Esophageal function testing Esophageal motility disorders in highresolution








- Slides: 44
Esophageal function testing: Esophageal motility disorders in high-resolution Dustin Carlson, MD, MSCI Assistant Professor of Medicine - Gastroenterology Northwestern University Director, Mario Tonelli Esophageal Function Lab Esophageal Center of Northwestern
Disclosures • Consulting (Medtronic, Inc) • Speaker (Medtronic, Inc) • License agreement surrounding FLIP panometry systems, methods, and apparatus granting rights to U. S. Patent Application Number 15/546, 986 and Canadian Patent Application Number 2, 975, 603 (Medtronic, Inc)
Esophageal Motility Evaluation OBJECTIVES 1. Understand indications and standard methods for evaluating esophageal motility and function 2. Understand the diagnostic approach and basic therapeutic strategies in achalasia 3. Appreciate the clinical implications of esophageal motility diagnosis beyond achalasia
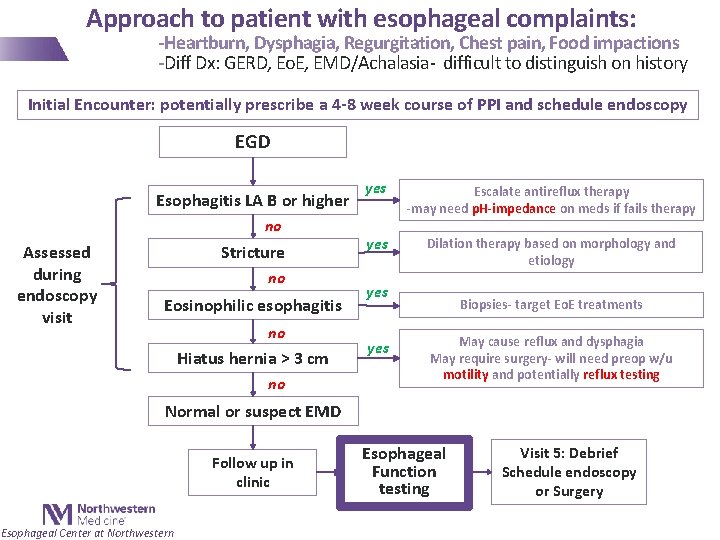
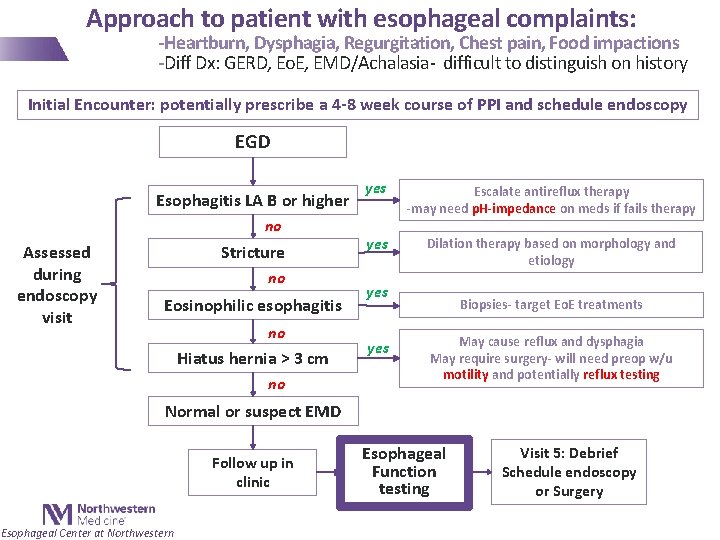
Approach to patient with esophageal complaints: -Heartburn, Dysphagia, Regurgitation, Chest pain, Food impactions -Diff Dx: GERD, Eo. E, EMD/Achalasia- difficult to distinguish on history Initial Encounter: potentially prescribe a 4 -8 week course of PPI and schedule endoscopy EGD Esophagitis LA B or higher no Assessed during endoscopy visit Stricture no Eosinophilic esophagitis no Hiatus hernia > 3 cm no yes Escalate antireflux therapy -may need p. H-impedance on meds if fails therapy yes Dilation therapy based on morphology and etiology yes Biopsies- target Eo. E treatments May cause reflux and dysphagia May require surgery- will need preop w/u motility and potentially reflux testing Normal or suspect EMD Follow up in clinic Esophageal Center at Northwestern Esophageal Function testing Visit 5: Debrief Schedule endoscopy or Surgery
Esophageal function testing • Esophageal reflux (p. H) monitoring - Evaluation of non-erosive gastroesophageal reflux: objective GERD diagnosis - Wireless (Bravo™) • 48 -96 hours - Catheter based (with or without impedance) • 24 hours • Esophageal manometry - High resolution manometry (HRM) - Evaluation of esophageal motility - Indications: 1. Non-obstructive dysphagia 2. Prior to anti-reflux surgery Esophageal Center at Northwestern
The manometry study • Transnasal catheter placement - After application of topical anesthetic to nare (lidocaine) • Catheter positioned spanning from oropharynx to a few cm into the stomach • Baseline recording/basal EGJ pressure • 10 supine, 5 -ml liquid swallows - Basis for Chicago Classification of esophageal motility diagnoses - Requires awake patient • +/-Supplementary maneuvers Esophageal Center at Northwestern
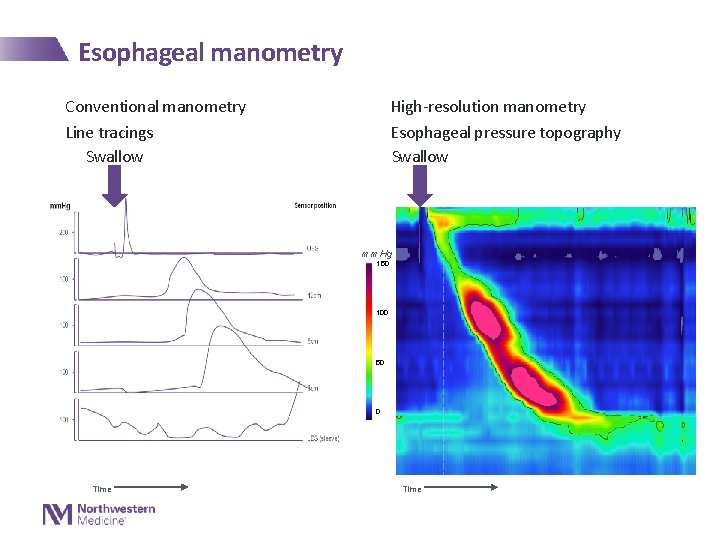
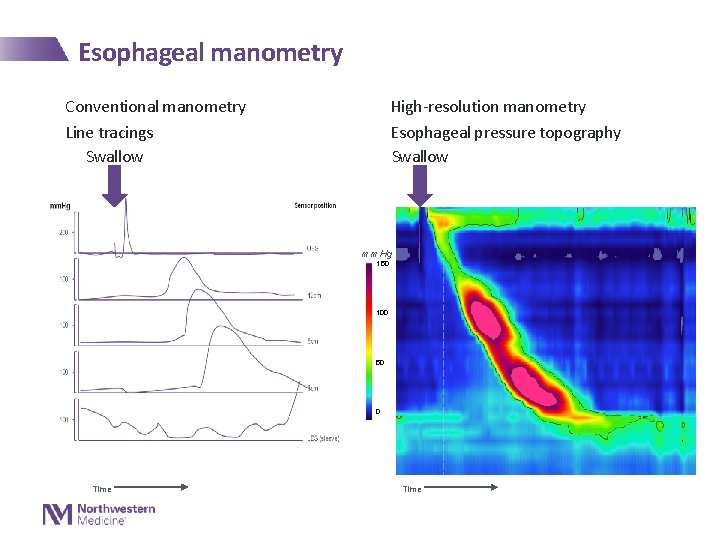
Esophageal manometry Conventional manometry Line tracings Swallow High-resolution manometry Esophageal pressure topography Swallow mm. Hg 150 100 50 0 Time
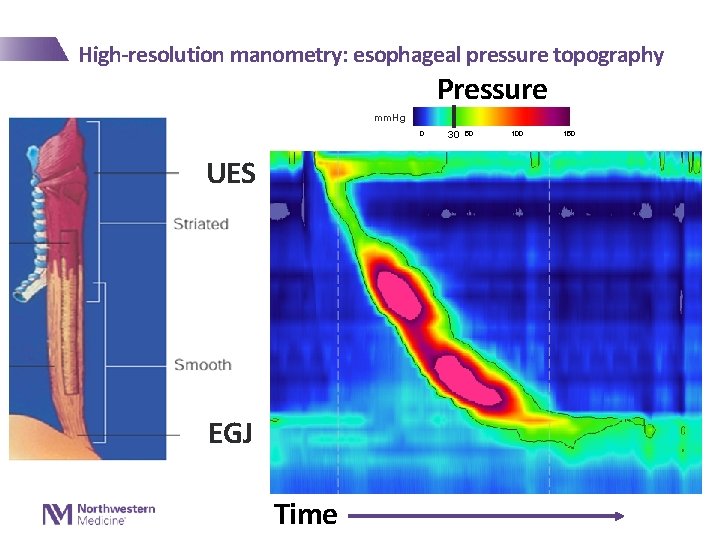
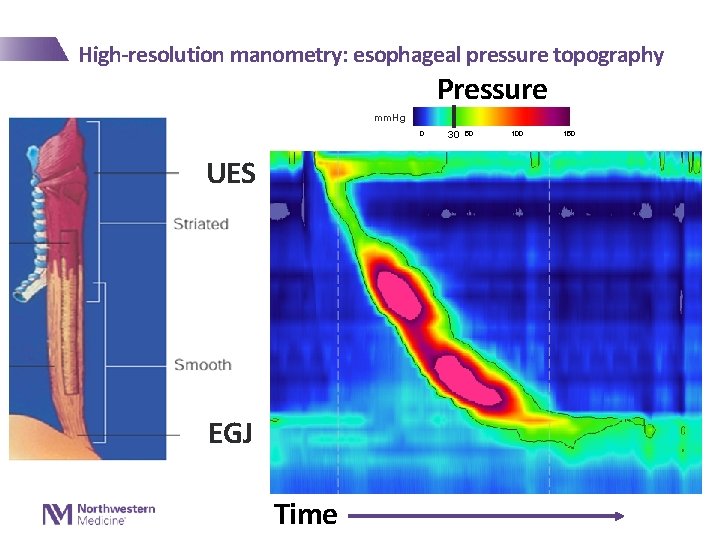
High-resolution manometry: esophageal pressure topography Pressure mm. Hg 0 UES EGJ Time 30 50 100 150
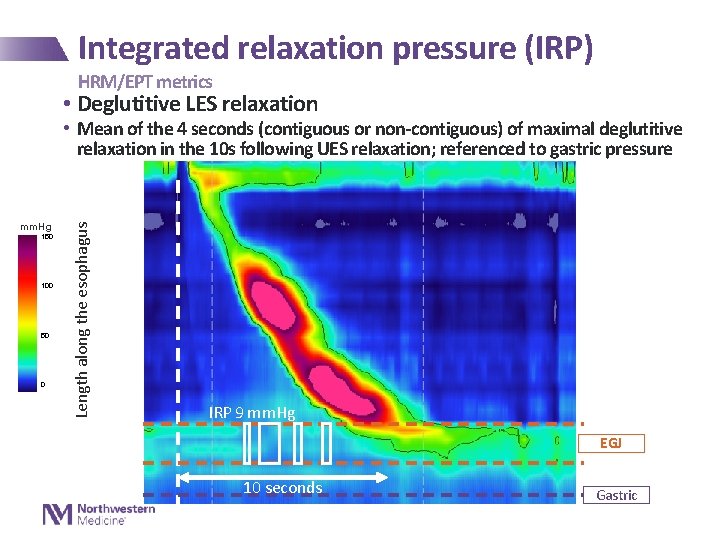
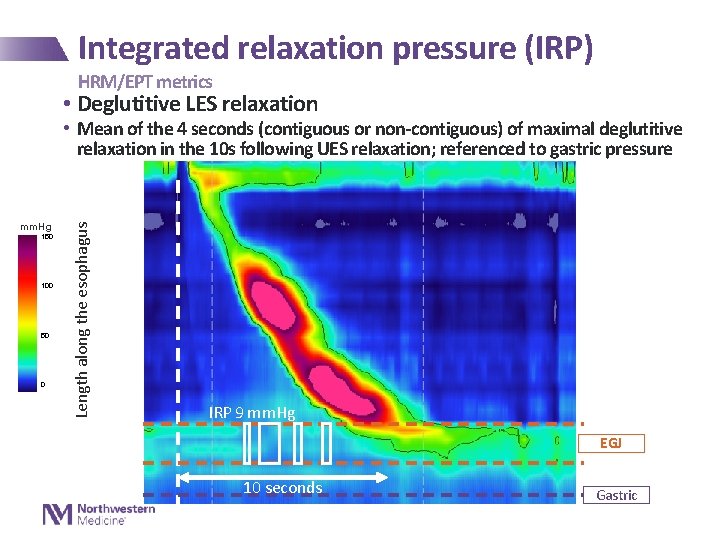
Integrated relaxation pressure (IRP) HRM/EPT metrics • Deglutitive LES relaxation mm. Hg 150 100 50 0 Length along the esophagus • Mean of the 4 seconds (contiguous or non-contiguous) of maximal deglutitive relaxation in the 10 s following UES relaxation; referenced to gastric pressure IRP 9 mm. Hg EGJ 10 seconds Gastric

Distal latency HRM/EPT metrics • Deglutitive inhibition of esophageal contraction • Time from swallow onset (UES relaxation) to contractile deceleration point (CDP) mm. Hg 150 100 50 30 0 Length along the esophagus UES Distal latency 7 seconds LES
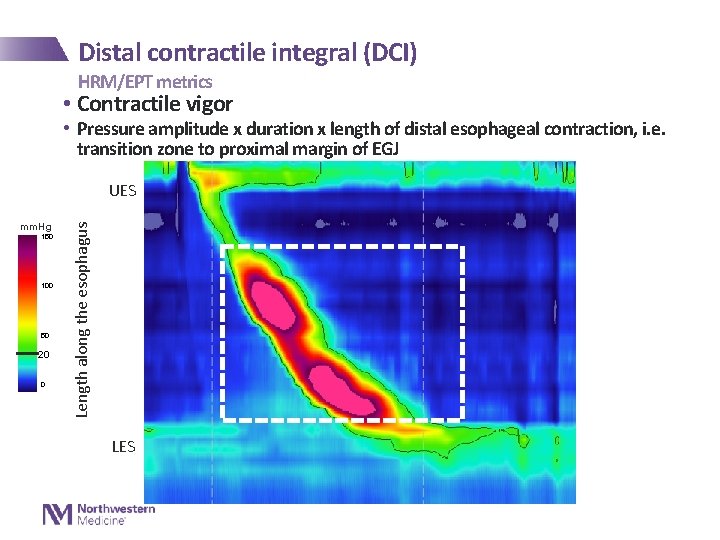
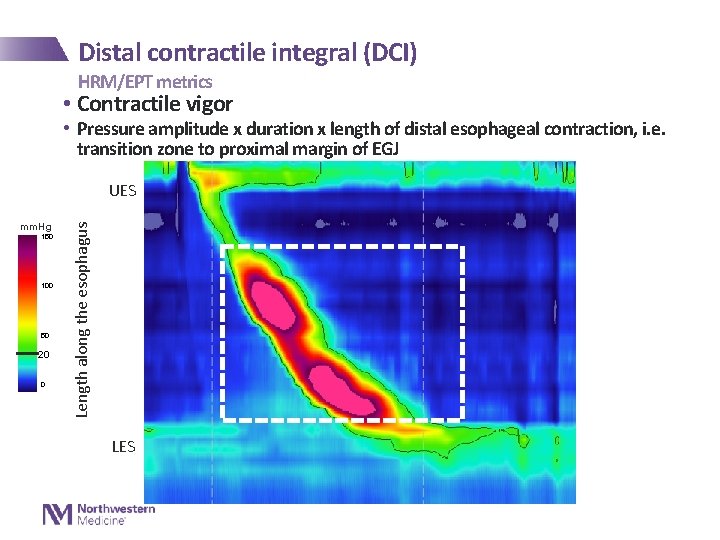
Distal contractile integral (DCI) HRM/EPT metrics • Contractile vigor • Pressure amplitude x duration x length of distal esophageal contraction, i. e. transition zone to proximal margin of EGJ mm. Hg 150 100 50 20 0 Length along the esophagus UES LES
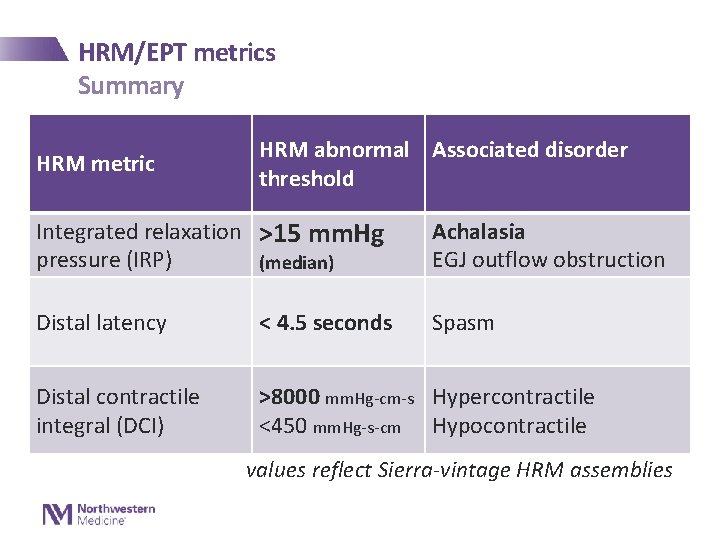
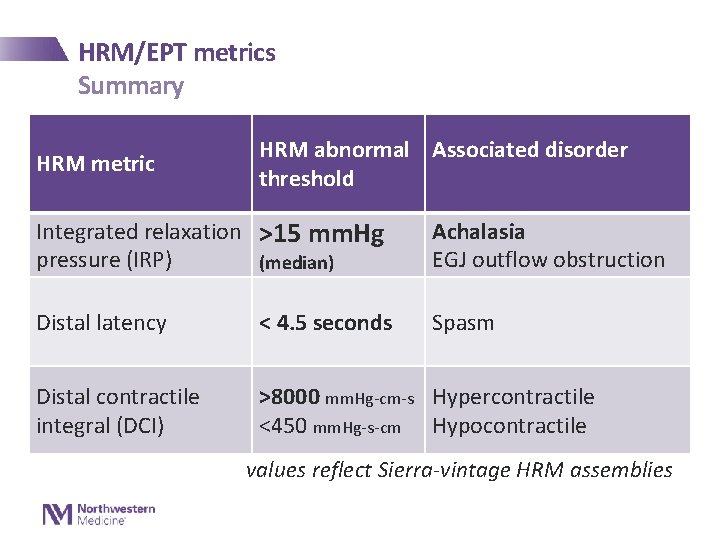
HRM/EPT metrics Summary HRM metric HRM abnormal Associated disorder threshold Integrated relaxation >15 mm. Hg pressure (IRP) (median) Achalasia EGJ outflow obstruction Distal latency < 4. 5 seconds Spasm Distal contractile integral (DCI) >8000 mm. Hg-cm-s Hypercontractile <450 mm. Hg-s-cm Hypocontractile values reflect Sierra-vintage HRM assemblies
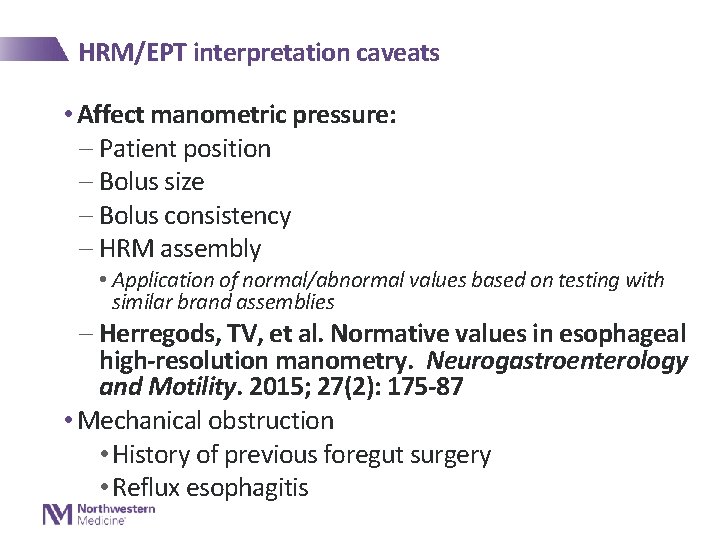
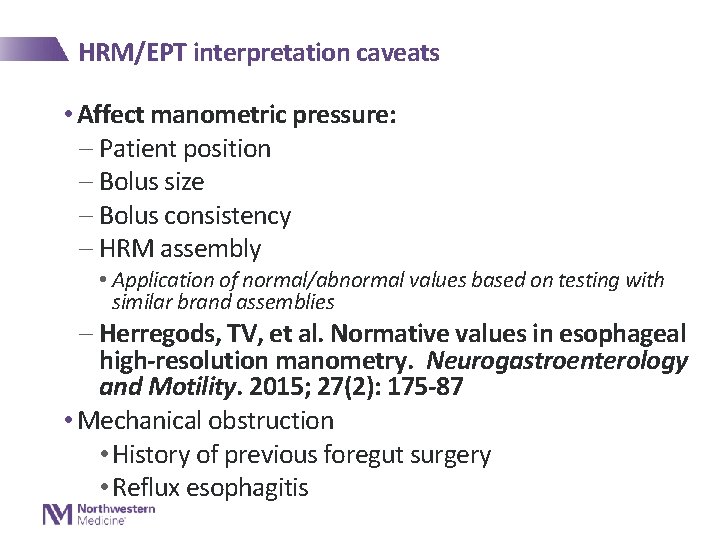
HRM/EPT interpretation caveats • Affect manometric pressure: - Patient position - Bolus size - Bolus consistency - HRM assembly • Application of normal/abnormal values based on testing with similar brand assemblies - Herregods, TV, et al. Normative values in esophageal high-resolution manometry. Neurogastroenterology and Motility. 2015; 27(2): 175 -87 • Mechanical obstruction • History of previous foregut surgery • Reflux esophagitis

HRM/EPT interpretation • Chicago classification of esophageal motility disorders - Evaluation for primary motor disorders • Patients evaluated for dysphagia or esophageal chest pain • Patients without previous foregut surgery or mechanical obstruction - Based on supine, 5 -ml, liquid swallows Kahrilas, et al. Neurogastroenterology and Motility. 2015; 27(2) Pandolfino et al, Amer J Gastroenterology. 2008 103(1): 627 -35
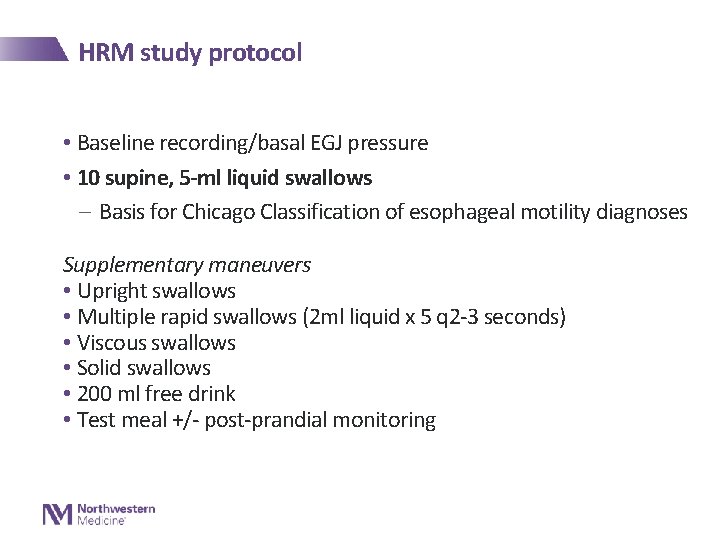
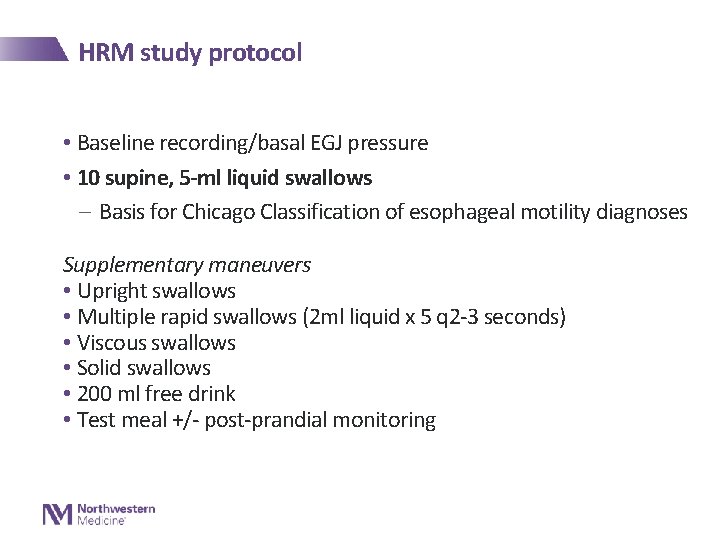
HRM study protocol • Baseline recording/basal EGJ pressure • 10 supine, 5 -ml liquid swallows - Basis for Chicago Classification of esophageal motility diagnoses Supplementary maneuvers • Upright swallows • Multiple rapid swallows (2 ml liquid x 5 q 2 -3 seconds) • Viscous swallows • Solid swallows • 200 ml free drink • Test meal +/- post-prandial monitoring
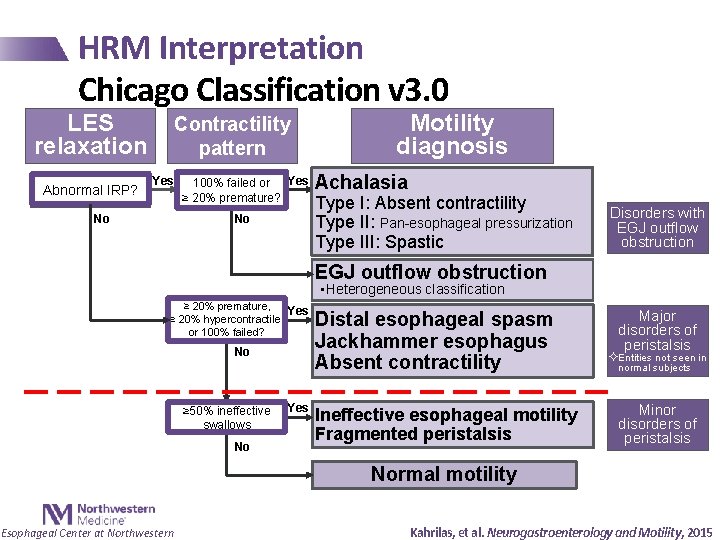
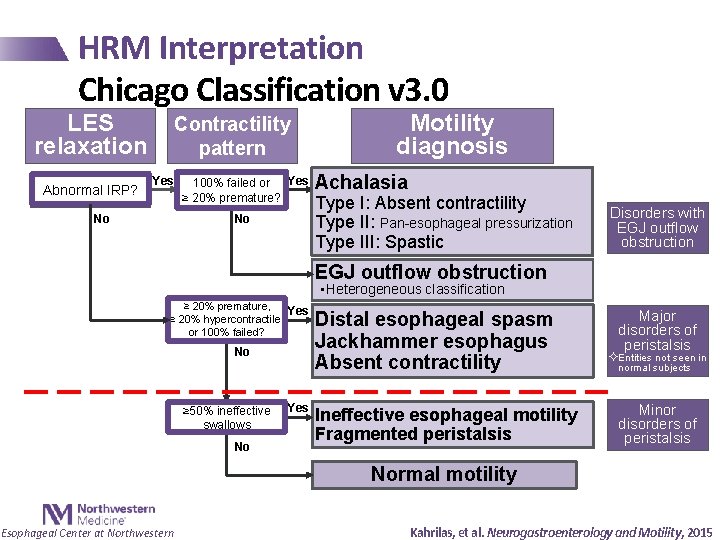
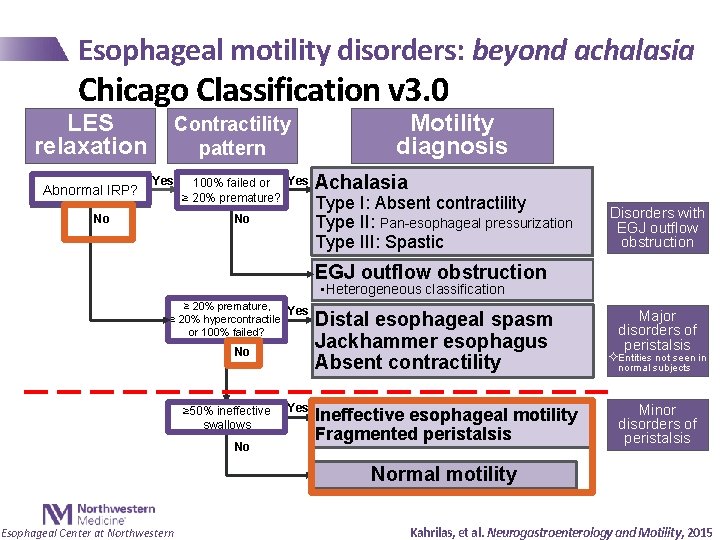
HRM Interpretation Chicago Classification v 3. 0 LES relaxation Abnormal IRP? Contractility pattern Yes No 100% failed or Yes ≥ 20% premature? No Motility diagnosis Achalasia Type I: Absent contractility Type II: Pan-esophageal pressurization Type III: Spastic Disorders with EGJ outflow obstruction • Heterogeneous classification ≥ 20% premature, Yes ≥ 20% hypercontractile, or 100% failed? No ≥ 50% ineffective swallows No Yes Distal esophageal spasm Jackhammer esophagus Absent contractility Ineffective esophageal motility Fragmented peristalsis Major disorders of peristalsis ²Entities not seen in normal subjects Minor disorders of peristalsis Normal motility Esophageal Center at Northwestern Kahrilas, et al. Neurogastroenterology and Motility, 2015
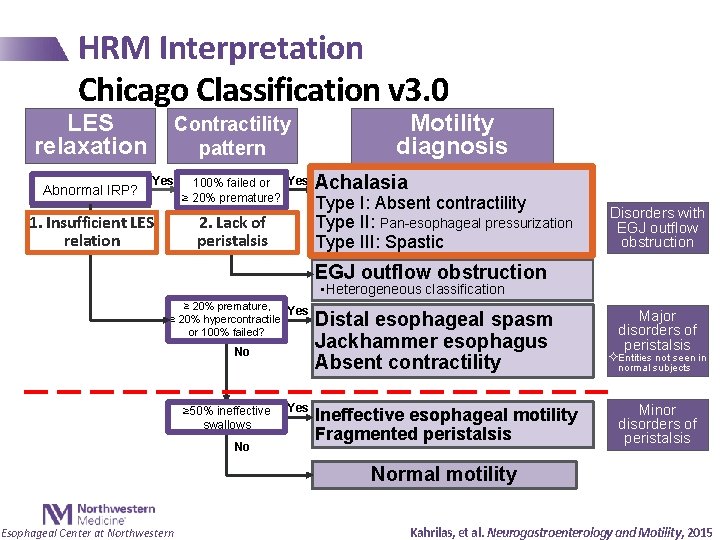
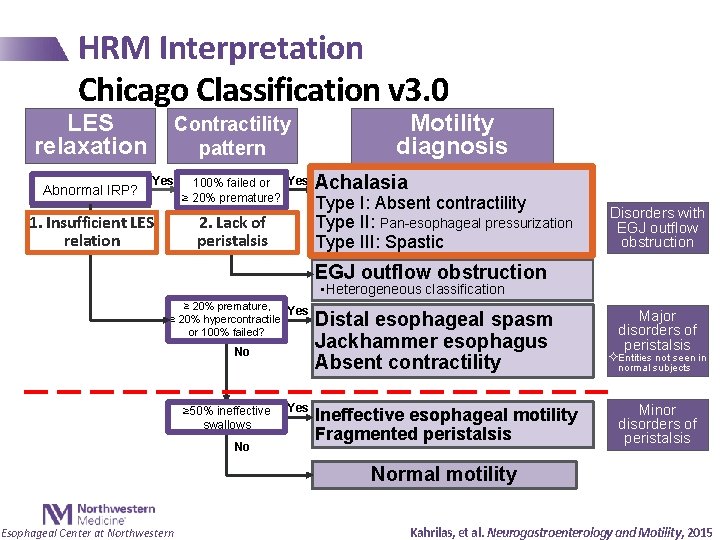
HRM Interpretation Chicago Classification v 3. 0 LES relaxation Abnormal IRP? Contractility pattern Yes 100% failed or Yes ≥ 20% premature? Noof 2. Lack No 1. Insufficient LES peristalsis relation Motility diagnosis Achalasia Type I: Absent contractility Type II: Pan-esophageal pressurization Type III: Spastic Disorders with EGJ outflow obstruction • Heterogeneous classification ≥ 20% premature, Yes ≥ 20% hypercontractile, or 100% failed? No ≥ 50% ineffective swallows No Yes Distal esophageal spasm Jackhammer esophagus Absent contractility Ineffective esophageal motility Fragmented peristalsis Major disorders of peristalsis ²Entities not seen in normal subjects Minor disorders of peristalsis Normal motility Esophageal Center at Northwestern Kahrilas, et al. Neurogastroenterology and Motility, 2015

Achalasia • Most well defined esophageal motility disorder • Diagnosis: - Abnormal LES relaxation pressure • IRP > upper limit of normal (e. g. 15 mm. Hg) - Absent (type I and II) or spastic (type III) contractility Esophageal Center at Northwestern
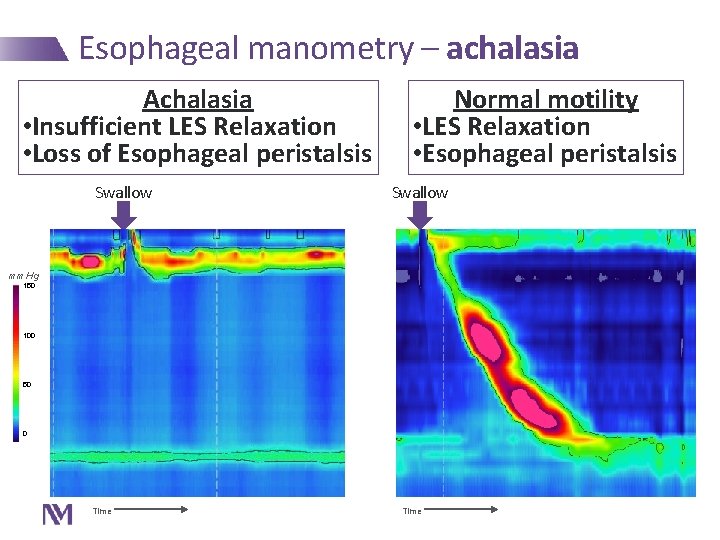
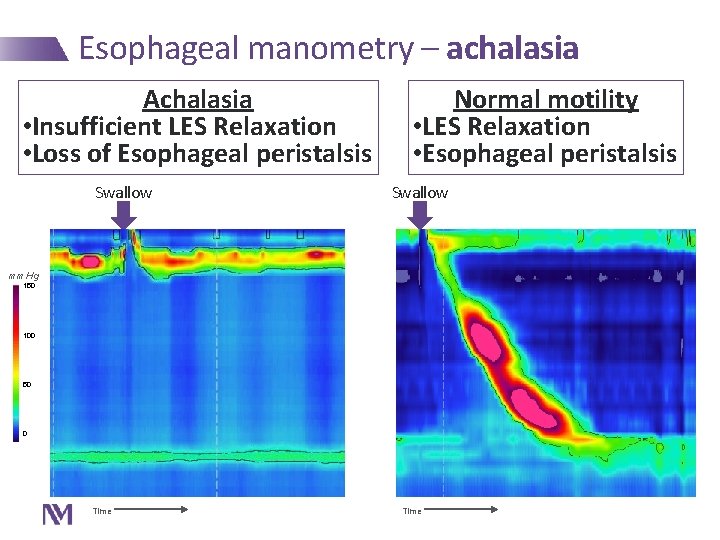
Esophageal manometry – achalasia Achalasia • Insufficient LES Relaxation • Loss of Esophageal peristalsis Swallow Normal motility • LES Relaxation • Esophageal peristalsis Swallow mm. Hg 150 100 50 0 Time
Achalasia • Most well defined esophageal motility disorder • Diagnosis: - Abnormal LES relaxation pressure • IRP > upper limit of normal (e. g. 15 mm. Hg) - Absent (type I and II) or spastic (type III) contractility • Effective interventions - Pneumatic dilation - Laparoscopic Heller’s myotomy - POEM (Per-Oral Endoscopic Myotomy) - Botulinum toxin injection Esophageal Center at Northwestern
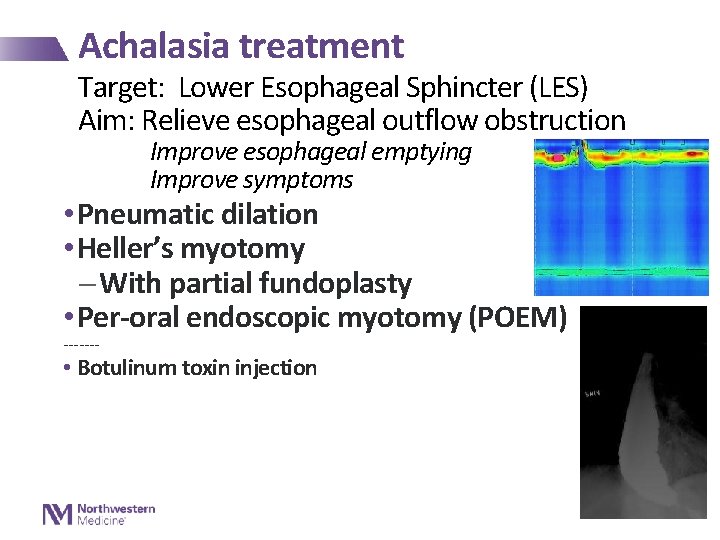
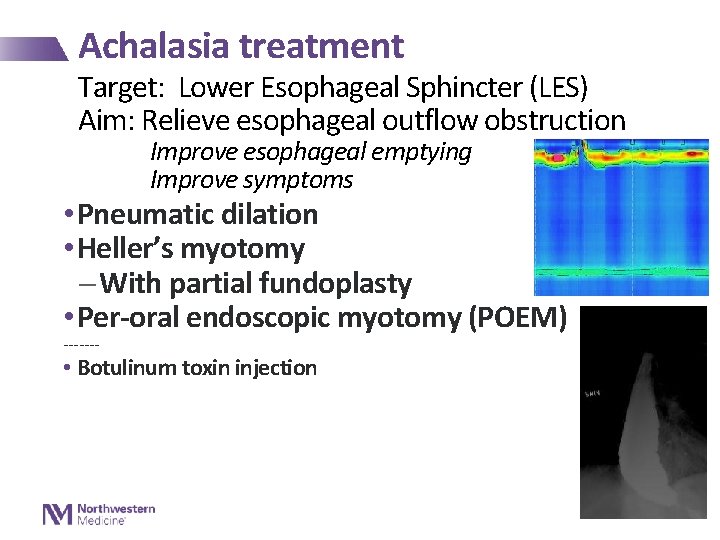
Achalasia treatment Target: Lower Esophageal Sphincter (LES) Aim: Relieve esophageal outflow obstruction Improve esophageal emptying Improve symptoms • Pneumatic dilation • Heller’s myotomy - With partial fundoplasty • Per-oral endoscopic myotomy (POEM) ------- • Botulinum toxin injection
Achalasia treatment • Botulinum toxin injection - Endoscopic - Pre-synaptic inhibition of acetylcholine release - ~50% reduction in LES pressure - 6 -24 month duration of effect - Typically reserved for non-surgical (or pneumatic dilation) candidates Vaezi, M, et al. ACG clinical guidelines. Amer J of Gastroenterol. 2013; 108.
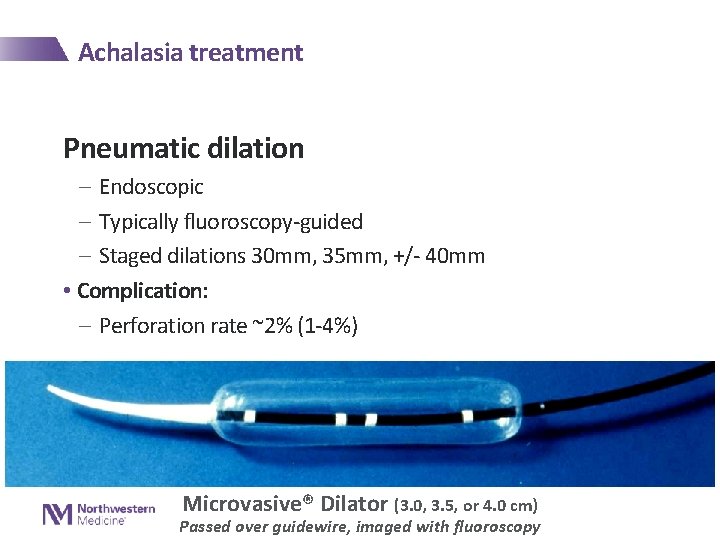
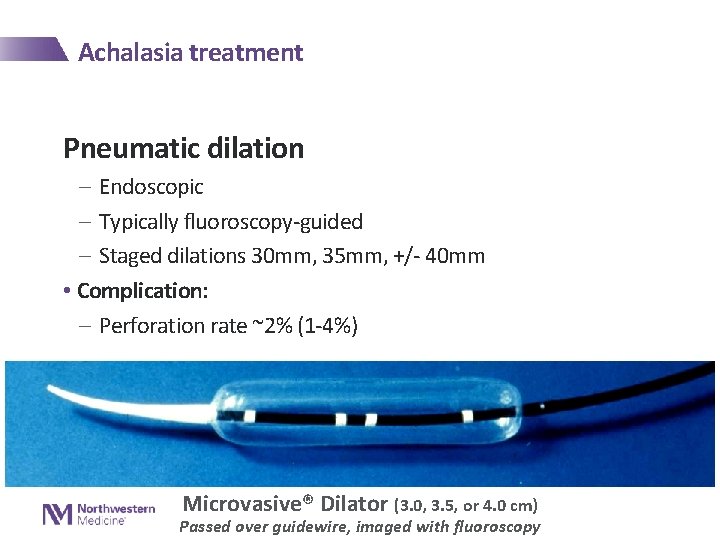
Achalasia treatment Pneumatic dilation - Endoscopic - Typically fluoroscopy-guided - Staged dilations 30 mm, 35 mm, +/- 40 mm • Complication: - Perforation rate ~2% (1 -4%) Microvasive® Dilator (3. 0, 3. 5, or 4. 0 cm) Passed over guidewire, imaged with fluoroscopy
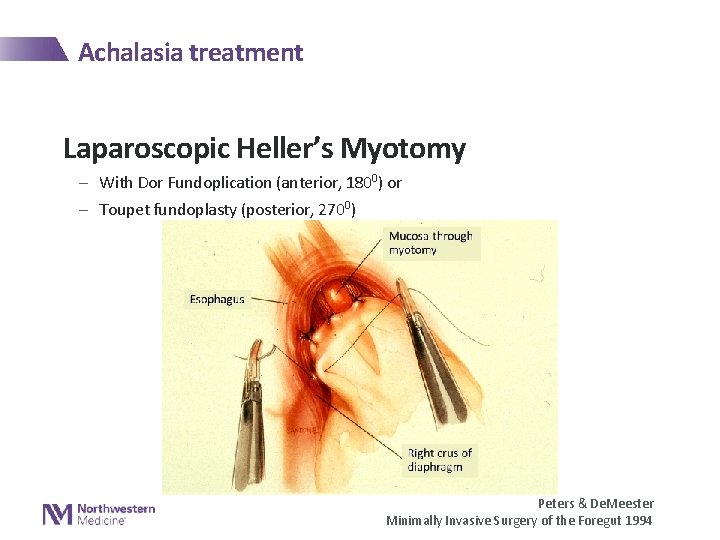
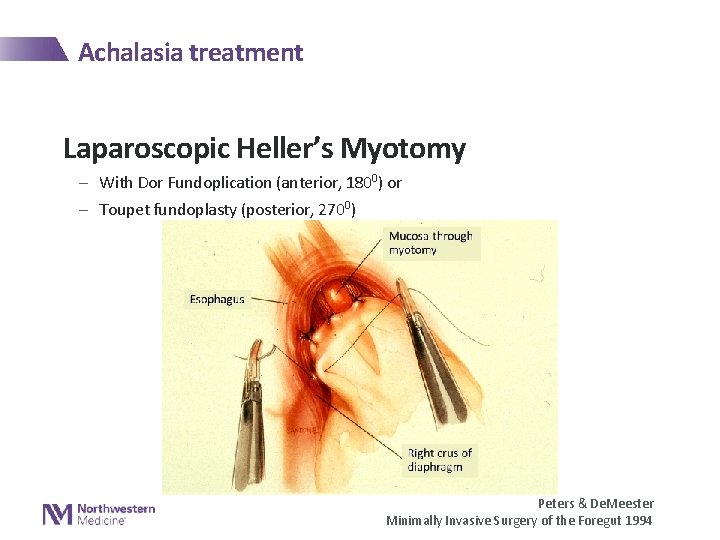
Achalasia treatment Laparoscopic Heller’s Myotomy - With Dor Fundoplication (anterior, 1800) or - Toupet fundoplasty (posterior, 2700) Peters & De. Meester Minimally Invasive Surgery of the Foregut 1994
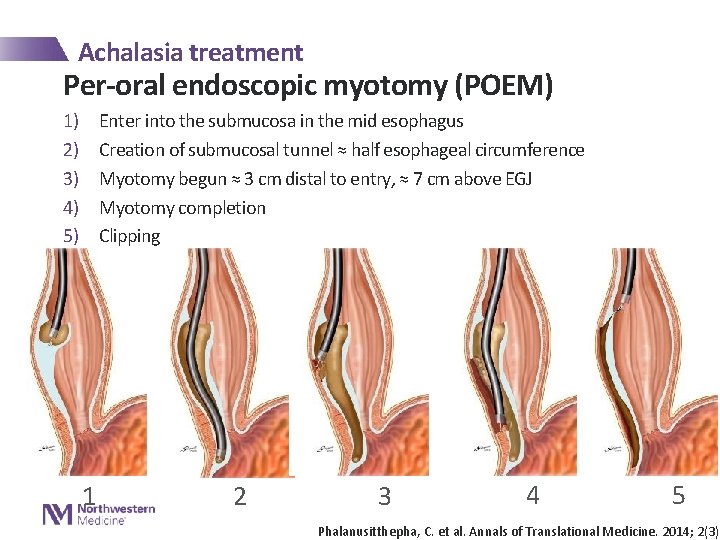
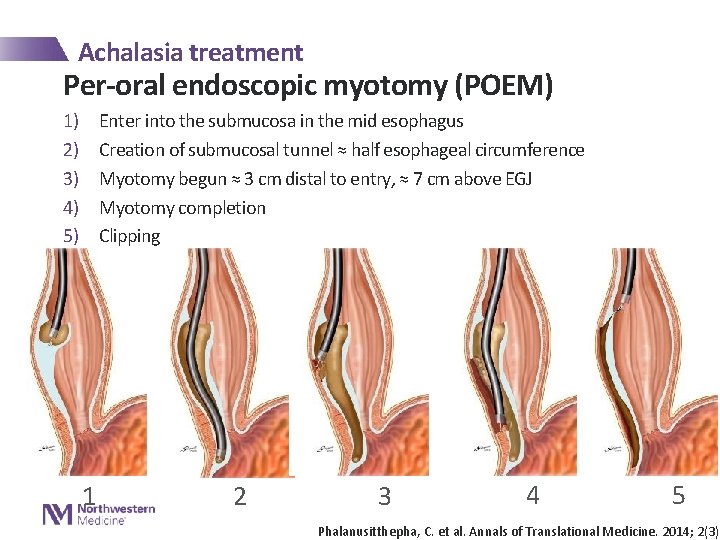
Achalasia treatment Per-oral endoscopic myotomy (POEM) 1) 2) 3) 4) 5) Enter into the submucosa in the mid esophagus Creation of submucosal tunnel ≈ half esophageal circumference Myotomy begun ≈ 3 cm distal to entry, ≈ 7 cm above EGJ Myotomy completion Clipping 1 2 3 4 5 Phalanusitthepha, C. et al. Annals of Translational Medicine. 2014; 2(3)
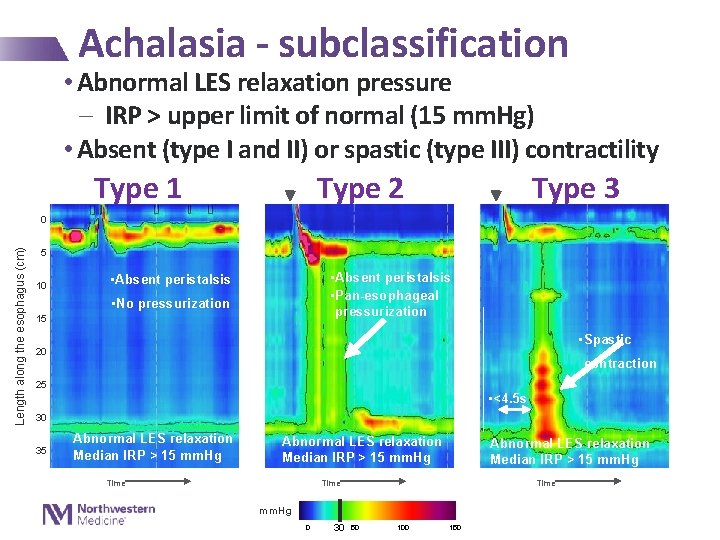
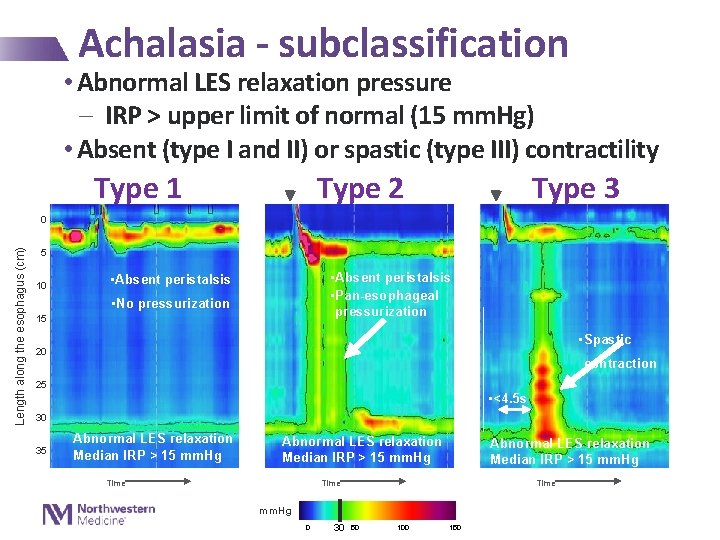
Achalasia - subclassification • Abnormal LES relaxation pressure - IRP > upper limit of normal (15 mm. Hg) • Absent (type I and II) or spastic (type III) contractility Type 1 Type 2 Type 3 Length along the esophagus (cm) 0 5 10 • Absent peristalsis • Pan-esophageal pressurization • Absent peristalsis • No pressurization 15 • Spastic 20 contraction 25 • <4. 5 s 30 35 Abnormal LES relaxation Median IRP > 15 mm. Hg Time mm. Hg 0 30 50 100 150
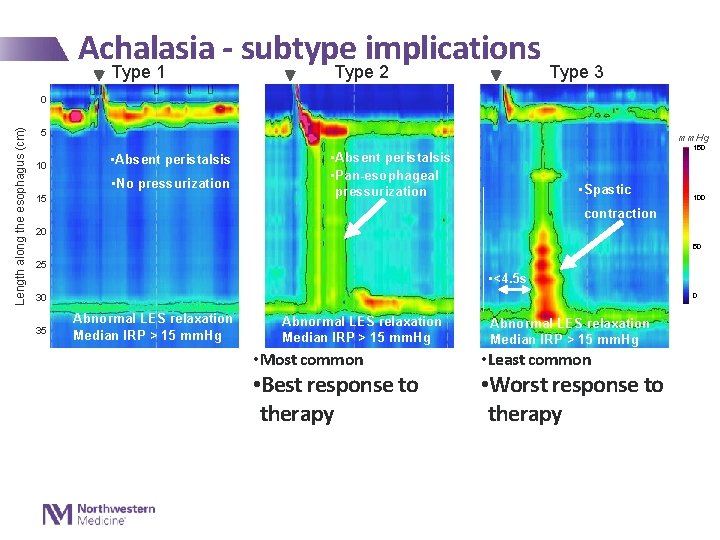
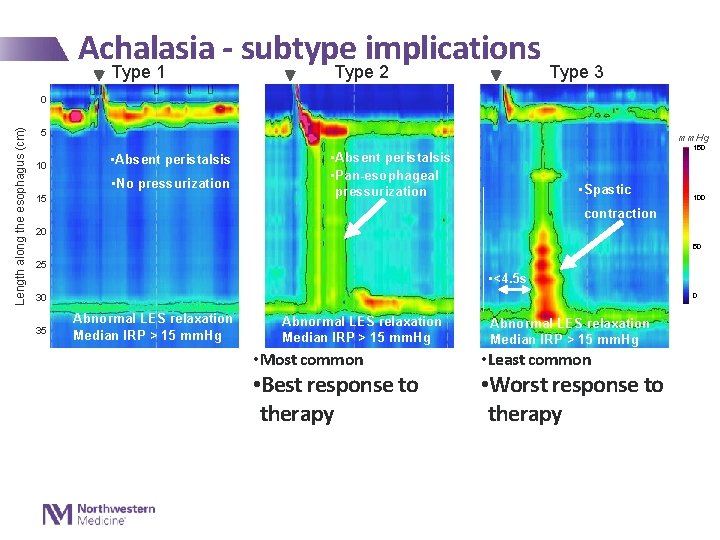
Achalasia - subtype implications Type 1 Type 2 Type 3 Length along the esophagus (cm) 0 5 10 mm. Hg • Absent peristalsis • No pressurization 15 150 • Absent peristalsis • Pan-esophageal pressurization • Spastic 100 contraction 20 50 25 • <4. 5 s 0 30 35 Abnormal LES relaxation Median IRP > 15 mm. Hg • Most common • Best response to therapy Abnormal LES relaxation Median IRP > 15 mm. Hg • Least common • Worst response to therapy
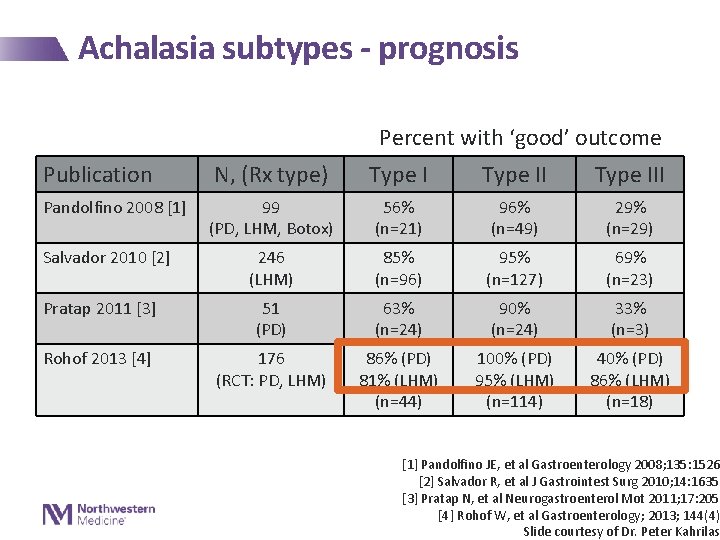
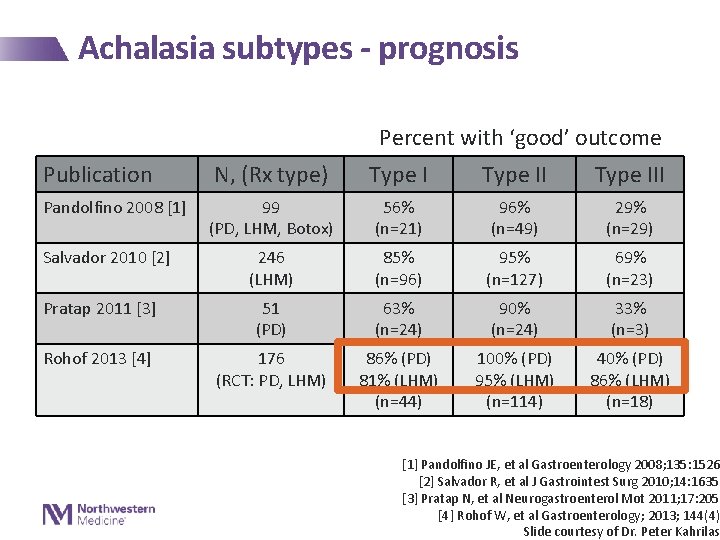
Achalasia subtypes - prognosis Percent with ‘good’ outcome Publication N, (Rx type) Type III 99 (PD, LHM, Botox) 56% (n=21) 96% (n=49) 29% (n=29) 246 (LHM) 85% (n=96) 95% (n=127) 69% (n=23) Pratap 2011 [3] 51 (PD) 63% (n=24) 90% (n=24) 33% (n=3) Rohof 2013 [4] 176 (RCT: PD, LHM) 86% (PD) 81% (LHM) (n=44) 100% (PD) 95% (LHM) (n=114) 40% (PD) 86% (LHM) (n=18) Pandolfino 2008 [1] Salvador 2010 [2] [1] Pandolfino JE, et al Gastroenterology 2008; 135: 1526 [2] Salvador R, et al J Gastrointest Surg 2010; 14: 1635 [3] Pratap N, et al Neurogastroenterol Mot 2011; 17: 205 [4] Rohof W, et al Gastroenterology; 2013; 144(4) Slide courtesy of Dr. Peter Kahrilas

Achalasia – subtype implications Type 1 Type 2 Type 3 Length along the esophagus (cm) 0 5 10 mm. Hg • Absent peristalsis • No pressurization 15 150 • Absent peristalsis • Pan-esophageal pressurization • Spastic 100 contraction 20 50 25 • <4. 5 s 0 30 35 Abnormal LES relaxation Median IRP > 15 mm. Hg • Most common • Best response to therapy Abnormal LES relaxation Median IRP > 15 mm. Hg • Least common • Worst response to therapy • Myotomy preferred treatment
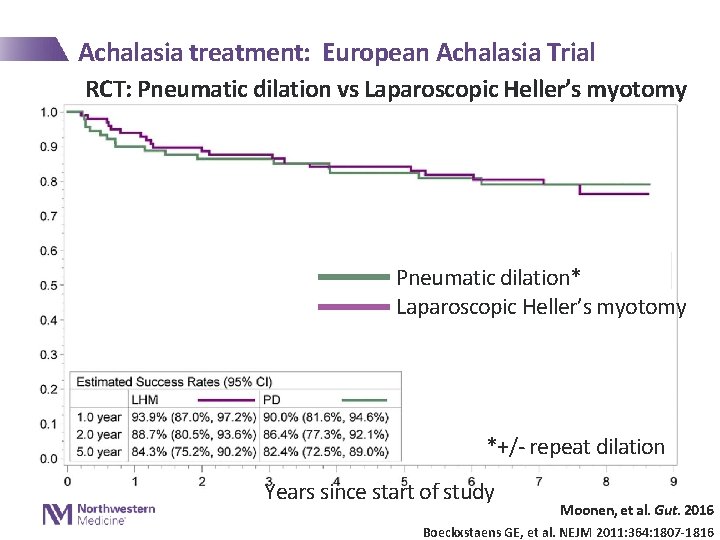
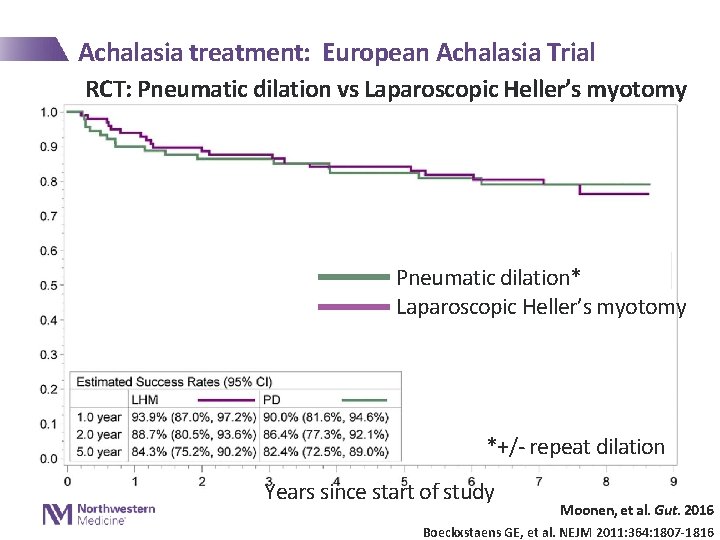
Achalasia treatment: European Achalasia Trial RCT: Pneumatic dilation vs Laparoscopic Heller’s myotomy Pneumatic dilation* Laparoscopic Heller’s myotomy *+/- repeat dilation Years since start of study Moonen, et al. Gut. 2016 Boeckxstaens GE, et al. NEJM 2011: 364: 1807 -1816
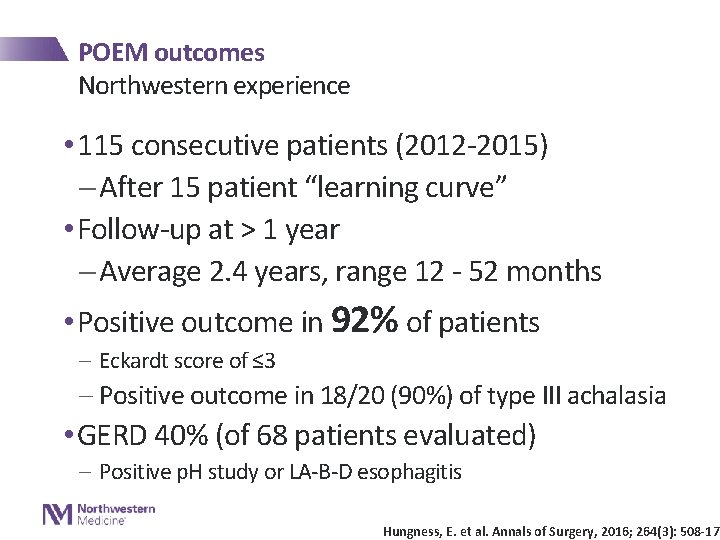
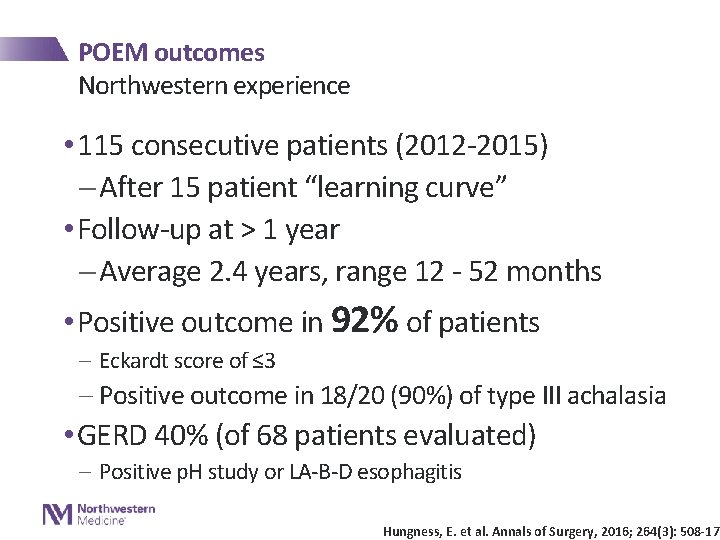
POEM outcomes Northwestern experience • 115 consecutive patients (2012 -2015) - After 15 patient “learning curve” • Follow-up at > 1 year - Average 2. 4 years, range 12 - 52 months • Positive outcome in 92% of patients - Eckardt score of ≤ 3 - Positive outcome in 18/20 (90%) of type III achalasia • GERD 40% (of 68 patients evaluated) - Positive p. H study or LA-B-D esophagitis Hungness, E. et al. Annals of Surgery, 2016; 264(3): 508 -17
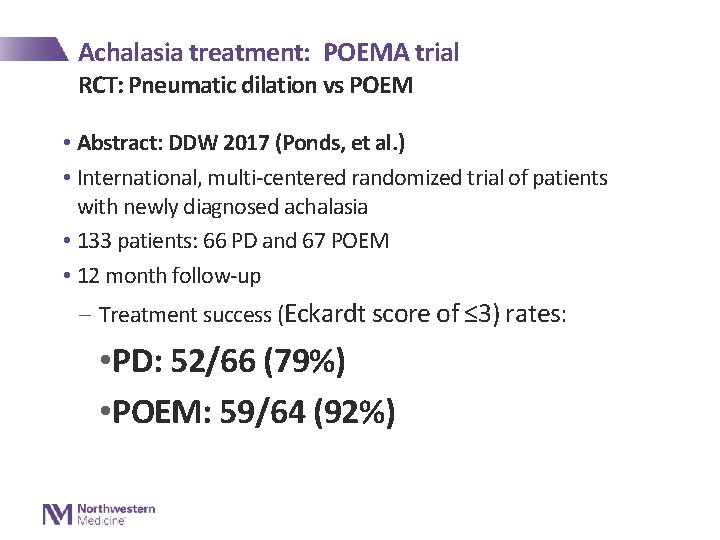
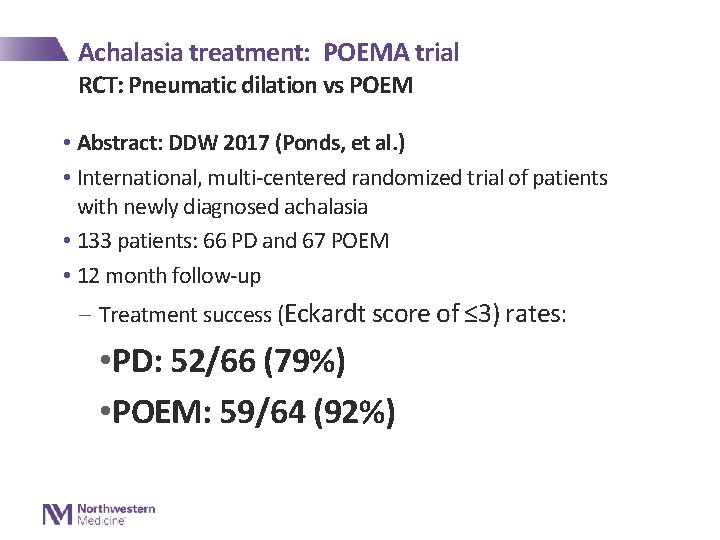
Achalasia treatment: POEMA trial RCT: Pneumatic dilation vs POEM • Abstract: DDW 2017 (Ponds, et al. ) • International, multi-centered randomized trial of patients with newly diagnosed achalasia • 133 patients: 66 PD and 67 POEM • 12 month follow-up - Treatment success (Eckardt score of ≤ 3) rates: • PD: 52/66 (79%) • POEM: 59/64 (92%)

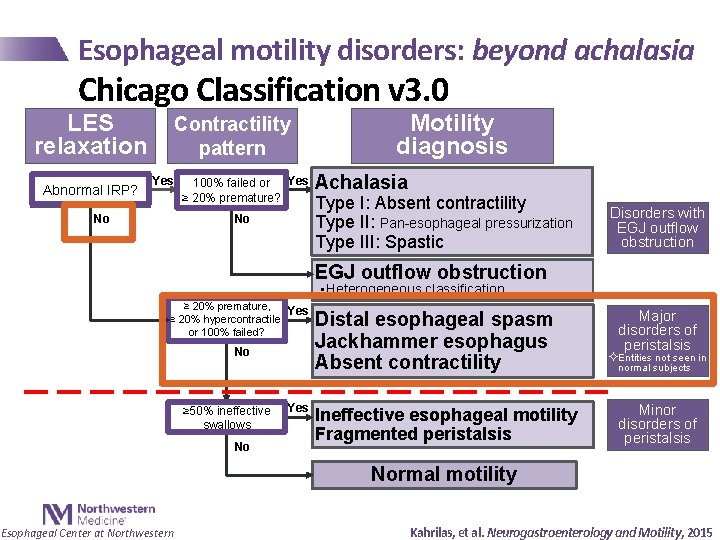
Esophageal motility disorders: beyond achalasia Chicago Classification v 3. 0 LES relaxation Abnormal IRP? Contractility pattern Yes No 100% failed or Yes ≥ 20% premature? No Motility diagnosis Achalasia Type I: Absent contractility Type II: Pan-esophageal pressurization Type III: Spastic Disorders with EGJ outflow obstruction • Heterogeneous classification ≥ 20% premature, Yes ≥ 20% hypercontractile, or 100% failed? No ≥ 50% ineffective swallows No Yes Distal esophageal spasm Jackhammer esophagus Absent contractility Ineffective esophageal motility Fragmented peristalsis Major disorders of peristalsis ²Entities not seen in normal subjects Minor disorders of peristalsis Normal motility Esophageal Center at Northwestern Kahrilas, et al. Neurogastroenterology and Motility, 2015
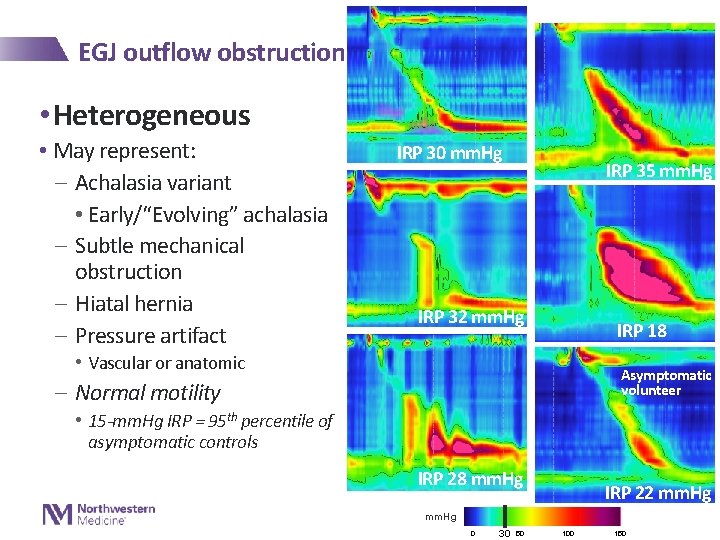
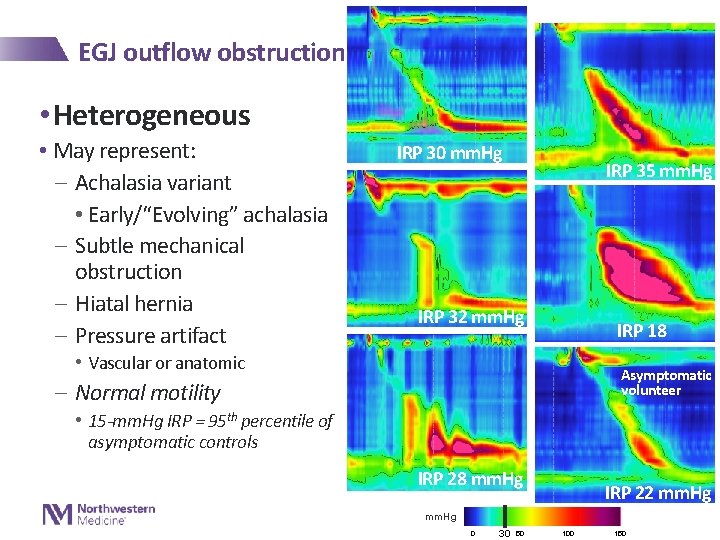
EGJ outflow obstruction • Heterogeneous • May represent: - Achalasia variant • Early/“Evolving” achalasia - Subtle mechanical obstruction - Hiatal hernia - Pressure artifact IRP 30 mm. Hg IRP 35 mm. Hg IRP 32 mm. Hg IRP 18 mm. Hg • Vascular or anatomic Asymptomatic volunteer - Normal motility • 15 -mm. Hg IRP = 95 th percentile of asymptomatic controls IRP 28 mm. Hg IRP 22 mm. Hg 0 30 50 100 150

EGJ outflow obstruction • Heterogeneous clinically • May represent: - Achalasia variant • Early/“Evolving” achalasia - Subtle mechanical obstruction - Hiatal hernia - Pressure artifact • Vascular or anatomic - Normal motility Variable management strategies Pneumatic/Heller/POEM/Botox Dilation GERD; HH repair GERD; Functional
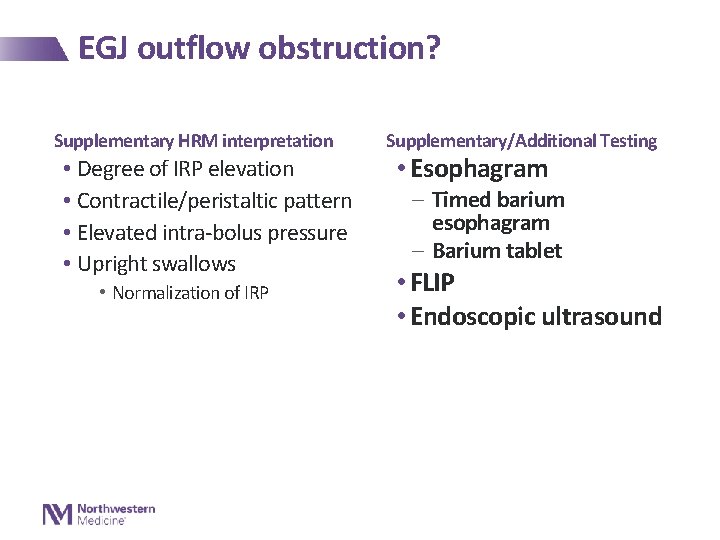
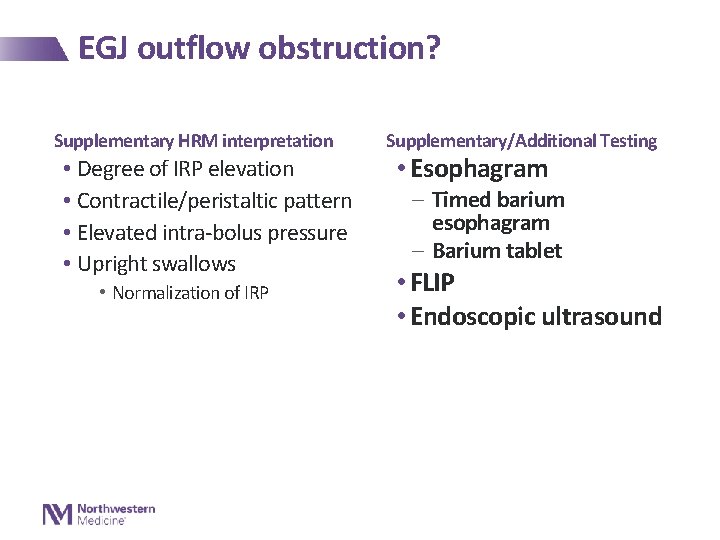
EGJ outflow obstruction? Supplementary HRM interpretation • Degree of IRP elevation • Contractile/peristaltic pattern • Elevated intra-bolus pressure • Upright swallows • Normalization of IRP Supplementary/Additional Testing • Esophagram - Timed barium esophagram - Barium tablet • FLIP • Endoscopic ultrasound
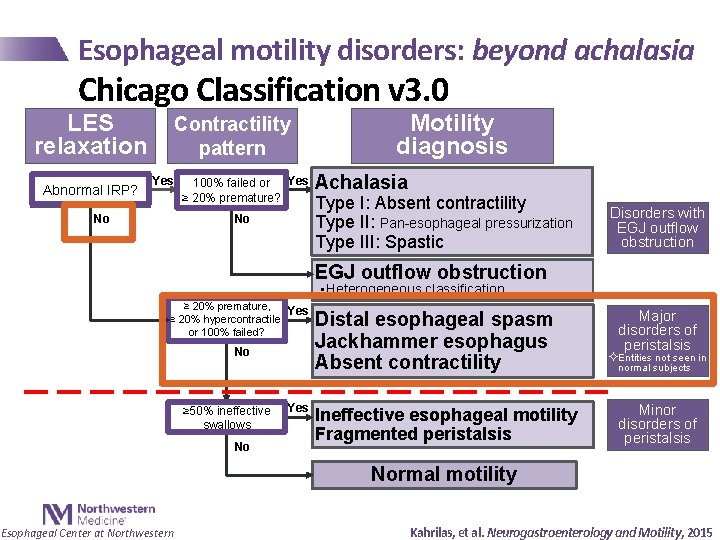
Esophageal motility disorders: beyond achalasia Chicago Classification v 3. 0 LES relaxation Abnormal IRP? Contractility pattern Yes No 100% failed or Yes ≥ 20% premature? No Motility diagnosis Achalasia Type I: Absent contractility Type II: Pan-esophageal pressurization Type III: Spastic Disorders with EGJ outflow obstruction • Heterogeneous classification ≥ 20% premature, Yes ≥ 20% hypercontractile, or 100% failed? No ≥ 50% ineffective swallows No Yes Distal esophageal spasm Jackhammer esophagus Absent contractility Ineffective esophageal motility Fragmented peristalsis Major disorders of peristalsis ²Entities not seen in normal subjects Minor disorders of peristalsis Normal motility Esophageal Center at Northwestern Kahrilas, et al. Neurogastroenterology and Motility, 2015
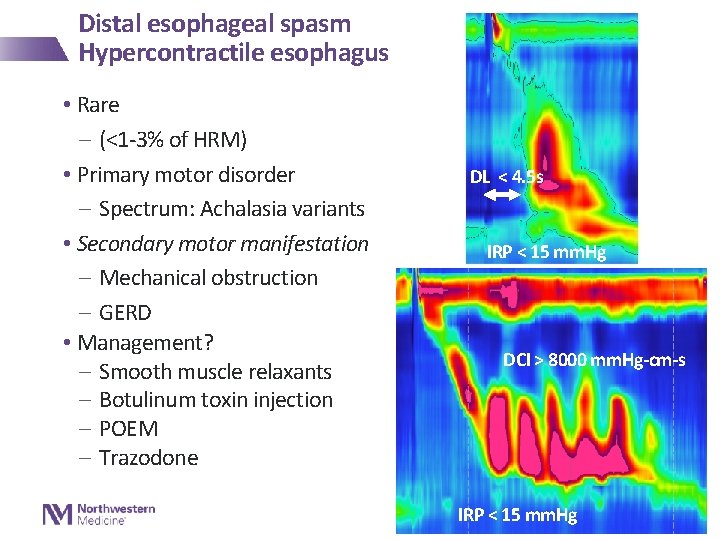
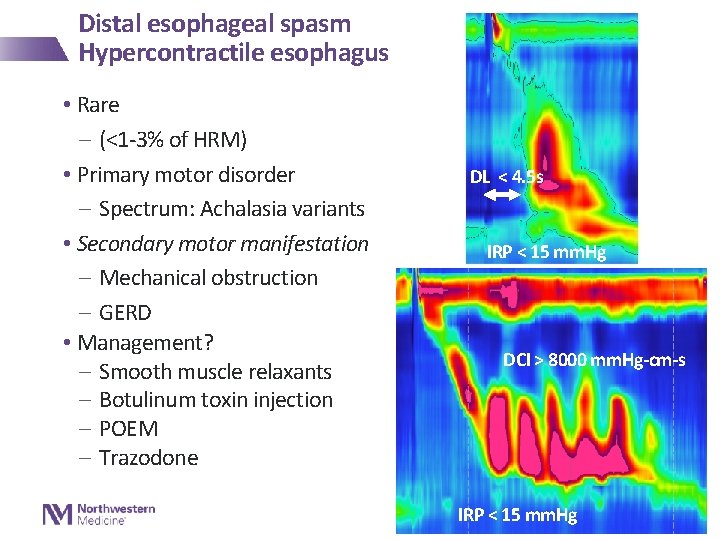
Distal esophageal spasm Hypercontractile esophagus • Rare - (<1 -3% of HRM) • Primary motor disorder - Spectrum: Achalasia variants • Secondary motor manifestation - Mechanical obstruction - GERD • Management? - Smooth muscle relaxants - Botulinum toxin injection - POEM - Trazodone DL < 4. 5 s IRP < 15 mm. Hg DCI > 8000 mm. Hg-cm-s IRP < 15 mm. Hg
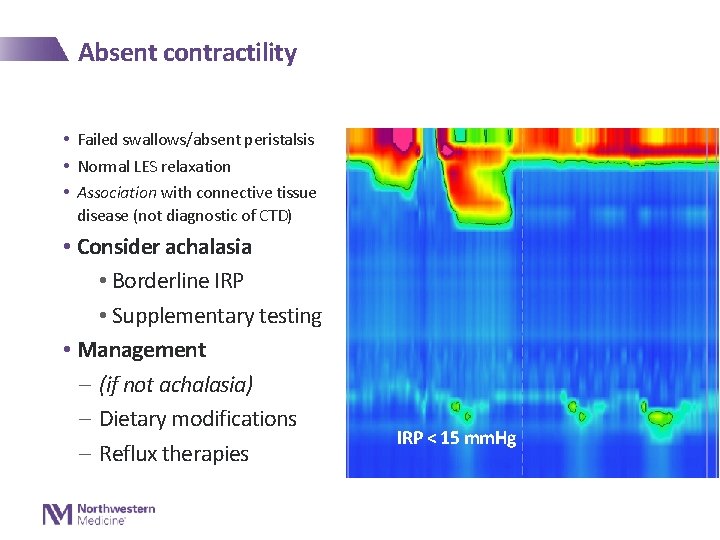
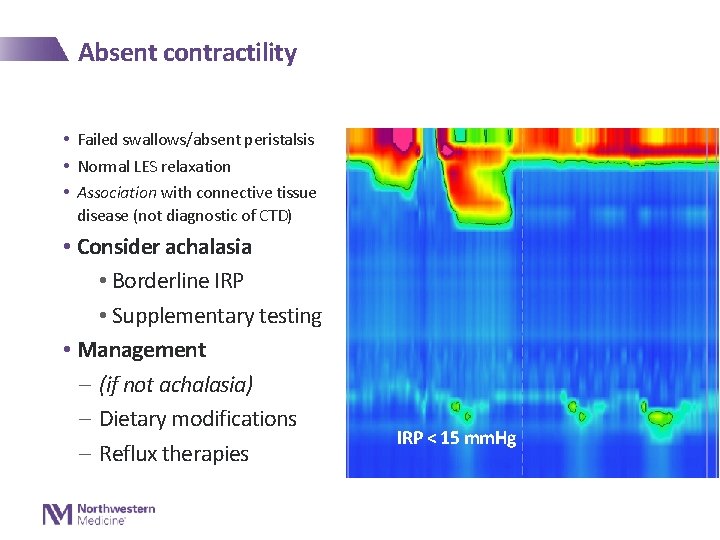
Absent contractility • Failed swallows/absent peristalsis • Normal LES relaxation • Association with connective tissue disease (not diagnostic of CTD) • Consider achalasia • Borderline IRP • Supplementary testing • Management - (if not achalasia) - Dietary modifications - Reflux therapies IRP < 15 mm. Hg
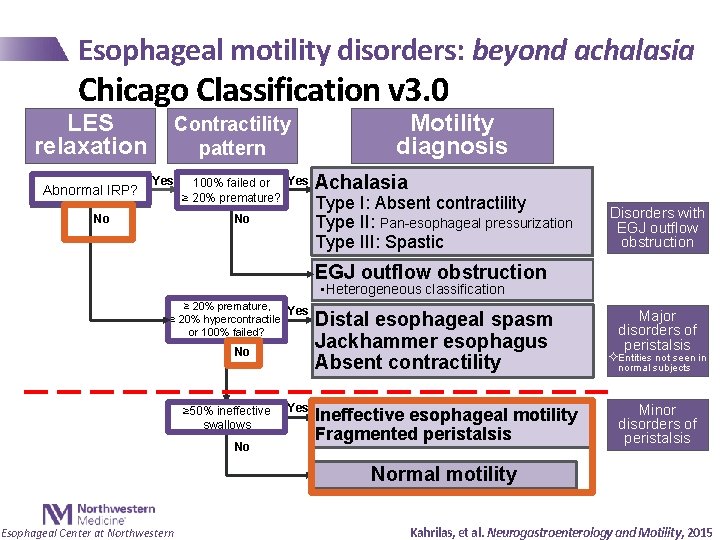
Esophageal motility disorders: beyond achalasia Chicago Classification v 3. 0 LES relaxation Abnormal IRP? Contractility pattern Yes No 100% failed or Yes ≥ 20% premature? No Motility diagnosis Achalasia Type I: Absent contractility Type II: Pan-esophageal pressurization Type III: Spastic Disorders with EGJ outflow obstruction • Heterogeneous classification ≥ 20% premature, Yes ≥ 20% hypercontractile, or 100% failed? No ≥ 50% ineffective swallows No Yes Distal esophageal spasm Jackhammer esophagus Absent contractility Ineffective esophageal motility Fragmented peristalsis Major disorders of peristalsis ²Entities not seen in normal subjects Minor disorders of peristalsis Normal motility Esophageal Center at Northwestern Kahrilas, et al. Neurogastroenterology and Motility, 2015

Functional dysphagia • Not meeting criteria for a major motility disorder • Consider evaluation for subtle mechanical obstruction - e. g. esophagram with barium tablet • Management - Dietary modifications - Reflux therapies - Empiric dilation - Neuromodulator/cognitive behavioral therapy/hypnosis - Observation and re-evaluation for progression
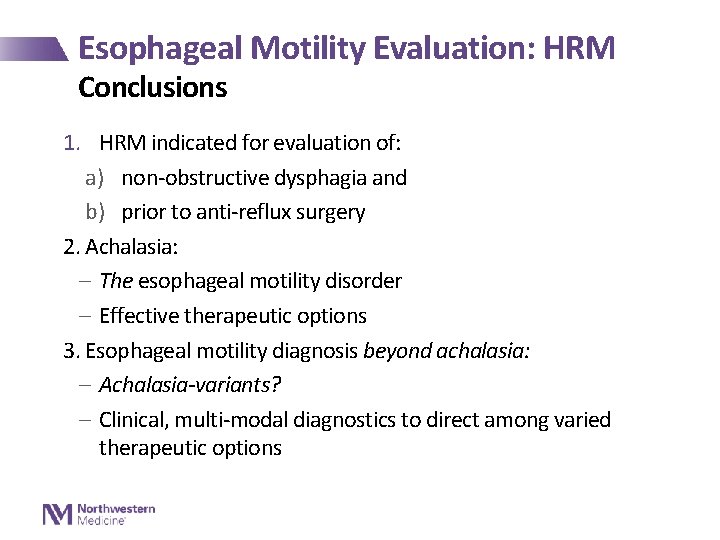
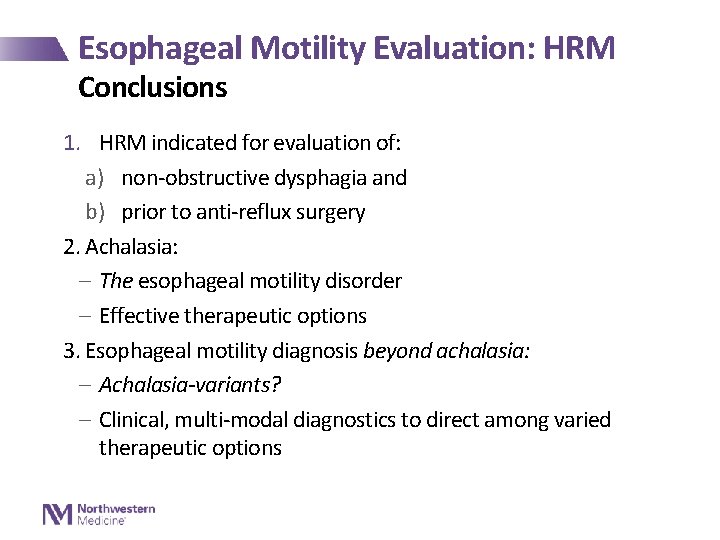
Esophageal Motility Evaluation: HRM Conclusions 1. HRM indicated for evaluation of: a) non-obstructive dysphagia and b) prior to anti-reflux surgery 2. Achalasia: - The esophageal motility disorder - Effective therapeutic options 3. Esophageal motility diagnosis beyond achalasia: - Achalasia-variants? - Clinical, multi-modal diagnostics to direct among varied therapeutic options
Acknowledgements Esophageal Center of Northwestern Clinical Research Team • Sandi Jelinek • Gwen Cassidy • Jackie Prescott • Alex Decorrevont • Francesca Shilati • Melina Masihi • Stephanie Peterson • Joe Triggs • Ryan Campagna • • • John Pandolfino Peter Kahrilas Ikuo Hirano Nimi Gonsalves Aziz Aadam Sri Komanduri Eric Hungness Ezra Teitelbaum Nat Soper David Odell Funding sources • NIDDK: - R 01 DK 079902 (PI: Pandolfino) - R 01 DK 092217 (PI: Pandolfino) - P 01 DK 117824 (PI: Pandolfino)

Thank You Questions? dustin-carlson@northwestern. edu