Pediatric Procedural Sedation Jana Stockwell MD FAAP Childrens





- Slides: 58
Pediatric Procedural Sedation Jana Stockwell, MD, FAAP Children’s Sedation Services Children’s Healthcare of Atlanta Emory University School of Medicine 1
Why Not Sedate? • “I’m gonna be so fast they won’t even feel it. ” • “They’re just crying because they’re being held down. ” • “Children don’t feel pain” • “Children don’t remember pain” 2
Why Sedate? • • Efficacy Satisfaction Quality of study Do unto others… – Same injury, adults sedated more 3
Goals • Guard safety & welfare of child • Minimize physical discomfort & pain • Control anxiety, maximize potential for amnesia • Control behavior & movement to complete procedure • Return patient to state safe for discharge 4
CHOA @ Egleston Program • CCM & ED physicians • Dedicated radiology & H/O sedation nurses • 4 locations • 2 -3 docs/day • >3, 000 sedations/year 5
Overview • Definitions • Choose wisely – Pick your patient – Pick your drugs – Pick your “no’s” – Pick your battles • On the horizon 6
Definitions • 1992 AAP (Peds 1992; 898: 110) – Conscious Sedation – Deep Sedation • 1998 ACEP (Ann Emer Med 1998; 31: 663) – Procedural Analgesia & Sedation • 2006 AAP & AAPD (Peds 2006; 118: 2587 -2602) – Minimal = anxiolysis – Moderate = conscious – Deep – General anesthesia 7
Joint Commission 2000 • Level 1: Minimal – Respond normally to verbal commands – Cognitive function and coordination impaired 8
Joint Commission 2000 • Level 2: Moderate sedation / analgesia – Respond to verbal or gentle tactile stimuli – No intervention to maintain airway – Adequate spontaneous ventilation 9
Joint Commission 2000 • Level 3: Deep sedation / analgesia – Respond purposefully following repeated or painful stimulation – Ability to maintain ventilatory function may be impaired 10
Never Land • Level ~3. 5 Dissociative Sedation – Cataleptic state – Maintain protective reflexes – Retain spontaneous respirations 11
Joint Commission 2000 • Level 4: Anesthesia – Not arousable, even with painful stimuli – Independent ventilatory function often impaired 12

Remember, it’s a… 13

Providers • • “Licensed independent practitioner” Know drugs and antidotes Ability to monitor Capable of rescue Re-assess immediately before sedation Immediately available Not doing the procedure 14
(Appropriate) Patients • Painful Procedures – – – Bone marrow Bx, BMA Wound debridement Renal Bx Abscess I&D Fracture reduction Cardioversion • Movement an issue – – – Suture difficult area Radiographic images Auditory brain response LP Casting 15
Inappropriate Patients • Airway issues – Small, tight jaw – Airway obstruction • Respiratory issues • “Super quick” – Lacerations to be fixed with Dermabond Primum non nocere 16
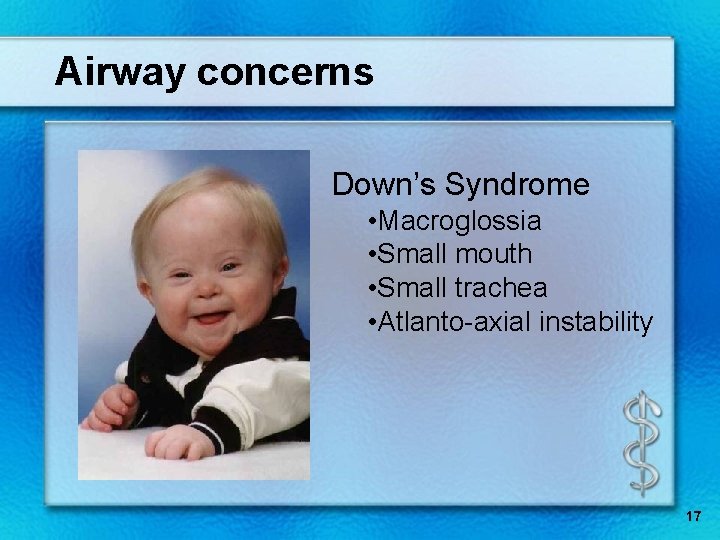
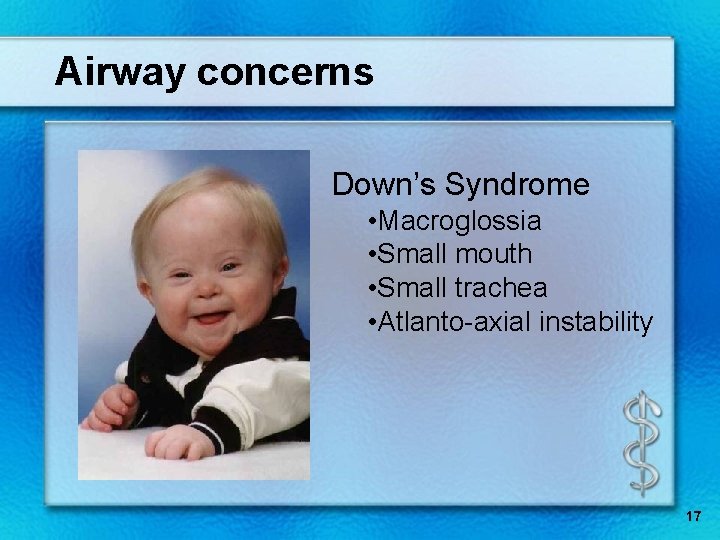
Airway concerns Down’s Syndrome • Macroglossia • Small mouth • Small trachea • Atlanto-axial instability 17
Airway concerns Pierre-Robin Sequence Beckwith-Wiedemann Syndrome 18

Other concerns • Pneumonia, asthma, BPD, tracheomalacia, OSA, tachypnea • CCHD, CHF, hypotension • Central apnea, seizures • GERD, hepatic disease • Renal disease, dehydration, abnormal electrolytes • Sepsis 19
Patient Assessment • American Society Anesthesiology (ASA) class • Allergies • NPO status • Health evaluation 20
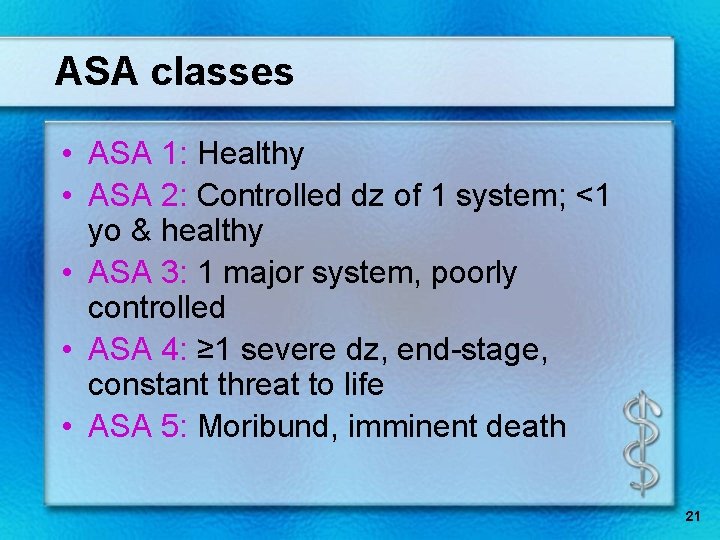
ASA classes • ASA 1: Healthy • ASA 2: Controlled dz of 1 system; <1 yo & healthy • ASA 3: 1 major system, poorly controlled • ASA 4: ≥ 1 severe dz, end-stage, constant threat to life • ASA 5: Moribund, imminent death 21
Allergies • Medications allergies – Previous anesthesia events? • Food allergies (egg, soy) • Tape, skin prep, etc 22
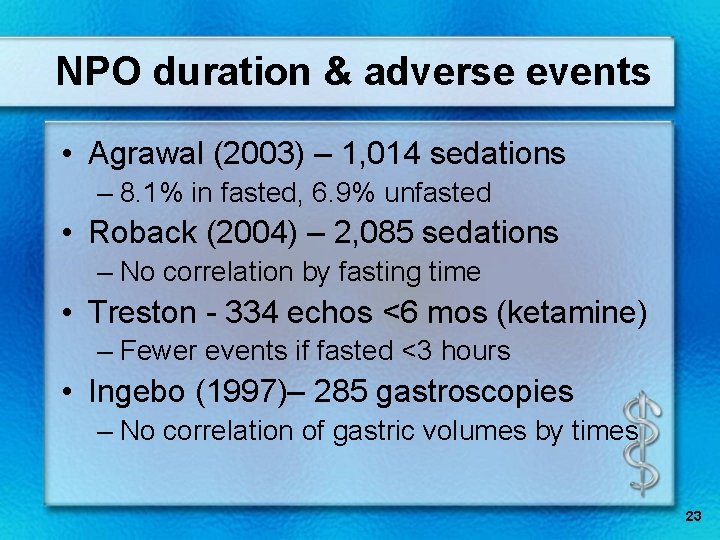
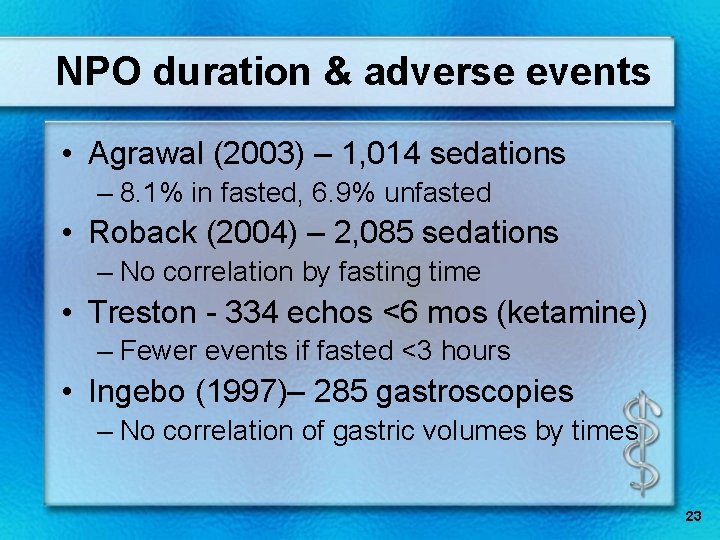
NPO duration & adverse events • Agrawal (2003) – 1, 014 sedations – 8. 1% in fasted, 6. 9% unfasted • Roback (2004) – 2, 085 sedations – No correlation by fasting time • Treston - 334 echos <6 mos (ketamine) – Fewer events if fasted <3 hours • Ingebo (1997)– 285 gastroscopies – No correlation of gastric volumes by times 23
NPO Status “…because the absolute risk of aspiration during procedural sedation is not yet known, guidelines for fasting periods before elective sedation should generally follow those used for elective general anesthesia. ” Pediatrics 2006; 118: 2587 24
NPO status (ASA) • • Solids, formula - 6 hours Clear liquids - 2 hours Breast milk - 4 hours Can take sip with meds 25
Preparation • Informed consent • Health evaluation – ROS – History (sedations? ) – Medications (including herbals) – Weight – VS, sat – Exam (airway, lungs, CV state, LOC) 26
Preparation • Additional person • “SOAPME” – Suction – Oxygen – Airways (BVM, oral, LMA, ETT) – Pharmacy (meds) – Monitors – Equipment (defibrillator, airway supplies, etc) 27
Reversal Agents • Naloxone – Competitively binds all 3 opiate receptors – IV, IM, SC, SL, ETT – 0. 1 mg/kg • Flumazenil – Can terminate paradoxical reactions – 0. 02 mg/kg – Lowers seizure threshold 28
Documentation & Monitoring • • • Time out Time-based record: Q 5 minutes SPO 2 & ETCO 2 HR BP LOC O 2 given Medications Interventions 29
Recovery and Discharge • • Continuous HR & sats until alert 1 person dedicated to patient Aldrete post-anesthetic score Post-sedation evaluation – Baseline cardiopulmonary status (VS) – Drinking – Level of consciousness – Locomotion / sitting • Written & verbal instructions 30
31
Git ‘er done • • • Hypnotics Sedatives Ketamine Etomidate Propofol Nitrous oxide 32
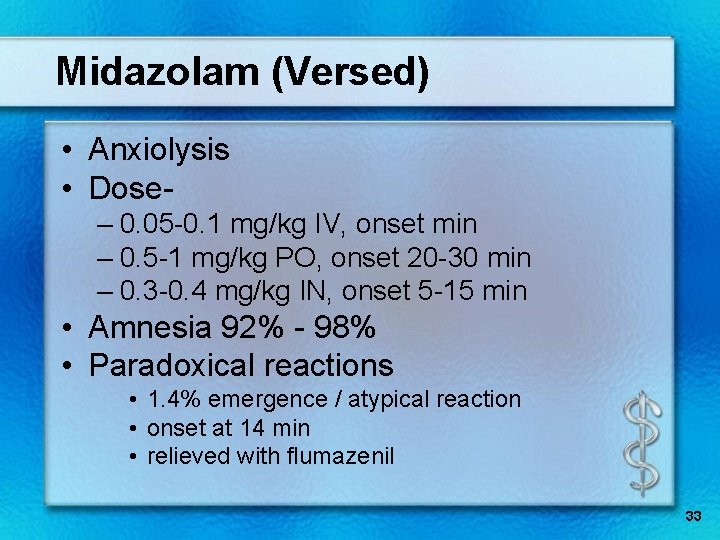
Midazolam (Versed) • Anxiolysis • Dose– 0. 05 -0. 1 mg/kg IV, onset min – 0. 5 -1 mg/kg PO, onset 20 -30 min – 0. 3 -0. 4 mg/kg IN, onset 5 -15 min • Amnesia 92% - 98% • Paradoxical reactions • 1. 4% emergence / atypical reaction • onset at 14 min • relieved with flumazenil 33

Hypnotics • • Chloral hydrate Pentobarbital Methohexital Etomidate 34
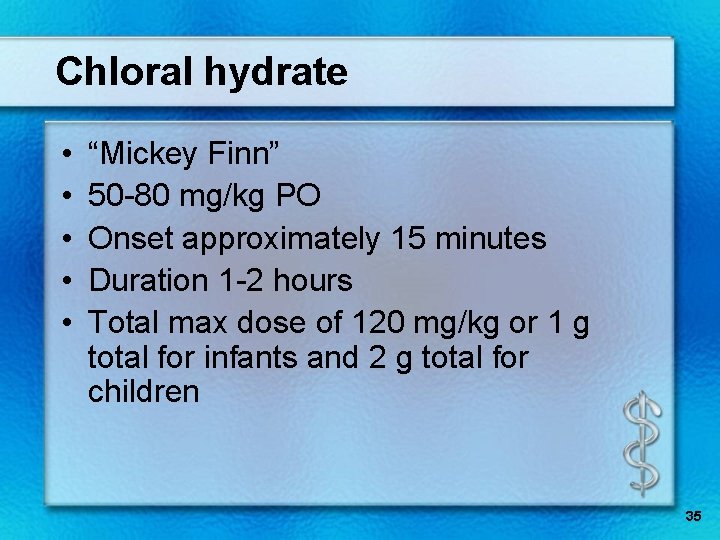
Chloral hydrate • • • “Mickey Finn” 50 -80 mg/kg PO Onset approximately 15 minutes Duration 1 -2 hours Total max dose of 120 mg/kg or 1 g total for infants and 2 g total for children 35
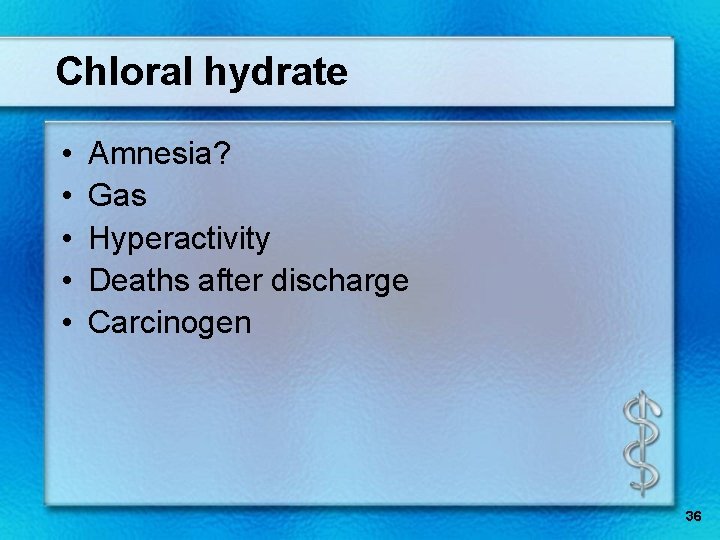
Chloral hydrate • • • Amnesia? Gas Hyperactivity Deaths after discharge Carcinogen 36
Barbiturates • • Depress RAS No analgesia May be hyperesthetic Amnesia 37
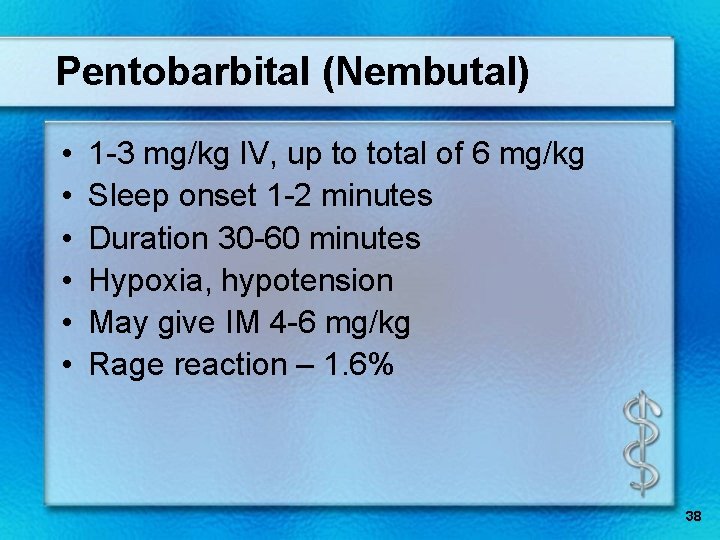
Pentobarbital (Nembutal) • • • 1 -3 mg/kg IV, up to total of 6 mg/kg Sleep onset 1 -2 minutes Duration 30 -60 minutes Hypoxia, hypotension May give IM 4 -6 mg/kg Rage reaction – 1. 6% 38
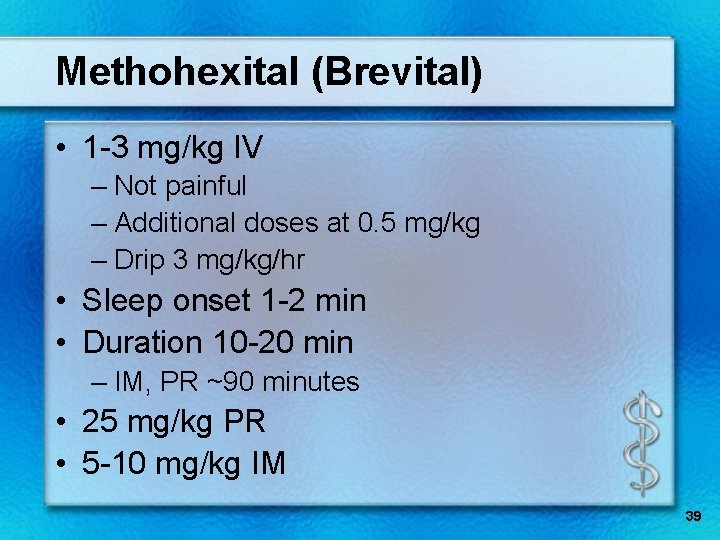
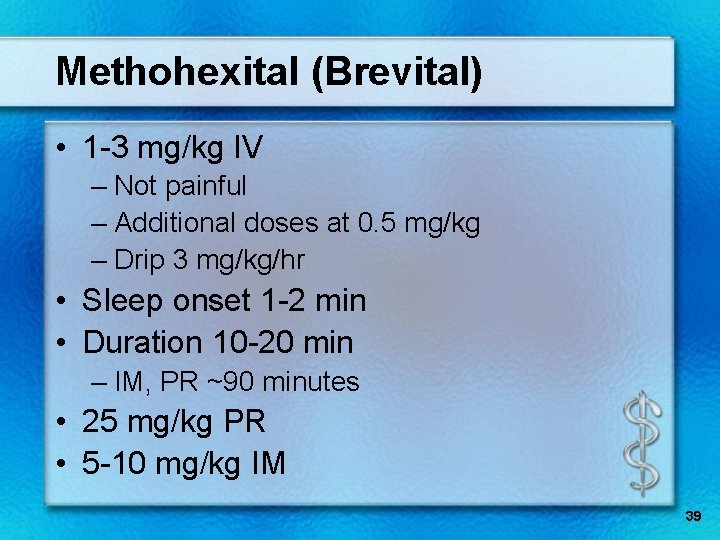
Methohexital (Brevital) • 1 -3 mg/kg IV – Not painful – Additional doses at 0. 5 mg/kg – Drip 3 mg/kg/hr • Sleep onset 1 -2 min • Duration 10 -20 min – IM, PR ~90 minutes • 25 mg/kg PR • 5 -10 mg/kg IM 39
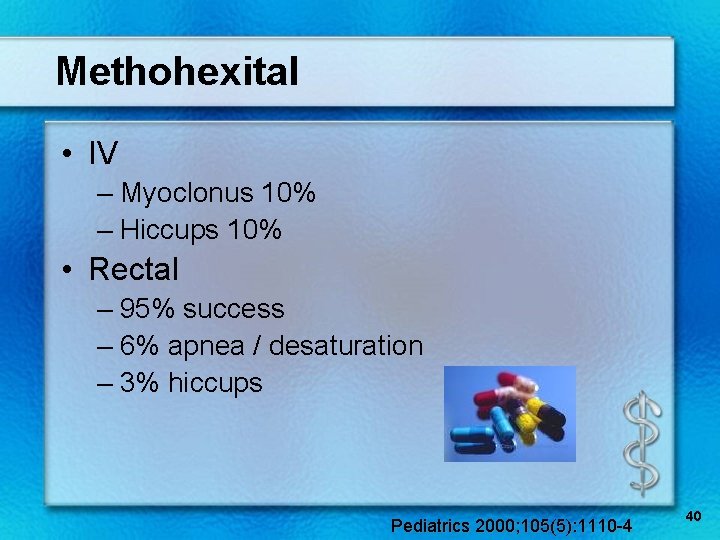
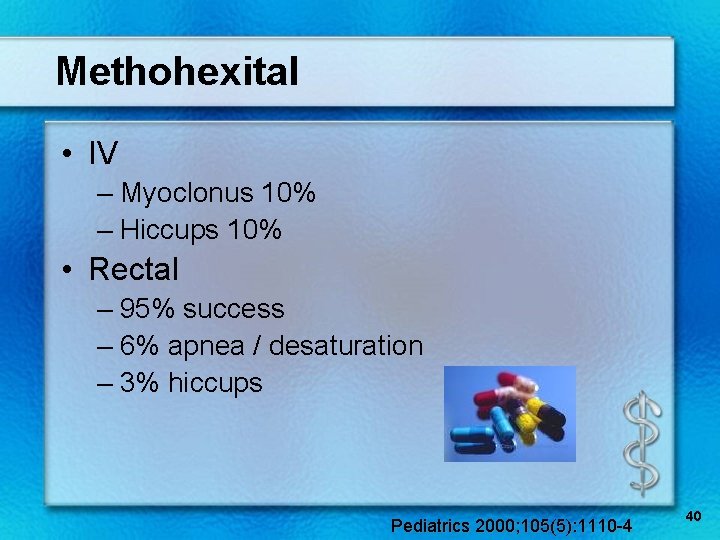
Methohexital • IV – Myoclonus 10% – Hiccups 10% • Rectal – 95% success – 6% apnea / desaturation – 3% hiccups Pediatrics 2000; 105(5): 1110 -4 40
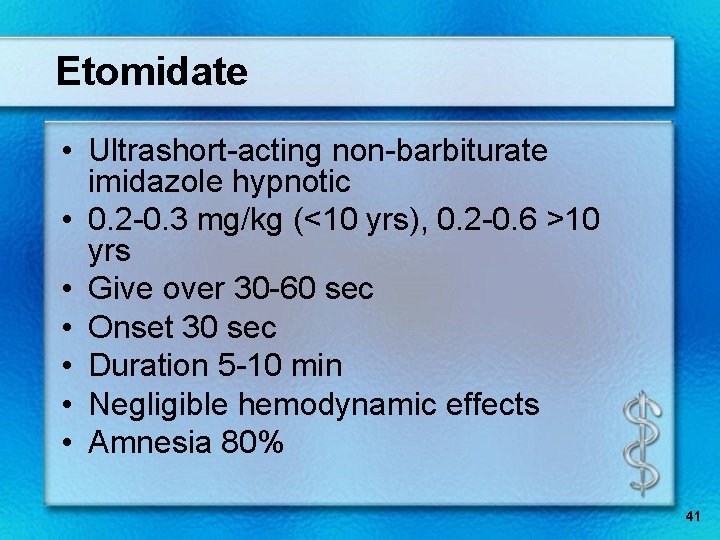
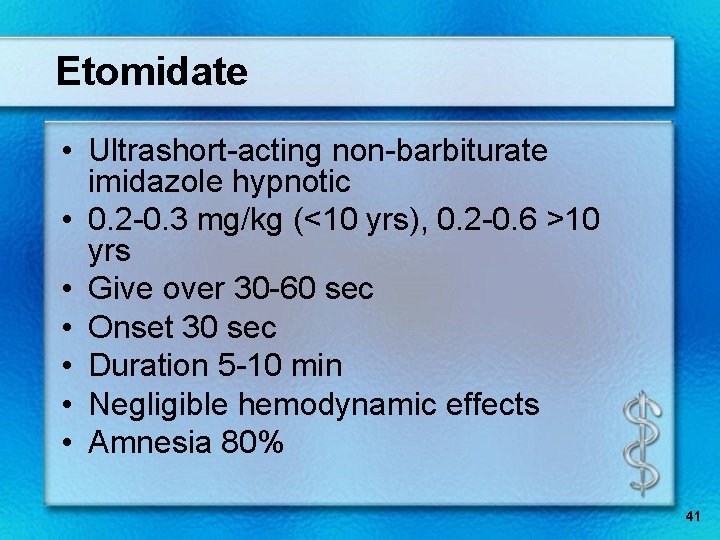
Etomidate • Ultrashort-acting non-barbiturate imidazole hypnotic • 0. 2 -0. 3 mg/kg (<10 yrs), 0. 2 -0. 6 >10 yrs • Give over 30 -60 sec • Onset 30 sec • Duration 5 -10 min • Negligible hemodynamic effects • Amnesia 80% 41
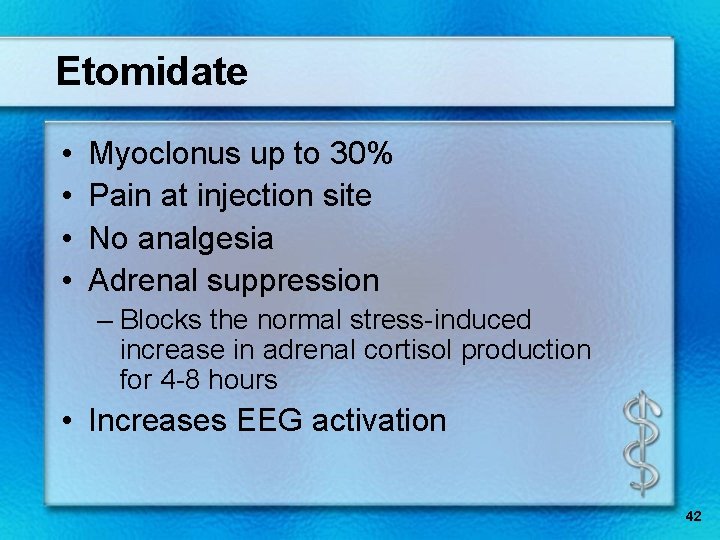
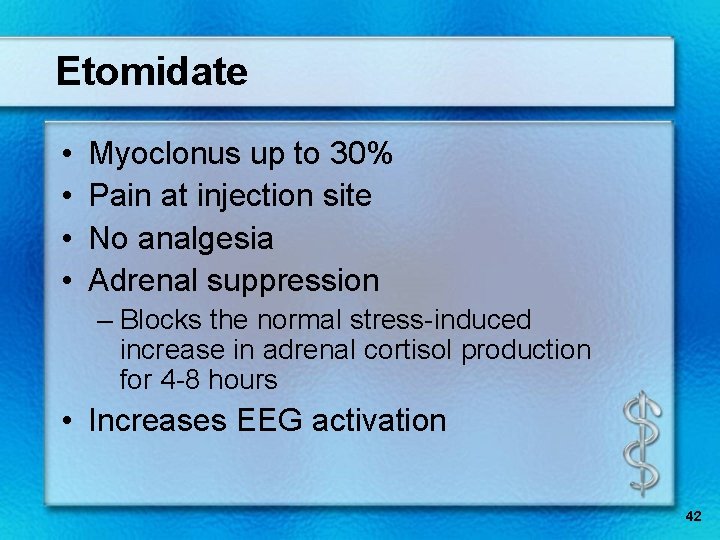
Etomidate • • Myoclonus up to 30% Pain at injection site No analgesia Adrenal suppression – Blocks the normal stress-induced increase in adrenal cortisol production for 4 -8 hours • Increases EEG activation 42
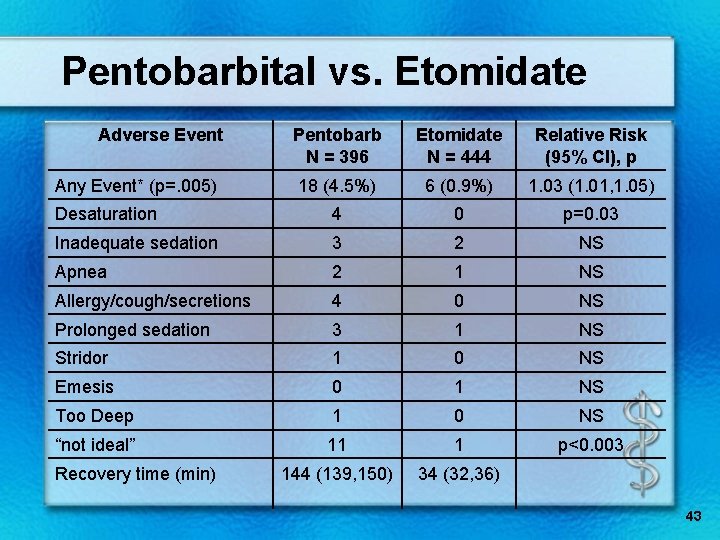
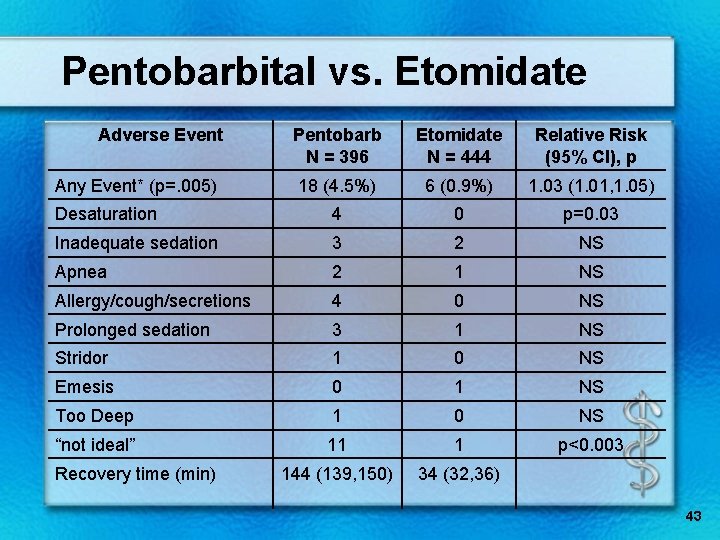
Pentobarbital vs. Etomidate Adverse Event Pentobarb N = 396 Etomidate N = 444 Relative Risk (95% CI), p 18 (4. 5%) 6 (0. 9%) 1. 03 (1. 01, 1. 05) Desaturation 4 0 p=0. 03 Inadequate sedation 3 2 NS Apnea 2 1 NS Allergy/cough/secretions 4 0 NS Prolonged sedation 3 1 NS Stridor 1 0 NS Emesis 0 1 NS Too Deep 1 0 NS “not ideal” 11 1 p<0. 003 144 (139, 150) 34 (32, 36) Any Event* (p=. 005) Recovery time (min) 43

44
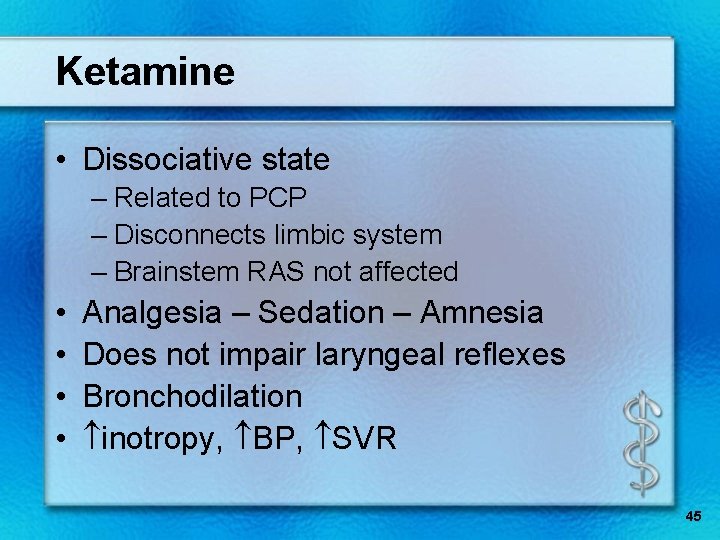
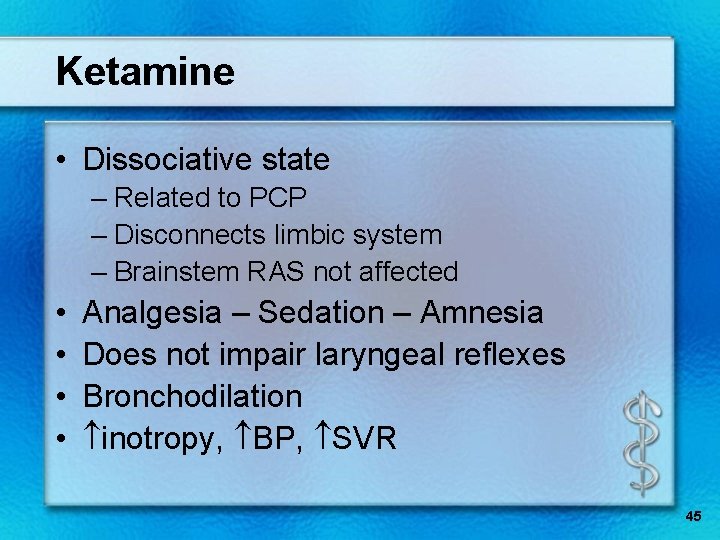
Ketamine • Dissociative state – Related to PCP – Disconnects limbic system – Brainstem RAS not affected • • Analgesia – Sedation – Amnesia Does not impair laryngeal reflexes Bronchodilation inotropy, BP, SVR 45
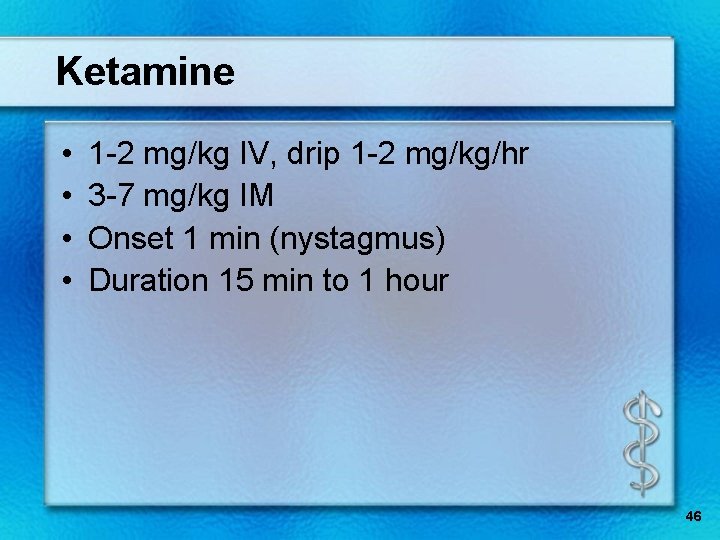
Ketamine • • 1 -2 mg/kg IV, drip 1 -2 mg/kg/hr 3 -7 mg/kg IM Onset 1 min (nystagmus) Duration 15 min to 1 hour 46
Ketamine • Secretions – Consider glycopyrrolate (Robinul) • Vomiting • Emergence 12% • Contraindications – ICP, glaucoma, open globe – <3 months of age – History of psychosis, porphyria 47
Propofol • • • Sedative-hypnotic 1 -3 mg/kg bolus over ~2 min 5 mg/kg/hr Infants need higher dose Sedative – Profound relaxation – Anti-emetic – Antiepileptic properties Fidget Yawn Out 48
Propofol • • Alkaline -- STINGS Contraindicated - egg or soy allergy Hypotension Rare bradycardia, acidosis leading to sudden death • No analgesia • Green urine 49
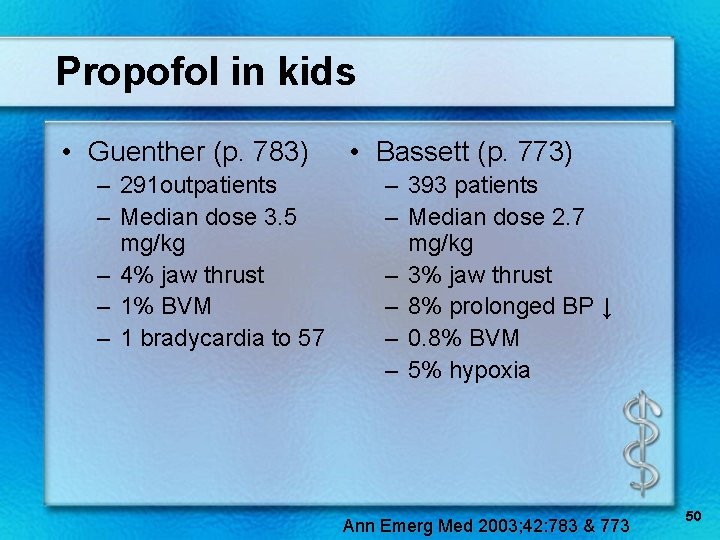
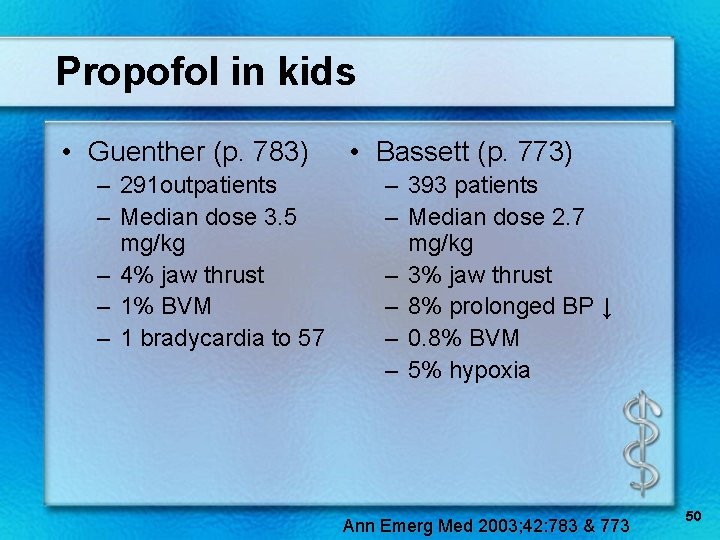
Propofol in kids • Guenther (p. 783) – 291 outpatients – Median dose 3. 5 mg/kg – 4% jaw thrust – 1% BVM – 1 bradycardia to 57 • Bassett (p. 773) – 393 patients – Median dose 2. 7 mg/kg – 3% jaw thrust – 8% prolonged BP ↓ – 0. 8% BVM – 5% hypoxia Ann Emerg Med 2003; 42: 783 & 773 50
Nitrous Oxide (NO 2) • • Sedative & analgesic Fi. O 2 0. 25 -1. 0 50% nitrous maximum In combo with ANY other sedation or narcotic = deep sedation • Need scavenger equipment • 10– 15% vomiting 51
Dexmedetomidine • α 2 -adrenergic receptor agonist – Sedative & analgesic effects • Non-invasive procedures in 48 kids – 15 after failing CH and/or midazolam • Dosage: – 0. 5 -1. 0 mcg/kg over 5 -10 min – Infusion 0. 5 -1. 0 mcg/kg/hr • Recovery (w/o other med) 69 ± 34 min • Minimal cardio-respiratory effect PCCM 2005; 6: 435 -9 52
Adverse events • • • >30, 000 ped sedations (26 hospitals) All providers, non-OR 50% propofol Docs: 28% ER, 28% ICU, 19% anesth. 0 deaths, 1 arrest, 1 aspiration Per 10, 000 sedations: – 24 apnea – 2 airway consult – 10 intubation – 27 oral airway – 7 admitted – 64 BVM Peds 2006; 118: 1087 53
Reducing errors • • • Fewer than 3 medications Experience Double check dosages Expect adverse events Ready to rescue! 54
“Just say no” • • • Music Video Quiet room Darken if possible Parents present 55
Goals – Sedation outside the OR • Guard safety & welfare of child • Minimize physical discomfort & pain • Control anxiety, maximize potential for amnesia • Control behavior & movement to complete procedure • Return patient to state safe for discharge 56
Meetings • Pediatric Sedation Outside the Operating Room – Boston – September 15 -16, 2007 • 2 nd International Multidisciplinary Conference on Pediatric Sedation – Savannah, GA – March, 2008 Society for Pediatric Sedation 57
Questions? 58
 Over-sedation
Over-sedation Poss sedation scale
Poss sedation scale Rikers sedation scale
Rikers sedation scale Rass sedation scale
Rass sedation scale Sédation
Sédation Richmond agitation sedation scale
Richmond agitation sedation scale Sccm pad guidelines
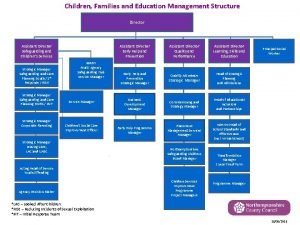
Sccm pad guidelines Childrens services walsall
Childrens services walsall Black childrens memorial
Black childrens memorial World book day quiz
World book day quiz Moli texaschildrens
Moli texaschildrens Levine childrens
Levine childrens Low grade fever
Low grade fever Christian children's fund inc
Christian children's fund inc National sovereignty and childrens day
National sovereignty and childrens day Manchester childrens university
Manchester childrens university History of childrens literature
History of childrens literature Childrens services
Childrens services Longman children's picture dictionary
Longman children's picture dictionary Kirklees safeguarding childrens board
Kirklees safeguarding childrens board Junior book awards 2018
Junior book awards 2018 Procedural constructs
Procedural constructs Procedural abstraction in c++
Procedural abstraction in c++ Liberty chapter 20
Liberty chapter 20 Procedural generation
Procedural generation Substantive vs procedural due process
Substantive vs procedural due process Sql procedural
Sql procedural Primary reliance on researcher to deal with procedural bias
Primary reliance on researcher to deal with procedural bias Logical cohesion example
Logical cohesion example Pluralist democracy
Pluralist democracy Biomedical concept of health
Biomedical concept of health Substantive vs procedural due process
Substantive vs procedural due process Dr eti poncorini
Dr eti poncorini Procedural knowledge in ai
Procedural knowledge in ai Function abstraction
Function abstraction Features of a procedural text
Features of a procedural text Apa pengertian dari procedural dependency
Apa pengertian dari procedural dependency Verilog procedural interface
Verilog procedural interface Equal protection clause
Equal protection clause Superpipeline
Superpipeline What is procedural programming
What is procedural programming Substantive vs procedural due process
Substantive vs procedural due process Dimension of classroom management
Dimension of classroom management Hrinfo dadeschools net dpgt
Hrinfo dadeschools net dpgt 2d procedural animation
2d procedural animation Procedural vs functional
Procedural vs functional Java scripting
Java scripting Encoding failure ap psychology
Encoding failure ap psychology Compare procedural semantics and declarative semantics.
Compare procedural semantics and declarative semantics. Due process definition law
Due process definition law What is procedural fluency
What is procedural fluency Isa 95 model
Isa 95 model Procedural abstraction c++
Procedural abstraction c++ Blender procedural generation
Blender procedural generation Verilog procedural assignment
Verilog procedural assignment Procedure justice
Procedure justice Procedural unconscionability
Procedural unconscionability Computable functions and predicates in ai
Computable functions and predicates in ai Procedural self
Procedural self