PROTEIN ENERGY MALNUTRITION DEFINITION A state of nutrition












- Slides: 68
PROTEIN ENERGY MALNUTRITION
DEFINITION ‘A state of nutrition in which a deficiency (or imbalance) of energy, protein & other nutrients causes measurable adverse effects on tissue/body structure & function & clinical outcome’
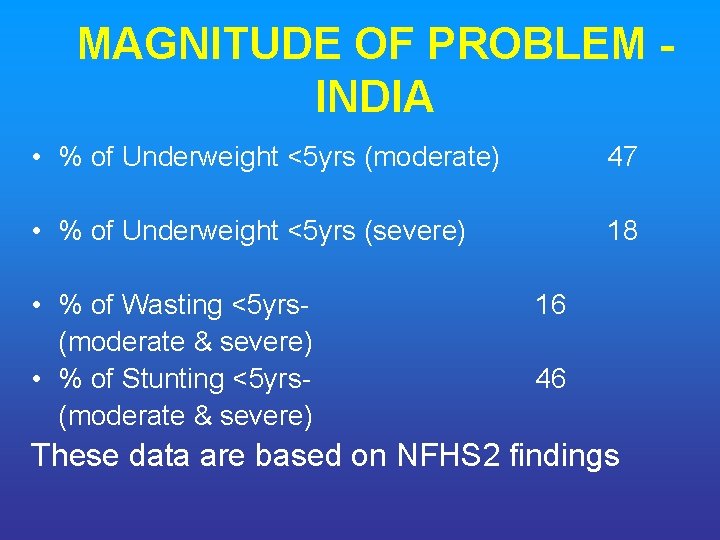
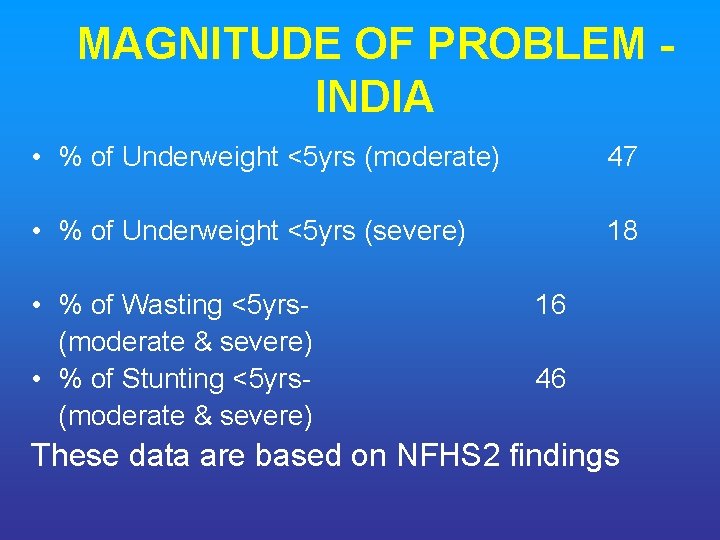
MAGNITUDE OF PROBLEM INDIA • % of Underweight <5 yrs (moderate) 47 • % of Underweight <5 yrs (severe) 18 • % of Wasting <5 yrs(moderate & severe) • % of Stunting <5 yrs(moderate & severe) 16 46 These data are based on NFHS 2 findings

BASIS OF CLASSIFICATION 1. Weight - for – Age 2. Weight- for – Age & Edema 3. Weight – for – Height & Height-forage 4. SD Scores 5. Mid-arm Circumference
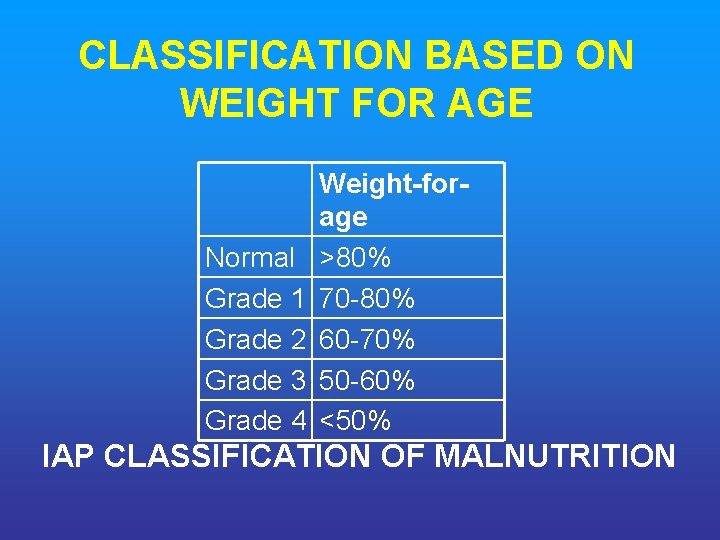
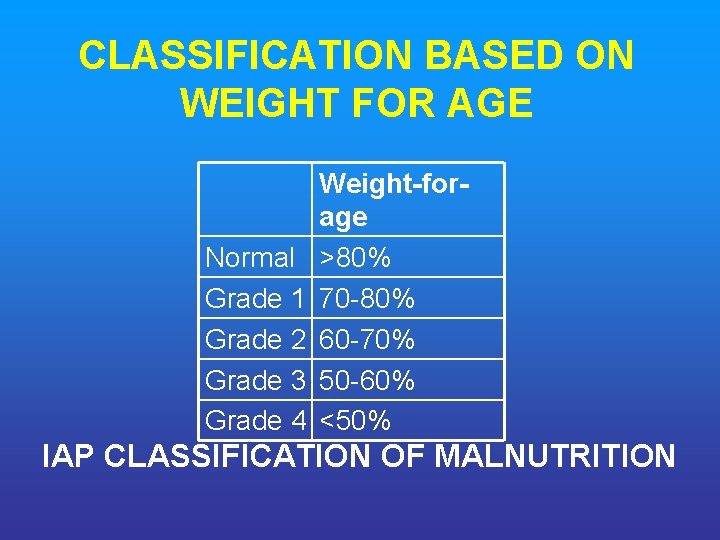
CLASSIFICATION BASED ON WEIGHT FOR AGE Weight for age Normal >80% Grade 1 70 -80% Grade 2 60 -70% Grade 3 50 -60% Grade 4 <50% IAP CLASSIFICATION OF MALNUTRITION
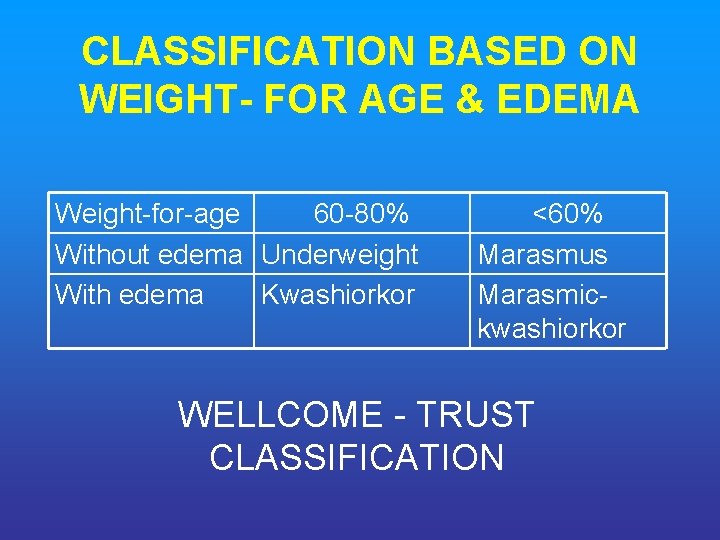
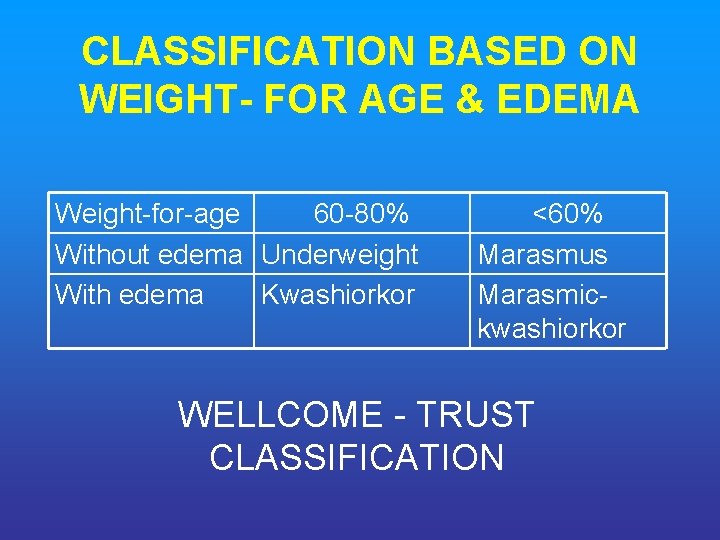
CLASSIFICATION BASED ON WEIGHT FOR AGE & EDEMA Weight-for-age 60 -80% Without edema Underweight With edema Kwashiorkor <60% Marasmus Marasmic- kwashiorkor WELLCOME - TRUST CLASSIFICATION

CLASIFICATION BASED ON WEIGHT FOR HEIGHT & HEIGHT FOR AGE Weight-for. Height >80% <80% Height-for-age >90% <90% Normal Stunted Wasted & Stunted WATERLOW CLASSIFICATION

CLASSIFICATION BASED ON SD SCORES Moderate malnutrition Symmetrical oedema Weight-for-height (measure of wasting) Height-for-age (measure of WHO stunting) Severe malnutrition No Yes Between -3 SD & - 2 SD score(70– 79%) SD-score <-3 (<70%) (severe wasting) Between SD-score <-3 (<85%) -3 SD & - 2 SD CLASSIFICATION OF (severe stunting) score (85– 89%) MALNUTRITION
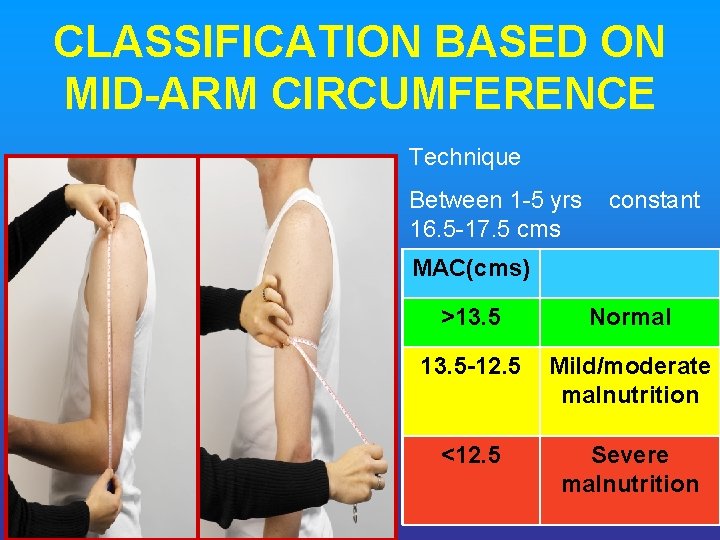
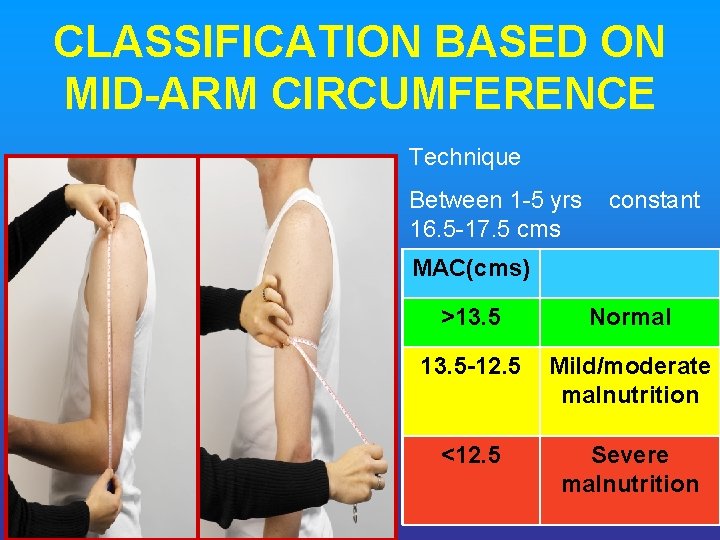
CLASSIFICATION BASED ON MID ARM CIRCUMFERENCE Technique Between 1 -5 yrs constant 16. 5 -17. 5 cms MAC(cms) >13. 5 Normal 13. 5 12. 5 Mild/moderate malnutrition <12. 5 Severe malnutrition
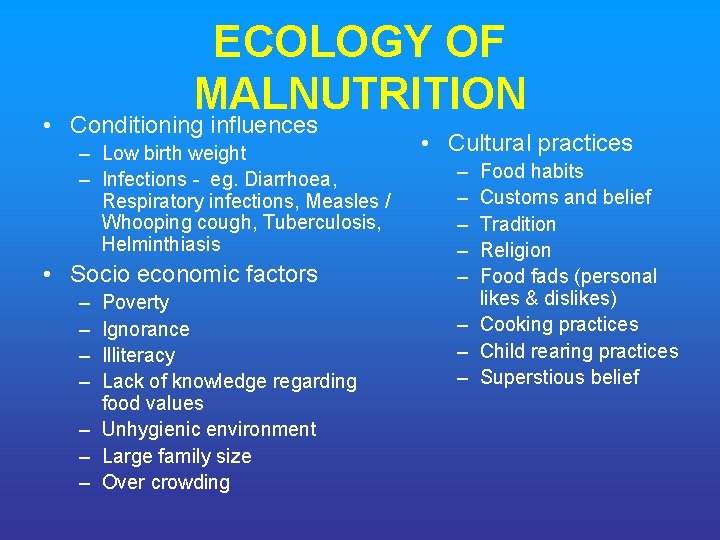
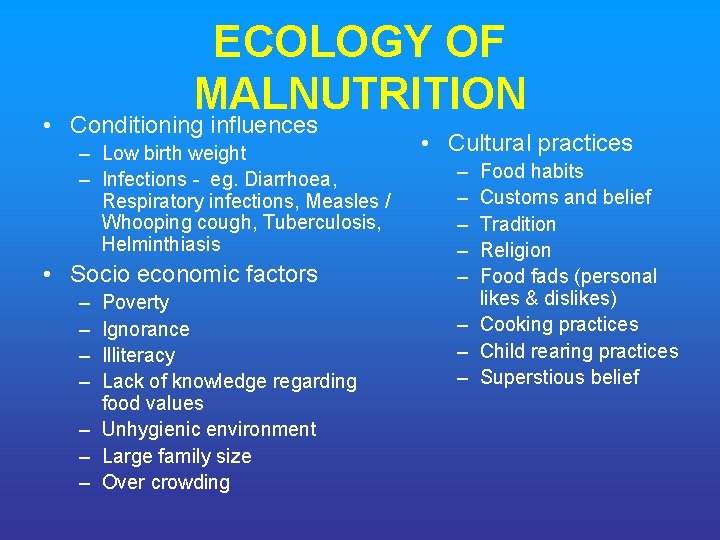
ECOLOGY OF MALNUTRITION • Conditioning influences – Low birth weight – Infections - eg. Diarrhoea, Respiratory infections, Measles / Whooping cough, Tuberculosis, Helminthiasis • Socio economic factors – – Poverty Ignorance Illiteracy Lack of knowledge regarding food values – Unhygienic environment – Large family size – Over crowding • Cultural practices – – – Food habits Customs and belief Tradition Religion Food fads (personal likes & dislikes) – Cooking practices – Child rearing practices – Superstious belief

THEORIES OF MALNUTRITION • • Protein deficiency Toxic theory Niacin theory Increased ferritin level Dr. Gopalan’s dysadaptation theory Free radical theory New theory Aflatoxin poisoning
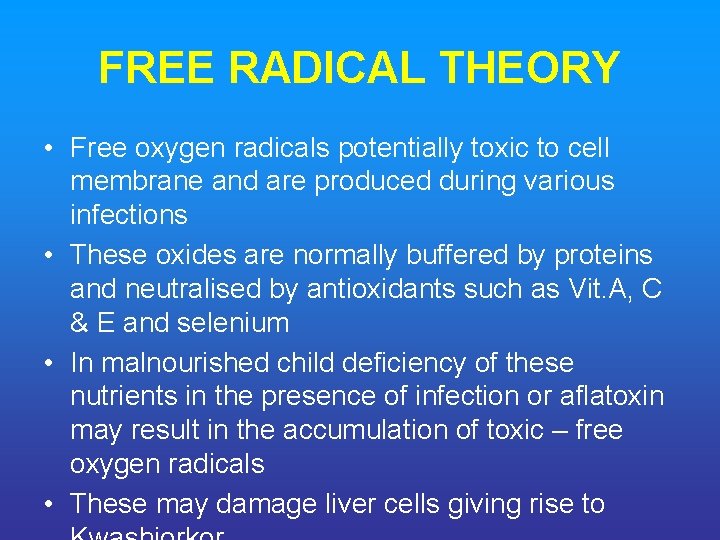
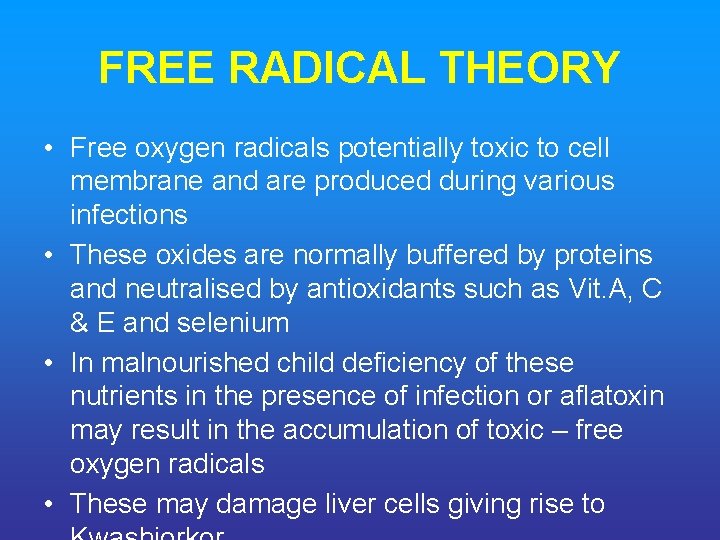
FREE RADICAL THEORY • Free oxygen radicals potentially toxic to cell membrane and are produced during various infections • These oxides are normally buffered by proteins and neutralised by antioxidants such as Vit. A, C & E and selenium • In malnourished child deficiency of these nutrients in the presence of infection or aflatoxin may result in the accumulation of toxic – free oxygen radicals • These may damage liver cells giving rise to
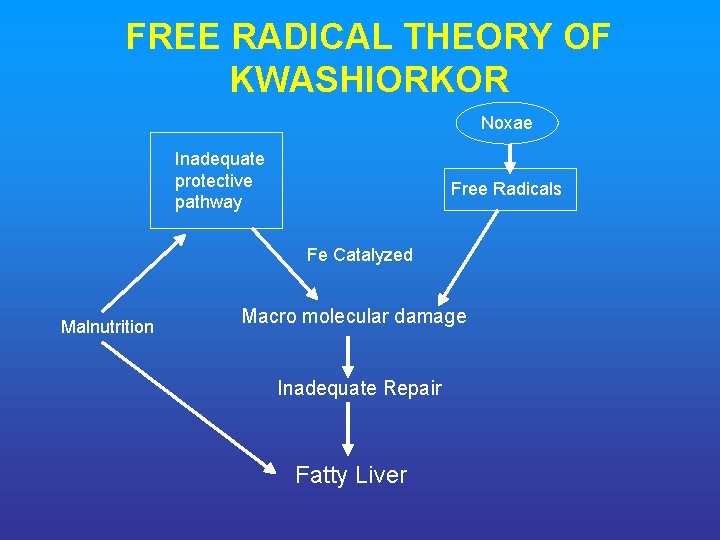
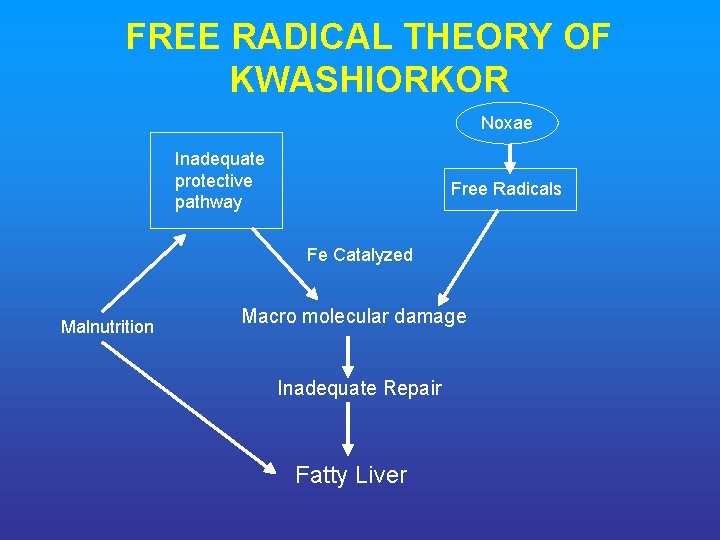
FREE RADICAL THEORY OF KWASHIORKOR Noxae Inadequate protective pathway Free Radicals Fe Catalyzed Malnutrition Macro molecular damage Inadequate Repair Fatty Liver
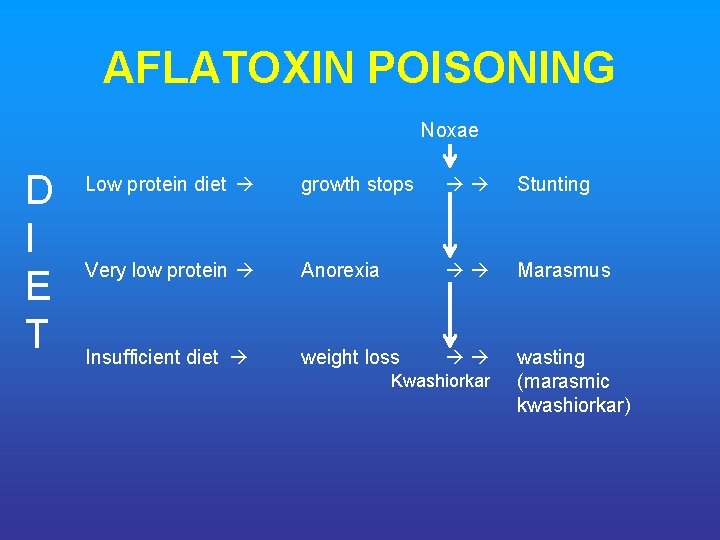
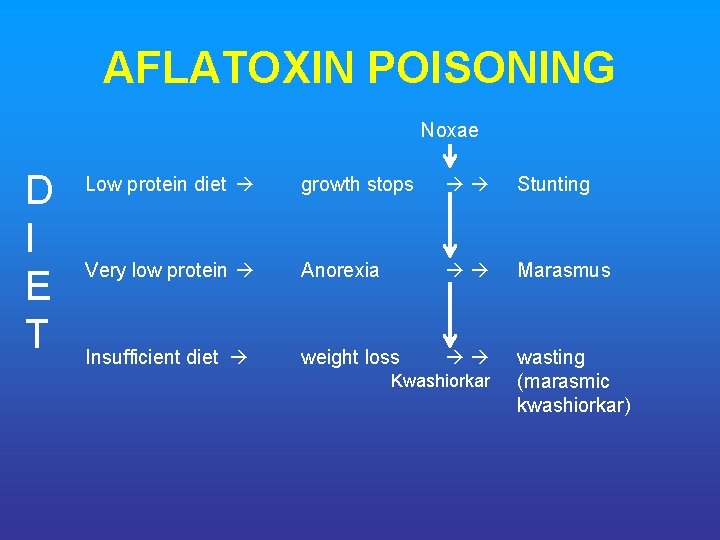
AFLATOXIN POISONING Noxae D I E T Low protein diet growth stops Stunting Very low protein Anorexia Marasmus Insufficient diet weight loss wasting (marasmic kwashiorkar) Kwashiorkar
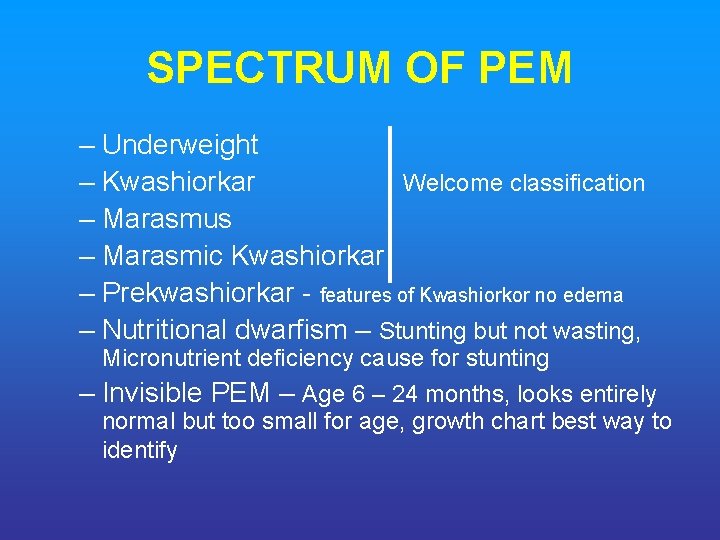
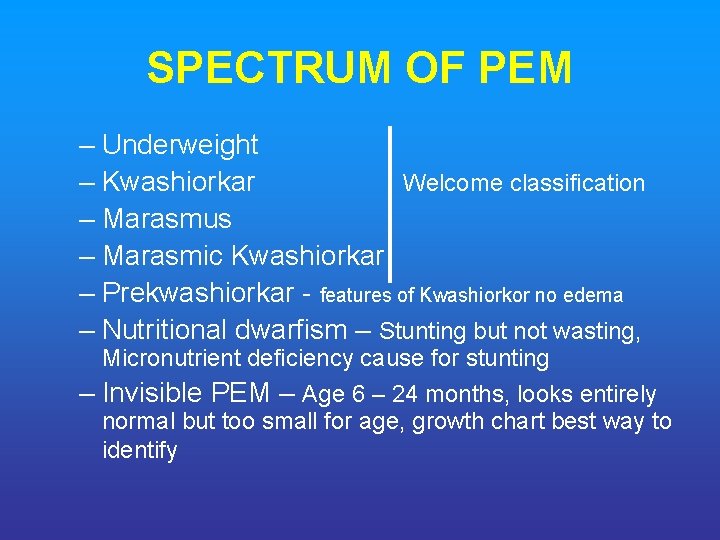
SPECTRUM OF PEM – Underweight – Kwashiorkar Welcome classification – Marasmus – Marasmic Kwashiorkar – Prekwashiorkar - features of Kwashiorkor no edema – Nutritional dwarfism – Stunting but not wasting, Micronutrient deficiency cause for stunting – Invisible PEM – Age 6 – 24 months, looks entirely normal but too small for age, growth chart best way to identify
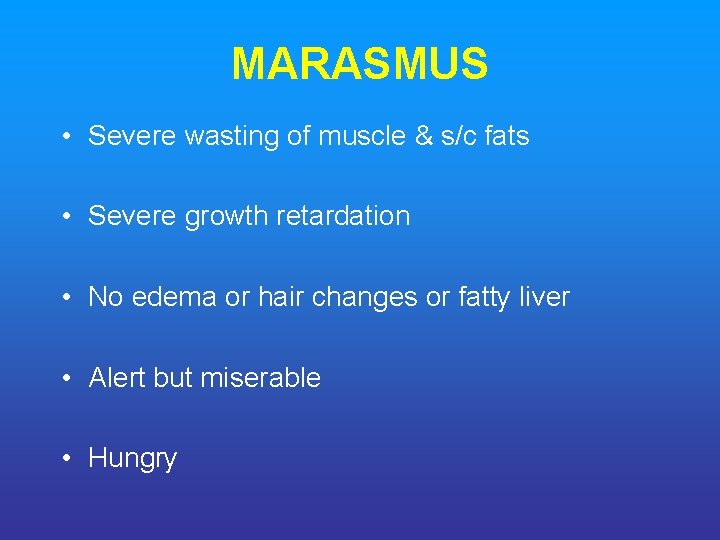
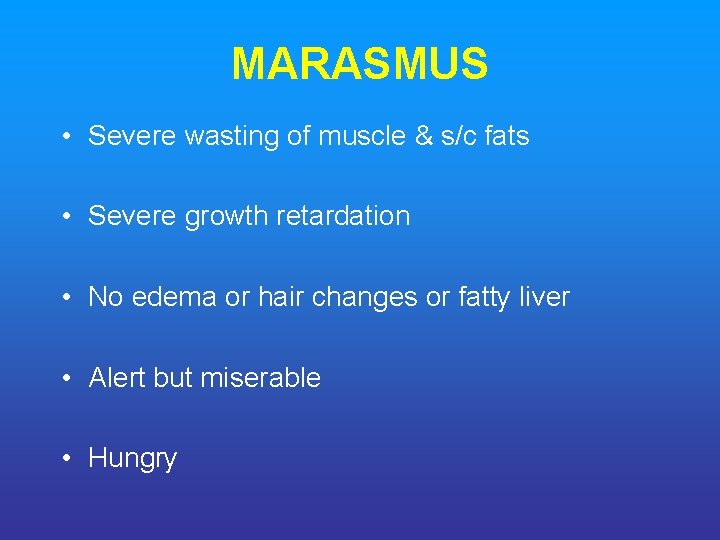
MARASMUS • Severe wasting of muscle & s/c fats • Severe growth retardation • No edema or hair changes or fatty liver • Alert but miserable • Hungry

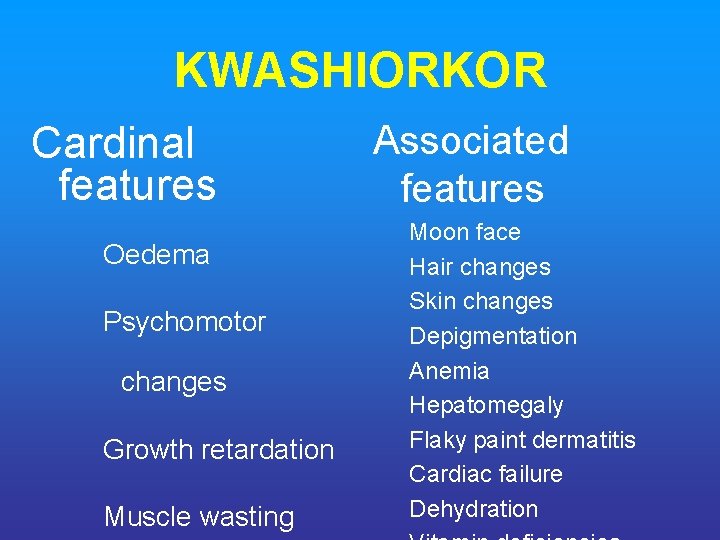
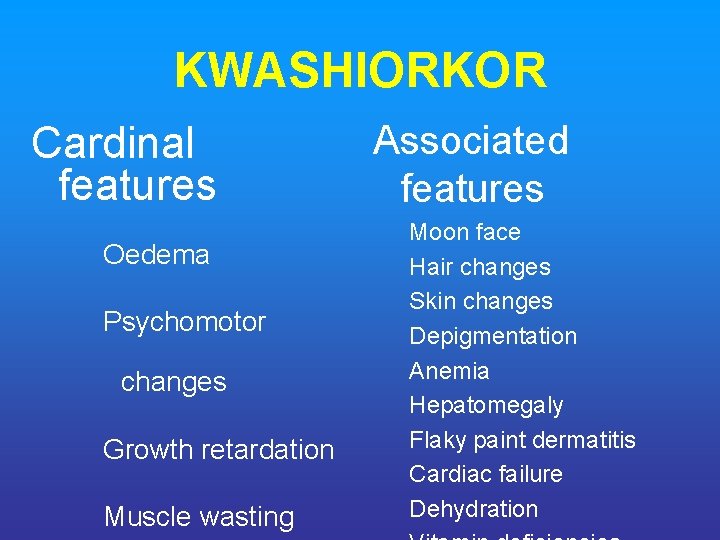
KWASHIORKOR Cardinal features Oedema Psychomotor changes Growth retardation Muscle wasting Associated features Moon face Hair changes Skin changes Depigmentation Anemia Hepatomegaly Flaky paint dermatitis Cardiac failure Dehydration


MARASMIC KWASHIORKOR • Syndrome seen in marasmic children, with severe muscle & fat wasting who suddenly develop oedema, due to increased protein deficiency than before. • Thus clinical features, combination of Marasmus & Kwashiorkor. • Anemia is moderate & one/ more Vitamin deficiencies may be evident.
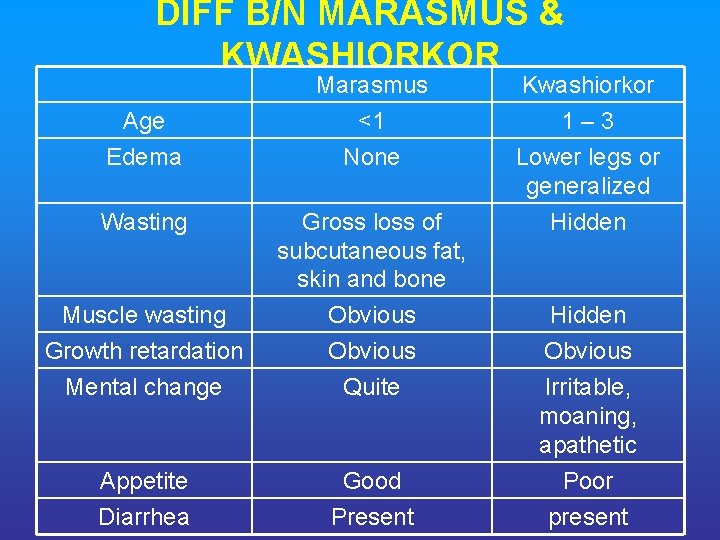
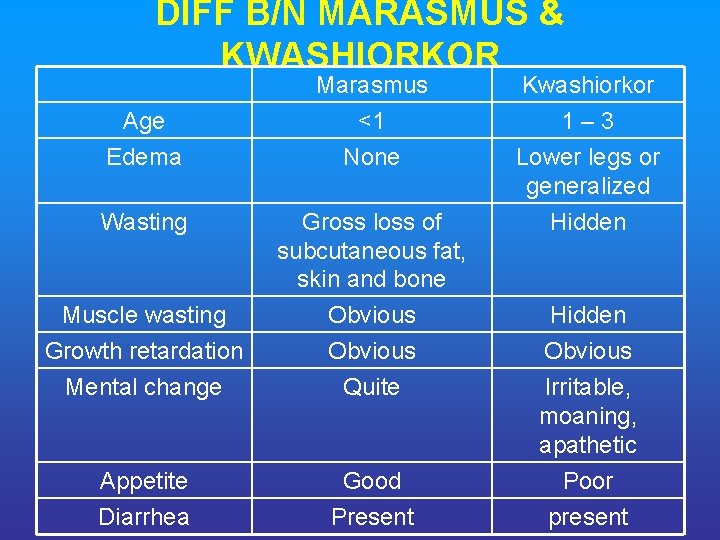
DIFF B/N MARASMUS & KWASHIORKOR Marasmus <1 None Kwashiorkor 1 – 3 Lower legs or generalized Hidden Muscle wasting Growth retardation Mental change Gross loss of subcutaneous fat, skin and bone Obvious Quite Appetite Diarrhea Good Present Age Edema Wasting Hidden Obvious Irritable, moaning, apathetic Poor present
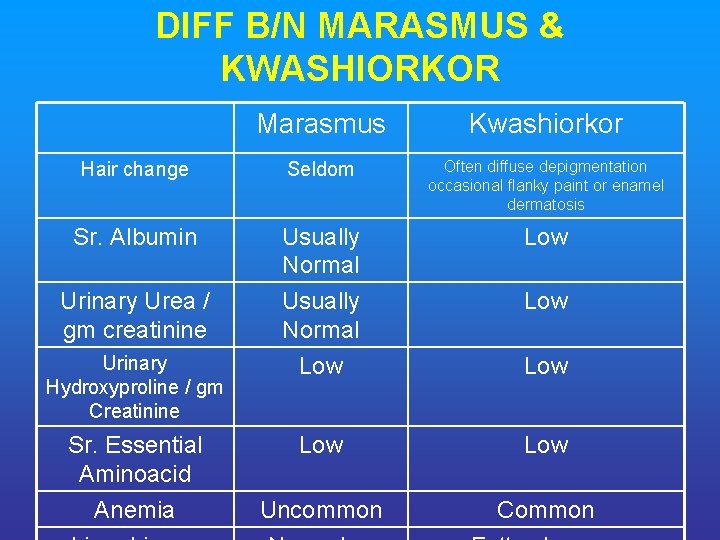
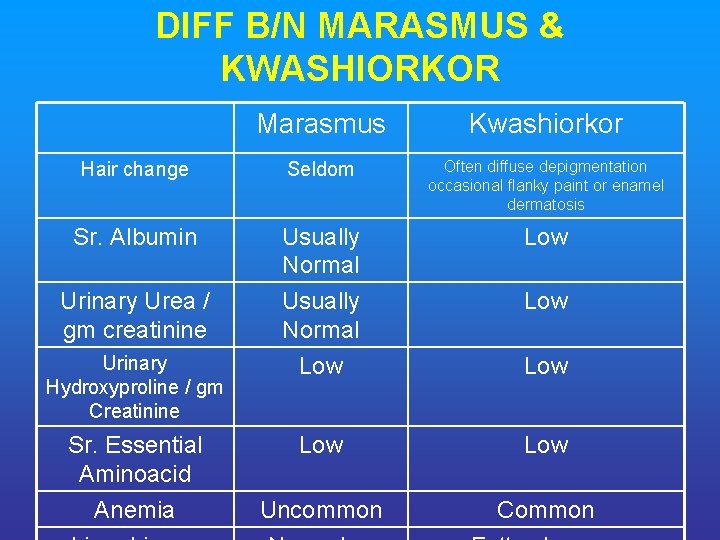
DIFF B/N MARASMUS & KWASHIORKOR Marasmus Kwashiorkor Hair change Seldom Often diffuse depigmentation occasional flanky paint or enamel dermatosis Sr. Albumin Usually Normal Low Urinary Urea / gm creatinine Usually Normal Low Low Uncommon Common Urinary Hydroxyproline / gm Creatinine Sr. Essential Aminoacid Anemia Low
INFECTION & IMMUNITY IN PEM • Infection & Immunity interrelated to PEM • Infectious disease worsens in PEM & vise versa PEM usually weakens resistance to infection, when worsens results in high mortality among toddlers & under 5 children • These children may present with episodes of acute infection or recurrent chronic insidious infection may go undetected unless specifically looked for i. e. Recurrent attacks of diarrhoeal diseases, pneumonia, septicaemia, measles, tuberculosis and malaria common, Urinary tract infection often occur but may go undetected, have to be suspected. • Intestinal parasitosis ascariasis, ankylostomiasis & Giardiasis frequent
IMMUNITY • Humoral : Ig G, Ig. M & Secretory Ig A not significantly affected in mild to moderate PEM, hence host respond well to bacterial challenges & viral vaccines. • But depressed in severe PEM with infections • Cell Mediated Immunity (CMI) : is impaired in all grades of PEM except Gr I, severely impaired in G III & Gr IV PEM & Kwashiorkor • This explains –ve Tuberculin test in Marasmus & Kwashiorkor in spite active TB • Following dietary treatment when the pt. improves, T Test may convert to +ve. • Serum C reactive Protein & Complement C 3 are depressed in severe PEM, but rise in presence of infection & behave as acute phase reactants.
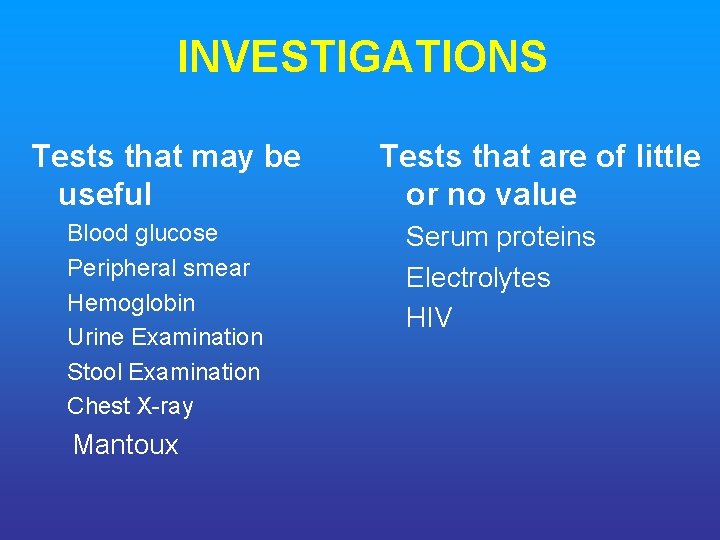
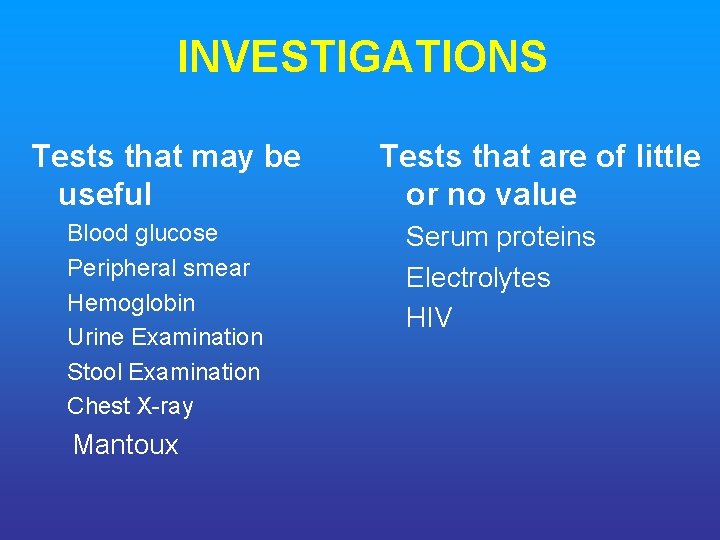
INVESTIGATIONS Tests that may be useful Blood glucose Peripheral smear Hemoglobin Urine Examination Stool Examination Chest X-ray Mantoux Tests that are of little or no value Serum proteins Electrolytes HIV
COMPLICATIONS • • Hypoglycemia Hypothermia Infections (bacterial, viral & fungal) Hypokalemia Hyponatremia Dehydration & shock Heart failure
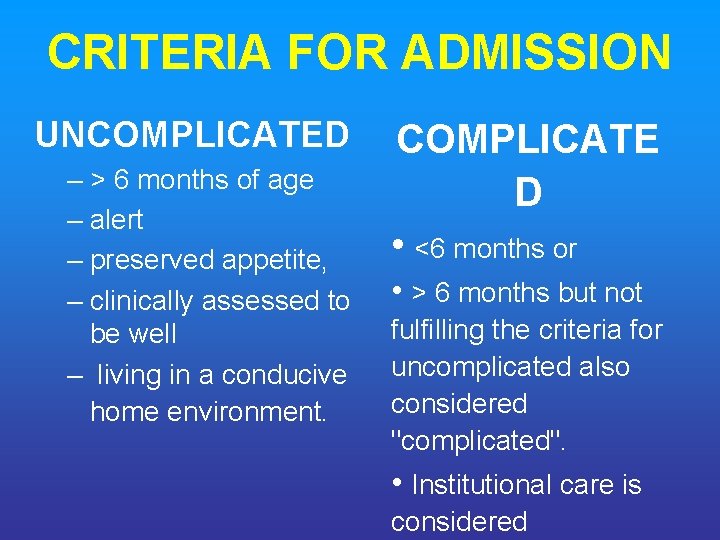
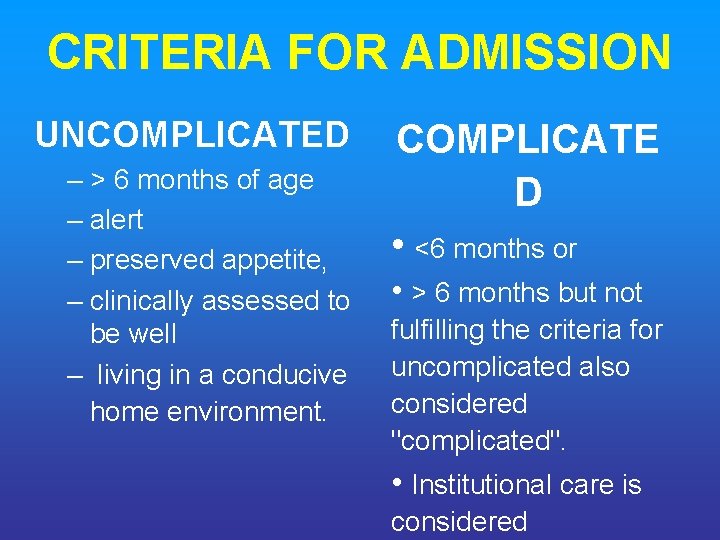
CRITERIA FOR ADMISSION UNCOMPLICATED – > 6 months of age – alert – preserved appetite, – clinically assessed to be well – living in a conducive home environment. COMPLICATE D • <6 months or • > 6 months but not fulfilling the criteria for uncomplicated also considered "complicated". • Institutional care is considered
WHO GUIDELINES FOR THE IN PATIENT TREATMENT OF SEVERELY MALNOURISHED CHILDREN
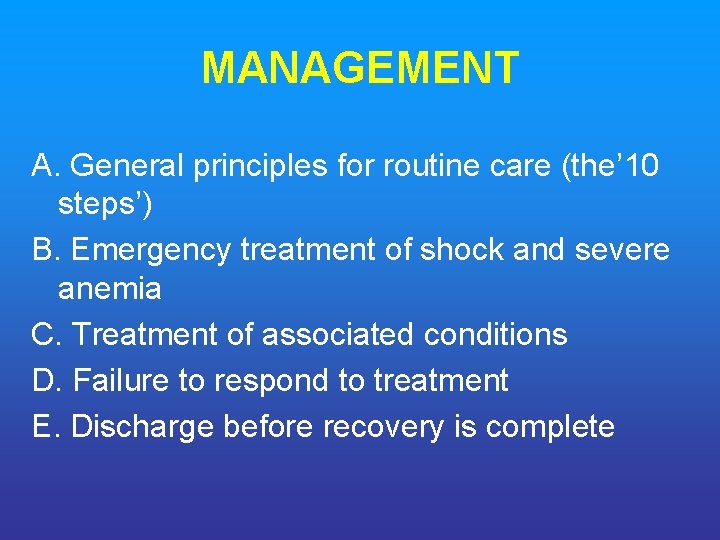
MANAGEMENT A. General principles for routine care (the’ 10 steps’) B. Emergency treatment of shock and severe anemia C. Treatment of associated conditions D. Failure to respond to treatment E. Discharge before recovery is complete
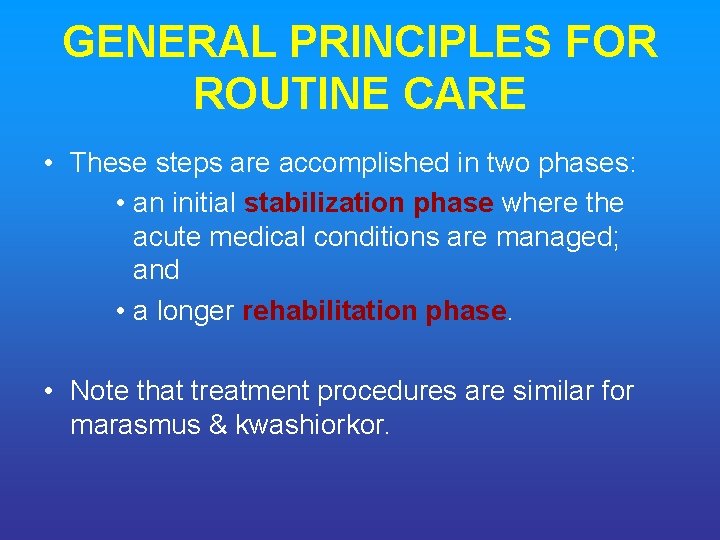
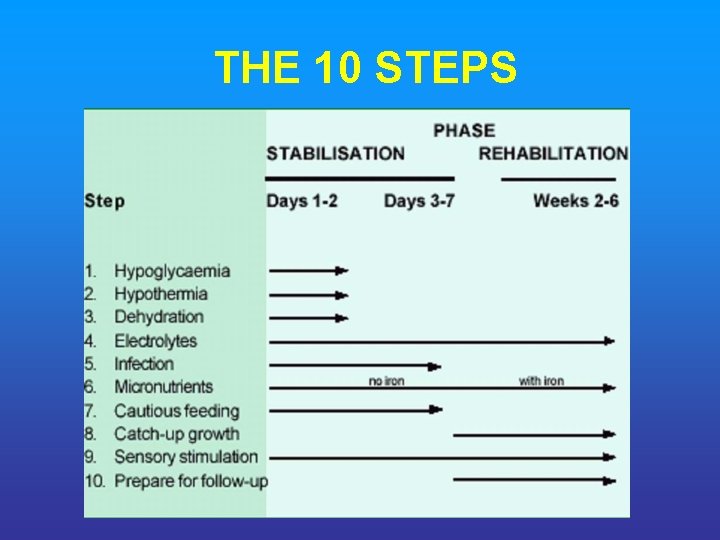
GENERAL PRINCIPLES FOR ROUTINE CARE • These steps are accomplished in two phases: • an initial stabilization phase where the acute medical conditions are managed; and • a longer rehabilitation phase. • Note that treatment procedures are similar for marasmus & kwashiorkor.
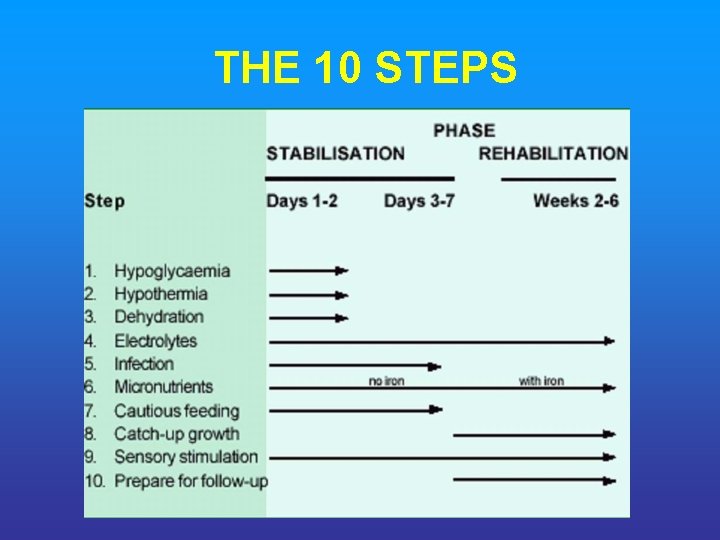
THE 10 STEPS
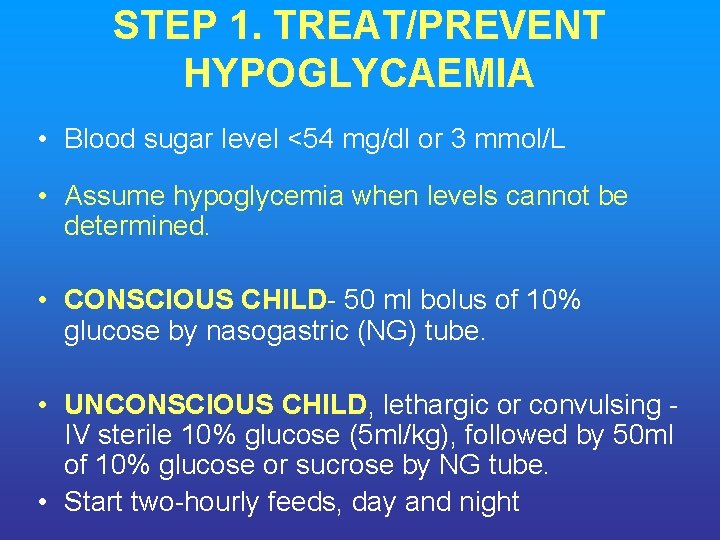
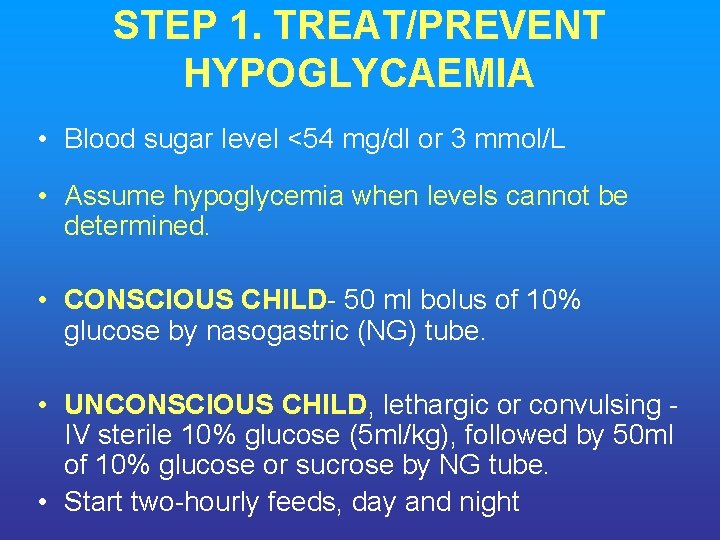
STEP 1. TREAT/PREVENT HYPOGLYCAEMIA • Blood sugar level <54 mg/dl or 3 mmol/L • Assume hypoglycemia when levels cannot be determined. • CONSCIOUS CHILD- 50 ml bolus of 10% glucose by nasogastric (NG) tube. • UNCONSCIOUS CHILD, lethargic or convulsing IV sterile 10% glucose (5 ml/kg), followed by 50 ml of 10% glucose or sucrose by NG tube. • Start two-hourly feeds, day and night
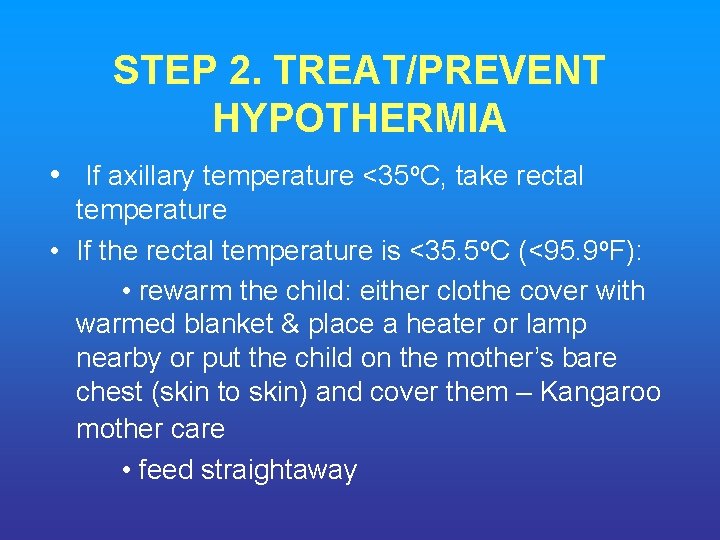
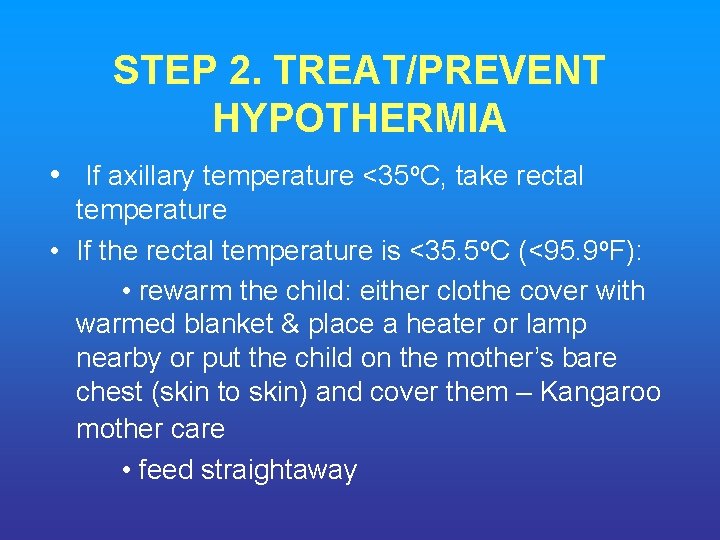
STEP 2. TREAT/PREVENT HYPOTHERMIA • If axillary temperature <35 o. C, take rectal temperature • If the rectal temperature is <35. 5 o. C (<95. 9 o. F): • rewarm the child: either clothe cover with warmed blanket & place a heater or lamp nearby or put the child on the mother’s bare chest (skin to skin) and cover them – Kangaroo mother care • feed straightaway
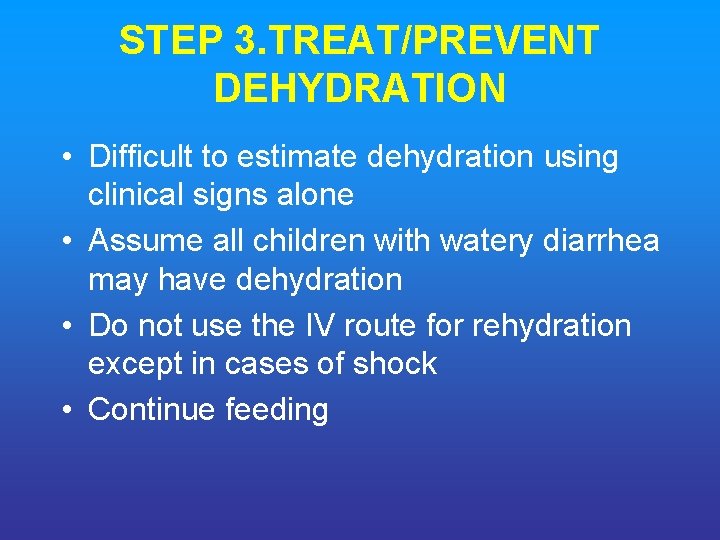
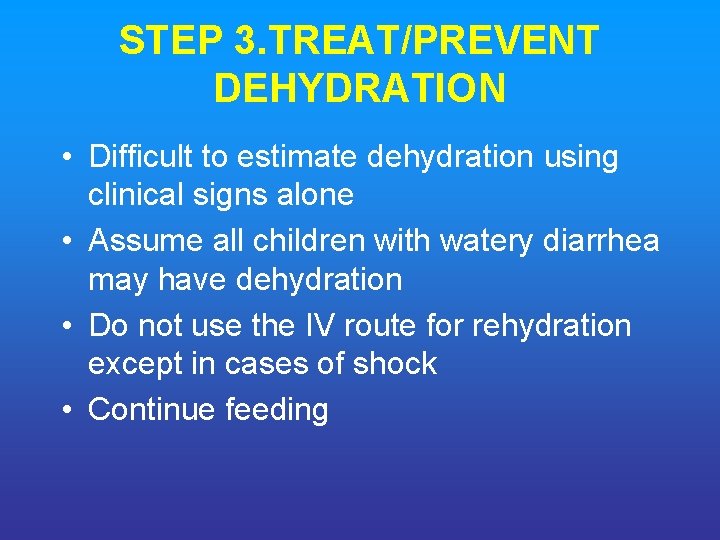
STEP 3. TREAT/PREVENT DEHYDRATION • Difficult to estimate dehydration using clinical signs alone • Assume all children with watery diarrhea may have dehydration • Do not use the IV route for rehydration except in cases of shock • Continue feeding
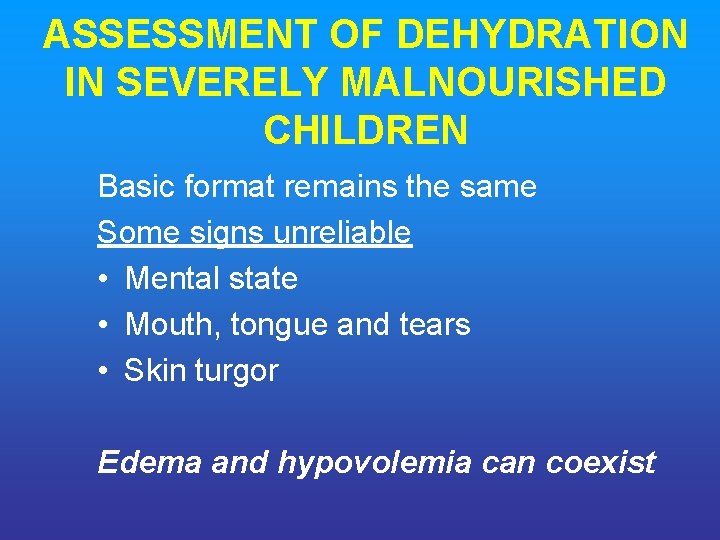
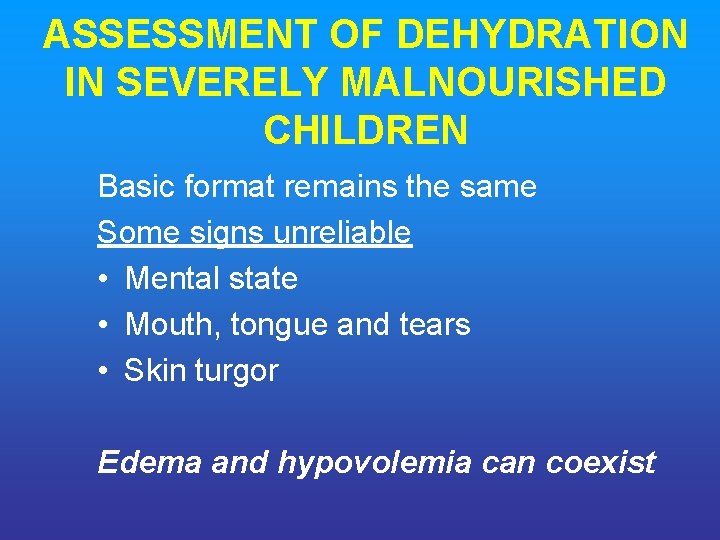
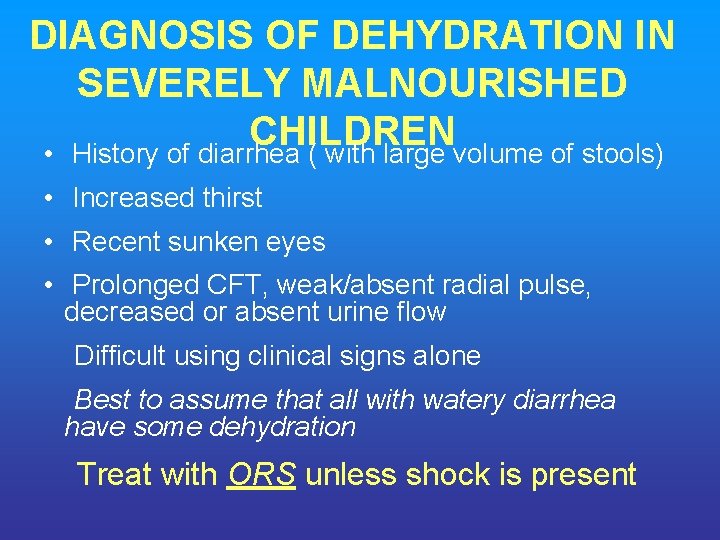
ASSESSMENT OF DEHYDRATION IN SEVERELY MALNOURISHED CHILDREN Basic format remains the same Some signs unreliable • Mental state • Mouth, tongue and tears • Skin turgor Edema and hypovolemia can coexist
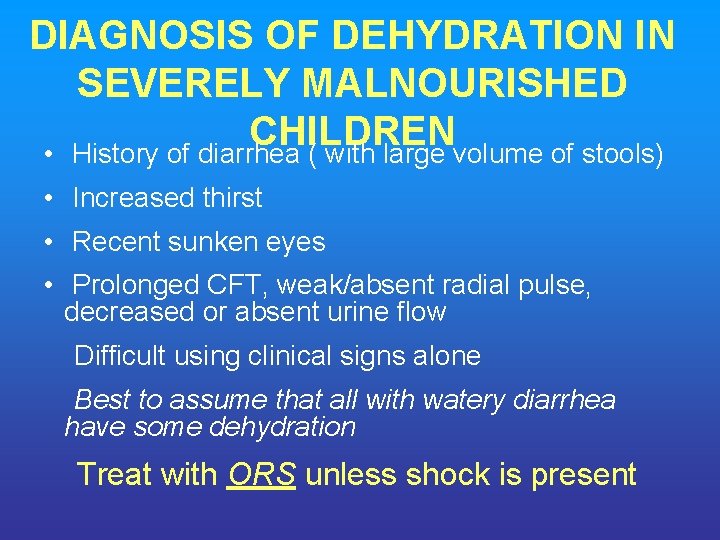
DIAGNOSIS OF DEHYDRATION IN SEVERELY MALNOURISHED CHILDREN • History of diarrhea ( with large volume of stools) • Increased thirst • Recent sunken eyes • Prolonged CFT, weak/absent radial pulse, decreased or absent urine flow Difficult using clinical signs alone Best to assume that all with watery diarrhea have some dehydration Treat with ORS unless shock is present
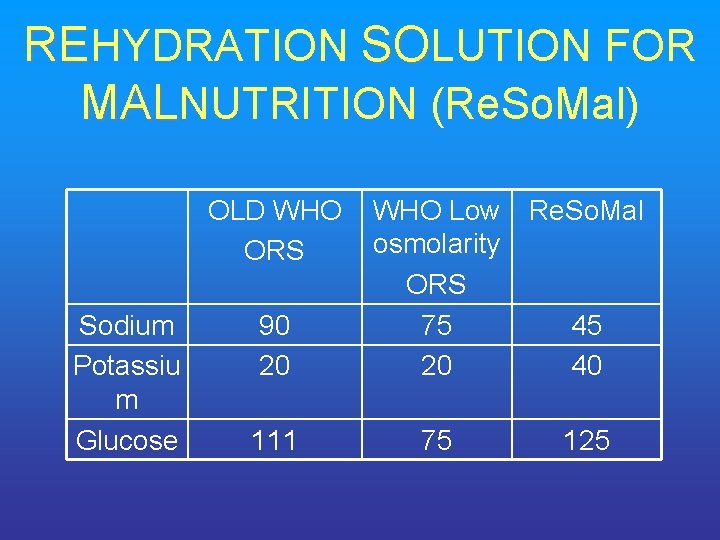
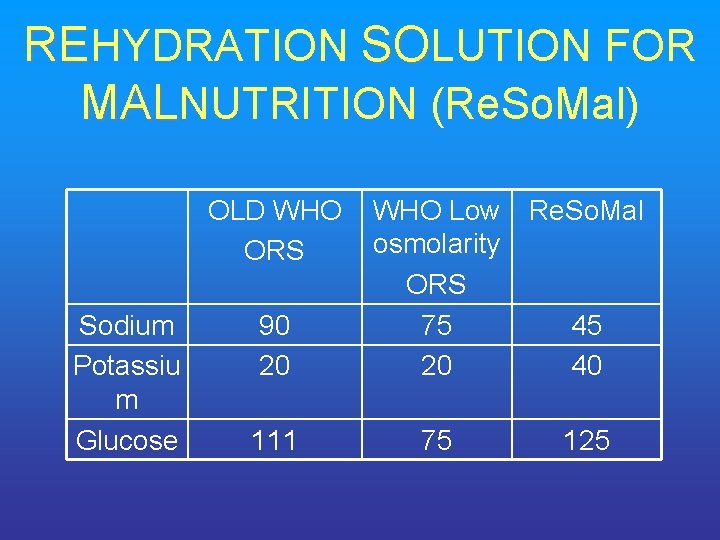
REHYDRATION SOLUTION FOR MALNUTRITION (Re. So. Mal) OLD WHO ORS Sodium Potassiu m Glucose 90 20 111 WHO Low Re. So. Mal osmolarity ORS 75 45 20 40 75 125
WHICH ORS SHOULD BE USED IN SEVERE MALNUTRITION? OPTIONS • Low osmolarity ORS with potassium supplements • Re. So. Mal (not available in India) IAP endorses the use of LOW OSMOLARITY WHO ORS for all types of diarrhea and nutritional status for logistics and programmatic advantages.
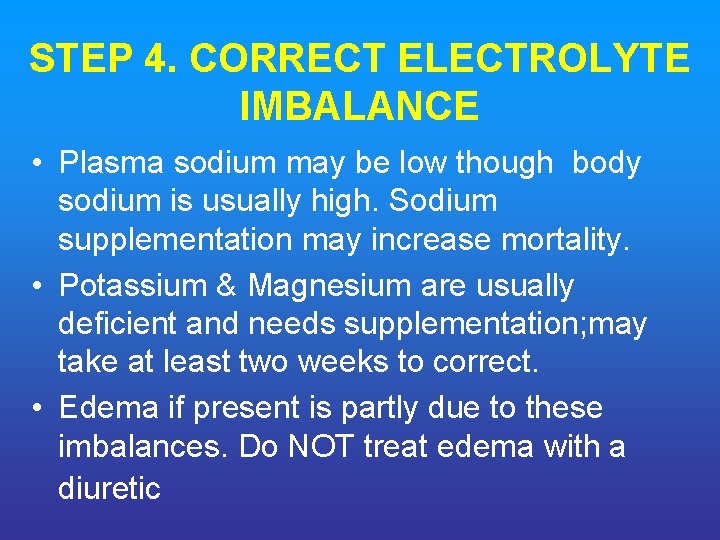
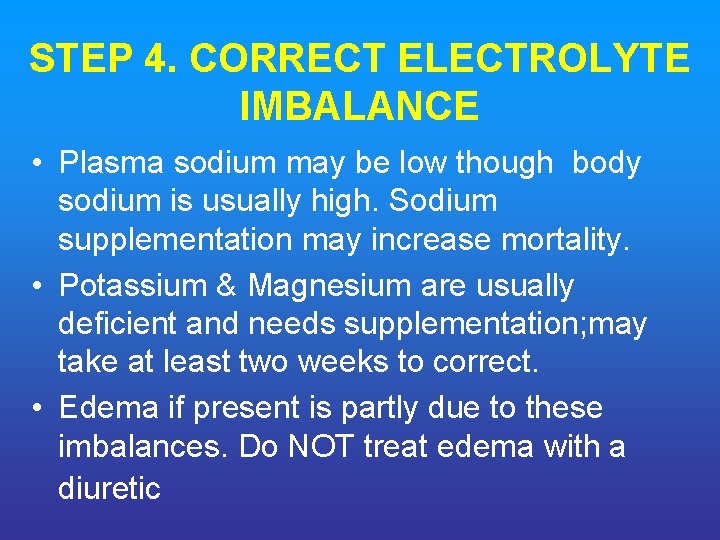
STEP 4. CORRECT ELECTROLYTE IMBALANCE • Plasma sodium may be low though body sodium is usually high. Sodium supplementation may increase mortality. • Potassium & Magnesium are usually deficient and needs supplementation; may take at least two weeks to correct. • Edema if present is partly due to these imbalances. Do NOT treat edema with a diuretic
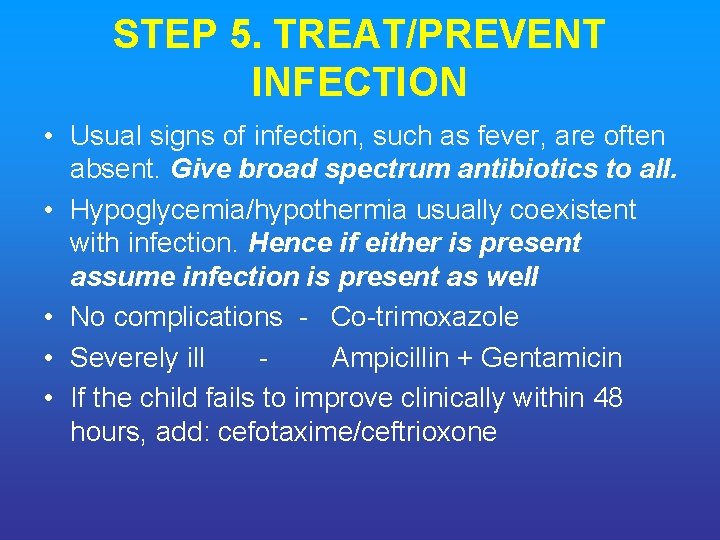
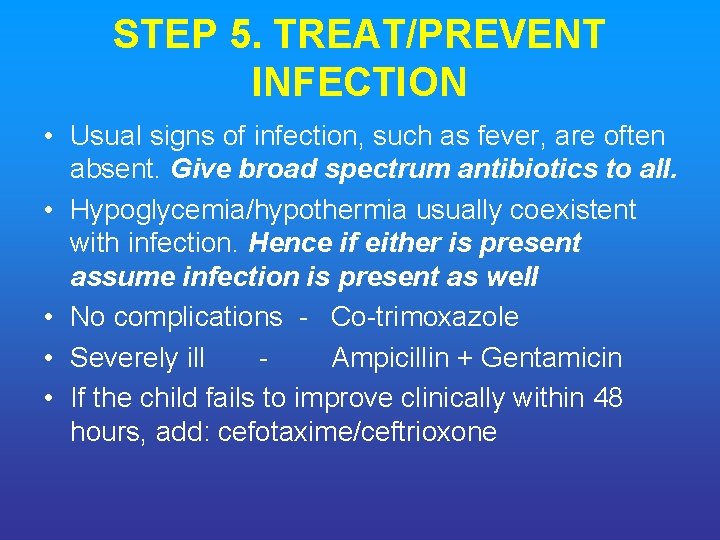
STEP 5. TREAT/PREVENT INFECTION • Usual signs of infection, such as fever, are often absent. Give broad spectrum antibiotics to all. • Hypoglycemia/hypothermia usually coexistent with infection. Hence if either is present assume infection is present as well • No complications - Co-trimoxazole • Severely ill Ampicillin + Gentamicin • If the child fails to improve clinically within 48 hours, add: cefotaxime/ceftrioxone
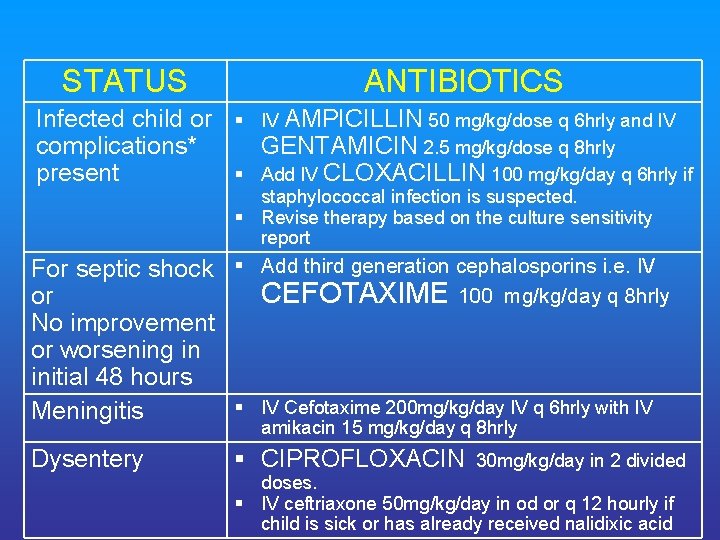
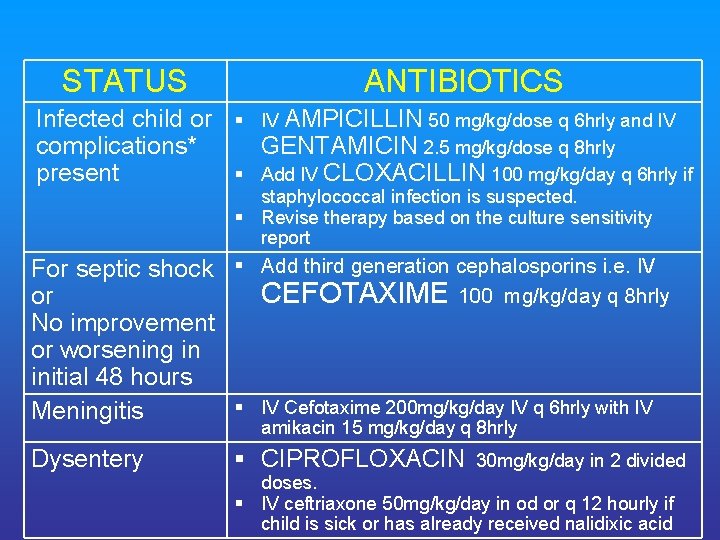
STATUS ANTIBIOTICS Infected child or complications* present § IV AMPICILLIN 50 mg/kg/dose q 6 hrly and IV GENTAMICIN 2. 5 mg/kg/dose q 8 hrly § Add IV CLOXACILLIN 100 mg/kg/day q 6 hrly if staphylococcal infection is suspected. § Revise therapy based on the culture sensitivity report For septic shock § Add third generation cephalosporins i. e. IV CEFOTAXIME 100 mg/kg/day q 8 hrly or No improvement or worsening in initial 48 hours § IV Cefotaxime 200 mg/kg/day IV q 6 hrly with IV Meningitis amikacin 15 mg/kg/day q 8 hrly Dysentery § CIPROFLOXACIN 30 mg/kg/day in 2 divided doses. § IV ceftriaxone 50 mg/kg/day in od or q 12 hourly if child is sick or has already received nalidixic acid
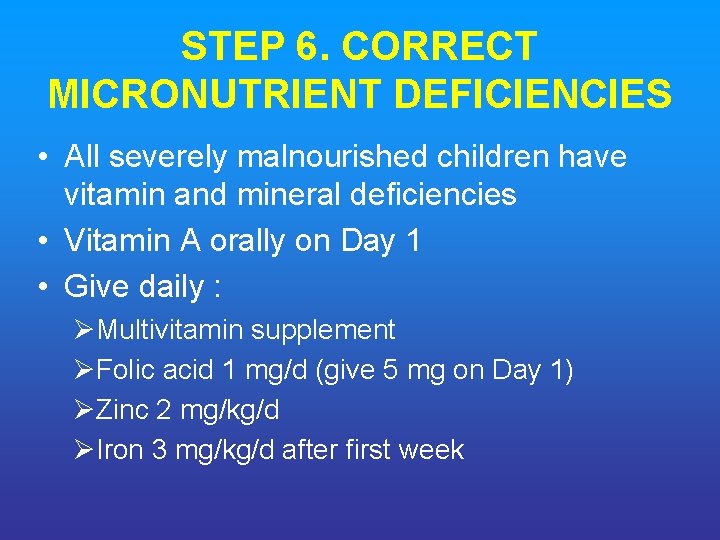
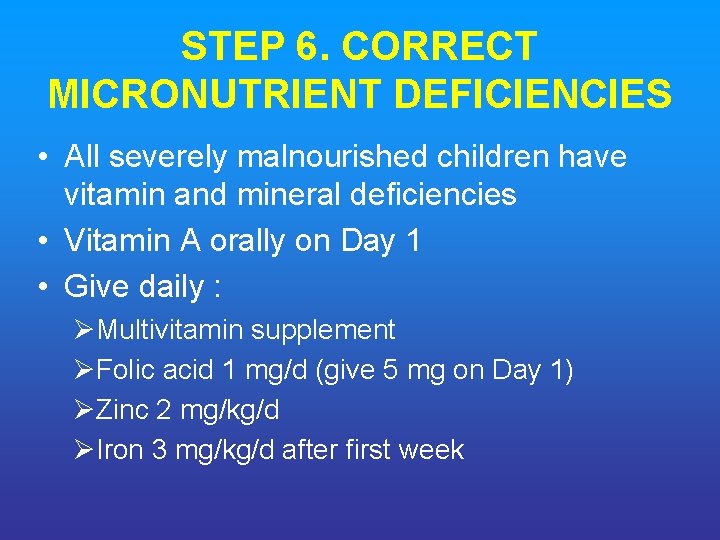
STEP 6. CORRECT MICRONUTRIENT DEFICIENCIES • All severely malnourished children have vitamin and mineral deficiencies • Vitamin A orally on Day 1 • Give daily : ØMultivitamin supplement ØFolic acid 1 mg/d (give 5 mg on Day 1) ØZinc 2 mg/kg/d ØIron 3 mg/kg/d after first week
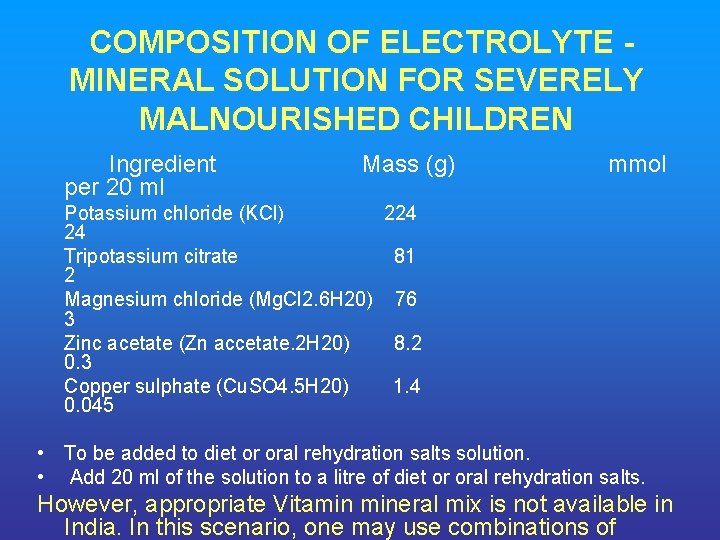
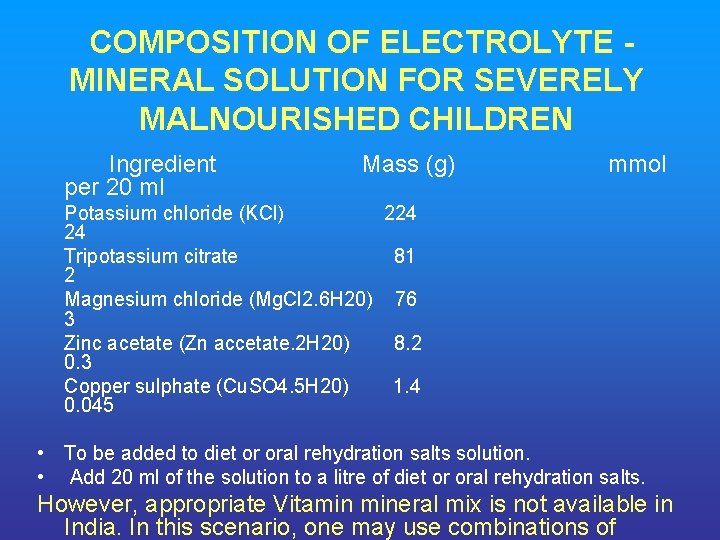
COMPOSITION OF ELECTROLYTE MINERAL SOLUTION FOR SEVERELY MALNOURISHED CHILDREN Ingredient Mass (g) mmol per 20 ml Potassium chloride (KCl) 224 24 Tripotassium citrate 81 2 Magnesium chloride (Mg. Cl 2. 6 H 20) 76 3 Zinc acetate (Zn accetate. 2 H 20) 8. 2 0. 3 Copper sulphate (Cu. SO 4. 5 H 20) 1. 4 0. 045 • To be added to diet or oral rehydration salts solution. • Add 20 ml of the solution to a litre of diet or oral rehydration salts. However, appropriate Vitamin mineral mix is not available in India. In this scenario, one may use combinations of
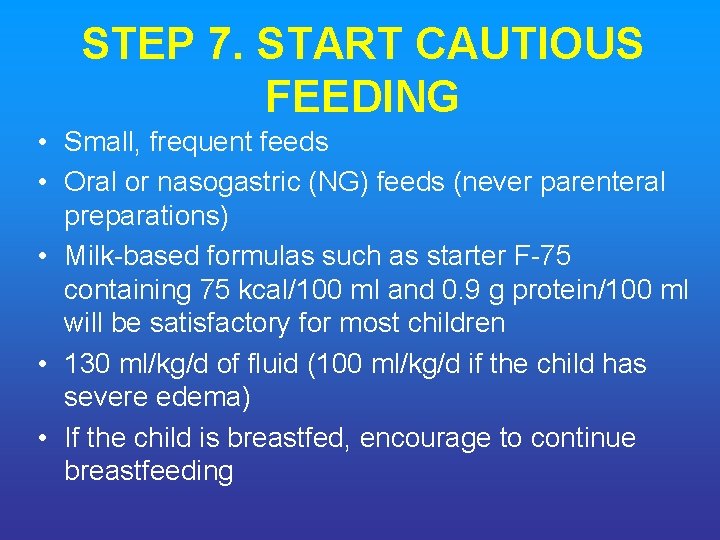
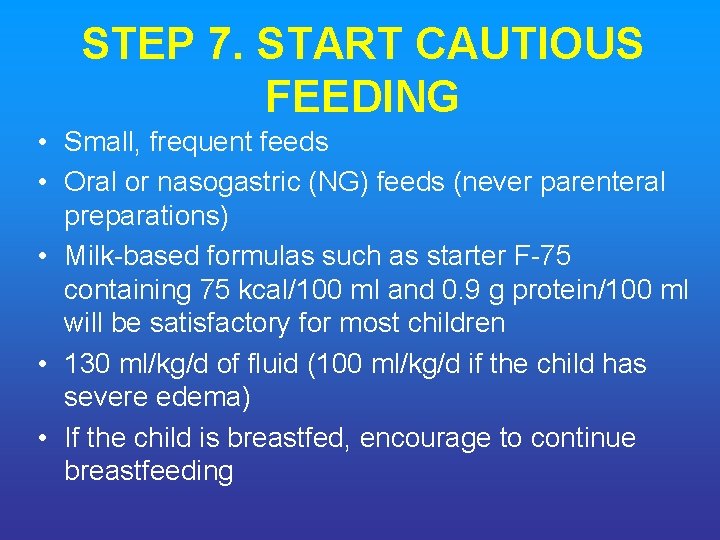
STEP 7. START CAUTIOUS FEEDING • Small, frequent feeds • Oral or nasogastric (NG) feeds (never parenteral preparations) • Milk-based formulas such as starter F-75 containing 75 kcal/100 ml and 0. 9 g protein/100 ml will be satisfactory for most children • 130 ml/kg/d of fluid (100 ml/kg/d if the child has severe edema) • If the child is breastfed, encourage to continue breastfeeding
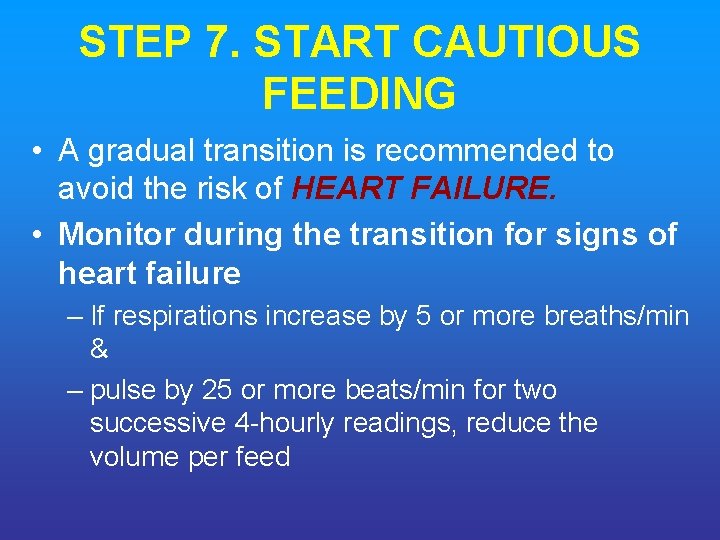
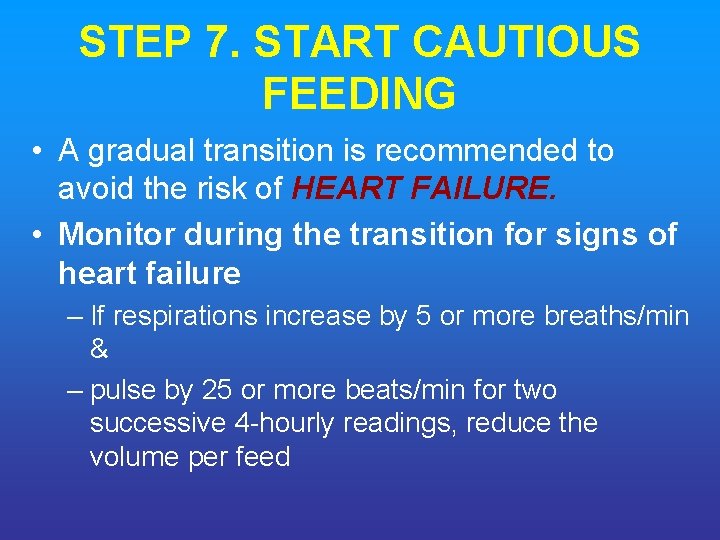
STEP 7. START CAUTIOUS FEEDING • A gradual transition is recommended to avoid the risk of HEART FAILURE. • Monitor during the transition for signs of heart failure – If respirations increase by 5 or more breaths/min & – pulse by 25 or more beats/min for two successive 4 -hourly readings, reduce the volume per feed
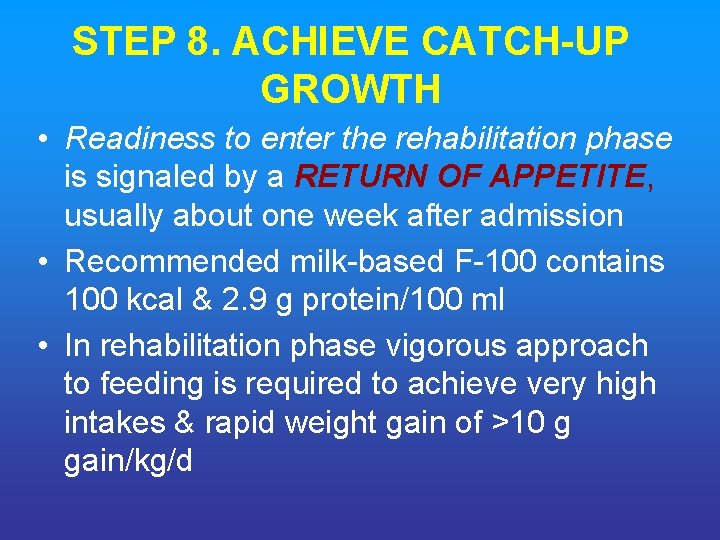
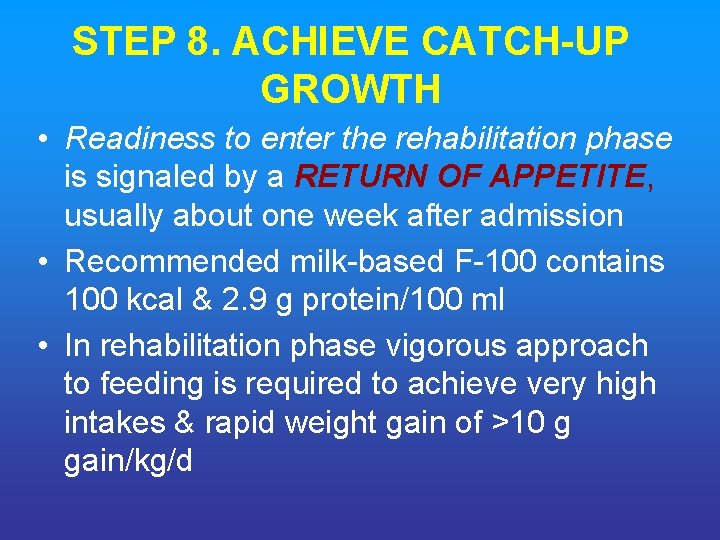
STEP 8. ACHIEVE CATCH UP GROWTH • Readiness to enter the rehabilitation phase is signaled by a RETURN OF APPETITE, usually about one week after admission • Recommended milk-based F-100 contains 100 kcal & 2. 9 g protein/100 ml • In rehabilitation phase vigorous approach to feeding is required to achieve very high intakes & rapid weight gain of >10 g gain/kg/d
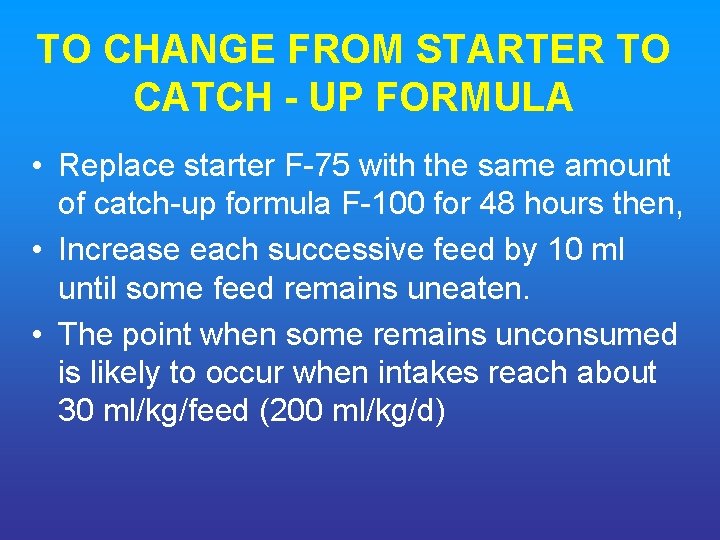
TO CHANGE FROM STARTER TO CATCH UP FORMULA • Replace starter F-75 with the same amount of catch-up formula F-100 for 48 hours then, • Increase each successive feed by 10 ml until some feed remains uneaten. • The point when some remains unconsumed is likely to occur when intakes reach about 30 ml/kg/feed (200 ml/kg/d)
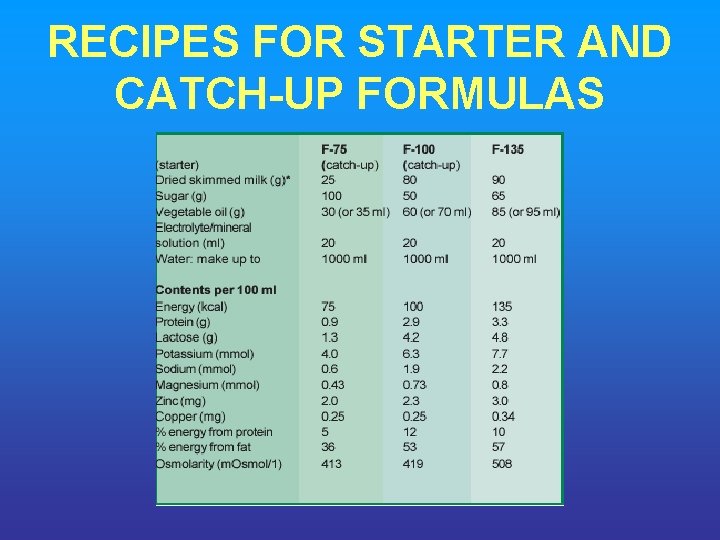
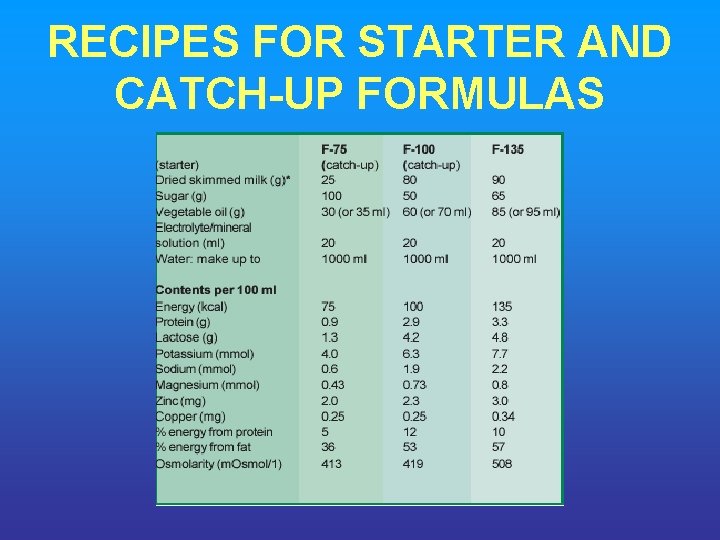
RECIPES FOR STARTER AND CATCH UP FORMULAS
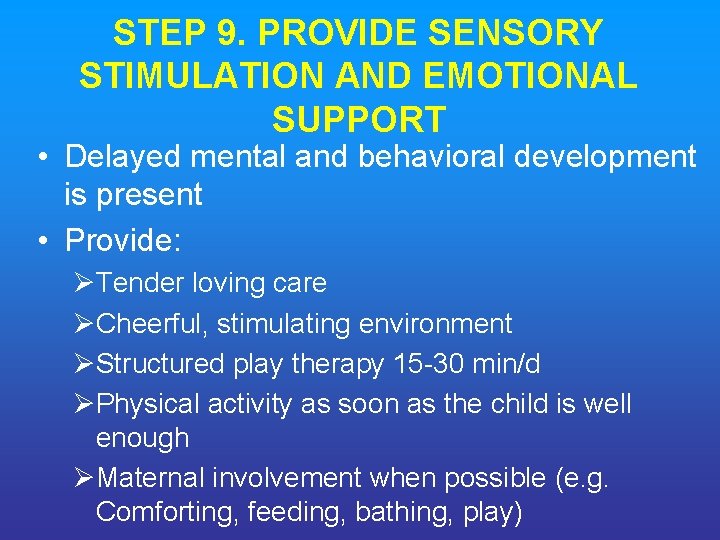
STEP 9. PROVIDE SENSORY STIMULATION AND EMOTIONAL SUPPORT • Delayed mental and behavioral development is present • Provide: ØTender loving care ØCheerful, stimulating environment ØStructured play therapy 15 -30 min/d ØPhysical activity as soon as the child is well enough ØMaternal involvement when possible (e. g. Comforting, feeding, bathing, play)
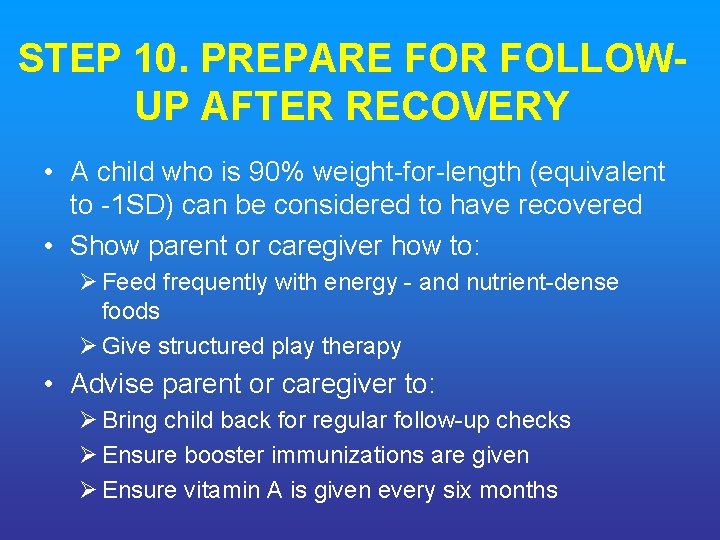
STEP 10. PREPARE FOR FOLLOW UP AFTER RECOVERY • A child who is 90% weight-for-length (equivalent to -1 SD) can be considered to have recovered • Show parent or caregiver how to: Ø Feed frequently with energy - and nutrient-dense foods Ø Give structured play therapy • Advise parent or caregiver to: Ø Bring child back for regular follow-up checks Ø Ensure booster immunizations are given Ø Ensure vitamin A is given every six months

EMERGENCY TREATMENT OF SHOCK AND SEVERE ANEMIA
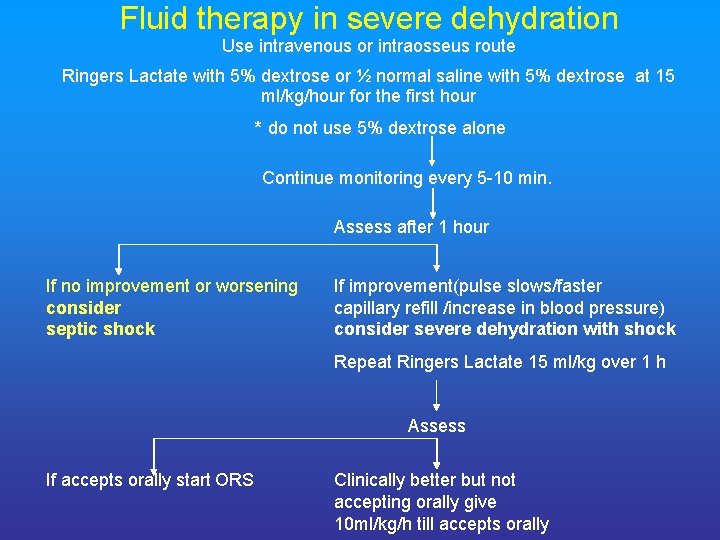
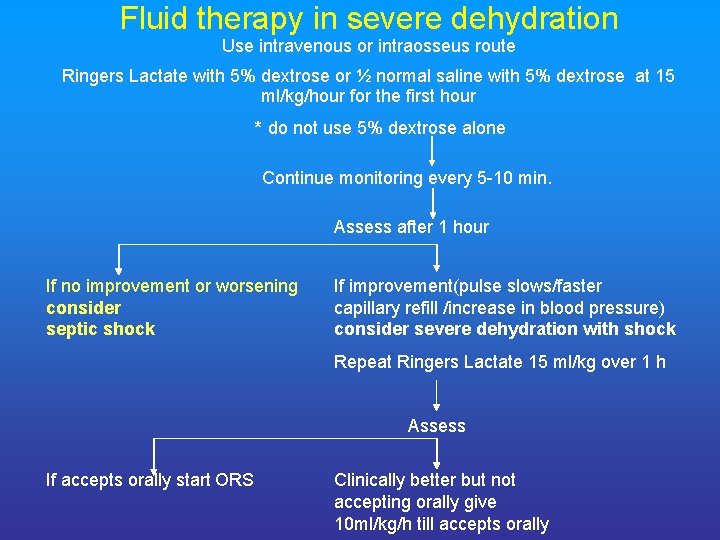
Fluid therapy in severe dehydration Use intravenous or intraosseus route Ringers Lactate with 5% dextrose or ½ normal saline with 5% dextrose at 15 ml/kg/hour for the first hour * do not use 5% dextrose alone Continue monitoring every 5 -10 min. Assess after 1 hour If no improvement or worsening consider septic shock If improvement(pulse slows/faster capillary refill /increase in blood pressure) consider severe dehydration with shock Repeat Ringers Lactate 15 ml/kg over 1 h Assess If accepts orally start ORS Clinically better but not accepting orally give 10 ml/kg/h till accepts orally
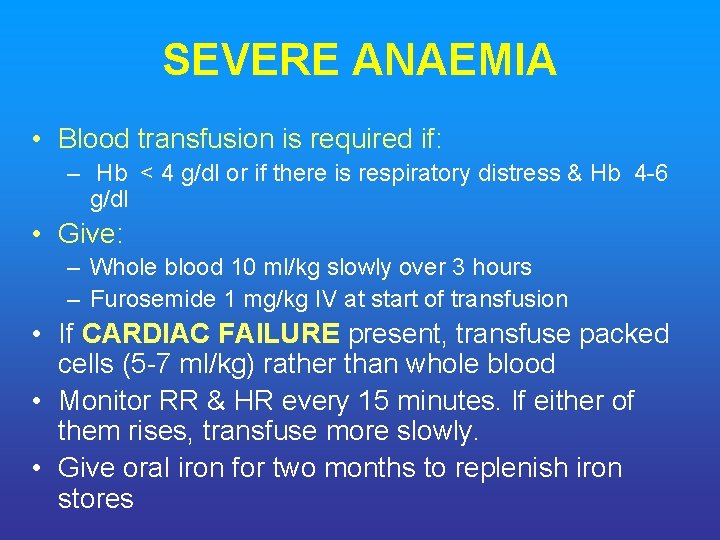
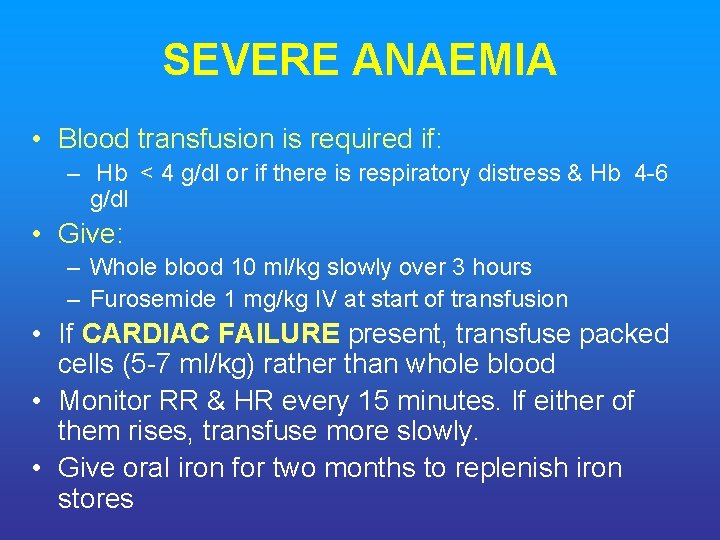
SEVERE ANAEMIA • Blood transfusion is required if: – Hb < 4 g/dl or if there is respiratory distress & Hb 4 -6 g/dl • Give: – Whole blood 10 ml/kg slowly over 3 hours – Furosemide 1 mg/kg IV at start of transfusion • If CARDIAC FAILURE present, transfuse packed cells (5 -7 ml/kg) rather than whole blood • Monitor RR & HR every 15 minutes. If either of them rises, transfuse more slowly. • Give oral iron for two months to replenish iron stores

TREATMENT OF ASSOCIATED CONDITIONS
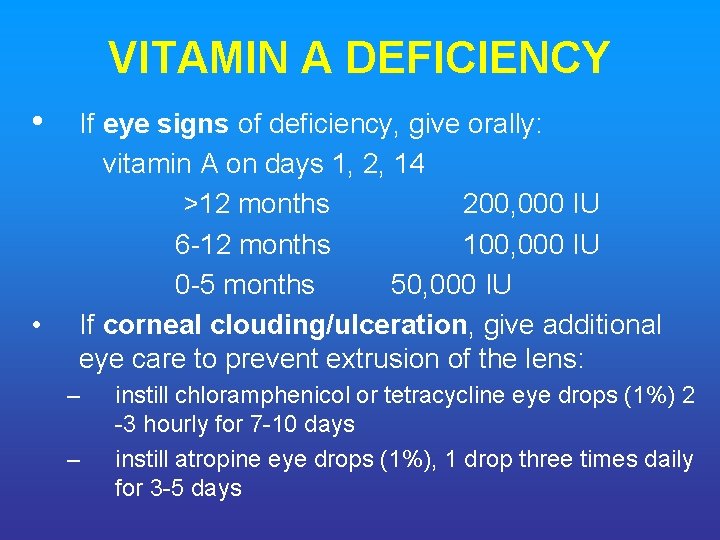
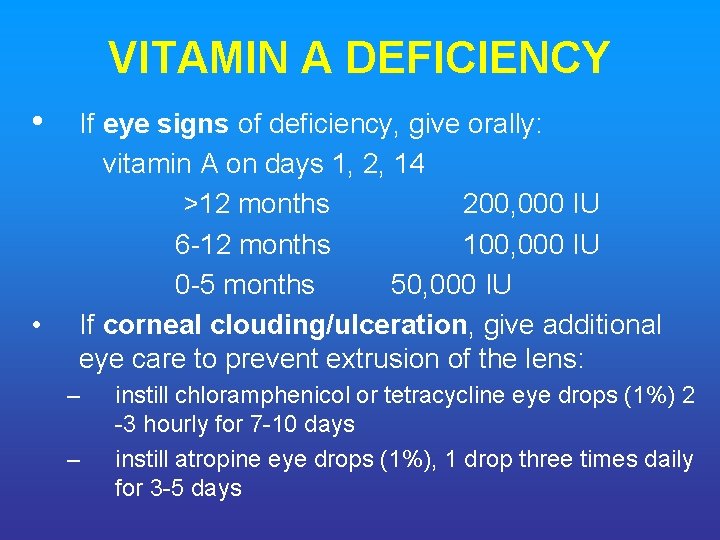
VITAMIN A DEFICIENCY • • If eye signs of deficiency, give orally: vitamin A on days 1, 2, 14 >12 months 200, 000 IU 6 -12 months 100, 000 IU 0 -5 months 50, 000 IU If corneal clouding/ulceration, give additional eye care to prevent extrusion of the lens: – – instill chloramphenicol or tetracycline eye drops (1%) 2 -3 hourly for 7 -10 days instill atropine eye drops (1%), 1 drop three times daily for 3 -5 days
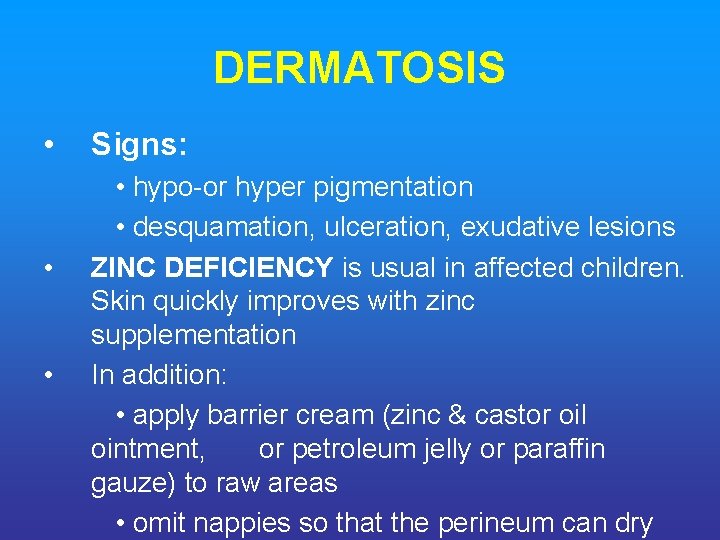
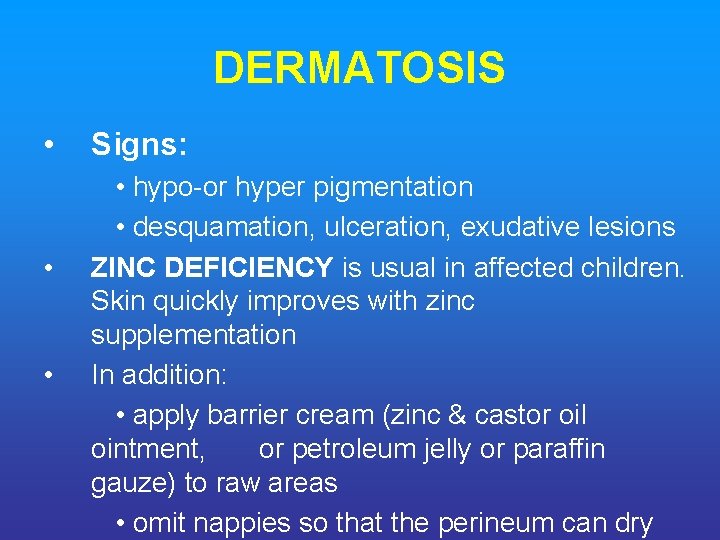
DERMATOSIS • • • Signs: • hypo-or hyper pigmentation • desquamation, ulceration, exudative lesions ZINC DEFICIENCY is usual in affected children. Skin quickly improves with zinc supplementation In addition: • apply barrier cream (zinc & castor oil ointment, or petroleum jelly or paraffin gauze) to raw areas • omit nappies so that the perineum can dry
CONTINUING DIARRHEA • Common feature but it should subside during the first week of treatment with cautious feeding. In the rehabilitation phase, loose, poorly formed stools are no cause for concern provided weight gain is satisfactory. • Mucosal damage & giardiasis – Stool microscopy – Give: metronidazole (7. 5 mg/kg 8 -hourly for 7 days)
CONTINUING DIARRHEA – Contd. . • Lactose intolerance. – Only rarely due to lactose intolerance. – Treat only if continuing diarrhea is preventing general improvement – Starter F-75 is a low-lactose feed. In exceptional cases: • substitute milk feeds with yogurt or lactose-free infant formula • reintroduce milk feeds gradually in the rehabilitation phase
OSMOTIC DIARRHEA • Suspected if diarrhea worsens substantially with hyperosmolar starter F 75 and • Ceases when the sugar content is reduced and osmolarity is <300 m. Osmol/l. • In these cases: use isotonic F-75 or low osmolar cereal-based F-75. Introduce F 100 gradually PARASITIC WORMS
TUBERCULOSIS (TB) If strongly suspected (contacts with adult TB patient, poor growth, despite good intake, chronic cough, chest infection not responding to antibiotics): – Mantoux test (false negatives are frequent) – Chest X-ray if possible – If test is positive or strong suspicion of TB, treat according to national TB guidelines

FAILURE TO RESPOND TO TREATMENT
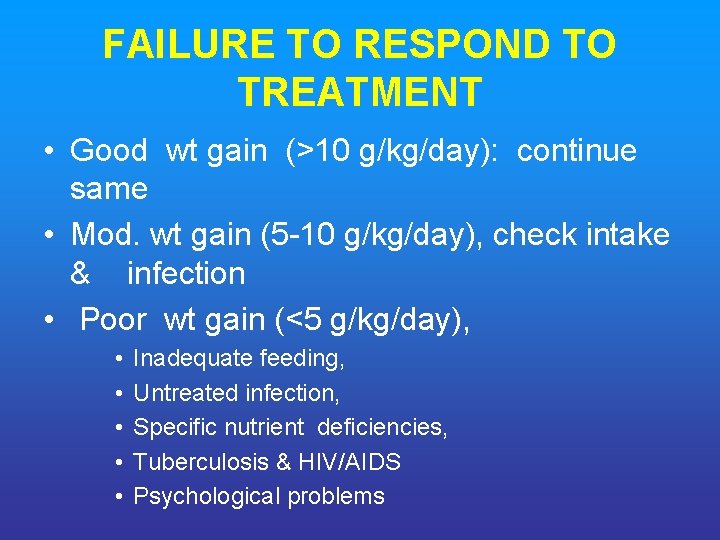
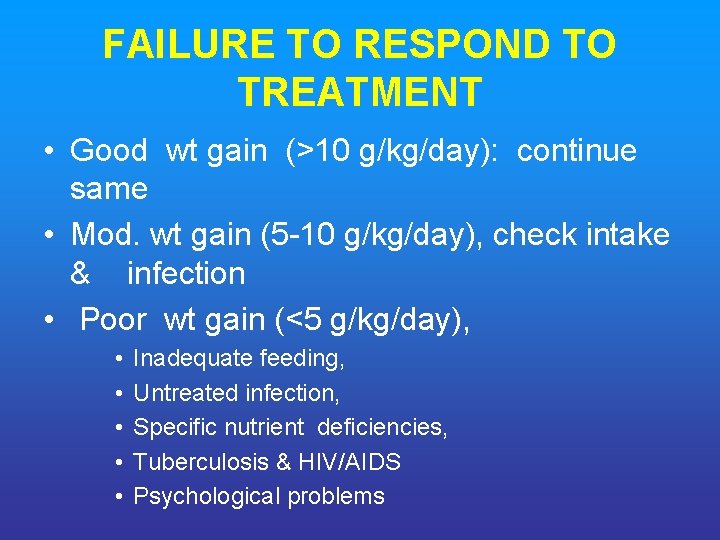
FAILURE TO RESPOND TO TREATMENT • Good wt gain (>10 g/kg/day): continue same • Mod. wt gain (5 -10 g/kg/day), check intake & infection • Poor wt gain (<5 g/kg/day), • • • Inadequate feeding, Untreated infection, Specific nutrient deficiencies, Tuberculosis & HIV/AIDS Psychological problems
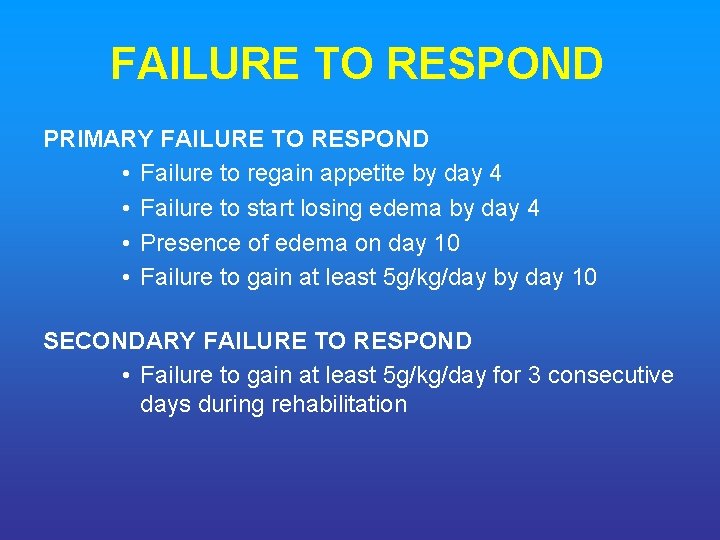
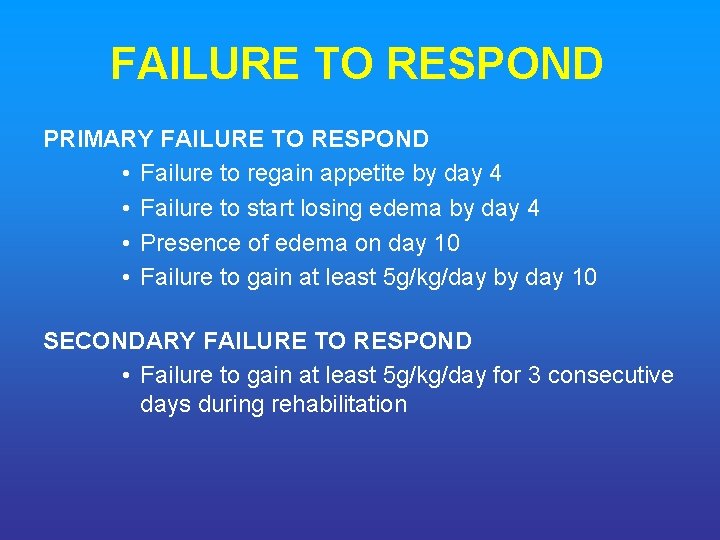
FAILURE TO RESPOND PRIMARY FAILURE TO RESPOND • Failure to regain appetite by day 4 • Failure to start losing edema by day 4 • Presence of edema on day 10 • Failure to gain at least 5 g/kg/day by day 10 SECONDARY FAILURE TO RESPOND • Failure to gain at least 5 g/kg/day for 3 consecutive days during rehabilitation
DISCHARGE BEFORE RECOVERY IS COMPLETE
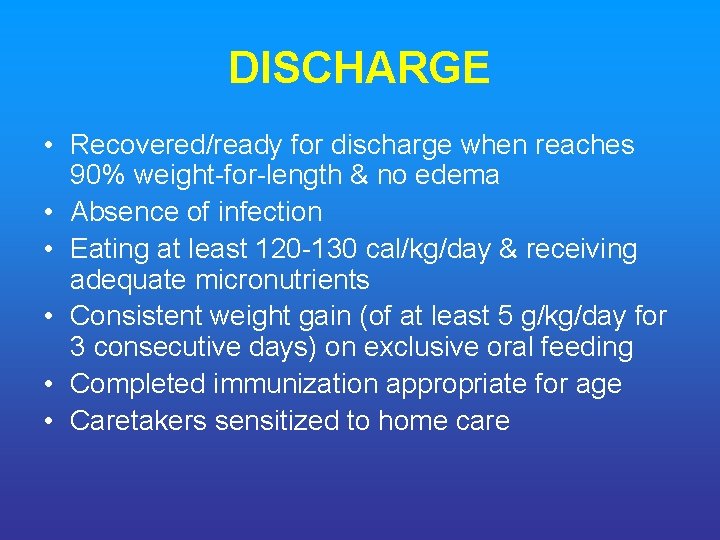
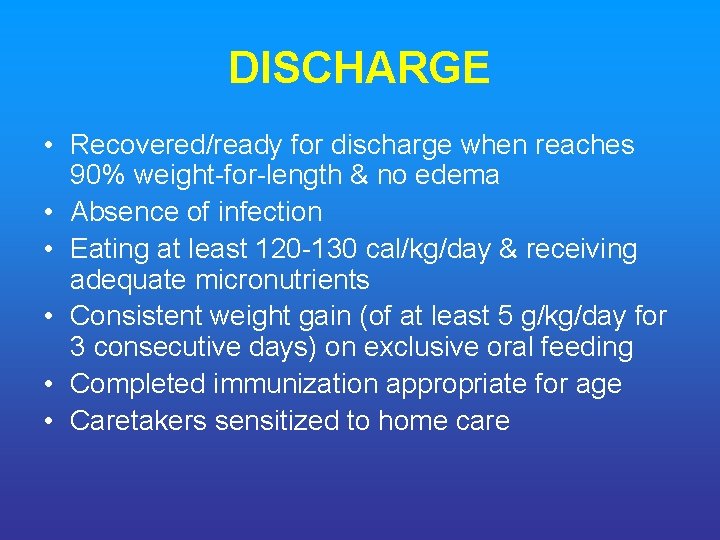
DISCHARGE • Recovered/ready for discharge when reaches 90% weight-for-length & no edema • Absence of infection • Eating at least 120 -130 cal/kg/day & receiving adequate micronutrients • Consistent weight gain (of at least 5 g/kg/day for 3 consecutive days) on exclusive oral feeding • Completed immunization appropriate for age • Caretakers sensitized to home care
CHILDREN DISCHARGED EARLY: WHAT TO DO Recovery complete if 90% W/L; But can be discharge early for domiciliary if • The child: > 1 yr; good appetite & wt gain; no edema, antibiotic treat completed. Vit, K, min. given 2 wks • The mother: available at home, motivated & trained to look after; have resources; reside near hospital. • Local Health Worker: Can provide support; trained;

CHILDREN DISCHARGED EARLY: WHAT TO DO Monitoring Feeding at Home Essential: • • • Feed frequently at least 5 times a day Modify home food to suit F-100 High energy snacks between meals Assistance to complete each meal Give electrolyte/ mineral solutions Breastfeeding should continue

Thank you
 Definition of protein-energy malnutrition
Definition of protein-energy malnutrition Assessment of pem
Assessment of pem Nursing management of anemia
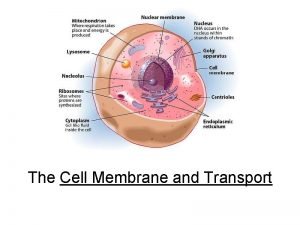
Nursing management of anemia Channel vs carrier proteins
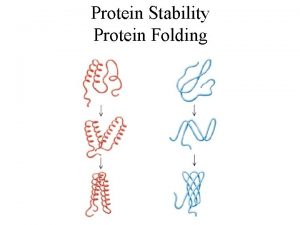
Channel vs carrier proteins Protein-protein docking
Protein-protein docking Appetite stimulant
Appetite stimulant Types of malnutrition
Types of malnutrition Malnutrition definition
Malnutrition definition Iatrogenic malnutrition
Iatrogenic malnutrition Energy energy transfer and general energy analysis
Energy energy transfer and general energy analysis Energy energy transfer and general energy analysis
Energy energy transfer and general energy analysis Endosperm of wheat
Endosperm of wheat Energy input and output nutrition
Energy input and output nutrition Unicef conceptual framework for malnutrition explained
Unicef conceptual framework for malnutrition explained Hypothemi
Hypothemi Moderate acute malnutrition
Moderate acute malnutrition What are the 4 types of malnutrition
What are the 4 types of malnutrition Holliday segar method
Holliday segar method Z score for malnutrition
Z score for malnutrition Marasmus disease
Marasmus disease Malnutrition
Malnutrition Anthropometric measurements ppt
Anthropometric measurements ppt Icd 10 ch
Icd 10 ch What is the difference between kwashiorkor and marasmus
What is the difference between kwashiorkor and marasmus Conceptual framework for malnutrition
Conceptual framework for malnutrition Malnutrition case study
Malnutrition case study Baggy pants sign in malnutrition
Baggy pants sign in malnutrition Aspen criteria for malnutrition
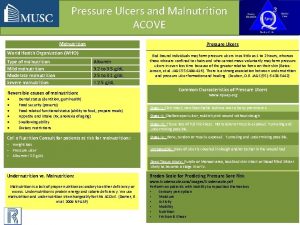
Aspen criteria for malnutrition Malnutrition
Malnutrition Nutritional needs in fundamentals of nursing
Nutritional needs in fundamentals of nursing Dehydration in malnutrition
Dehydration in malnutrition Chief complaint of malnutrition
Chief complaint of malnutrition Kwashiorkor vs marasmus
Kwashiorkor vs marasmus Malnutrition pics
Malnutrition pics Malnutrition
Malnutrition Conclusion of nutritional problems in india
Conclusion of nutritional problems in india Malnutrition
Malnutrition Malnutrition quality improvement initiative
Malnutrition quality improvement initiative Conclusion of malnutrition
Conclusion of malnutrition Malnutrition conclusion
Malnutrition conclusion Prevention of malnutrition
Prevention of malnutrition Malnutrition flowchart
Malnutrition flowchart Measures to control malnutrition
Measures to control malnutrition Malnutrition physical exam
Malnutrition physical exam Nutrition survey definition
Nutrition survey definition Nutrition monitoring definition
Nutrition monitoring definition Introduction to sports nutrition
Introduction to sports nutrition Define nutritional epidemiology
Define nutritional epidemiology Food and nutrition security definition
Food and nutrition security definition What is nutritional health
What is nutritional health Culinary nutritional arts
Culinary nutritional arts Microbial nutrition definition
Microbial nutrition definition Nutrition emergency definition
Nutrition emergency definition Metabolism nutrition definition
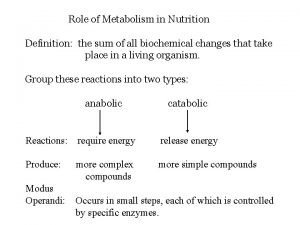
Metabolism nutrition definition What is nutrition quackery
What is nutrition quackery Protein denaturation definition
Protein denaturation definition Protein function
Protein function Definition of protein
Definition of protein Wikipedia
Wikipedia Novel protein definition
Novel protein definition Properties of liquid
Properties of liquid State to state regionalism
State to state regionalism Synchronous counter design
Synchronous counter design Software implementation of state graph
Software implementation of state graph T state vs r state
T state vs r state Subshell orbital
Subshell orbital Difference between hemoglobin and myoglobin
Difference between hemoglobin and myoglobin Absorptive state and postabsorptive state
Absorptive state and postabsorptive state Glycolysis gluconeogenesis glycogenolysis glycogenesis
Glycolysis gluconeogenesis glycogenolysis glycogenesis