The Syn Cardia Cardio West TM Total Artificial








- Slides: 39
The Syn. Cardia Cardio. West. TM Total Artificial Heart Marvin J. Slepian, M. D. Sarver Heart Center University of Arizona Tucson, Arizona 2010

Syn. Cardia Cardio. West TAH: Indication for Use As an in-hospital bridge to transplantation in cardiac transplant candidates at imminent risk of death due to irreversible biventricular failure
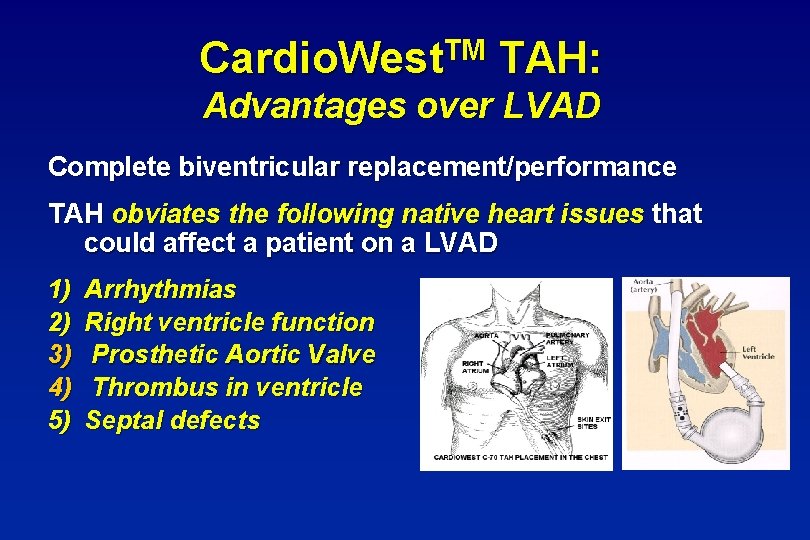
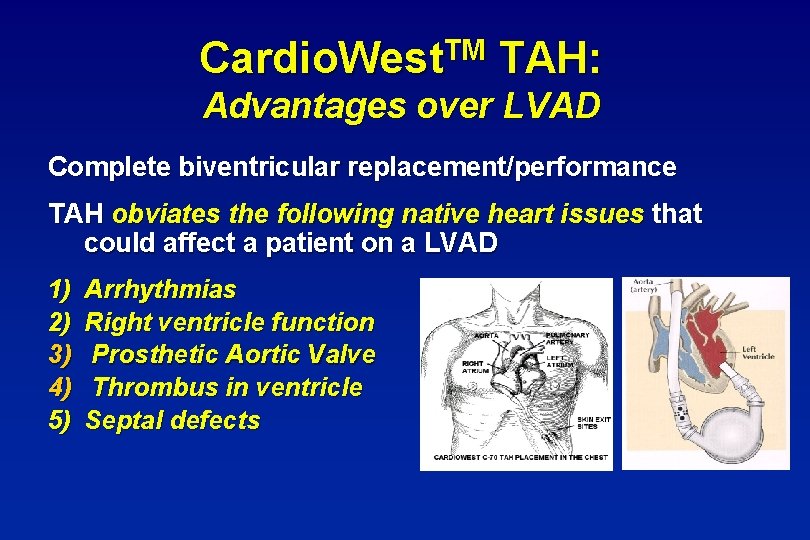
TM Cardio. West TAH: Advantages over LVAD Complete biventricular replacement/performance TAH obviates the following native heart issues that could affect a patient on a LVAD 1) 2) 3) 4) 5) Arrhythmias Right ventricle function Prosthetic Aortic Valve Thrombus in ventricle Septal defects
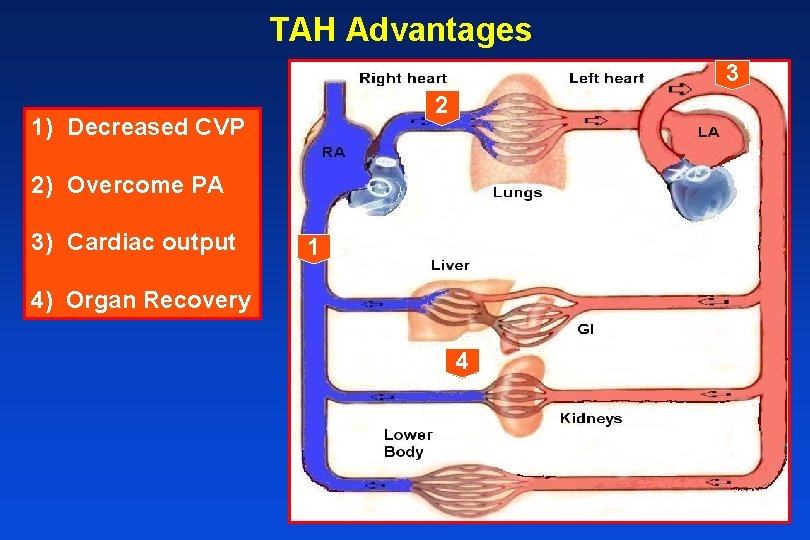
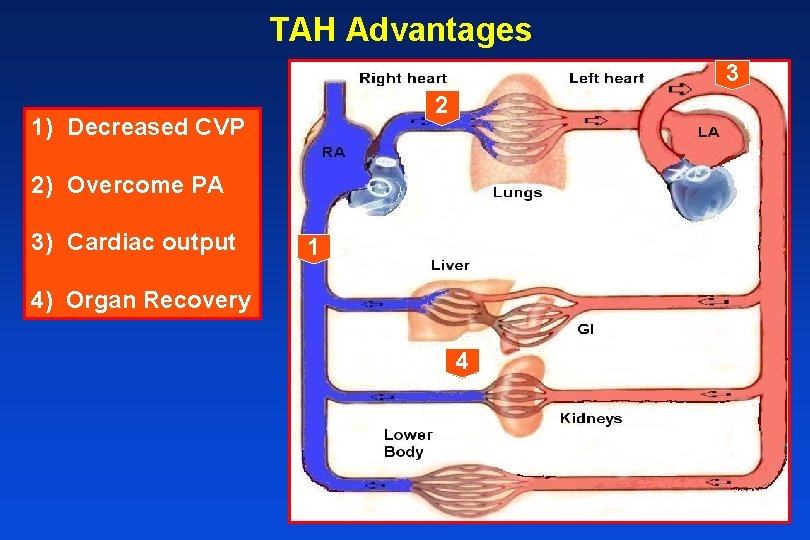
TAH Advantages 3 2 1) Decreased CVP 2) Overcome PA 3) Cardiac output 1 4) Organ Recovery 4
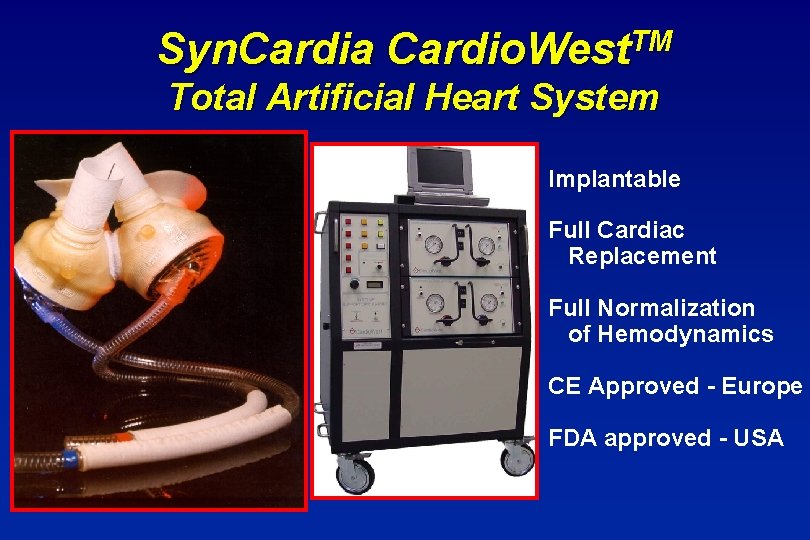
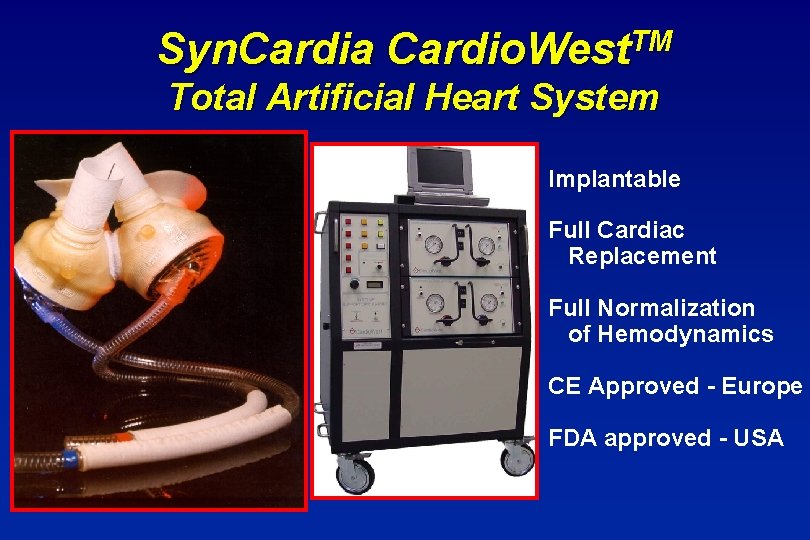
Syn. Cardia Cardio. West. TM Total Artificial Heart System Implantable Full Cardiac Replacement Full Normalization of Hemodynamics CE Approved - Europe FDA approved - USA
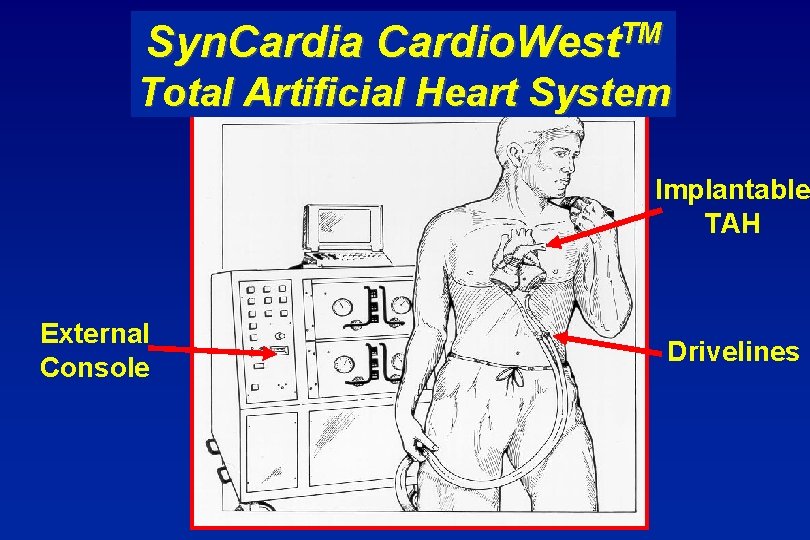
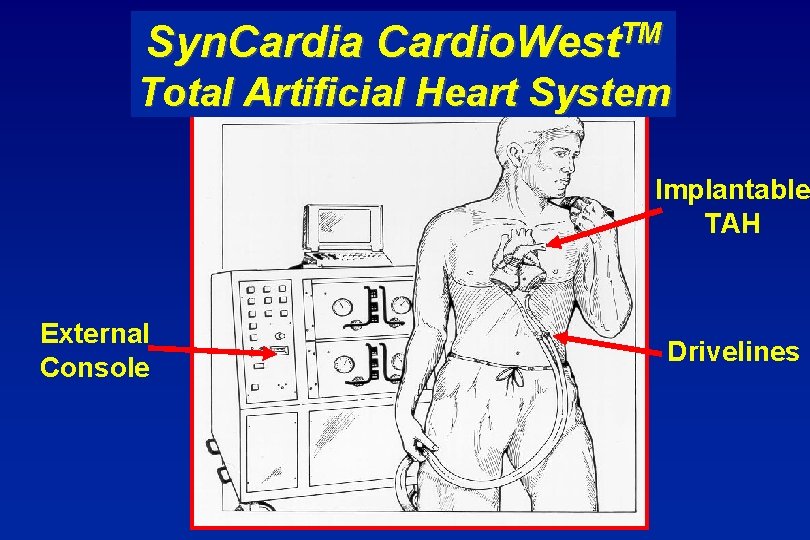
Syn. Cardia TM Cardio. West Total Artificial Heart System Implantable TAH External Console Drivelines
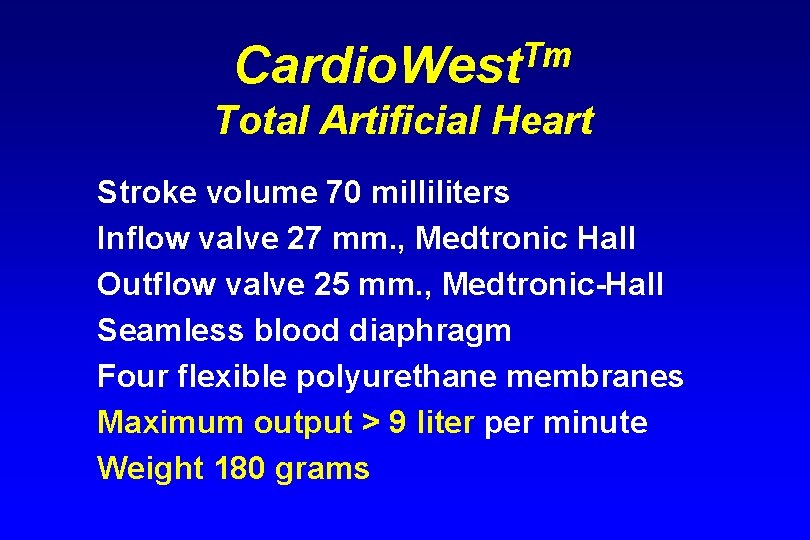
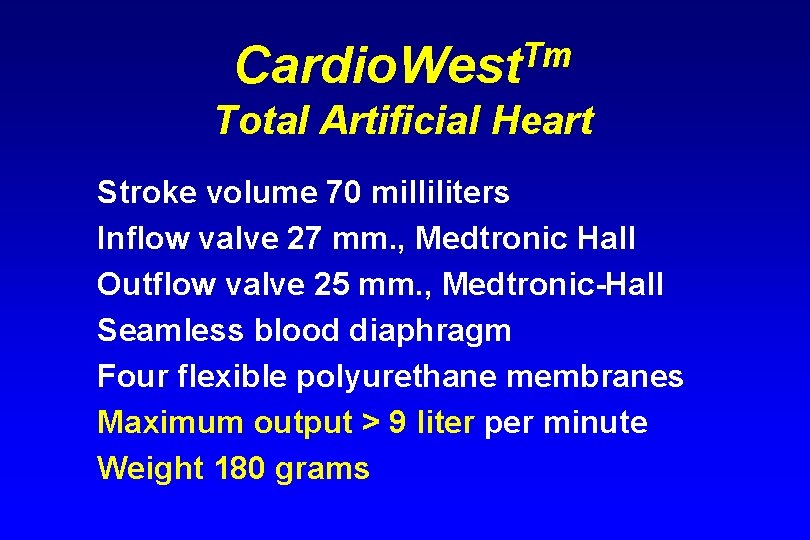
Tm Cardio. West Total Artificial Heart Stroke volume 70 milliliters Inflow valve 27 mm. , Medtronic Hall Outflow valve 25 mm. , Medtronic-Hall Seamless blood diaphragm Four flexible polyurethane membranes Maximum output > 9 liter per minute Weight 180 grams
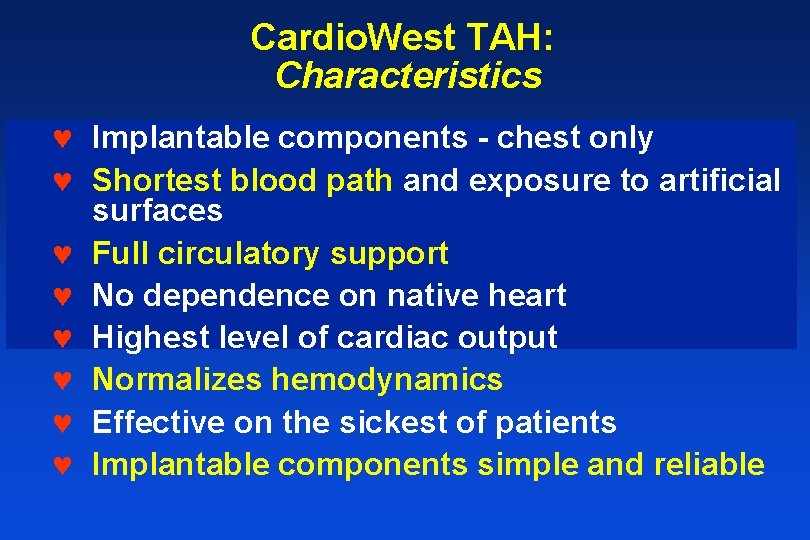
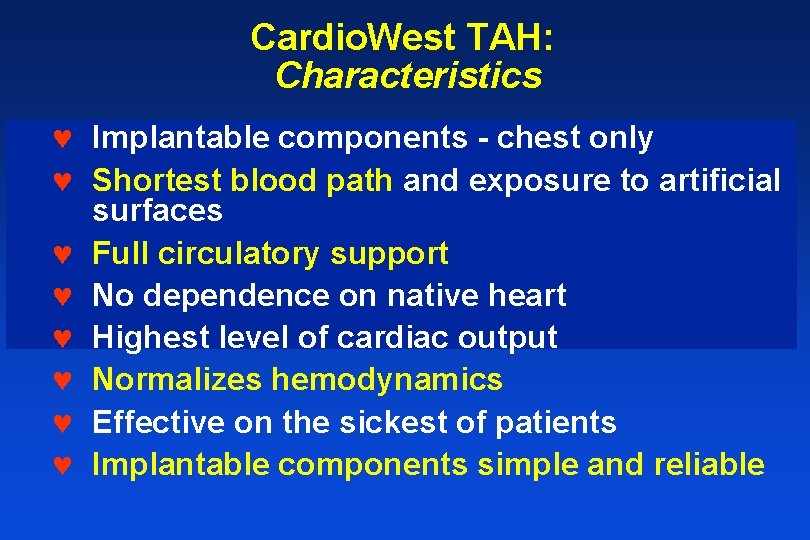
Cardio. West TAH: Characteristics © Implantable components - chest only © Shortest blood path and exposure to artificial surfaces © Full circulatory support © No dependence on native heart © Highest level of cardiac output © Normalizes hemodynamics © Effective on the sickest of patients © Implantable components simple and reliable
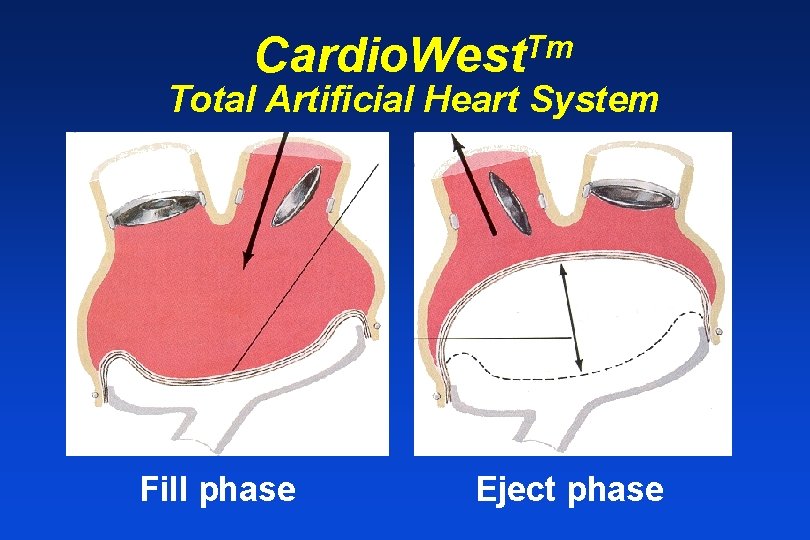
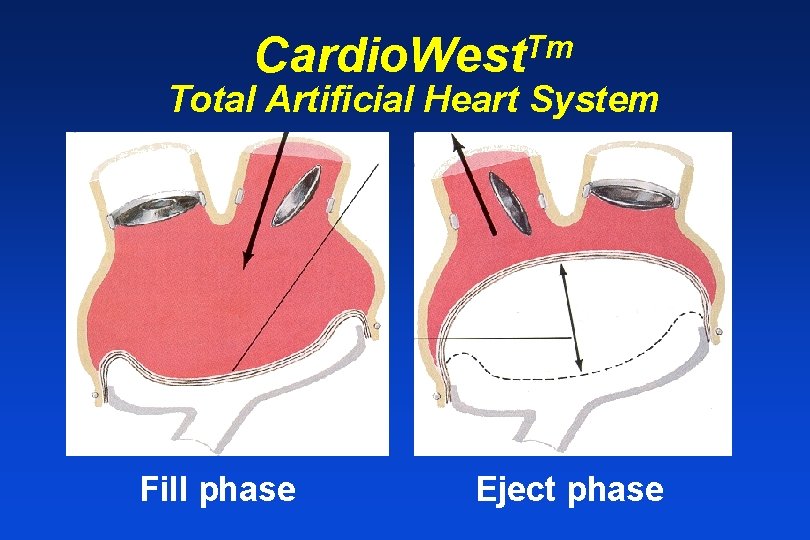
Tm Cardio. West Total Artificial Heart System Fill phase Eject phase
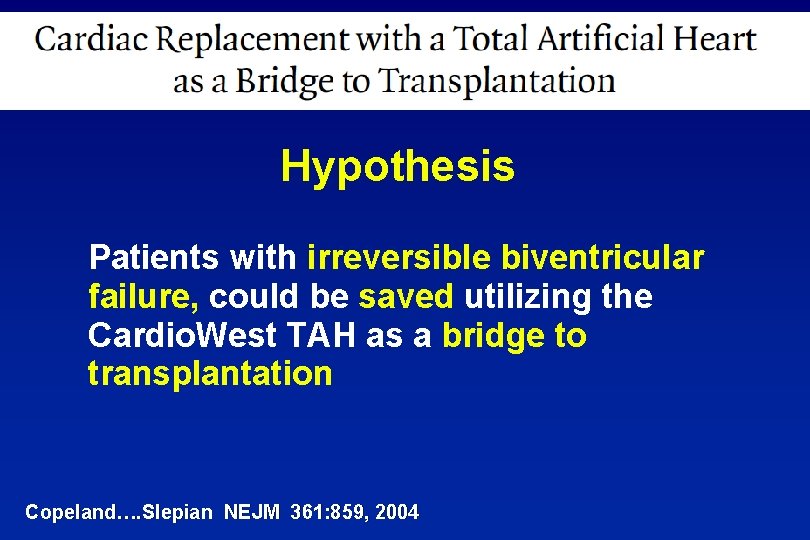
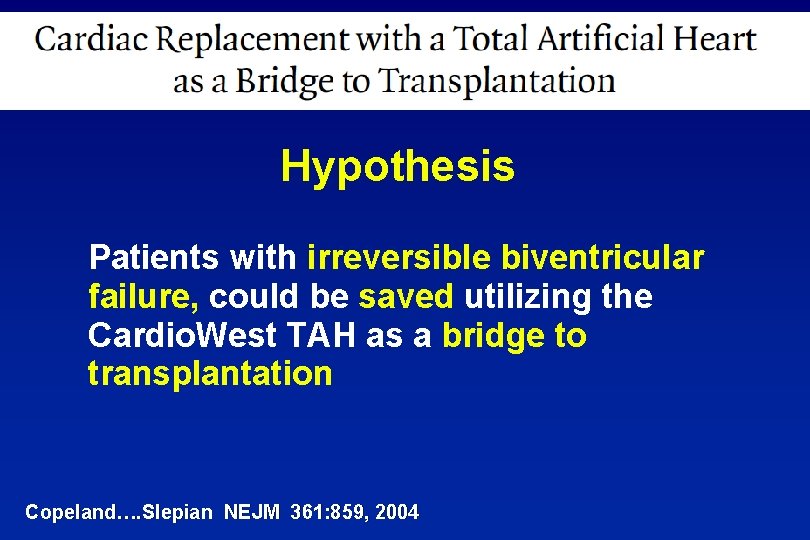
Hypothesis Patients with irreversible biventricular failure, could be saved utilizing the Cardio. West TAH as a bridge to transplantation Copeland…. Slepian NEJM 361: 859, 2004
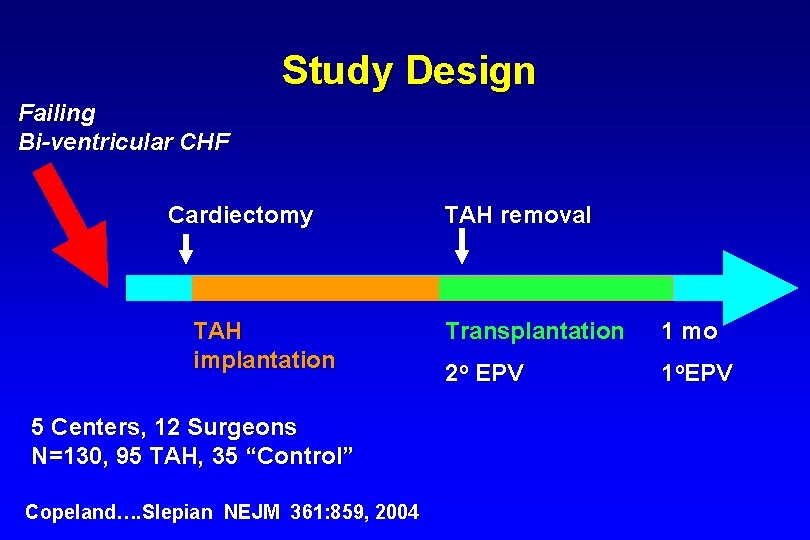
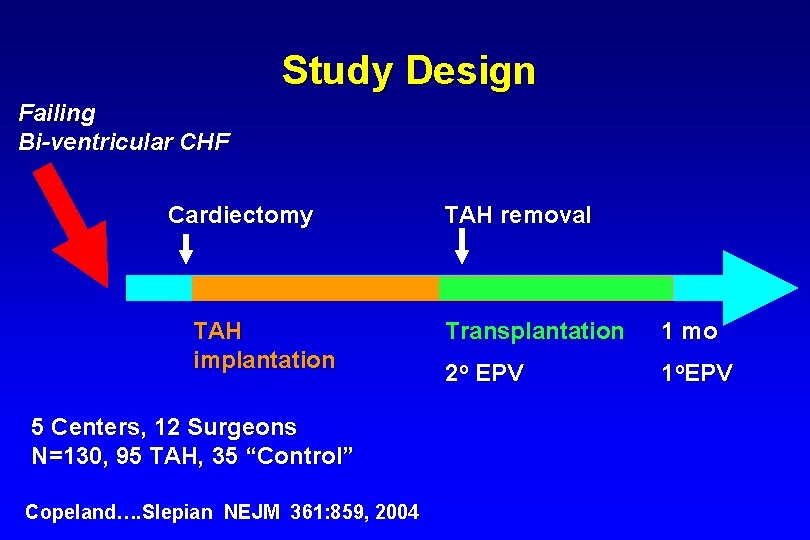
Study Design Failing Bi-ventricular CHF Cardiectomy TAH implantation 5 Centers, 12 Surgeons N=130, 95 TAH, 35 “Control” Copeland…. Slepian NEJM 361: 859, 2004 TAH removal Transplantation 1 mo 2 o EPV 1 o. EPV
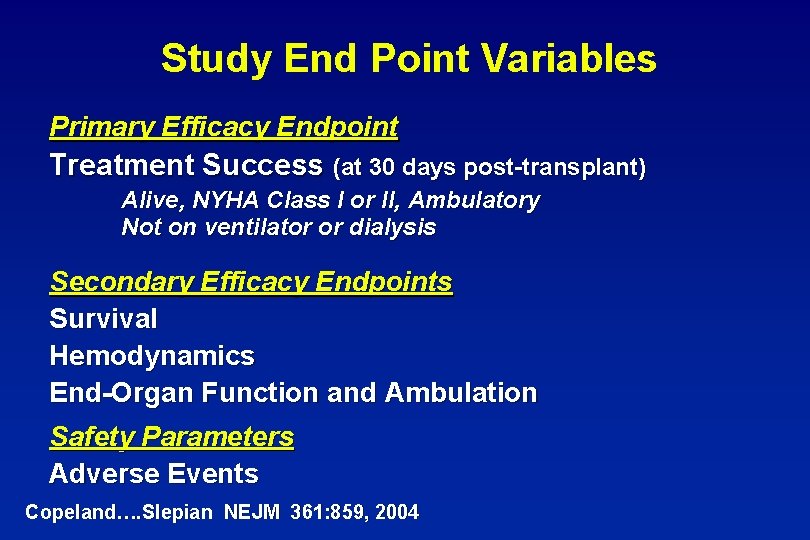
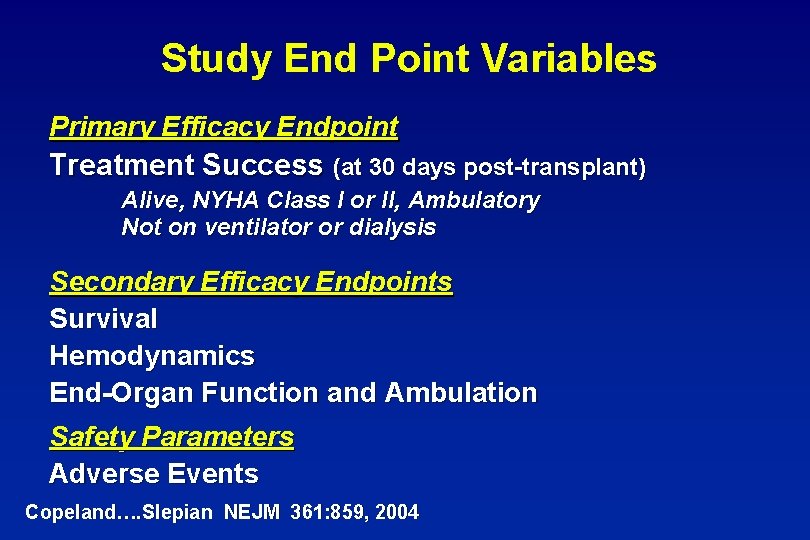
Study End Point Variables Primary Efficacy Endpoint Treatment Success (at 30 days post-transplant) Alive, NYHA Class I or II, Ambulatory Not on ventilator or dialysis Secondary Efficacy Endpoints Survival Hemodynamics End-Organ Function and Ambulation Safety Parameters Adverse Events Copeland…. Slepian NEJM 361: 859, 2004
Primary End Point: Treatment Success ü ü ü Copeland…. Slepian NEJM 361: 859, 2004 Alive 30 days post TX NYHA Class I or II Ambulatory Not on a ventilator Not on dialysis
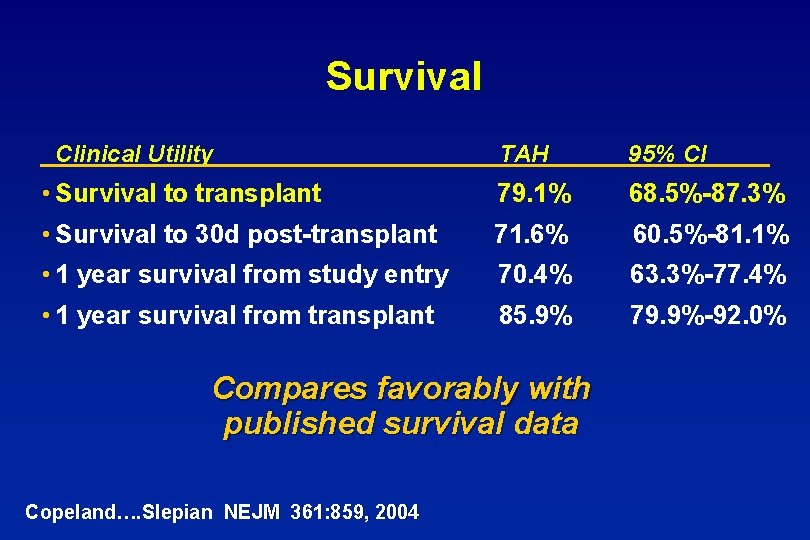
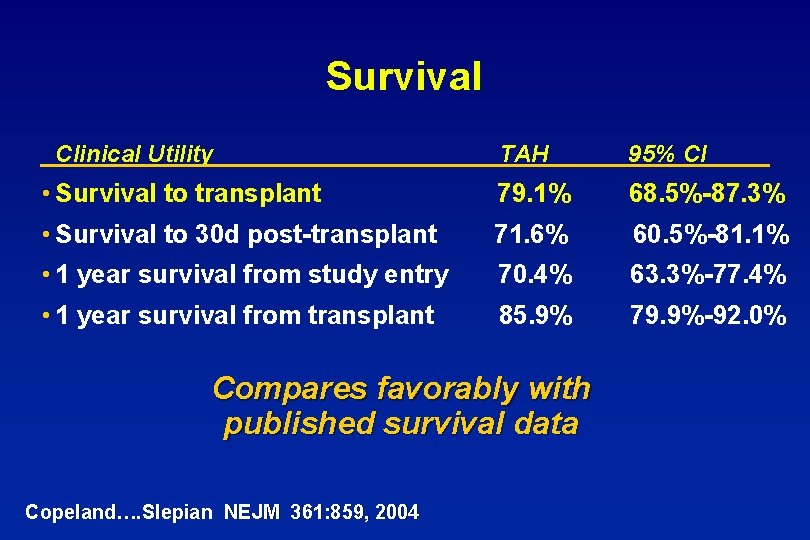
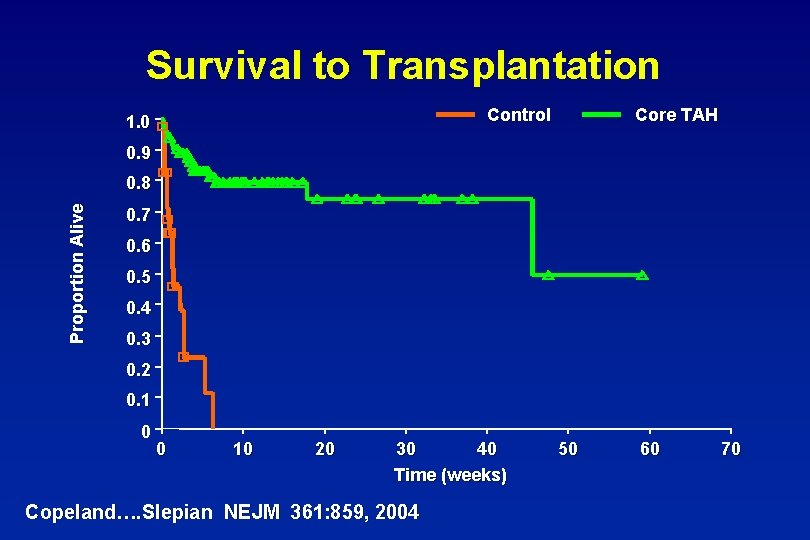
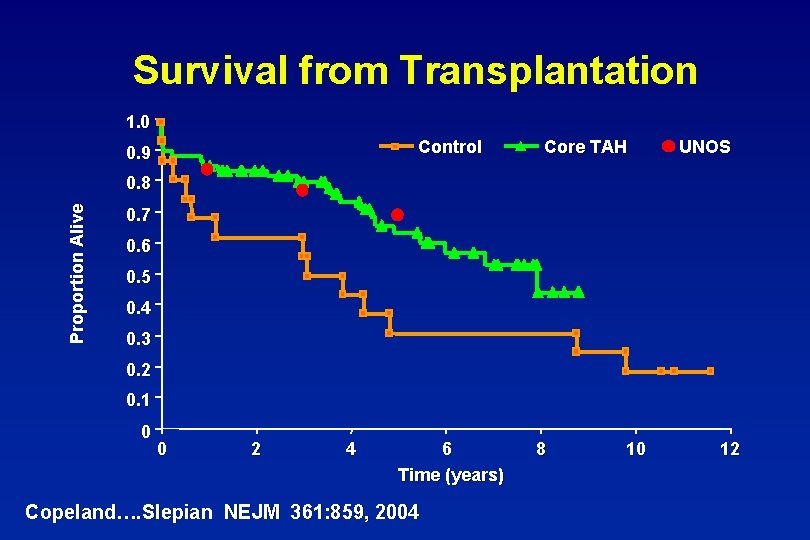
Survival Clinical Utility TAH 95% CI • Survival to transplant 79. 1% 68. 5%-87. 3% • Survival to 30 d post-transplant 71. 6% 60. 5%-81. 1% • 1 year survival from study entry 70. 4% 63. 3%-77. 4% • 1 year survival from transplant 85. 9% 79. 9%-92. 0% Compares favorably with published survival data Copeland…. Slepian NEJM 361: 859, 2004
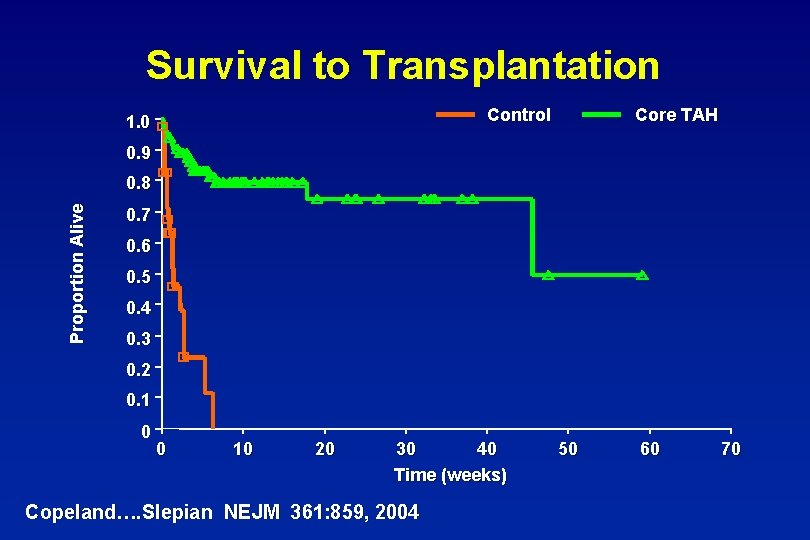
Survival to Transplantation Control 1. 0 Core TAH 0. 9 Proportion Alive 0. 8 0. 7 0. 6 0. 5 0. 4 0. 3 0. 2 0. 1 0 0 10 20 30 40 Time (weeks) Copeland…. Slepian NEJM 361: 859, 2004 50 60 70
Time to Transplant (Mean) Median = 47 days (longest 414 days) Median = 6 days Total Study Days 6, 411 Cores 299 Copeland…. Slepian NEJM 361: 859, 2004 Controls
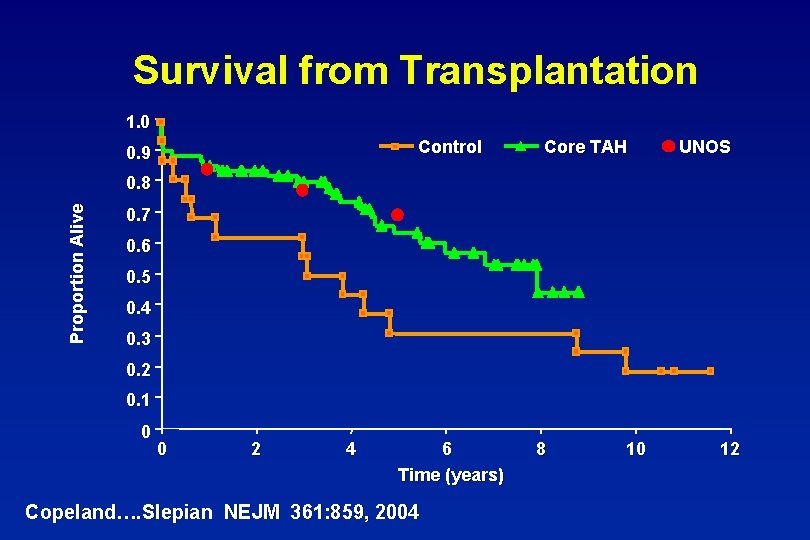
Survival from Transplantation 1. 0 Control 0. 9 Core TAH UNOS Proportion Alive 0. 8 0. 7 0. 6 0. 5 0. 4 0. 3 0. 2 0. 1 0 0 2 4 6 Time (years) Copeland…. Slepian NEJM 361: 859, 2004 8 10 12
Ambulation (Core TAH) Able to Get-out-of-Bed Able to Walk >100 Ft (% of Patients) From Kaplan Meier Estimates Copeland…. Slepian NEJM 361: 859, 2004
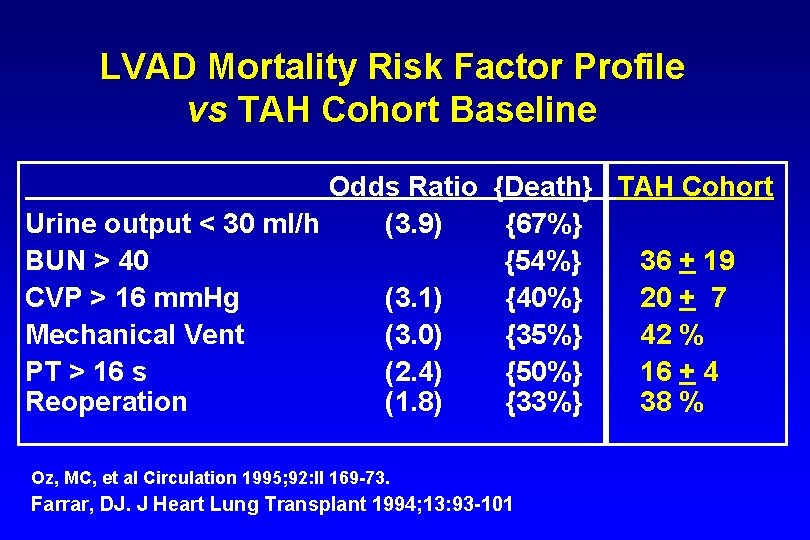
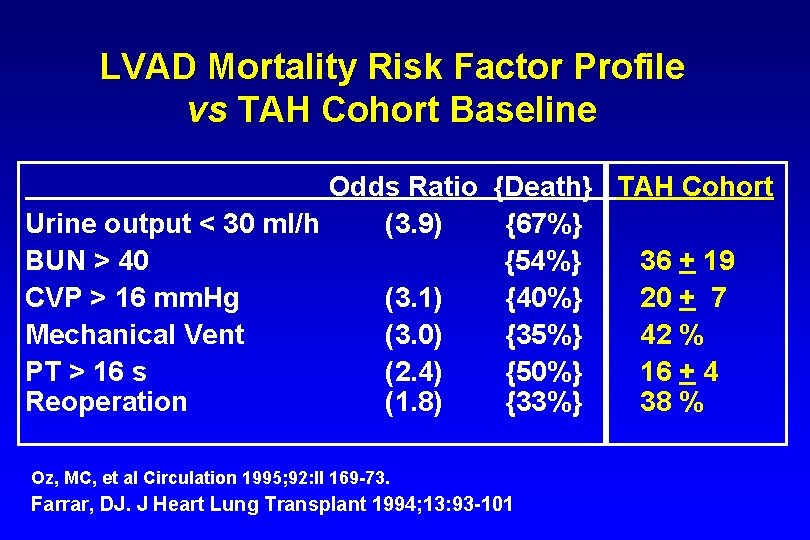
LVAD Mortality Risk Factor Profile vs TAH Cohort Baseline Odds Ratio {Death} TAH Cohort Urine output < 30 ml/h (3. 9) {67%} BUN > 40 {54%} 36 + 19 CVP > 16 mm. Hg (3. 1) {40%} 20 + 7 Mechanical Vent (3. 0) {35%} 42 % PT > 16 s (2. 4) {50%} 16 + 4 Reoperation (1. 8) {33%} 38 % Oz, MC, et al Circulation 1995; 92: II 169 -73. Farrar, DJ. J Heart Lung Transplant 1994; 13: 93 -101
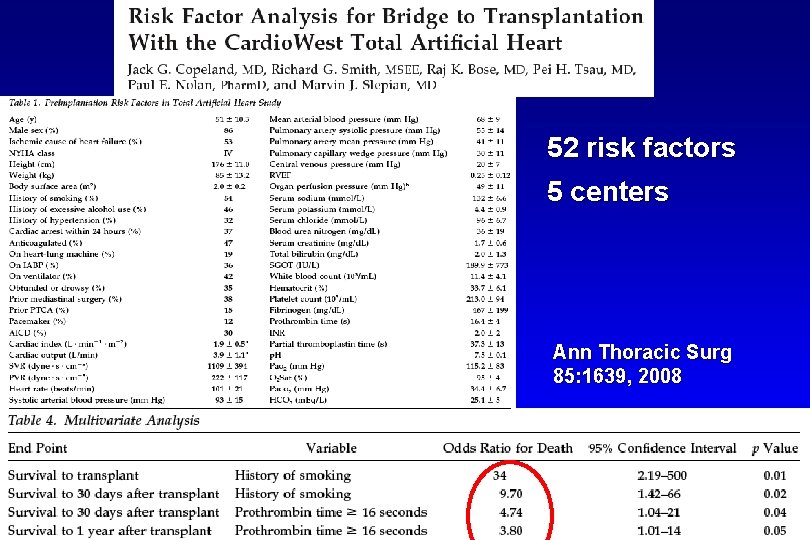
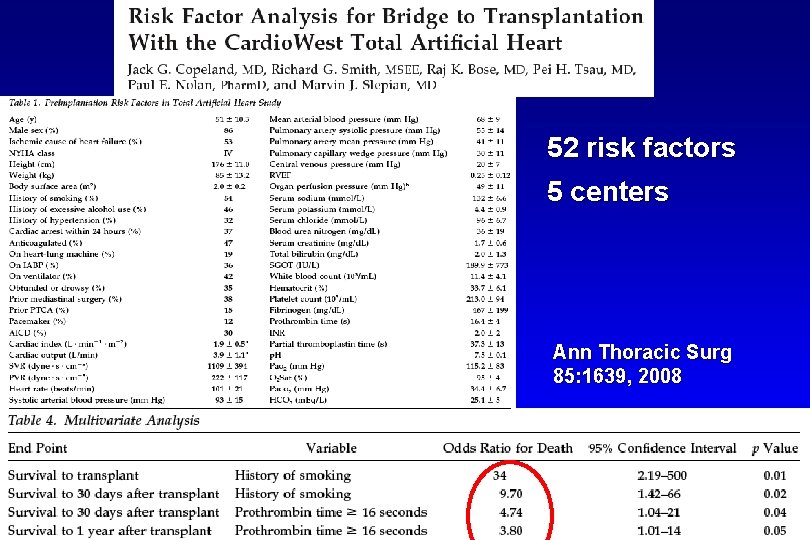
52 risk factors 5 centers Ann Thoracic Surg 85: 1639, 2008
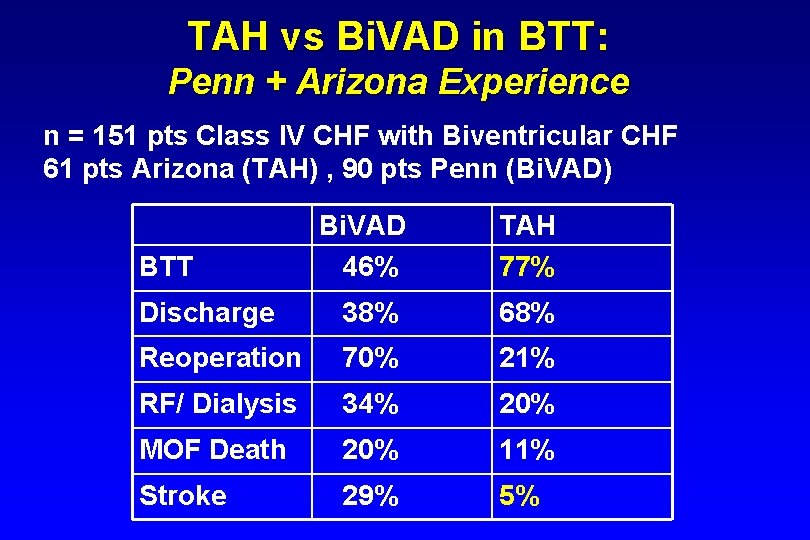
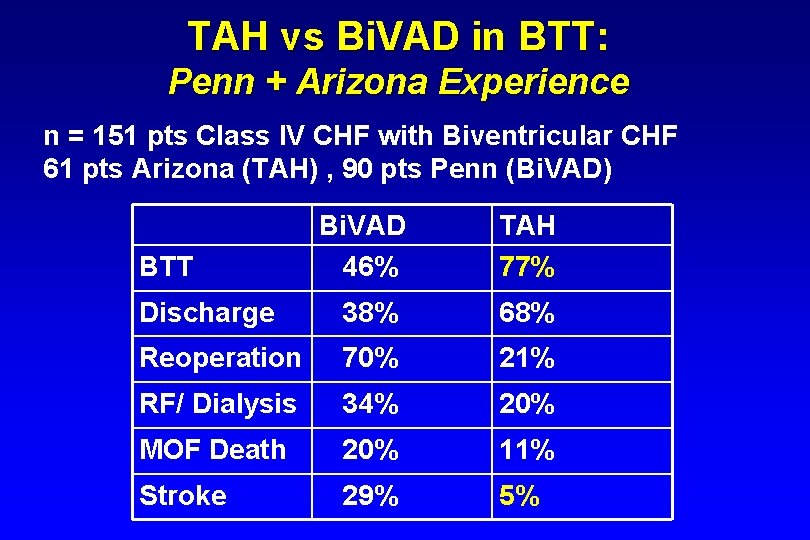
TAH vs Bi. VAD in BTT: Penn + Arizona Experience n = 151 pts Class IV CHF with Biventricular CHF 61 pts Arizona (TAH) , 90 pts Penn (Bi. VAD) Bi. VAD 46% TAH 77% Discharge 38% 68% Reoperation 70% 21% RF/ Dialysis 34% 20% MOF Death 20% 11% Stroke 29% 5% BTT
BIVAD/TAH: Flow vs BSA Cardio. West TAH Thoratec BIVAD Flow L/M
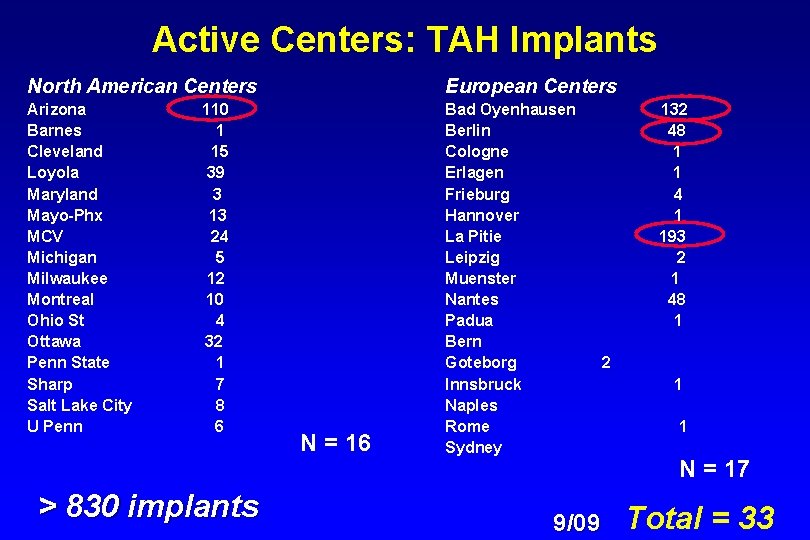
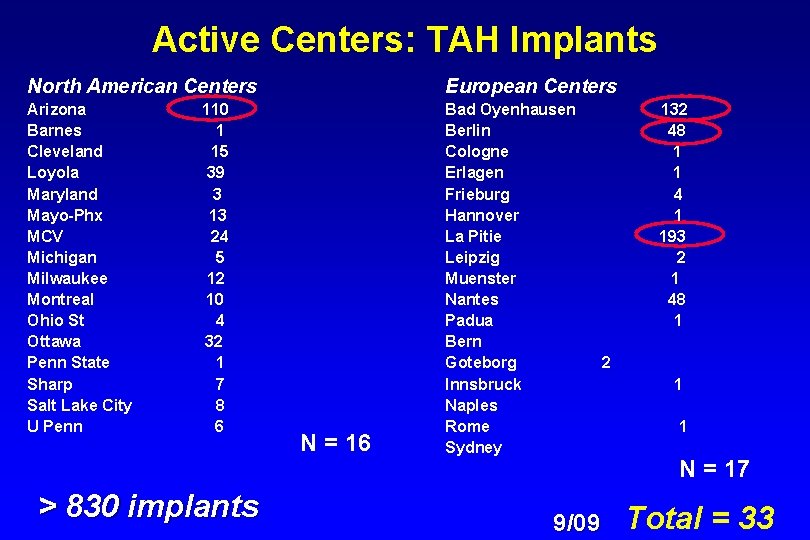
Active Centers: TAH Implants North American Centers European Centers Arizona Barnes Cleveland Loyola Maryland Mayo-Phx MCV Michigan Milwaukee Montreal Ohio St Ottawa Penn State Sharp Salt Lake City U Penn Bad Oyenhausen Berlin Cologne Erlagen Frieburg Hannover La Pitie Leipzig Muenster Nantes Padua Bern Goteborg Innsbruck Naples Rome Sydney 110 1 15 39 3 13 24 5 12 10 4 32 1 7 8 6 > 830 implants N = 16 9/09 132 48 1 1 4 1 193 2 1 48 1 2 1 1 N = 17 Total = 33
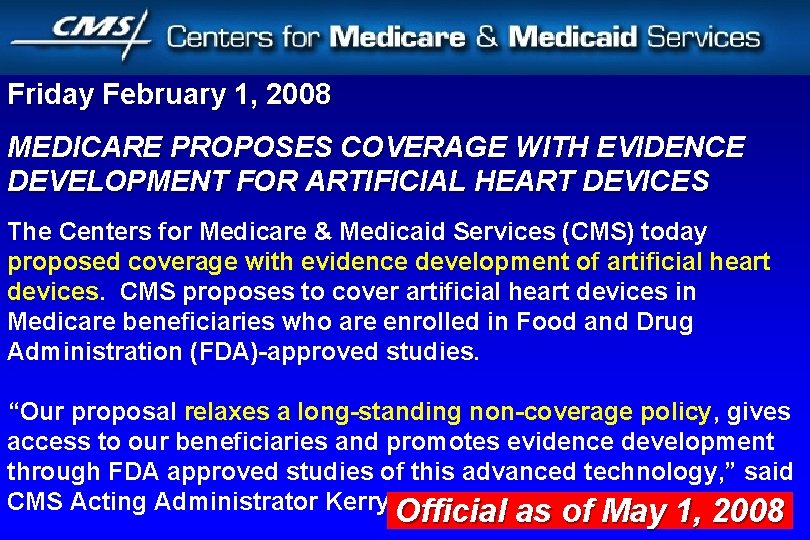
Friday February 1, 2008 MEDICARE PROPOSES COVERAGE WITH EVIDENCE DEVELOPMENT FOR ARTIFICIAL HEART DEVICES The Centers for Medicare & Medicaid Services (CMS) today proposed coverage with evidence development of artificial heart devices. CMS proposes to cover artificial heart devices in Medicare beneficiaries who are enrolled in Food and Drug Administration (FDA)-approved studies. “Our proposal relaxes a long-standing non-coverage policy, gives access to our beneficiaries and promotes evidence development through FDA approved studies of this advanced technology, ” said CMS Acting Administrator Kerry Official Weems. as of May 1, 2008 Official as of May 1, 2008
2008



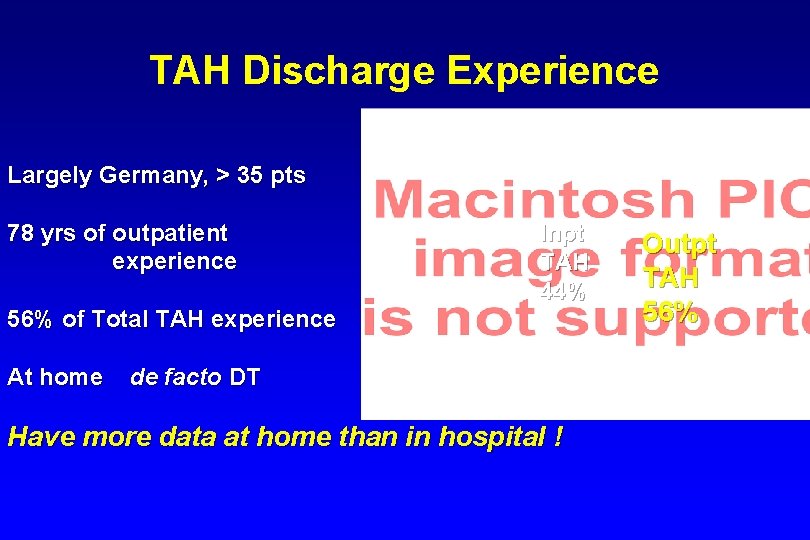
TAH Discharge Experience Largely Germany, > 35 pts 78 yrs of outpatient experience Inpt TAH 44% 56% of Total TAH experience At home de facto DT Have more data at home than in hospital ! Outpt TAH 56%
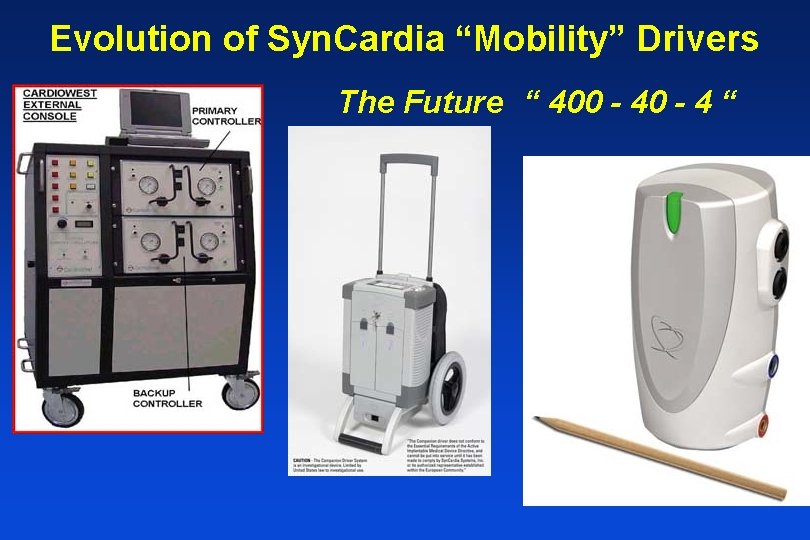
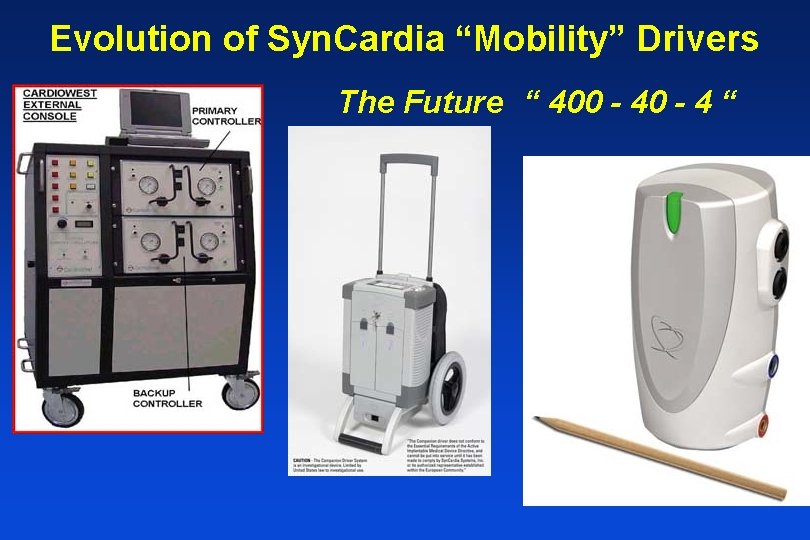
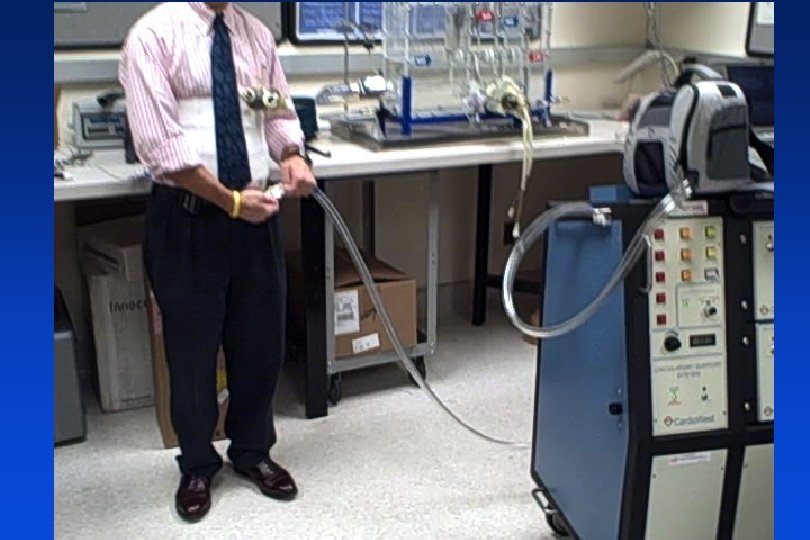
Evolution of Syn. Cardia “Mobility” Drivers The Future “ 400 - 4 “

Syn. Cardia New Replacement TAH-t Driver “Companion System”

Companion Driver. TM


Syn. Cardia Freedom Driver
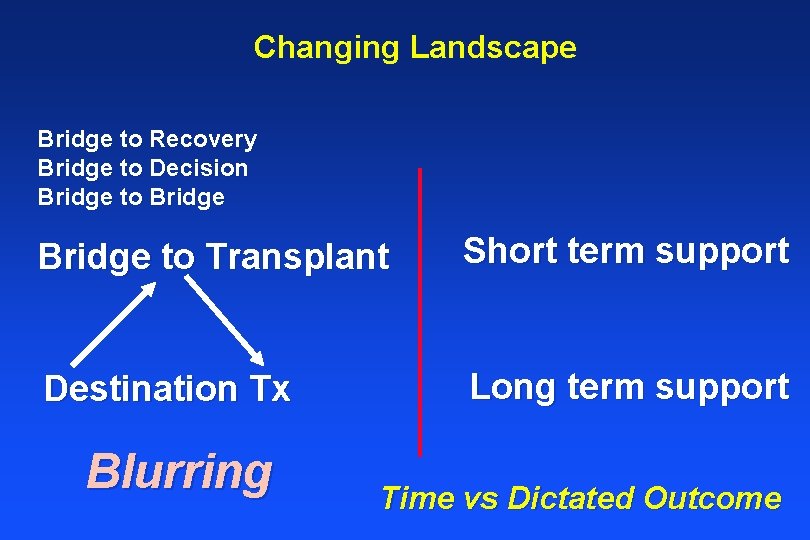
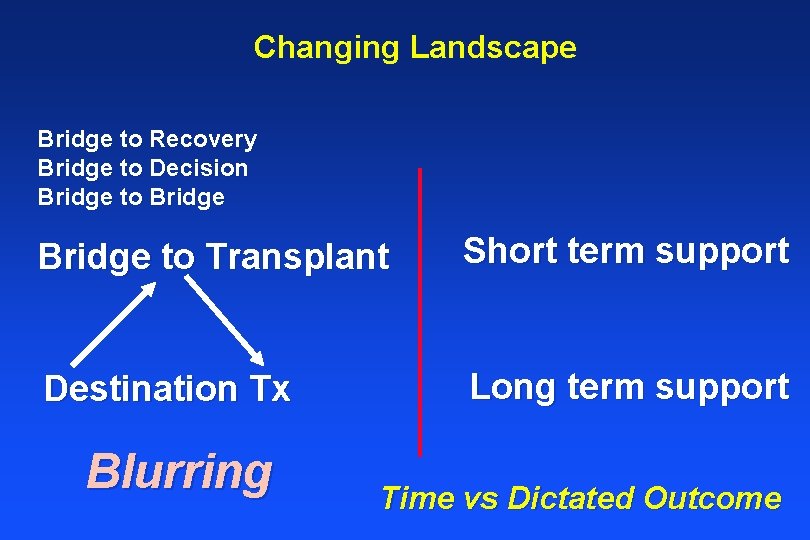
Changing Landscape Bridge to Recovery Bridge to Decision Bridge to Transplant Short term support Destination Tx Long term support Blurring Time vs Dictated Outcome
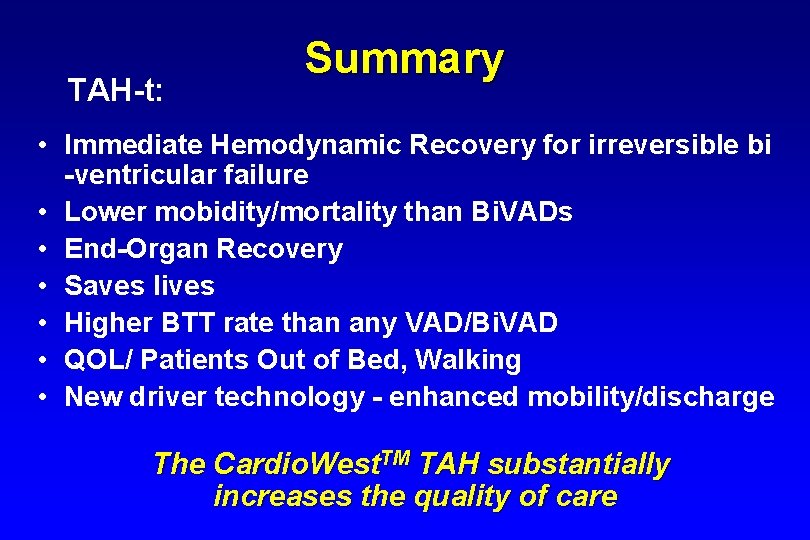
TAH-t: Summary • Immediate Hemodynamic Recovery for irreversible bi -ventricular failure • Lower mobidity/mortality than Bi. VADs • End-Organ Recovery • Saves lives • Higher BTT rate than any VAD/Bi. VAD • QOL/ Patients Out of Bed, Walking • New driver technology - enhanced mobility/discharge The Cardio. West. TM TAH substantially increases the quality of care
 Syn cardia
Syn cardia Pneumocardia
Pneumocardia Syn cardia
Syn cardia Kata sinkronik berasal dari
Kata sinkronik berasal dari Quimo
Quimo Triad of achalasia cardia
Triad of achalasia cardia Valve of kerkring
Valve of kerkring Cardia gaster
Cardia gaster Brandy cardia
Brandy cardia Achalasia of cardia
Achalasia of cardia Achalasia of cardia definition
Achalasia of cardia definition Cardia gaster
Cardia gaster Cardia
Cardia Total order planning in artificial intelligence
Total order planning in artificial intelligence Ejemplo de examen fisico segmentario
Ejemplo de examen fisico segmentario Hipoplazie malara
Hipoplazie malara Site:slidetodoc.com
Site:slidetodoc.com Tonus cardio moderateur
Tonus cardio moderateur Sufijo latria ejemplos
Sufijo latria ejemplos Cardiovision
Cardiovision Trusight cardio
Trusight cardio Nssttc
Nssttc Nébilox
Nébilox Electro cardio gram
Electro cardio gram Softecg
Softecg Hypertension portale
Hypertension portale Index cardio thoracique normal
Index cardio thoracique normal 4tech cardio
4tech cardio Cardio sense
Cardio sense Index cardio thoracique normal
Index cardio thoracique normal Atl cardio
Atl cardio Cardio map
Cardio map Pa cardio
Pa cardio Cauze reversibile de stop cardio-respirator
Cauze reversibile de stop cardio-respirator Semnele stopului cardiorespirator
Semnele stopului cardiorespirator Vddi cardio
Vddi cardio Discovery cardio care programme
Discovery cardio care programme Calcul index cardio thoracique
Calcul index cardio thoracique Horizontal fissure of left lung
Horizontal fissure of left lung Cardio alex
Cardio alex