MANAGEMENT OF MALNUTRITION Severe Acute Malnutrition Weight for



- Slides: 24

MANAGEMENT OF MALNUTRITION
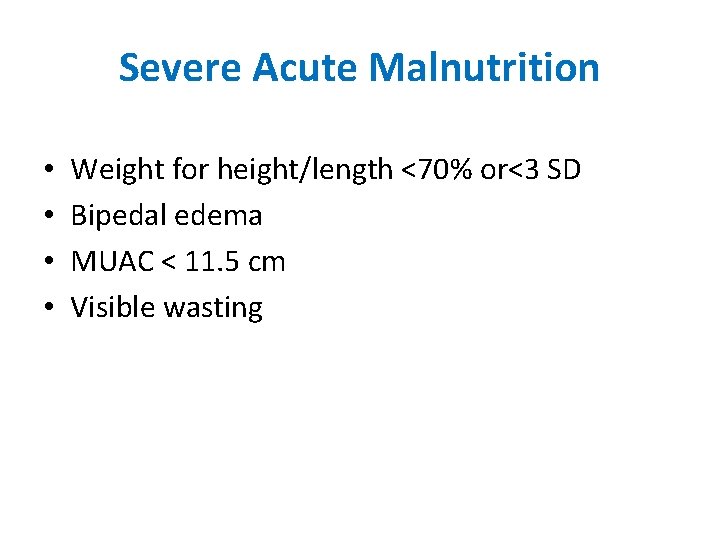
Severe Acute Malnutrition • • Weight for height/length <70% or<3 SD Bipedal edema MUAC < 11. 5 cm Visible wasting
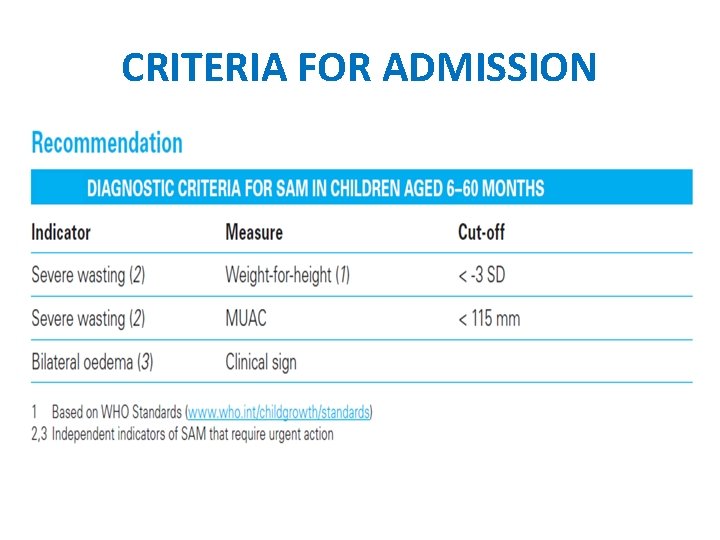
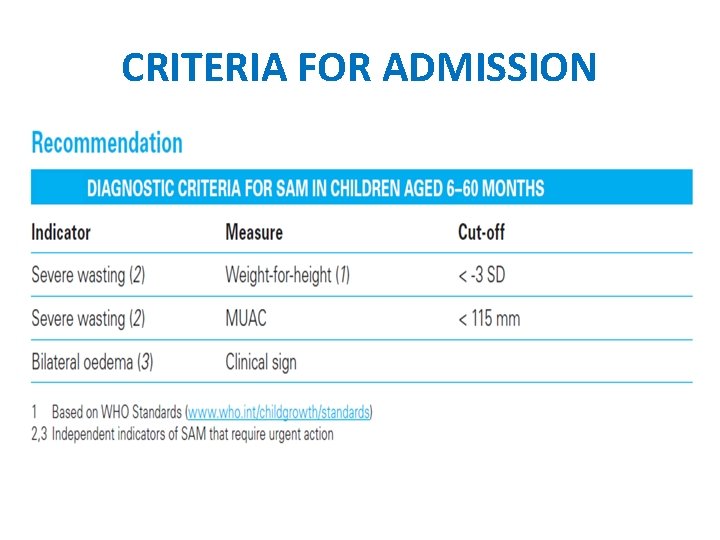
CRITERIA FOR ADMISSION

INITIAL ASSESSMENT • History • Examination
STEPS OF MANAGEMENT 1. Treat/prevent hypoglycemia 2. Treat/prevent hypothermia 3. Treat/prevent dehydration 4. Correct electrolyte imbalance 5. Treat/prevent infection
STEPS OF MANAGEMENT 6. Correct micronutrient deficiencies 7. Start cautious feeding 8. Achieve catch-up growth 9. Provide sensory stimulation and emotional support 10. Followup after recovery
HYPOGLYCEMIA • Blood glucose <54 mg% or 3 mmol/l • Symptomatic or asymptomatic • Hypoglycemia, hypothermia, infection occur as a triad • Treatment: – 10% dextrose orally/NG Tube/IV – Start feeds
HYPOTHERMIA • Rectal temp <35. 5 deg. C • Axillary temp <35 deg. C • Treatment: – Feeding – Covering – Rewarming – Antibiotics
DEHYDRATION • Assessment of severity difficult • Treatment: reduced osmolarity ORS • IVF for severe dehydration
DYSELECTROLYTEMIA • Excess of body sodium • Low serum potassium and magnesium • Treatment: – supplement potassium : 3 -4 meq/kg/day – Magsulf : 0. 3 ml/kg IM
INFECTIONS • Clinical signs may be subtle • Investigations to be done • Treatment: – broad spectrum antibiotics
MICRONUTRIENT DEFICIENCY • Upto twice the RDA • Do not give Iron till 1 week
INITIATE REFEEDING • Initiate feeding as soon as possible with feeds: – osmolality <350 mosm/l – Lactose not more than 2 -3 g/kg/d – Appropriate renal solute load
INITIATE REFEEDING • Initiate feeding as soon as possible with feeds – Adequate bioavailability of micronutrient – Initial percentage of calories from proteins of 5% – Adequate bioavailability of micronutrients – Low viscosity, easy to prepare and socially acceptable – Adequate storage, cooking and refrigeration
INITIATE REFEEDING • Start feeding early • Recommended energy intake : – 100 kcal/kg/d – Protein : 1 -1. 5 g/kg/d • Total fluid recommended: 130 ml/kg/d • Continue breast feeding ad libitum
TYPES OF DIETS • F 75 • F 100 • RUTF (Ready to Use Therapeutic Food ) • Home based food
CATCH UP GROWTH • Calorie intake increased to 150 -200 kcal/kg/d • Proteins: 4 -6 g/kg/d
SENSORY STIMULATION AND EMOTIONAL SUPPORT • Cheerful stimulating environment • Age appropriate structured play • Age appropriate physical activity • Tender loving care
PREPARE FOR FOLLOWUP • Primary failure: – Failure to regain appetite by d 4 – Failure to start losing edema by d 4 – Presence of edema on d 10 – Failure to gain at least 5 g/kg/d by d 10
PREPARE FOR FOLLOWUP • Secondary failure: – Failure to gain at-least 4 g/kg/d for 3 consecutive days during the rehabilitative phase
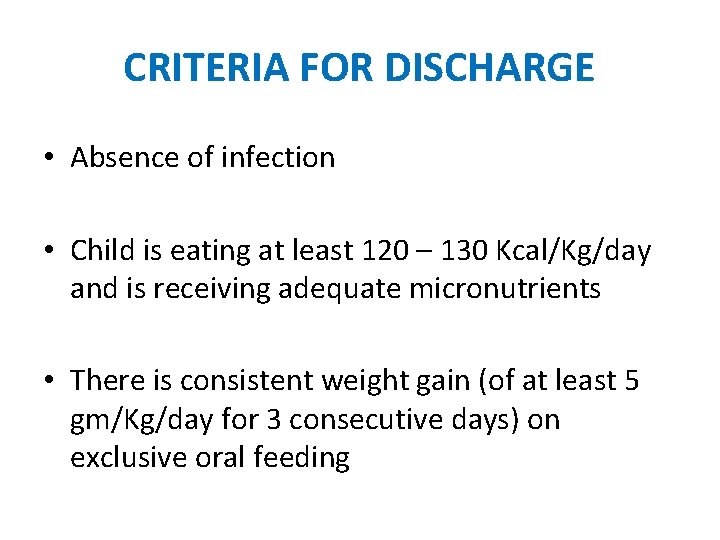
CRITERIA FOR DISCHARGE • Absence of infection • Child is eating at least 120 – 130 Kcal/Kg/day and is receiving adequate micronutrients • There is consistent weight gain (of at least 5 gm/Kg/day for 3 consecutive days) on exclusive oral feeding
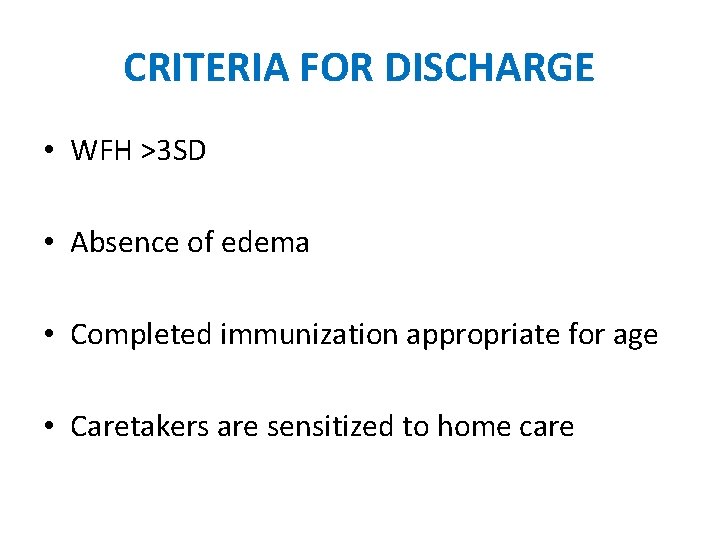
CRITERIA FOR DISCHARGE • WFH >3 SD • Absence of edema • Completed immunization appropriate for age • Caretakers are sensitized to home care

Thanks!
 Malnutrition case presentation
Malnutrition case presentation Moderate acute malnutrition
Moderate acute malnutrition Tolerable weight is a body weight
Tolerable weight is a body weight What is a “bulk-gaining industry”?
What is a “bulk-gaining industry”? Assessment of pem
Assessment of pem Pancreatitis nursing management
Pancreatitis nursing management Kontinuitetshantering i praktiken
Kontinuitetshantering i praktiken Typiska drag för en novell
Typiska drag för en novell Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Ekologiskt fotavtryck
Ekologiskt fotavtryck Varför kallas perioden 1918-1939 för mellankrigstiden
Varför kallas perioden 1918-1939 för mellankrigstiden En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Adressändring ideell förening
Adressändring ideell förening Tidbok för yrkesförare
Tidbok för yrkesförare Sura för anatom
Sura för anatom Förklara densitet för barn
Förklara densitet för barn Datorkunskap för nybörjare
Datorkunskap för nybörjare Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Att skriva debattartikel
Att skriva debattartikel För och nackdelar med firo
För och nackdelar med firo Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Lufttryck formel
Lufttryck formel Svenskt ramverk för digital samverkan
Svenskt ramverk för digital samverkan Jag har gått inunder stjärnor text
Jag har gått inunder stjärnor text