Malnutrition Disorders Introduction Malnutrition means more than feeling





- Slides: 31

Malnutrition Disorders
Introduction Malnutrition means more than feeling hungry or not having enough food to eat. It is a condition that develops when the body does not get the proper amount of protein, calories, vitamins and other nutrients it needs to maintain healthy tissues and organ function.
Prevalence of malnutrition Malnutrition remains of the worlds highest priority health issues not only because its effects are so widespread and long lasting, but also because it can be eradicated. More than 35% of all preschool age children in developing countries are under weight. The unicef report found that 146 million children under five years in the developing world are suffering from insufficient food intake, repeated infections diseases, muscle wasting and vitamin deficiencies.
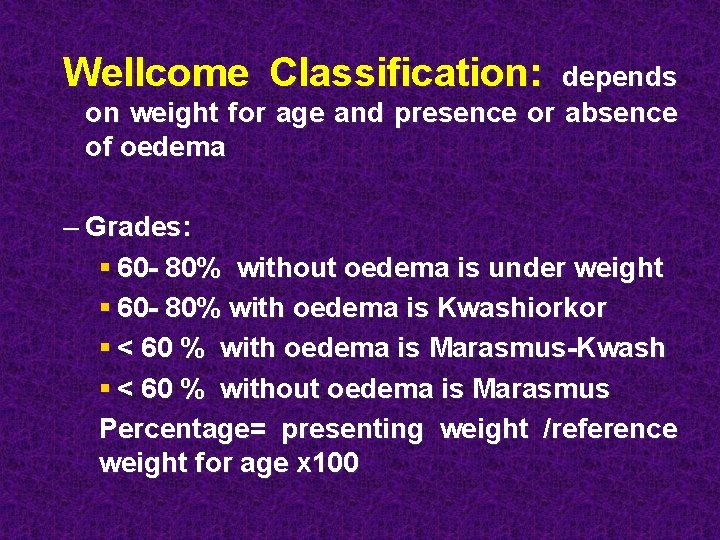
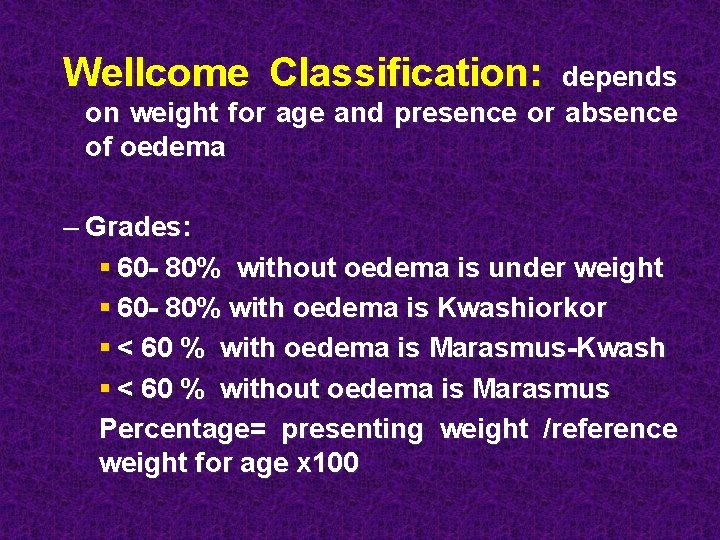
Wellcome Classification: depends on weight for age and presence or absence of oedema – Grades: § 60 - 80% without oedema is under weight § 60 - 80% with oedema is Kwashiorkor § < 60 % with oedema is Marasmus-Kwash § < 60 % without oedema is Marasmus Percentage= presenting weight /reference weight for age x 100
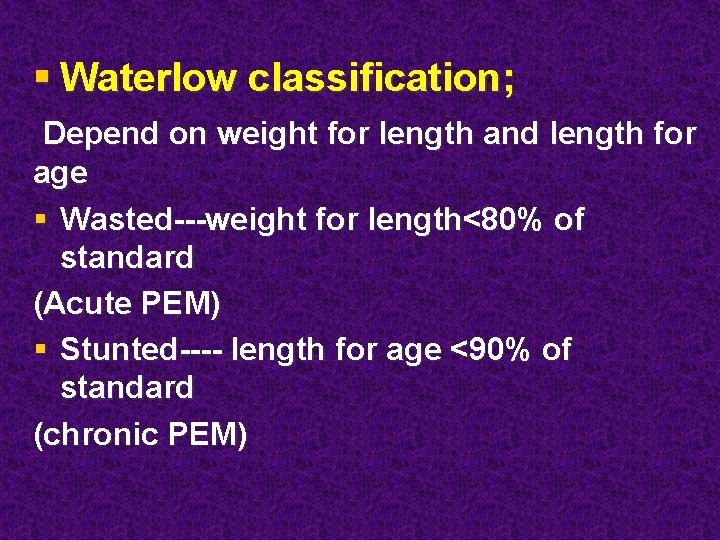
§ Waterlow classification; Depend on weight for length and length for age § Wasted---weight for length<80% of standard (Acute PEM) § Stunted---- length for age <90% of standard (chronic PEM)
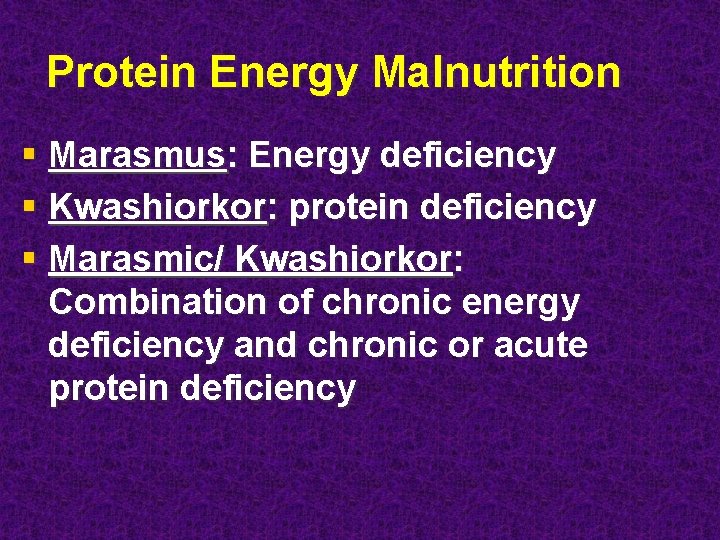
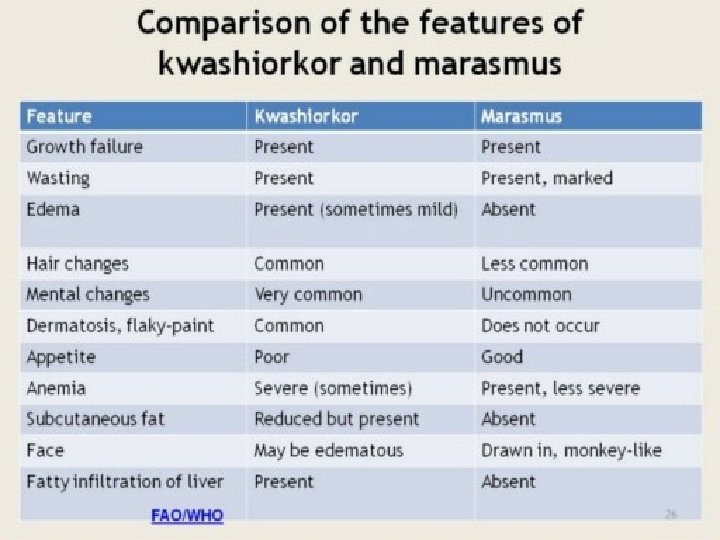
Protein Energy Malnutrition § Marasmus: Energy deficiency § Kwashiorkor: protein deficiency § Marasmic/ Kwashiorkor: Combination of chronic energy deficiency and chronic or acute protein deficiency
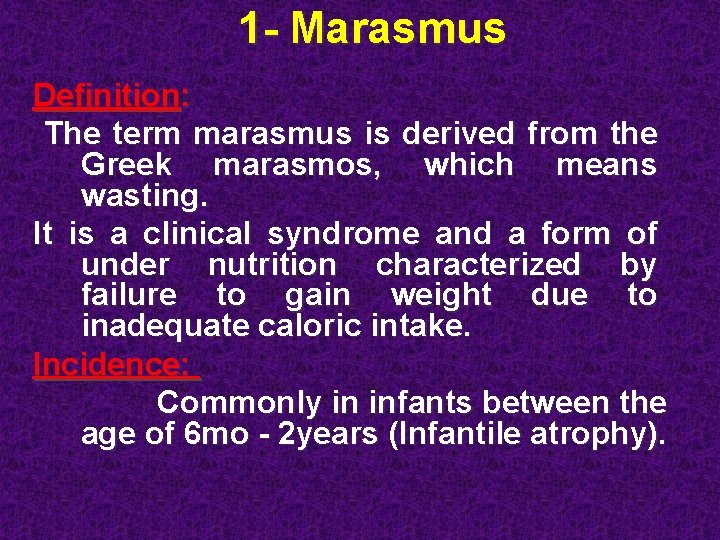
1 - Marasmus Definition: The term marasmus is derived from the Greek marasmos, which means wasting. It is a clinical syndrome and a form of under nutrition characterized by failure to gain weight due to inadequate caloric intake. Incidence: Commonly in infants between the age of 6 mo - 2 years (Infantile atrophy).
1 - Marasmus A- Nutritional marasmus § 1 - Early onset; early failure of breast feeding and the use of diluted formula leads to recurrent diarrhea § 2 - Late onset; Prolonged breast feeding with low energy coplimentary food § 3 - Poverty and ignorance of the mother are the usual precipitating factors§ 4 - Low socio economic status
1 - Marasmus B- Secondary marasmus 1 - Chronic repeated vomiting 2 - Infection : Acute or chronic as T. B, otitis media pyelonephritis 3 - Gastroenteritis: (acute or chronic ) 4 - Malabsorption 5 - Parasitic infestation Ascaris, ankylostoma , giardia 6 - Congenital anomalies as: Cardiac (P. D. A, V. S. D, F 4) , Renal (renal agenesis, obstructive uropathy) , G. I. T (pyloric stenosis ) 7 - Metabolic diseases. : Galactosemia, Fructose intolerance, RTA 8 - Mechanical ; cerebral palsy, cleft lip or palate 9 - Increased requirement ; fever 10 - Endocrine causes ( DM. hyperthyroidism )
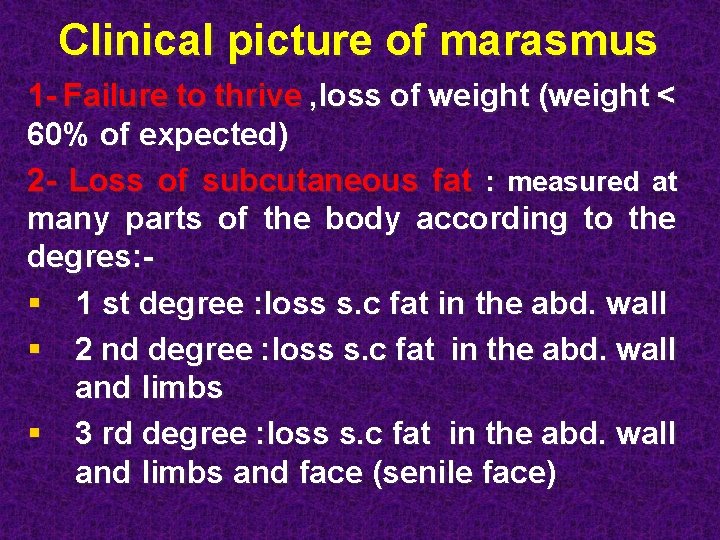
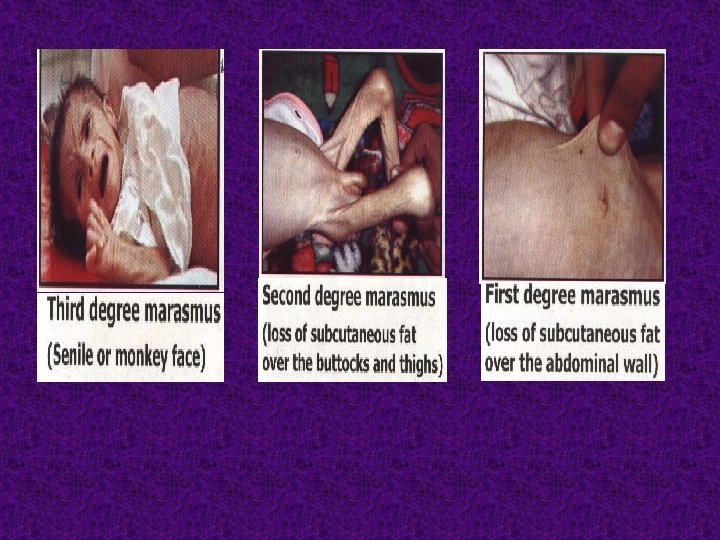
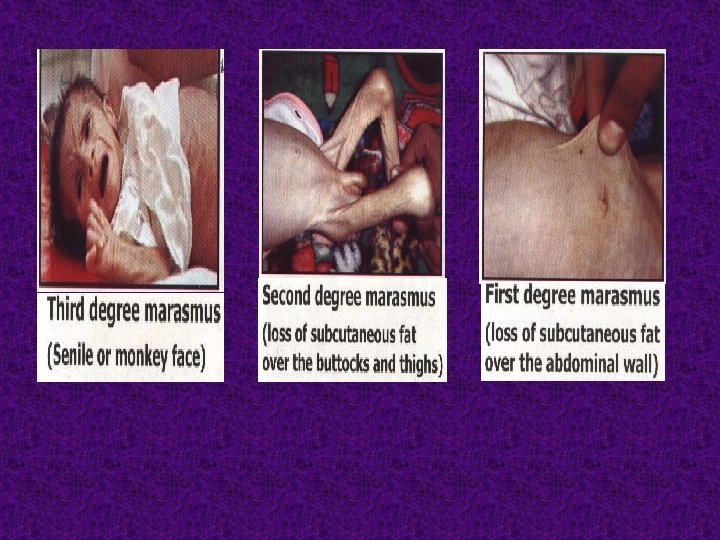
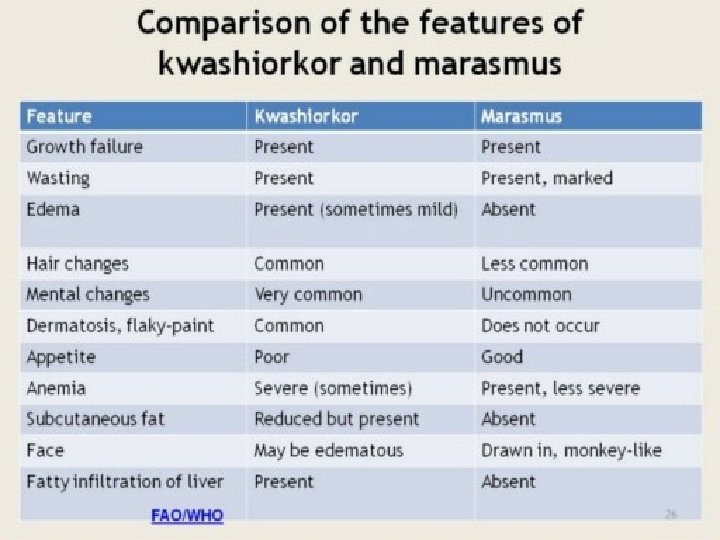
Clinical picture of marasmus 1 - Failure to thrive , loss of weight (weight < 60% of expected) 2 - Loss of subcutaneous fat : measured at many parts of the body according to the degres: § 1 st degree : loss s. c fat in the abd. wall § 2 nd degree : loss s. c fat in the abd. wall and limbs § 3 rd degree : loss s. c fat in the abd. wall and limbs and face (senile face)
Clinical picture of marasmus 3 - Muscle wasting ( thin muscles and prominence of bony surfaces ) 4 - General appearance ; anxious, irritable, hungry, but with infection the child show poor appetite, lethargy 5 - Associated deficiencies; iorn and vitamin A

13
Kwashiorkor § Cecilly Williams, a British nurse, had introduced the word Kwashiorkor to the medical literature in 1933. The word is taken from the Ga language in Ghana & used to describe the sickness of weaning (“the sickness the older child gets when the next baby is born”).
Kwashiorkor Definition It is a clinical syndrome and a form of malnutrition characterized by slow rate of growth due to deficient of protein intake, (adequate supply of calories). Incidence Commonly in toddlers between the age 1 -3 years, following or with weaning
Etiology of Kwashiorkor § 1 -protein intake is deficient --- while energy intake is marginal ---the mother stops breast feeding due to pregnancy and replace it with starchy food § 2 - Infections---- Malnourished child develop diarrhea--- KWO § 3 - Maternal deprivation --- the birth of another infant deprives the child from breast feeding
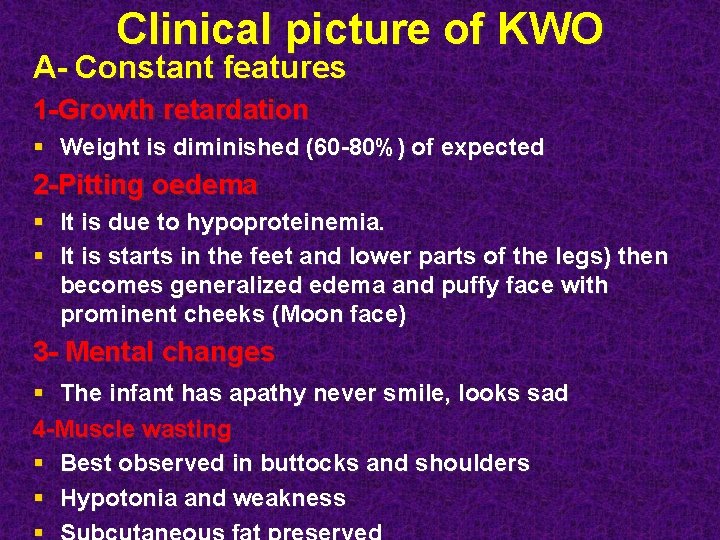
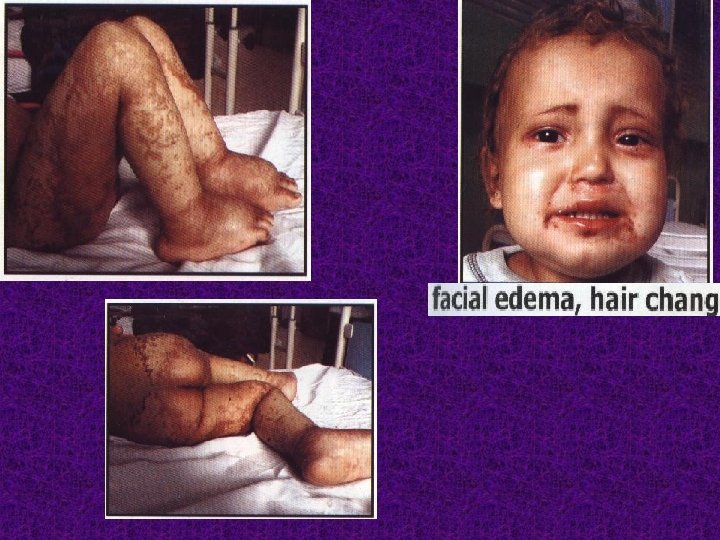
Clinical picture of KWO A- Constant features 1 -Growth retardation § Weight is diminished (60 -80%) of expected 2 -Pitting oedema § It is due to hypoproteinemia. § It is starts in the feet and lower parts of the legs) then becomes generalized edema and puffy face with prominent cheeks (Moon face) 3 - Mental changes § The infant has apathy never smile, looks sad 4 -Muscle wasting § Best observed in buttocks and shoulders § Hypotonia and weakness
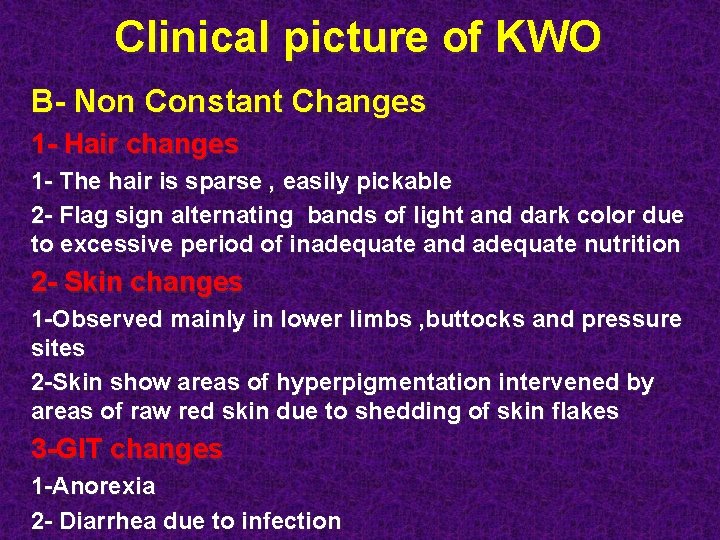
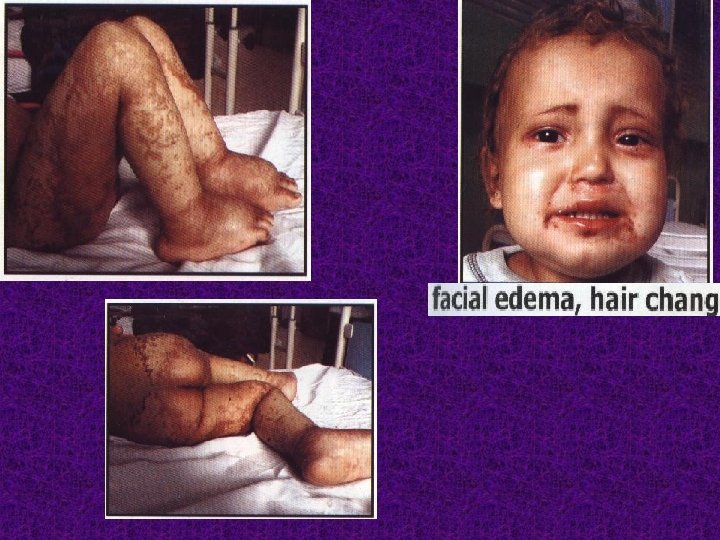
Clinical picture of KWO B- Non Constant Changes 1 - Hair changes 1 - The hair is sparse , easily pickable 2 - Flag sign alternating bands of light and dark color due to excessive period of inadequate and adequate nutrition 2 - Skin changes 1 -Observed mainly in lower limbs , buttocks and pressure sites 2 -Skin show areas of hyperpigmentation intervened by areas of raw red skin due to shedding of skin flakes 3 -GIT changes 1 -Anorexia 2 - Diarrhea due to infection
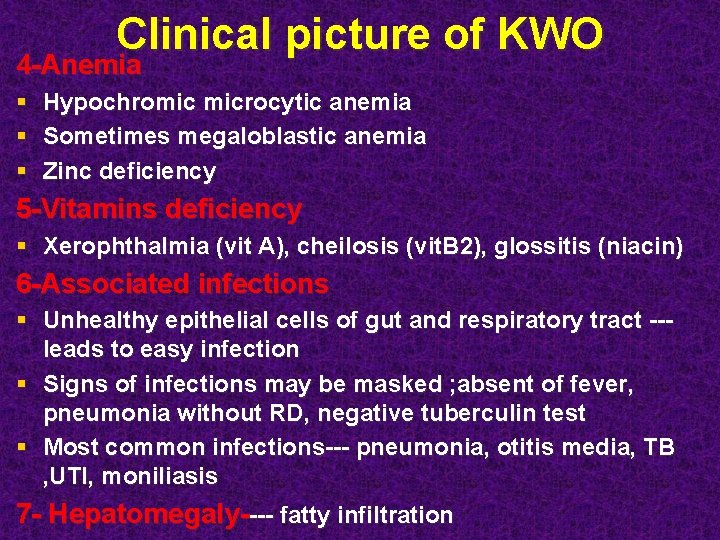
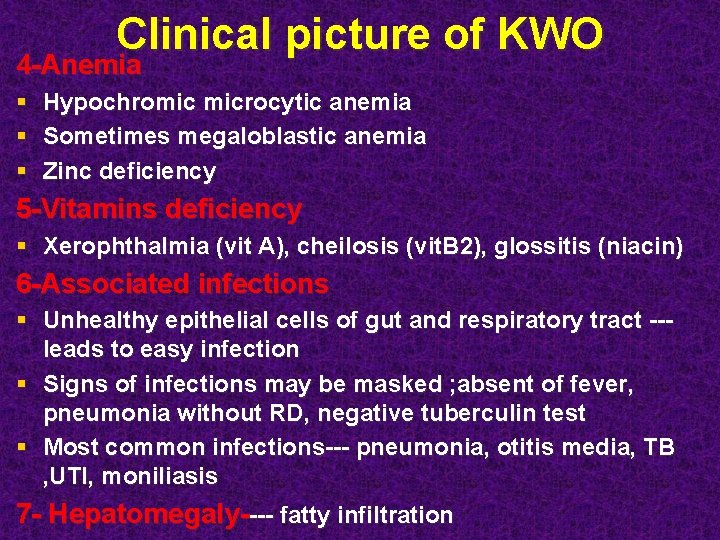
Clinical picture of KWO 4 -Anemia § Hypochromic microcytic anemia § Sometimes megaloblastic anemia § Zinc deficiency 5 -Vitamins deficiency § Xerophthalmia (vit A), cheilosis (vit. B 2), glossitis (niacin) 6 -Associated infections § Unhealthy epithelial cells of gut and respiratory tract --leads to easy infection § Signs of infections may be masked ; absent of fever, pneumonia without RD, negative tuberculin test § Most common infections--- pneumonia, otitis media, TB , UTI, moniliasis 7 - Hepatomegaly---- fatty infiltration

21
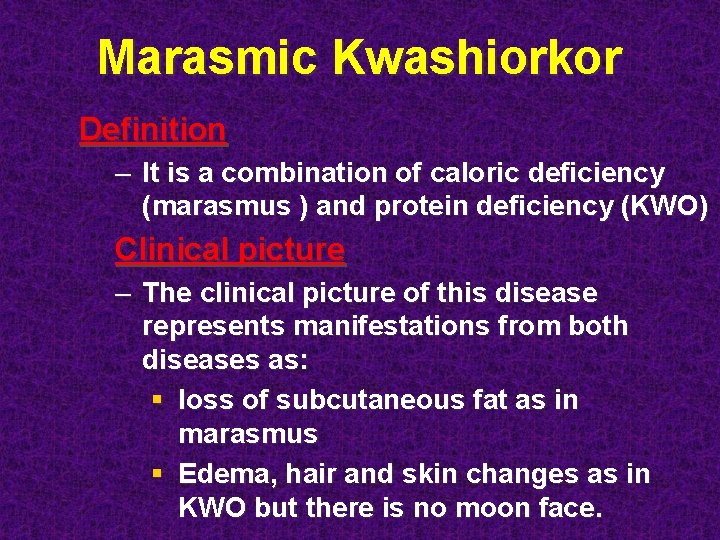
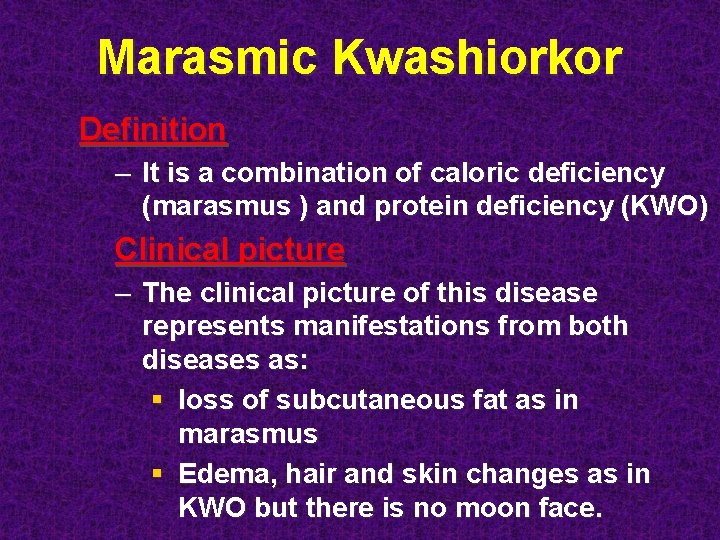
Marasmic Kwashiorkor Definition – It is a combination of caloric deficiency (marasmus ) and protein deficiency (KWO) Clinical picture – The clinical picture of this disease represents manifestations from both diseases as: § loss of subcutaneous fat as in marasmus § Edema, hair and skin changes as in KWO but there is no moon face.
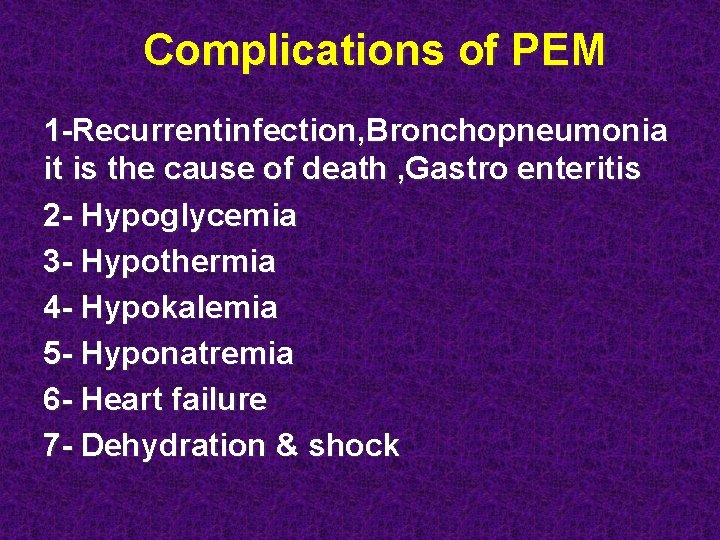
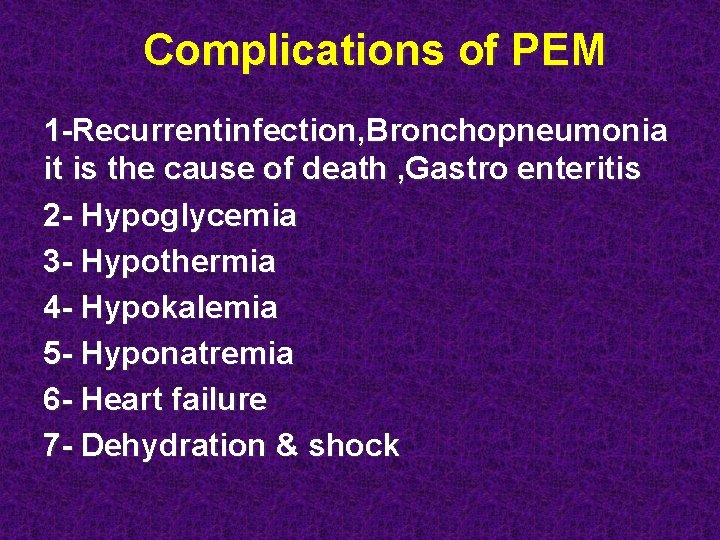
Complications of PEM 1 -Recurrentinfection, Bronchopneumonia it is the cause of death , Gastro enteritis 2 - Hypoglycemia 3 - Hypothermia 4 - Hypokalemia 5 - Hyponatremia 6 - Heart failure 7 - Dehydration & shock
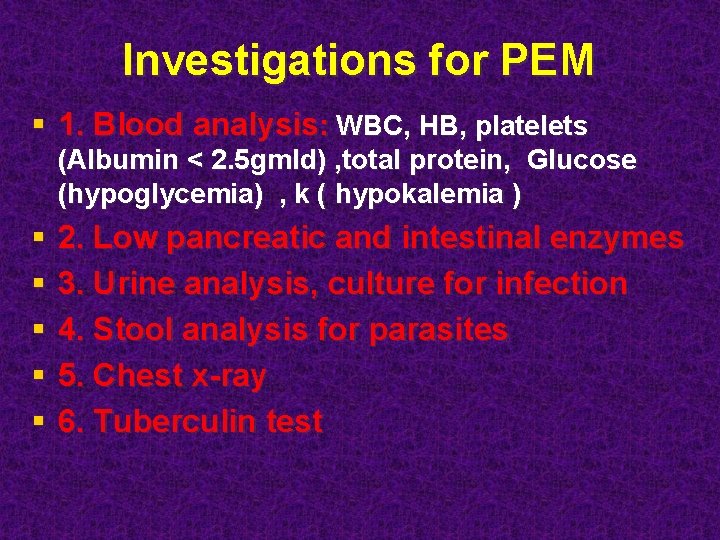
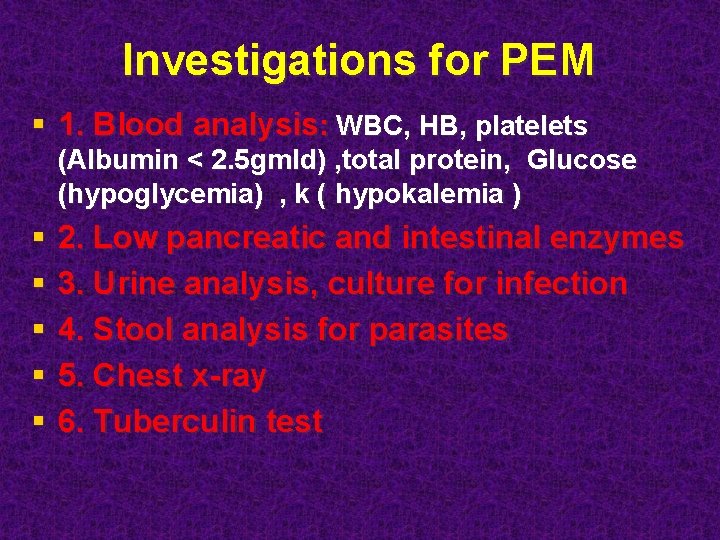
Investigations for PEM § 1. Blood analysis: WBC, HB, platelets (Albumin < 2. 5 gmld) , total protein, Glucose (hypoglycemia) , k ( hypokalemia ) § § § 2. Low pancreatic and intestinal enzymes 3. Urine analysis, culture for infection 4. Stool analysis for parasites 5. Chest x-ray 6. Tuberculin test
25
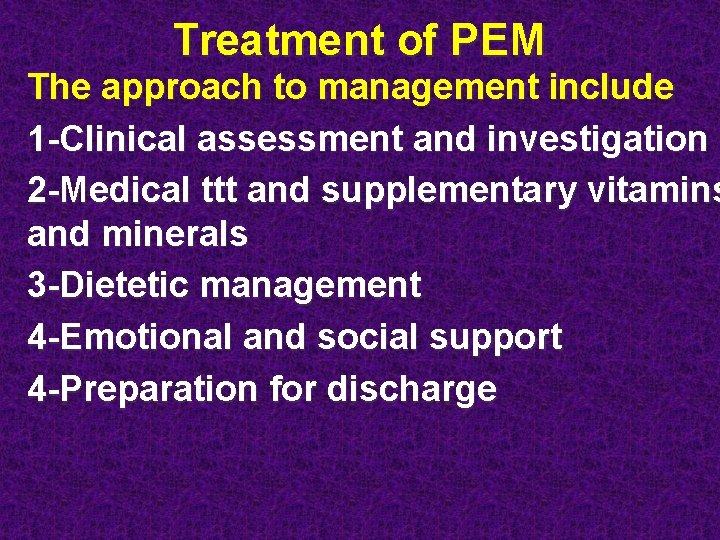
Treatment of PEM The approach to management include 1 -Clinical assessment and investigation 2 -Medical ttt and supplementary vitamins and minerals 3 -Dietetic management 4 -Emotional and social support 4 -Preparation for discharge
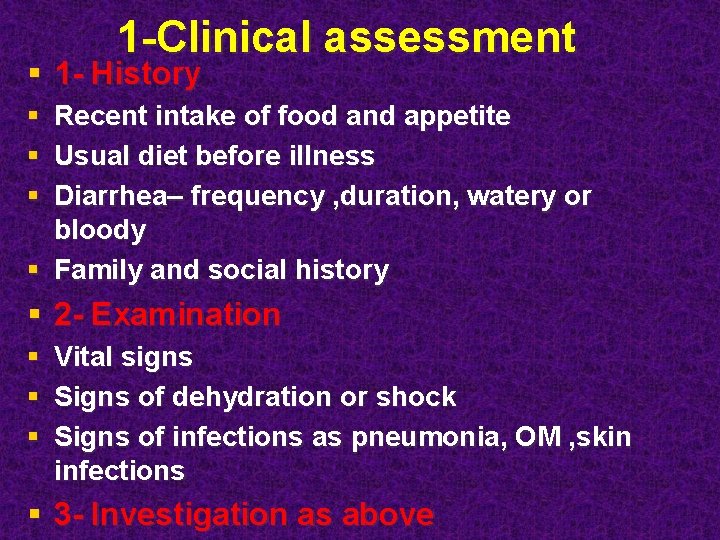
1 -Clinical assessment § 1 - History § Recent intake of food and appetite § Usual diet before illness § Diarrhea– frequency , duration, watery or bloody § Family and social history § 2 - Examination § Vital signs § Signs of dehydration or shock § Signs of infections as pneumonia, OM , skin infections § 3 - Investigation as above
§ § 2 -Medical treatment 1 -Rehydration 2 -Infections --- most cases suffer from infections even if there is no infection and give broad spectrum antibiotics (amoxicillin and gentamicin) § 3 -Hypothermia --- by clothing and head cap § 4 -Hypoglycemia --- start immediately feeding or give glucose 10% § 5 -Electrolytes imbalance § Potassium— 3 -4 mmol/kg/day § Magnesium---0. 4 -0. 6 mmol/kg/day § 6 -Eye problems – vit A and antibiotics eye drops § 7 -Sever anemia --- blood transfusion if Hg<4 g/dl or if there is RD or heart failure

2 -Medical treatment § 8 -Skin lesions § § Soak in 1%potassium permanganate for 10 min daily Cream as zinc and castor oil Gentian violet or nystatin cream for skin sores Zinc supplementation § 9 -Treatment of diarrhea § 10 -Vitamins and minerals/day/orally § § Folate Zinc Copper, magnesium Vitamin A 50. 000 -200, 000 IU
3 - Dietetic management § 1 -Frequent small feeds in the early stages to improve tolerance § 2 - NGT is usually required due to anorexia § 3 - Half concentration in first 2 days and gradually increase to full concentration § There is 2 types of formula § 1 - Starter formula (75 kcl) for first 7 days ------ and consist of (yoghurt or cow milk, sucrose, oil and water) full Cream and skimmed dried milk § 2 -Catch up formula (100 kcl) after the first 7 days ----- and consist of the same above but with increase in their amounts § Start with 130 ml/kg/day then gradually increase to 200 ml/kg/day

THANK YOU
 More more more i want more more more more we praise you
More more more i want more more more more we praise you More more more i want more more more more we praise you
More more more i want more more more more we praise you Generous kelimesinin comparative hali
Generous kelimesinin comparative hali Half life more than 2 less than 4
Half life more than 2 less than 4 Better than god
Better than god Introduction of malnutrition
Introduction of malnutrition Percents less than 1
Percents less than 1 Greater than less than fractions
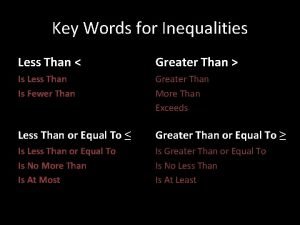
Greater than less than fractions Less than keywords
Less than keywords Fractions odd one out
Fractions odd one out Jesus lord of heaven
Jesus lord of heaven Dot
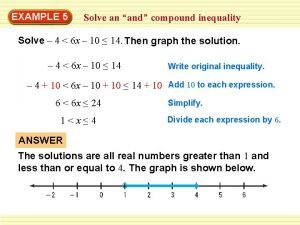
Dot Compound inequality examples
Compound inequality examples Climbed in a sentence
Climbed in a sentence Context evaluation of curriculum
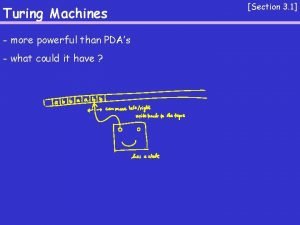
Context evaluation of curriculum Turing machine is more powerful than pda
Turing machine is more powerful than pda Which equation represents sublimation?
Which equation represents sublimation? Ted s flight
Ted s flight How to cite more than one author
How to cite more than one author Research terminologies
Research terminologies At least inequality sign
At least inequality sign Device made up of more than one simple machine
Device made up of more than one simple machine Software is more than just a
Software is more than just a Meherjan passage bangla meaning
Meherjan passage bangla meaning Ella's job responsibilities include
Ella's job responsibilities include Nothing on earth is more international than disease
Nothing on earth is more international than disease Nothing is more precious than health
Nothing is more precious than health Not just bingo march
Not just bingo march Can an atom have more neutrons than protons
Can an atom have more neutrons than protons Mass volume density video
Mass volume density video Pegawai pemasaran
Pegawai pemasaran Cummings love is thicker than forget
Cummings love is thicker than forget