Introduction to Contraception Anita Jaynes CNM MS University















- Slides: 69
Introduction to Contraception Anita Jaynes, CNM, MS University of Nebraska Medical Center Obstetrics & Gynecology
3, 000 unintended pregnancies occur in the U. S. each year. 50% of U. S. pregnancies are unintended.
Women’s Reproductive Life Scan The reproductive years are defined as ages 15 -44. Of the 39 years spent in the reproductive stages of life, women spend an average of 20 years trying to avoid pregnancy.

Who needs contraception? Every reproductive-age woman who is at risk for “sperm exposure” and who does not currently desire pregnancy.
Who does not need contraception? women who self-identify as lesbian celibate women who do not want contraception − for any reason! women who desire pregnancy
Don’t be an ass! Don’t ASSume anything − ASK! “Do you need contraception? ” not “What kind of birth control do you use?
What is the “best” contraceptive method? • The best contraceptive method for an individual woman is a method that is: – medically appropriate – effective in preventing pregnancy – used consistently and correctly – satisfactory to the woman at her stage of life
Life Stage: Menarche to First Intercourse • Fertility goals: – postpone pregnancy – preserve future fertility • Sexual behavior: – no intercourse yet – possibly experimenting with kissing, petting, etc. • Contraceptive need: – education
Life Stage: First Intercourse to First Birth • Fertility goals: – postpone pregnancy – preserve future fertility • Sexual behavior: – ? multiple partners – frequent intercourse – spontaneous, unpredictable intercourse • Contraceptive needs: – – efficacy reversibility not coitus-linked STI prevention
Life Stage: First Birth to Last Pregnancy • Fertility goals: – space pregnancies – preserve future fertility • Sexual behavior: – one partner (? ) – moderate to low frequency of intercourse – predictable intercourse • Contraceptive needs: – – efficacy reversibility ? OK if coitus-linked ? need for STI prevention
Life Stage: Last Birth to Menopause • Fertility goals: – no further pregnancies – no need to preserve fertility • Sexual behavior: – one partner (? ) – low to moderate frequency of intercourse – predictable intercourse • Contraceptive needs: – – efficacy may be irreversible ? OK if coitus-linked ? need for STI prevention
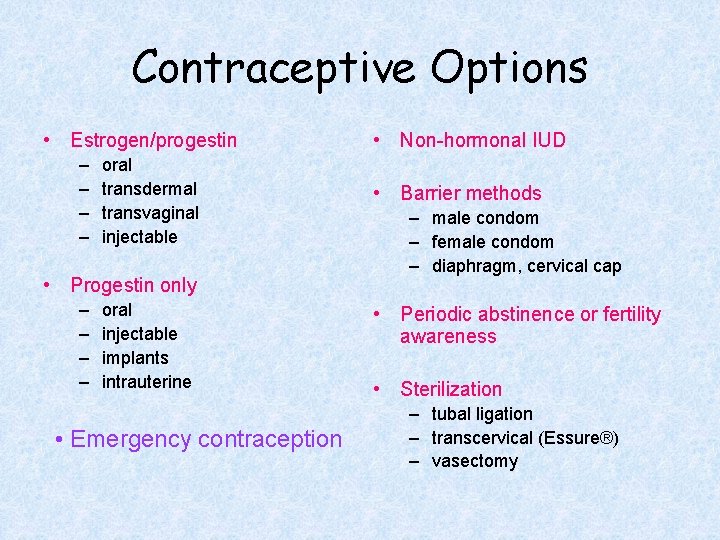
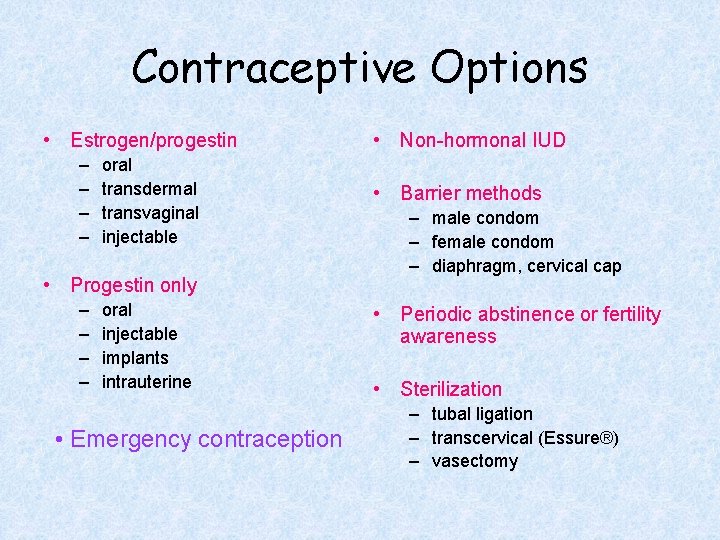
Contraceptive Options • Estrogen/progestin – – oral transdermal transvaginal injectable • Progestin only – – oral injectable implants intrauterine • Emergency contraception • Non-hormonal IUD • Barrier methods – male condom – female condom – diaphragm, cervical cap • Periodic abstinence or fertility awareness • Sterilization – tubal ligation – transcervical (Essure®) – vasectomy
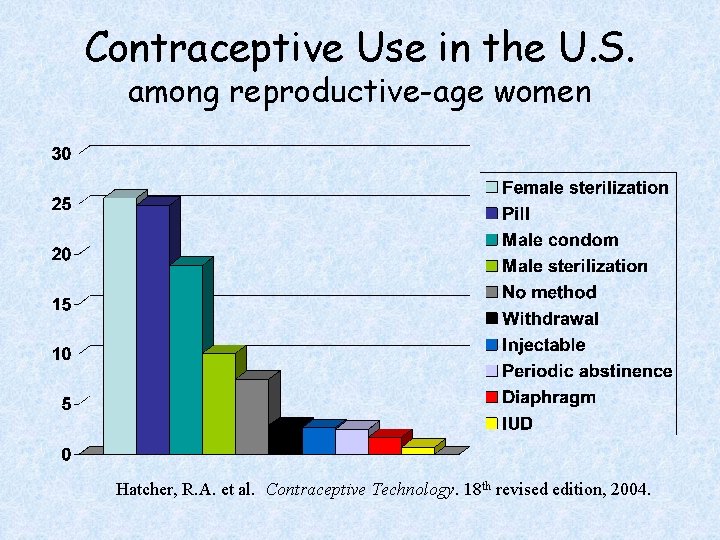
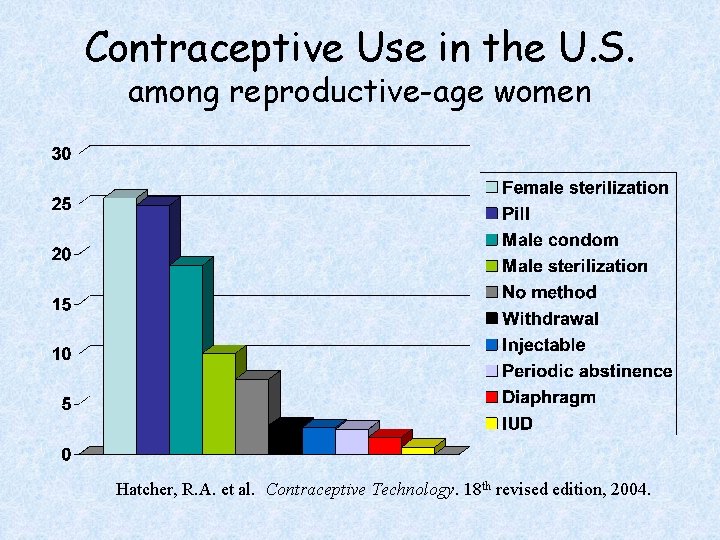
Contraceptive Use in the U. S. among reproductive-age women Hatcher, R. A. et al. Contraceptive Technology. 18 th revised edition, 2004.

Contraceptive Considerations • Effectiveness • Frequency of intercourse • Sexual behavior • Desire for future fertility • Cost of method • Side effects • Contraindications • Noncontraceptive benefits • Patient’s perceptions and misconceptions • Patient’s health status and medical conditions
“The great question that has never been answered, and which I have not yet been able to answer, despite my thirty years of research into the feminine soul, is ‘What does a woman want? ’” − Sigmund Freud What does a woman want from a contraceptive? • Is it safe? • Does it work? • Will my partner accept it? • Can I afford it? And some women will ask − • Does it cause an abortion?

Is it safe? Voluntary risks in perspective ACTIVITY YEAR CHANCE OF DEATH IN A Motorcycling 1 in 1, 000 Automobile driving 1 in 5, 900 Playing football 1 in 25, 000 Canoeing 1 in 100, 000 Age < 35, nonsmoker, OCP use 1 in 200, 000 IUD use 1 in 10, 000 Laparoscopic tubal ligation 1 in 38, 500 Vasectomy 1 in 1, 000
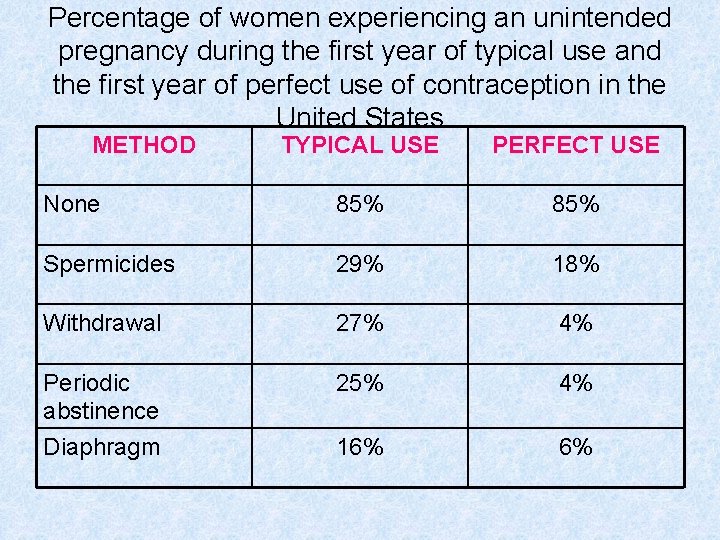
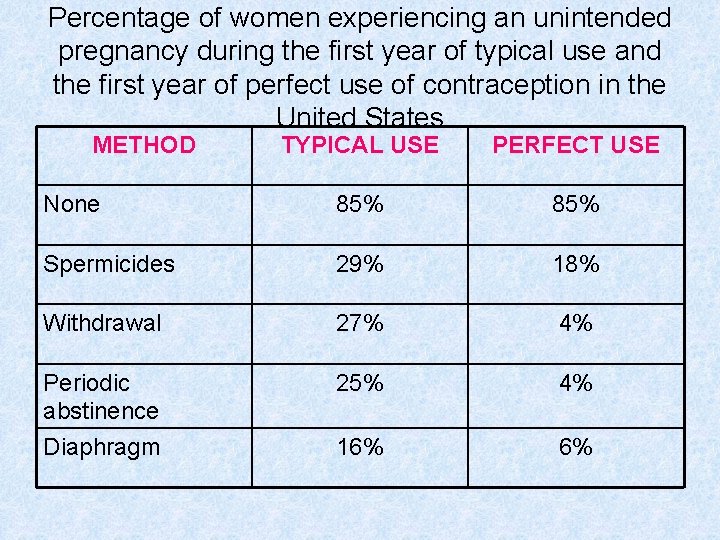
Percentage of women experiencing an unintended pregnancy during the first year of typical use and the first year of perfect use of contraception in the United States METHOD TYPICAL USE PERFECT USE None 85% Spermicides 29% 18% Withdrawal 27% 4% Periodic abstinence Diaphragm 25% 4% 16% 6%
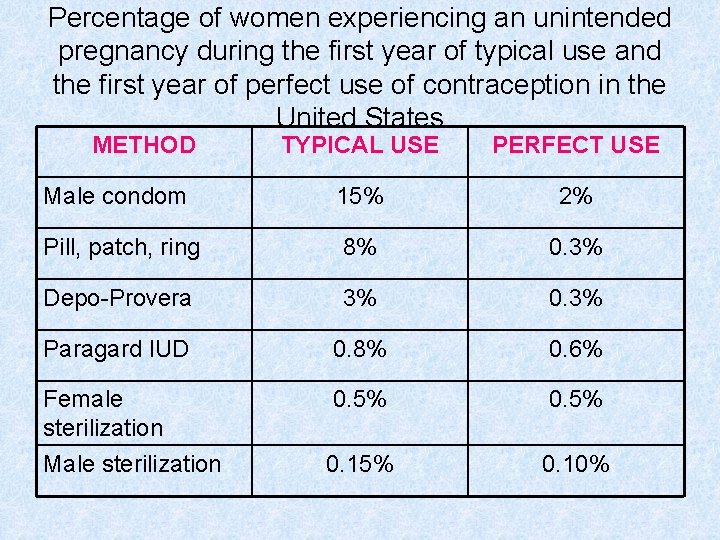
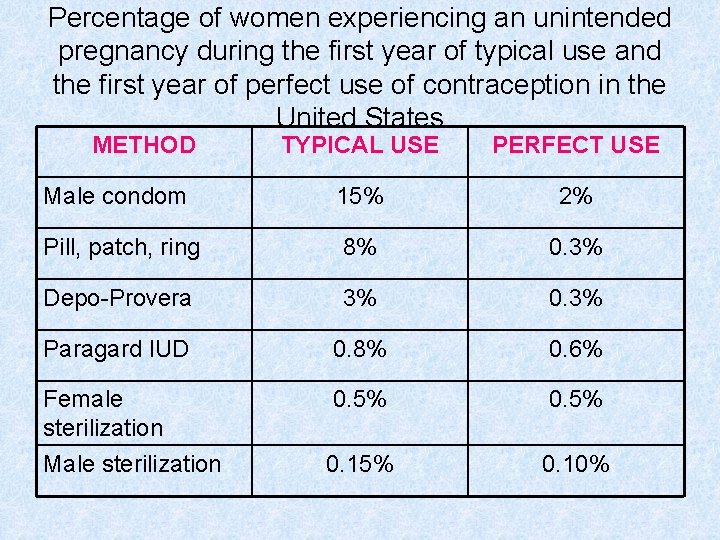
Percentage of women experiencing an unintended pregnancy during the first year of typical use and the first year of perfect use of contraception in the United States METHOD TYPICAL USE PERFECT USE Male condom 15% 2% Pill, patch, ring 8% 0. 3% Depo-Provera 3% 0. 3% Paragard IUD 0. 8% 0. 6% Female sterilization Male sterilization 0. 5% 0. 15% 0. 10%

Combination Contraceptives (Estrogen & Progestin)
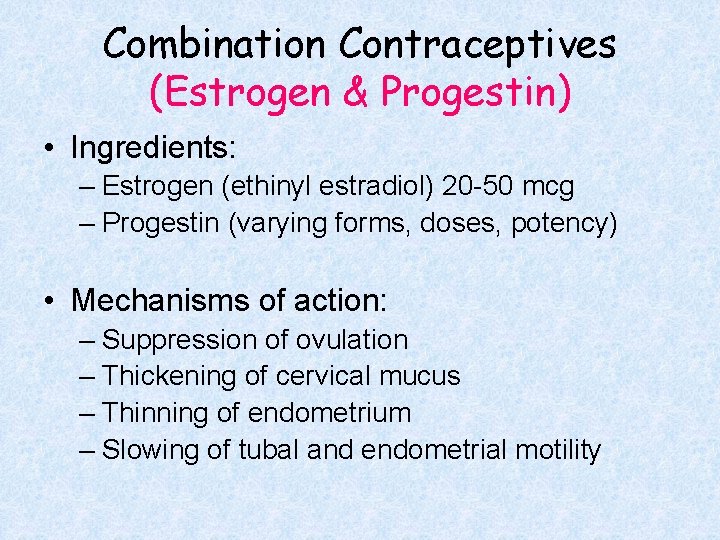
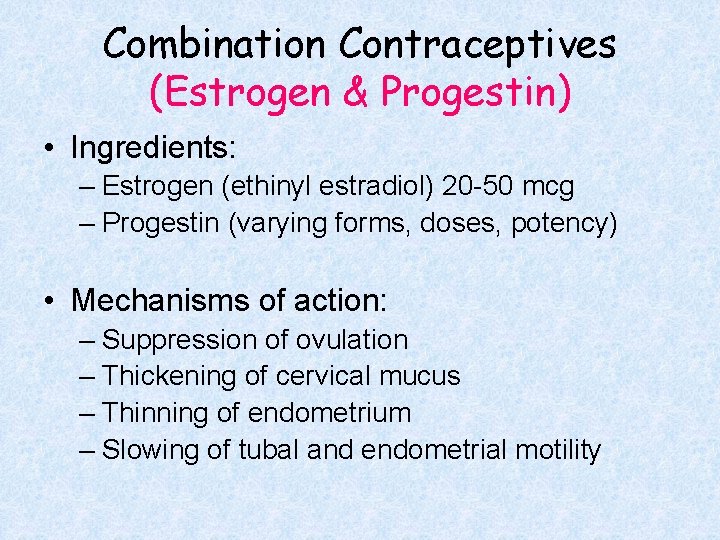
Combination Contraceptives (Estrogen & Progestin) • Ingredients: – Estrogen (ethinyl estradiol) 20 -50 mcg – Progestin (varying forms, doses, potency) • Mechanisms of action: – Suppression of ovulation – Thickening of cervical mucus – Thinning of endometrium – Slowing of tubal and endometrial motility
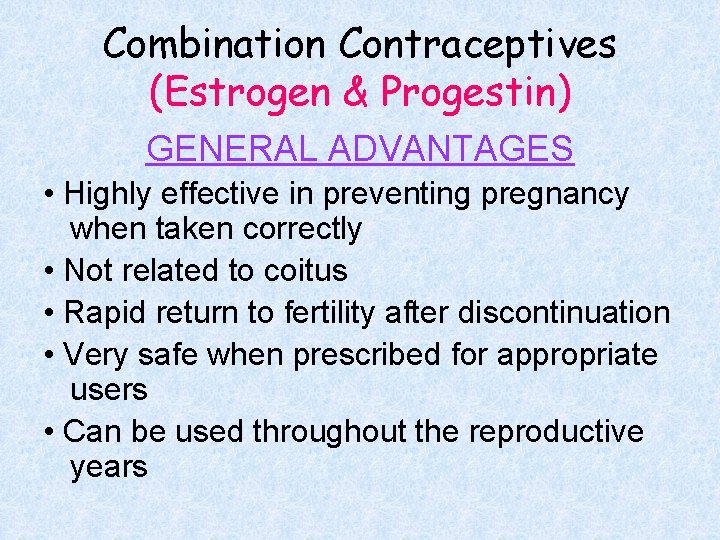
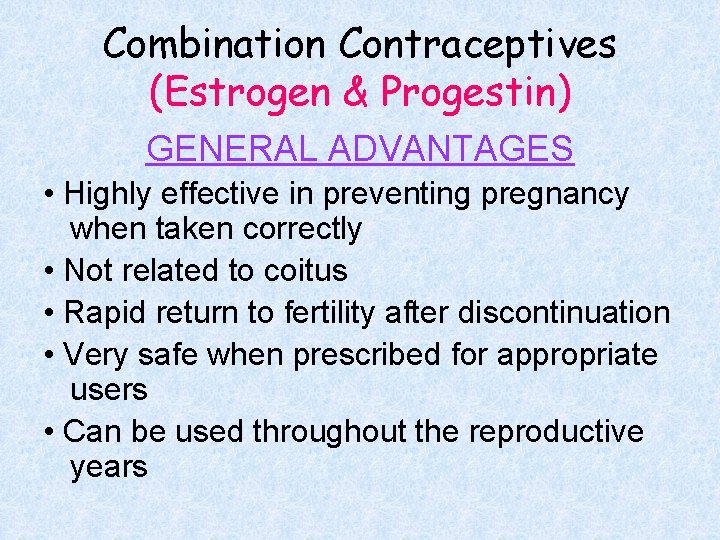
Combination Contraceptives (Estrogen & Progestin) GENERAL ADVANTAGES • Highly effective in preventing pregnancy when taken correctly • Not related to coitus • Rapid return to fertility after discontinuation • Very safe when prescribed for appropriate users • Can be used throughout the reproductive years
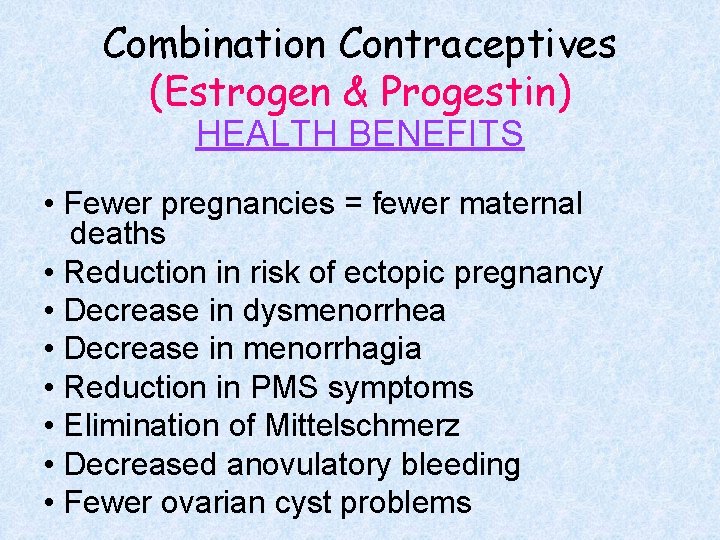
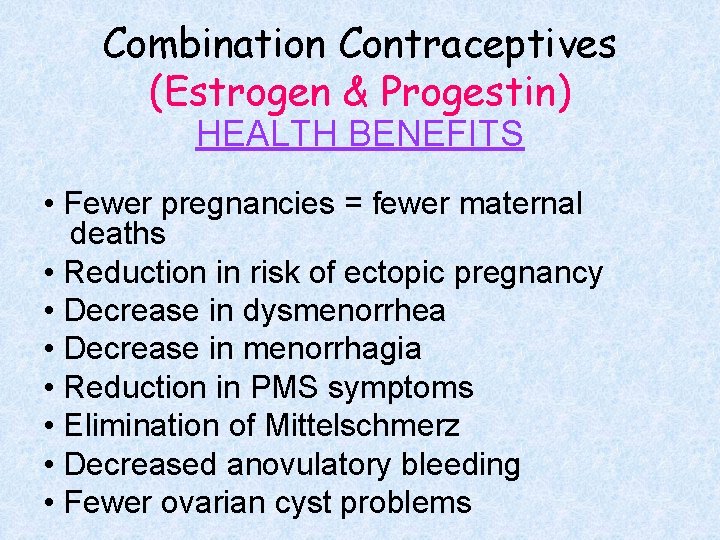
Combination Contraceptives (Estrogen & Progestin) HEALTH BENEFITS • Fewer pregnancies = fewer maternal deaths • Reduction in risk of ectopic pregnancy • Decrease in dysmenorrhea • Decrease in menorrhagia • Reduction in PMS symptoms • Elimination of Mittelschmerz • Decreased anovulatory bleeding • Fewer ovarian cyst problems
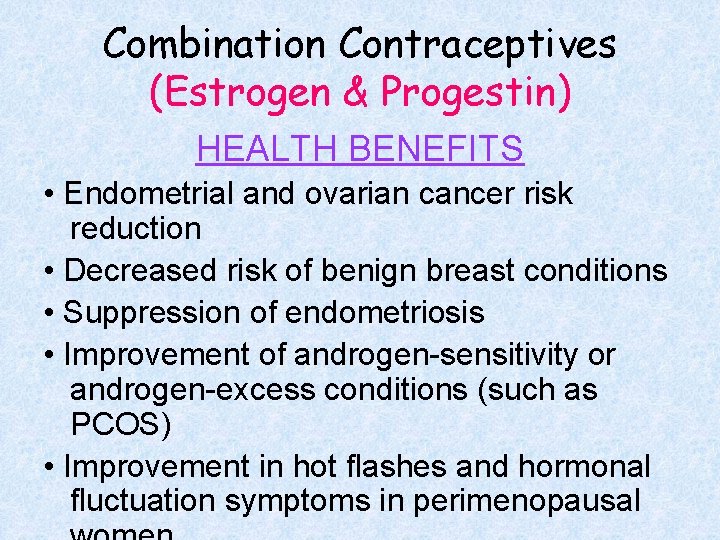
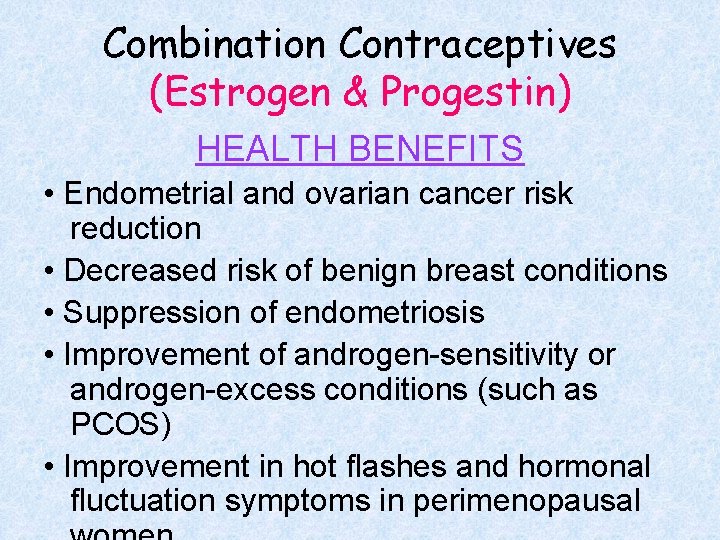
Combination Contraceptives (Estrogen & Progestin) HEALTH BENEFITS • Endometrial and ovarian cancer risk reduction • Decreased risk of benign breast conditions • Suppression of endometriosis • Improvement of androgen-sensitivity or androgen-excess conditions (such as PCOS) • Improvement in hot flashes and hormonal fluctuation symptoms in perimenopausal
Combination Contraceptives (Estrogen & Progestin) GENERAL DISADVANTAGES • Must be taken consistently and correctly to be effective • Storage, access, lack of privacy • Can interfere with lactation • No protection against STIs • Common side effects include: nausea, vomiting weight gain decreased libido headaches breast tenderness skin hyperpigmentation
Combination Contraceptives (Estrogen & Progestin) COMPLICATIONS • Venous thromboembolism • Myocardial infarction and stroke • Hypertension DO NOT Rx TO WOMEN AGE > 35 WHO SMOKE!
Combination Contraceptives (Estrogen & Progestin) CONTRAINDICATIONS • Personal history of thrombosis; known clotting disorder (factor V Leiden mutation, etc. ) • Personal history of stroke or MI • Labile hypertension • Estrogen-sensitive malignancy (such as breast CA) • Active liver disease • Migraines with focal neurologic symptoms

How to Take Birth Control Pills The 28 -day pack contains 21 active pills + 7 placebo pills. Getting started: • “First day” start • Sunday start • “Quick Start” Continuing: one pill per day, every day. Withdrawal bleeding will occur during the placebo week. ≈ $35. 00 per cycle
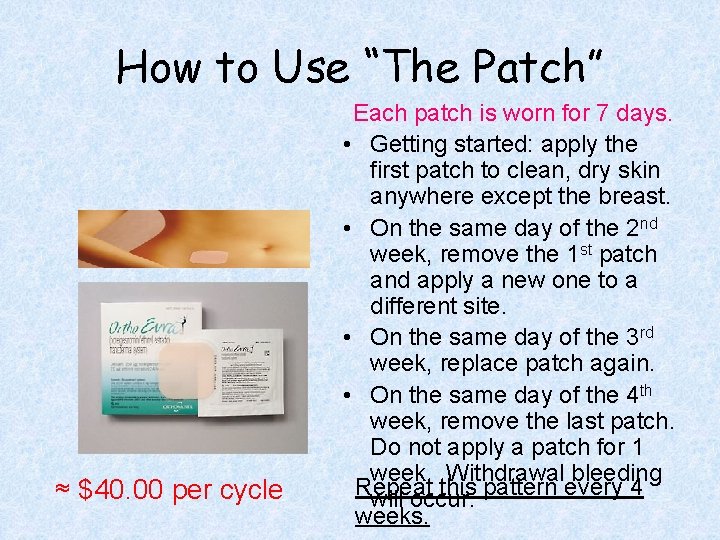
How to Use “The Patch” ≈ $40. 00 per cycle Each patch is worn for 7 days. • Getting started: apply the first patch to clean, dry skin anywhere except the breast. • On the same day of the 2 nd week, remove the 1 st patch and apply a new one to a different site. • On the same day of the 3 rd week, replace patch again. • On the same day of the 4 th week, remove the last patch. Do not apply a patch for 1 week. Withdrawal bleeding Repeat this pattern every 4 will occur. weeks.
How to Use “The Ring” • Getting started: squeeze the ring between your thumb and index finger. Insert it in the vagina. • Leave the ring in place for 21 days (3 weeks). • At the end of the 21 days, remove the ring by inserting a finger in the vagina and pulling it out. • Discard the ring and wait 7 days. Withdrawal bleeding will occur. • Repeat the pattern (3 ≈ $40. 00 per cycle

“Extended Use” Regimens Monthly withdrawal bleeding is NOT necessary! Seasonale provides 84 active pills followed by 7 placebo pills for 4 “periods” a year. Any monophasic pill, the patch, or the ring can be used on an extended basis. ≈ $100. 00 per pack

Progestin-Only Contraceptives
Progestin-Only Contraceptives Mechanisms of action: • Inhibition of ovulation • Prevention of sperm penetration by thickening and decreasing the quantity of cervical mucus • Endometrial atrophy
Progestin-Only Contraceptives ADVANTAGES OF ALL METHODS • No estrogen • Reversible • Amenorrhea or scanty bleeding • Improvement in dysmenorrhea, menorrhagia, PMS, endometriosis symptoms • Decreased risk of endometrial or ovarian cancer • Decreased risk of PID • Compatible with breast-feeding
Progestin-Only Contraceptives DISADVANTAGES OF ALL METHODS • Menstrual cycle disturbances • Weight gain • Depression • Lack of protection against STIs
Progestin-Only Pills Cycle consists of 28 active pills; there is no “placebo week” Vulnerable efficacy! Each pill must be taken on time at 24 hour intervals. BRAND NAMES: Micronor Nor-QD Ovrette ≈ $45. 00 per cycle Compatible with breast-feeding & recommended in combination with lactational amenorrhea.
Depo-Provera Advantages: • highly effective • discreet & private • use not linked to coitus • requires user to “remember” only 4 times a year Disadvantages: • weight gain • impossible to discontinue immediately • delayed return to fertility • adverse effects on lipids • decreased bone mineral density Depo-Provera = depot medroxyprogesterone acetate 150 mg IM q 12 weeks

Progestin Implants áNorplant (off the market) Implanon FDA-approved & coming soon Advantages: • highly effective • eliminate “user error” • long-term • reversible Disadvantages: • high initial cost • insertion & removal require specialized training • cannot be easily discontinued
Intrauterine Devices (IUDs) GENERAL ADVANTAGES • highly effective, no “user error” • convenient • long-lasting • reversible • discreet • cost-effective in the long run • low incidence of side effects • independent of coitus
Intrauterine Devices (IUDs) GENERAL DISADVANTAGES: • menstrual problems • discomfort with insertion • expulsion of the device • perforation of the uterus • requires office visit with trained professional for insertion & removal • high initial cost • no protection from STIs
Intrauterine Devices (IUDs) MYTH: IUDs increase the risk of PID. FACT: IUDs have no effect on the risk of upper genital tract infection. STIs cause PID − IUDs do not. MYTH: IUDs cause abortions. FACT: IUDs prevent fertilization and thus are true contra-ceptives, not abortifacients. MYTH: IUDs increase the risk of ectopic pregnancy. FACT: IUDs reduce the risk of ectopic pregnancy because IUDs prevent all types of pregnancy. MYTH: Only parous women are IUD candidates. FACT: Nulliparous women are more likely to expel
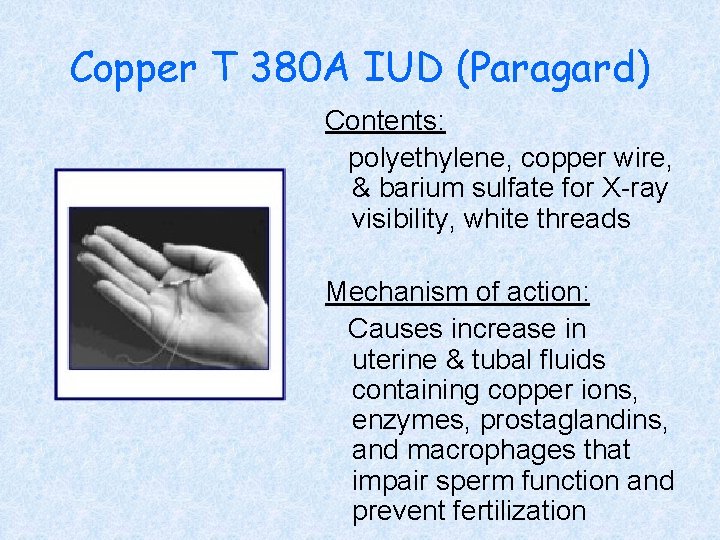
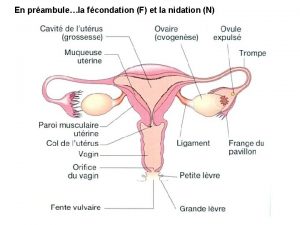
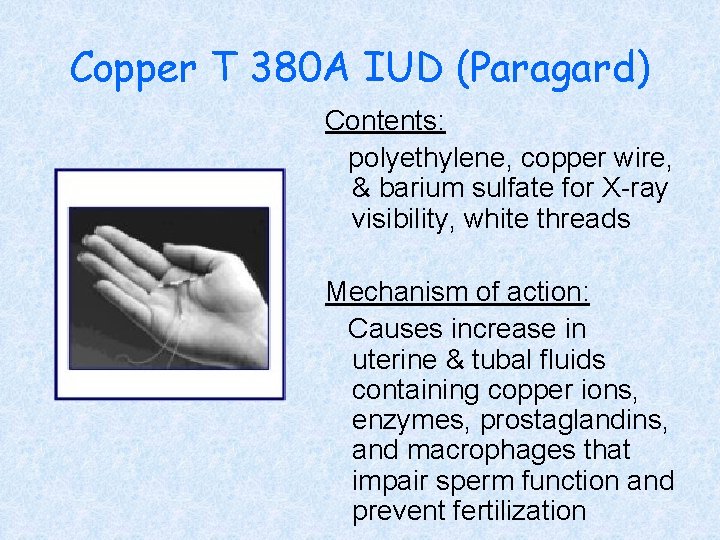
Copper T 380 A IUD (Paragard) Contents: polyethylene, copper wire, & barium sulfate for X-ray visibility, white threads Mechanism of action: Causes increase in uterine & tubal fluids containing copper ions, enzymes, prostaglandins, and macrophages that impair sperm function and prevent fertilization
Copper T 380 A IUD (Paragard) ADVANTAGES SPECIFIC TO THE Cu 380 A: • Can remain in place for up to 10 years • Nonhormonal • Normal menstrual pattern continues DISADVANTAGES SPECIFIC TO THE Cu 380 A: • Can cause heavier menses with more severe cramping, especially in the first few cycles
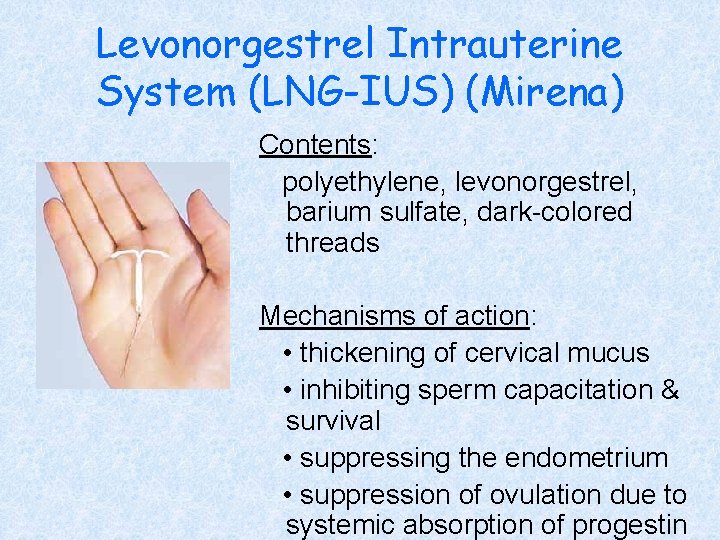
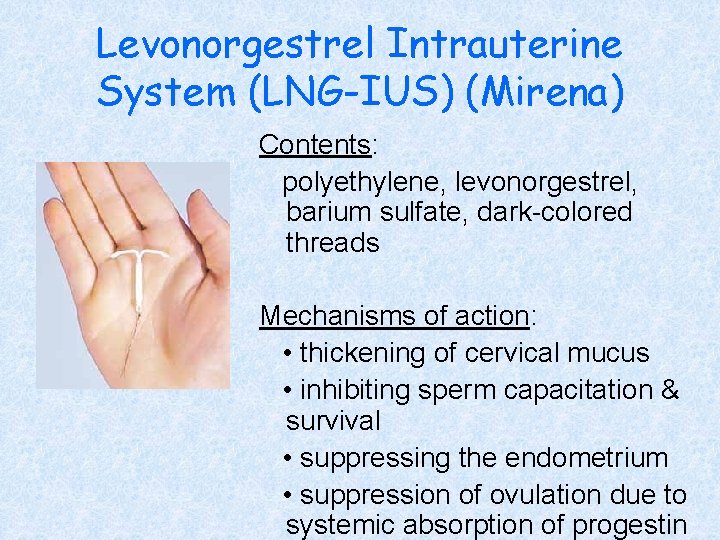
Levonorgestrel Intrauterine System (LNG-IUS) (Mirena) Contents: polyethylene, levonorgestrel, barium sulfate, dark-colored threads Mechanisms of action: • thickening of cervical mucus • inhibiting sperm capacitation & survival • suppressing the endometrium • suppression of ovulation due to systemic absorption of progestin
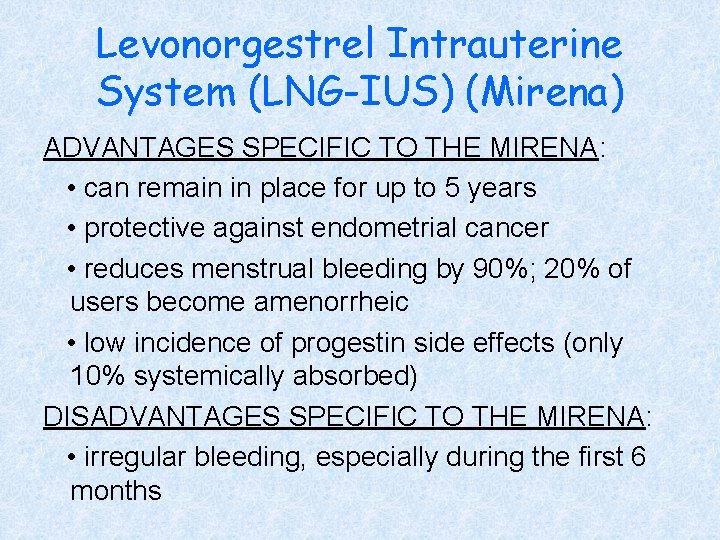
Levonorgestrel Intrauterine System (LNG-IUS) (Mirena) ADVANTAGES SPECIFIC TO THE MIRENA: • can remain in place for up to 5 years • protective against endometrial cancer • reduces menstrual bleeding by 90%; 20% of users become amenorrheic • low incidence of progestin side effects (only 10% systemically absorbed) DISADVANTAGES SPECIFIC TO THE MIRENA: • irregular bleeding, especially during the first 6 months
Barrier Methods
Male Condoms Mechanism of action: acts as a physical barrier; prevents pregnancy by blocking passage of semen Types available: • latex (natural rubber) • natural membrane (lamb intestine) • polyurethane • spermicidal 50¢-$1. 00 each
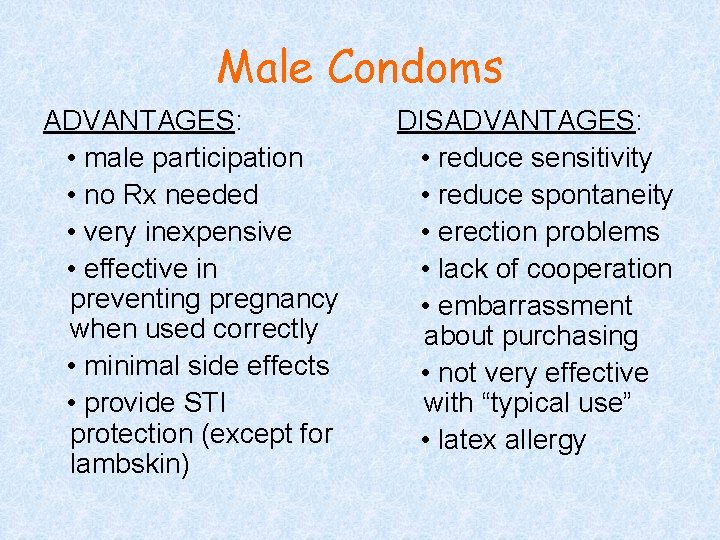
Male Condoms ADVANTAGES: • male participation • no Rx needed • very inexpensive • effective in preventing pregnancy when used correctly • minimal side effects • provide STI protection (except for lambskin) DISADVANTAGES: • reduce sensitivity • reduce spontaneity • erection problems • lack of cooperation • embarrassment about purchasing • not very effective with “typical use” • latex allergy

Male Condoms FAILURE RATES: perfect use 2% typical use 15% MINIMIZING USER ERROR • Use with every act of intercourse • Use “from start to finish” • Unroll condom onto penis (do not unroll first; do not test by filling with air or water first) • Hold rim during withdrawal to prevent slippage or leakage • Have several condoms available

Female Condoms • No Rx needed • One-time use • Includes a lubricant • Spermicide not recommended • Can be inserted up to 8 hours prior to intercourse; can remain in place for up to 8 hours • Protects against STIs • Failure rates: perfect use 5% typical use 21% ≈ $3. 50 each

Diaphragms & Cervical Caps Mechanism of action: • physical barrier to prevent sperm from reaching the cervix • chemical to kill sperm (spermicide) Advantages: • no hormones • virtually no side effects Disadvantages: • require professional fitting • require user skill and commitment
Spermicides Mechanism of action: Nonoxynol-9 is a surfactant that destroys the sperm cell membrane. Advantages: • available without Rx • easy to use, can use FAILURE RATES intermittently without (when used alone) advance planning perfect use 18% Disadvantages: typical use 29% • no protection against STIs • frequent (> 2 x/day) use may $10 -15 per package
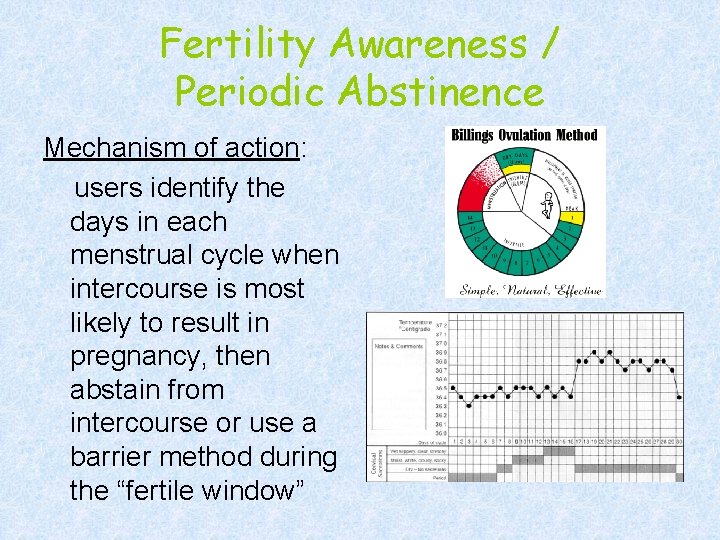
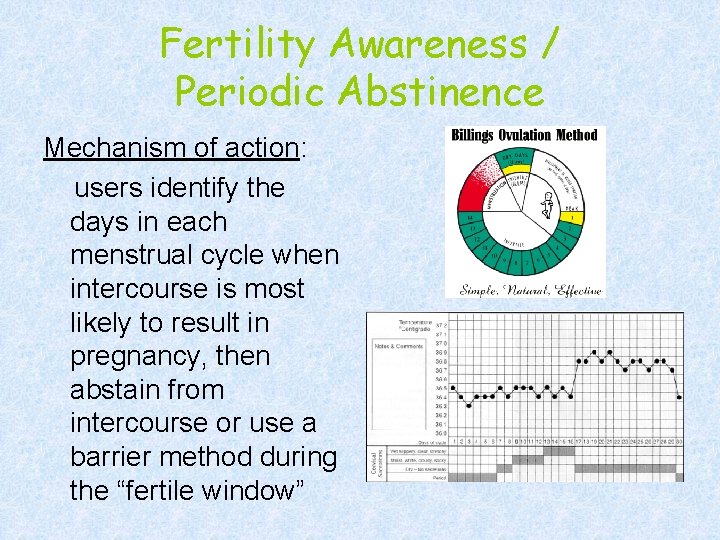
Fertility Awareness / Periodic Abstinence Mechanism of action: users identify the days in each menstrual cycle when intercourse is most likely to result in pregnancy, then abstain from intercourse or use a barrier method during the “fertile window”
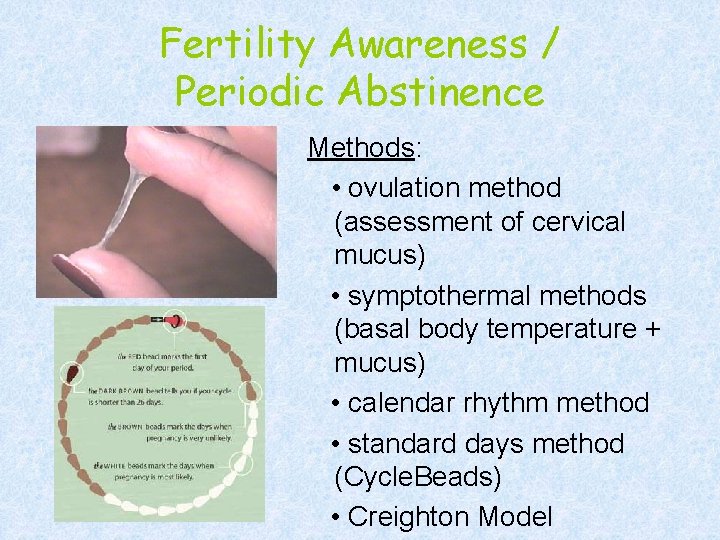
Fertility Awareness / Periodic Abstinence Methods: • ovulation method (assessment of cervical mucus) • symptothermal methods (basal body temperature + mucus) • calendar rhythm method • standard days method (Cycle. Beads) • Creighton Model

Fertility Awareness / Periodic Abstinence Advantages: • No hormones • No side effects • Enables a woman to understand her body’s cycles • Promotes cooperation between partners • Can also be used to achieve pregnancy or to identify infertility problems • The only method approved by the Catholic Church Disadvantages: • Methods require varying amounts of training & cost • Detracts from spontaneity, causes friction between partners if not in agreement • Difficult to use if: − recent childbirth − breastfeeding − recent menarche − approaching menopause − recent discontinuation of a hormonal method − irregular cycles − unable to interpret fertility
Sterilization is chosen by 39% of couples who use contraception in the U. S. 28% of reproductive age women undergo tubal ligation and 10% of men undergo vasectomy.
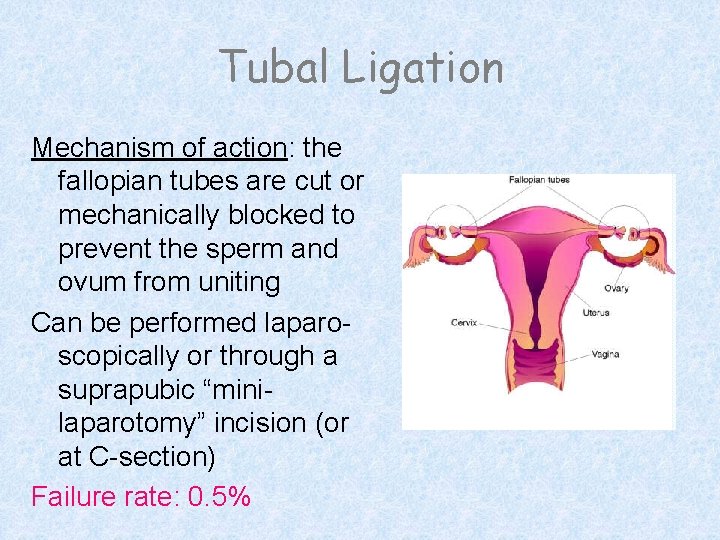
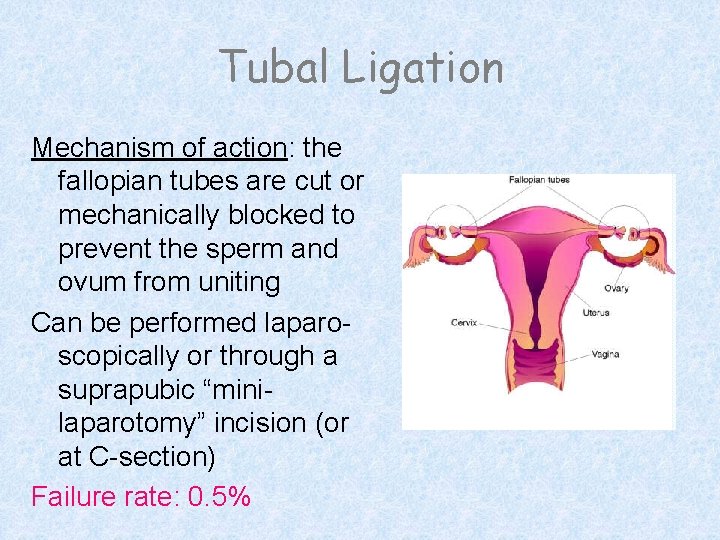
Tubal Ligation Mechanism of action: the fallopian tubes are cut or mechanically blocked to prevent the sperm and ovum from uniting Can be performed laparoscopically or through a suprapubic “minilaparotomy” incision (or at C-section) Failure rate: 0. 5%
Tubal Ligation Advantages: • permanent • highly effective • safe • quick recovery • lack of significant longterm side effects • cost effective • partner cooperation not required • not coitus-linked Disadvantages: • possibility of patient regret • difficult to reverse • future pregnancy could require assistive reproductive tech-nology (such as IVF) • more expensive than vasectomy

Transcervical Sterilization Essure™ Mechanism of Action: Using a hysteroscopic approach, one Essure micro-insert is placed in the proximal section of each fallopian tube lumen. The micro-insert expands upon release, acutely anchoring itself in the fallopian tube. The micro-insert subsequently elicits a benign tissue response. Tissue in-growth into the micro -insert anchors the device and occludes the fallopian tube, resulting in sterilization. FAILURE RATE: 0. 2% after 3 years

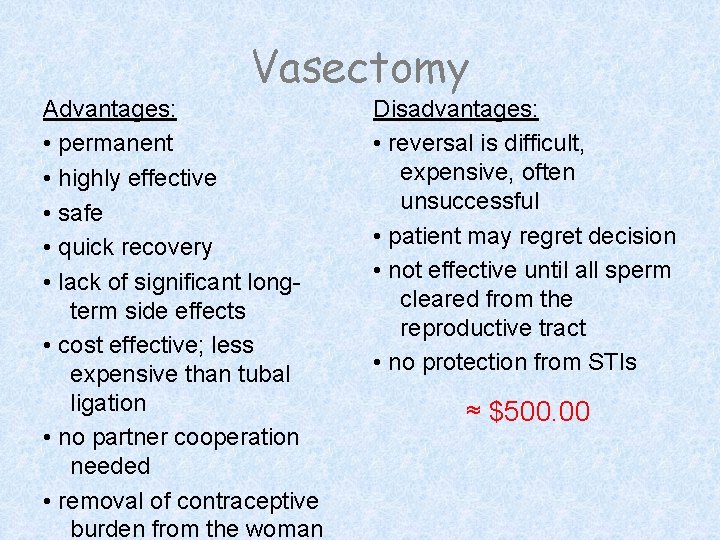
Vasectomy Mechanism of action: each vas deferens is cut to prevent the passage of sperm into the ejaculated seminal fluid FAILURE RATE: perfect use 0. 10% typical use 0. 15%
Vasectomy Advantages: • permanent • highly effective • safe • quick recovery • lack of significant longterm side effects • cost effective; less expensive than tubal ligation • no partner cooperation needed • removal of contraceptive burden from the woman Disadvantages: • reversal is difficult, expensive, often unsuccessful • patient may regret decision • not effective until all sperm cleared from the reproductive tract • no protection from STIs ≈ $500. 00
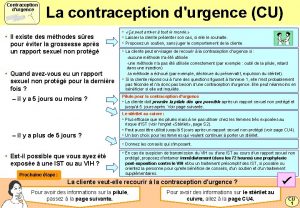
Emergency Contraception Definition: emergency contraceptives are methods a woman can use after intercourse to prevent pregnancy Methods: • Plan B − the only dedicated product marketed specifically for emergency contraception • Off-label use of progestin-only contraceptive pills
Emergency Contraception Indications for use: • contraceptive failure (condom broke, pills forgotten) • error in withdrawal or periodic abstinence • rape • any unintended “sperm exposure” Contraindications: • EC pregnancy could prevent about ½ of unintended pregnancies − 1. 5 million pregnancies in the U. S. every year.
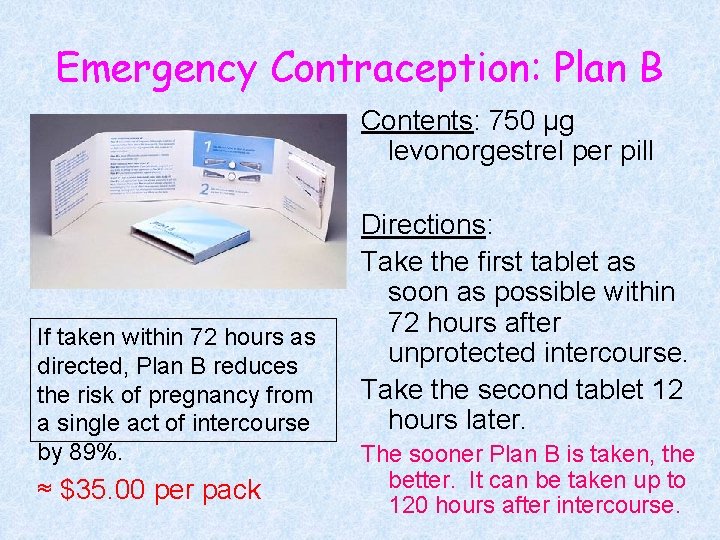
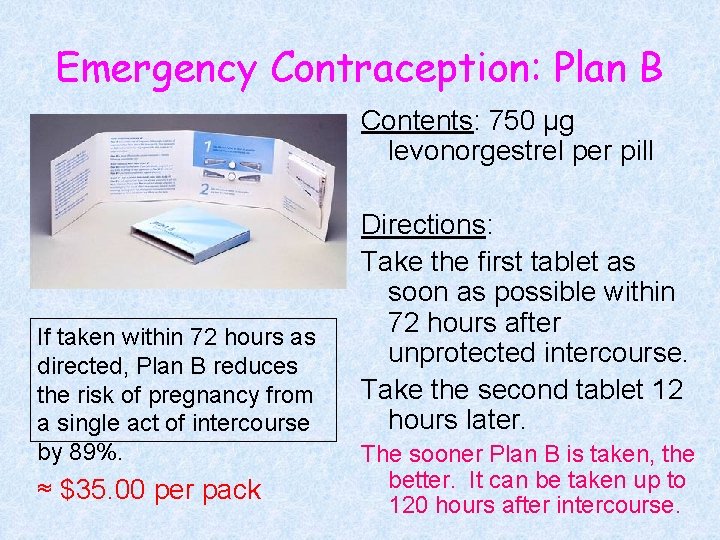
Emergency Contraception: Plan B Contents: 750 µg levonorgestrel per pill If taken within 72 hours as directed, Plan B reduces the risk of pregnancy from a single act of intercourse by 89%. ≈ $35. 00 per pack Directions: Take the first tablet as soon as possible within 72 hours after unprotected intercourse. Take the second tablet 12 hours later. The sooner Plan B is taken, the better. It can be taken up to 120 hours after intercourse.
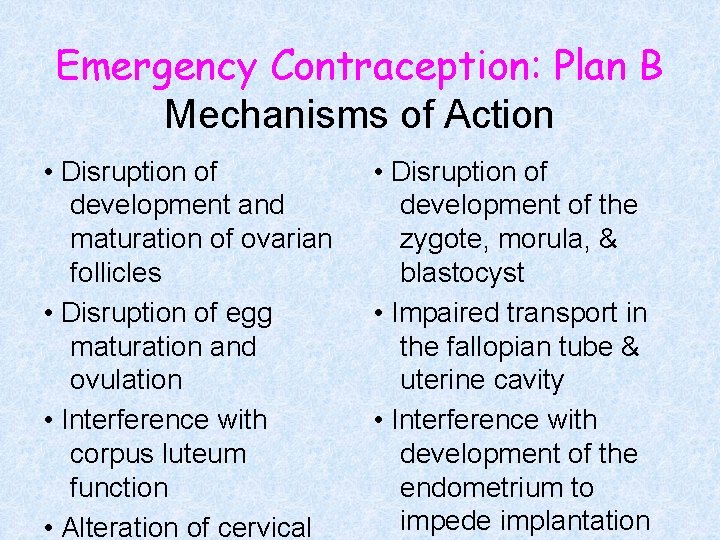
Emergency Contraception: Plan B Mechanisms of Action • Disruption of development and maturation of ovarian follicles • Disruption of egg maturation and ovulation • Interference with corpus luteum function • Alteration of cervical • Disruption of development of the zygote, morula, & blastocyst • Impaired transport in the fallopian tube & uterine cavity • Interference with development of the endometrium to impede implantation
When does pregnancy start? ? ? The American College of Obstetricians and Gynecologists (ACOG), the Food and Drug Administration (FDA), and the National Institutes of Health (NIH) have defined implantation as the beginning of pregnancy. If fertilization has occurred, implantation starts about leading 7 Plan B disrupts the events up to implantation. days after After ovulation. implantation, it has no effect.
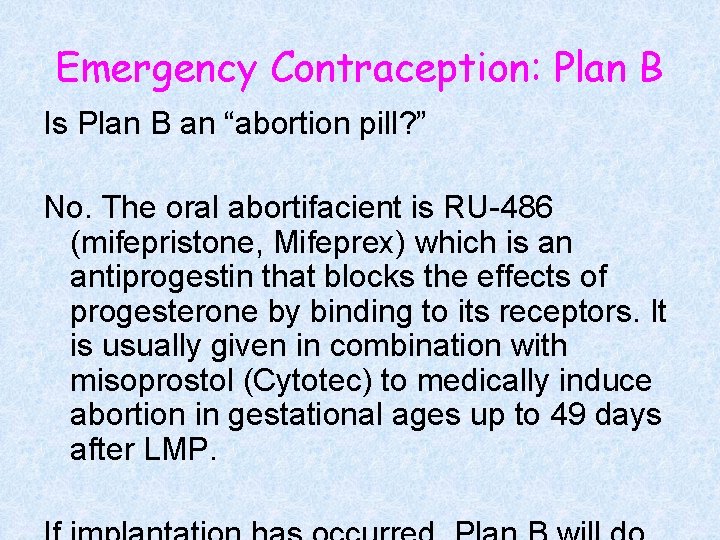
Emergency Contraception: Plan B Is Plan B an “abortion pill? ” No. The oral abortifacient is RU-486 (mifepristone, Mifeprex) which is an antiprogestin that blocks the effects of progesterone by binding to its receptors. It is usually given in combination with misoprostol (Cytotec) to medically induce abortion in gestational ages up to 49 days after LMP.
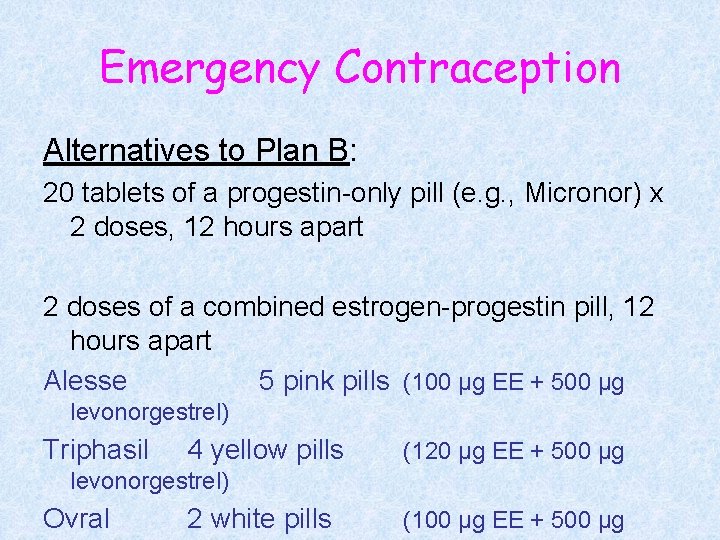
Emergency Contraception Alternatives to Plan B: 20 tablets of a progestin-only pill (e. g. , Micronor) x 2 doses, 12 hours apart 2 doses of a combined estrogen-progestin pill, 12 hours apart Alesse 5 pink pills (100 µg EE + 500 µg levonorgestrel) Triphasil 4 yellow pills (120 µg EE + 500 µg levonorgestrel) Ovral 2 white pills (100 µg EE + 500 µg
Emergency Contraception Standards of care: • providing information • providing post-coital treatment • providing advance Rxwoman, every visit. ” “Every www. not-2 -late. com 1 -888 -NOT-2 -LATE − ACOG

Go get΄em!
 Addison jaynes
Addison jaynes Jeremy jaynes
Jeremy jaynes Cnm 190
Cnm 190 Fort worth midwife associates
Fort worth midwife associates Nmcid
Nmcid Ogn and pgn full form in contraception
Ogn and pgn full form in contraception Victorian era birth control
Victorian era birth control Cape cervicale caya
Cape cervicale caya Contraception for over 40s
Contraception for over 40s Contraception
Contraception Diaphragme contraception
Diaphragme contraception Voluntary surgical contraception
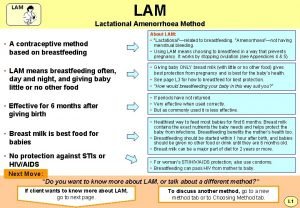
Voluntary surgical contraception What is lam contraception
What is lam contraception Tableau comparatif contraception
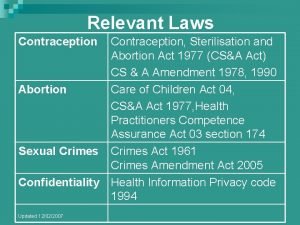
Tableau comparatif contraception Contraception sterilisation and abortion act 1977
Contraception sterilisation and abortion act 1977 詹景裕
詹景裕 Anita schnetzer
Anita schnetzer Anita mustać
Anita mustać Anita cremers
Anita cremers Anita archer rewards
Anita archer rewards Anita forsyth
Anita forsyth Anita rice
Anita rice Apos estudar na europa anita malfatti retornou
Apos estudar na europa anita malfatti retornou Bso
Bso Anita walz
Anita walz Anita curty
Anita curty Anita somani md
Anita somani md Anita archer quotes
Anita archer quotes Anita archer
Anita archer Zdania przeciwstawne
Zdania przeciwstawne Anita woolfolk educational psychology
Anita woolfolk educational psychology Anita gudelj
Anita gudelj Anita showalter
Anita showalter Anita bajic
Anita bajic Dr anita ravi
Dr anita ravi Transverse metatarsal ligament
Transverse metatarsal ligament Anita kullen
Anita kullen Anita zenger
Anita zenger Dr anita kulkarni
Dr anita kulkarni Anita humphrey
Anita humphrey Anita archer active participation
Anita archer active participation Anita lilian zuppo abed
Anita lilian zuppo abed Anita ghulam ali
Anita ghulam ali Anita park purdue
Anita park purdue Computer fundamentals by anita goel
Computer fundamentals by anita goel Anita nyberg
Anita nyberg Clado anita
Clado anita Anita steiner kommunikation
Anita steiner kommunikation Anita regmi case
Anita regmi case Anita doutt
Anita doutt Anita malmgren
Anita malmgren Myeloma euronet
Myeloma euronet Anita lee-post
Anita lee-post Anita lee-post
Anita lee-post Anita kristina
Anita kristina Primarna devijantnost
Primarna devijantnost Cubismo cézanniano
Cubismo cézanniano Anita orozco
Anita orozco Anita krueger md
Anita krueger md Socioterapija
Socioterapija Anita
Anita Sobre a exposição de anita malfatti em 1917
Sobre a exposição de anita malfatti em 1917 Anita donaldson
Anita donaldson Dr labancz anita
Dr labancz anita Anita ndanu
Anita ndanu Anita heinzmann
Anita heinzmann Anita burgund
Anita burgund Anita belin
Anita belin Anita fletcher
Anita fletcher Anita archer explicit instruction
Anita archer explicit instruction