Mental Health in International Settings Sally Mathiesen Ph





- Slides: 84
Mental Health in International Settings Sally Mathiesen, Ph. D, LCSW Professor San Diego State University School of Social Work Council on Social Work Education | www. cswe. org
Purpose of This Module • To help social workers appreciate the human rights issues that may accompany mental health disorders around the world • To provide an opportunity to discuss the variety of treatments available • To further develop critical thinking skills regarding evidence-based interventions for the population
Suggested Use of the Module – Location in Curriculum • The module could be presented in an elective course on mental health or international studies or placed within an advanced practice course • The module could be presented over one 3 -hour course period (the equivalent of one class session in a semester), with the readings done in advance and small group critique and discussion of the assignment at the end of the class period.
Learning Objectives • Develop enhanced understanding of the complexity of services needed for the population of individuals with mental illness. • Compare and contrast the available resources for treatments for individuals with mental illness in countries around the world. • Incorporate knowledge of mental disorders into treatment planning with enhanced understanding of individual and cultural differences. • Understand critique evidence-based practices for those diagnosed with mental illness.
Connections to EPAS Core Competencies EPAS competencies addressed in this module: • EPAS 2. 1. 3: Apply critical thinking to inform and communicate professional judgments. • EPAS 2. 1. 4: Engage in diversity and difference in practice. • EPAS 2. 1. 5: Advance human rights and social and economic justice • EPAS 2. 1. 6: Engage in research-informed practice and practice-informed research.
Why Global Learning Is Important • Understanding the nature of mental health as a global concept is crucial given the diversity of individuals and families within the United States • Research that has been conducted on a global scale informs social workers working in any location about effective treatment strategies
Relevance of Global Learning for Practice • Global learning prepares social workers to understand inherent differences in complex mental health issues • Knowledge of effective practices that have been used in diverse settings increases social workers’ ability to respond appropriately to clients that have different backgrounds and experiences
The Right to Health • The right to the enjoyment of the highest attainable standard of physical and mental health, to give it its full name, is not new. • Internationally, it was first articulated in the 1946 Constitution of the World Health Organization (WHO). • Source: Committee on Economic, Social & Cultural Rights, and the Office of the High Commissioner for Human Rights.
The Right to Health The WHO preamble defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity. ” Source: Committee on Economic, Social & Cultural Rights, and the Office of the High Commissioner for Human Rights.
What Is Mental Health?
Mental Health “There is no health without mental health. ” (WHO, 2007)
Mental Health Mental health… is more than the absence of mental disorders
Mental Health It is the foundation for wellbeing and effective functioning for the individual and the community This view of mental health is consistent with wide and varied interpretations across cultures
Mental Health Mental health… is linked to behavior • Mental, social, and behavioral health problems may interact to intensify their effects on behavior and well-being
Mental Health Mental health… is determined by socioeconomic and environmental factors
Mental Health “Mental health: A state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community” (WHO, 2007)
Mental Health Greater vulnerability to mental health disorders for disadvantaged people may be related to factors such as – insecurity and hopelessness, – rapid social change, – risks of violence, – physical ill health (WHO, 2007)
Connecting Effectively With Diverse Communities • The greater need for mental health services for disadvantaged individuals requires service providers to bridge some of the barriers that may exist • Cultural competence is a key factor in facilitating mental health treatment for all groups
Accessing Communities: Cultural Competence What Is Cultural Competence? Davis (1997) operationally defined cultural competency as the integration and transformation of knowledge, information, and data about individuals and groups of people into specific clinical standards, skills, service approaches, techniques, and marketing programs that match the individual’s culture and increase the quality and appropriateness of health care and outcomes.
Cultural Competence In the United States diverse communities often do not have adequate access to mental health treatment because of a “variety of barriers, including lack of knowledge about available interventions, transportation difficulties, competing familial responsibilities such as child care, family privacy or shame, or community stigma associated with seeking help from mainstream providers” (Saldana, 2001, p. 16).
Outreach Strategies to Diverse Communities Saldana (2001) provides strategies useful for connecting with those in diverse communities that may also be used internationally: • Enlist local residents of the community • Use a home visit to support information and education
Outreach Strategies to Diverse Communities • Become knowledgeable about indigenous healing resources • Establish a mentor/buddy system with one who is knowledgeable about mainstream approaches and who knows individual families • Consider using some interventions in places that represent community gathering spots (schools, centers, stores, etc. )
What Do We Know About Global Mental Health Needs? • Who is being treated for mental health issues around the world? • How can we estimate the current gaps and prepare for future needs?
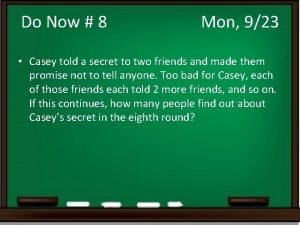
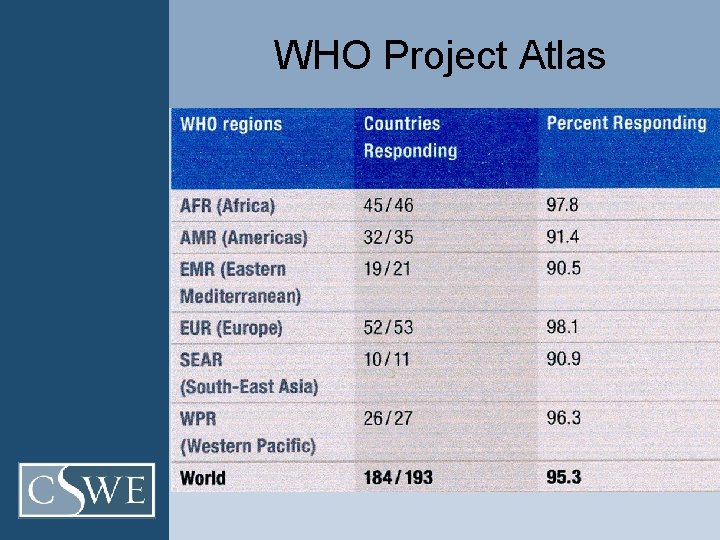
World Health Organization (2011) • WHO launched Project Atlas in 2000 to respond to the large gaps in the collection and dissemination of information about mental health service delivery in countries around the world • “It replaces impressions and opinions with facts and figures” (WHO, 2011, p. 7).
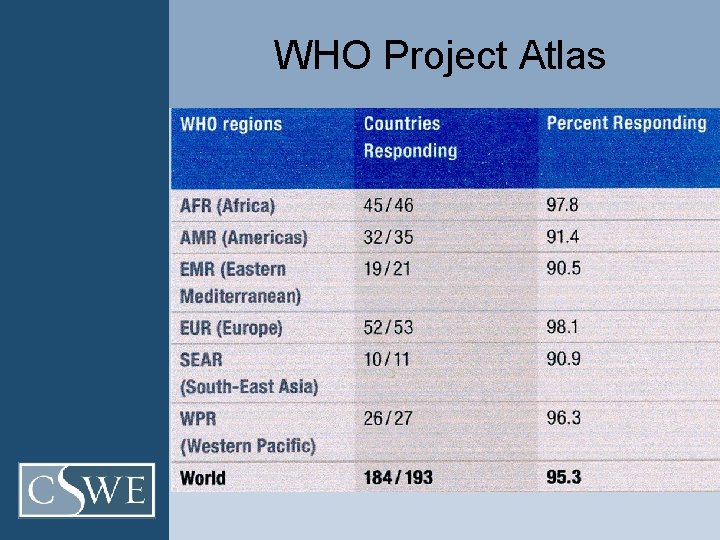
WHO Project Atlas
WHO Mental Health Atlas 2011 FOUR MAIN FINDINGS
1: RESOURCES TO TREAT AND PREVENT MENTAL DISORDERS REMAIN INSUFFICIENT (WHO, 2011) • Globally, spending on mental health is less than two U. S. dollars person, per year and less than 25 cents in lowincome countries. • Almost half of the world's population lives in countries where, on average, there is one psychiatrist or fewer to serve 200, 000 people.
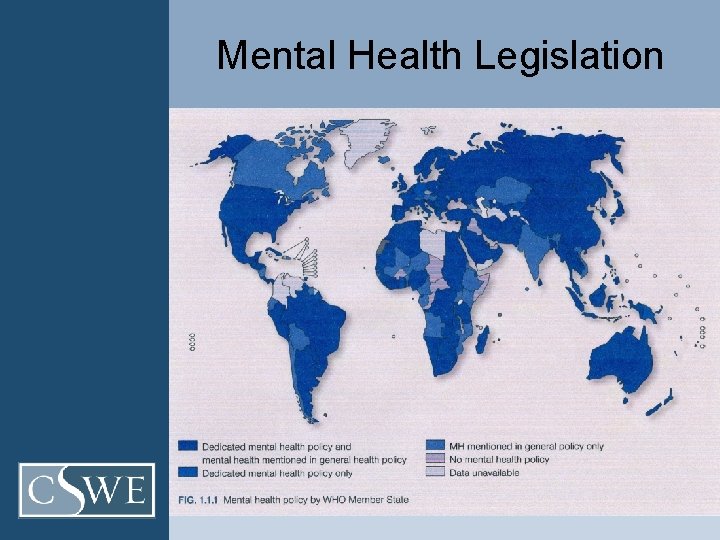
2: RESOURCES FOR MENTAL HEALTH ARE INEQUITABLY DISTRIBUTED (WHO, 2011) n Only 36% of people living in low-income countries are covered by mental health legislation. n In contrast, the corresponding rate for highincome countries is 92%. Dedicated mental health legislation can help to legally reinforce the goals of policies and plans in line with international human rights and practice standards.
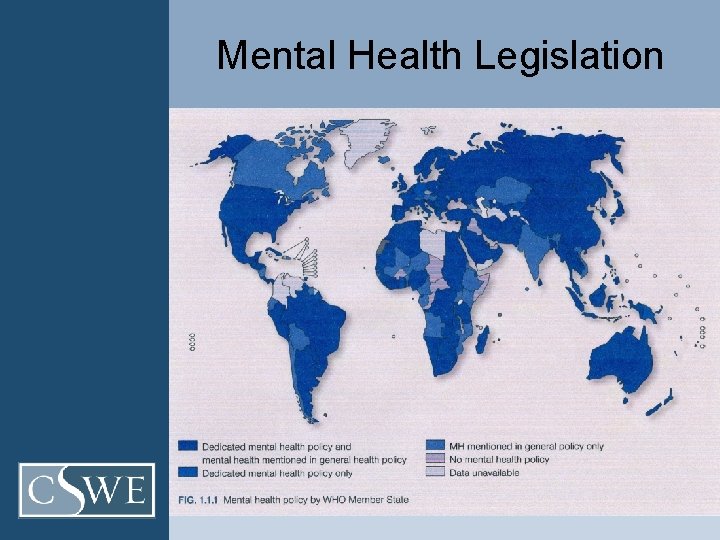
Mental Health Legislation
INEQUITABLE RESOURCE DISTRIBUTION (cont. ) • Outpatient mental health facilities are 58 times more prevalent in highincome compared with low-income countries. • User/consumer organizations are present in 83% of high-income countries in comparison to 49% of low -income countries
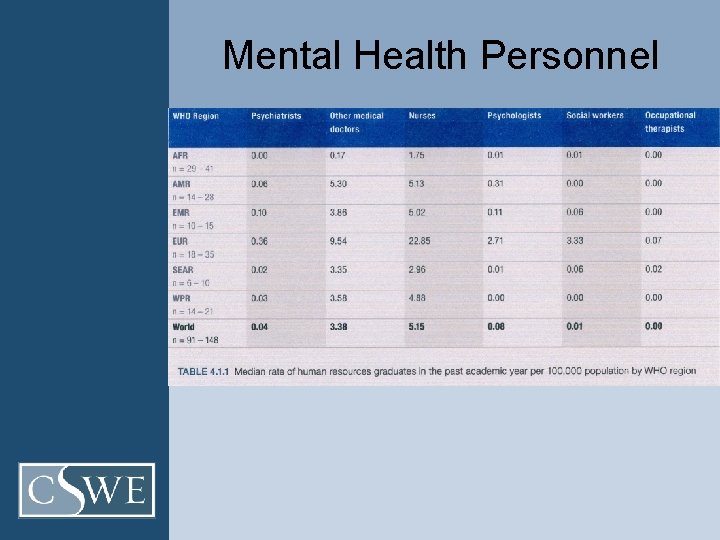
Mental Health Personnel
3. RESOURCES FOR MENTAL HEALTH ARE INEFFICIENTLY USED (WHO, 2011) • Globally, 63% of psychiatric beds are located in mental hospitals, and 67% of mental health spending is directed toward these institutions.
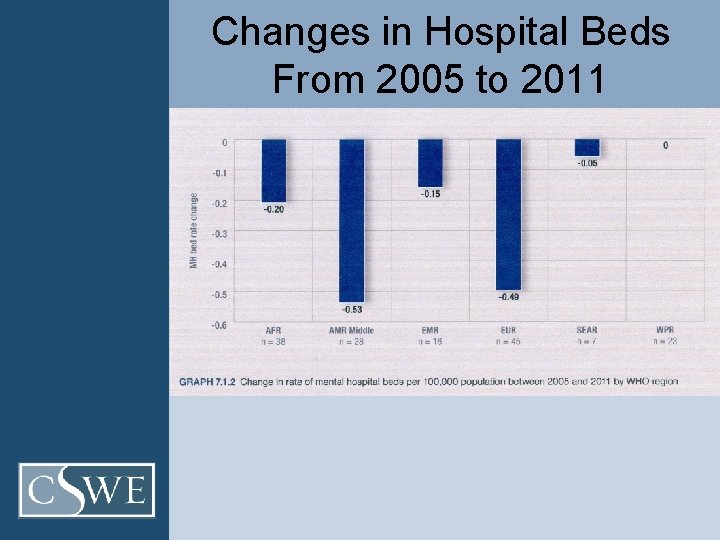
4. INSTITUTIONAL CARE FOR MENTAL DISORDERS MAY BE SLOWLY DECREASING WORLDWIDE (WHO, 2011) Though resources remain concentrated in mental hospitals, a modest decrease in mental hospital beds was found from 2005 to 2011 at the global level and in almost every income and regional group.
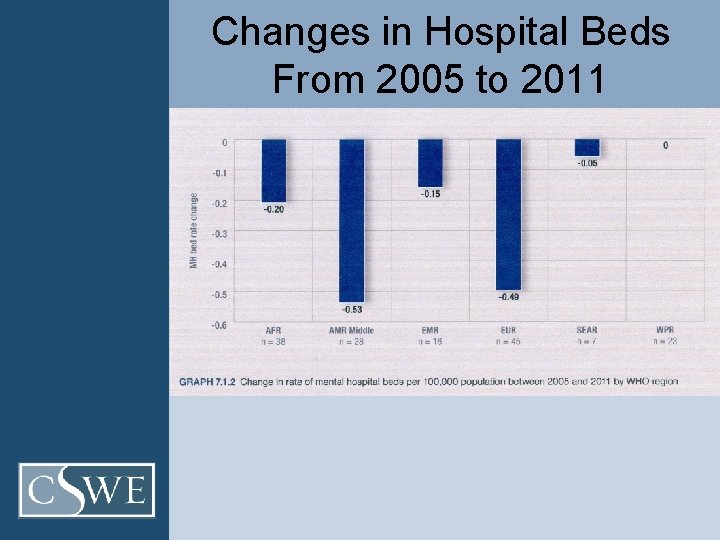
Changes in Hospital Beds From 2005 to 2011
Mental Health Substance abuse, violence, abuse of women and children, HIV/AIDs, depression, and anxiety are more prevalent and difficult to cope with when combined with • • high unemployment low income limited education stressful work conditions gender discrimination social exclusion unhealthy lifestyle human rights violations (WHO, 2007)
Mental Health & Human Rights The Universal Declaration of Human Rights: “All human beings are born free and equal in dignity and rights. ”
But human beings are flawed in their actions toward each other
Mental Health & Human Rights • In many cases, persons with psychosocial or intellectual disabilities suffer. “They are treated without their free and informed consent—a clear and serious violation of their right to health” (Committee on Economic, Social & Cultural Rights, p. 6)
Mental Health & Human Rights • In other cases these disabilities are neither diagnosed nor treated or accommodated for, and their significance is generally overlooked. • “E. g. , in 2001, most middle- and low-income countries devoted less than 1 percent of their health expenditures to mental health. ” • .
Mental Health & Human Rights • “As a result, mental health care, including essential medication such as psychotropic drugs, is inaccessible or unaffordable to many” (Committee on Economic, Social & Cultural Rights, and Office of the High Commissioner for Human Rights, p. 6)
Mental Health & Human Rights Human rights violations for those with mental disorders have been documented around the world.
Examples • Continuous shackling and beatings due to cultural beliefs that mental illness is evil • Children tied to their beds without stimulation or rehabilitation for their condition • Keeping patients lock in “caged beds” for days or weeks or longer (Source: WHO Resource Book on Mental Health, Human Rights and Legislation)

Common Human Rights Violations of People With Mental Disorders • Lack of Access – Some countries may lack adequate services; others may limit access to certain population segments. – 32% of countries have no community care facilities – 30% of countries have no specified budget for mental health; of those that do, 20% spend less than 1% on mental health – Number of psychiatrists ranges from 10 per 100, 000 to 1 per 300, 000 • WHO recommendation: Mental health care should be available at the community level for anyone who needs it
Human Rights Violations (cont. ) • Inappropriate forced admission or treatment in mental health facilities – Informed consent is often not sought – People are forced to remain against their will for weeks, months, years in psychiatric institutions or other mental health facilities WHO recommendation: Informed consent must form the basis of all mental health care; rigorous and ongoing procedural safeguards need to be in place to protect against abuse of involuntary admission and treatment
Human Rights Violations (cont. ) • Violations within psychiatric institutions – People restrained with rusting metal shackles, caged beds, other inhumane treatment – People living in filthy conditions, lacking clothes, clean water, food, heating, proper bedding, or hygiene facilities – People isolated from society in large institutions, far from family and loved ones • WHO recommendation: Countries should set up monitoring bodies to ensure that human rights are being respected in all mental health facilities
Human Rights Violations (cont. ) • Inappropriate detention in prison – In some countries people with mental disorders are in prison due to a lack of mental health services or lack of a diagnosis/treatment for their condition; “prisoners” continue to go unnoticed, undiagnosed, untreated • WHO recommendation: People with mental disorders should be diverted away from criminal justice systems and toward mental health services
Human Rights Violations (cont. ) n Due primarily to stigma, people experience discrimination and violations of basic rights – People often deprived of civil rights (right to vote, marry, have children) – People experience discrimination in all areas of life (employment, education, right to shelter) • WHO recommendation: People with mental disorders have the same human rights as everyone else; due to vulnerability, countries have a responsibility to protect them from discrimination
Gender as an Example (WHO Atlas, 2005) • Communication between health workers and women patients is extremely authoritarian in many countries, making a woman's disclosure of psychological and emotional distress difficult and often stigmatized • Up to 20% of those attending primary health care in developing countries suffer from anxiety and/or depressive disorders.
Gender as an Example (cont. ) • In most centers these patients are not recognized and therefore not treated. When women dare to disclose their problems, many health workers tend to have gender biases that lead them to either overtreat or undertreat women.
Effective Strategies Research shows that three main factors are highly protective against the development of mental problems, especially depression: 1. Psychological support from family, friends, or health providers is powerfully protective. 2. Having sufficient autonomy to exercise some control in response to severe events. 3. Access to some material resources that allow the possibility of making choices in the face of severe events. (WHO Atlas, 2005)

• If there is tremendous unmet need for treatment and widespread violations of human rights…. • If we are fallible in our observations and beliefs, how can we be sure that we are doing with our clients is effective?

Which direction is best for treatment of this vulnerable population?
Evidence-Based Practices
World Health Organization Efforts n WHO has identified low cost, high impact evidence-based interventions to promote mental health, even in poor populations. n WHO is working with governments and provides technical material and advice to implement policies, plans, and programs.
Interventions • Early childhood interventions (e. g. , home visiting for pregnant women, prevention of alcohol abuse by mothers, preschool psychosocial interventions, combined nutritional and psychosocial interventions for disadvantaged populations) • Support to children (e. g. , skill-building programs, child and youth development programs) • Socioeconomic empowerment of women (e. g. , improving access to education, microcredit schemes)
Interventions (cont. ) • Social support for older populations (e. g. , befriending initiatives, community and day centers for older adults) • Programs targeting vulnerable groups including minorities, indigenous people, migrants, and those affected by conflicts and disasters (e. g. , psychosocial interventions after disasters) • Mental health promotion activities in schools (e. g. , supporting ecological changes in schools, child-friendly schools)

Interventions (cont. ) • Mental health interventions at work (e. g. , stress prevention) • Housing policies (e. g. , housing improvement) • Violence prevention programs (e. g. , community policing initiatives) • Community development programs (e. g. , “Communities That Care” initiatives, integrated rural development)
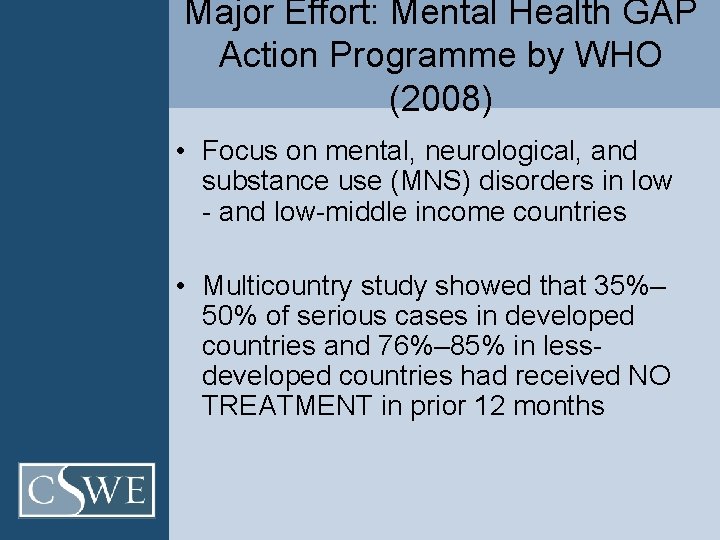
Major Effort: Mental Health GAP Action Programme by WHO (2008) • Focus on mental, neurological, and substance use (MNS) disorders in low - and low-middle income countries • Multicountry study showed that 35%– 50% of serious cases in developed countries and 76%– 85% in lessdeveloped countries had received NO TREATMENT in prior 12 months
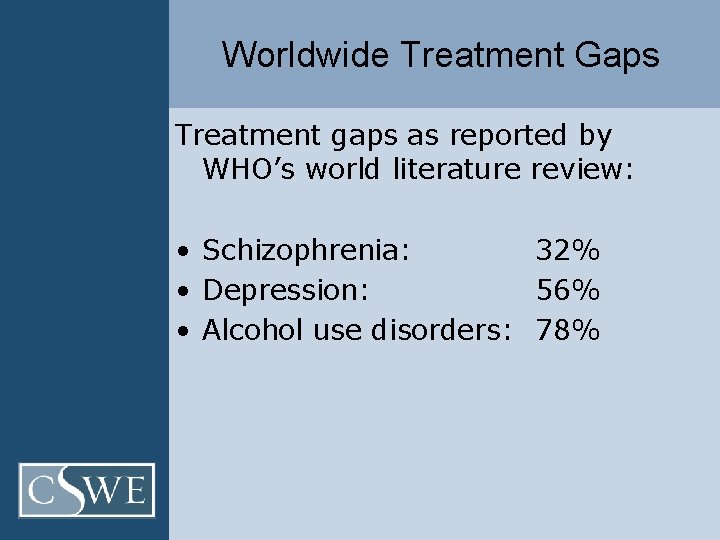
Worldwide Treatment Gaps Treatment gaps as reported by WHO’s world literature review: • Schizophrenia: 32% • Depression: 56% • Alcohol use disorders: 78%
Mental Health Gap Program • To reinforce commitment of governments, international organizations, and other stakeholders to increase financial and human resource allocation to MNS disorders • To achieve higher coverage of key interventions in low- and lower-middle income countries with large proportions of MNS disorders
Gap Program… • Priority conditions were identified – Common in all countries where prevalence has been examined – Substantially interfere with abilities of children to learn and with the abilities of adults to function with families, at work, in society – Disability and premature mortality is substantial – Economic burdens are devastating for poor countries
Priority Conditions • Depression • Schizophrenia and other psychotic disorders • Suicide • Epilepsy • Dementia • Disorders due to alcohol use • Disorders due to illicit drug use • Mental disorders in children
Gap Program… • Intervention packages presented – Prevention/management of each priority condition – Chosen based on evidence of effectiveness, feasibility of scaling up the intervention – Interventions should be delivered in a variety of packages, not freestanding – Will need to be adapted for countries, regions on basis of prevalence and burden, cost, feasibility, and acceptability of the interventions
GAP Program… • Countries chosen for intensified support – Most of global burden of MNS disorders occurs in low- and lower-middle income countries; they also have the highest resource gaps • Three rank-ordered lists created: 1. Total number of lost DALYs (disabilityadjusted life years) was used as a summary measure of population health 2. MNS burden (added if not included in #1) 3. Gross national income was used as an indicator of relative poverty (added if not already on prior lists)
Examples: Intensified Support African Region • Nigeria: Low-income (GNI per capita=640 US in 2006) • Large population • DALYs=1780/100, 000 due to MNS • Mental health professionals=4. 13/100, 000 Americas Region • Colombia: Low middle income (GNI per capita=2740 US in 2006) • Smaller population than Nigeria • DALYs=3054/100, 000 due to MNS • Mental health professionals: 2/100, 000
Depression & Example • Treatment with antidepressant medications (use trained primary health-care professionals) • Psychosocial interventions (e. g. , cognitive-behavioral therapy or problem solving; referrals and supervisory support by specialists) • View video clip: “I had a black dog…his name was depression. ” http: //www. youtube. com/watch? v=Xi. Crni LQGYc
Schizophrenia & Other Psychotic Disorders • Treatment with antipsychotic medications (use trained primary health-care professional within community) • Family or community psychosocial interventions (e. g. , community-based rehabilitation, referral and supervisory support by specialists)
Suicide • Restriction of access to common methods of suicide (multisectoral measures related to public health such as restricted availability of toxic pesticides, secure storage of supplies) • Prevention and treatment of depression and alcohol and drug dependence (see interventions for depression, disorders due to alcohol and illicit drug use)
Example From WHO • View video clip: Hidden Pictures: A Personal Journey Into Global Mental Health http: //www. youtube. com/watch? v=dv_ex aj 2 ofg&feature=youtu. be
Who Is Responsible for Treatment?
According to WHO GAP Plan. . . • Scaling up for mental health care is a social, political, and institutional process • Joint responsibility lies with – – – Governments Health professionals for MNS disorders Civil society Communities Families Support from the international community
Selected Personal Observations • Americas • Mexico: Effects of growth of tourism in Cabo on quality of life, environment • South East Asia • Thailand: Effects post-tsunami; grassroots organizations developing to rebuild area • Mental health treatment is difficult in rural areas • Africa • Zimbabwe: Effects of immigration between countries in Africa on crime, family structure, mental health
Selected Personal Observations • Western Pacific – Caribbean: In recent past, only the UN Declaration of Human Rights served as basis for social workers removing children from unfit parents (no specific legal support); now have Child Abuse Law • Europe – Immigration issues interacting with mental health, such as French laws permitting asylum seekers to enter country, many from Northern Africa; but 95% are assessed and deemed ineligible for services and remain in country – Drug treatment in Hungary: strong alcohol/driving laws, but treatment is focused on drug use (up to 1 year residential paid for largely by government)
Social Workers WHO Definition: – Social worker: A professional having completed a formal training in social work at a recognized, university-level school for a diploma or degree in social work. (WHO-AIMS, 2005, p. 11).
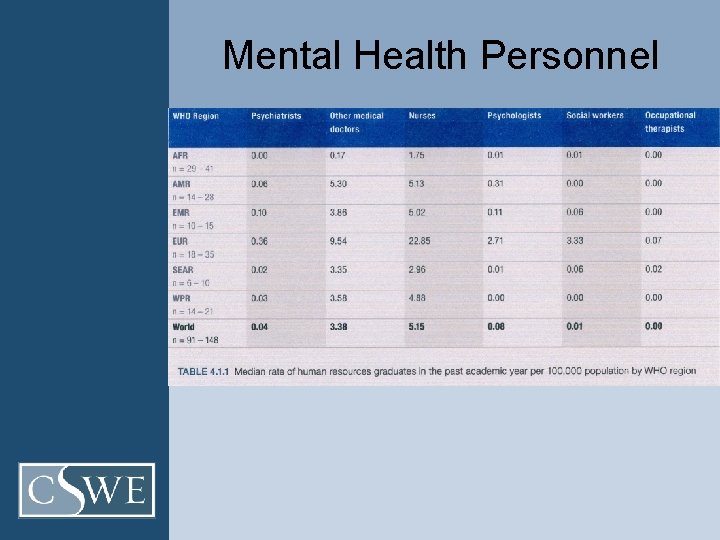
Availability of Social Workers • Globally, WHO reported that in 2011 there were more nurses (5. 15/100, 000) than any other mental health professional group • A much smaller pool of psychologists, psychiatrists, social workers, and occupational therapists graduated in the past year • (See complete details by region in charts in Human Resource Chapter, WHO, 2011)
Provide Hope
Focus on Strengths, Not Problems
Small Group Discussion • Form small groups to discuss the class exercise provided • Focus on one of the top three priority conditions: depression, schizophrenia, suicide • Explore changes from 2005– 2011 (chapter in Atlas, 2011) • Consider how evidence-based practice may be used most effectively and the challenges presented, based on the evidence from the Atlas.
Resources for Small Group Discussion • Amnesty International: Mental Health http: //www. amnesty. ie/mentalhealth-0 • British National Health Service (NHS) http: //www. nhs. uk/NHSEngland/About. NHS services/mentalhealthservices/Pages/Availabl services. aspx • Human Rights Watch: Mental Health http: //www. hrw. org/taxonomy/term/704/all • MH GAP Report: Intervention Guide. http: //whqlibdoc. who. int/publications/2010/9789241548069_en g. pdf • You. Tube http: //www. youtube. com/watch? v=dv_exaj 2 ofg&feature=youtu. be http: //www. who. int/features/mental_health/ sustaining_mental_health/en/index. html
Resources for Small Group Discussion • WHO-AIMS (Assessment Instrument for Mental Health Systems (Version 2. 2) (2005). Geneva, Switzerland. • World Health Organization (WHO) (2005). World health statistics. Geneva, Switzerland http: //www. who. int/whr/2005/en/ • World Health Organization (WHO) (2007). World health statistics. Geneva, Switzerland http: //www. who. int/whr/2007/en/ • WHO (2011). Mental health country profiles. http: //www. who. int/mental_health/evidence/ atlas/profiles/en/index. html • World Bank MDGs http: //www. worldbank. org/mdgs/
Selected References Davis, K. (1997). Race, health status, and managed care, In L. Epstein & F. Brisbane (eds. ), Cultural competence series. Rockville, MD: Center for Substance Abuse Prevention. Institute of Medicine. (2001). To err is human: Building a safer health system. Available from http: //www. iom. edu/Reports/1999/to-err-is-human-building-asafer-health-system. aspx Sackett, D. L. , Rosenberg, , W. M. , Gray, J. A. , Haynes, R. B. , & Richardson, W. S. (1996). Evidence-based medicine: What it is and what it isn’t. British Medical Journal, 312, 71– 72. Sackett, D. L. , Straus, S. E. , Richardson, W. S. , Rosenberg, W. M. , & Haynes, R. B. (2000). Evidence-based medicine: How to practice and teach evidence-based medicine (2 nd ed. ). London, UK: Churchill Livingston. Saldana, D. (2001). Cultural competency: A practical guide for mental health service providers. Austin, TX: Hogg Foundation for Mental Health, University of Texas Austin.
Selected References • United Nations Committee on Economic, Social & Cultural Rights, Office of the High Commissioner for Human Rights: http: //www. ohchr. org/EN/HRBodies/CESCR/Pages/CESCRIndex. aspx • World Health Organization (WHO). (2005). WHO atlas of 2005. Retrieved from http: //www. who. int/mental_health/evidence/Atlas_training_final. pdf • World Health Organization (WHO). (2005). WHO resource book on mental health, human rights and legislation. Retrieved from http: //www. who. int/mental_health/policy/who_rb_mnh_hr_leg_FINAL_1 1_07_05. pdf • World Health Organization (WHO). (2008). Mental health gap project. Retrieved from http: //whqlibdoc. who. int/publications/2010/9789241548069_eng. pdf • World Health Organization (WHO). (2011). Mental health atlas of 2011. Geneva, Switzerland: Author.
Hyperlinks for Video Clips • Hidden Pictures: A Personal Journey Into Global Mental Health http: //www. youtube. com/watch? v=dv_exaj 2 o fg&feature=youtu. be • I Had a Black Dog…His Name Was Depression http: //www. youtube. com/watch? v=Xi. Crni. LQG Yc

Slides developed by Sally Mathiesen, Ph. D, LCSW Professor SDSU School of Social Work Smathiesen@sbcglobal. net
 Chapter 20 mental health and mental illness
Chapter 20 mental health and mental illness Mental health jeopardy questions
Mental health jeopardy questions Communication cycle health and social care
Communication cycle health and social care Handling information in care settings
Handling information in care settings Sally wants to select an entire paragraph
Sally wants to select an entire paragraph Ttm taiwan
Ttm taiwan Annilihated
Annilihated Cibtac level 4
Cibtac level 4 Sally and her family
Sally and her family Sally tennant orthopaedic
Sally tennant orthopaedic Lily collins rosie dunne
Lily collins rosie dunne Sally nitm
Sally nitm Business agility metrics
Business agility metrics Pemdas meaning
Pemdas meaning Noun as direct object
Noun as direct object Please excuse my dear aunt sally
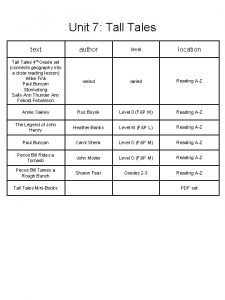
Please excuse my dear aunt sally Tall tale story
Tall tale story Where did they go last weekend read and say
Where did they go last weekend read and say Catcher in the rye chapter 13 analysis
Catcher in the rye chapter 13 analysis Sally reardon
Sally reardon Sally guzman edmonds school district
Sally guzman edmonds school district What sally said theme
What sally said theme Sally neuberger
Sally neuberger Sally d'angelo torrent
Sally d'angelo torrent Alliterati
Alliterati Sally manke
Sally manke Sally haslanger mit
Sally haslanger mit Sally elatta
Sally elatta Sally dickerson
Sally dickerson Eumetazoa phylum
Eumetazoa phylum Example of allusion
Example of allusion Umich ap exam credit
Umich ap exam credit Sally tompkins
Sally tompkins Sally lannin
Sally lannin Sally likes
Sally likes Grab some paper
Grab some paper Sally trembath psychologist
Sally trembath psychologist Sally
Sally Sally is the girl with eyes like egypt
Sally is the girl with eyes like egypt Sally puzey
Sally puzey Sally left the party to take cathy home
Sally left the party to take cathy home Sally dickinson fao
Sally dickinson fao Sally–anne test
Sally–anne test Sally–anne test
Sally–anne test Tongue twisters in english betty bought some butter
Tongue twisters in english betty bought some butter Cvs vs amniocentesis venn diagram
Cvs vs amniocentesis venn diagram Sally hayes catcher in the rye
Sally hayes catcher in the rye Sally hanley
Sally hanley Sally (run, runs) to the park every day.
Sally (run, runs) to the park every day. Sally seidel
Sally seidel Dr sally brown
Dr sally brown Ashley is comparing three investment accounts
Ashley is comparing three investment accounts Sally otto
Sally otto Michelle monestime
Michelle monestime Listen carefully. i'm going to give you
Listen carefully. i'm going to give you Sally barakat
Sally barakat Sally floyd
Sally floyd Sally schmidt
Sally schmidt Sally jordan model
Sally jordan model Sally simpson umd
Sally simpson umd Apicatt
Apicatt Lenawee county cmh
Lenawee county cmh Van buren county cmh
Van buren county cmh Chapter 3 achieving mental and emotional health answer key
Chapter 3 achieving mental and emotional health answer key Together for mental health
Together for mental health Mental health act 2007 made simple
Mental health act 2007 made simple Wellbeing triangle
Wellbeing triangle Titles for mental health presentations
Titles for mental health presentations Health committee introduction
Health committee introduction Kings fund
Kings fund Define mental health nursing
Define mental health nursing Introduction of nursing process
Introduction of nursing process Mental health programme
Mental health programme Objectives of community mental health
Objectives of community mental health Benefits of phr
Benefits of phr How to make a mind map in photoshop
How to make a mind map in photoshop Middle tennessee mental health institute
Middle tennessee mental health institute Toolbox talk mental health
Toolbox talk mental health Golden thread clinical documentation
Golden thread clinical documentation Mental health equity
Mental health equity Mental health ordinance
Mental health ordinance Schizophrenia def
Schizophrenia def Objective about mental health
Objective about mental health Mental health and older adults
Mental health and older adults Mental health problems examples
Mental health problems examples