Nottingham lung cancer CARE service Cachexia Anorexia and




![Top 10 symptoms or issues Percentage [95% CI] of patients reporting 'very much' or Top 10 symptoms or issues Percentage [95% CI] of patients reporting 'very much' or](https://slidetodoc.com/presentation_image_h/0d7c1ce7a05c84e79b26fc48c2ba58c7/image-15.jpg)




- Slides: 36
Nottingham lung cancer CARE service (Cachexia, Anorexia and Related Experiences) Dr Andrew Wilcock DM FRCP Clinical Reader in Palliative Medicine and Medical Oncology, Honorary Consultant Physician Nottingham University Hospitals NHS Trust

Who are we? Multidisciplinary team: dietitian, OT, physio, therapy assistant and data manager

Nottingham lung cancer CARE service • 3 -year service project funded by • overseen by a steering committee.
Lung cancer CARE service • dedicated to all people with thoracic cancer • particular focus on the effects of cachexia • fulfils national guidance – HNA – rehabilitation • integrated with lung cancer and specialist palliative care services.
Nottingham lung cancer CARE service Aims: • increase understanding of the supportive care needs, with particular emphasis on common distressing symptoms, maximising function and independence • offer best available evidence-based care
Nottingham lung cancer CARE service Aims: • continually evaluate the efficacy of the care in order to improve the care offered • develop a model of care that could be rolled out to other centres and people with other types of cancer.
Why a focus on cachexia syndrome? • lung cancer has a high incidence of cachexia even at diagnosis • cachexia contributes to high morbidity and mortality • costs result from reduced independence • no established treatments • major unmet need in lung cancer.
Outcomes of interest • • • activity holistic needs assessment nutritional assessment and support hospital bed use, place of death other outcomes available/in progress.
Activity In 2 years saw over 540 new patients: • 1, 100 new and 4, 900 f. u. episodes of care • 3, 200 face to face • 80% of new, 12% of f. u. in patients home.

HNA: SPARC© questionnaire • helps identify patients who may benefit from additional supportive/palliative care • self-completed, but help from lay or professional carer’s permitted • begins with explanatory paragraph; leave blank if unsure

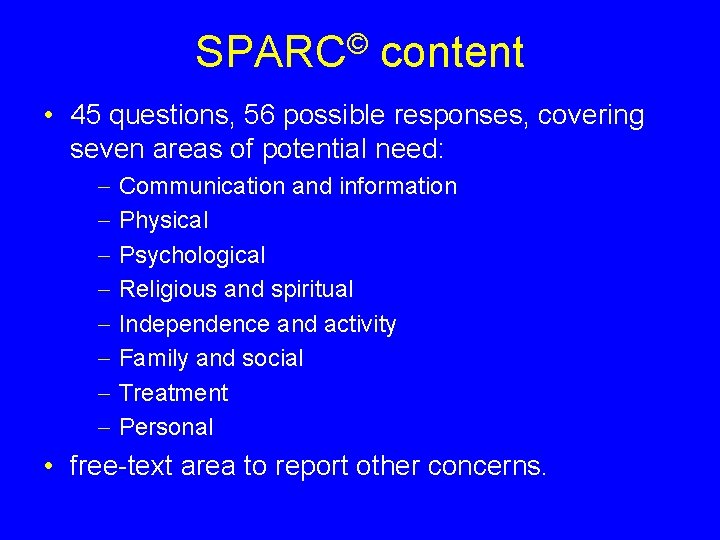
SPARC© content • 45 questions, 56 possible responses, covering seven areas of potential need: Communication and information Physical Psychological Religious and spiritual Independence and activity Family and social Treatment Personal • free-text area to report other concerns.
SPARC© use in Nottingham • all patients invited to complete the SPARC after diagnosis • results discussed at a weekly MDT meeting • generally, patients scoring ‘Quite a bit’ or ‘Very much’ in particular issues will also be contacted for further assessment by the appropriate team member • all patients assessed by the dietitian.
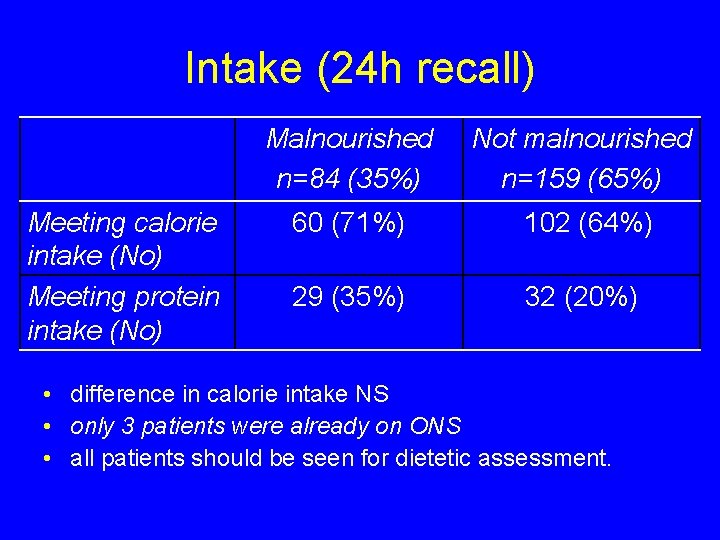
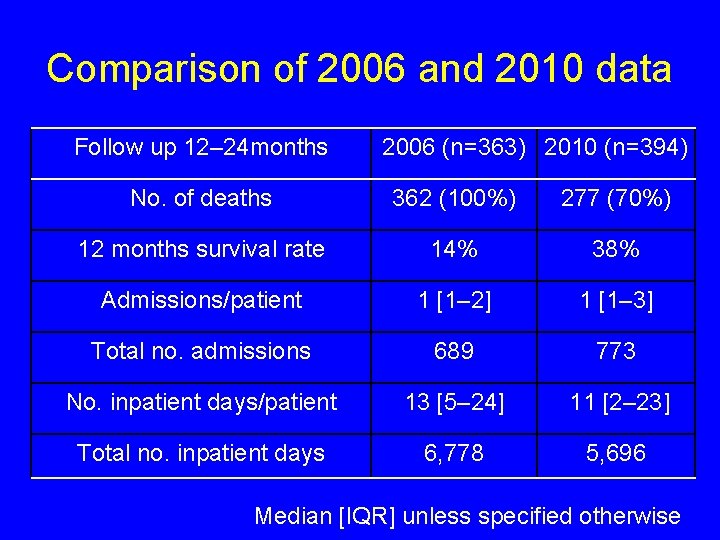
Needs identified (n=650) • all patients reported distress with at least one symptom or issue • median [IQR] number of symptoms or issues causing distress or bother: 2 [0– 5] ‘very much’, 4 [2– 7] ‘quite a bit’ 10 [8– 14] ‘a little’
![Top 10 symptoms or issues Percentage 95 CI of patients reporting very much or Top 10 symptoms or issues Percentage [95% CI] of patients reporting 'very much' or](https://slidetodoc.com/presentation_image_h/0d7c1ce7a05c84e79b26fc48c2ba58c7/image-15.jpg)
Top 10 symptoms or issues Percentage [95% CI] of patients reporting 'very much' or 'quite a bit' of distress or bother Feeling tired 51 [47– 55] Shortness of breath 49 [45– 53] Concern about effects of illness on family Change in weight Problems sleeping at night Cough Feeling sleepy during the day Loss of appetite Pain Feeling anxious 40 [37– 44] 40 39 37 36 35 34 [36– 44] [35– 43] [33– 41] [32– 40] [32– 39] [31– 38] 34 [30– 37]
Implications Based on the developers’ recommendations: • all patients should be brought to the attention of the clinical team • 161 (25%) early attention • 443 (68%) immediate attention.
Nutritional assessment and support In keeping with national guidance


Dietetic evaluation • • • initially, all patients seen by dietitian 243 patients seen in 1 st year generally within 4– 8 weeks of diagnosis unique dataset previously limited to subsets of patients: – chemotherapy – surgery.
Dietetic evaluation • screened using NICE guidance – simple – quick.
Malnourished patients should be considered for nutrition support: • BMI <18. 5 kg/m 2 • unintentional weight loss >10% in last 3 6 months • BMI <20 kg/m 2 and >5% weight loss in last 3 6 months.
Dietetic evaluation • • 84 malnourished (35%) 159 not malnourished (65%) little difference in age, sex, diagnosis, stage 15 (18%) malnourished receiving treatment with curative intent.
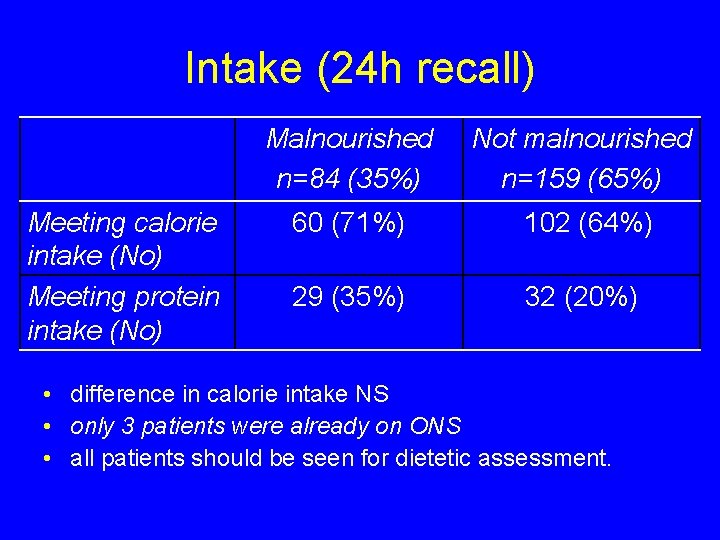
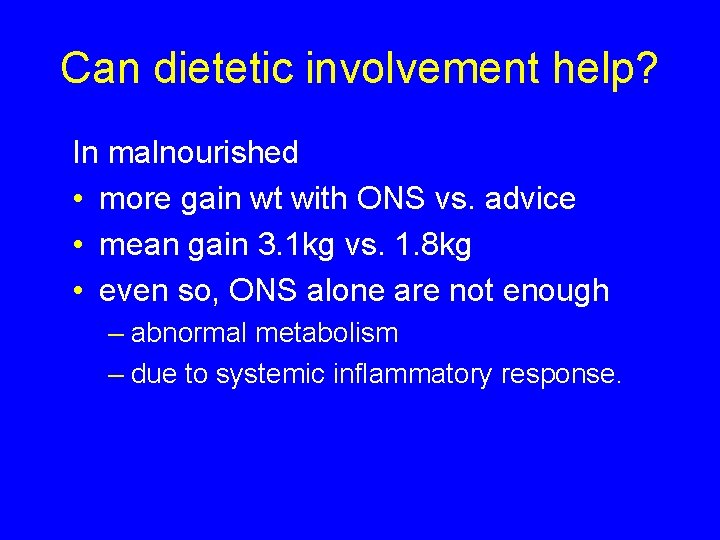
Intake (24 h recall) Meeting calorie intake (No) Meeting protein intake (No) Malnourished n=84 (35%) Not malnourished n=159 (65%) 60 (71%) 102 (64%) 29 (35%) 32 (20%) • difference in calorie intake NS • only 3 patients were already on ONS • all patients should be seen for dietetic assessment.
Can dietetic involvement help? In malnourished • more gain wt with ONS vs. advice • mean gain 3. 1 kg vs. 1. 8 kg • even so, ONS alone are not enough – abnormal metabolism – due to systemic inflammatory response.
Can dietetic involvement help? Essentially, irrespective of nutritional status: • 69% maintain (42%) or gain (27%) weight • 31% lose weight.
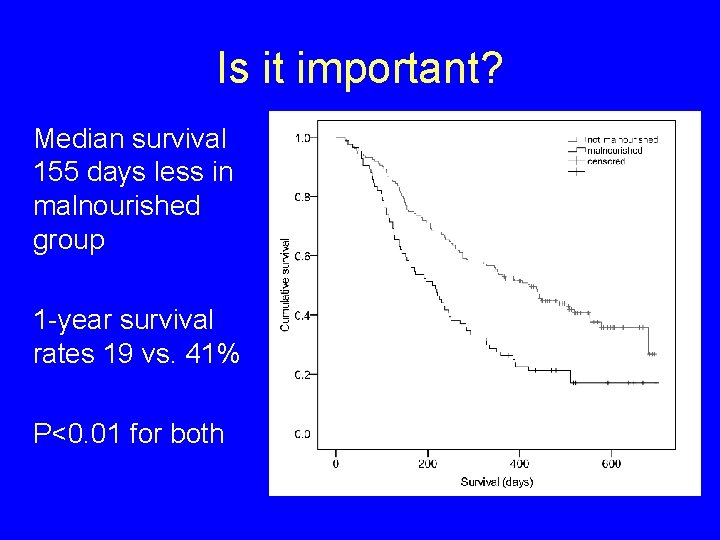
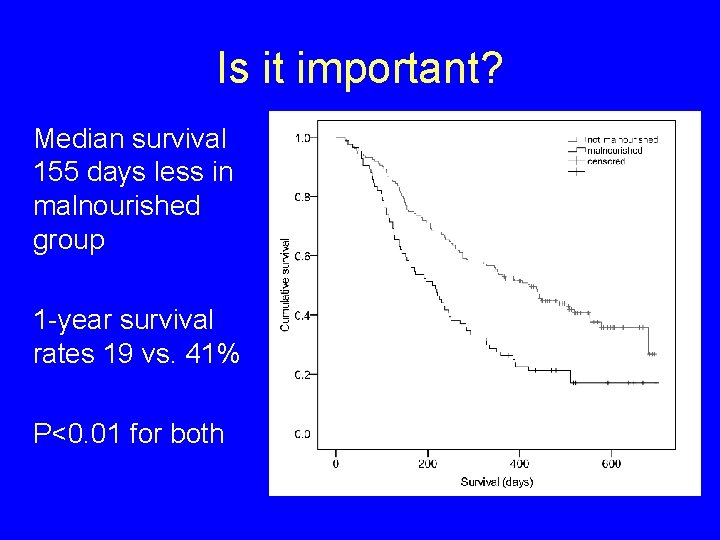
Is it important? Median survival 155 days less in malnourished group 1 -year survival rates 19 vs. 41% P<0. 01 for both
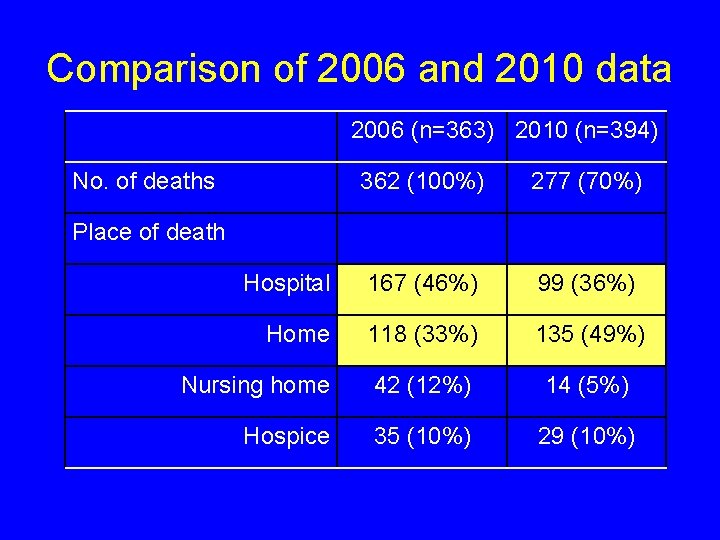
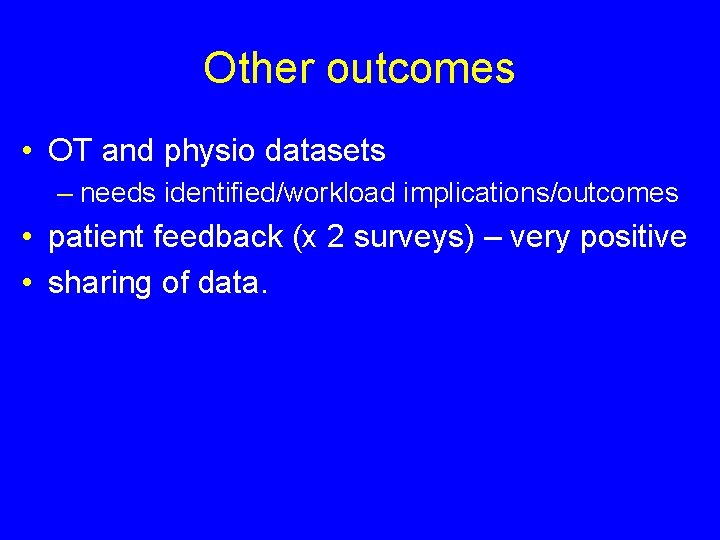
Hospital bed use and place of death Comparison of pre- (2006) and post- (2010) CARE service
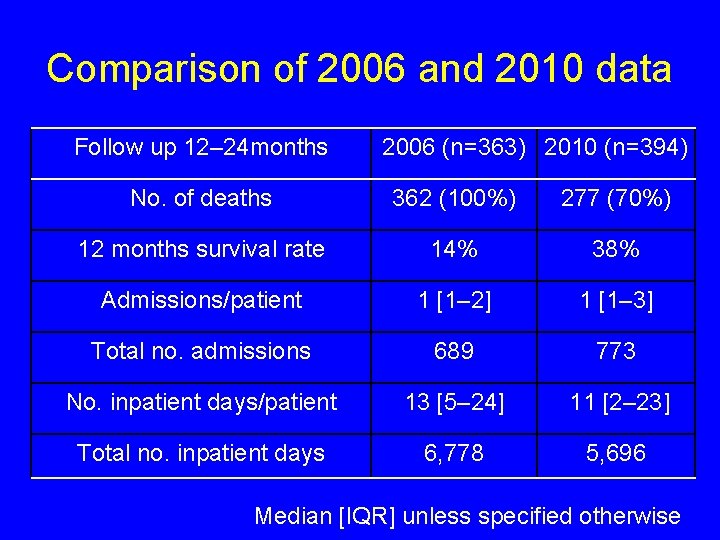
Comparison of 2006 and 2010 data Follow up 12– 24 months 2006 (n=363) 2010 (n=394) No. of deaths 362 (100%) 277 (70%) 12 months survival rate 14% 38% Admissions/patient 1 [1– 2] 1 [1– 3] Total no. admissions 689 773 No. inpatient days/patient 13 [5– 24] 11 [2– 23] Total no. inpatient days 6, 778 5, 696 Median [IQR] unless specified otherwise
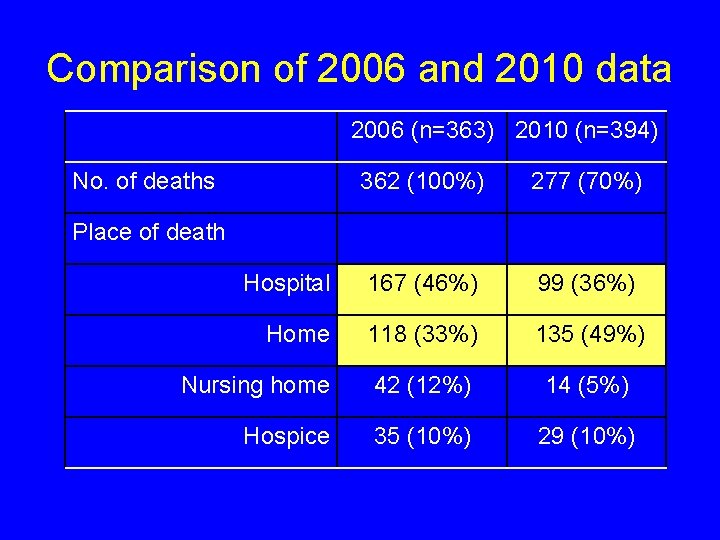
Comparison of 2006 and 2010 data 2006 (n=363) 2010 (n=394) No. of deaths 362 (100%) 277 (70%) Hospital 167 (46%) 99 (36%) Home 118 (33%) 135 (49%) Nursing home 42 (12%) 14 (5%) Hospice 35 (10%) 29 (10%) Place of death
Other outcomes • OT and physio datasets – needs identified/workload implications/outcomes • patient feedback (x 2 surveys) – very positive • sharing of data.
Links established include • Department of Health Lung Cancer and Mesothelioma Advisory Board • UK Lung Cancer Care Coalition • National Cancer Action Team: Holistic Assessment Team (exemplar of good practice) • National Cancer Action Team: Cancer and Palliative Care Rehabilitation Workforce Project.
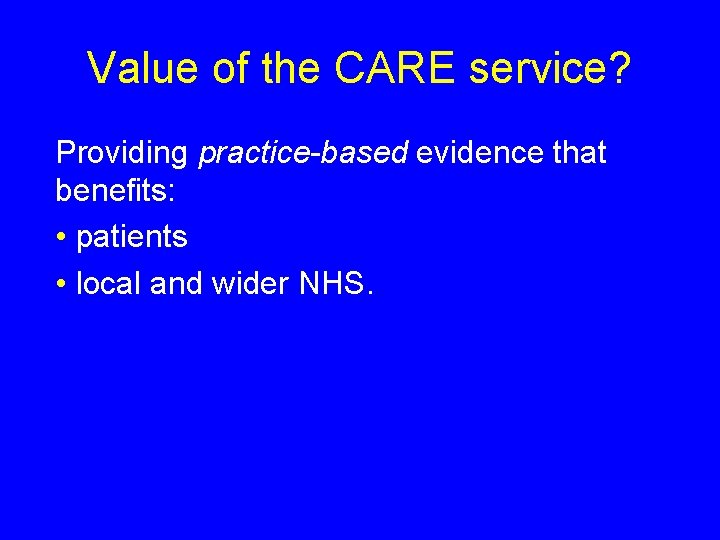
Value of the CARE service? Providing practice-based evidence that benefits: • patients • local and wider NHS.

Winner of Pfizer Oncology Team of the Year 2011

The future? • funding from MCS until end June 2012 • ongoing funding in current climate uncertain • currently evaluating impact in providing proactive rehabilitation to specialist palliative care outpatients/day care • tendering to provide specialist palliative care rehabilitation service.
Thank you for listening. Questions?
 Anorexia cachexia palliative care
Anorexia cachexia palliative care Benign and malignant tumor
Benign and malignant tumor Kwashiorkor pictures
Kwashiorkor pictures Tnm stage lung cancer
Tnm stage lung cancer Cerebral salt wasting
Cerebral salt wasting Gesundheit central european lung cancer patient ne
Gesundheit central european lung cancer patient ne Lung cancer location
Lung cancer location Lung cancer screening shared decision making tool
Lung cancer screening shared decision making tool Nursing diagnosis of lung cancer
Nursing diagnosis of lung cancer Optimal lung cancer pathway
Optimal lung cancer pathway Optimal lung cancer pathway
Optimal lung cancer pathway Lifetime risk of lung cancer
Lifetime risk of lung cancer Anorexia palliative care
Anorexia palliative care Levels of nursing care primary secondary tertiary
Levels of nursing care primary secondary tertiary Personal care products and cancer risk
Personal care products and cancer risk Care plan of breast cancer
Care plan of breast cancer Oncology nursing management in cancer care
Oncology nursing management in cancer care International society of nurses in cancer care
International society of nurses in cancer care Nursing care plan for breast cancer ppt
Nursing care plan for breast cancer ppt Nursing care plan of cancer patients ppt
Nursing care plan of cancer patients ppt Long term anorexia effects
Long term anorexia effects Lesson 6 anorexia nervosa and bulimia
Lesson 6 anorexia nervosa and bulimia Anorexia and stomach ulcers
Anorexia and stomach ulcers Anorexia and bulimia venn diagram
Anorexia and bulimia venn diagram Nottingham and nottinghamshire ics
Nottingham and nottinghamshire ics Nottingham north and east ccg
Nottingham north and east ccg Winona ryder anorexia
Winona ryder anorexia Freud anorexia
Freud anorexia Male
Male Bulimiq
Bulimiq Type of anorexia
Type of anorexia Social learning theory anorexia
Social learning theory anorexia Intervention anorexia episodes
Intervention anorexia episodes Dominique anorexia
Dominique anorexia Bullimia nervosa definition
Bullimia nervosa definition Historia natural de la enfermedad anorexia
Historia natural de la enfermedad anorexia Cid bulimia
Cid bulimia