KDIGO Clinical Practice Guideline for the Diagnosis Evaluation
- Slides: 35
KDIGO Clinical Practice Guideline for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease. Mineral and Bone Disorder (CKD-MBD)
KDIGO Mission Statement Improve the care and outcomes of kidney disease patients worldwide through promoting coordination, collaboration and integration of initiatives to develop and implement clinical practice guidelines.
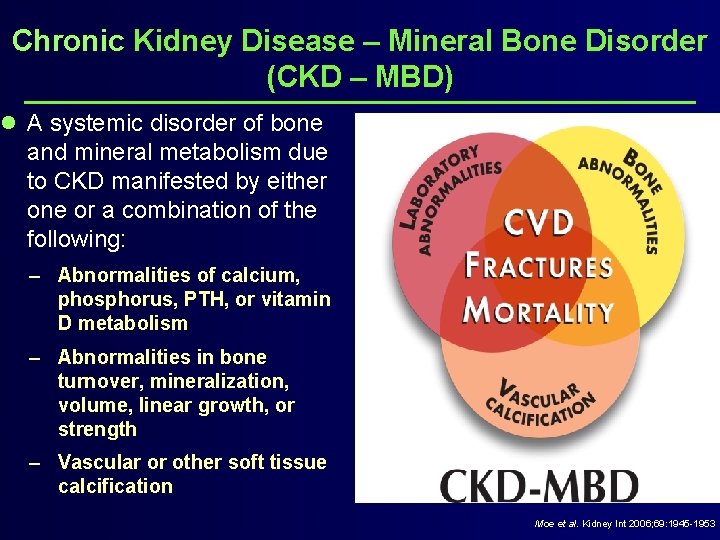
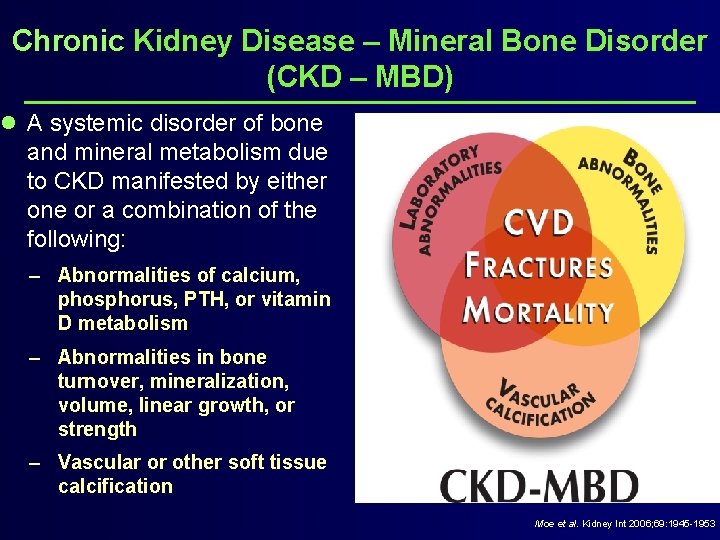
Chronic Kidney Disease – Mineral Bone Disorder (CKD – MBD) l A systemic disorder of bone and mineral metabolism due to CKD manifested by either one or a combination of the following: – Abnormalities of calcium, phosphorus, PTH, or vitamin D metabolism – Abnormalities in bone turnover, mineralization, volume, linear growth, or strength – Vascular or other soft tissue calcification Moe et al. Kidney Int 2006; 69: 1945 -1953
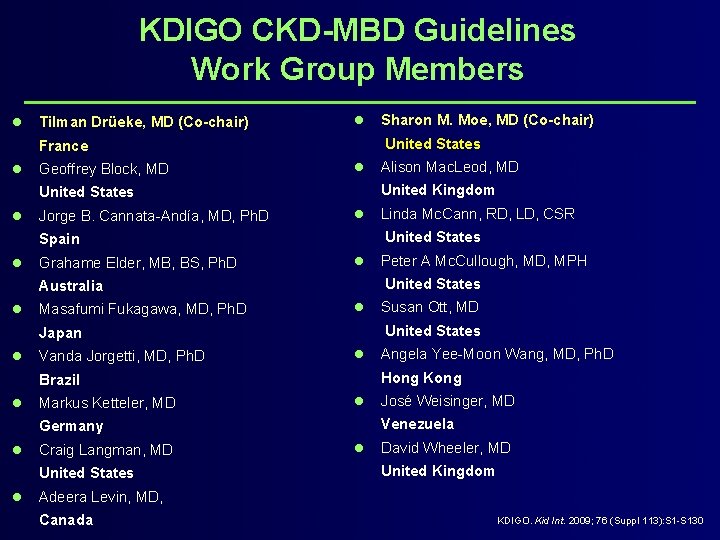
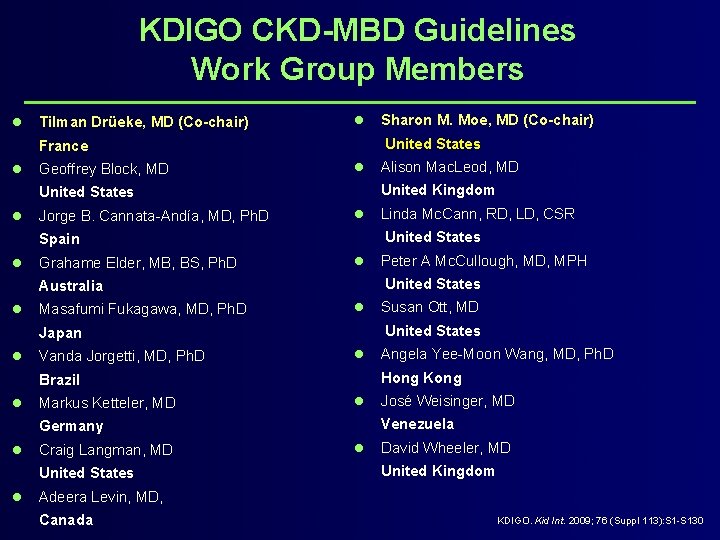
KDIGO CKD-MBD Guidelines Work Group Members l Tilman Drüeke, MD (Co-chair) l United States France l Geoffrey Block, MD l Jorge B. Cannata-Andía, MD, Ph. D l Grahame Elder, MB, BS, Ph. D l Masafumi Fukagawa, MD, Ph. D l Vanda Jorgetti, MD, Ph. D l Markus Ketteler, MD l Craig Langman, MD United States l José Weisinger, MD Venezuela Germany l Angela Yee-Moon Wang, MD, Ph. D Hong Kong Brazil l Susan Ott, MD United States Japan l Peter A Mc. Cullough, MD, MPH United States Australia l Linda Mc. Cann, RD, LD, CSR United States Spain l Alison Mac. Leod, MD United Kingdom United States l Sharon M. Moe, MD (Co-chair) l David Wheeler, MD United Kingdom Adeera Levin, MD, Canada KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
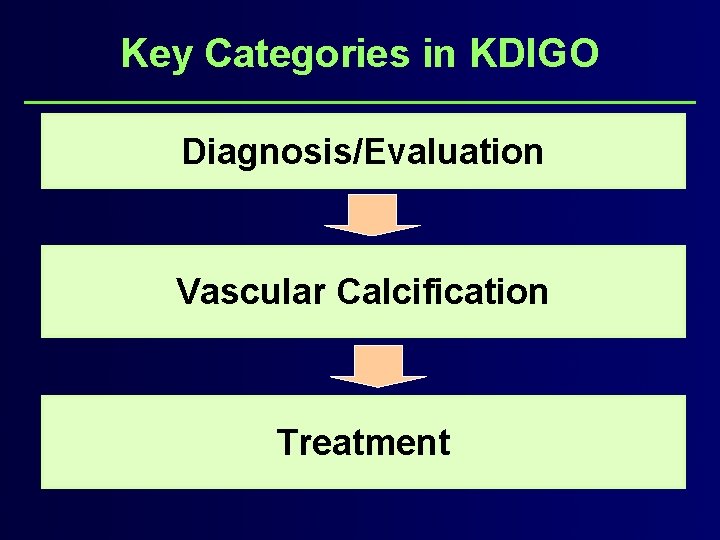
Key Categories in KDIGO Diagnosis/Evaluation Vascular Calcification Treatment
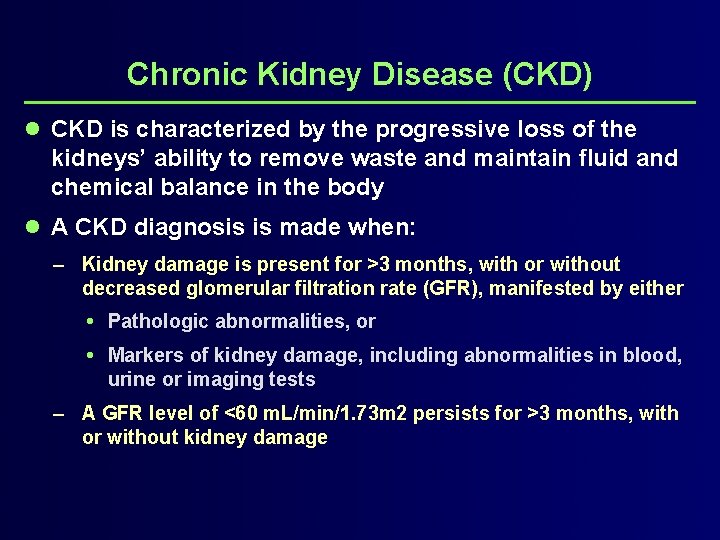
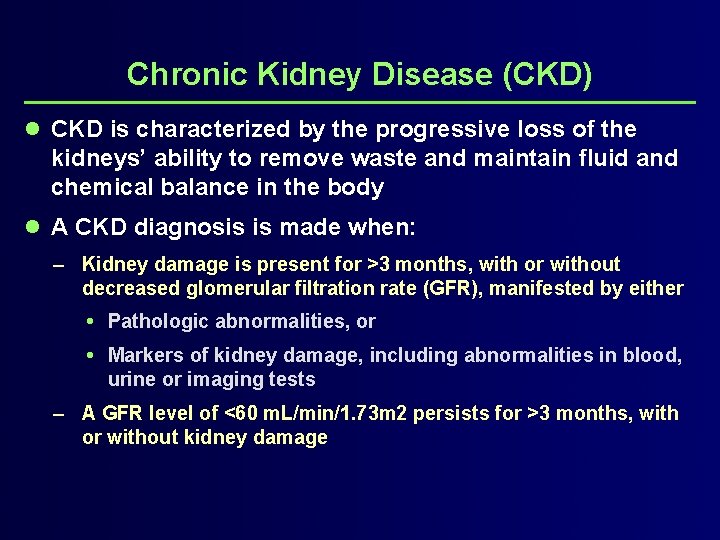
Chronic Kidney Disease (CKD) l CKD is characterized by the progressive loss of the kidneys’ ability to remove waste and maintain fluid and chemical balance in the body l A CKD diagnosis is made when: – Kidney damage is present for >3 months, with or without decreased glomerular filtration rate (GFR), manifested by either Pathologic abnormalities, or Markers of kidney damage, including abnormalities in blood, urine or imaging tests – A GFR level of <60 m. L/min/1. 73 m 2 persists for >3 months, with or without kidney damage
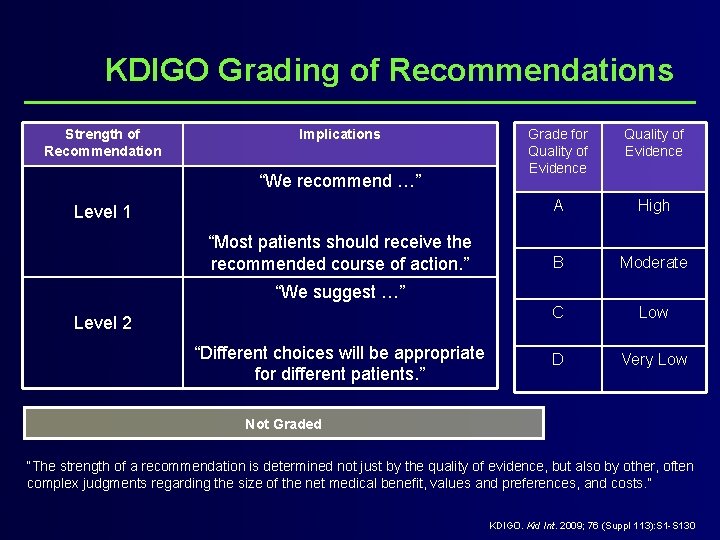
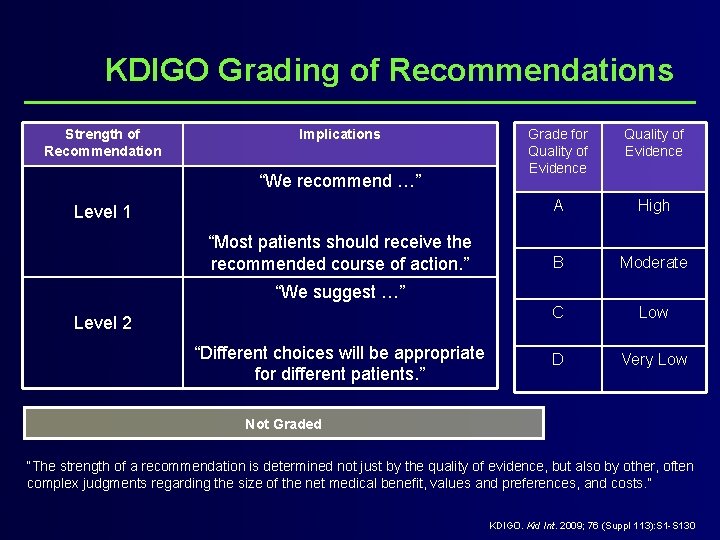
KDIGO Grading of Recommendations Strength of Recommendation Implications “We recommend …” Level 1 “Most patients should receive the recommended course of action. ” Grade for Quality of Evidence A High B Moderate C Low D Very Low “We suggest …” Level 2 “Different choices will be appropriate for different patients. ” Not Graded “The strength of a recommendation is determined not just by the quality of evidence, but also by other, often complex judgments regarding the size of the net medical benefit, values and preferences, and costs. ” KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
KDIGO: Diagnosis of CKD-MBD Biochemical Abnormalities
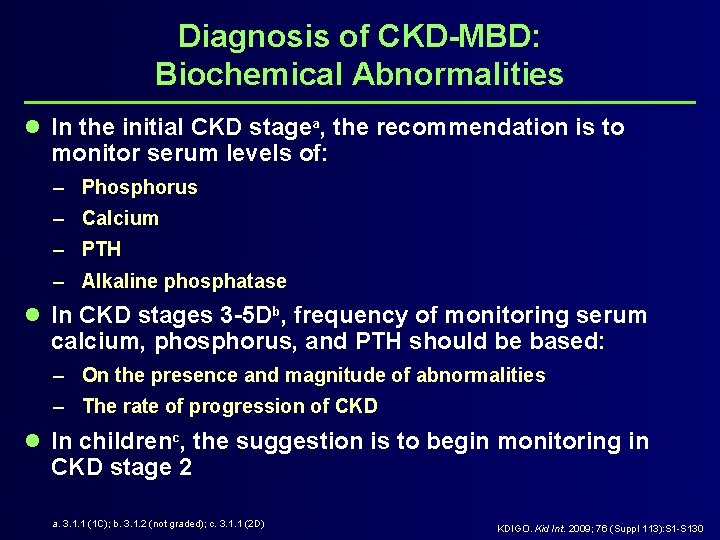
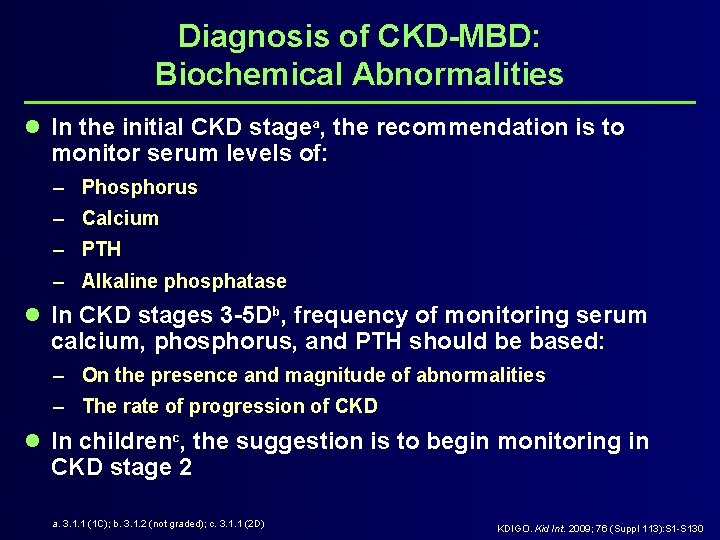
Diagnosis of CKD-MBD: Biochemical Abnormalities l In the initial CKD stagea, the recommendation is to monitor serum levels of: – Phosphorus – Calcium – PTH – Alkaline phosphatase l In CKD stages 3 -5 Db, frequency of monitoring serum calcium, phosphorus, and PTH should be based: – On the presence and magnitude of abnormalities – The rate of progression of CKD l In childrenc, the suggestion is to begin monitoring in CKD stage 2 a. 3. 1. 1 (1 C); b. 3. 1. 2 (not graded); c. 3. 1. 1 (2 D) KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
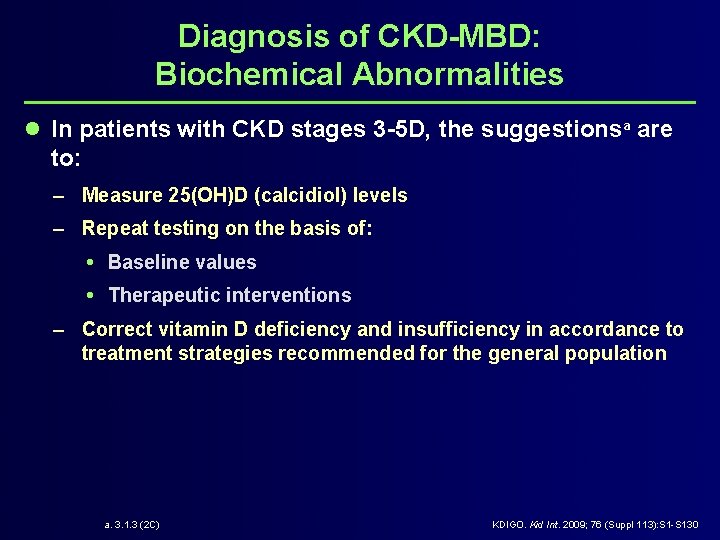
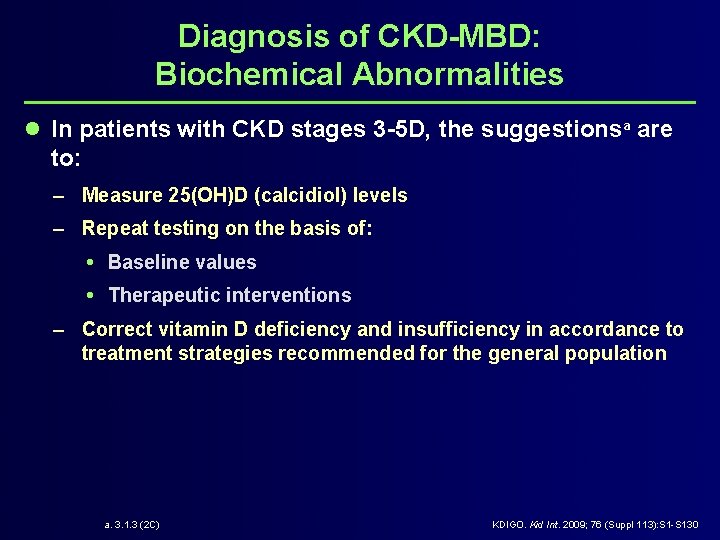
Diagnosis of CKD-MBD: Biochemical Abnormalities l In patients with CKD stages 3 -5 D, the suggestionsa are to: – Measure 25(OH)D (calcidiol) levels – Repeat testing on the basis of: Baseline values Therapeutic interventions – Correct vitamin D deficiency and insufficiency in accordance to treatment strategies recommended for the general population a. 3. 1. 3 (2 C) KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
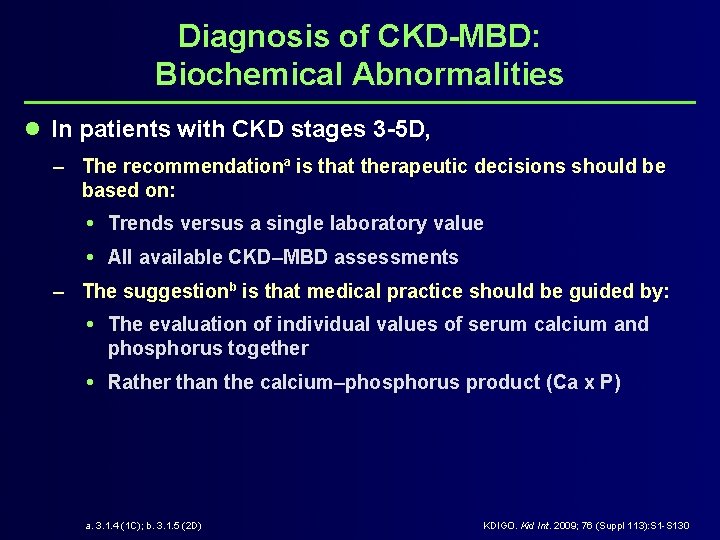
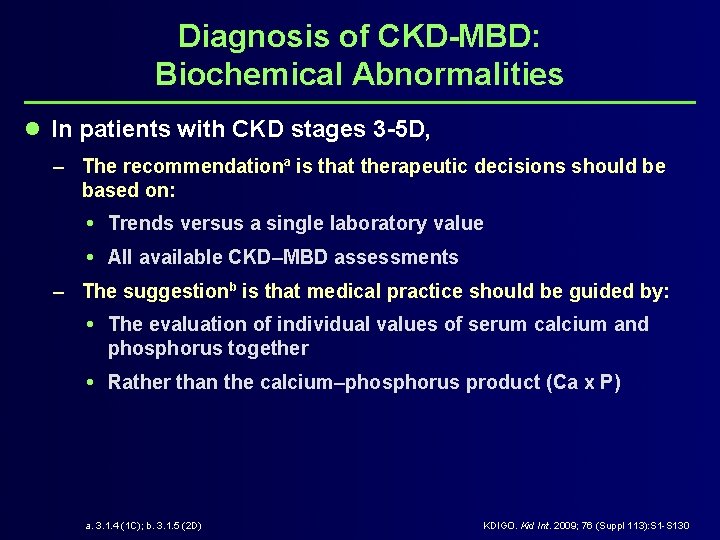
Diagnosis of CKD-MBD: Biochemical Abnormalities l In patients with CKD stages 3 -5 D, – The recommendationa is that therapeutic decisions should be based on: Trends versus a single laboratory value All available CKD–MBD assessments – The suggestionb is that medical practice should be guided by: The evaluation of individual values of serum calcium and phosphorus together Rather than the calcium–phosphorus product (Ca x P) a. 3. 1. 4 (1 C); b. 3. 1. 5 (2 D) KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
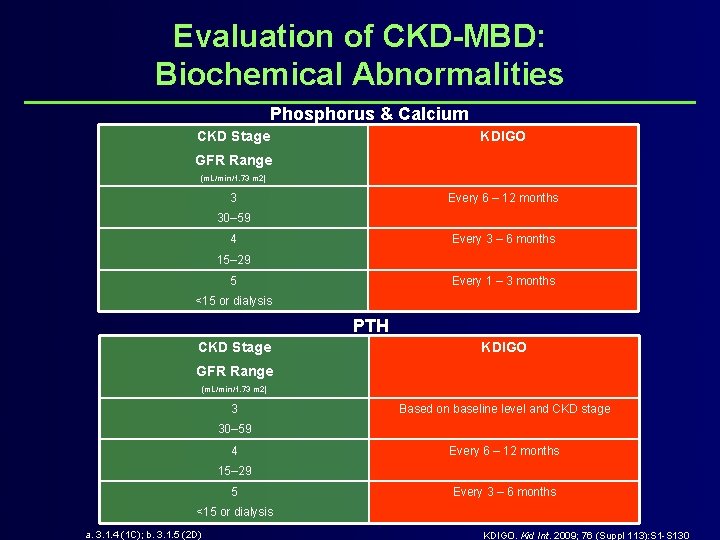
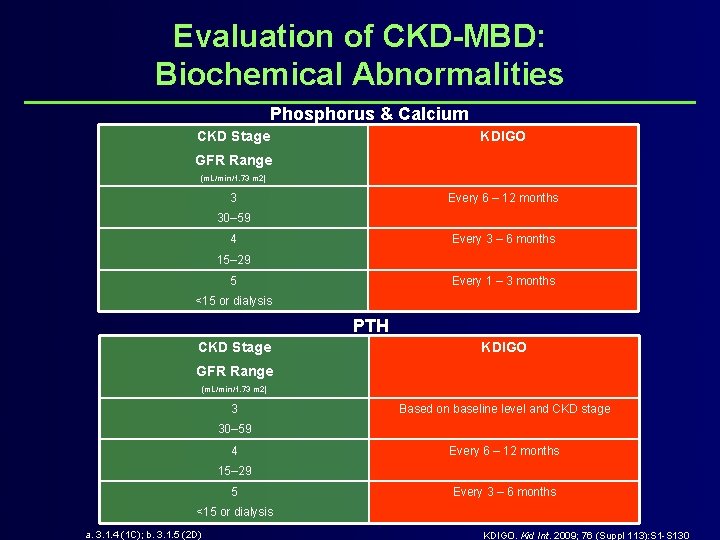
Evaluation of CKD-MBD: Biochemical Abnormalities Phosphorus & Calcium CKD Stage KDIGO GFR Range (m. L/min/1. 73 m 2) 3 Every 6 – 12 months 30– 59 4 Every 3 – 6 months 15– 29 5 Every 1 – 3 months <15 or dialysis PTH CKD Stage KDIGO GFR Range (m. L/min/1. 73 m 2) 3 Based on baseline level and CKD stage 30– 59 4 Every 6 – 12 months 15– 29 5 Every 3 – 6 months <15 or dialysis a. 3. 1. 4 (1 C); b. 3. 1. 5 (2 D) KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
KDIGO: Diagnosis of CKD-MBD Vascular Calcification
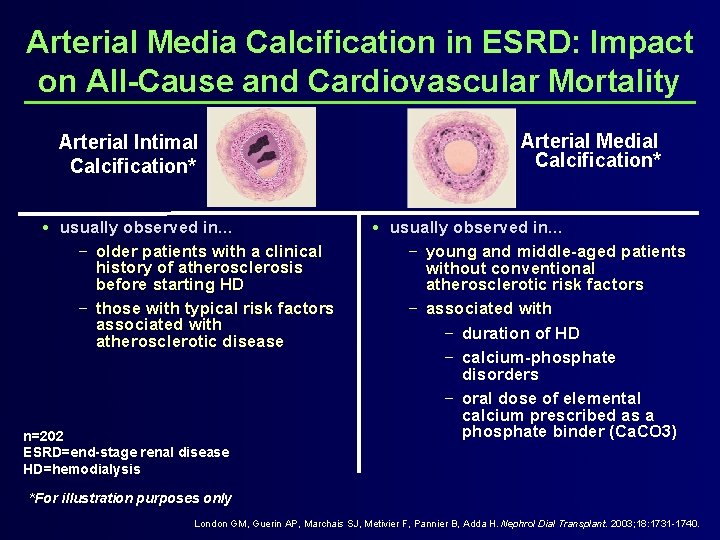
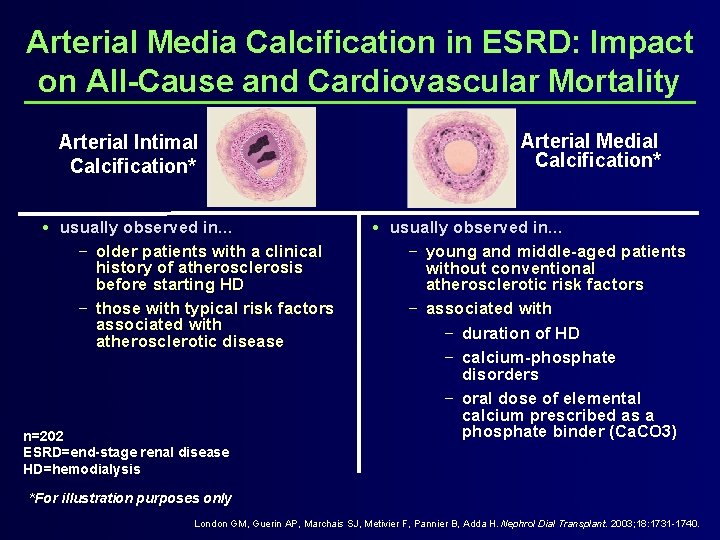
Arterial Media Calcification in ESRD: Impact on All-Cause and Cardiovascular Mortality Arterial Intimal Calcification* usually observed in… − older patients with a clinical history of atherosclerosis before starting HD − those with typical risk factors associated with atherosclerotic disease n=202 ESRD=end-stage renal disease HD=hemodialysis Arterial Medial Calcification* usually observed in… − young and middle-aged patients without conventional atherosclerotic risk factors − associated with − duration of HD − calcium-phosphate disorders − oral dose of elemental calcium prescribed as a phosphate binder (Ca. CO 3) *For illustration purposes only London GM, Guerin AP, Marchais SJ, Metivier F, Pannier B, Adda H. Nephrol Dial Transplant. 2003; 18: 1731 -1740.
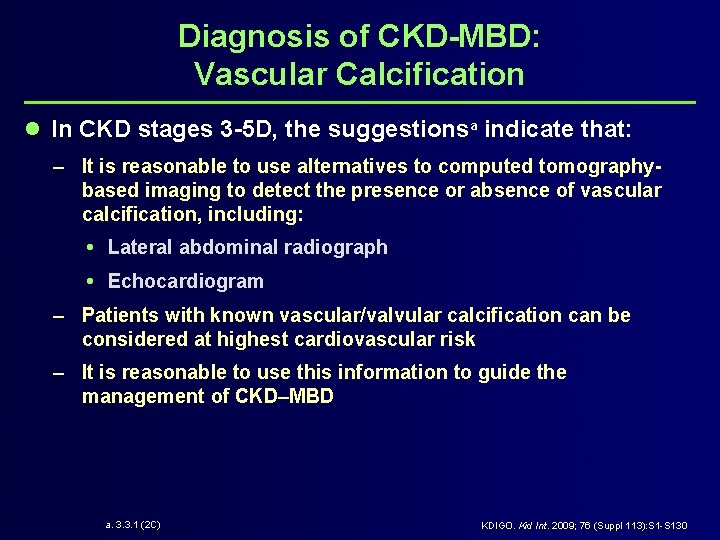
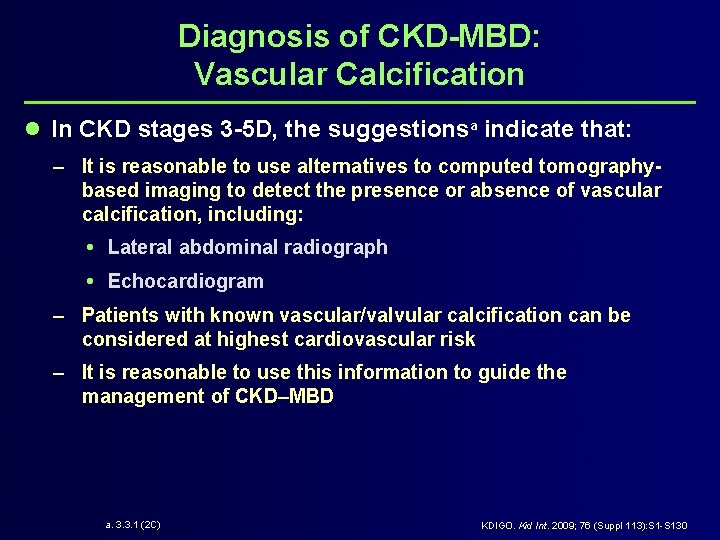
Diagnosis of CKD-MBD: Vascular Calcification l In CKD stages 3 -5 D, the suggestionsa indicate that: – It is reasonable to use alternatives to computed tomographybased imaging to detect the presence or absence of vascular calcification, including: Lateral abdominal radiograph Echocardiogram – Patients with known vascular/valvular calcification can be considered at highest cardiovascular risk – It is reasonable to use this information to guide the management of CKD–MBD a. 3. 3. 1 (2 C) KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
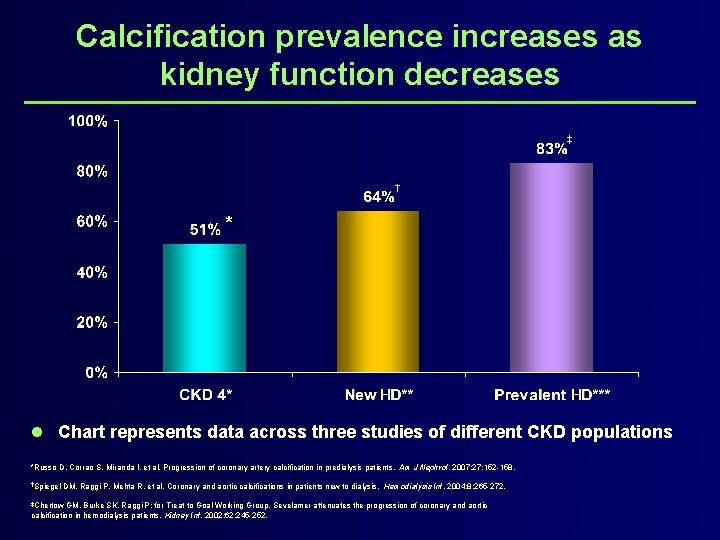
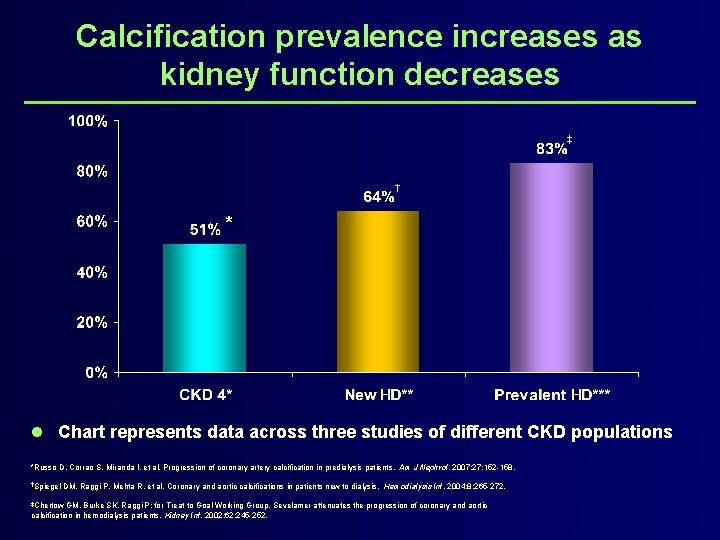
Calcification prevalence increases as kidney function decreases ‡ † * l Chart represents data across three studies of different CKD populations *Russo D, Corrao S, Miranda I, et al. Progression of coronary artery calcification in predialysis patients. Am J Nephrol. 2007; 27: 152 -158. †Spiegel DM, Raggi P, Mehta R, et al. Coronary and aortic calcifications in patients new to dialysis. Hemodialysis Int. 2004; 8: 265 -272. ‡Chertow GM, Burke SK, Raggi P; for Treat to Goal Working Group. Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patients. Kidney Int. 2002; 62: 245 -252.
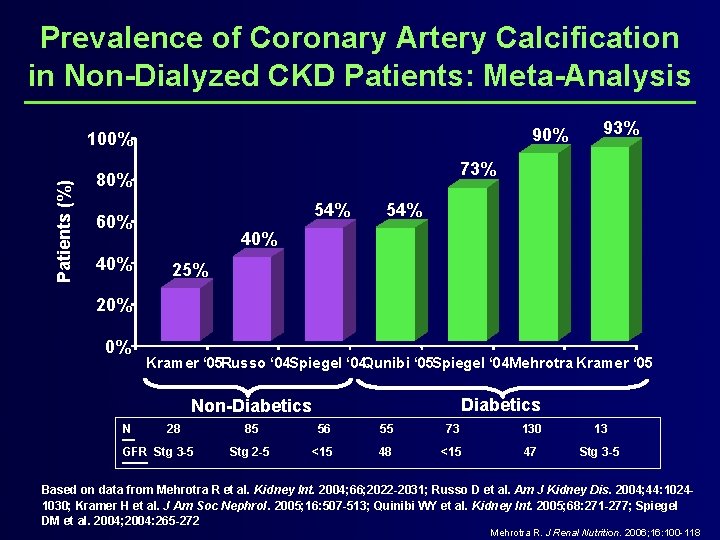
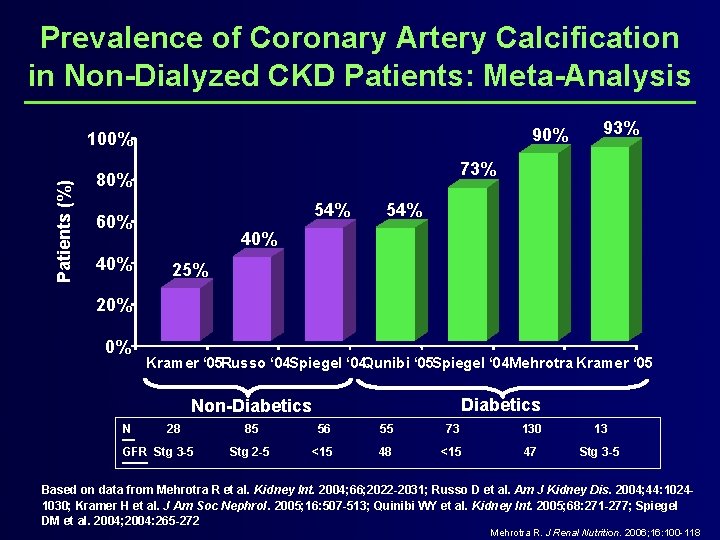
Prevalence of Coronary Artery Calcification in Non-Dialyzed CKD Patients: Meta-Analysis 90% Patients (%) 100% 73% 80% 54% 60% 40% 93% 54% 40% 25% 20% 0% Kramer ‘ 05 Russo ‘ 04 Spiegel ‘ 04 Qunibi ‘ 05 Spiegel ‘ 04 Mehrotra Kramer ‘ 05 Diabetics Non-Diabetics N 28 GFR Stg 3 -5 85 56 55 73 130 13 Stg 2 -5 <15 48 <15 47 Stg 3 -5 Based on data from Mehrotra R et al. Kidney Int. 2004; 66; 2022 -2031; Russo D et al. Am J Kidney Dis. 2004; 44: 10241030; Kramer H et al. J Am Soc Nephrol. 2005; 16: 507 -513; Quinibi WY et al. Kidney Int. 2005; 68: 271 -277; Spiegel DM et al. 2004; 2004: 265 -272 Mehrotra R. J Renal Nutrition. 2006; 16: 100 -118
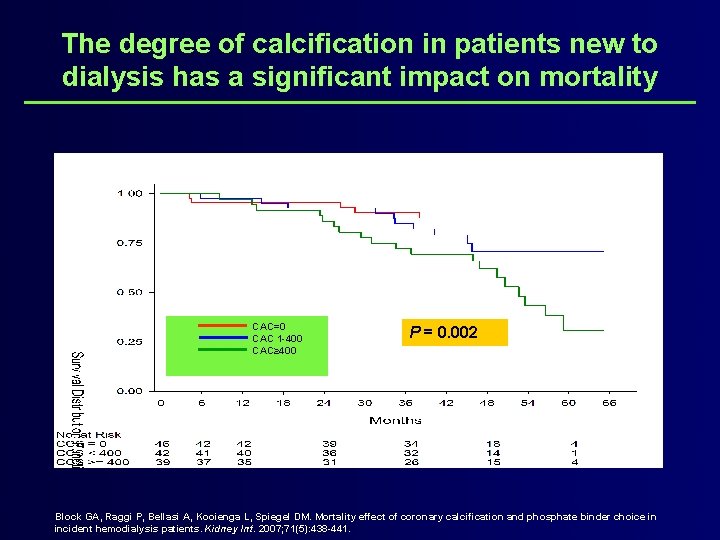
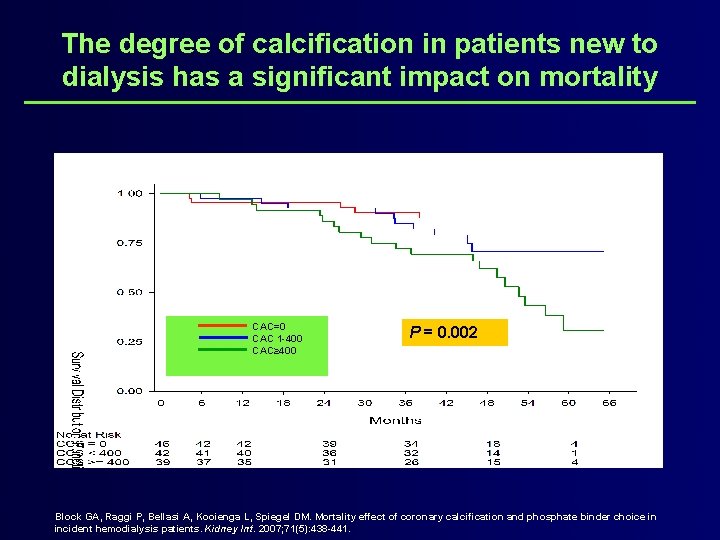
The degree of calcification in patients new to dialysis has a significant impact on mortality CAC=0 CAC 1 -400 CAC≥ 400 P = 0. 002 Block GA, Raggi P, Bellasi A, Kooienga L, Spiegel DM. Mortality effect of coronary calcification and phosphate binder choice in incident hemodialysis patients. Kidney Int. 2007; 71(5): 438 -441.
Treatment of CKD-MBD: Phosphorus and Calcium
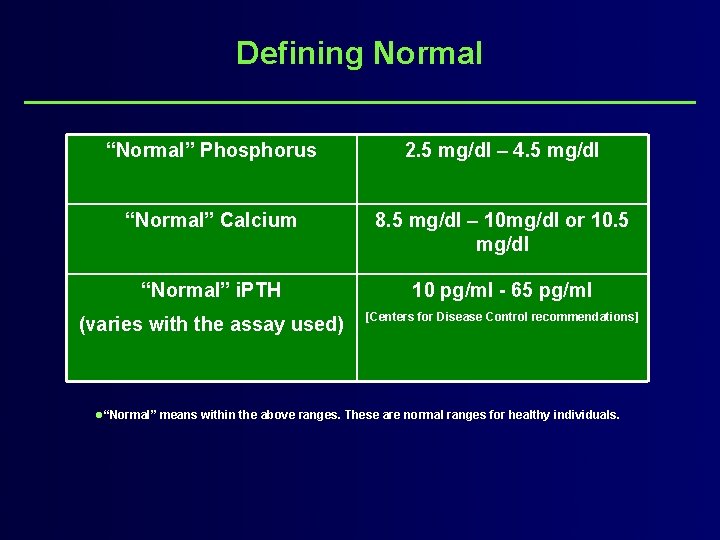
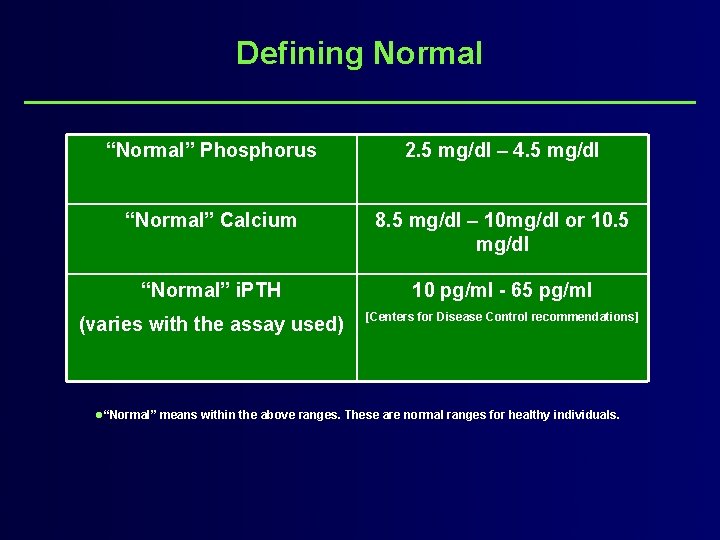
Defining Normal “Normal” Phosphorus 2. 5 mg/dl – 4. 5 mg/dl “Normal” Calcium 8. 5 mg/dl – 10 mg/dl or 10. 5 mg/dl “Normal” i. PTH 10 pg/ml - 65 pg/ml (varies with the assay used) [Centers for Disease Control recommendations] l“Normal” means within the above ranges. These are normal ranges for healthy individuals.
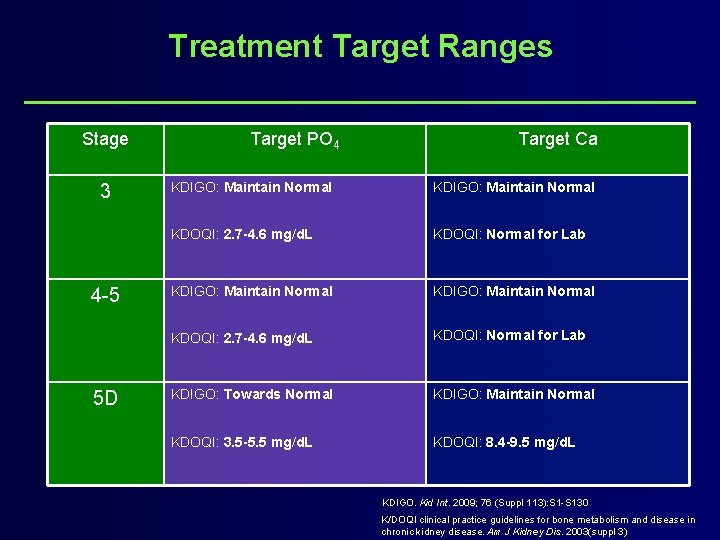
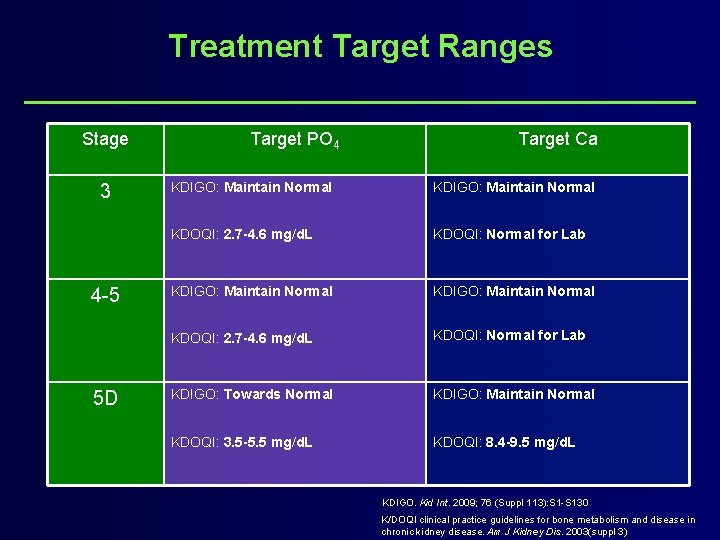
Treatment Target Ranges Stage 3 4 -5 5 D Target PO 4 Target Ca KDIGO: Maintain Normal KDOQI: 2. 7 -4. 6 mg/d. L KDOQI: Normal for Lab KDIGO: Towards Normal KDIGO: Maintain Normal KDOQI: 3. 5 -5. 5 mg/d. L KDOQI: 8. 4 -9. 5 mg/d. L KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130 K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003(suppl 3)
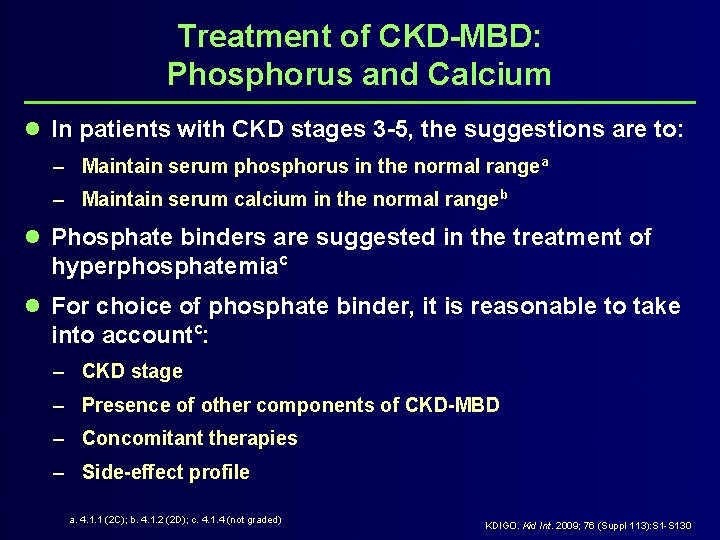
Treatment of CKD-MBD: Phosphorus and Calcium l In patients with CKD stages 3 -5, the suggestions are to: – Maintain serum phosphorus in the normal rangea – Maintain serum calcium in the normal rangeb l Phosphate binders are suggested in the treatment of hyperphosphatemiac l For choice of phosphate binder, it is reasonable to take into accountc: – CKD stage – Presence of other components of CKD-MBD – Concomitant therapies – Side-effect profile a. 4. 1. 1 (2 C); b. 4. 1. 2 (2 D); c. 4. 1. 4 (not graded) KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
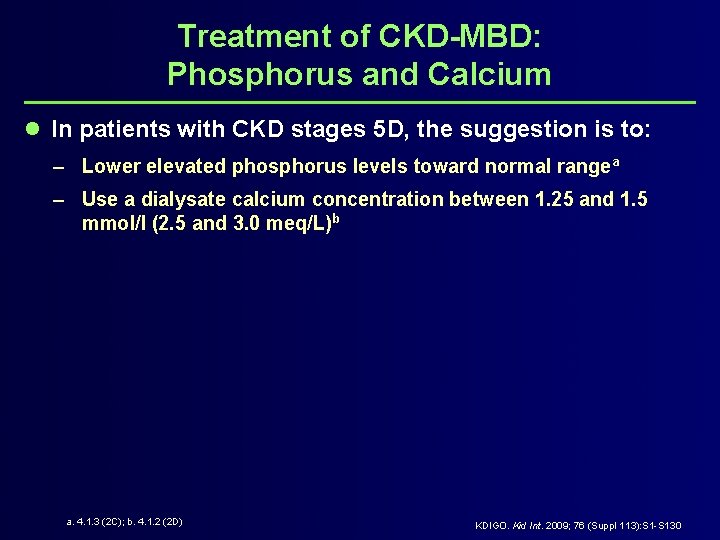
Treatment of CKD-MBD: Phosphorus and Calcium l In patients with CKD stages 5 D, the suggestion is to: – Lower elevated phosphorus levels toward normal rangea – Use a dialysate calcium concentration between 1. 25 and 1. 5 mmol/l (2. 5 and 3. 0 meq/L)b a. 4. 1. 3 (2 C); b. 4. 1. 2 (2 D) KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
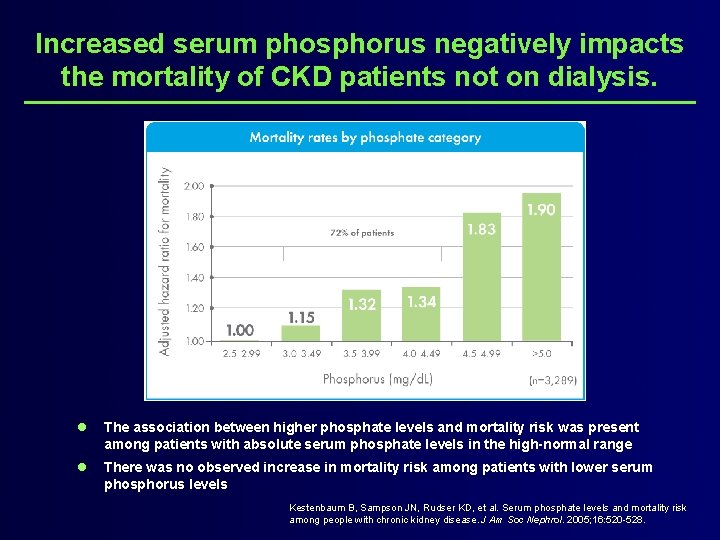
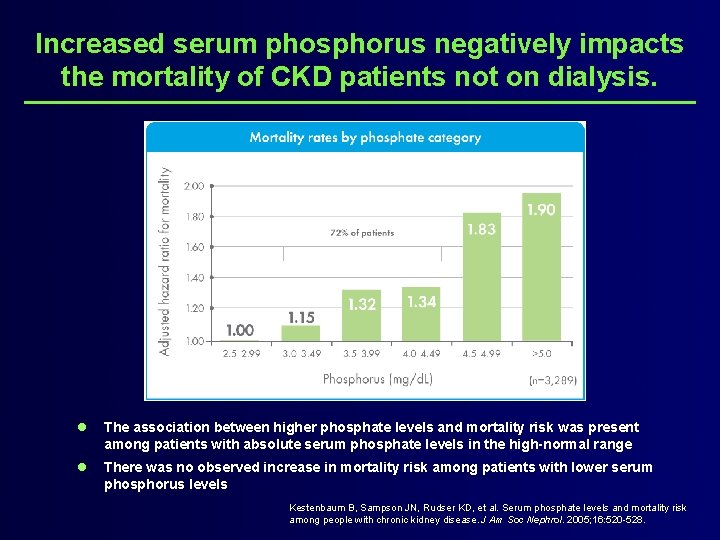
Increased serum phosphorus negatively impacts the mortality of CKD patients not on dialysis. l The association between higher phosphate levels and mortality risk was present among patients with absolute serum phosphate levels in the high-normal range l There was no observed increase in mortality risk among patients with lower serum phosphorus levels Kestenbaum B, Sampson JN, Rudser KD, et al. Serum phosphate levels and mortality risk among people with chronic kidney disease. J Am Soc Nephrol. 2005; 16: 520 -528.
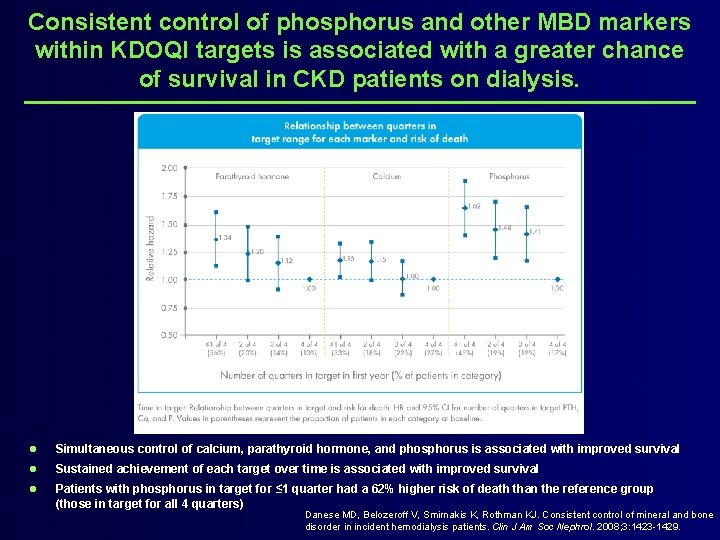
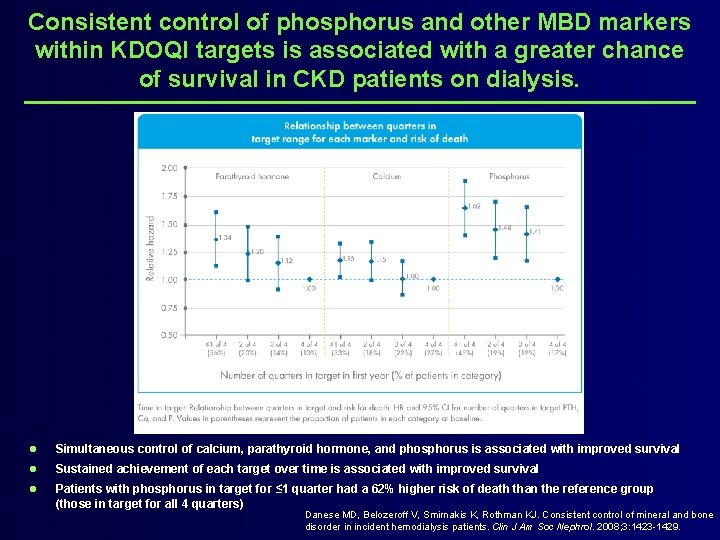
Consistent control of phosphorus and other MBD markers within KDOQI targets is associated with a greater chance of survival in CKD patients on dialysis. l Simultaneous control of calcium, parathyroid hormone, and phosphorus is associated with improved survival l Sustained achievement of each target over time is associated with improved survival l Patients with phosphorus in target for ≤ 1 quarter had a 62% higher risk of death than the reference group (those in target for all 4 quarters) Danese MD, Belozeroff V, Smirnakis K, Rothman KJ. Consistent control of mineral and bone disorder in incident hemodialysis patients. Clin J Am Soc Nephrol. 2008; 3: 1423 -1429.
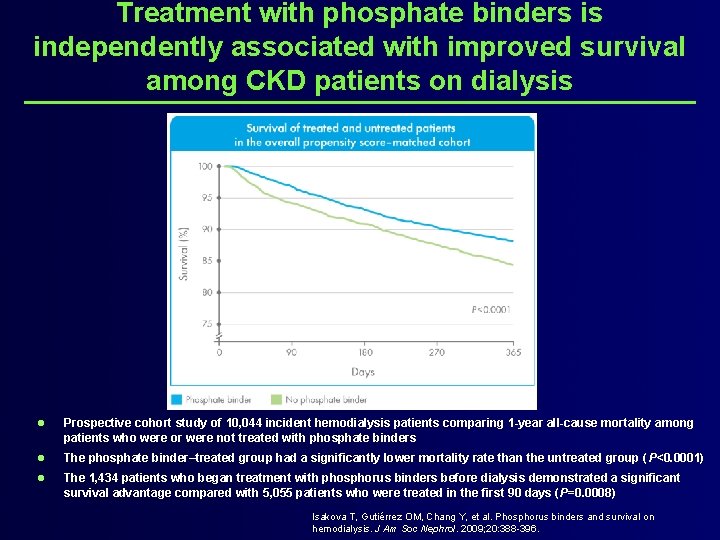
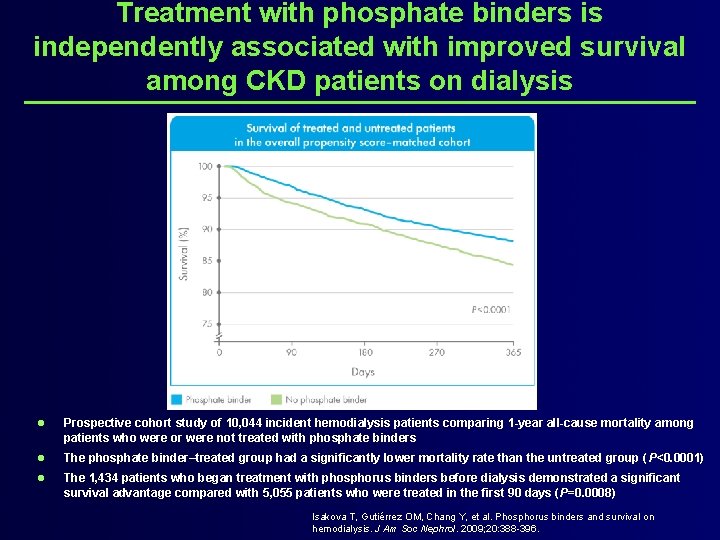
Treatment with phosphate binders is independently associated with improved survival among CKD patients on dialysis l Prospective cohort study of 10, 044 incident hemodialysis patients comparing 1 -year all-cause mortality among patients who were or were not treated with phosphate binders l The phosphate binder–treated group had a significantly lower mortality rate than the untreated group ( P<0. 0001) l The 1, 434 patients who began treatment with phosphorus binders before dialysis demonstrated a significant survival advantage compared with 5, 055 patients who were treated in the first 90 days (P=0. 0008) Isakova T, Gutiérrez OM, Chang Y, et al. Phosphorus binders and survival on hemodialysis. J Am Soc Nephrol. 2009; 20: 388 -396.
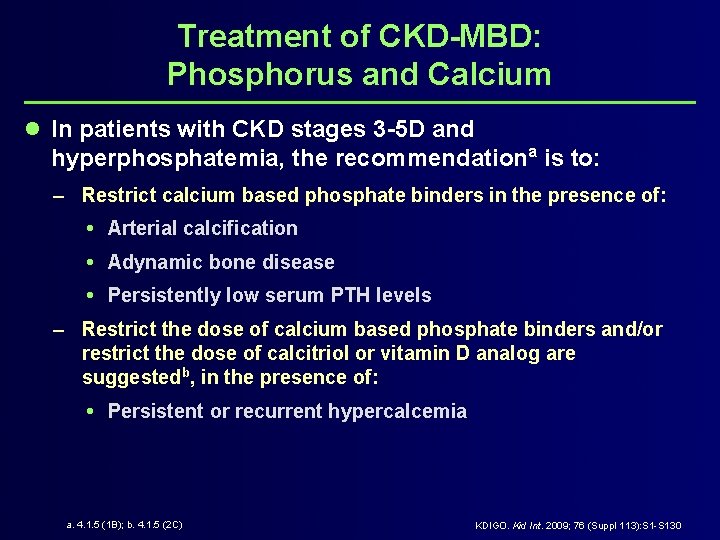
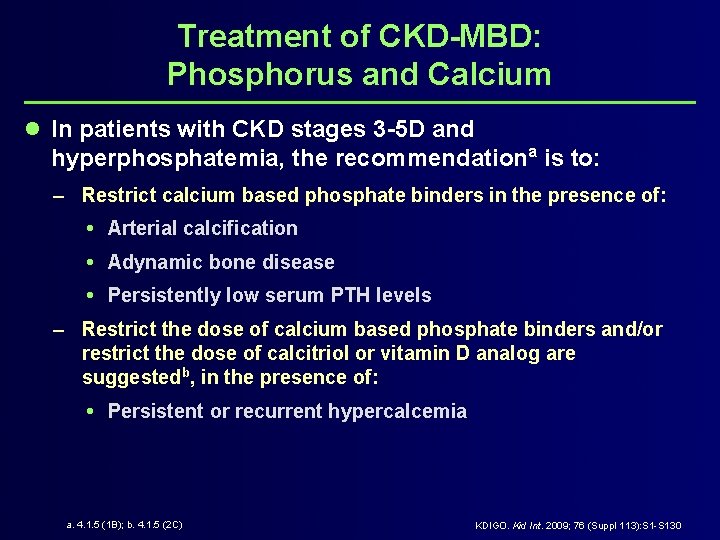
Treatment of CKD-MBD: Phosphorus and Calcium l In patients with CKD stages 3 -5 D and hyperphosphatemia, the recommendationa is to: – Restrict calcium based phosphate binders in the presence of: Arterial calcification Adynamic bone disease Persistently low serum PTH levels – Restrict the dose of calcium based phosphate binders and/or restrict the dose of calcitriol or vitamin D analog are suggestedb, in the presence of: Persistent or recurrent hypercalcemia a. 4. 1. 5 (1 B); b. 4. 1. 5 (2 C) KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
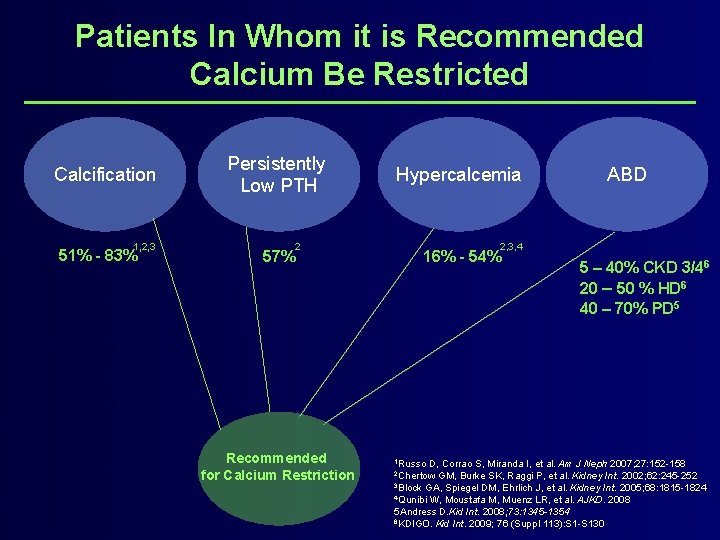
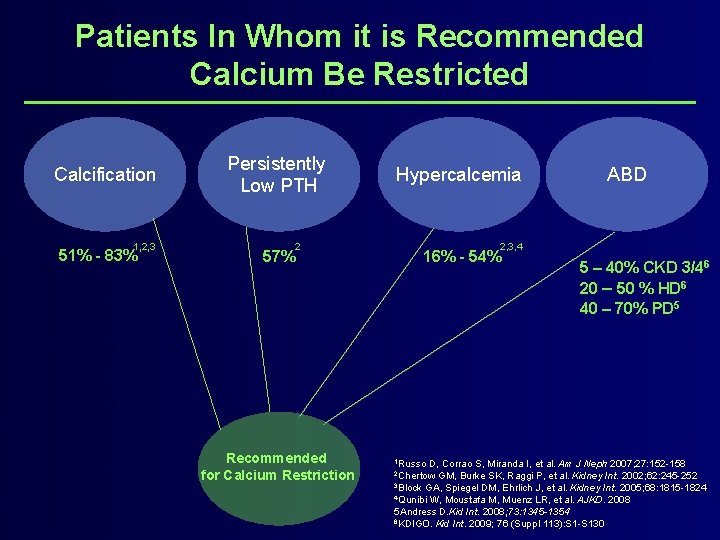
Patients In Whom it is Recommended Calcium Be Restricted Calcification 1, 2, 3 51% - 83% Persistently Low PTH 57% 2 Recommended for Calcium Restriction Hypercalcemia ABD 2, 3, 4 16% - 54% 1 Russo 5 – 40% CKD 3/46 20 – 50 % HD 6 40 – 70% PD 5 D, Corrao S, Miranda I, et al. Am J Neph 2007; 27: 152 -158 GM, Burke SK, Raggi P, et al. Kidney Int. 2002; 62: 245 -252 3 Block GA, Spiegel DM, Ehrlich J, et al. Kidney Int. 2005; 68: 1815 -1824 4 Qunibi W, Moustafa M, Muenz LR, et al. AJKD. 2008 5 Andress D. Kid Int. 2008; 73: 1345 -1354 6 KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130 2 Chertow
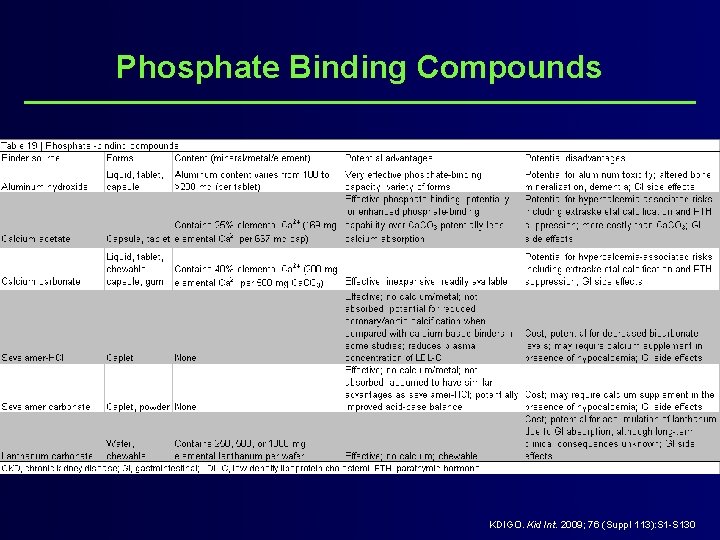
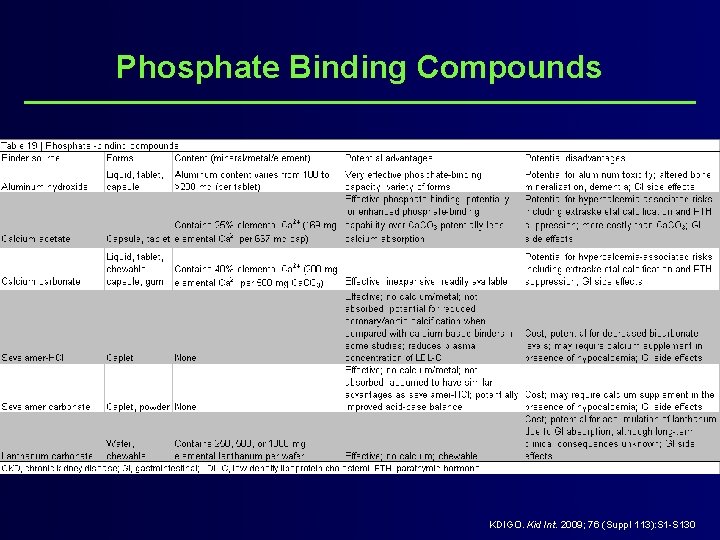
Phosphate Binding Compounds KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
PTH Levels
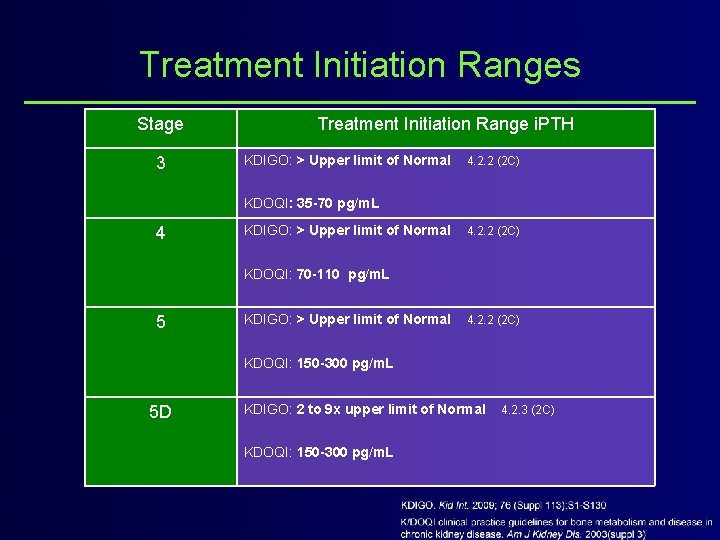
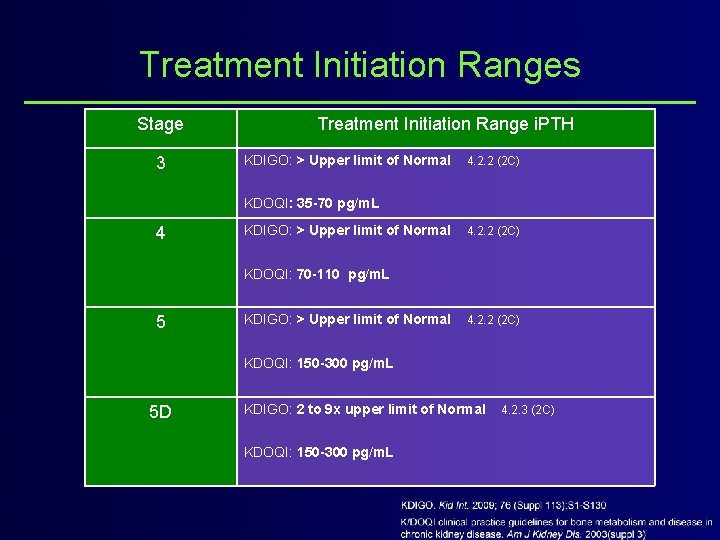
Treatment Initiation Ranges Stage 3 Treatment Initiation Range i. PTH KDIGO: > Upper limit of Normal 4. 2. 2 (2 C) KDOQI: 35 -70 pg/m. L 4 KDIGO: > Upper limit of Normal 4. 2. 2 (2 C) KDOQI: 70 -110 pg/m. L 5 KDIGO: > Upper limit of Normal 4. 2. 2 (2 C) KDOQI: 150 -300 pg/m. L 5 D KDIGO: 2 to 9 x upper limit of Normal KDOQI: 150 -300 pg/m. L 4. 2. 3 (2 C)
Treatment of Abnormal PTH levels in CKD-MBD l In patients with CKD stages 3 -5 not on dialysis, the optimal PTH level is unknown l In patients with levels of intact PTH (i. PTH) above the upper normal limit of the assay, the suggestiona is to, first evaluate for: – Hyperphosphatemia – Hypocalcemia – Vitamin D deficiency l It is reasonable to correct these abnormalities with any or all of the followingb: – Reducing dietary phosphate intake and administering phosphate binders, calcium supplements, and/or native vitamin D l The suggestionc is to treat with calcitriol or vitamin D analogs if: – Serum PTH is progressively rising and remains persistently above the upper limit of normal for the assay despite correction of modifiable factors a. 4. 2. 1 (2 C); b. 4. 2. 1 (not graded); c. 4. 2. 2 (2 C) KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
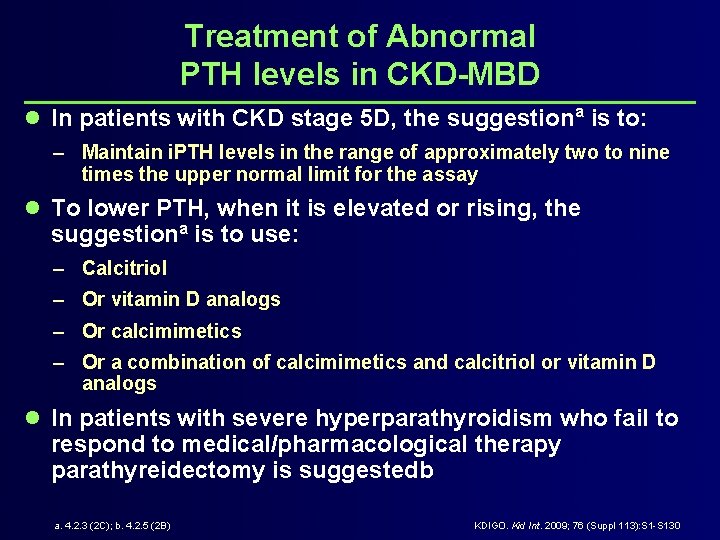
Treatment of Abnormal PTH levels in CKD-MBD l In patients with CKD stage 5 D, the suggestiona is to: – Maintain i. PTH levels in the range of approximately two to nine times the upper normal limit for the assay l To lower PTH, when it is elevated or rising, the suggestiona is to use: – Calcitriol – Or vitamin D analogs – Or calcimimetics – Or a combination of calcimimetics and calcitriol or vitamin D analogs l In patients with severe hyperparathyroidism who fail to respond to medical/pharmacological therapy parathyreidectomy is suggestedb a. 4. 2. 3 (2 C); b. 4. 2. 5 (2 B) KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
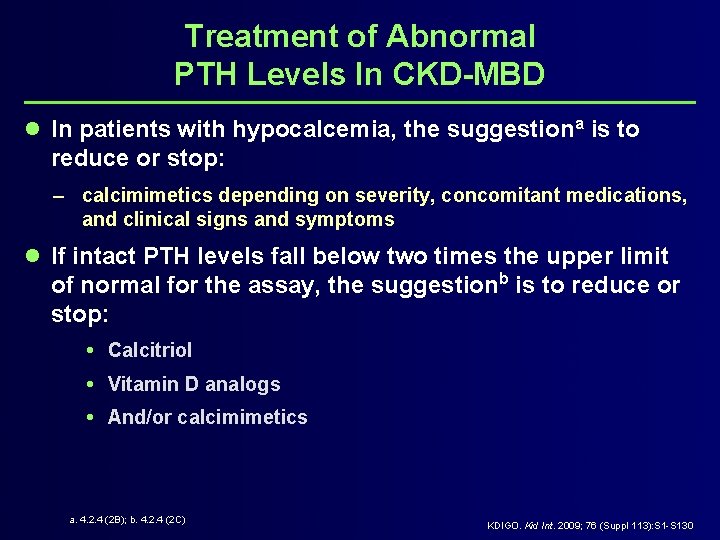
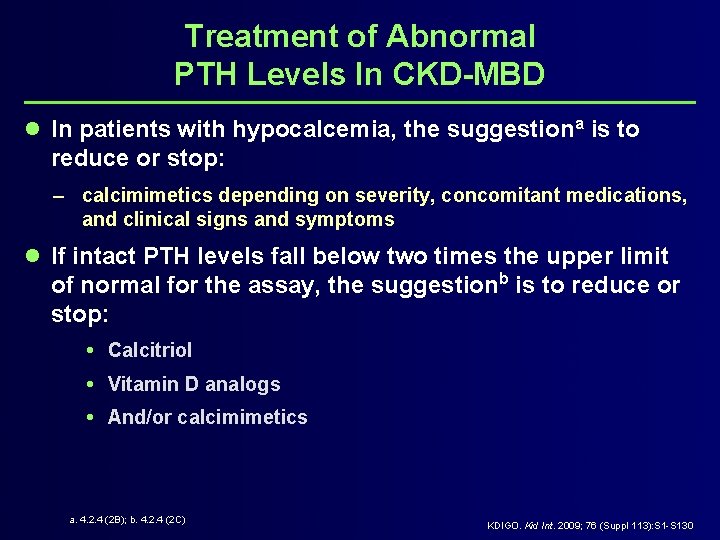
Treatment of Abnormal PTH Levels In CKD-MBD l In patients with hypocalcemia, the suggestiona is to reduce or stop: – calcimimetics depending on severity, concomitant medications, and clinical signs and symptoms l If intact PTH levels fall below two times the upper limit of normal for the assay, the suggestionb is to reduce or stop: Calcitriol Vitamin D analogs And/or calcimimetics a. 4. 2. 4 (2 B); b. 4. 2. 4 (2 C) KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130
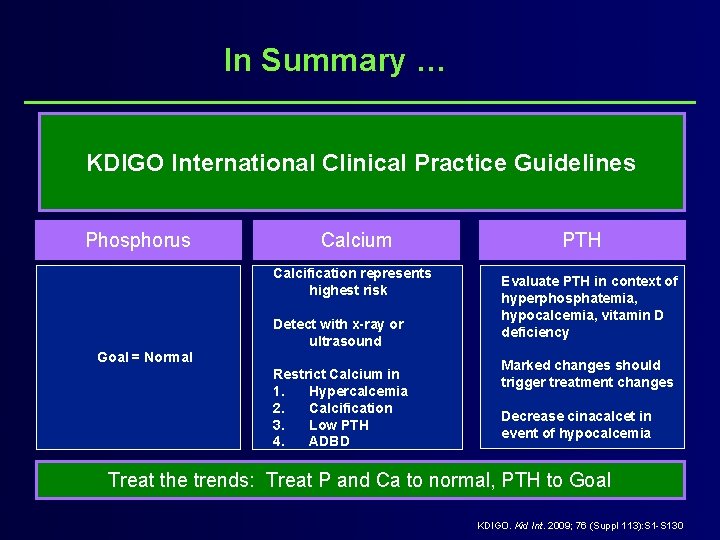
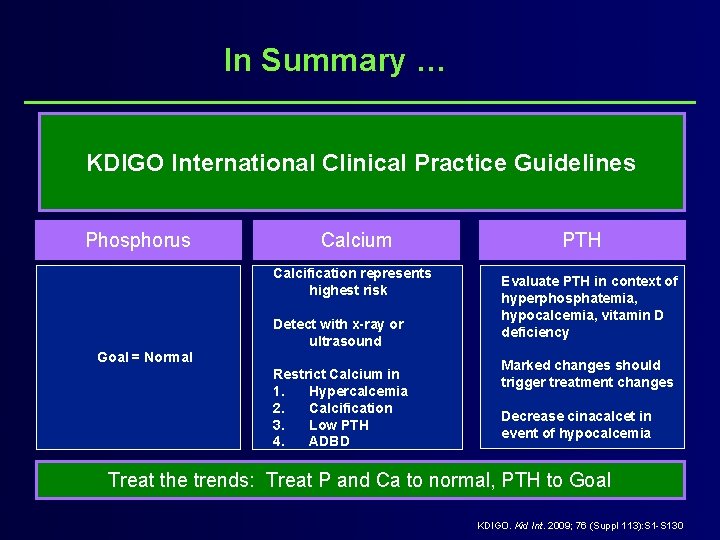
In Summary … KDIGO International Clinical Practice Guidelines Phosphorus Calcium Calcification represents highest risk Detect with x-ray or ultrasound Goal = Normal Restrict Calcium in 1. Hypercalcemia 2. Calcification 3. Low PTH 4. ADBD PTH Evaluate PTH in context of hyperphosphatemia, hypocalcemia, vitamin D deficiency Marked changes should trigger treatment changes Decrease cinacalcet in event of hypocalcemia Treat the trends: Treat P and Ca to normal, PTH to Goal KDIGO. Kid Int. 2009; 76 (Suppl 113): S 1 -S 130