Paediatric Procedural Sedation v 2011 Royal Children Hospital

- Slides: 29
Paediatric Procedural Sedation v. 2011 Royal Children Hospital ECIICN Victorian Managed Insurance Authority
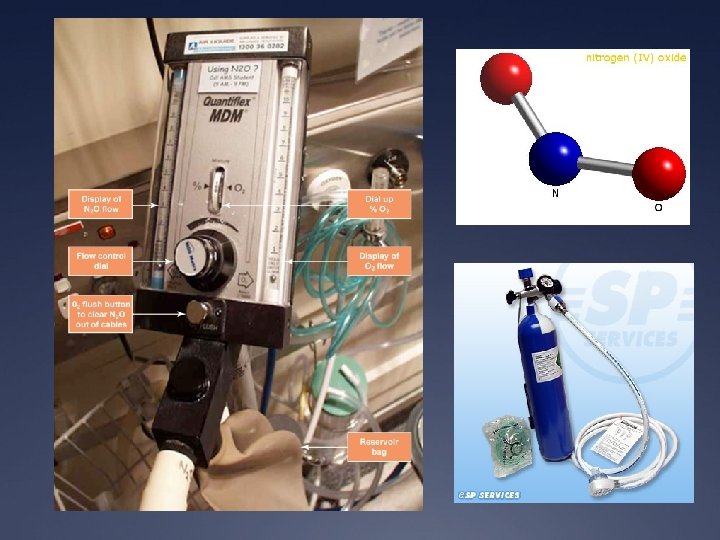
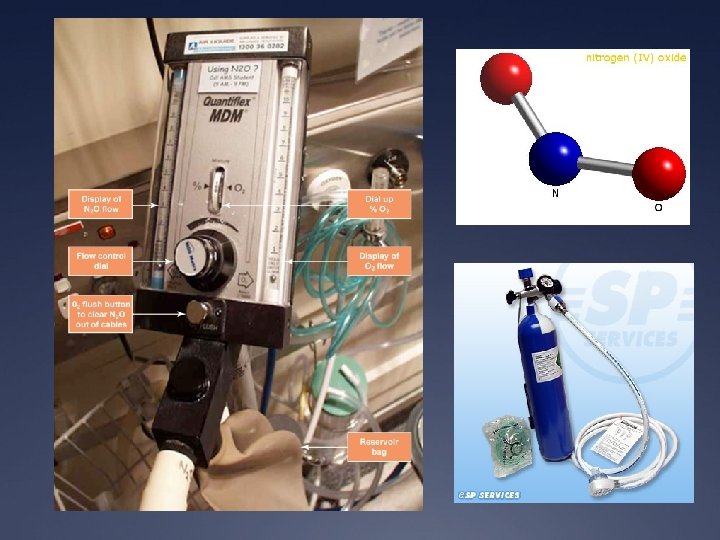
Program Ü Talk Ü Read handout on nitrous connections Ü Nitrous machine practical set up
Goal Ü Physical and psychological distress Ü Optimal environment for success Analgesia Anxiolysis Amnesia Awareness
Who is this talk for ? Ü Deliver quality care consistent with evidence base Ü Minimise risk and adverse events Ü Able to administer procedural sedation safely Ü Able to recognise and address undesirable events (rescue capacity)
Ü http: //www. youtube. com/watch? v=t. GNy. WDlu. ELQ Ü http: //www. youtube. com/watch? v=gm. Nwp. Jf 1 z. UQ Beware in asthmatics / RTI
General principles Ü Will my sedation plan achieve the best outcome for THIS patient ? Ü Successful sedation doesn’t always guarantee success of procedure or best outcome Ü What simple things can I do to reduce anxiety and need for sedation? Ü Preparation and post-procedural issues Ü Patient, Staff, Place
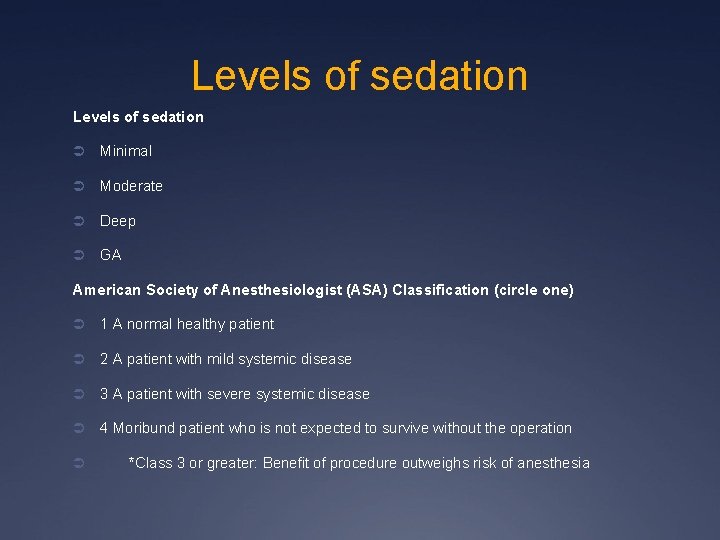
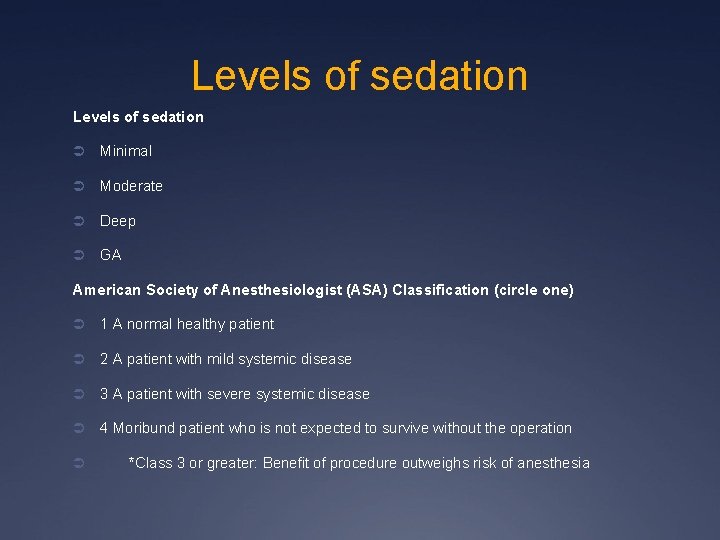
Levels of sedation Ü Minimal Ü Moderate Ü Deep Ü GA American Society of Anesthesiologist (ASA) Classification (circle one) Ü 1 A normal healthy patient Ü 2 A patient with mild systemic disease Ü 3 A patient with severe systemic disease Ü 4 Moribund patient who is not expected to survive without the operation Ü *Class 3 or greater: Benefit of procedure outweighs risk of anesthesia
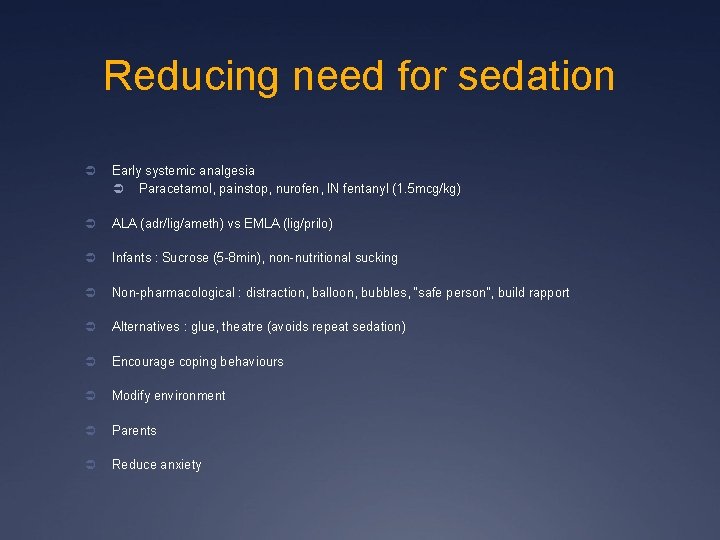
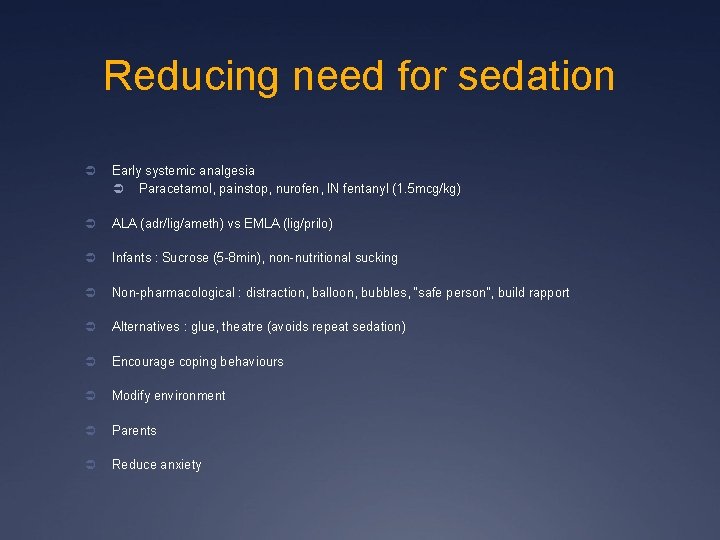
Reducing need for sedation Ü Early systemic analgesia Ü Paracetamol, painstop, nurofen, IN fentanyl (1. 5 mcg/kg) Ü ALA (adr/lig/ameth) vs EMLA (lig/prilo) Ü Infants : Sucrose (5 -8 min), non-nutritional sucking Ü Non-pharmacological : distraction, balloon, bubbles, “safe person”, build rapport Ü Alternatives : glue, theatre (avoids repeat sedation) Ü Encourage coping behaviours Ü Modify environment Ü Parents Ü Reduce anxiety
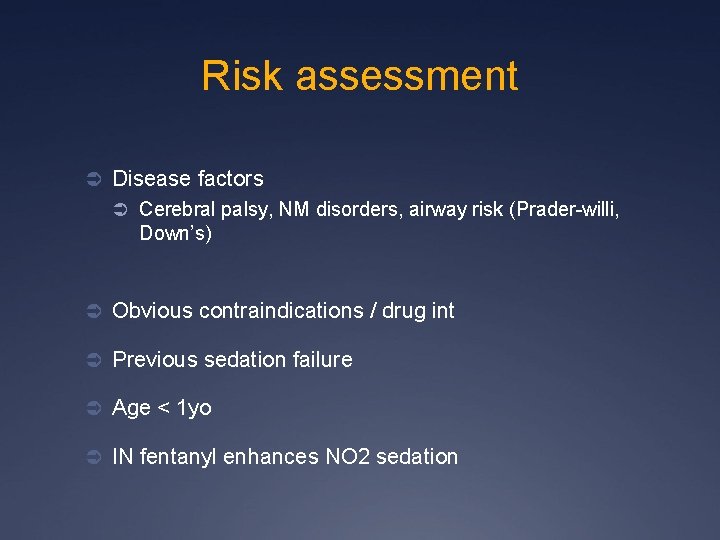
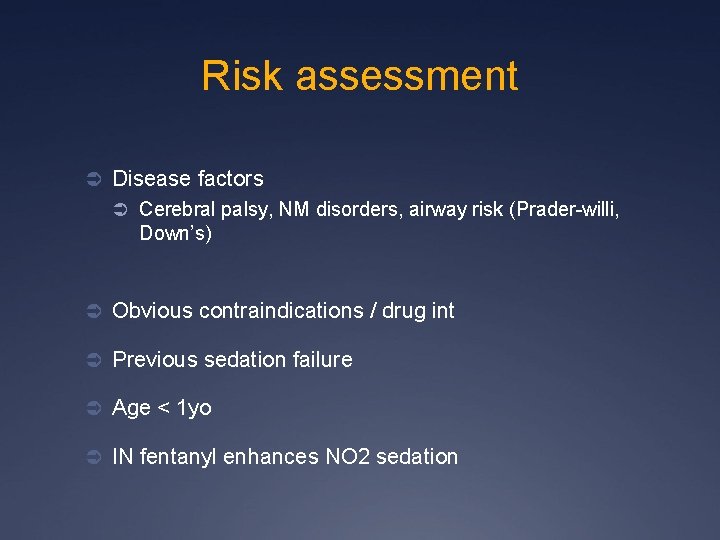
Risk assessment Ü Disease factors Ü Cerebral palsy, NM disorders, airway risk (Prader-willi, Down’s) Ü Obvious contraindications / drug int Ü Previous sedation failure Ü Age < 1 yo Ü IN fentanyl enhances NO 2 sedation
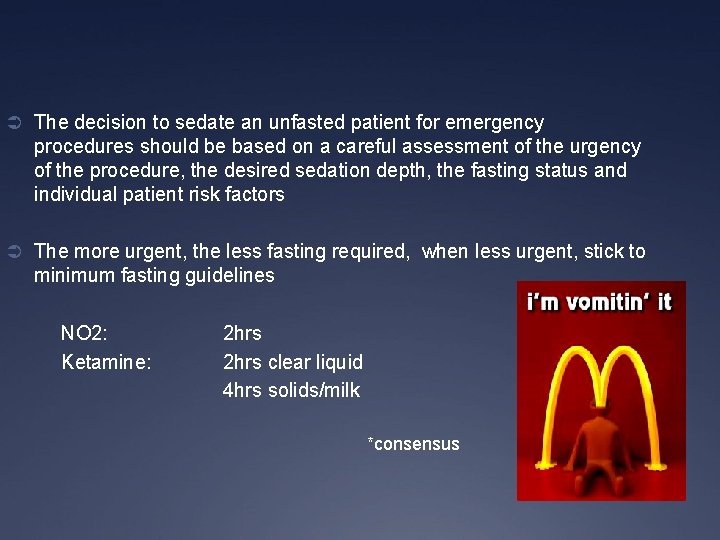
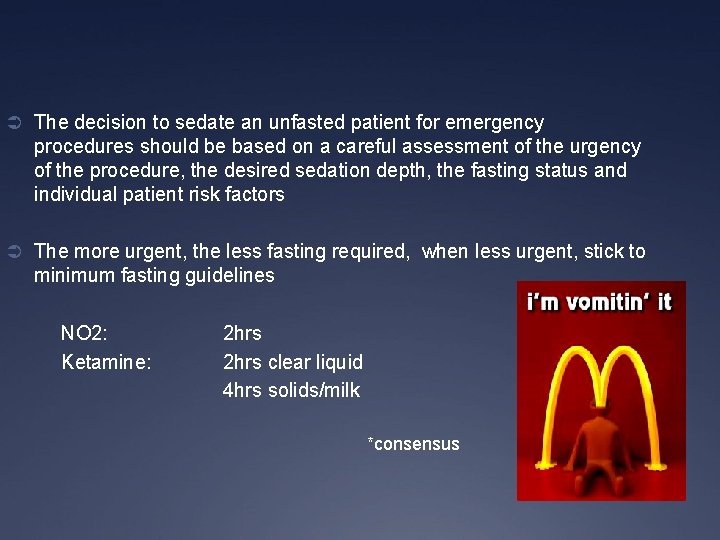
Ü The decision to sedate an unfasted patient for emergency procedures should be based on a careful assessment of the urgency of the procedure, the desired sedation depth, the fasting status and individual patient risk factors Ü The more urgent, the less fasting required, when less urgent, stick to minimum fasting guidelines NO 2: Ketamine: 2 hrs clear liquid 4 hrs solids/milk *consensus
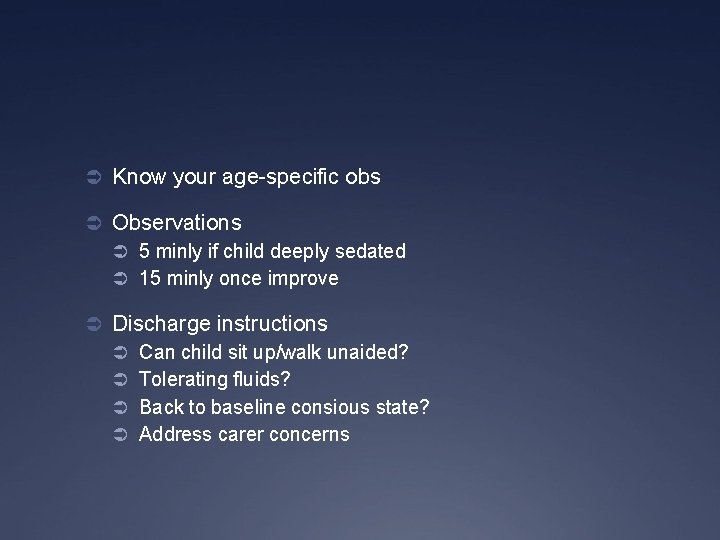
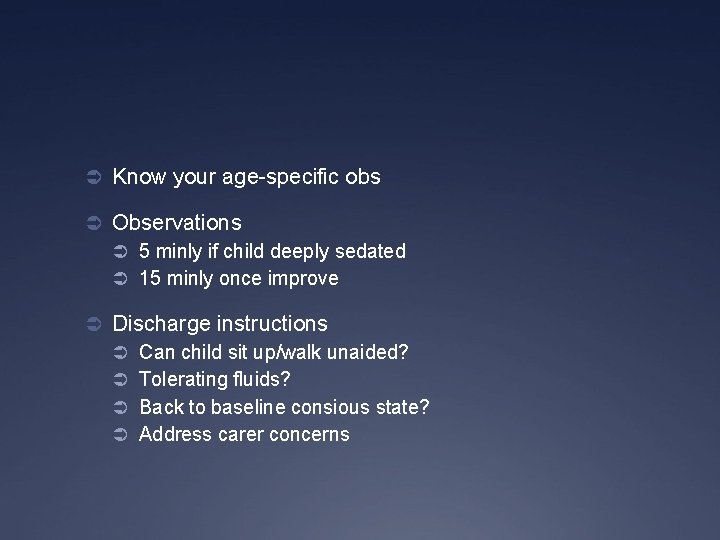
Ü Know your age-specific obs Ü Observations Ü 5 minly if child deeply sedated Ü 15 minly once improve Ü Discharge instructions Ü Can child sit up/walk unaided? Ü Tolerating fluids? Ü Back to baseline consious state? Ü Address carer concerns
N 20 Ü Inert colourless odourless Ü First synthesized in 1772 Joseph Priestley Ü “laughing gas” – Sir Humphry Davy Ü Promotes opioid peptide release from midbrain Ü Weak anaesthetic Ü Low solubility => rapid onset
N 20 pros ? Ü Short acting, titratable Ü Fast onset 3 -5 mins, fast offset Ü Inhalational analgesia and anasthesia Ü Safe Ü Requires a good seal with dedicated administrator
N 20 cons ? Ü Vomiting (6% at home), light-headedness Ü Excessive sedation (caution URTI) Ü Requires cooperative child Ü Pregnant staff exclusion Ü Efficacy – not for all Ü Not useful for certain procedures Ü BM / Neurotoxicity, B 12 def (rare)
N 20 tips Ü Check supply Ü Check connections Ü Scavenger – medium flow Ü Suction Ü Bag : encourage blowing, hose : elephant nose Ü Additional O 2 mask/BVM Ü Flavoured scents Ü Familiarise child with equipment Ü OK to apply obs post. NO 2 taking effect
Ü Dose ?
Handout “Use of Nitrous Oxide in the ED”
“Vitamin K” Ü Dissociative anaesthetic Ü Hallucinatory reactions abused Ü Nightmares Ü Delirium
Ketamine pros Ü Major advantages Ü Immobilisation Ü Maintenance of airway and resp drive Ü Profound analgesia Ü Mechanism of action Ü Cardiac stable
Ketamine cons? Ü Overall uncommon and minor Ü Vomiting 8. 6% Ü Emergence 7. 6% Ü Airway / Resp 3. 9% Ü No association with fasting Ü IV vs IM Ü Longer onset and longer LOS with IM Ü Balanced with distress of IV insertion
Respiratory Ü Resp depression (very young, rapid push) Ü Stridor (malpositioning of the airway) Ü Laryngospasm Ü 0. 002 -0. 3% incidence, 1/22 cases required ETT Ü Idiosyncratic Ü Airway support, PEEP and wait Ü Hypersalivation (X atropine, may increase events)
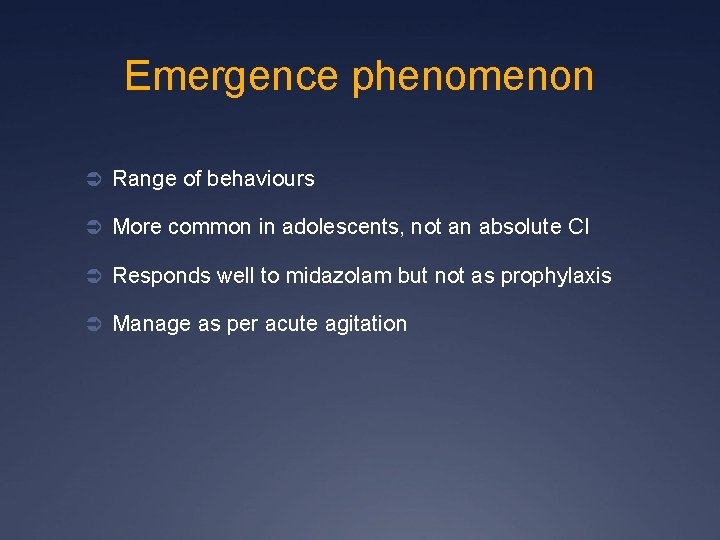
Emergence phenomenon Ü Range of behaviours Ü More common in adolescents, not an absolute CI Ü Responds well to midazolam but not as prophylaxis Ü Manage as per acute agitation
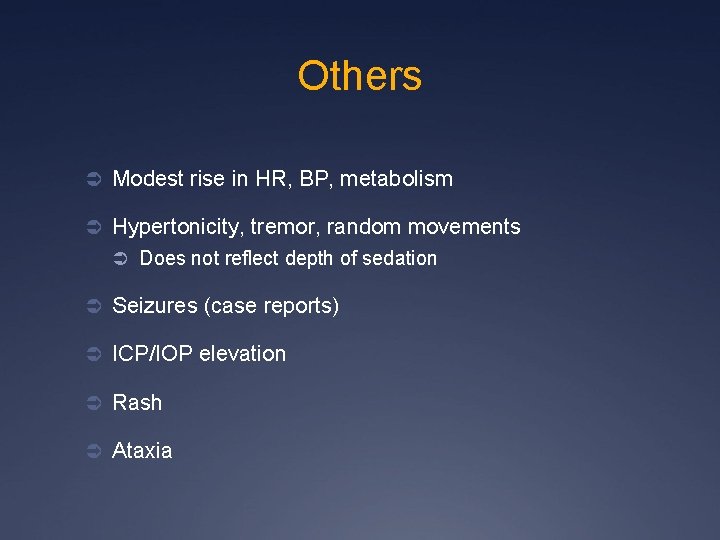
Others Ü Modest rise in HR, BP, metabolism Ü Hypertonicity, tremor, random movements Ü Does not reflect depth of sedation Ü Seizures (case reports) Ü ICP/IOP elevation Ü Rash Ü Ataxia
CI Ü Children < one year / >12 years Ü Previous adverse reaction to ketamine Ü Active respiratory tract infection or disease Ü Procedures involving the lower airway or pharynx Ü Heart disease Ü Bowel obstruction Ü Psychosis / ADHD Ü Porphyria Ü Thyrotoxicosis Ü Unstable epilepsy Ü Glaucoma Ü Central nervous system masses, hydrocephalus
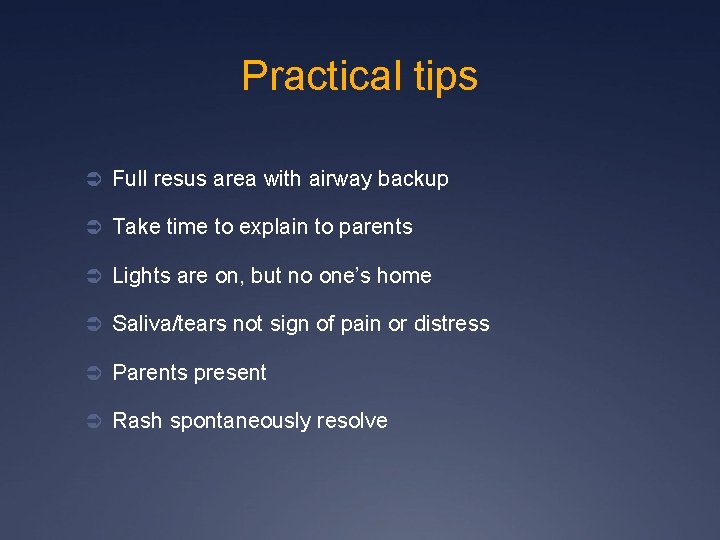
Practical tips Ü Full resus area with airway backup Ü Take time to explain to parents Ü Lights are on, but no one’s home Ü Saliva/tears not sign of pain or distress Ü Parents present Ü Rash spontaneously resolve
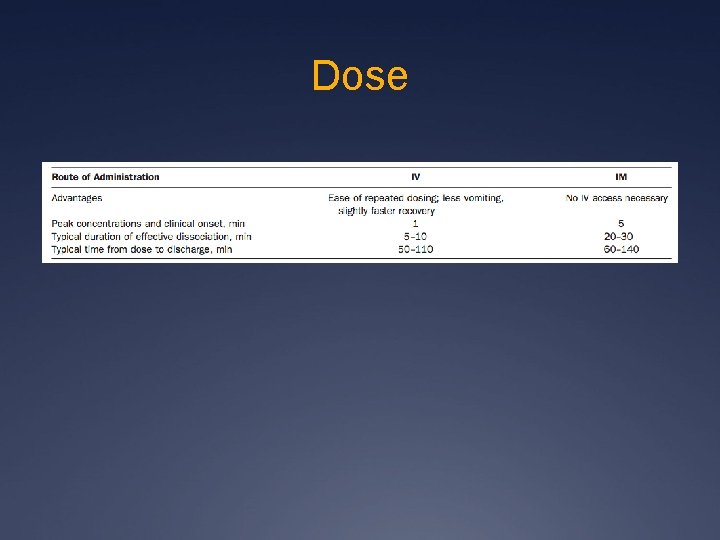
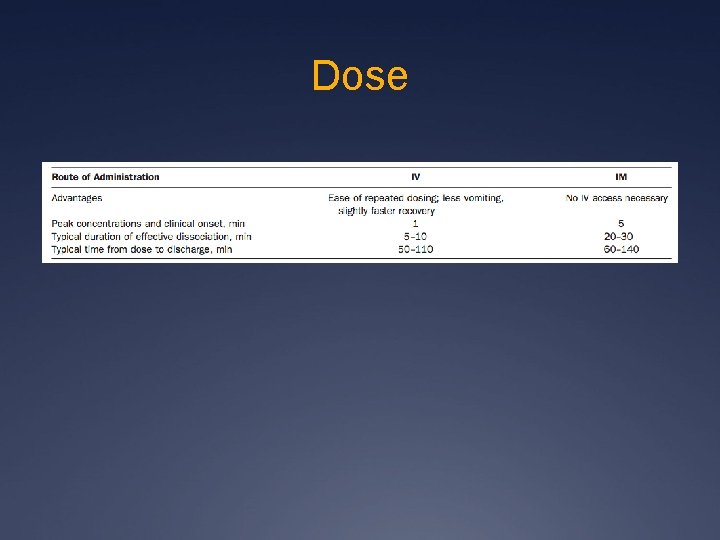
Dose

 Sccm sedation guidelines
Sccm sedation guidelines Over-sedation
Over-sedation Poss sedation scale
Poss sedation scale Rikers sedation scale
Rikers sedation scale Rass sedation scale
Rass sedation scale Sédation
Sédation Richmond agitation sedation scale
Richmond agitation sedation scale Royal surrey hospital buses
Royal surrey hospital buses Professor abudu royal orthopaedic hospital
Professor abudu royal orthopaedic hospital Arthur davison
Arthur davison Abolfazl asudeh
Abolfazl asudeh Texas children's pawsitive play
Texas children's pawsitive play Wilhelmina children's hospital
Wilhelmina children's hospital Children's hospital lahore
Children's hospital lahore Severance children's hospital
Severance children's hospital Moli texas children's
Moli texas children's Physical environment for a sick child in pediatric ward
Physical environment for a sick child in pediatric ward Pews chart nz
Pews chart nz Paediatric et tube size formula
Paediatric et tube size formula Paediatric fluid balance chart
Paediatric fluid balance chart Paediatric chalk mixture
Paediatric chalk mixture Drug calculation
Drug calculation Supracondylar fracture rch
Supracondylar fracture rch Definition of pediatric nursing
Definition of pediatric nursing Concept of child care
Concept of child care Paediatric respiratory history
Paediatric respiratory history Pediatric triangle assessment
Pediatric triangle assessment Azioni blsp
Azioni blsp Mallampati grad
Mallampati grad North thames paediatric network
North thames paediatric network