Medical Necessity QuandaryCDI to the Rescue Glenn Krauss


















- Slides: 48

Medical Necessity Quandary-CDI to the Rescue Glenn Krauss, BBA, RHIA, CCS-P, CPUR, CCDS, C-CDI, C-DAM CEO & Founder, Core-CDI

How is medical necessity defined from a clinician’s perspective? Objectives What are the key elements of documentation that drive establishment of medical necessity? Why medical necessity is not just a requirement for facility payment from payers 2

What Is In it for Me (Physician) WIFFM? Objectives Why does achievement of medical necessity require a non -siloed team approach by healthcare stakeholders? How to truly engage physicians as willing participants in learning about, becoming more proficient in and employing best practice standards and principles of documentation clearly representative of physician clinical judgment, medical necessity and establishment of medical necessity? 3
Challenges of Medical Necessity • Medical necessity • Moving target • Subject to interpretation • Payers control the purse strings • Arbitrarily applied • Reimbursement Driven • Varied standards • Varied screening criteria • Clinical Documentation dependent 4

5
Medical Necessity. Administrative • Medical Necessity • 1862 (a)(1)(a) Title XVIII SSA 42 CFR • Notwithstanding any other provision of this title, no payment may be made under part A or part B for any expenses incurred for items or services— (A) which, except for items and services described in a succeeding subparagraph or additional preventive services (as described in section 1395 x(ddd)(1) of this title), are not reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, 6
Medical Necessity. Administrative • Medical Necessity Definitions • Medical Necessity definitions are different for physicians than for other providers, and for seniors than for other adults. • Medical Necessity for Physicians • Medical Necessity for Other Providers • Healthcare for Seniors Definition of Medical Necessity for Physicians • Healthcare for Seniors Definition of Medical Necessity for other Health Care Providers 7
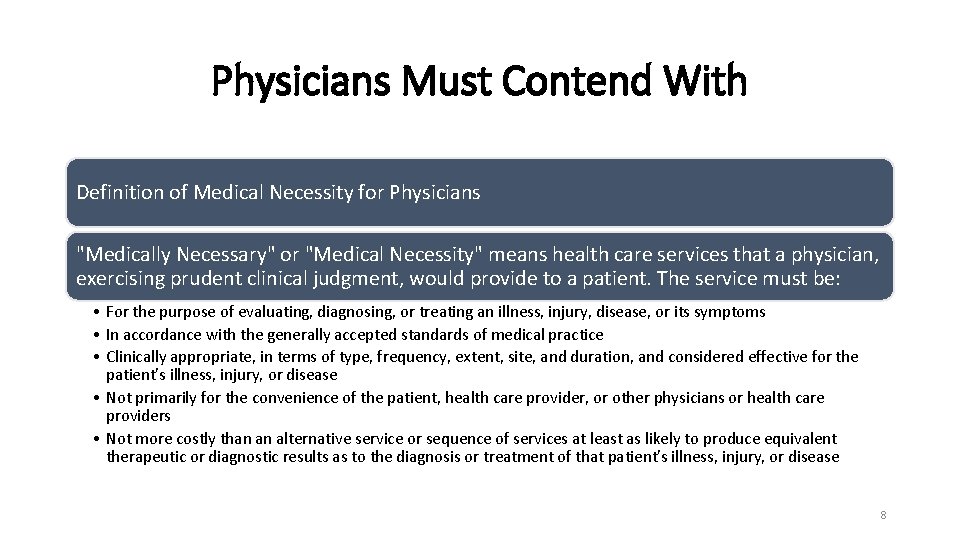
Physicians Must Contend With Definition of Medical Necessity for Physicians "Medically Necessary" or "Medical Necessity" means health care services that a physician, exercising prudent clinical judgment, would provide to a patient. The service must be: • For the purpose of evaluating, diagnosing, or treating an illness, injury, disease, or its symptoms • In accordance with the generally accepted standards of medical practice • Clinically appropriate, in terms of type, frequency, extent, site, and duration, and considered effective for the patient's illness, injury, or disease • Not primarily for the convenience of the patient, health care provider, or other physicians or health care providers • Not more costly than an alternative service or sequence of services at least as likely to produce equivalent therapeutic or diagnostic results as to the diagnosis or treatment of that patient's illness, injury, or disease 8
Standards of Medical Practice • For these purposes, "generally accepted standards of medical practice" means: • Standards that are based on credible scientific evidence published in peer-reviewed, medical literature generally recognized by the relevant medical community • Physician Specialty Society recommendations • The views of physicians practicing in the relevant clinical area • Any other relevant factors 9

10 The Constant
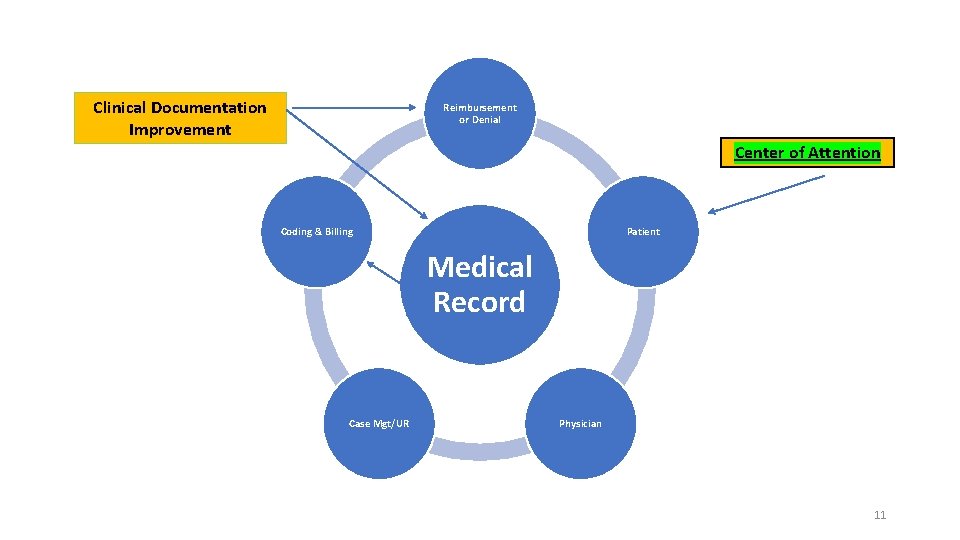
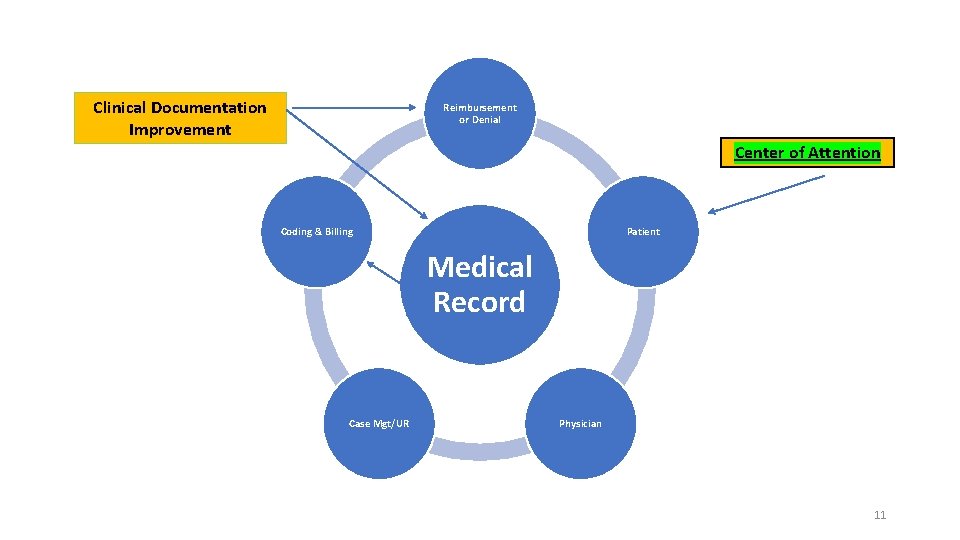
Clinical Documentation Improvement Reimbursement or Denial Center of Attention Coding & Billing Patient Medical Record Case Mgt/UR Physician 11

12
13 Medical Necessity. Proper Context • Medical Necessity • Communication of Patient Care vs. Clinical Documentation • Clinical documentation = Diagnoses • Patient Story Diagnoses • Patient story • Clinical information • Clinical facts • Context
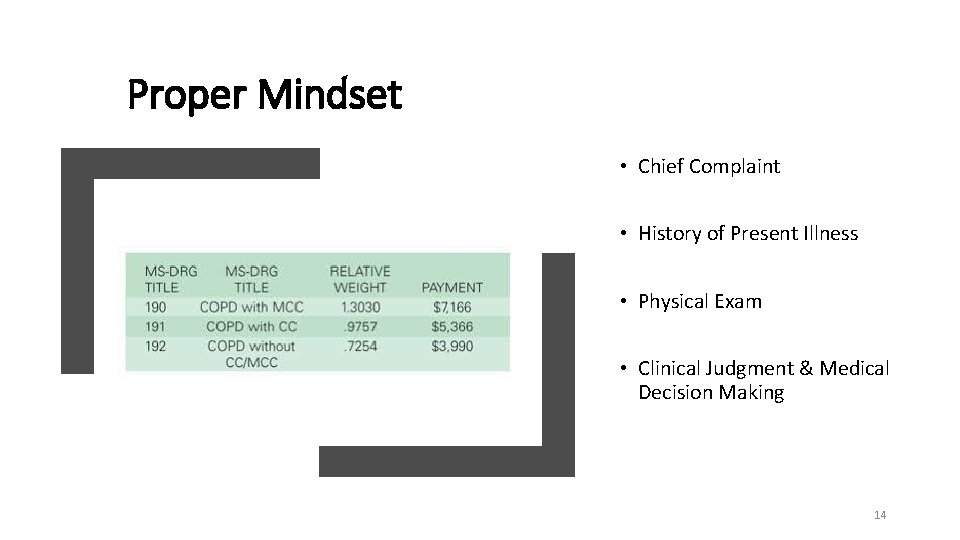
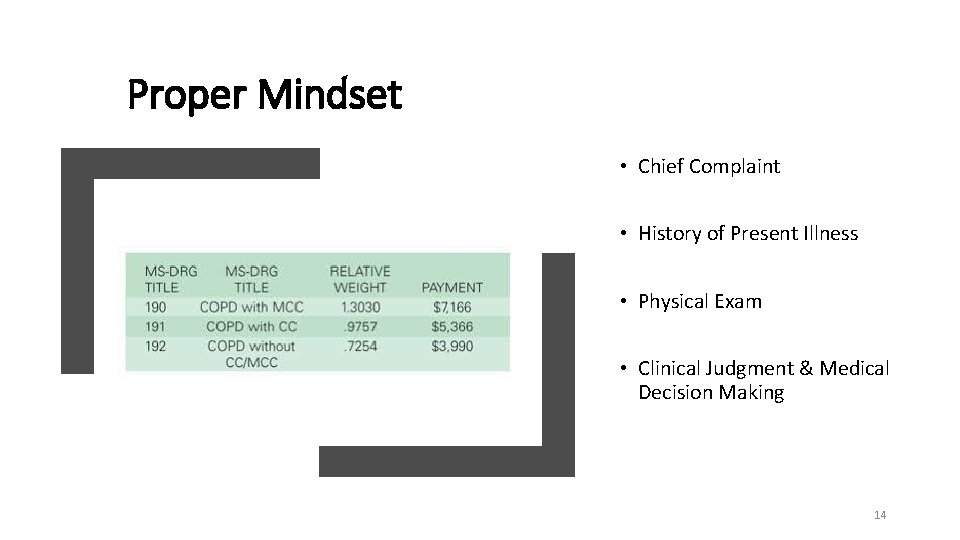
Proper Mindset • Chief Complaint • History of Present Illness • Physical Exam • Clinical Judgment & Medical Decision Making 14

15
The Plain Truth • Fifty-percent of medical necessity denials are avoidable • Better more effective communication • • Emergency Department History & Physicals Progress Notes Discharge Summary • CDI Plays a vital role 16
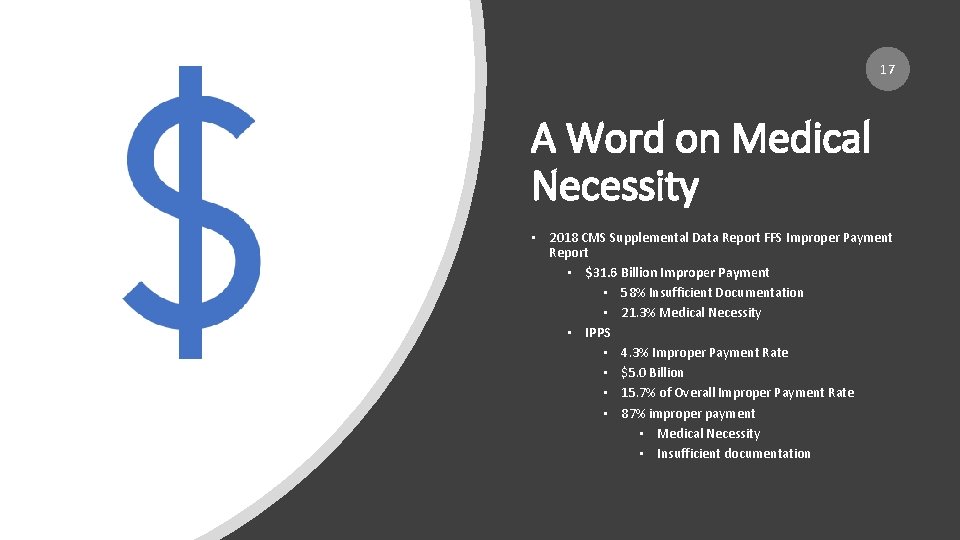
17 A Word on Medical Necessity • 2018 CMS Supplemental Data Report FFS Improper Payment Report • $31. 6 Billion Improper Payment • 58% Insufficient Documentation • 21. 3% Medical Necessity • IPPS • 4. 3% Improper Payment Rate • $5. 0 Billion • 15. 7% of Overall Improper Payment Rate • 87% improper payment • Medical Necessity • Insufficient documentation
Improper Payment Categories Insufficient Documentation • Claims are placed into this category when the medical documentation submitted is inadequate to support payment for the services billed. In other words, the CERT contractor reviewers could not conclude that the billed services were actually provided, were provided at the level billed, and/or were medically necessary. Claims are also placed into this category when a specific documentation element that is required as a condition of payment is missing, such as a physician signature on an order, or a form that is required to be completed in its entirety. 18

Improper Payment Categories MEDICAL NECESSITY CLAIMS ARE PLACED INTO THIS CATEGORY WHEN THE CERT CONTRACTOR REVIEWERS RECEIVE ADEQUATE DOCUMENTATION FROM THE MEDICAL RECORDS SUBMITTED TO MAKE AN INFORMED DECISION THAT THE SERVICES BILLED WERE NOT MEDICALLY NECESSARY BASED UPON MEDICARE COVERAGE AND PAYMENT POLICIES. 19
Practically Speaking • Documentation of Medical Necessity • Number, acuity, severity and duration of problems addressed by physician • Extent to which comorbidities impact complexity in management of acute clinical conditions • Context of previous management of same conditions • Number of body areas and organ systems the physician must contend within clinical management • Challenges and complexity of arriving at a diagnosis (es) and development of a reasonable management action plan 20

Do Your Part • Medical necessity cannot be quantified using a points system. Determining the medically necessary LOS involves many factors and is not the same from patient to patient and day to day. Medical necessity is determined through a culmination of vital factors, including, but not limited to: • Clinical judgment • Standards of practice • Why the patient needs to be seen (chief complaint), • Any acute exacerbations/onsets of medical conditions or injuries, • The stability/acuity of the patient, • Multiple medical co-morbidities, • And the management of the patient for that specific DOS 21
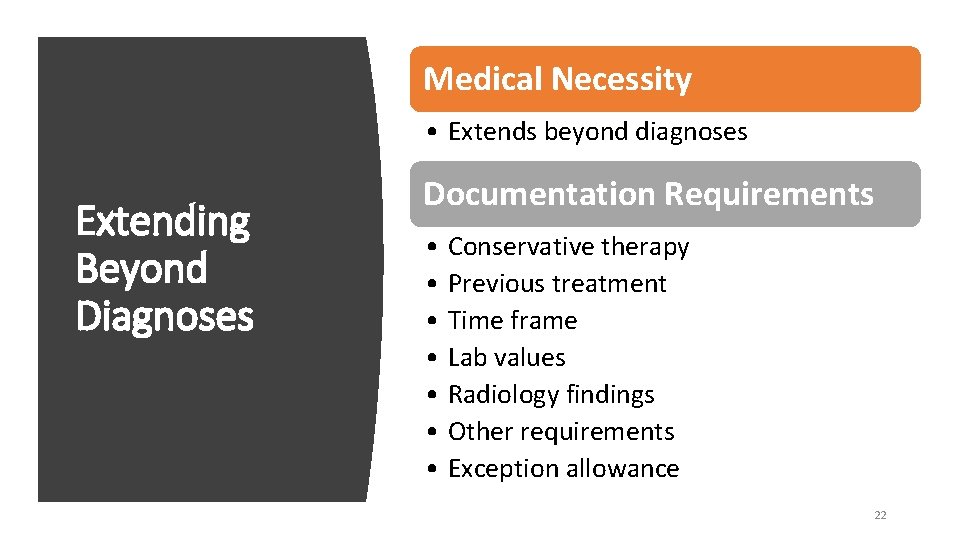
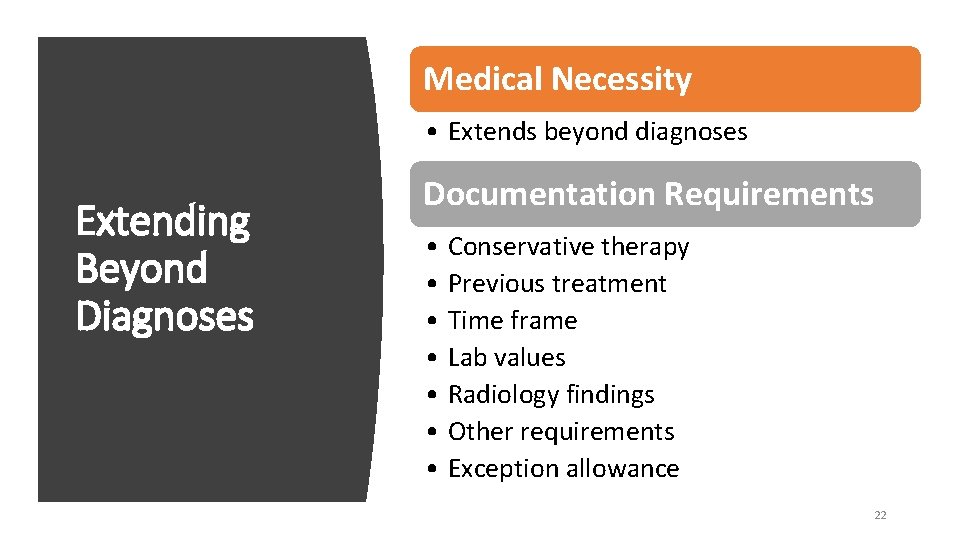
Medical Necessity • Extends beyond diagnoses Extending Beyond Diagnoses Documentation Requirements • Conservative therapy • Previous treatment • Time frame • Lab values • Radiology findings • Other requirements • Exception allowance 22
In a Nutshell It is the accurate documentation of the services rendered for the patient’s needs at the time that determines the level of E & M code to be selected, not the volume of documentation. This is why the thorough documentation of the patient’s condition, the services rendered, and the reason(s) for those services is so important. Time is also not the determining factor in billing of this code. Medically necessary E/M visits for the diagnosis or treatment of an illness or injury or to improve the functioning of a malformed body member are payable under the fee physician schedule under Medicare Part B. Medical necessity of E/M services depends upon the condition of the patient, the services required to treat that patient at that time, and are generally expressed in two ways: frequency of services and intensity of services (Current Procedural Terminology (CPT) level. 23
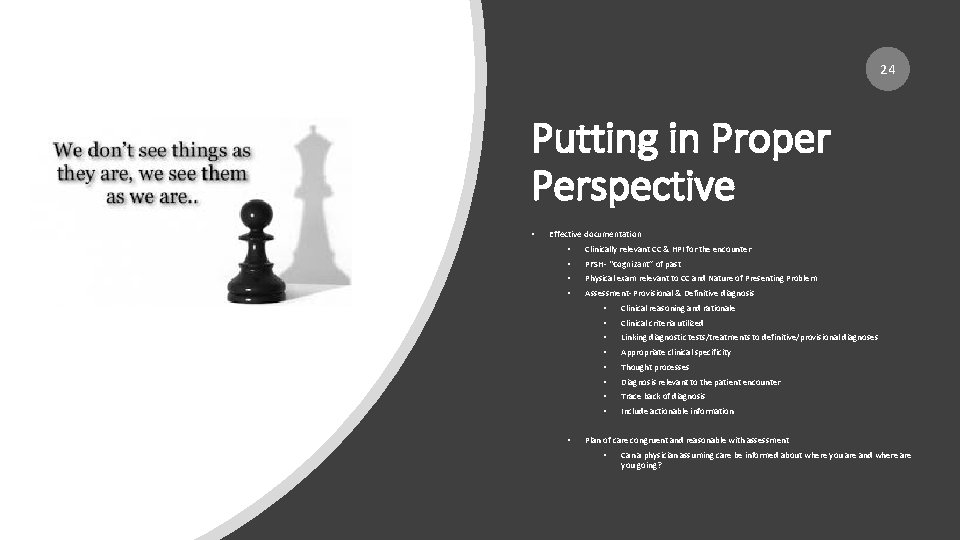
24 Putting in Proper Perspective • Effective documentation • Clinically relevant CC & HPI for the encounter • PFSH- “Cognizant” of past • Physical exam relevant to CC and Nature of Presenting Problem • Assessment- Provisional & Definitive diagnosis • • Clinical reasoning and rationale • Clinical criteria utilized • Linking diagnostic tests/treatments to definitive/provisional diagnoses • Appropriate clinical specificity • Thought processes • Diagnosis relevant to the patient encounter • Trace back of diagnosis • Include actionable information Plan of care congruent and reasonable with assessment • Can a physician assuming care be informed about where you are and where are you going?
• Medical Necessity is Not Only A Hospital Thing! • Medical necessity of a service is the overarching criterion for payment in addition to the individual requirements of a CPT code. • It would not be medically necessary or appropriate to bill a higher level of evaluation and management service when a lower level of service is warranted. • The volume of documentation should not be the primary influence upon which a specific level of service is billed. • Documentation should support the level of service reported. • The service should be documented during, or as soon as practicable after it is provided in order to maintain an accurate medical record. Message to Physicians • Chapter 12 , Section 30. 6. 1 A Clams Processing Manual 25

26

Developing Your Road Map BREAK DOWN SILOS ESTABLISH PARTNERSHIPS CHANGE MINDSETFACILITATORS COMMUNICATION VS. “DIAGNOSIS GATHERER” FORGE RELATIONSHIP CREATE A VISION OF CDI- “TEAM-APPROACH” 27
Speaking of Mission • Clinical Documentation Improvement is defined by the completeness, consistency, organization and accuracy of the medical record, reflecting the physician's clinical judgment and medical decision making. • CDI supports positive outcomes in patient care, quality, cost, resource consumption, fee for value, net patient revenue, transformation from denials and appeals to denials avoidance and overall revenue cycle processes. • CDI will consistently strive to insure accurate and complete capture of all clinically relevant compliant diagnoses to the extent possible accompanied by accurate capture and reflection of the true patient story with sufficient detail and clarity in support of medical necessity. 28
Mission Possible • This new paradigm requires a wholesale shift in the mission, goals, and objectives of any CDI program. • Goals, objectives, and mission of CDI should be to improve actual processes of clinical documentation, striving to achieve meaningful and lasting changes in physician behavioral patterns of clinical documentation that optimally reflect communication of patient care, regardless of stakeholder including third-party payers 29

Physician CDI Professional Patient Case Management 30

First Things First The Chicken The Egg • Emergency Department • What is wrong with the patient, how did it manifest, what did it look like? • Admission • Patient Story • Treat & Street vs. Hospitalization • History & Physical • Progress Notes • Consultant Notes • Discharge Summary • Physical Exam • Diagnostic Work-Up • Clinical Impression • Plan of Care-Treatment 31

https: //www. youtube. com/watch? v=Cz. Juf. BRb. Z 1 c 32

Right Care Right Time Right Reason Facilitators in Communication Right Venue Right Clinical Judgment, Medical Decision-Making, Thought Processes Right Documentation Right Plan of Care 33
Focusing on the Right Thing • Eight “W’s” of Documentation • Where has the patient been? • Where is the patient now? • What is the physician thinking? • Why is the thinking? • Where is the physician going? • Why is the physician going? • What is he going to do when he gets there? • What alternate plan for further workup 34
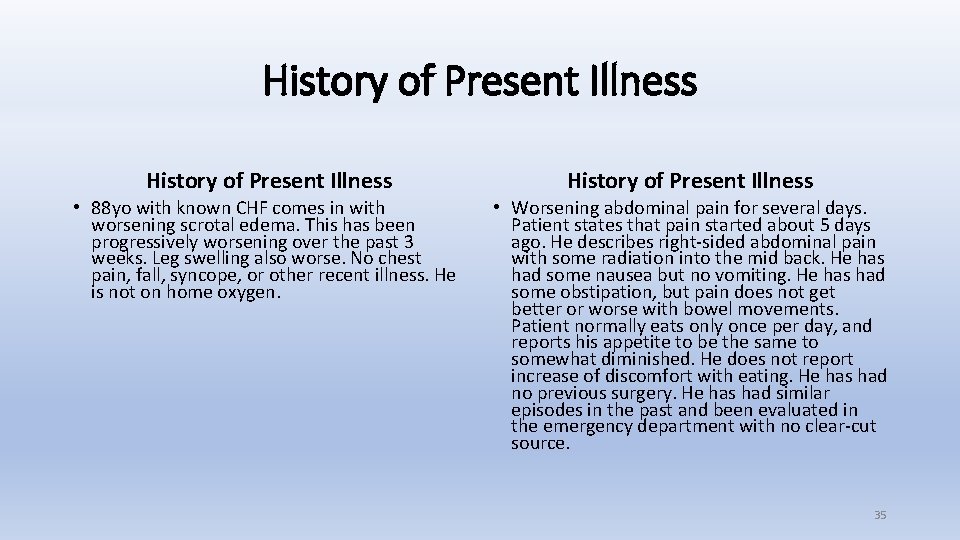
History of Present Illness • 88 yo with known CHF comes in with worsening scrotal edema. This has been progressively worsening over the past 3 weeks. Leg swelling also worse. No chest pain, fall, syncope, or other recent illness. He is not on home oxygen. • Worsening abdominal pain for several days. Patient states that pain started about 5 days ago. He describes right-sided abdominal pain with some radiation into the mid back. He has had some nausea but no vomiting. He has had some obstipation, but pain does not get better or worse with bowel movements. Patient normally eats only once per day, and reports his appetite to be the same to somewhat diminished. He does not report increase of discomfort with eating. He has had no previous surgery. He has had similar episodes in the past and been evaluated in the emergency department with no clear-cut source. 35

36
Nature of Present Problem • A presenting problem is a disease, condition, illness, injury, symptom, sign, finding, complaint, or other reason for encounter, with or without a diagnosis being established at the time of the encounter. • Five types of presenting problem • Minimal • Self-limited or minor • Low severity • Moderate severity • High severity 37
What’s The Problem? ? ? • Chief Complaint • A CC is a concise statement that describes the symptom, problem, condition, diagnosis, or reason for the patient encounter. • The CC is usually stated in the patient’s own words. • For example, patient complains of upset stomach, aching joints, and fatigue. • The medical record should clearly reflect the CC. Patients Own Words 38
History of Present Illness • History of Present Illness (HPI) • HPI is a chronological description of the development of the patient’s present illness from the first sign and/or symptom or from the previous encounter to the present. HPI elements are: • Location (example: left leg) • Quality (example: aching, burning, radiating pain) • Severity (example: 10 on a scale of 1 to 10) • Duration (example: started 3 days ago) • Timing (example: constant or comes and goes) • Context (example: lifted large object at work) • Modifying factors (example: better when heat is applied) • Associated signs and symptoms (example: numbness in toes) 39
40
HPI- Your Best Friend • HPI • Prism through medical necessity established • Establishes medical necessity for physician work performed • Establishes medical necessity for physician ordered workup, treatment • Aids in the development of definitive and/or provisional diagnosis • Solidifies & supports clinical judgment and medical decision making • Think 2021 - Wholesale E & M changes 41
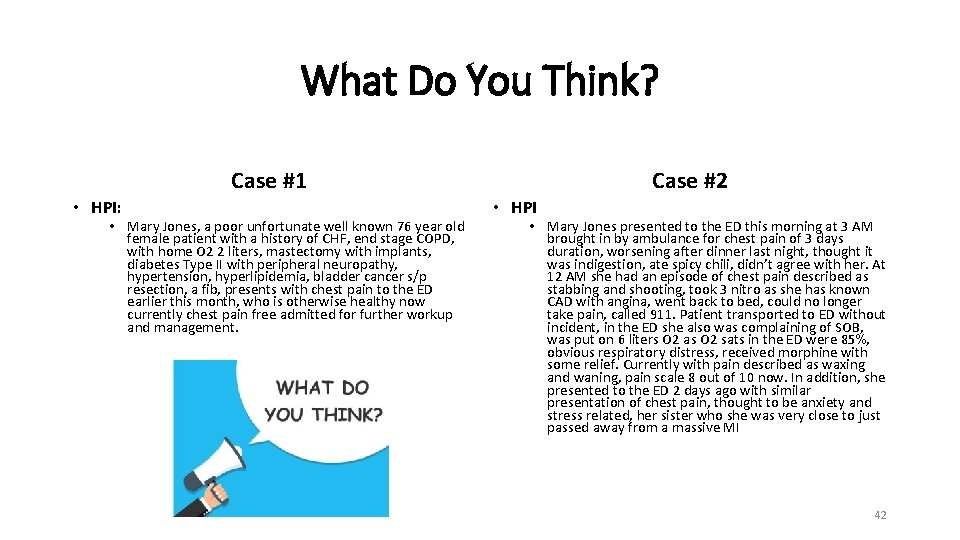
What Do You Think? Case #1 • HPI: • Mary Jones, a poor unfortunate well known 76 year old female patient with a history of CHF, end stage COPD, with home O 2 2 liters, mastectomy with implants, diabetes Type II with peripheral neuropathy, hypertension, hyperlipidemia, bladder cancer s/p resection, a fib, presents with chest pain to the ED earlier this month, who is otherwise healthy now currently chest pain free admitted for further workup and management. Case #2 • HPI • Mary Jones presented to the ED this morning at 3 AM brought in by ambulance for chest pain of 3 days duration, worsening after dinner last night, thought it was indigestion, ate spicy chili, didn’t agree with her. At 12 AM she had an episode of chest pain described as stabbing and shooting, took 3 nitro as she has known CAD with angina, went back to bed, could no longer take pain, called 911. Patient transported to ED without incident, in the ED she also was complaining of SOB, was put on 6 liters O 2 as O 2 sats in the ED were 85%, obvious respiratory distress, received morphine with some relief. Currently with pain described as waxing and waning, pain scale 8 out of 10 now. In addition, she presented to the ED 2 days ago with similar presentation of chest pain, thought to be anxiety and stress related, her sister who she was very close to just passed away from a massive MI 42

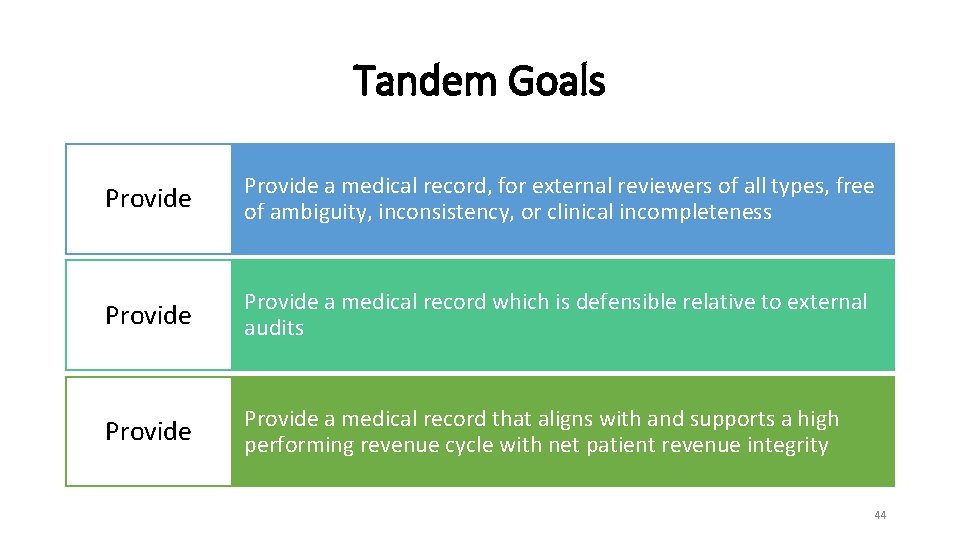
Working in Tandem. Goals • Tandem Goals • Achieve the highest order of specific, accurate, detailed medical documentation whereby to ensure the most precise final coding, so that the institution receives the optimal and appropriate reimbursement to which it is entitled based upon care provided and resources consumed • Produce a medical record, which is the most efficacious communication tool for all healthcare providers rendering care in each case • Provide accurate, specific, detailed medical documentation whereby to effect enhanced patient safety, as well as efficiencyeffectiveness of care efforts 43
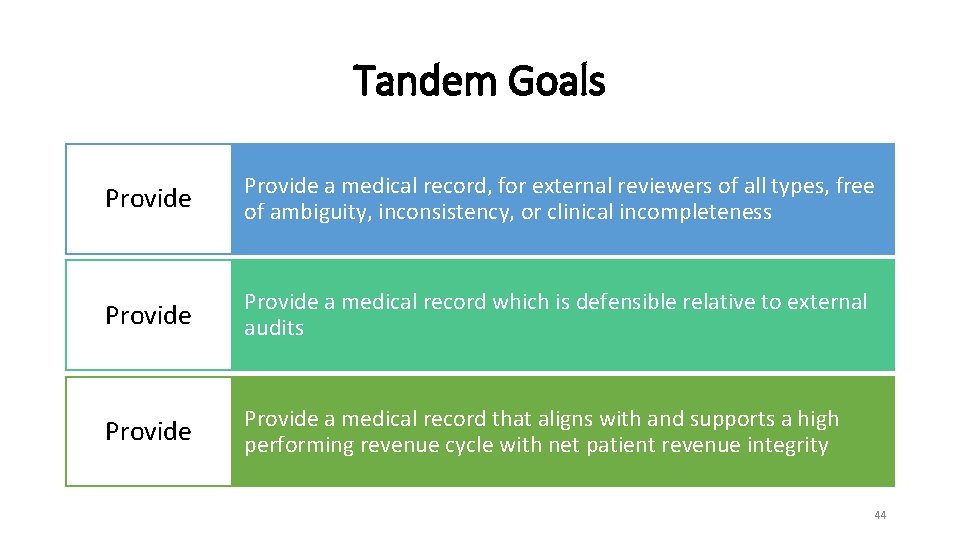
Tandem Goals Provide a medical record, for external reviewers of all types, free of ambiguity, inconsistency, or clinical incompleteness Provide a medical record which is defensible relative to external audits Provide a medical record that aligns with and supports a high performing revenue cycle with net patient revenue integrity 44
Take Home Points • Medical record: • “Communication Tool” vs. “Reimbursement Tool” • The primary purpose of clinical documentation should be to support patient care and improve clinical outcomes through enhanced communication • The clinical record should include the patient’s story in as much detail as is required to retell the story. • The medical record was first used by physicians to record their findings and actions and as a vehicle to communicate with other physicians who might care for the patient in the future • Clinical Documentation in the 21 st Century: Executive Summary of a Policy Position Paper ACP, January 2015 45
Challenge the status quo Expand your skill sets, core competencies and knowledgebase Take Home Points Medical necessity establishment is everyone’s responsibility Learn from mistakes and oversights Get your seat at the denials table 46

47
Contact Information • Glenn Krauss, BBA, RHIA, CCS-P, CPUR, CCDS, CCDI, C-DAM • CEO & Founder, Core-CDI • Co-Founder, Top Gun Audit School • Glenn. Krauss@Core-CDI. com • (603) 303 -3337 48
 Hpi example
Hpi example Glenn krauss
Glenn krauss Rethrog
Rethrog Frank krauss durham
Frank krauss durham Pio russo krauss
Pio russo krauss Neuroop
Neuroop Pio russo krauss
Pio russo krauss Krauss craft
Krauss craft Expressing ability
Expressing ability What is the necessity of starter in 3 phase induction motor
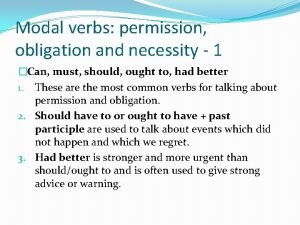
What is the necessity of starter in 3 phase induction motor Chapter 9 modals part 1
Chapter 9 modals part 1 Business necessity definition
Business necessity definition Advokate police
Advokate police Modal verbs introduction
Modal verbs introduction Necessity of fuse
Necessity of fuse False necessity trap
False necessity trap Modal verbs of obligation prohibition and permission
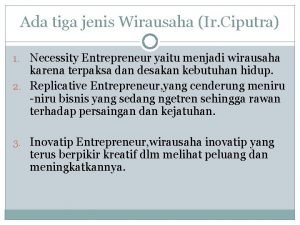
Modal verbs of obligation prohibition and permission Tujuan dan manfaat etika wirausaha
Tujuan dan manfaat etika wirausaha Netiquette
Netiquette Explain the necessity of irrigation
Explain the necessity of irrigation What year did george washington attacks ft necessity
What year did george washington attacks ft necessity Glenn hoffman umb
Glenn hoffman umb Glenn dion
Glenn dion Glenn bard
Glenn bard Glenn reinman
Glenn reinman Maysam alie-bazzi
Maysam alie-bazzi Glenn waning electric
Glenn waning electric Glenn parker huntsville al
Glenn parker huntsville al Glenn okun net worth
Glenn okun net worth Glenn fagan
Glenn fagan Veia braquiocefálica
Veia braquiocefálica Scott glenn rutgers
Scott glenn rutgers Tony lee glenn
Tony lee glenn Glenn maloney - ssb
Glenn maloney - ssb Glen samaai
Glen samaai Glenn bard
Glenn bard Glenn nathan
Glenn nathan Glenn fagan
Glenn fagan Glenn karisch
Glenn karisch Glenn bard
Glenn bard Glenn haddox
Glenn haddox Redaction criticism definition
Redaction criticism definition Glenn heirman
Glenn heirman Speaker
Speaker Metaparadigmas de faye glenn abdellah
Metaparadigmas de faye glenn abdellah Glenn nathan
Glenn nathan Glenn ahrens
Glenn ahrens Glenn hubbard inside job
Glenn hubbard inside job Glenn procedure
Glenn procedure