New Paradigms for the Prevention of Cardiovascular Disease






- Slides: 65
New Paradigms for the Prevention of Cardiovascular Disease Tara Dall, MD Advanced Lipidology Delafield, Wisconsin Assistant Clinical Professor Medical College of WI Diplomate, American Board of Clinical Lipidology www. advlip. com
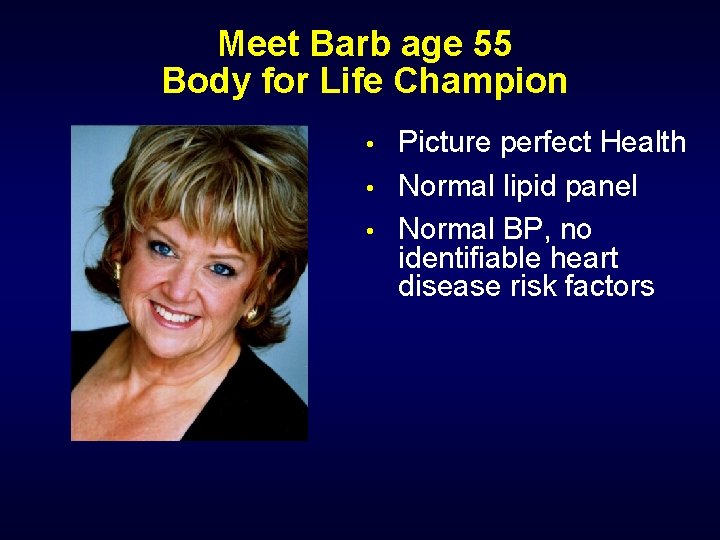
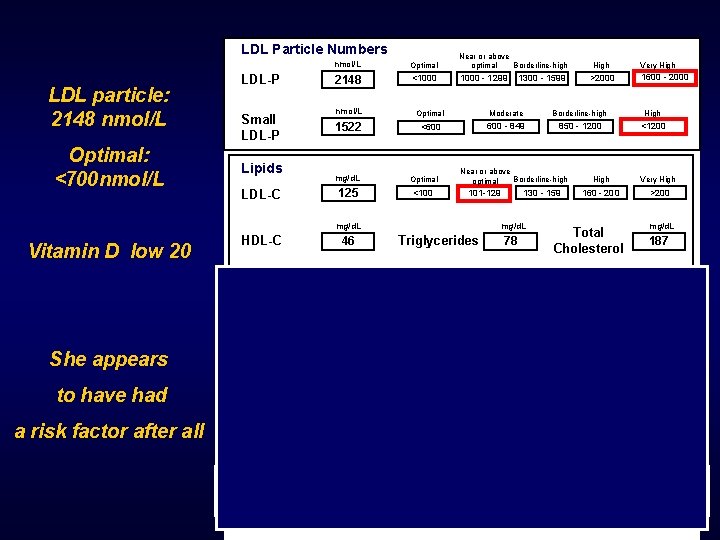
Meet Barb age 55 Body for Life Champion • • • Picture perfect Health Normal lipid panel Normal BP, no identifiable heart disease risk factors
Barb Suffered a Massive Heart Attack at age 59 • • But she had “Normal Cholesterol”, Normal BP, no traditional heart disease risk factors Was there any additional testing that would have identified her as high risk?
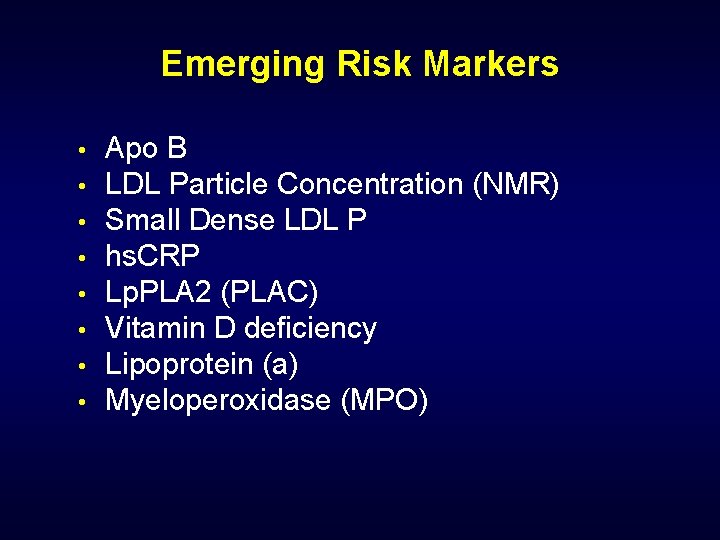
Emerging Risk Markers • • Apo B LDL Particle Concentration (NMR) Small Dense LDL P hs. CRP Lp. PLA 2 (PLAC) Vitamin D deficiency Lipoprotein (a) Myeloperoxidase (MPO)
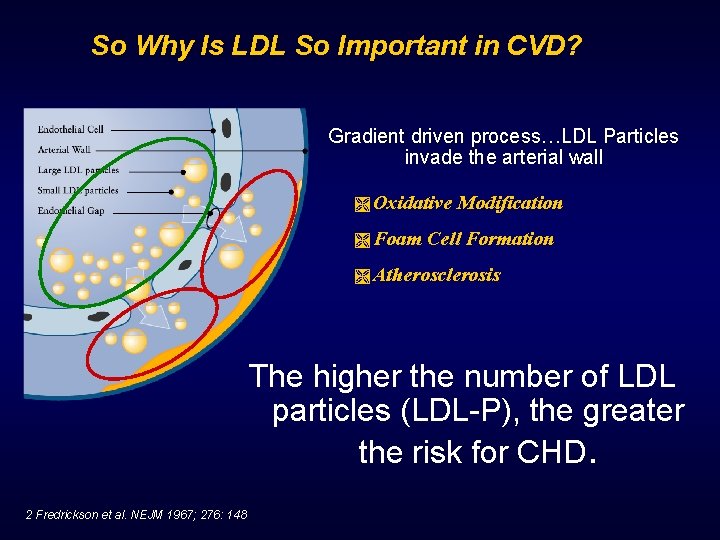
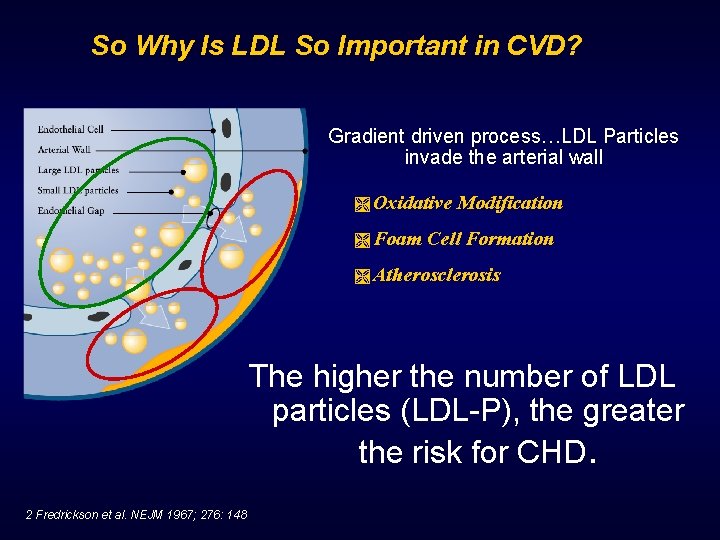
So Why Is LDL So Important in CVD? Gradient driven process…LDL Particles invade the arterial wall Ì Oxidative Ì Foam Modification Cell Formation Ì Atherosclerosis The higher the number of LDL particles (LDL-P), the greater the risk for CHD. 2 Fredrickson et al. NEJM 1967; 276: 148
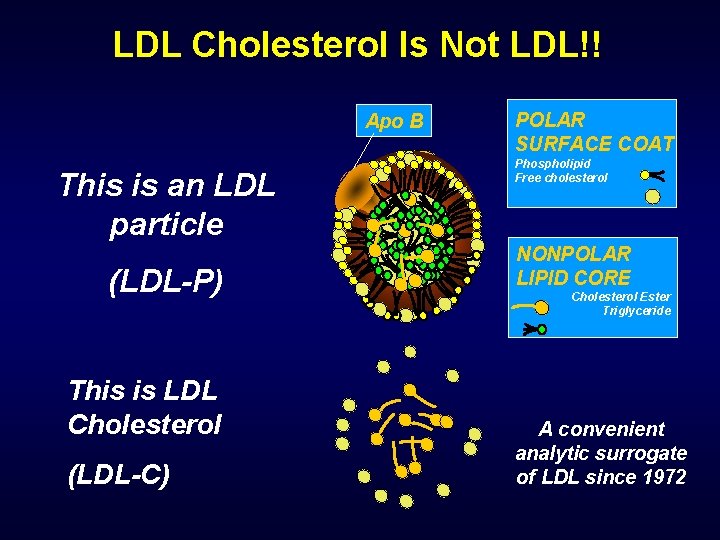
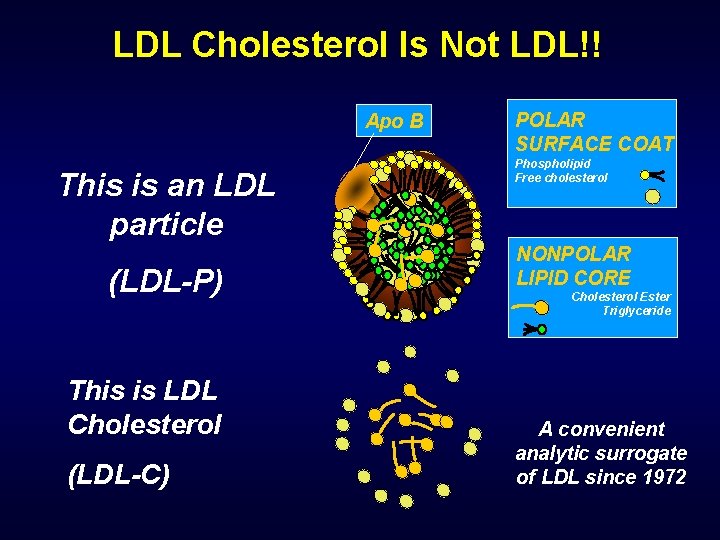
LDL Cholesterol Is Not LDL!! Apo B This is an LDL particle (LDL-P) This is LDL Cholesterol (LDL-C) POLAR SURFACE COAT Phospholipid Free cholesterol NONPOLAR LIPID CORE Cholesterol Ester Triglyceride A convenient analytic surrogate of LDL since 1972
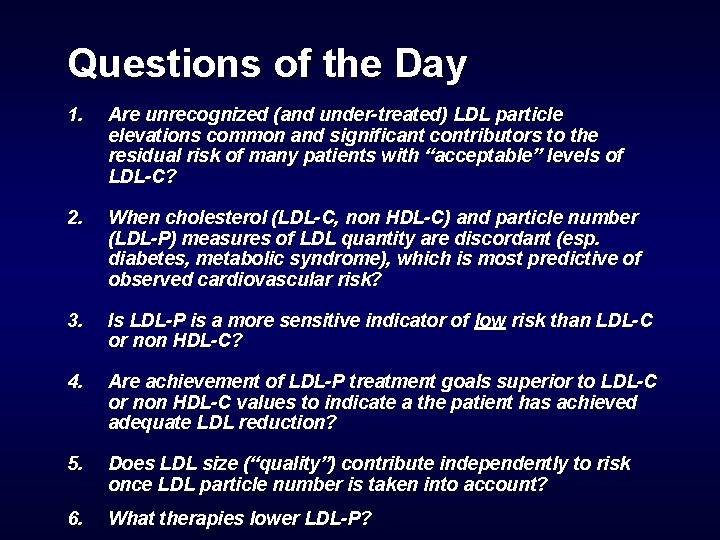
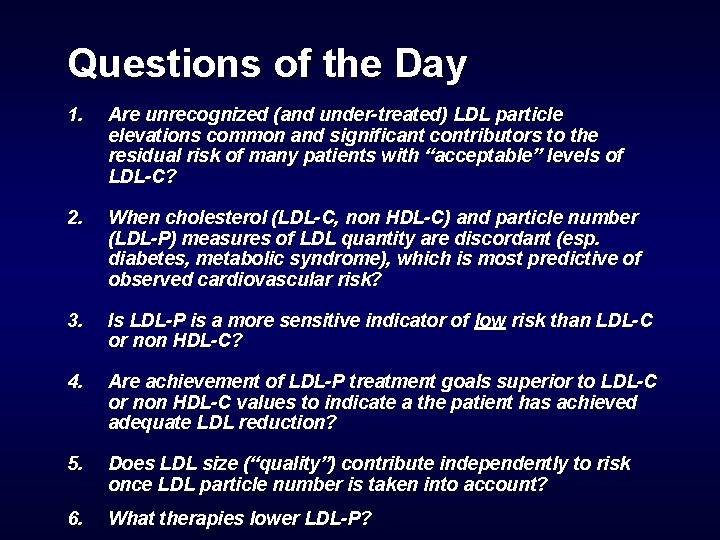
Questions of the Day 1. Are unrecognized (and under-treated) LDL particle elevations common and significant contributors to the residual risk of many patients with “acceptable” levels of LDL-C? 2. When cholesterol (LDL-C, non HDL-C) and particle number (LDL-P) measures of LDL quantity are discordant (esp. diabetes, metabolic syndrome), which is most predictive of observed cardiovascular risk? 3. Is LDL-P is a more sensitive indicator of low risk than LDL-C or non HDL-C? 4. Are achievement of LDL-P treatment goals superior to LDL-C or non HDL-C values to indicate a the patient has achieved adequate LDL reduction? 5. Does LDL size (“quality”) contribute independently to risk once LDL particle number is taken into account? 6. What therapies lower LDL-P?
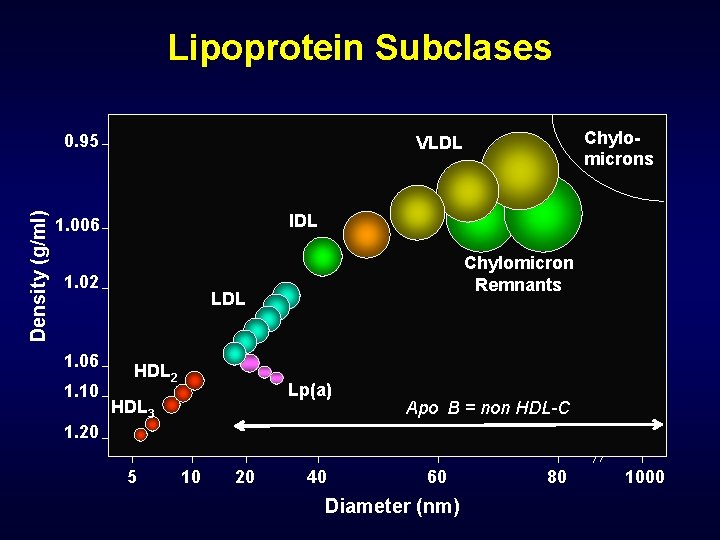
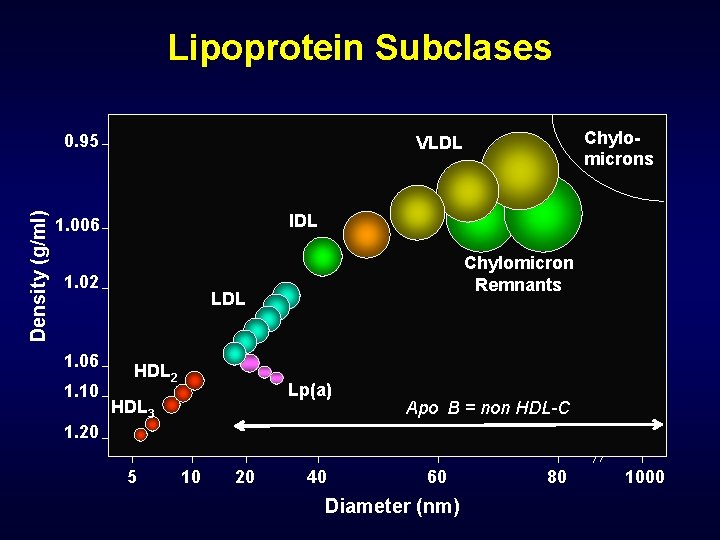
Lipoprotein Subclases Density (g/ml) 0. 95 IDL 1. 006 1. 02 1. 06 1. 10 Chylomicrons VLDL Chylomicron Remnants LDL HDL 2 Lp(a) HDL 3 Apo B = non HDL-C 1. 20 5 10 20 40 60 Diameter (nm) 80 1000
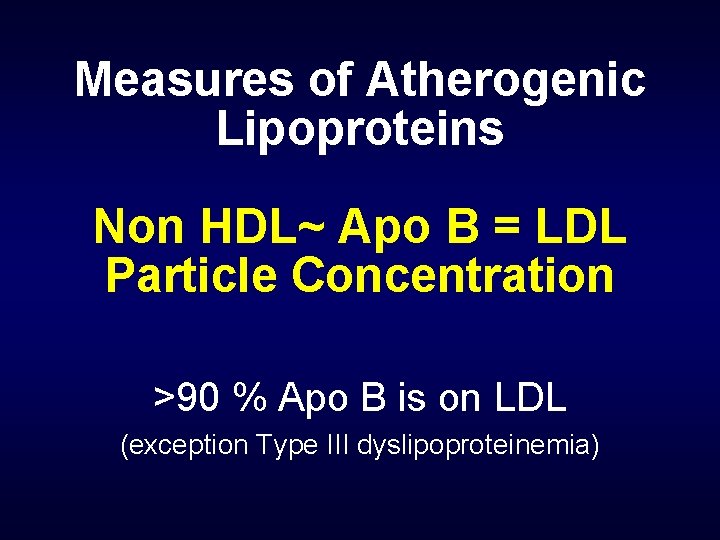
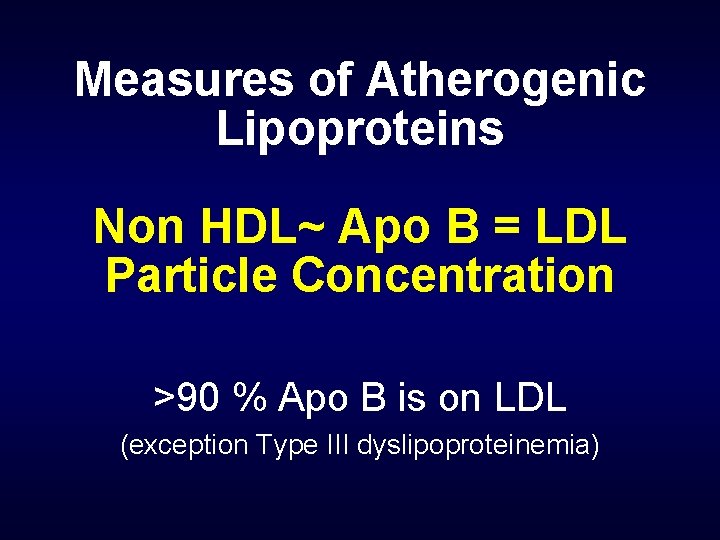
Measures of Atherogenic Lipoproteins Non HDL~ Apo B = LDL Particle Concentration >90 % Apo B is on LDL (exception Type III dyslipoproteinemia)
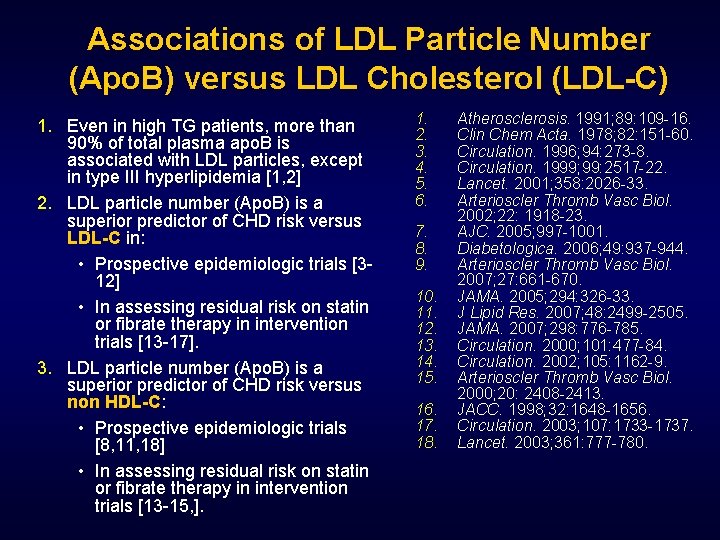
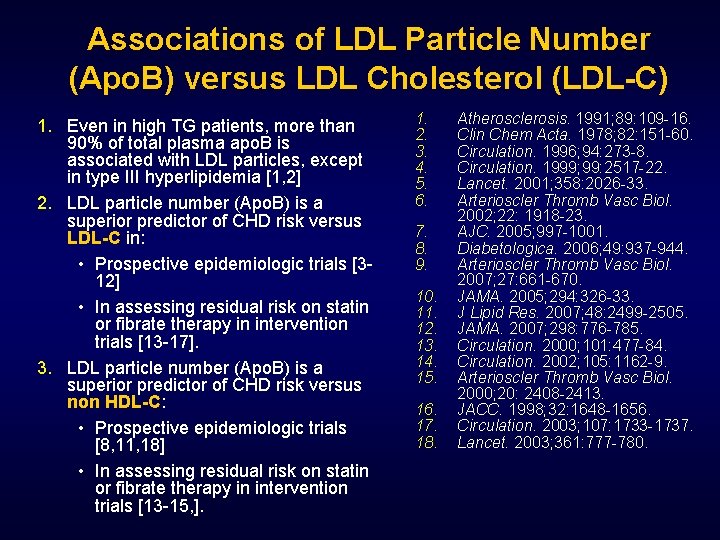
Associations of LDL Particle Number (Apo. B) versus LDL Cholesterol (LDL-C) 1. Even in high TG patients, more than 90% of total plasma apo. B is associated with LDL particles, except in type III hyperlipidemia [1, 2] 2. LDL particle number (Apo. B) is a superior predictor of CHD risk versus LDL-C in: • Prospective epidemiologic trials [312] • In assessing residual risk on statin or fibrate therapy in intervention trials [13 -17]. 3. LDL particle number (Apo. B) is a superior predictor of CHD risk versus non HDL-C: • Prospective epidemiologic trials [8, 11, 18] • In assessing residual risk on statin or fibrate therapy in intervention trials [13 -15, ]. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. Atherosclerosis. 1991; 89: 109 -16. Clin Chem Acta. 1978; 82: 151 -60. Circulation. 1996; 94: 273 -8. Circulation. 1999; 99: 2517 -22. Lancet. 2001; 358: 2026 -33. Arterioscler Thromb Vasc Biol. 2002; 22: 1918 -23. AJC. 2005; 997 -1001. Diabetologica. 2006; 49: 937 -944. Arterioscler Thromb Vasc Biol. 2007; 27: 661 -670. JAMA. 2005; 294: 326 -33. J Lipid Res. 2007; 48: 2499 -2505. JAMA. 2007; 298: 776 -785. Circulation. 2000; 101: 477 -84. Circulation. 2002; 105: 1162 -9. Arterioscler Thromb Vasc Biol. 2000; 20: 2408 -2413. JACC. 1998; 32: 1648 -1656. Circulation. 2003; 107: 1733 -1737. Lancet. 2003; 361: 777 -780.
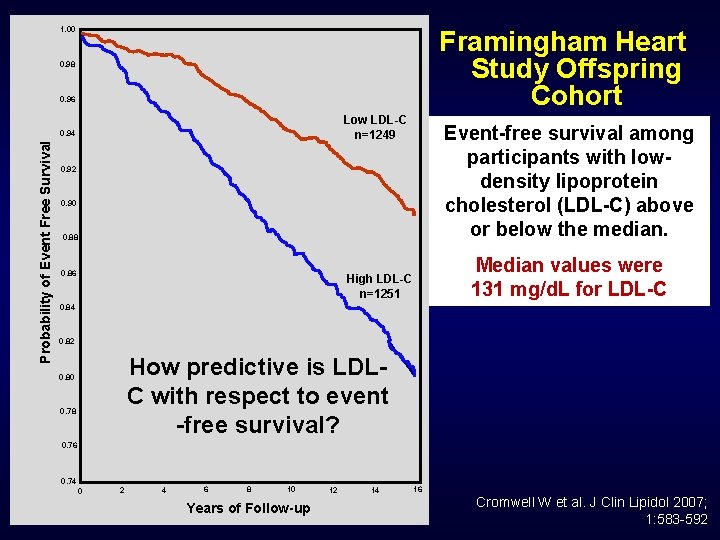
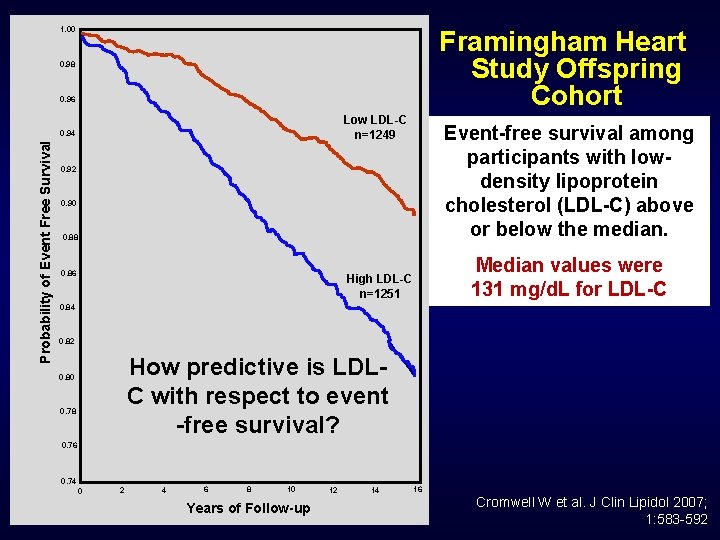
1. 00 Framingham Heart Study Offspring Cohort 0. 98 0. 96 Low LDL-C n=1249 Probability of Event Free Survival 0. 94 Event-free survival among participants with lowdensity lipoprotein cholesterol (LDL-C) above or below the median. 0. 92 0. 90 0. 88 0. 86 Median values were 131 mg/d. L for LDL-C High LDL-C n=1251 0. 84 0. 82 How predictive is LDLC with respect to event -free survival? 0. 80 0. 78 0. 76 0. 74 0 2 4 6 8 10 Years of Follow-up 12 14 16 Cromwell W et al. J Clin Lipidol 2007; 1: 583 -592
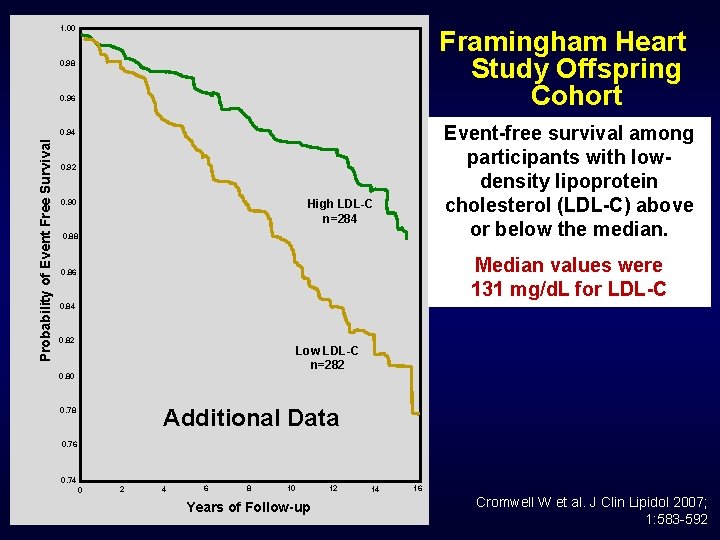
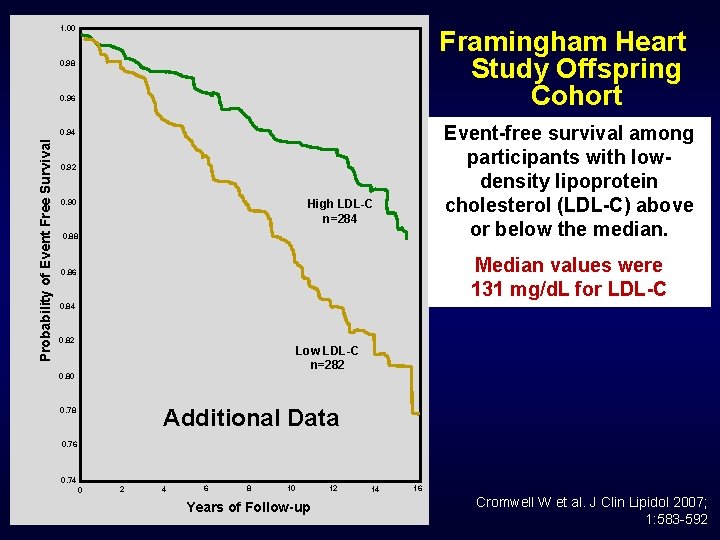
1. 00 Framingham Heart Study Offspring Cohort 0. 98 0. 96 Event-free survival among participants with lowdensity lipoprotein cholesterol (LDL-C) above or below the median. Probability of Event Free Survival 0. 94 0. 92 High LDL-C n=284 0. 90 0. 88 Median values were 131 mg/d. L for LDL-C 0. 86 0. 84 0. 82 Low LDL-C n=282 0. 80 Additional Data 0. 78 0. 76 0. 74 0 2 4 6 8 10 Years of Follow-up 12 14 16 Cromwell W et al. J Clin Lipidol 2007; 1: 583 -592
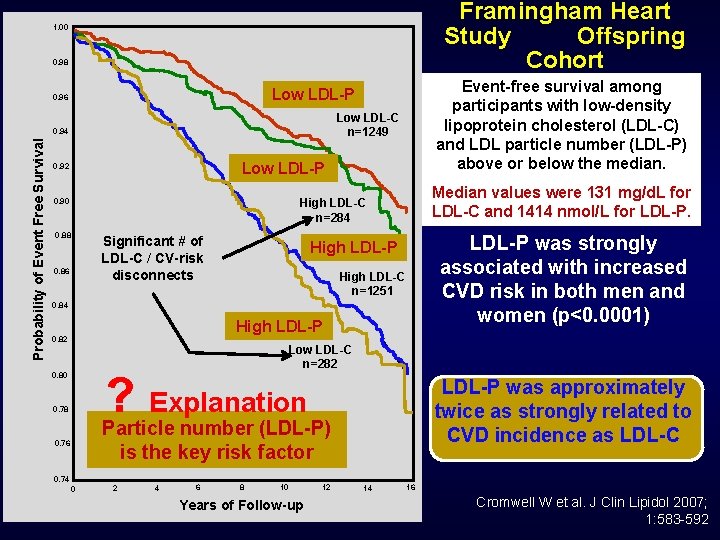
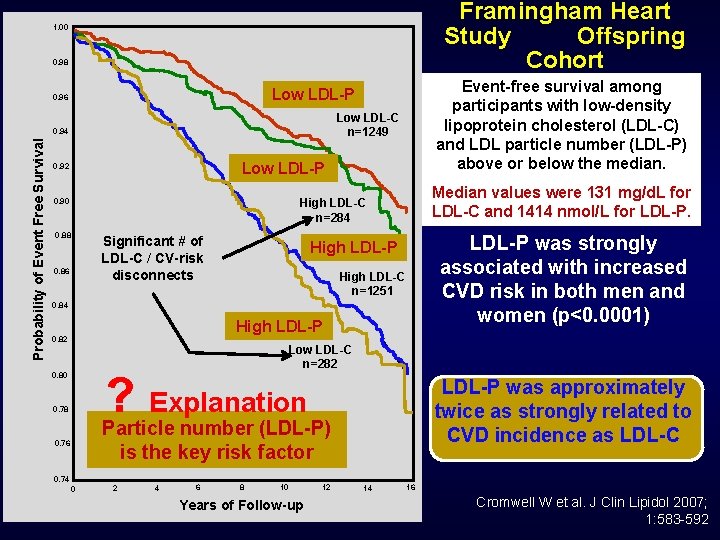
Framingham Heart Study Offspring Cohort 1. 00 0. 98 Low LDL-C n=1249 0. 94 Probability of Event Free Survival Event-free survival among participants with low-density lipoprotein cholesterol (LDL-C) and LDL particle number (LDL-P) above or below the median. Low LDL-P 0. 96 Low LDL-P 0. 92 Median values were 131 mg/d. L for LDL-C and 1414 nmol/L for LDL-P. High LDL-C n=284 0. 90 0. 88 0. 86 Significant # of LDL-C / CV-risk disconnects LDL-P was strongly associated with increased CVD risk in both men and women (p<0. 0001) High LDL-P High LDL-C n=1251 0. 84 High LDL-P 0. 82 Low LDL-C n=282 ? Explanation Particle number (LDL-P) 0. 80 0. 78 0. 76 LDL-P was approximately twice as strongly related to CVD incidence as LDL-C is the key risk factor 0. 74 0 2 4 6 8 10 Years of Follow-up 12 14 16 Cromwell W et al. J Clin Lipidol 2007; 1: 583 -592
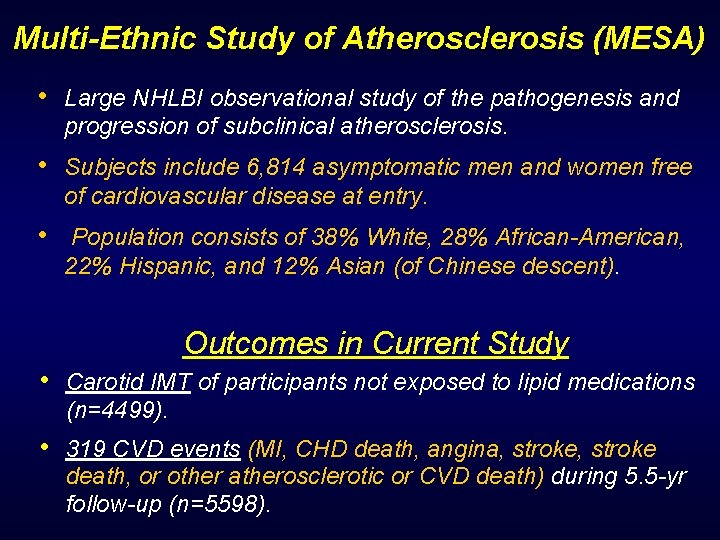
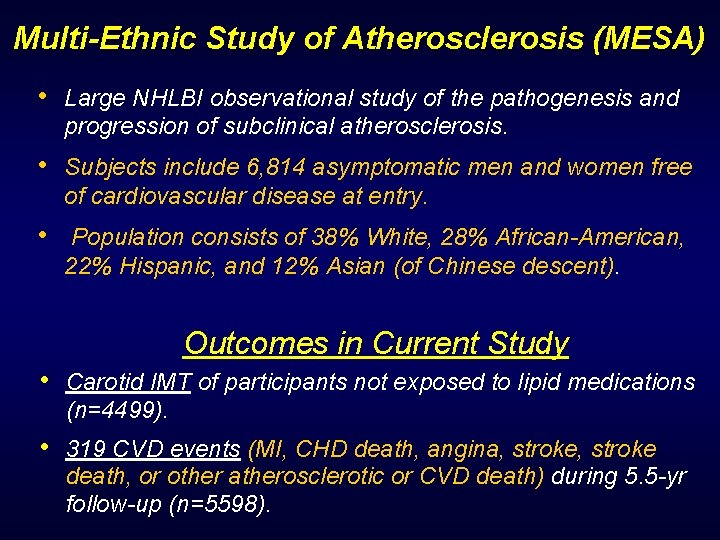
Multi-Ethnic Study of Atherosclerosis (MESA) • Large NHLBI observational study of the pathogenesis and progression of subclinical atherosclerosis. • Subjects include 6, 814 asymptomatic men and women free of cardiovascular disease at entry. • Population consists of 38% White, 28% African-American, 22% Hispanic, and 12% Asian (of Chinese descent). Outcomes in Current Study • Carotid IMT of participants not exposed to lipid medications (n=4499). • 319 CVD events (MI, CHD death, angina, stroke death, or other atherosclerotic or CVD death) during 5. 5 -yr follow-up (n=5598).
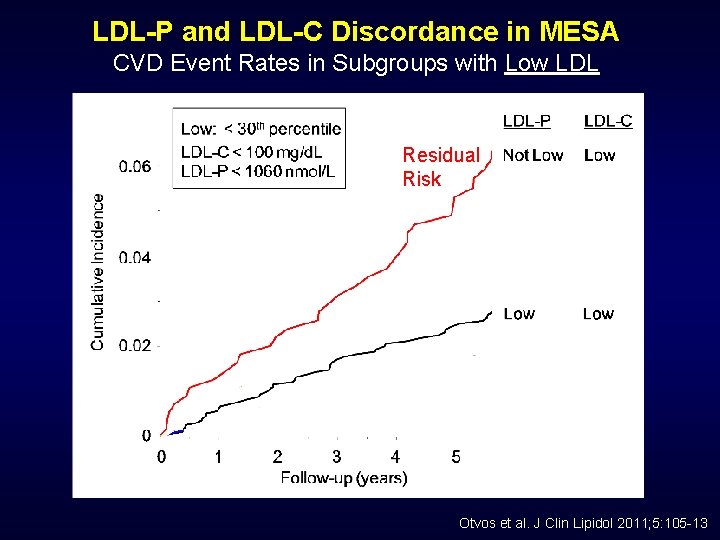
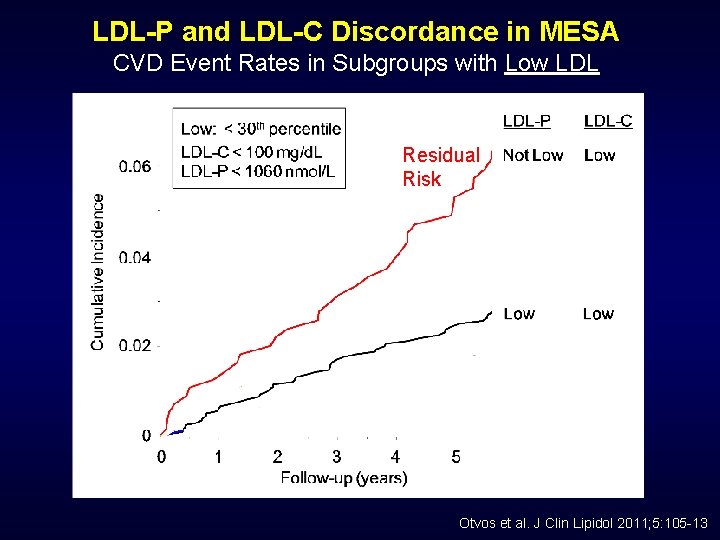
LDL-P and LDL-C Discordance in MESA CVD Event Rates in Subgroups with Low LDL Residual Risk Otvos et al. J Clin Lipidol 2011; 5: 105 -13
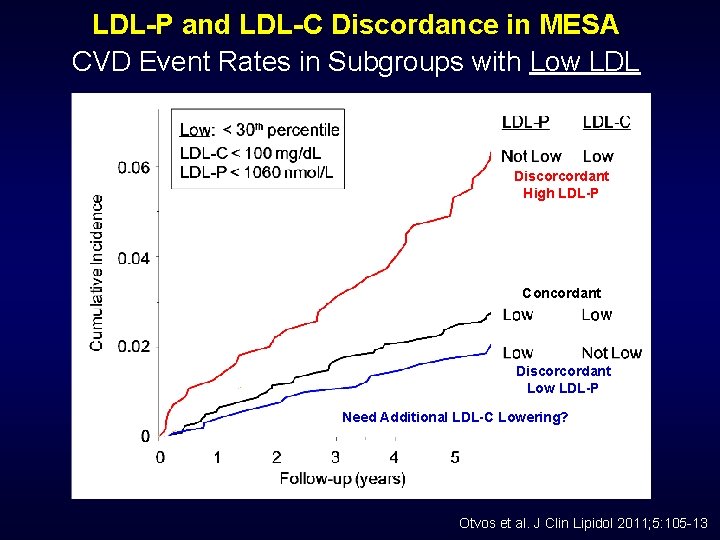
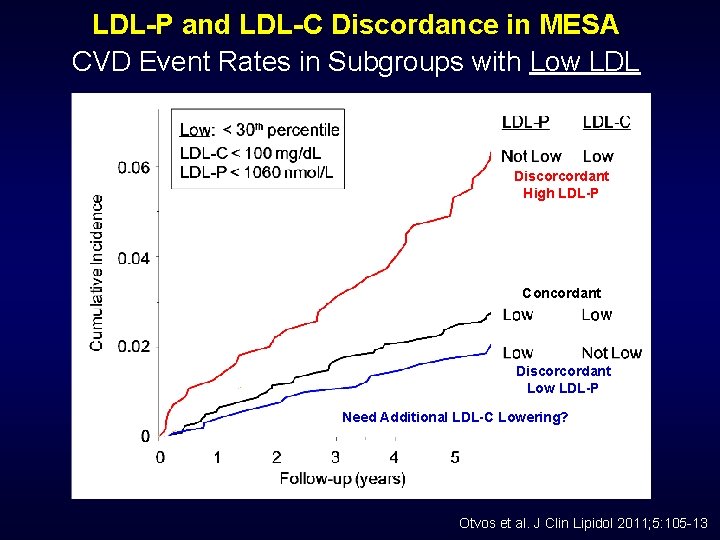
LDL-P and LDL-C Discordance in MESA CVD Event Rates in Subgroups with Low LDL Residual Risk Discorcordant High LDL-P Concordant Discorcordant Low LDL-P Need Additional LDL-C Lowering? Otvos et al. J Clin Lipidol 2011; 5: 105 -13
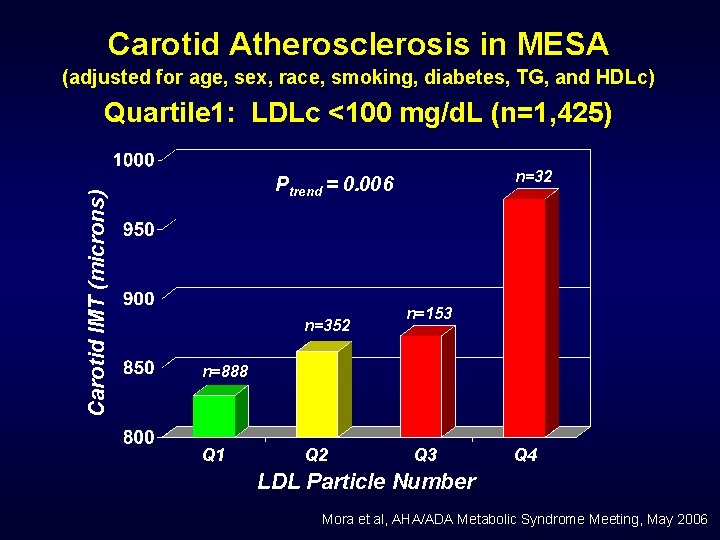
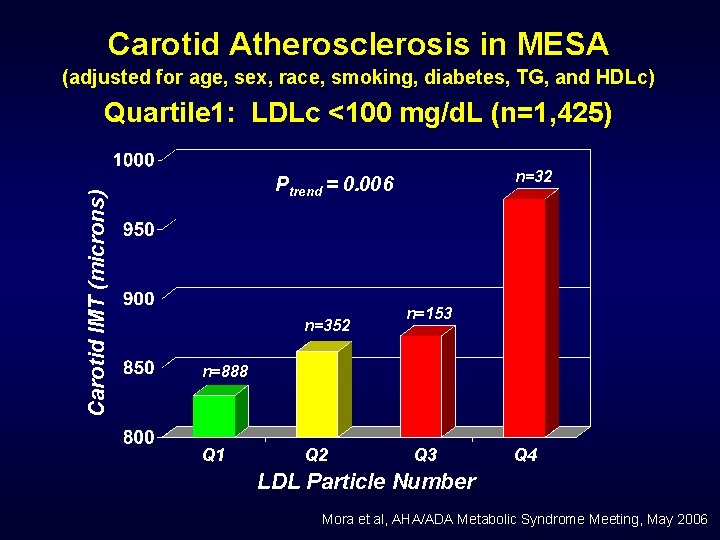
Carotid Atherosclerosis in MESA (adjusted for age, sex, race, smoking, diabetes, TG, and HDLc) Carotid IMT (microns) Quartile 1: LDLc <100 mg/d. L (n=1, 425) n=32 Ptrend = 0. 006 n=352 n=153 n=888 Q 1 Q 2 Q 3 Q 4 LDL Particle Number Mora et al, AHA/ADA Metabolic Syndrome Meeting, May 2006
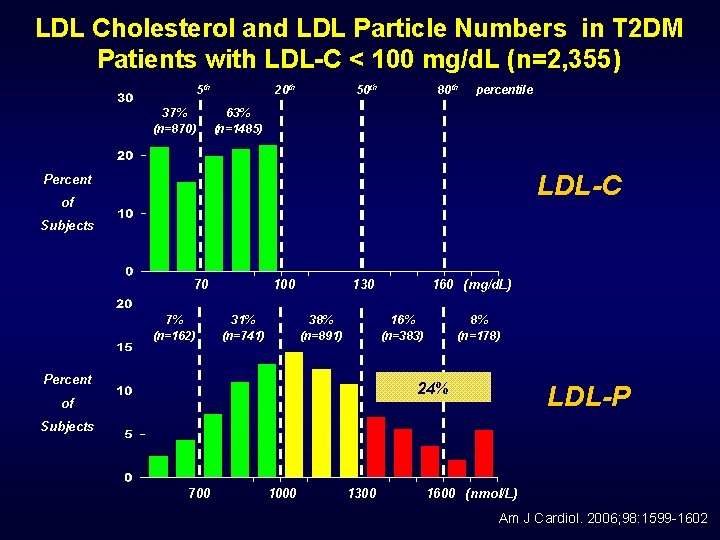
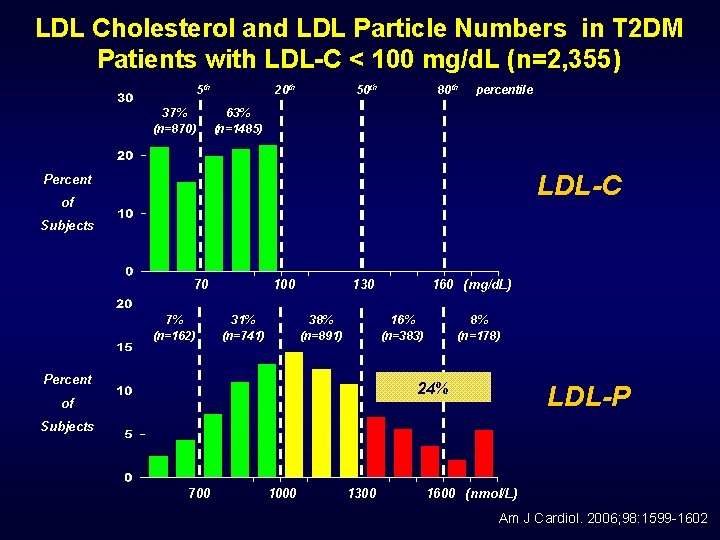
LDL Cholesterol and LDL Particle Numbers in T 2 DM Patients with LDL-C < 100 mg/d. L (n=2, 355) 5 th 37% (n=870) 20 th 50 th 80 th percentile 63% (n=1485) LDL-C Percent of Subjects 70 7% (n=162) 100 31% (n=741) 130 38% (n=891) 160 (mg/d. L) 16% (n=383) Percent 8% (n=178) 24% of LDL-P Subjects 700 1000 1300 1600 (nmol/L) Am J Cardiol. 2006; 98: 1599 -1602
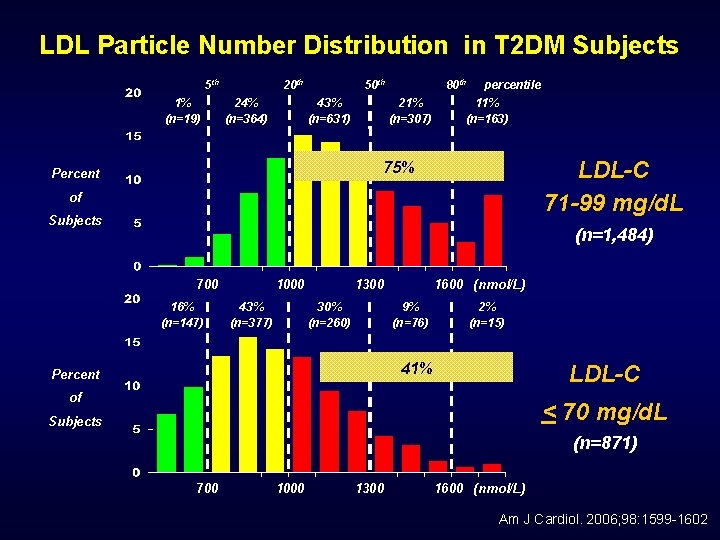
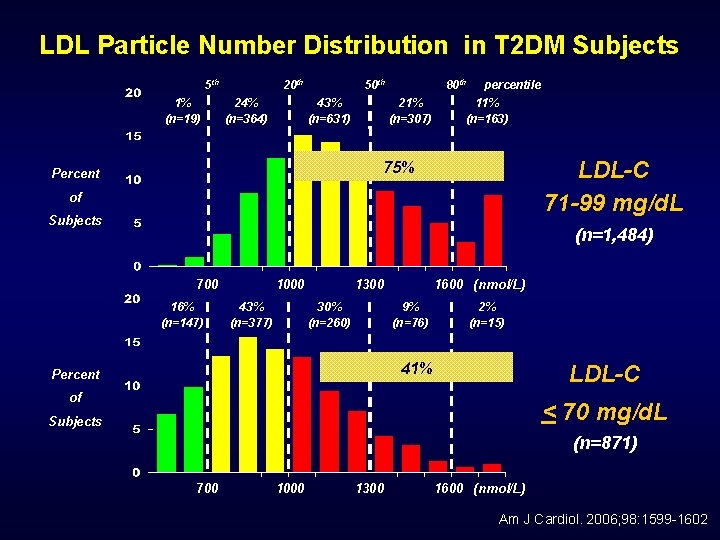
LDL Particle Number Distribution in T 2 DM Subjects 5 th 1% (n=19) 20 th 24% (n=364) 50 th 43% (n=631) 80 th 21% (n=307) percentile 11% (n=163) LDL-C 71 -99 mg/d. L 75% Percent of Subjects (n=1, 484) 700 16% (n=147) 1000 43% (n=377) 1300 30% (n=260) 1600 (nmol/L) 9% (n=76) 2% (n=15) 41% Percent LDL-C of < 70 mg/d. L Subjects (n=871) 700 1000 1300 1600 (nmol/L) Am J Cardiol. 2006; 98: 1599 -1602
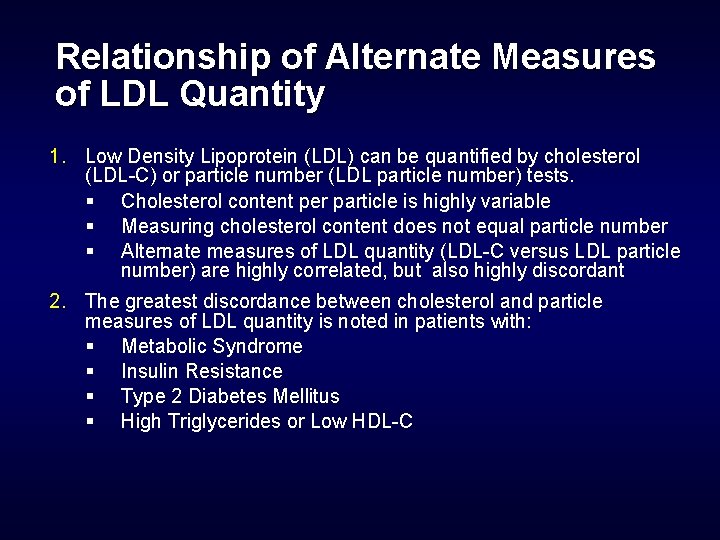
Relationship of Alternate Measures of LDL Quantity 1. Low Density Lipoprotein (LDL) can be quantified by cholesterol (LDL-C) or particle number (LDL particle number) tests. § Cholesterol content per particle is highly variable § Measuring cholesterol content does not equal particle number § Alternate measures of LDL quantity (LDL-C versus LDL particle number) are highly correlated, but also highly discordant 2. The greatest discordance between cholesterol and particle measures of LDL quantity is noted in patients with: § Metabolic Syndrome § Insulin Resistance § Type 2 Diabetes Mellitus § High Triglycerides or Low HDL-C
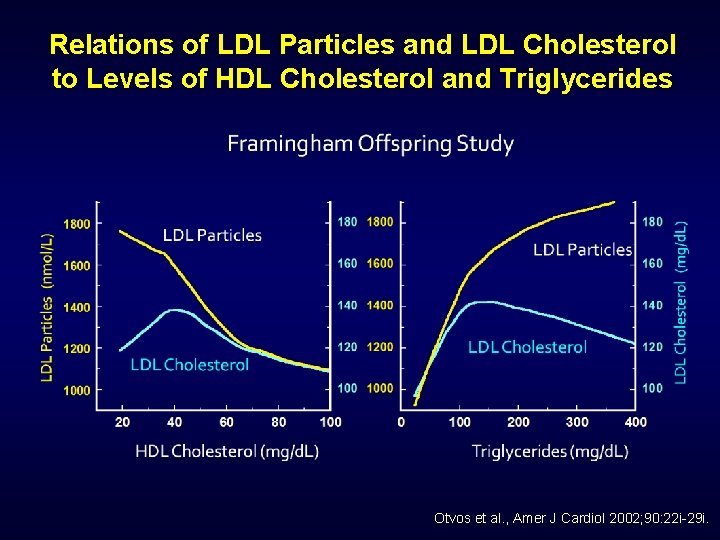
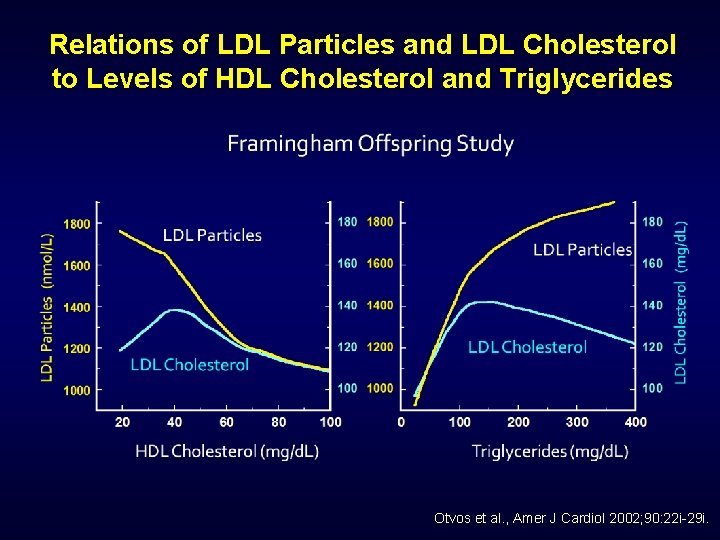
Relations of LDL Particles and LDL Cholesterol to Levels of HDL Cholesterol and Triglycerides Otvos et al. , Amer J Cardiol 2002; 90: 22 i-29 i.
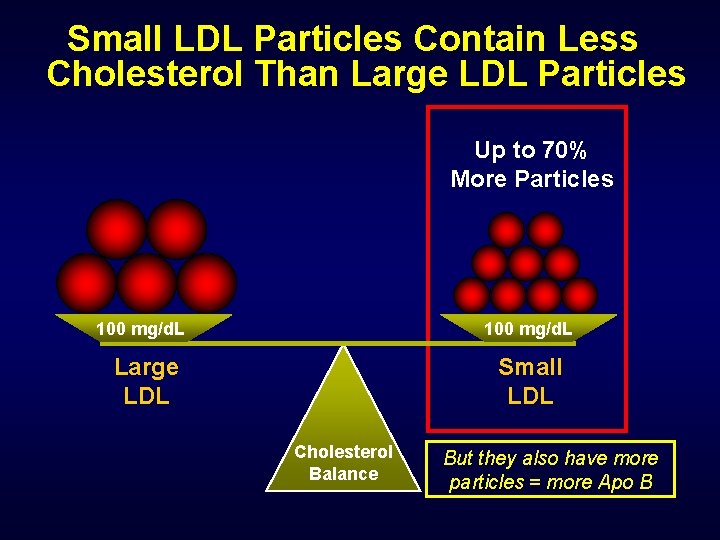
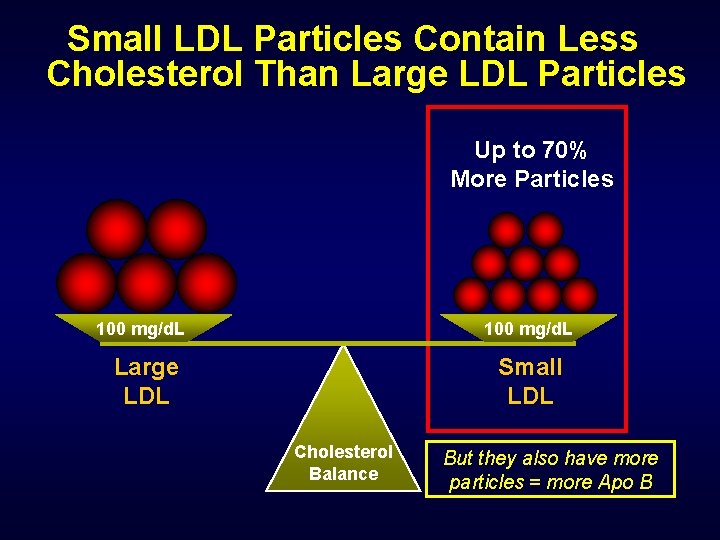
Small LDL Particles Contain Less Cholesterol Than Large LDL Particles Up to 70% More Particles 100 mg/d. L Large LDL Small LDL Cholesterol Balance But they also have more particles = more Apo B
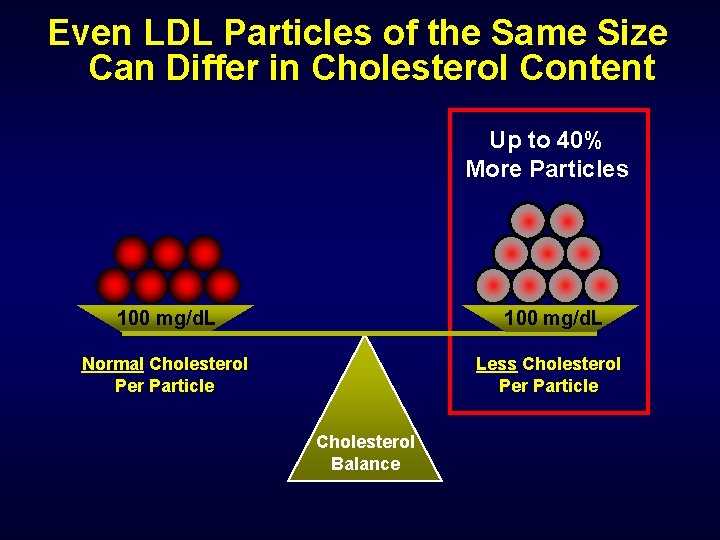
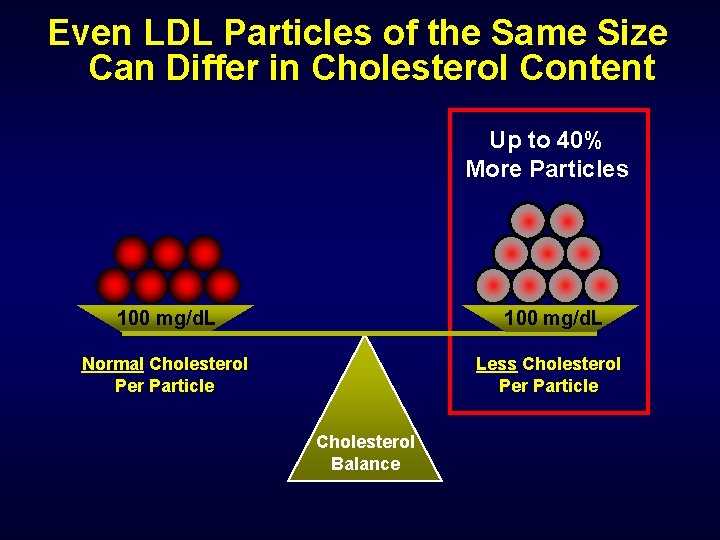
Even LDL Particles of the Same Size Can Differ in Cholesterol Content Up to 40% More Particles 100 mg/d. L Normal Cholesterol Per Particle Less Cholesterol Per Particle Cholesterol Balance
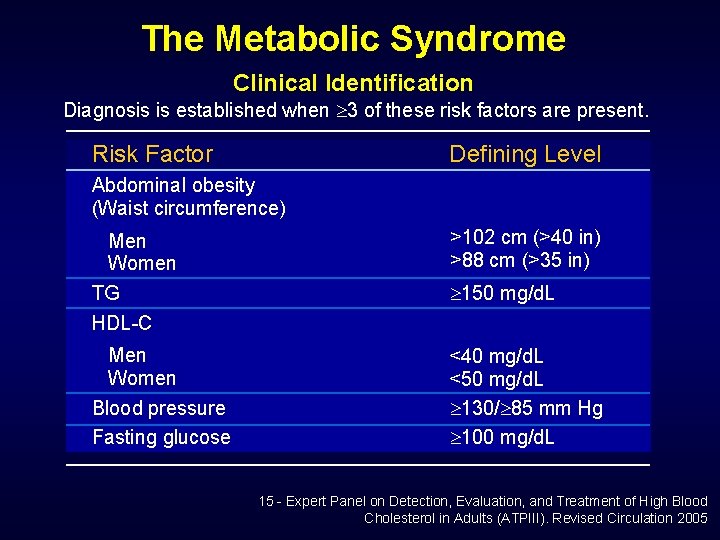
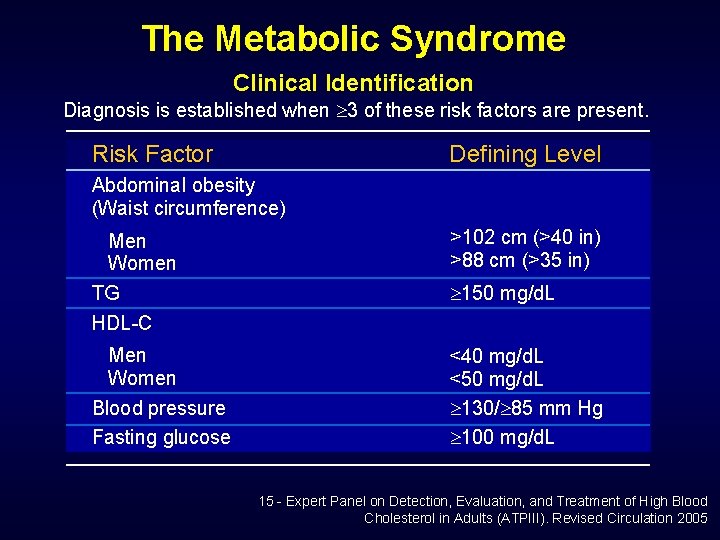
The Metabolic Syndrome Clinical Identification Diagnosis is established when 3 of these risk factors are present. Risk Factor Defining Level Abdominal obesity (Waist circumference) Men Women TG HDL-C >102 cm (>40 in) >88 cm (>35 in) Men Women Blood pressure Fasting glucose <40 mg/d. L <50 mg/d. L 130/ 85 mm Hg 100 mg/d. L 150 mg/d. L 15 - Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (ATPIII). Revised Circulation 2005
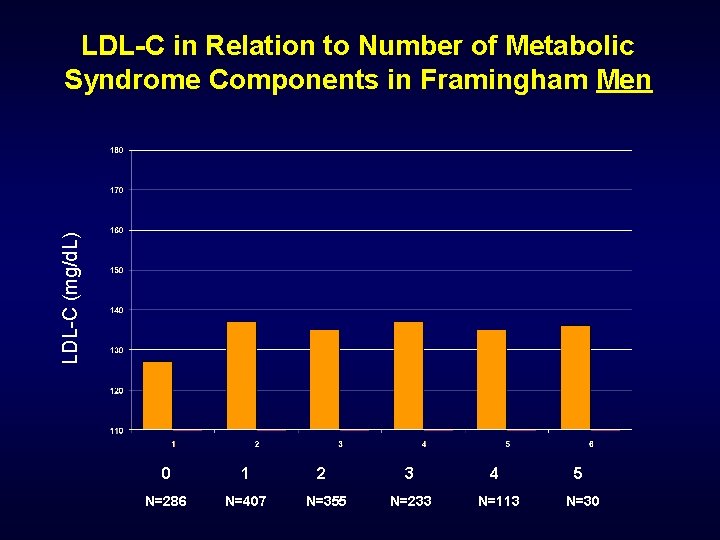
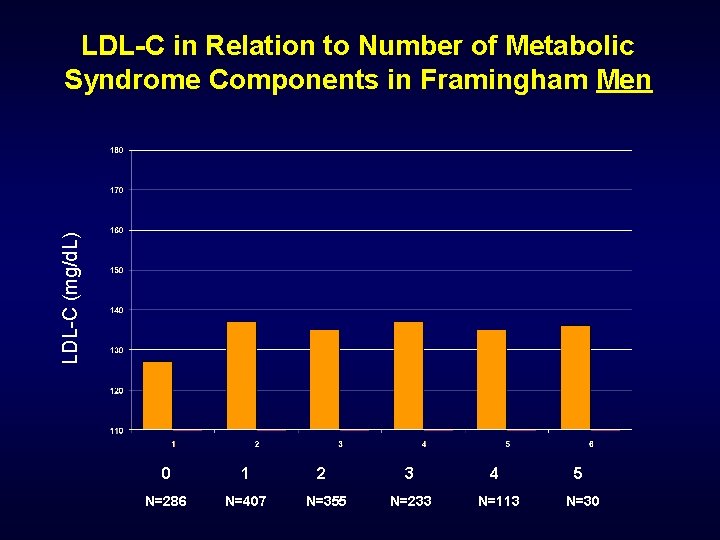
LDL-C (mg/d. L) LDL-C in Relation to Number of Metabolic Syndrome Components in Framingham Men 0 1 N=286 N=407 2 N=355 3 N=233 4 N=113 5 N=30
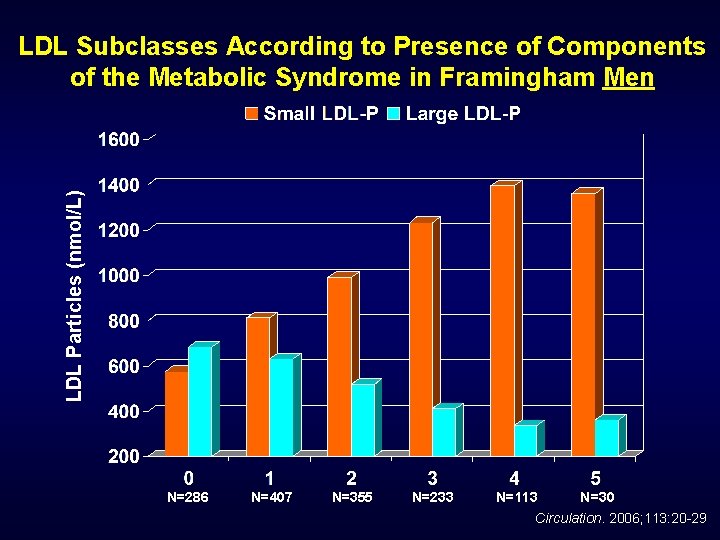
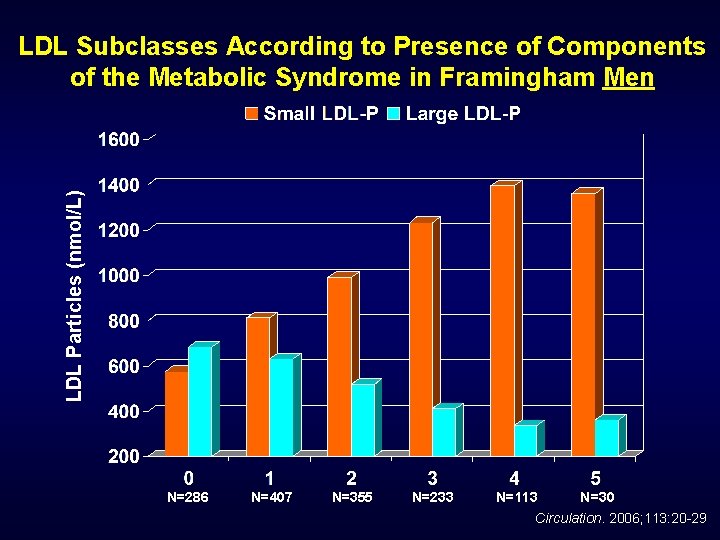
LDL Particles (nmol/L) LDL Subclasses According to Presence of Components of the Metabolic Syndrome in Framingham Men N=286 N=407 N=355 N=233 N=113 N=30 Circulation. 2006; 113: 20 -29
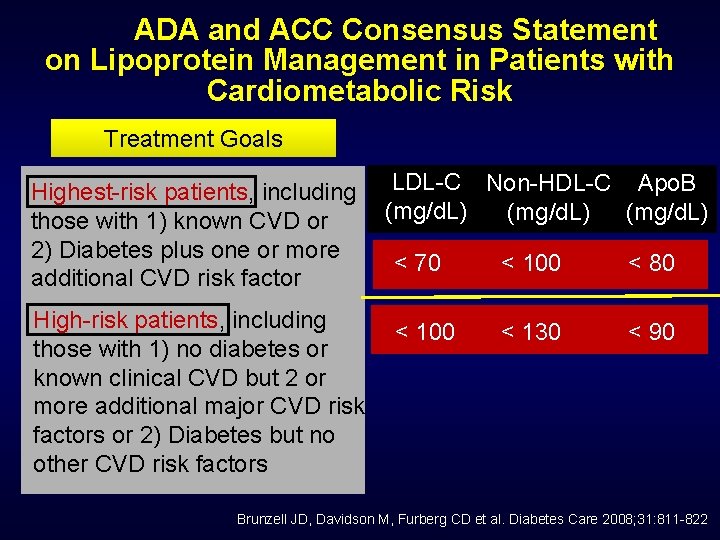
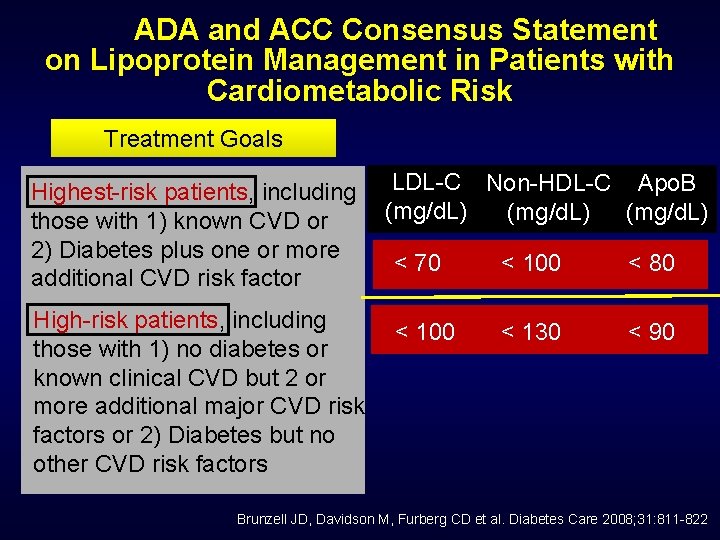
ADA and ACC Consensus Statement on Lipoprotein Management in Patients with Cardiometabolic Risk Treatment Goals Highest-risk patients, including those with 1) known CVD or 2) Diabetes plus one or more additional CVD risk factor High-risk patients, including those with 1) no diabetes or known clinical CVD but 2 or more additional major CVD risk factors or 2) Diabetes but no other CVD risk factors LDL-C Non-HDL-C Apo. B (mg/d. L) < 70 < 100 < 80 < 100 < 130 < 90 Brunzell JD, Davidson M, Furberg CD et al. Diabetes Care 2008; 31: 811 -822
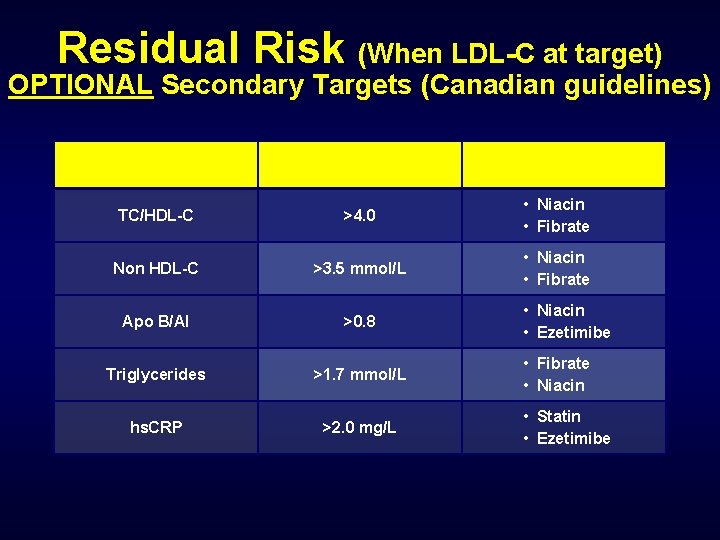
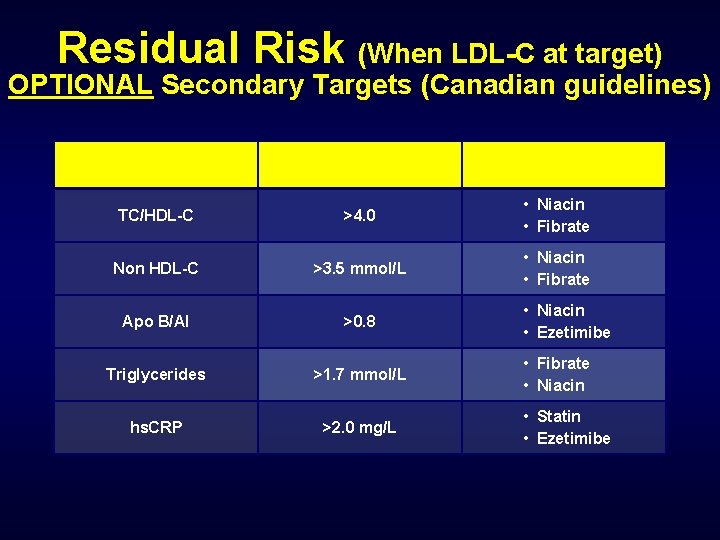
Residual Risk (When LDL-C at target) OPTIONAL Secondary Targets (Canadian guidelines) Test Cut-point Intervention TC/HDL-C >4. 0 • Niacin • Fibrate Non HDL-C >3. 5 mmol/L • Niacin • Fibrate Apo B/AI >0. 8 Triglycerides >1. 7 mmol/L hs. CRP >2. 0 mg/L • Niacin • Ezetimibe • Fibrate • Niacin • Statin • Ezetimibe
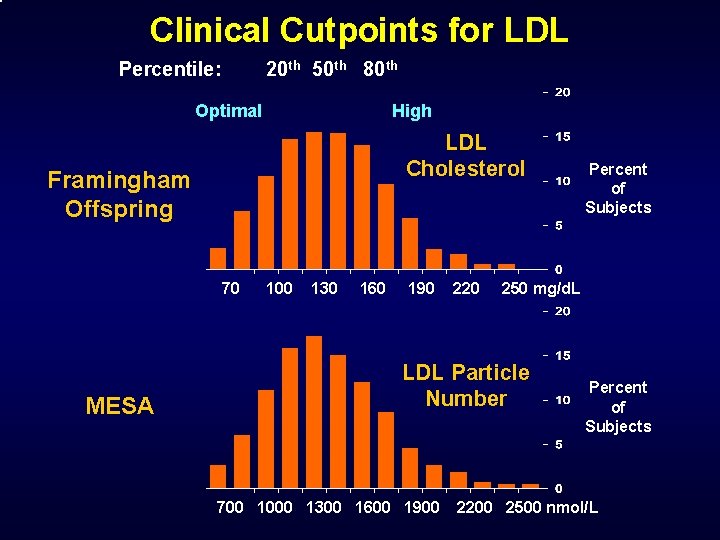
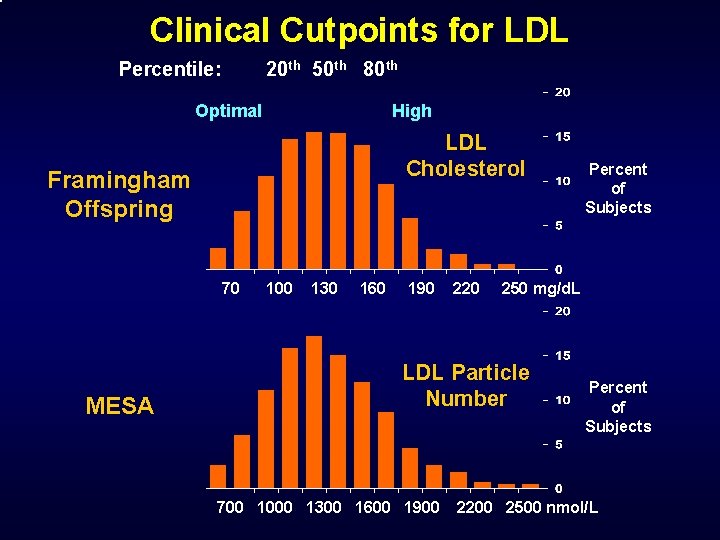
Clinical Cutpoints for LDL Percentile: 20 th 50 th 80 th Optimal High LDL Cholesterol Framingham Offspring 70 MESA 100 130 160 190 220 250 mg/d. L LDL Particle Number 700 1000 1300 1600 1900 Percent of Subjects 2200 2500 nmol/L

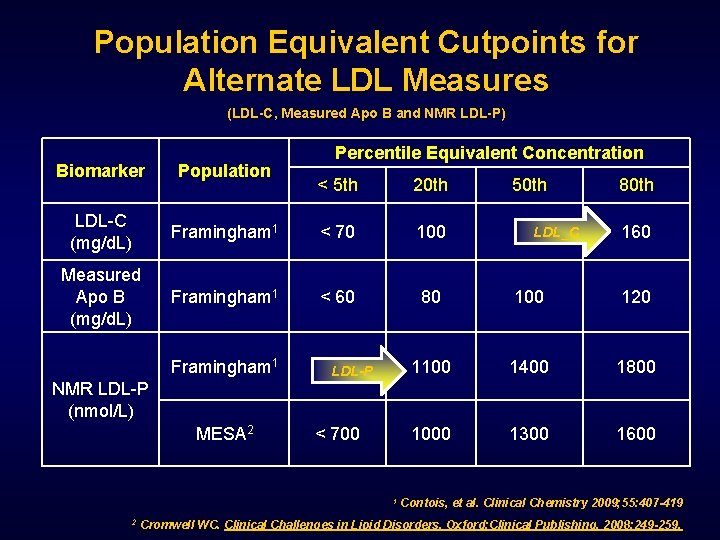
Population Equivalent Cutpoints for Alternate LDL Measures (LDL-C, Measured Apo B and NMR LDL-P) Biomarker Population LDL-C (mg/d. L) Measured Apo B (mg/d. L) Percentile Equivalent Concentration < 5 th 20 th 50 th 80 th Framingham 1 < 70 100 130 160 Framingham 1 < 60 80 100 120 Framingham 1 < 850 1100 1400 1800 MESA 2 < 700 1000 1300 1600 NMR LDL-P (nmol/L) 1 2 Contois, et al. Clinical Chemistry 2009; 55: 407 -419 Cromwell WC. Clinical Challenges in Lipid Disorders. Oxford: Clinical Publishing, 2008: 249 -259.
Clinical Application
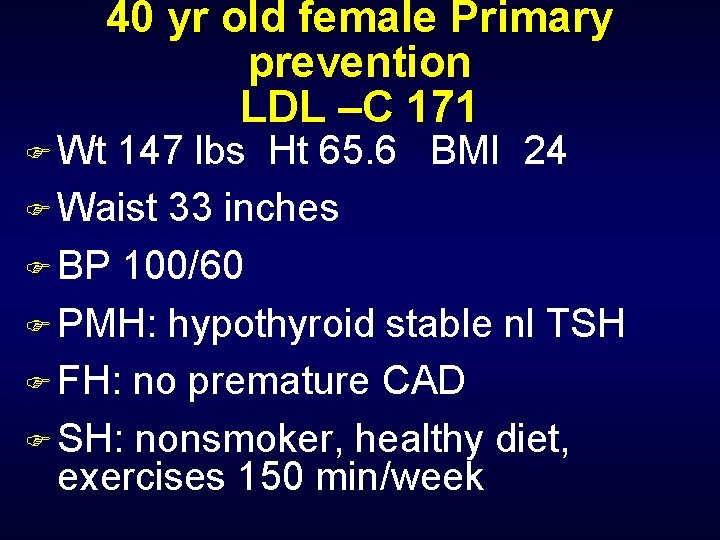
40 yr old female Primary prevention LDL –C 171 F Wt 147 lbs Ht 65. 6 BMI 24 F Waist 33 inches F BP 100/60 F PMH: hypothyroid stable nl TSH F FH: no premature CAD F SH: nonsmoker, healthy diet, exercises 150 min/week
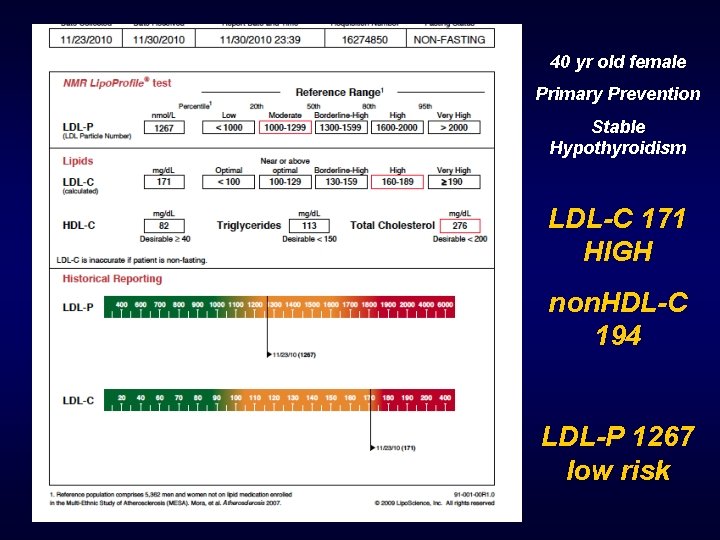
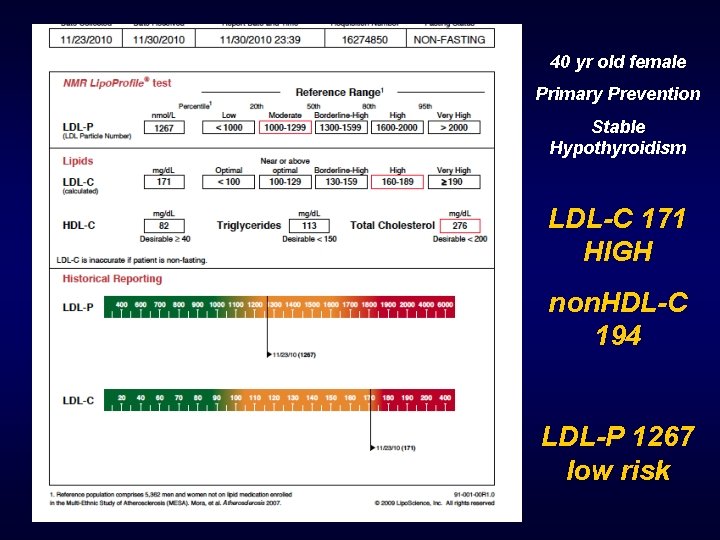
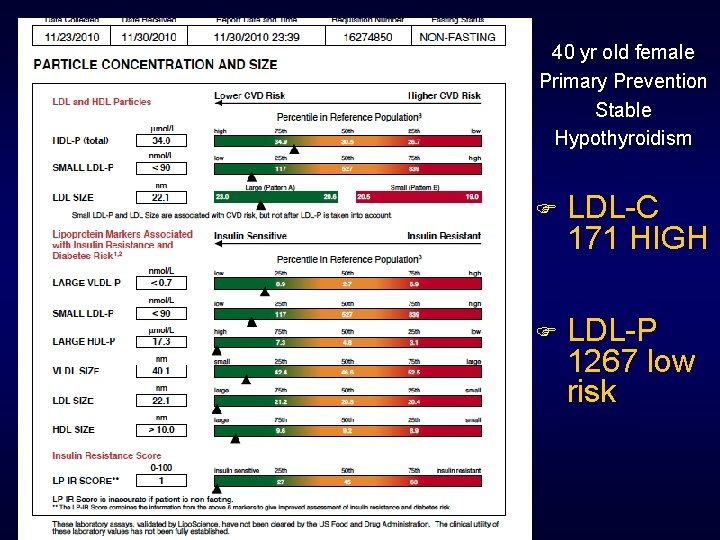
40 yr old female Primary Prevention Stable Hypothyroidism LDL-C 171 HIGH non. HDL-C 194 LDL-P 1267 low risk
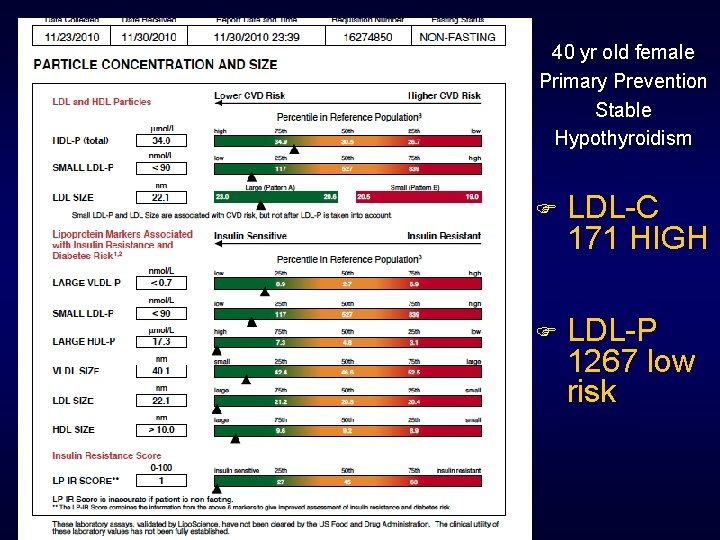
40 yr old female Primary Prevention Stable Hypothyroidism F LDL-C 171 HIGH F LDL-P 1267 low risk
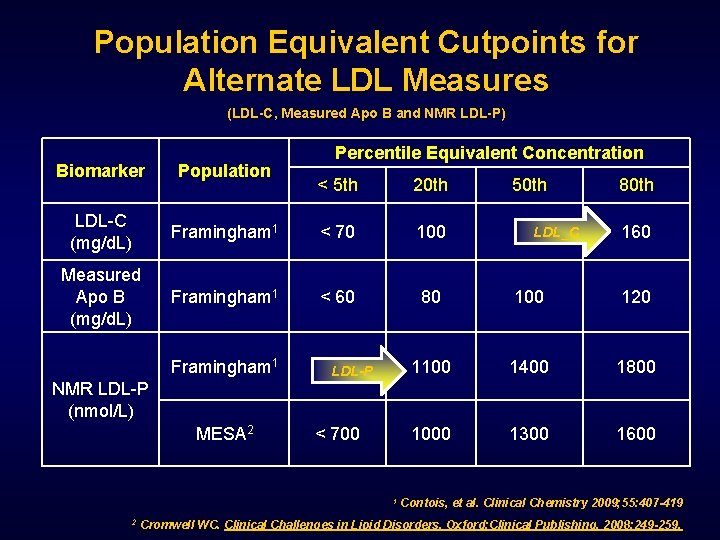
Population Equivalent Cutpoints for Alternate LDL Measures (LDL-C, Measured Apo B and NMR LDL-P) Biomarker Population LDL-C (mg/d. L) Measured Apo B (mg/d. L) Percentile Equivalent Concentration < 5 th 20 th 50 th 80 th Framingham 1 < 70 100 LDL_C 130 160 Framingham 1 < 60 80 100 120 Framingham 1 < 850 LDL-P 1100 1400 1800 < 700 1000 1300 1600 NMR LDL-P (nmol/L) MESA 2 1 2 Contois, et al. Clinical Chemistry 2009; 55: 407 -419 Cromwell WC. Clinical Challenges in Lipid Disorders. Oxford: Clinical Publishing, 2008: 249 -259.
2 New Patient referrals Secondary Prevention 3/2011 F Both patients recent Myocardial Infarction referred for lipid treatment and work up genetic etiology F Both patients on Moderate dose stain at time NMR drawn
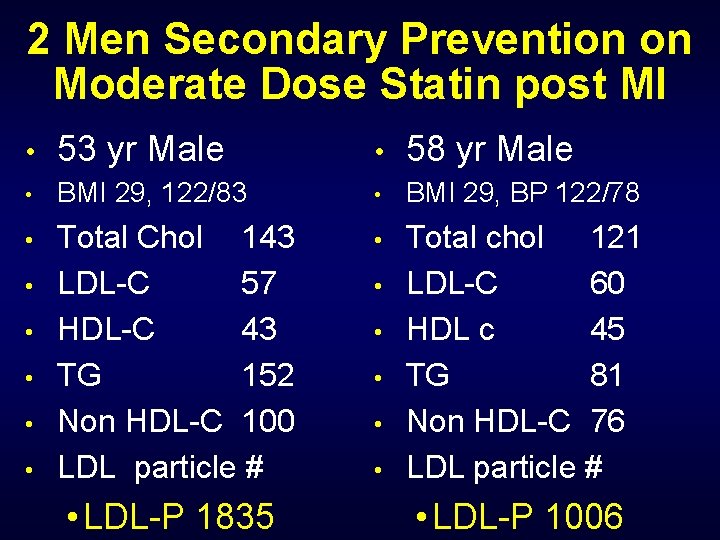
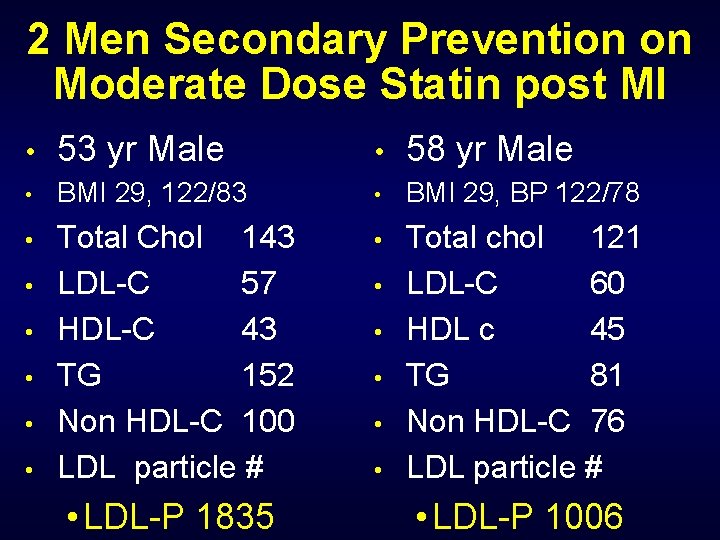
2 Men Secondary Prevention on Moderate Dose Statin post MI • 53 yr Male • 58 yr Male • BMI 29, 122/83 • BMI 29, BP 122/78 • Total Chol 143 LDL-C 57 HDL-C 43 TG 152 Non HDL-C 100 LDL particle # • Total chol 121 LDL-C 60 HDL c 45 TG 81 Non HDL-C 76 LDL particle # • • • LDL-P 1835 • • • LDL-P 1006
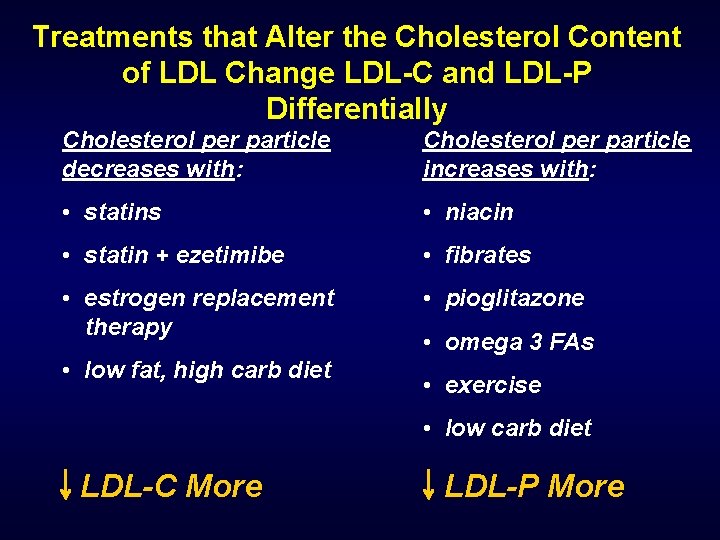
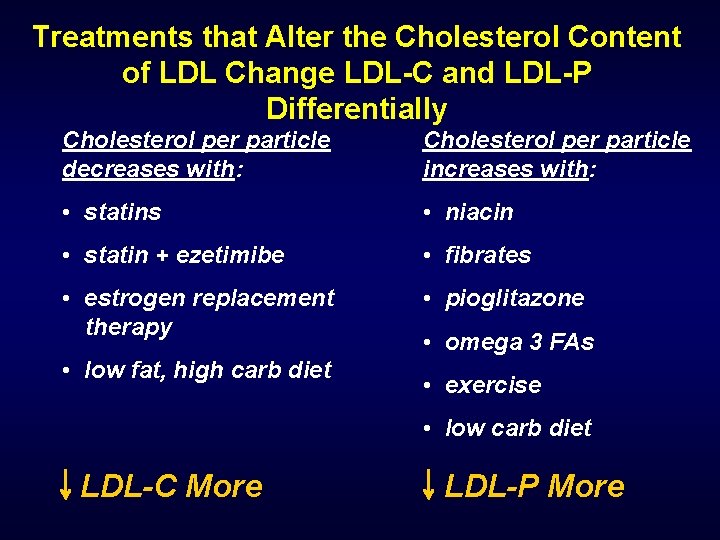
Treatments that Alter the Cholesterol Content of LDL Change LDL-C and LDL-P Differentially Cholesterol per particle decreases with: Cholesterol per particle increases with: • statins • niacin • statin + ezetimibe • fibrates • estrogen replacement therapy • pioglitazone • low fat, high carb diet • omega 3 FAs • exercise • low carb diet LDL-C More LDL-P More
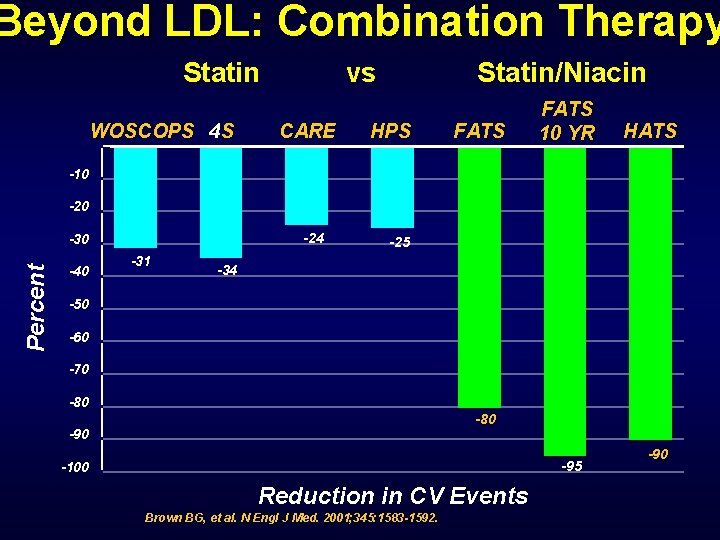
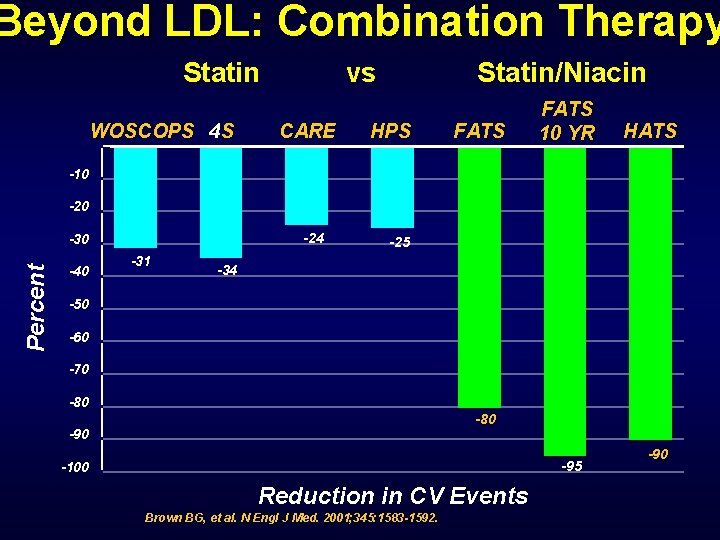
Beyond LDL: Combination Therapy Statin 0 WOSCOPS 4 S vs CARE Statin/Niacin HPS FATS 10 YR HATS -10 -24 Percent -30 -40 -31 -25 -34 -50 -60 -70 -80 -95 -100 Reduction in CV Events Brown BG, et al. N Engl J Med. 2001; 345: 1583 -1592. -90
Lipoprotein Associated Phospholipase A 2 Lp. PLA 2 (PLAC test) Cardiospecific inflammatory marker
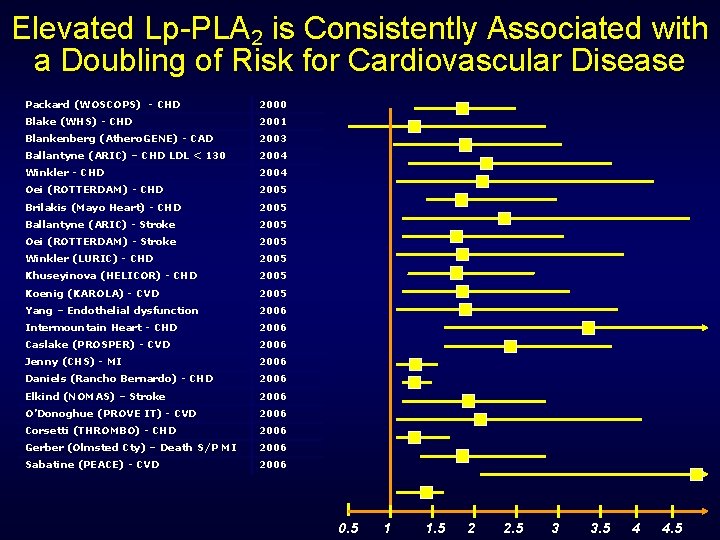
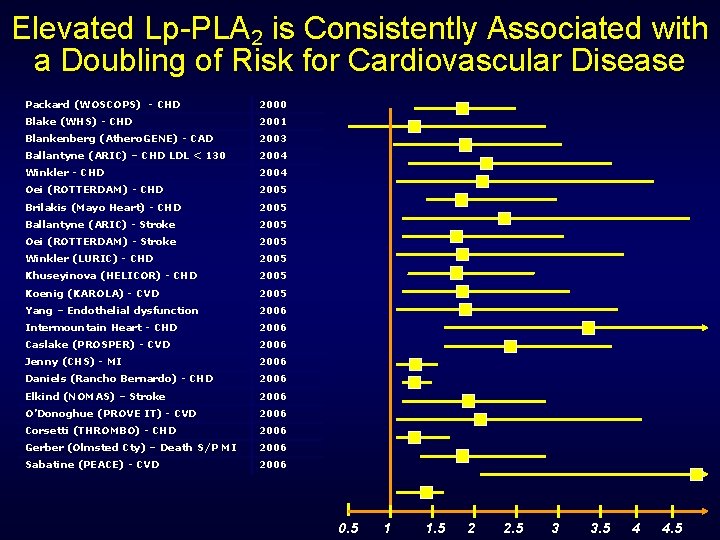
Elevated Lp-PLA 2 is Consistently Associated with a Doubling of Risk for Cardiovascular Disease Packard (WOSCOPS) - CHD 2000 Blake (WHS) - CHD 2001 Blankenberg (Athero. GENE) - CAD 2003 Ballantyne (ARIC) – CHD LDL < 130 2004 Winkler - CHD 2004 Oei (ROTTERDAM) - CHD 2005 Brilakis (Mayo Heart) - CHD 2005 Ballantyne (ARIC) - Stroke 2005 Oei (ROTTERDAM) - Stroke 2005 Winkler (LURIC) - CHD 2005 Khuseyinova (HELICOR) - CHD 2005 Koenig (KAROLA) - CVD 2005 Yang – Endothelial dysfunction 2006 Intermountain Heart - CHD 2006 Caslake (PROSPER) - CVD 2006 Jenny (CHS) - MI 2006 Daniels (Rancho Bernardo) - CHD 2006 Elkind (NOMAS) – Stroke 2006 O’Donoghue (PROVE IT) - CVD 2006 Corsetti (THROMBO) - CHD 2006 Gerber (Olmsted Cty) – Death S/P MI 2006 Sabatine (PEACE) - CVD 2006 0. 5 1 1. 5 2 2. 5 3 3. 5 4 4. 5
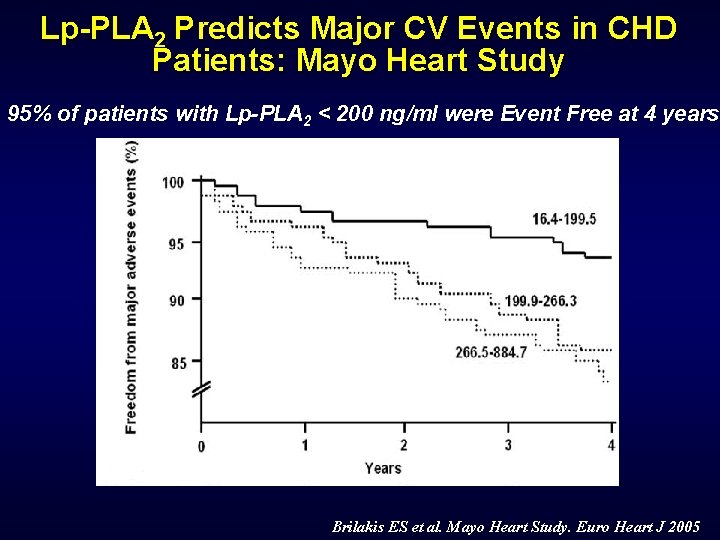
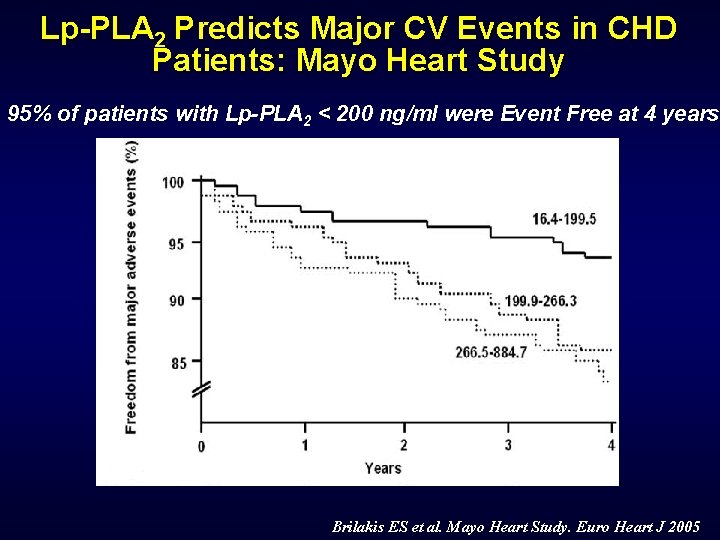
Lp-PLA 2 Predicts Major CV Events in CHD Patients: Mayo Heart Study 95% of patients with Lp-PLA 2 < 200 ng/ml were Event Free at 4 years Brilakis ES et al. Mayo Heart Study. Euro Heart J 2005
Case
C. F. 44 yr white male with Type I DM and normal Lipid profile Needs convincing to take a Statin LDL cholesterol 74
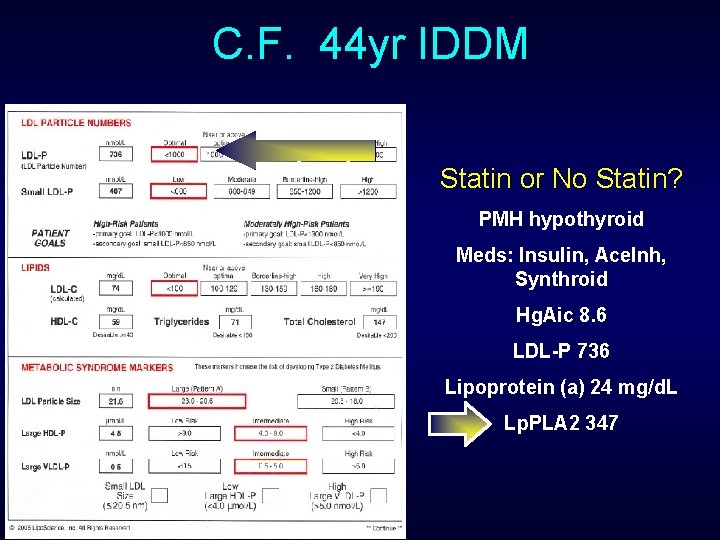
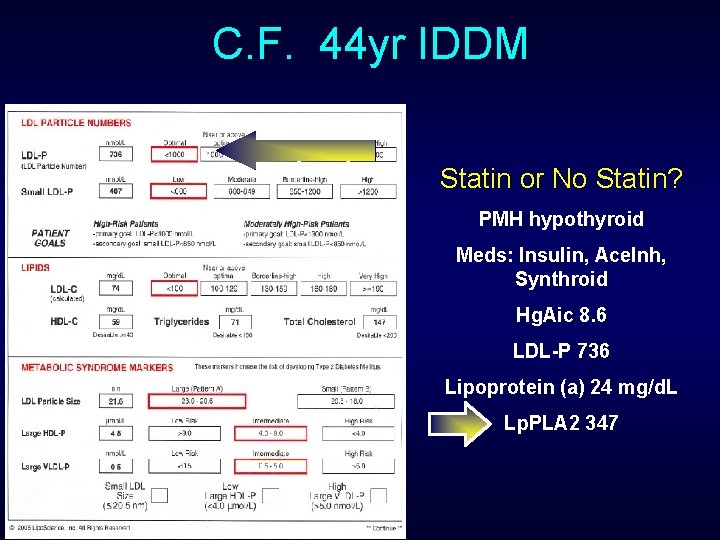
C. F. 44 yr IDDM Statin or No Statin? PMH hypothyroid Meds: Insulin, Ace. Inh, Synthroid Hg. Aic 8. 6 LDL-P 736 Lipoprotein (a) 24 mg/d. L Lp. PLA 2 347
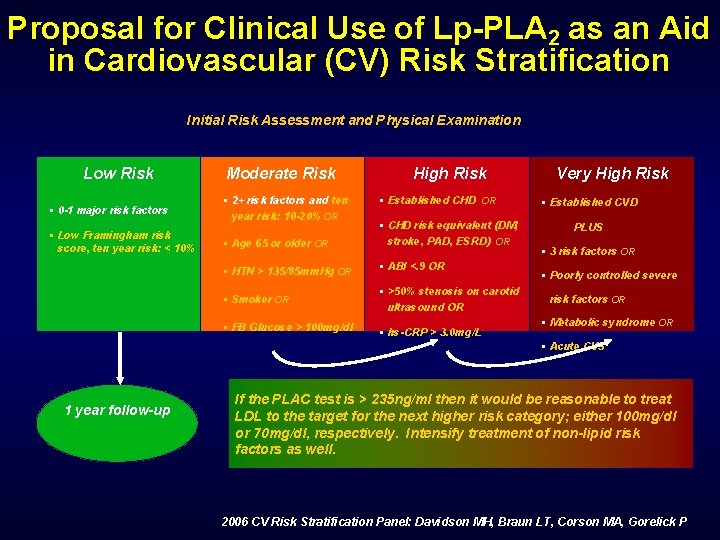
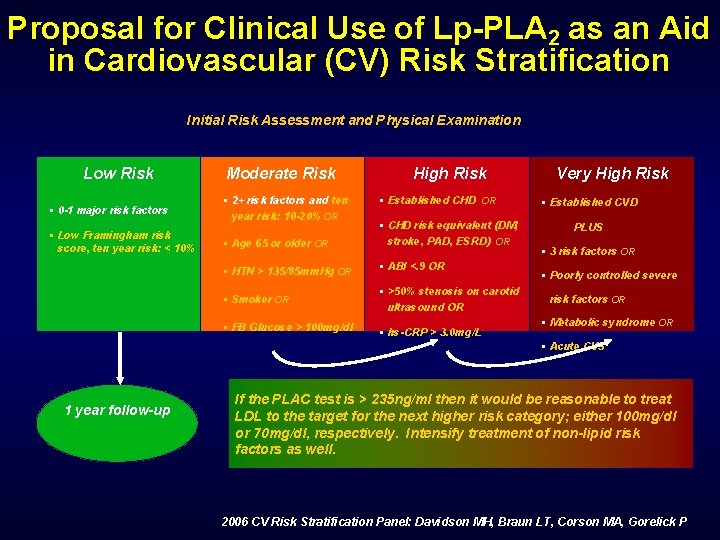
Proposal for Clinical Use of Lp-PLA 2 as an Aid in Cardiovascular (CV) Risk Stratification Initial Risk Assessment and Physical Examination Low Risk § 0 -1 major risk factors § Low Framingham risk score, ten year risk: < 10% Moderate Risk § 2+ risk factors and ten year risk: 10 -20% OR High Risk § Established CHD OR § Age 65 or older OR § CHD risk equivalent (DM, stroke, PAD, ESRD) OR § HTN > 135/85 mm. Hg OR § ABI <. 9 OR § Smoker OR § >50% stenosis on carotid ultrasound OR § FB Glucose > 100 mg/dl § hs-CRP > 3. 0 mg/L Very High Risk § Established CVD PLUS § 3 risk factors OR § Poorly controlled severe risk factors OR § Metabolic syndrome OR § Acute CVS 1 year follow-up If the PLAC test is > 235 ng/ml then it would be reasonable to treat LDL to the target for the next higher risk category; either 100 mg/dl or 70 mg/dl, respectively. Intensify treatment of non-lipid risk factors as well. 2006 CV Risk Stratification Panel: Davidson MH, Braun LT, Corson MA, Gorelick P
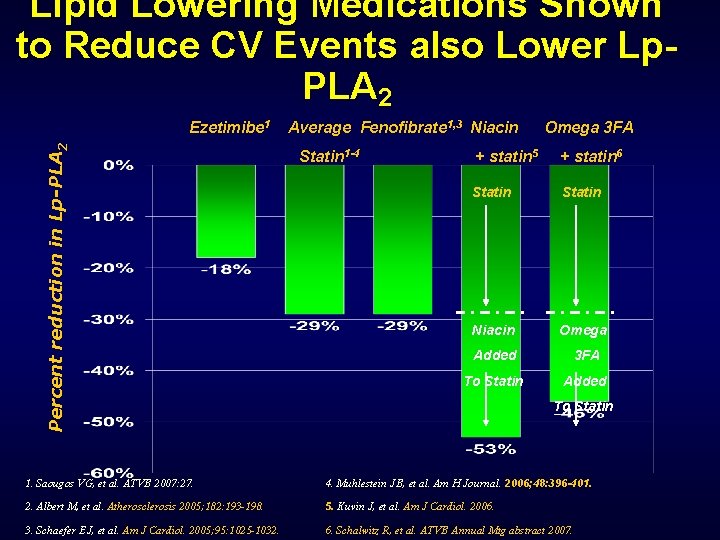
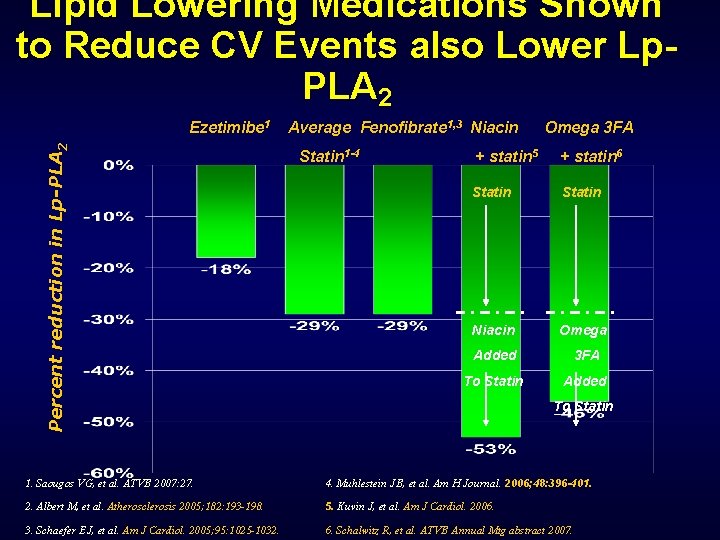
Lipid Lowering Medications Shown to Reduce CV Events also Lower Lp. PLA 2 Percent reduction in Lp-PLA 2 Ezetimibe 1 Average Fenofibrate 1, 3 Niacin Statin 1 -4 Omega 3 FA + statin 5 + statin 6 Statin Niacin Omega Added 3 FA To Statin Added To Statin 1. Saougos VG, et al. ATVB 2007: 27. 4. Muhlestein JB, et al. Am H Journal. 2006; 48: 396 -401. 2. Albert M, et al. Atherosclerosis 2005; 182: 193 -198. 5. Kuvin J, et al. Am J Cardiol. 2006. 3. Schaefer EJ, et al. Am J Cardiol. 2005; 95: 1025 -1032. 6. Schalwitz R, et al. ATVB Annual Mtg abstract 2007.

Lipoprotein (a)
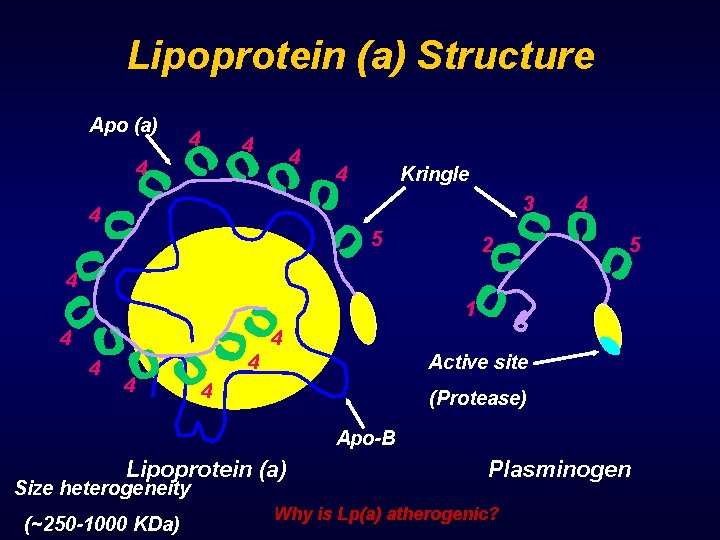
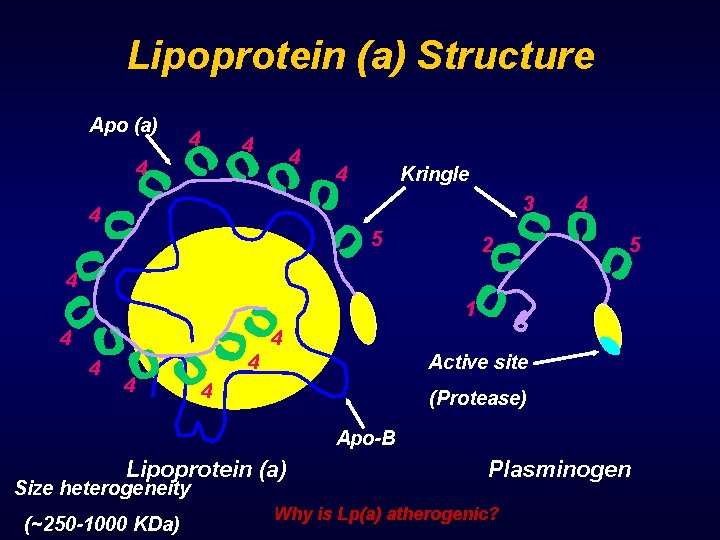
Lipoprotein (a) Structure Apo (a) 4 4 4 Kringle 3 4 5 2 4 5 4 1 4 4 4 Active site 4 (Protease) Apo-B Lipoprotein (a) Size heterogeneity (~250 -1000 KDa) Plasminogen Why is Lp(a) atherogenic?
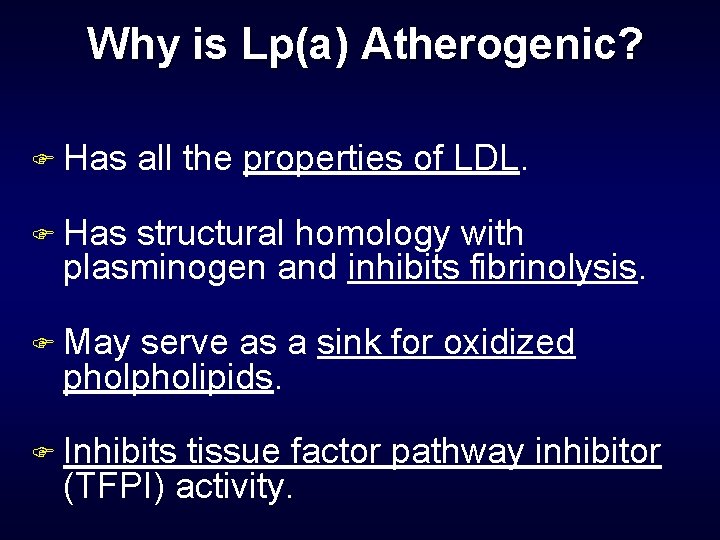
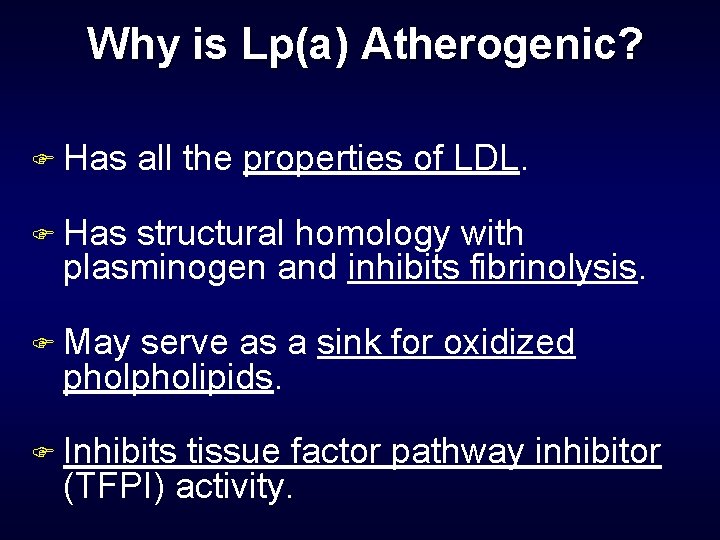
Why is Lp(a) Atherogenic? F Has all the properties of LDL. F Has structural homology with plasminogen and inhibits fibrinolysis. F May serve as a sink for oxidized pholipids. F Inhibits tissue factor pathway inhibitor (TFPI) activity.
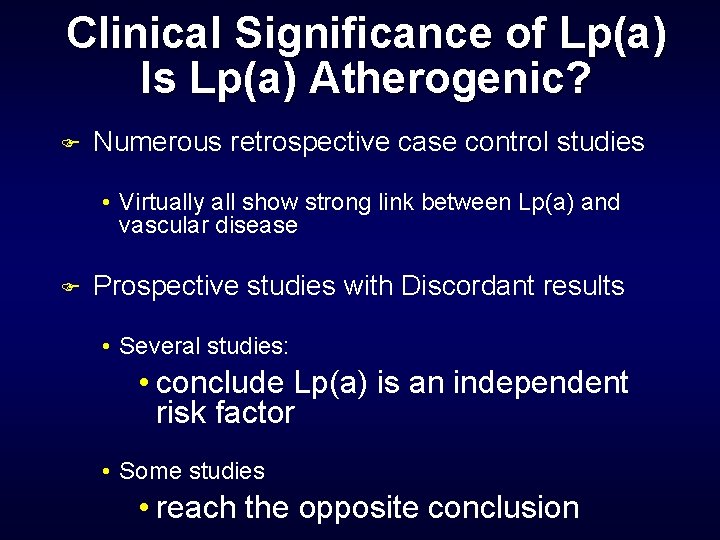
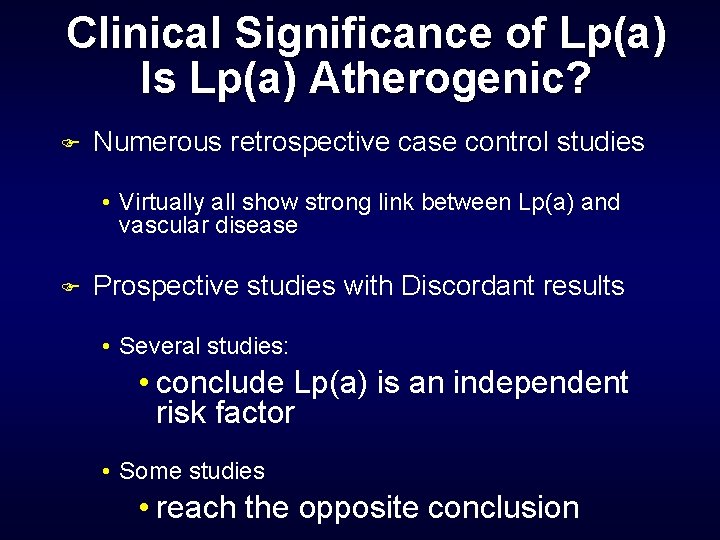
Clinical Significance of Lp(a) Is Lp(a) Atherogenic? F Numerous retrospective case control studies • Virtually all show strong link between Lp(a) and vascular disease F Prospective studies with Discordant results • Several studies: • conclude Lp(a) is an independent risk factor • Some studies • reach the opposite conclusion
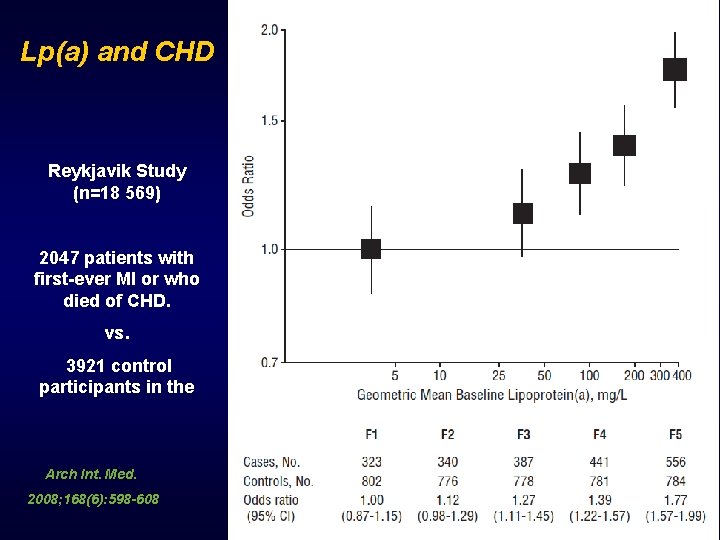
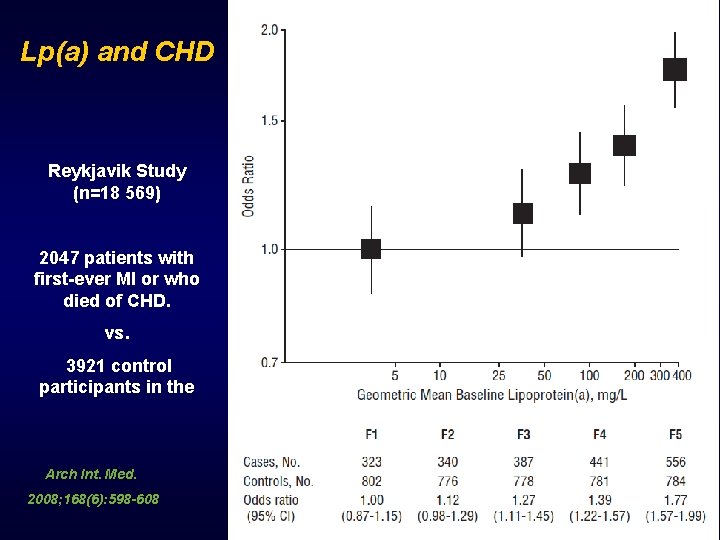
Lp(a) and CHD Reykjavik Study (n=18 569) 2047 patients with first-ever MI or who died of CHD. vs. 3921 control participants in the Arch Int. Med. 2008; 168(6): 598 -608
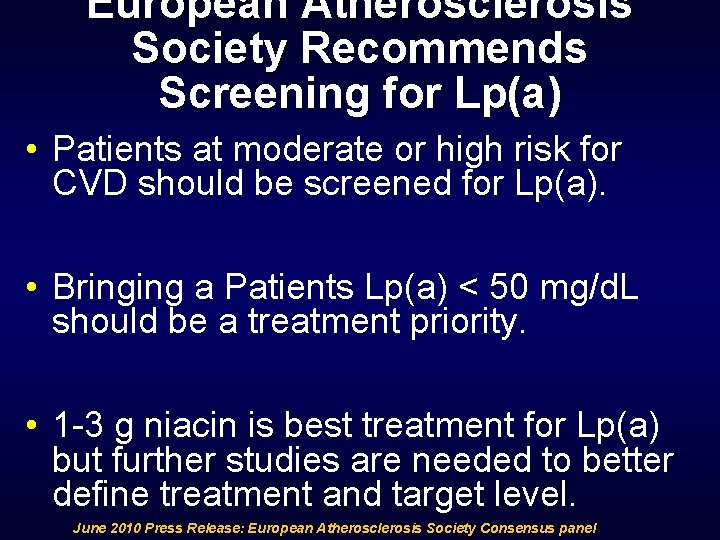
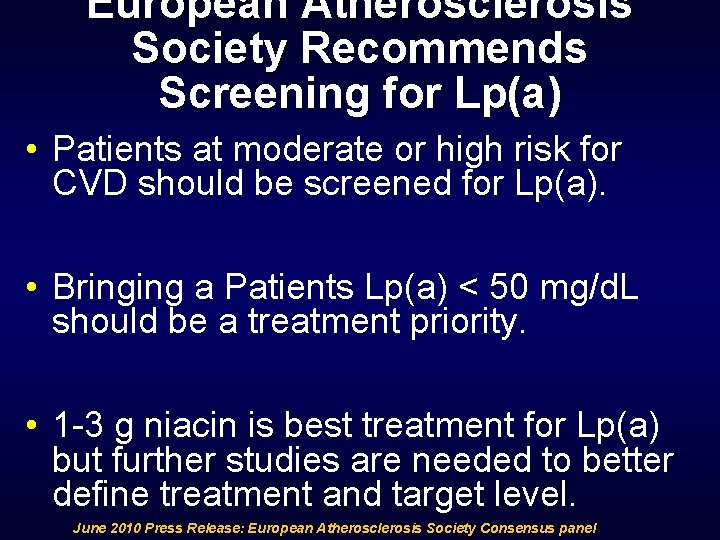
European Atherosclerosis Society Recommends Screening for Lp(a) • Patients at moderate or high risk for CVD should be screened for Lp(a). • Bringing a Patients Lp(a) < 50 mg/d. L should be a treatment priority. • 1 -3 g niacin is best treatment for Lp(a) but further studies are needed to better define treatment and target level. June 2010 Press Release: European Atherosclerosis Society Consensus panel
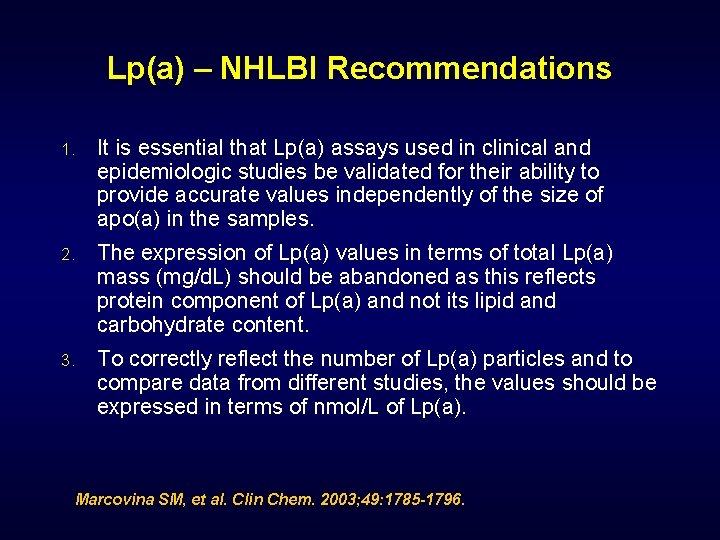
Lp(a) – NHLBI Recommendations 1. It is essential that Lp(a) assays used in clinical and epidemiologic studies be validated for their ability to provide accurate values independently of the size of apo(a) in the samples. 2. The expression of Lp(a) values in terms of total Lp(a) mass (mg/d. L) should be abandoned as this reflects protein component of Lp(a) and not its lipid and carbohydrate content. 3. To correctly reflect the number of Lp(a) particles and to compare data from different studies, the values should be expressed in terms of nmol/L of Lp(a). Marcovina SM, et al. Clin Chem. 2003; 49: 1785 -1796.
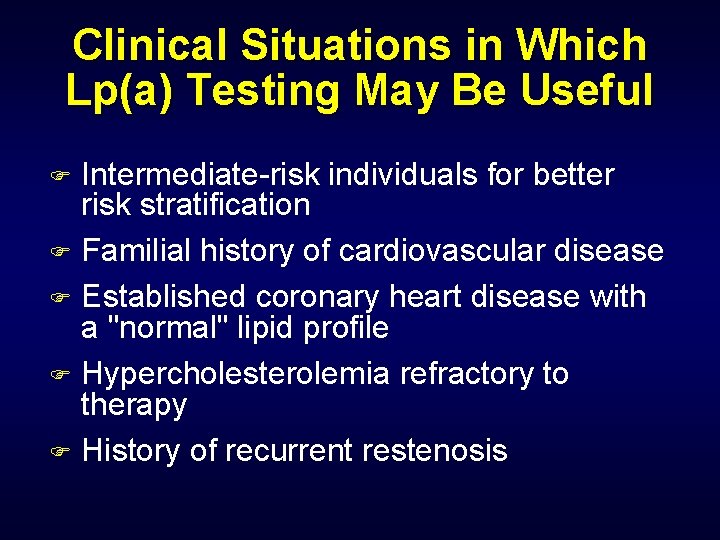
Clinical Situations in Which Lp(a) Testing May Be Useful Intermediate-risk individuals for better risk stratification F Familial history of cardiovascular disease F Established coronary heart disease with a "normal" lipid profile F Hypercholesterolemia refractory to therapy F History of recurrent restenosis F
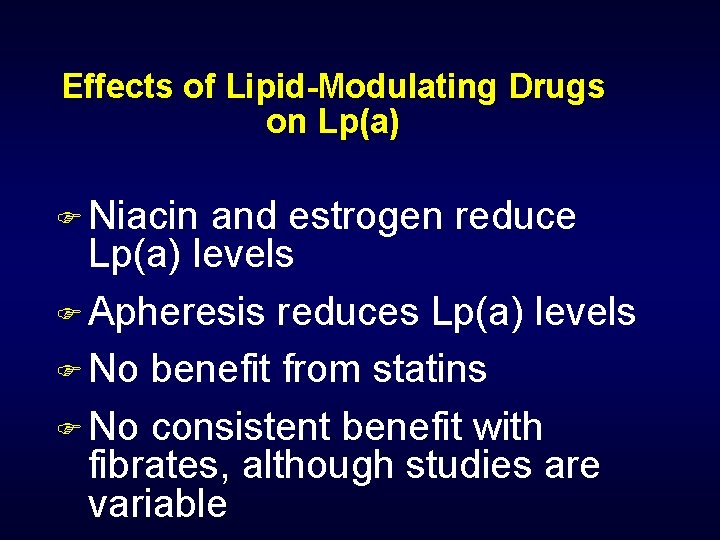
Effects of Lipid-Modulating Drugs on Lp(a) F Niacin and estrogen reduce Lp(a) levels F Apheresis reduces Lp(a) levels F No benefit from statins F No consistent benefit with fibrates, although studies are variable

hs. CRP

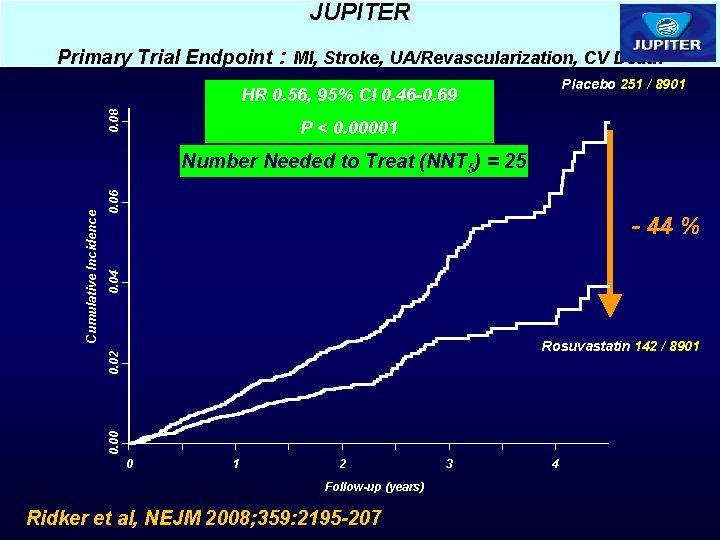
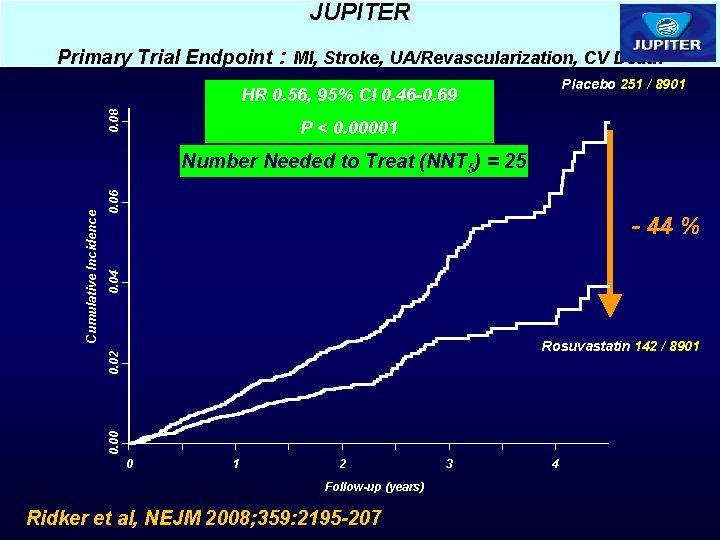
JUPITER Primary Trial Endpoint : MI, Stroke, UA/Revascularization, CV Death Placebo 251 / 8901 0. 08 HR 0. 56, 95% CI 0. 46 -0. 69 P < 0. 00001 0. 06 0. 04 - 44 % Rosuvastatin 142 / 8901 0. 00 0. 02 Cumulative Incidence Number Needed to Treat (NNT 5) = 25 0 1 2 Follow-up (years) Ridker et al, NEJM 2008; 359: 2195 -207 3 4
Drugs and CRP F Statins lower hs. CRP F Niaspan lower hs. CRP F Fibrates lower hs. CRP F Omega 3 Fatty Acids lower hs. CRP F Glitazones lower hs. CRP F Estrogen increases hs. CRP

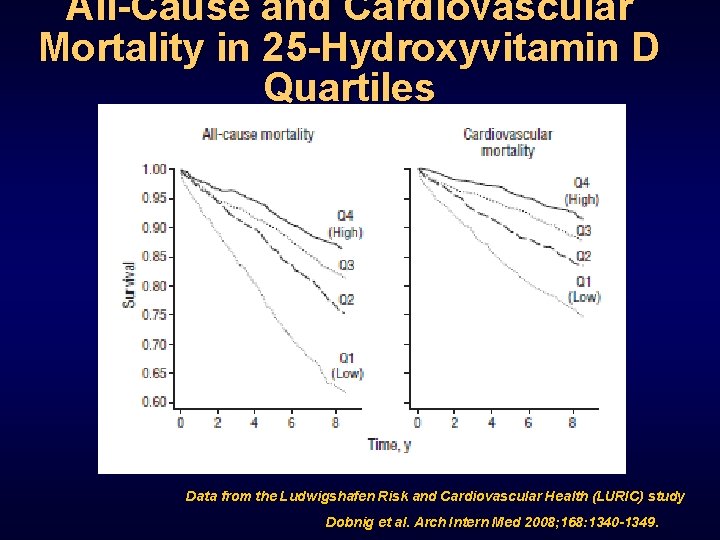
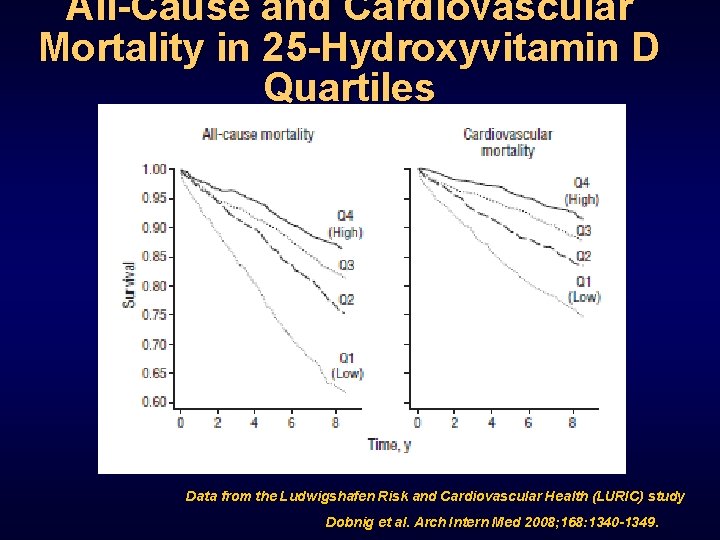
All-Cause and Cardiovascular Mortality in 25 -Hydroxyvitamin D Quartiles Data from the Ludwigshafen Risk and Cardiovascular Health (LURIC) study Dobnig et al. Arch Intern Med 2008; 168: 1340 -1349.
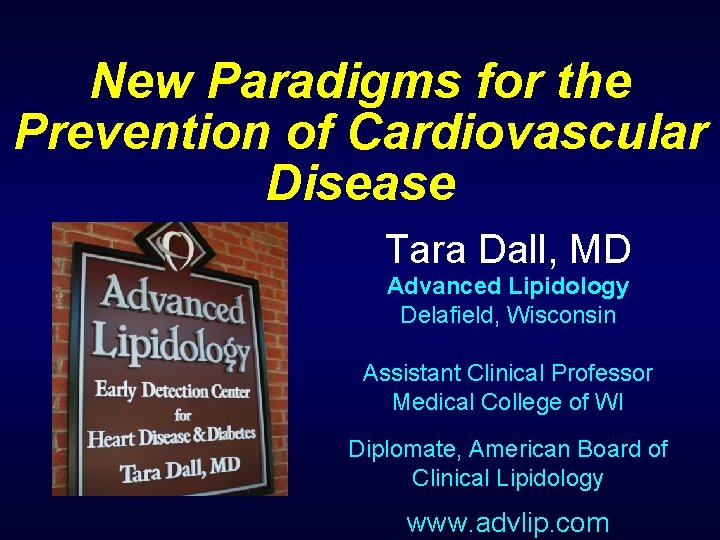
Could Barb’s Massive Heart Attack been prevented? No risk factors? Lets look at her NMR lipoprofile
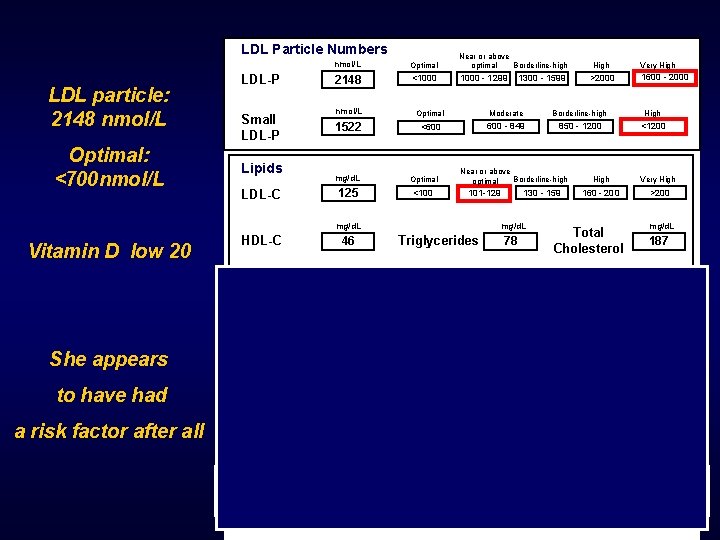
LDL Particle Numbers LDL particle: 2148 nmol/L Optimal: <700 nmol/L LDL-P Small LDL-P Lipids LDL-C nmol/L Optimal Near or above optimal Borderline-high 2148 <1000 - 1299 HDL-C High Very High 1600 - 2000 >2000 nmol/L Optimal Moderate Borderline-high High 1522 <600 - 849 850 - 1200 <1200 mg/d. L Optimal 125 <100 Near or above Borderline-high optimal 101 -129 mg/d. L Vitamin D low 20 1300 - 1599 46 130 - 159 mg/d. L Triglycerides 78 High Very High 160 - 200 >200 Total Cholesterol mg/d. L 187 Subclass Particle Numbers VLDL Subclasses She appears to have had a risk factor after all P E R C E N T I L E LDL Subclasses HDL Subclasses 75 th 50 th 25 th Large Medium VLDL-P Small VLDL-P IDL-P Large LDL-P Small LDL-P Large HDL-P Medium HDL-P Small HDL-P

Questions? taradall@advlip. com www. advlip. com
 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Chapter 11 the cardiovascular system
Chapter 11 the cardiovascular system Cardiovascular disease risk factor
Cardiovascular disease risk factor Puncture resistant container
Puncture resistant container Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention European centre for disease prevention and control
European centre for disease prevention and control Health promotion and levels of disease prevention
Health promotion and levels of disease prevention Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Health promotion and levels of disease prevention
Health promotion and levels of disease prevention Bharathi viswanathan
Bharathi viswanathan Peter hall policy paradigms
Peter hall policy paradigms Careershodh
Careershodh Paradigms and principles 7 habits
Paradigms and principles 7 habits Vertical
Vertical Paradigm of interaction examples
Paradigm of interaction examples Distributed systems principles and paradigms
Distributed systems principles and paradigms Message ordering paradigms
Message ordering paradigms Distributed systems principles and paradigms
Distributed systems principles and paradigms Is a paradigm of distributed computing to provide
Is a paradigm of distributed computing to provide 3 paradigms
3 paradigms Interpretivism in consumer behaviour
Interpretivism in consumer behaviour Boyfriend/girlfriend centered paradigm
Boyfriend/girlfriend centered paradigm Binding in programming paradigms
Binding in programming paradigms Ktu programming paradigms notes
Ktu programming paradigms notes Development support communication slideshare
Development support communication slideshare Issues of multimedia authoring
Issues of multimedia authoring Decide evaluation framework
Decide evaluation framework Current paradigms in psychopathology
Current paradigms in psychopathology R programming language paradigms
R programming language paradigms Php paradigms
Php paradigms Paradigms and principles
Paradigms and principles Distributed systems principles and paradigms
Distributed systems principles and paradigms Paradigms of development
Paradigms of development Distributed systems principles and paradigms
Distributed systems principles and paradigms True capillaries
True capillaries Riesgo cardiovascular por perimetro abdominal
Riesgo cardiovascular por perimetro abdominal Maniobra de azulay
Maniobra de azulay What makes up the circulatory system
What makes up the circulatory system Rias hipertension arterial
Rias hipertension arterial Pithed rat model
Pithed rat model National cardiovascular partners
National cardiovascular partners Its tubular dude
Its tubular dude Cardiovascular drift
Cardiovascular drift Crash course heart
Crash course heart Cengage chapter 5
Cengage chapter 5 Chapter 46 the child with a cardiovascular alteration
Chapter 46 the child with a cardiovascular alteration Chapter 26 the child with a cardiovascular disorder
Chapter 26 the child with a cardiovascular disorder Chapter 25 assessment of cardiovascular function
Chapter 25 assessment of cardiovascular function Figure 11-7 veins labeled
Figure 11-7 veins labeled Figure 11-12 is a diagram of a capillary bed
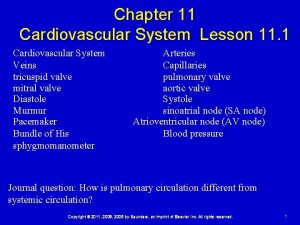
Figure 11-12 is a diagram of a capillary bed Lesson 11 cardiovascular system
Lesson 11 cardiovascular system Lesson 11 cardiovascular system
Lesson 11 cardiovascular system American board of cardiovascular medicine
American board of cardiovascular medicine Advanced cardiovascular life support
Advanced cardiovascular life support Centro cardiovascular
Centro cardiovascular Tissues in circulatory system
Tissues in circulatory system Caracteristicas de las venas
Caracteristicas de las venas Cardiovascular research institute basel
Cardiovascular research institute basel Introduction of cardiovascular system
Introduction of cardiovascular system What is cardiovascular endurance in health related fitness
What is cardiovascular endurance in health related fitness Cardiovascular system
Cardiovascular system Salud cardiovascular
Salud cardiovascular Strength in mapeh
Strength in mapeh Salud cardiovascular
Salud cardiovascular Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system