Pathology of The Gastrointestinal tract Ghadeer Hayel MD


- Slides: 33
Pathology of The Gastrointestinal tract Ghadeer Hayel, MD
1. The ORAL Cavity ORAL INFLAMMATORY LESIONS
aphthous ulcers (canker sores) Ø Common superficial mucosal ulcerations, in 1 st & 2 nd decades, & extremely painful. Ø Cause is unknown; but tend to be familal and ass with celiac disease, inflammatory bowel disease, and Behçet disease. Ø solitary or multiple. Ø Mostly resolve in 7 to 10 days but can recur. 3

aphthous ulcers (canker sores) Shallow, with a hyperemic base covered by a thin exudate and rimmed by a narrow zone of erythema. Discontinuity of epithelium + dense inflammation 4
Herpes Simplex Virus Infections(HSV) Ø Most orofacial herpetic infections (HSV-1), remainder HSV-2 (genital herpes). Ø (1) primary self-limited infection, (2) reactivated when there is a compromise in host resistance. Ø Primary: in children (age 2 -4) often asymptomatic. but 1020% develop acute herpetic gingivostomatitis (vesicles and ulcerations throughout the oral cavity). Ø Most adults harbor latent HSV-1 (in nerves ganglia) Ø Reactivation: Recurrent herpetic stomatitis “cold sore” 5
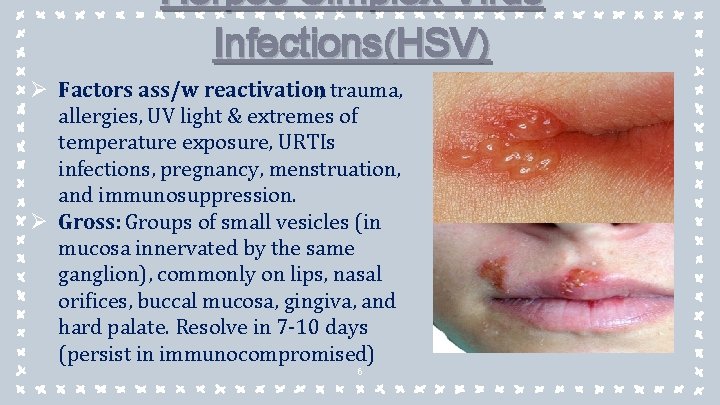
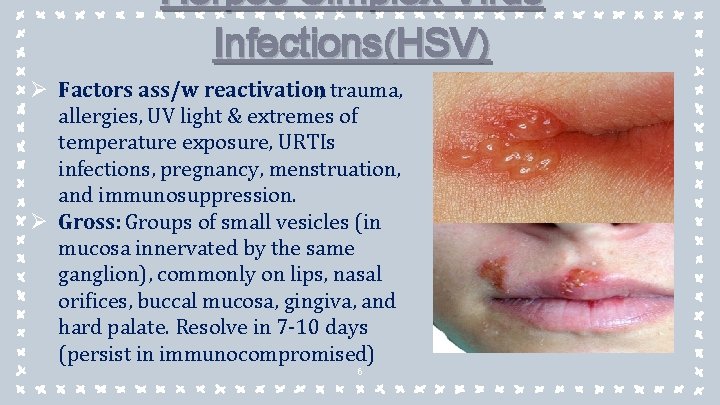
Herpes Simplex Virus Infections(HSV) Ø Factors ass/w reactivation; trauma, allergies, UV light & extremes of temperature exposure, URTIs infections, pregnancy, menstruation, and immunosuppression. Ø Gross: Groups of small vesicles (in mucosa innervated by the same ganglion), commonly on lips, nasal orifices, buccal mucosa, gingiva, and hard palate. Resolve in 7 -10 days (persist in immunocompromised) 6
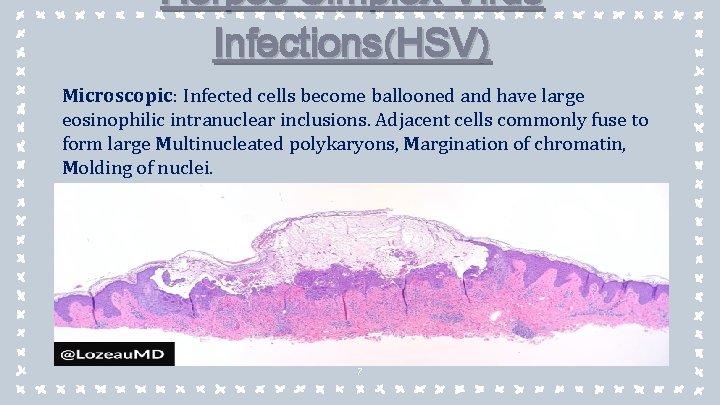
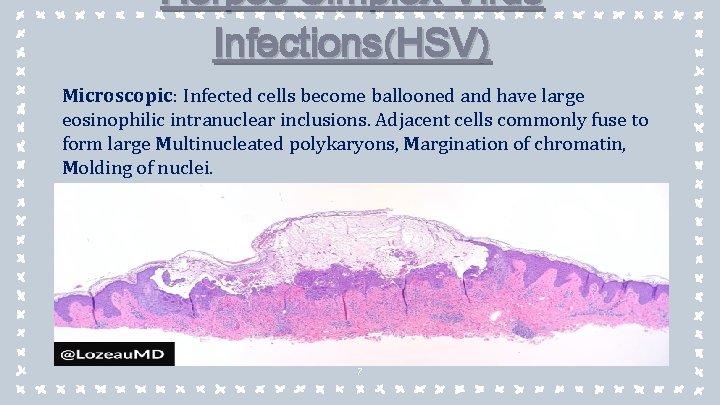
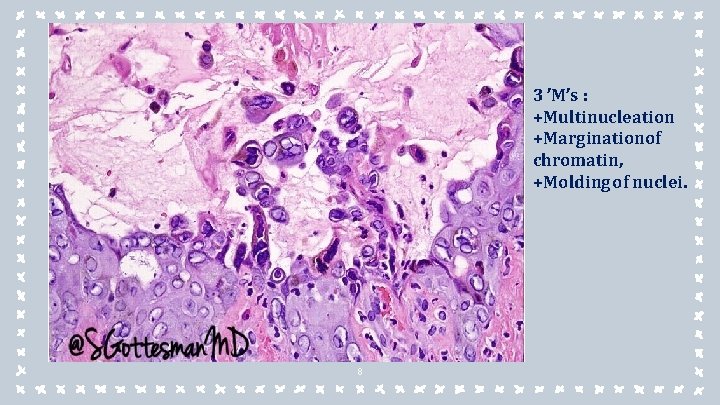
Herpes Simplex Virus Infections(HSV) Microscopic : Infected cells become ballooned and have large eosinophilic intranuclear inclusions. Adjacent cells commonly fuse to form large Multinucleated polykaryons, Margination of chromatin, Molding of nuclei. 7
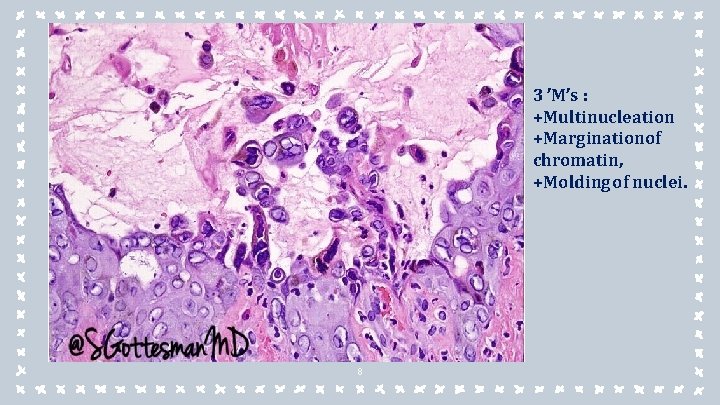
3 ’M’s : +Multinucleation +Marginationof chromatin, +Molding of nuclei. 8
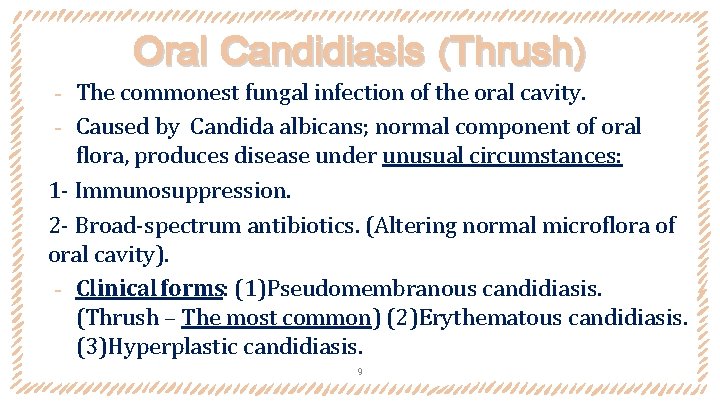
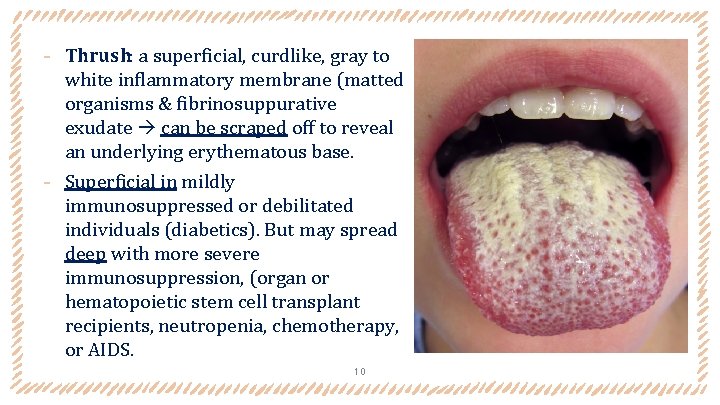
Oral Candidiasis (Thrush) The commonest fungal infection of the oral cavity. ‐ Caused by Candida albicans; normal component of oral flora, produces disease under unusual circumstances: 1 - Immunosuppression. 2 - Broad-spectrum antibiotics. (Altering normal microflora of oral cavity). ‐ Clinical forms: (1)Pseudomembranous candidiasis. (Thrush – The most common) (2)Erythematous candidiasis. (3)Hyperplastic candidiasis. ‐ 9
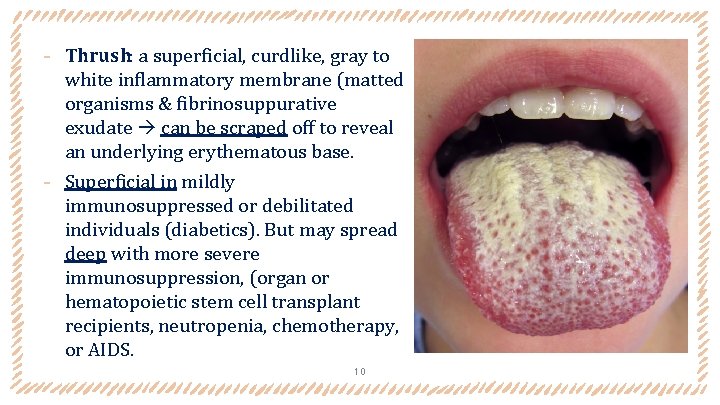
‐ Thrush: a superficial, curdlike, gray to white inflammatory membrane (matted organisms & fibrinosuppurative exudate can be scraped off to reveal an underlying erythematous base. ‐ Superficial in mildly immunosuppressed or debilitated individuals (diabetics). But may spread deep with more severe immunosuppression, (organ or hematopoietic stem cell transplant recipients, neutropenia, chemotherapy, or AIDS. 10
1. The ORAL Cavity PROLIFERATIVE AND NEOPLASTIC LESIONS OF THE ORAL CAVITY
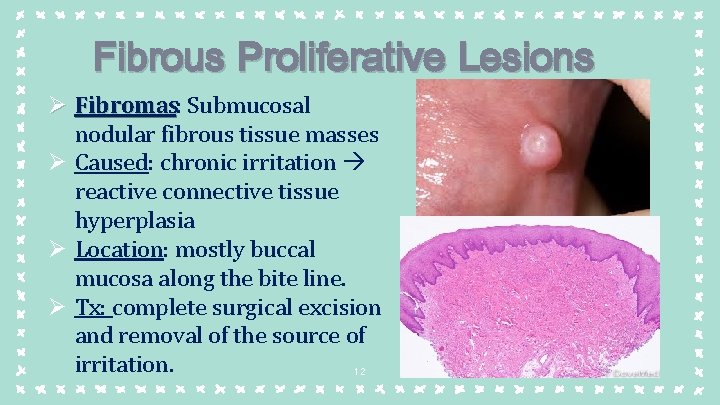
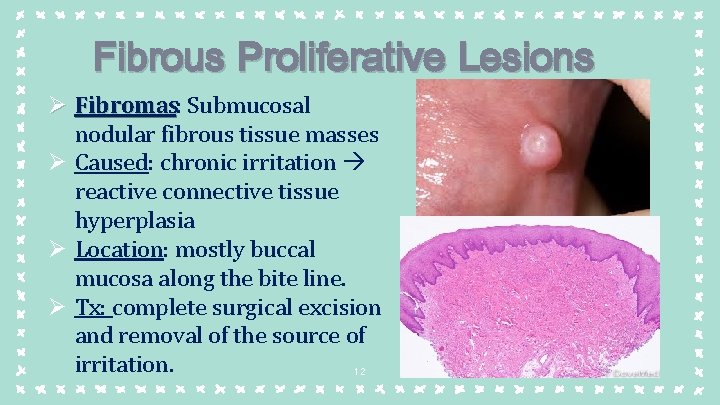
Fibrous Proliferative Lesions Ø Fibromas: Fibromas Submucosal nodular fibrous tissue masses Ø Caused: chronic irritation reactive connective tissue hyperplasia Ø Location: mostly buccal mucosa along the bite line. Ø Tx: complete surgical excision and removal of the source of irritation. 12
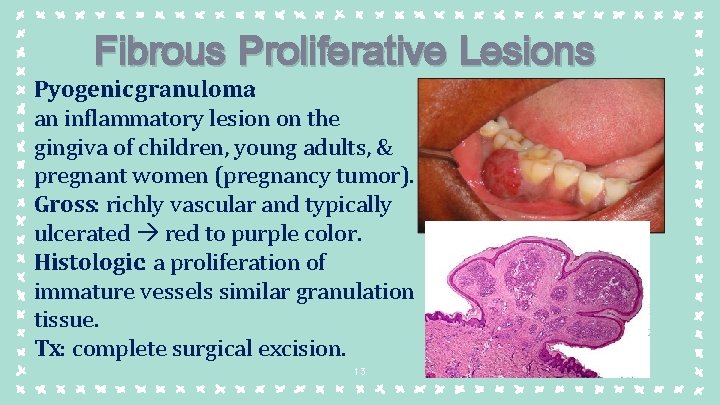
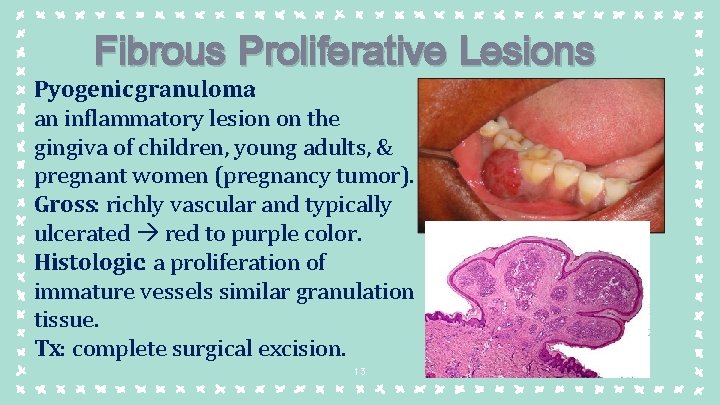
Fibrous Proliferative Lesions Pyogenic granuloma: an inflammatory lesion on the gingiva of children, young adults, & pregnant women (pregnancy tumor). Gross: richly vascular and typically ulcerated red to purple color. Histologic: a proliferation of immature vessels similar granulation tissue. Tx: complete surgical excision. 13
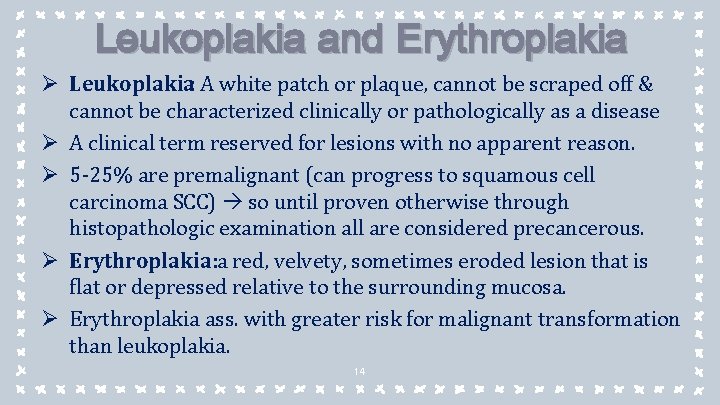
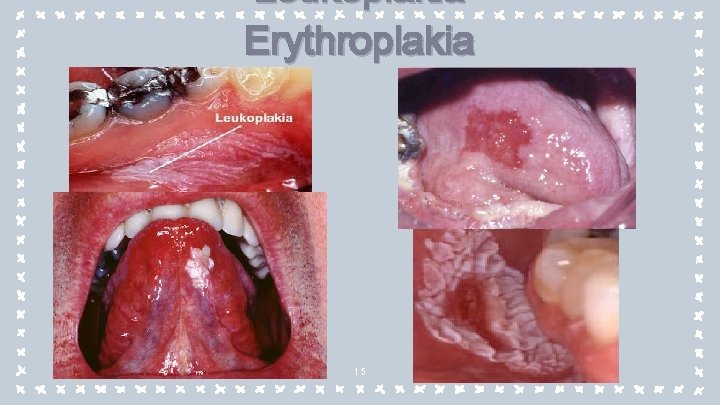
Leukoplakia and Erythroplakia Ø Leukoplakia: A white patch or plaque, cannot be scraped off & cannot be characterized clinically or pathologically as a disease Ø A clinical term reserved for lesions with no apparent reason. Ø 5 -25% are premalignant (can progress to squamous cell carcinoma SCC) so until proven otherwise through histopathologic examination all are considered precancerous. Ø Erythroplakia: a red, velvety, sometimes eroded lesion that is flat or depressed relative to the surrounding mucosa. Ø Erythroplakia ass. with greater risk for malignant transformation than leukoplakia. 14
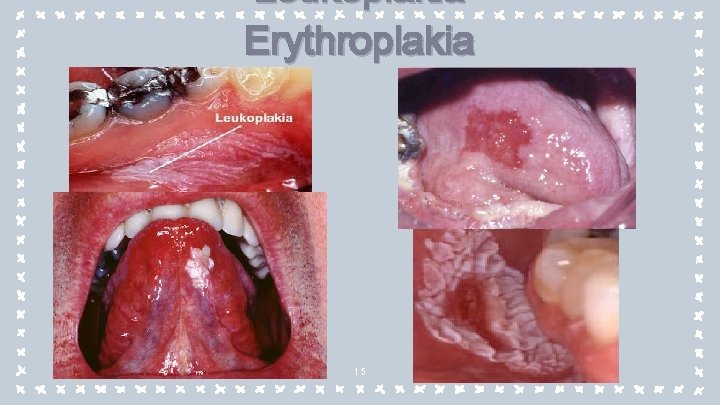
Leukoplakia Erythroplakia 15
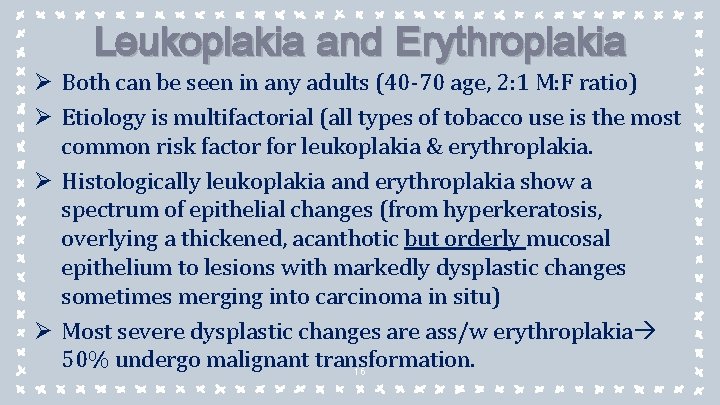
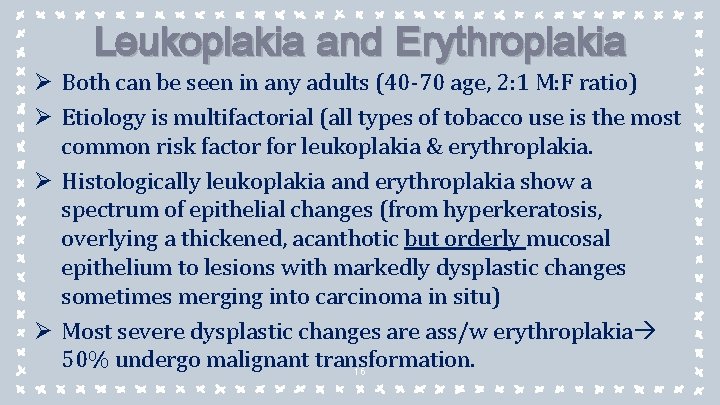
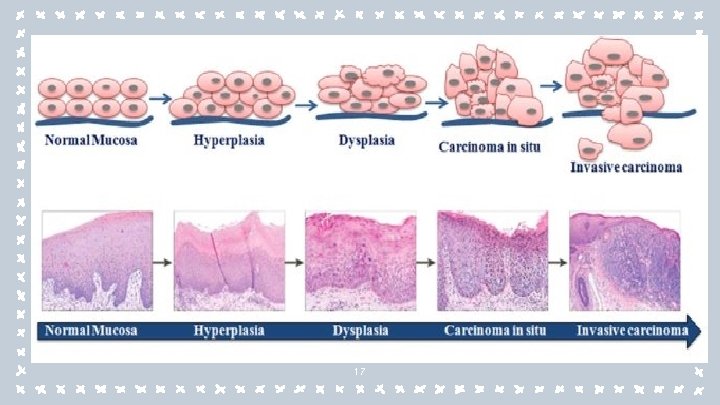
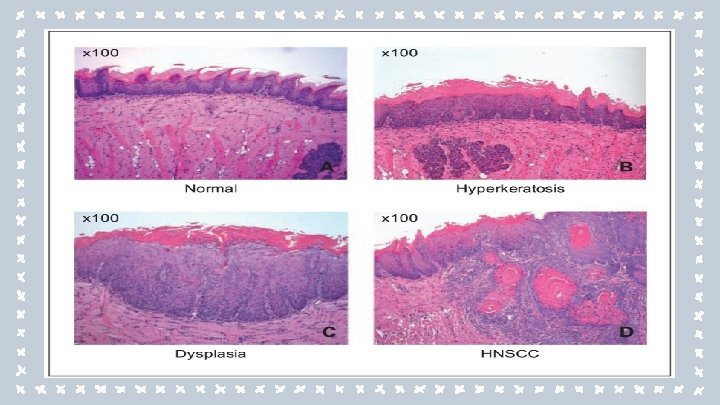
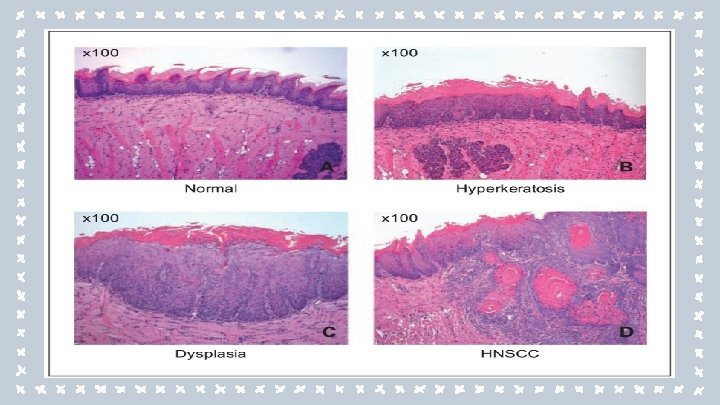
Leukoplakia and Erythroplakia Ø Both can be seen in any adults (40 -70 age, 2: 1 M: F ratio) Ø Etiology is multifactorial (all types of tobacco use is the most common risk factor for leukoplakia & erythroplakia. Ø Histologically leukoplakia and erythroplakia show a spectrum of epithelial changes (from hyperkeratosis, overlying a thickened, acanthotic but orderly mucosal epithelium to lesions with markedly dysplastic changes sometimes merging into carcinoma in situ) Ø Most severe dysplastic changes are ass/w erythroplakia 50% undergo malignant transformation. 16
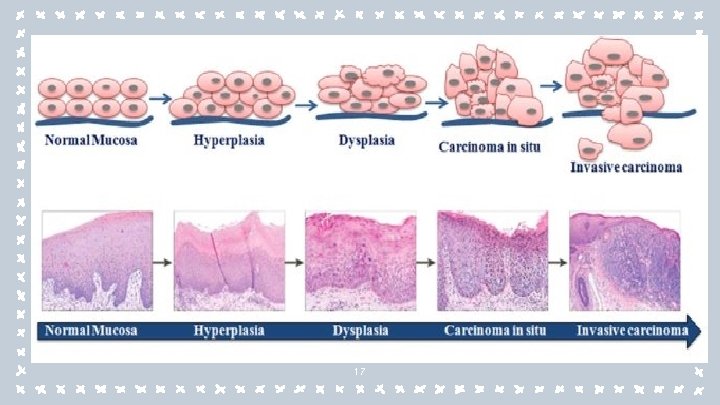
17
18
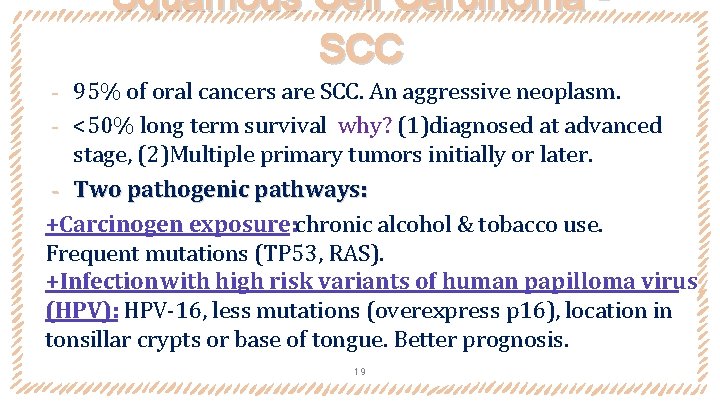
Squamous Cell Carcinoma SCC 95% of oral cancers are SCC. An aggressive neoplasm. ‐ <50% long term survival why? (1)diagnosed at advanced stage, (2)Multiple primary tumors initially or later. ‐ Two pathogenic pathways: +Carcinogen exposure: chronic alcohol & tobacco use. Frequent mutations (TP 53, RAS). +Infection with high risk variants of human papilloma virus (HPV): HPV-16, less mutations (overexpress p 16), location in tonsillar crypts or base of tongue. Better prognosis. ‐ 19
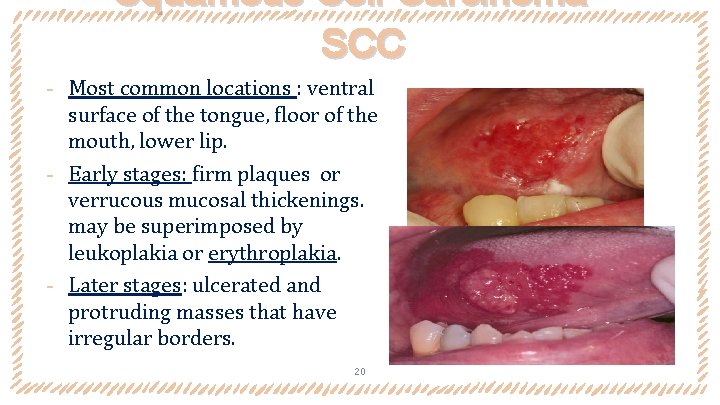
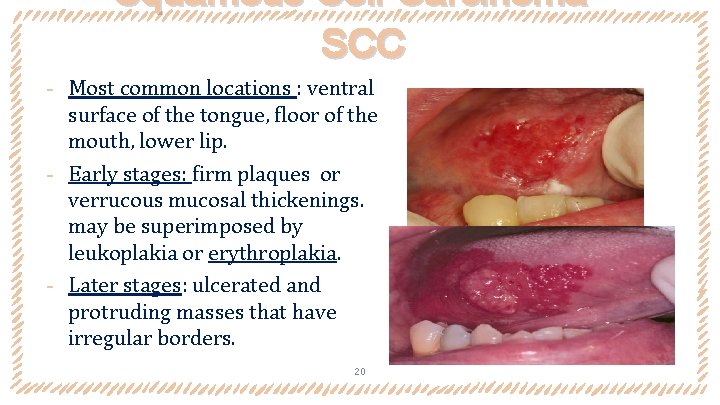
Squamous Cell Carcinoma SCC ‐ Most common locations : ventral surface of the tongue, floor of the mouth, lower lip. ‐ Early stages: firm plaques or verrucous mucosal thickenings. may be superimposed by leukoplakia or erythroplakia. ‐ Later stages: ulcerated and protruding masses that have irregular borders. 20
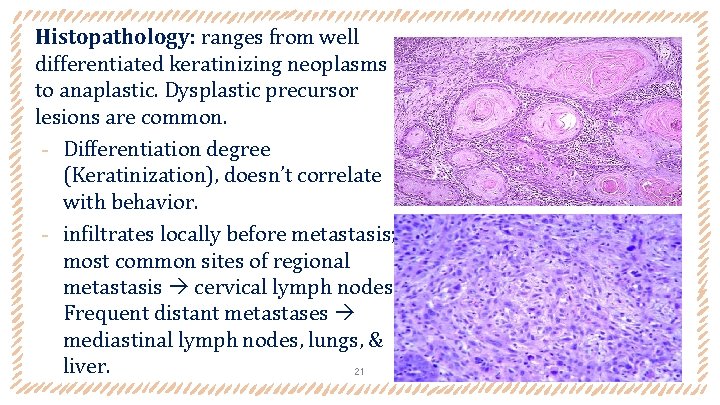
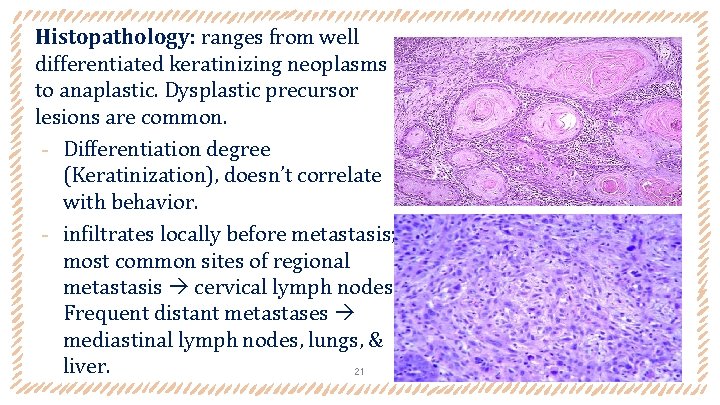
Histopathology: ranges from well differentiated keratinizing neoplasms to anaplastic. Dysplastic precursor lesions are common. ‐ Differentiation degree (Keratinization), doesn’t correlate with behavior. ‐ infiltrates locally before metastasis; most common sites of regional metastasis cervical lymph nodes. Frequent distant metastases mediastinal lymph nodes, lungs, & liver. 21
1. The ORAL Cavity DISEASES OF SALIVARY GLAND
Xerostomia Ø Dry mouth decrease production of saliva. Ø 20% of people >70 years. Ø Part of Sjögren syndrome, & complication after radiation therapy. Ø Side effect of many common drug classes: anticholinergic, anti-depressant/anti-psychotic, diuretic, anti-hypertensive, sedative, muscle relaxant, analgesic, and anti-histaminic agents. Ø Increased risk for dental caries and candidiasis, in addition to difficulty in speaking and swallowing. 23
Sialadenitis Ø Inflammation of the salivary glands. Ø Etiology: trauma, viral or bacterial infection, or autoimmune disease. Ø Viral sialadenitis: The most common is mumps, produce enlargement of all salivary glands (predominantly parotids) +In Children: a self-limited benign condition. +In adults: it can cause pancreatitis or orchitis (sometimes causes sterility). 24
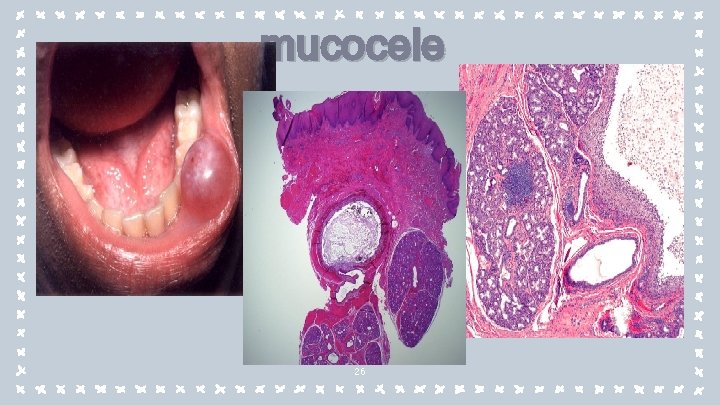
mucocele Ø The most common inflammatory lesion of the salivay glands Etiology: Blockage or rupture of a salivary gland duct leakage of saliva into the surrounding connective tissue stroma. Ø Ages: toddlers, young adults, & older adults. Ø Presentation: a fluctuant swelling of lower lip (change in size in association with meals). Ø Histologic: a cyst-like space lined by granulation tissue or fibrous connective tissue & filled with mucin & inflammatory cells (macrophages) Ø Tx: Complete excision of the cyst and the minor salivary gland. 25
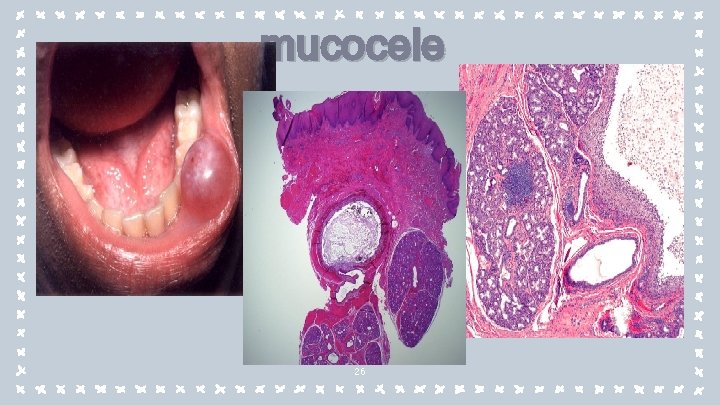
mucocele 26

Bacterial sialadenitis Ø Major salivary glands disease (submandibular glands). Ø Pathogens: Staphylococcus aureus and Streptococcus viridans. Ø Etiologies: Duct obstruction by stones (sialolithiasis), impacted food debris or by edema due to injury. Ø Systemic dehydration, with decreased salivary secretions, may predispose to suppurative bacterial parotitis in older adult following major thoracic or abdominal surgery. Ø May be ass/w suppurative necrosis and abscess formation. 27
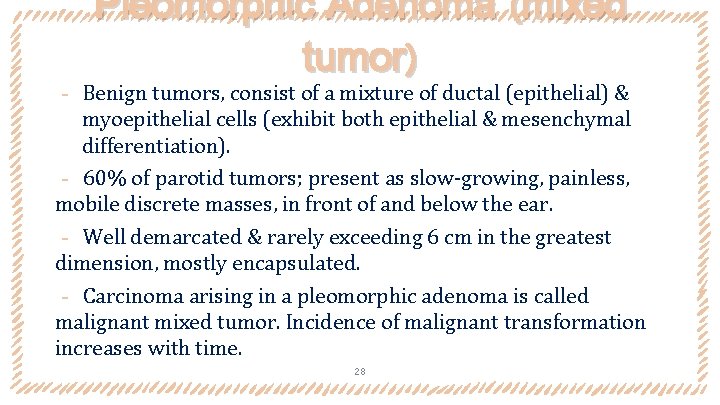
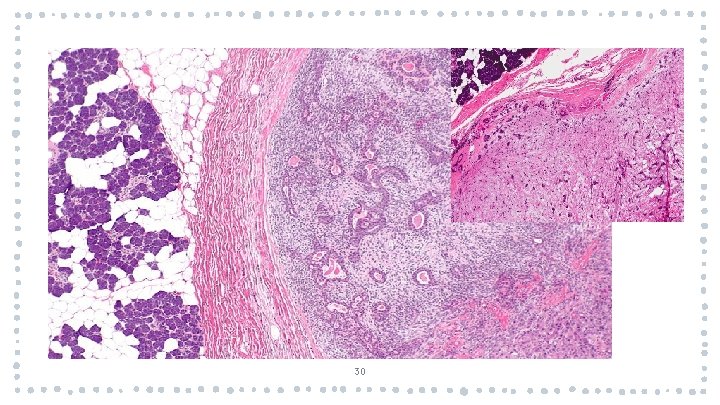
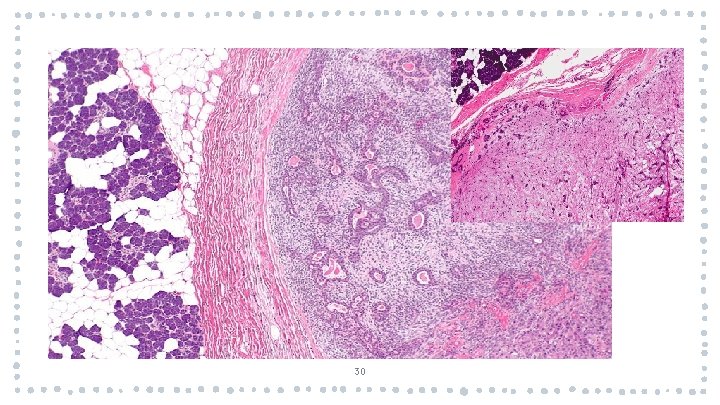
Pleomorphic Adenoma (mixed tumor) ‐ Benign tumors, consist of a mixture of ductal (epithelial) & myoepithelial cells (exhibit both epithelial & mesenchymal differentiation). ‐ 60% of parotid tumors; present as slow-growing, painless, mobile discrete masses, in front of and below the ear. ‐ Well demarcated & rarely exceeding 6 cm in the greatest dimension, mostly encapsulated. ‐ Carcinoma arising in a pleomorphic adenoma is called malignant mixed tumor. Incidence of malignant transformation increases with time. 28
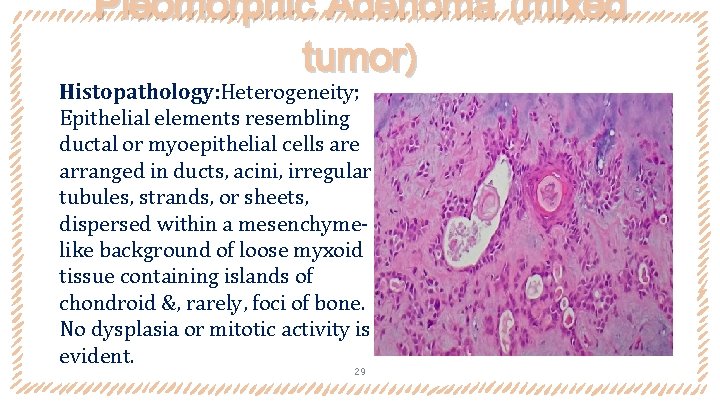
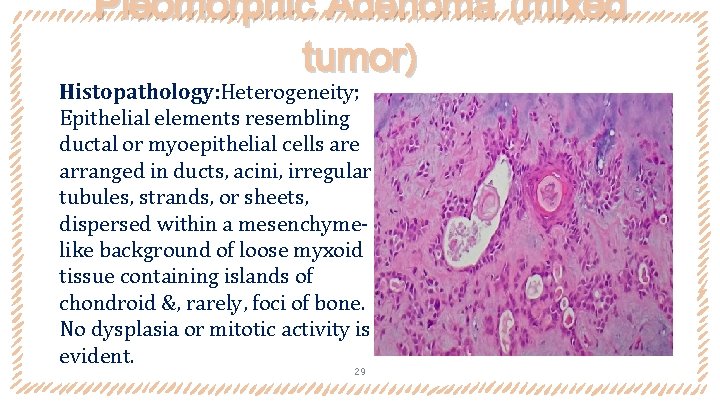
Pleomorphic Adenoma (mixed tumor) Histopathology: Heterogeneity; Epithelial elements resembling ductal or myoepithelial cells are arranged in ducts, acini, irregular tubules, strands, or sheets, dispersed within a mesenchymelike background of loose myxoid tissue containing islands of chondroid &, rarely, foci of bone. No dysplasia or mitotic activity is evident. 29
30
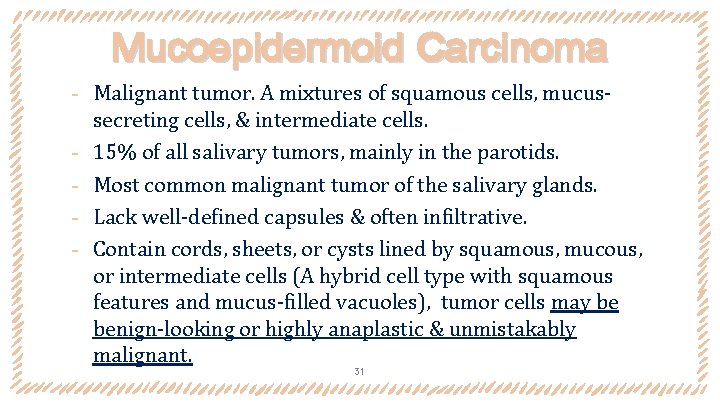
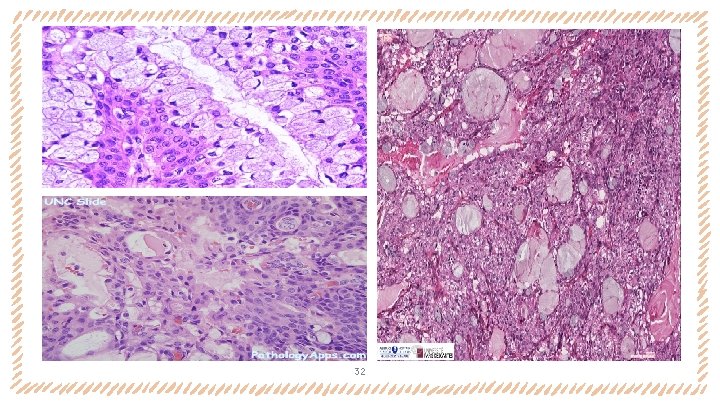
Mucoepidermoid Carcinoma ‐ Malignant tumor. A mixtures of squamous cells, mucus‐ ‐ secreting cells, & intermediate cells. 15% of all salivary tumors, mainly in the parotids. Most common malignant tumor of the salivary glands. Lack well-defined capsules & often infiltrative. Contain cords, sheets, or cysts lined by squamous, mucous, or intermediate cells (A hybrid cell type with squamous features and mucus-filled vacuoles), tumor cells may be benign-looking or highly anaplastic & unmistakably malignant. 31
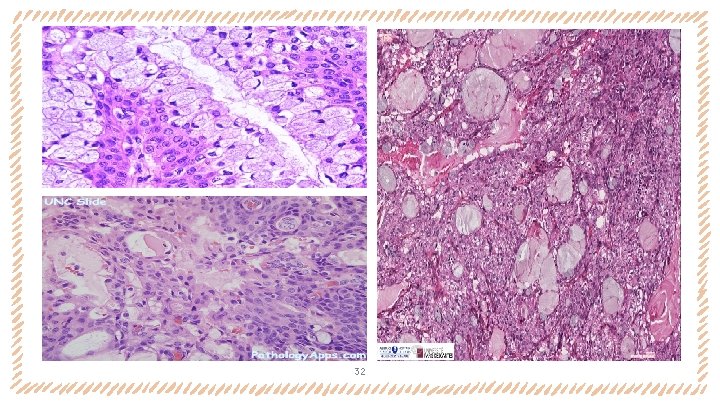
32
”The books that help you most are those which make you think the most. The hardest way of learning is that of easy reading; but a great book that comes from a great thinker is a ship of thought, deep freighted with truth and beauty. ” Pablo Neruda 33
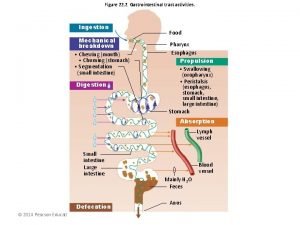
 Composition of stomach
Composition of stomach Alimentary canal diagram
Alimentary canal diagram Gastrointestinal tract
Gastrointestinal tract Gastrointestinal tract
Gastrointestinal tract Ghadeer khum
Ghadeer khum Olivospinal tract vs tectospinal tract
Olivospinal tract vs tectospinal tract Extrapyramidal tract function
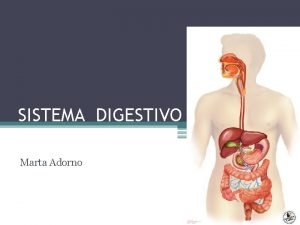
Extrapyramidal tract function Cavidade abdominal
Cavidade abdominal Chapter 15 the gastrointestinal system
Chapter 15 the gastrointestinal system Intestinal villus
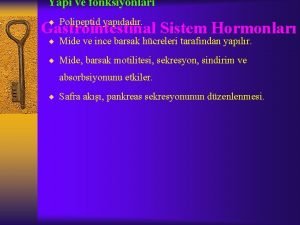
Intestinal villus Sekretin ailesi
Sekretin ailesi Embryo folding
Embryo folding Borborygmi
Borborygmi Encéfalo
Encéfalo Gastrointestinal hormones
Gastrointestinal hormones Gastrointestinal
Gastrointestinal Gastrointestinal medical terminology breakdown
Gastrointestinal medical terminology breakdown Motilidad gastrointestinal
Motilidad gastrointestinal Embriologia del sistema gastrointestinal
Embriologia del sistema gastrointestinal Functional constipation vs hirschsprung
Functional constipation vs hirschsprung Dr sigid djuniawan
Dr sigid djuniawan Metformin and constipation
Metformin and constipation Dumping syndrome signs
Dumping syndrome signs Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Peroral ne demek
Peroral ne demek Docimasia gastrointestinal de breslau
Docimasia gastrointestinal de breslau Nutrition focused physical assessment
Nutrition focused physical assessment Pneumatic reduction of intussusception
Pneumatic reduction of intussusception Tư thế ngồi viết
Tư thế ngồi viết Thế nào là số nguyên tố
Thế nào là số nguyên tố đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton ưu thế lai là gì
ưu thế lai là gì