OESOPHAGEAL MOTILITY DISORDERS ACHALASIA CARDIA DEFINITION It is













- Slides: 43
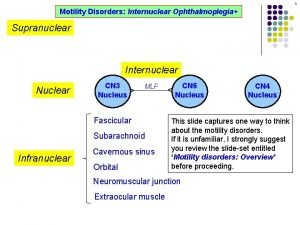
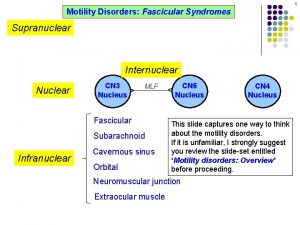
OESOPHAGEAL MOTILITY DISORDERS

ACHALASIA CARDIA
DEFINITION Ø It is failure of relaxation of cardia (oesophagogastric junction) Ø due to disorganised oesophageal peristalsis, Ø as a result of failure of integration of parasympathetic impulses Ø causing functional obstruction • (Achalasia means failure to relax—Greek).

AETIO-PATHOLOGY Degeneration or absence of ganglion cells of Auerbach’s plexus throughout the body of the oesophagus is a definite histological feature neurological basis Defect – central nuclei / vagus i. Emotional stress ii. External compression/trauma iii. Chaga’s disease (Trypanosoma cruzi) iv. Infection

CLINICAL FEATURES 1. Dysphagia – Low, retrosternal – Cold > warm – Liquids > solids 2. Regurgitation – At night / supine – Not sour tasting 3. Weight loss

INVESTIGATIONS 1. Barium swallow • Pencil like smooth narrowing of lower oeso phagus—Bird beak appearance • Dilatation of proximal oesophagus • Absence of fundic gas bubble • Sigmoid oesophagus or megaoesophagus
2. Chest Xray 3. Oesophageal Manometry 4. Oesophagoscopy
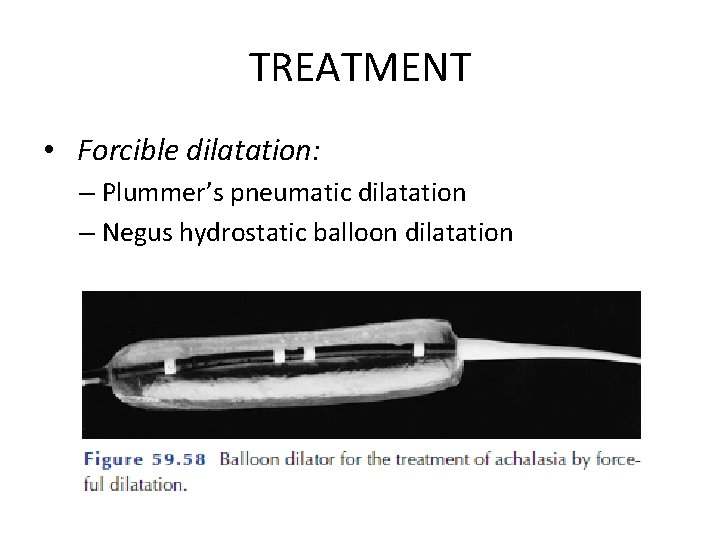
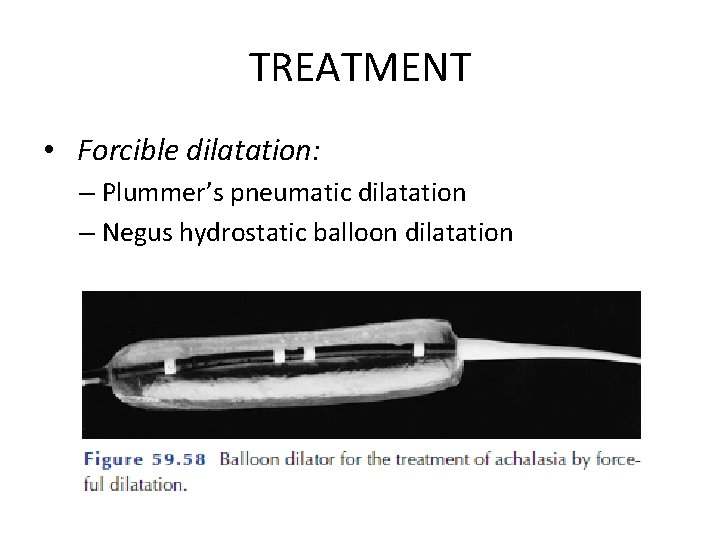
TREATMENT • Forcible dilatation: – Plummer’s pneumatic dilatation – Negus hydrostatic balloon dilatation

• Modified Heller’s cardiomyotomy

• Drugs – Botulinum toxin A – Nitroglycernie, nifedipine
• PSEUDOACHALASIA is an achalasia-like disorder that is usually produced by adenocarcinoma of the cardia, but has also been described in relation to benign tumours at this level. • Due to inability of the LES to relax, linked to the loss of body peristalsis • Other cancers outside the oesophagus (bronchus, pancreas) have also been associated with pseudoachalasia.
DIFFUSE OESOPHAGEAL SPASM/ CORKSCREW OESOPHAGUS
Ø Incoordinate contractions of the oesophagus, causing dysphagia and/or chest pain. Ø May have a psychic component. H/O IBS, spastic colon, pylorospasm may be associated
CLINICAL FEATURES • F>M • Pain – Discomfort/ severe and colicky, behind the lower sternum – May radiate to back and arms resembling angina – Greatest during periods of emotional stress • Dysphagia • Regurgitation - rare
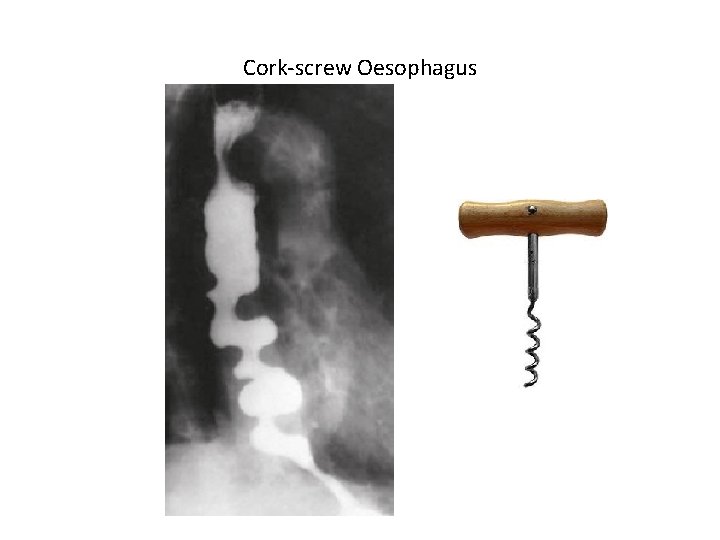
INVESTIGATIONS 1. ECG 2. Barium meal – – Curling / corkscrew oesophagus Bird-beak like taper of distal oesophagus Oesophageal wall thickening Oesophageal pulsion diverticulum 3. Oesophagoscopy 4. Oesophageal Manometry
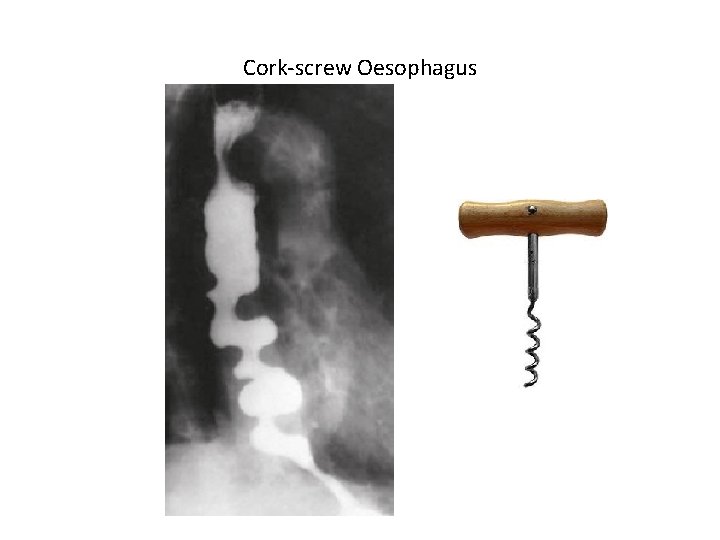
Cork-screw Oesophagus
TREATMENT 1. Medical – Sublingual nitroglycerine 2. Oesophageal dilatation 3. Extended Oesophagomyotomy
NUTCRACKER OESOPHAGUS
• Is a condition in which peristaltic pressures of more than 180 mm. Hg develop. • It is said to cause chest pain

OESOPHAGEAL INVOLVEMENT IN AUTOIMMUNE DISEASE
• • • Systemic sclerosis, Polymyositis, Dermatomyositis, Systemic lupus erythematosus, Polyarteritis nodosa or Rheumatoid disease.
PATHOGENESIS • Most involve weak peristalsis • Swallowing difficulties may be compounded by – pharyngeal problems in the disorders that primarily affect skeletal muscle (e. g. polymyositis) or – extraoesophageal problems - involvement of the cricoarytenoid joint in rheumatoid disease or dry mouth in Sjögren’s syndrome. • In systemic sclerosis, smooth muscle atrophy causes hypoperistalsis. The LOS is involved, leading to a loss of the antireflux barrier.
CLINICAL FEATURES • Range from mild to severe dysphagia • Accompanied by regurgitation and aspiration • Reflux can be severe and is exacerbated by weak acid clearance so that strictures can occur
TREATMENT • There are no drugs that specifically correct the motor disorder, and medical treatment is mainly directed at minimising reflux-induced damage with PPIs. • A small number of patients may require antireflux surgery.
EOSINOPHILIC OESOPHAGITIS • Occurs in children and adults either alone or as a manifestation of eosinophilic gastroenteritis. • It is characterised by eosinophilic infiltration of the oesophageal wall • Presumably of allergic or idiopathic origin.
EOSINOPHILIC OESOPHAGITIS CLINICAL FEATURES: • Dysphagia • History of atopy. DIAGNOSIS: Endoscopy – Narrow and friable oesophagus and may include mucosal rings. – Deep ulcers leading to stricture development, especially in the proximal oesophagus. – The diagnosis is established by endoscopic biopsy.

EOSINOPHILIC OESOPHAGITIS TREATMENT: 1. Elimination diets, topical and systemic steroids short term relief 2. Immunotherapy directed against interleukin (IL) -5, which has a major role in eosinophil recruitment, seems to be a promising innovative approach. 3. Although endoscopic dilatation has been recommended, this can create deep ulcers and further scarring, so should be used with caution and only when the above therapies fail.
OESOPHAGEAL DIVERTICULUM
DEFINITION: It is the protrusion of the oesophageal mucous membrane through the oesophageal wall. CLASSIFICATION: i. True variety – contains all layers (mucosa, submucosa and muscle layers) ii. False variety – contains only mucosa and submucosa

i. Pulsion diverticulum – arises due to elevated intraluminal pressure which forces the mucosa and submucosa to herniate through the oesophageal musculature – false diverticulum ii. Traction diverticulum – forms as a result of traction effect by chronically inflamed and granulomatous mediastinal lymph nodes that adhere to the oesophageal wall.
SITES: 1. Pharyngo-oesophageal : At the junction of pharynx and oesophagus 2. Para-bronchial (Mid oesophageal): Near the bifurcation of trachea 3. Epiphrenic (Sub diaphragmatic): At the distal oesophagus Ø Parabronchial – true; Pharyngo-oesophageal and Subdiaphragmatic – false Ø All varieties are acquired.
PHARYNGO-OESOPHAGEAL DIVERTICULUM ZENKER’S DIVERTICULUM • Commonest variety • >50 yrs ETIOPATHOGENESIS: Premature contraction of the cricopharyngeus muscle during swallowing
Increases intraluminal pressure Mucosa and submucosa of the pharyngooesophageal junction prolapse posteriorly through the Killians triangle (Cricopharyngeus muscle inferiorly and oblique fibres of the thyropharyngeus superiorly)

The diverticulum develops and insinuates itself in the prevertebral space between the oesophagus and the cervical vertebrae CLINICAL FEATURES 1. Cervical dysphagia 2. Effortless regurgitation – more during sleep airway contamination and aspiration pneumonitis 3. Gurgling sensation in the neck while swallowing
INVESTIGATIONS: 1. Barium study 2. Oesophageal manometry TREATENT: 1. Correct dehydration 2. Treat pneumonitis/lung abscess 3. Surgery – Cricopharyngeal myotomy and resection of the diverticulum


PARABRONCHIAL / MIDOESOPHAGEAL DIVERTICULUM • Least common • Can occur anywhere in the middle 1/3 of oesophagus – MC at the bifurcation of the trachea • Commonly associated with granulomatous infection of mediastinal LN (Tuberculosis, histoplasmosis)

CLINICAL FEATURES: • Asymptomatic • Diagnosis is made incidentally by barium oesophagogram for other conditions. TREATMENT: • Asymptomatic – left alone • Treatment for tuberculosis • If a fistulous communication is present - division
EPIPHRENIC DIVERTICULUM SITE – Distal oesophagus 10 cm from the cardia ETIOPATHOGENESIS: • It is due to an oesophageal motility disorder • May be associated with diffuse spasm, achalasia, oesophageal sliding hernia, reflux oesophagitis and stricture
CLINICAL FEATURES: • Asymptomatic • Dysphagia and retrosternal pain with associated conditions DIAGNOSIS: 1. Barium oesophagogram 2. Manometric study 3. Oesophagoscopy
TREATMENT: • Mildly symptomatic patients require no treatment • Severe dysphagia and chest pain resection of the diverticulum along with a long thoracic oesophagomyotomy from the level of the arch of the aorta to the OG junction, through a left thoracotomy.
 Definition of achalasia cardia
Definition of achalasia cardia Achalasia of cardia
Achalasia of cardia Triad of achalasia cardia
Triad of achalasia cardia Oesophageal doppler
Oesophageal doppler Kopeloff and beerman's modification
Kopeloff and beerman's modification Motility agar test
Motility agar test Chicago classification of achalasia
Chicago classification of achalasia Chicago classification manometry
Chicago classification manometry Foreign body retrieval hood protector
Foreign body retrieval hood protector Quimo
Quimo Normal semen report
Normal semen report Motility vs mobility
Motility vs mobility Motility test positive and negative
Motility test positive and negative Ducti hepatici
Ducti hepatici Entamoeba
Entamoeba Tsi
Tsi Gliding motility
Gliding motility Cardia gaster
Cardia gaster Syn cardia
Syn cardia Brandy cardia
Brandy cardia Cardia
Cardia Syn cardia
Syn cardia Pneumocardia
Pneumocardia Plicae circularis
Plicae circularis Hanging drop method for motility
Hanging drop method for motility Work related musculoskeletal disorders definition
Work related musculoskeletal disorders definition Physiological disorders unit 14
Physiological disorders unit 14 Physiological disorders unit 14
Physiological disorders unit 14 Neurocognitive disorders
Neurocognitive disorders Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders Flinders model of care
Flinders model of care Assistive technology for behavior
Assistive technology for behavior Somatic symptom disorder
Somatic symptom disorder Egodystonic
Egodystonic Types of sensory disorders
Types of sensory disorders Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Puberty and autism spectrum disorders
Puberty and autism spectrum disorders Medical model psychology
Medical model psychology What are the 10 personality disorders
What are the 10 personality disorders Cluster b personality disorder
Cluster b personality disorder Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Avoidant personality disorder
Avoidant personality disorder