Nutritional diseases Proteinenergy malnutrition Kwashiorkor acute form of



- Slides: 30
Nutritional diseases
Protein-energy malnutrition
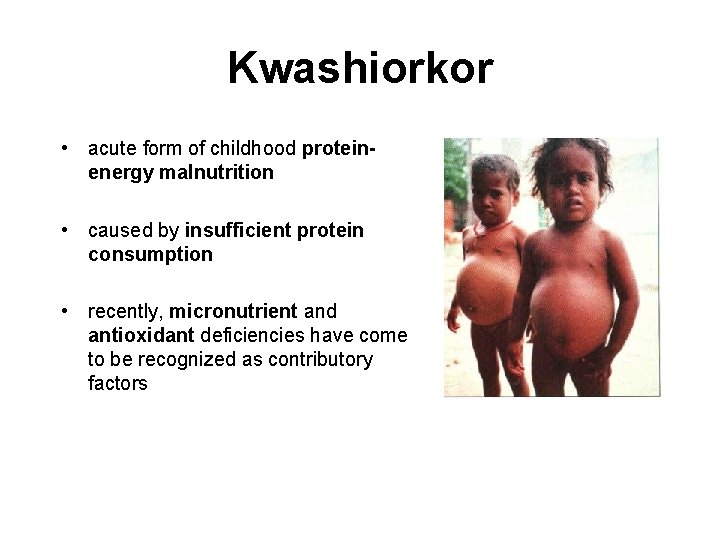
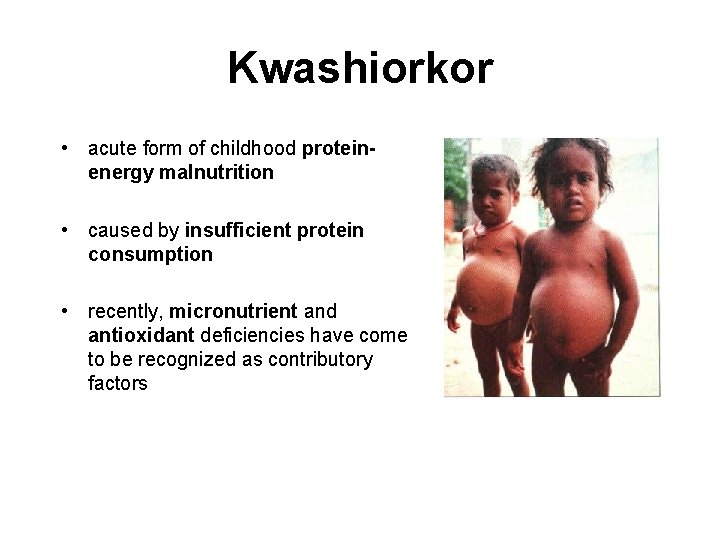
Kwashiorkor • acute form of childhood proteinenergy malnutrition • caused by insufficient protein consumption • recently, micronutrient and antioxidant deficiencies have come to be recognized as contributory factors
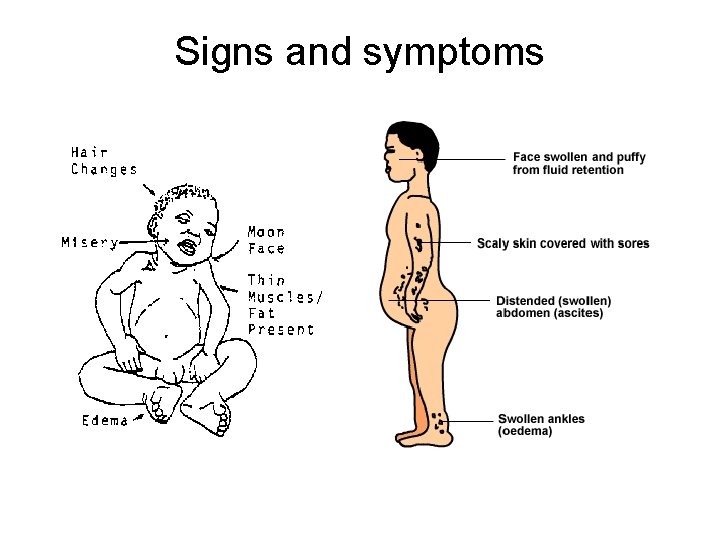
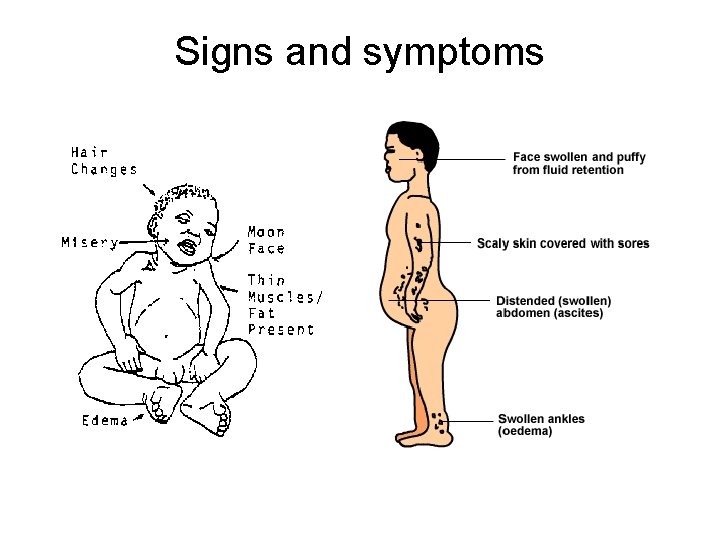
Signs and symptoms

Pathophysiology • cell membranes are damaged throughout the body • egress of potassium and water from cells • intracellular water moves to the extracellular space, resulting in oedema • profound reduction in whole body potassium to about 35 mmol/kg (44 mmol/kg is normal) • life-threatening hypokalaemia, and hypophosphataemia are observed in severe cases
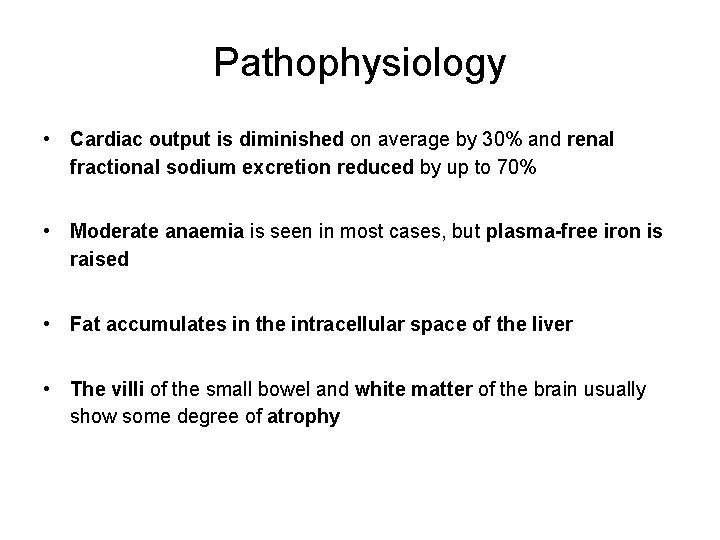
Pathophysiology • Cardiac output is diminished on average by 30% and renal fractional sodium excretion reduced by up to 70% • Moderate anaemia is seen in most cases, but plasma-free iron is raised • Fat accumulates in the intracellular space of the liver • The villi of the small bowel and white matter of the brain usually show some degree of atrophy
Treatment • Treatment depends on the severity of the condition. • Patients who are in shock need immediate treatment to restore blood volume and maintain blood pressure. • Calories are given first in the form of carbohydrates, simple sugars, and fats. • Proteins are started after other sources of calories have already provided energy. • Vitamin and mineral supplements are essential.
Treatment • Treating kwashiorkor in its late stages will improve the child's general health. However, the child may be left with permanent physical and mental problems. • If treatment is not given or comes too late, this condition is life-threatening.
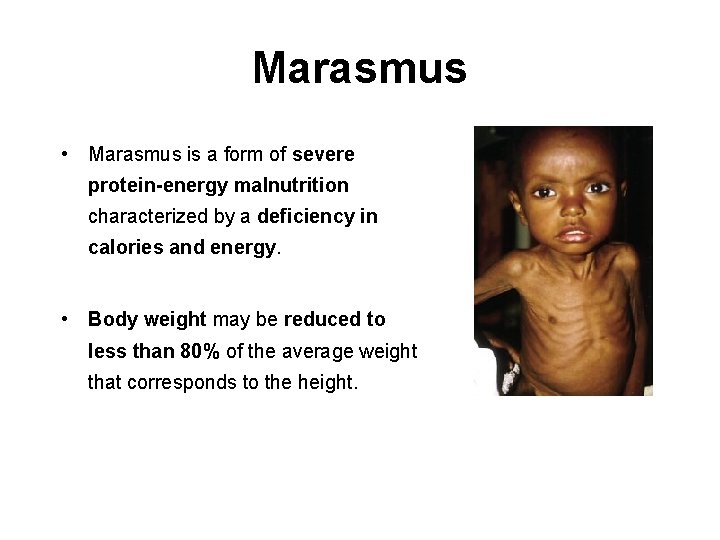
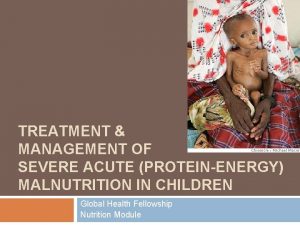
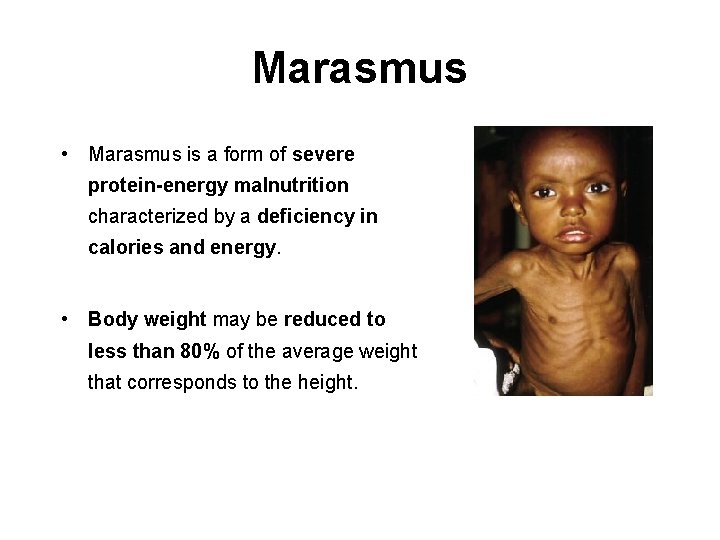
Marasmus • Marasmus is a form of severe protein-energy malnutrition characterized by a deficiency in calories and energy. • Body weight may be reduced to less than 80% of the average weight that corresponds to the height.
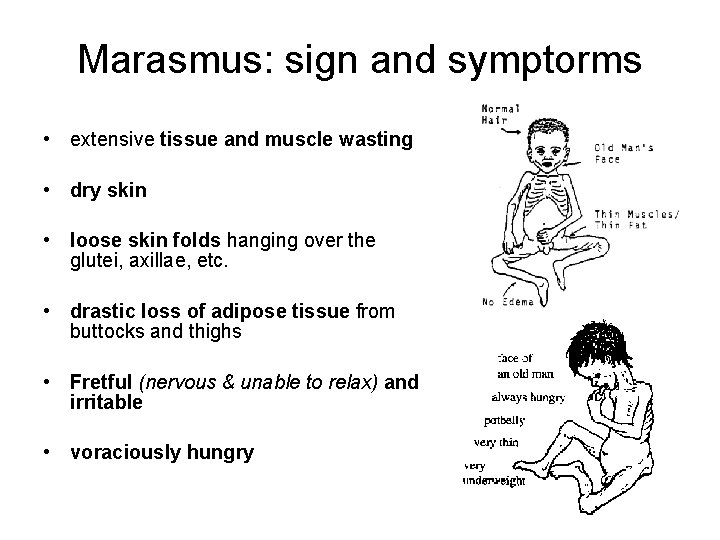
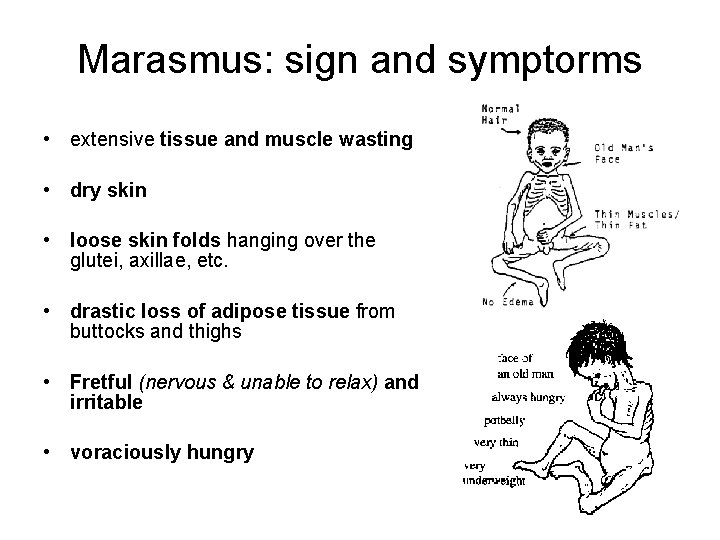
Marasmus: sign and symptorms • extensive tissue and muscle wasting • dry skin • loose skin folds hanging over the glutei, axillae, etc. • drastic loss of adipose tissue from buttocks and thighs • Fretful (nervous & unable to relax) and irritable • voraciously hungry
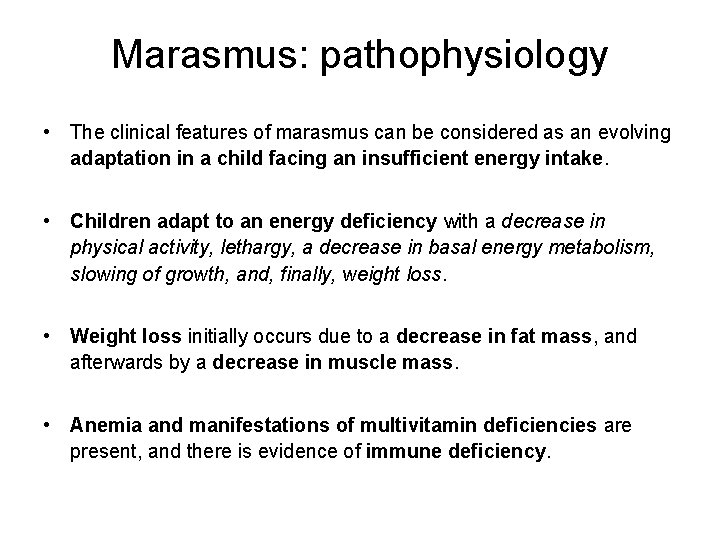
Marasmus: pathophysiology • The clinical features of marasmus can be considered as an evolving adaptation in a child facing an insufficient energy intake. • Children adapt to an energy deficiency with a decrease in physical activity, lethargy, a decrease in basal energy metabolism, slowing of growth, and, finally, weight loss. • Weight loss initially occurs due to a decrease in fat mass, and afterwards by a decrease in muscle mass. • Anemia and manifestations of multivitamin deficiencies are present, and there is evidence of immune deficiency.
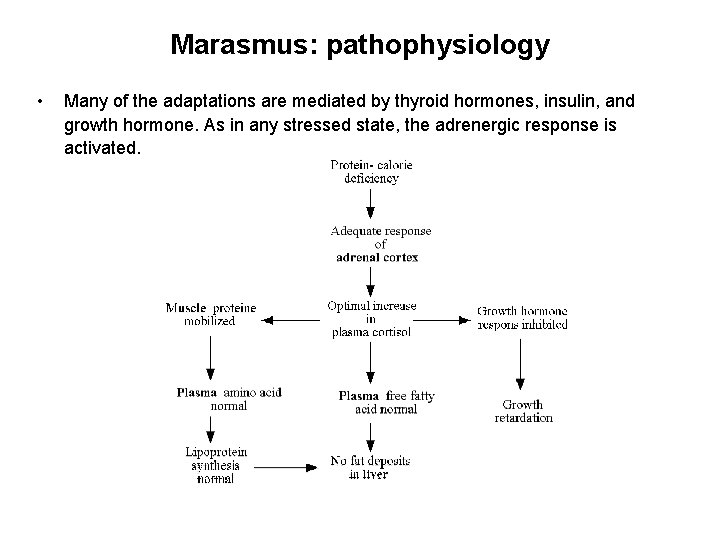
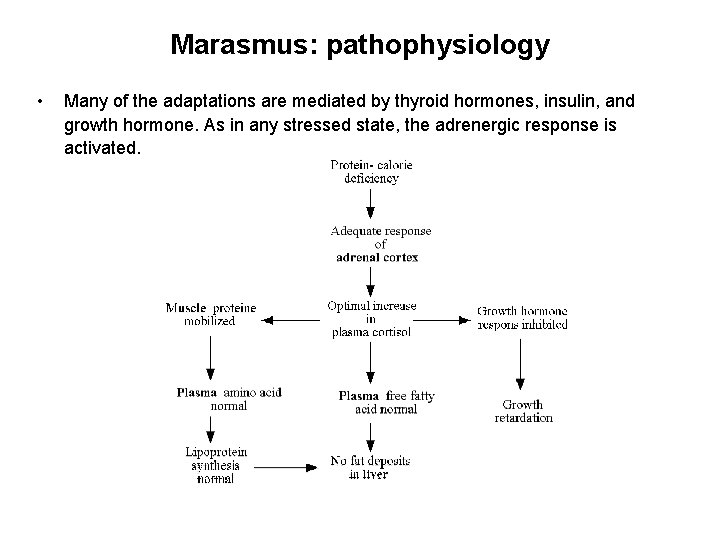
Marasmus: pathophysiology • Many of the adaptations are mediated by thyroid hormones, insulin, and growth hormone. As in any stressed state, the adrenergic response is activated.
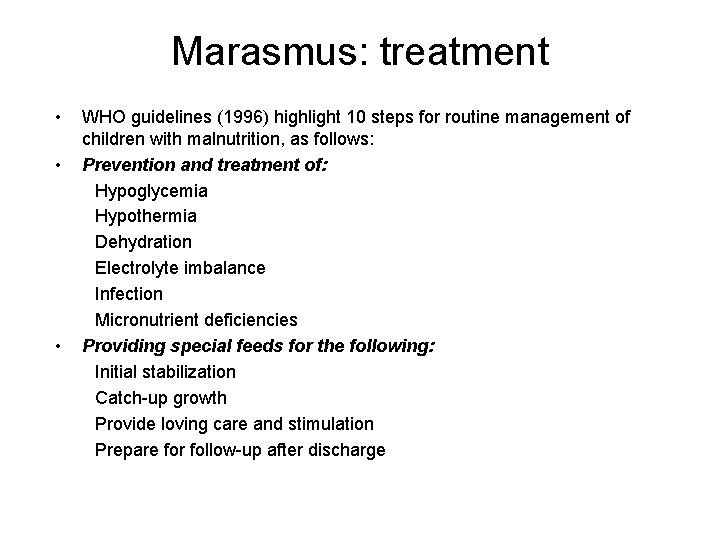
Marasmus: treatment • • • WHO guidelines (1996) highlight 10 steps for routine management of children with malnutrition, as follows: Prevention and treatment of: Hypoglycemia Hypothermia Dehydration Electrolyte imbalance Infection Micronutrient deficiencies Providing special feeds for the following: Initial stabilization Catch-up growth Provide loving care and stimulation Prepare for follow-up after discharge
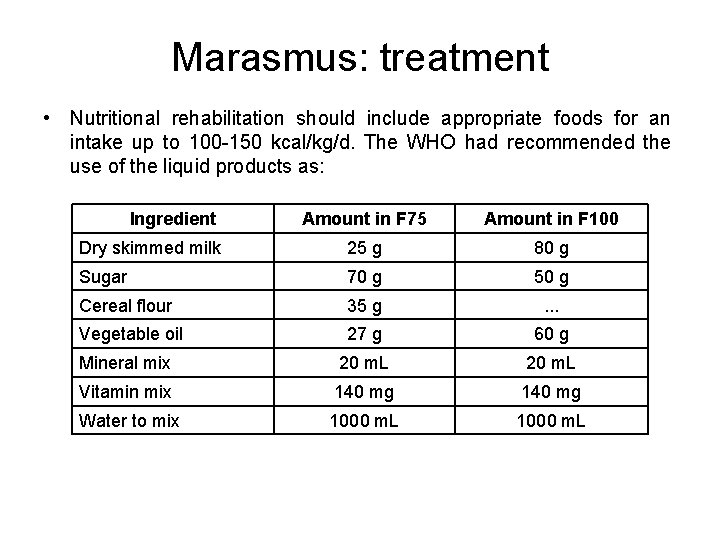
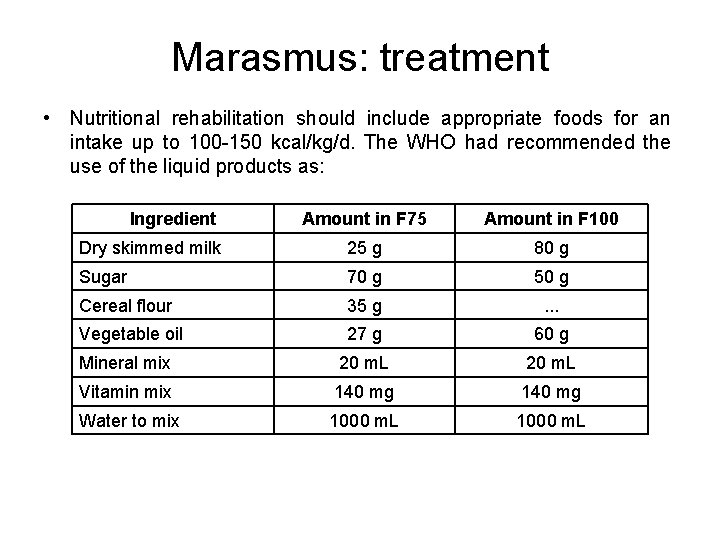
Marasmus: treatment • Nutritional rehabilitation should include appropriate foods for an intake up to 100 -150 kcal/kg/d. The WHO had recommended the use of the liquid products as: Ingredient Amount in F 75 Amount in F 100 Dry skimmed milk 25 g 80 g Sugar 70 g 50 g Cereal flour 35 g . . . Vegetable oil 27 g 60 g Mineral mix 20 m. L Vitamin mix 140 mg Water to mix 1000 m. L
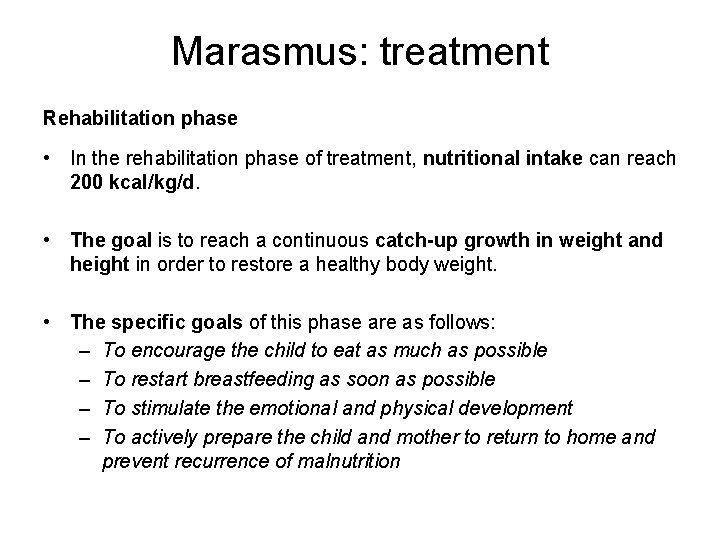
Marasmus: treatment Rehabilitation phase • In the rehabilitation phase of treatment, nutritional intake can reach 200 kcal/kg/d. • The goal is to reach a continuous catch-up growth in weight and height in order to restore a healthy body weight. • The specific goals of this phase are as follows: – To encourage the child to eat as much as possible – To restart breastfeeding as soon as possible – To stimulate the emotional and physical development – To actively prepare the child and mother to return to home and prevent recurrence of malnutrition
Deficiency states of vitamins and minerals
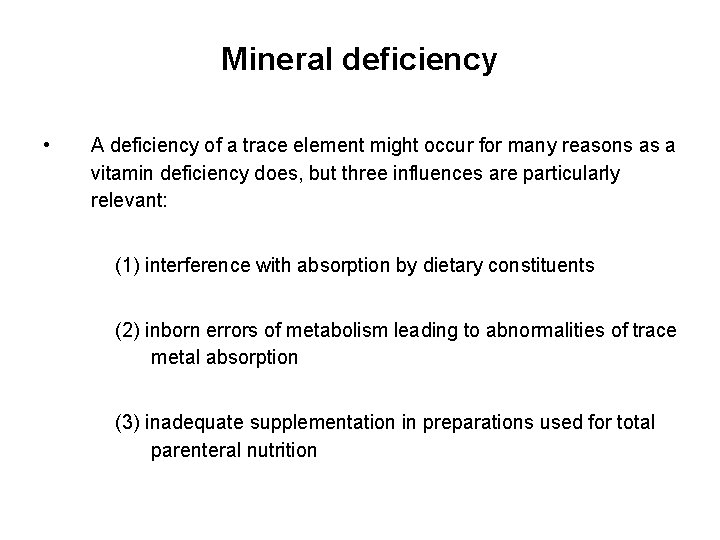
Mineral deficiency • A deficiency of a trace element might occur for many reasons as a vitamin deficiency does, but three influences are particularly relevant: (1) interference with absorption by dietary constituents (2) inborn errors of metabolism leading to abnormalities of trace metal absorption (3) inadequate supplementation in preparations used for total parenteral nutrition
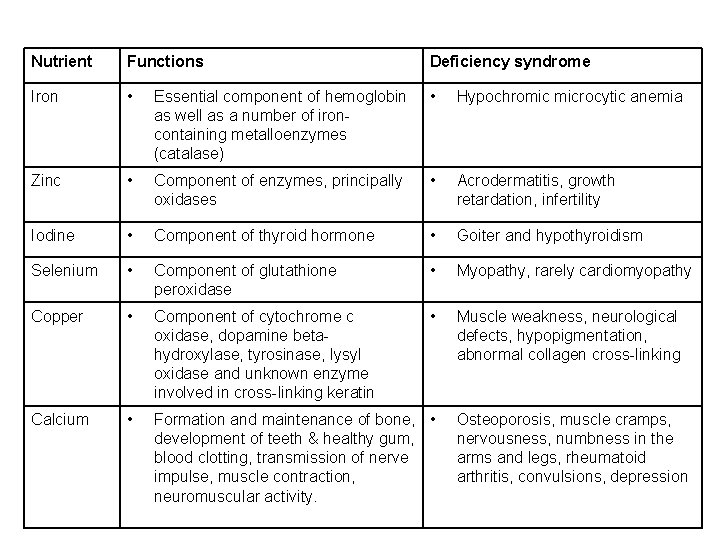
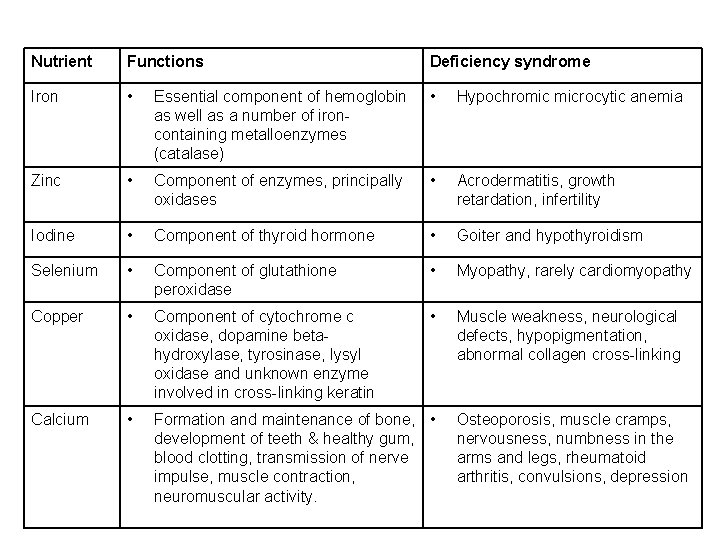
Nutrient Functions Deficiency syndrome Iron • Essential component of hemoglobin as well as a number of ironcontaining metalloenzymes (catalase) • Hypochromic microcytic anemia Zinc • Component of enzymes, principally oxidases • Acrodermatitis, growth retardation, infertility Iodine • Component of thyroid hormone • Goiter and hypothyroidism Selenium • Component of glutathione peroxidase • Myopathy, rarely cardiomyopathy Copper • Component of cytochrome c oxidase, dopamine betahydroxylase, tyrosinase, lysyl oxidase and unknown enzyme involved in cross-linking keratin • Muscle weakness, neurological defects, hypopigmentation, abnormal collagen cross-linking Calcium • Formation and maintenance of bone, • development of teeth & healthy gum, blood clotting, transmission of nerve impulse, muscle contraction, neuromuscular activity. Osteoporosis, muscle cramps, nervousness, numbness in the arms and legs, rheumatoid arthritis, convulsions, depression
Iron deficiency Iron absorption and distribution
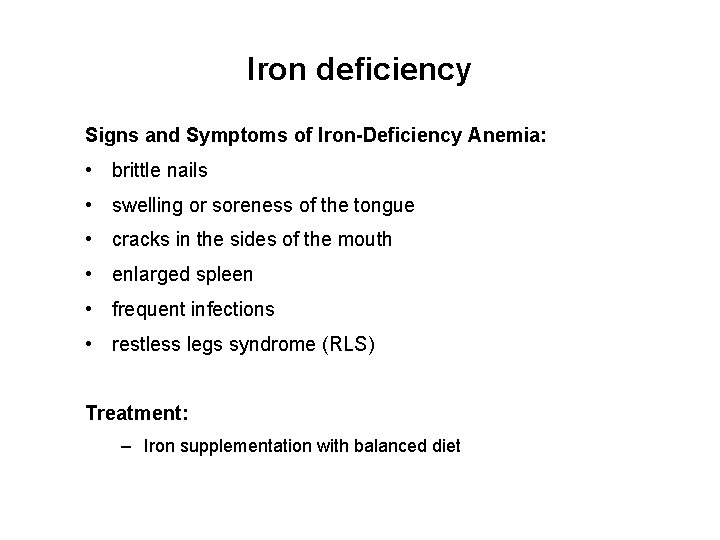
Iron deficiency Signs and Symptoms of Iron-Deficiency Anemia: • brittle nails • swelling or soreness of the tongue • cracks in the sides of the mouth • enlarged spleen • frequent infections • restless legs syndrome (RLS) Treatment: – Iron supplementation with balanced diet
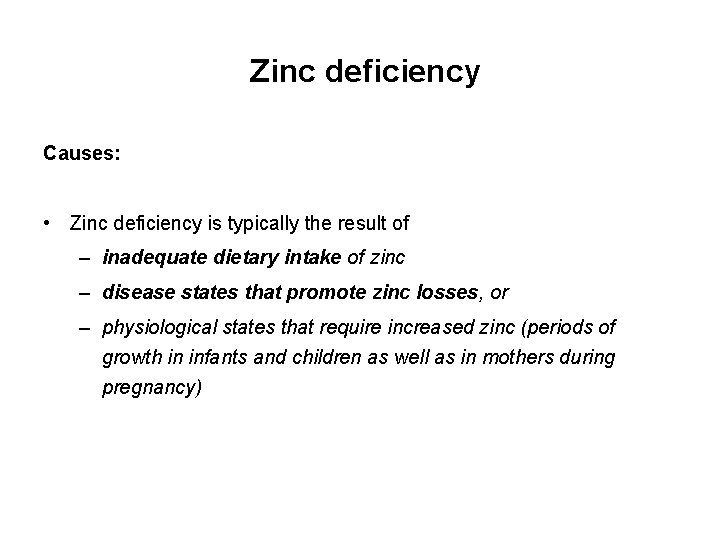
Zinc deficiency Causes: • Zinc deficiency is typically the result of – inadequate dietary intake of zinc – disease states that promote zinc losses, or – physiological states that require increased zinc (periods of growth in infants and children as well as in mothers during pregnancy)
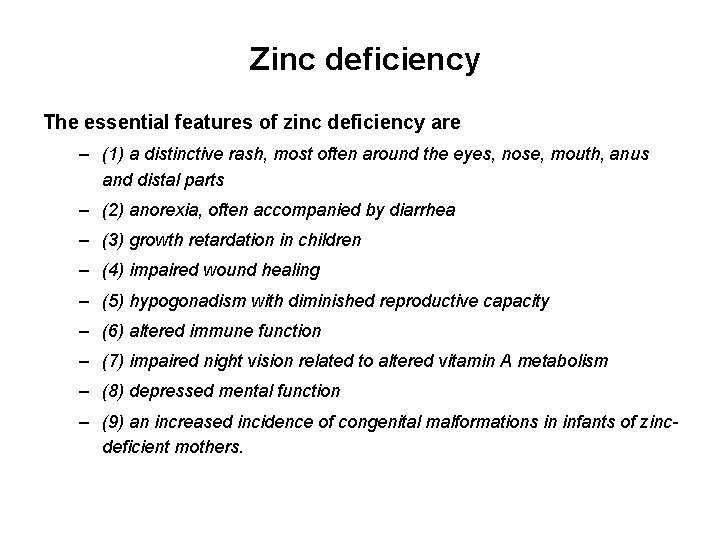
Zinc deficiency The essential features of zinc deficiency are – (1) a distinctive rash, most often around the eyes, nose, mouth, anus and distal parts – (2) anorexia, often accompanied by diarrhea – (3) growth retardation in children – (4) impaired wound healing – (5) hypogonadism with diminished reproductive capacity – (6) altered immune function – (7) impaired night vision related to altered vitamin A metabolism – (8) depressed mental function – (9) an increased incidence of congenital malformations in infants of zincdeficient mothers.
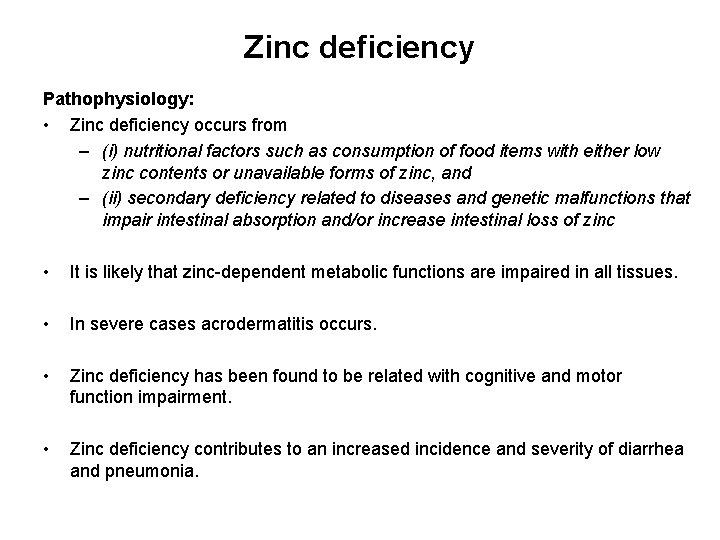
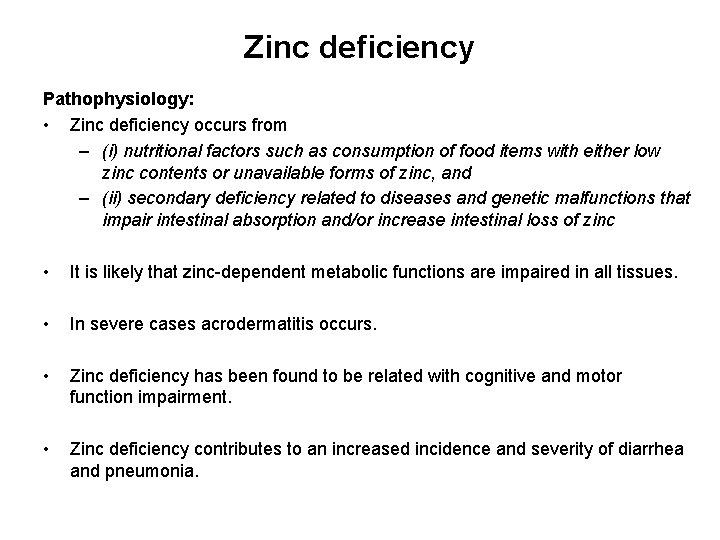
Zinc deficiency Pathophysiology: • Zinc deficiency occurs from – (i) nutritional factors such as consumption of food items with either low zinc contents or unavailable forms of zinc, and – (ii) secondary deficiency related to diseases and genetic malfunctions that impair intestinal absorption and/or increase intestinal loss of zinc • It is likely that zinc-dependent metabolic functions are impaired in all tissues. • In severe cases acrodermatitis occurs. • Zinc deficiency has been found to be related with cognitive and motor function impairment. • Zinc deficiency contributes to an increased incidence and severity of diarrhea and pneumonia.
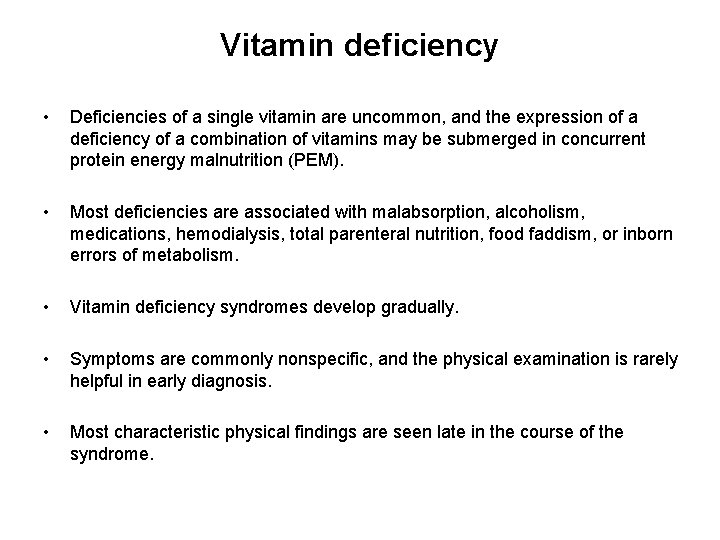
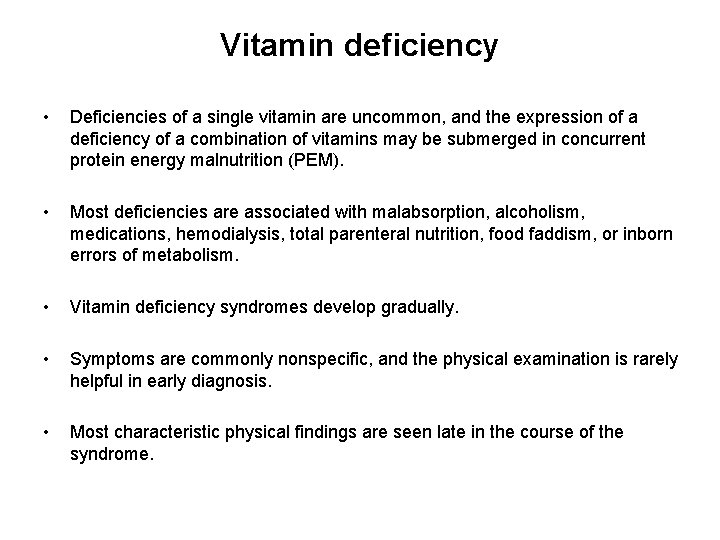
Vitamin deficiency • Deficiencies of a single vitamin are uncommon, and the expression of a deficiency of a combination of vitamins may be submerged in concurrent protein energy malnutrition (PEM). • Most deficiencies are associated with malabsorption, alcoholism, medications, hemodialysis, total parenteral nutrition, food faddism, or inborn errors of metabolism. • Vitamin deficiency syndromes develop gradually. • Symptoms are commonly nonspecific, and the physical examination is rarely helpful in early diagnosis. • Most characteristic physical findings are seen late in the course of the syndrome.
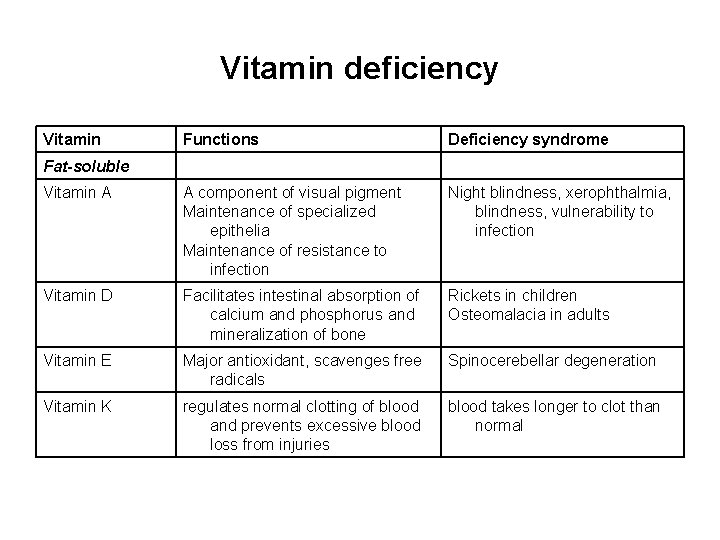
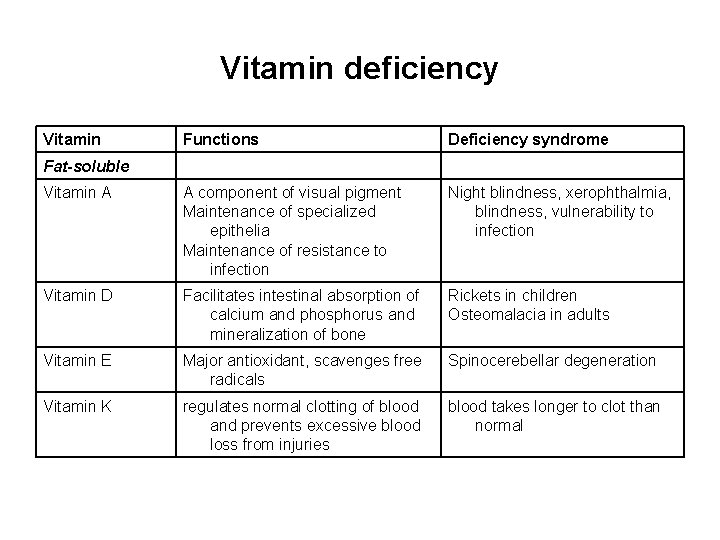
Vitamin deficiency Vitamin Functions Deficiency syndrome Vitamin A A component of visual pigment Maintenance of specialized epithelia Maintenance of resistance to infection Night blindness, xerophthalmia, blindness, vulnerability to infection Vitamin D Facilitates intestinal absorption of calcium and phosphorus and mineralization of bone Rickets in children Osteomalacia in adults Vitamin E Major antioxidant, scavenges free radicals Spinocerebellar degeneration Vitamin K regulates normal clotting of blood and prevents excessive blood loss from injuries blood takes longer to clot than normal Fat-soluble
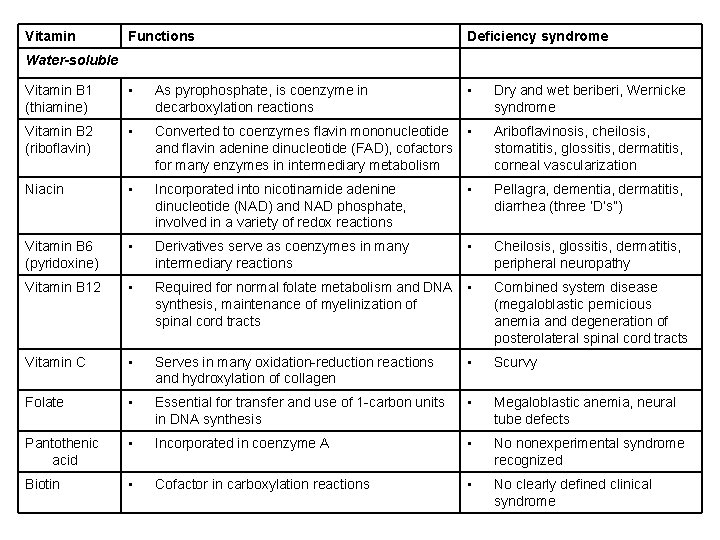
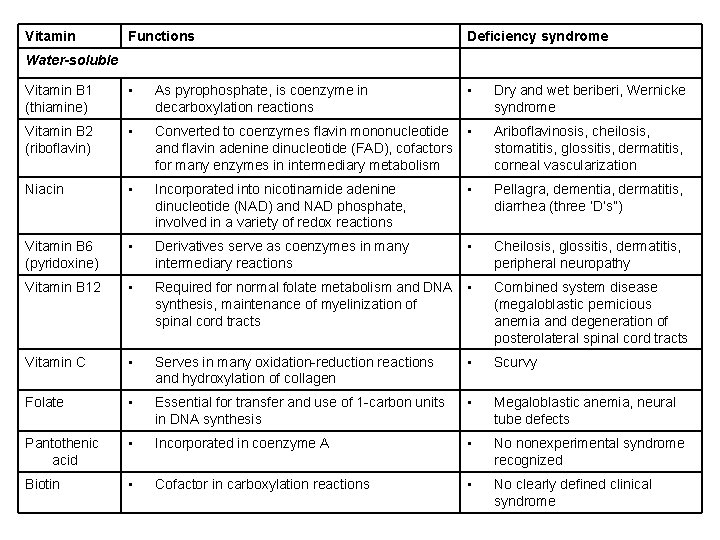
Vitamin Functions Deficiency syndrome Vitamin B 1 (thiamine) • As pyrophosphate, is coenzyme in decarboxylation reactions • Dry and wet beri, Wernicke syndrome Vitamin B 2 (riboflavin) • Converted to coenzymes flavin mononucleotide and flavin adenine dinucleotide (FAD), cofactors for many enzymes in intermediary metabolism • Ariboflavinosis, cheilosis, stomatitis, glossitis, dermatitis, corneal vascularization Niacin • Incorporated into nicotinamide adenine dinucleotide (NAD) and NAD phosphate, involved in a variety of redox reactions • Pellagra, dementia, dermatitis, diarrhea (three ‘D’s”) Vitamin B 6 (pyridoxine) • Derivatives serve as coenzymes in many intermediary reactions • Cheilosis, glossitis, dermatitis, peripheral neuropathy Vitamin B 12 • Required for normal folate metabolism and DNA synthesis, maintenance of myelinization of spinal cord tracts • Combined system disease (megaloblastic pernicious anemia and degeneration of posterolateral spinal cord tracts Vitamin C • Serves in many oxidation-reduction reactions and hydroxylation of collagen • Scurvy Folate • Essential for transfer and use of 1 -carbon units in DNA synthesis • Megaloblastic anemia, neural tube defects Pantothenic acid • Incorporated in coenzyme A • No nonexperimental syndrome recognized Biotin • Cofactor in carboxylation reactions • No clearly defined clinical syndrome Water-soluble
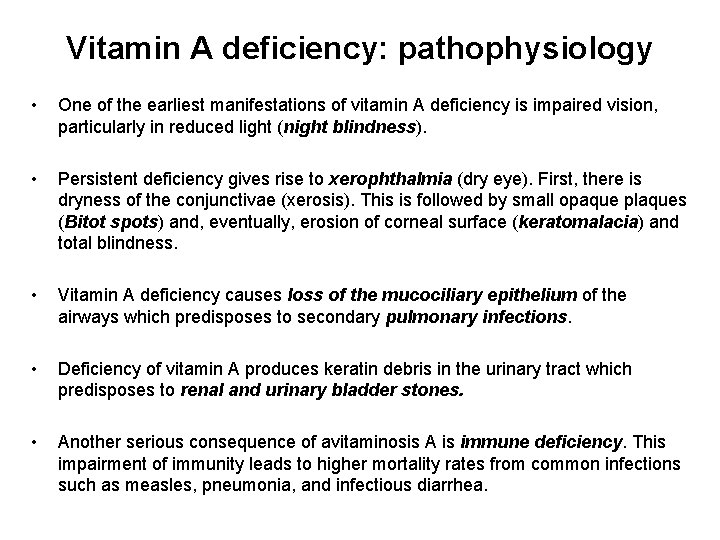
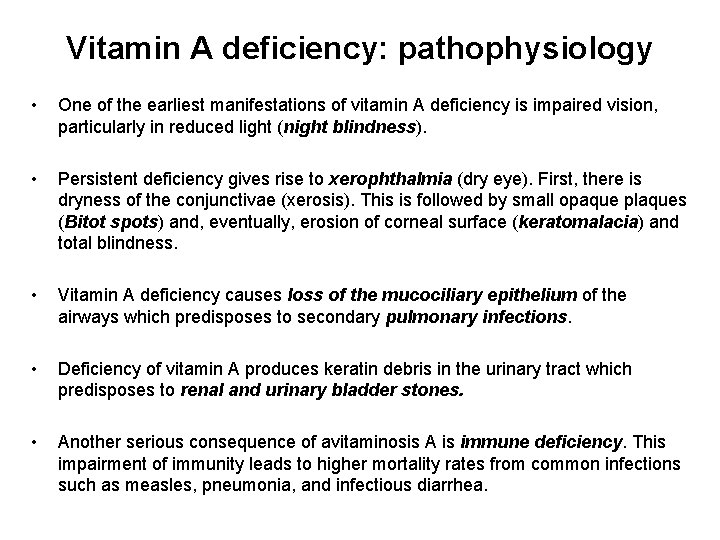
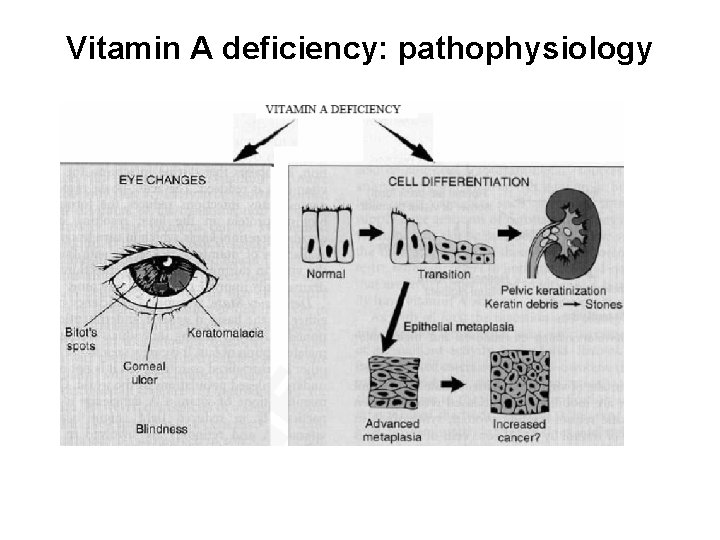
Vitamin A deficiency: pathophysiology • One of the earliest manifestations of vitamin A deficiency is impaired vision, particularly in reduced light (night blindness). • Persistent deficiency gives rise to xerophthalmia (dry eye). First, there is dryness of the conjunctivae (xerosis). This is followed by small opaque plaques (Bitot spots) and, eventually, erosion of corneal surface (keratomalacia) and total blindness. • Vitamin A deficiency causes loss of the mucociliary epithelium of the airways which predisposes to secondary pulmonary infections. • Deficiency of vitamin A produces keratin debris in the urinary tract which predisposes to renal and urinary bladder stones. • Another serious consequence of avitaminosis A is immune deficiency. This impairment of immunity leads to higher mortality rates from common infections such as measles, pneumonia, and infectious diarrhea.
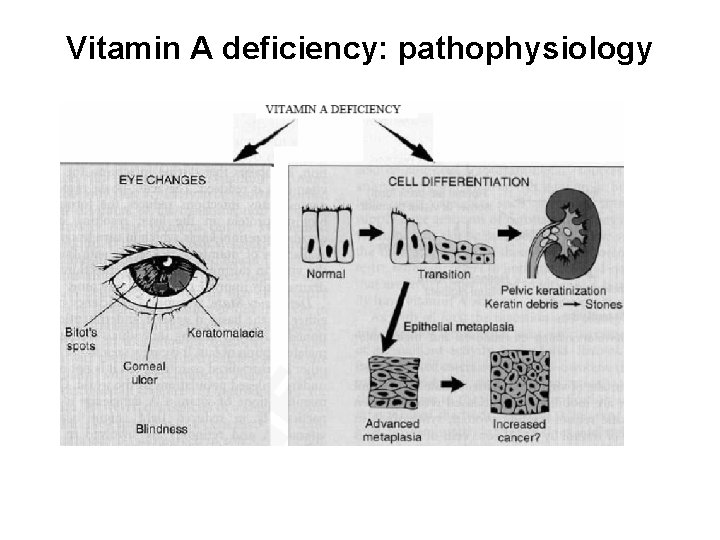
Vitamin A deficiency: pathophysiology

Vitamin A deficiency Treatment • Night blindness, poor wound healing, and other signs of early deficiency can be effectively treated orally with 30, 000 international units of vitamin A daily for 1 week. • Advanced deficiency with corneal damage calls for administration of 20, 000 international units/kg orally for at least 5 days.

Thank you
 Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Hyperglyceremia
Hyperglyceremia Nutritional diseases
Nutritional diseases Nutritional diseases
Nutritional diseases Moderate acute malnutrition
Moderate acute malnutrition Malnutrition case
Malnutrition case Marasmus vs kwashiorkor
Marasmus vs kwashiorkor Kwashiorkor and marasmus
Kwashiorkor and marasmus Marasmo y kwashiorkor
Marasmo y kwashiorkor Clasificación de wellcome
Clasificación de wellcome Nursing diagnosis of marasmus
Nursing diagnosis of marasmus Kwashiorkor
Kwashiorkor Kwashiorkor vs marasmus
Kwashiorkor vs marasmus Marasmo
Marasmo Pem komplikasyonları nelerdir
Pem komplikasyonları nelerdir Vegetarian diet
Vegetarian diet Wellcome classification
Wellcome classification Cachexia vs marasmus
Cachexia vs marasmus Kwashiorkor and marasmus
Kwashiorkor and marasmus Causes of kwashiorkor
Causes of kwashiorkor Pengertian kwashiorkor
Pengertian kwashiorkor Mini nutritional assessment short form
Mini nutritional assessment short form Acute resuscitation plan
Acute resuscitation plan Conceptual framework on the causes of malnutrition
Conceptual framework on the causes of malnutrition Hypothemi
Hypothemi Wellcome classification
Wellcome classification Kanawati index
Kanawati index Holliday segar calories
Holliday segar calories Maternal and child malnutrition
Maternal and child malnutrition Definition malnutrition
Definition malnutrition Malnutrition
Malnutrition