Nutrition in the Patient with Anorexia and Cachexia

- Slides: 21
Nutrition in the Patient with Anorexia and Cachexia Jeanette N. Keith, M. D. Associate Professor of Medicine Departments of Nutrition Sciences and Medicine University of Alabama at Birmingham
Protein-Energy Malnutrition Two major types • Marasmus • Kwashiorkor (AKA: Protein Calorie Malnutrition) Heimburger DC, Ard JD. Handbook of Clinical Nutrition 4/e, 2006
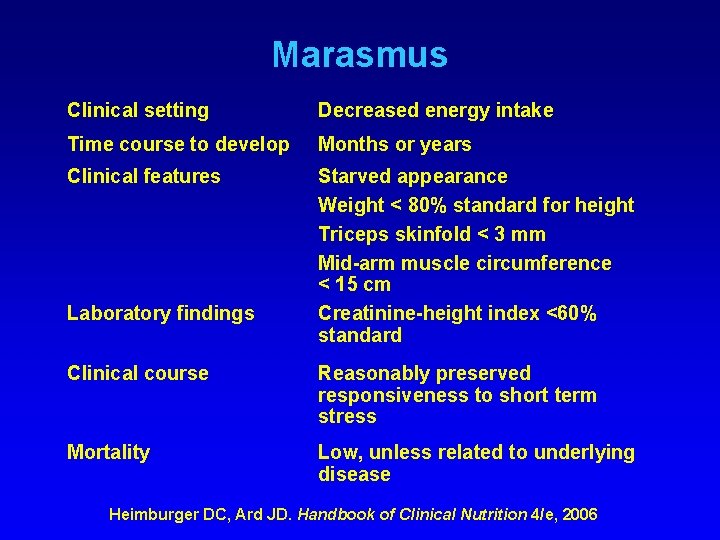
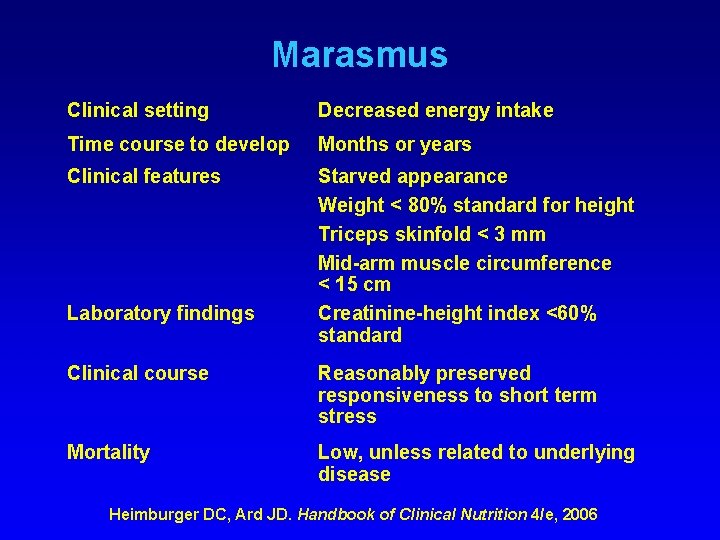
Marasmus Clinical setting Decreased energy intake Time course to develop Months or years Clinical features Starved appearance Weight < 80% standard for height Triceps skinfold < 3 mm Mid-arm muscle circumference < 15 cm Creatinine-height index <60% standard Laboratory findings Clinical course Reasonably preserved responsiveness to short term stress Mortality Low, unless related to underlying disease Heimburger DC, Ard JD. Handbook of Clinical Nutrition 4/e, 2006
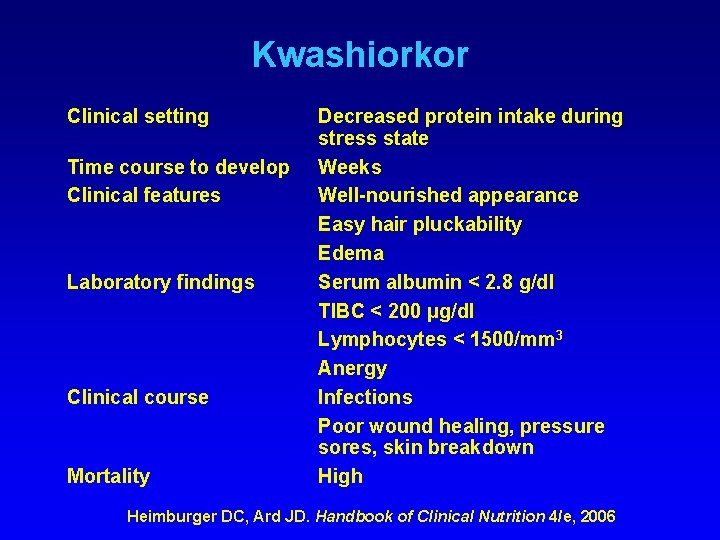
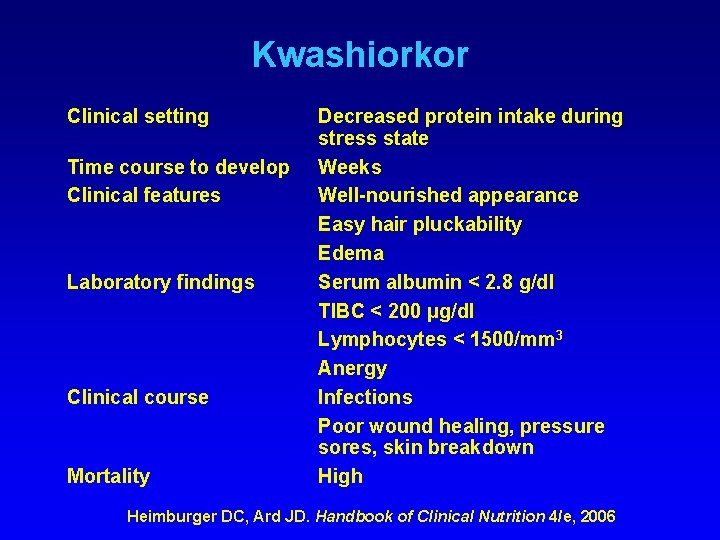
Kwashiorkor Clinical setting Time course to develop Clinical features Laboratory findings Clinical course Mortality Decreased protein intake during stress state Weeks Well-nourished appearance Easy hair pluckability Edema Serum albumin < 2. 8 g/dl TIBC < 200 μg/dl Lymphocytes < 1500/mm 3 Anergy Infections Poor wound healing, pressure sores, skin breakdown High Heimburger DC, Ard JD. Handbook of Clinical Nutrition 4/e, 2006
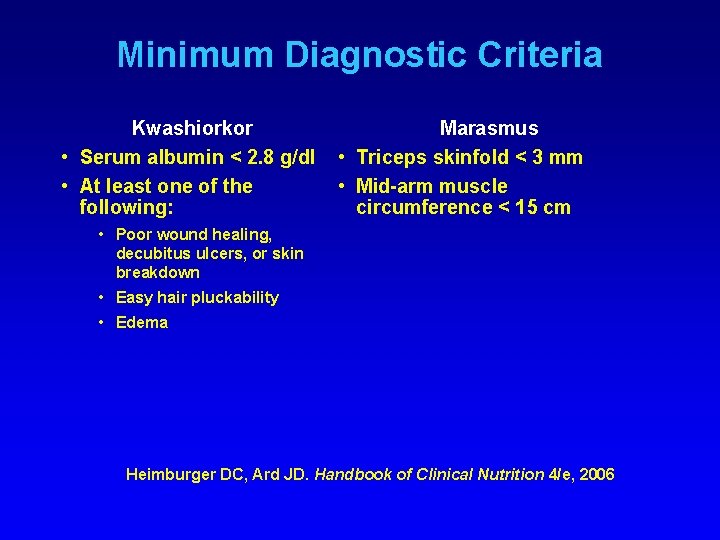
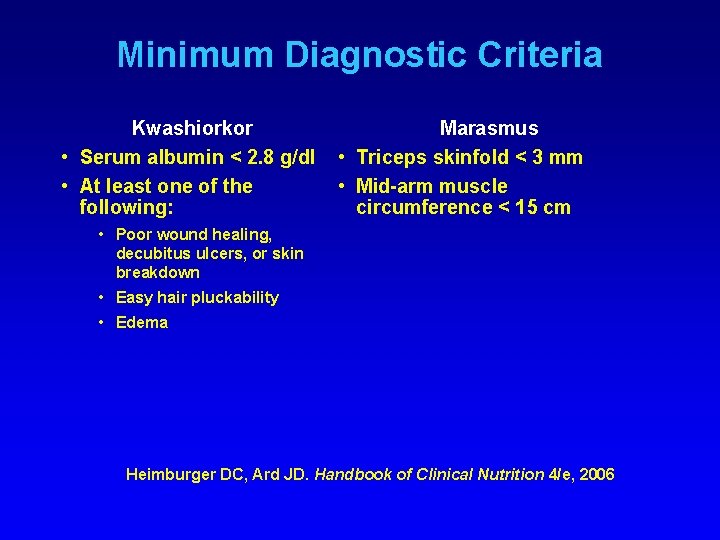
Minimum Diagnostic Criteria Kwashiorkor • Serum albumin < 2. 8 g/dl • At least one of the following: Marasmus • Triceps skinfold < 3 mm • Mid-arm muscle circumference < 15 cm • Poor wound healing, decubitus ulcers, or skin breakdown • Easy hair pluckability • Edema Heimburger DC, Ard JD. Handbook of Clinical Nutrition 4/e, 2006
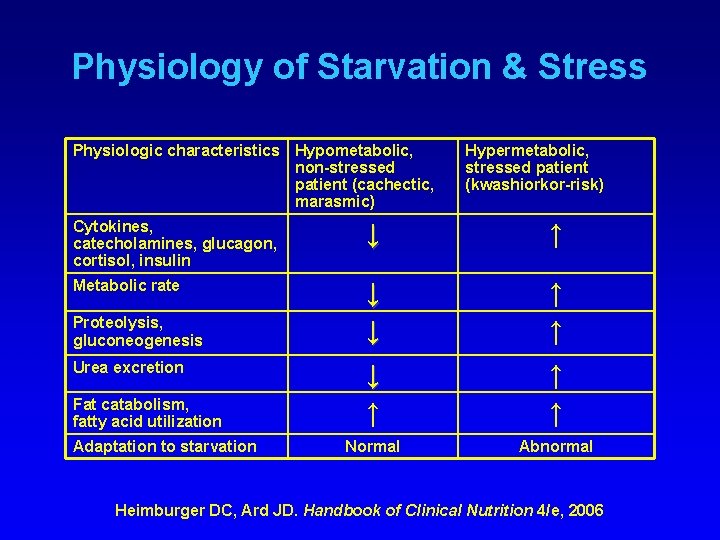
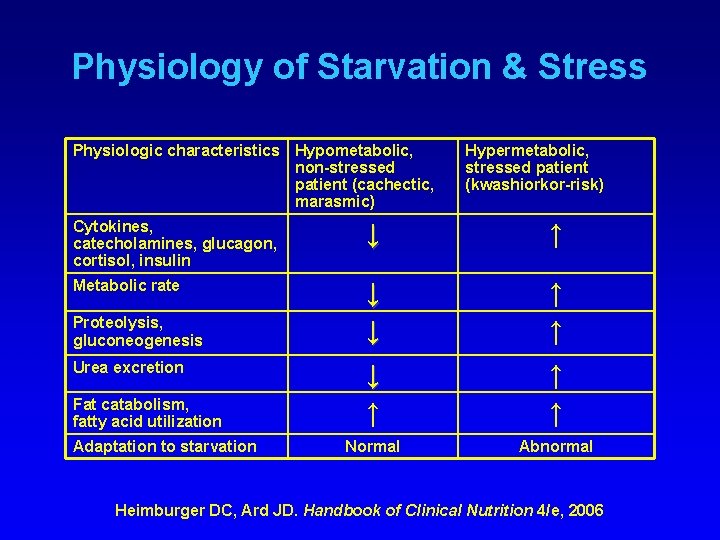
Physiology of Starvation & Stress Physiologic characteristics Hypometabolic, non-stressed patient (cachectic, marasmic) Hypermetabolic, stressed patient (kwashiorkor-risk) Cytokines, catecholamines, glucagon, cortisol, insulin ↓ ↑ Metabolic rate ↓ ↓ ↑ ↑ ↑ Normal Abnormal Proteolysis, gluconeogenesis Urea excretion Fat catabolism, fatty acid utilization Adaptation to starvation Heimburger DC, Ard JD. Handbook of Clinical Nutrition 4/e, 2006
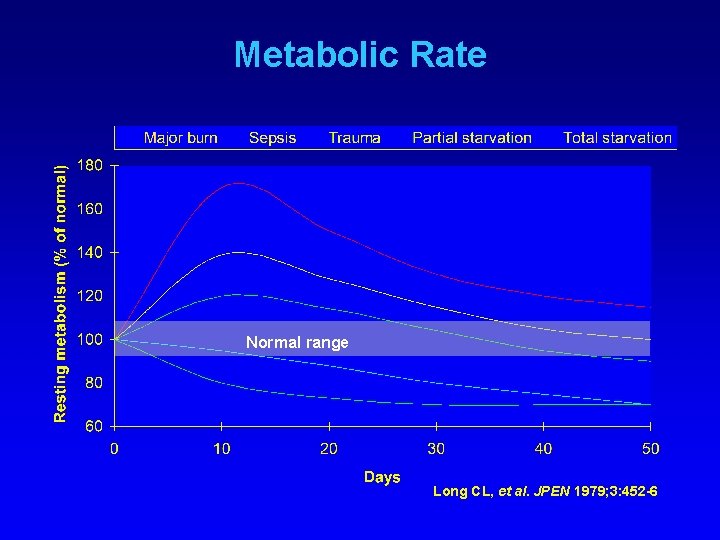
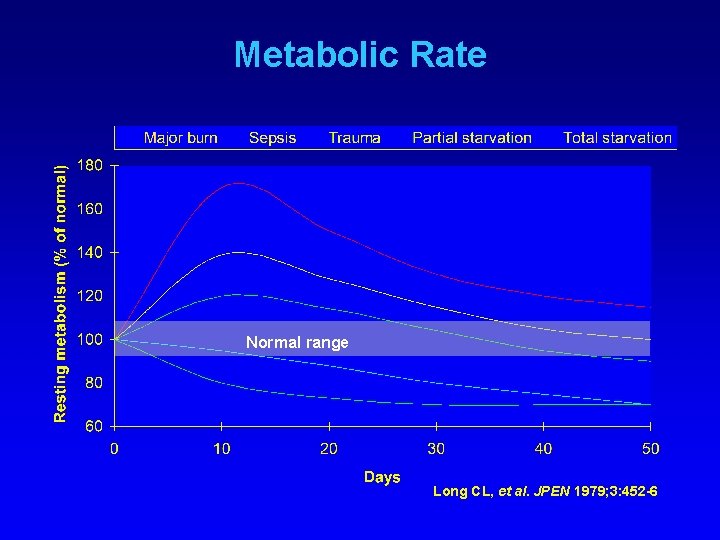
Metabolic Rate Normal range Long CL, et al. JPEN 1979; 3: 452 -6
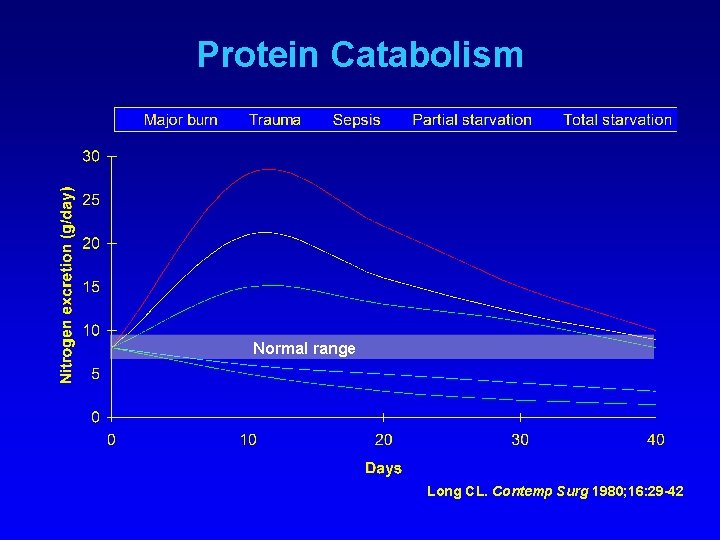
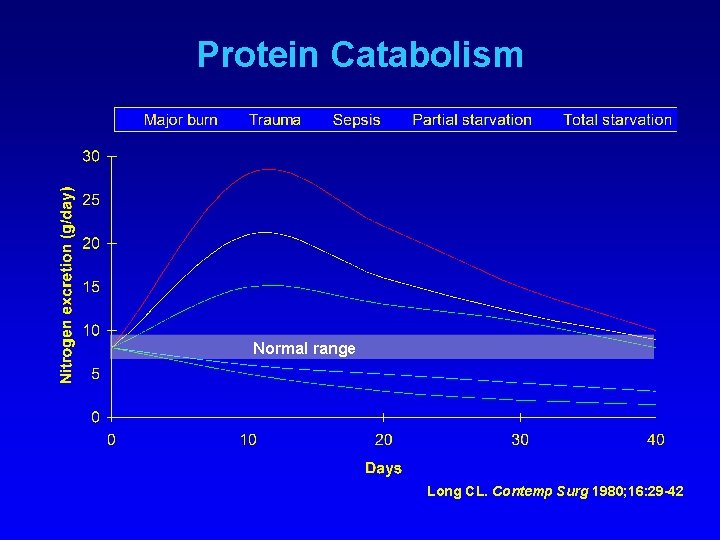
Protein Catabolism Normal range Long CL. Contemp Surg 1980; 16: 29 -42
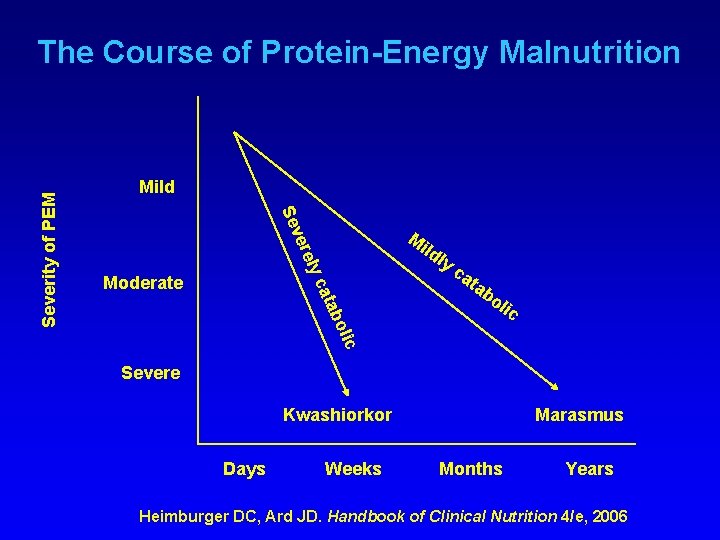
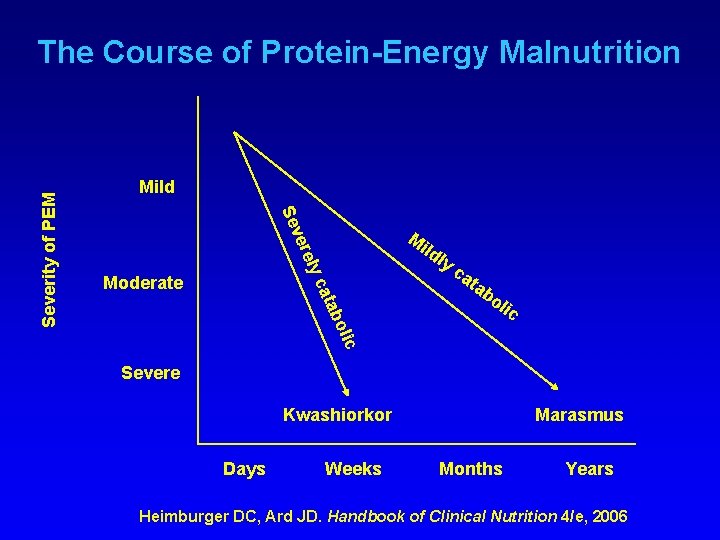
Mild Se M ver ild ly ely Moderate ca ta bo lic abo cat Severity of PEM The Course of Protein-Energy Malnutrition Severe Kwashiorkor Days Weeks Marasmus Months Years Heimburger DC, Ard JD. Handbook of Clinical Nutrition 4/e, 2006

Case Presentation • 27 -year old female with a 35 pound weight loss in the last six months presents to your morning clinic with her mother • In the last two weeks, she has lost an additional 10 pounds. She reports decreased po intake, mild epigastric discomfort and bloating • The patient’s main concern is the loss of appetite, and fatigue • She is 5’ 7” tall and weighs 67 pounds, (BP 90/40, P 60, R 18, T 97. 8)
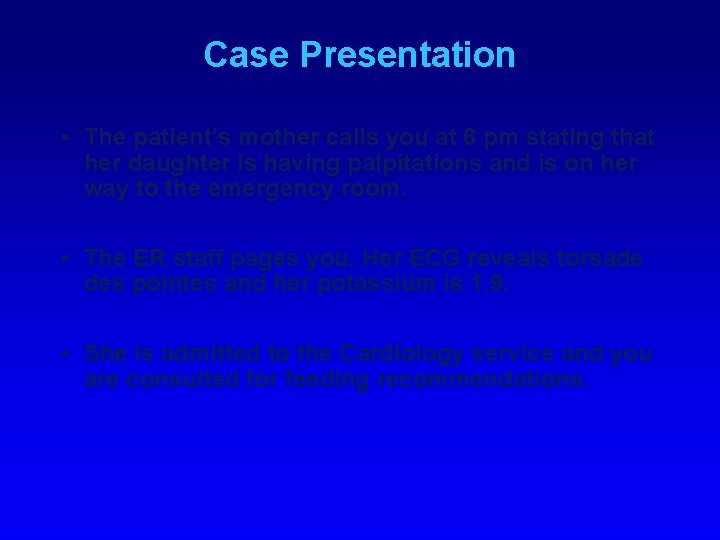
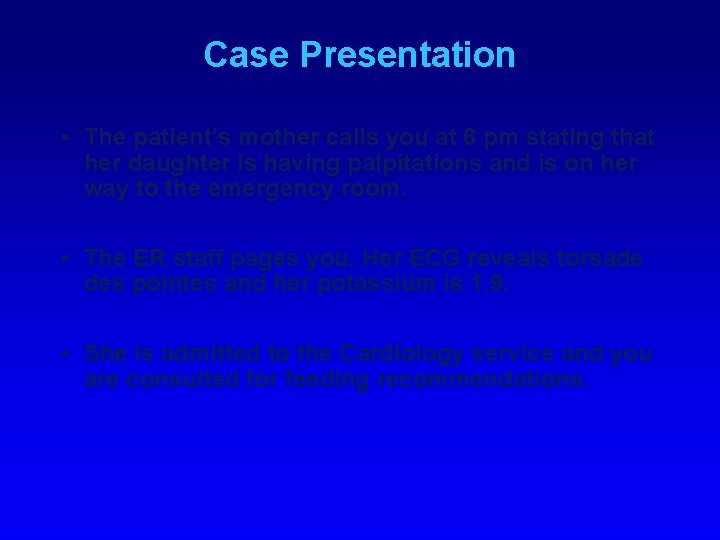
Case Presentation • The patient’s mother calls you at 6 pm stating that her daughter is having palpitations and is on her way to the emergency room. • The ER staff pages you. Her ECG reveals torsade des pointes and her potassium is 1. 9. • She is admitted to the Cardiology service and you are consulted for feeding recommendations.
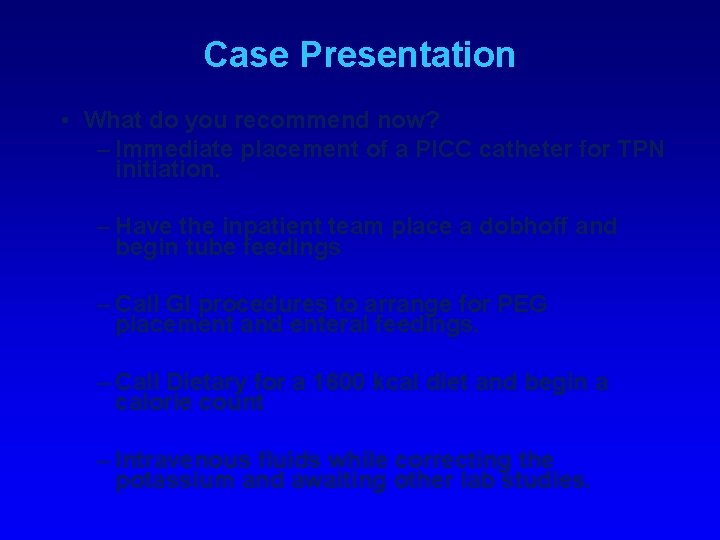
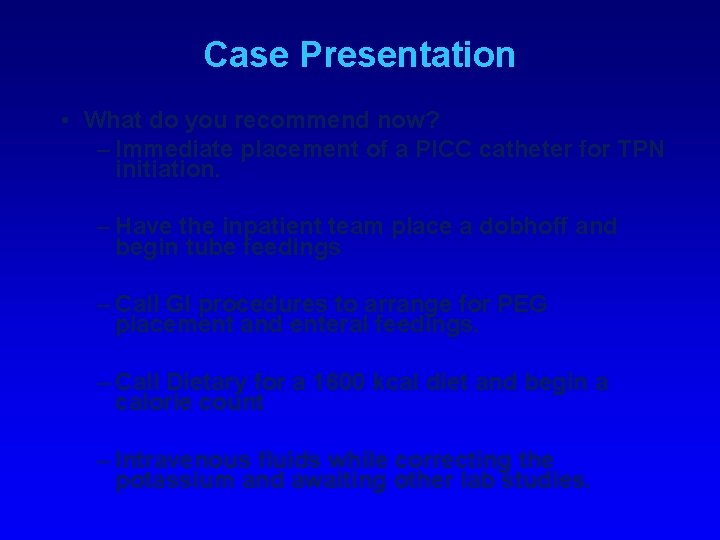
Case Presentation • What do you recommend now? – Immediate placement of a PICC catheter for TPN initiation. – Have the inpatient team place a dobhoff and begin tube feedings – Call GI procedures to arrange for PEG placement and enteral feedings. – Call Dietary for a 1600 kcal diet and begin a calorie count – Intravenous fluids while correcting the potassium and awaiting other lab studies.
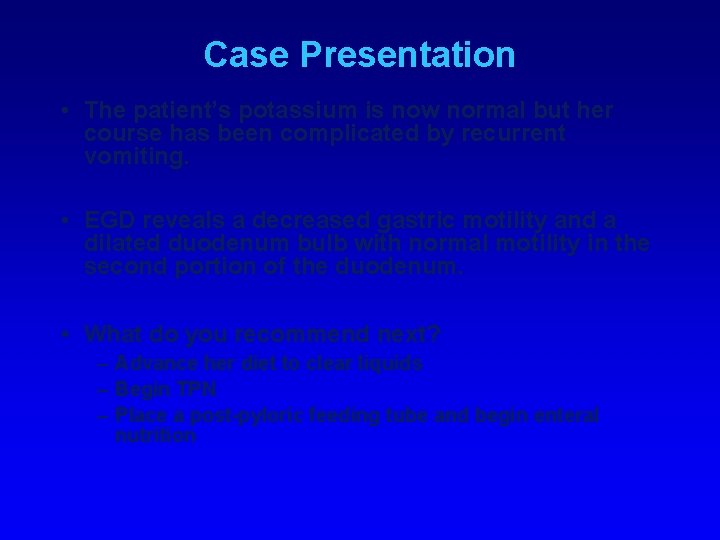
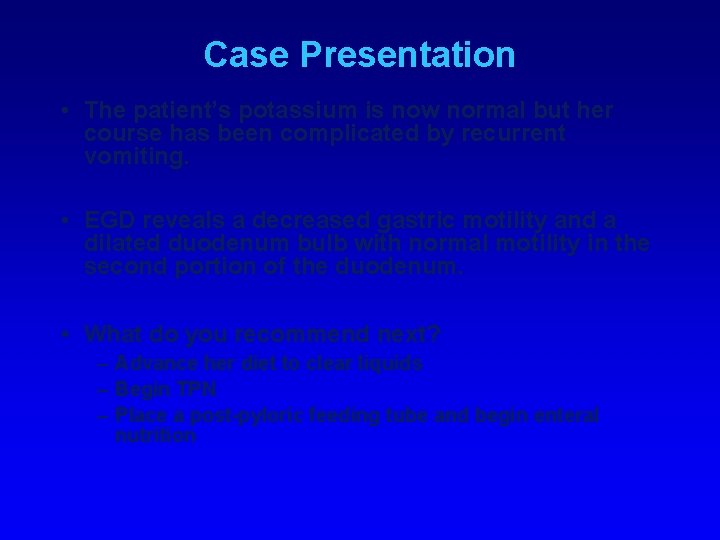
Case Presentation • The patient’s potassium is now normal but her course has been complicated by recurrent vomiting. • EGD reveals a decreased gastric motility and a dilated duodenum bulb with normal motility in the second portion of the duodenum. • What do you recommend next? – Advance her diet to clear liquids – Begin TPN – Place a post-pyloric feeding tube and begin enteral nutrition
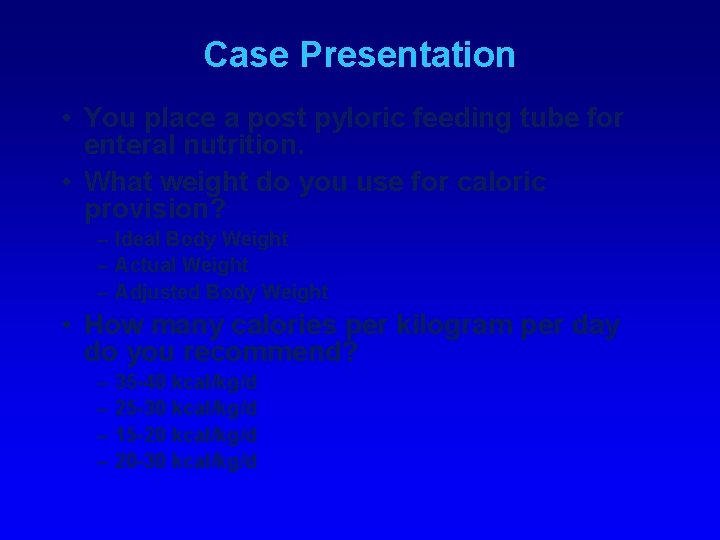
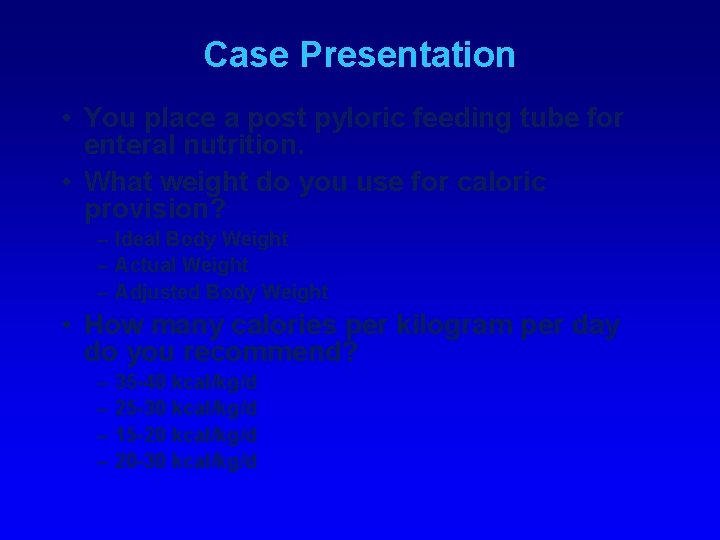
Case Presentation • You place a post pyloric feeding tube for enteral nutrition. • What weight do you use for caloric provision? – Ideal Body Weight – Actual Weight – Adjusted Body Weight • How many calories per kilogram per day do you recommend? – – 35 -40 kcal/kg/d 25 -30 kcal/kg/d 15 -20 kcal/kg/d 20 -30 kcal/kg/d
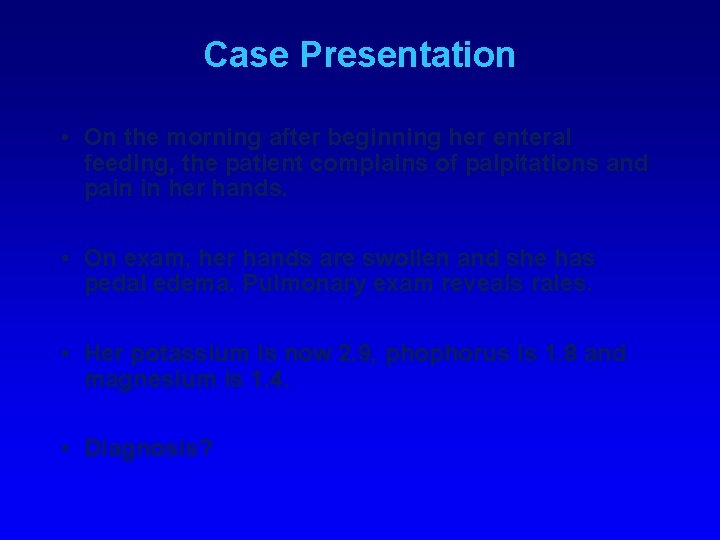
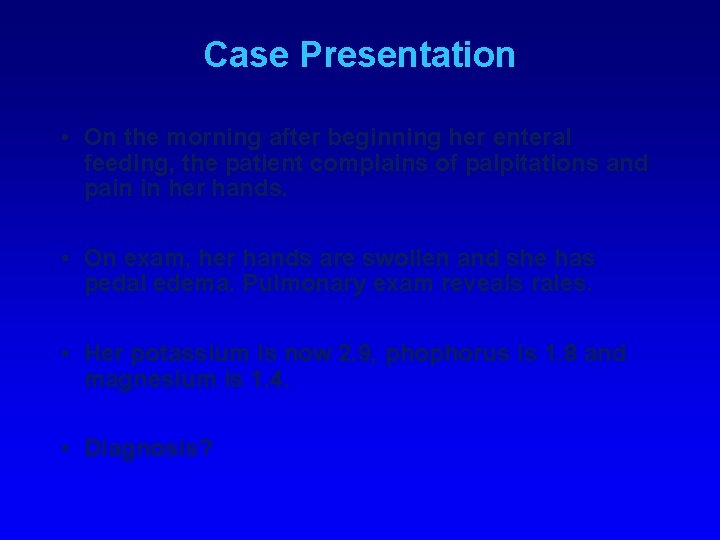
Case Presentation • On the morning after beginning her enteral feeding, the patient complains of palpitations and pain in her hands. • On exam, her hands are swollen and she has pedal edema. Pulmonary exam reveals rales. • Her potassium is now 2. 9, phophorus is 1. 8 and magnesium is 1. 4. • Diagnosis?
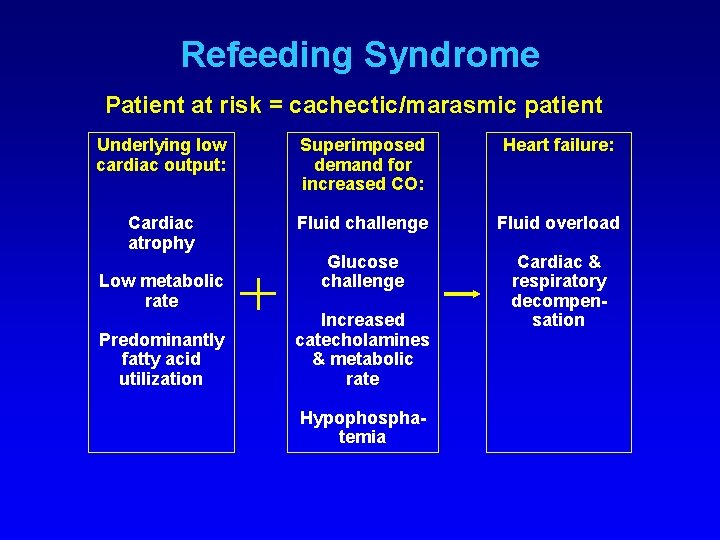
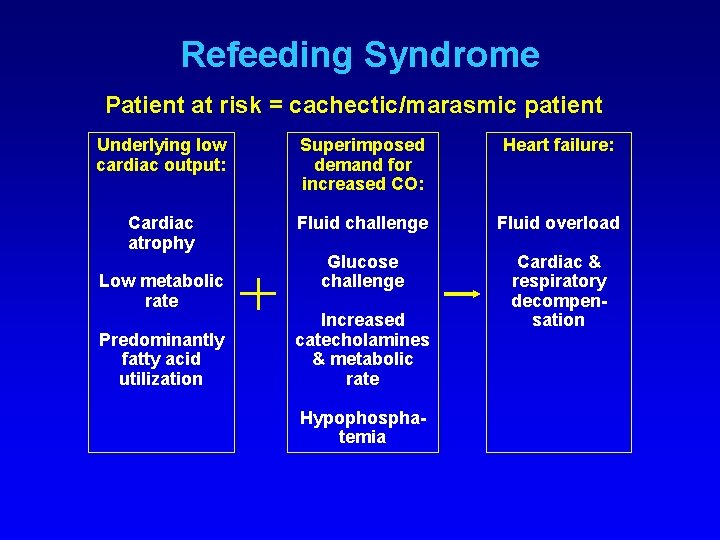
Refeeding Syndrome Patient at risk = cachectic/marasmic patient Underlying low cardiac output: Superimposed demand for increased CO: Heart failure: Cardiac atrophy Fluid challenge Fluid overload Glucose challenge Cardiac & respiratory decompensation Low metabolic rate Predominantly fatty acid utilization Increased catecholamines & metabolic rate Hypophosphatemia
Case Presentation • The patient is admitted to inpatient psychiatry for the treatment of anorexia/bulimia nervosa. • After 4 weeks on tube feedings, she was successfully transitioned to oral diet. • At discharge, her weight was 99 pounds.
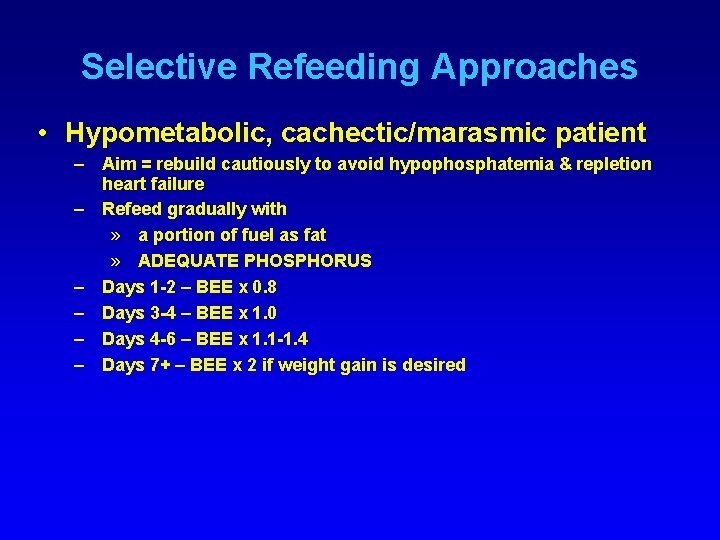
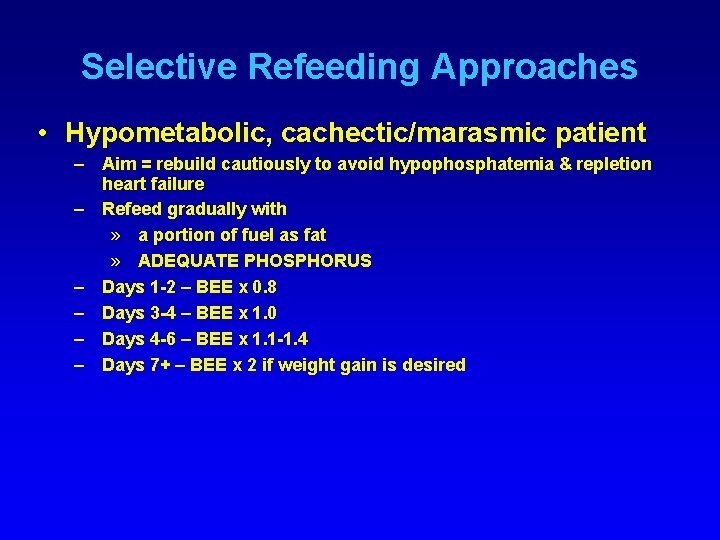
Selective Refeeding Approaches • Hypometabolic, cachectic/marasmic patient – Aim = rebuild cautiously to avoid hypophosphatemia & repletion heart failure – Refeed gradually with » a portion of fuel as fat » ADEQUATE PHOSPHORUS – Days 1 -2 – BEE x 0. 8 – Days 3 -4 – BEE x 1. 0 – Days 4 -6 – BEE x 1. 1 -1. 4 – Days 7+ – BEE x 2 if weight gain is desired
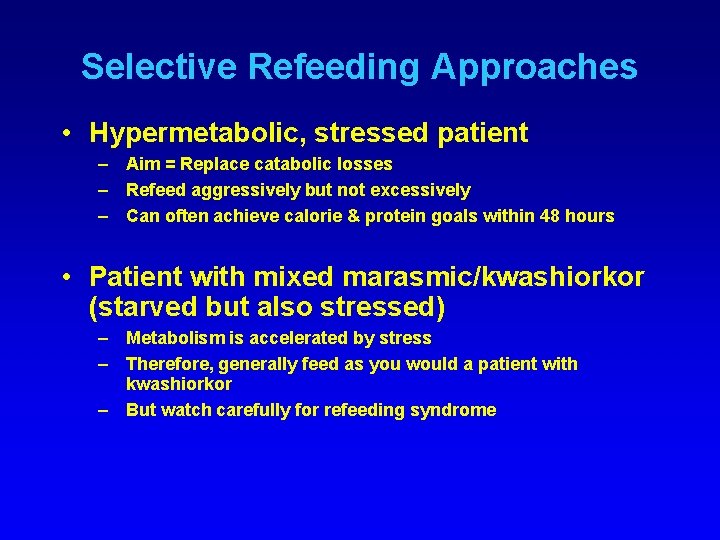
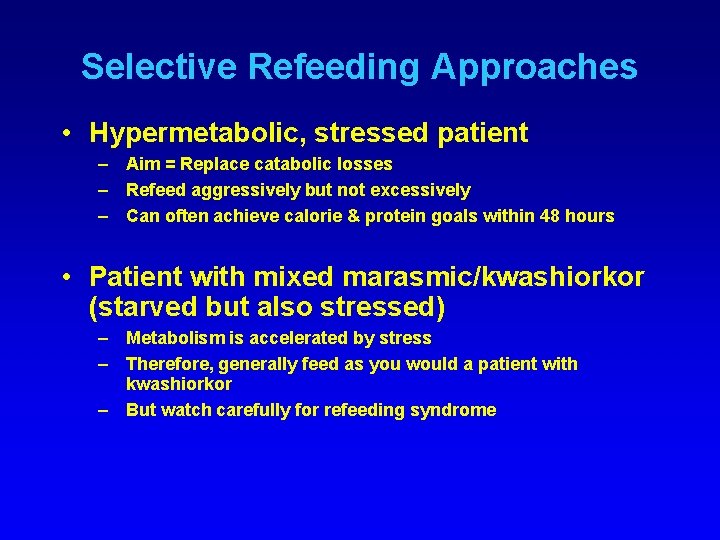
Selective Refeeding Approaches • Hypermetabolic, stressed patient – Aim = Replace catabolic losses – Refeed aggressively but not excessively – Can often achieve calorie & protein goals within 48 hours • Patient with mixed marasmic/kwashiorkor (starved but also stressed) – Metabolism is accelerated by stress – Therefore, generally feed as you would a patient with kwashiorkor – But watch carefully for refeeding syndrome
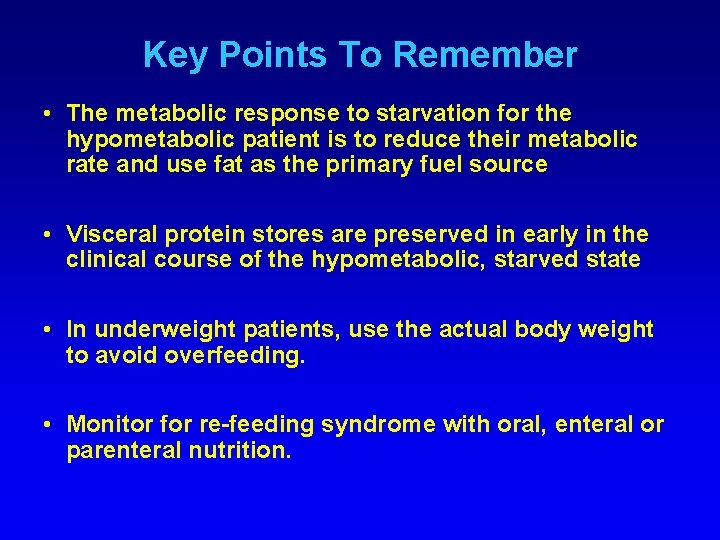
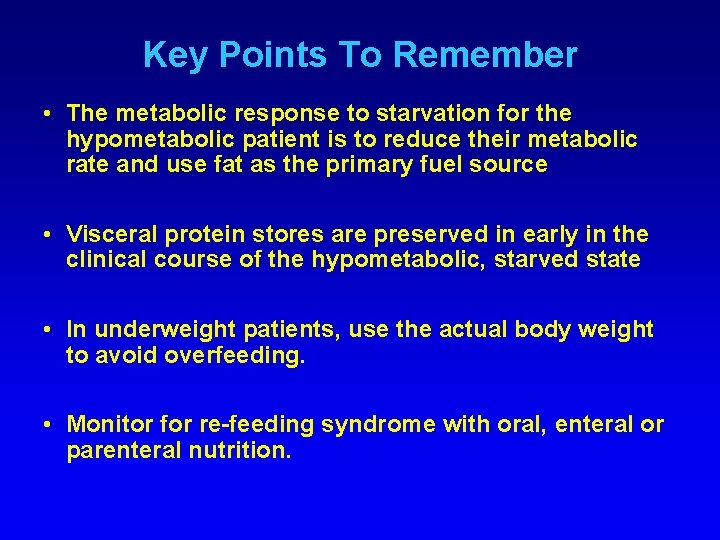
Key Points To Remember • The metabolic response to starvation for the hypometabolic patient is to reduce their metabolic rate and use fat as the primary fuel source • Visceral protein stores are preserved in early in the clinical course of the hypometabolic, starved state • In underweight patients, use the actual body weight to avoid overfeeding. • Monitor for re-feeding syndrome with oral, enteral or parenteral nutrition.
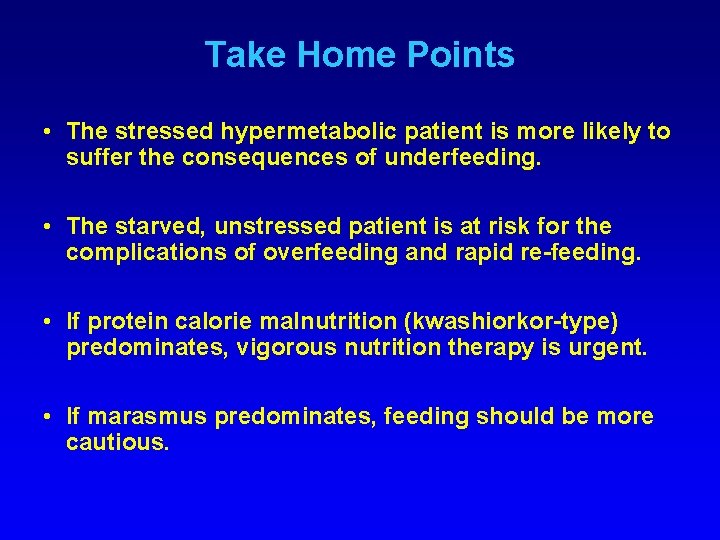
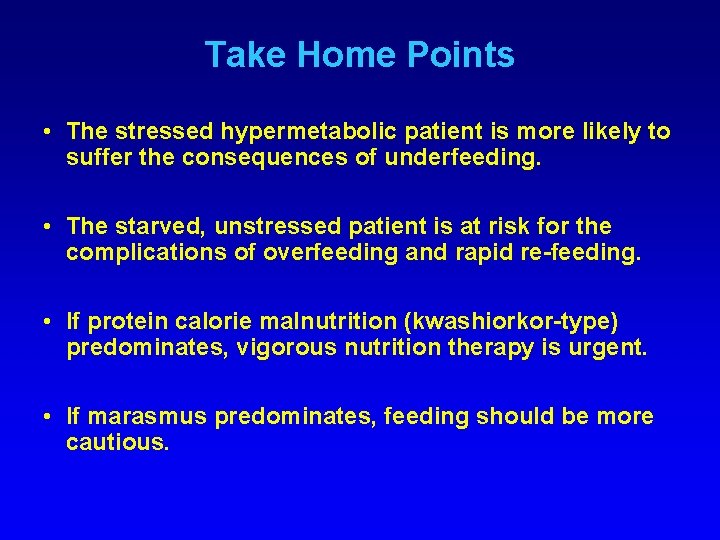
Take Home Points • The stressed hypermetabolic patient is more likely to suffer the consequences of underfeeding. • The starved, unstressed patient is at risk for the complications of overfeeding and rapid re-feeding. • If protein calorie malnutrition (kwashiorkor-type) predominates, vigorous nutrition therapy is urgent. • If marasmus predominates, feeding should be more cautious.
 Anorexia cachexia palliative care
Anorexia cachexia palliative care Benign and malignant tumor
Benign and malignant tumor Cachexia vs marasmus
Cachexia vs marasmus Lesson 6 anorexia nervosa and bulimia
Lesson 6 anorexia nervosa and bulimia Patient 2 patient
Patient 2 patient Anorexia nervosa long term effects
Anorexia nervosa long term effects Excessive acid production
Excessive acid production Anorexia and bulimia venn diagram
Anorexia and bulimia venn diagram Anorexia palliative care
Anorexia palliative care Winona ryder anorexia
Winona ryder anorexia Psychodynamic explanation of anorexia
Psychodynamic explanation of anorexia Case study on anorexia nervosa
Case study on anorexia nervosa Symtom anorexia
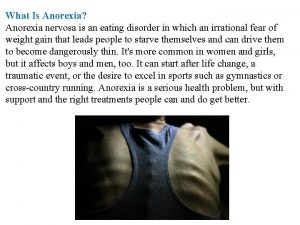
Symtom anorexia Anorexia nervosa ppt
Anorexia nervosa ppt Social learning theory anorexia
Social learning theory anorexia Bulimia vs anorexia usmle
Bulimia vs anorexia usmle Dominique anorexia
Dominique anorexia Definition of bullimia
Definition of bullimia Historia natural de la enfermedad de la anorexia
Historia natural de la enfermedad de la anorexia Cid de bulimia
Cid de bulimia Health consequences of anorexia
Health consequences of anorexia Obesidad
Obesidad