MIHP NEW PROVIDER ORIENTATIO N DAY 5 2






- Slides: 92
MIHP NEW PROVIDER ORIENTATIO N DAY 5

2 Maternal Infant Health Program Quality
3 “SUCCESSFUL IMPLEMENTATION OF A QUALITY IMPROVEMENT PROGRAM BEGINS WITH AN HONEST AND OBJECTIVE ASSESSMENT OF AN ORGANIZATION'S CURRENT CULTURE, AND ITS COMMITMENT TO IMPROVING THE QUALITY OF ITS CARE AND SERVICES. ” RETRIEVED ON 4/3/18 FROM HTTP: //WWW. HRSA. GOV/QUALITY/TOOLBOX/METHODOLO GY/QUALITYIMPROVEMENT/
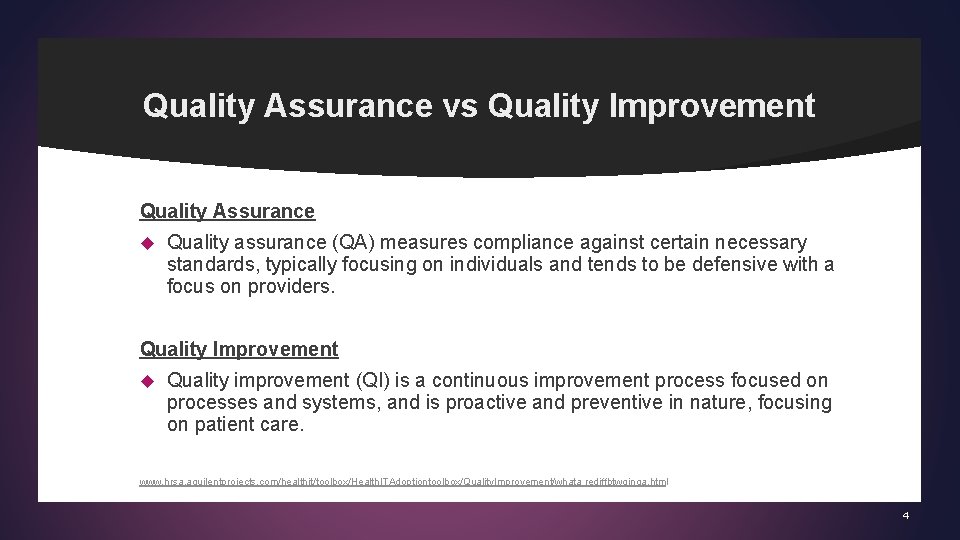
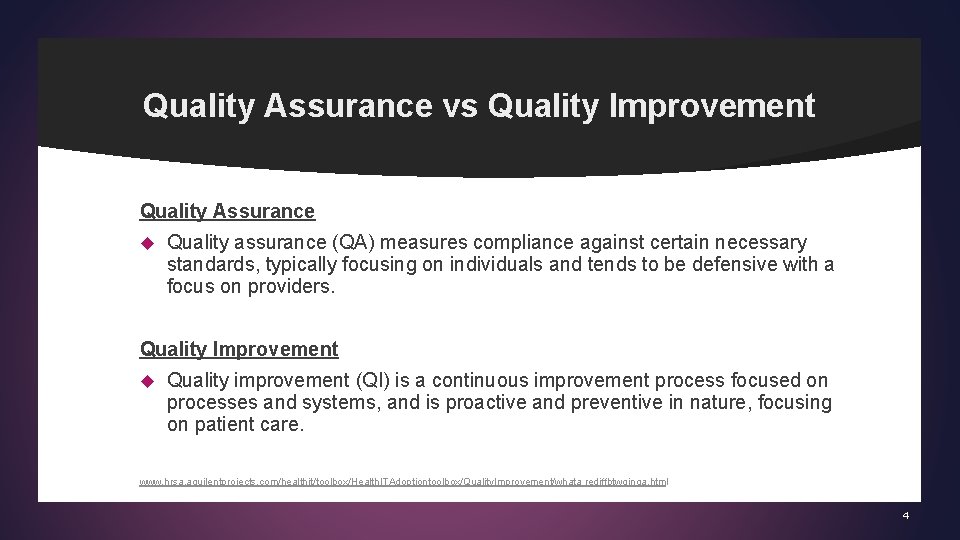
Quality Assurance vs Quality Improvement Quality Assurance Quality assurance (QA) measures compliance against certain necessary standards, typically focusing on individuals and tends to be defensive with a focus on providers. Quality Improvement Quality improvement (QI) is a continuous improvement process focused on processes and systems, and is proactive and preventive in nature, focusing on patient care. www. hrsa. aquilentprojects. com/healthit/toolbox/Health. ITAdoptiontoolbox/Quality. Improvement/whata rediffbtwqinqa. html 4
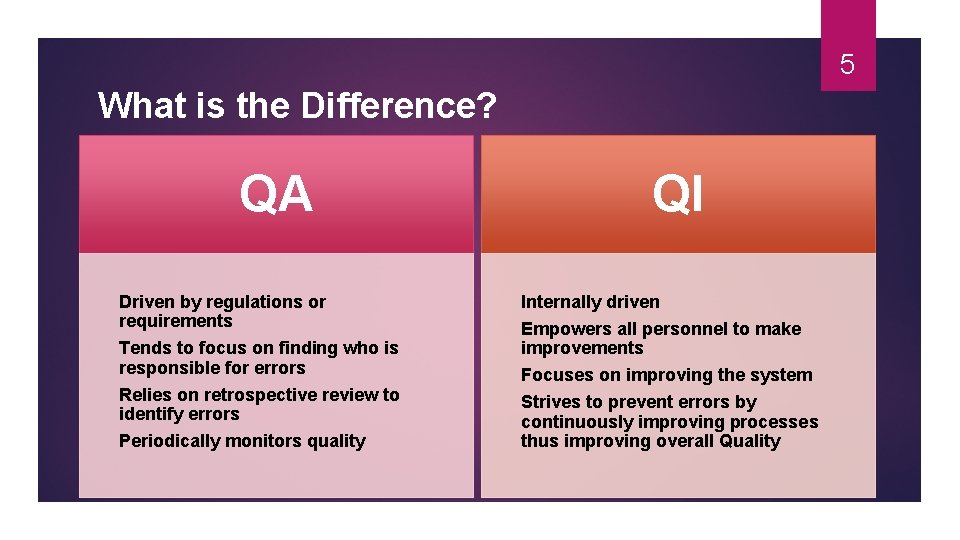
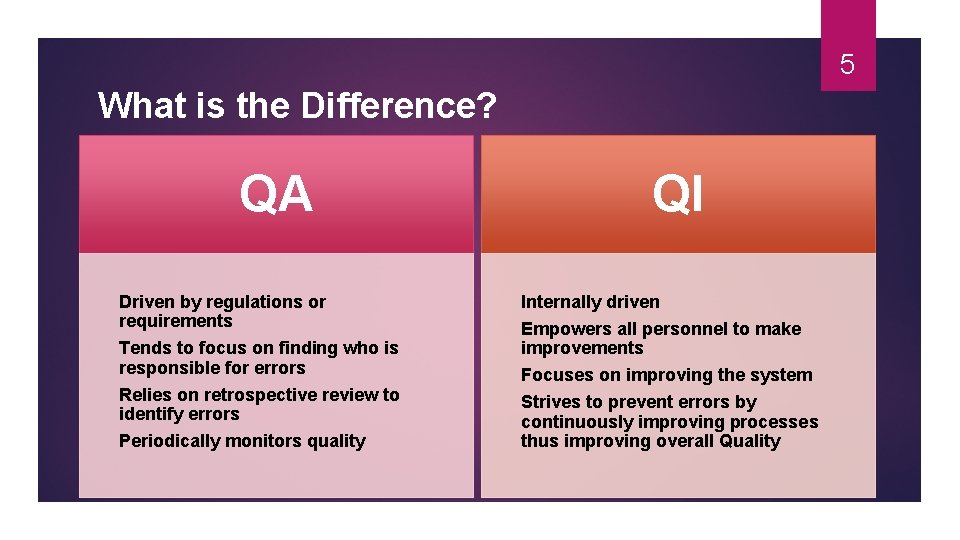
5 What is the Difference? QA Driven by regulations or requirements Tends to focus on finding who is responsible for errors Relies on retrospective review to identify errors Periodically monitors quality QI Internally driven Empowers all personnel to make improvements Focuses on improving the system Strives to prevent errors by continuously improving processes thus improving overall Quality

6 Collect data and let it inform you! STANDARDS AND MEASURES DEVELOPED FOR QUALITY ASSURANCE CAN INFORM THE QUALITY IMPROVEMENT PROCESS HTTP: //WWW. HRSA. AQUILENTPROJECTS. COM/HEALTHIT/TOOLBOX/HEALTHITADOPTION TOOLBOX/QUALITYIMPROVEMENT/WHATA REDIFFBTWQINQA. HTML
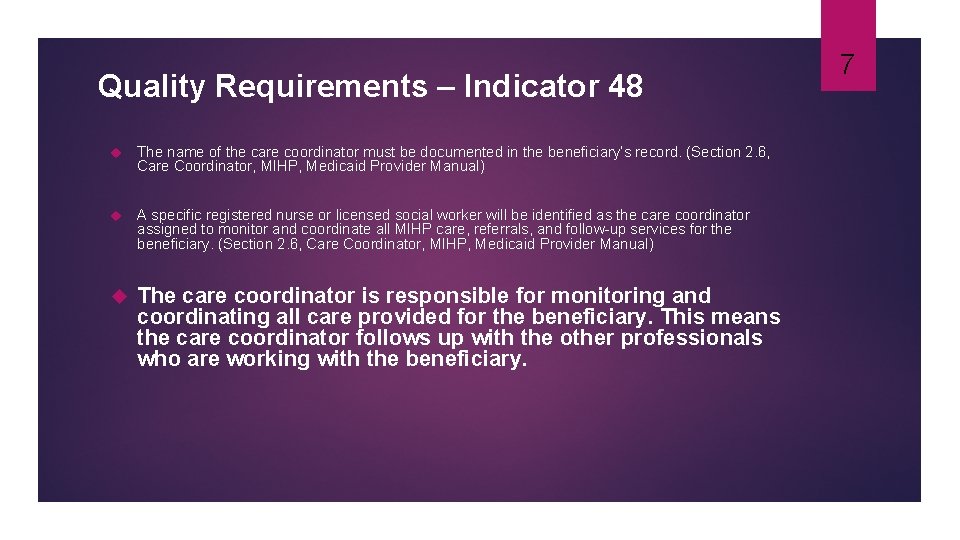
Quality Requirements – Indicator 48 The name of the care coordinator must be documented in the beneficiary’s record. (Section 2. 6, Care Coordinator, MIHP, Medicaid Provider Manual) A specific registered nurse or licensed social worker will be identified as the care coordinator assigned to monitor and coordinate all MIHP care, referrals, and follow-up services for the beneficiary. (Section 2. 6, Care Coordinator, MIHP, Medicaid Provider Manual) The care coordinator is responsible for monitoring and coordinating all care provided for the beneficiary. This means the care coordinator follows up with the other professionals who are working with the beneficiary. 7
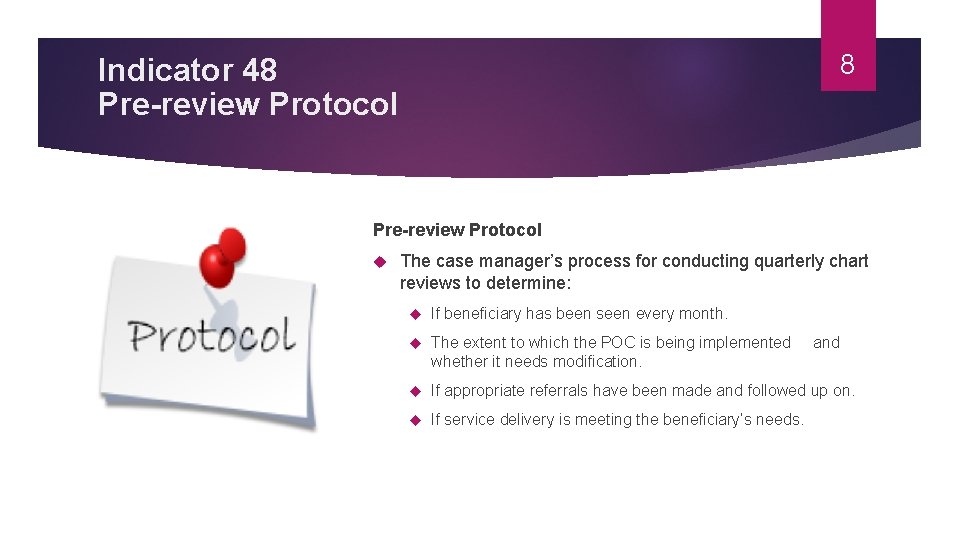
8 Indicator 48 Pre-review Protocol The case manager’s process for conducting quarterly chart reviews to determine: If beneficiary has been seen every month. The extent to which the POC is being implemented and whether it needs modification. If appropriate referrals have been made and followed up on. If service delivery is meeting the beneficiary’s needs.
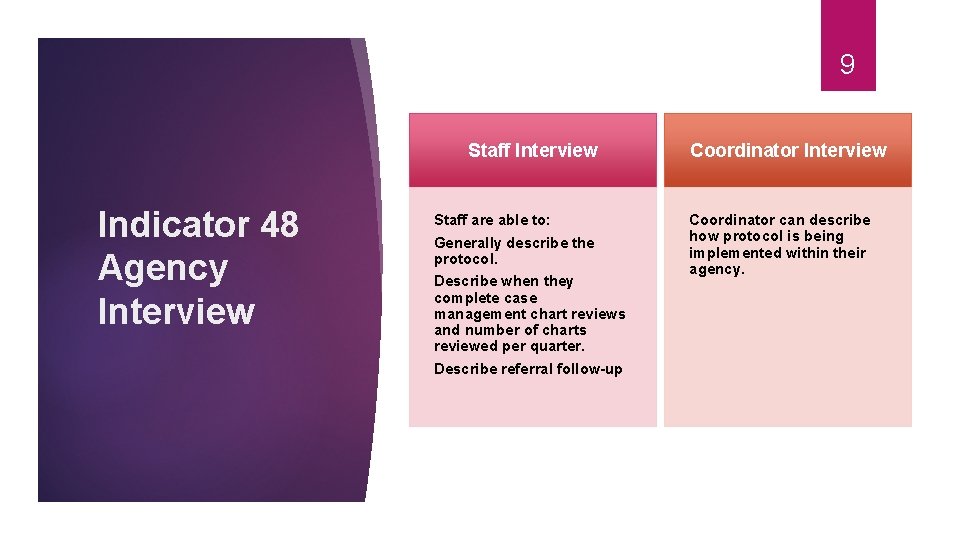
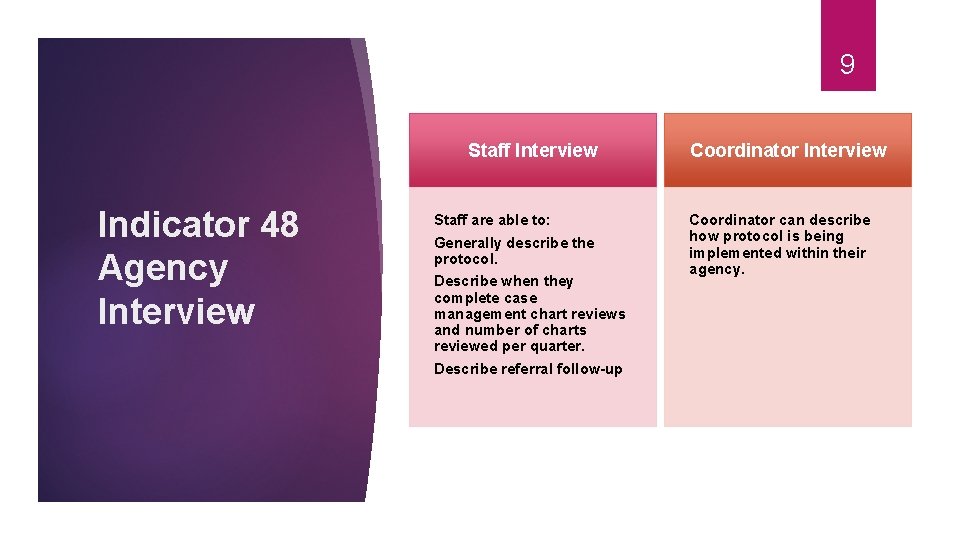
9 Staff Interview Indicator 48 Agency Interview Staff are able to: Generally describe the protocol. Describe when they complete case management chart reviews and number of charts reviewed per quarter. Describe referral follow-up Coordinator Interview Coordinator can describe how protocol is being implemented within their agency.
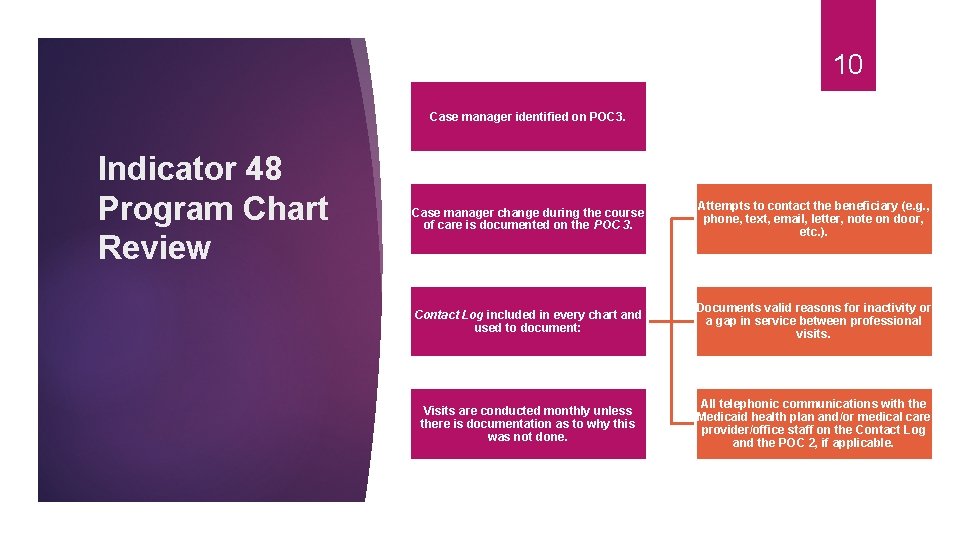
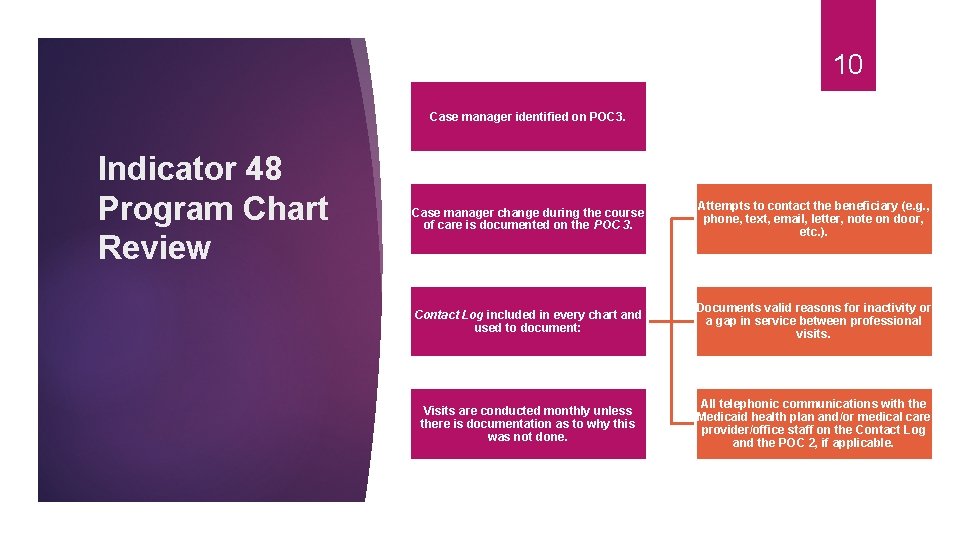
10 Case manager identified on POC 3. Indicator 48 Program Chart Review Case manager change during the course of care is documented on the POC 3. Attempts to contact the beneficiary (e. g. , phone, text, email, letter, note on door, etc. ). Contact Log included in every chart and used to document: Documents valid reasons for inactivity or a gap in service between professional visits. Visits are conducted monthly unless there is documentation as to why this was not done. All telephonic communications with the Medicaid health plan and/or medical care provider/office staff on the Contact Log and the POC 2, if applicable.
Quality Requirements – Indicator 49 MIHP coordinators are expected to routinely conduct their own internal quality assurance activities, including chart reviews and billing audits. (Section 5, 1 -1 -19 MIHP Operations Guide) 11
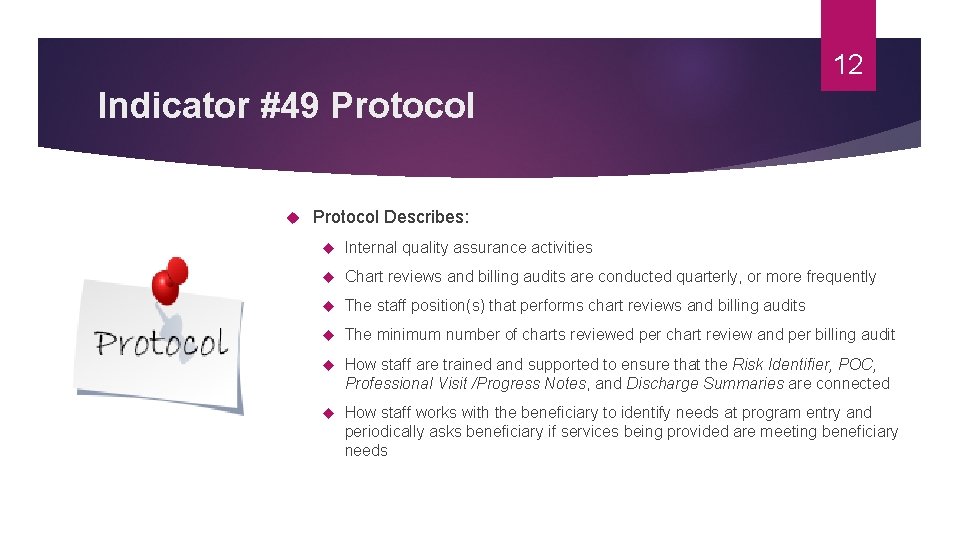
12 Indicator #49 Protocol Describes: Internal quality assurance activities Chart reviews and billing audits are conducted quarterly, or more frequently The staff position(s) that performs chart reviews and billing audits The minimum number of charts reviewed per chart review and per billing audit How staff are trained and supported to ensure that the Risk Identifier, POC, Professional Visit /Progress Notes, and Discharge Summaries are connected How staff works with the beneficiary to identify needs at program entry and periodically asks beneficiary if services being provided are meeting beneficiary needs
13 Indicator #49 Staff Interview indicates that staff can: Generally describe the protocol Explain how the Risk Identifier, POC, Professional Visit Progress Notes, and Discharge Summaries are connected
Indicator #49 Onsite Document Review of Documentation Completed forms or tools for program chart audit Completed forms or tools for billing chart audit Indicates that reviews and audits are being conducted through review of completed tools and evidence throughout rating of certification indicators Program and billing chart reviews conducted at least quarterly Staff participating in chart reviews. 14
15 Administrative Data collected via administrative claims data from the Medicaid data warehouse (CHAMPS) Risk identifier data collected via risk screener database Data assists in identifying areas of strength and opportunity
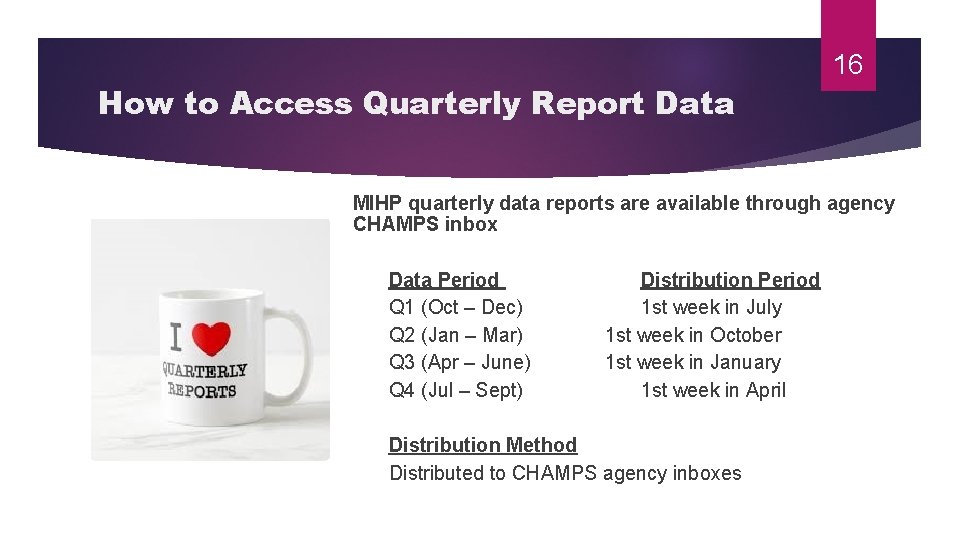
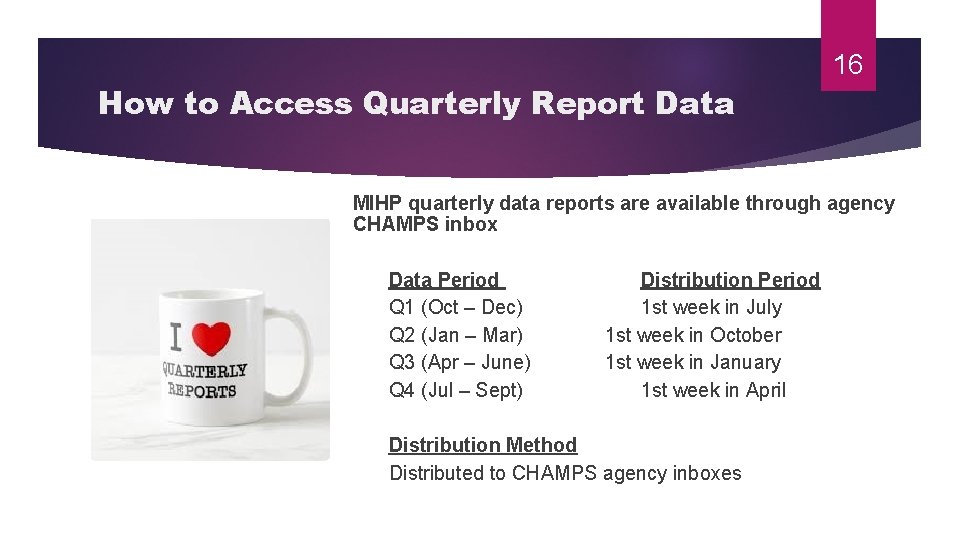
16 How to Access Quarterly Report Data MIHP quarterly data reports are available through agency CHAMPS inbox Data Period Distribution Period Q 1 (Oct – Dec) 1 st week in July Q 2 (Jan – Mar) 1 st week in October Q 3 (Apr – June) 1 st week in January Q 4 (Jul – Sept) 1 st week in April Distribution Method Distributed to CHAMPS agency inboxes
17 17 Quarterly reports include: MIHP Quarterly Report Data Screens Completed Discharges Completed Demographics Risk Screening Domain Scores Referrals Breastfeeding Information
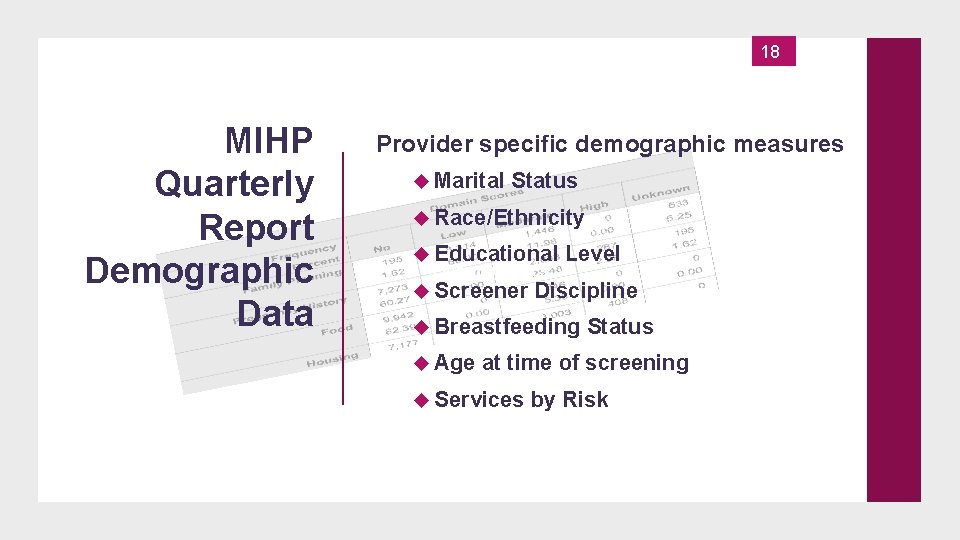
18 MIHP Quarterly Report Demographic Data 18 Provider specific demographic measures Marital Status Race/Ethnicity Educational Level Demographics Screener Discipline Breastfeeding Status Age at time of screening Services by Risk

19 Using MIHP Quarterly Reports Why do I have all of this data? and. . . Demographics What do I do with it?
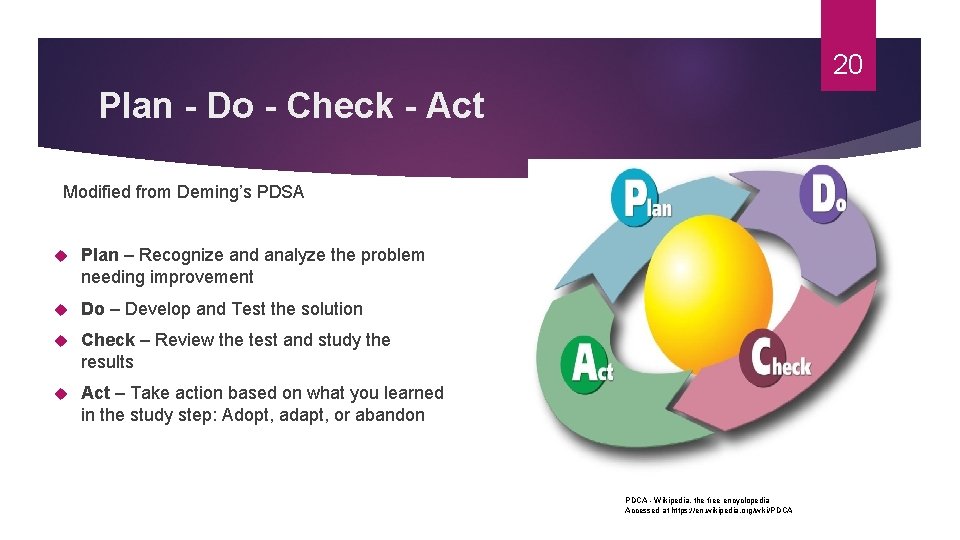
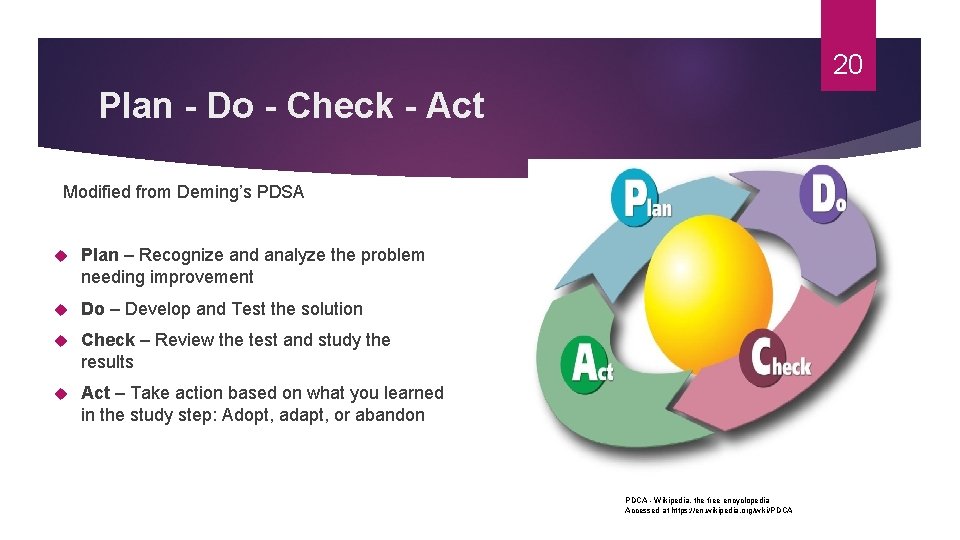
20 Plan - Do - Check - Act Modified from Deming’s PDSA Plan – Recognize and analyze the problem needing improvement Do – Develop and Test the solution Check – Review the test and study the results Act – Take action based on what you learned in the study step: Adopt, adapt, or abandon PDCA - Wikipedia, the free encyclopedia Accessed at https: //en. wikipedia. org/wiki/PDCA
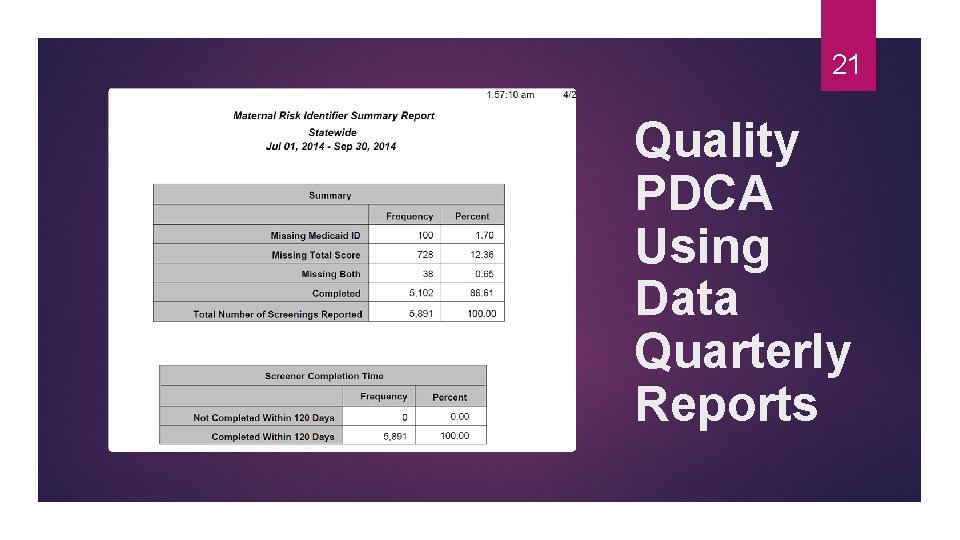
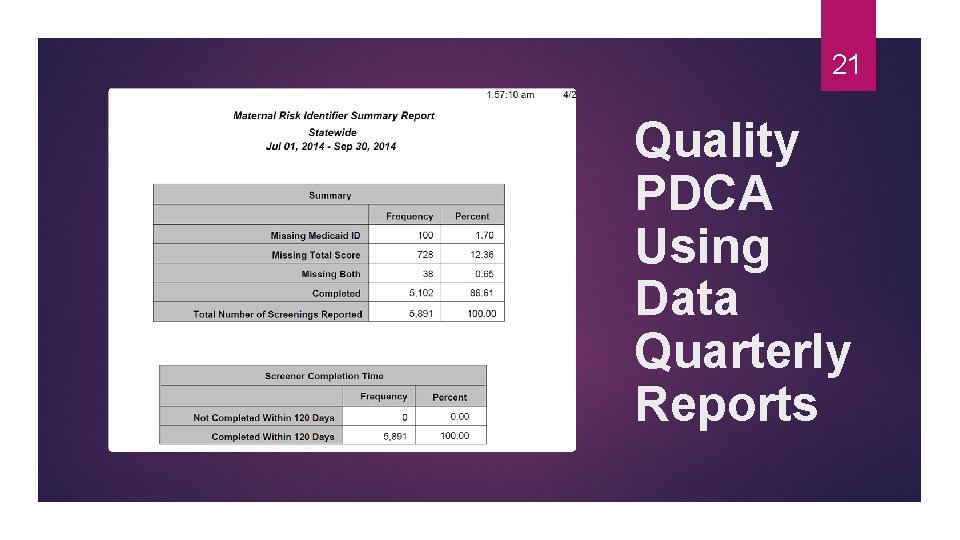
21 Quality PDCA Using Data Quarterly Reports
PDCA Plan Recognize and analyze the problem needing improvement The problem, 13% of the agency’s Risk Identifiers are incomplete. Largest percent (12. 3%) due to no total score. 22
23 Why is this a problem? No risk score means no POC for the beneficiary PD CA Agency is “holding” the risk identifier in the database preventing another agency from seeing mom Limits services to a high risk population Agency can’t bill until RI is complete
PDCA Analyze data further looking for incomplete risk identifiers by individual staff Look for trends Form the plan to improve the problem 24
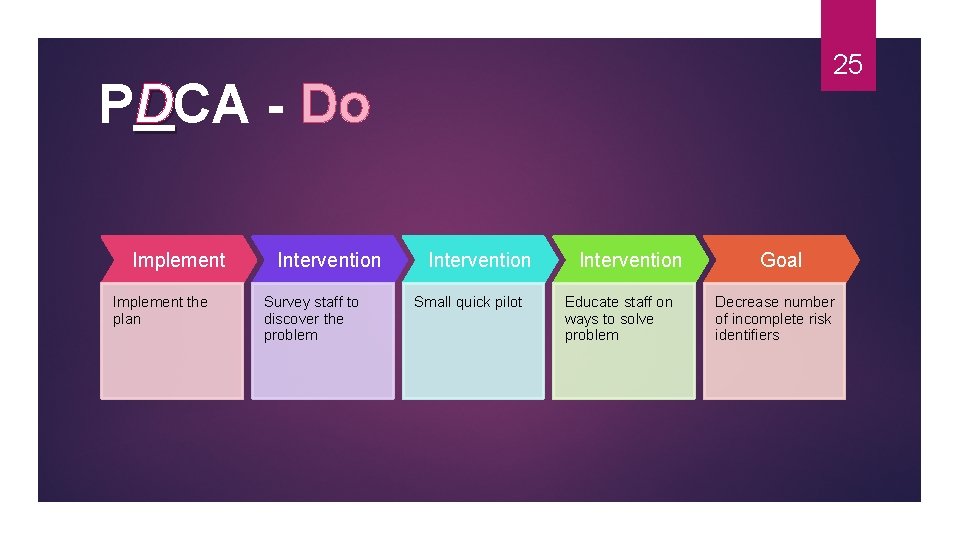
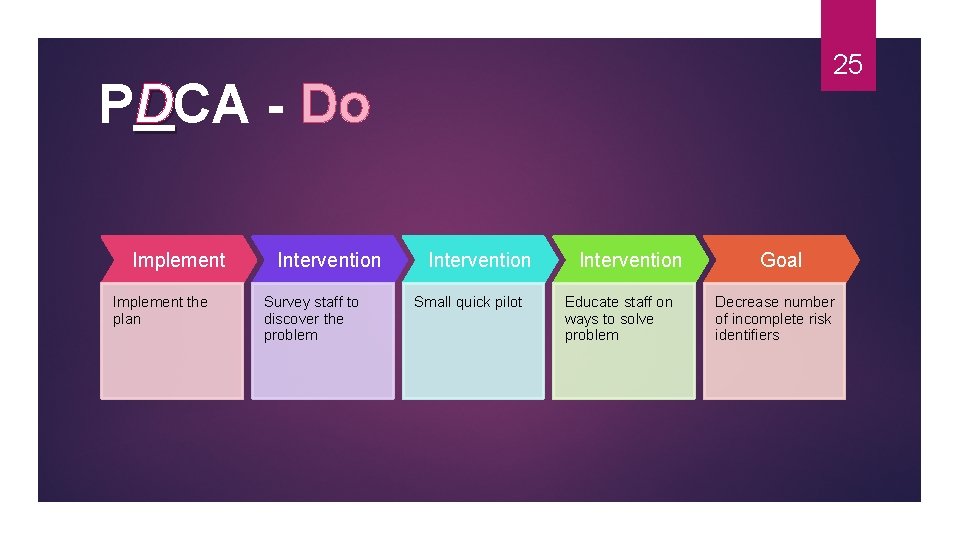
PDCA - Do Implement the plan Intervention Survey staff to discover the problem 25 Intervention Small quick pilot Intervention Educate staff on ways to solve problem Goal Decrease number of incomplete risk identifiers
26 PDCA CHECK AND ASSESS THE INTERVENTION RESULTS This Photo by Unknown Author is licensed under CC BY-SA
PDCA Check – Review the intervention results Assess the number of Incomplete risk identifiers Number increased, decreased, stagnant How close to your goal? 27
28 PDCA Act – Take action based on the assessment of the plan Adopt, adapt, or abandon
PDCA Act – Take action based on the assessment of the plan and then: Adopt The plan worked Adapt The plan worked but fell short of the goal Reassess Adjust plan Abandon The plan did not work Need a new plan Back to the drawing board 29
Take Away Points Don’t assume you know what the problem is - - Do the PLANNING Check data and every available resource to discover the true problem Ask staff to help assess the problem Survey clients when appropriate DO Interventions - - brainstorm with staff to plan the intervention that will work best in your agency Pick a goal and timeline to CHECK the results of the interventions Decide what your ACTion will be and your next steps. . . Adopt, Adapt, or Abandon 30

31 REMEMBER The ultimate goal of quality improvement is to deliver MIHP services that improve outcomes for Michigan families
Questions 32

33 MIHP Chart Review WHY, WHEN, WHO, AND HOW
34 To assure quality of care is being provided to MIHP beneficiaries Importance of Chart Review To assure all staff are aware of and following program requirements To assure billing is being done appropriately
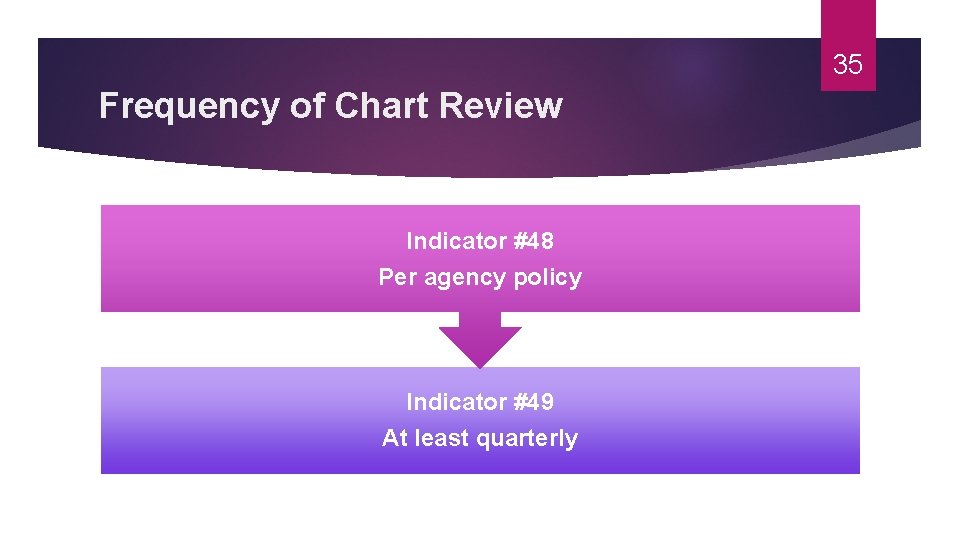
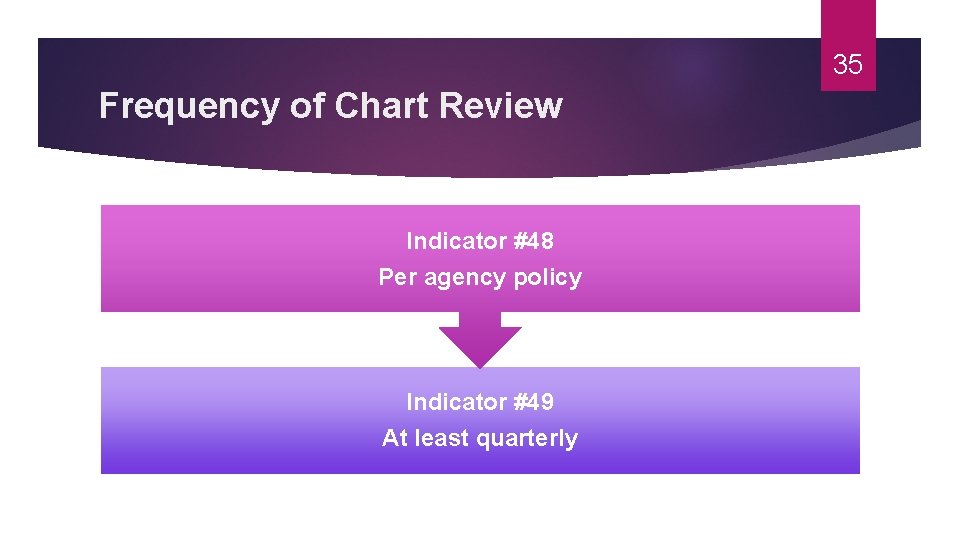
35 Frequency of Chart Review Indicator #48 Per agency policy Indicator #49 At least quarterly
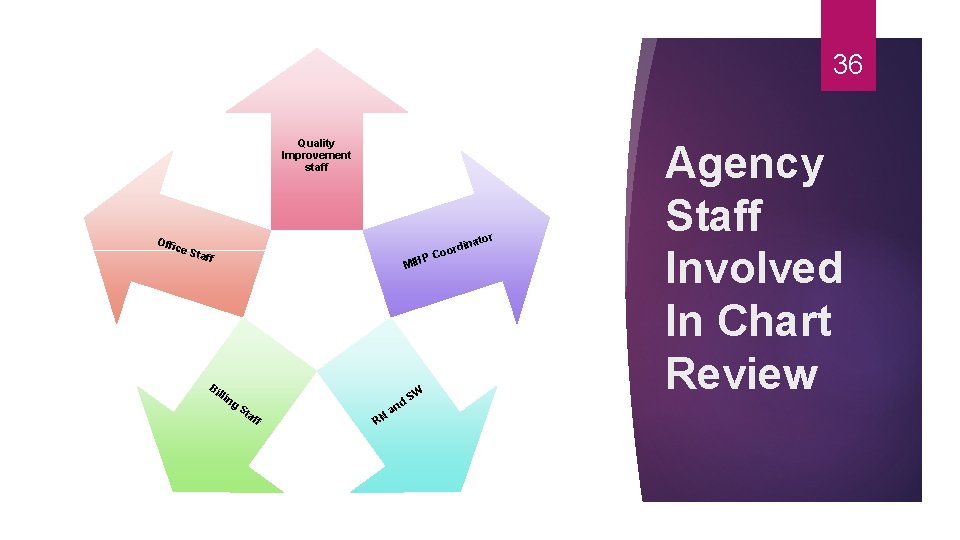
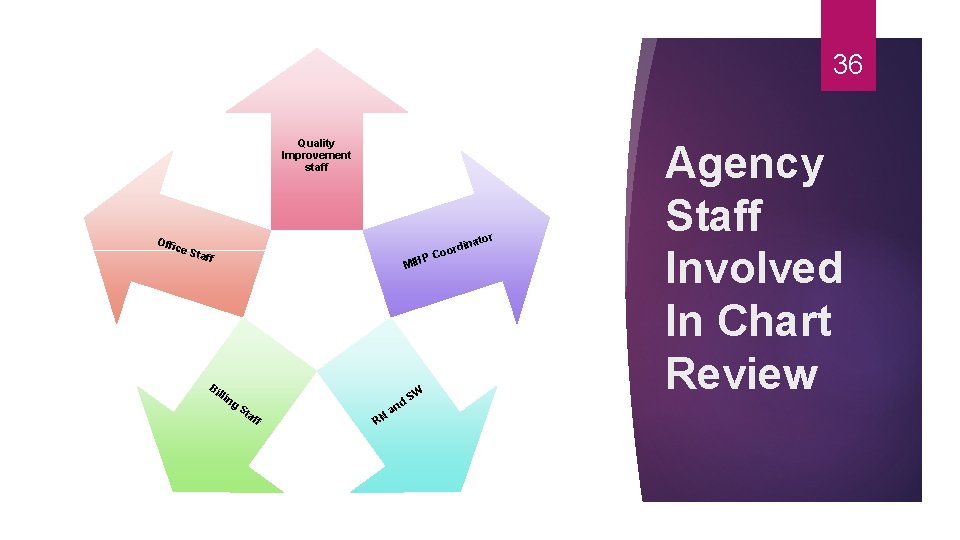
36 Quality Improvement staff or Offi ce S taff P C Bi MIH llin g S St af f RN d an W inat oord Agency Staff Involved In Chart Review
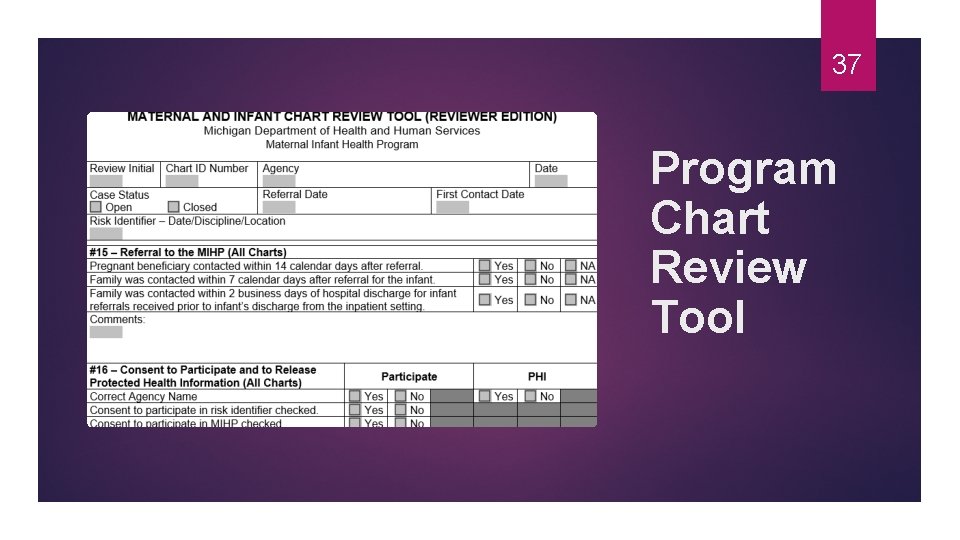
37 Program Chart Review Tool
Program Chart Review Tool #15 – Referral to the MIHP (All Program Charts) #16 – Consent to Participate and to Release Protected Health Information (All Program and Billing Charts) #35 -Risk Identifier (RI) and Authorization of Services (All Program Charts) 38
39 Program Chart Review Tool #32 – Medical Care Provider Notification (All Program Charts) #33 – Coordination with Medicaid Health Plans (All Program Charts)
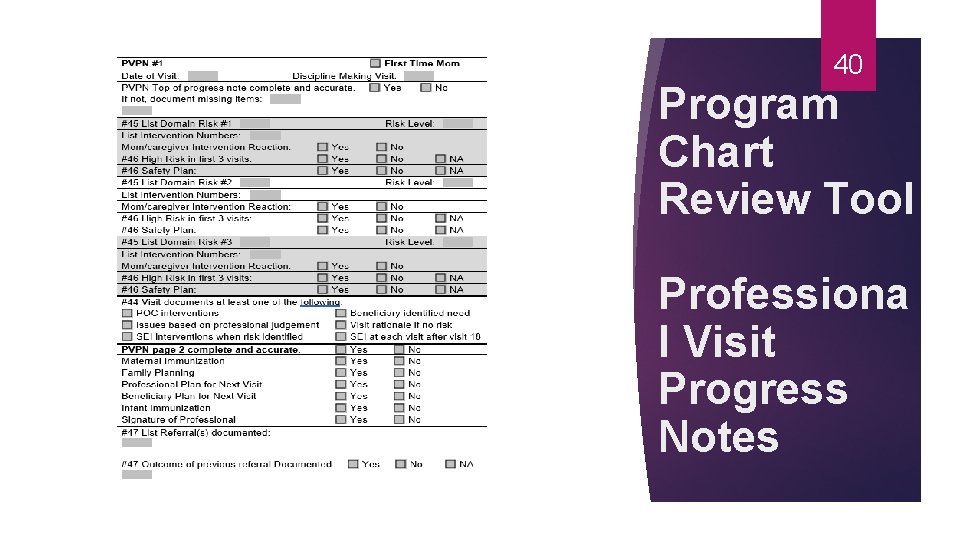
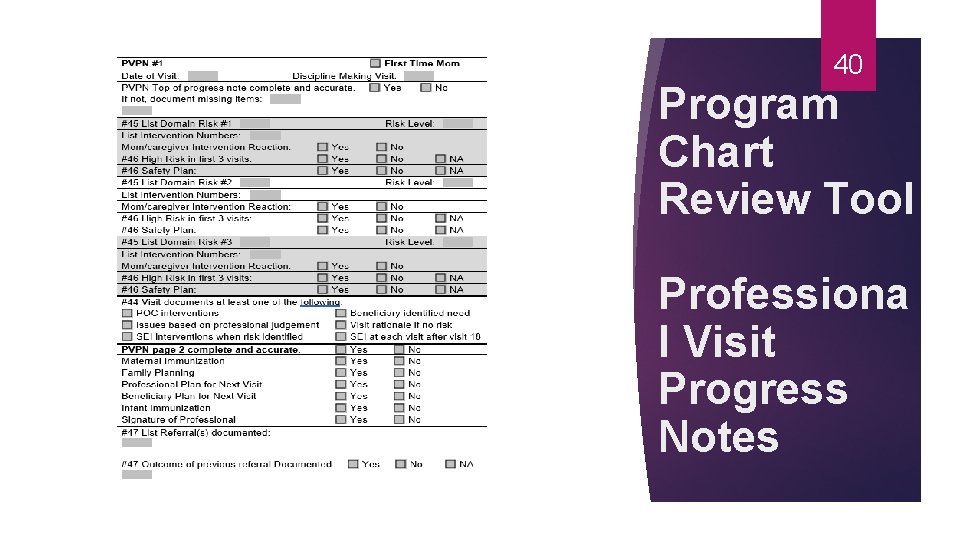
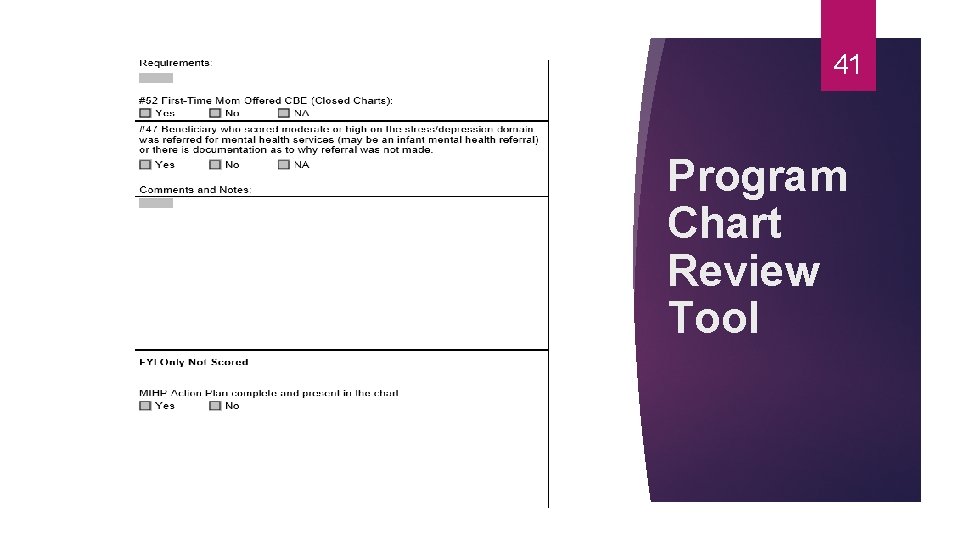
40 Program Chart Review Tool Professiona l Visit Progress Notes
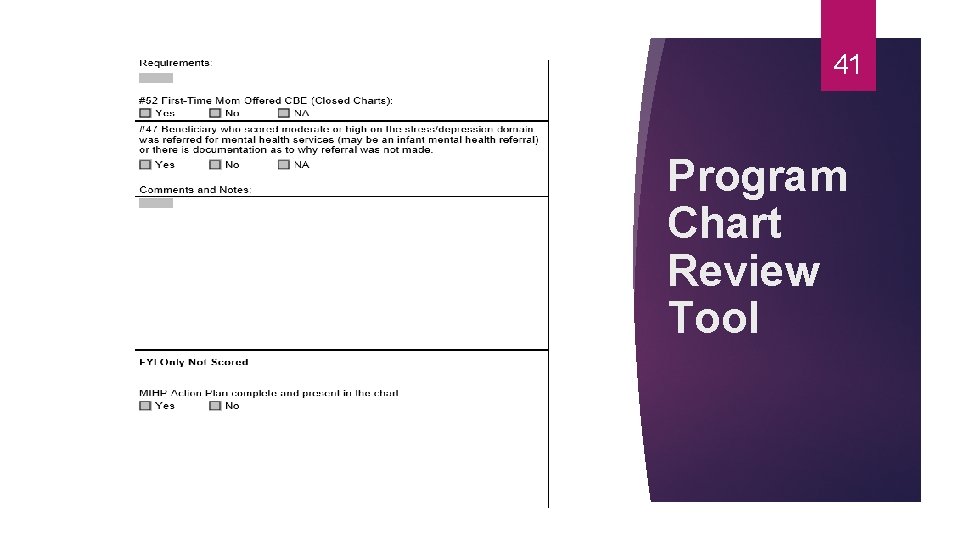
41 Program Chart Review Tool
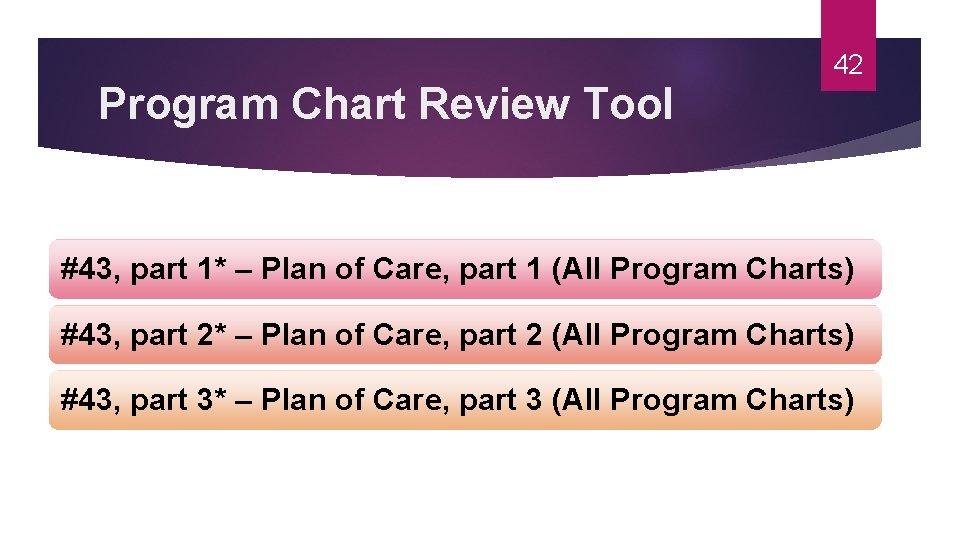
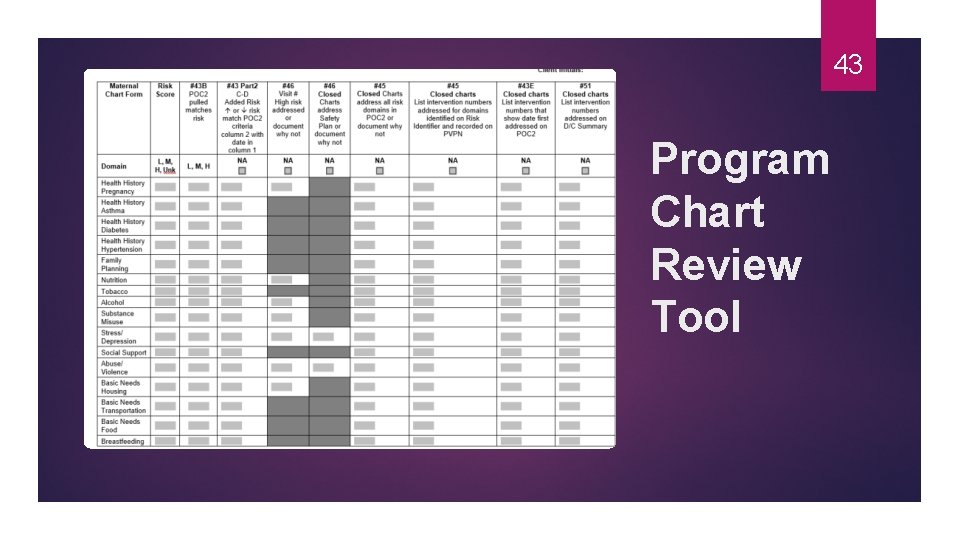
Program Chart Review Tool 42 #43, part 1* – Plan of Care, part 1 (All Program Charts) #43, part 2* – Plan of Care, part 2 (All Program Charts) #43, part 3* – Plan of Care, part 3 (All Program Charts)
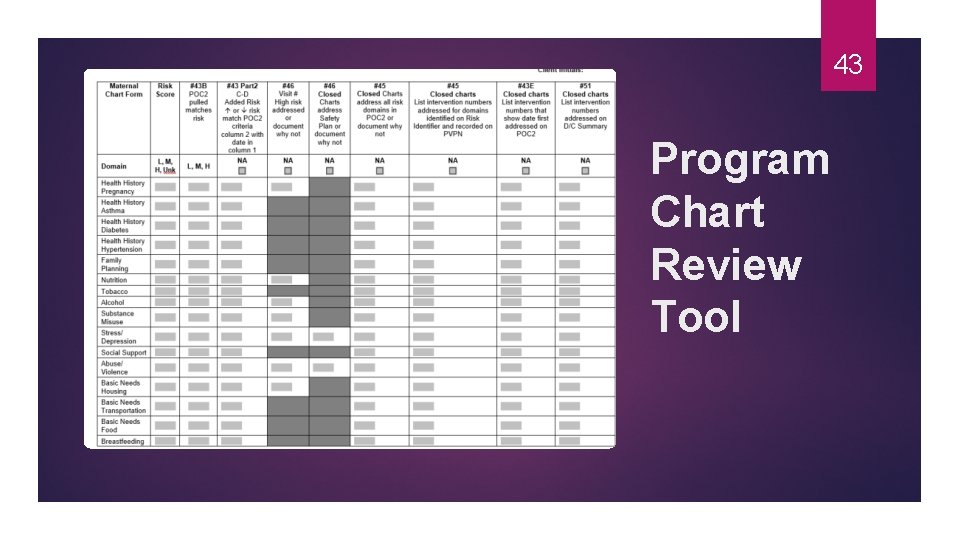
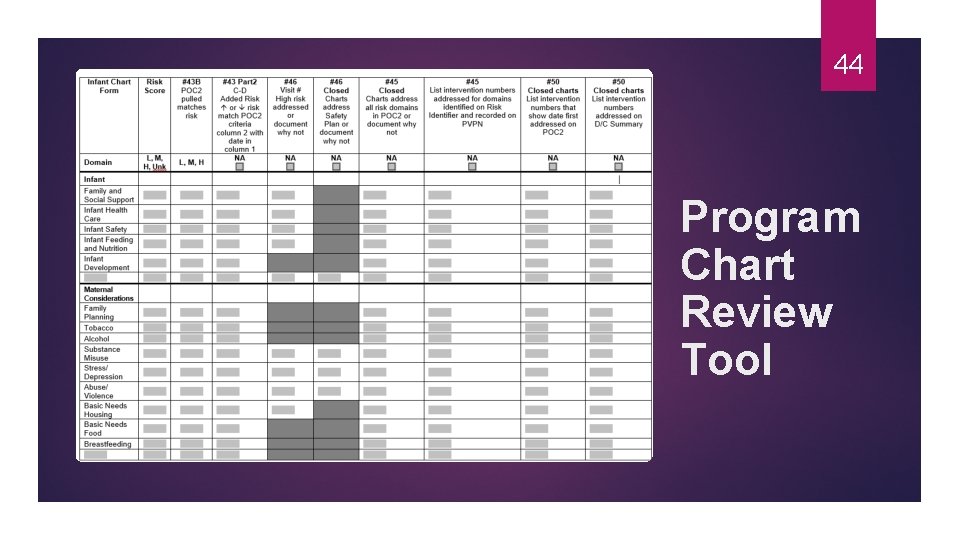
43 Program Chart Review Tool
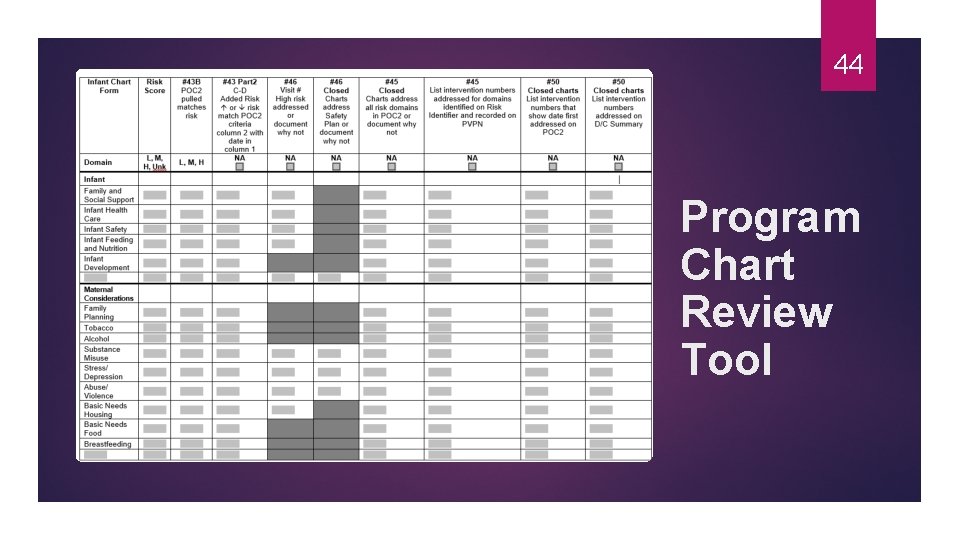
44 Program Chart Review Tool
Program Chart Review Tool 45 #43, part 2* – Accurate Plan of Care, part 2 (All Program Charts) #45 – Address all Risk Domains and Document Appropriately (Closed Program Charts) #46 – High Risk and Safety Plan (All Program Charts) #51 – Interventions numbers on D/C summary (Closed Program Charts)
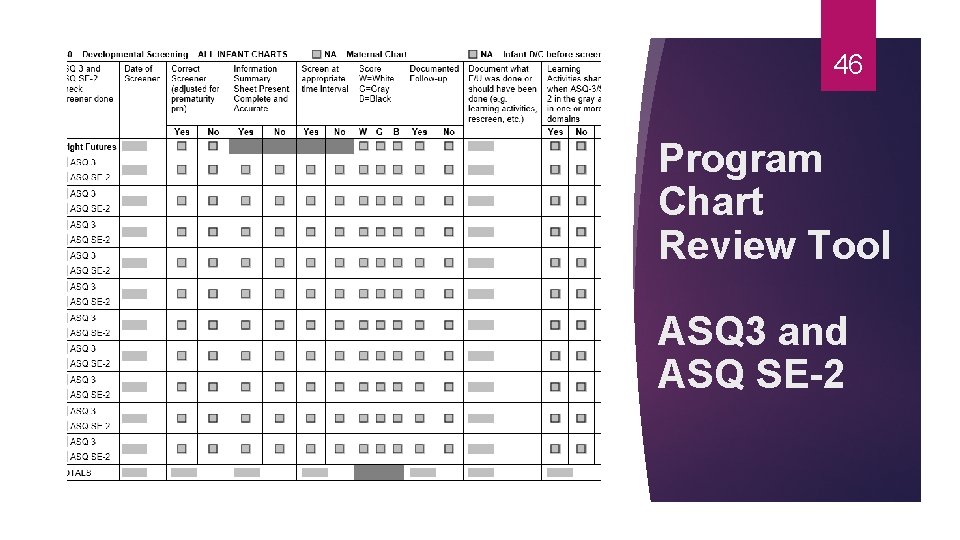
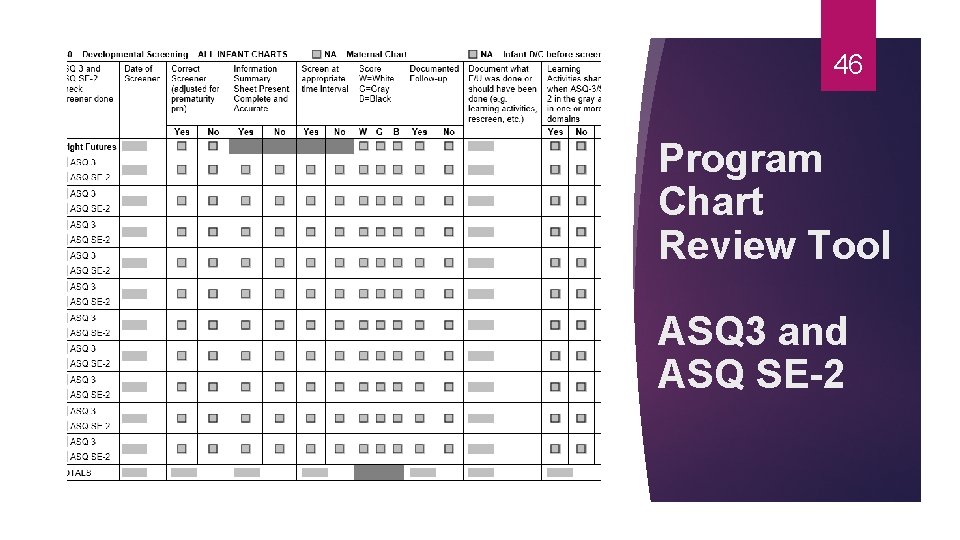
46 Program Chart Review Tool ASQ 3 and ASQ SE-2
Program Chart Review Tool 47 #40, part 1* – Protocol (All Infant Program Charts) #40, part 2* – Conducting/Documenting Screening (All Infant Program Charts) #40, part 3* – Screening Follow-up (All Infant Program Charts)
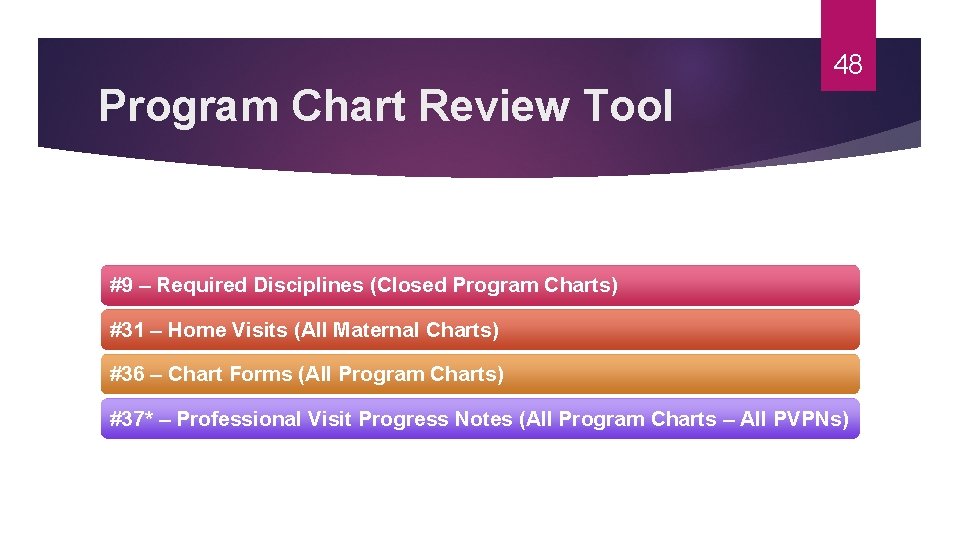
48 Program Chart Review Tool #9 – Required Disciplines (Closed Program Charts) #31 – Home Visits (All Maternal Charts) #36 – Chart Forms (All Program Charts) #37* – Professional Visit Progress Notes (All Program Charts – All PVPNs)
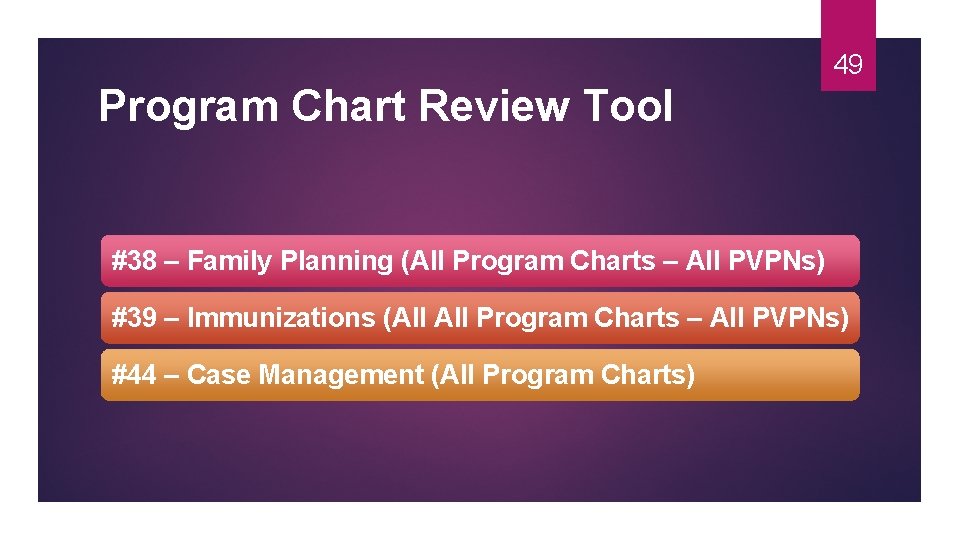
49 Program Chart Review Tool #38 – Family Planning (All Program Charts – All PVPNs) #39 – Immunizations (All Program Charts – All PVPNs) #44 – Case Management (All Program Charts)
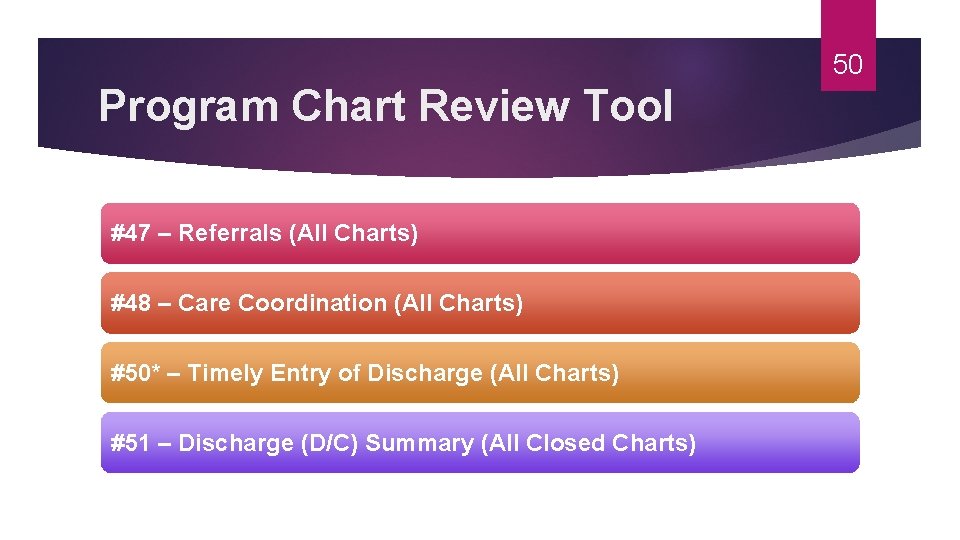
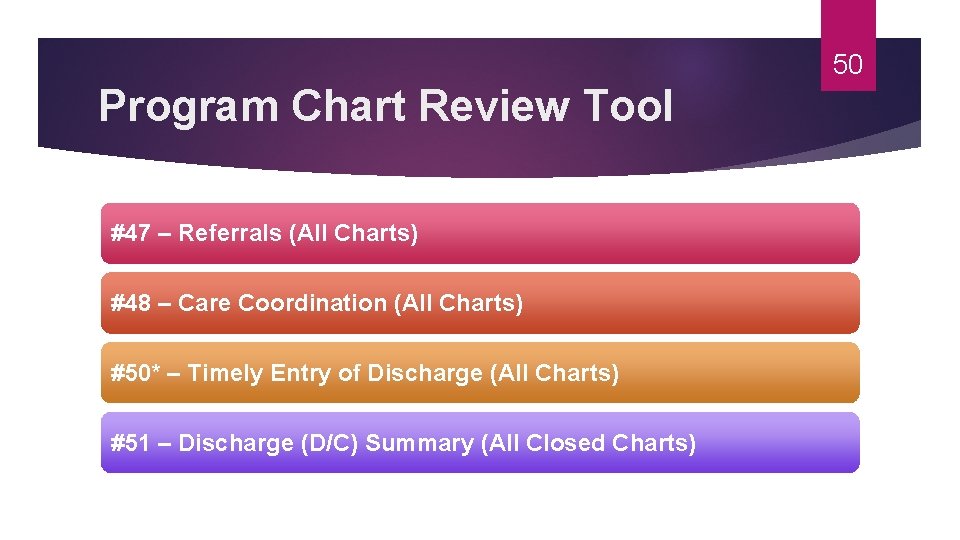
50 Program Chart Review Tool #47 – Referrals (All Charts) #48 – Care Coordination (All Charts) #50* – Timely Entry of Discharge (All Charts) #51 – Discharge (D/C) Summary (All Closed Charts)
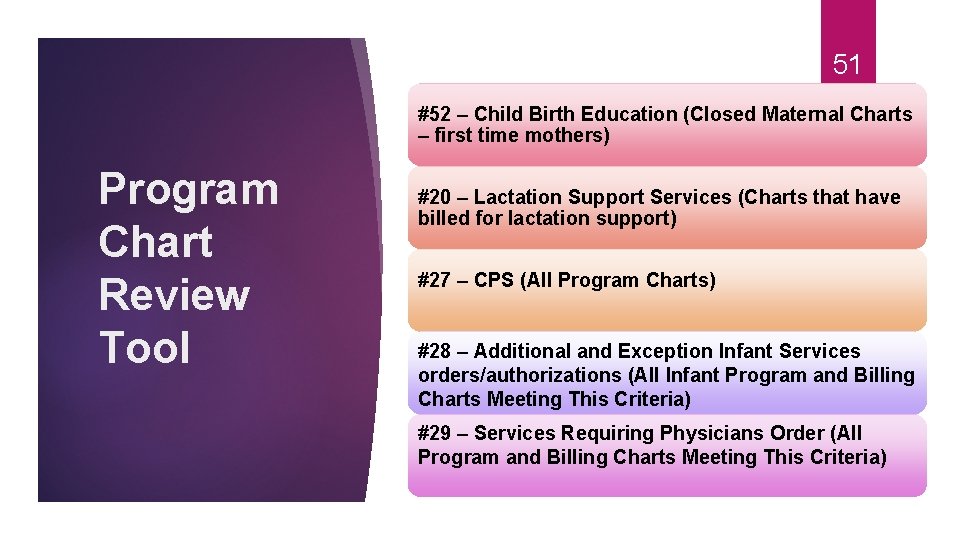
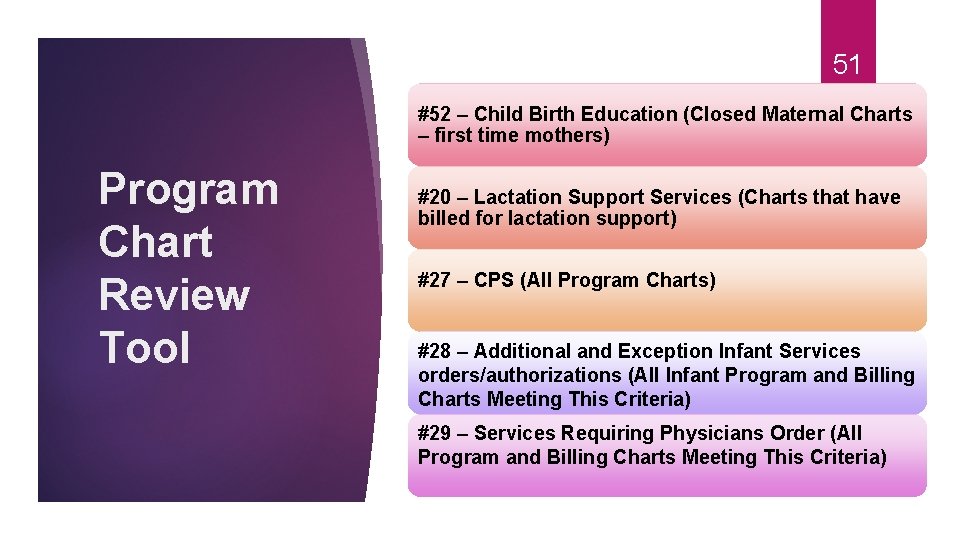
51 #52 – Child Birth Education (Closed Maternal Charts – first time mothers) Program Chart Review Tool #20 – Lactation Support Services (Charts that have billed for lactation support) #27 – CPS (All Program Charts) #28 – Additional and Exception Infant Services orders/authorizations (All Infant Program and Billing Charts Meeting This Criteria) #29 – Services Requiring Physicians Order (All Program and Billing Charts Meeting This Criteria)
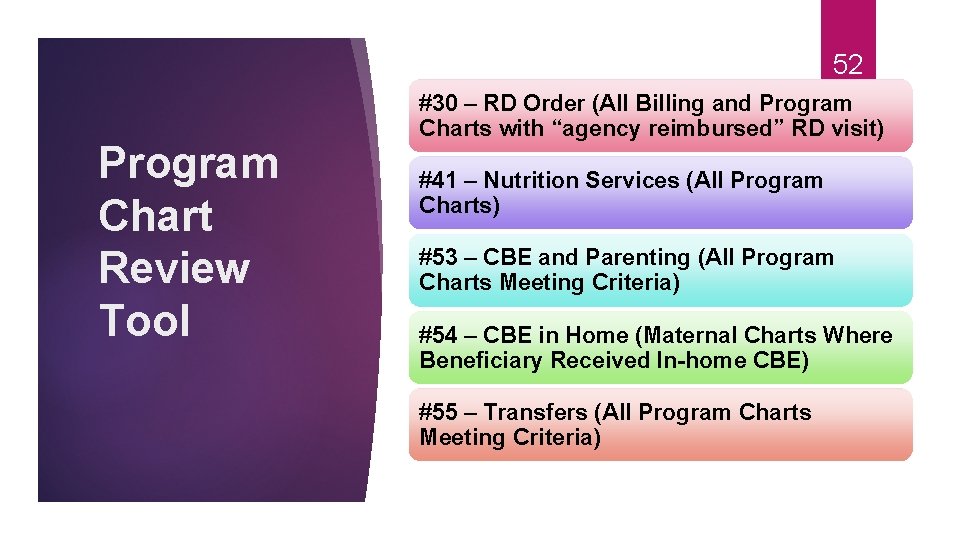
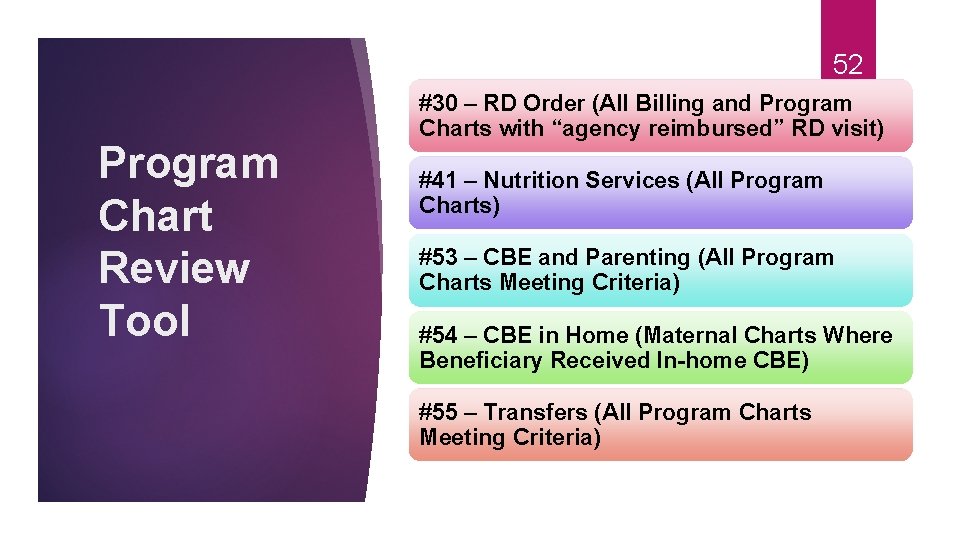
52 Program Chart Review Tool #30 – RD Order (All Billing and Program Charts with “agency reimbursed” RD visit) #41 – Nutrition Services (All Program Charts) #53 – CBE and Parenting (All Program Charts Meeting Criteria) #54 – CBE in Home (Maternal Charts Where Beneficiary Received In-home CBE) #55 – Transfers (All Program Charts Meeting Criteria)
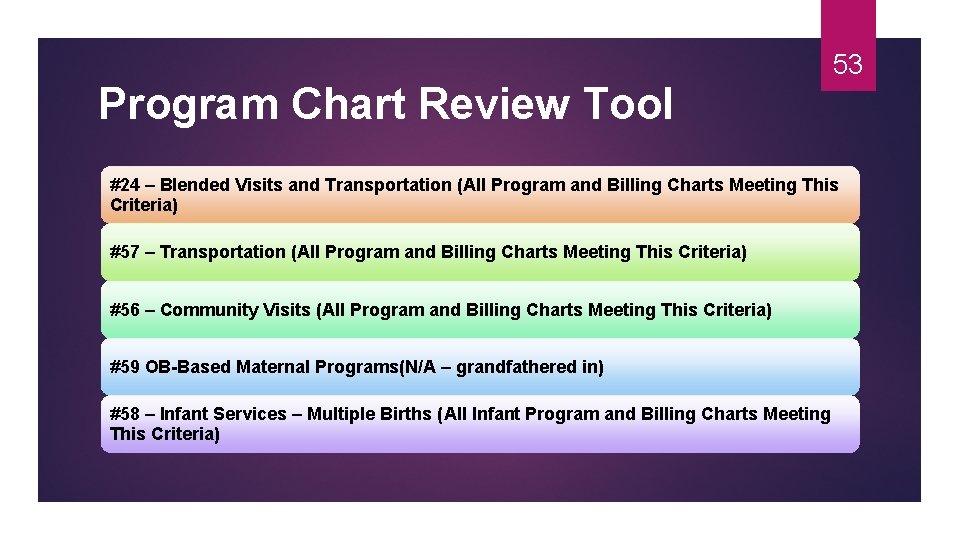
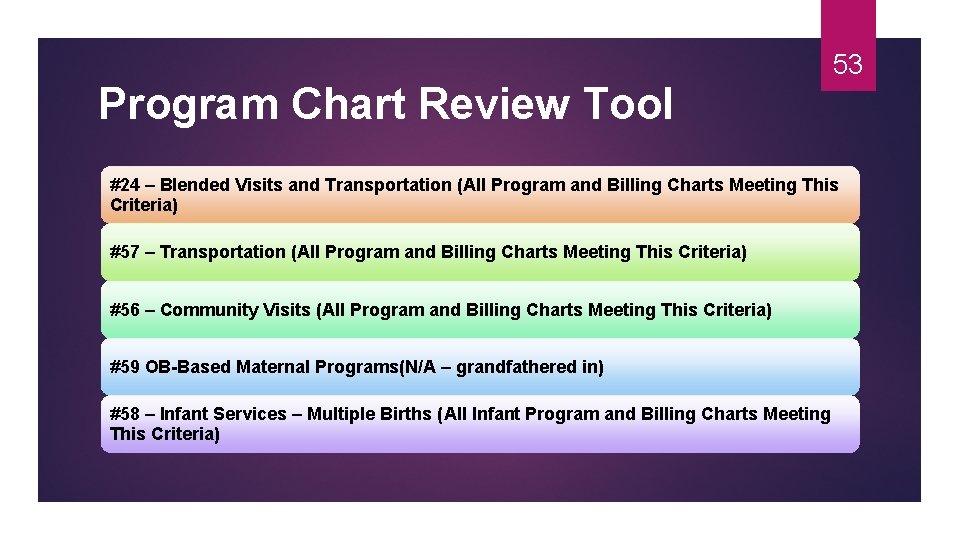
Program Chart Review Tool 53 #24 – Blended Visits and Transportation (All Program and Billing Charts Meeting This Criteria) #57 – Transportation (All Program and Billing Charts Meeting This Criteria) #56 – Community Visits (All Program and Billing Charts Meeting This Criteria) #59 OB-Based Maternal Programs(N/A – grandfathered in) #58 – Infant Services – Multiple Births (All Infant Program and Billing Charts Meeting This Criteria)

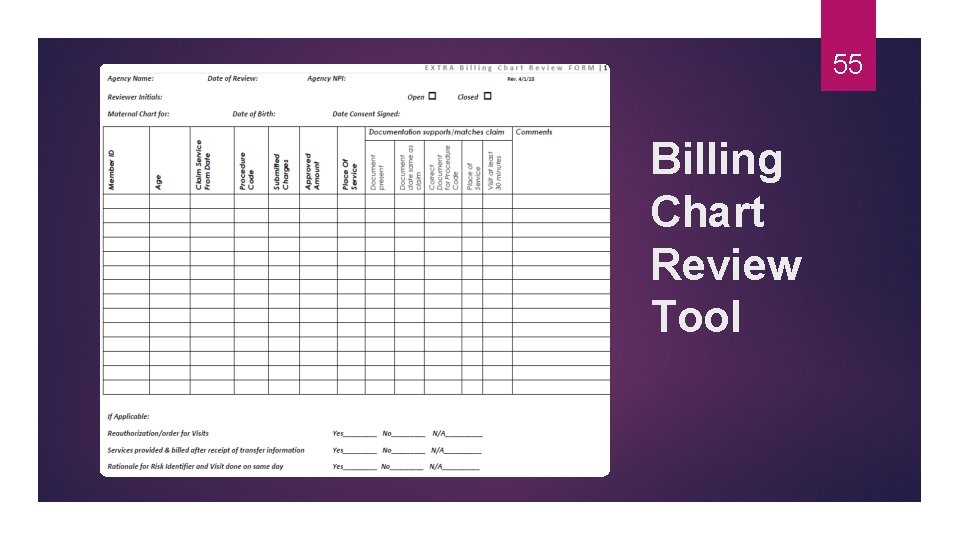
54 Billing Chart Review Indicator #16 Indicator #18 Indicator #19 Indicator #21 Indicator #28 Indicator #24 Indicator #23 Indicator #22 Indicator #29 Indicator #53 Indicator #54 Indicator # 57
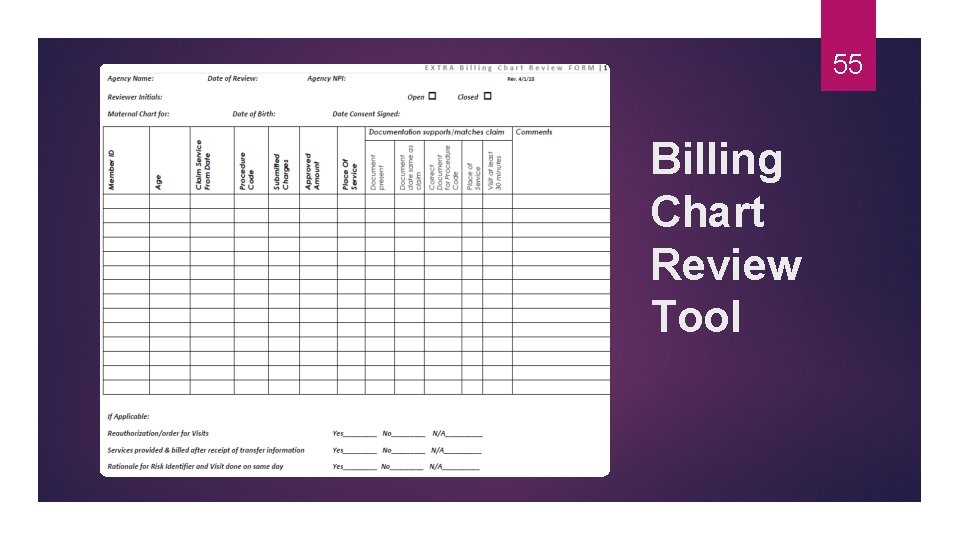
55 Billing Chart Review Tool
Questions 56
Record Revision Request 57
58 MIHP Database All completed Risk Identifiers and Discharges will be listed as a Y (Yes) under the status column in the MIHP database All incomplete Risk Identifiers and Discharges will be listed as a N (No) under the status column in the MIHP database
Incomplete Risk Identifiers and Discharges The MIHP Agency may delete or update an incomplete (N) record at any time 59
60 Completed Risk Identifiers and Discharges Completed (Y) Risk Identifiers and Discharges may be updated by the agency who entered it in the MIHP database, within 30 days of completion.
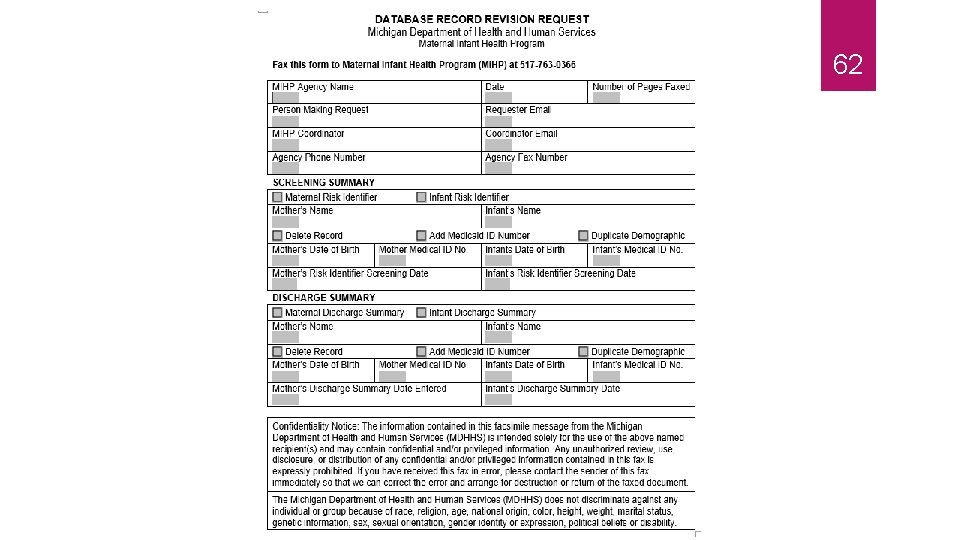
61 When to Fax the Record Revision Request to MDHHS MIHP for Risk Identifiers If a completed (Y) Risk Identifier needs to be updated, after 30 days of completion, it must instead, be deleted and re-entered If a completed (Y) Risk Identifier needs to be deleted, it can only be deleted by the MDHHS MIHP state staff Utilize the MIHP Database Record Revision Request Form, on the website to make this request
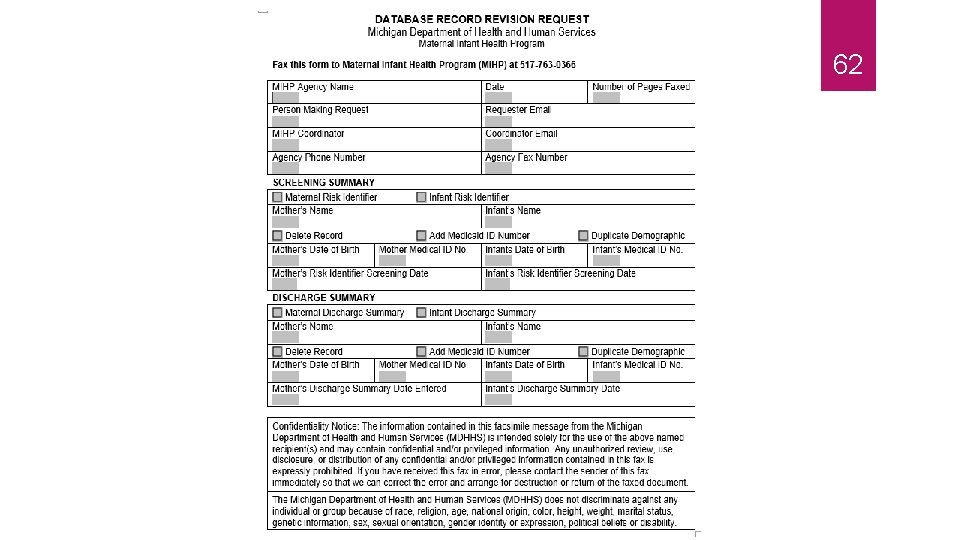
62
63 When to Fax the Record Revision Request to MDHHS MIHP for Discharges Similar to completed (Y) Risk Identifiers, completed (Y) Discharges can only be deleted by MDHHS MIHP staff. Utilize the MIHP Database Record Revision Request Form, on the website to make this request
64 Questions?
MIHP Discharge Summaries TELLING THE STORY
A Discharge Summary Must be Completed for All MIHP Beneficiaries 66 For every pregnant woman, who receives at least a Maternal Risk Identifier (MRI) For every infant, who receives at least an Infant Risk Identifier (IRI)
The Discharge Summary is Linked to the Risk Identifier through CHAMPS auto-populates the Discharge Summary with beneficiary name and date of birth (DOB), which are tied to the Medicaid number If name or DOB is inaccurate, it must be corrected by the assigned caseworker at local Department of Health and Human Services (DHHS) office 67
A Risk Identifier is Always Tied to the MIHP Agency That Completed It 68
An MIHP Agency May Complete a Discharge Summary for their Enrolled Beneficiary 69 Even if the MRI or IRI was entered by another MIHP
Receiving Agency Completes the Discharge Summary for a Transferred Beneficiary 70
Complete a Full or Abbreviated Discharge Summary 71 MIHP agencies complete a full Discharge Summary or an abbreviated Discharge Summary This depends on the type of MIHP services the beneficiary received
72 When to enter a Full Discharge Summary A full Discharge Summary is required if services have been billed beyond completion of the Risk Identifier In this case, an agency would check “Yes” on the radio button titled Full Discharge Required?
73 Click the Radio Button Only Once Full Discharge Summary? ü Yes? ü No?
Complete an Abbreviated Discharge Summary 74 If an agency clicks “No” to the Full Discharge Summary question, an abbreviated Discharge Summary will be created All sections will be grayed out except: Basics Infant Safety “Progress During Interventions” Breastfeeding “Progress During Interventions” Family Planning “Progress During Interventions”
Abbreviated Discharge Summary Streamlines the Process This function streamlines the discharge process for MIHP beneficiaries who have been provided a “Risk Identifier only. ” This includes: The second, third, etc. infant in a multiple birth set Beneficiaries who consent to the Risk Identifier, but not to other MIHP services Beneficiaries who are lost to service after the Risk Identifier visit 75
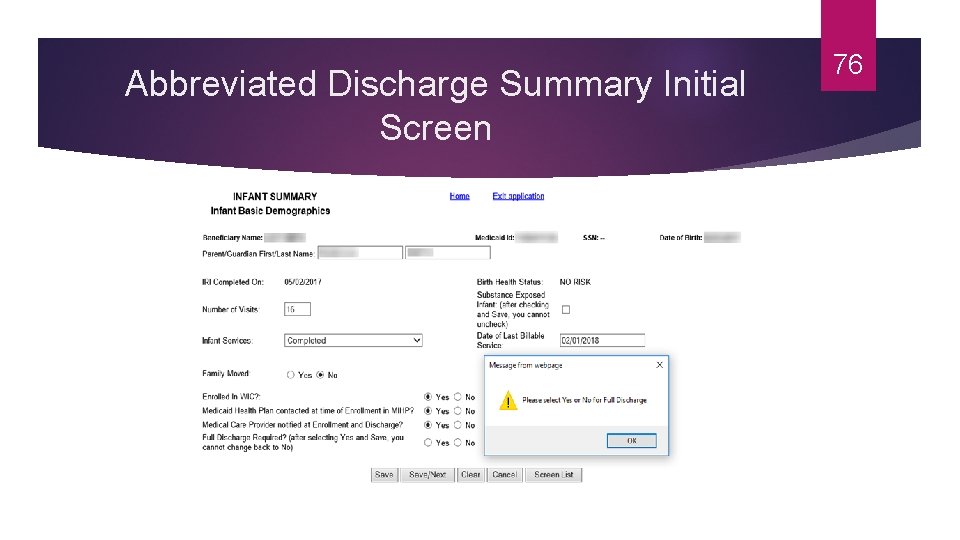
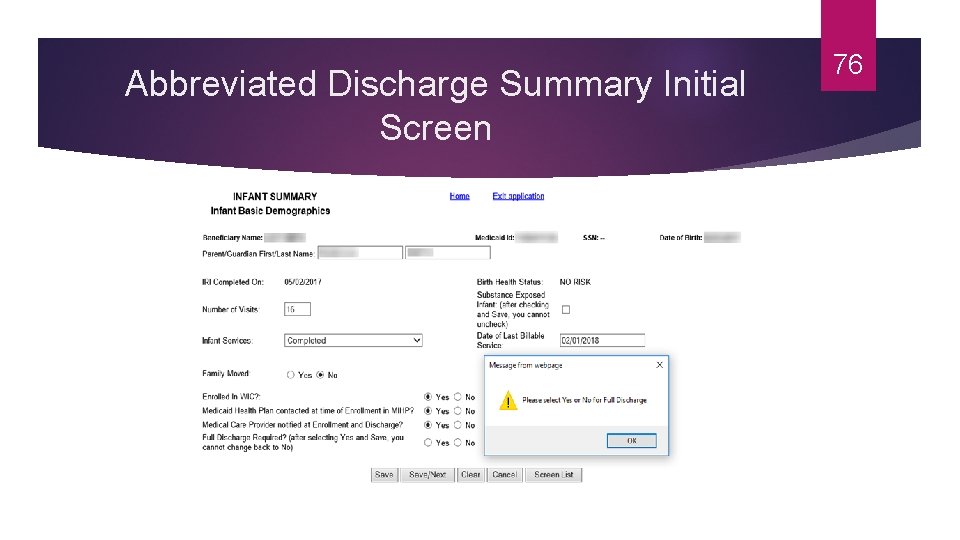
Abbreviated Discharge Summary Initial Screen 76
77 Full Discharge Summary Requirements All sections must be completed
78 How to Enter a Discharge Summary Gather all chart materials Great time to complete a final quality assurance check
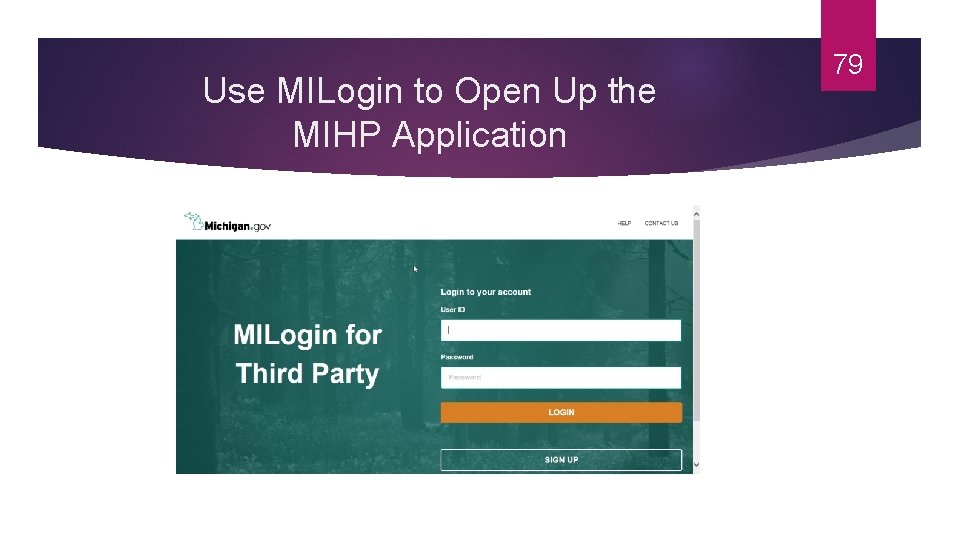
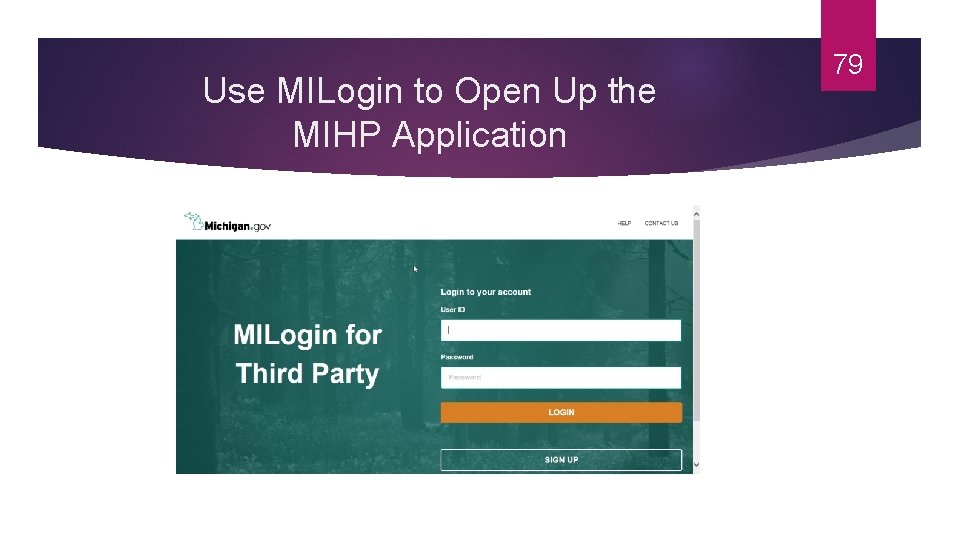
Use MILogin to Open Up the MIHP Application 79
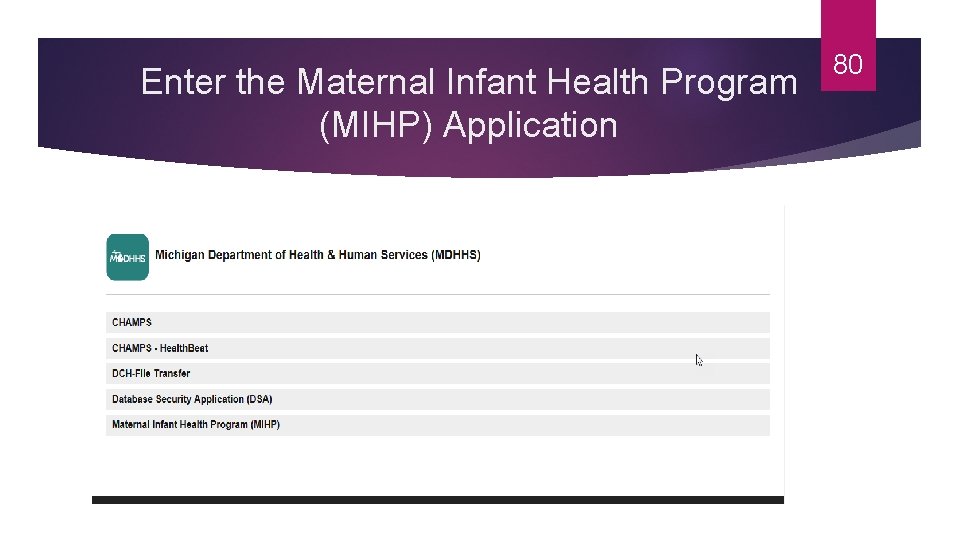
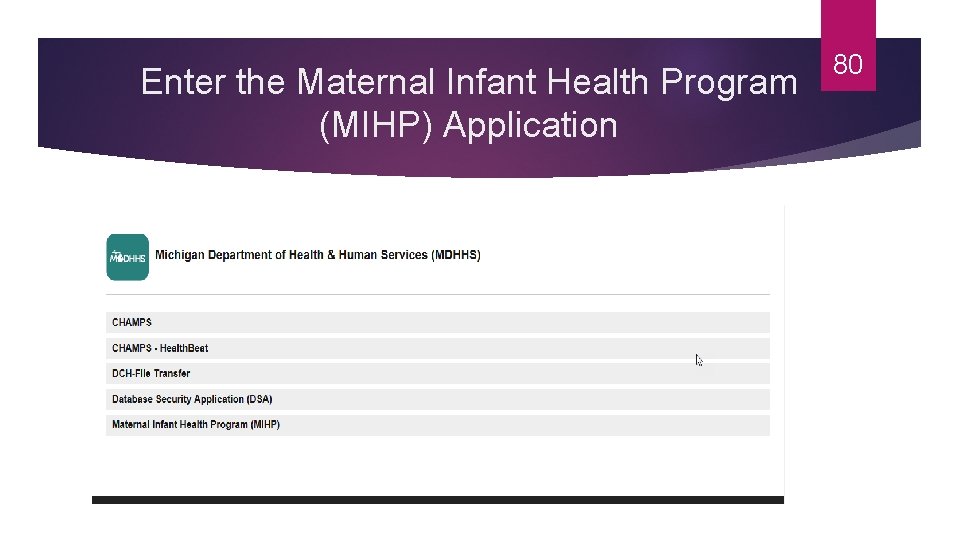
Enter the Maternal Infant Health Program (MIHP) Application 80
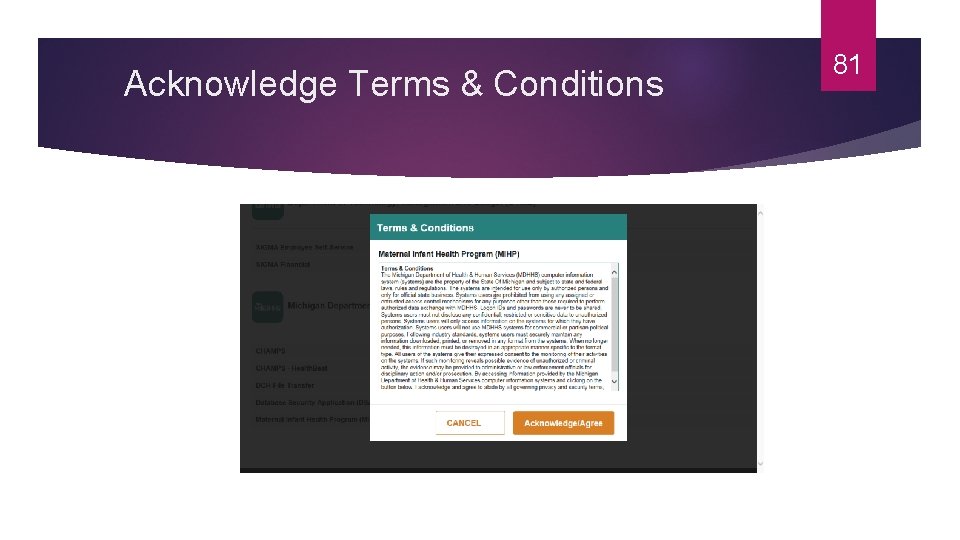
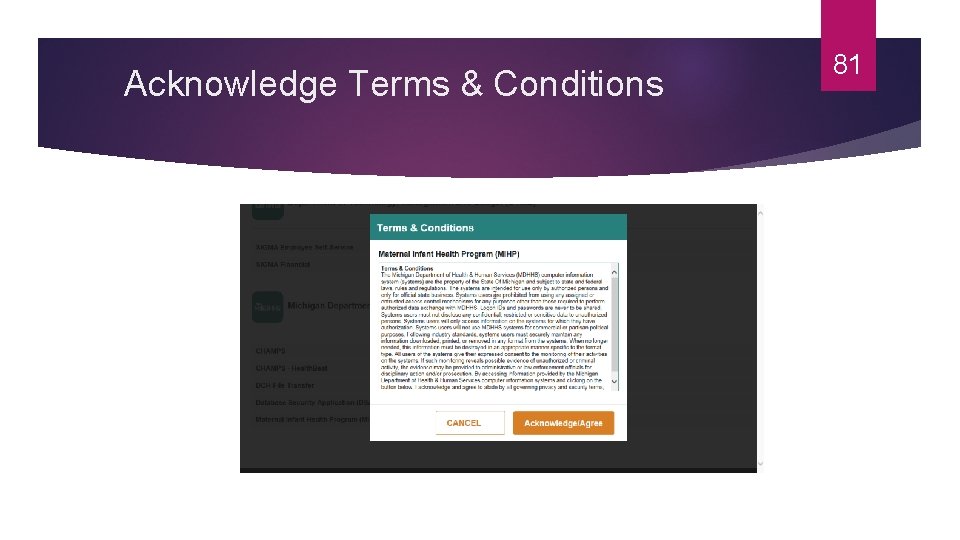
Acknowledge Terms & Conditions 81
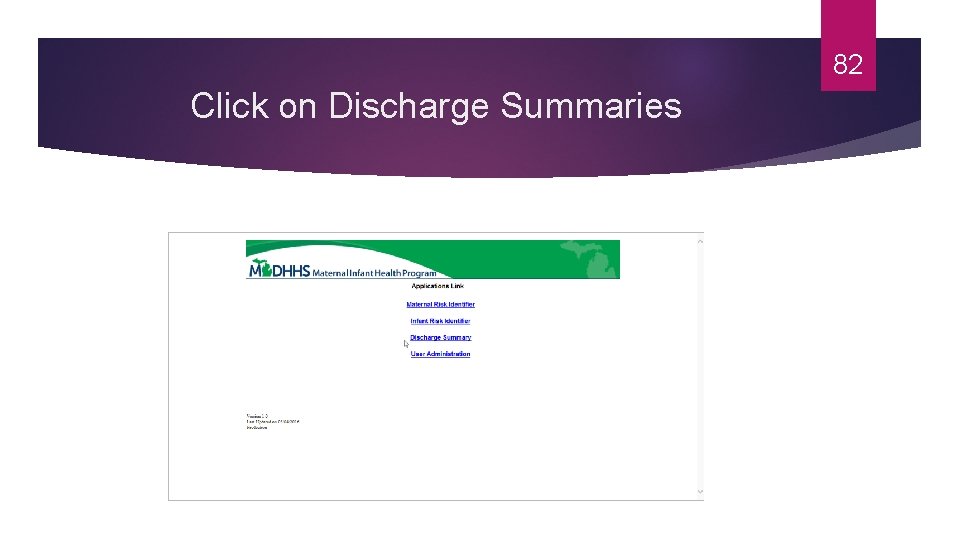
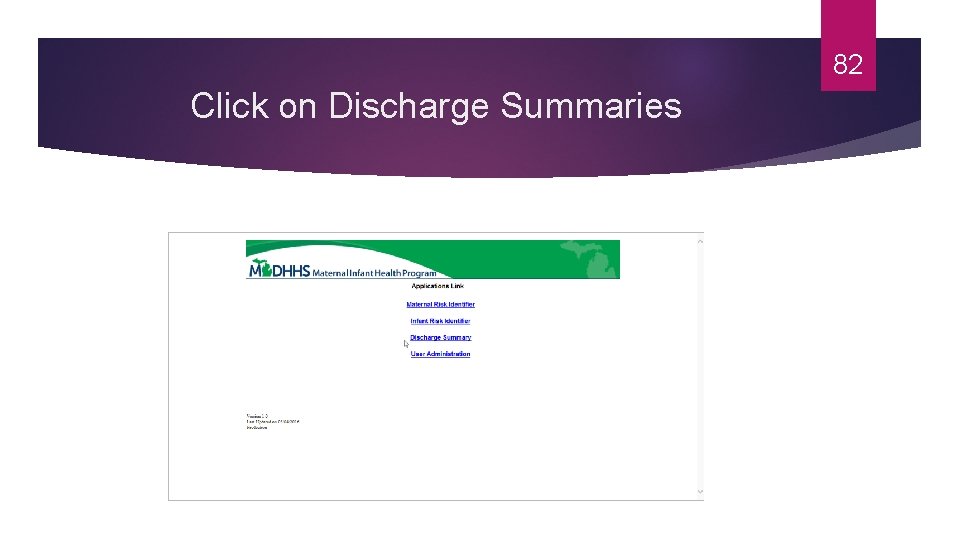
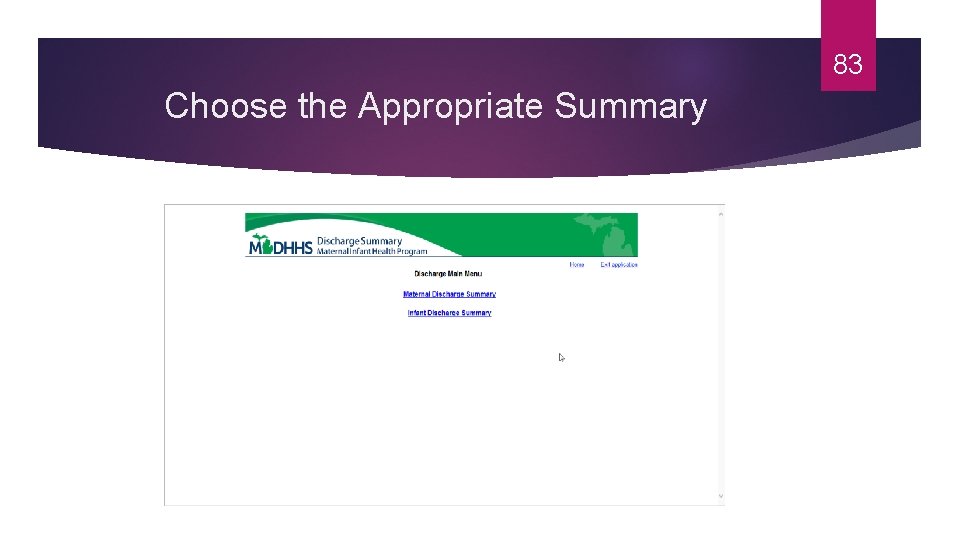
82 Click on Discharge Summaries
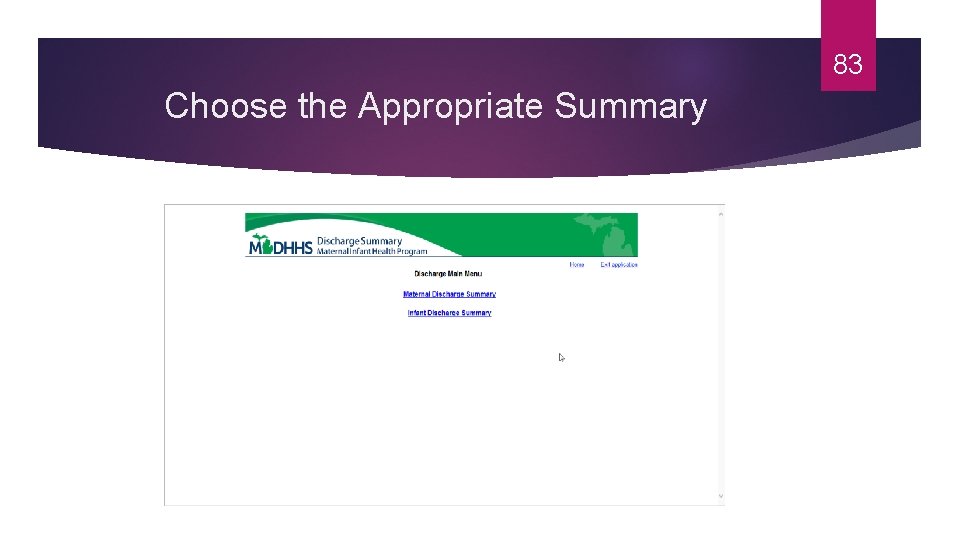
83 Choose the Appropriate Summary
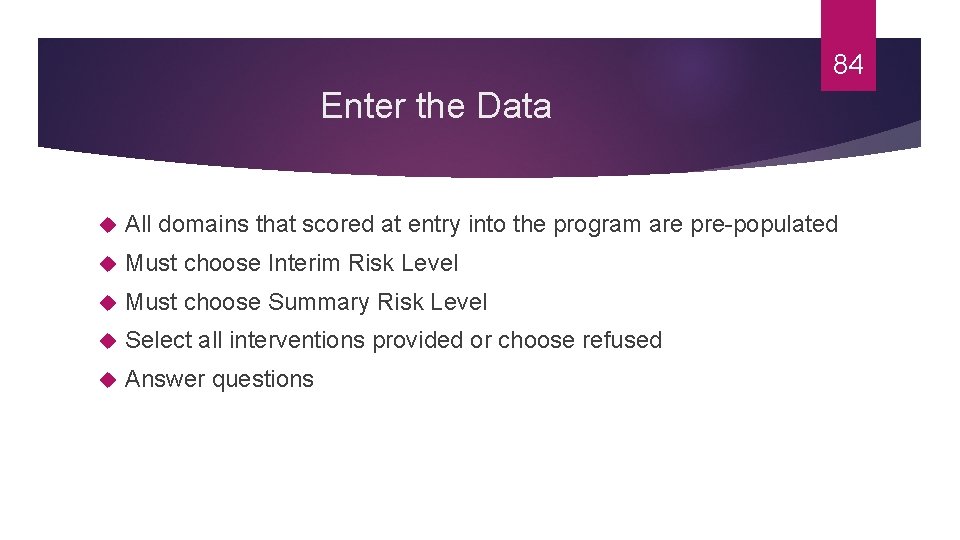
84 Enter the Data All domains that scored at entry into the program are pre-populated Must choose Interim Risk Level Must choose Summary Risk Level Select all interventions provided or choose refused Answer questions
85 Let’s Enter One Together
Review Data Entries Before Submitting the Discharge Summary Check entries before pressing submit 86
Correcting Data Entries After the Discharge Summary is Submitted If a Discharge Summary was completed in the past 30 days, an agency may correct entries May only correct once If a Discharge Summary needs to be deleted, you must send in deletion request to MDHHS MIHP staff and then re-enter the entire discharge summary 87
Timely Completion Will Avoid Citation at Certification Review 88
89 Timely Completion The Discharge Summaries must be entered into the MDHHS MIHP database within 30 days after: The pregnant woman’s MIHP eligibility period ends The infant services are concluded (e. g. , infant ages out of the program; all available visits have been used; services are no longer required; parent or caregiver requests discontinuation of services; the family moves, etc. ) or there are four consecutive months of inactivity, unless there is documentation in the chart that the case is being kept open for a specific purpose and the purpose is stated.
90 Take-Away Points A Discharge Summary (DS) must be completed for every Risk Identifier (RI) A RI is always tied to the MIHP agency that completed it An agency can complete a DS even if the RI was done by a different agency (in the case of a transfer) The DS is either full or abbreviated
91 More Take-Away Points An abbreviated DS is allowed in a few situations Review entries before submitting the DS May correct entries if the DS was completed within the last 30 days Not submitting the DS within required timelines will result in a citation at certification review
92 Questions?