Pediatric Case Conference Anaphylaxis R 1 General Data





- Slides: 44
Pediatric Case Conference Anaphylaxis 報告:R 1郭靖怡 指導醫師: 吳孟書醫師
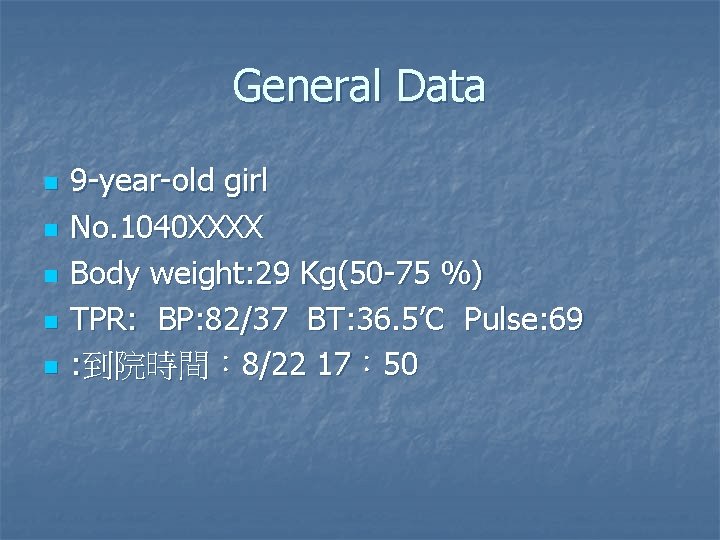
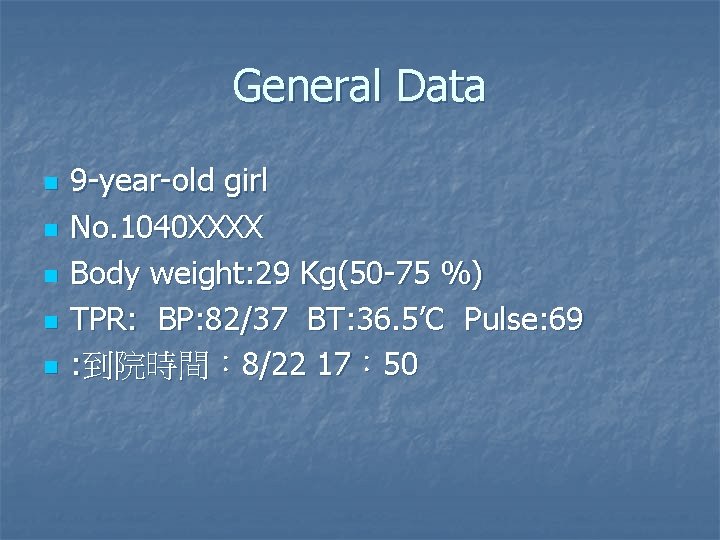
General Data n n n 9 -year-old girl No. 1040 XXXX Body weight: 29 Kg(50 -75 %) TPR: BP: 82/37 BT: 36. 5’C Pulse: 69 : 到院時間: 8/22 17: 50

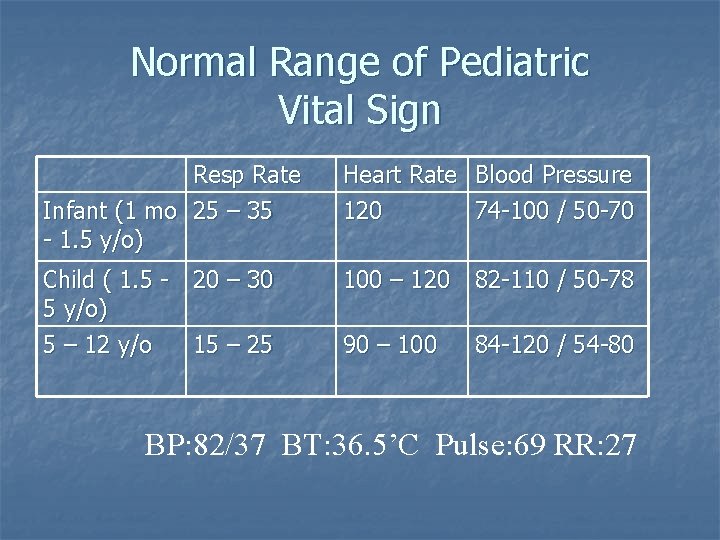
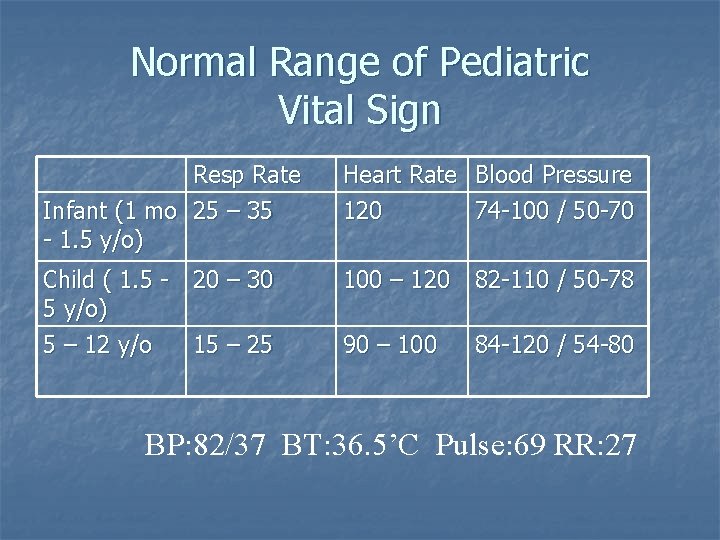
Normal Range of Pediatric Vital Sign Resp Rate Infant (1 mo 25 – 35 - 1. 5 y/o) Heart Rate 120 Blood Pressure 74 -100 / 50 -70 Child ( 1. 5 - 20 – 30 5 y/o) 5 – 12 y/o 15 – 25 100 – 120 82 -110 / 50 -78 90 – 100 84 -120 / 54 -80 BP: 82/37 BT: 36. 5’C Pulse: 69 RR: 27
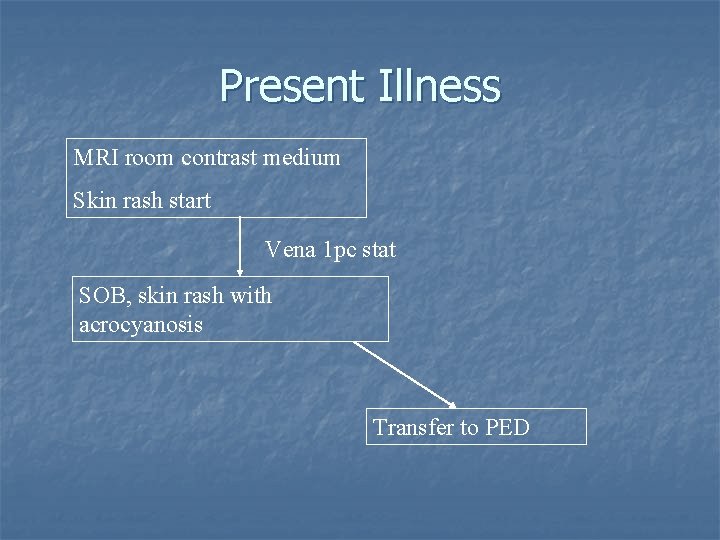
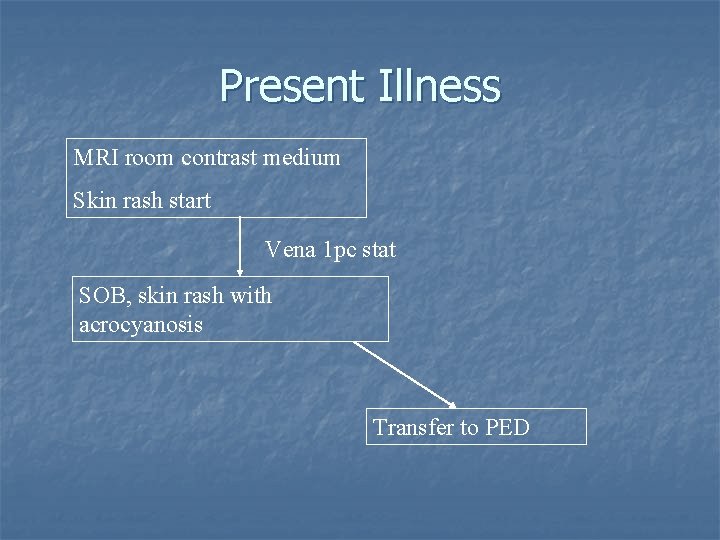
Present Illness MRI room contrast medium Skin rash start Vena 1 pc stat SOB, skin rash with acrocyanosis Transfer to PED
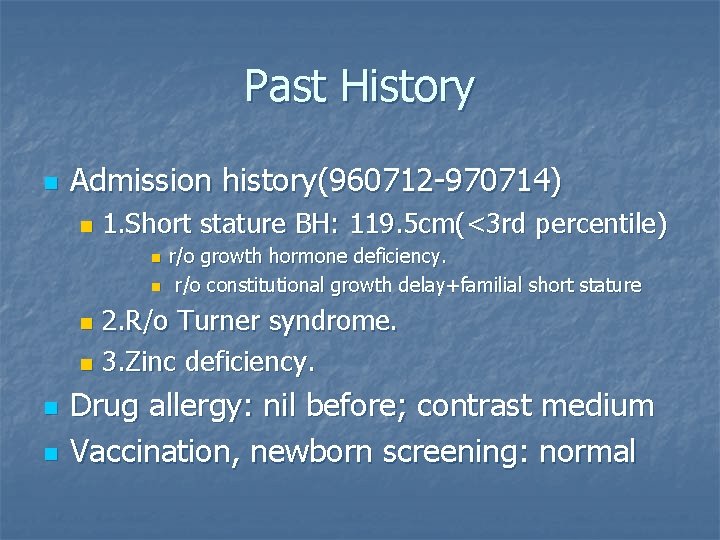
Past History n Admission history(960712 -970714) n 1. Short stature BH: 119. 5 cm(<3 rd percentile) n n r/o growth hormone deficiency. r/o constitutional growth delay+familial short stature 2. R/o Turner syndrome. n 3. Zinc deficiency. n n n Drug allergy: nil before; contrast medium Vaccination, newborn screening: normal
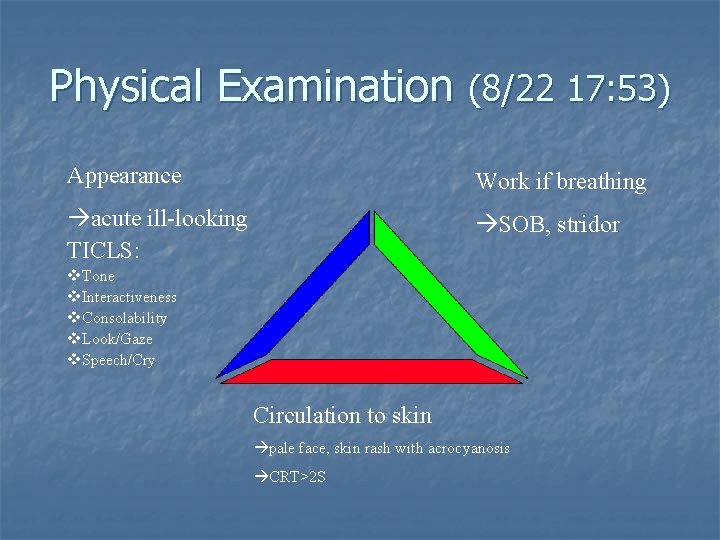
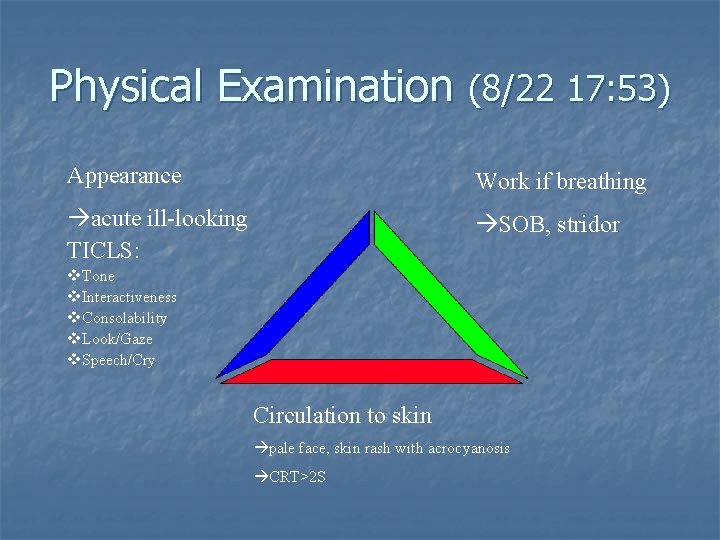
Physical Examination (8/22 17: 53) Appearance Work if breathing acute ill-looking TICLS: SOB, stridor v. Tone v. Interactiveness v. Consolability v. Look/Gaze v. Speech/Cry Circulation to skin pale face, skin rash with acrocyanosis CRT>2 S
What would you do next?
Evaluate patient n n PAT ABCED
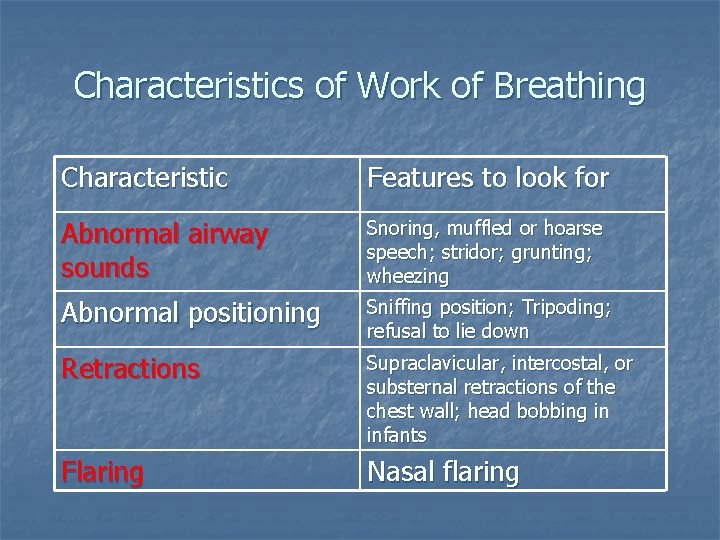
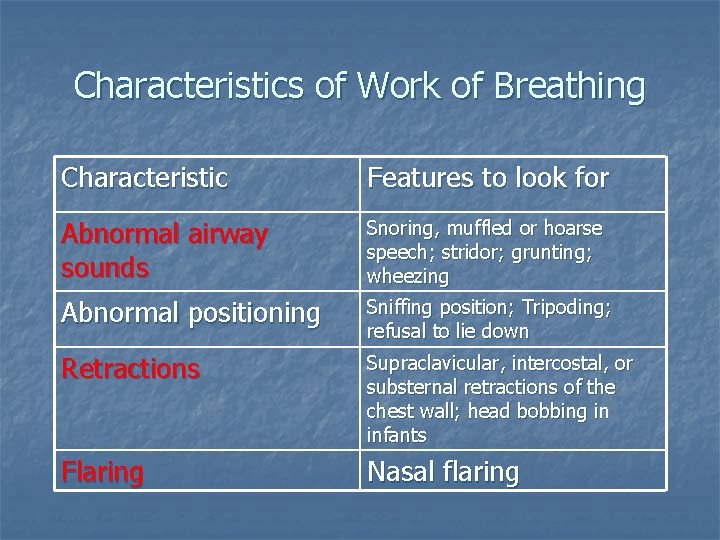
Characteristics of Work of Breathing Characteristic Features to look for Abnormal airway sounds Snoring, muffled or hoarse speech; stridor; grunting; wheezing Abnormal positioning Sniffing position; Tripoding; refusal to lie down Retractions Supraclavicular, intercostal, or substernal retractions of the chest wall; head bobbing in infants Flaring Nasal flaring
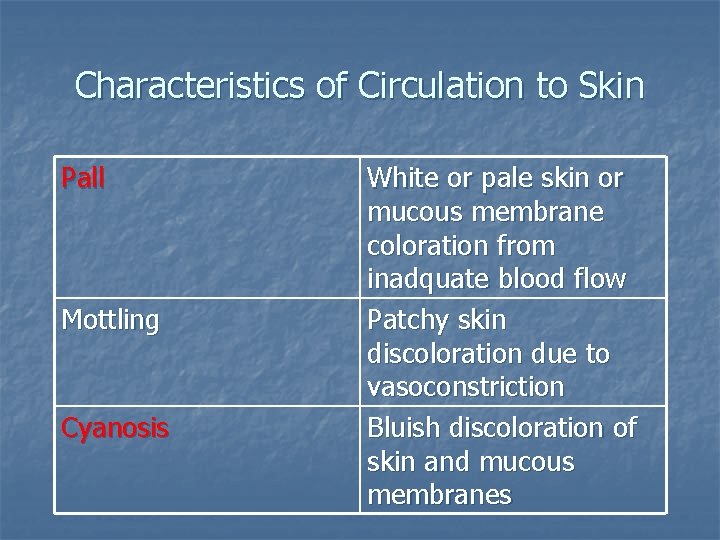
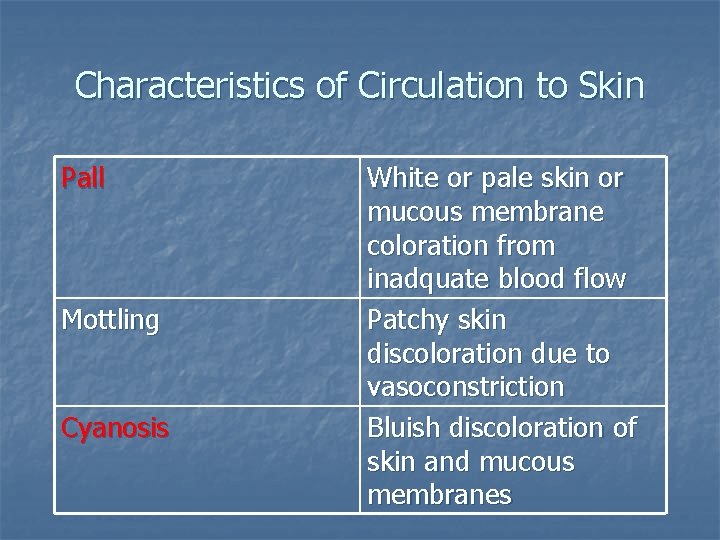
Characteristics of Circulation to Skin Pall Mottling Cyanosis White or pale skin or mucous membrane coloration from inadquate blood flow Patchy skin discoloration due to vasoconstriction Bluish discoloration of skin and mucous membranes
Assessing the Pediatric ABCDEs n n n Airway Breathing Circulation Disability Exposure
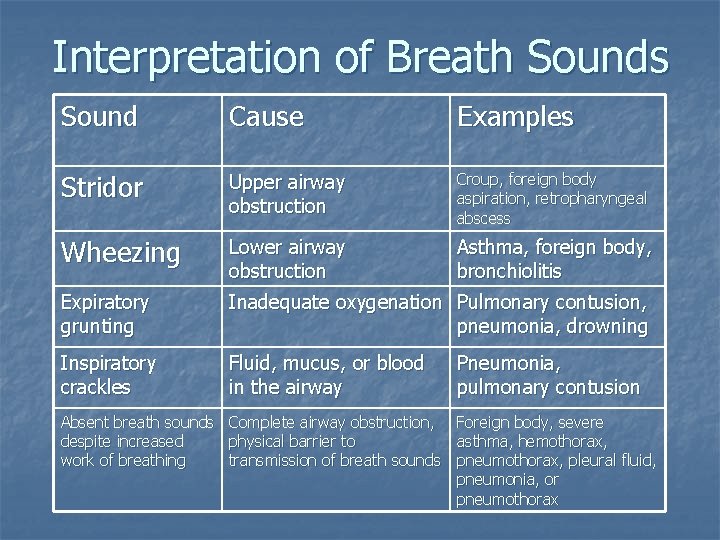
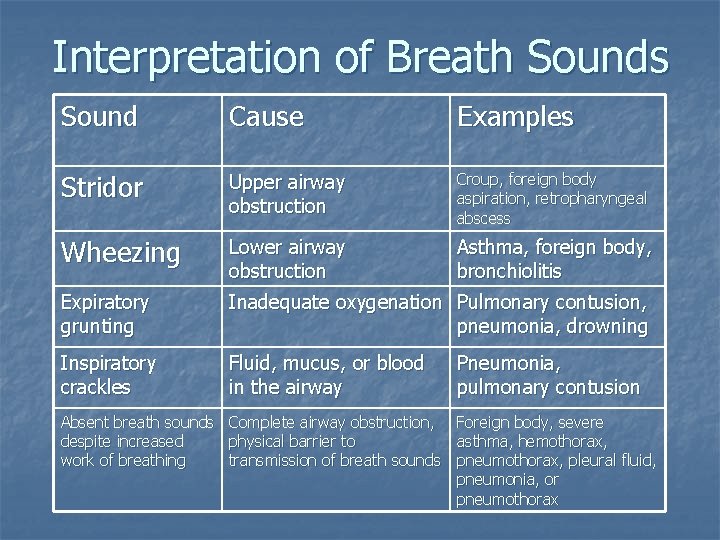
Interpretation of Breath Sounds Sound Cause Examples Stridor Upper airway obstruction Croup, foreign body aspiration, retropharyngeal abscess Wheezing Lower airway obstruction Asthma, foreign body, bronchiolitis Expiratory grunting Inadequate oxygenation Pulmonary contusion, pneumonia, drowning Inspiratory crackles Fluid, mucus, or blood in the airway Pneumonia, pulmonary contusion Absent breath sounds despite increased work of breathing Complete airway obstruction, physical barrier to transmission of breath sounds Foreign body, severe asthma, hemothorax, pneumothorax, pleural fluid, pneumonia, or pneumothorax
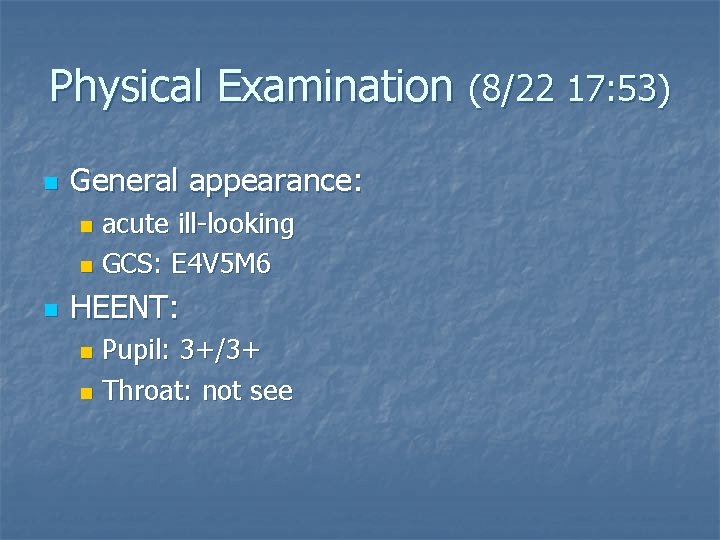
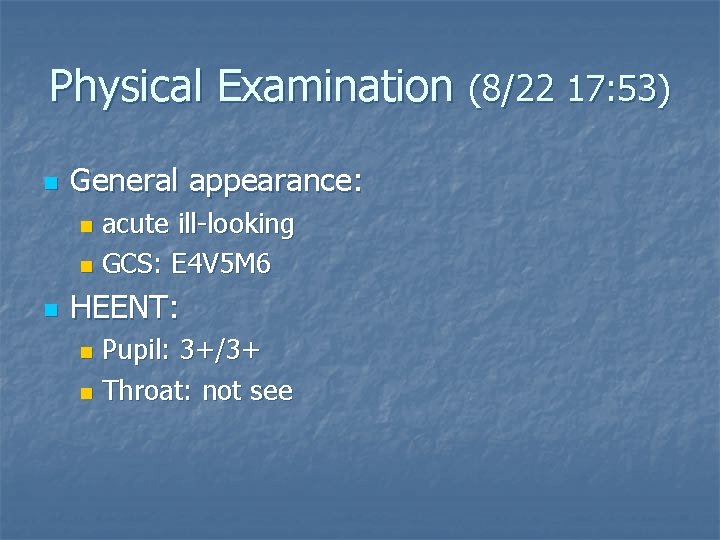
Physical Examination (8/22 17: 53) n General appearance: acute ill-looking n GCS: E 4 V 5 M 6 n n HEENT: Pupil: 3+/3+ n Throat: not see n
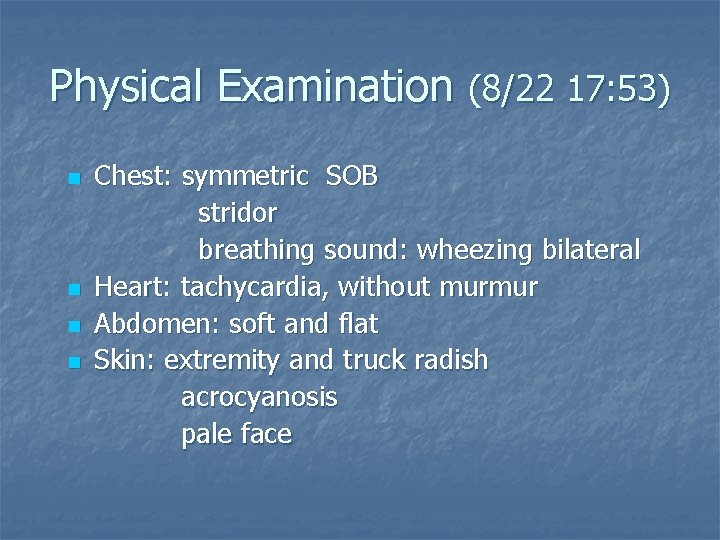
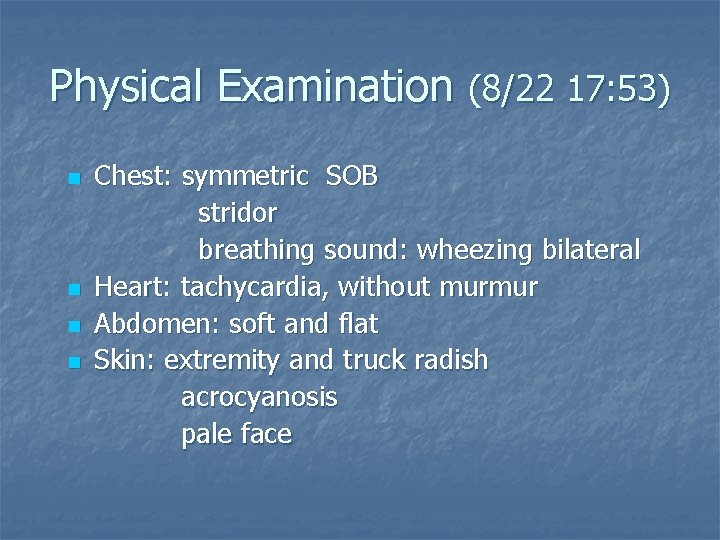
Physical Examination (8/22 17: 53) n n Chest: symmetric SOB stridor breathing sound: wheezing bilateral Heart: tachycardia, without murmur Abdomen: soft and flat Skin: extremity and truck radish acrocyanosis pale face
What Action will You Take?

Initial Impression n Anaphylaxis of MRI contrast medium
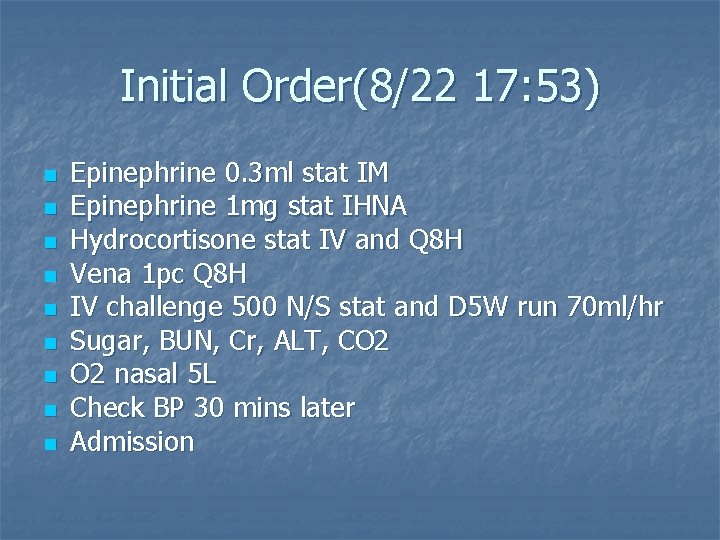
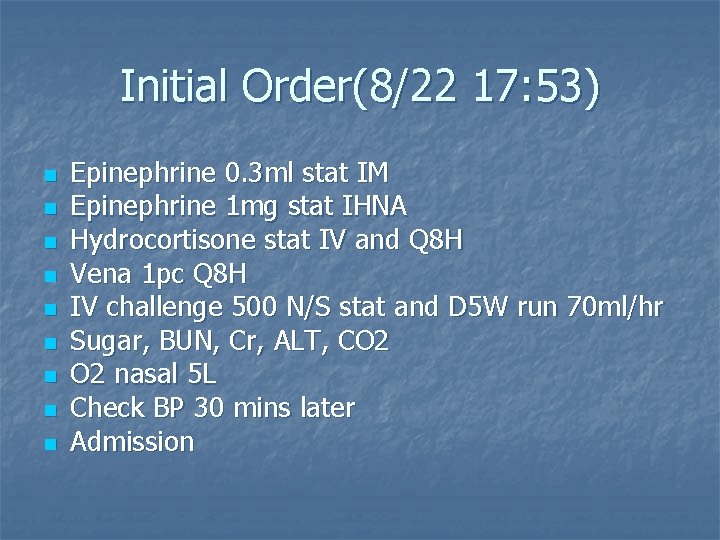
Initial Order(8/22 17: 53) n n n n n Epinephrine 0. 3 ml stat IM Epinephrine 1 mg stat IHNA Hydrocortisone stat IV and Q 8 H Vena 1 pc Q 8 H IV challenge 500 N/S stat and D 5 W run 70 ml/hr Sugar, BUN, Cr, ALT, CO 2 nasal 5 L Check BP 30 mins later Admission

After Epinephrine Use
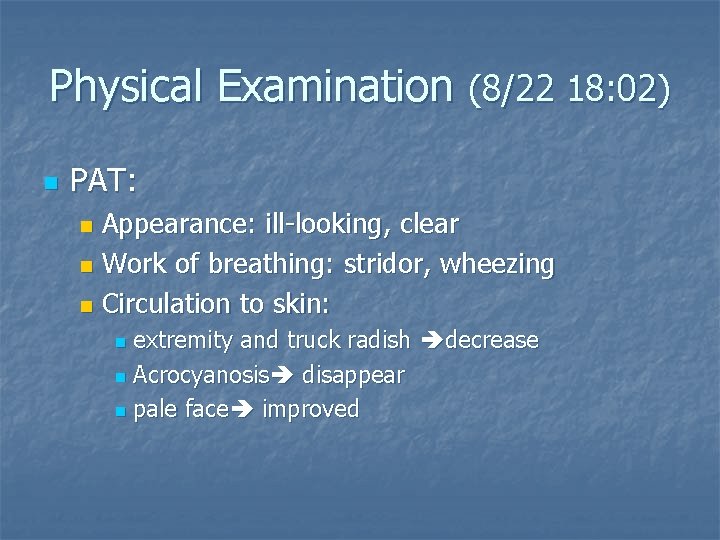
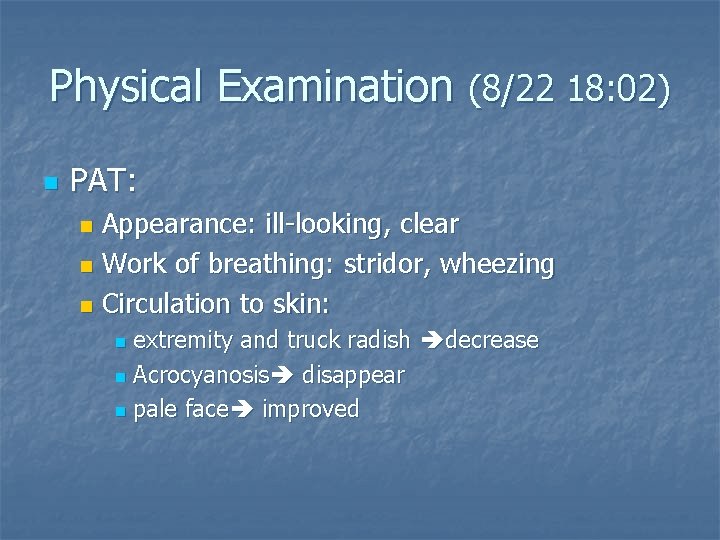
Physical Examination (8/22 18: 02) n PAT: Appearance: ill-looking, clear n Work of breathing: stridor, wheezing n Circulation to skin: n extremity and truck radish decrease n Acrocyanosis disappear n pale face improved n
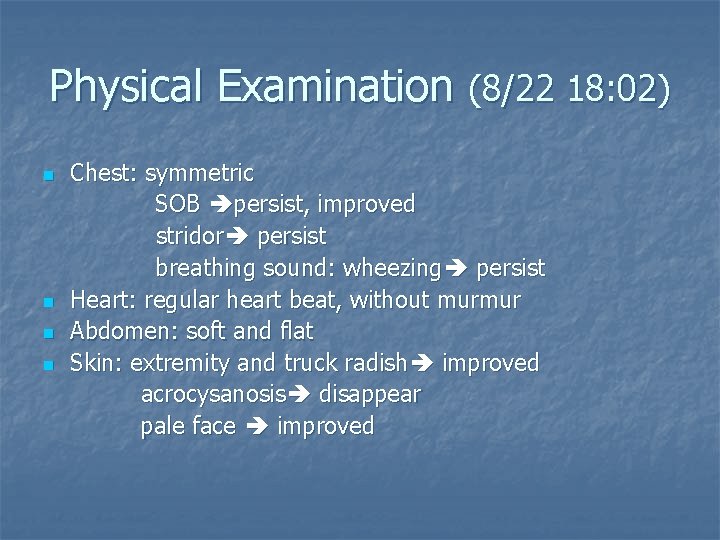
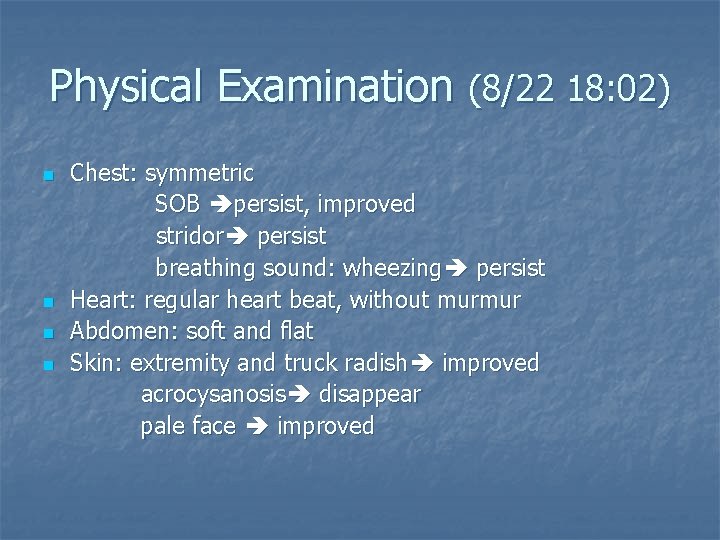
Physical Examination (8/22 18: 02) n n Chest: symmetric SOB persist, improved stridor persist breathing sound: wheezing persist Heart: regular heart beat, without murmur Abdomen: soft and flat Skin: extremity and truck radish improved acrocysanosis disappear pale face improved
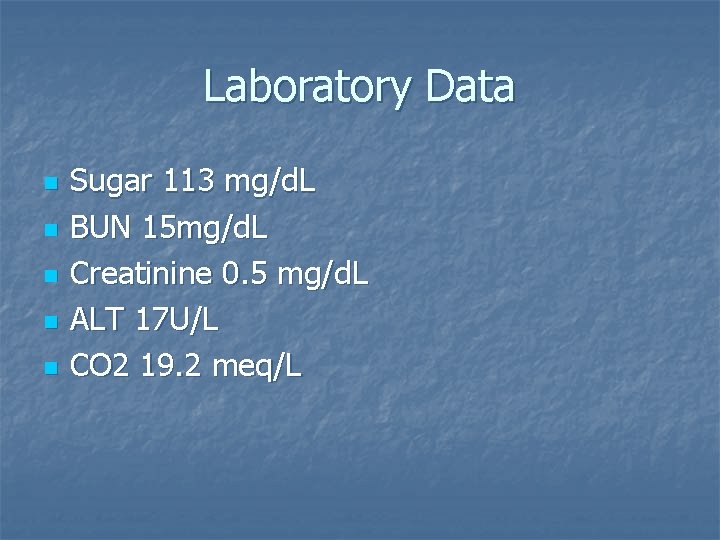
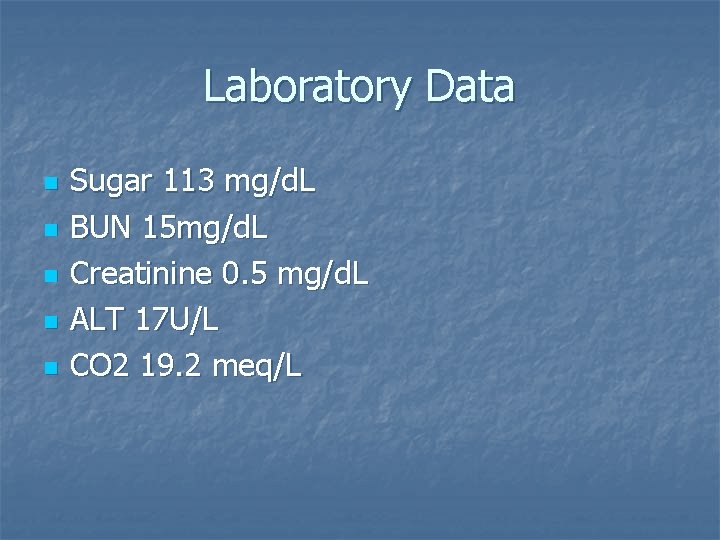
Laboratory Data n n n Sugar 113 mg/d. L BUN 15 mg/d. L Creatinine 0. 5 mg/d. L ALT 17 U/L CO 2 19. 2 meq/L
Discussion Anaphylaxis
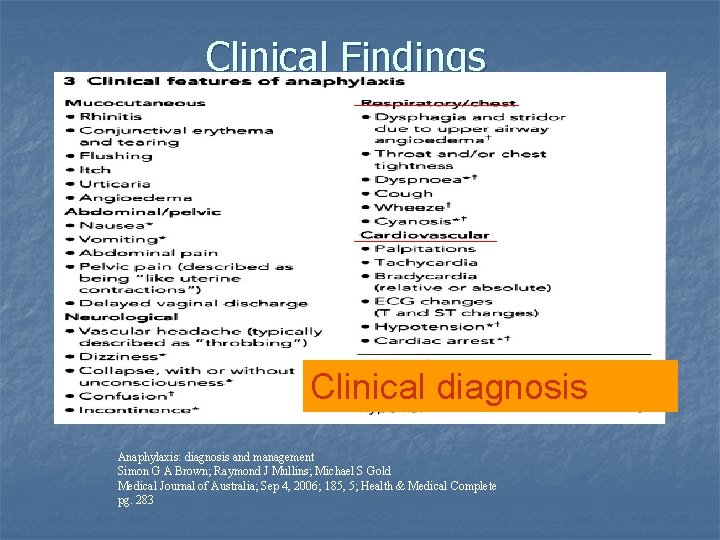
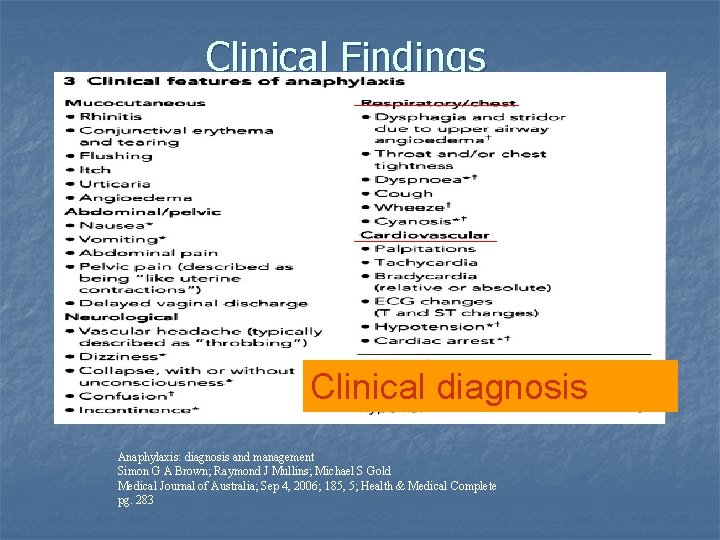
Clinical Findings Clinical diagnosis Anaphylaxis: diagnosis and management Simon G A Brown; Raymond J Mullins; Michael S Gold Medical Journal of Australia; Sep 4, 2006; 185, 5; Health & Medical Complete pg. 283
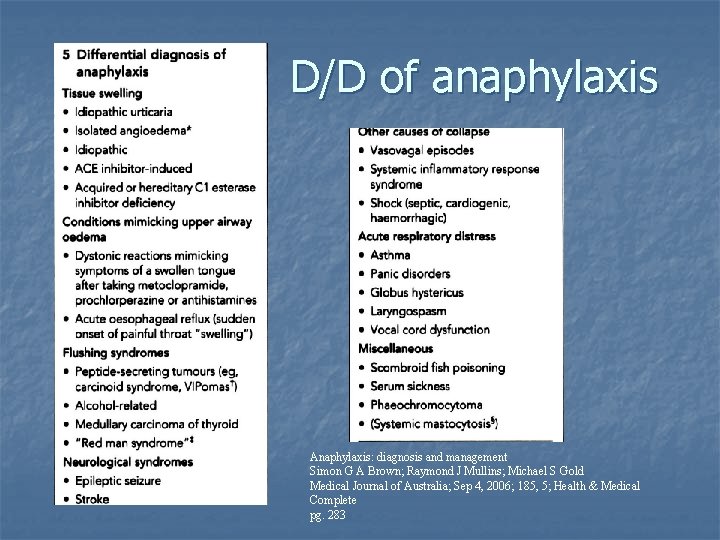
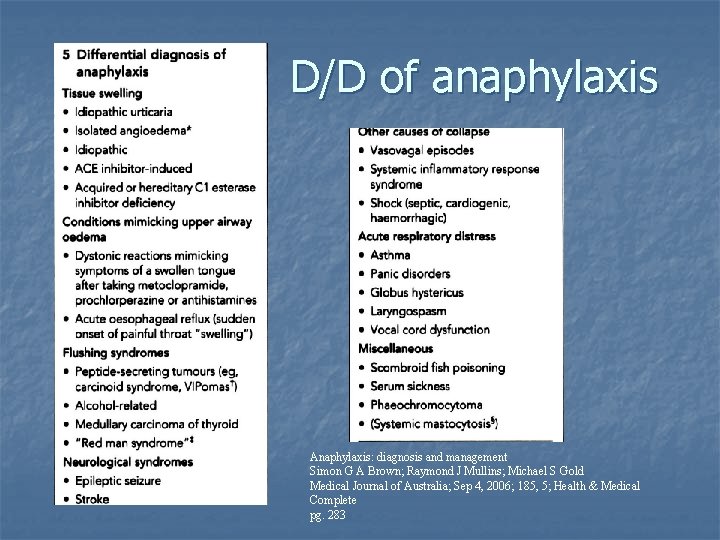
D/D of anaphylaxis Anaphylaxis: diagnosis and management Simon G A Brown; Raymond J Mullins; Michael S Gold Medical Journal of Australia; Sep 4, 2006; 185, 5; Health & Medical Complete pg. 283
Pathophysiology n n n Classic Ig. E-mediated reaction Immune complexes or other agents capable of activating the complement cascade C 3 a, C 5 a mast cell and basophils Unknow mechanism Textbook of Pediatric Emergency medicine 3 rd edition P 869 -871
n n Vasodilation Fluid extravasation Smoth muscle constriction Increased mucosal secretions Textbook of Pediatric Emergency medicine 3 rd edition P 869 -871
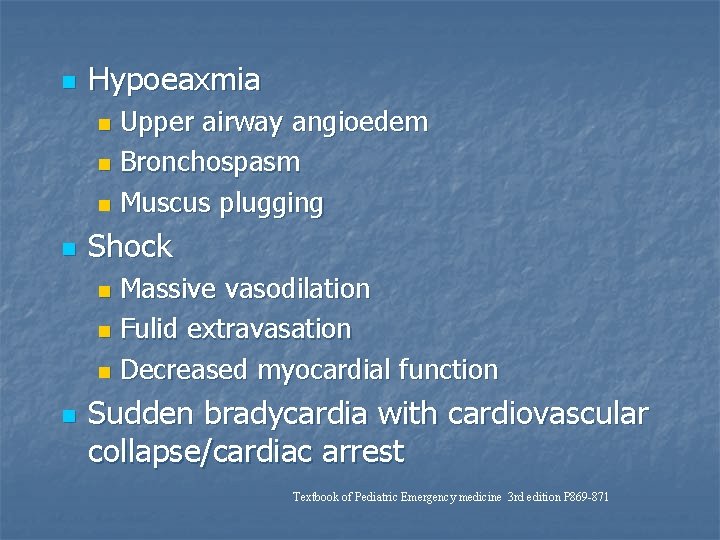
n Hypoeaxmia Upper airway angioedem n Bronchospasm n Muscus plugging n n Shock Massive vasodilation n Fulid extravasation n Decreased myocardial function n n Sudden bradycardia with cardiovascular collapse/cardiac arrest Textbook of Pediatric Emergency medicine 3 rd edition P 869 -871
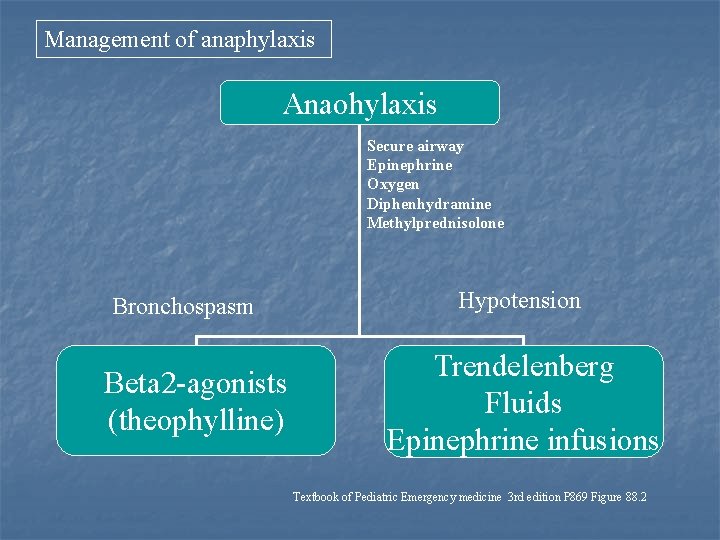
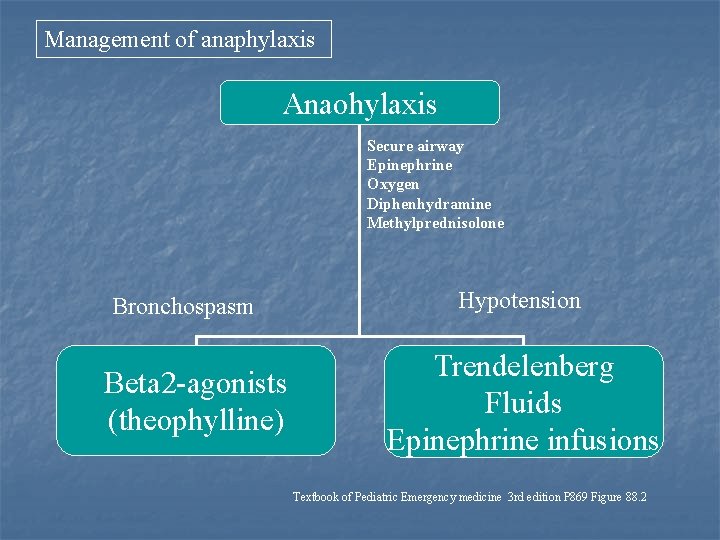
Management of anaphylaxis Anaohylaxis Secure airway Epinephrine Oxygen Diphenhydramine Methylprednisolone Bronchospasm Beta 2 -agonists (theophylline) Hypotension Trendelenberg Fluids Epinephrine infusions Textbook of Pediatric Emergency medicine 3 rd edition P 869 Figure 88. 2
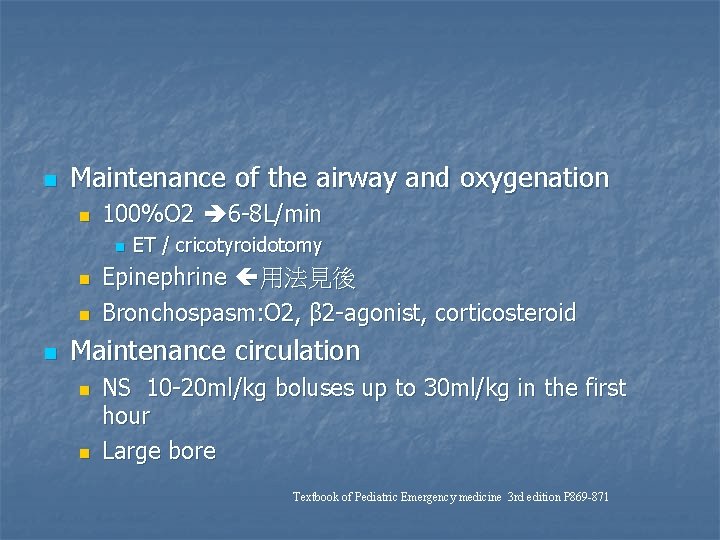
n Maintenance of the airway and oxygenation n 100%O 2 6 -8 L/min n n ET / cricotyroidotomy Epinephrine 用法見後 Bronchospasm: O 2, β 2 -agonist, corticosteroid Maintenance circulation n n NS 10 -20 ml/kg boluses up to 30 ml/kg in the first hour Large bore Textbook of Pediatric Emergency medicine 3 rd edition P 869 -871
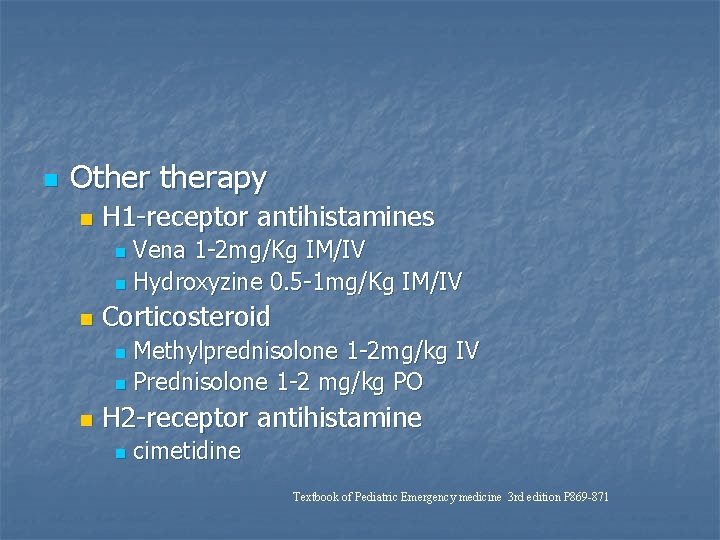
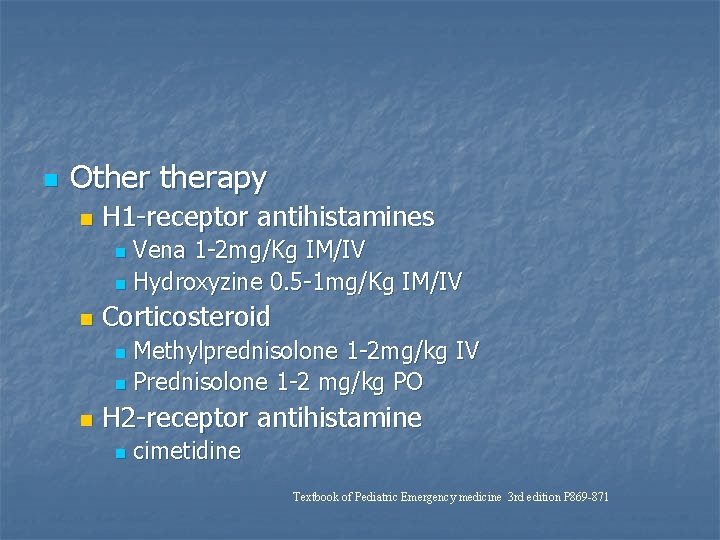
n Otherapy n H 1 -receptor antihistamines Vena 1 -2 mg/Kg IM/IV n Hydroxyzine 0. 5 -1 mg/Kg IM/IV n n Corticosteroid Methylprednisolone 1 -2 mg/kg IV n Prednisolone 1 -2 mg/kg PO n n H 2 -receptor antihistamine n cimetidine Textbook of Pediatric Emergency medicine 3 rd edition P 869 -871
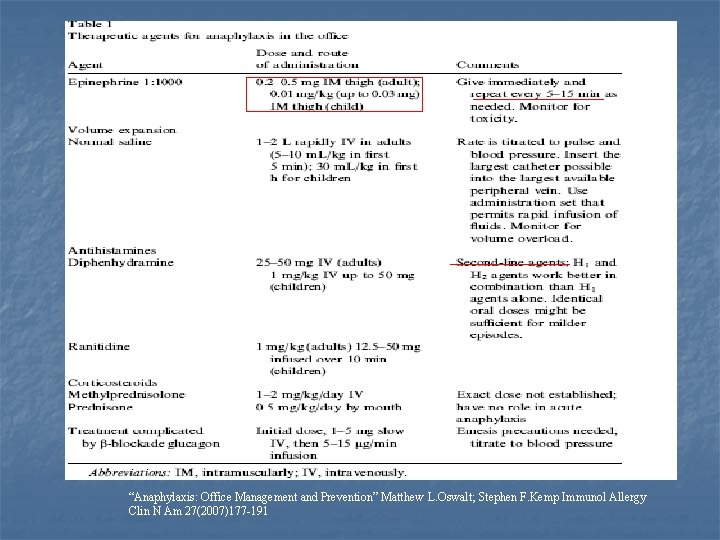
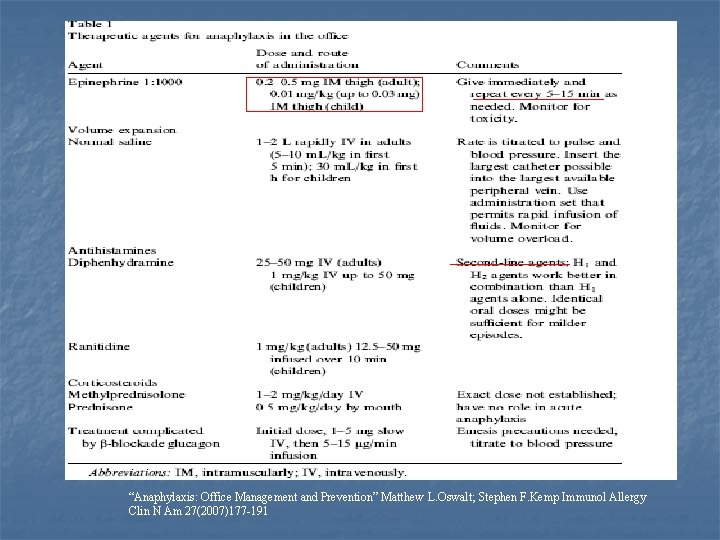
“Anaphylaxis: Office Management and Prevention” Matthew L. Oswalt; Stephen F. Kemp Immunol Allergy Clin N Am 27(2007)177 -191
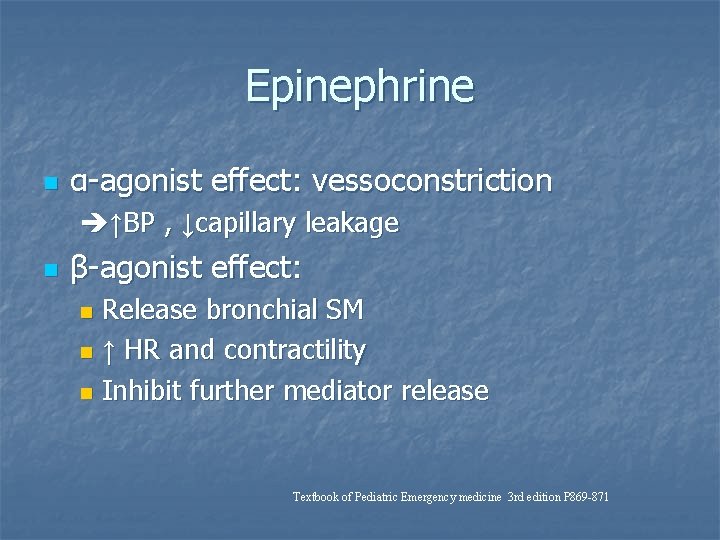
Epinephrine n α-agonist effect: vessoconstriction ↑BP , ↓capillary leakage n β-agonist effect: Release bronchial SM n ↑ HR and contractility n Inhibit further mediator release n Textbook of Pediatric Emergency medicine 3 rd edition P 869 -871


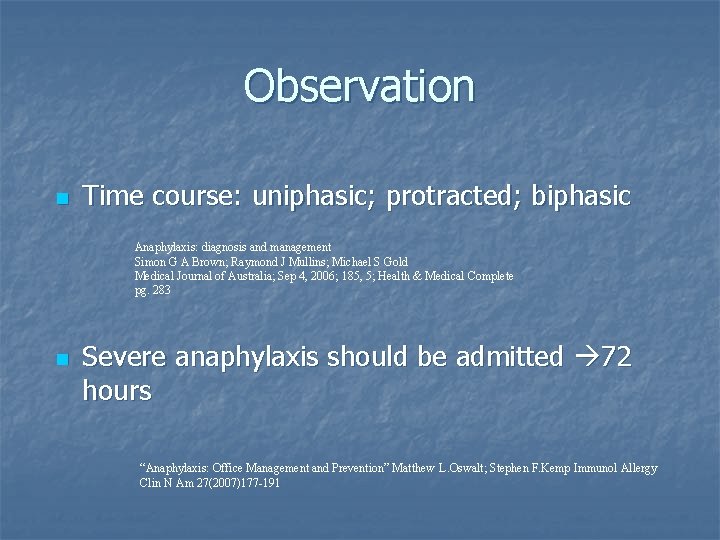
Observation n Time course: uniphasic; protracted; biphasic Anaphylaxis: diagnosis and management Simon G A Brown; Raymond J Mullins; Michael S Gold Medical Journal of Australia; Sep 4, 2006; 185, 5; Health & Medical Complete pg. 283 n Severe anaphylaxis should be admitted 72 hours “Anaphylaxis: Office Management and Prevention” Matthew L. Oswalt; Stephen F. Kemp Immunol Allergy Clin N Am 27(2007)177 -191
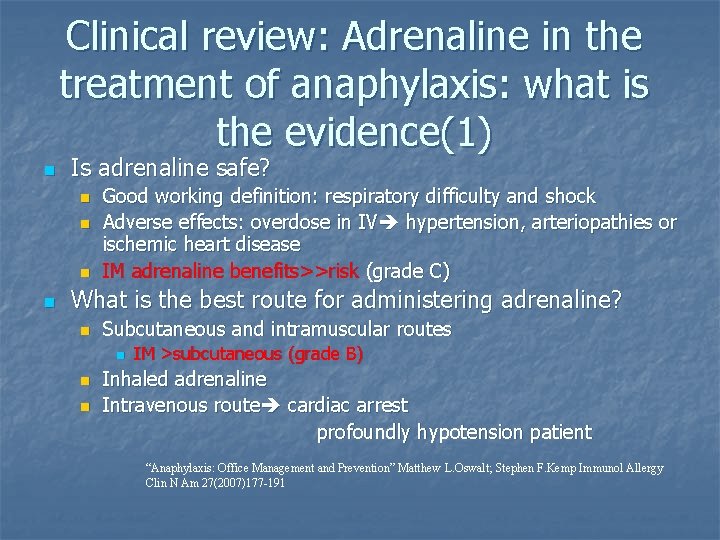
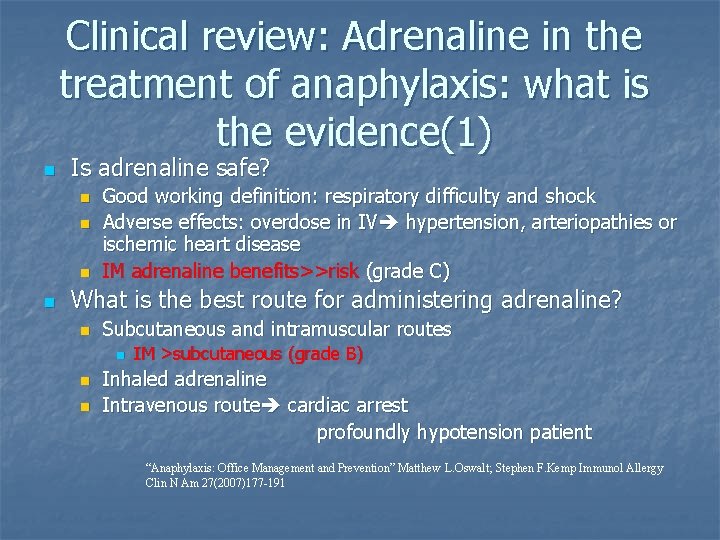
Clinical review: Adrenaline in the treatment of anaphylaxis: what is the evidence(1) n Is adrenaline safe? n n Good working definition: respiratory difficulty and shock Adverse effects: overdose in IV hypertension, arteriopathies or ischemic heart disease IM adrenaline benefits>>risk (grade C) What is the best route for administering adrenaline? n Subcutaneous and intramuscular routes n n n IM >subcutaneous (grade B) Inhaled adrenaline Intravenous route cardiac arrest profoundly hypotension patient “Anaphylaxis: Office Management and Prevention” Matthew L. Oswalt; Stephen F. Kemp Immunol Allergy Clin N Am 27(2007)177 -191
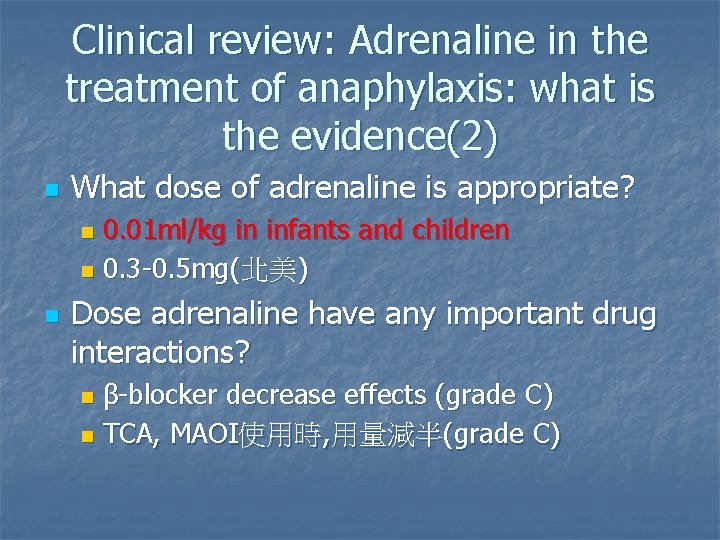
Clinical review: Adrenaline in the treatment of anaphylaxis: what is the evidence(2) n What dose of adrenaline is appropriate? 0. 01 ml/kg in infants and children n 0. 3 -0. 5 mg(北美) n n Dose adrenaline have any important drug interactions? β-blocker decrease effects (grade C) n TCA, MAOI使用時, 用量減半(grade C) n
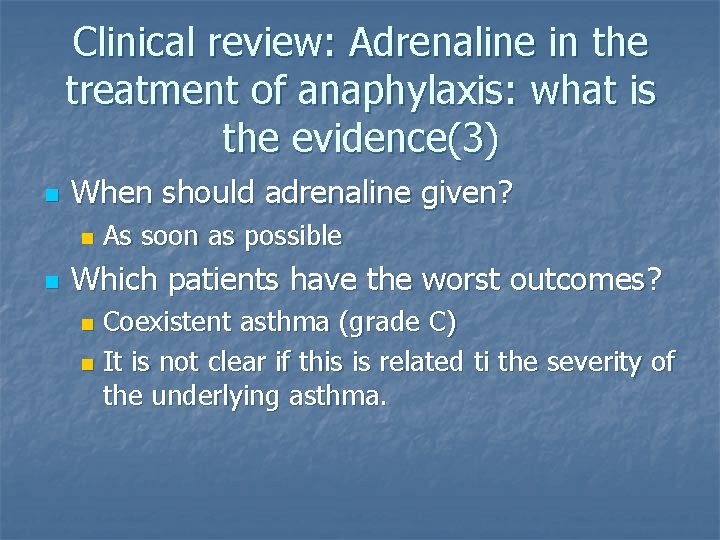
Clinical review: Adrenaline in the treatment of anaphylaxis: what is the evidence(3) n When should adrenaline given? n n As soon as possible Which patients have the worst outcomes? Coexistent asthma (grade C) n It is not clear if this is related ti the severity of the underlying asthma. n
So, what should I do more in the first visit?
n n n See patient’s mucosa Position Monitor TPR more frequently
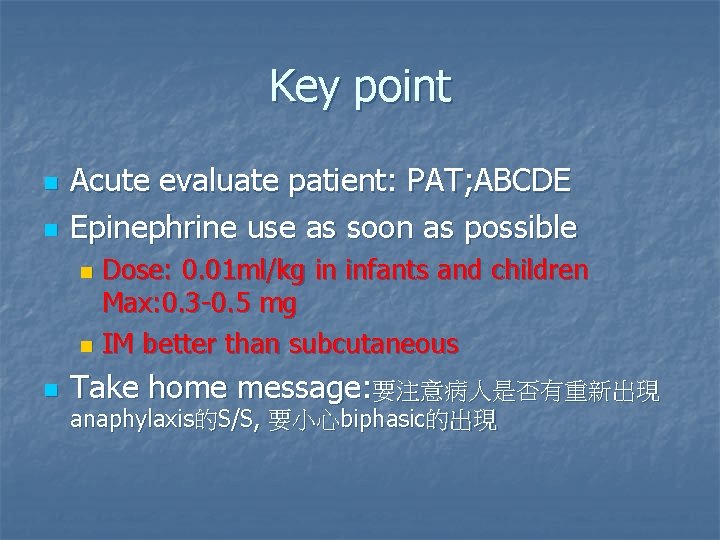
Key point n n Acute evaluate patient: PAT; ABCDE Epinephrine use as soon as possible Dose: 0. 01 ml/kg in infants and children Max: 0. 3 -0. 5 mg n IM better than subcutaneous n n Take home message: 要注意病人是否有重新出現 anaphylaxis的S/S, 要小心biphasic的出現
Thanks you