Vivida Health Provider Transition Training Provider Relations 20202021


- Slides: 29

Vivida Health Provider Transition Training Provider Relations 2020/2021 Confidential – Do Not Distribute 0
Provider Service Network (PSN) Transition to New Third Party Administrator (TPA) Claims Submission Prior Authorization Requests Provider Portal Access Continuity During Transition Confidential – Do Not Distribute 1
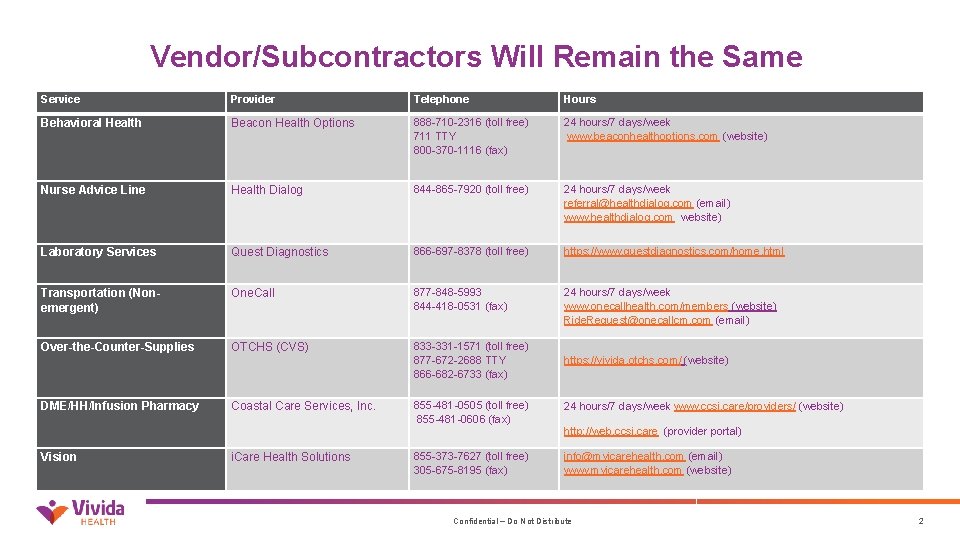
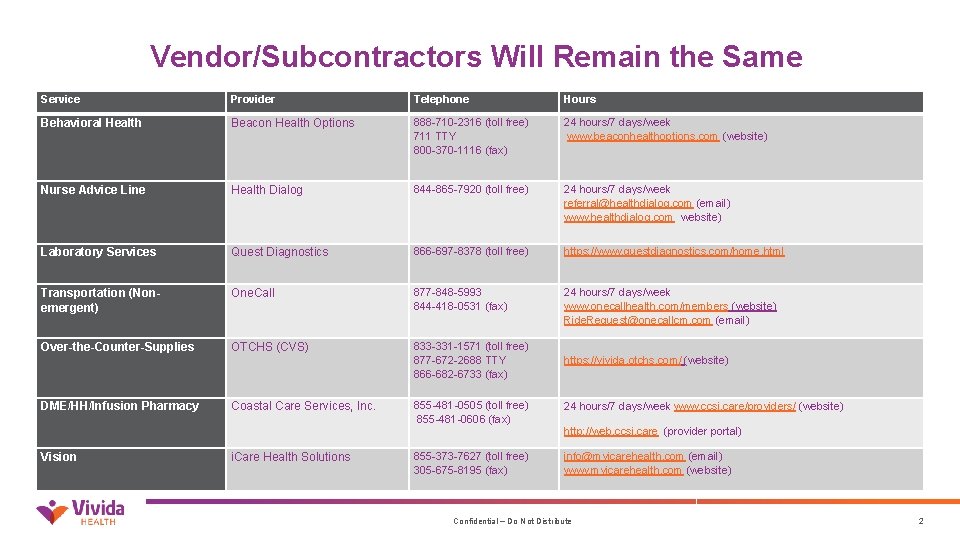
Vendor/Subcontractors Will Remain the Same Service Provider Telephone Hours Behavioral Health Beacon Health Options 888 -710 -2316 (toll free) 711 TTY 800 -370 -1116 (fax) 24 hours/7 days/week www. beaconhealthoptions. com (website) Nurse Advice Line Health Dialog 844 -865 -7920 (toll free) 24 hours/7 days/week referral@healthdialog. com (email) www. healthdialog. com website) Laboratory Services Quest Diagnostics 866 -697 -8378 (toll free) https: //www. questdiagnostics. com/home. html Transportation (Nonemergent) One. Call 877 -848 -5993 844 -418 -0531 (fax) 24 hours/7 days/week www. onecallhealth. com/members (website) Ride. Request@onecallcm. com (email) Over-the-Counter-Supplies OTCHS (CVS) 833 -331 -1571 (toll free) 877 -672 -2688 TTY 866 -682 -6733 (fax) DME/HH/Infusion Pharmacy Vision Coastal Care Services, Inc. i. Care Health Solutions https: //vivida. otchs. com/ (website) 855 -481 -0505 (toll free) 855 -481 -0606 (fax) 24 hours/7 days/week www. ccsi. care/providers/ (website) 855 -373 -7627 (toll free) 305 -675 -8195 (fax) info@myicarehealth. com (email) www. myicarehealth. com (website) http: //web. ccsi. care (provider portal) Confidential – Do Not Distribute 2
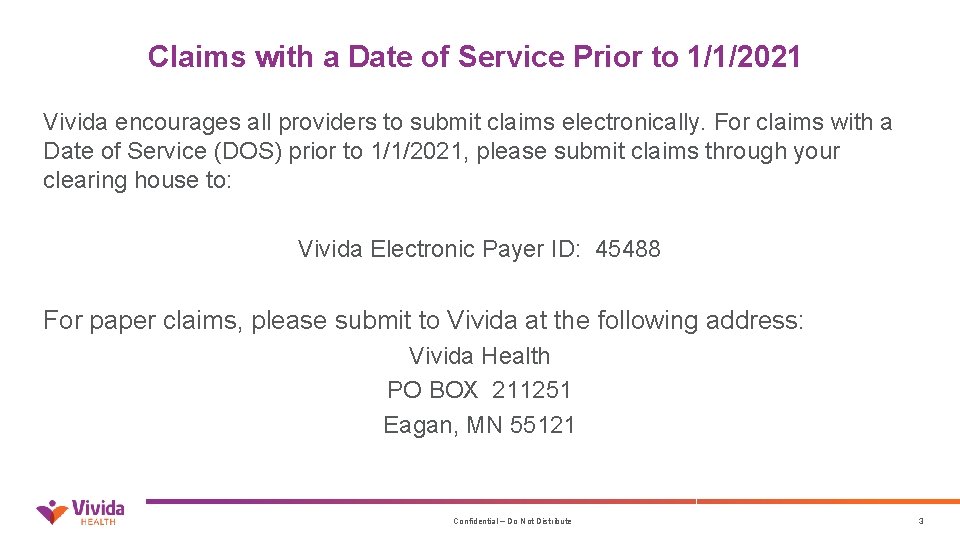
Claims with a Date of Service Prior to 1/1/2021 Vivida encourages all providers to submit claims electronically. For claims with a Date of Service (DOS) prior to 1/1/2021, please submit claims through your clearing house to: Vivida Electronic Payer ID: 45488 For paper claims, please submit to Vivida at the following address: Vivida Health PO BOX 211251 Eagan, MN 55121 Confidential – Do Not Distribute 3
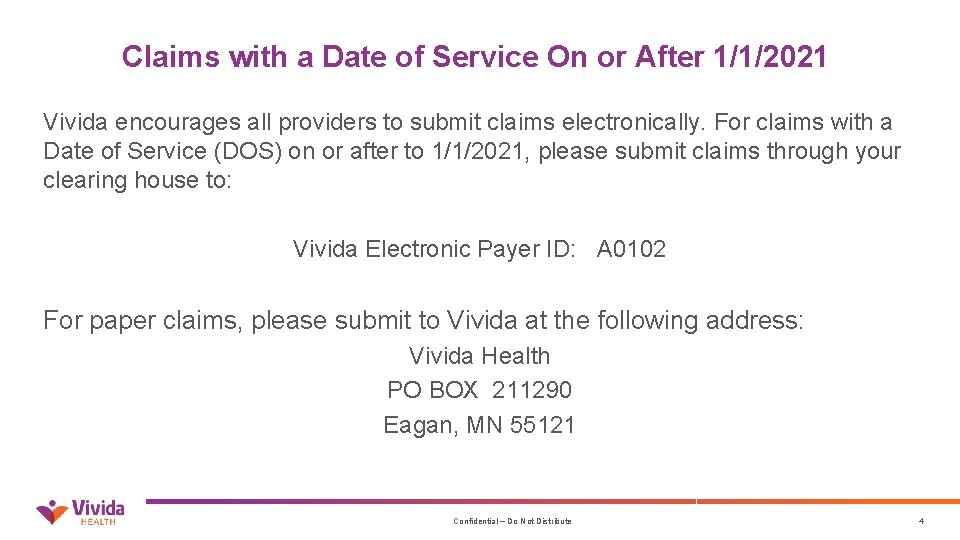
Claims with a Date of Service On or After 1/1/2021 Vivida encourages all providers to submit claims electronically. For claims with a Date of Service (DOS) on or after to 1/1/2021, please submit claims through your clearing house to: Vivida Electronic Payer ID: A 0102 For paper claims, please submit to Vivida at the following address: Vivida Health PO BOX 211290 Eagan, MN 55121 Confidential – Do Not Distribute 4
Corrected Claims with a Date of Service Prior to 1/1/2021 Corrected claims can be sent electronically. All corrected claims should have the corrected claim indicator (a 7) on the claim and the original claim number that you are correcting. Claims originally denied for missing/invalid information for inappropriate coding should be submitted as corrected claims. In addition to writing “corrected” on the claim, the corrected information should be circled so that it can be identified. Claims originally denied for additional information should be sent as a resubmitted claim. In addition to writing “resubmitted” on the claim, the additional/new information should be attached. Corrected and resubmitted paper claims are scanned during reprocessing. Please use blue or black ink only, and refrain from using red ink, white out, and/or highlighting that could affect the legibility of the scanned claim. Corrected/Resubmitted paper claims should be sent to: Vivida Health PO BOX 211251 Eagan, MN 55121 Confidential – Do Not Distribute 5
Corrected Claims with a Date of Service on or After 1/1/2021 Corrected claims can be sent electronically. All corrected claims should have the corrected claim indicator (a 7) on the claim and the original claim number that you are correcting. Claims originally denied for missing/invalid information for inappropriate coding should be submitted as corrected claims. In addition to writing “corrected” on the claim, the corrected information should be circled so that it can be identified. Claims originally denied for additional information should be sent as a resubmitted claim. In addition to writing “resubmitted” on the claim, the additional/new information should be attached. Corrected and resubmitted paper claims are scanned during reprocessing. Please use blue or black ink only, and refrain from using red ink, white out, and/or highlighting that could affect the legibility of the scanned claim. Corrected/Resubmitted paper claims should be sent to: Vivida Health PO BOX 211290 Eagan, MN 55121 Confidential – Do Not Distribute 6
Electronic Funds Transfer (EFT) Vivida is working with ILS / EClaims to deliver claim payments via electronic remittance advice (ERA) and electronic funds transfer (EFT). ERA/EFT is a convenient, paperless and secure way to receive claim payments. The below information is needed for Online Registration includes: • Tax ID • Email Address • Legal Business Name • Business Address/Phone • Principal Name (primary decision maker) • Billing NPI Number • Bank Name • Bank Routing Number To register please email Vivida. EFT@ilshealth. com. Confidential – Do Not Distribute 7
Provider Handbook Updates The Provider Handbook explains the policies, procedures and requirements of delivering healthcare services to Vivida members including your responsibilities as a participating provider. It is a guide to answer questions about member benefits, claim submissions, and many other issues. This information has been updated to reflect the updated information related to the transition to the new TPA. The Provider Handbook is available online at www. Vivida. Health. com. Providers may request printed copies of the Provider Handbook, at no cost, by contacting Provider Services at 1 -844 -243 -5175. Updates to this Provider Handbook will be posted on Vivida’s website on a periodic basis. Confidential – Do Not Distribute 8
Provider Directory Vivida providers may access a copy of the Provider Directory online at www. Vivida. Health. com Providers may request a printed copy of the Provider Directory by contacting Provider Services at 1 -844 -243 -5175. Confidential – Do Not Distribute 9
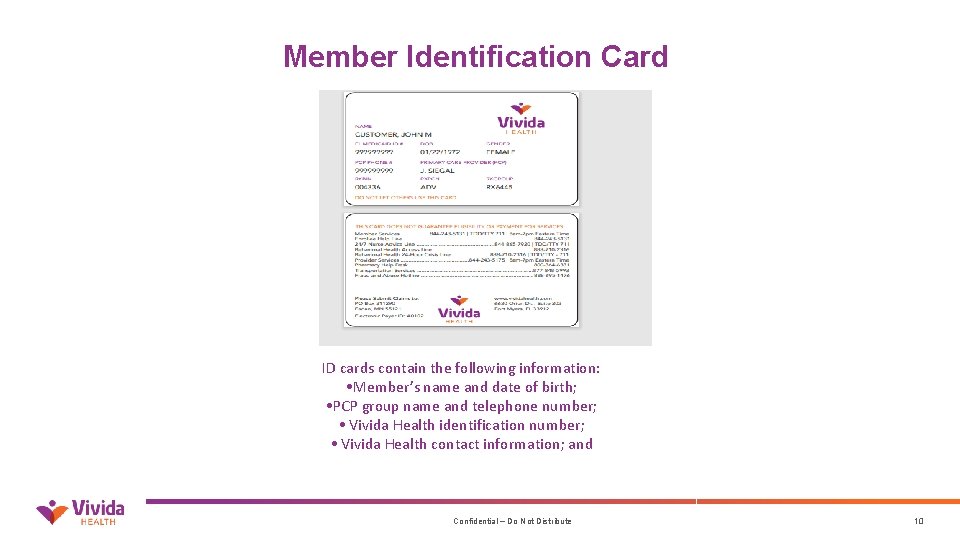
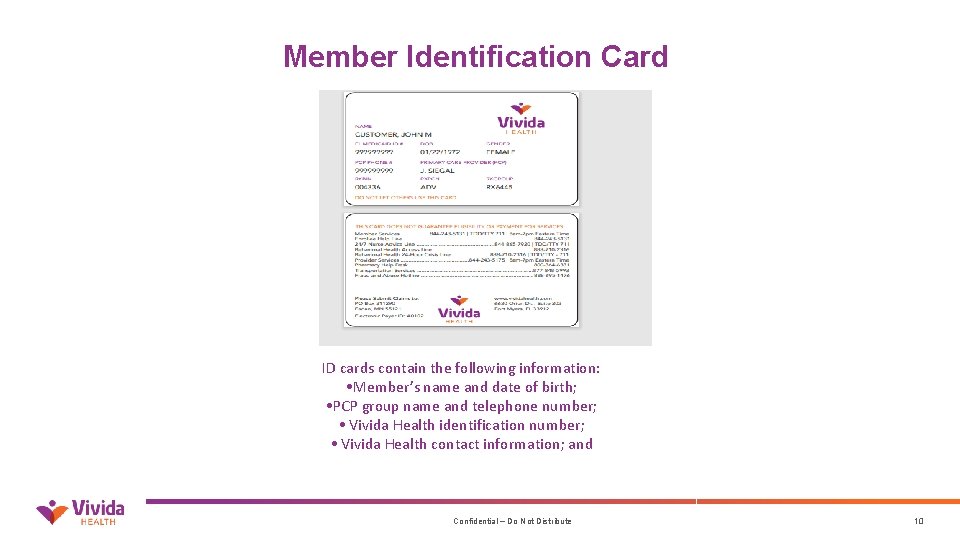
Member Identification Card ID cards contain the following information: • Member’s name and date of birth; • PCP group name and telephone number; • Vivida Health identification number; • Vivida Health contact information; and Confidential – Do Not Distribute 10
Verifying Member Eligibility Participating providers are responsible for verifying member eligibility before providing services as eligibility may vary per month. Providers may verify eligibility using the following methods: • Online – Log into the Provider Portal at www. Vivida. Health. com • IVR Automated System at 1 -844 -243 -5131 • Customer Service 1 -844 -243 -5131 Confidential – Do Not Distribute 11
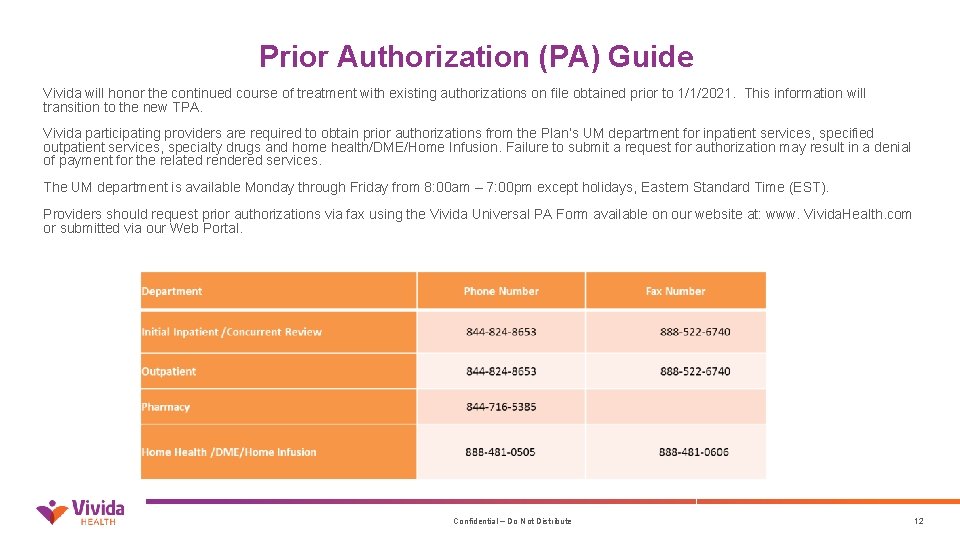
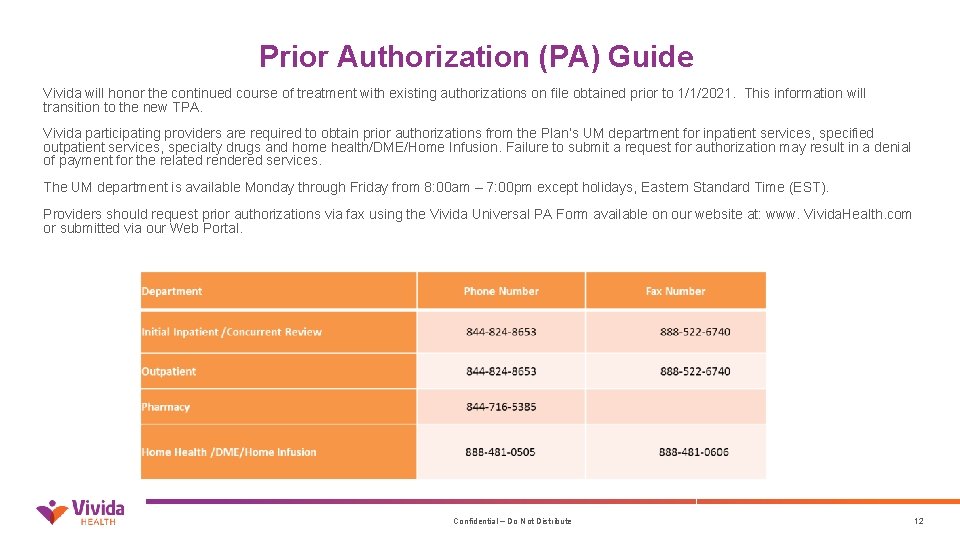
Prior Authorization (PA) Guide Vivida will honor the continued course of treatment with existing authorizations on file obtained prior to 1/1/2021. This information will transition to the new TPA. Vivida participating providers are required to obtain prior authorizations from the Plan’s UM department for inpatient services, specified outpatient services, specialty drugs and home health/DME/Home Infusion. Failure to submit a request for authorization may result in a denial of payment for the related rendered services. The UM department is available Monday through Friday from 8: 00 am – 7: 00 pm except holidays, Eastern Standard Time (EST). Providers should request prior authorizations via fax using the Vivida Universal PA Form available on our website at: www. Vivida. Health. com or submitted via our Web Portal. Confidential – Do Not Distribute 12
Prior Authorization (PA) Guide Providing complete information allows for timely processing by the Prior Authorization Department. The following information is generally requested for all authorizations. • • • Member name Member identification number Provider ID and NPI number or name of the treating physician Facility ID and NPI number or name where services will be rendered (when appropriate) Provider and/or facility fax number Date(s) of service Diagnosis and diagnostic codes CPT codes Any relevant clinical information to support medical necessity of request The Prior Authorization (PA) Guides including specialty drugs are available on our website, at: www. vividahealth. com Confidential – Do Not Distribute 13
Provider Notifications It is important for Vivida to keep its provider network information up-to-date. Up-to-date provider information allows Vivida to accurately generate provider directories, process claims and communicate with its network of providers. Providers must notify Vivida in writing at least 60 days in advance when possible of changes, such as: • Change in practice ownership or Federal TAX ID number • Practice name change • A change in practice address, phone or fax numbers • Change in practice office hours • New office site location • Primary Care Providers (PCP) only: If your practice is open or closed to new patients The provider data change form can be found at www. vividahealth. com – provider portal link Provider must notify Vivida immediately if any of the following actions occur: • Provider’s business license to practice in any state is suspended, surrendered, revoked, terminated, or subject to terms of probation or other restrictions • Provider is the subject of any criminal investigation or proceeding • Provider is convicted for crimes involving moral turpitude or felonies • Provider is named in any civil claim, or any criminal investigation or proceeding • Provider becomes incapacitated such that the incapacity may interfere with member care for 24 hours • Provider’s professional or general liability insurance is reduced or canceled • Any other action or occurrence which affects the provider’s ability to carry out its duties under the provider contract agreement Send changes via: email at providerrelations@vividahealth. com or fax: 1 -888 -396 -1226 Confidential – Do Not Distribute 14
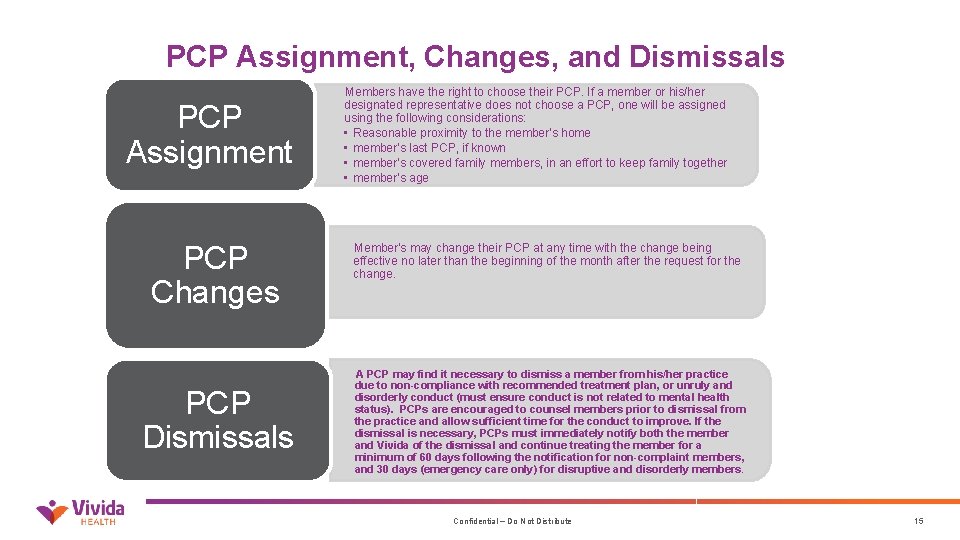
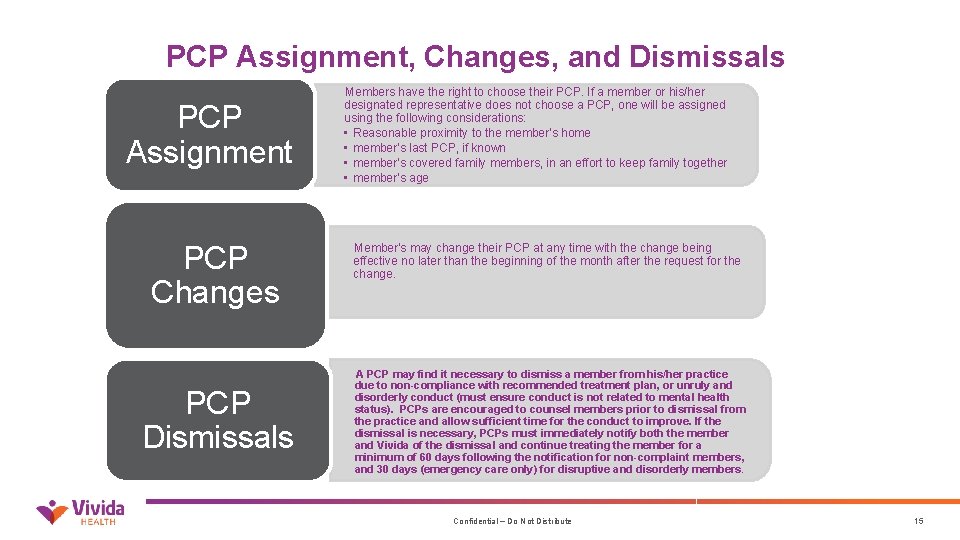
PCP Assignment, Changes, and Dismissals PCP Assignment PCP Changes PCP Dismissals Members have the right to choose their PCP. If a member or his/her designated representative does not choose a PCP, one will be assigned using the following considerations: • Reasonable proximity to the member’s home • member’s last PCP, if known • member’s covered family members, in an effort to keep family together • member’s age Member's may change their PCP at any time with the change being effective no later than the beginning of the month after the request for the change. A PCP may find it necessary to dismiss a member from his/her practice due to non-compliance with recommended treatment plan, or unruly and disorderly conduct (must ensure conduct is not related to mental health status). PCPs are encouraged to counsel members prior to dismissal from the practice and allow sufficient time for the conduct to improve. If the dismissal is necessary, PCPs must immediately notify both the member and Vivida of the dismissal and continue treating the member for a minimum of 60 days following the notification for non-complaint members, and 30 days (emergency care only) for disruptive and disorderly members. Confidential – Do Not Distribute 15
Translation Services Members may receive interpreter services at no cost when necessary to access covered services. Interpreter services available include verbal translation and sign language for the hearing impaired. Providers should assist in the coordination of interpreter services for members by contacting Vivida Member Services at 1 -844 -243 -5131. Confidential – Do Not Distribute 16
Care Management is a collaborative process of assessment, planning, facilitation, care coordination, evaluation, and advocacy for options and services to meet an individual’s and family’s comprehensive healthcare needs through communication and available resources to promote quality cost-effective outcomes. Members who may benefit from case management are those with ongoing complex medical needs or those at risk for an avoidable adverse outcome/event. Providers, as well as members and other interested parties, may request Care Management services. Providers may contact Provider Services at 1 -844 -243 -5175 to request Care Management If you would like to speak with the Care Manager once he or she is assigned, notify the Provider Services Department. Participation in Care Management is voluntary, and the member has the right to decline any or all parts of the program. Confidential – Do Not Distribute 17
Grievances & Appeals Vivida has dedicated staff to assist providers with the resolution of filed complaints. Provider may file a complaint by: • Phone: 1 -844 -243 -5175 • Fax: 1 -888 -396 -1226 • Email: appeals@vividahealth. com • Mail: Vivida Health Attn: Grievance & Appeals Department 6630 Orion Drive, Ste 203 Fort Myers, FL 33912 Non- Claim related issues: • Vivida shall allow providers forty-five (45) days to file a written Complaint. • Within three (3) business days of receipt of a Complaint, notify the provider (verbally or in writing) that the Complaint has been received and the expected date of resolution; • Thoroughly investigate each provider Complaint using applicable statutory regulatory, contractual, and provider agreement provisions; collect all pertinent facts from all parties; and apply applicable plan written procedures; • Provide written notice of the status to the provider every fifteen (15) days thereafter; and • Resolve all Complaints within ninety (90) days of receipt and provide written notice of the disposition and the basis of the resolution to the provider within three (3) business days of resolution. Claim related issues: • Allow providers ninety days (90) from the date of the final determination for the primary payer to file a written Complaint for claims issues; • Within three (3) business days of receipt of a claim Complaint, notify the provider (verbally or in writing) that the Complaint has been received and the expected date of resolution; • Within fifteen (15) days of receipt of a claim Complaint, provide written notice of the status of the Complaint to the Agency and to the provider. For claims issues that require additional time to research, Vivida must submit a written request to the Agency within three (3) business days of receipt of the Complaint that includes: o An explanation for the need of an extension; and o The expected time needed beyond the fifteen (15) days for research and response. o Approval is contingent upon Agency review. o Vivida must provide written notice of the status to the provider every fifteen (15) days thereafter; and • In accordance with 641. 3155, F. S. , resolve all claims Complaints within sixty (60) days of receipt and provide written notice of the disposition and the basis of the resolution to the provider within three (3) business days of resolution. Confidential – Do Not Distribute 18
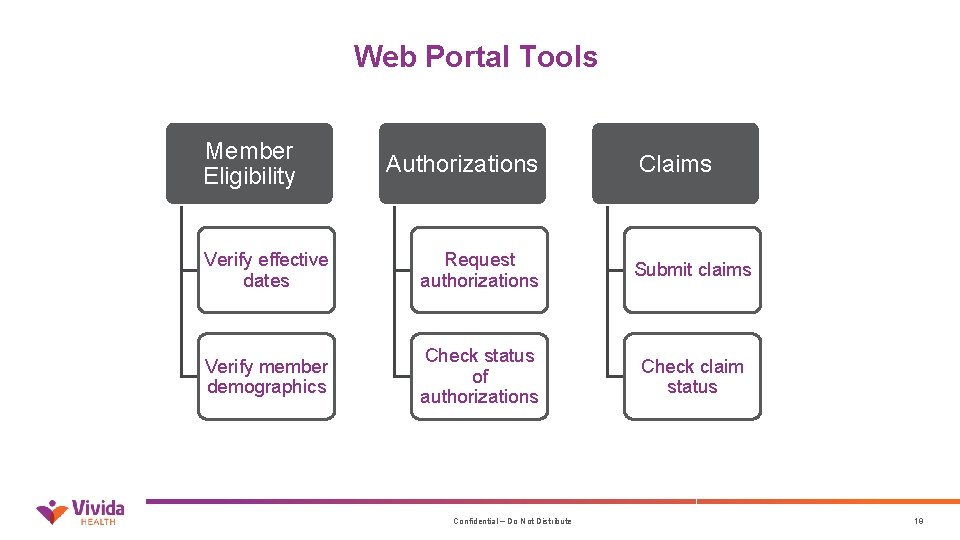
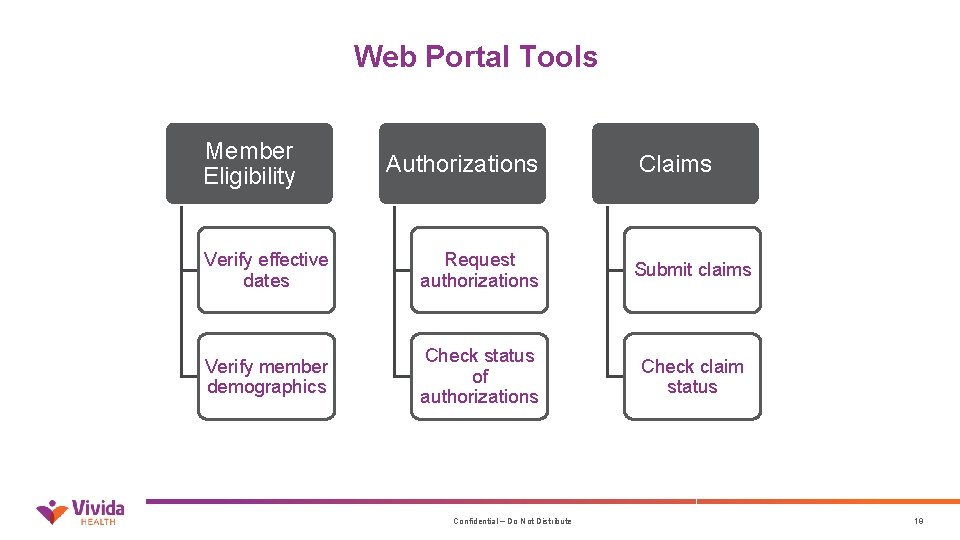
Web Portal Tools Member Eligibility Authorizations Claims Verify effective dates Request authorizations Submit claims Verify member demographics Check status of authorizations Check claim status Confidential – Do Not Distribute 19
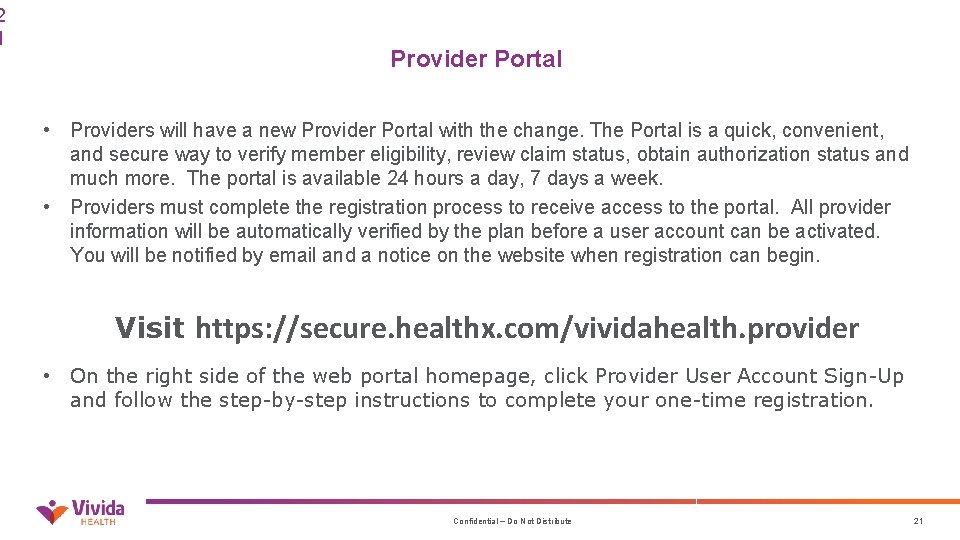
2 0 Provider Portal – Claims and Processed Authorizations • Providers will have a new Provider Portal with the TPA change for activities, authorization and claims after 1/1/2021. Should you have inquiries for activities prior to 1/1/2021 – please review the existing portal. The Portal is a quick, convenient, and secure way to verify member eligibility, review claim status, obtain authorization status and much more. The portal is available 24 hours a day, 7 days a week. • Providers must complete the registration process to receive access to the portal. All provider information will be automatically verified by the plan before a user account can be activated. The registration is now open for all providers! • Registration is quick and easy! Visit https: //secure. healthx. com/vividahealth. provider • On the right side of the web portal homepage, click Provider User Account Sign-Up and follow the step-by-step instructions to complete your one-time registration. Confidential – Do Not Distribute 20
2 1 Provider Portal • Providers will have a new Provider Portal with the change. The Portal is a quick, convenient, and secure way to verify member eligibility, review claim status, obtain authorization status and much more. The portal is available 24 hours a day, 7 days a week. • Providers must complete the registration process to receive access to the portal. All provider information will be automatically verified by the plan before a user account can be activated. You will be notified by email and a notice on the website when registration can begin. Visit https: //secure. healthx. com/vividahealth. provider • On the right side of the web portal homepage, click Provider User Account Sign-Up and follow the step-by-step instructions to complete your one-time registration. Confidential – Do Not Distribute 21
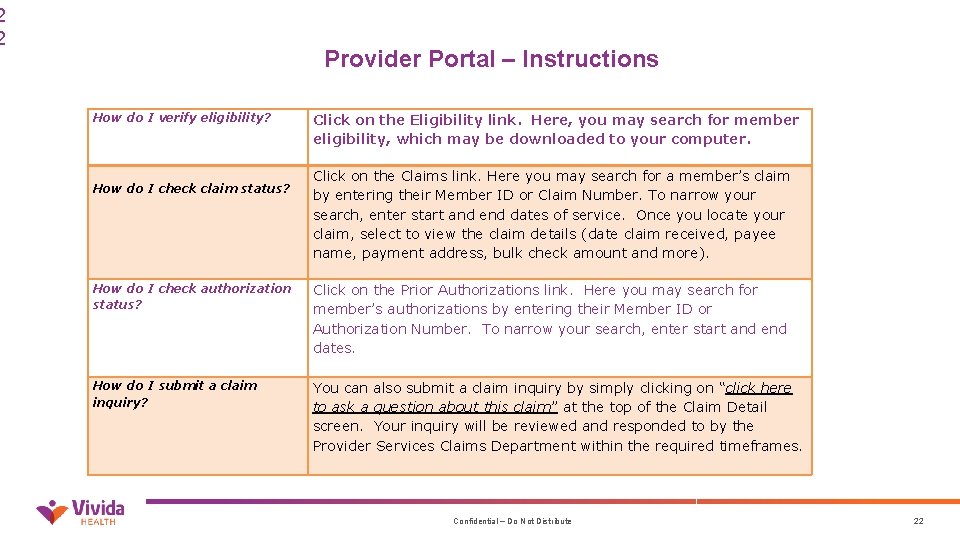
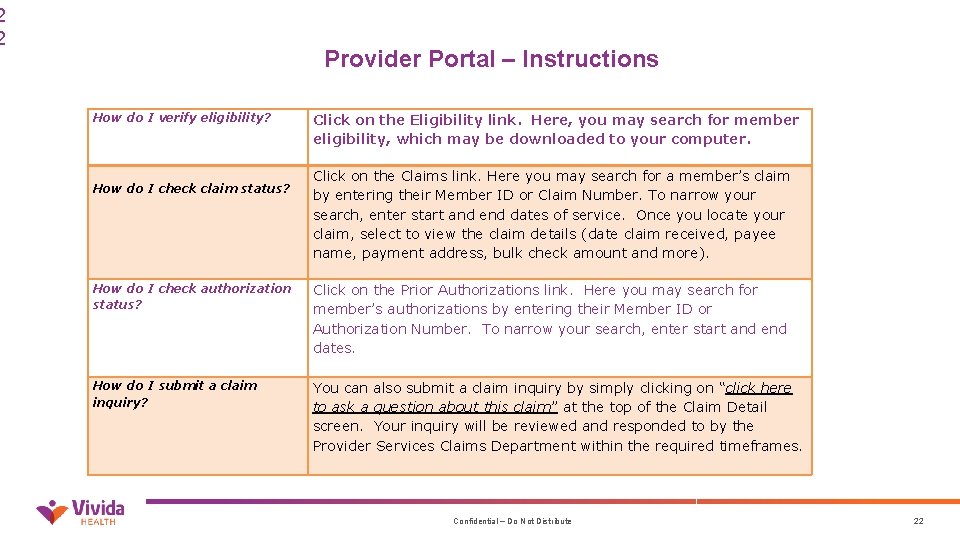
2 2 Provider Portal – Instructions How do I verify eligibility? How do I check claim status? Click on the Eligibility link. Here, you may search for member eligibility, which may be downloaded to your computer. Click on the Claims link. Here you may search for a member’s claim by entering their Member ID or Claim Number. To narrow your search, enter start and end dates of service. Once you locate your claim, select to view the claim details (date claim received, payee name, payment address, bulk check amount and more). How do I check authorization status? Click on the Prior Authorizations link. Here you may search for member’s authorizations by entering their Member ID or Authorization Number. To narrow your search, enter start and end dates. How do I submit a claim inquiry? You can also submit a claim inquiry by simply clicking on “click here to ask a question about this claim” at the top of the Claim Detail screen. Your inquiry will be reviewed and responded to by the Provider Services Claims Department within the required timeframes. Confidential – Do Not Distribute 22
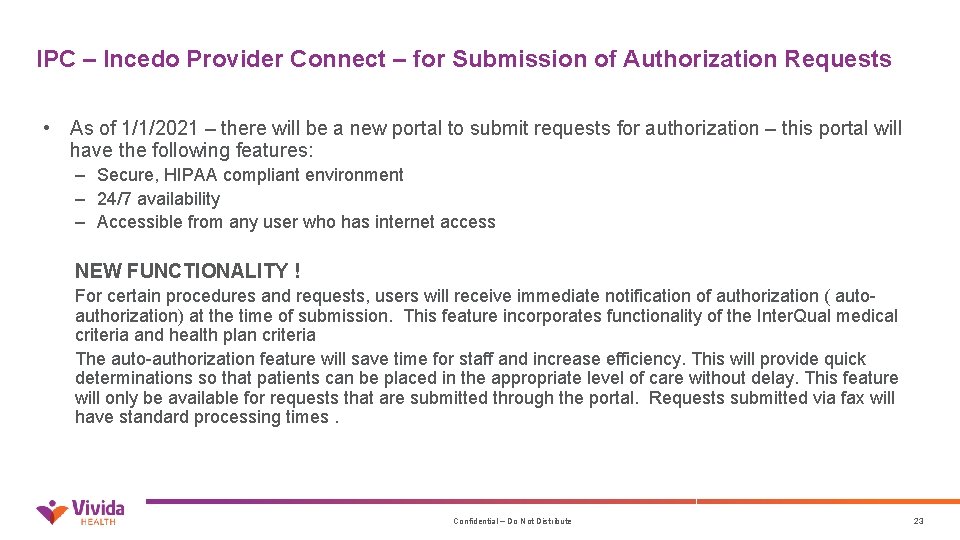
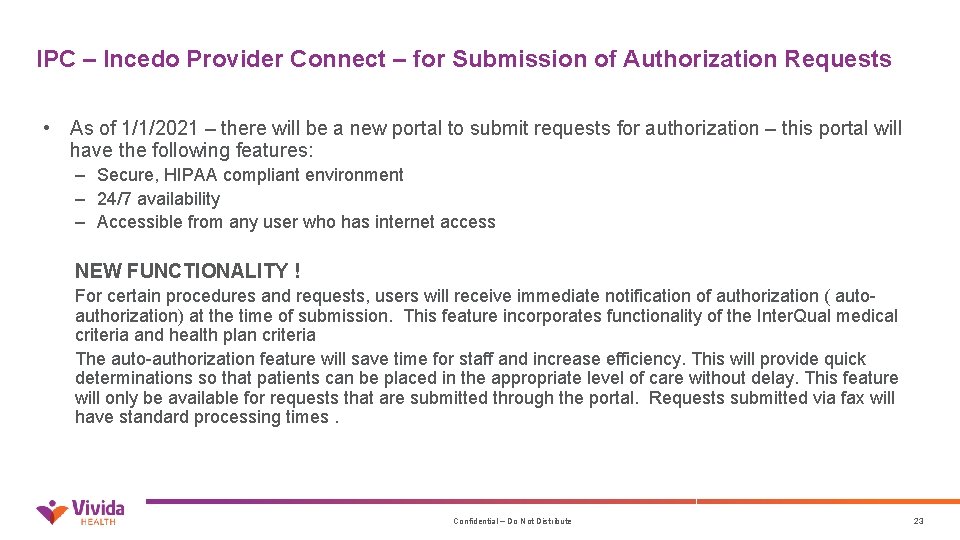
IPC – Incedo Provider Connect – for Submission of Authorization Requests • As of 1/1/2021 – there will be a new portal to submit requests for authorization – this portal will have the following features: – Secure, HIPAA compliant environment – 24/7 availability – Accessible from any user who has internet access NEW FUNCTIONALITY ! For certain procedures and requests, users will receive immediate notification of authorization ( autoauthorization) at the time of submission. This feature incorporates functionality of the Inter. Qual medical criteria and health plan criteria The auto-authorization feature will save time for staff and increase efficiency. This will provide quick determinations so that patients can be placed in the appropriate level of care without delay. This feature will only be available for requests that are submitted through the portal. Requests submitted via fax will have standard processing times. Confidential – Do Not Distribute 23
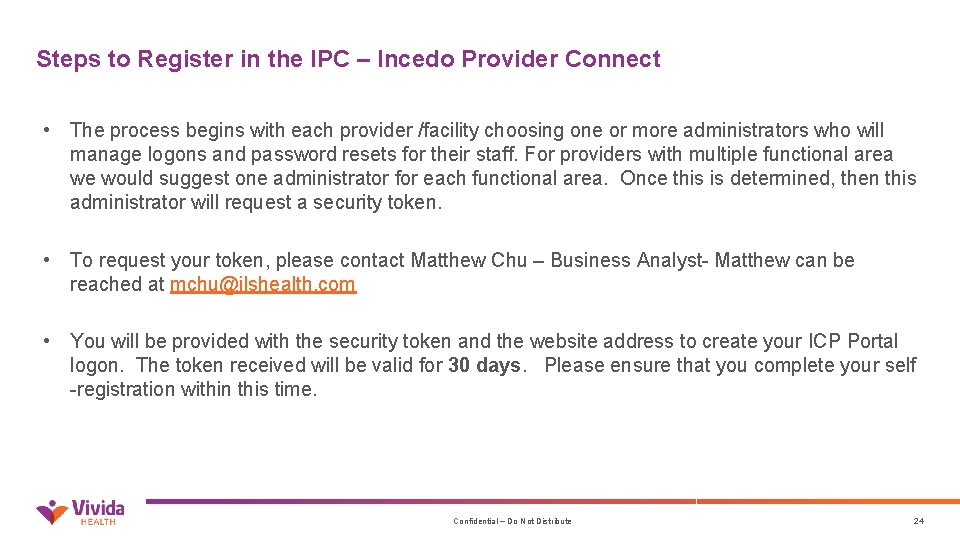
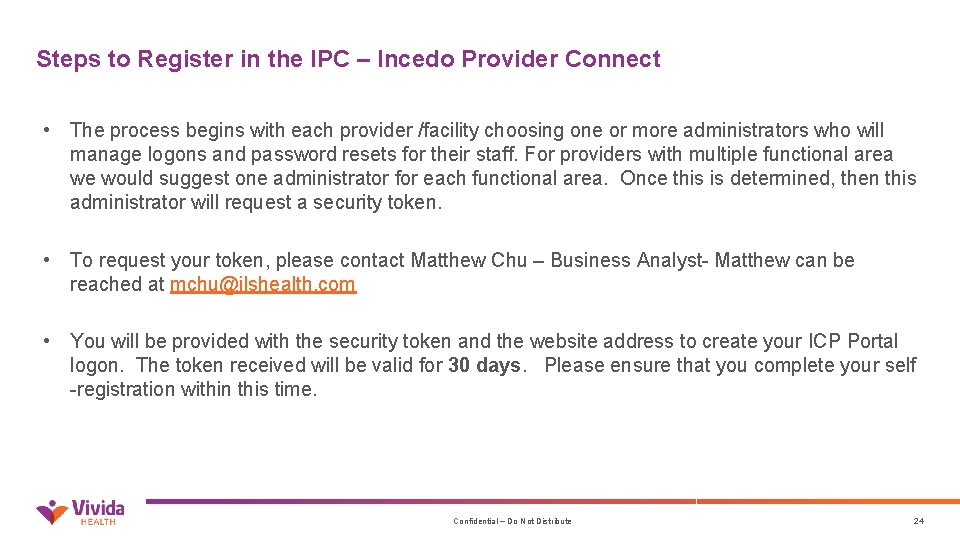
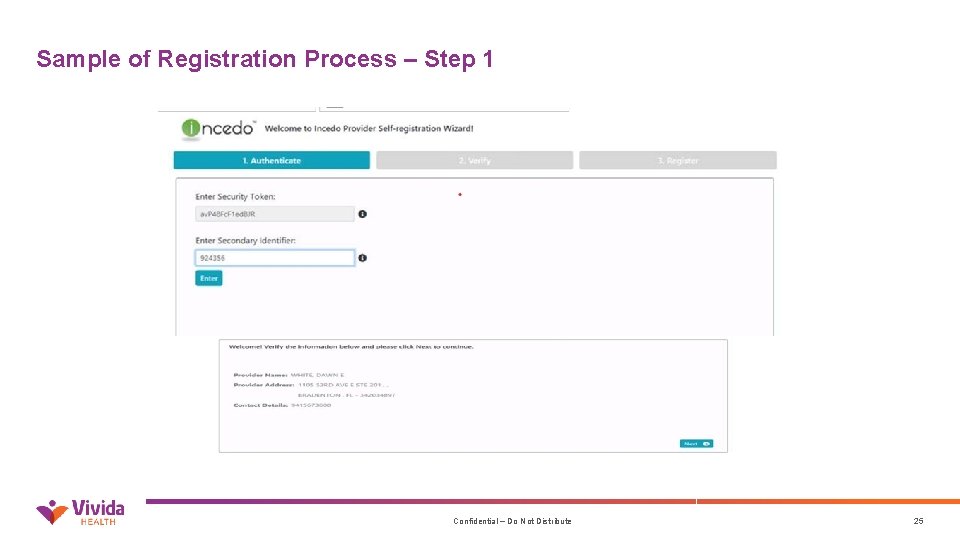
Steps to Register in the IPC – Incedo Provider Connect • The process begins with each provider /facility choosing one or more administrators who will manage logons and password resets for their staff. For providers with multiple functional area we would suggest one administrator for each functional area. Once this is determined, then this administrator will request a security token. • To request your token, please contact Matthew Chu – Business Analyst- Matthew can be reached at mchu@ilshealth. com • You will be provided with the security token and the website address to create your ICP Portal logon. The token received will be valid for 30 days. Please ensure that you complete your self -registration within this time. Confidential – Do Not Distribute 24
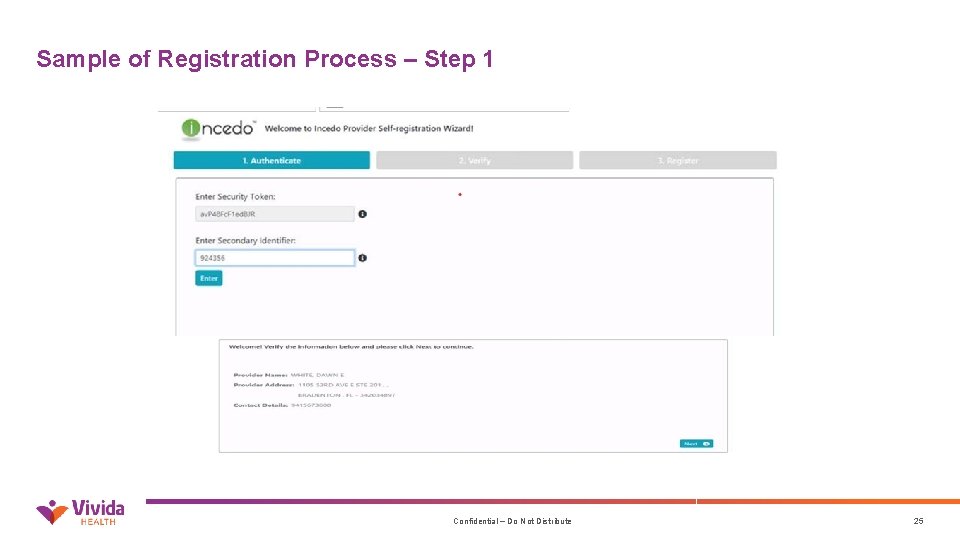
Sample of Registration Process – Step 1 Confidential – Do Not Distribute 25
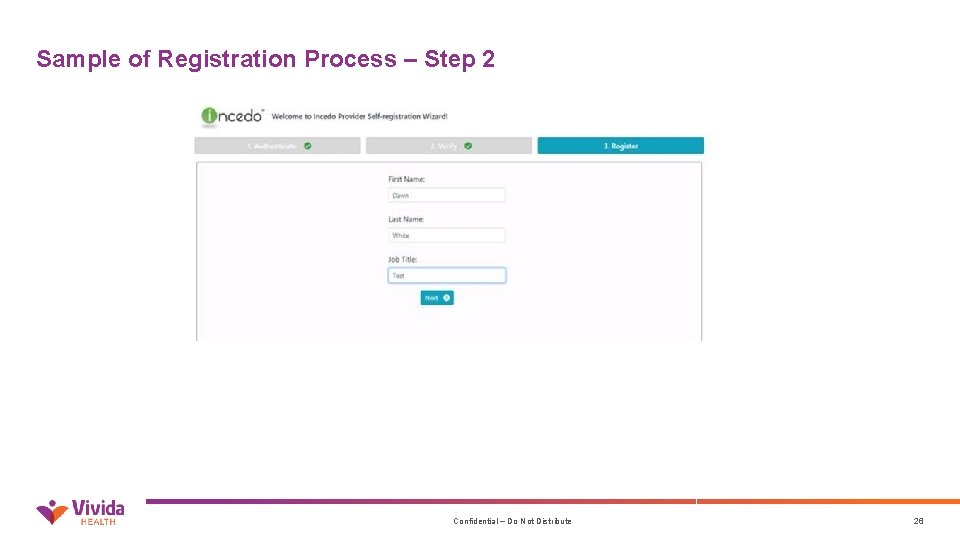
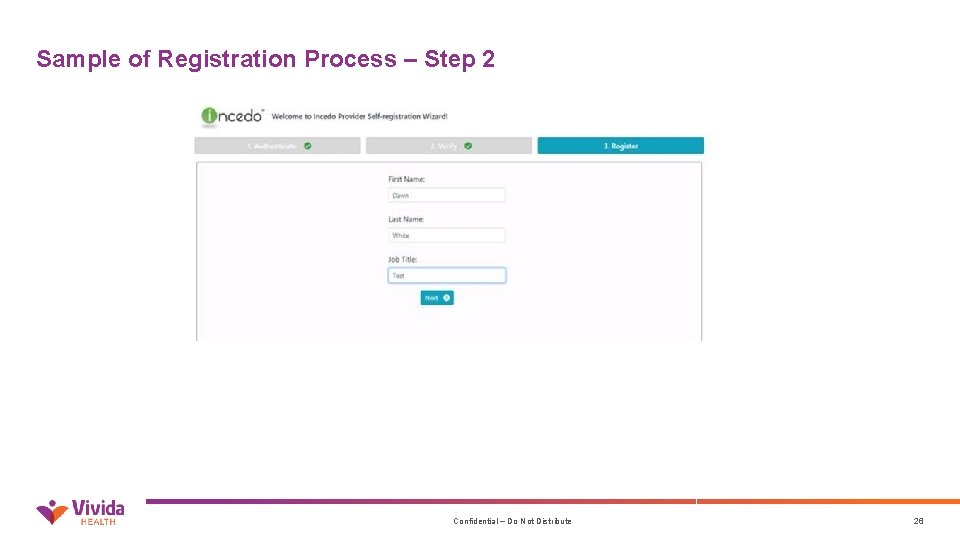
Sample of Registration Process – Step 2 Confidential – Do Not Distribute 26
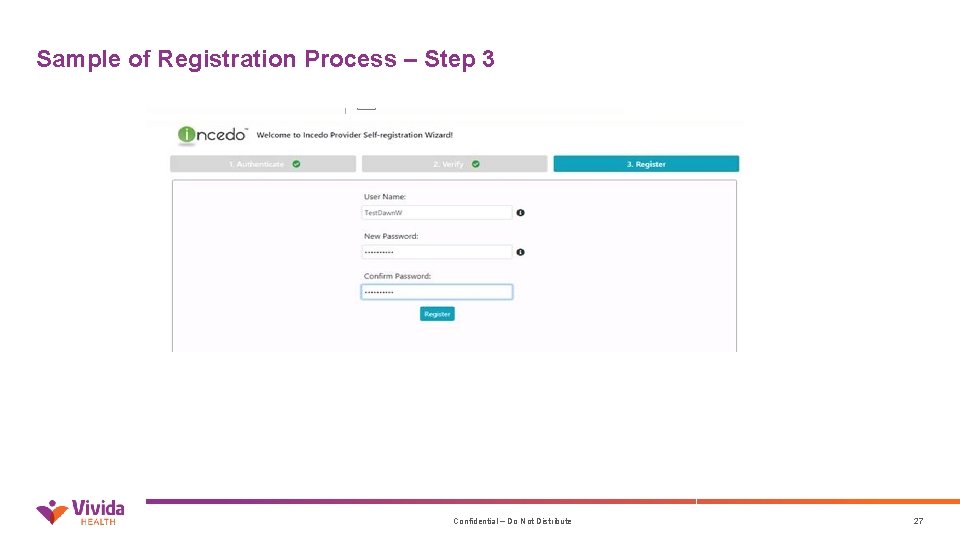
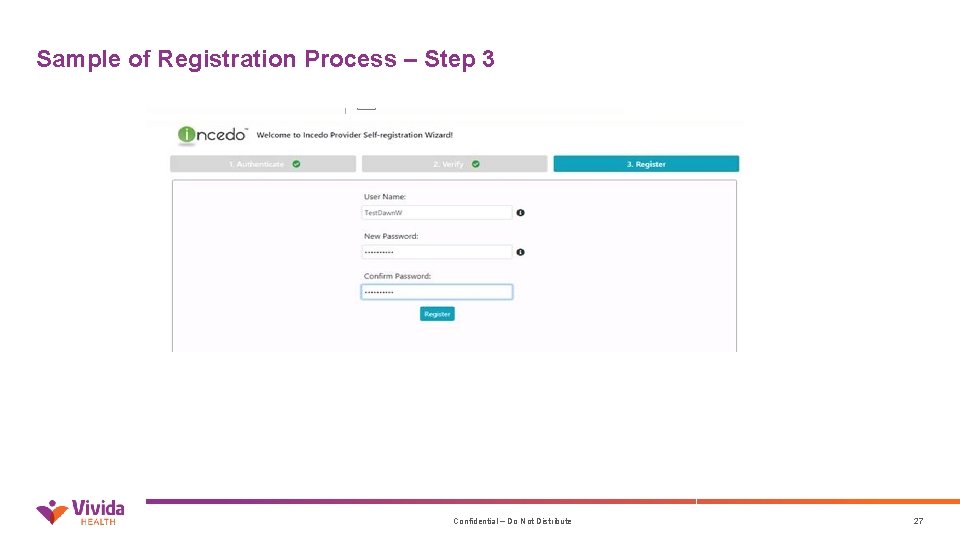
Sample of Registration Process – Step 3 Confidential – Do Not Distribute 27

6630 Orion Dr. Fort Myers, FL 33912 Confidential – Do Not Distribute 28