PARANEOPLASTIC SYNDROMES Steven K Gerhardt M D Neurology






- Slides: 41

PARANEOPLASTIC SYNDROMES Steven K. Gerhardt, M. D. Neurology Consultants of Dallas 3/9/2021
DEFINITION u u “All neurologic abnormalities not caused by the cancer’s spread to the nervous system are paraneoplastic” “Remote effects of cancer on the nervous system”

PARANEOPLASTIC SYNDROMES u Neurologic symptoms of paraneoplastic syndromes usually precede the identification of the cancer

PARANEOPLASTIC SYNDROMES u Usually when the paraneoplastic -related cancer is identified, it is small, nonmetastatic, and indolently growing

PARANEOPLASTIC SYNDROMES u Neurologic disability caused by paraneoplastic syndromes is often profound in the absence of any other cancer symptoms
PARANEOPLASTIC SYNDROMES u Paraneoplastic syndromes are generally, but not always, irreversible
Paraneoplastic Syndromes May Affect Any Portion of the Nervous System u u u Cerebral cortex Brainstem Spinal cord Peripheral nerves Neuromuscular junction Muscle
Importance of Paraneoplastic Syndromes u Although rare, recognition by the physician is important: u Neurologic symptoms precede and prompt the diagnosis of systemic cancer in about 50% of patients u Some syndromes direct search to particular organs u In many cases the syndrome’s onset is while the cancer is small and curable

Pathogenesis u u u Onconeuronal Immunity “Tumor expression of proteins that normally are restricted to the nervous system triggers an immune response against the tumor that also affects the nervous system” Only a small amount of tumor may trigger response
Pathogenesis continued u u u Tests for antibodies against the cancerexpressed neuronal proteins Some disorders caused by antibodies u Myasthenia gravis u LEMS Other disorders most likely caused by B and T cell mechanisms of neuronal injury
Diagnosis u Paraneoplastic syndromes occur in patients: u not known to have cancer (most common) u with active cancer u in remission after treatment u exclude other cancerassociated process
Diagnosis u u u with Known Cancer Search for metastases u MRI of involved site u CSF cytology Search for nonmetastatic disorders u Vascular, infectious, metabolic disorders, chemotherapy, radiation therapy Serum/CSF for autoantibodies
Diagnosis without Known Cancer u u Exclude other causes of nervous system dysfunction Search for Cancer u CXR, pelvic examination, u mammograms, examine lymph nodes, serum cancer markers (CEA) u CSF for cells, Ig. G, OCB, cytology examination u Serum/CSF for autoantibodies u If CSF or autoantibodies positive then follow and search again
Diagnosis u Suggestive clinical features: u Subacute onset, progress over weeks to months u Severe neurologic disability u One portion of nervous system more than widespread involvement u Some syndromes present stereotypically
Diagnosis Autoantibodies u Presence of autoantibodies: u helps to confirm the clinical diagnosis u focus the search for an underlying malignancy u Anti-Hu, Anti-Yo, Anti-Ri, Anti -Tr, Anti-CV 2, etc.
Treatment u u Unrewarding in general Most patient left with severe neurologic disability Immunosuppression ineffective in most, except LEMS ? rapid onset without diagnosis or treatment before irreversible neuronal damage has occurred
Frequency of Paraneoplastic Syndromes u u “Clinically significant paraneoplastic syndromes probably occur in fewer than 1% of patients with cancer” If a patient without a known cancer presents with one of the “classic” paraneoplastic syndromes the likelihood he/she has cancer is considerable u i. e. , LEMS 60% paraneoplastic u Subacute cerebellar degeneration 50%
“Classic Paraneoplastic Syndromes” u A group of disorders, when present, strongly suggests an underlying cancer u Lambert-Eaton myasthenic syndrome (LEMS) u Opsoclonus/myoclonus found in children u Subacute cerebellar degeneration u Encephalomyelitis u Subacute motor neuronopathy u Sensory neuronopathy
“Non-classic” Paraneoplastic Syndromes u u u Second group of clinical syndromes “sometimes” associated with cancer More often appearing in the absence of a neoplasm u Polymyositis u Amyotrophic lateral sclerosis u Sensorimotor polyneuropathy Extensive search for a neoplasm is generally unwarranted
“Classic Paraneoplastic Syndromes” Specific Syndromes u u u Paraneoplastic cerebellar degeneration Most common Best characterized Rare disorder u 300 cases report by 1995 A group of related disorders that differ in clinical features, prognosis, and types of malignancies
Paraneoplastic Cerebellar Degeneration u u Disorders can be separated by characteristic antibodies to particular tumor-associated antibodies PCD can be associated with any cancer, but most common: u lung cancer (small-cell) u ovarian u uterine u lymphomas
Paraneoplastic Cerebellar Degeneration u u u Neurologic symptoms prompt patient to see doctor before cancer is symptomatic Cancer is usually found months to 2 -4 years after onset of neurologic symptoms Sometimes only at autopsy
Paraneoplastic Cerebellar Degeneration u Clinical features: u slight incoordination in walking u rapidly evolving over weeks to months with progressive gait ataxia u incoordination in arms, legs and trunk u dysarthria u nystagmus with oscillopsia
Paraneoplastic Cerebellar Degeneration u Within a few months it reaches its peak and then stabilizes u most cannot walk without support u cannot sit unsupported u handwriting is impossible u eating independently difficult u speech very difficult to understand u oscillopsia may prevent reading u diplopia & vertigo
Paraneoplastic Cerebellar Degeneration u u u Neurologic signs always bilateral, usually symmetric Deficits frequently limited to cerebellar dysfunction Other neurologic deficits (mild) u sensorineural hearing loss u dysphagia u hyperreflexia u extrapyramidal signs u peripheral neuropathy u dementia
Paraneoplastic Cerebellar Degeneration u Laboratory evaluation u diffuse cerebellar atrophy months to years after onset on head imaging u CSF (early) u increased lymphocytes u slightly elevated protein and Ig. G concentrations u Pleocytosis resolves with time
Paraneoplastic Cerebellar Degeneration u Autoantibodies in serum and CSF u found in a subset of patients u number is unknown react with Purkinje cells of cerebellum & tumor u well characterized u u anti-Yo, anti-Hu, anti-Ri, anti-Tr, anti. CV 2, anti-Ma proteins,
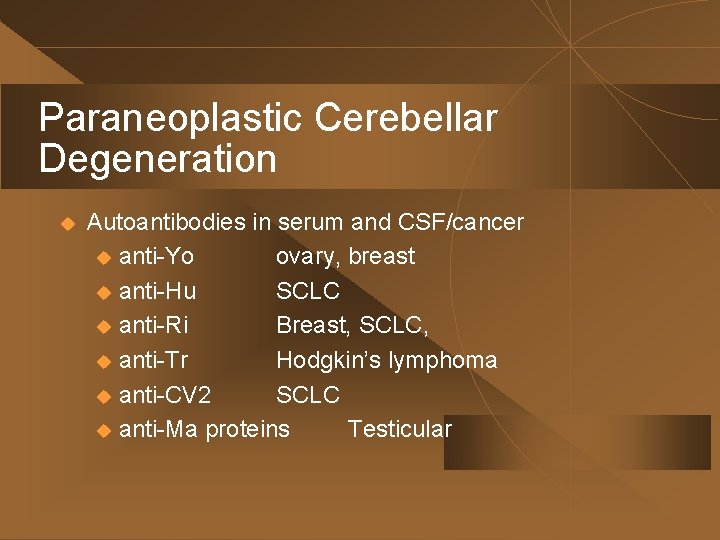
Paraneoplastic Cerebellar Degeneration u Autoantibodies in serum and CSF/cancer u anti-Yo ovary, breast u anti-Hu SCLC u anti-Ri Breast, SCLC, u anti-Tr Hodgkin’s lymphoma u anti-CV 2 SCLC u anti-Ma proteins Testicular
Paraneoplastic Cerebellar Degeneration u Pathology u CNS may be normal at autopsy u usually the cerebellum is atrophic with abnormally widened sulci and small gyri u microscopic u extensive/complete loss of Purkinje cells of the cerebellar cortex u pathologic changes sometimes involving other parts of nervous system
Paraneoplastic Cerebellar Degeneration u Diagnosis u recognize characteristic clinical syndrome u exclude other causes of late-onset cerebellopathy u Leptomeningeal metastasis u infections u toxicity of chemotherapies u viral brainstem encephalitis u demyelinating disease u Creutzfeld-Jakob disease u infarction, hypothyroidism u alcoholic and hereditary cerebellar degenerations
Paraneoplastic Cerebellar Degeneration u u Once the disease peaks it doesn’t usually change Treatment or cure of underlying cancer usually doesn’t help Immune suppression (steroids) or plasmapheresis is not effective ? clonazepam for ataxia
More “Classic” Syndromes Sensory Neuronopathy (SN) u u <20% paraneoplastic Also occurs in patients with autoimmune disorders, Sjogren’s syndrome 2/3 of paraneoplastic SN have small-cell lung cancer Neurologic syndrome usually precedes diagnosis of cancer u dysesthetic pain and numbness of distal extremities u severe sensory ataxia u all sensory modalities affected, loss of DTRs u motor nerve action potentials are normal
Subacute Motor Neuronopathy (Spinal Muscular Atrophy) u u u Rare complication of Hodgkin’s and other lymphomas Subacute, progressive, painless, patchy lower motor neuron weakness Affects legs more than arms Profound weakness Degeneration of neurons in the anterior horns of the spinal cord
Encephalomyelitis u u Cancer patients with clinical signs of damage to more than one area of the nervous system Limbic encephalitis u rare complication of small-cell lung cancer u personality/mood changes develop over days or weeks u severe impairment of recent memory u sometimes with agitation, confusion, hallucinations, & seizures u brain MRI: normal or signal changes in the medial temporal lobe(s) u may improve with treatment of underlying tumor
Opsoclonus/Myoclonus Found in Children u u Opsoclonus u involuntary, arrhythmic, multidirectional, highamplitude conjugate saccades u associated with myoclonus u may have cerebellar signs 50% of children harbor a neuroblastoma Neurologic signs precede discovery of tumor in 50% Anti-Ri antibody associated with opsoclonus
Photoreceptor Degeneration u u u Cancer-associated retinopathy (CAR) Rare syndrome Small-cell lung cancer, melanoma, gynecologic tumors Episodic visual obscurations, night blindness, lightinduced glare, photosensitivity, impaired color vision progressing to painless vision loss Typically precedes diagnosis of cancer ? prednisone
Lambert-Eaton Myasthenic Syndrome (LEMS) u u Presynaptic disorder of neuromuscular transmission Proximal weakness, areflexia or hyporeflexia, autonomic dysfunction 45% to 60% associated with SCLC, reported also with renal cell carcinoma, lymphoma and breast Syndrome precedes tumor diagnosis by several months to years
Lambert-Eaton Myasthenic Syndrome (LEMS) u u u Onset with proximal lower extremity weakness Later proximal upper extremity weakness Respiratory and craniobulbar involvement uncommon Autonomic dysfunction prominent u dry mouth, dry eyes, impotence, orthostatic hypotension, hyperhidrosis Facilitation with sustained contraction >100% CMAP increase with repetitive stimulation
Lambert-Eaton Myasthenic Syndrome (LEMS) u u >92% with antibodies against P/Q-type voltage-gated calcium channels (presynaptic) Impaired influx of calcium into nerve terminal with reduced neuromuscular junction transmission A LEMS diagnosis warrants a thorough investigation for underlying carcinoma, SCLC Careful observation and serial evaluations until tumor found
Lambert-Eaton Myasthenic Syndrome (LEMS) u u Unlike most paraneoplastic syndromes LEMS usually responds to: u plasmapheresis u corticosteroids u azathioprine u intravenous immunoglobin Long-term treatment often needed

Summary u u Paraneoplastic syndromes are rare Often precede the diagnosis of cancer Thought to result from cross-reactivity of antibodies to a common antigen within tumor and nervous tumor Disability persists despite treatment of underlying tumor
 Dr steven gerhardt
Dr steven gerhardt Acnthosis
Acnthosis Martin gerhardt
Martin gerhardt Maniobra de yodice
Maniobra de yodice Bert gerhardt
Bert gerhardt Differential diagnosis of stroke
Differential diagnosis of stroke Post castration syndrome gynecology
Post castration syndrome gynecology Nemeskéri ágnes szövettan
Nemeskéri ágnes szövettan What is geriatric syndromes
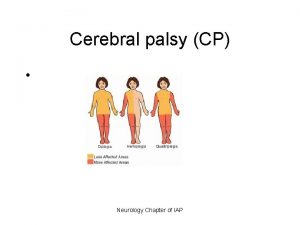
What is geriatric syndromes Cerebellar syndromes
Cerebellar syndromes Neuroendocrine syndrome in gynecology
Neuroendocrine syndrome in gynecology The walton centre for neurology and neurosurgery
The walton centre for neurology and neurosurgery Tufts anesthesiology residency
Tufts anesthesiology residency Dr raeburn
Dr raeburn Neurology sonography
Neurology sonography Monomyth amplification
Monomyth amplification Neurology
Neurology Nheent
Nheent Nlff neurology
Nlff neurology Neuro exam strength
Neuro exam strength Difference between fine touch and crude touch
Difference between fine touch and crude touch Dr bajaj neurologist
Dr bajaj neurologist Robert layzer md
Robert layzer md Neurology
Neurology Oregon neurology associates
Oregon neurology associates Umass pharmacy residency
Umass pharmacy residency Rachel ditrapani md
Rachel ditrapani md Dr kirk kleinfeld
Dr kirk kleinfeld Uf neurology residency
Uf neurology residency Joseph berger md neurology
Joseph berger md neurology Surgery shelf percentiles
Surgery shelf percentiles Neurology near loomis
Neurology near loomis Midwest neurology
Midwest neurology Department of neurology
Department of neurology Mary bridge pediatric neurology
Mary bridge pediatric neurology Mayzent fdo
Mayzent fdo Midwest neurology
Midwest neurology Contrallateral
Contrallateral Rrerl
Rrerl Steven rudich
Steven rudich Russell kahn
Russell kahn Steven rochford
Steven rochford