PAPULOSQUAMOUS DISEASES I Pityriasis rosea Lichen planus PITYRIASIS






























- Slides: 43
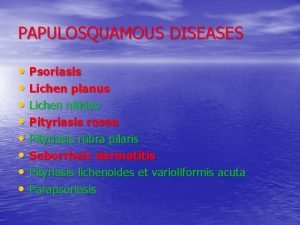
PAPULOSQUAMOUS DISEASES (I) • Pityriasis rosea • Lichen planus
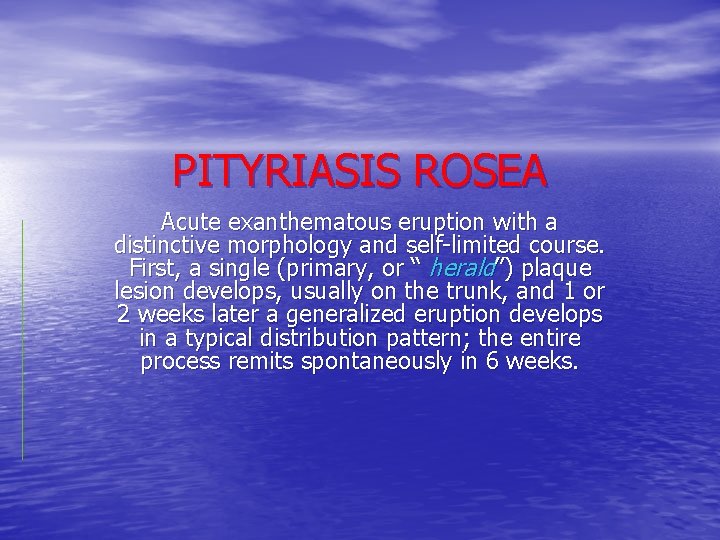
PITYRIASIS ROSEA Acute exanthematous eruption with a distinctive morphology and self-limited course. First, a single (primary, or “ herald”) plaque lesion develops, usually on the trunk, and 1 or 2 weeks later a generalized eruption develops in a typical distribution pattern; the entire process remits spontaneously in 6 weeks.
Epidemioloy and etiology • Age of onset: 10 to 43 years, but can occur rarely in infants and old persons. • Season: Spring and fall. • Etiology: Herpes virus type 7 is suspected.
Skin lesions • Herald Patch: 80% of patients. • Exanthem: Usually confined to trunk and • proximal aspects of the arms and legs. Fine scaling oval papules and plaques with marginal collarette. Rarely on face. Atypical Pityriasis Rosea: The lesions may be present only on the face and neck. The primary plaque may be absent, may be the sole manifestation of the disease, or may be multiple. The vesicles may be present.
• Differential diagnosis: Drug eruptions( e. g. , captopril, barbiturates), secondary syphilis, , guttate psoriasis, tinea corporis, erythema multiforme. • Course: Spontaneous remission in 6 to 12 weeks or less. Recurrences are uncommon. • Management: Mainly symptomatic. Oral antihistamines and/or topical antipruritic lotions, topical glucocorticoids, UVB phototherapy or natural sunlight, short course of systemic glucocorticoids.









LICHEN PLANUS Lichen planus is an idiopathic, acute or chronic inflammatory dermatosis involving skin, hair, nails and / or mucous membranes, characterized by flat-topped, pink to violaceous, shiny, pruritic polygonal papules on the skin and milky white reticulated papules in the mouth. (Four P’s: papule, purple, polygonal, pruritic)
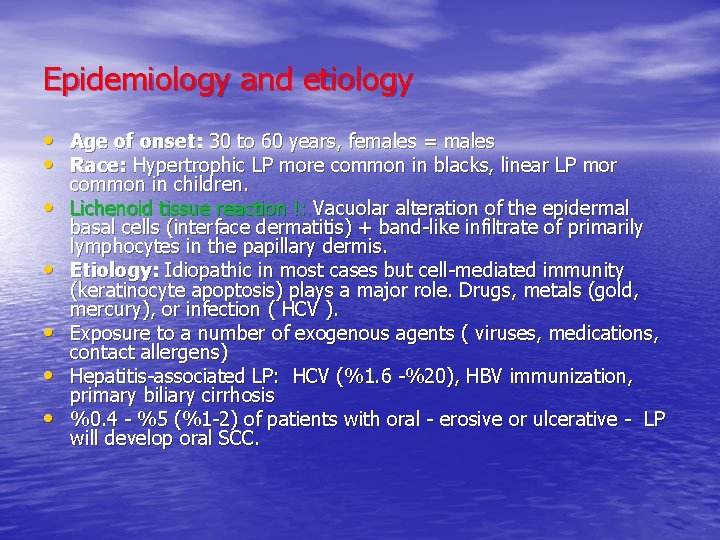
Epidemiology and etiology • • Age of onset: 30 to 60 years, females = males Race: Hypertrophic LP more common in blacks, linear LP mor common in children. Lichenoid tissue reaction !: Vacuolar alteration of the epidermal basal cells (interface dermatitis) + band-like infiltrate of primarily lymphocytes in the papillary dermis. Etiology: Idiopathic in most cases but cell-mediated immunity (keratinocyte apoptosis) plays a major role. Drugs, metals (gold, mercury), or infection ( HCV ). Exposure to a number of exogenous agents ( viruses, medications, contact allergens) Hepatitis-associated LP: HCV (%1. 6 -%20), HBV immunization, primary biliary cirrhosis %0. 4 - %5 (%1 -2) of patients with oral - erosive or ulcerative - LP will develop oral SCC.
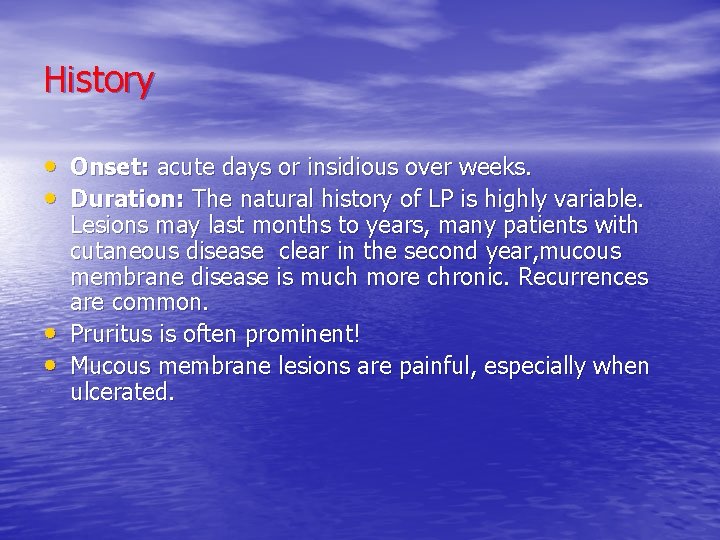
History • Onset: acute days or insidious over weeks. • Duration: The natural history of LP is highly variable. • • Lesions may last months to years, many patients with cutaneous disease clear in the second year, mucous membrane disease is much more chronic. Recurrences are common. Pruritus is often prominent! Mucous membrane lesions are painful, especially when ulcerated.
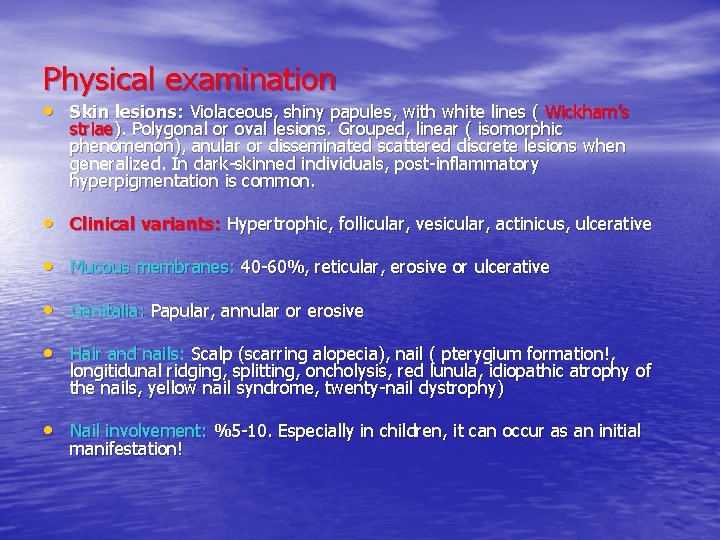
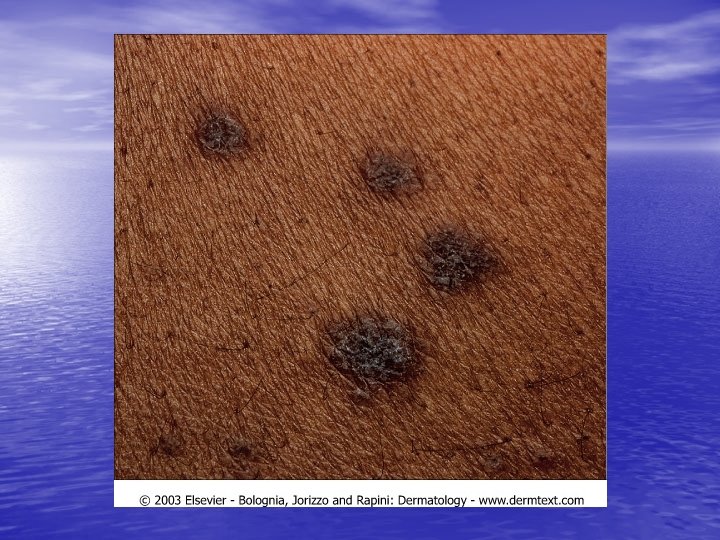
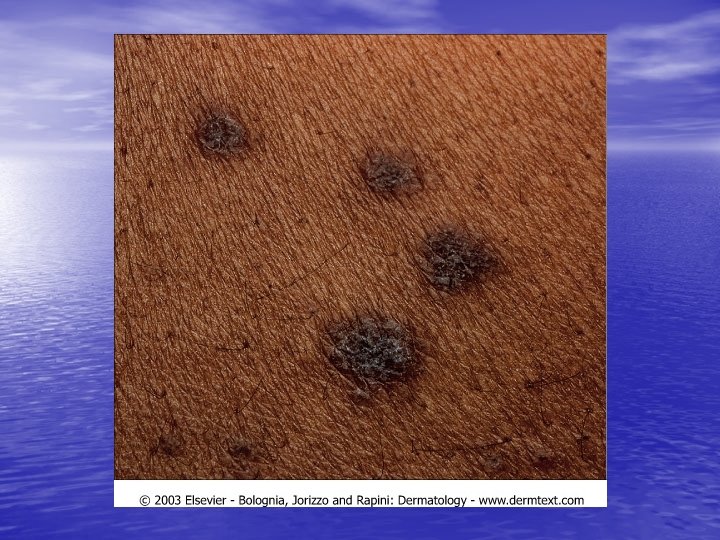
Physical examination • Skin lesions: Violaceous, shiny papules, with white lines ( Wickham’s striae). Polygonal or oval lesions. Grouped, linear ( isomorphic phenomenon), anular or disseminated scattered discrete lesions when generalized. In dark-skinned individuals, post-inflammatory hyperpigmentation is common. • Clinical variants: Hypertrophic, follicular, vesicular, actinicus, ulcerative • Mucous membranes: 40 -60%, reticular, erosive or ulcerative • Genitalia: Papular, annular or erosive • Hair and nails: Scalp (scarring alopecia), nail ( pterygium formation!, longitidunal ridging, splitting, oncholysis, red lunula, idiopathic atrophy of the nails, yellow nail syndrome, twenty-nail dystrophy) • Nail involvement: %5 -10. Especially in children, it can occur as an initial manifestation!
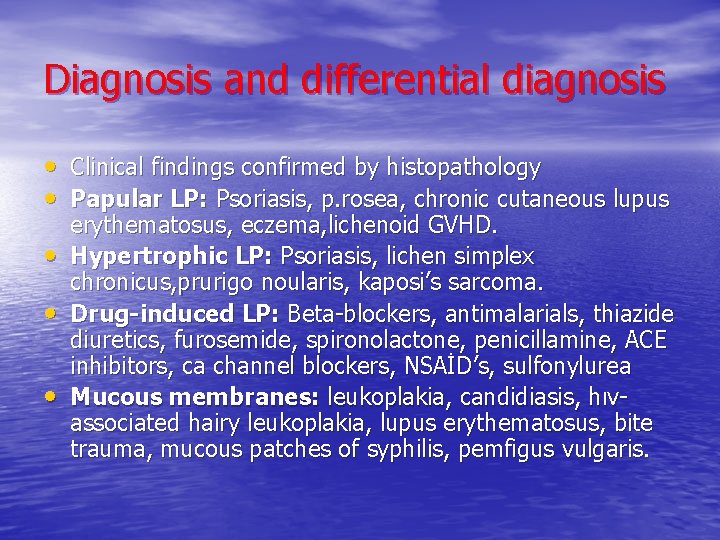
Diagnosis and differential diagnosis • Clinical findings confirmed by histopathology • Papular LP: Psoriasis, p. rosea, chronic cutaneous lupus • • • erythematosus, eczema, lichenoid GVHD. Hypertrophic LP: Psoriasis, lichen simplex chronicus, prurigo noularis, kaposi’s sarcoma. Drug-induced LP: Beta-blockers, antimalarials, thiazide diuretics, furosemide, spironolactone, penicillamine, ACE inhibitors, ca channel blockers, NSAİD’s, sulfonylurea Mucous membranes: leukoplakia, candidiasis, hıvassociated hairy leukoplakia, lupus erythematosus, bite trauma, mucous patches of syphilis, pemfigus vulgaris.
• Course: Cutaneous LP usually persists for • months, but in some cases, for years; oral LP often for decades. The incidence oral cancer (squamous cell carcinoma) is increased by 5%. Patients should be followed at regular intervals. Differential diagnosis: Lichenoid drug eruptions, p. rosea, psoriasis, syphilis, PLEVA, lupus, in situ scc, lichen simplex chronicus, fixed drug eruption
Management • Topical therapy: – Glucocorticoids (topical or intralesional) – Cyclosporine and Tacrolimus Solutions • Systemic therapy: – – Cyclosporine Glucocorticoids Systemic retinoids ( Acitretin) PUVA Photochemotherpy • Others: Mycophenolate mofetil, enoxaparin, azathioprine.





















 Disorder of skin and subcutaneous tissue adalah
Disorder of skin and subcutaneous tissue adalah Pityriasis rosea
Pityriasis rosea Hanging curtain sign
Hanging curtain sign Grattage test definition
Grattage test definition Pityriasis rosea liečba
Pityriasis rosea liečba Psoriasis
Psoriasis Papule
Papule Polügonaalne
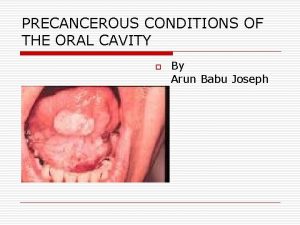
Polügonaalne Differential diagnosis of osmf
Differential diagnosis of osmf Richen luber planus
Richen luber planus Pes transverso planus
Pes transverso planus Pes transversoplanus
Pes transversoplanus Medial longitudinal ark takviyesi
Medial longitudinal ark takviyesi Secreção rosea espumosa
Secreção rosea espumosa Chytridiomycota
Chytridiomycota Xantho medical term
Xantho medical term Rosea hudsygdom
Rosea hudsygdom Pityriasis ros
Pityriasis ros Pityriasis stéatoïde
Pityriasis stéatoïde What is trichoptilosis milady
What is trichoptilosis milady Enophtalmus
Enophtalmus Lichenophyta
Lichenophyta Basidiomycotina
Basidiomycotina Draw flow chart of aseptate division of fungi
Draw flow chart of aseptate division of fungi Lichen sclerosus vulvare
Lichen sclerosus vulvare Lichens classification
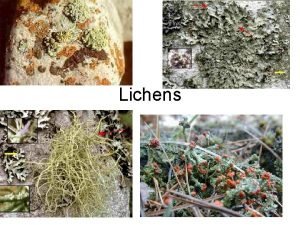
Lichens classification Menopausa sintomi iniziali
Menopausa sintomi iniziali Lichen symbiose
Lichen symbiose What are lichen
What are lichen N
N Lichen is an association of
Lichen is an association of Anatomi lichen
Anatomi lichen Virginia mainardi
Virginia mainardi Fungus lichen and conks
Fungus lichen and conks Pretibial miksödem
Pretibial miksödem Similarities between primary and secondary succession
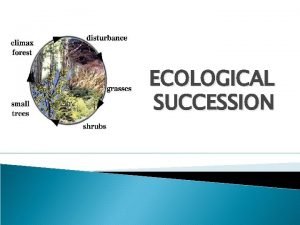
Similarities between primary and secondary succession Lichen association of
Lichen association of Lichen
Lichen Lichen as food
Lichen as food Bartholin cyst treatment
Bartholin cyst treatment Lichen thallus
Lichen thallus Giovanni lupoli
Giovanni lupoli Squamous cell carcinoma
Squamous cell carcinoma Minerals sources functions and deficiency chart
Minerals sources functions and deficiency chart