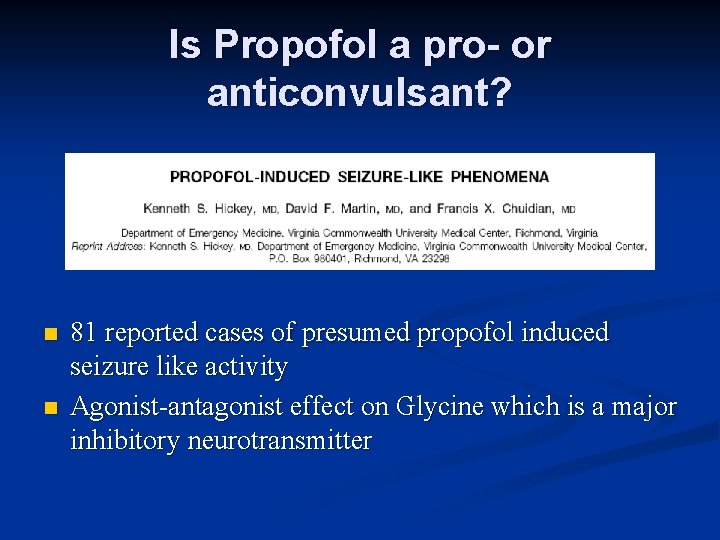
Is Propofol a pro- or anticonvulsant? n n 81 reported cases of presumed propofol induced seizure like activity Agonist-antagonist effect on Glycine which is a major inhibitory neurotransmitter
Prospective study n Effects of IV propofol on EEG n 25 children with epilepsy n 25 children with learning disorders n Undergoing elective sedation for MRI n
n Results No child in either group had increased spikewave pattern with propofol n Depression in spike-wave pattern in the children with epilepsy was seen n n Supported the concept of propofol being a sedative-hypnotic agent with anticonvulsant properties
Aspiration case in literature
65 yo. F with HTN n Trimalleolar fracture n Morphine/fentanyl/Propofol for first PSA with no significant complications n Second PSA in attempt to improve the reduction n n 6 hrs after last meal n Propofol/fentanyl n 10 mins after propofol bolus the patient vomited into the mask and aspirated
n Sats were 86% initially n n Patient remained hypoxic with sats 84% on RA n n Airway was suctioned and BVM was started with improvement to sats 97% Inspiratory and expiratory wheezes throughout RSI was performed and admitted to ICU where she was ventilated for 12 hrs then slowly weaned
Etomidate
Etomidate n n n Initially described for RSI in peds Rapid onset of sedation, brief half-life, short recovery period and minimal effects on cardiopulmonary systems Adverse effects n n n Potential for adrenal suppression Pain at injection site Myoclonus Quickly and easily induce deep sedation and/or general anesthesia. More studied for PSA in the adult population in United States
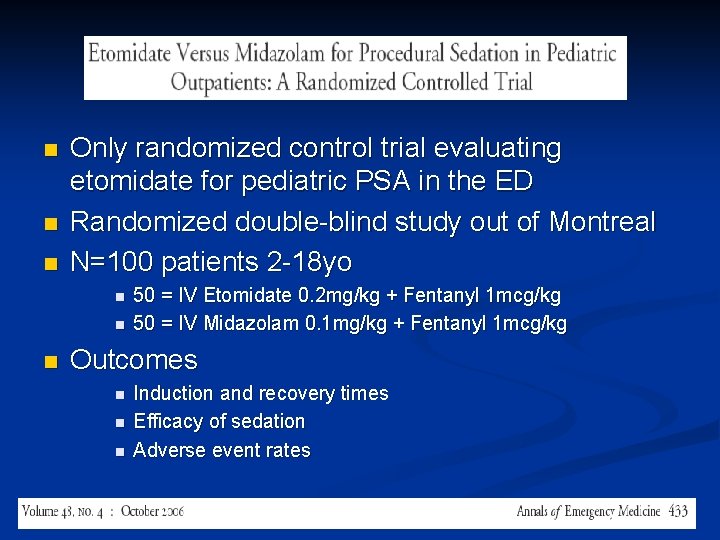
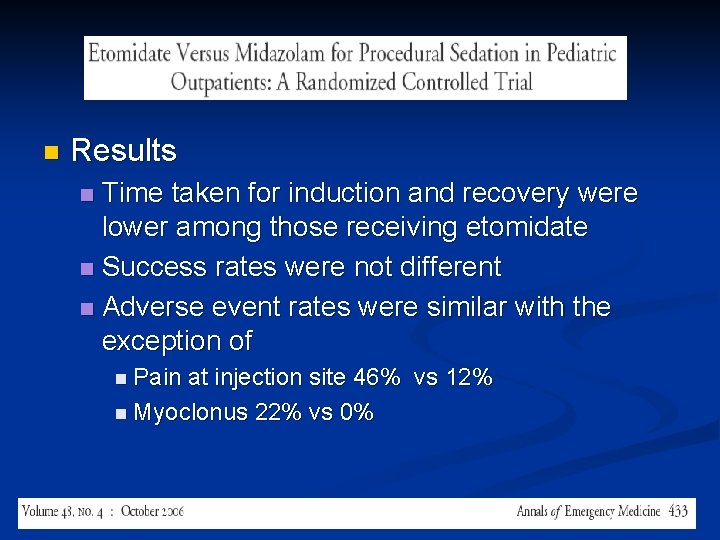
n n n Only randomized control trial evaluating etomidate for pediatric PSA in the ED Randomized double-blind study out of Montreal N=100 patients 2 -18 yo n n n 50 = IV Etomidate 0. 2 mg/kg + Fentanyl 1 mcg/kg 50 = IV Midazolam 0. 1 mg/kg + Fentanyl 1 mcg/kg Outcomes n n n Induction and recovery times Efficacy of sedation Adverse event rates
n Results Time taken for induction and recovery were lower among those receiving etomidate n Success rates were not different n Adverse event rates were similar with the exception of n n Pain at injection site 46% vs 12% n Myoclonus 22% vs 0%
Etomidate Need a large series to better establish the safety profile of etomidate for PSA in pediatrics n A randomized trial comparing etomidate, propofol and ketamine would be of great interest…. . n Any takers?
Propofol infusion syndrome
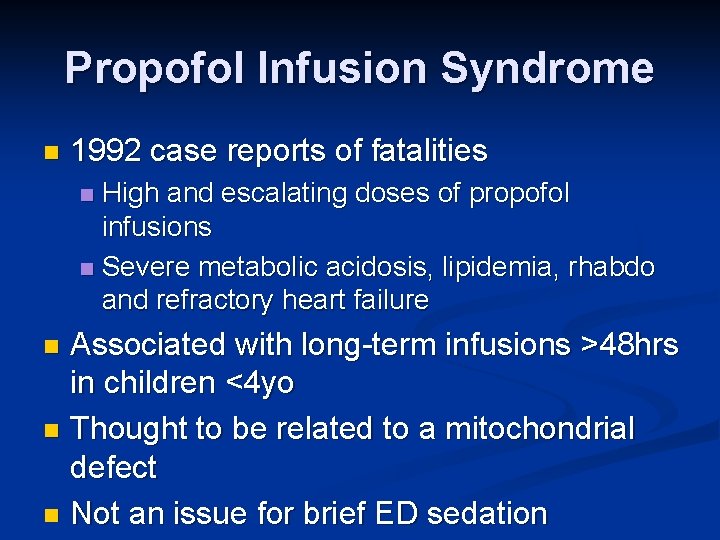
Propofol Infusion Syndrome n 1992 case reports of fatalities High and escalating doses of propofol infusions n Severe metabolic acidosis, lipidemia, rhabdo and refractory heart failure n Associated with long-term infusions >48 hrs in children <4 yo n Thought to be related to a mitochondrial defect n Not an issue for brief ED sedation n
Preoxygenation protocol
Pre-oxygenation with procedural sedation n n Published adverse event rates during pediatric ED procedural sedation vary between 2% and 18% Consistently the most common adverse event is transient hypoxia n n Children’s basal oxygen use/kg is twice that of adults Smaller FRC Shorter “safe apnea” period before desaturation Transient hypoxia is predictably seen with propofol n n Very common with Midazolam and Fentanyl Less likely with Ketamine unless co-administration with other
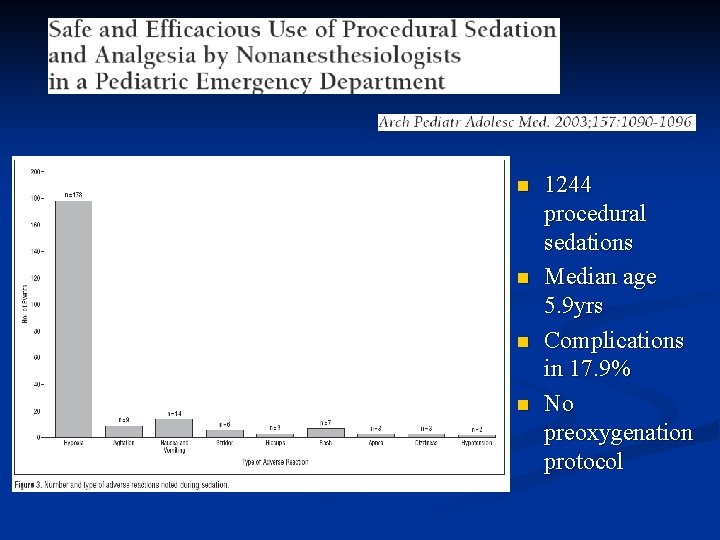
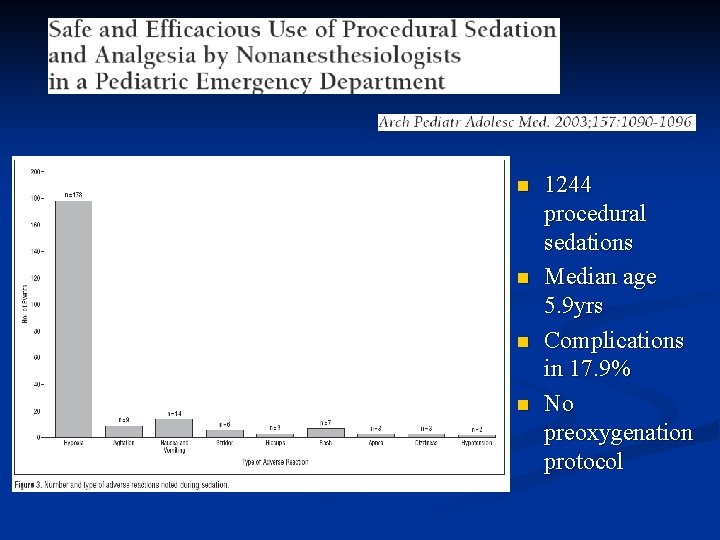
n n 1244 procedural sedations Median age 5. 9 yrs Complications in 17. 9% No preoxygenation protocol
