Anaphylaxis A Lifethreatening Emergency Anaphylaxis A serious allergic













- Slides: 48

Anaphylaxis A Life-threatening Emergency 朱士傑 風濕免疫過敏科
Anaphylaxis ¢ A serious allergic reaction that is rapid in onset and may cause death
Anaphylactoid Reaction ¢ Ig. E-independent ¢ Clincially indistingushable from anaphylaxis ¢ 不建議使用
Anaphylaxis ¢ Incidence ¦ increasing (youngest, food) ¦ 21 – 49. 8 per 100, 000 personyears ( person-years) ¦Under diagnosis, under-reporting, a variety of definition
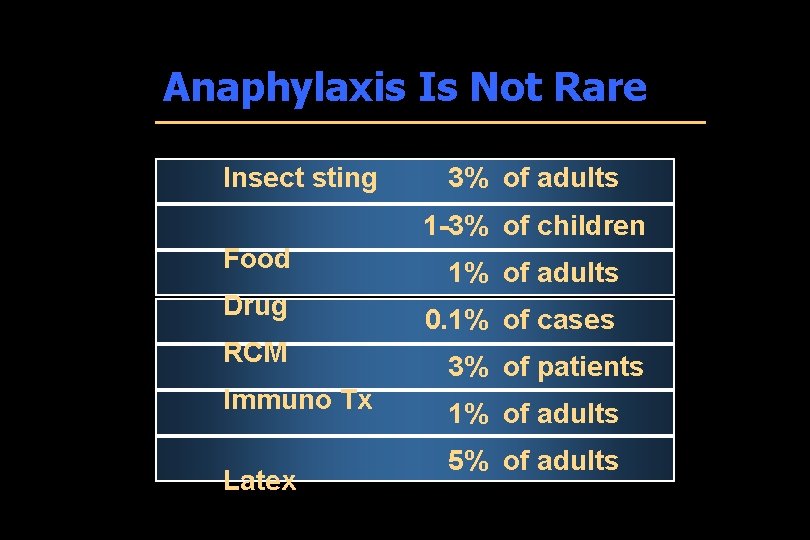
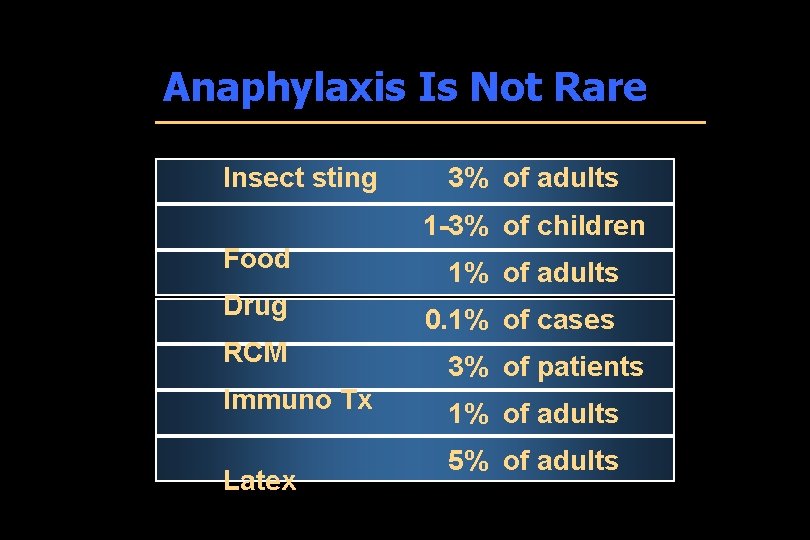
Anaphylaxis Is Not Rare Insect sting 3% of adults 1 -3% of children Food 1% of adults Drug 0. 1% of cases RCM 3% of patients Immuno Tx 1% of adults Latex 5% of adults
Mechanisms of Anaphylaxis n Type I hypersensitivity reaction n Allergen exposure n Production of allergen-specific Ig. E n Ig. E-sensitized mast cells and basophils n Ig. E-mediated degranulation upon reexposure to allergen
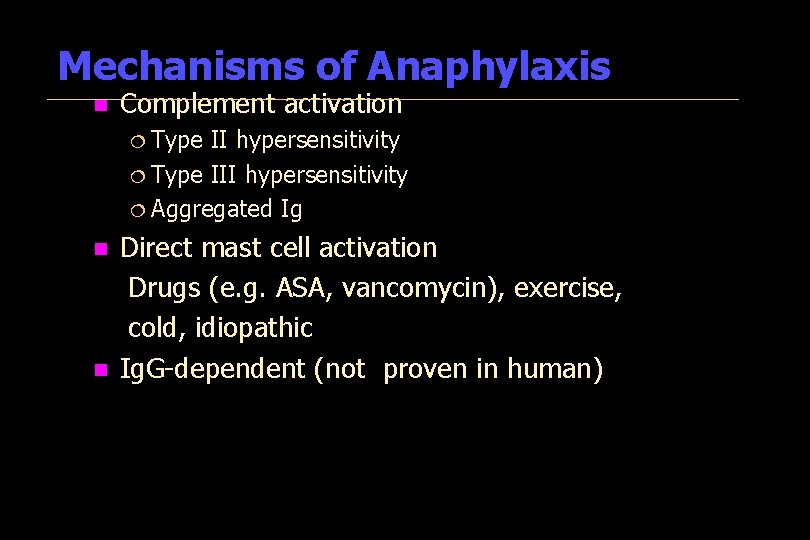
Mechanisms of Anaphylaxis n Complement activation ¦ Type II hypersensitivity ¦ Type III hypersensitivity ¦ Aggregated Ig Direct mast cell activation Drugs (e. g. ASA, vancomycin), exercise, cold, idiopathic n Ig. G-dependent (not proven in human) n
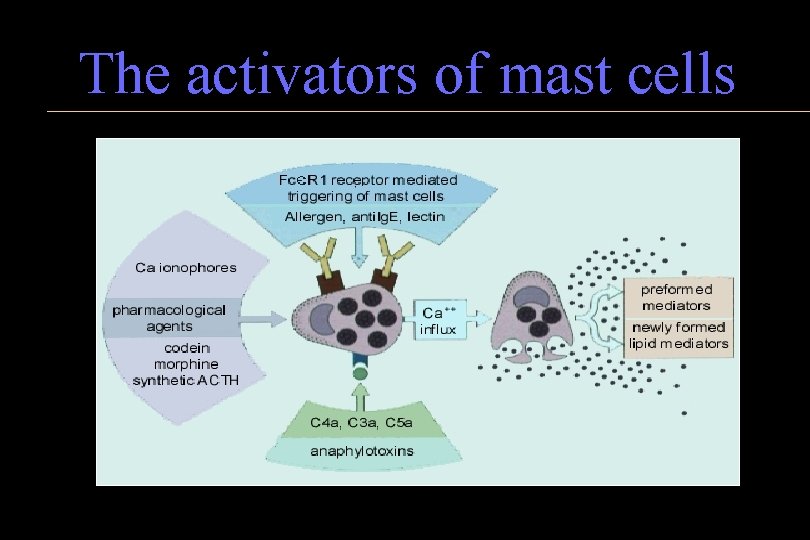
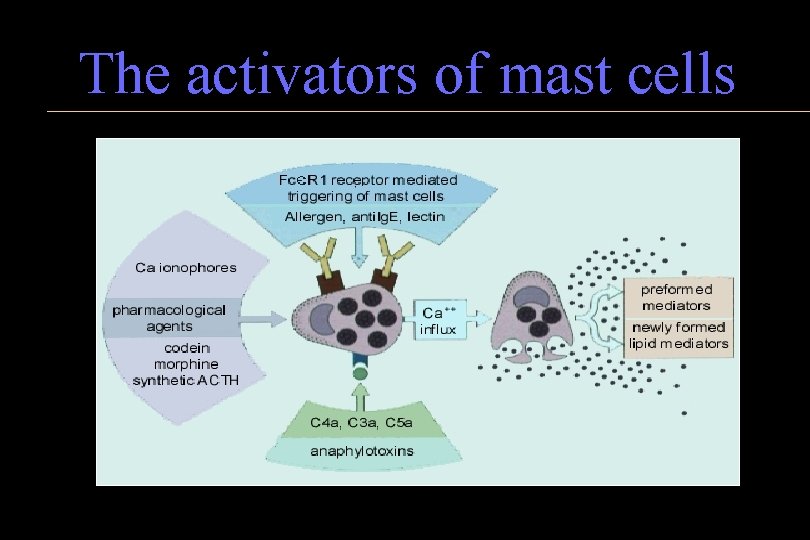
The activators of mast cells

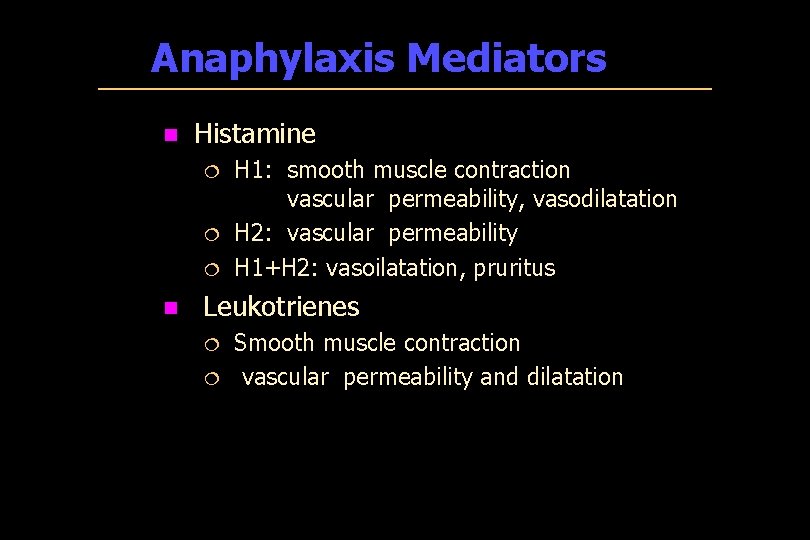
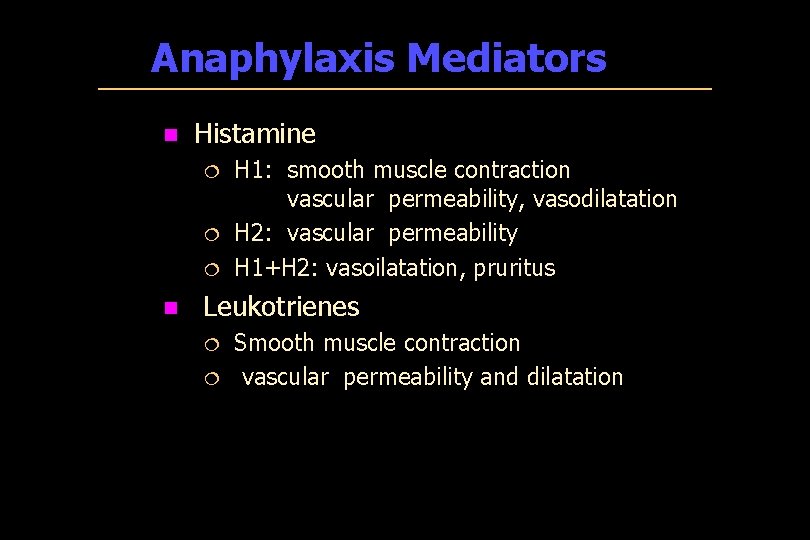
Anaphylaxis Mediators n Histamine ¦ ¦ ¦ n H 1: smooth muscle contraction vascular permeability, vasodilatation H 2: vascular permeability H 1+H 2: vasoilatation, pruritus Leukotrienes ¦ ¦ Smooth muscle contraction vascular permeability and dilatation
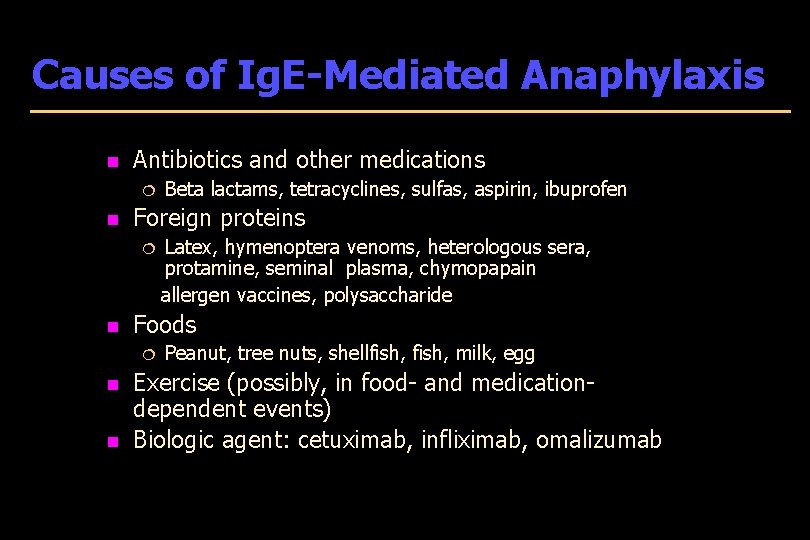
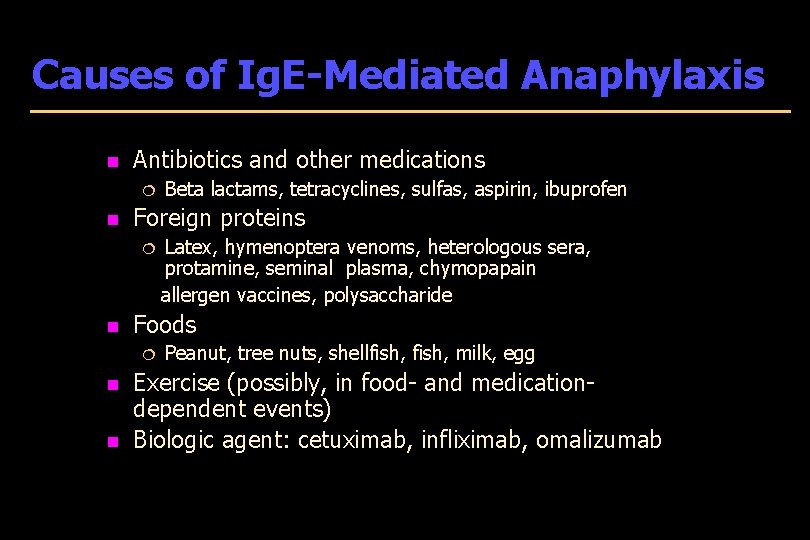
Causes of Ig. E-Mediated Anaphylaxis n Antibiotics and other medications ¦ n Beta lactams, tetracyclines, sulfas, aspirin, ibuprofen Foreign proteins Latex, hymenoptera venoms, heterologous sera, protamine, seminal plasma, chymopapain allergen vaccines, polysaccharide ¦ n Foods ¦ n n Peanut, tree nuts, shellfish, milk, egg Exercise (possibly, in food- and medicationdependent events) Biologic agent: cetuximab, infliximab, omalizumab
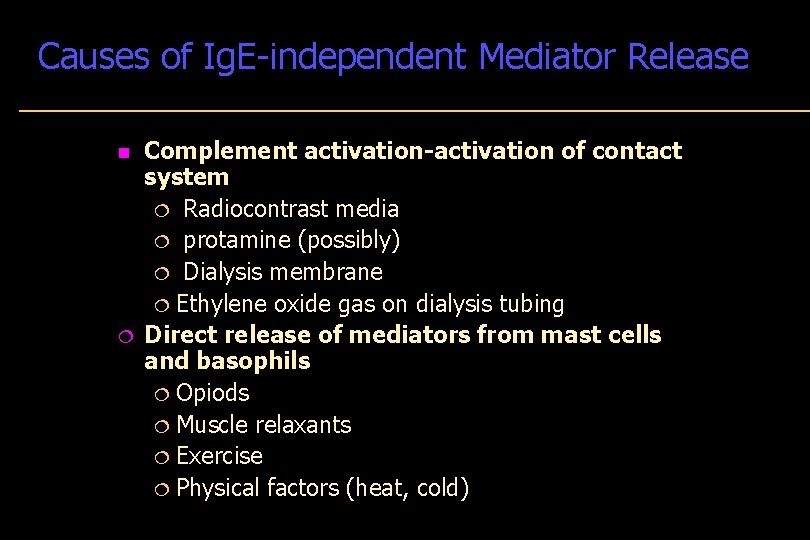
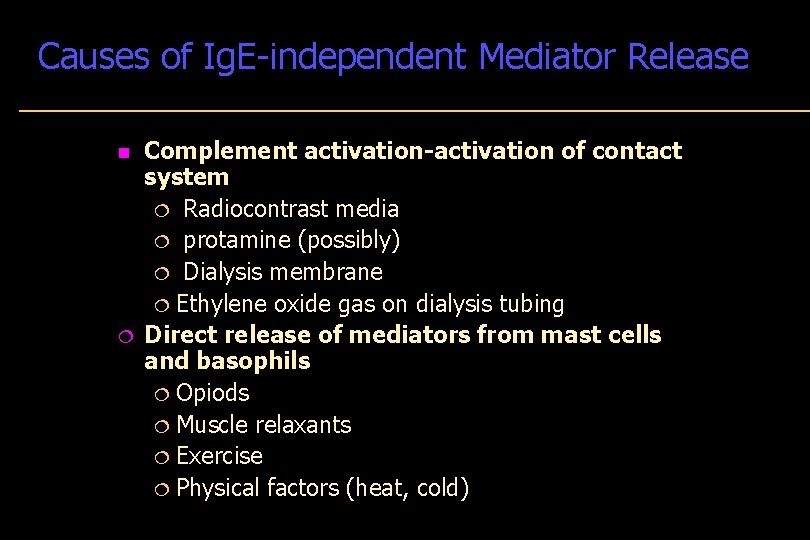
Causes of Ig. E-independent Mediator Release n ¦ Complement activation-activation of contact system ¦ Radiocontrast media ¦ protamine (possibly) ¦ Dialysis membrane ¦ Ethylene oxide gas on dialysis tubing Direct release of mediators from mast cells and basophils ¦ Opiods ¦ Muscle relaxants ¦ Exercise ¦ Physical factors (heat, cold)
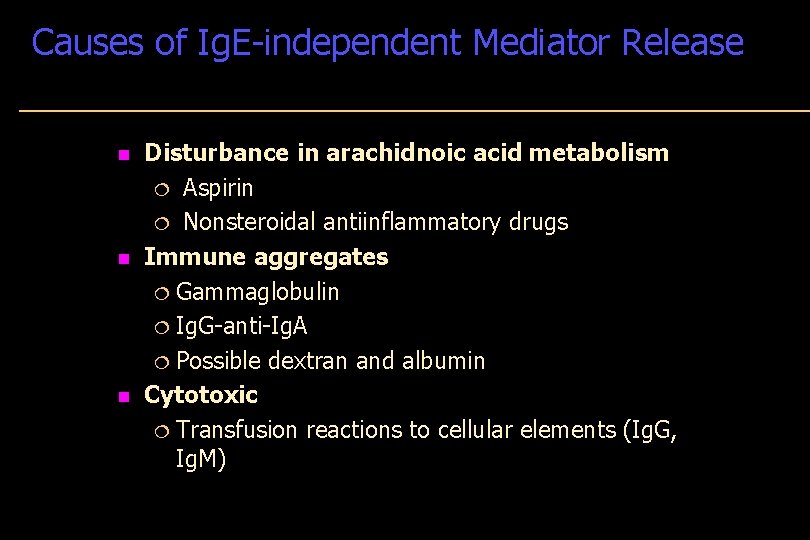
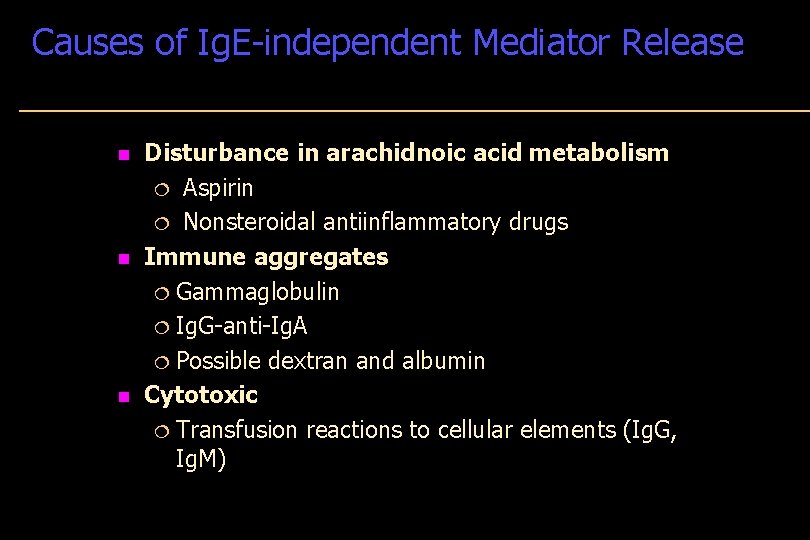
Causes of Ig. E-independent Mediator Release n n n Disturbance in arachidnoic acid metabolism ¦ Aspirin ¦ Nonsteroidal antiinflammatory drugs Immune aggregates ¦ Gammaglobulin ¦ Ig. G-anti-Ig. A ¦ Possible dextran and albumin Cytotoxic ¦ Transfusion reactions to cellular elements (Ig. G, Ig. M)
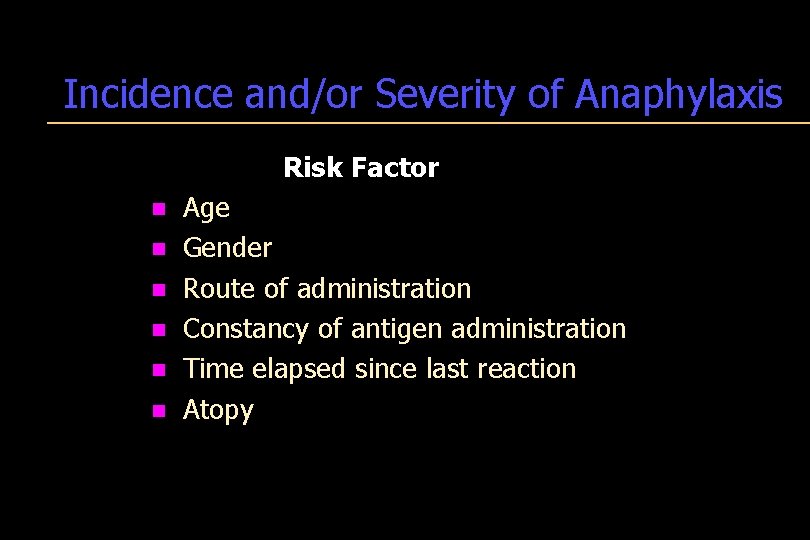
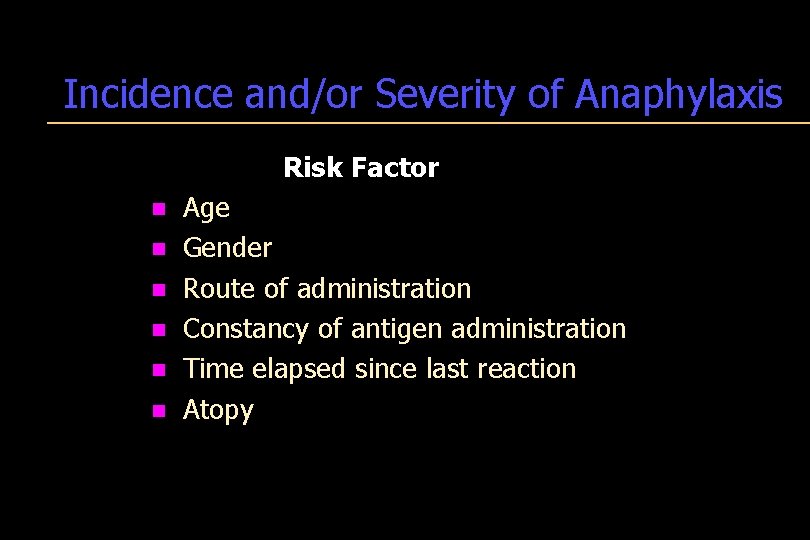
Incidence and/or Severity of Anaphylaxis Risk Factor n Age n Gender n Route of administration n Constancy of antigen administration n Time elapsed since last reaction n Atopy
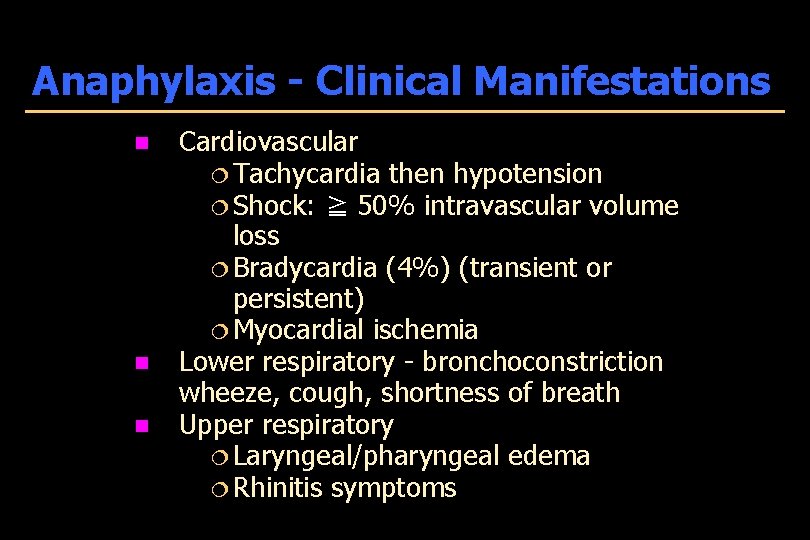
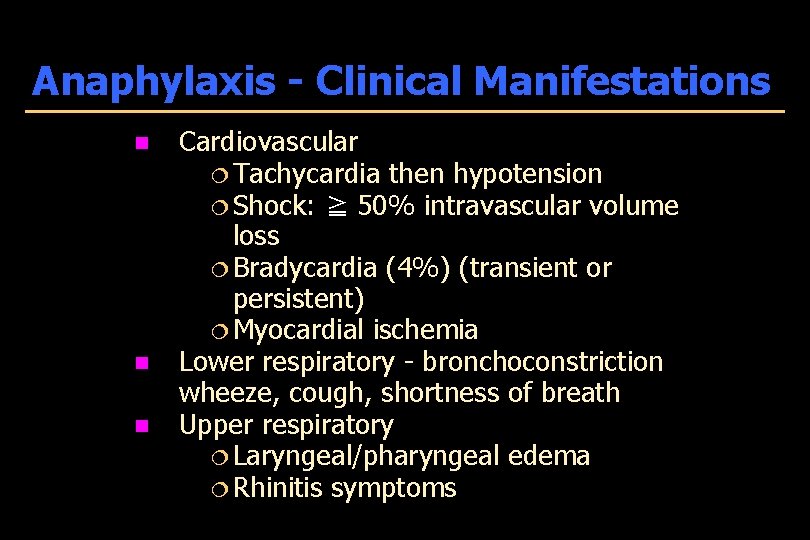
Anaphylaxis - Clinical Manifestations n n n Cardiovascular ¦ Tachycardia then hypotension ¦ Shock: ≧ 50% intravascular volume loss ¦ Bradycardia (4%) (transient or persistent) ¦ Myocardial ischemia Lower respiratory - bronchoconstriction wheeze, cough, shortness of breath Upper respiratory ¦ Laryngeal/pharyngeal edema ¦ Rhinitis symptoms
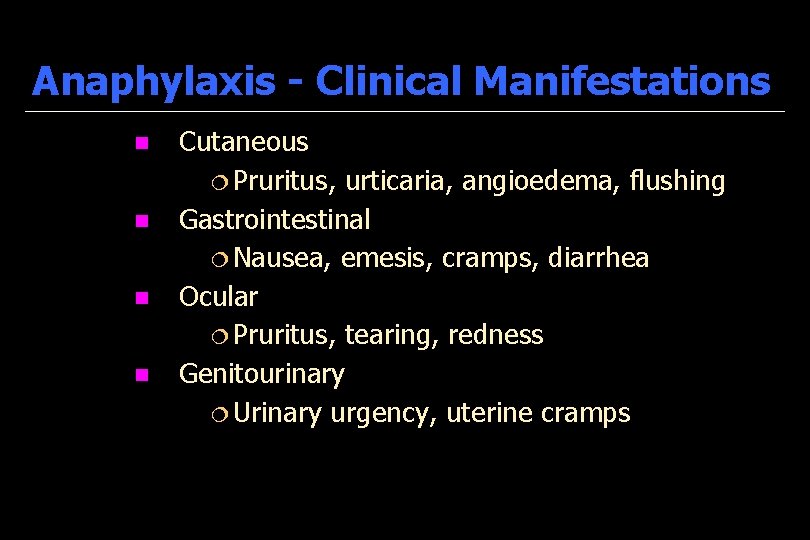
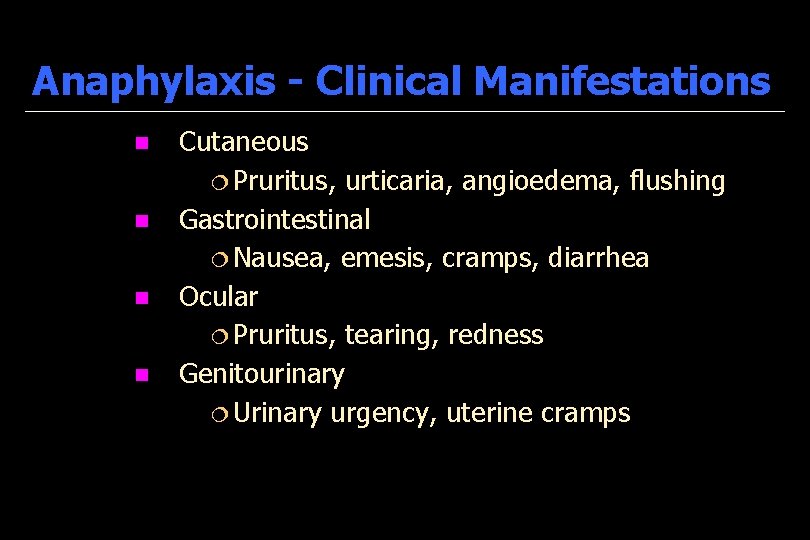
Anaphylaxis - Clinical Manifestations n n Cutaneous ¦ Pruritus, urticaria, angioedema, flushing Gastrointestinal ¦ Nausea, emesis, cramps, diarrhea Ocular ¦ Pruritus, tearing, redness Genitourinary ¦ Urinary urgency, uterine cramps

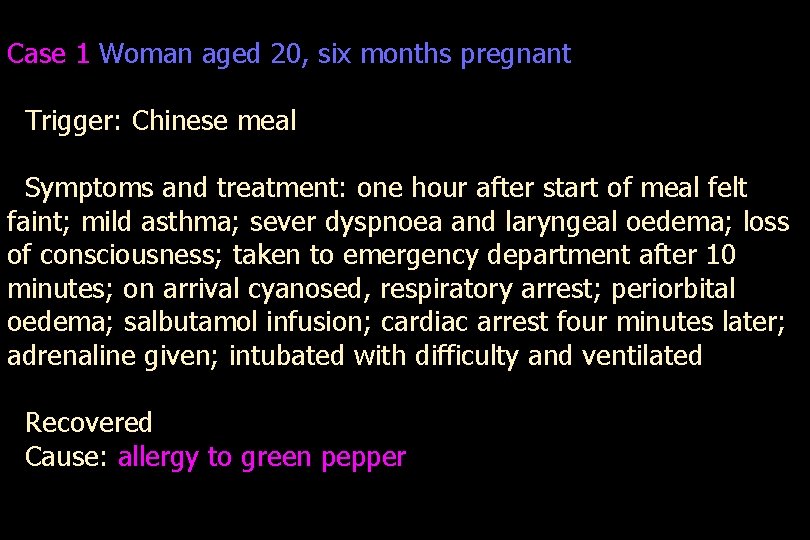
Case 1 Woman aged 20, six months pregnant Trigger: Chinese meal Symptoms and treatment: one hour after start of meal felt faint; mild asthma; sever dyspnoea and laryngeal oedema; loss of consciousness; taken to emergency department after 10 minutes; on arrival cyanosed, respiratory arrest; periorbital oedema; salbutamol infusion; cardiac arrest four minutes later; adrenaline given; intubated with difficulty and ventilated Recovered Cause: allergy to green pepper
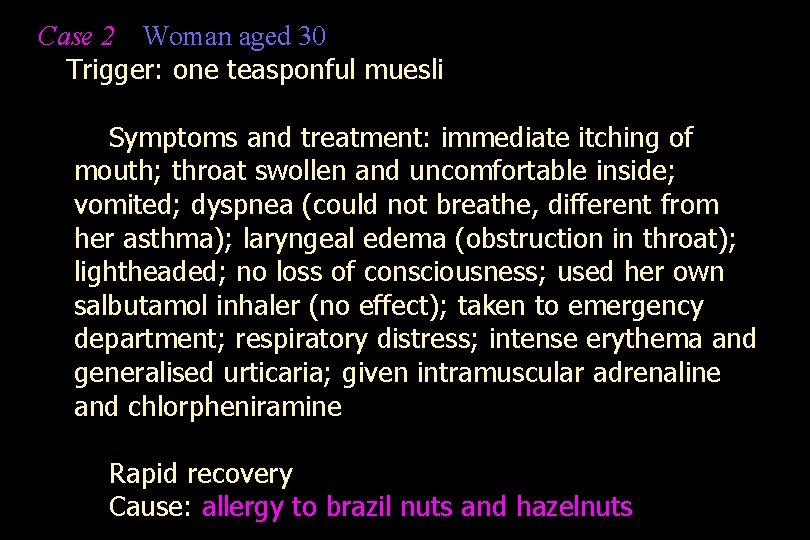
Case 2 Woman aged 30 Trigger: one teasponful muesli Symptoms and treatment: immediate itching of mouth; throat swollen and uncomfortable inside; vomited; dyspnea (could not breathe, different from her asthma); laryngeal edema (obstruction in throat); lightheaded; no loss of consciousness; used her own salbutamol inhaler (no effect); taken to emergency department; respiratory distress; intense erythema and generalised urticaria; given intramuscular adrenaline and chlorpheniramine Rapid recovery Cause: allergy to brazil nuts and hazelnuts
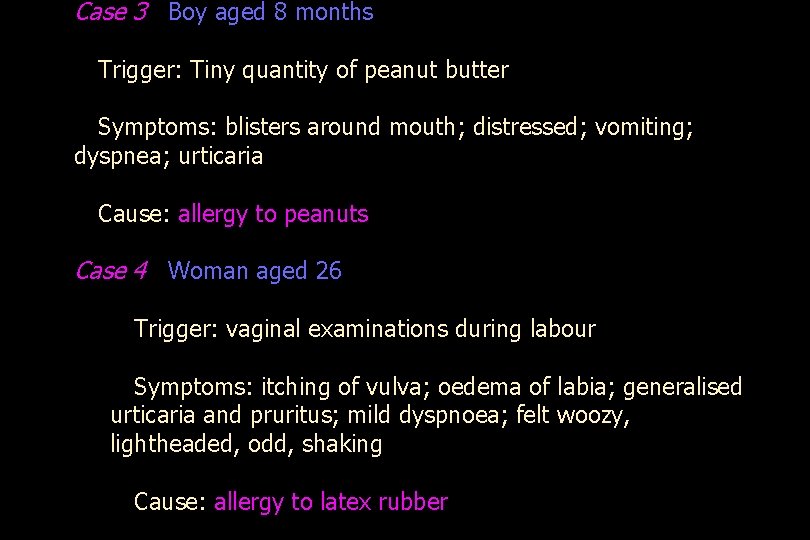
Case 3 Boy aged 8 months Trigger: Tiny quantity of peanut butter Symptoms: blisters around mouth; distressed; vomiting; dyspnea; urticaria Cause: allergy to peanuts Case 4 Woman aged 26 Trigger: vaginal examinations during labour Symptoms: itching of vulva; oedema of labia; generalised urticaria and pruritus; mild dyspnoea; felt woozy, lightheaded, odd, shaking Cause: allergy to latex rubber

Anaphylaxis -Temporal Pattern n Uniphasic Biphasic (3%-20%) ¦Same manifestations as at presentation recur up to 8 hours later Protracted ¦Up to 32 hours ¦May not be prevented by glucocorticoids
Food-Related Anaphylaxis n. Frequency: ~ 150 deaths / year n The most common single cause of anaphylaxis in ED in USA. (young) n. Risk: Underlying asthma Delayed epinephrine Symptom denial Previous severe reaction n. History: known allergic food n. Key foods: peanut/ nuts / shellfish n. Biphasic reaction n. Lack of cutaneous symptoms n. Schools, no predictive markers n. Exercise
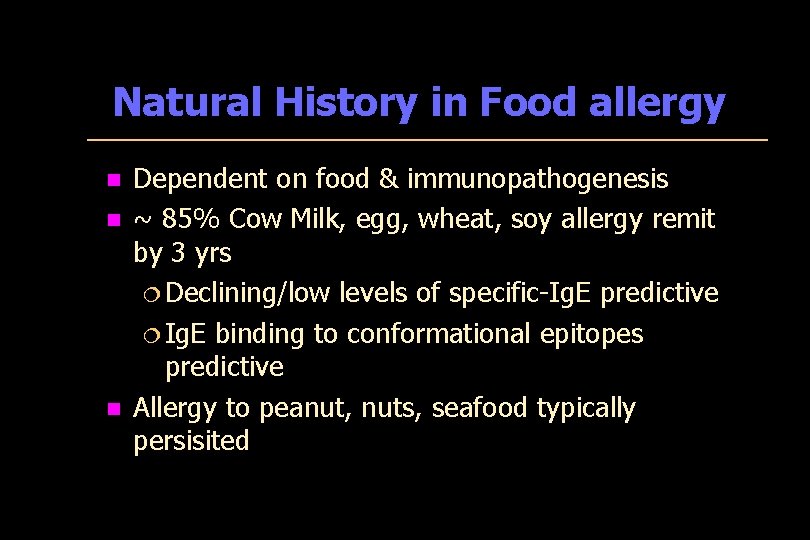
Natural History in Food allergy n n n Dependent on food & immunopathogenesis ~ 85% Cow Milk, egg, wheat, soy allergy remit by 3 yrs ¦ Declining/low levels of specific-Ig. E predictive ¦ Ig. E binding to conformational epitopes predictive Allergy to peanut, nuts, seafood typically persisited
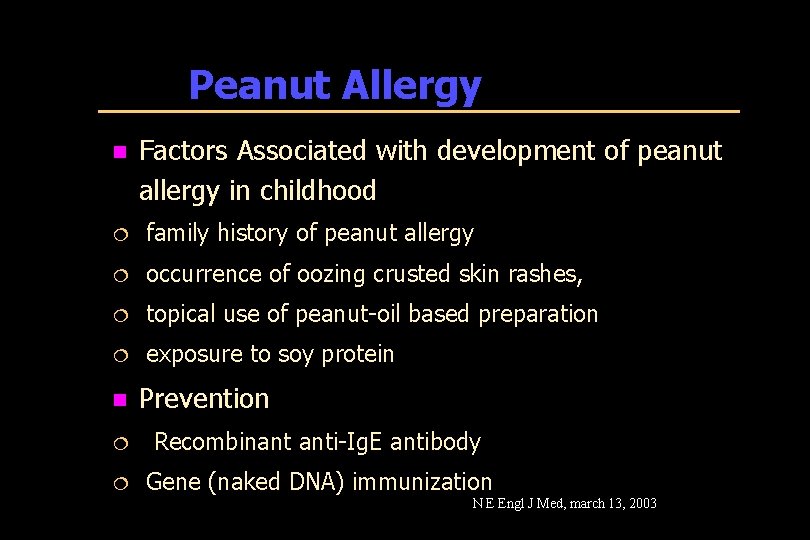
Peanut Allergy n Factors Associated with development of peanut allergy in childhood ¦ family history of peanut allergy ¦ occurrence of oozing crusted skin rashes, ¦ topical use of peanut-oil based preparation ¦ exposure to soy protein n Prevention ¦ Recombinant anti-Ig. E antibody ¦ Gene (naked DNA) immunization N E Engl J Med, march 13, 2003
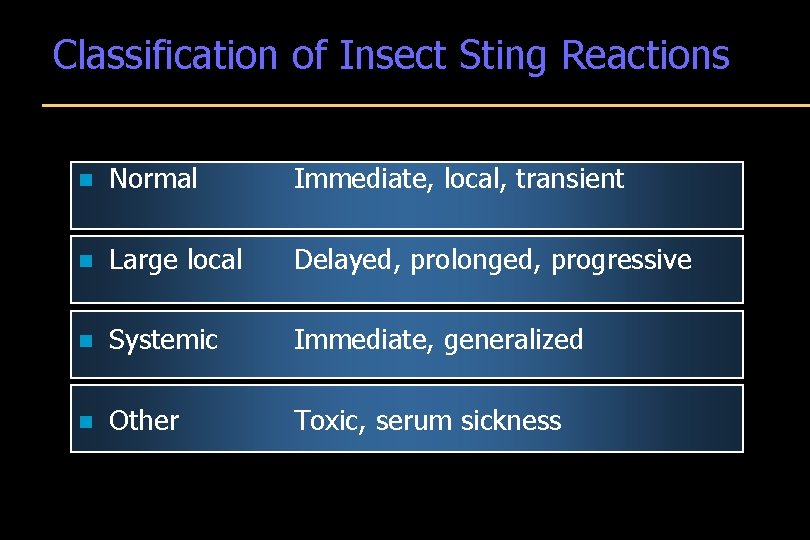
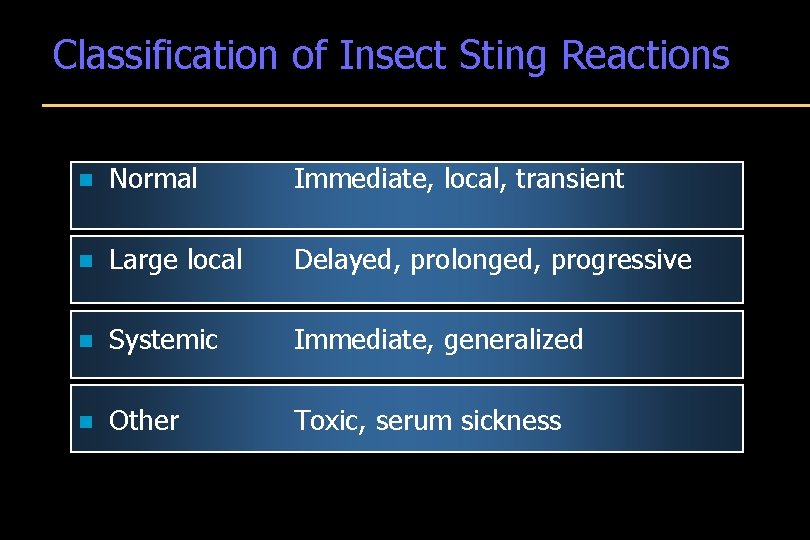
Classification of Insect Sting Reactions n Normal Immediate, local, transient n Large local Delayed, prolonged, progressive n Systemic Immediate, generalized n Other Toxic, serum sickness
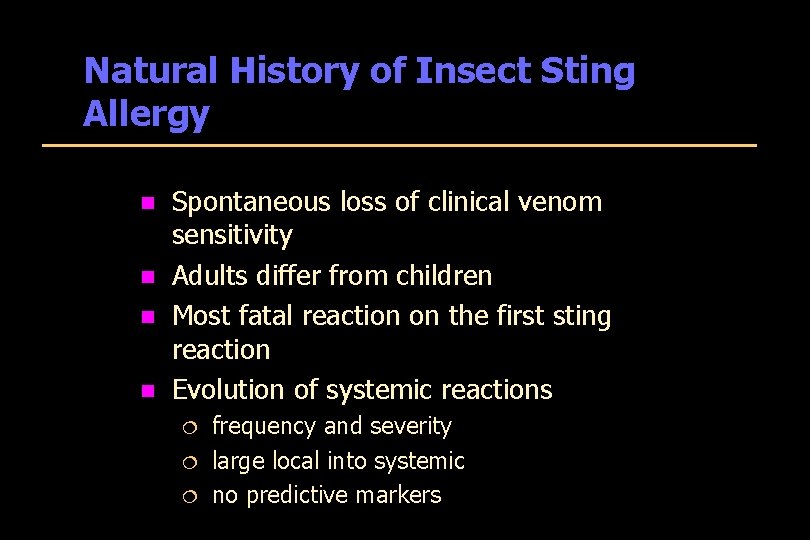
Natural History of Insect Sting Allergy n n Spontaneous loss of clinical venom sensitivity Adults differ from children Most fatal reaction on the first sting reaction Evolution of systemic reactions ¦ ¦ ¦ frequency and severity large local into systemic no predictive markers
Insect sting and bites Anaphylaxis Indications for Venom Immunotherapy 98% efficacy n Medical criteria ¦ ¦ n history of systemic reaction positive venom skin test Non-medical considerations ¦ ¦ age of patient alterations in life style co-existing diseases costs
Allergen Immunotherapy - Systemic Reactions n n n 10 -15% during initial immunotherapy, 1 -3% during maintenance Most in < 20 minutes, but severity worse with later onset Systemic reactions not preceded or predicted by large local reactions Not correlated with asthma in all studies Related to: dose/vial errors, unstable asthma, seasonal flare, extreme sensitivity, ß blockers, new vial / new extract, rush schedule Fatal reactions: 58 observed over 25 years: ¦ ¦ ¦ 90% in < 30 minutes 50% delayed use of epinephrine 25% prior systemic reactions – 30% due to errors – 50% with acute asthma – 25% peak pollen season
Anaphylaxis Exercise-Induced Syndrome n n n Prodrome - flushing, pruritus, fatigue Early - urticaria, angioedema Established - stridor, GI symptoms, collapse Late - headache Precipitating Events: isometric and isotonic exercise; hot environment, foods, medications Temporally unpredictable

Anaphylaxis Exercise-Induced Syndrome Treatment / Prevention Avoidance of exercise, especially in heat n Avoidance of allergenic foods before exercise n Buddy system-epinephrine n

Latex Allergy
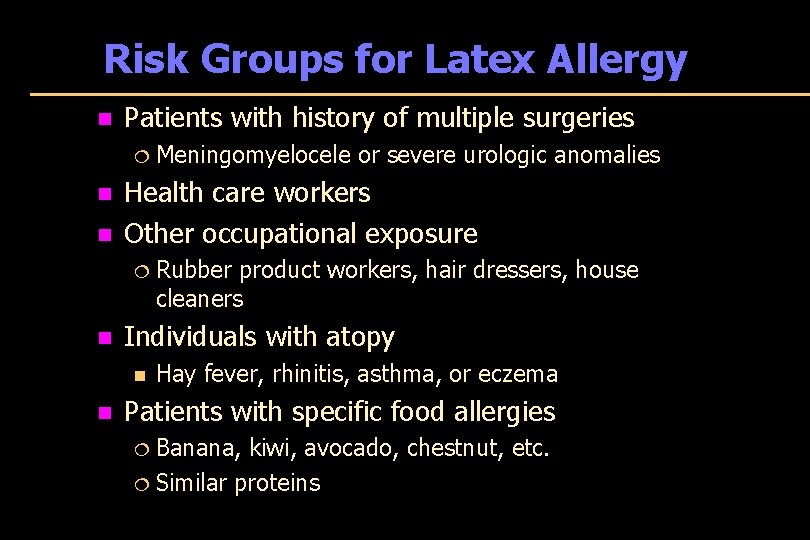
Risk Groups for Latex Allergy n Patients with history of multiple surgeries ¦ Meningomyelocele or severe urologic anomalies n n Health care workers Other occupational exposure ¦ Rubber product workers, hair dressers, house cleaners n Individuals with atopy n n Hay fever, rhinitis, asthma, or eczema Patients with specific food allergies ¦ Banana, kiwi, avocado, chestnut, etc. ¦ Similar proteins
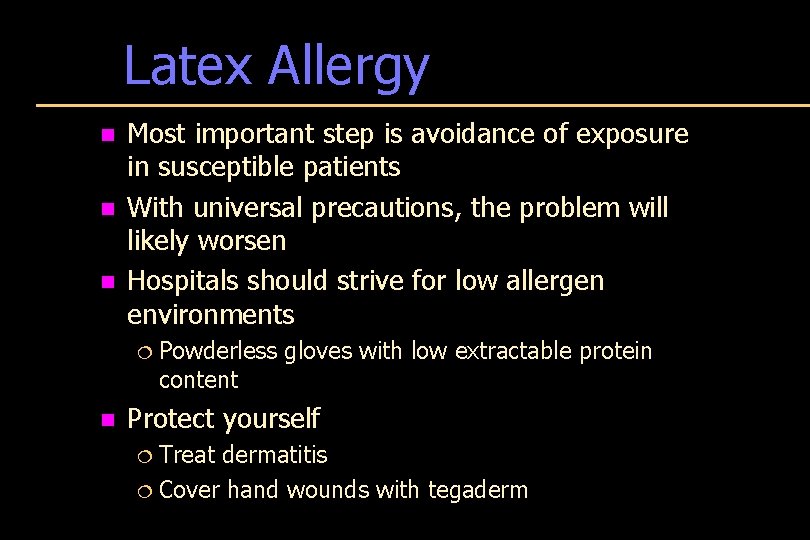
Latex Allergy n n n Most important step is avoidance of exposure in susceptible patients With universal precautions, the problem will likely worsen Hospitals should strive for low allergen environments ¦ Powderless gloves with low extractable protein content n Protect yourself ¦ Treat dermatitis ¦ Cover hand wounds with tegaderm
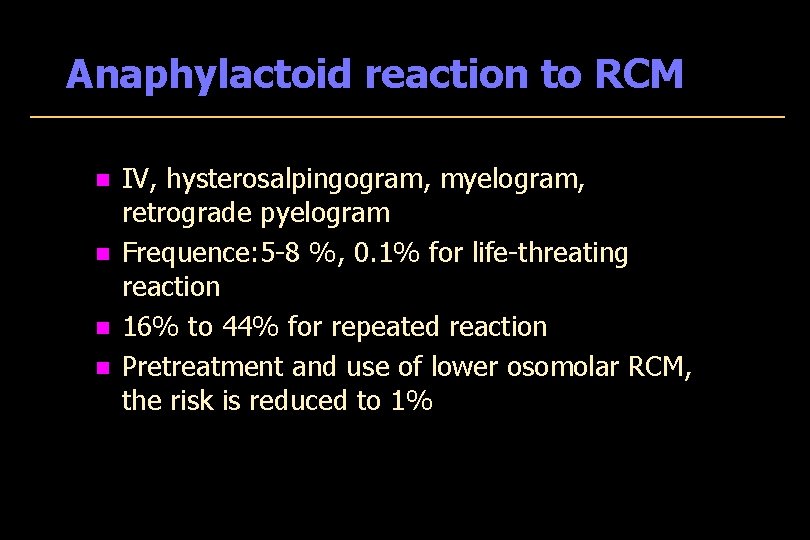
Anaphylactoid reaction to RCM n n IV, hysterosalpingogram, myelogram, retrograde pyelogram Frequence: 5 -8 %, 0. 1% for life-threating reaction 16% to 44% for repeated reaction Pretreatment and use of lower osomolar RCM, the risk is reduced to 1%
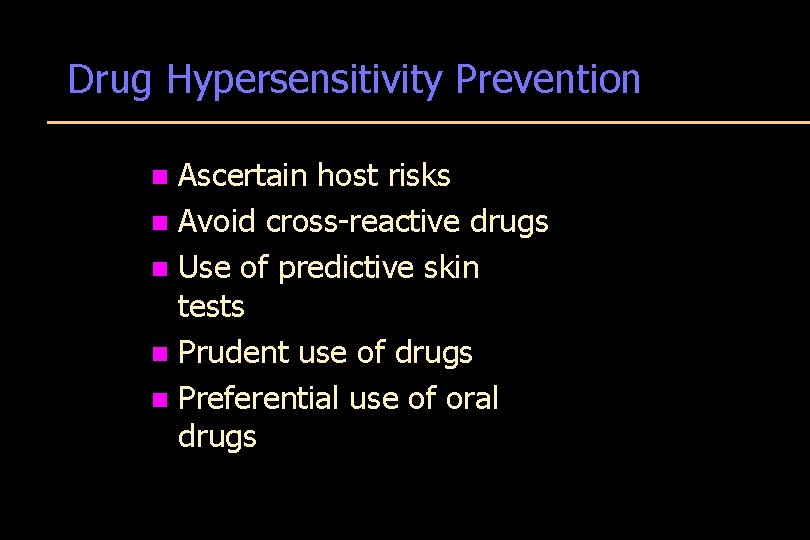
Drug Hypersensitivity Prevention Ascertain host risks n Avoid cross-reactive drugs n Use of predictive skin tests n Prudent use of drugs n Preferential use of oral drugs n

Anaphylaxis Fatalities ≈ 4% n Increased Risk ¦beta blockade, ACE inhibitors, severe hypotension, bradycardia, sustained bronchospasm, poor response to epinephrine ¦Adrenal Insufficiency ¦Asthma ¦Coronary Artery Disease n
Anaphylaxis Fatalities Post Mortem Findings n n n Airway (laryngeal) and tissue (visceral) edema Pulmonary hyperinflation Tissue eosinophilia Elevated serum tryptase Myocardial injury

Anaphylaxis Diagnosis Clinical Features n Histamine n Serum Tryptase measurable up to 6 hours n
Prevention of Anaphylaxis n History: drug, venom, food, latex reactions ¦ n n n Avoidance, Medic-Alert and ID card Penicillin skin tests & desensitization Administer drugs orally rather than parenterally when possible Hymenoptera avoidance & immunotherapy Iodinated Dye Pretreatment Avoid ¦ ¦ ¦ ß blockade in those on immunotherapy or at risk of Hymenoptera anaphylaxis Immunotherapy in those on ß blockers ACE inhibitors in food / Hymenoptera anaphylaxis

Management n n ABC’s, early airway intervention as needed Early administration of epinephrine n 0. 01 mg/kg - 0. 3 - 0. 5 mg, IM. Maximum dose, 0. 5 mg. n IV – 5 -10 μg (0. 2 μg/kg) for hypotension) 0. 1 - 0. 5 mg in cardiovascular collapse Remove allergen (stingers), or apply tourniquet if exposure site on extremity 2 large bore IV lines : n Volume resuscitate with crystalloid or colloid solutions
Management continued n n Glucagon 1 -5 mg IV (if epinephrine contraindicated or ineffective) (activate adenylate cyclase) Anti-histamines: ¦ ¦ n n n Benadryl 50 mg iv Pepcid 20 mg iv; Ranitidine 50 mg iv Corticosteroids (Hydrocortisone, prednisone, Methylprednisolone) Vasopressors: dopamine, levarterenol, vasopressin Ongoing evaluation of airway / vital signs
Anaphylaxis Treatment n Corticosteroids ¦ Not effective in protracted anaphylaxis ¦ Effective in iodinated dye prophylaxis ¦ The efficacy in anaphylaxis not established n Prolonged resuscitation

Risk Management for Anaphylaxis n Ask the questions n Prescribe epinephrine injector n Refer to allergy specialist

Epi. Pen® auto-injector


 Allergic fungal sinusitis treatment
Allergic fungal sinusitis treatment Rhinitis medicamentosa
Rhinitis medicamentosa Chronic allergies icd 10
Chronic allergies icd 10 Aria management
Aria management Aria classification of allergic rhinitis
Aria classification of allergic rhinitis Allergic crease adalah
Allergic crease adalah Types of allergic reactions
Types of allergic reactions Allergic crease
Allergic crease Black mucus
Black mucus Allergic crease adalah
Allergic crease adalah Catarahh
Catarahh Homeopathy for allergic rhinitis: a systematic review
Homeopathy for allergic rhinitis: a systematic review Irritant contact dermatitis vs allergic contact dermatitis
Irritant contact dermatitis vs allergic contact dermatitis Allergic granulomatous angiitis
Allergic granulomatous angiitis Blood transfusion complications
Blood transfusion complications Wolowitz allergic reaction
Wolowitz allergic reaction Management of allergic rhinitis
Management of allergic rhinitis Management of allergic rhinitis
Management of allergic rhinitis Nap 6 recommendations
Nap 6 recommendations Hypersensitivity types examples
Hypersensitivity types examples Anaphylaxis onset
Anaphylaxis onset Anaphylaxis ig
Anaphylaxis ig Interprofessional care for anaphylaxis
Interprofessional care for anaphylaxis Causes of anaphylactic reaction
Causes of anaphylactic reaction Anaphylaxis treatment
Anaphylaxis treatment Brighton collaboration
Brighton collaboration Dose of epinephrine in anaphylaxis
Dose of epinephrine in anaphylaxis Anaphylaxis photos
Anaphylaxis photos Anaphylaxis
Anaphylaxis Reaction
Reaction Angioedema anaphylaxis
Angioedema anaphylaxis Biphasic anaphylaxis
Biphasic anaphylaxis Epiglotitis
Epiglotitis Nap 6 summary
Nap 6 summary Latex allergy
Latex allergy Anaphylaxis photos
Anaphylaxis photos Allergist delta dental
Allergist delta dental Serious tone
Serious tone Sardina
Sardina Serious injury and fatality prevention
Serious injury and fatality prevention Serious game lego
Serious game lego The only serious philosophical question
The only serious philosophical question In a recent car accident tamiko
In a recent car accident tamiko Quick comparative and superlative
Quick comparative and superlative Challenge 1 astd
Challenge 1 astd Comparative superlative forms
Comparative superlative forms Tidy comparative and superlative form
Tidy comparative and superlative form Serious adverse event reconciliation
Serious adverse event reconciliation Substantial risk of serious prejudice
Substantial risk of serious prejudice