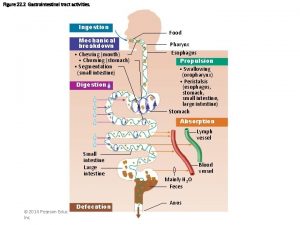
Gastric Motility Functions of gastric motility 1 Store
- Slides: 15
Gastric Motility Functions of gastric motility 1. Store food 2. Gradually release it into small intestine 3. Mix food with gastric secretions
Food Storage in the Stomach can enlarge as food enters, but intragastric pressure is nearly constant at volumes below 1 liter (for most of us). This is called receptive relaxation. At higher volumes, intragastric pressure increases dramatically. Mechanism: Smooth muscle can change length over a wide range with little change in resting tension. In the stomach, this occurs via a reflex mediated by the vagus nerve.
Mixing and Propulsion of Gastric Contents When stomach isn’t empty, peristalsis occurs in stomach. Gastric peristalsis begins in fundus, travels to antrum. Antral muscle is thicker than elsewhere, so antral contractions are stronger. Lumen in peristaltic wave is pretty big, so mixing occurs as content moves in both directions. Since gastroduodenal sphincter is normally partly open, each peristaltic wave pushes some gastric content into duodenum (first segment of small intestine). This is the mechanism of stomach emptying The greater the volume in the stomach, the more frequent the peristaltic waves. Thus, the rate of stomach emptying is related to the amount in the stomach.
Control of Gastric Peristalsis Local, as described. There also neural and humoral controls. Distension activates stretch receptors in gastric wall. This initiates short and long reflexes that increase gastric motility Partially digested protein causes release of the hormone, gastrin, from G-cells in the antrum. Gastrin is secreted into circulation, reaches gastric muscle cells and stimulates gastric peristalsis. Duodenal cells secrete hormones in response to fat and acidity. They reach the stomach via the circulation and inhibit gastric peristalsis. There also neural reflexes originating in the duodenum that inhibit gastric peristalsis. Some involve the little brain, some involve the CNS Why does a high fat meal increase alcohol tolerance?
Gastric Secretion There are 1 -2 liters of saliva per day; the stomach secretes 2 -3 liters/day. That’s about 4 liters/day, not counting what we ingest. Three kinds of gastric glands secrete into the lumen 1. Mucus, secreted by mucous cells (= mucous neck cells) 2. Pepsinogen, a protease precursor secreted by chief cells 3. HCl, secreted by parietal cells Parietal cells secrete 300 m. Osm HCl (p. H = 1 -2). This acidifies lumen, converting pepsinogen into pepsin and providing the low p. H at which pepsin works best, breaks down ingested connective tissue, and is bactericidal. Gastric p. H falls from 7. 8 to 4 within 20 minutes of eating. Gastrin (secreted by G-cells in response to partially digested protein in stomach) stimulates gastric motility and HCl secretion.
Control of Gastric HCl Secretion 1. Cephalic phase: Sight or smell of food, food in the mouth, activate conditioned reflexes that elicit HCl secretion before food enters stomach. Efferent arm of the reflex is vagal stimulation of parietal cells and submucosal plexus, which then stimulates G-cells. 2. Gastric phase: Partially digested protein in stomach stimulates parietal and G-cells via submucosal plexus. Gastric distension stimulates G-cells via submucosal plexus. Low p. H in stomach inhibits G-cells 3. Intestinal phase: Same systems in duodenum that inhibit gastric motility also inhibit gastric secretion of HCl
Gastric Secretion of Pepsinogen Chief cells secrete pepsinogen, precursor of the only gastric enzyme, pepsin (a protease). Conversion of pepsinogen to pepsin is initiated by acidity in stomach, then by pepsin itself. Optimum for protein digestion by pepsin is p. H 2 to 3; intragastric p. H is maintained around that level. Protein digestion is quite incomplete in stomach, although some proteins is digested to amino acids. In addition to protein being partly digested in stomach, there is some starch hydrolysis from swallowed salivary amylase. It doesn’t work below p. H 4, so gastric starch digestion only occurs during first 20 minutes or so of a meal. On the other hand, salivary amylase digests more starch in the stomach than in the mouth.
Absorption in the Stomach There’s no active reabsorption in the stomach, although a few things can diffuse into the circulation across the stomach wall. Most notable is alcohol. More about this soon.
Pancreatic Secretion of Sodium Bicarbonate “Pancreas” = exocrine pancreas. Endocrine pancreas will come later. Pancreatic cells are arranged in clusters called acini; they’re acinar cells. They secrete into ducts that empty into pancreatic duct, which leads to the proximal end of the duodenum. Pancreatic secretions are alkaline (iso-osmotic sodium bicarbonate solutions), and neutralize gastric acid. The alkalinity also provides optimal p. H for the many digestive enzymes secreted by acinar cells. For anyone interested, the chemistry of bicarbonate secretion is described in Sherwood. It’s similar to the one by which parietal cells secrete HCl, but in the opposite direction. Net effect of gastric secretion of HCl and pancreatic secretion of sodium bicarbonate is that plasma p. H is unaffected.
Pancreatic Secretion of Digestive Enzymes There are pancreatic enzymes that can digest every digestible thing we eat. Pancreatic proteases (trypsin, chymotrypsin, aminopeptidase, carboxypeptidase, and a few others) are secreted as inactive precursors (“proenzymes”). Enterokinase is a protease secreted into the duodenal lumen by glands in the submucosa. It converts trypsinogen to trypsin. Trypsin converts more trypsinogen to trypsin, also converts the other protease proenzymes to active forms.
Pancreatic amylase hydrolyzes starch (and starch partly digested by salivary amylase) into disaccharides – molecules consisting of two simple sugar molecules joined together. Pancreatic lipases digest various kinds of lipids. Triglycerides, the most common dietary fats, are digested into free fatty acids and glycerol. Pancreatic nucleases digest RNA and DNA.
Control of Pancreatic Secretion Mainly via hormones secreted into circulation by cells of duodenum. Secretin, secreted in response to acidity in duodenum, elicits bicarbonate secretion by pancreas Cholecystokinin (= CCK) is secreted in response to partially digested protein and fat. It stimulates enzyme secretion by pancreas.
Hepatic Secretion Liver secretes bile. Important thing in bile is bile salts, which are detergents. They reduce surface tension at oil/water interfaces, reducing the size of fat droplets (that’s what the detergent you use to wash dishes does). Reducing size of fat droplets increases surface-to-volume ratio of fat. Lipases act only on the surfaces of fat droplets, so this greatly increases rate of fat digestion. Bile is more or less continuously produced. It flows into gallbladder, where it’s stored. Gallbladder vigorously reabsorbs Na, water follows osmotically. This concentrates bile. CCK (secreted into bloodstream by duodenal cells in response to fat and partially digested protein) stimulates gallbladder contraction. This forces bile into duodenum.
Enterohepatic Circulation Bile salts adhere to intestinal fat droplets. As fats are digested and absorbed, bile salts end up in lumen of intestine. Ileum (distal fourth of small intestine) has active transport systems that reabsorb bile salts, so very little is lost in feces. Splanchnic circulation takes them straight back to the liver. They’re removed from the circulation by liver, secreted into bile again. The cycle of secretion by the liver and reabsorption from circulation by the liver is called enterohepatic circulation.
Regulation of Hepatic Secretion Most hepatic secretion is bile salts that were reabsorbed from the ileum. They are actively transported from the hepatic cells into the bile ducts; water follows osmotically. Since the transport rate depends on bile salt concentration in liver, the most bile is secreted when the most bile salts are being reabsorbed. Thus, bile secretion is highest during digestion of a meal, lowest during fasting. This is why people without gallbladders do OK – the surgery that removes the gallbladder re-routes the bile from the liver straight to the duodenum. People without gallbladders don’t do so well with high fat meals because they can’t accelerate delivery of concentrated bile to duodenum. Having a high fat meal causes fatty diarrhea for them. They rarely do it more than once.
 Row store vs column store
Row store vs column store Row store vs column store
Row store vs column store Entamoeba histolytica motility
Entamoeba histolytica motility üyou
üyou Motility vs mobility
Motility vs mobility Mr test
Mr test Motility test positive and negative
Motility test positive and negative Salmonella
Salmonella Hanging drop method diagram
Hanging drop method diagram Reproduccion bacteriana
Reproduccion bacteriana Opalescent sperm
Opalescent sperm Absolute value function to piecewise function
Absolute value function to piecewise function Evaluating functions
Evaluating functions Evaluating functions and operations on functions
Evaluating functions and operations on functions Gastric gland
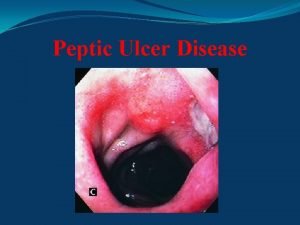
Gastric gland Ulcers in the antrum
Ulcers in the antrum