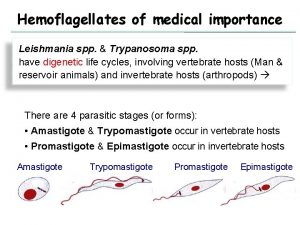
Leishmaniasis Promastigotes of Leishmania Amastigote of Leishmania The



- Slides: 31
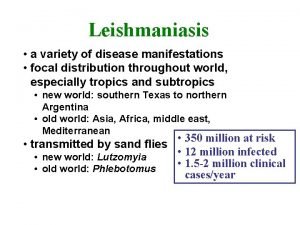
Leishmaniasis
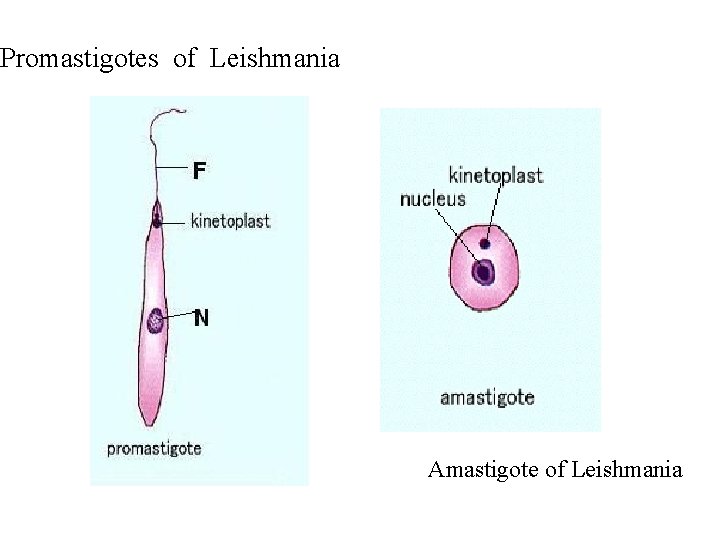
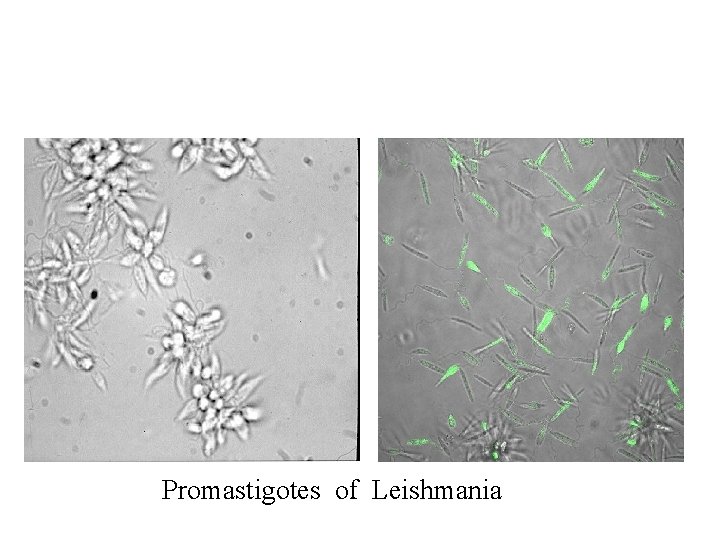
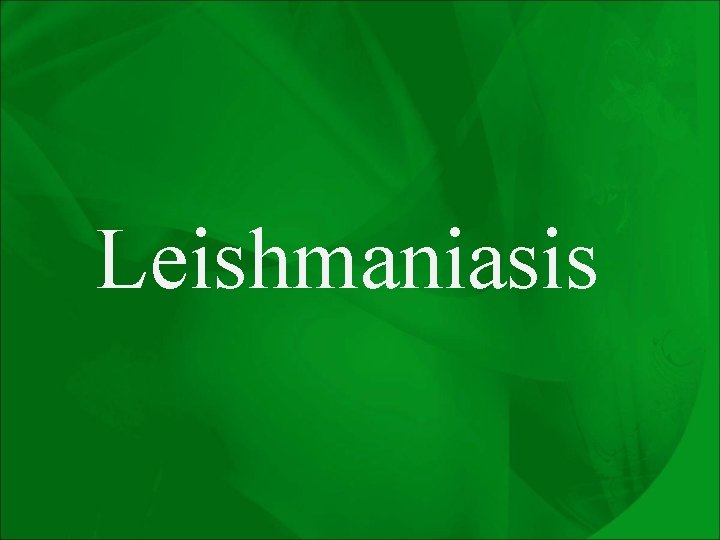
Promastigotes of Leishmania Amastigote of Leishmania
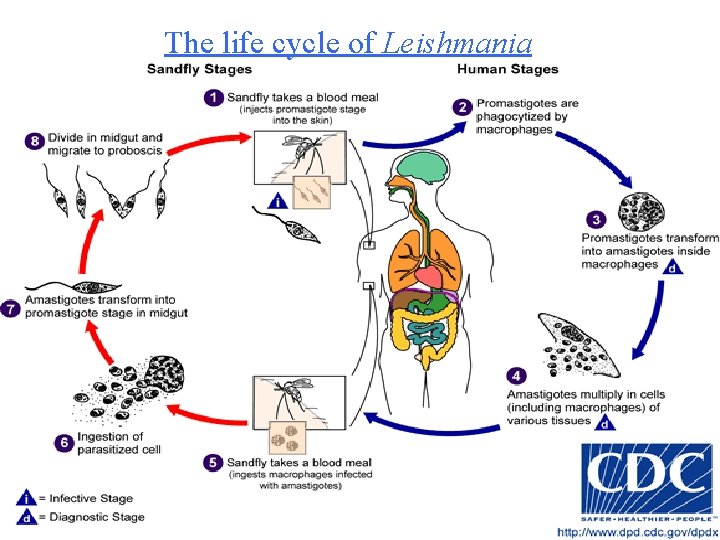
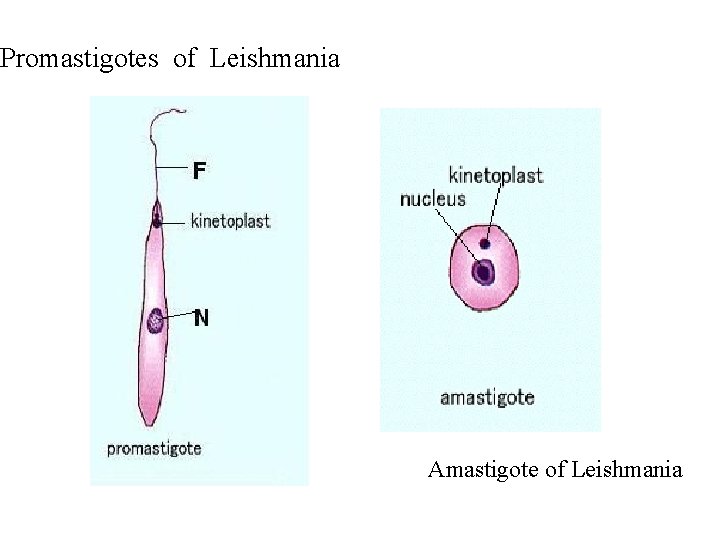
The life cycle of Leishmania
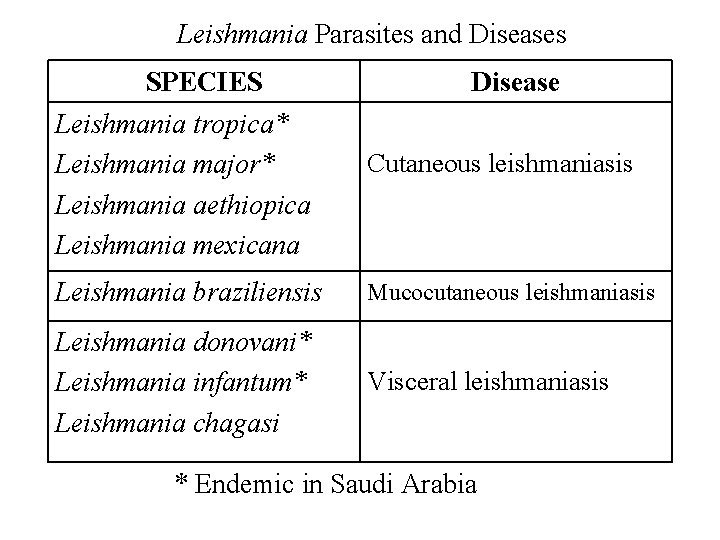
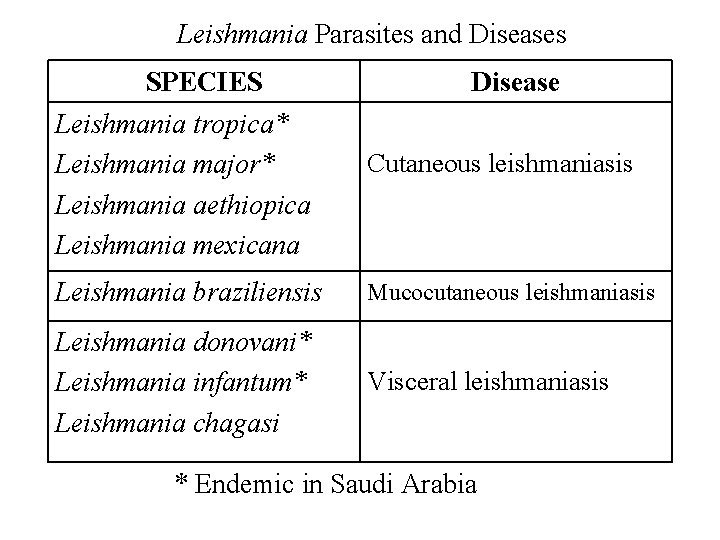
Leishmania Parasites and Diseases SPECIES Leishmania tropica* Leishmania major* Leishmania aethiopica Leishmania mexicana Disease Cutaneous leishmaniasis Leishmania braziliensis Mucocutaneous leishmaniasis Leishmania donovani* Leishmania infantum* Leishmania chagasi Visceral leishmaniasis * Endemic in Saudi Arabia

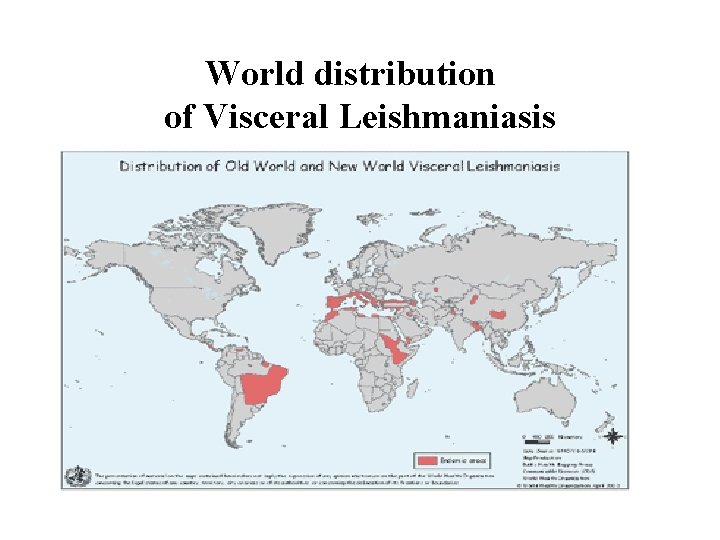
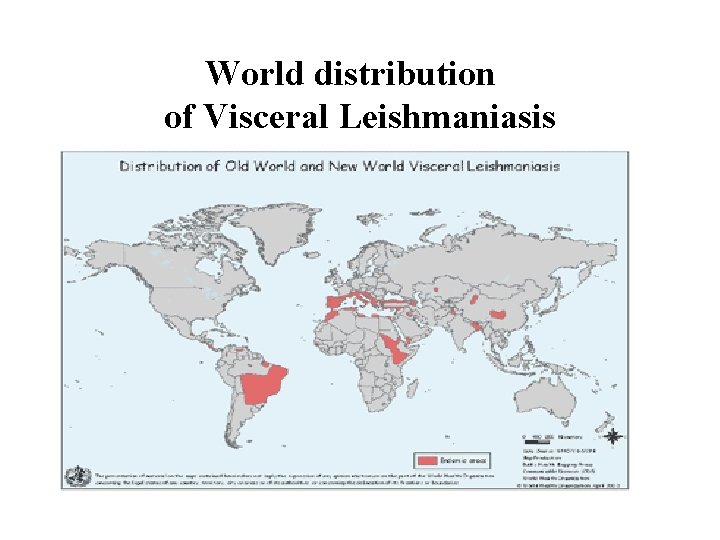
World distribution of Visceral Leishmaniasis
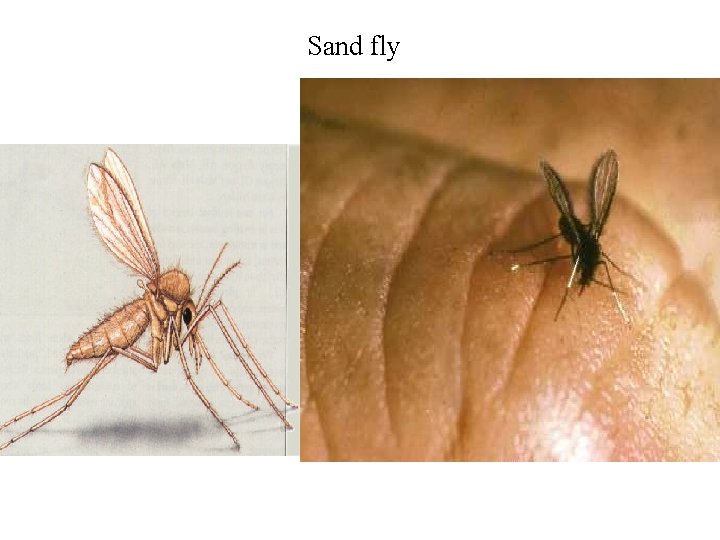
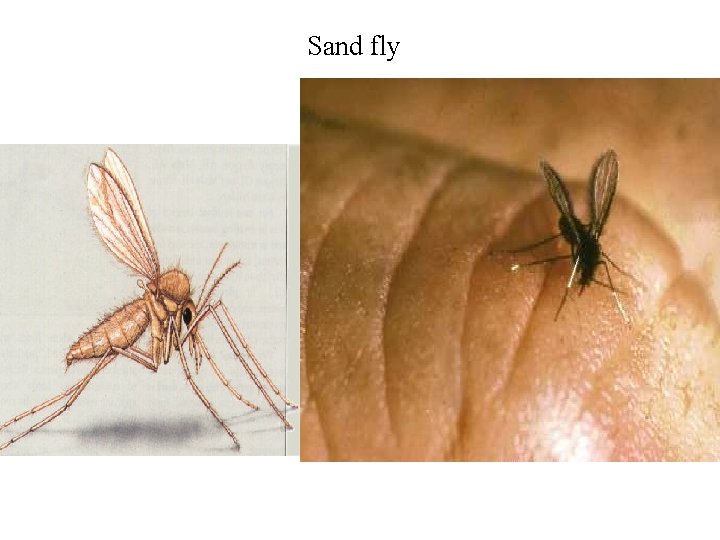
Sand fly
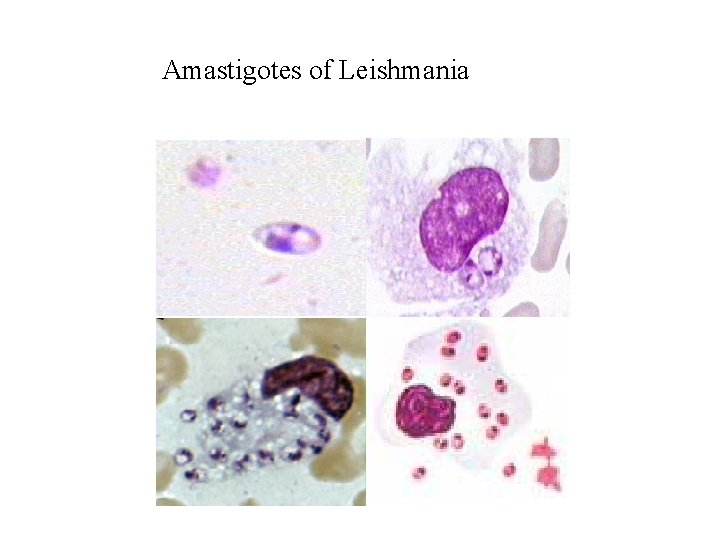
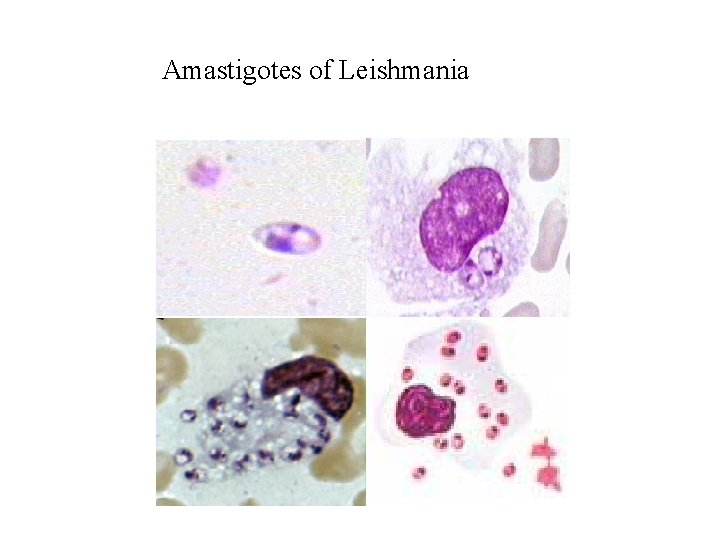
Amastigotes of Leishmania
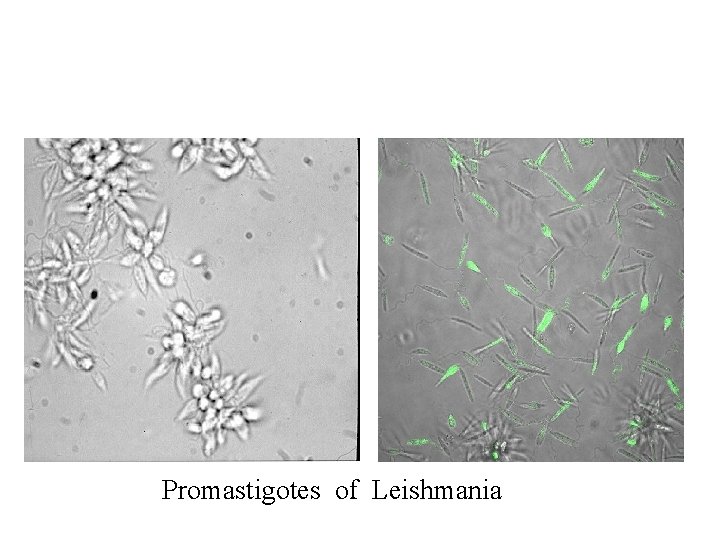
Promastigotes of Leishmania
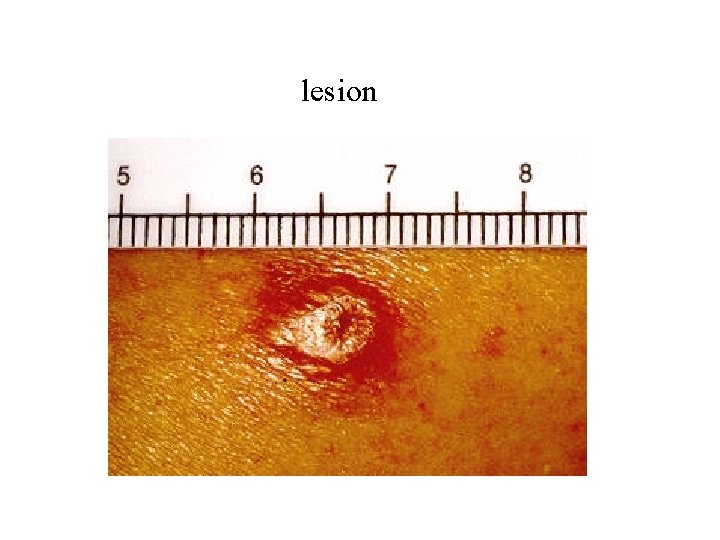
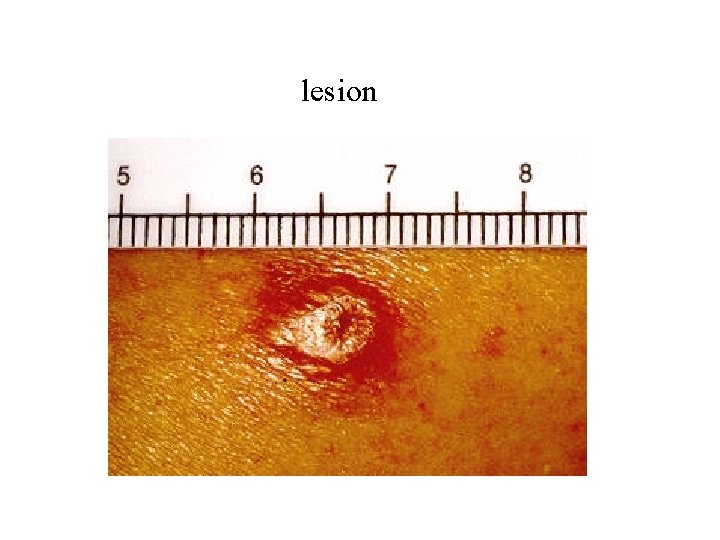
lesion
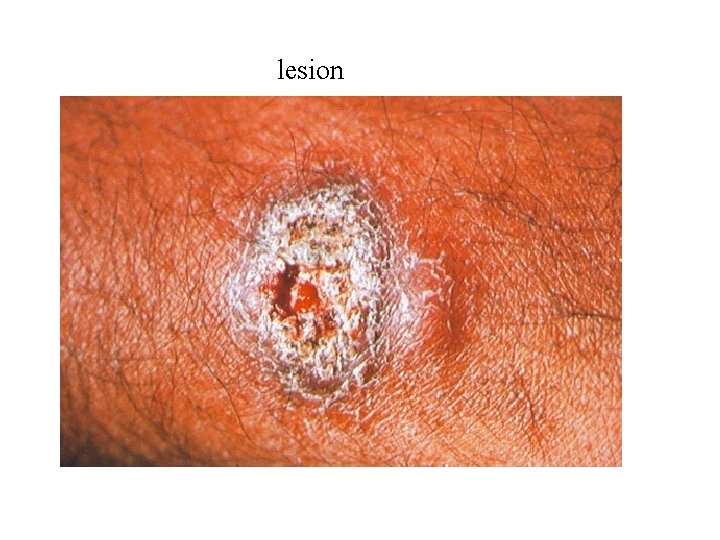
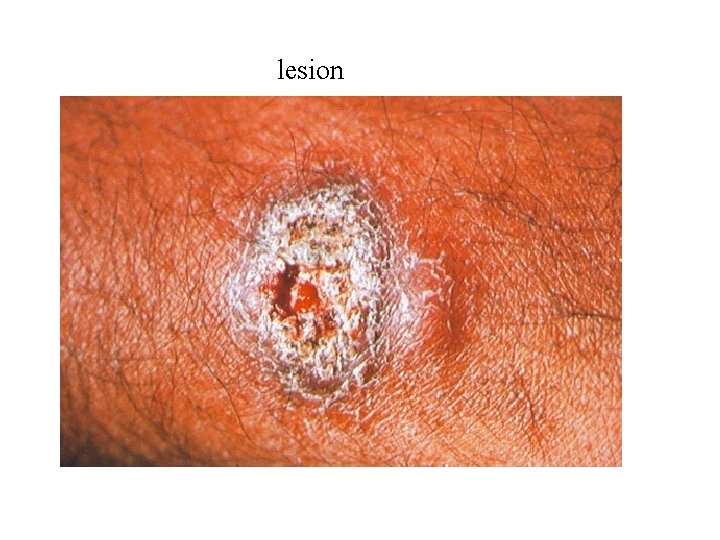
lesion
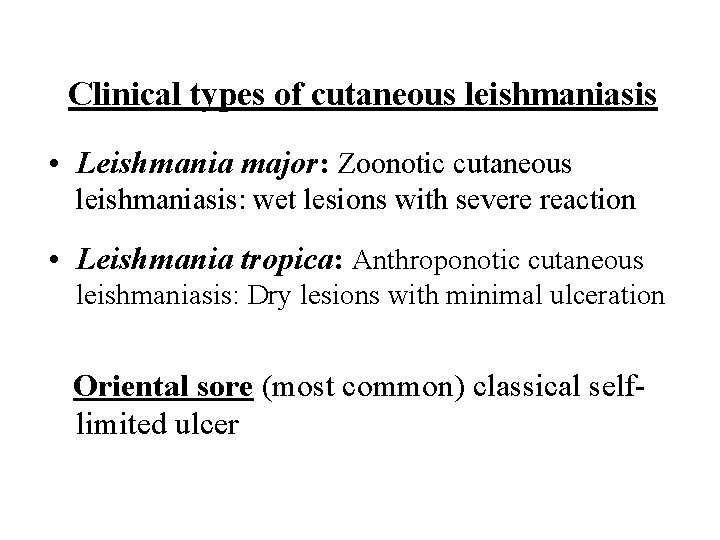
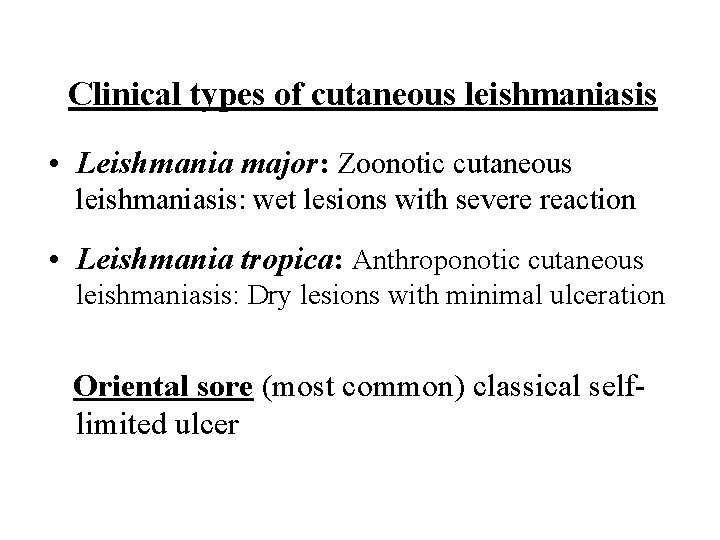
Clinical types of cutaneous leishmaniasis • Leishmania major: Zoonotic cutaneous leishmaniasis: wet lesions with severe reaction • Leishmania tropica: Anthroponotic cutaneous leishmaniasis: Dry lesions with minimal ulceration Oriental sore (most common) classical selflimited ulcer

Uncommon types • Diffuse cutaneous leishmaniasis (DCL): Caused by L. aethiopica, diffuse nodular nonulcerating lesions. Low immunity to Leishmania antigens, numerous parasites. • Leishmaniasis recidiva (lupoid leishmaniasis): Severe immunological reaction to leishmania antigen leading to persistent dry skin lesions, few parasites.

Diffuse cutaneous leishmaniasis Leishmaniasis recidiva
cutaneous leishmaniasis Diagnosis: • Smear: Giemsa stain – microscopy for LD bodies (amastigotes) • Biopsy: microscopy for LD bodies or culture in NNN medium for promastigotes
NNN medium
Pentostam ( sodium stibogluconate) for treatment of all types of leishmaniasis
Visceral leishmaniasis • • There are geographical variations. The diseases is called kala-azar Leishmania infantum mainly affect children Leishmania donovani mainly affects adults
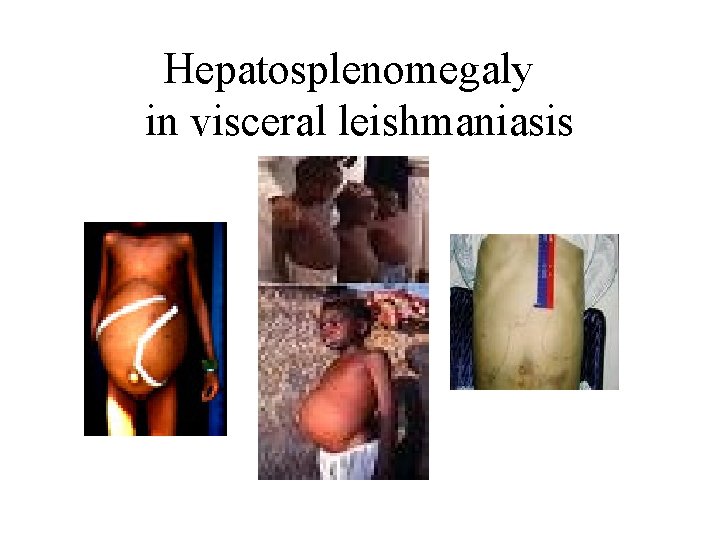
Presentation • Fever • Splenomegaly, hepatosplenomegaly • Weight loss • Anaemia • Epistaxis • Cough • Diarrhoea
Untreated disease can be fatal After recovery it might produce a condition called post kala-azar dermal leishmaniasis (PKDL)
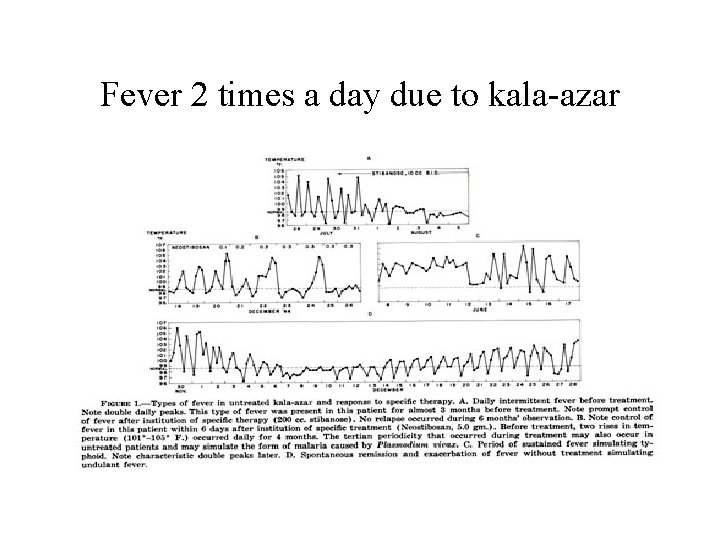
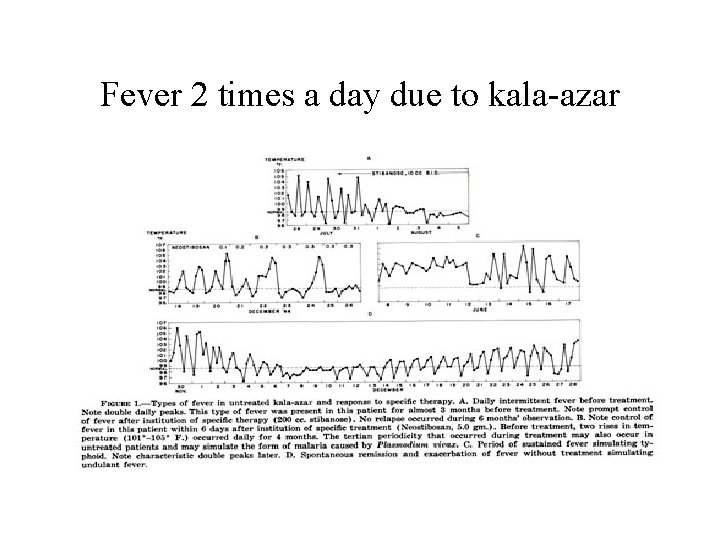
Fever 2 times a day due to kala-azar
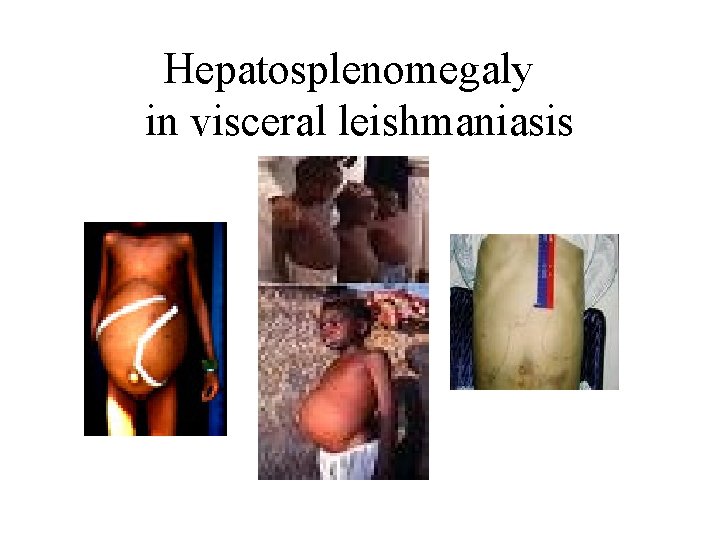
Hepatosplenomegaly in visceral leishmaniasis
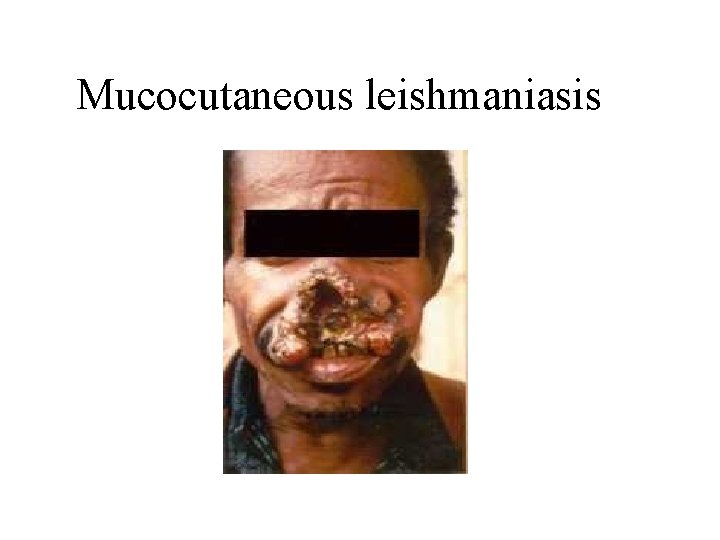
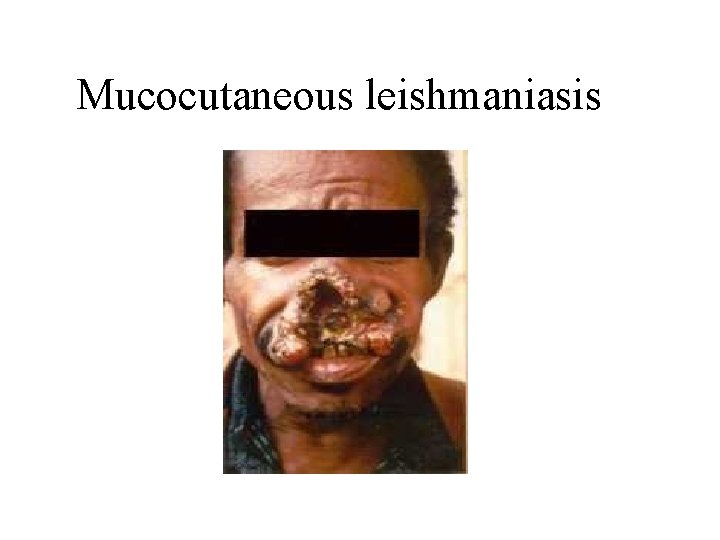
Mucocutaneous leishmaniasis
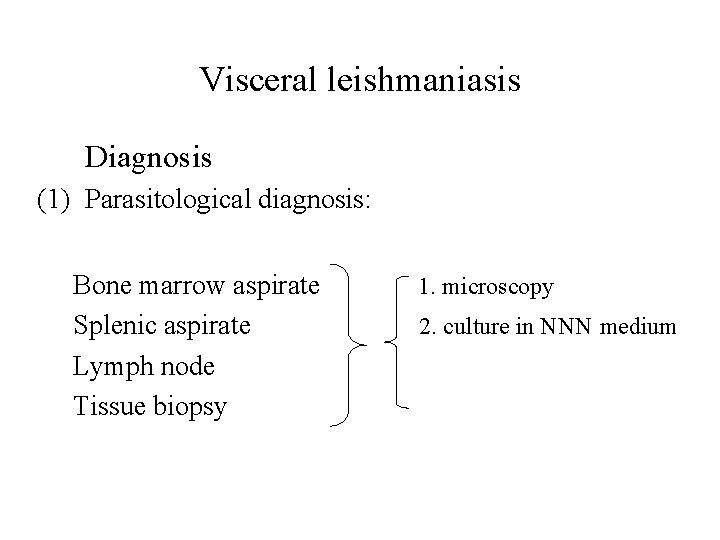
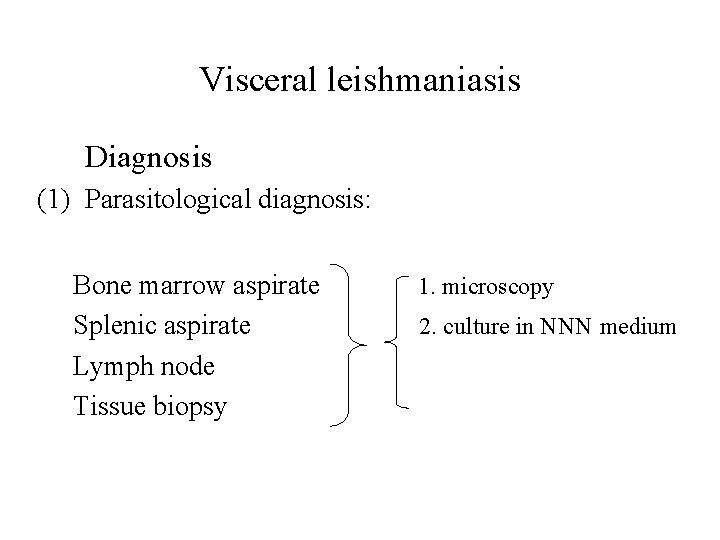
Visceral leishmaniasis Diagnosis (1) Parasitological diagnosis: Bone marrow aspirate Splenic aspirate Lymph node Tissue biopsy 1. microscopy 2. culture in NNN medium
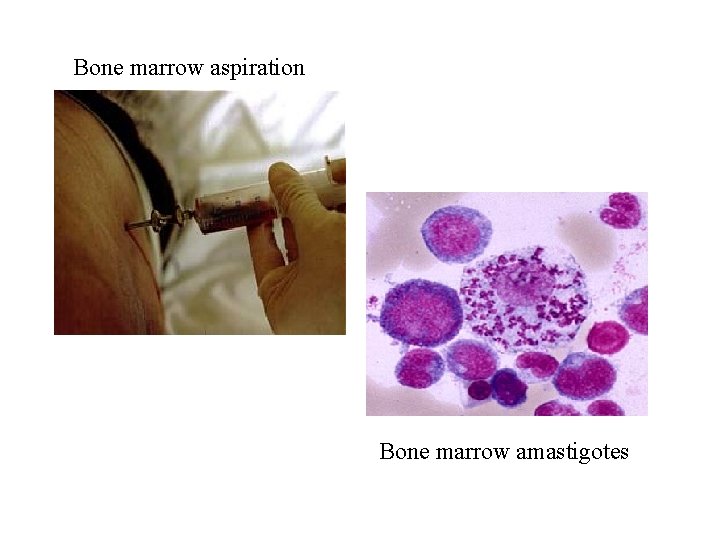
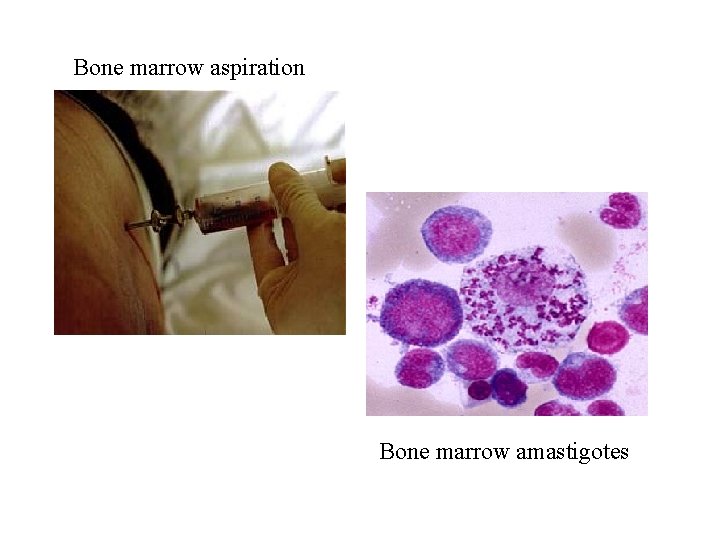
Bone marrow aspiration Bone marrow amastigotes
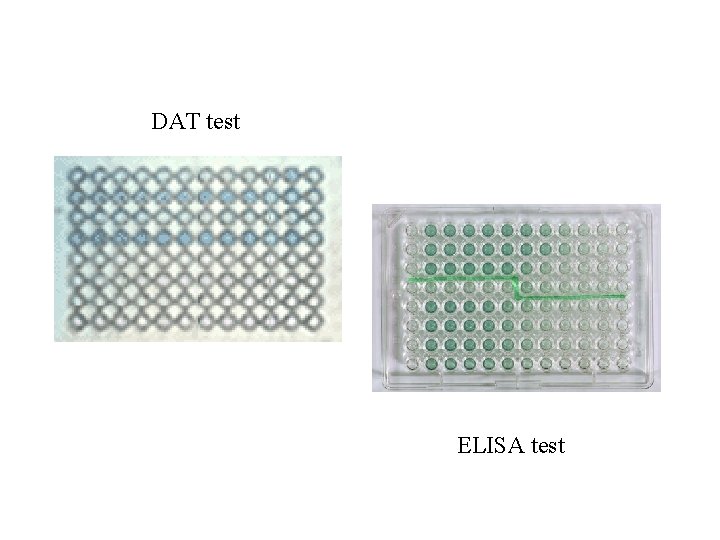
(2) Immunological Diagnosis: • Specific serologic tests: Direct Agglutination Test (DAT), ELISA, IFAT • r. K 39 antigen-based immunochromatographic tes. TWO LIMITATIONS FOR SEROLOGIC TESTS: – Do not diagnose relapses. – In endemic areas it is sometimes +ve in healthy individuals.
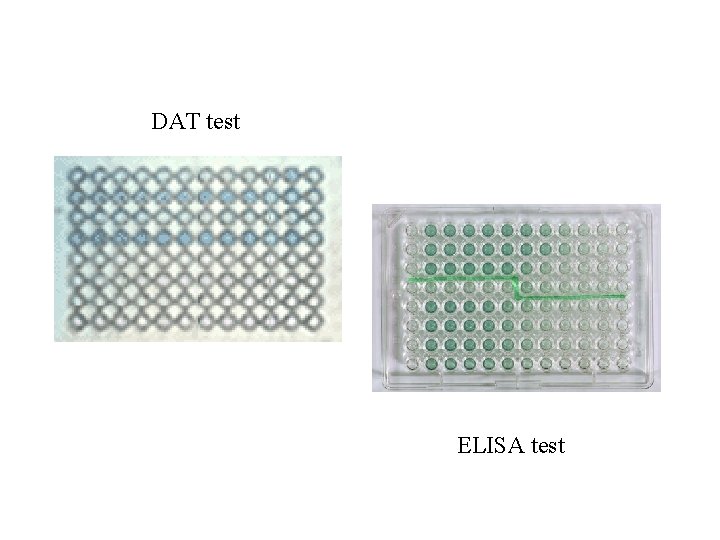
DAT test ELISA test
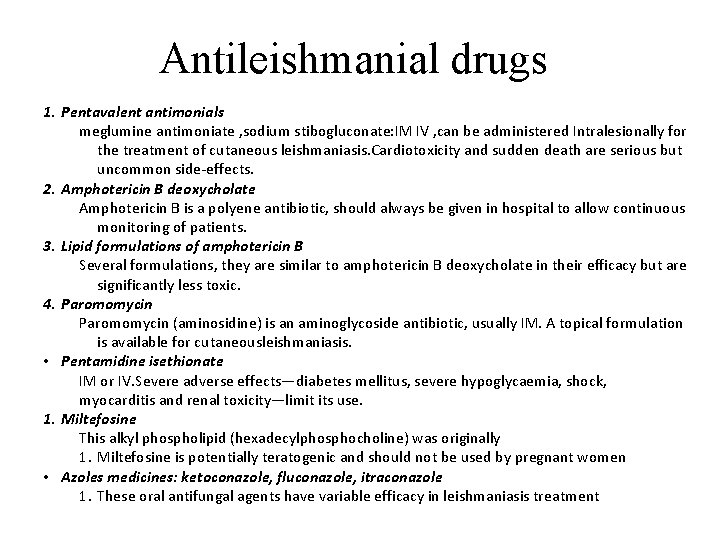
Antileishmanial drugs 1. Pentavalent antimonials meglumine antimoniate , sodium stibogluconate: IM IV , can be administered Intralesionally for the treatment of cutaneous leishmaniasis. Cardiotoxicity and sudden death are serious but uncommon side-effects. 2. Amphotericin B deoxycholate Amphotericin B is a polyene antibiotic, should always be given in hospital to allow continuous monitoring of patients. 3. Lipid formulations of amphotericin B Several formulations, they are similar to amphotericin B deoxycholate in their efficacy but are significantly less toxic. 4. Paromomycin (aminosidine) is an aminoglycoside antibiotic, usually IM. A topical formulation is available for cutaneousleishmaniasis. • Pentamidine isethionate IM or IV. Severe adverse effects—diabetes mellitus, severe hypoglycaemia, shock, myocarditis and renal toxicity—limit its use. 1. Miltefosine This alkyl phospholipid (hexadecylphosphocholine) was originally 1. Miltefosine is potentially teratogenic and should not be used by pregnant women • Azoles medicines: ketoconazole, fluconazole, itraconazole 1. These oral antifungal agents have variable efficacy in leishmaniasis treatment
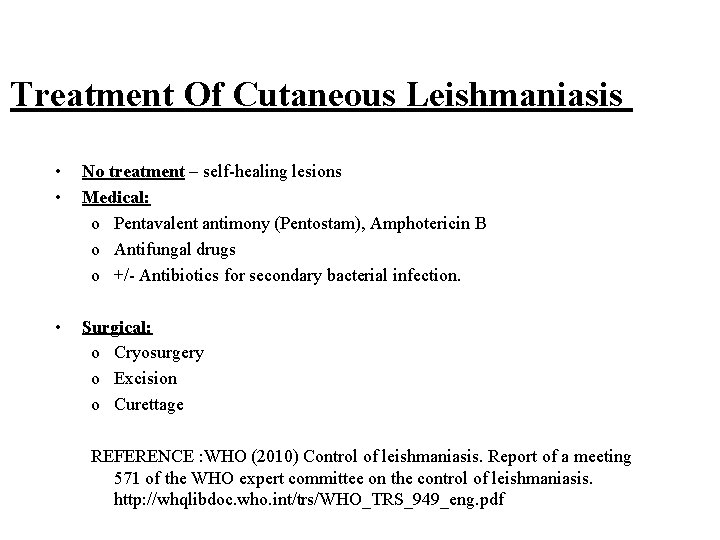
Treatment Of Cutaneous Leishmaniasis • • No treatment – self-healing lesions Medical: o Pentavalent antimony (Pentostam), Amphotericin B o Antifungal drugs o +/- Antibiotics for secondary bacterial infection. • Surgical: o Cryosurgery o Excision o Curettage REFERENCE : WHO (2010) Control of leishmaniasis. Report of a meeting 571 of the WHO expert committee on the control of leishmaniasis. http: //whqlibdoc. who. int/trs/WHO_TRS_949_eng. pdf
Treatment of visceral leishmanisis • Recommended treatment varies in different endemic areas: – Pentavalent antimony- sodium stibogluconate (Pentostam) – Amphotericin B Treatment of complications: • Anaemia • Bleeding • Infections etc. REFERENCE : WHO (2010) Control of leishmaniasis. Report of a meeting 571 of the WHO expert committee on the control of leishmaniasis. http: //whqlibdoc. who. int/trs/WHO_TRS_949_eng. pdf
 Amastigote and promastigote
Amastigote and promastigote Chagoma
Chagoma Visceral leishmaniasis
Visceral leishmaniasis Site:slidetodoc.com
Site:slidetodoc.com Tarık zaher
Tarık zaher Leishmaniasis
Leishmaniasis Cl
Cl Penyakit kala azar
Penyakit kala azar Characteristics of diptera
Characteristics of diptera Leishmaniasis
Leishmaniasis Visceral leishmaniasis
Visceral leishmaniasis Leishmaniasis
Leishmaniasis Visceral leishmaniasis
Visceral leishmaniasis Life cycle of african sleeping sickness
Life cycle of african sleeping sickness Leishmania
Leishmania Protozoario leishmania
Protozoario leishmania Promastigote
Promastigote Leishmania disease
Leishmania disease Tricomonase vaginalis
Tricomonase vaginalis Leishmania
Leishmania Leishmania disease
Leishmania disease Leishmania
Leishmania Leishmania spp
Leishmania spp Flebotomo
Flebotomo Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là giọng cùng tên? *
Thế nào là giọng cùng tên? * Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chúa yêu trần thế
Chúa yêu trần thế Lời thề hippocrates
Lời thề hippocrates