TREATMENT MANAGEMENT OF SEVERE ACUTE PROTEINENERGY MALNUTRITION IN


- Slides: 27
TREATMENT & MANAGEMENT OF SEVERE ACUTE (PROTEIN-ENERGY) MALNUTRITION IN CHILDREN Global Health Fellowship Nutrition Module
Severe Malnutrition Medical & social disorder End result of chronic nutritional & emotional deprivation Management requires medical & social interventions
Underlying causes of poor diet & excess disease (UNICEF) Insufficient access to food Inadequate maternal & child care Poor environment Inadequate or lack of access to health services
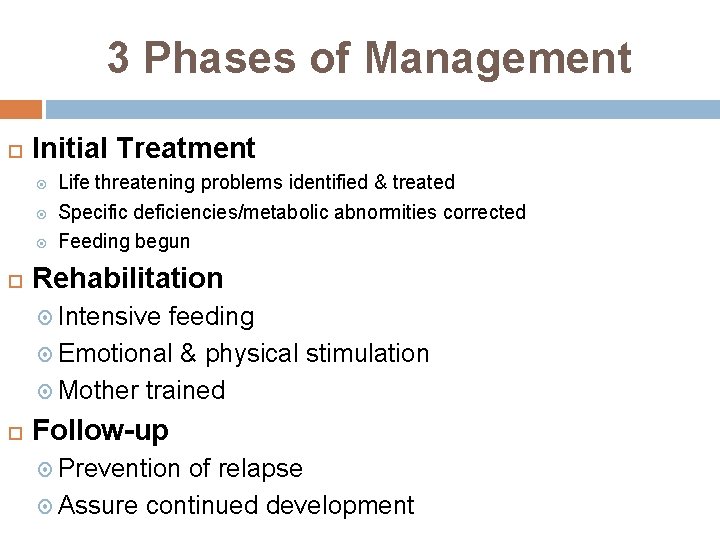
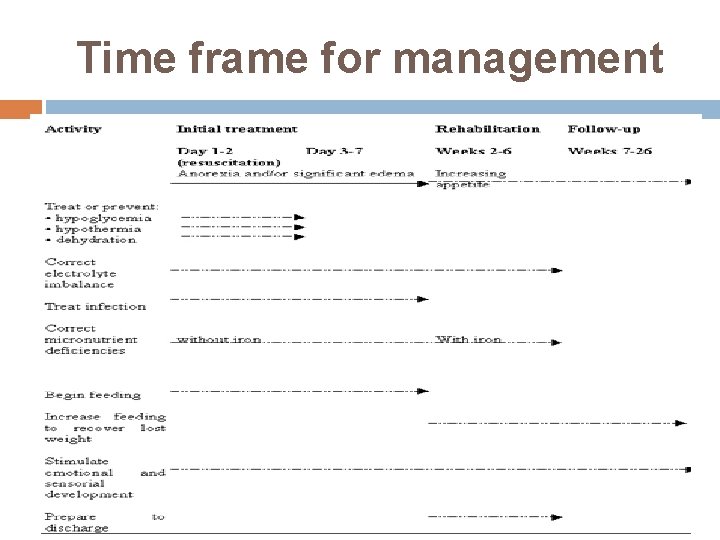
3 Phases of Management Initial Treatment Life threatening problems identified & treated Specific deficiencies/metabolic abnormities corrected Feeding begun Rehabilitation Intensive feeding Emotional & physical stimulation Mother trained Follow-up Prevention of relapse Assure continued development

Treatment Facilities Initial treatment & beginning of rehabilitation SAM with complication (anorexia, infection, dehydration) Residential care in special nutrition unit SAM w/out complications, s/p inpt has appetite. gaining weight, stable Nutritional rehabilitation center: day hospital, 1 ary health center CTC
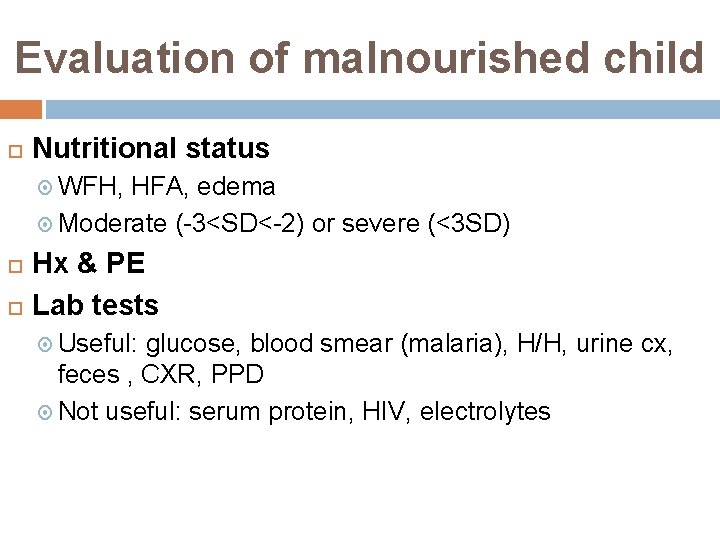
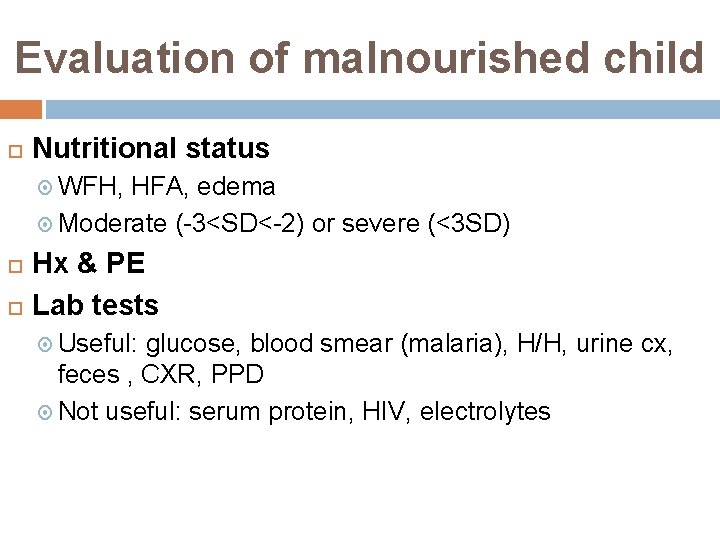
Evaluation of malnourished child Nutritional status WFH, HFA, edema Moderate (-3<SD<-2) or severe (<3 SD) Hx & PE Lab tests Useful: glucose, blood smear (malaria), H/H, urine cx, feces , CXR, PPD Not useful: serum protein, HIV, electrolytes
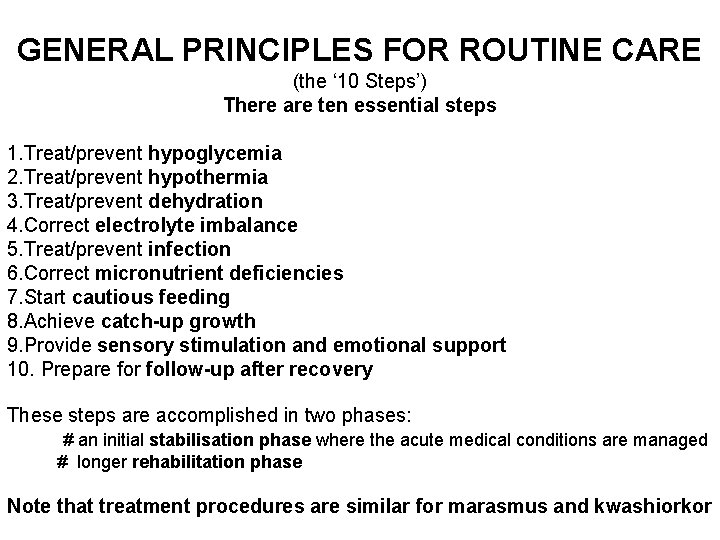
GENERAL PRINCIPLES FOR ROUTINE CARE (the ‘ 10 Steps’) There are ten essential steps 1. Treat/prevent hypoglycemia 2. Treat/prevent hypothermia 3. Treat/prevent dehydration 4. Correct electrolyte imbalance 5. Treat/prevent infection 6. Correct micronutrient deficiencies 7. Start cautious feeding 8. Achieve catch-up growth 9. Provide sensory stimulation and emotional support 10. Prepare for follow-up after recovery These steps are accomplished in two phases: # an initial stabilisation phase where the acute medical conditions are managed # longer rehabilitation phase Note that treatment procedures are similar for marasmus and kwashiorkor
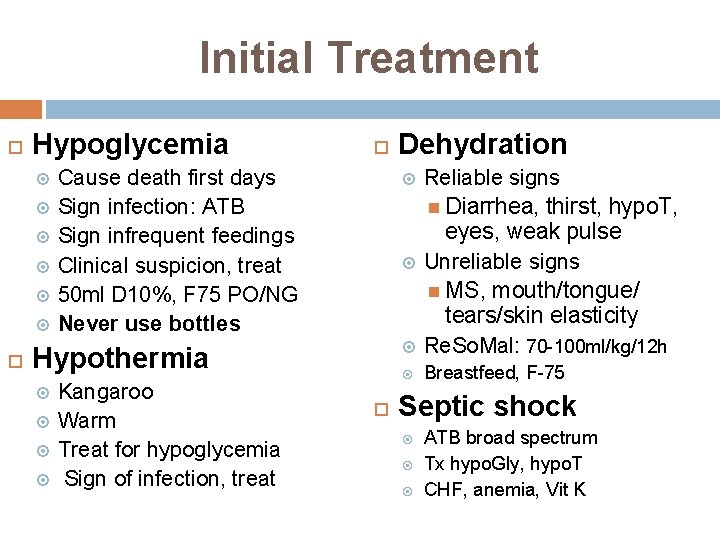
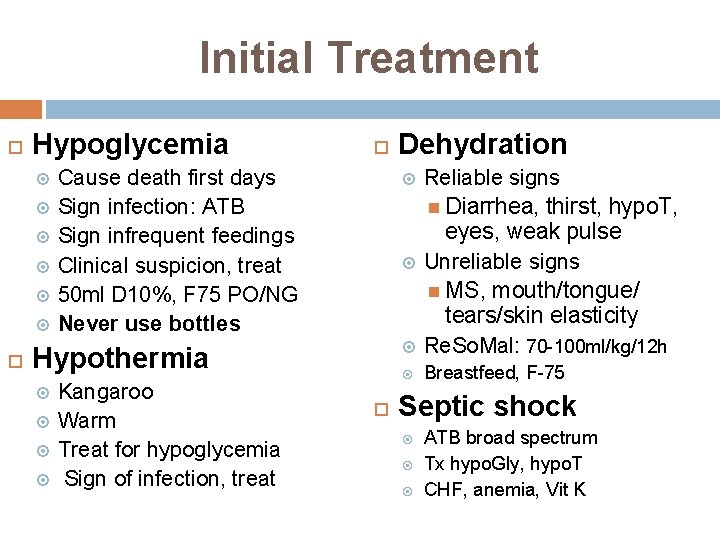
Initial Treatment Hypoglycemia Cause death first days Sign infection: ATB Sign infrequent feedings Clinical suspicion, treat 50 ml D 10%, F 75 PO/NG Never use bottles Kangaroo Warm Treat for hypoglycemia Sign of infection, treat Reliable signs Diarrhea, thirst, hypo. T, eyes, weak pulse Unreliable signs MS, mouth/tongue/ tears/skin elasticity Re. So. Mal: 70 -100 ml/kg/12 h Breastfeed, F-75 Hypothermia Dehydration Septic shock ATB broad spectrum Tx hypo. Gly, hypo. T CHF, anemia, Vit K
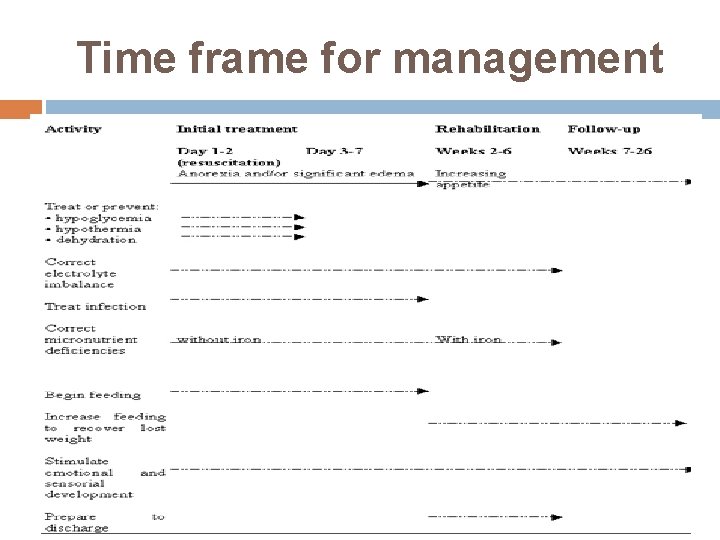
Time frame for management
Re. So. Mal Severely malnourished children K deficient, high Na levels Mg, Zn, copper deficiency Commercially available Dilute 1 packet of standard WHO ORS in 2 l water + 50 g of sucrose (25 g/l) + 40 ml (20 ml/l) mineral mix solution 5 ml/kg PO/NG q 30 min Cont till thirst & urine
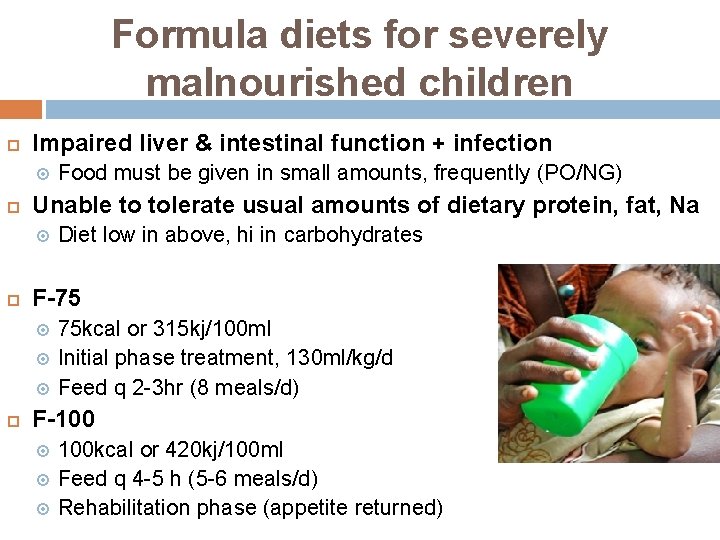
Formula diets for severely malnourished children Impaired liver & intestinal function + infection Unable to tolerate usual amounts of dietary protein, fat, Na Diet low in above, hi in carbohydrates F-75 Food must be given in small amounts, frequently (PO/NG) 75 kcal or 315 kj/100 ml Initial phase treatment, 130 ml/kg/d Feed q 2 -3 hr (8 meals/d) F-100 100 kcal or 420 kj/100 ml Feed q 4 -5 h (5 -6 meals/d) Rehabilitation phase (appetite returned)
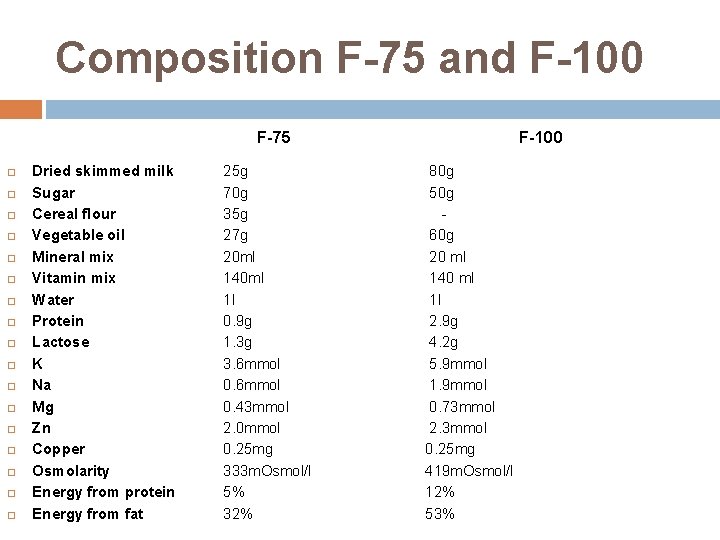
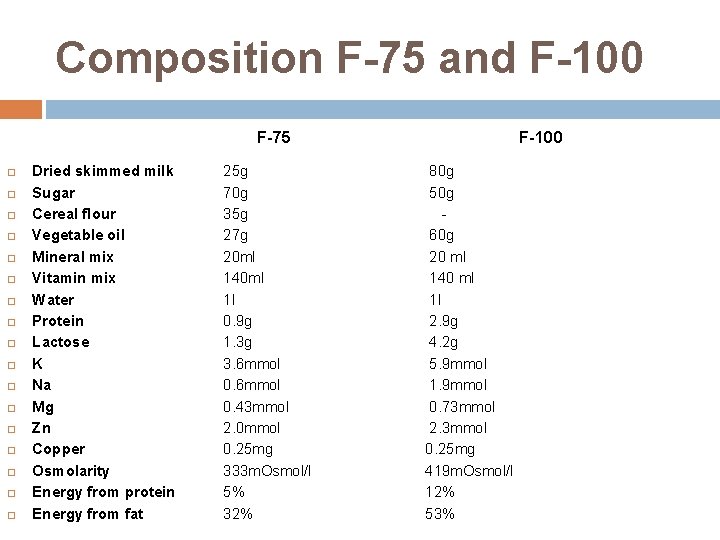
Composition F-75 and F-100 F-75 Dried skimmed milk Sugar Cereal flour Vegetable oil Mineral mix Vitamin mix Water Protein Lactose K Na Mg Zn Copper Osmolarity Energy from protein Energy from fat 25 g 70 g 35 g 27 g 20 ml 140 ml 1 l 0. 9 g 1. 3 g 3. 6 mmol 0. 43 mmol 2. 0 mmol 0. 25 mg 333 m. Osmol/l 5% 32% F-100 80 g 50 g 60 g 20 ml 140 ml 1 l 2. 9 g 4. 2 g 5. 9 mmol 1. 9 mmol 0. 73 mmol 2. 3 mmol 0. 25 mg 419 m. Osmol/l 12% 53%
Continue Breastfeeding
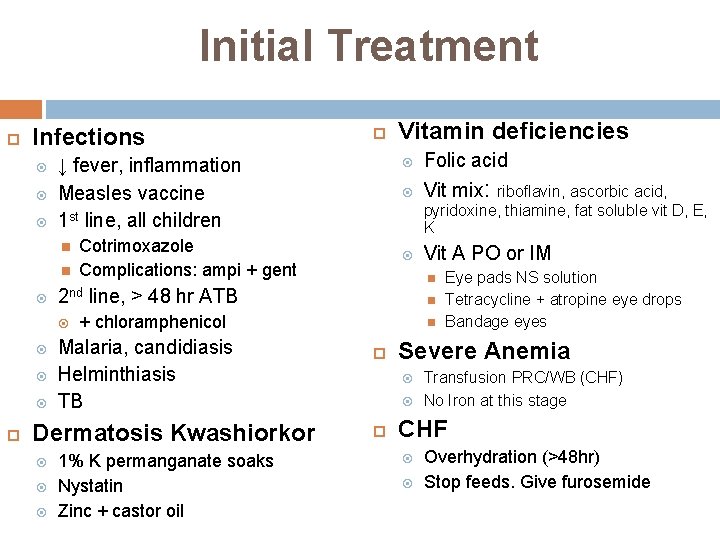
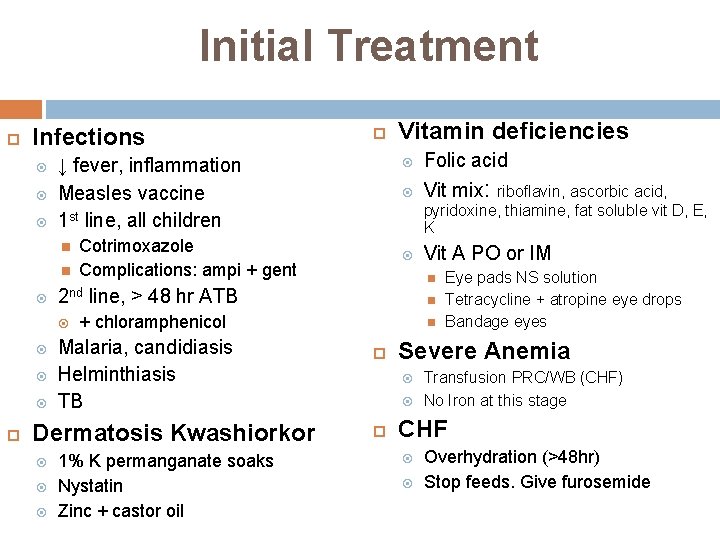
Initial Treatment Infections ↓ fever, inflammation Measles vaccine 1 st line, all children Cotrimoxazole Complications: ampi + gent Folic acid Vit mix: Vit A PO or IM Malaria, candidiasis Helminthiasis TB 1% K permanganate soaks Nystatin Zinc + castor oil riboflavin, ascorbic acid, pyridoxine, thiamine, fat soluble vit D, E, K + chloramphenicol Dermatosis Kwashiorkor Vitamin deficiencies 2 nd line, > 48 hr ATB Severe Anemia Eye pads NS solution Tetracycline + atropine eye drops Bandage eyes Transfusion PRC/WB (CHF) No Iron at this stage CHF Overhydration (>48 hr) Stop feeds. Give furosemide

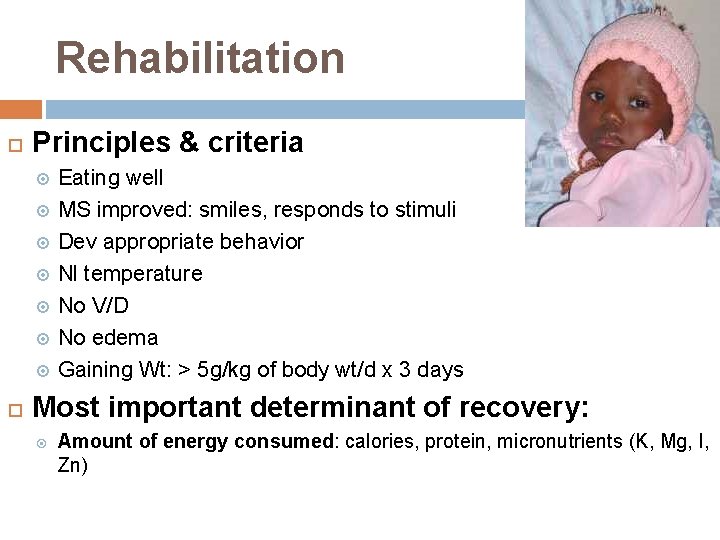
Rehabilitation Principles & criteria Eating well MS improved: smiles, responds to stimuli Dev appropriate behavior Nl temperature No V/D No edema Gaining Wt: > 5 g/kg of body wt/d x 3 days Most important determinant of recovery: Amount of energy consumed: calories, protein, micronutrients (K, Mg, I, Zn)
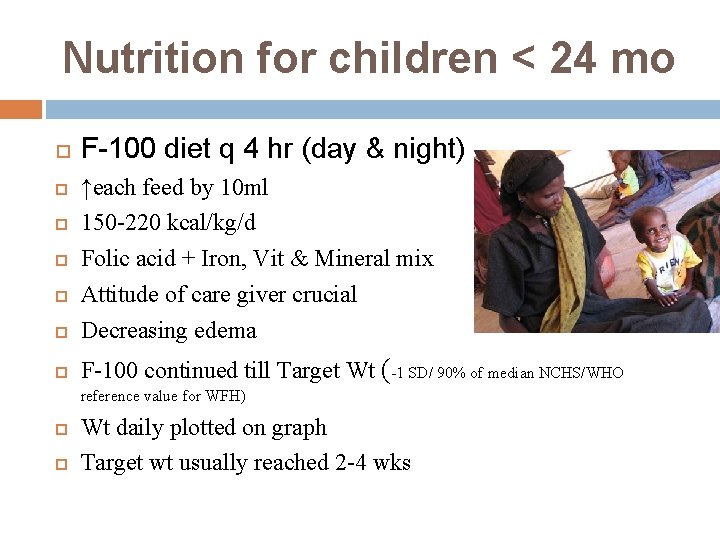
Nutrition for children < 24 mo F-100 diet q 4 hr (day & night) ↑each feed by 10 ml 150 -220 kcal/kg/d Folic acid + Iron, Vit & Mineral mix Attitude of care giver crucial Decreasing edema F-100 continued till Target Wt (-1 SD/ 90% of median NCHS/WHO reference value for WFH) Wt daily plotted on graph Target wt usually reached 2 -4 wks
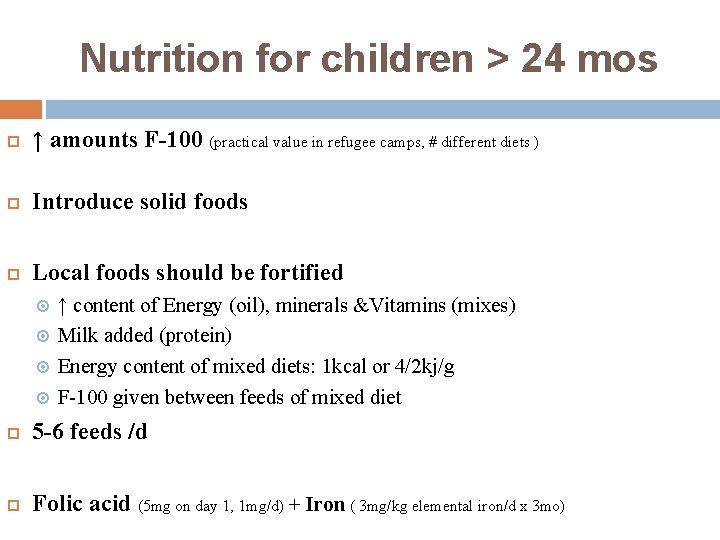
Nutrition for children > 24 mos ↑ amounts F-100 (practical value in refugee camps, # different diets ) Introduce solid foods Local foods should be fortified ↑ content of Energy (oil), minerals &Vitamins (mixes) Milk added (protein) Energy content of mixed diets: 1 kcal or 4/2 kj/g F-100 given between feeds of mixed diet 5 -6 feeds /d Folic acid (5 mg on day 1, 1 mg/d) + Iron ( 3 mg/kg elemental iron/d x 3 mo)
Emotional & physical stimulation 1 ary/2 ary prevention DD, MR, ED Start during rehabilitation Avoid sensory deprivation Maternal presence Environment Play activities, peer interactions Physical activities
Rehabilitation Parental teaching Correct feeding/food preparation practices, Stimulation, play, hygiene Treatment diarrhea, infections When to seek medical care Preparation for D/C Reintegration into family & community Prevent malnutrition recurrence
Criteria for D/C Child Mother WFH reached -1 SD Eating appropriate amount of diet that mother can prepare at home Gaining wt at normal or ↑rate Vit/mineral deficiencies treated/corrected Infections treated Full immunizations Able & willing to care for child Knows proper food preparation Knows appropriate toys & play for child Knows home treatment fever, diarrhea, ARI Health worker Able to ensure F/U child & support for mother
Follow up Child usually remains stunted w/ DD Prevention of recurrence severe malnutrition Strategy for tracing children F/U: 1, 2, 4 weeks, then 3 & 6 mos, then 2 x/yr till age 3 yrs WFH no less than -1 SD Assess overall health, feeding, play Immunizations, treatments, vitamin/minerals Record progress
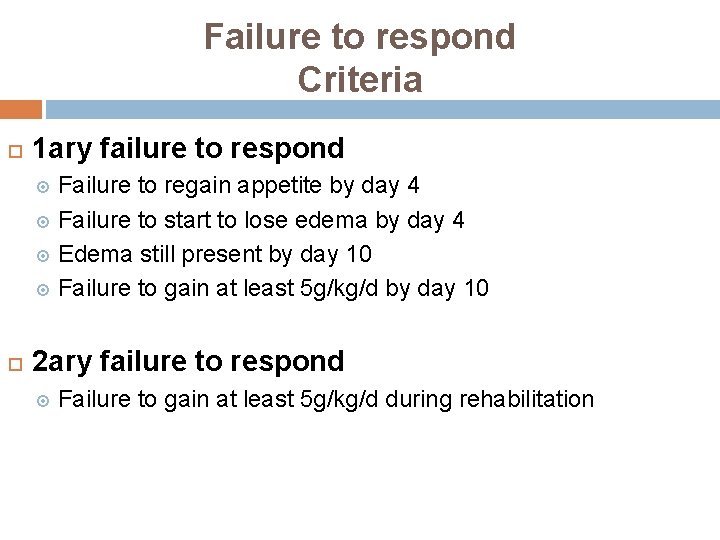
Failure to respond Criteria 1 ary failure to respond Failure to regain appetite by day 4 Failure to start to lose edema by day 4 Edema still present by day 10 Failure to gain at least 5 g/kg/d by day 10 2 ary failure to respond Failure to gain at least 5 g/kg/d during rehabilitation
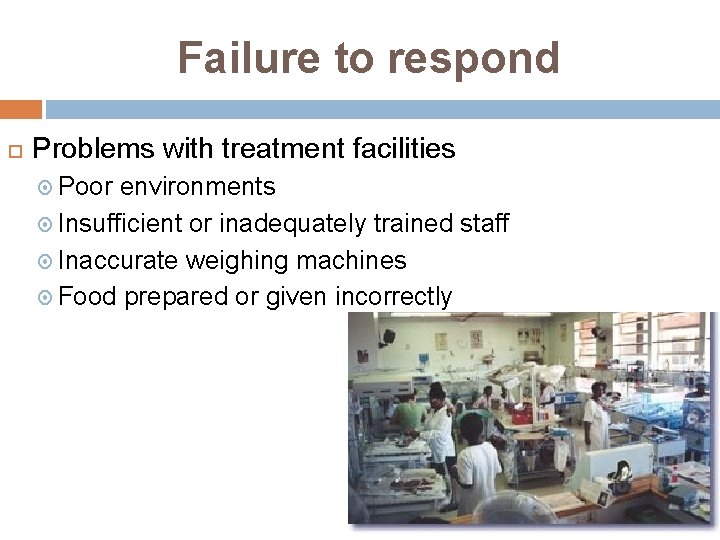
Failure to respond Problems with treatment facilities Poor environments Insufficient or inadequately trained staff Inaccurate weighing machines Food prepared or given incorrectly
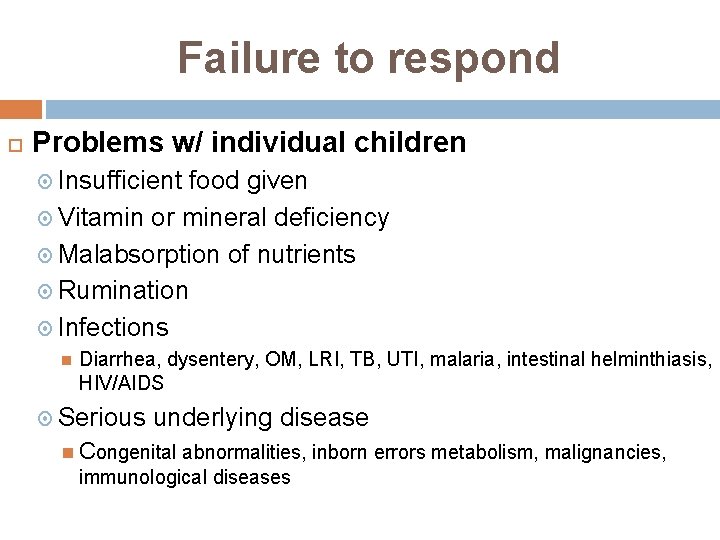
Failure to respond Problems w/ individual children Insufficient food given Vitamin or mineral deficiency Malabsorption of nutrients Rumination Infections Diarrhea, dysentery, OM, LRI, TB, UTI, malaria, intestinal helminthiasis, HIV/AIDS Serious underlying disease Congenital abnormalities, inborn errors metabolism, malignancies, immunological diseases
Fight Malnutrition
 Severe acute malnutrition case presentation
Severe acute malnutrition case presentation Moderate acute malnutrition
Moderate acute malnutrition Dr sofi
Dr sofi Severe asthma treatment
Severe asthma treatment Parietal pain
Parietal pain Hydropic gallbladder
Hydropic gallbladder Acute abdomen causes
Acute abdomen causes Gout treatment
Gout treatment Pancreatitis alcohol
Pancreatitis alcohol Nursing management of kwashiorkor
Nursing management of kwashiorkor Pancreatitis nursing diagnosis
Pancreatitis nursing diagnosis Conceptual framework of malnutrition
Conceptual framework of malnutrition Water law classification of malnutrition
Water law classification of malnutrition Wellcome classification
Wellcome classification Objectives for malnutrition
Objectives for malnutrition Holliday segar method
Holliday segar method Z score for malnutrition
Z score for malnutrition Appetite stimulant
Appetite stimulant Kwashiorkor and marasmus
Kwashiorkor and marasmus Malnutrition conclusion
Malnutrition conclusion Malnutrition definition
Malnutrition definition Z score for malnutrition
Z score for malnutrition Icd 10 hipotiroid
Icd 10 hipotiroid Iatrogenic malnutrition
Iatrogenic malnutrition Orbital fat pads malnutrition
Orbital fat pads malnutrition Conceptual framework of malnutrition
Conceptual framework of malnutrition Resomal
Resomal Aspen criteria for malnutrition
Aspen criteria for malnutrition