Pathophysiology of respiration Mgr Barbora Konen Ph D
Pathophysiology of respiration Mgr. Barbora Konečná, Ph. D.
Respiration system • Brings O and eliminates CO • Keeps p. H of an organism 2 2 • 4 steps of respiration: 1. Ventilation – exchange of gases between lungs and background 2. Outside breathing – exchange of gases between alveoli and blood 3. Transport – towards or away from tissues (by cardiovascular system) 4. Inner breathing – echange of gases between blood and tissue
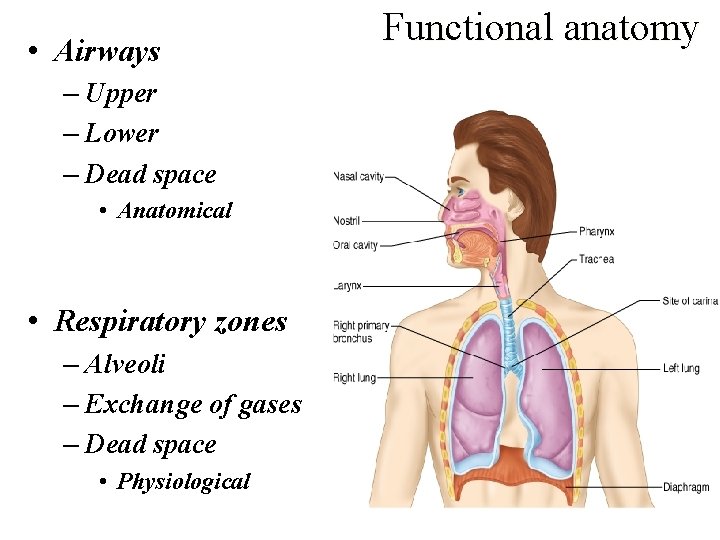
• Airways – Upper – Lower – Dead space • Anatomical • Respiratory zones – Alveoli – Exchange of gases – Dead space • Physiological Functional anatomy
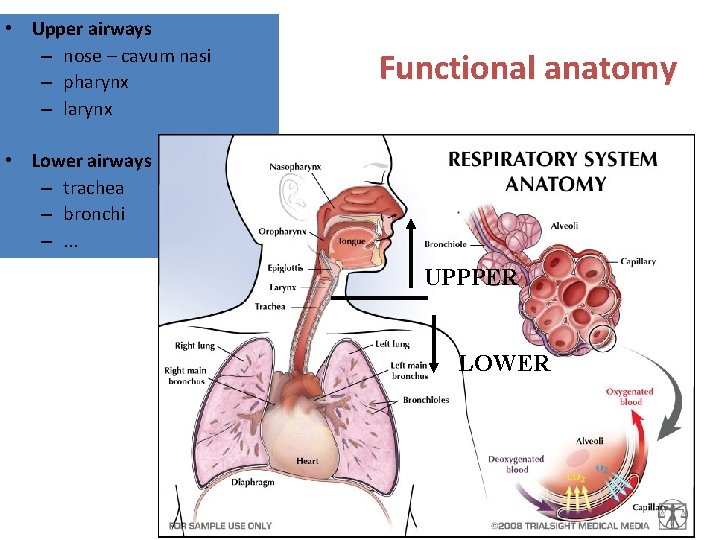
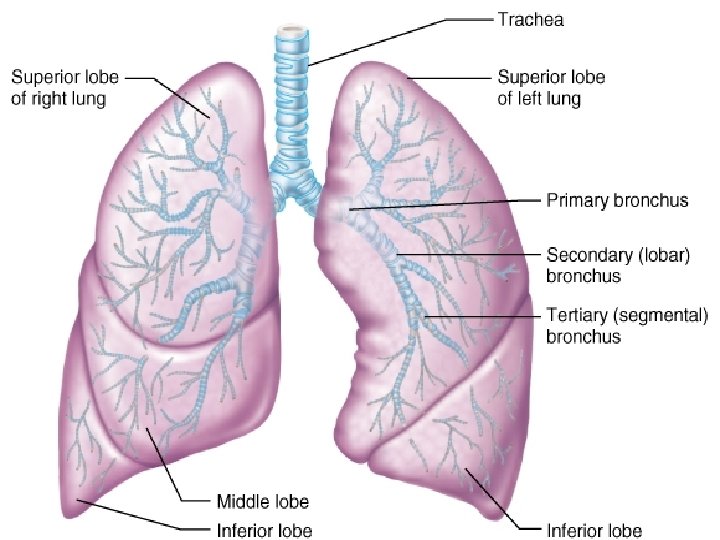
• Upper airways – nose – cavum nasi – pharynx – larynx Functional anatomy • Lower airways – trachea – bronchi –. . . UPPPER LOWER
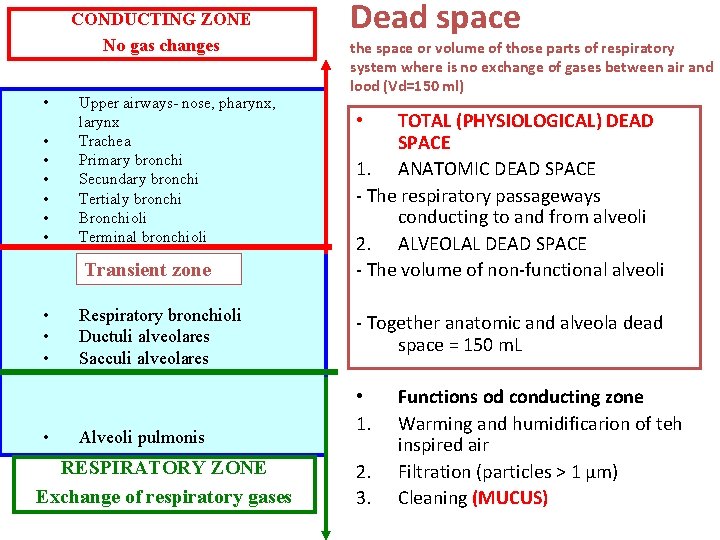
CONDUCTING ZONE No gas changes • • Upper airways- nose, pharynx, larynx Trachea Primary bronchi Secundary bronchi Tertialy bronchi Bronchioli Terminal bronchioli Transient zone • • Respiratory bronchioli Ductuli alveolares Sacculi alveolares Alveoli pulmonis RESPIRATORY ZONE Exchange of respiratory gases Dead space the space or volume of those parts of respiratory system where is no exchange of gases between air and lood (Vd=150 ml) TOTAL (PHYSIOLOGICAL) DEAD SPACE 1. ANATOMIC DEAD SPACE - The respiratory passageways conducting to and from alveoli 2. ALVEOLAL DEAD SPACE - The volume of non-functional alveoli • - Together anatomic and alveola dead space = 150 m. L • 1. 2. 3. Functions od conducting zone Warming and humidificarion of teh inspired air Filtration (particles > 1 µm) Cleaning (MUCUS)
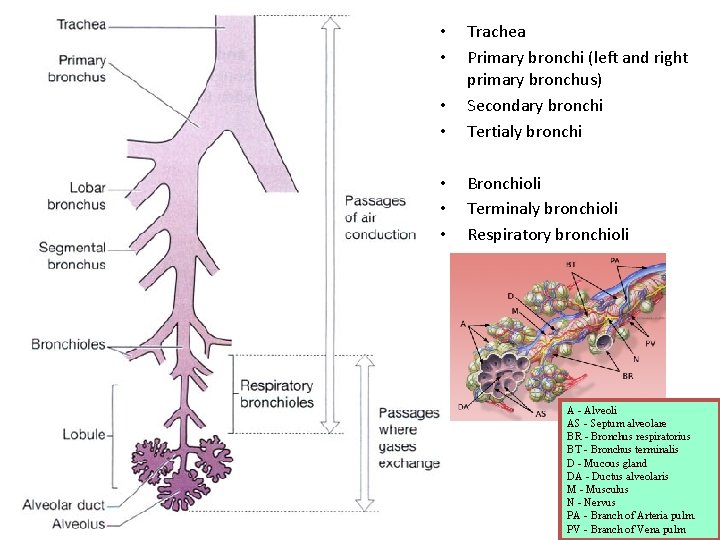
• • Trachea Primary bronchi (left and right primary bronchus) Secondary bronchi Tertialy bronchi • • • Bronchioli Terminaly bronchioli Respiratory bronchioli • • A - Alveoli AS - Septum alveolare BR - Bronchus respiratorius BT - Bronchus terminalis D - Mucous gland DA - Ductus alveolaris M - Musculus N - Nervus PA - Branch of Arteria pulm. PV - Branch of Vena pulm
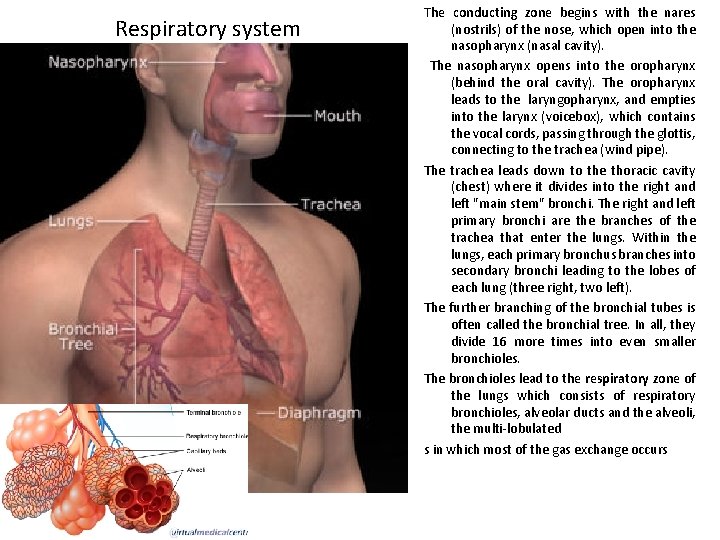
Respiratory system The conducting zone begins with the nares (nostrils) of the nose, which open into the nasopharynx (nasal cavity). The nasopharynx opens into the oropharynx (behind the oral cavity). The oropharynx leads to the laryngopharynx, and empties into the larynx (voicebox), which contains the vocal cords, passing through the glottis, connecting to the trachea (wind pipe). The trachea leads down to the thoracic cavity (chest) where it divides into the right and left "main stem" bronchi. The right and left primary bronchi are the branches of the trachea that enter the lungs. Within the lungs, each primary bronchus branches into secondary bronchi leading to the lobes of each lung (three right, two left). The further branching of the bronchial tubes is often called the bronchial tree. In all, they divide 16 more times into even smaller bronchioles. The bronchioles lead to the respiratory zone of the lungs which consists of respiratory bronchioles, alveolar ducts and the alveoli, the multi-lobulated s in which most of the gas exchange occurs
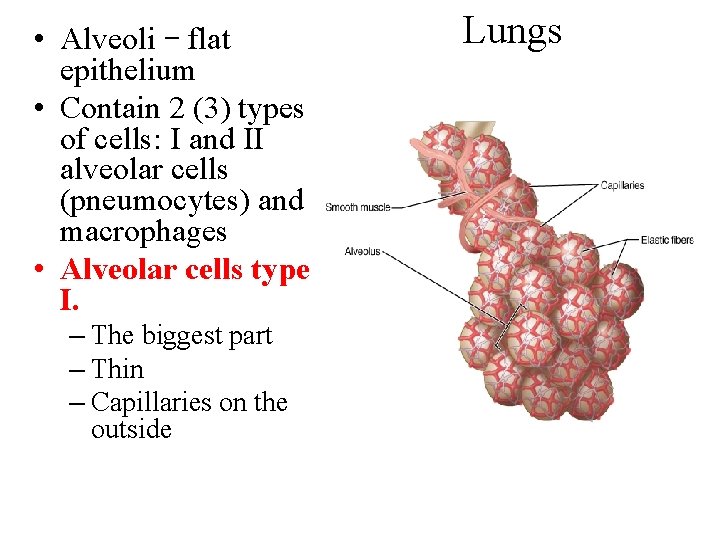
• Alveoli – flat epithelium • Contain 2 (3) types of cells: I and II alveolar cells (pneumocytes) and macrophages • Alveolar cells type I. – The biggest part – Thin – Capillaries on the outside Lungs
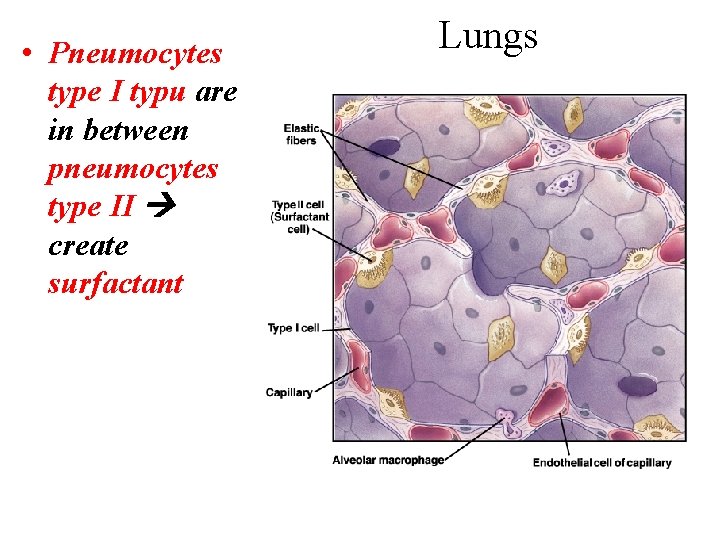
• Pneumocytes type I typu are in between pneumocytes type II create surfactant Lungs
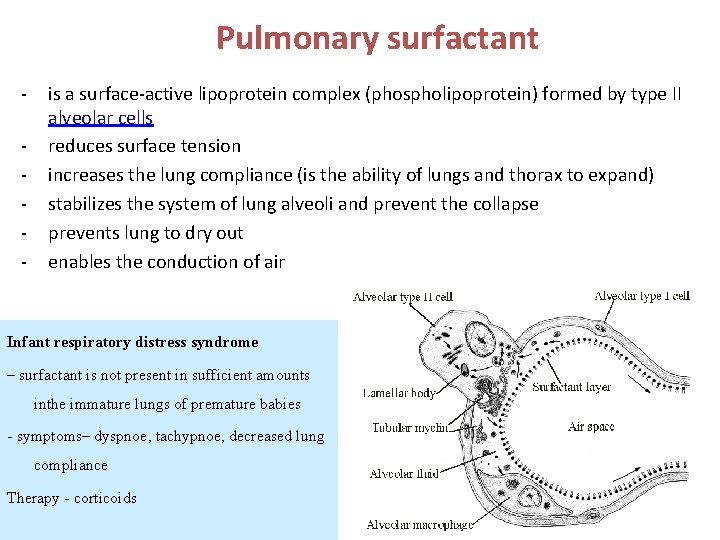
Pulmonary surfactant - is a surface-active lipoprotein complex (phospholipoprotein) formed by type II alveolar cells reduces surface tension increases the lung compliance (is the ability of lungs and thorax to expand) stabilizes the system of lung alveoli and prevent the collapse prevents lung to dry out enables the conduction of air Infant respiratory distress syndrome – surfactant is not present in sufficient amounts inthe immature lungs of premature babies - symptoms– dyspnoe, tachypnoe, decreased lung compliance Therapy - corticoids
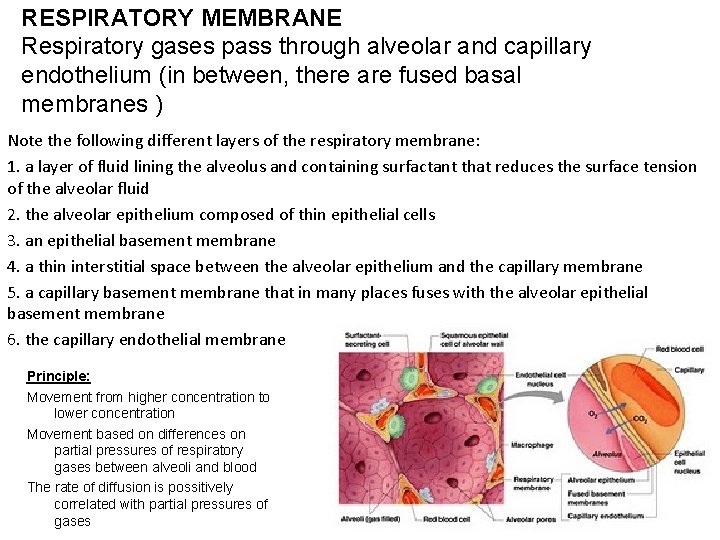
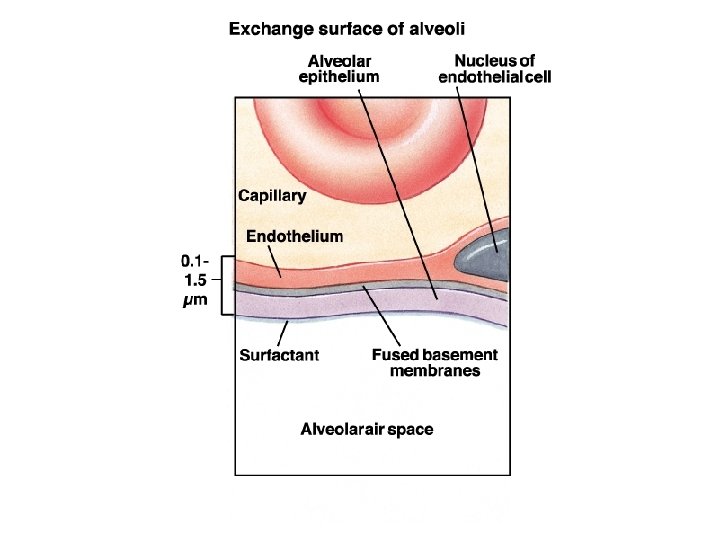
RESPIRATORY MEMBRANE Respiratory gases pass through alveolar and capillary endothelium (in between, there are fused basal membranes ) Note the following different layers of the respiratory membrane: 1. a layer of fluid lining the alveolus and containing surfactant that reduces the surface tension of the alveolar fluid 2. the alveolar epithelium composed of thin epithelial cells 3. an epithelial basement membrane 4. a thin interstitial space between the alveolar epithelium and the capillary membrane 5. a capillary basement membrane that in many places fuses with the alveolar epithelial basement membrane 6. the capillary endothelial membrane Principle: Movement from higher concentration to lower concentration Movement based on differences on partial pressures of respiratory gases between alveoli and blood The rate of diffusion is possitively correlated with partial pressures of gases
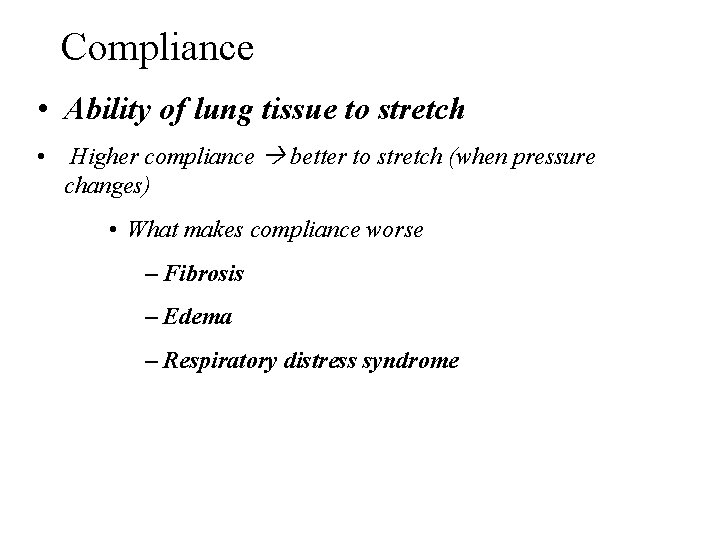
Compliance • Ability of lung tissue to stretch • Higher compliance better to stretch (when pressure changes) • What makes compliance worse – Fibrosis – Edema – Respiratory distress syndrome
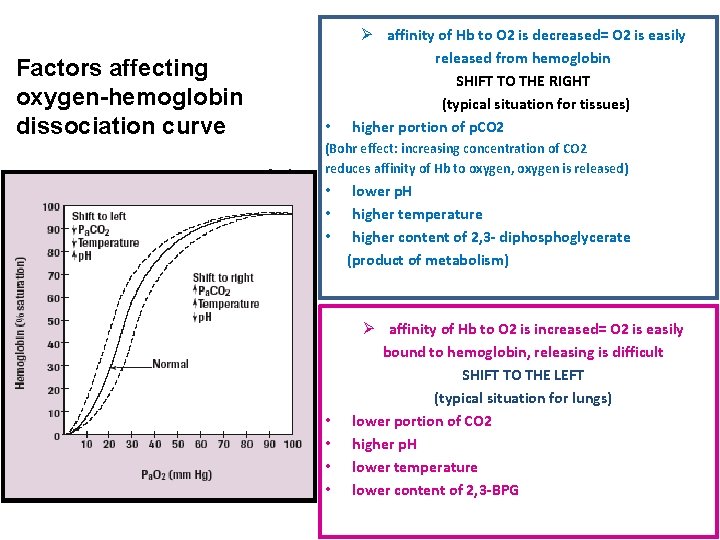
Factors affecting oxygen-hemoglobin dissociation curve • Ø affinity of Hb to O 2 is decreased= O 2 is easily released from hemoglobin SHIFT TO THE RIGHT (typical situation for tissues) higher portion of p. CO 2 (Bohr effect: increasing concentration of CO 2 reduces affinity of Hb to oxygen, oxygen is released) • • lower p. H higher temperature higher content of 2, 3 - diphosphoglycerate (product of metabolism) Ø affinity of Hb to O 2 is increased= O 2 is easily bound to hemoglobin, releasing is difficult SHIFT TO THE LEFT (typical situation for lungs) lower portion of CO 2 higher p. H lower temperature lower content of 2, 3 -BPG
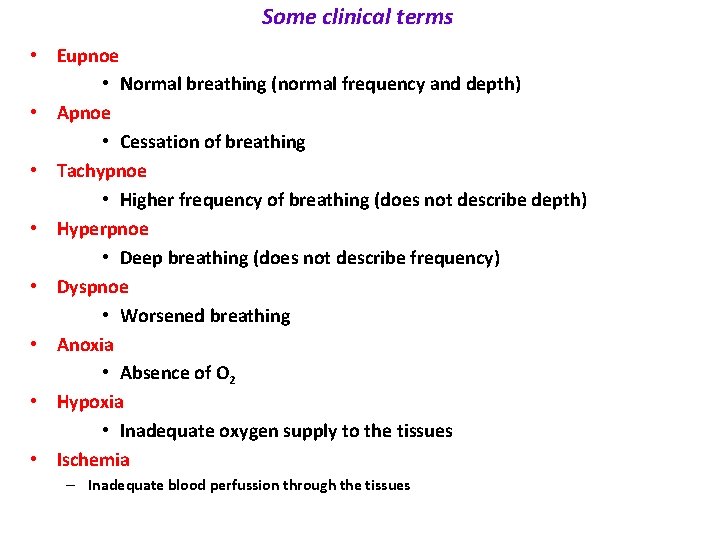
Some clinical terms • Eupnoe • Normal breathing (normal frequency and depth) • Apnoe • Cessation of breathing • Tachypnoe • Higher frequency of breathing (does not describe depth) • Hyperpnoe • Deep breathing (does not describe frequency) • Dyspnoe • Worsened breathing • Anoxia • Absence of O 2 • Hypoxia • Inadequate oxygen supply to the tissues • Ischemia – Inadequate blood perfussion through the tissues
Some clinical terms • Hyperventilation • Increased amount of ventilated air • Hypoventilation • Decreased amount of ventilated air
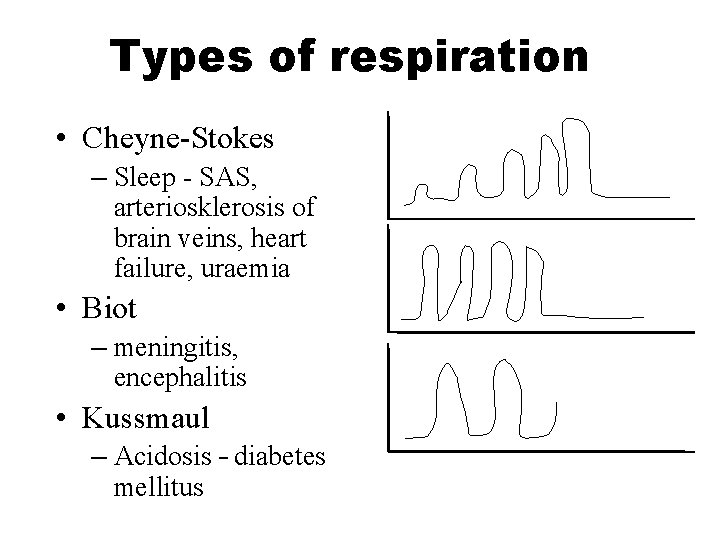
Types of respiration • Cheyne-Stokes – Sleep - SAS, arteriosklerosis of brain veins, heart failure, uraemia • Biot – meningitis, encephalitis • Kussmaul – Acidosis – diabetes mellitus
Dyspnoe • Symptome • Subjective feeling (we cannot measure it!) • Described as heavy/short breath • Respirations frequency, p. O 2, levels of blood gases do not have to correlate with the feeling • Discrepancies between the need and the ability of an organism to ensure respiration
Causes of dyspnoe • • Nervousness Obstruction Bronchospasm Hypoxemia Pleural effusion Pneumonia Edema • • • Pulmonary embolism Thick mucus secretion Anaemia Metabolism Family / financial / emotional / etc. issues
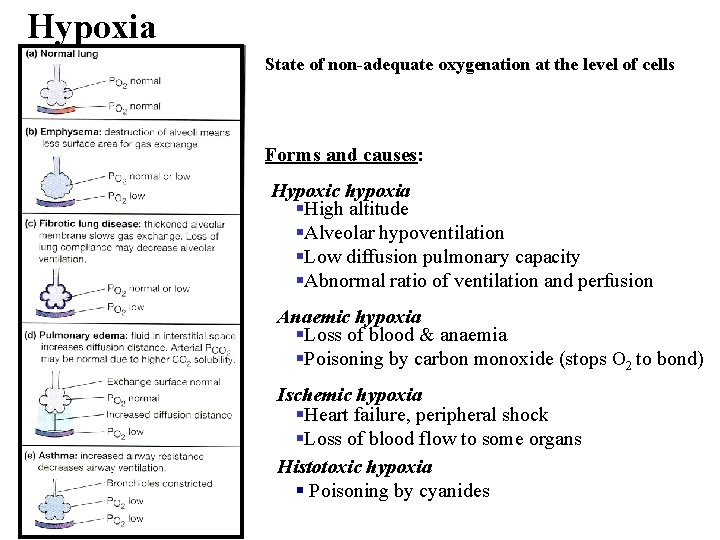
Hypoxia State of non-adequate oxygenation at the level of cells Forms and causes: Hypoxic hypoxia High altitude Alveolar hypoventilation Low diffusion pulmonary capacity Abnormal ratio of ventilation and perfusion Anaemic hypoxia Loss of blood & anaemia Poisoning by carbon monoxide (stops O 2 to bond) Ischemic hypoxia Heart failure, peripheral shock Loss of blood flow to some organs Histotoxic hypoxia Poisoning by cyanides
Chronic obstructive pulmonary disease (COPD) • Often • Medicable, easy to prevent • Continuous progression, airflow linked with immune response in airways • 3 subtypes/parts – Chronic bronchitis – Emphysema – Asthma
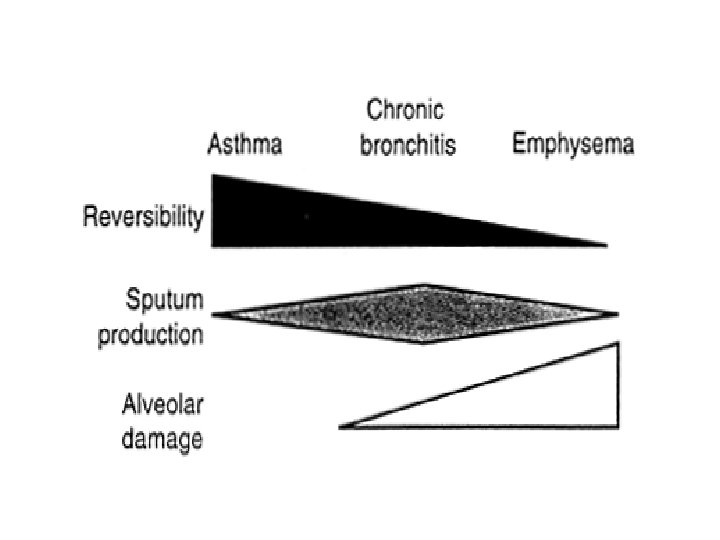
Chronic bronchitis • Chronic persistent cough lasting for at least 3 months for two consecutive years in patients where other causes of cough were excluded • Bigger bronchial submucosis glands (hyperplasia) • Terminal airways –easily susceptible to be obstructed with mucus • Increased airflow resistance • Abraded airways and decreased activity of the mucociliary apparatus increase the risk of infection
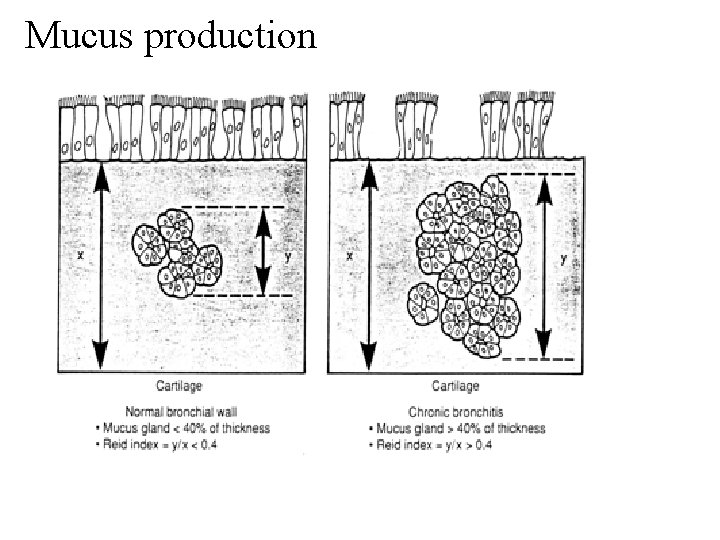
Mucus production
Asthma - definition • Chronic inflammatory obstruction of bronchi characterized by episodic, reversible bronchospasms with dyspnoea of the expiratory type as a result of the exacerbated response by bronchoconstriction to various stimuli (allergies) • Multicellular answer
Etiology of asthma • Today it is believed that asthma is the result of a combination of genetic predisposing factors and the external environment • Main triggers: – Cigarett smoke – Polluted air – Animals – Virus respiratory infections – Alergens of cockroaches – Weather changes
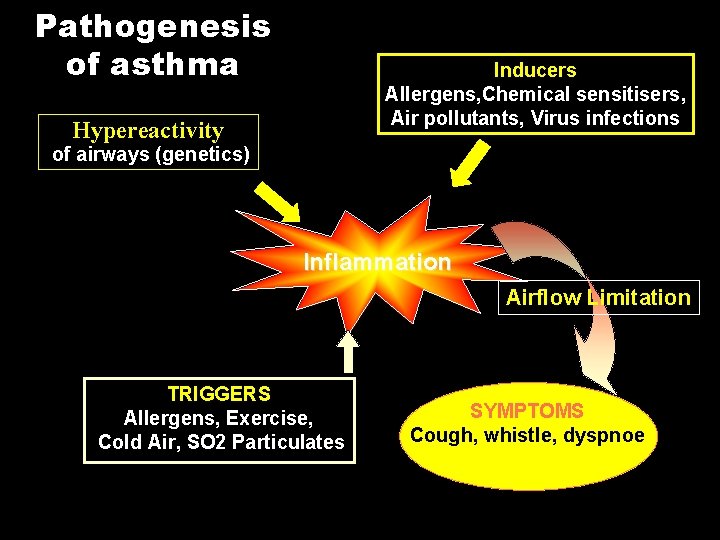
Pathogenesis of asthma Inducers Allergens, Chemical sensitisers, Air pollutants, Virus infections Hypereactivity of airways (genetics) Inflammation Airflow Limitation TRIGGERS Allergens, Exercise, Cold Air, SO 2 Particulates SYMPTOMS Cough, whistle, dyspnoe

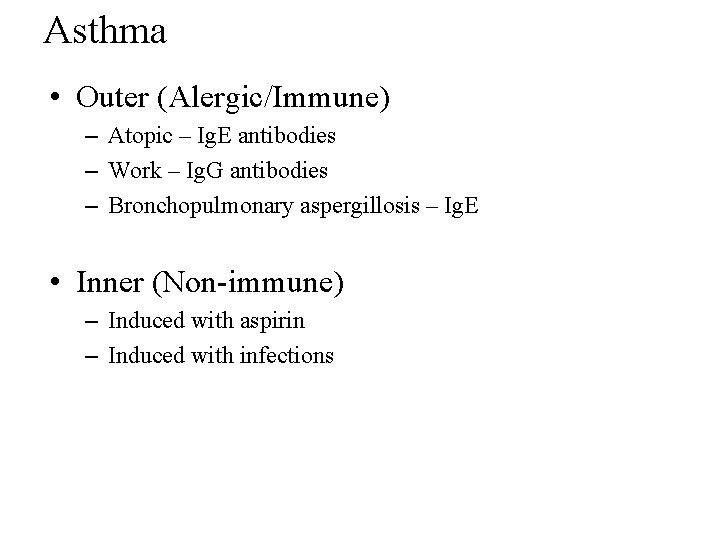
Asthma • Outer (Alergic/Immune) – Atopic – Ig. E antibodies – Work – Ig. G antibodies – Bronchopulmonary aspergillosis – Ig. E • Inner (Non-immune) – Induced with aspirin – Induced with infections
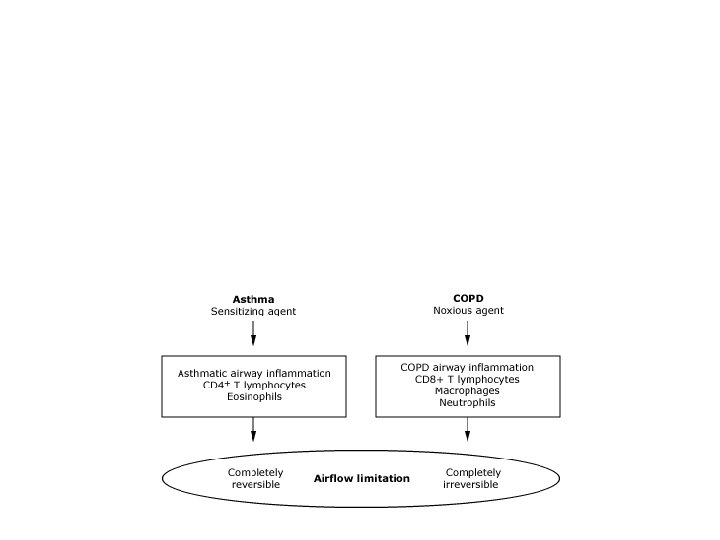
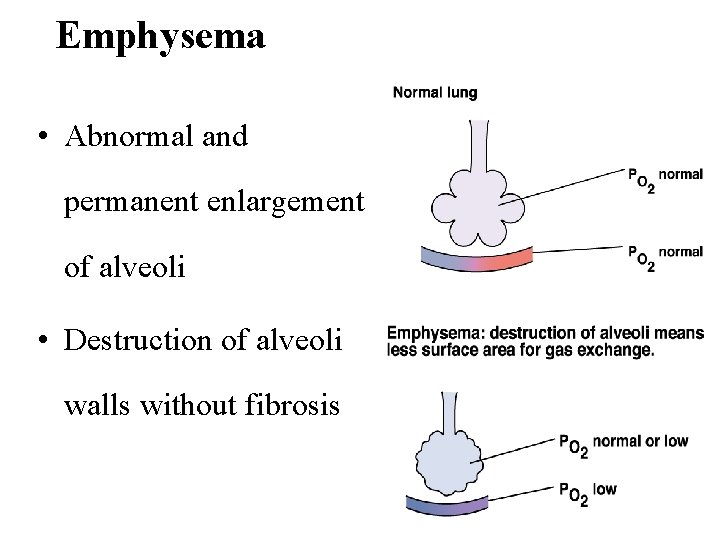
Emphysema • Abnormal and permanent enlargement of alveoli • Destruction of alveoli walls without fibrosis
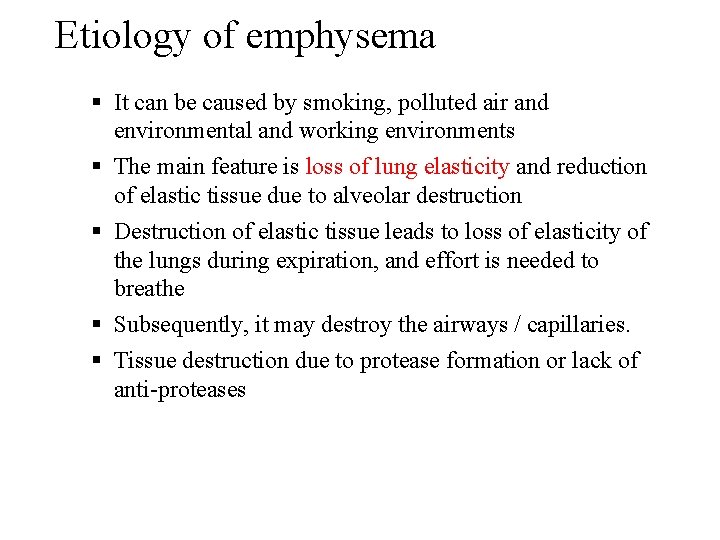
Etiology of emphysema It can be caused by smoking, polluted air and environmental and working environments The main feature is loss of lung elasticity and reduction of elastic tissue due to alveolar destruction Destruction of elastic tissue leads to loss of elasticity of the lungs during expiration, and effort is needed to breathe Subsequently, it may destroy the airways / capillaries. Tissue destruction due to protease formation or lack of anti-proteases
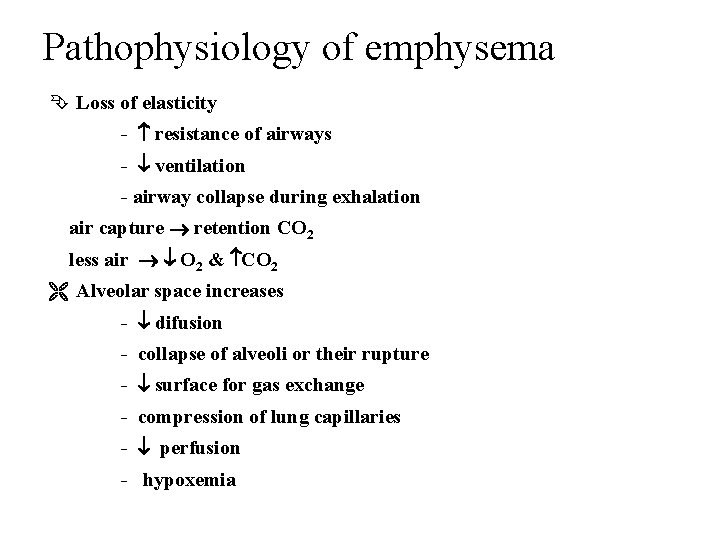
Pathophysiology of emphysema Loss of elasticity - resistance of airways - ventilation - airway collapse during exhalation air capture retention CO 2 less air O 2 & CO 2 Alveolar space increases - difusion - collapse of alveoli or their rupture - surface for gas exchange - compression of lung capillaries - perfusion - hypoxemia
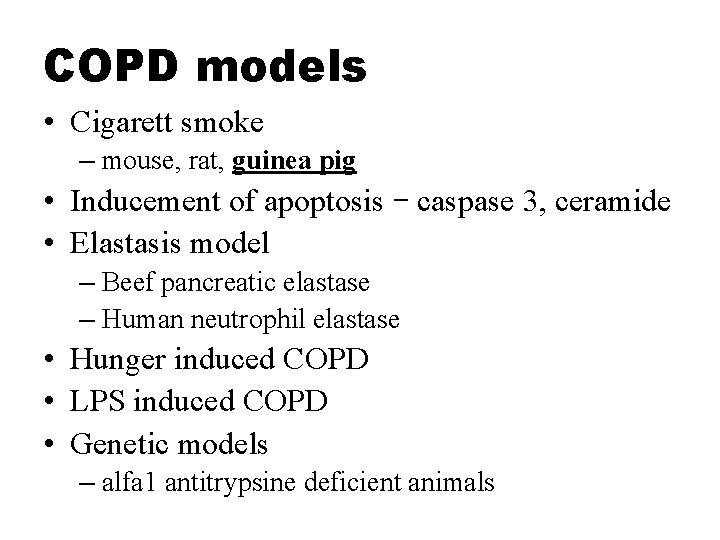
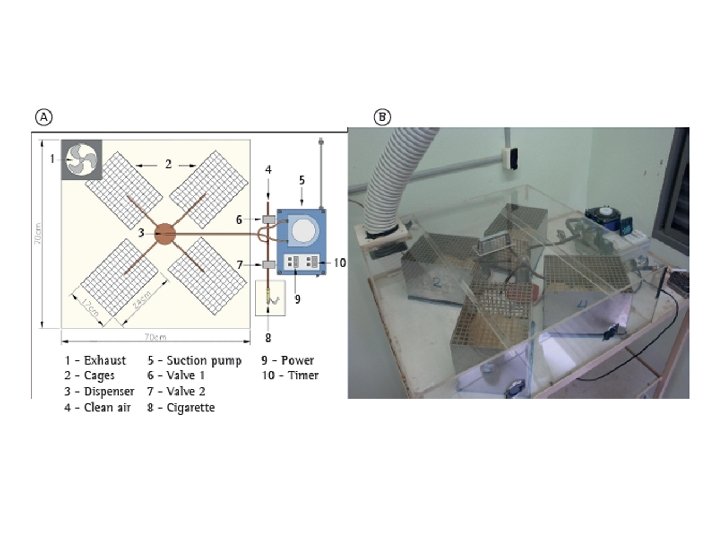
COPD models • Cigarett smoke – mouse, rat, guinea pig • Inducement of apoptosis – caspase 3, ceramide • Elastasis model – Beef pancreatic elastase – Human neutrophil elastase • Hunger induced COPD • LPS induced COPD • Genetic models – alfa 1 antitrypsine deficient animals
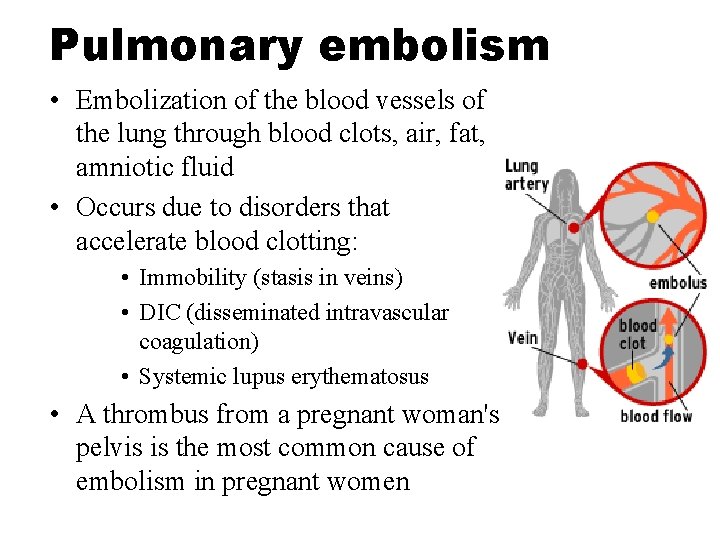
Pulmonary embolism • Embolization of the blood vessels of the lung through blood clots, air, fat, amniotic fluid • Occurs due to disorders that accelerate blood clotting: • Immobility (stasis in veins) • DIC (disseminated intravascular coagulation) • Systemic lupus erythematosus • A thrombus from a pregnant woman's pelvis is the most common cause of embolism in pregnant women
Pulmonary embolism – Virchow’s triad • Stasis of blood in veins • Vascular wall disorder • Hypercoagulation • 4 categories – massive – for example major pulmonary artery involvement – pulmonary infarction – death of a part of a tissue – without infarction – not so serious embolus – multiple pulmonary embolus
Animal models of pulmonary embolism • Farmacological – Thrombine, collagen+adrenaline • Photochemical methods – Green laser damages cell wall oxidative stress damage on blood vessel wall thrombus on the damaged endothelium
Acute Respiratory Distress Syndrome – ARDS • Pulmonary edema resulting not from cardiac failure • Progressive refractory hypoxemia (not responding to compensatory mechanisms or treatment) • Severe dyspnoea – Diffusion of bilateral infiltrates • Physiological changes – Damage to the lung endothelium causes increased lung permeability – The fluid escapes into interstitium, causing pulmonary edema • Complications of hospitalized patients – Serious medical - surgical problem – It does not have to be related to lung damage – Mortality is about 50 -60%
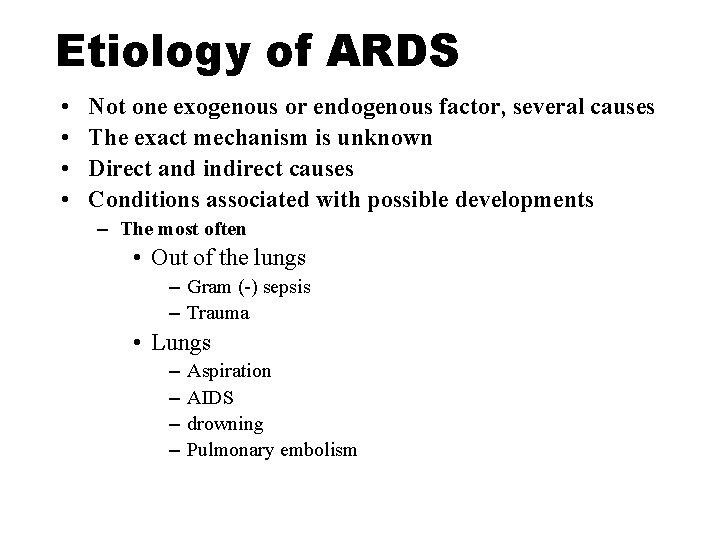
Etiology of ARDS • • Not one exogenous or endogenous factor, several causes The exact mechanism is unknown Direct and indirect causes Conditions associated with possible developments – The most often • Out of the lungs – Gram (-) sepsis – Trauma • Lungs – – Aspiration AIDS drowning Pulmonary embolism
Etiology of ARDS • Others – – – – embolism by amniotic fluid heart infarction drugs multiple fractures / polytrauma heatstroke peritonitis multiple blood transfusions
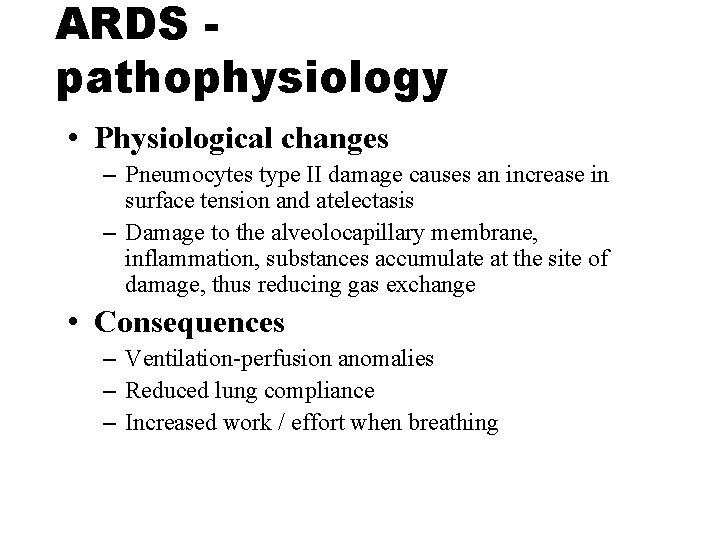
ARDS pathophysiology • Physiological changes – Pneumocytes type II damage causes an increase in surface tension and atelectasis – Damage to the alveolocapillary membrane, inflammation, substances accumulate at the site of damage, thus reducing gas exchange • Consequences – Ventilation-perfusion anomalies – Reduced lung compliance – Increased work / effort when breathing
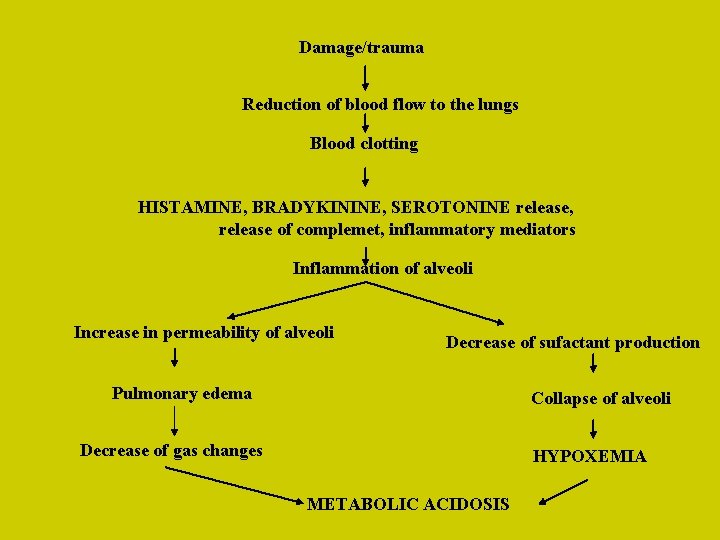
Damage/trauma Reduction of blood flow to the lungs Blood clotting HISTAMINE, BRADYKININE, SEROTONINE release, release of complemet, inflammatory mediators Inflammation of alveoli Increase in permeability of alveoli Decrease of sufactant production Pulmonary edema Collapse of alveoli Decrease of gas changes HYPOXEMIA METABOLIC ACIDOSIS
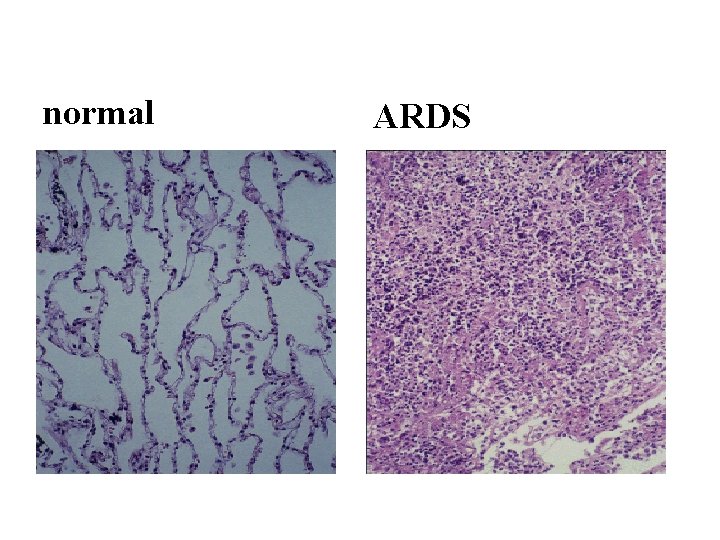
normal • normal ARDS
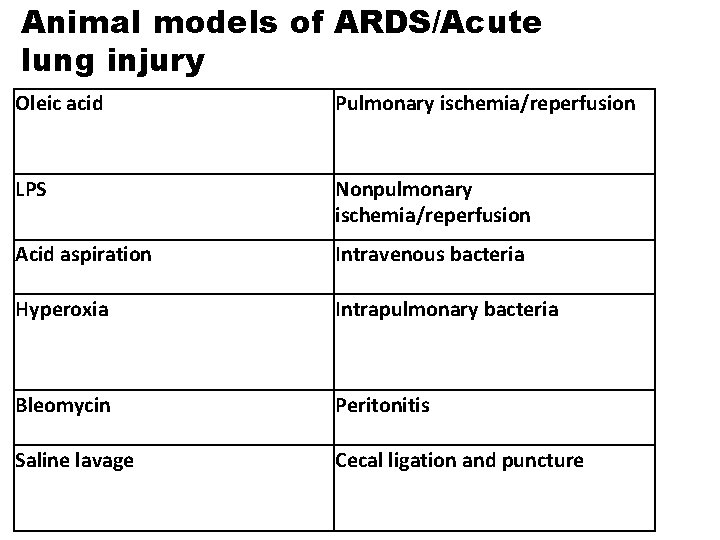
Animal models of ARDS/Acute lung injury Oleic acid Pulmonary ischemia/reperfusion LPS Nonpulmonary ischemia/reperfusion Acid aspiration Intravenous bacteria Hyperoxia Intrapulmonary bacteria Bleomycin Peritonitis Saline lavage Cecal ligation and puncture
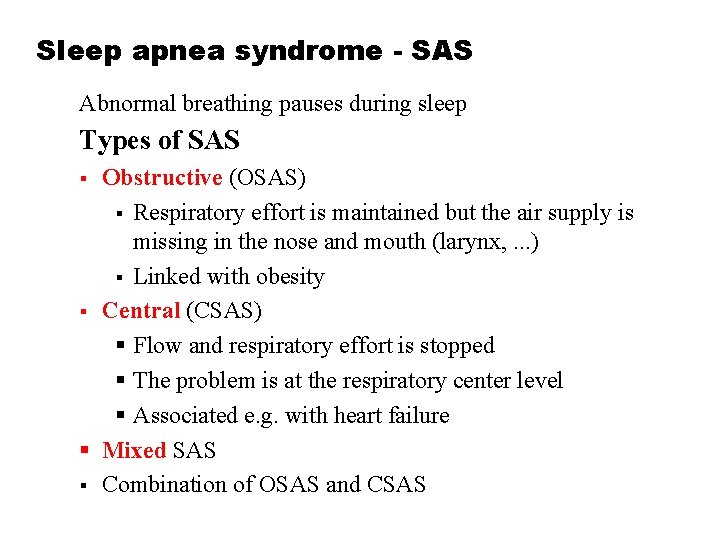
Sleep apnea syndrome - SAS Abnormal breathing pauses during sleep Types of SAS Obstructive (OSAS) Respiratory effort is maintained but the air supply is missing in the nose and mouth (larynx, . . . ) Linked with obesity Central (CSAS) Flow and respiratory effort is stopped The problem is at the respiratory center level Associated e. g. with heart failure Mixed SAS Combination of OSAS and CSAS
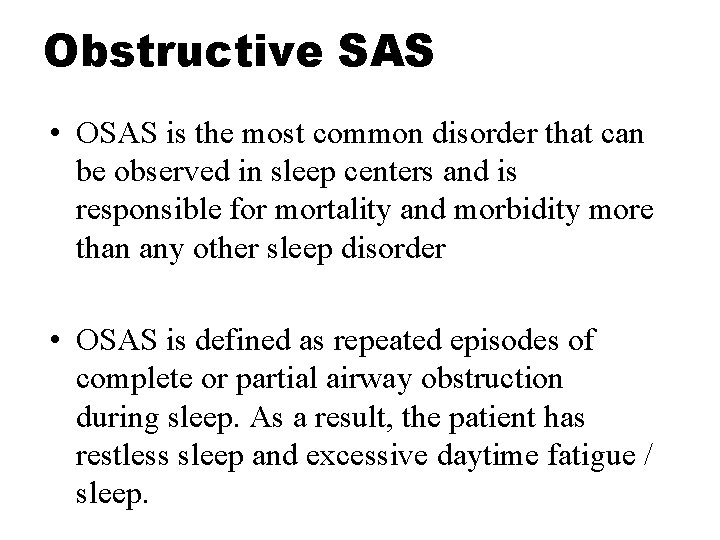
Obstructive SAS • OSAS is the most common disorder that can be observed in sleep centers and is responsible for mortality and morbidity more than any other sleep disorder • OSAS is defined as repeated episodes of complete or partial airway obstruction during sleep. As a result, the patient has restless sleep and excessive daytime fatigue / sleep.
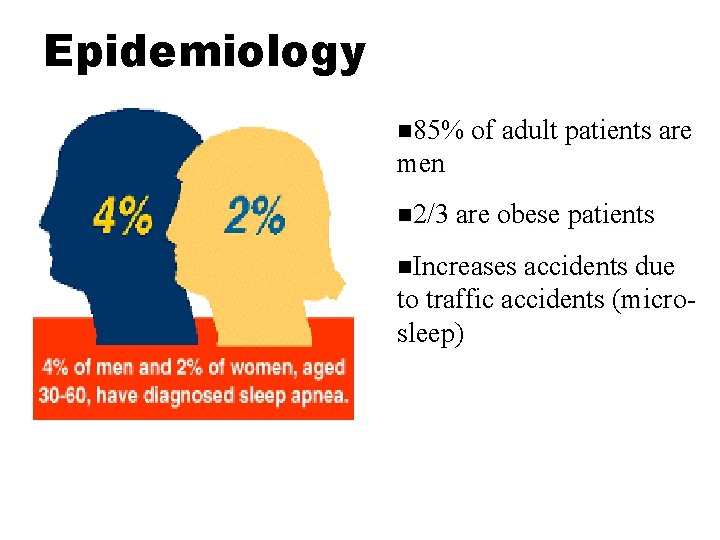
Epidemiology 85% of adult patients are men 2/3 are obese patients Increases accidents due to traffic accidents (microsleep)
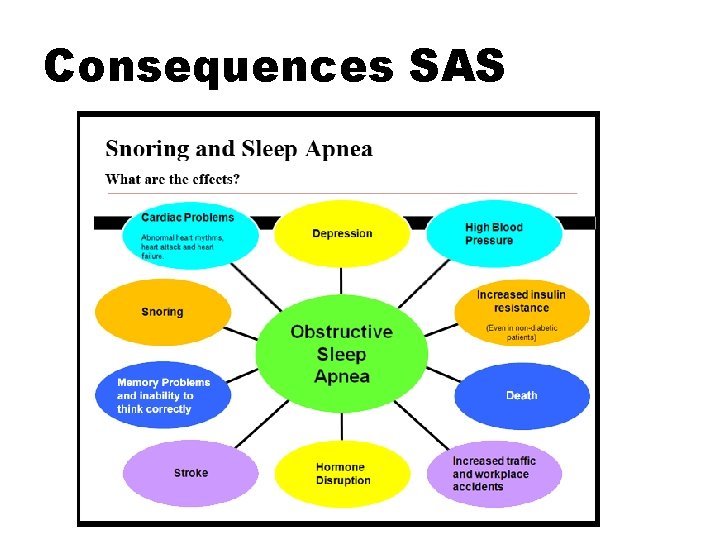
Consequences SAS

Main symptoms • • loud snoring - disturbed sleep night's wheezing and suffocation confirmed daily fatigue and sleepiness short rough neck

Therapy
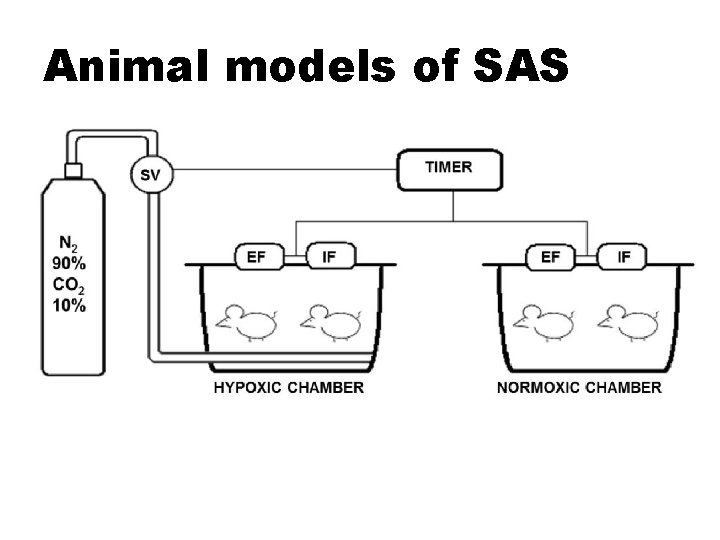
Animal models of SAS
Pneumothorax • PATOPHYSIOLOGY – presence of air in the thoracic cavity • Open pneumothorax • The air comes rapidly to the chest, and comes out during expiration • Tension pneumothorax – thorax closed: the air accumulates during breathing, as it can not escape – It increases the intra-ocular pressure that pushes the undamaged part of the lungs, then the mediastinum and the heart, and the other side of the lungs. Reduced venous return to the right rupture due to pressure on lower and upper vein
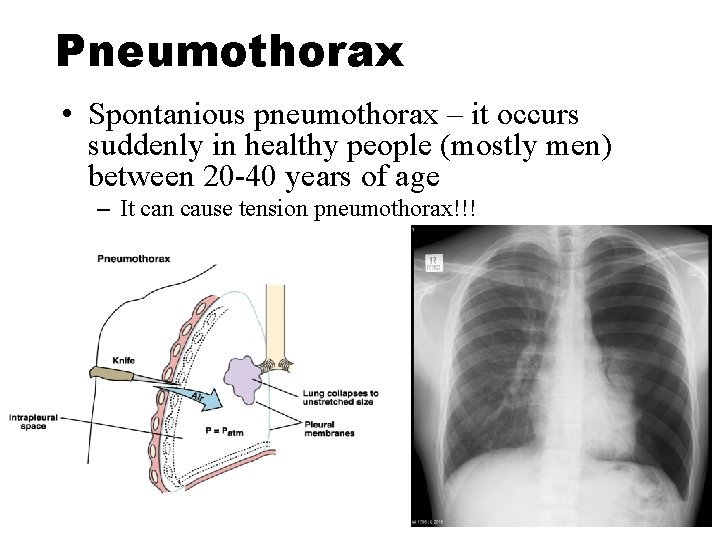
Pneumothorax • Spontanious pneumothorax – it occurs suddenly in healthy people (mostly men) between 20 -40 years of age – It can cause tension pneumothorax!!!

Thank you for your attention www. imbm. sk basa. konecna@gmail. com
- Slides: 57