Musculoskeletal disorders Systemic Connective Tissue Disorders Inflammatory Joint


- Slides: 63
Musculoskeletal disorders • • • Systemic Connective Tissue Disorders Inflammatory Joint diseases Osteoarthritis Fibromyalgia Diseases of bone
SYSTEMIC CONNECTIVE TISSUE DISORDERS
SYSTEMIC CONNECTIVE TISSUE DISORDERS • • • SLE Scleroderma Mixed CTD Sjoren’s syndrome Polymyositis and dermatomyositis Systemic vasculitis
SYSTEMIC LUPUS ERYTHEMATOSUS (SLE)
• SLE is a chronic autoimmune multisystem connective tissue disease. • In autoimmune diseases, the immune system attacks the body’s cells and tissue, resulting in inflammation and tissue damage. • SLE most often affects the heart, joints, skin, lungs, blood vessels, liver, kidney, and nervous system. • The course of the disease is unpredictable, with periods of illness (called flares) alternating with remissions. • Peak age: 2 nd-3 rd decade • Female : male ratio =9: 1
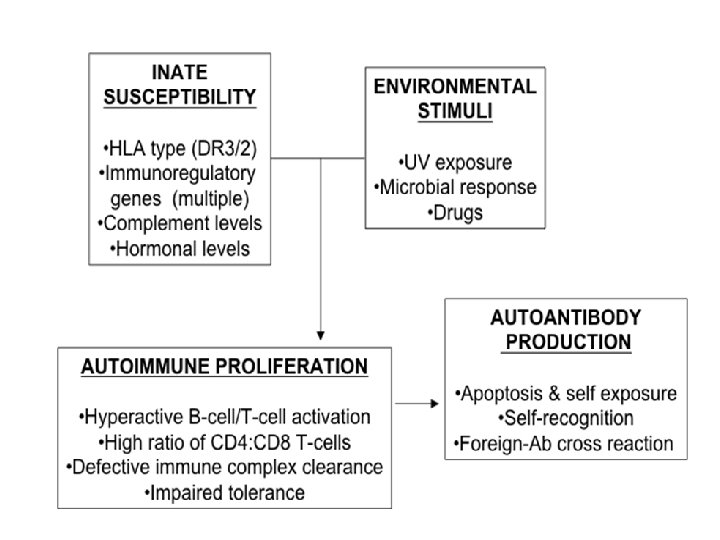
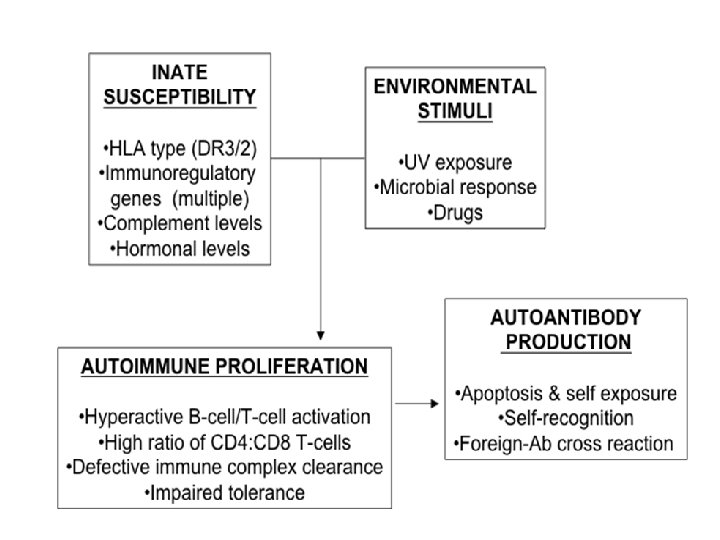
Etiology: • Exact cause of SLE is unknown. • The predisposing factors are: 1. Genetic predisposition – – – Genes are located in the HLA region on chromosome 6 Mutations may occur randomly (de novo) or it may be inherited When triggered by environmental factors 2. Environmental factors like : • • • UV rays(sunlight) Drugs: Hydralazine , procainamide , Isoniazid , methyldopa and chlorpromazipine, Penicillamine, sulfasalazine, lithium and lovastin Extreme stress Viral infection Pregnancy and puerperium
Pathogenesis: • This is Multifactorial disorder in which there is profound disturbance of immune regulation • Defect of suppressor T lymphocytes is associated with uncontrolled production of auto antibodies and immune complexes ØInflammatory process in SLE may occur by the two mechanisms: 1. Auto antibodies react with cell nuclei therefore antigen-antibody reaction results in inflammation. 2. Deposition of immune complexes in the tissues causing vasculitis.
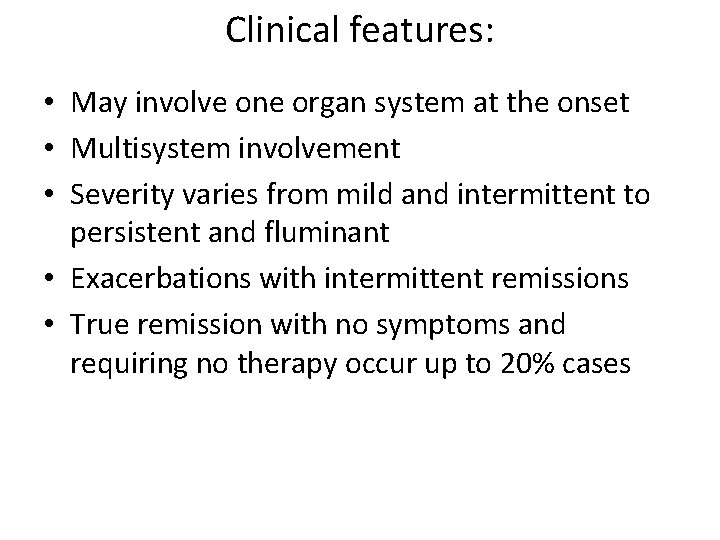
Clinical features: • May involve one organ system at the onset • Multisystem involvement • Severity varies from mild and intermittent to persistent and fluminant • Exacerbations with intermittent remissions • True remission with no symptoms and requiring no therapy occur up to 20% cases
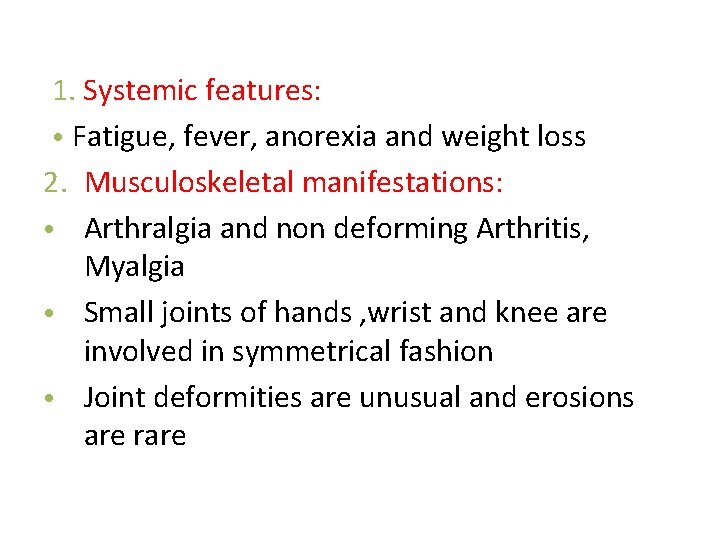
1. Systemic features: • Fatigue, fever, anorexia and weight loss 2. Musculoskeletal manifestations: • Arthralgia and non deforming Arthritis, Myalgia • Small joints of hands , wrist and knee are involved in symmetrical fashion • Joint deformities are unusual and erosions are rare
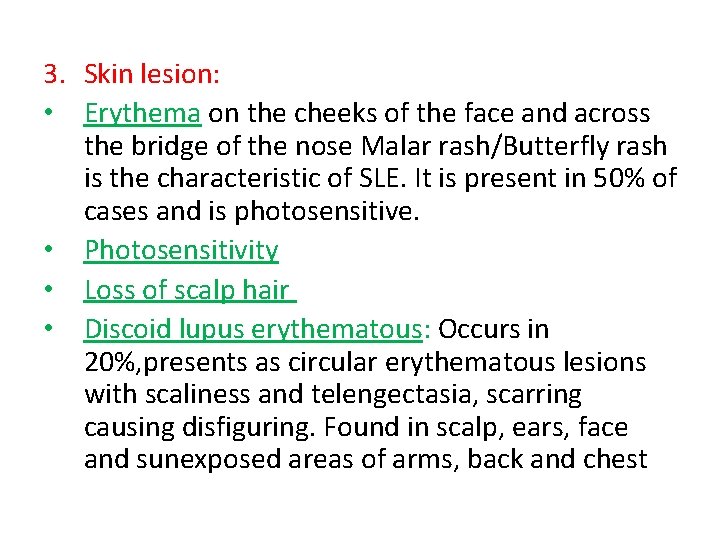
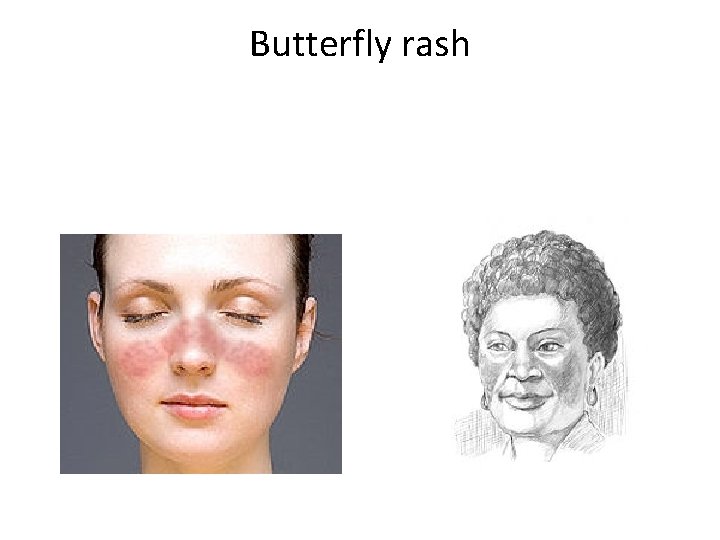
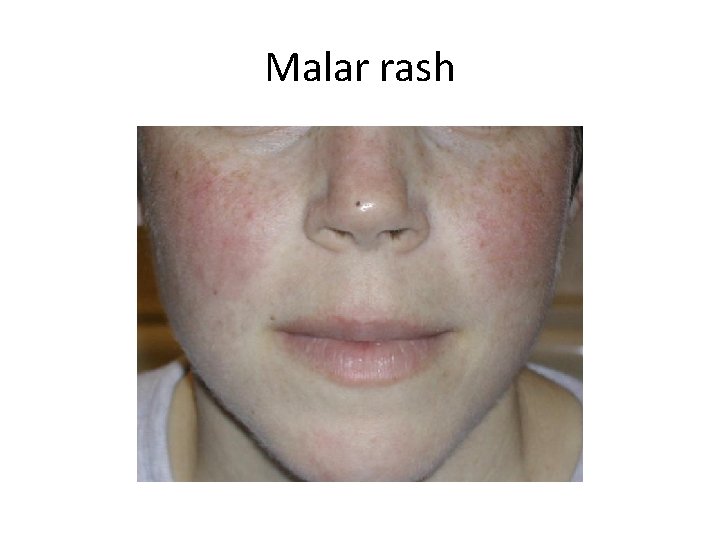
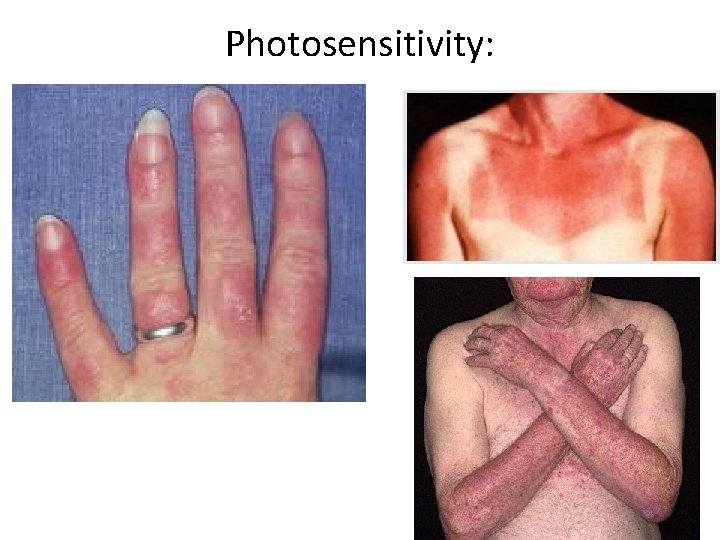
3. Skin lesion: • Erythema on the cheeks of the face and across the bridge of the nose Malar rash/Butterfly rash is the characteristic of SLE. It is present in 50% of cases and is photosensitive. • Photosensitivity • Loss of scalp hair • Discoid lupus erythematous: Occurs in 20%, presents as circular erythematous lesions with scaliness and telengectasia, scarring causing disfiguring. Found in scalp, ears, face and sunexposed areas of arms, back and chest
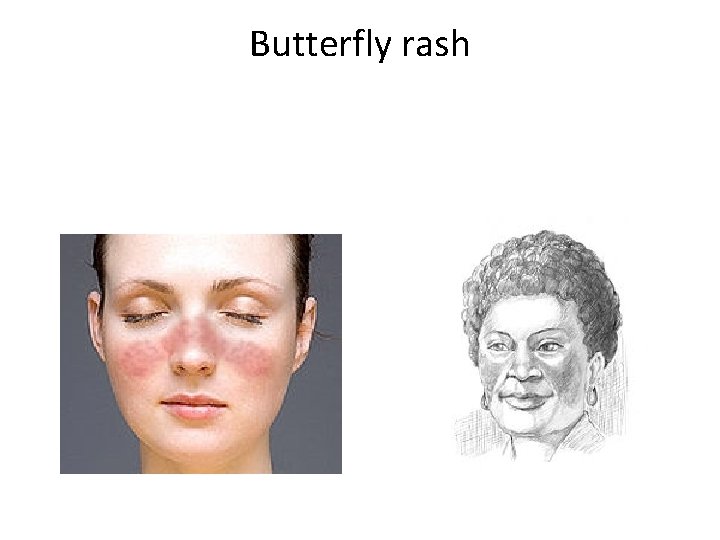
Butterfly rash
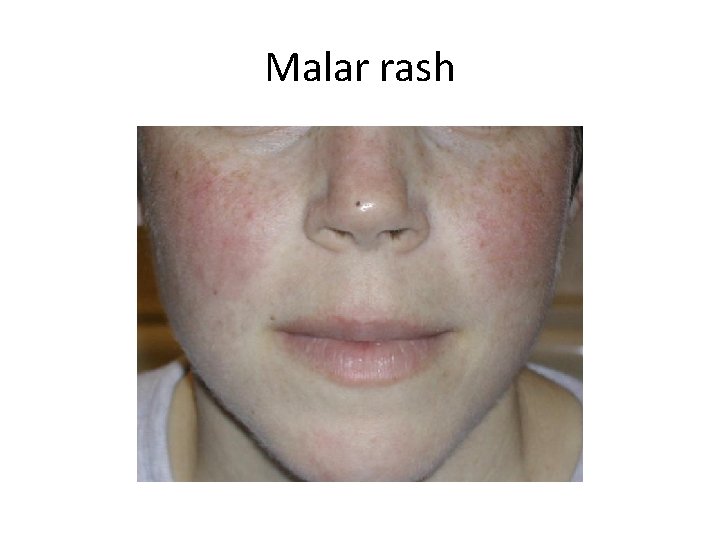
Malar rash
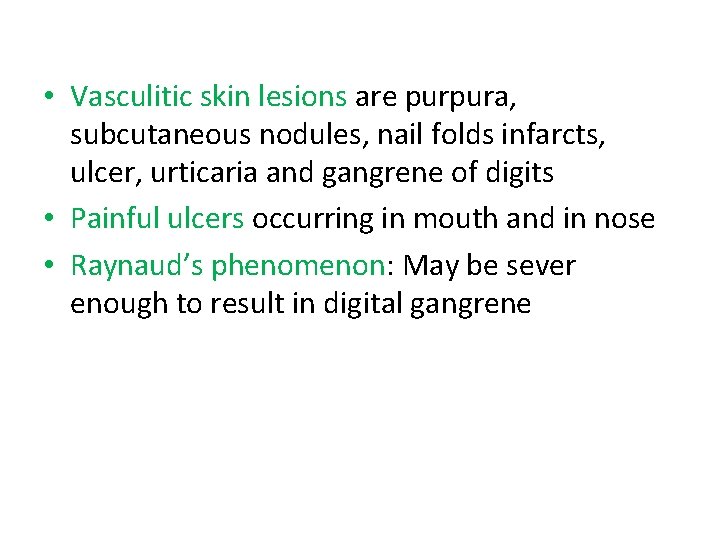
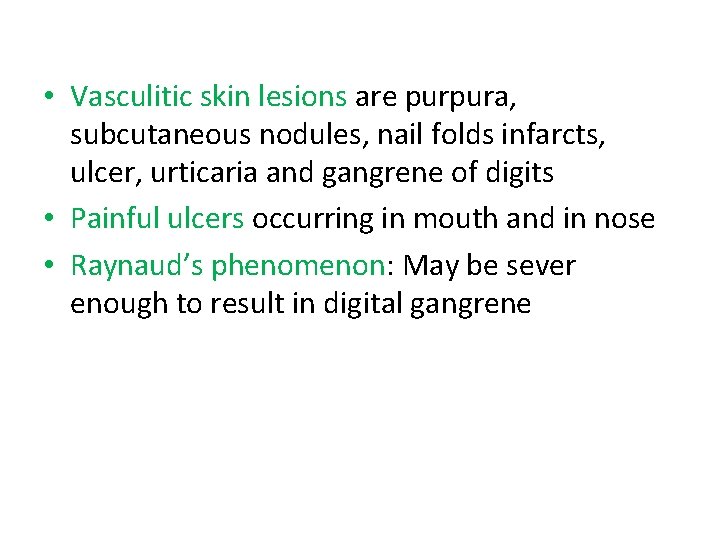
• Vasculitic skin lesions are purpura, subcutaneous nodules, nail folds infarcts, ulcer, urticaria and gangrene of digits • Painful ulcers occurring in mouth and in nose • Raynaud’s phenomenon: May be sever enough to result in digital gangrene

Raynaud’s phenomenon:
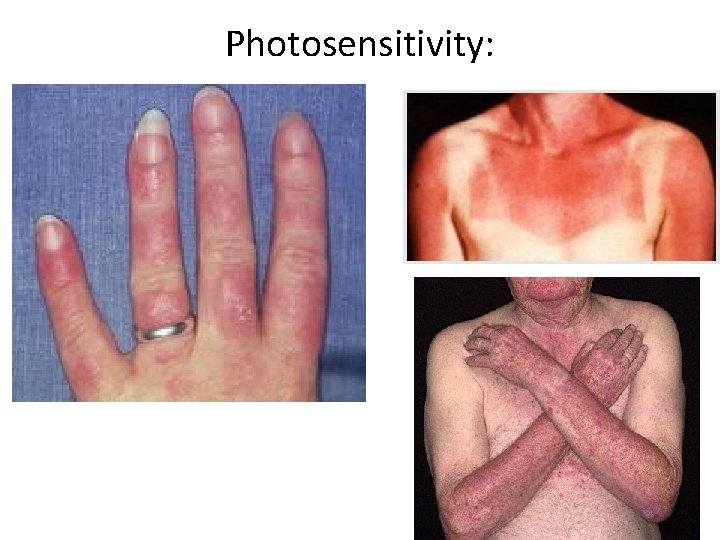
Photosensitivity:

Discoid rash
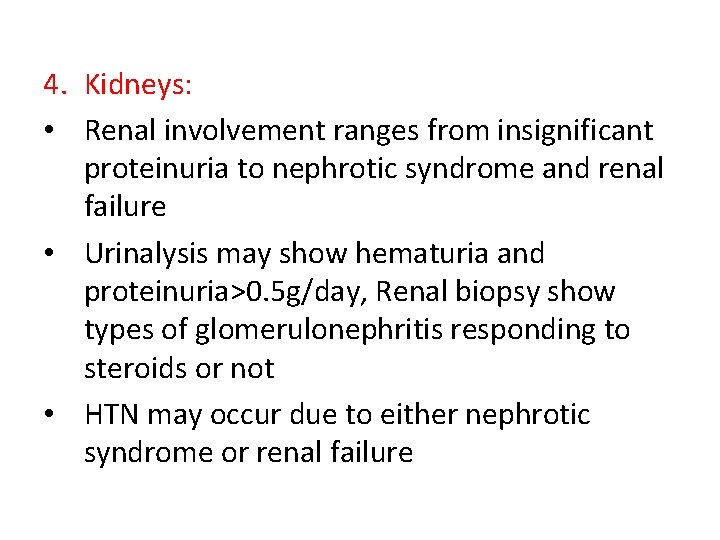
4. Kidneys: • Renal involvement ranges from insignificant proteinuria to nephrotic syndrome and renal failure • Urinalysis may show hematuria and proteinuria>0. 5 g/day, Renal biopsy show types of glomerulonephritis responding to steroids or not • HTN may occur due to either nephrotic syndrome or renal failure
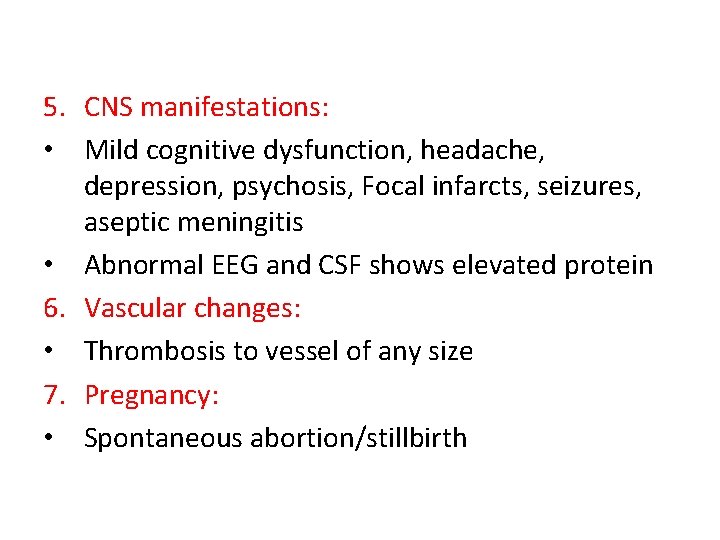
5. CNS manifestations: • Mild cognitive dysfunction, headache, depression, psychosis, Focal infarcts, seizures, aseptic meningitis • Abnormal EEG and CSF shows elevated protein 6. Vascular changes: • Thrombosis to vessel of any size 7. Pregnancy: • Spontaneous abortion/stillbirth
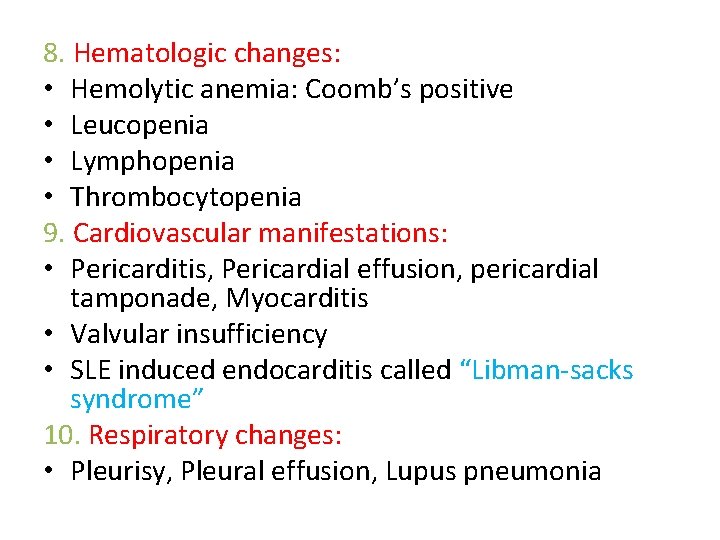
8. Hematologic changes: • Hemolytic anemia: Coomb’s positive • Leucopenia • Lymphopenia • Thrombocytopenia 9. Cardiovascular manifestations: • Pericarditis, Pericardial effusion, pericardial tamponade, Myocarditis • Valvular insufficiency • SLE induced endocarditis called “Libman-sacks syndrome” 10. Respiratory changes: • Pleurisy, Pleural effusion, Lupus pneumonia
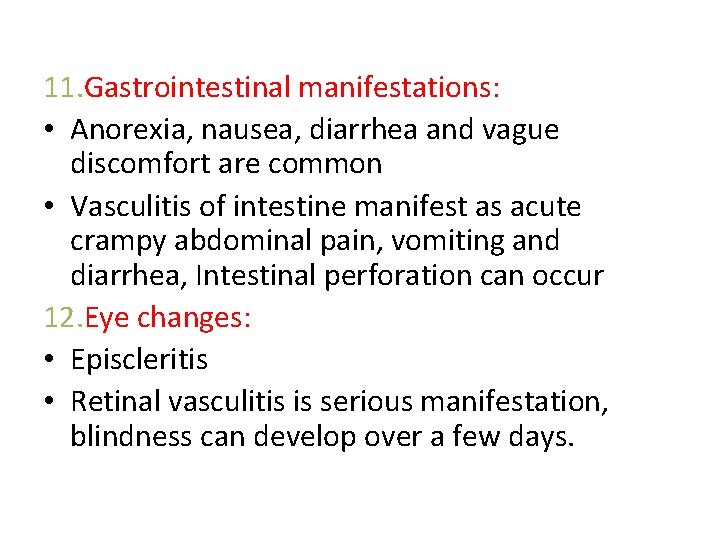
11. Gastrointestinal manifestations: • Anorexia, nausea, diarrhea and vague discomfort are common • Vasculitis of intestine manifest as acute crampy abdominal pain, vomiting and diarrhea, Intestinal perforation can occur 12. Eye changes: • Episcleritis • Retinal vasculitis is serious manifestation, blindness can develop over a few days.
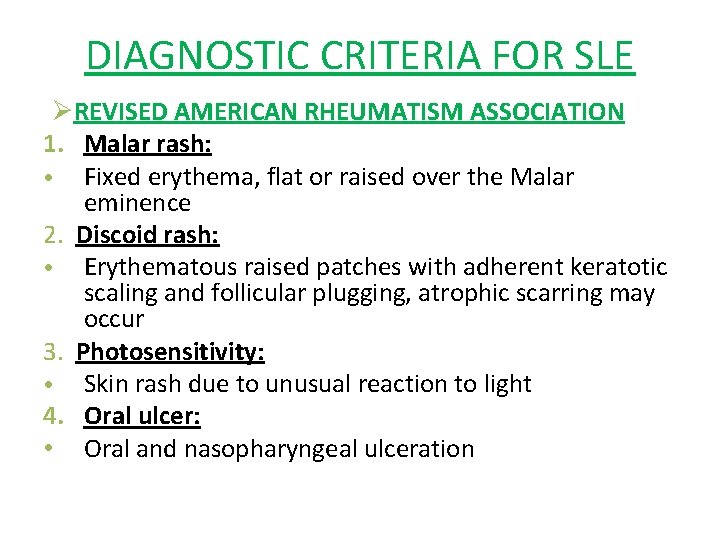
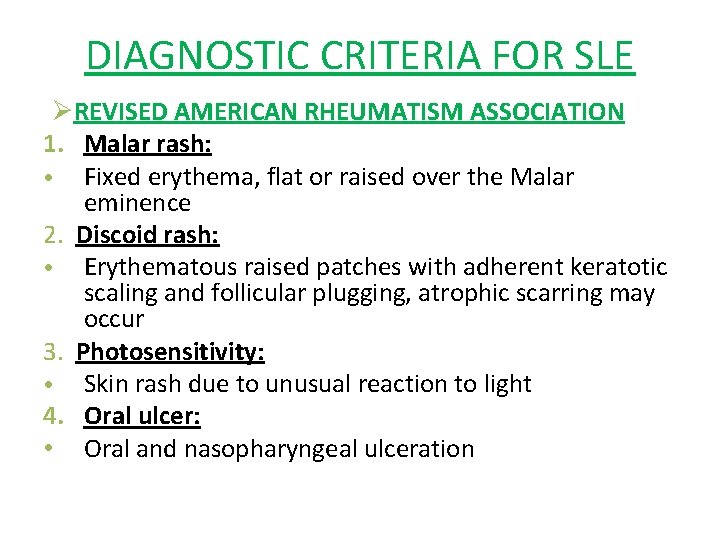
DIAGNOSTIC CRITERIA FOR SLE ØREVISED AMERICAN RHEUMATISM ASSOCIATION 1. Malar rash: • Fixed erythema, flat or raised over the Malar eminence 2. Discoid rash: • Erythematous raised patches with adherent keratotic scaling and follicular plugging, atrophic scarring may occur 3. Photosensitivity: • Skin rash due to unusual reaction to light 4. Oral ulcer: • Oral and nasopharyngeal ulceration
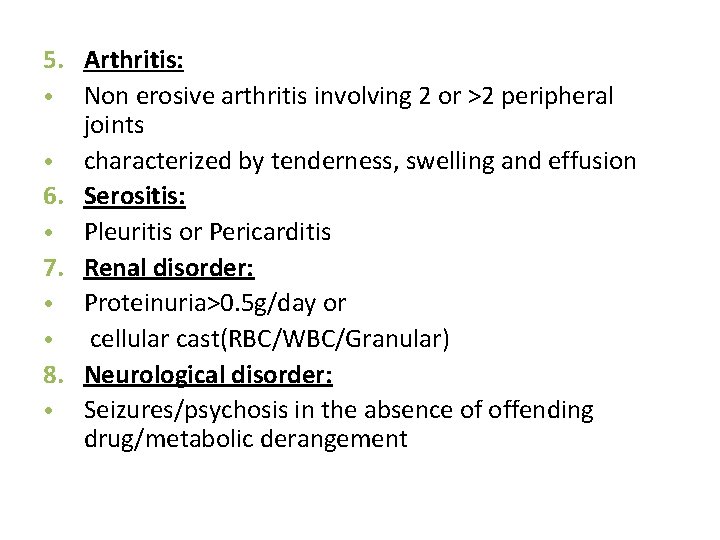
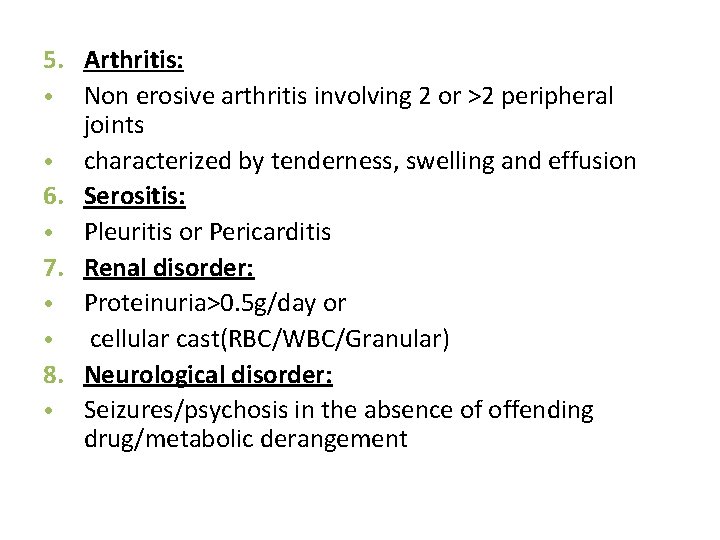
5. Arthritis: • Non erosive arthritis involving 2 or >2 peripheral joints • characterized by tenderness, swelling and effusion 6. Serositis: • Pleuritis or Pericarditis 7. Renal disorder: • Proteinuria>0. 5 g/day or • cellular cast(RBC/WBC/Granular) 8. Neurological disorder: • Seizures/psychosis in the absence of offending drug/metabolic derangement
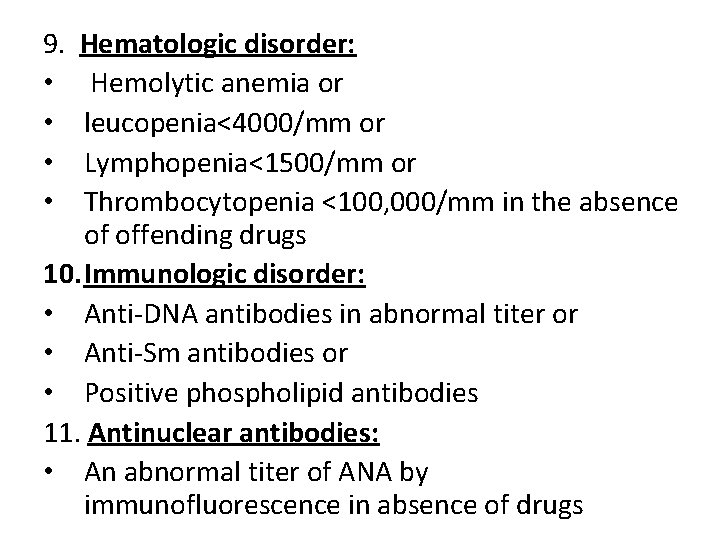
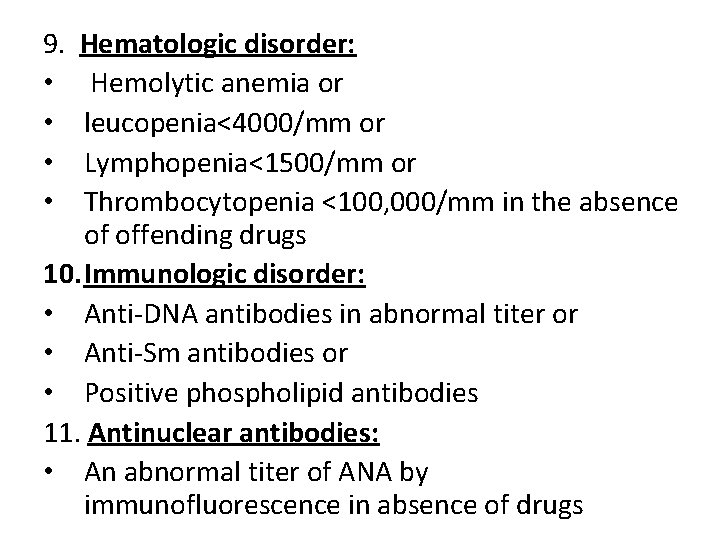
9. • • Hematologic disorder: Hemolytic anemia or leucopenia<4000/mm or Lymphopenia<1500/mm or Thrombocytopenia <100, 000/mm in the absence of offending drugs 10. Immunologic disorder: • Anti-DNA antibodies in abnormal titer or • Anti-Sm antibodies or • Positive phospholipid antibodies 11. Antinuclear antibodies: • An abnormal titer of ANA by immunofluorescence in absence of drugs
Diagnosis: • Presence of 4 criteria at anytime during course of disease. • Specificity: 98% • Sensitivity: 97%
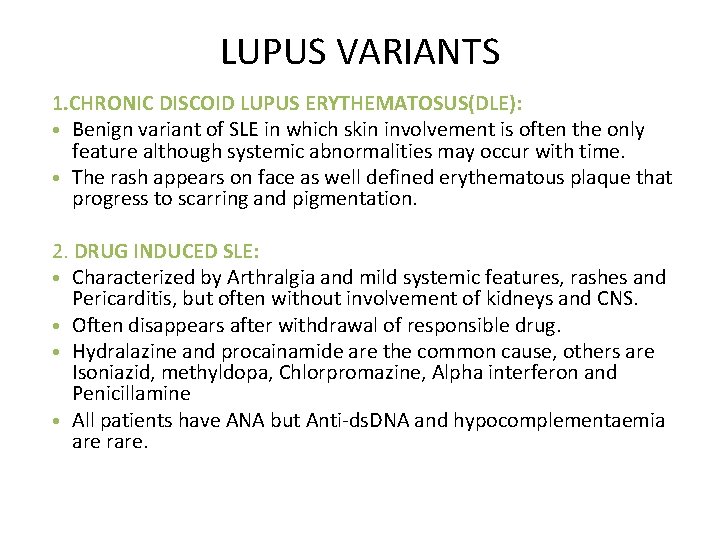
LUPUS VARIANTS 1. CHRONIC DISCOID LUPUS ERYTHEMATOSUS(DLE): • Benign variant of SLE in which skin involvement is often the only feature although systemic abnormalities may occur with time. • The rash appears on face as well defined erythematous plaque that progress to scarring and pigmentation. 2. DRUG INDUCED SLE: • Characterized by Arthralgia and mild systemic features, rashes and Pericarditis, but often without involvement of kidneys and CNS. • Often disappears after withdrawal of responsible drug. • Hydralazine and procainamide are the common cause, others are Isoniazid, methyldopa, Chlorpromazine, Alpha interferon and Penicillamine • All patients have ANA but Anti-ds. DNA and hypocomplementaemia are rare.
3. SLE AND PREGNANCY: • SLE patients in remission are not likely to have exacerbations during pregnancy, however women with active SLE, especially those with renal disease, have increased frequency of exacerbations of their disease. • Pre-eclampsia is a frequent complication of pregnancy • Fertility rates are normal but spontaneous abortion occur in 10 -30% of women. • Disease flares in a small proportion, especially during the first weeks of postpartum
Prognosis: • Disease pursues a relapsing and remitting course. • 10 year survival rates are >85% • In some patients there is severe impairment of vital organs such as lungs, heart, brain or kidneys • Infection specially with opportunistic organisms have become the number one cause of death followed by active SLE, mainly due to renal and CNS disease.
Poor prognostic factors: • Hypertension • High serum creatinine • Anemia • Hypoalbuminemia • Hypocomplementaemia at the time of diagnosis • Thrombocytopenia • Severe CNS involvement • Presence of antibodies against Phospholipids § 20% patients achieve remissions-transient § Likelihood of remission increase with each decade after diagnosis § Increase morbidity § Death due to: Renal failure and Thrombo-embolism
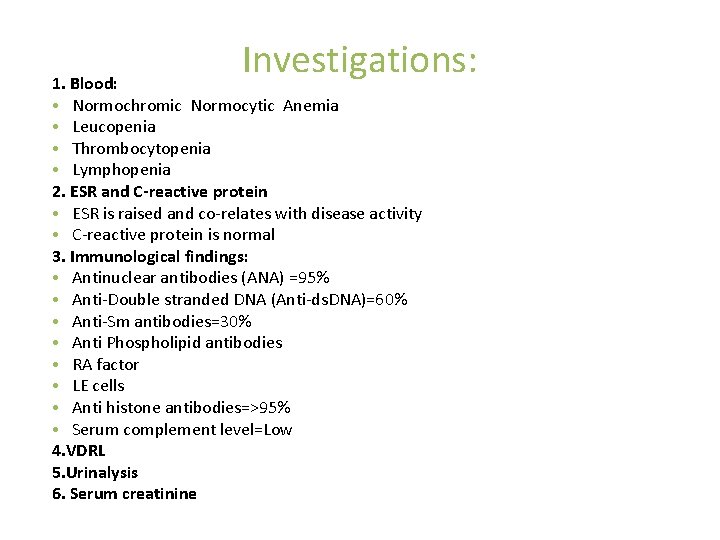
Investigations: 1. Blood: • Normochromic Normocytic Anemia • Leucopenia • Thrombocytopenia • Lymphopenia 2. ESR and C-reactive protein • ESR is raised and co-relates with disease activity • C-reactive protein is normal 3. Immunological findings: • Antinuclear antibodies (ANA) =95% • Anti-Double stranded DNA (Anti-ds. DNA)=60% • Anti-Sm antibodies=30% • Anti Phospholipid antibodies • RA factor • LE cells • Anti histone antibodies=>95% • Serum complement level=Low 4. VDRL 5. Urinalysis 6. Serum creatinine
Treatment: • There is no cure of SLE therefore management plan is: 1. To control exacerbation 2. To suppress symptoms to an acceptable level 3. Treatment option depends upon severity of disease.
1. NSAIDS: • Mild disease with Arthralgia, arthritis, fever and mild Serositis 2. Glucocorticoids: • Systemic Glucocorticoids are reserved for patients with life threating manifestations of SLE such as CNS or Renal involvement, myocarditis, Pericarditis or significant thrombocytopenia • In active SLE with fever and pleurisy start Prednisolone 1 -2 mg/kg orally in 2 -3 divided doses • After the controlling of disease only one morning dose is given • Thereafter the daily dose should be tapered. • With remission of disease withdraw steroids after few weeks or kept to maintenance level of around 10 -15 mg daily or alternate day regimen
• In life threating, severely disabling patients including those with proliferative glomerulonephritis can be started with 3 -5 days of 1 g IV “Pulses” of Methylprednisolone followed by maintenance dose of daily or alternate day Prednisolone.
Steroid pulse therapy: • Prednisolone 40 -60 mg/day • Methylprednisolone 0. 5 -1 g/day Cyclophosphamide pulse therapy: • 500 -750 mg/m 2 monthly and • Monthly for every 6 months • 3 monthly for 6 months then • Every 6 months once for 2 years ADR: Hemorrhagic cystitis, Bone marrow suppression, Hepatotoxicity
3. Chloroquine: • Useful in management of troublesome skin lesions or Arthralgia that cannot be controlled with NSAIDS • Dose of Hydroxychloroquine is 400 mg daily 4. Immunosuppressive drugs: • Drugs such as Azathioprine, Cyclophosphamide and Chlorambucil are used in: 1. Patients with severe focal or diffuse proliferative Glomerulonephritis not responding adequately to corticosteroids. 2. Patients in whom maintenance dose of steroid is so high as to cause severe side effects 3. Steroid resistant patients. 5. Immunomodulators: • Mycophenolate mofetil • Tacrolimus
Monitoring: • • Complete blood count: TLC, DLC, Hb, Platelet Urine: Proteinuria, cast ANA level Anti-d. S-DNA
SCLERODERMA
• This is a generalized connective tissue disorder characterized by fibrosis and degenerative changes in the skin , Blood vessels and Visceral organs. Etiology and incidence: • Unknown , May be immunologically mediated • Environmental risk factors : Silica dust, Vinyl chloride, Resins • F: M ratio=4: 1 • Peak age of onset: 30 -50 years
Types of Scleroderma: • Scleroderma is classified according to degree and extent of skin thickening 1. Systemic scleroderma: • Diffuse Cutaneous scleroderma • Limited Cutaneous scleroderma 2. Localized scleroderma: • Morphea • Linear scleroderma 3. In combination of other connective tissue disease: • Overlap syndrome • Mixed connective tissue disease.
1. Systemic Scleroderma: Diffuse cutaneous scleroderma: • It is characterized by the rapid development of symmetric skin thickening or tightening of proximal and distal extremity, face, and trunk. • These patients are at greater risk for developing kidney and other visceral involvement early in the course of disease. Limited cutaneous scleroderma: • It is characterized by symmetric skin thickening limited to the distal extremities and face. • It is also called as CREST syndrome. [Calcinosis, Raynaud's phenomenon, Esophageal dysmotility, Sclerodactyly, and Telengectasia] • Prognosis is better than diffuse variety because of much lower frequency of internal organ involvement.
2. Localized scleroderma: • It is limited to skin, subcutaneous tissue and muscle without systemic involvement. 1. Morphea: • Occurs as a single or multiple plaques of skin indurations and skin discoloration which evolve in sclerotic lesions 2. Linear scleroderma: • It appears as a linear streaks or bands most commonly on extremities and less frequently on forehead, trunk or fronto-parietal scalp.
Clinical features: 1. Raynaud’s phenomenon: • Severe Raynaud’s phenomenon is usually the presenting complaint. • It presents with three color changing, initially pallor, then blue due to peripheral cyanosis and then red due to reactive hyperemia along with tingling sensation. 2. Cutaneous changes: a. Hand: • Non pitting edema and indurations with restriction of movement • Later skin becomes shiny with atrophy and ulcerations of the finger tips b. Face: • In advanced cases the face may become taut and difficulty in opening the mouth. • Thinning and furrowing of the lips
3. Musculoskeletal: Arthralgia Mild non-erosive inflammatory arthritis Morning stiffness Muscle weakness and wasting due to tissue atrophy and low grade Myositis • Restricted hand movement. 4. GI: • Reflux oesophagitis • Esophageal dysmotility • Dysphasia and heart burn • Small bowel can be involved, producing Malabsorption from bacterial overgrowth due to dilatation and atony. • •
5. Respiratory: • Pulmonary hypertension • Lower lobe fibrosis leads to cyst formation and honeycombing in advance disease. 6. Cardiovascular: • Diffuse myocardial fibrosis with development of arrhythmias • Pericarditis , cardiomyopathy , heart block and aortic valve lesion may occur. 7. Renal: • Renal failure and malignant hypertension
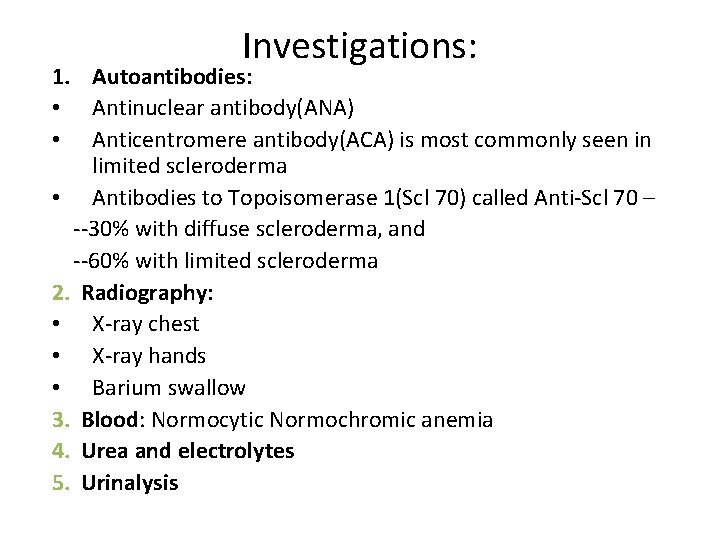
Investigations: 1. Autoantibodies: • Antinuclear antibody(ANA) • Anticentromere antibody(ACA) is most commonly seen in limited scleroderma • Antibodies to Topoisomerase 1(Scl 70) called Anti-Scl 70 – --30% with diffuse scleroderma, and --60% with limited scleroderma 2. Radiography: • X-ray chest • X-ray hands • Barium swallow 3. Blood: Normocytic Normochromic anemia 4. Urea and electrolytes 5. Urinalysis
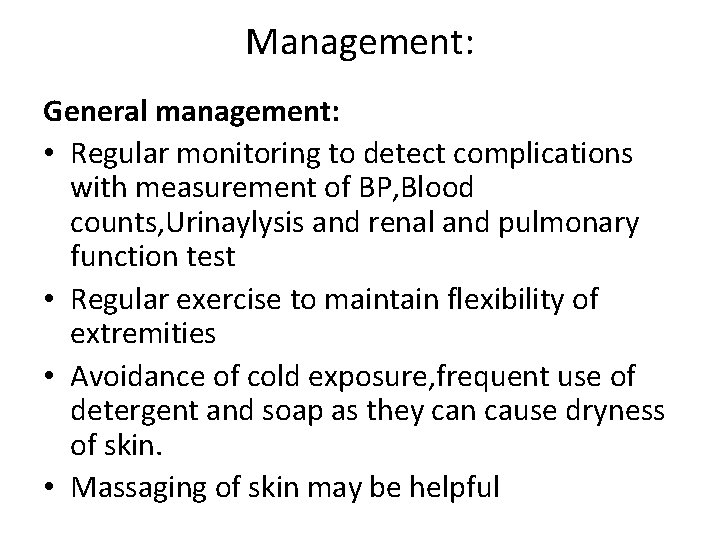
Management: General management: • Regular monitoring to detect complications with measurement of BP, Blood counts, Urinaylysis and renal and pulmonary function test • Regular exercise to maintain flexibility of extremities • Avoidance of cold exposure, frequent use of detergent and soap as they can cause dryness of skin. • Massaging of skin may be helpful
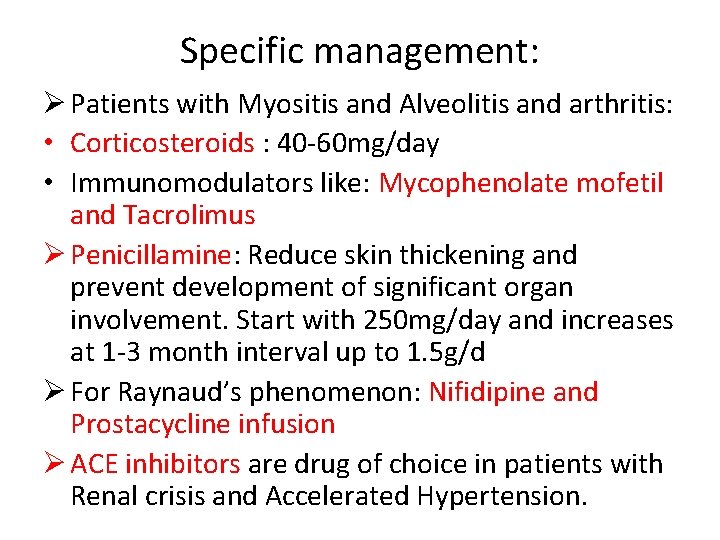
Specific management: Ø Patients with Myositis and Alveolitis and arthritis: • Corticosteroids : 40 -60 mg/day • Immunomodulators like: Mycophenolate mofetil and Tacrolimus Ø Penicillamine: Reduce skin thickening and prevent development of significant organ involvement. Start with 250 mg/day and increases at 1 -3 month interval up to 1. 5 g/d Ø For Raynaud’s phenomenon: Nifidipine and Prostacycline infusion Ø ACE inhibitors are drug of choice in patients with Renal crisis and Accelerated Hypertension.
POLYMYOSITIS AND DERMATOMYOSITIS
Polymyositis: • Disorder of the muscle in which the pathological features are necrosis of muscle fibers together with evidence of regeneration and inflammation. • It presents with proximal muscle weakness and wasting • When Polymyositis is accompanied by skin rash, it is called dermatomyositis.
DERMATOMYOSITIS • Autoimmune disease 1. Cutaneous: • Gottron’s papule • Heliotrope rash • Abnormal nail fold capillaries 2. Musculoskeletal: • Arthralgia • Myositis: Proximal muscle weakness, pain 3. Systemic • Fever, loss of weight Ø Investigations: • Creatinine kinase • EMG • Muscle biopsy
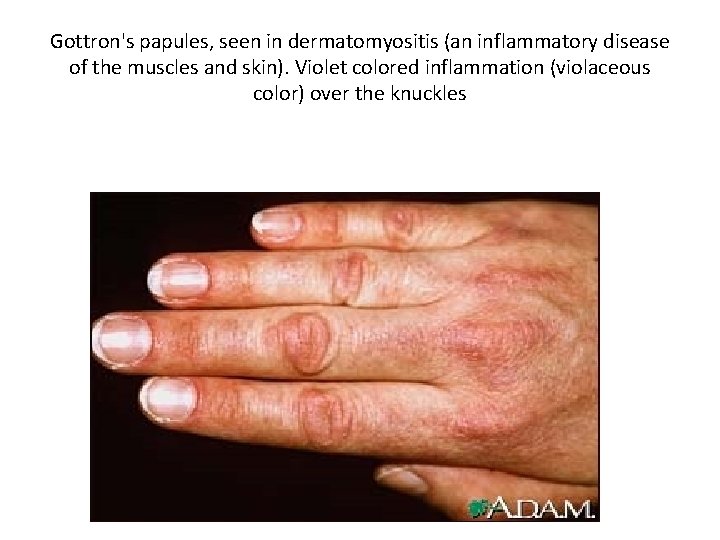
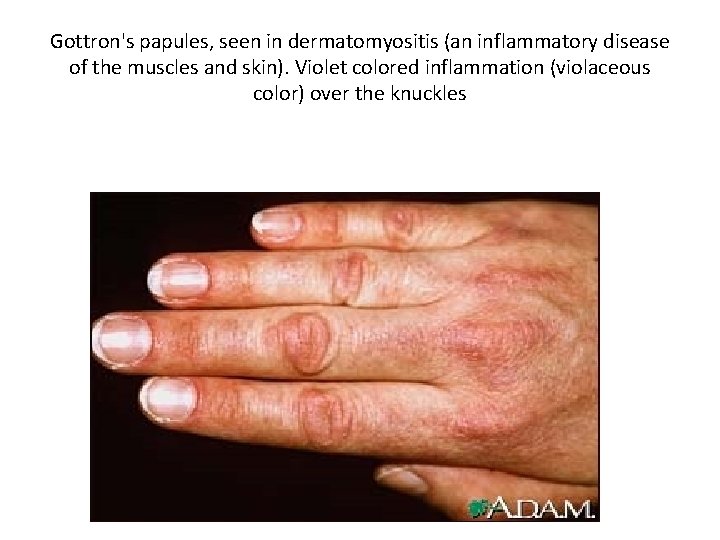
Gottron's papules, seen in dermatomyositis (an inflammatory disease of the muscles and skin). Violet colored inflammation (violaceous color) over the knuckles
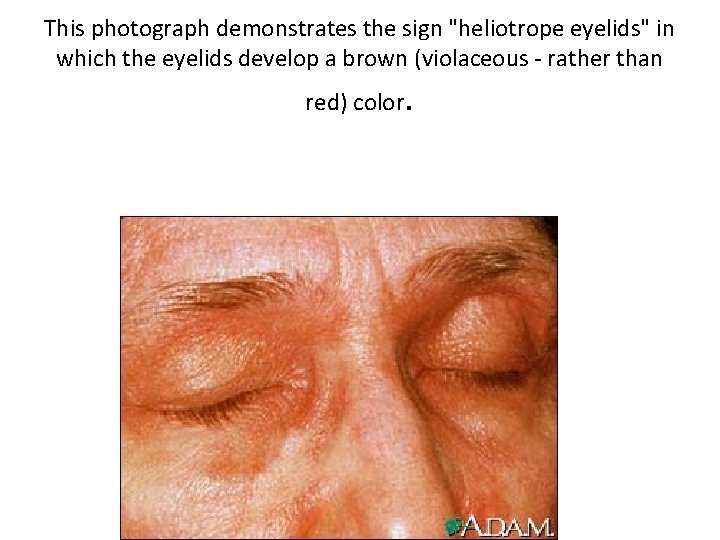
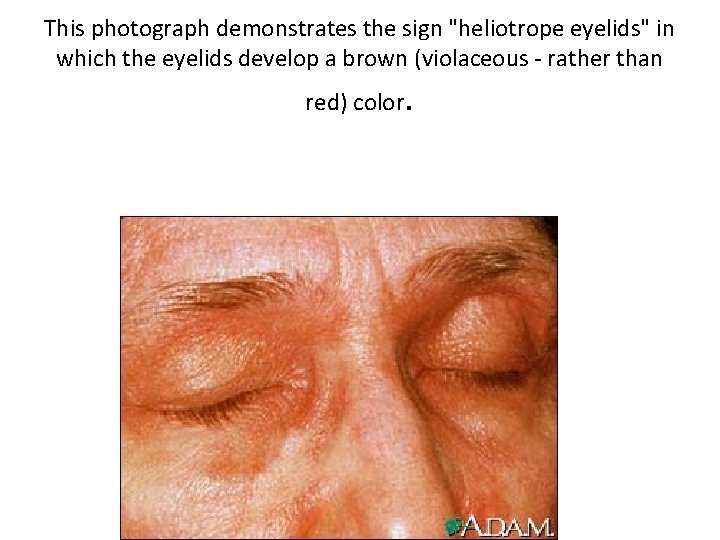
This photograph demonstrates the sign "heliotrope eyelids" in which the eyelids develop a brown (violaceous - rather than red) color .
Management: 1. Steroid: • Prednisolone 2. Immunosuppresive therapy: • Azathioprine • Methotrexate 3. Intravenous immunoglobulins
SJOGREN’S SYNDROME
SJOGREN’S SYNDROME • Autoimmune disorder of unknown etiology • Occurs as a result of chronic dysfunction of exocrine glands and is characterized by: § Dryness of mouth, eyes, and other areas covered by mucus membranes • Onset: 40 -50 years • F: M=9: 1
Clinical features: Ø Salivary gland lacrimal glands are mainly affected 1. Salavary gland enlargement • Decrease salivary secretion—Dryness of mouth i. e Xerostomia leading to difficulty in speaking and swallowing, and to severe dental caries. There may be loss of taste and smell 2. Ocular: • Decrease tear production • Keratoconjunctivitis sicca– Results from inadequate tear production caused by lymphocyte and plasma cell infitration of lacrimal glands 3. Pancreatitis, Pleuritis, neuropsychiatric dysfunction and vasculitis may be present. 4. Renal tubular acidosis and chronic interestitial nephritis may also occur.
Investigations: 1. Autoantibodies: • ANA • Rheumatoid Factor • Anti-Ro, Anti-La 2. Schirmer’s test • To determine/demonstrate decrease tear production 3. Raised ESR 4. Salivary gland biopsy
Management: 1. General • Artificial tear drop • Oral gel for shooting effect 2. Steroid : • Prednisolone 3. Immunosuppressive: • Azathioprine • Methotrexate.
MIXED CONNECTIVE TISSUE DISORDER
Mixed connective tissue disease(MCTD) v The condition is characterized by overlapping clinical features suggesting : – – SLE Scleroderma Rheumatoid arthritis Myositis v These conditions should be associated with very high titers of circulating autoantibodies to nuclear RNP, (Anti-n. RNP) v With time in many patients, the manifestations evolve to one of the predominant disease such as scleroderma or SLE
Clinical features: • Age: 3 rd-4 th decade, F: M=4: 1 • Raynaud’s phenomenon, Puffy hands, Arthralgia and myalgia are common presenting features • High grade fever, Polymyositis, Arthritis • Sclerodermal changes are usually limited to distal extremities • Some present with Butterfly rash and other features of SLE • Deformities of hands similar to RA may present without erosions • Esophageal dysmotility is present causing dysphagia: 70% • Lung involvement: Pleurisy, Diffuse interstitial Pulmonary fibrosis and Pulmonary Hypertension • ESR and Muscle enzymes are moderately raised
Investigation: • Anemia, Coomb’s test positive>60% • Leucopenia, Thrombocytopenia • Hypergammaglobinemia • RA factor positive in >50% Management: • Depends upon predominant cause.