SYNDROMES MASQUERADING AS INFECTIONS Syndromes that masquerade as











- Slides: 53
SYNDROMES MASQUERADING AS INFECTIONS

Syndromes that masquerade as infections • We will tackle questions and cases • Fever is often a presenting symptom • Or can present in a way that is similar to an infectious syndrome like pneumonia, cellulitis, wound infection, or septic arthritis • There are many; we will cover a few today
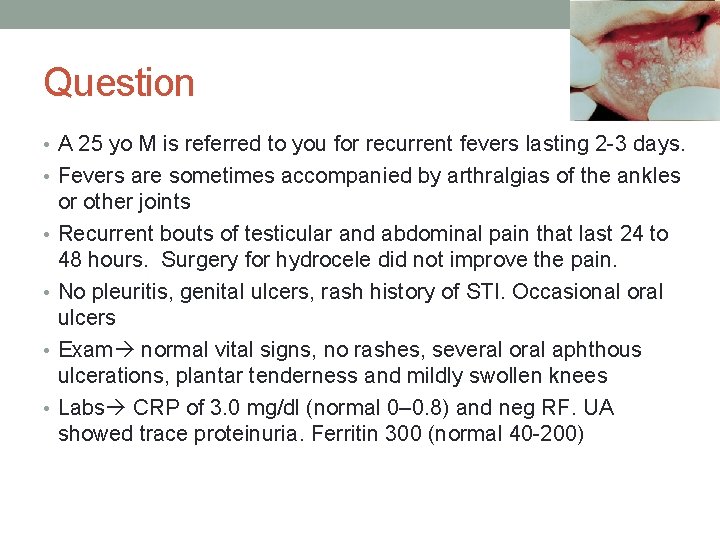
Question • A 25 yo M is referred to you for recurrent fevers lasting 2 -3 days. • Fevers are sometimes accompanied by arthralgias of the ankles • • or other joints Recurrent bouts of testicular and abdominal pain that last 24 to 48 hours. Surgery for hydrocele did not improve the pain. No pleuritis, genital ulcers, rash history of STI. Occasional oral ulcers Exam normal vital signs, no rashes, several oral aphthous ulcerations, plantar tenderness and mildly swollen knees Labs CRP of 3. 0 mg/dl (normal 0– 0. 8) and neg RF. UA showed trace proteinuria. Ferritin 300 (normal 40 -200)

Question • The most likely diagnosis is • A. Familial Mediterranean Fever • B. Adult Still’s Disease • C. Kikuchi’s Disease • D. Behcet’s disease
Question • The most likely diagnosis is • A. Familial Mediterranean Fever • B. Adult Still’s Disease • C. Kikuchi’s Disease • D. Behcet’s disease
Familial Mediterranean Fever • Autosomal recessive • Occurs primarily in Jews, Armenians, Turks, Arabs in the Mediterranean basin, central Asia, and Japan • Can occur at any age, but 80% of cases occur before age of 20 • M: F 1. 5 -2 • Episodic attacks • last from 24 -72 hours • Moderate to high fever • Painful serositis including abdominal pain • Mutation in MEFV gene leading to alteration in pyrin protein • Treatment: colchicine
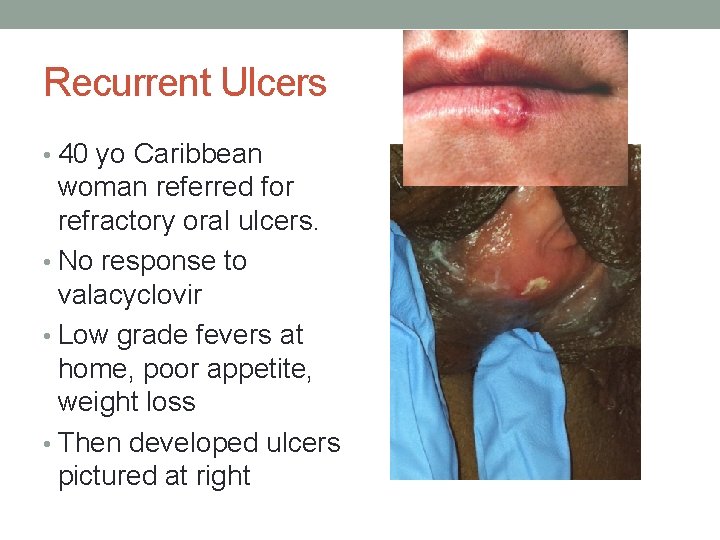
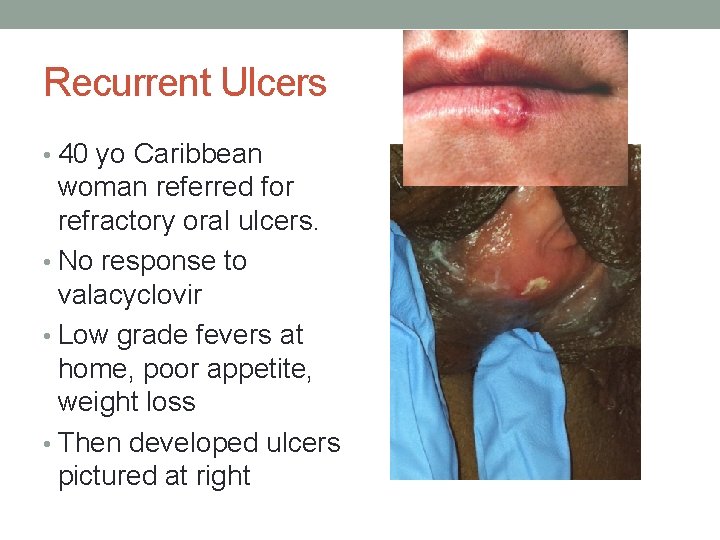
Recurrent Ulcers • 40 yo Caribbean woman referred for refractory oral ulcers. • No response to valacyclovir • Low grade fevers at home, poor appetite, weight loss • Then developed ulcers pictured at right
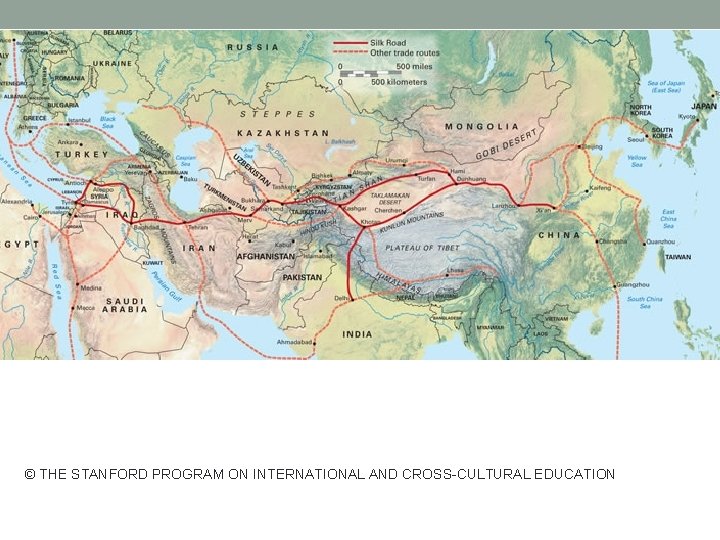
© THE STANFORD PROGRAM ON INTERNATIONAL AND CROSS-CULTURAL EDUCATION
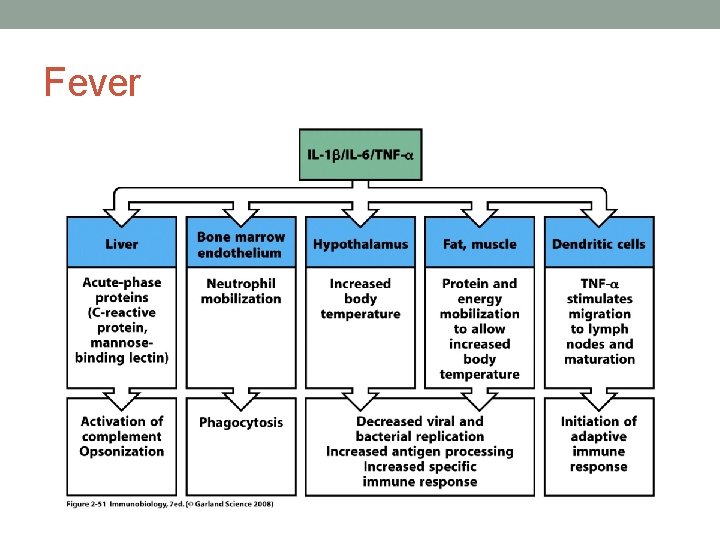
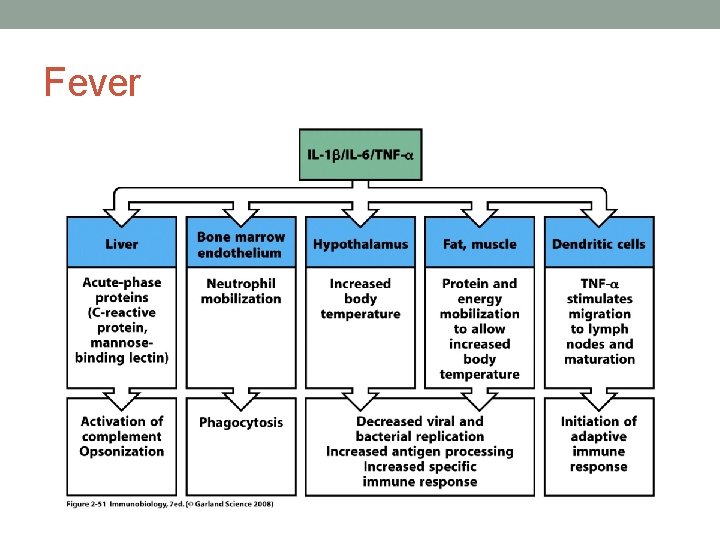
Fever
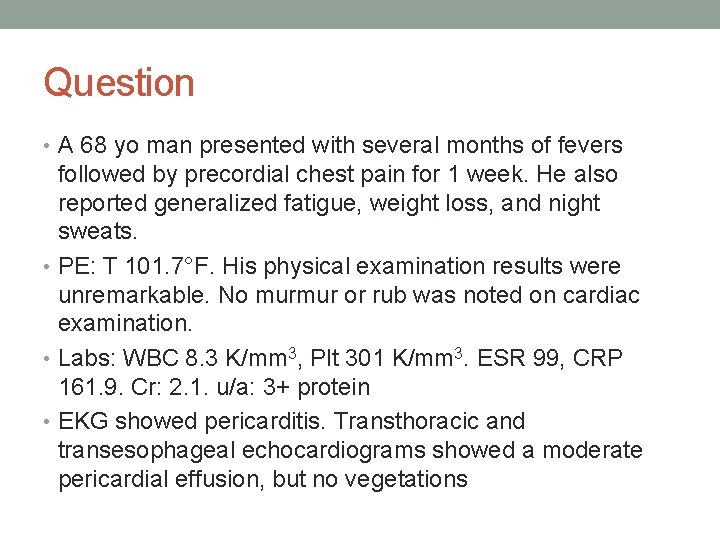
Question • A 68 yo man presented with several months of fevers followed by precordial chest pain for 1 week. He also reported generalized fatigue, weight loss, and night sweats. • PE: T 101. 7°F. His physical examination results were unremarkable. No murmur or rub was noted on cardiac examination. • Labs: WBC 8. 3 K/mm 3, Plt 301 K/mm 3. ESR 99, CRP 161. 9. Cr: 2. 1. u/a: 3+ protein • EKG showed pericarditis. Transthoracic and transesophageal echocardiograms showed a moderate pericardial effusion, but no vegetations
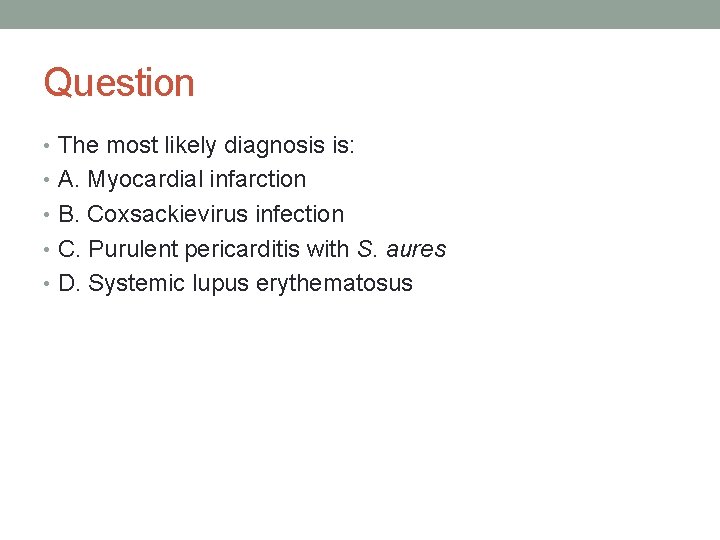
Question • The most likely diagnosis is: • A. Myocardial infarction • B. Coxsackievirus infection • C. Purulent pericarditis with S. aures • D. Systemic lupus erythematosus
Question • The most likely diagnosis is: • A. Myocardial infarction • B. Coxsackievirus infection • C. Purulent pericarditis with S. aureus • D. Systemic lupus erythematosus Antinuclear antibody titer was 1: 340 (n = <1: 40) and an anti –double-stranded DNA titer was 1: 640
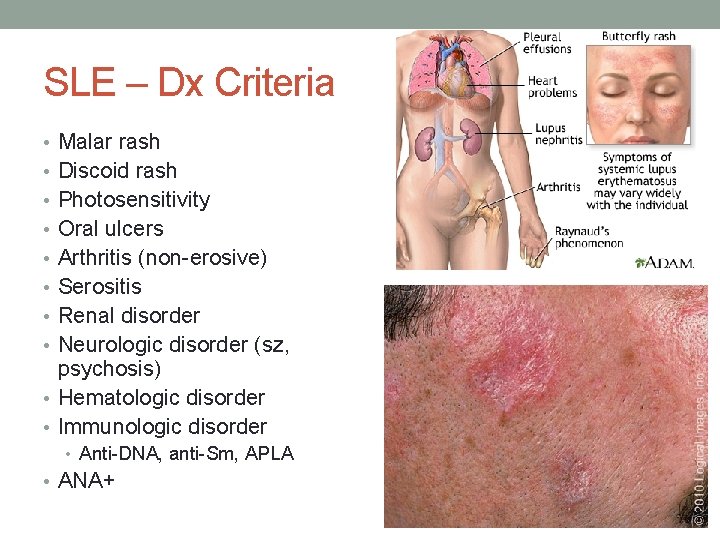
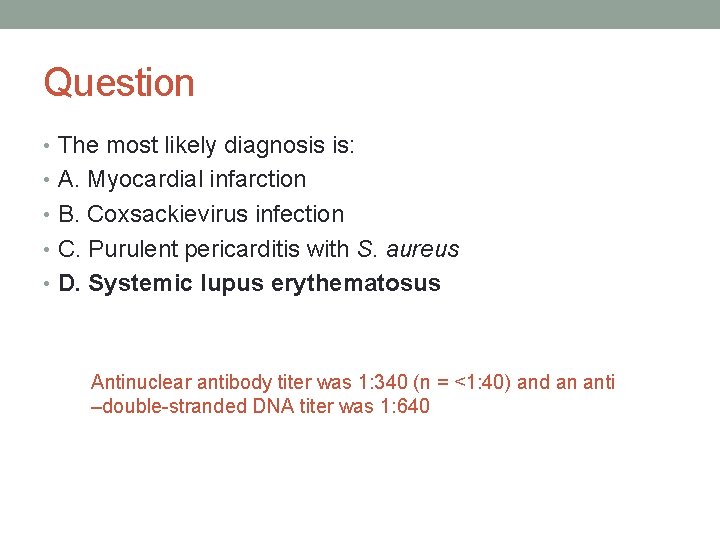
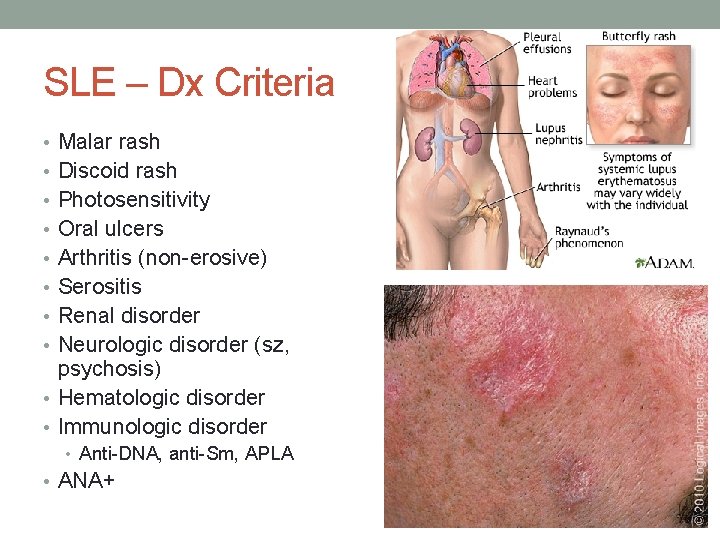
SLE – Dx Criteria • Malar rash • Discoid rash • Photosensitivity • Oral ulcers • Arthritis (non-erosive) • Serositis • Renal disorder • Neurologic disorder (sz, psychosis) • Hematologic disorder • Immunologic disorder • Anti-DNA, anti-Sm, APLA • ANA+
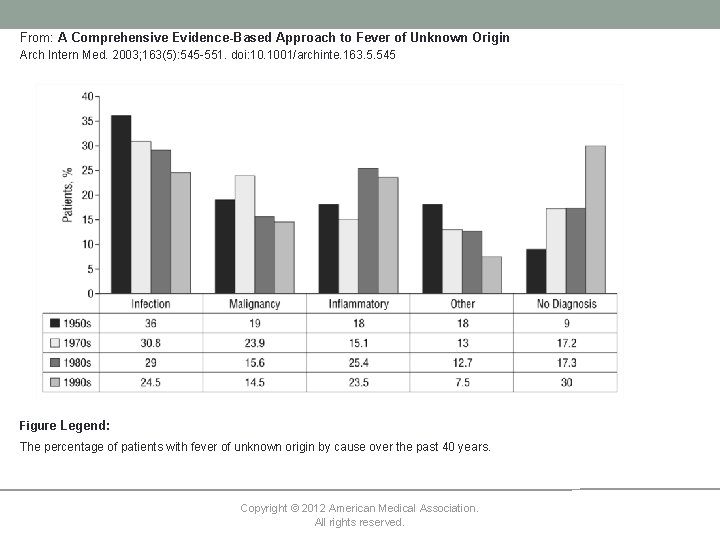
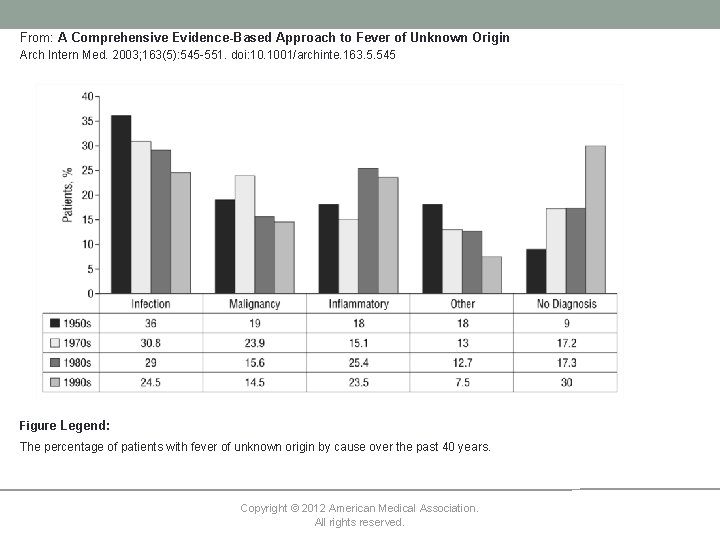
From: A Comprehensive Evidence-Based Approach to Fever of Unknown Origin Arch Intern Med. 2003; 163(5): 545 -551. doi: 10. 1001/archinte. 163. 5. 545 Figure Legend: The percentage of patients with fever of unknown origin by cause over the past 40 years. Copyright © 2012 American Medical Association. All rights reserved.
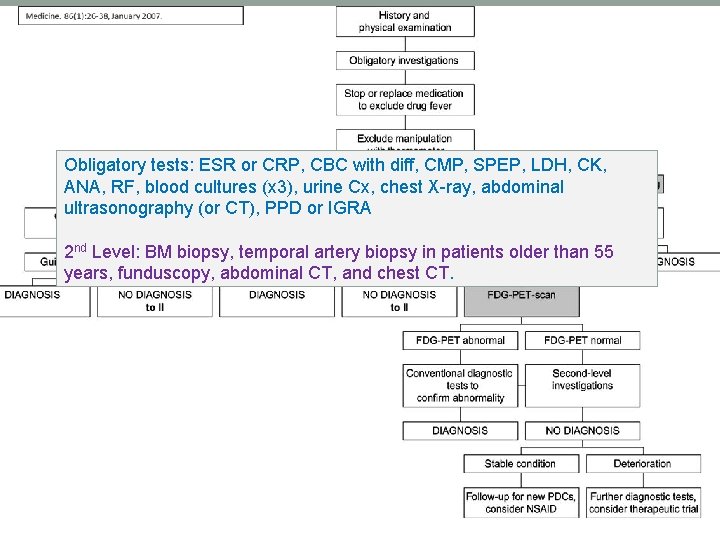
• What is the workup for FUO?
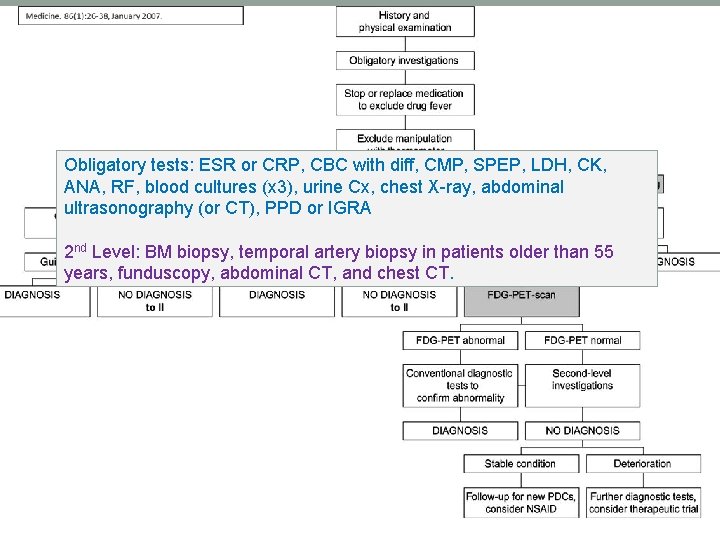
Obligatory tests: ESR or CRP, CBC with diff, CMP, SPEP, LDH, CK, ANA, RF, blood cultures (x 3), urine Cx, chest X-ray, abdominal ultrasonography (or CT), PPD or IGRA 2 nd Level: BM biopsy, temporal artery biopsy in patients older than 55 years, funduscopy, abdominal CT, and chest CT.
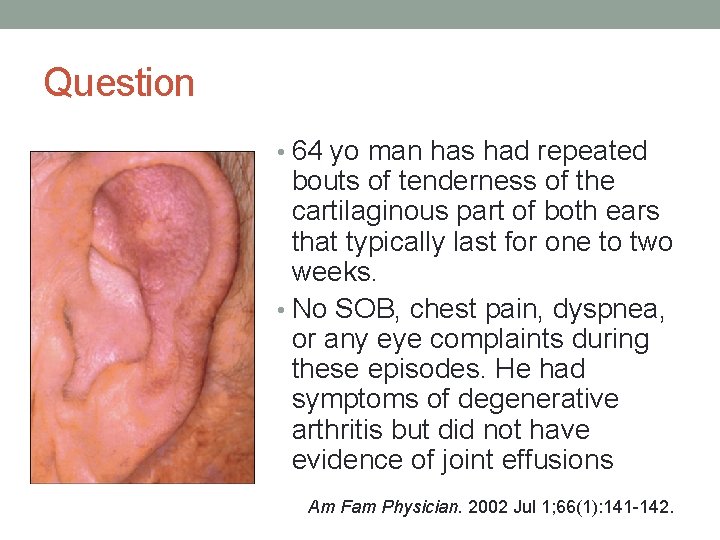
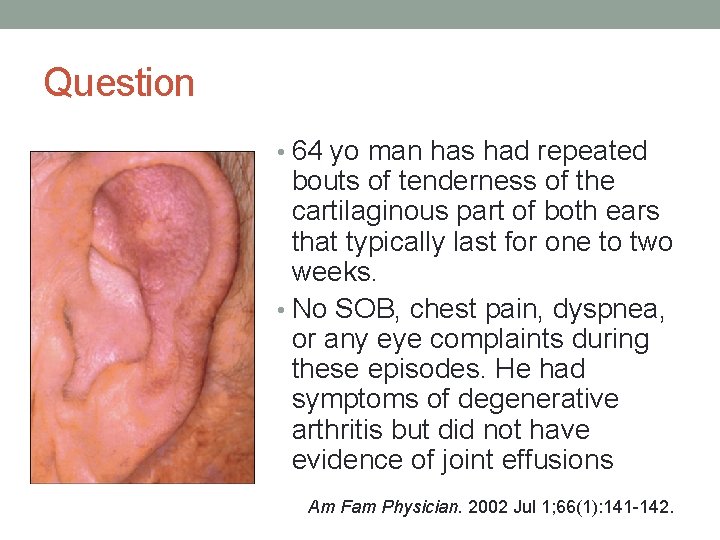
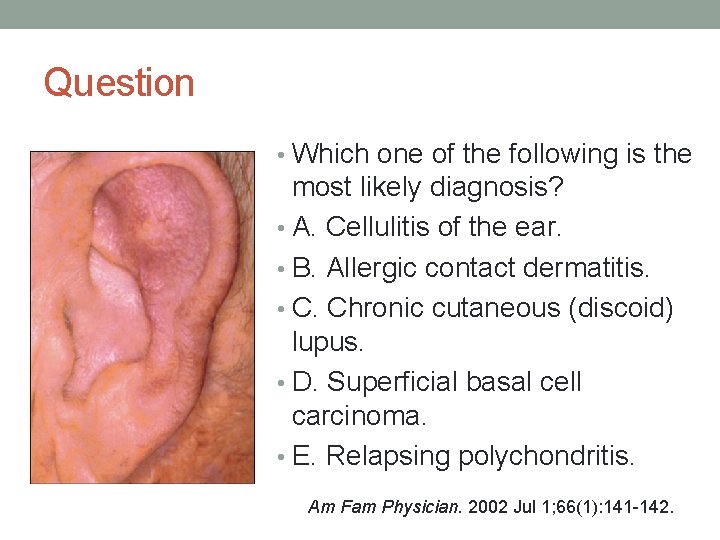
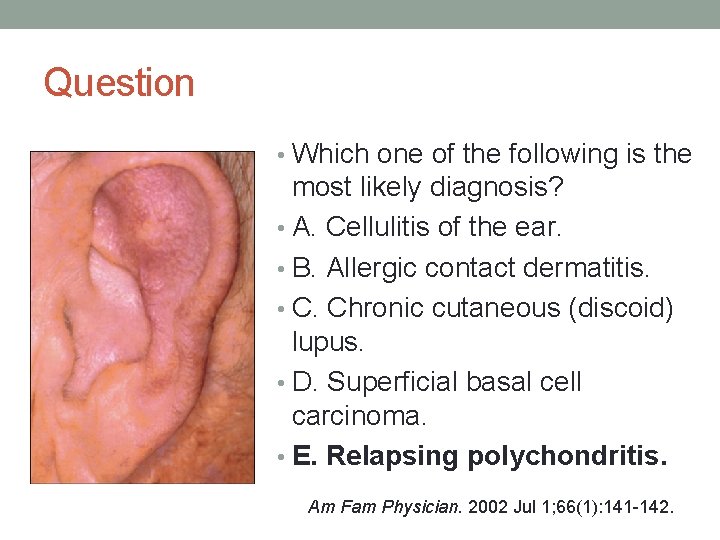
Question • 64 yo man has had repeated bouts of tenderness of the cartilaginous part of both ears that typically last for one to two weeks. • No SOB, chest pain, dyspnea, or any eye complaints during these episodes. He had symptoms of degenerative arthritis but did not have evidence of joint effusions Am Fam Physician. 2002 Jul 1; 66(1): 141 -142.
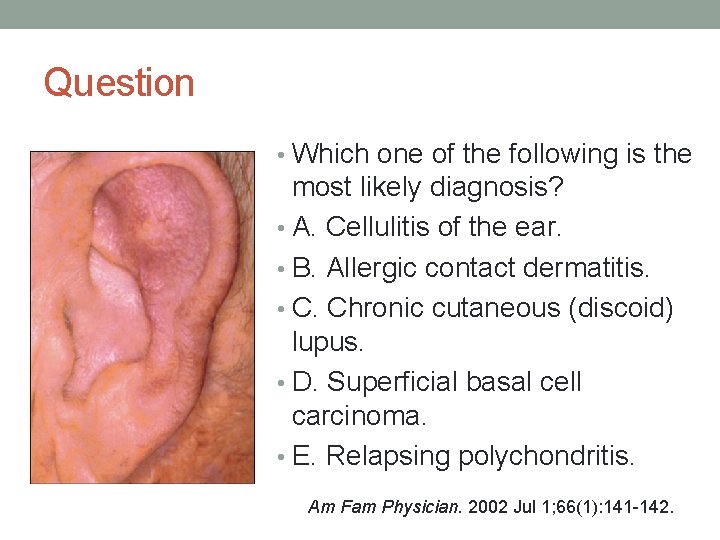
Question • Which one of the following is the most likely diagnosis? • A. Cellulitis of the ear. • B. Allergic contact dermatitis. • C. Chronic cutaneous (discoid) lupus. • D. Superficial basal cell carcinoma. • E. Relapsing polychondritis. Am Fam Physician. 2002 Jul 1; 66(1): 141 -142.
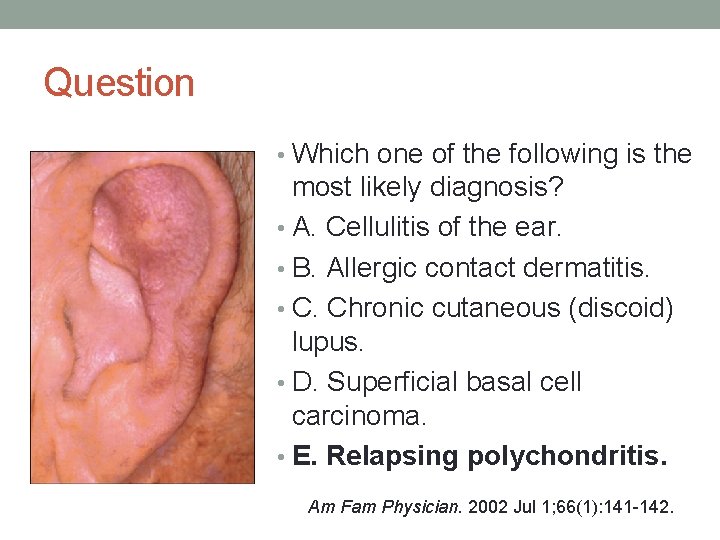
Question • Which one of the following is the most likely diagnosis? • A. Cellulitis of the ear. • B. Allergic contact dermatitis. • C. Chronic cutaneous (discoid) lupus. • D. Superficial basal cell carcinoma. • E. Relapsing polychondritis. Am Fam Physician. 2002 Jul 1; 66(1): 141 -142.

www. uptodate. com www. nejm. org
Relapsing Polychondritis • Systemic inflammatory process that affects cartilage • Can involve • Ears (auricular chondritis) • Joints (nonerosive, seronegative inflammatory polyarthritis) • Nose (nasal chondritis) • Eyes (conjunctivitis, keratitis, scleritis/episcleritis, uveitis) • Respiratory tract chondritis (laryngeal and/or tracheal cartilages) • Ears/vestibular system (neurosensory hearing loss, tinnitus, and/or vertigo) • Heart (valvular disease) • Clinical diagnostic criteria • Occurs in all races and groups, male = female • Treated with glucocorticoids, other immunosuppressants
Saddle Nose Deformity • Syphilis • Lepromatous leprosy • Relapsing polychondritis • Granulomatosis with polyangiitis (Wegner’s granlulomatosis) • Cocaine abuse

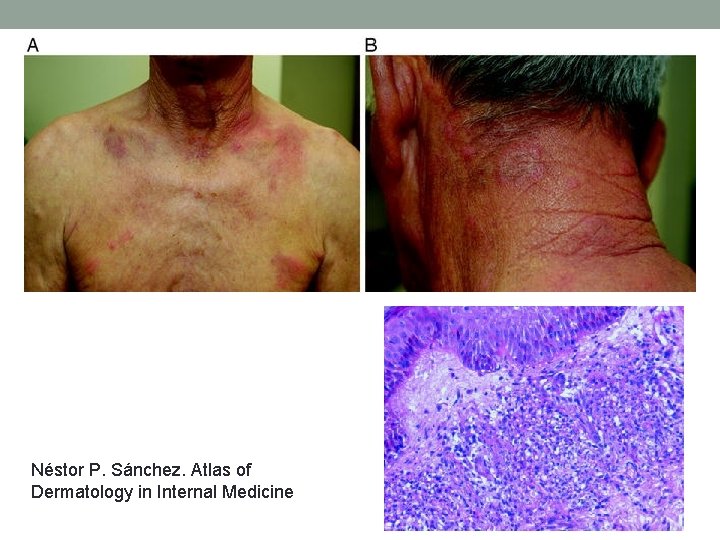
Question • A 54 yo man with a history of laryngeal cancer was admitted to the hospital for evaluation of fever and of a painful, erythematous eruption on back and chest. The patient denied any recent trauma, travel, gardening, or exposure to animals. No recent chemotherapy or radiation treatments. • PE T 101. 4, well demarcated, ecchymotic, tender, plaques were noted on back and chest, neck. • Labs WBC 13 k (86% PMN), Plt 404, Cr 1. 3. • The patient was given broad-spectrum antibiotics, but his condition did not improve.
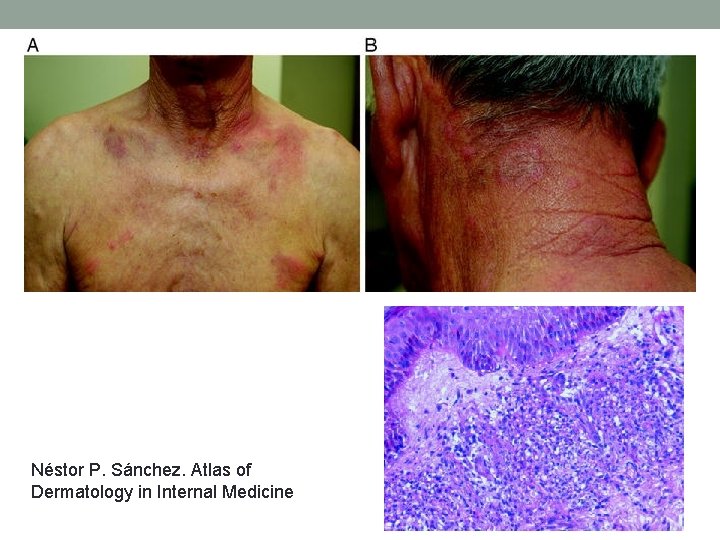
Néstor P. Sánchez. Atlas of Dermatology in Internal Medicine

Question • The most likely diagnosis is: • A. Sweet’s syndrome • B. Drug eruption • C. Dermatomyositis • D. HSV
Question • The most likely diagnosis is: • A. Sweet’s syndrome • B. Drug eruption • C. Dermatomyositis • D. HSV
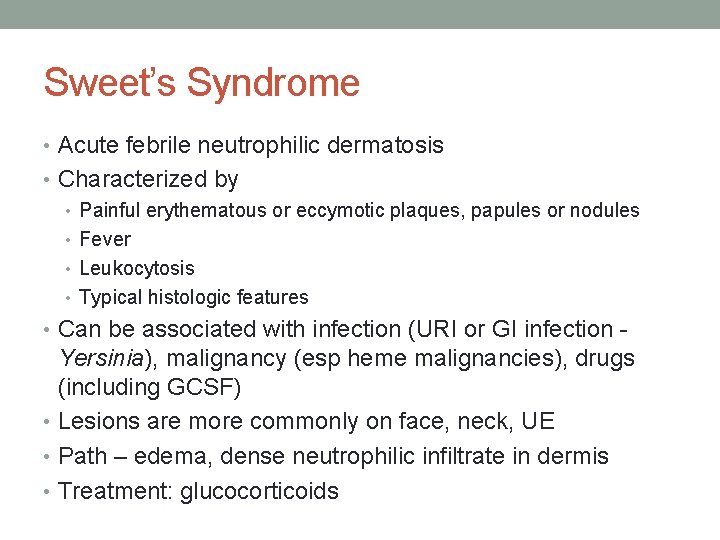
Sweet’s Syndrome • Acute febrile neutrophilic dermatosis • Characterized by • Painful erythematous or eccymotic plaques, papules or nodules • Fever • Leukocytosis • Typical histologic features • Can be associated with infection (URI or GI infection - Yersinia), malignancy (esp heme malignancies), drugs (including GCSF) • Lesions are more commonly on face, neck, UE • Path – edema, dense neutrophilic infiltrate in dermis • Treatment: glucocorticoids
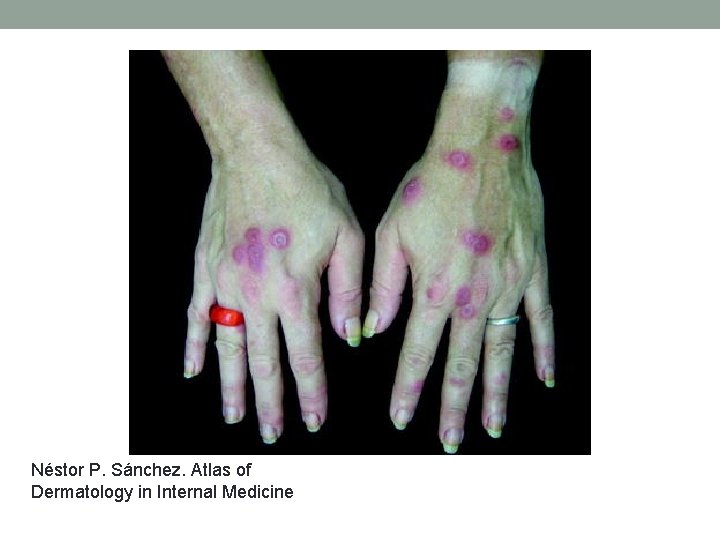
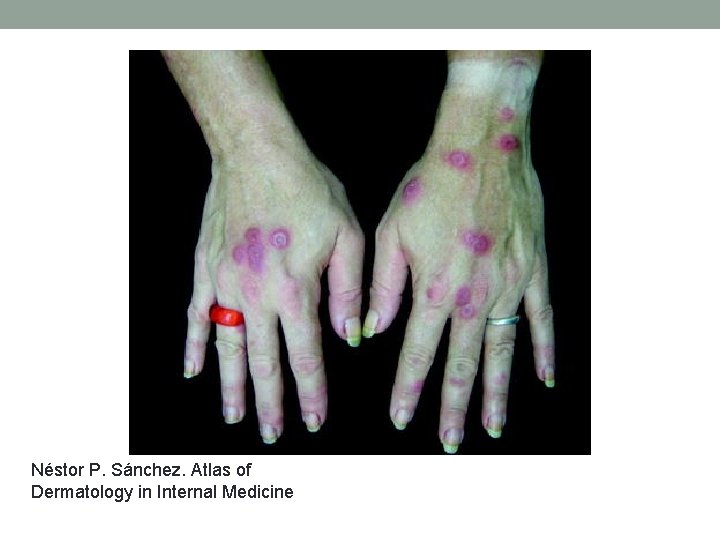
Néstor P. Sánchez. Atlas of Dermatology in Internal Medicine


Dermatomyositis http: //dermatlas. med. jhmi. edu Am Fam Physician. 2002 Oct 1; 66(7): 1285 -1286.

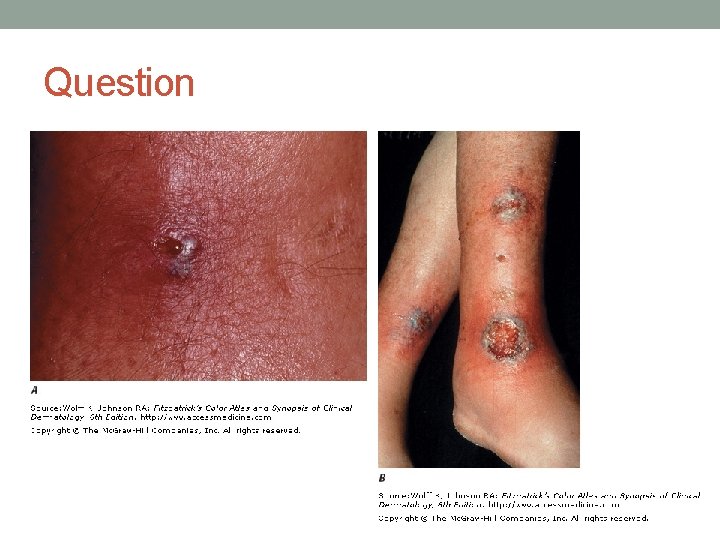
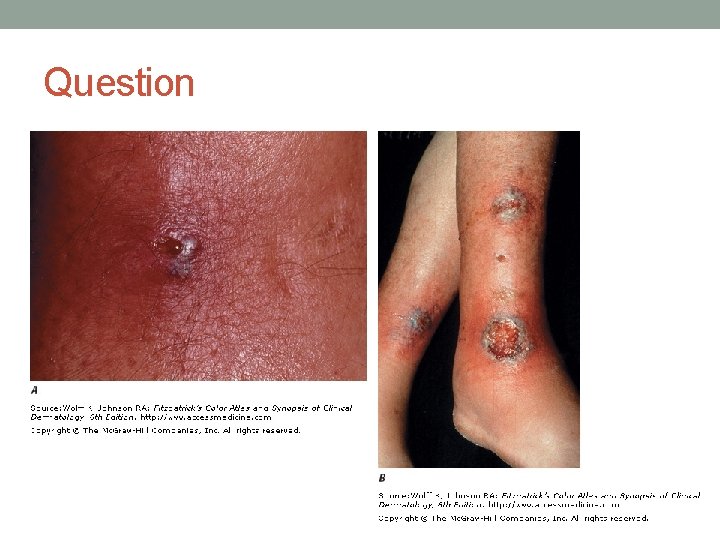
Question • These skin lesions are associated with: • A. Amyloidosis • B. Ulcerative colitis • C. Vibrio species infection • D. Cryptococcal infection
Question
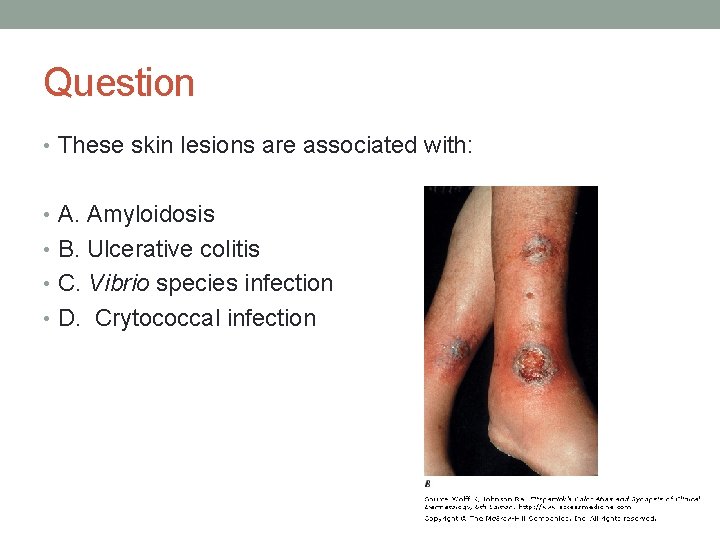
Question • These skin lesions are associated with: • A. Amyloidosis • B. Ulcerative colitis • C. Vibrio species infection • D. Crytococcal infection
Question • These skin lesions are associated with: • A. Amyloidosis • B. Ulcerative colitis • C. Vibrio species infection • D. Crytococcal infection
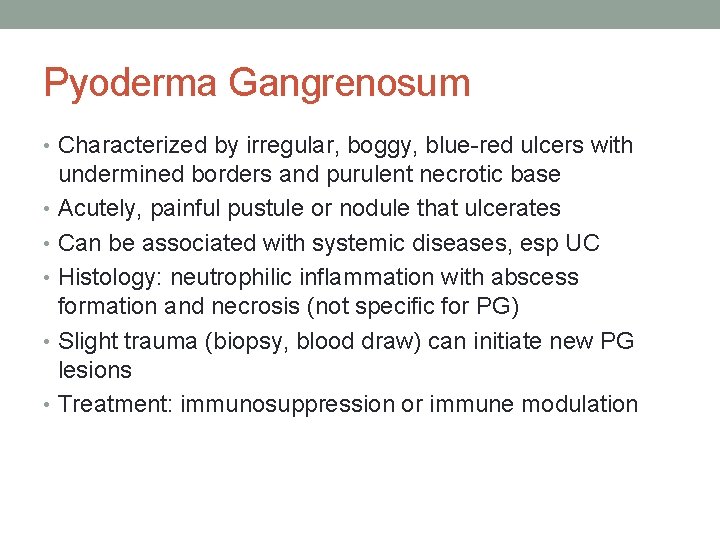
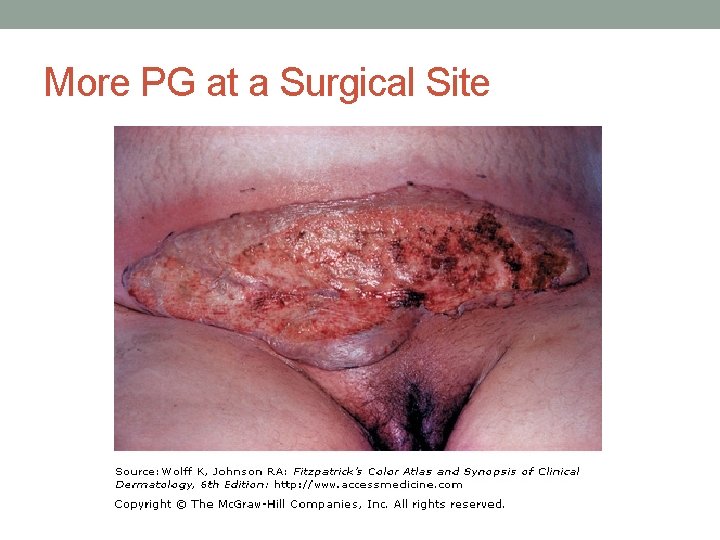
Pyoderma Gangrenosum • Characterized by irregular, boggy, blue-red ulcers with undermined borders and purulent necrotic base • Acutely, painful pustule or nodule that ulcerates • Can be associated with systemic diseases, esp UC • Histology: neutrophilic inflammation with abscess formation and necrosis (not specific for PG) • Slight trauma (biopsy, blood draw) can initiate new PG lesions • Treatment: immunosuppression or immune modulation

http: //dermatlas. med. jhmi. edu
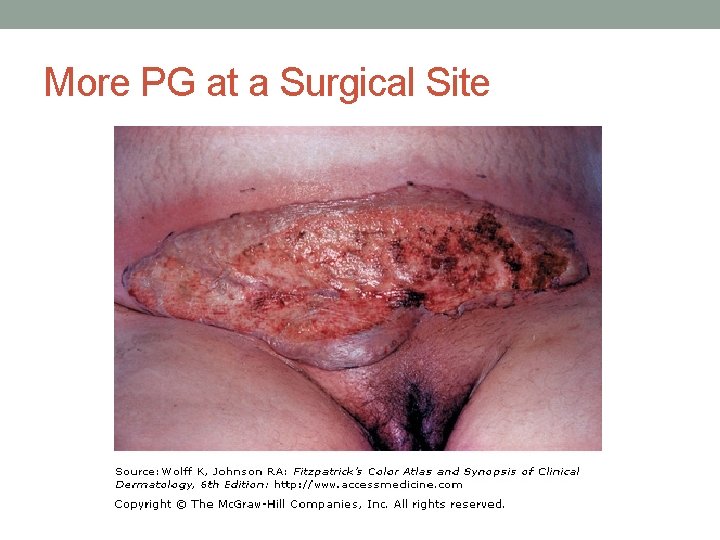
More PG at a Surgical Site

Question • A 45 yo W is evaluated for a 2 -month history of fatigue, nonproductive cough, decreased appetite, intermittent fever, RUQ pain, and a 4. 5 -kg (10. 0 -lb) weight loss. • PE T 37. 8°C (100. 0°F), BP 104/68, HR 100/min, and RR 16, BMI 28. Several erythematous 5 - to 10 -mm maculopapular lesions on face. Cardiopulm normal, Hepatomegaly. B/L inguinal LAD • Labs: • hgbn 12. 2 g/d. L; phos 4. 0 mg/d. L; ca 11. 2 mg/d. L, Cr, 2. 0 mg/d. L • urinalysis, 1+ protein; 20 leukocytes/hpf • PPD negative. Urine cx negative • Chest radiograph shows bilateral hilar lymphadenopathy. Renal u/s: rt kidney is 13. 7 cm and lt kidney is 15. 4 cm. No hydro, no stones Ann Intern Med. 01 May 2012; 156(9): ITC 5 -1 http: //dermatlas. med. jhmi. edu
Question • Which of the following is the most likely diagnosis? • A. Amyloidosis • B. Sarcoidosis • C. The Sjögren syndrome • D. Systemic lupus erythematosus Ann Intern Med. 01 May 2012; 156(9): ITC 5 -1
Question • Which of the following is the most likely diagnosis? • A. Amyloidosis • B. Sarcoidosis • C. The Sjögren syndrome • D. Systemic lupus erythematosus Ann Intern Med. 01 May 2012; 156(9): ITC 5 -1
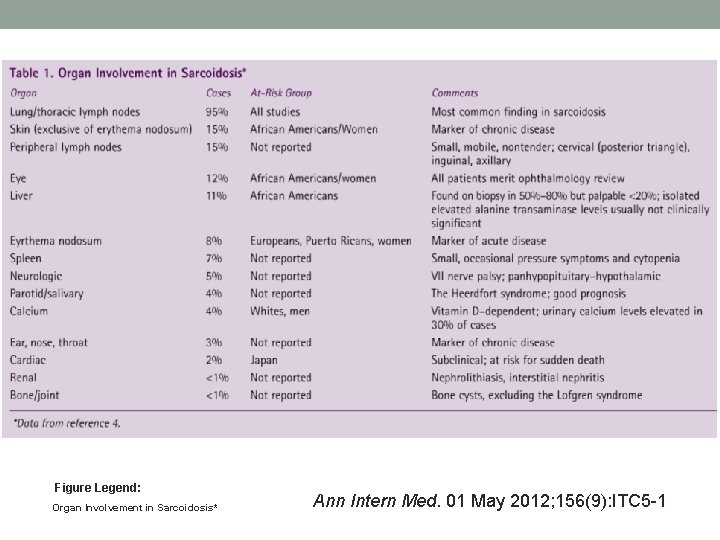
Sarcoidosis • Idiopathic granulomatous disease • Can affect any organ • In the US, more common in African Americans • Common presenting signs and symptoms: cough, fever and weight loss, chest pain, painful ankle swelling, painful nodules on shins, eye pain • Variable clinical course • Clinical features, imaging, histopathology contribute to the diagnosis • Treatment: prednisone
Question • A 21 yo man is evaluated for a 5 -day history of pain and swelling in the right ankle. 7 days ago, he developed a nodule on the left leg. He has no history of trauma to either of these sites. • PE: VS are normal. The right ankle is warm and swollen, and range of motion elicits pain. He also has a warm, firm, 2 -cm erythematous nodule over the anterior left lower extremity that is tender to palpation and has been present for 7 days. • A plain x-ray of the right ankle is normal. • Arthrocentesis of the right ankle is performed, and synovial fluid analysis reveals a leukocyte count of 3000/μL (80% lymphocytes, 12% macrophages). No crystals.
Question • Which of the following is the most likely diagnosis? • A. Bacterial arthritis • B. Crystal-induced arthritis • C. Osteoarthritis • D. Sarcoidosis

Question • Which of the following is the most likely diagnosis? • A. Bacterial arthritis • B. Crystal-induced arthritis • C. Osteoarthritis • D. Sarcoidosis • Lofgren syndrome: acute monoarticular arthritis (ankles typically), erythema nodusum, and hilar LAD.
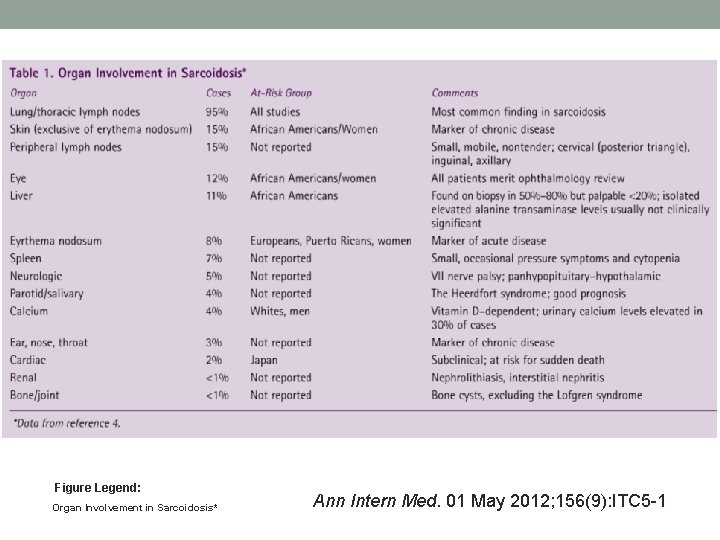
Figure Legend: Organ Involvement in Sarcoidosis* Ann Intern Med. 01 May 2012; 156(9): ITC 5 -1
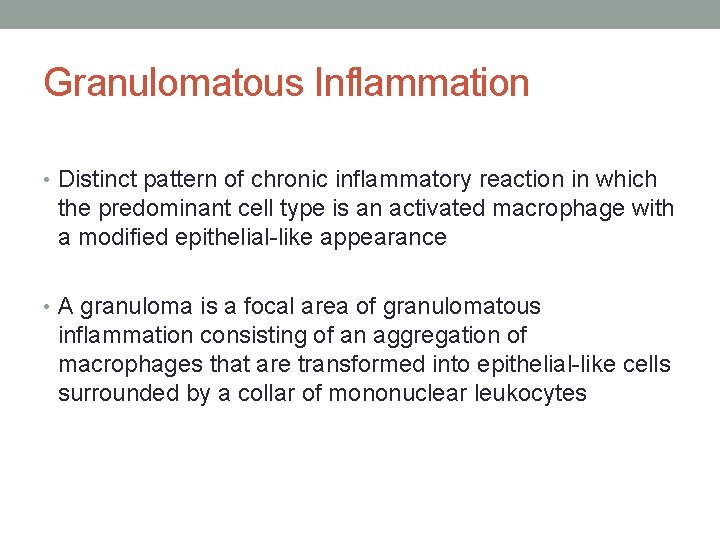
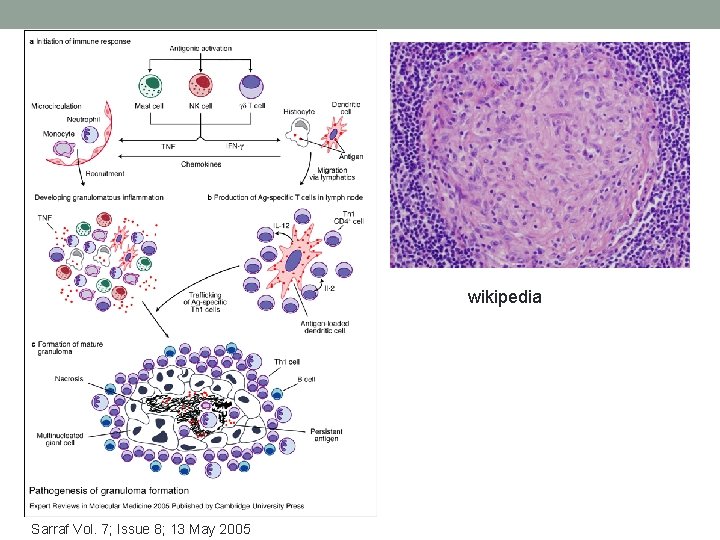
Granulomatous Inflammation • Distinct pattern of chronic inflammatory reaction in which the predominant cell type is an activated macrophage with a modified epithelial-like appearance • A granuloma is a focal area of granulomatous inflammation consisting of an aggregation of macrophages that are transformed into epithelial-like cells surrounded by a collar of mononuclear leukocytes
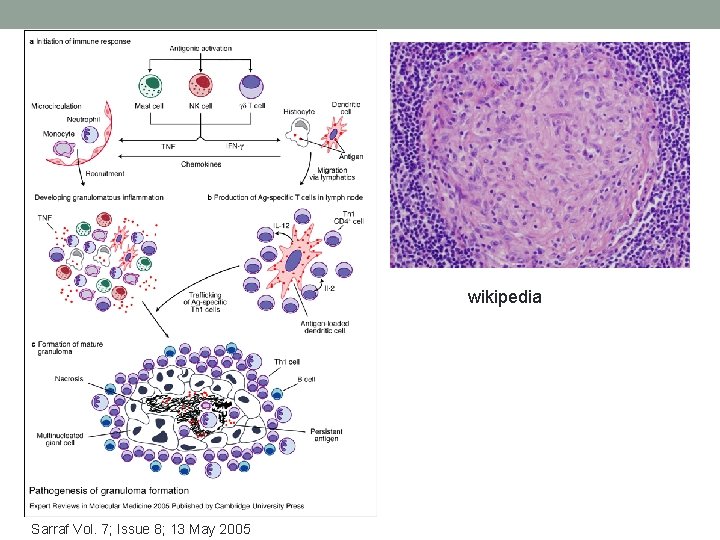
wikipedia Sarraf Vol. 7; Issue 8; 13 May 2005
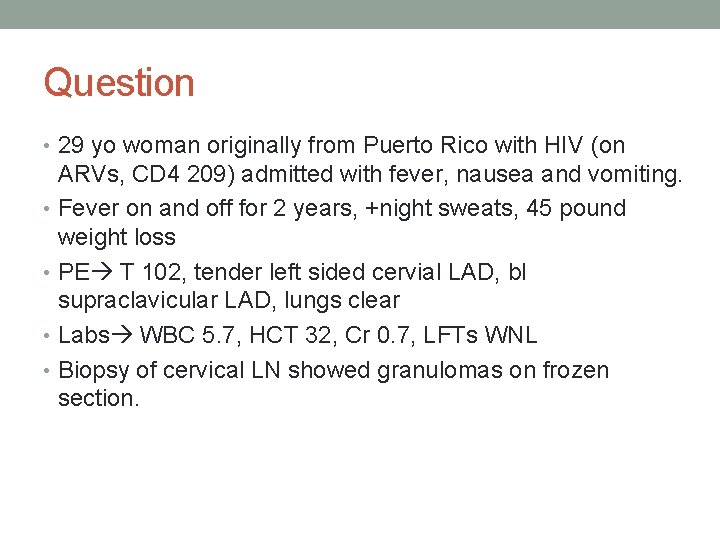
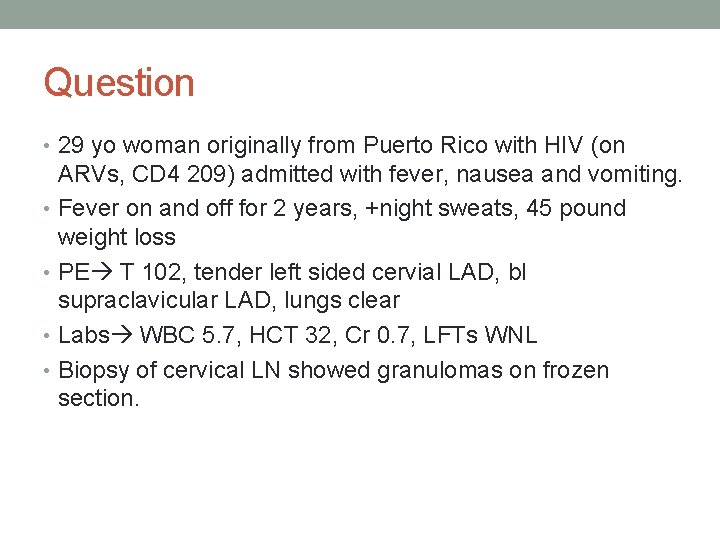
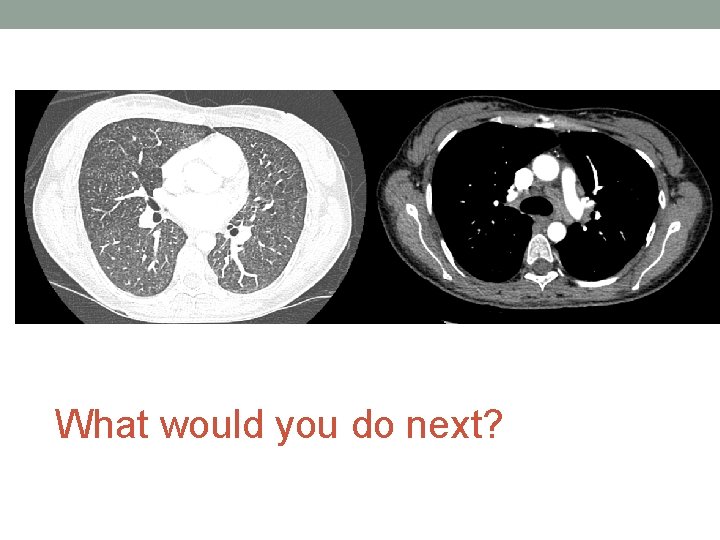
Question • 29 yo woman originally from Puerto Rico with HIV (on ARVs, CD 4 209) admitted with fever, nausea and vomiting. • Fever on and off for 2 years, +night sweats, 45 pound weight loss • PE T 102, tender left sided cervial LAD, bl supraclavicular LAD, lungs clear • Labs WBC 5. 7, HCT 32, Cr 0. 7, LFTs WNL • Biopsy of cervical LN showed granulomas on frozen section.
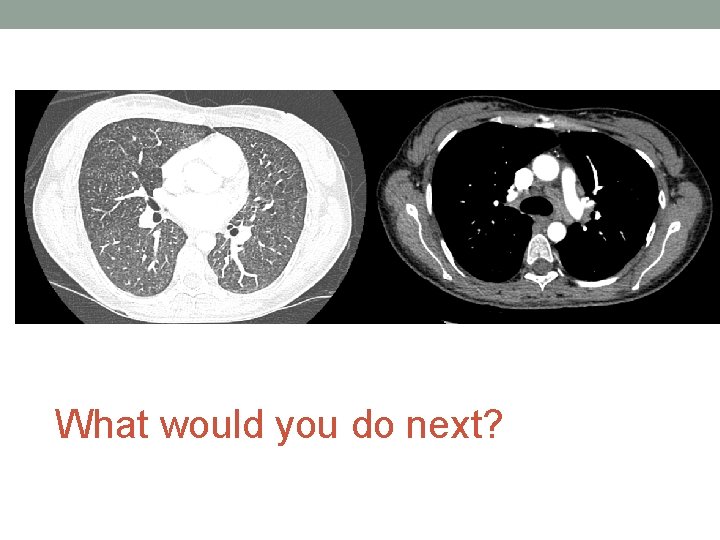
What would you do next?
• Team started empiric TB treatment • Final path: lymph nodes with necrotizing granulomas • GMS stain showed small budding yeast • Culture positive for fungi at 10 days that ultimately grew Histoplasma capsulatum.
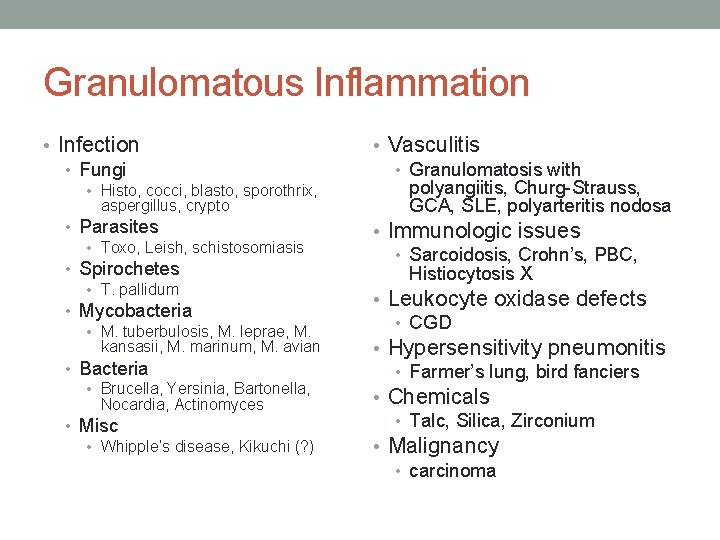
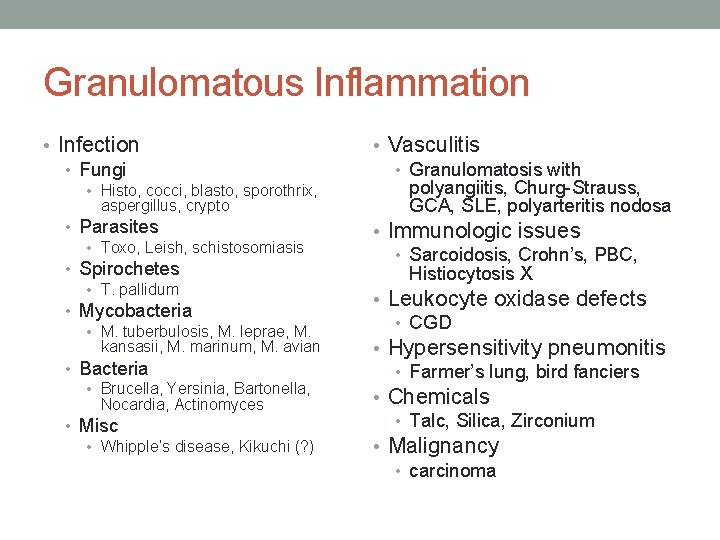
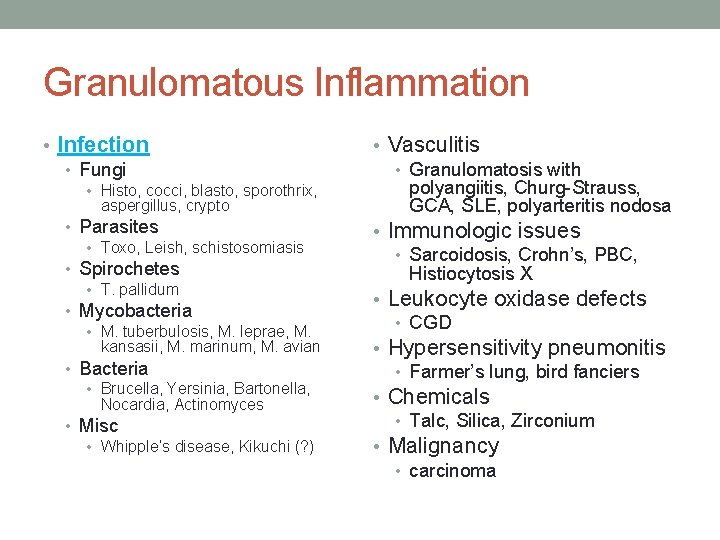
Granulomatous Inflammation • Infection • Fungi • Histo, cocci, blasto, sporothrix, aspergillus, crypto • Parasites • Toxo, Leish, schistosomiasis • Spirochetes • T. pallidum • Mycobacteria • M. tuberbulosis, M. leprae, M. kansasii, M. marinum, M. avian • Bacteria • Brucella, Yersinia, Bartonella, Nocardia, Actinomyces • Misc • Whipple’s disease, Kikuchi (? ) • Vasculitis • Granulomatosis with polyangiitis, Churg-Strauss, GCA, SLE, polyarteritis nodosa • Immunologic issues • Sarcoidosis, Crohn’s, PBC, Histiocytosis X • Leukocyte oxidase defects • CGD • Hypersensitivity pneumonitis • Farmer’s lung, bird fanciers • Chemicals • Talc, Silica, Zirconium • Malignancy • carcinoma
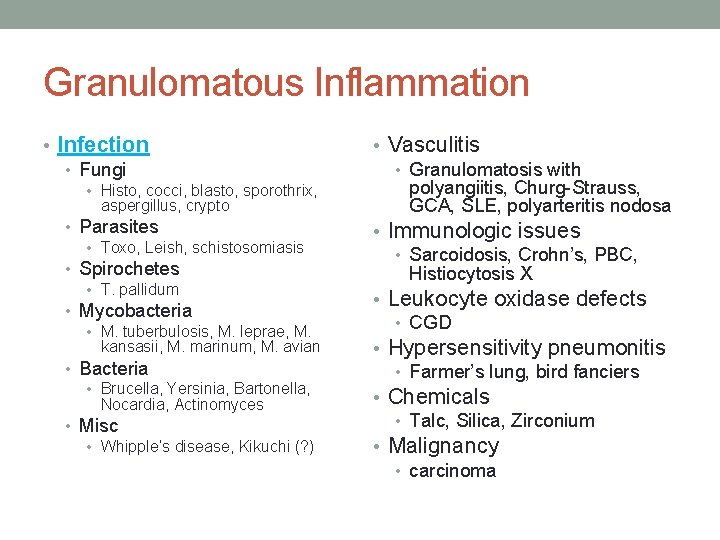
Granulomatous Inflammation • Infection • Fungi • Histo, cocci, blasto, sporothrix, aspergillus, crypto • Parasites • Toxo, Leish, schistosomiasis • Spirochetes • T. pallidum • Mycobacteria • M. tuberbulosis, M. leprae, M. kansasii, M. marinum, M. avian • Bacteria • Brucella, Yersinia, Bartonella, Nocardia, Actinomyces • Misc • Whipple’s disease, Kikuchi (? ) • Vasculitis • Granulomatosis with polyangiitis, Churg-Strauss, GCA, SLE, polyarteritis nodosa • Immunologic issues • Sarcoidosis, Crohn’s, PBC, Histiocytosis X • Leukocyte oxidase defects • CGD • Hypersensitivity pneumonitis • Farmer’s lung, bird fanciers • Chemicals • Talc, Silica, Zirconium • Malignancy • carcinoma
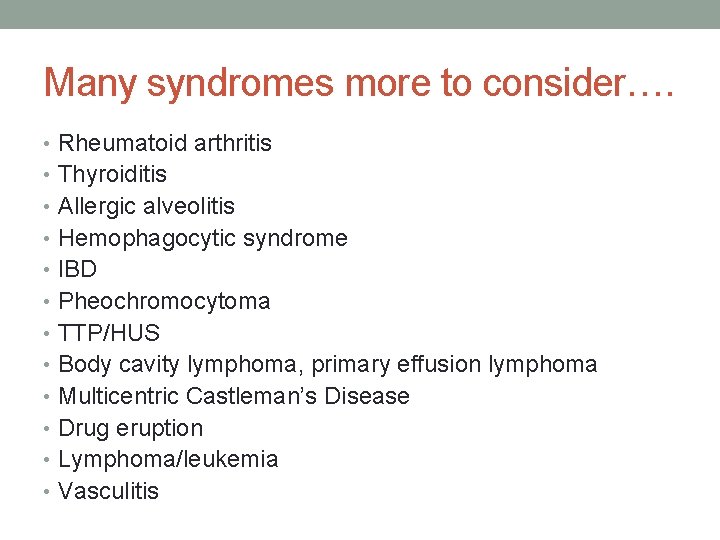
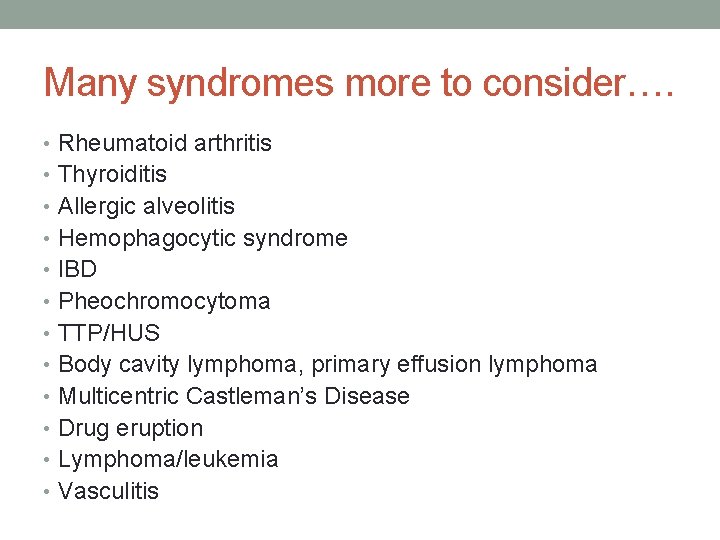
Many syndromes more to consider…. • Rheumatoid arthritis • Thyroiditis • Allergic alveolitis • Hemophagocytic syndrome • IBD • Pheochromocytoma • TTP/HUS • Body cavity lymphoma, primary effusion lymphoma • Multicentric Castleman’s Disease • Drug eruption • Lymphoma/leukemia • Vasculitis
 Tôn thất thuyết là ai
Tôn thất thuyết là ai Phân độ lown
Phân độ lown Chiến lược kinh doanh quốc tế của walmart
Chiến lược kinh doanh quốc tế của walmart Gây tê cơ vuông thắt lưng
Gây tê cơ vuông thắt lưng Block nhĩ thất độ 1
Block nhĩ thất độ 1 Tìm vết của mặt phẳng
Tìm vết của mặt phẳng Sau thất bại ở hồ điển triệt
Sau thất bại ở hồ điển triệt Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Con hãy đưa tay khi thấy người vấp ngã
Con hãy đưa tay khi thấy người vấp ngã Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Cerebellar syndromes
Cerebellar syndromes What is geriatric syndromes
What is geriatric syndromes Neuroendocrine syndrome in gynecology
Neuroendocrine syndrome in gynecology Cerebellar syndromes
Cerebellar syndromes Differential diagnosis of stroke
Differential diagnosis of stroke Neuroendocrine syndrome in gynecology
Neuroendocrine syndrome in gynecology Cryptosporidiose
Cryptosporidiose Methotrexate and yeast infections
Methotrexate and yeast infections Genital infections
Genital infections Storch infections
Storch infections Eye infections
Eye infections Opportunistic infections
Opportunistic infections Amber blumling
Amber blumling Storch infections
Storch infections Postpartum infections
Postpartum infections Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Nosocomial infections
Nosocomial infections Bone and joint infections
Bone and joint infections Opportunistic infections
Opportunistic infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Understanding the mirai botnet
Understanding the mirai botnet Acute gingival infections
Acute gingival infections Agere masquerade
Agere masquerade Masquerade falsification and repudiation
Masquerade falsification and repudiation History masquerade masks
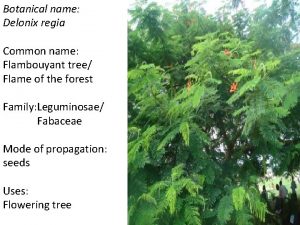
History masquerade masks Common name and uses of delonix regia
Common name and uses of delonix regia Wesley boone bronx masquerade
Wesley boone bronx masquerade Masquerade syndrome
Masquerade syndrome His masquerade of a jester irony
His masquerade of a jester irony Gartner authentication
Gartner authentication