Musculoskeletal System KNH 413 Skeletal System Cartilage ligaments




- Slides: 73
Musculoskeletal System KNH 413
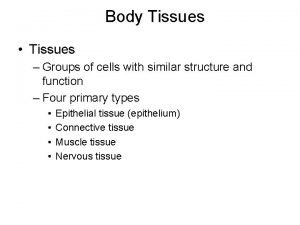
Skeletal System Cartilage, ligaments, tendons, bones Metabolically active cells and tissue Continual state of change
Skeletal System Cartilage – flexible yet firm connective tissue consisting of cells and collagen fibers Chondroblasts/chondrocytes – cells Collagen – fibrous protein, most common protein in the body Chondroitin sulphate – most common polysaccharide of cartilage
Skeletal System Bone – osseous tissue Organic – mineralized or calcified by inorganic component; flexibility Inorganic - hydroxyapatite; stiffness, weight bearing Ready source of calcium and phosphorus for extracellular fluids Hydroxyapaptite (99%) Readily available pool (1%)
Skeletal System Bone Abnormalities in serum calcium critical Hypocalcemia – excessive excitability of the nervous system, tetany , respiratory arrest, convulsions Hypercalcemia – fatigue, depression, metal confusion, anorexia, nausea, vomiting, constipation, hypercalciuria
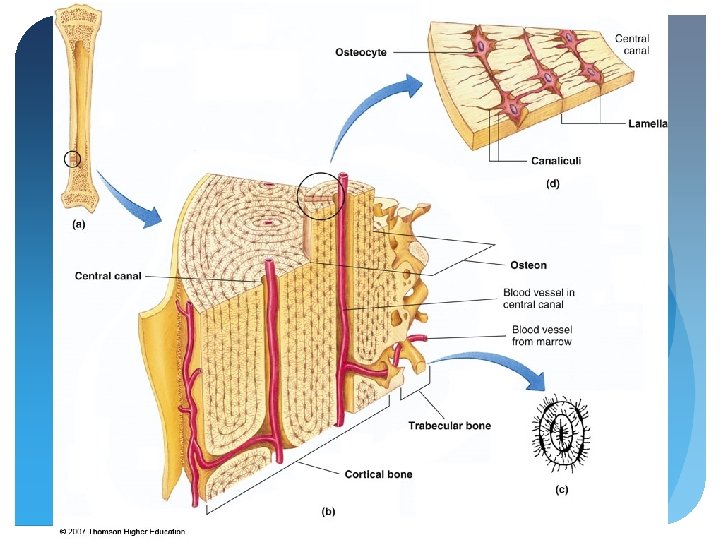
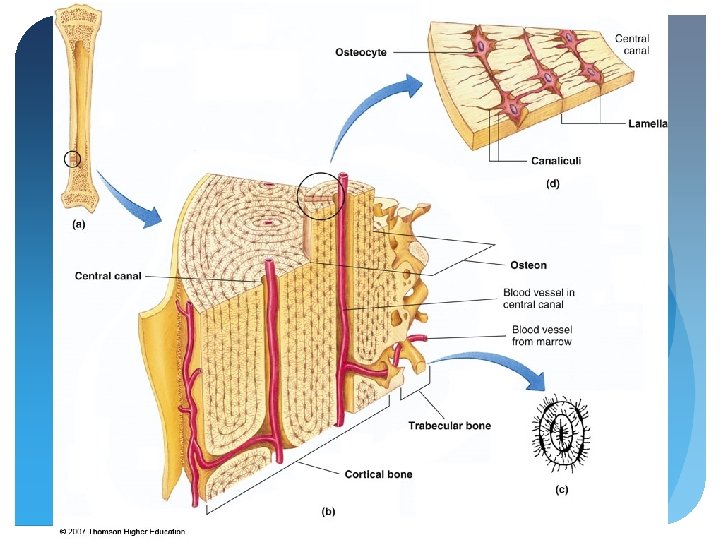
Skeletal System Cells of Osseous Tissue Osteogenic cells – stem cells that differentiate into osteoblasts Osteoblasts - bone-building cells Osteocytes – mature osteoblasts, majority of cells in bone Osteoclasts – bone-removing cells that secrete HCl; bone resorption
Skeletal System Skeletal growth and development Continual state of change; linear and circumferential growth, and in response to changes in forces applied to them - remodeling Osteoclasts remove bone from low-stress areas, osteoblasts lay down new bone in high-stress areas
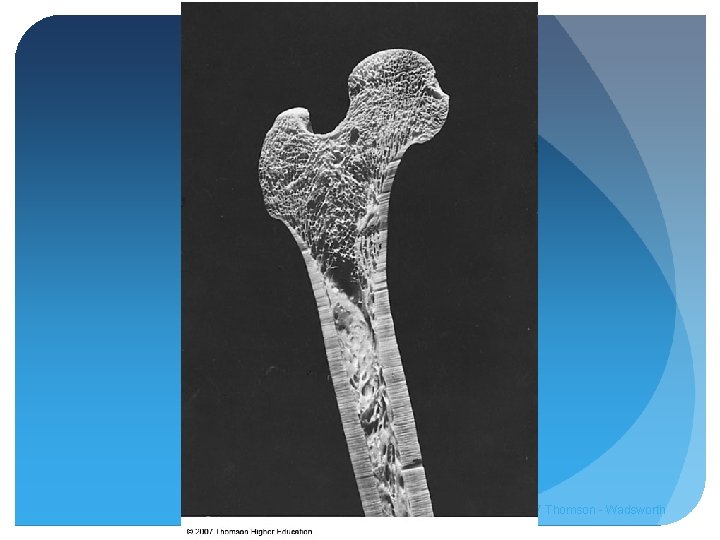
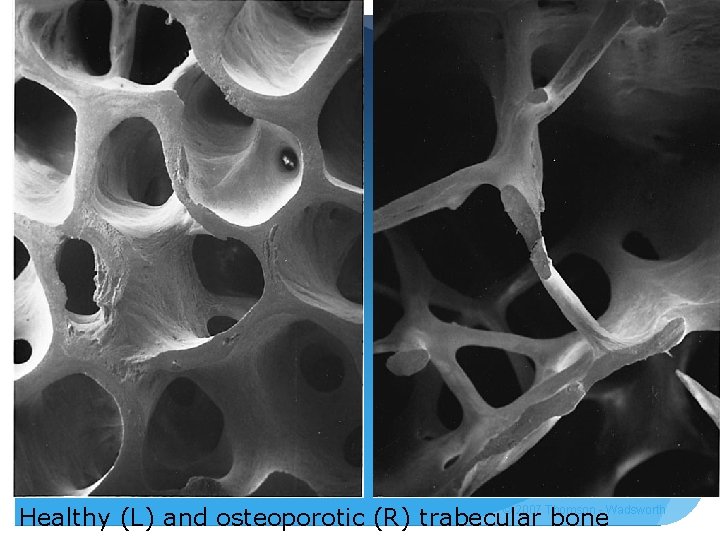
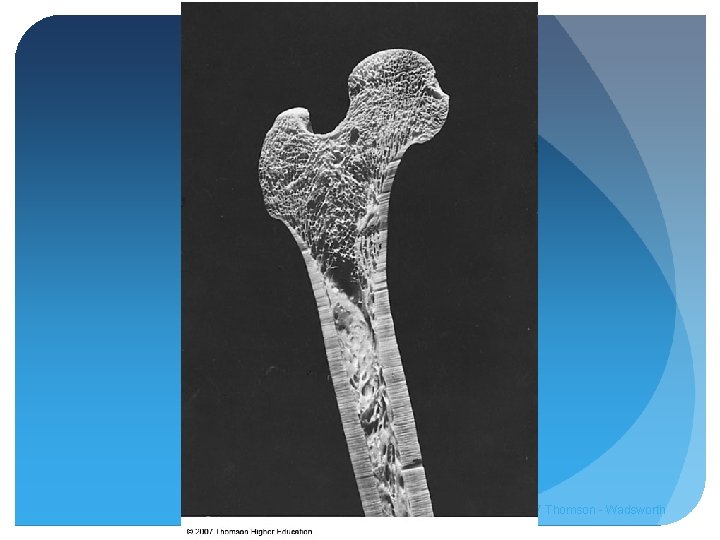
Skeletal System Cortical bone Dense, outer surface of most bones, shafts of long bones, and caps over end of long bones 75% of skeletal weight Trabecular bone Loosely organized with a sponge-like appearance; lattice-like pattern “Ends” of long bones, primary bone of vertebrae, pelvis, sternum, scapula 25% of skeletal weight © 2007 Thomson - Wadsworth
© 2007 Thomson - Wadsworth
© 2007 Thomson - Wadsworth
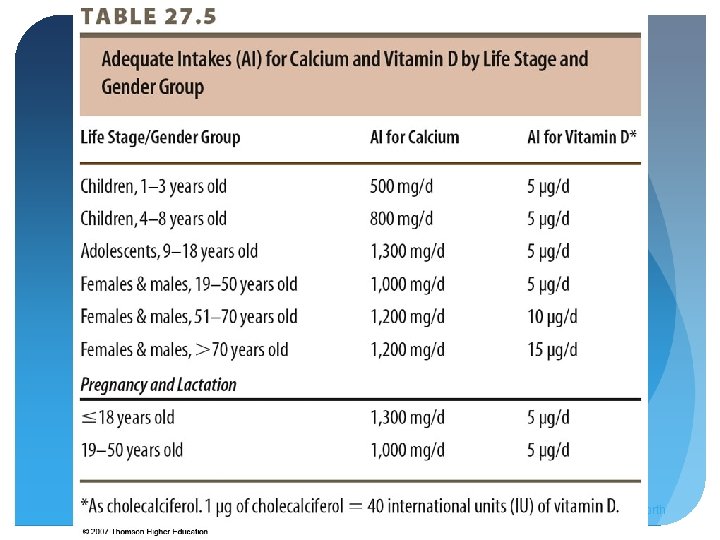
Skeletal System Hormonal control of bone metabolism Calcium and phosphorus homeostasis Cortisol, growth hormone, thyroid hormones Primary regulators: parathyroid hormone (PTH), calcitonin, vitamin D
Skeletal System PTH – increases blood calcium when low Increase in osteoclasts and bone resorption Inhibition of collagen synthesis and bone deposition Calcium resorption by kidneys Final step in vitamin D synthesis, enabling intestinal absorption of calcium
Skeletal System Calcitonin – decreases blood calcium when high Inhibits activity of osteoclasts Stimulates osteoblasts Reduces renal reabsorption of calcium and phosphate
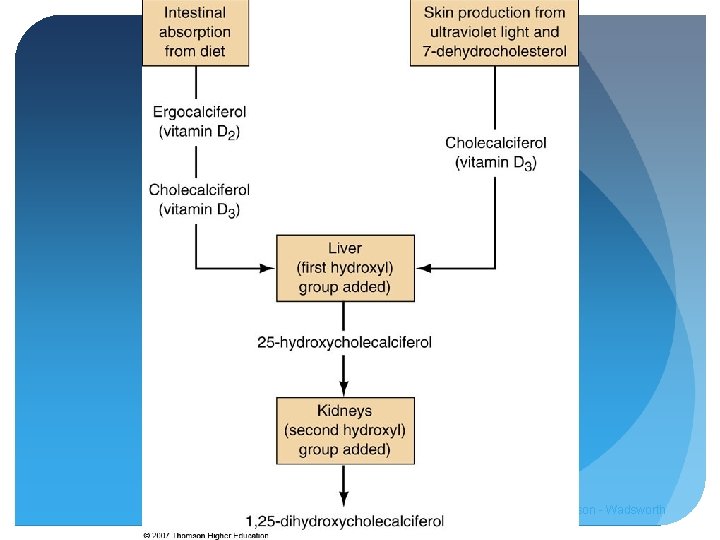
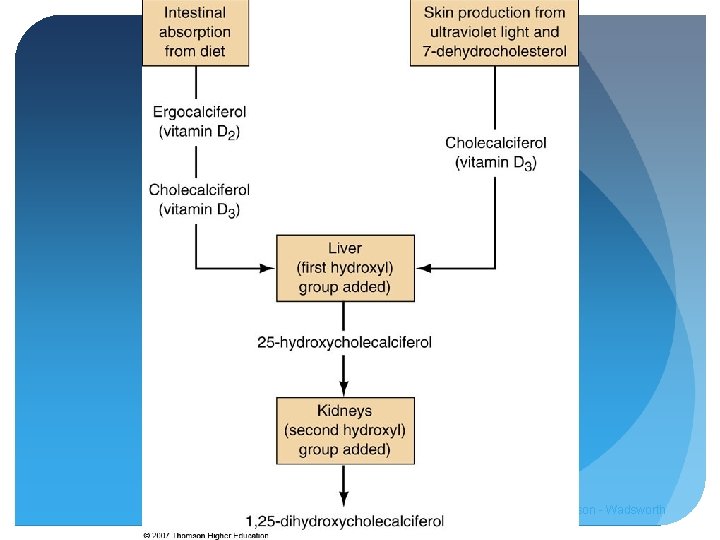
Skeletal System Vitamin D – increases blood concentrations of calcium and phosphorus Promotes their absorption in GI Promotes reabsorption by kidneys Stimulates osteoclast formation and release of calcium and phosphorus from bone
Skeletal System Vitamin D – Ergocalciferol - dietary Cholecalciferol – dietary, exposure to sunlight Both biologically inactive until modified by liver and kidney to 1, 25 dihydroxyvitamin D
© 2007 Thomson - Wadsworth
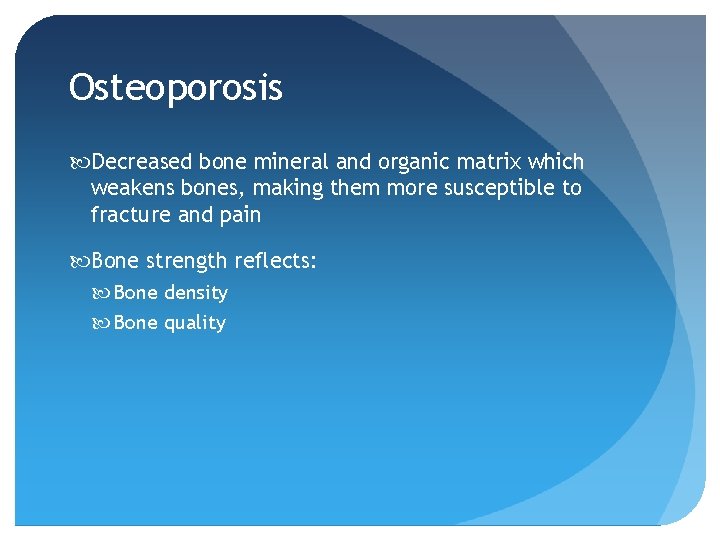
Osteoporosis Decreased bone mineral and organic matrix which weakens bones, making them more susceptible to fracture and pain Bone strength reflects: Bone density Bone quality
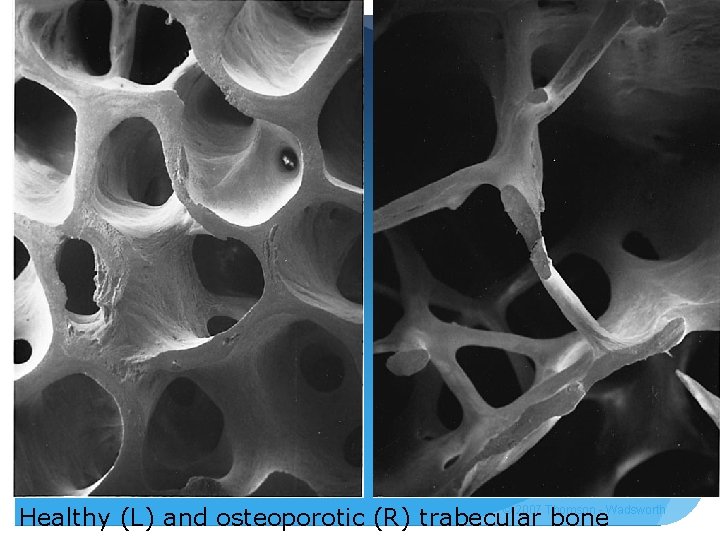
© 2007 Thomson - Wadsworth Healthy (L) and osteoporotic (R) trabecular bone
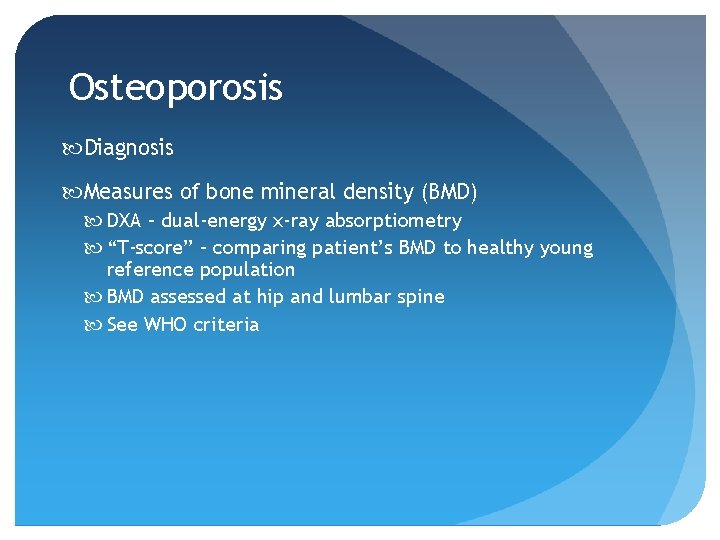
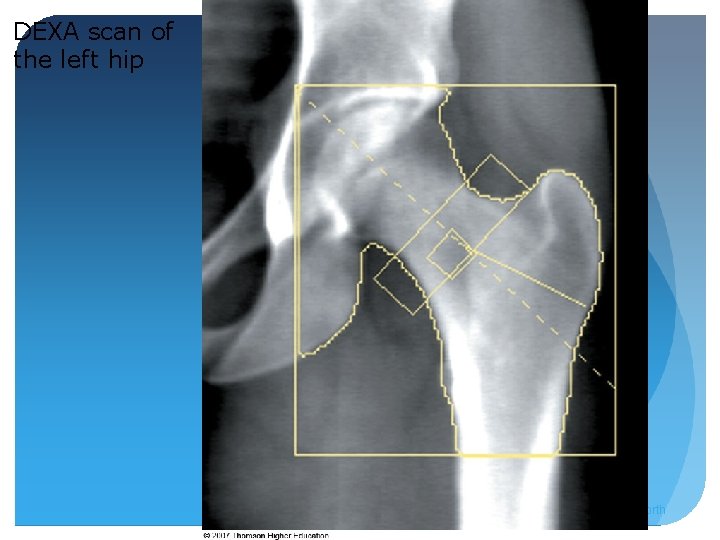
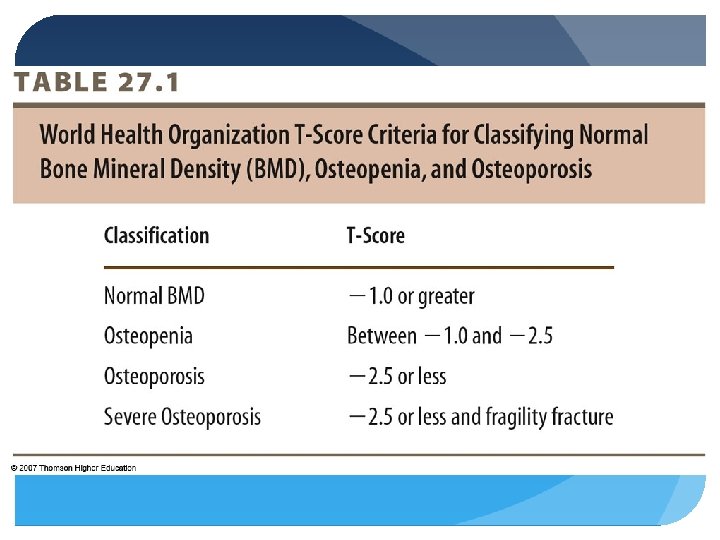
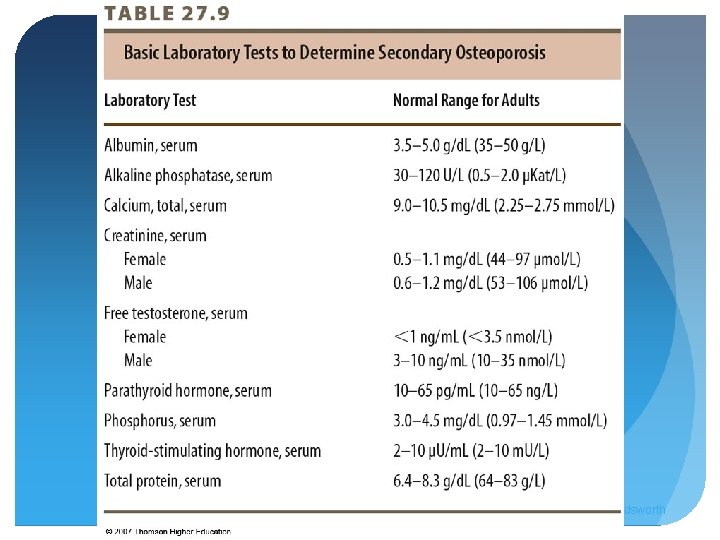
Osteoporosis Diagnosis Measures of bone mineral density (BMD) DXA – dual-energy x-ray absorptiometry “T-score” – comparing patient’s BMD to healthy young reference population BMD assessed at hip and lumbar spine See WHO criteria
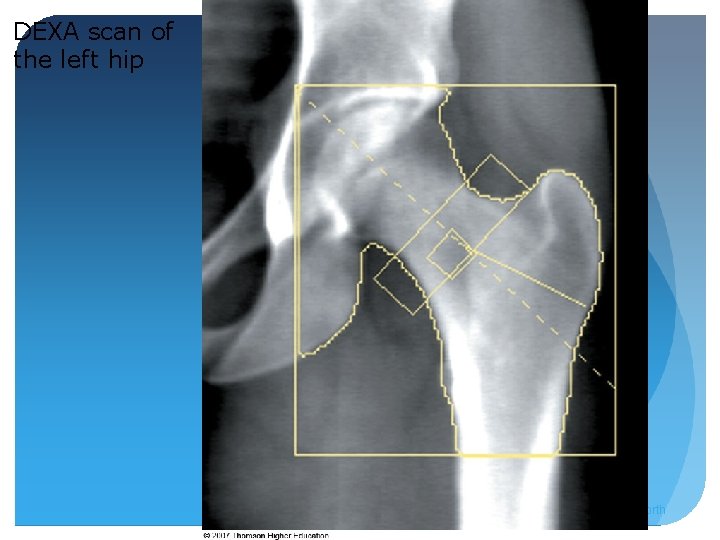
DEXA scan of the left hip © 2007 Thomson - Wadsworth
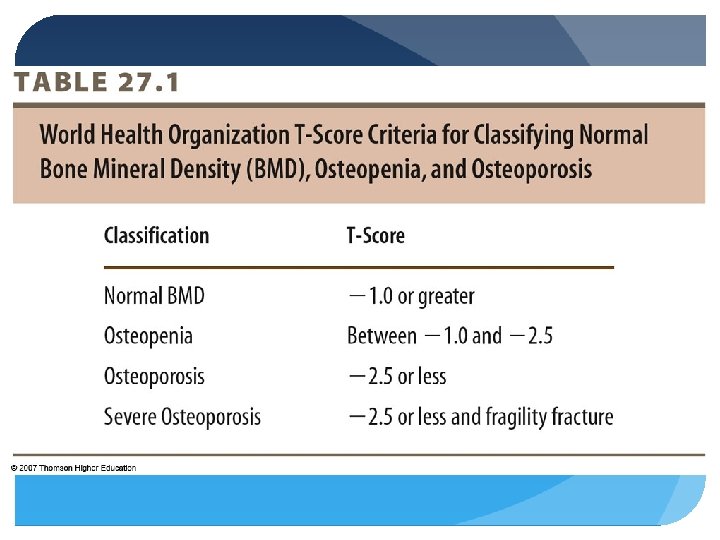
Osteoporosis Diagnosis Others: Quantitative ultrasound of the heel used in conjunction with risk assessment – useful for screening Osteopenia – bone mineral density is low but not low enough to be classified as osteoporosis, although fracture risk is increased
Osteoporosis BMD increases rapidly during growth spurt (ages 11 -14 y) Maximum density reached in late 20 s or 30 s Females lose BMD at faster rate than men Rate of loss increases during menopause
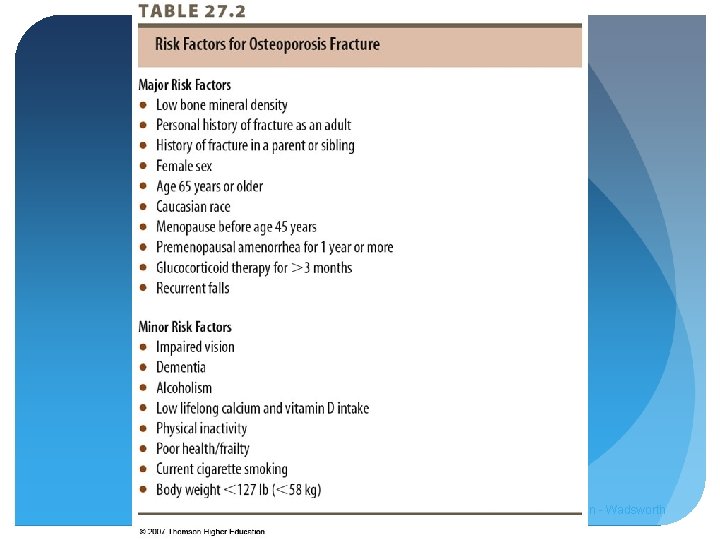
Osteoporosis Fractures Most common sites: hip, spine, wrist Kyphosis – unnatural curvature of back, and loss of height d/t compression fractures of spine Hip fractures have severe impact on morbidity and mortality 20% die within first year, 20% end up in nursing homes
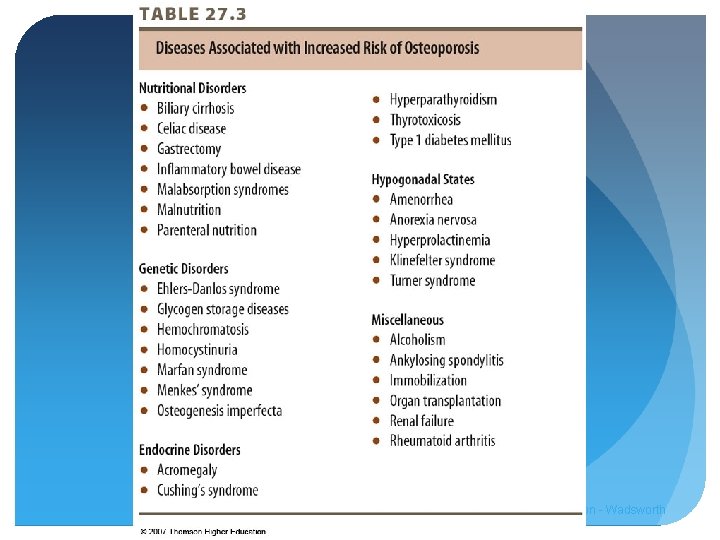
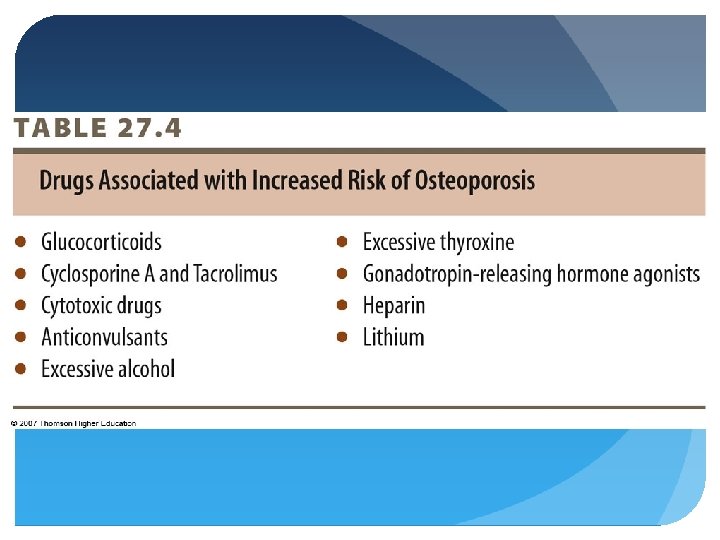
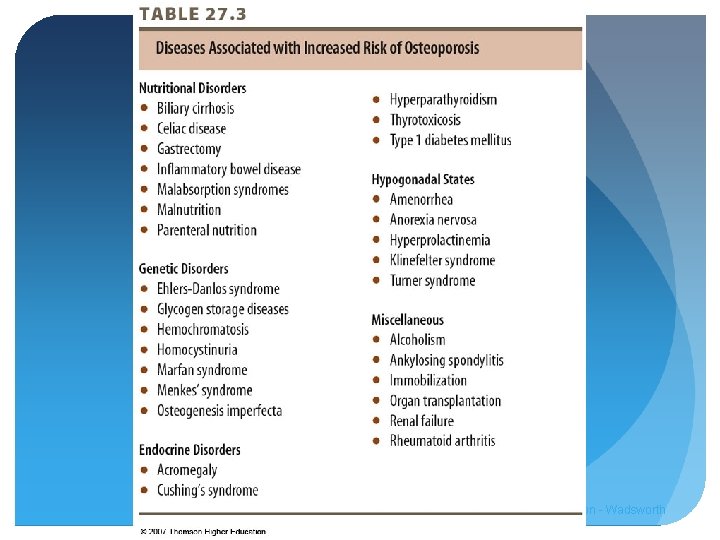
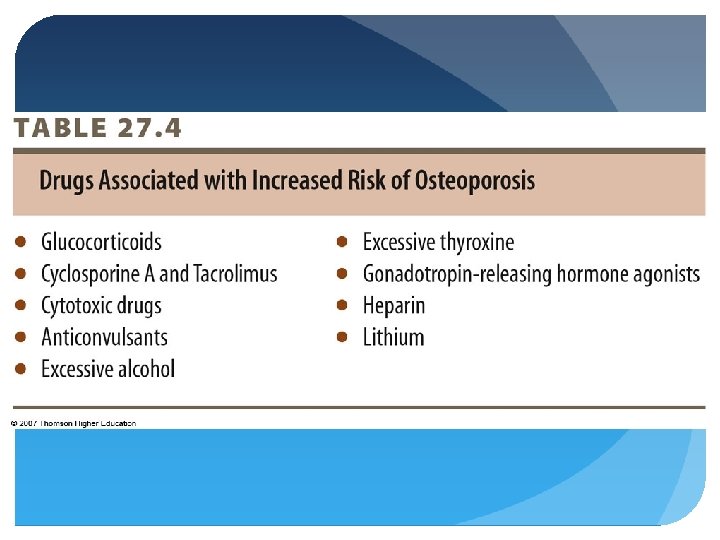
Osteoporosis Etiology Primary – disease of elderly, cumulative impact of bone mineral loss and deterioration of bone with age; “agerelated, ” “postmenopausal” Secondary - disease and drug associated 2/3 of cases in men
© 2007 Thomson - Wadsworth
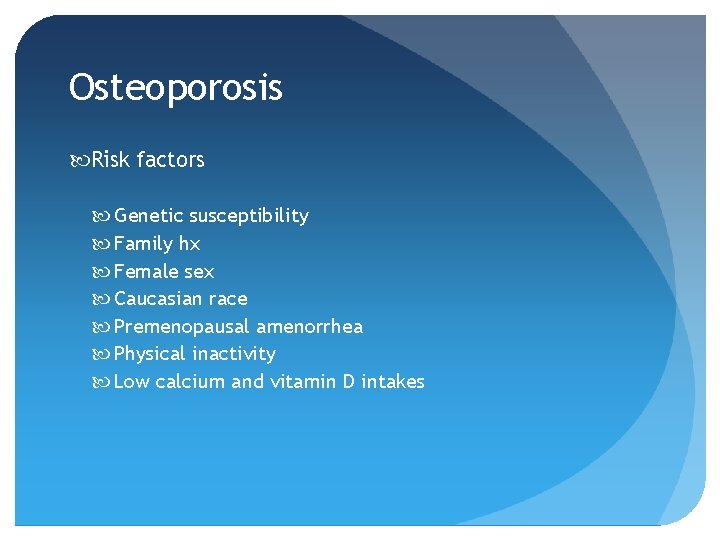
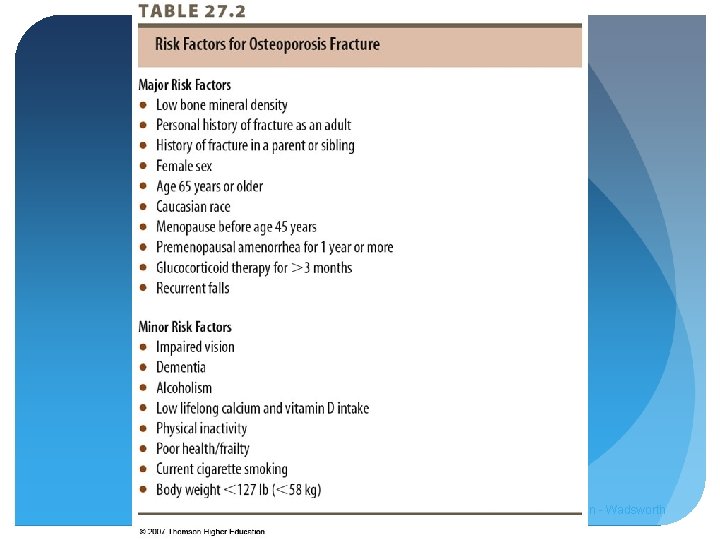
Osteoporosis Risk factors Genetic susceptibility Family hx Female sex Caucasian race Premenopausal amenorrhea Physical inactivity Low calcium and vitamin D intakes
© 2007 Thomson - Wadsworth
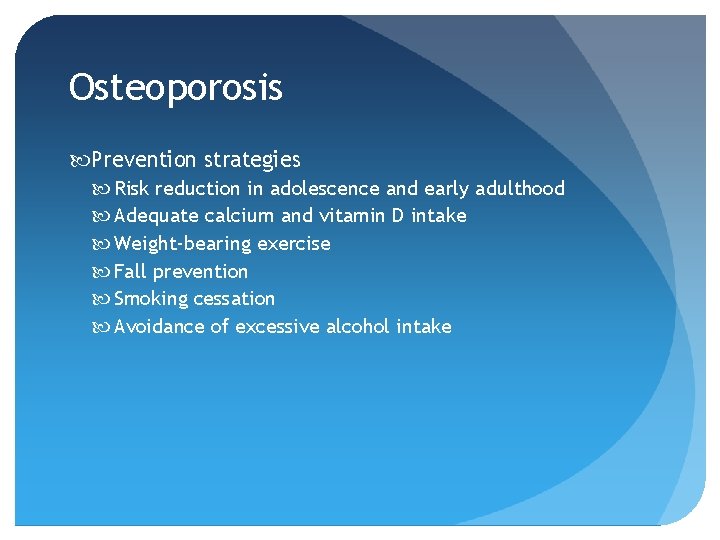
Osteoporosis Prevention strategies Risk reduction in adolescence and early adulthood Adequate calcium and vitamin D intake Weight-bearing exercise Fall prevention Smoking cessation Avoidance of excessive alcohol intake
© 2007 Thomson - Wadsworth
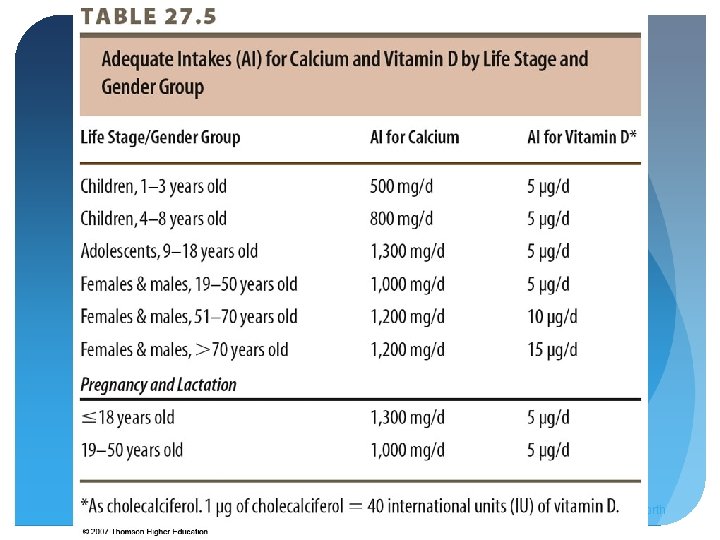
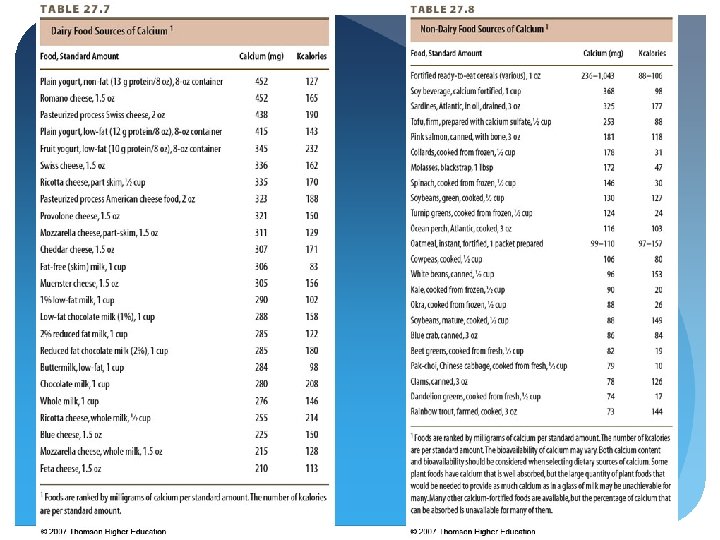
Osteoporosis Calcium Maintenance of serum calcium levels to combat bone resorption Achieve peak bone mass and minimize bone mineral loss Lower intakes of animal protein, sodium, caffeine Increased consumption of fruits, vegetables, legumes, whole grains More physical activity Sun exposure
Osteoporosis Calcium Consume calcium-rich foods Calcium-fortified foods Calcium supplements Calcium carbonate – least expensive, taken with meals, not at the same time as iron Calcium citrate – taken any time Calcium with vitamin D Avoid dolomite and bonemeal – lead contamination Divided doses to improve absorption
© 2007 Thomson - Wadsworth
Osteoporosis Vitamin D Overt deficiency – rickets in children, osteomalacia in adults Insufficiency found in dark-skinned, older, in northern latitudes (above 40 degree N) Supplementation with vitamin D and calcium Fortified dairy products Exposure to adequate sunlight

Osteoporosis Physical activity BMD increases with weight-bearing or impact-type activity Very high levels can be detrimental if oligomenorrhea or amenorrhea present
Osteoporosis Cigarette smoking Lower BMD, increased bone mineral loss, increased risk of fractures Nicotine and cadmium toxic to osteoblasts Reduced intestinal calcium absorption Lower intakes of vitamin D, and lower serum vitamin D
Osteoporosis Alcohol Decreased BMD, reduced bone formation, increased risk of fractures Increased calcium and magnesium losses Adversely impacts vitamin D and overall nutritional status Increased risk of falls
Osteoporosis Phosphorus – essential for bone formation Carbonated soft-drinks have negligible effect on calcium excretion High protein or sodium - increase urinary calcium losses Potassium, magnesium, fruits, vegetables associated with higher BMD
Osteoporosis Medical management Risk factor modification Dietary treatment Drug therapy
© 2007 Thomson - Wadsworth
Osteoporosis Pharmacologic prevention and treatment Estrogens/ hormone therapy Selective estrogen receptor modulators (SERMs) Bisphonates Teriparatide (synthetic PTH) Drug-nutrient interactions
Paget Disease Localized, progressive, crippling disorder of bone remodeling d/t overactive osteoclasts and bone resorption followed by rapid formation of new bone which is structurally inferior Bowing, deformity, fracture, poor healing Upper femur, pelvis, vertebral bodies, skull, tibia Genetic and viral factors Adequate intake of vitamin D and calcium important
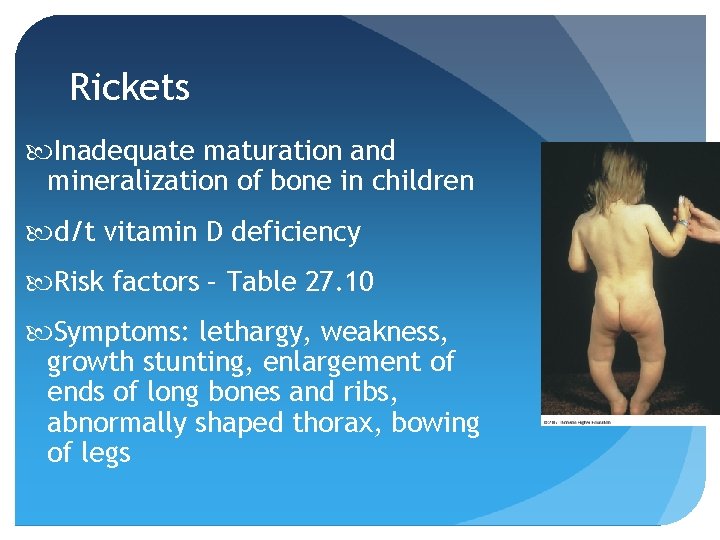
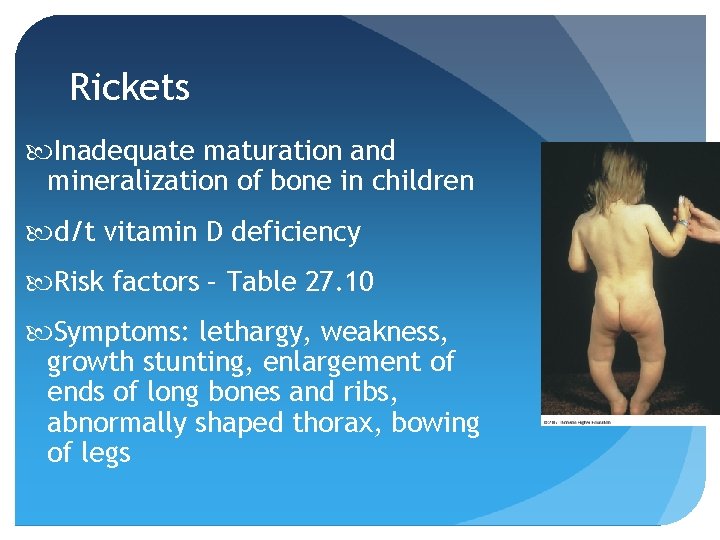
Rickets Inadequate maturation and mineralization of bone in children d/t vitamin D deficiency Risk factors – Table 27. 10 Symptoms: lethargy, weakness, growth stunting, enlargement of ends of long bones and ribs, abnormally shaped thorax, bowing of legs

Rickets Prevention Exclusively breast fed infants should receive supplement of 200 IU vitamin D Fortified infant formulas If receiving less than 500 m. L/day, should be given multivitamin supplement After 1 year – vitamin D-fortified cow’s milk
Rickets Treatment Balanced, age-appropriate diet Adequate vitamin D, calcium, phosphorus
Osteomalacia Organic matrix of bones inadequately mineralized in adults Muscular weakness, bone pain, deformities of ribs, pelvis, legs d/t vitamin D deficiency, impaired D action, calcium deficiency, hypophosphatemia
Osteomalacia Treatment Address underlying cause Multivitamin supplementation Calcium supplementation Pharmacological doses of vitamin D
Arthritic Conditions Affect joints, tissues surrounding joints, and connective tissues Osteoarthritis, rheumatoid arthritis, gout (affecting all ages) Risk factors - modifiable: Overweight Joint injuries Infections
Arthritic Conditions Risk factors - nonmodifiable: Female sex – 60% of cases Age Family hx
Osteoarthritis Most common, leading cause of physical disability Disease process involving all structures of the joint Loss of load-bearing articular cartilage Inflammation Joint pain, stiffness, limited movement, wasting of periarticular muscles, joint instability and deformity

Osteoarthritis Major risk factors Age Female sex Family hx Major trauma to joint or soft tissue Repetitive joint stress related to occupation Obesity
Osteoarthritis Treatment Reduce joint inflammation & pain, maintain mobility, minimize disability Improve body posture Proper footwear Weight reduction Periodic rest of affected joint Heat Physical activity/ therapeutic exercise
Osteoarthritis Treatment Drug therapy – pain relief NSAIDs Glucosamine and chondroitin
Rheumatoid Arthritis Chronic inflammatory disease; synovial membrane becomes inflamed resulting in swelling, stiffness, pain, limited range of motion, joint deformity, disability Characterized by periods of exacerbation and remission Autoimmune response
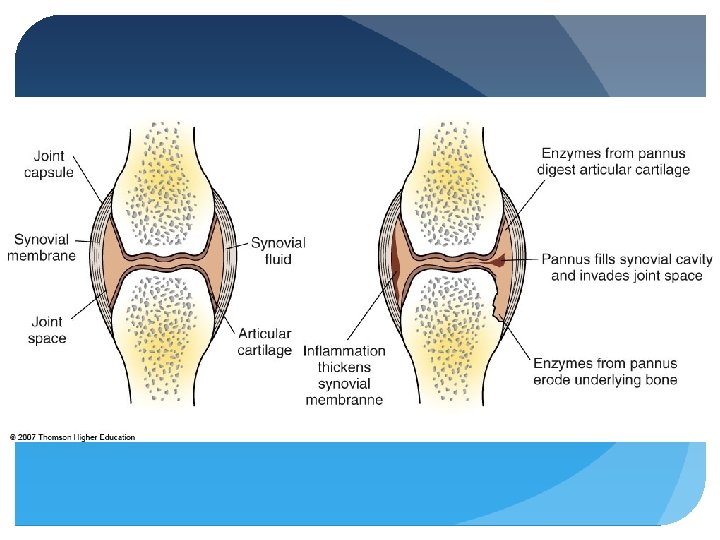
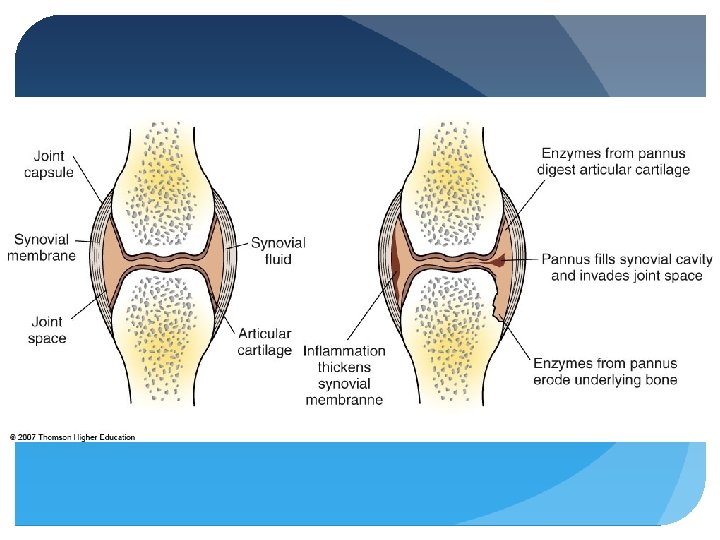
Rheumatoid Arthritis Inflammation of joints of hands, wrists, knees, & feet results in warmth, redness, swelling, stiffness, and pain Inflammation results in thickening of synovial membrane known as pannus – see Fig. 27. 10 Enzymes from pannus digest adjacent bone and cartilage
Rheumatoid Arthritis Treatment Reduce pain and inflammation, protect joint, maintain function, control systemic infections Pharmacological agents: NSAIDs, glucocorticoids, immunosuppressives, DMARDs
Rheumatoid Arthritis Diet Increase consumption of fruits and vegetables/ antioxidants Include sources of EPA and DHA Fish oil supplementation Exclusion of red meats, dairy, cereals, wheat gluten Evaluate and test for food allergy
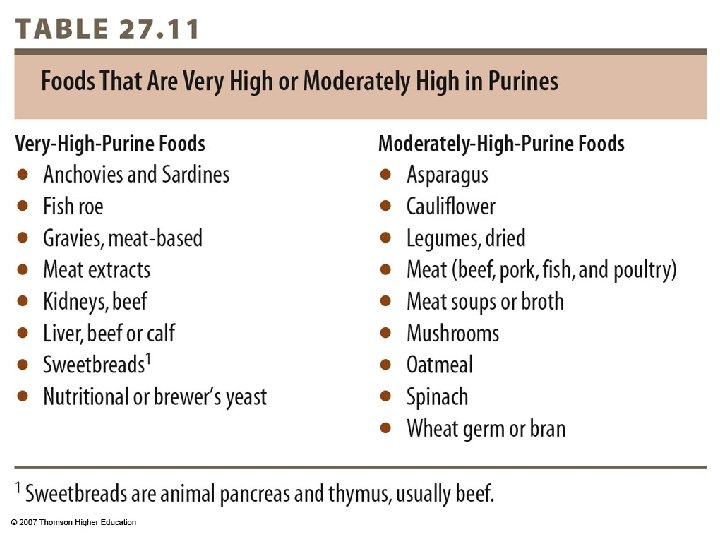
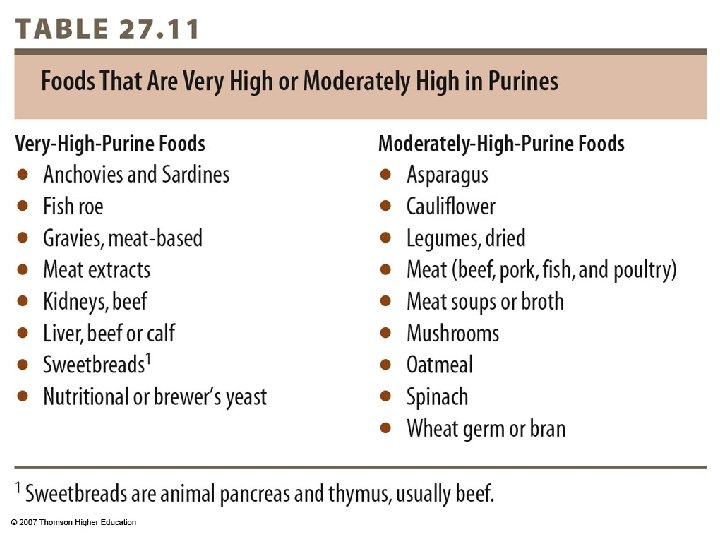
Gout Inflammatory disease resulting in swelling, redness, heat, pain, and stiffness in affected joint d/t elevated serum concentrations of uric acid, formation of uric acid crystals End product of purine (adenine and guanine) metabolism
Gout Hyperuricemia results from overproduction of uric acid, inadequate elimination by the kidneys, or combination Most painful arthritic condition Risk factors: genetics, male sex, older age, overweight, excessive alcohol consumption, eating foods rich in purines, exposure to lead, certain drugs
Gout Most commonly affects great toe, instep, ankles, heels, knees, wrists, elbows, fingers Rapid occurrence Sudden severe pain; swelling; shiny, red skin around joint; extreme tenderness Typically resolves 5 -10 days, may reoccur
Gout Acute attack may be precipitated by: Excessive exercise Certain medications: aspirin, diuretics, nicotinic acid, cyclosporine, levodopa Purine-rich foods Excessive alcohol consumption Crash dieting
© 2007 Thomson - Wadsworth

Gout Treatment: NSAIDs, glucocorticoids, colchicine Treat uricemia Lifestyle modifications
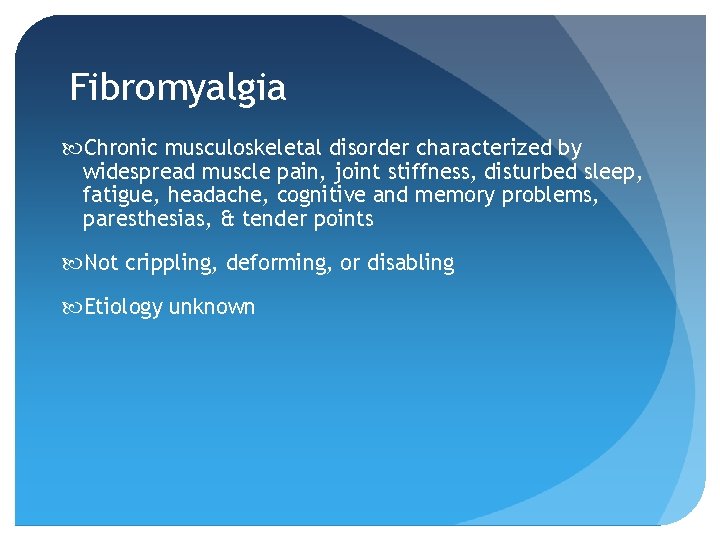
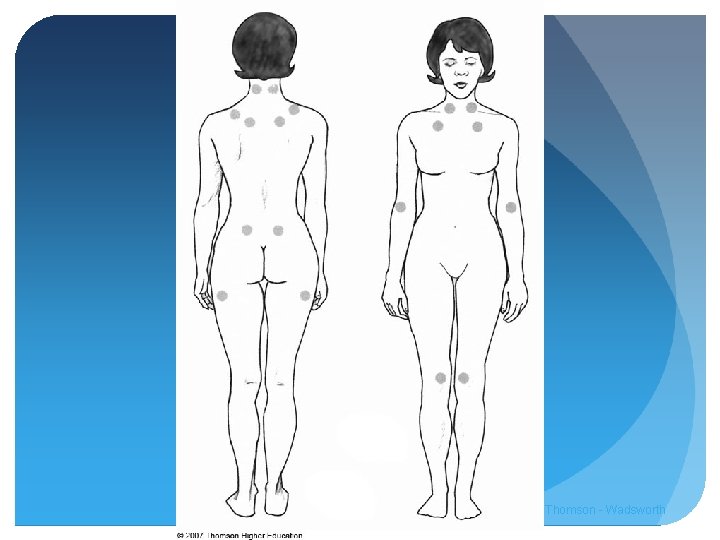
Fibromyalgia Chronic musculoskeletal disorder characterized by widespread muscle pain, joint stiffness, disturbed sleep, fatigue, headache, cognitive and memory problems, paresthesias, & tender points Not crippling, deforming, or disabling Etiology unknown
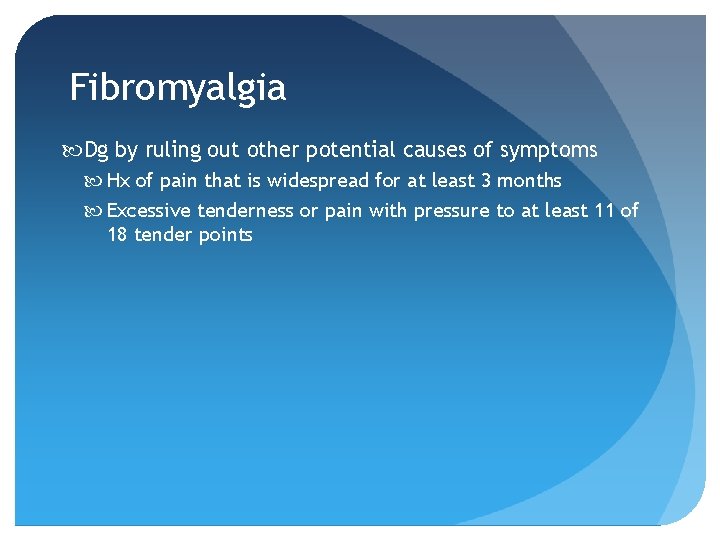
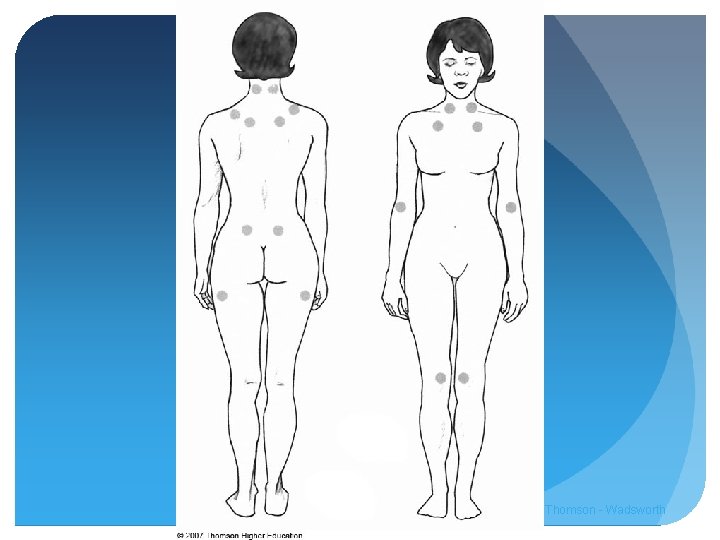
Fibromyalgia Dg by ruling out other potential causes of symptoms Hx of pain that is widespread for at least 3 months Excessive tenderness or pain with pressure to at least 11 of 18 tender points
© 2007 Thomson - Wadsworth
Fibromyalgia Treatment Improve sleep, treat depression, anxiety and pain, improve ability to relax Antidepressants, counseling Regular physical activity Cognitive behavioral therapy Intensive patient education
Fibromyalgia Diet Avoidance of certain foods has worked for some Low-sodium, uncooked vegan diet has shown promise ? MSG avoidance Lack of sound scientific evidence at this time
 Respiratory system maintain homeostasis
Respiratory system maintain homeostasis Knh
Knh Knh
Knh Fin 413
Fin 413 Doe evms
Doe evms Cs 413 bilkent
Cs 413 bilkent Hino 413
Hino 413 Read pp
Read pp 500 en yakın onluğa yuvarlama
500 en yakın onluğa yuvarlama Slidetodoc.com
Slidetodoc.com A 413
A 413 Doe 413 evms
Doe 413 evms Chapter 21 the musculoskeletal system
Chapter 21 the musculoskeletal system Musculoskeletal system
Musculoskeletal system Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders Chapter 15 musculoskeletal system
Chapter 15 musculoskeletal system Unit 41 musculoskeletal system
Unit 41 musculoskeletal system Musculoskeletal system
Musculoskeletal system Musculoskeletal system medical terminology
Musculoskeletal system medical terminology Diseases of the musculoskeletal system
Diseases of the musculoskeletal system Assessment of the musculoskeletal system
Assessment of the musculoskeletal system Muscle strength scale
Muscle strength scale Musculoskeletal system
Musculoskeletal system Objective data for musculoskeletal system
Objective data for musculoskeletal system Ovary diagram
Ovary diagram Musculoskeletal icd 10
Musculoskeletal icd 10 Kode icd 10 fraktur coccygeus
Kode icd 10 fraktur coccygeus Chapter 41 musculoskeletal care modalities
Chapter 41 musculoskeletal care modalities Chapter 24 the child with a musculoskeletal condition
Chapter 24 the child with a musculoskeletal condition Musculoskeletal fitness
Musculoskeletal fitness Work related musculoskeletal disorders definition
Work related musculoskeletal disorders definition Musculoskeletal pronounce
Musculoskeletal pronounce West coast musculoskeletal
West coast musculoskeletal Mpsq
Mpsq Subcostal retractions
Subcostal retractions Musculoskeletal integrity
Musculoskeletal integrity Musculoskeletal injury
Musculoskeletal injury Musculoskeletal
Musculoskeletal Musculoskeletal
Musculoskeletal Sathish srinivasan
Sathish srinivasan Cochrane musculoskeletal group
Cochrane musculoskeletal group Musculoskeletal mri anatomy
Musculoskeletal mri anatomy Splenocolic ligament
Splenocolic ligament Thyrohyoid membrane is pierced by
Thyrohyoid membrane is pierced by Arteries of the gluteal region
Arteries of the gluteal region Cow eye dissection steps
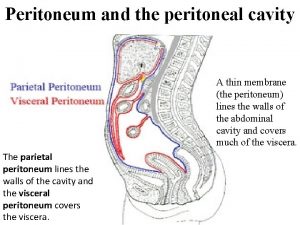
Cow eye dissection steps Parietal and visceral peritoneum
Parietal and visceral peritoneum Alveolar crest
Alveolar crest Diaphragmatic surface of liver
Diaphragmatic surface of liver Triangular ligament liver
Triangular ligament liver Semons law
Semons law Cow eye pupil
Cow eye pupil Peritoneal space
Peritoneal space Spine landmarks
Spine landmarks Characteristics of ligaments
Characteristics of ligaments Pintos ligament
Pintos ligament Knee joint ligaments
Knee joint ligaments Ligaments in collarbone
Ligaments in collarbone Paracolic gutter
Paracolic gutter Articulatio cubiti ligaments
Articulatio cubiti ligaments Ligaments jaunes hypertrophiés
Ligaments jaunes hypertrophiés What are the nine parts of the nail unit
What are the nine parts of the nail unit Similar pictures
Similar pictures What type of connective tissue are tendons and ligaments
What type of connective tissue are tendons and ligaments Vena porta anatomy
Vena porta anatomy Muscles of the pelvic girdle
Muscles of the pelvic girdle Suspensory ligaments eye
Suspensory ligaments eye Voice box in respiratory system
Voice box in respiratory system Tendons in elbow
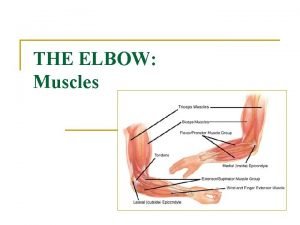
Tendons in elbow Leg tendons and ligaments
Leg tendons and ligaments Peroneus longus peroneus brevis
Peroneus longus peroneus brevis Ligament falciforme du foie
Ligament falciforme du foie Normal extension of shoulder
Normal extension of shoulder Pubocervical
Pubocervical