Preeclampsia Carla Morrow DNP CNM Dallas Midwife Associates



- Slides: 33
Preeclampsia Carla Morrow DNP, CNM Dallas Midwife Associates
First described in the literature over 150 years ago

10% of all pregnancies worldwide Incidence and Sequela Increased by 25% over the past two decades in the US Leading cause of maternal and perinatal morbidity and mortality with estimated 50, 000 to 60, 000 preeclampsia related deaths per year world wide Hypertensive disorders of pregnancy are major contributors to prematurity
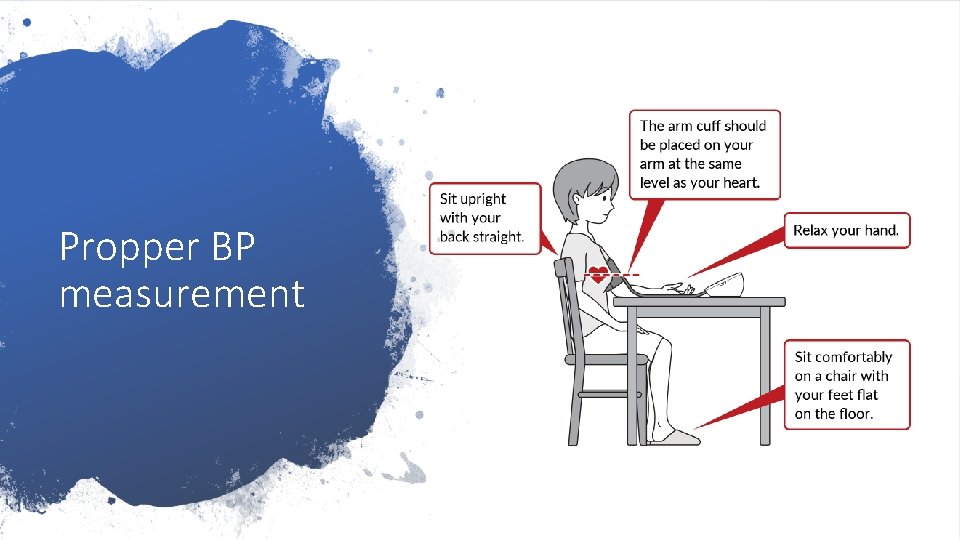
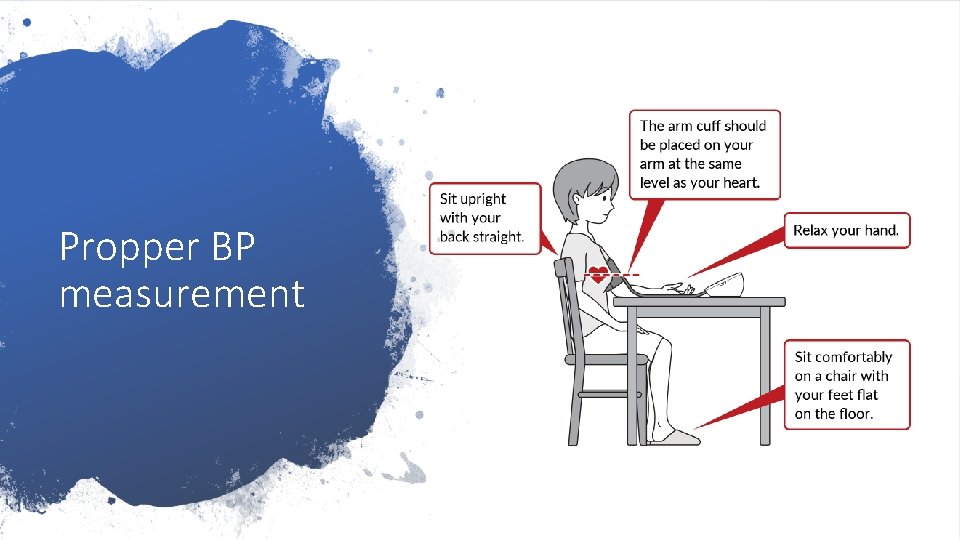
Propper BP measurement
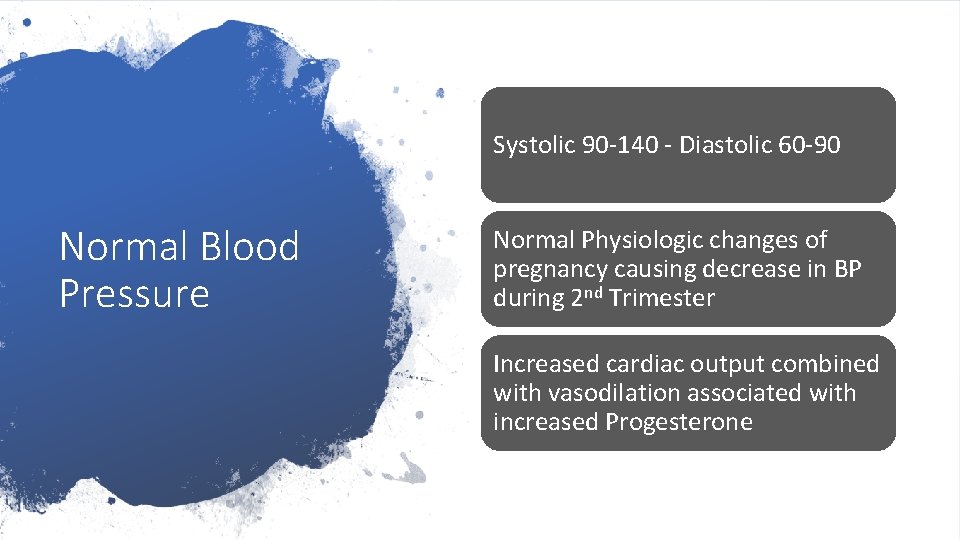
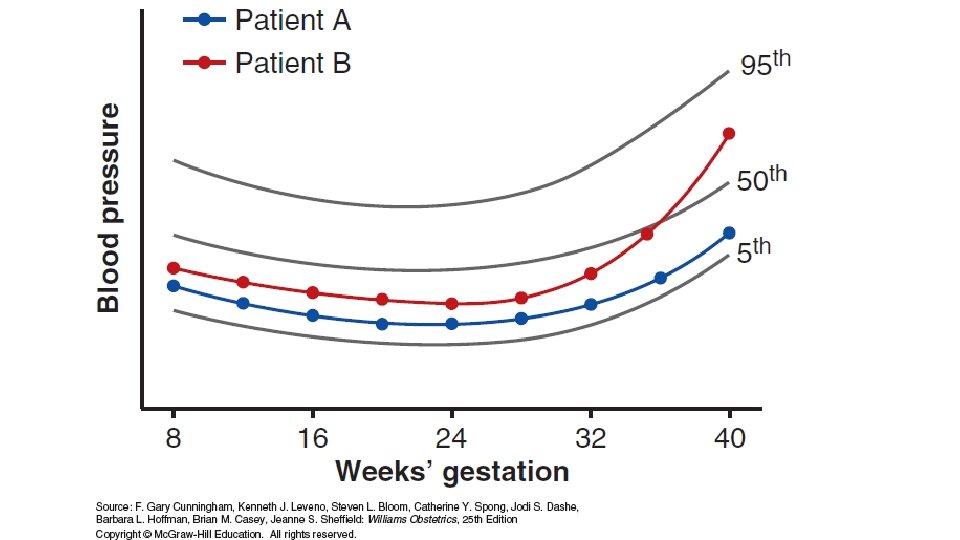
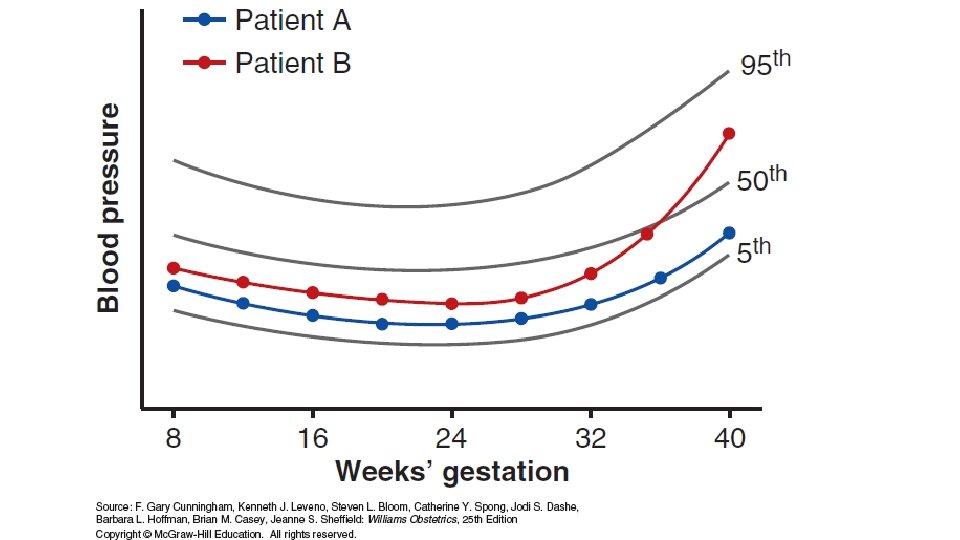
Systolic 90 -140 - Diastolic 60 -90 Normal Blood Pressure Normal Physiologic changes of pregnancy causing decrease in BP during 2 nd Trimester Increased cardiac output combined with vasodilation associated with increased Progesterone
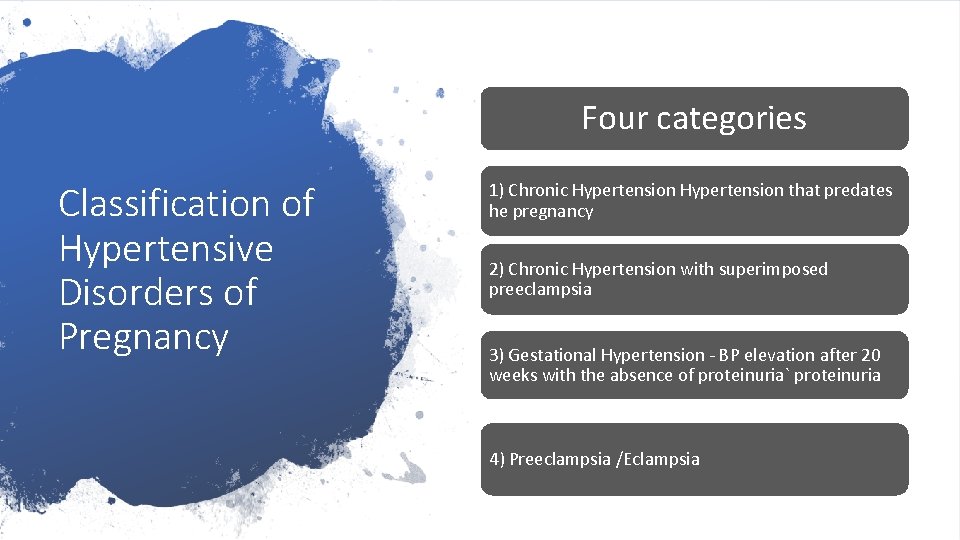
Four categories Classification of Hypertensive Disorders of Pregnancy 1) Chronic Hypertension that predates he pregnancy 2) Chronic Hypertension with superimposed preeclampsia 3) Gestational Hypertension - BP elevation after 20 weeks with the absence of proteinuria` proteinuria 4) Preeclampsia /Eclampsia
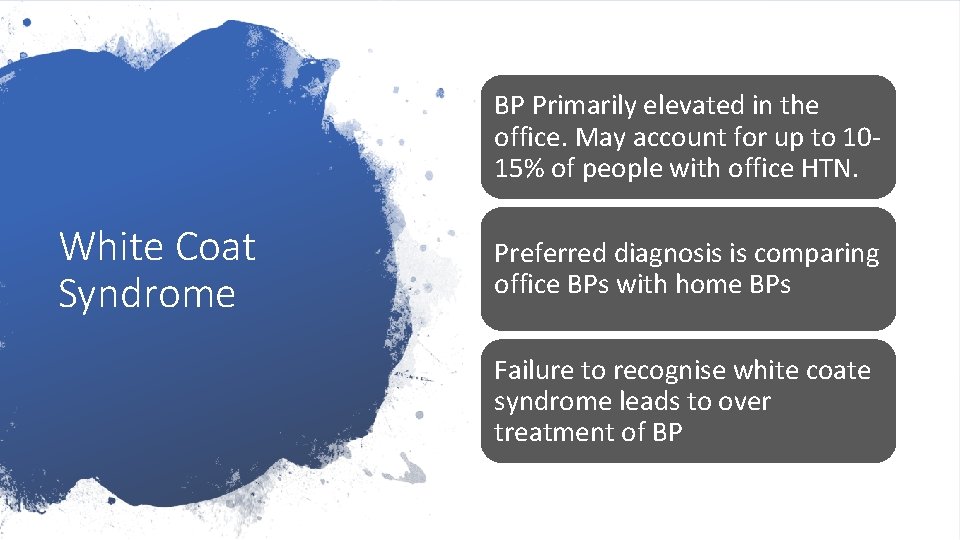
BP Primarily elevated in the office. May account for up to 1015% of people with office HTN. White Coat Syndrome Preferred diagnosis is comparing office BPs with home BPs Failure to recognise white coate syndrome leads to over treatment of BP
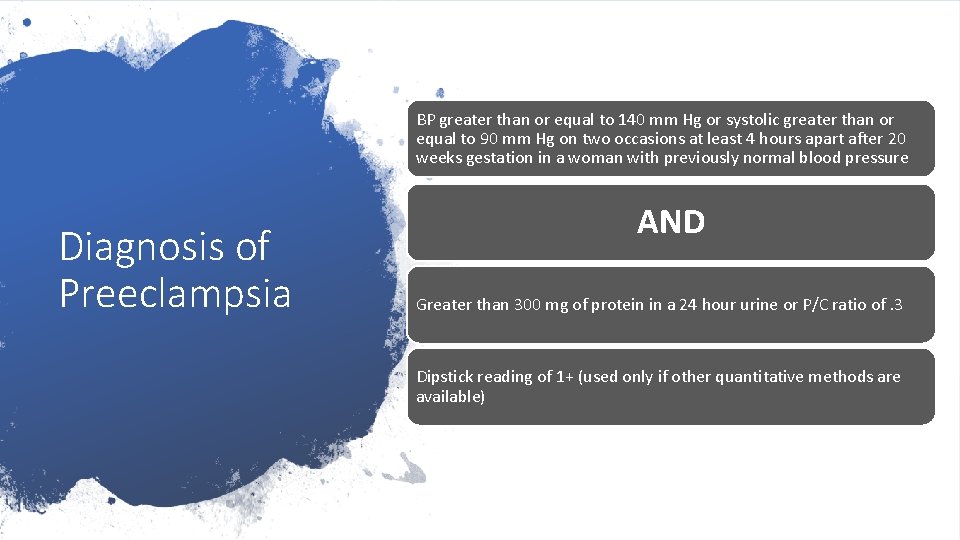
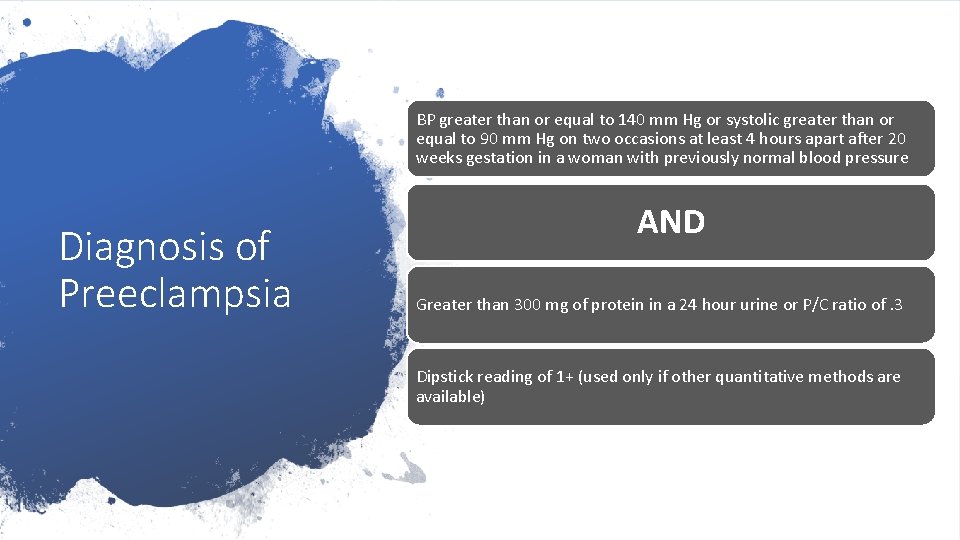
BP greater than or equal to 140 mm Hg or systolic greater than or equal to 90 mm Hg on two occasions at least 4 hours apart after 20 weeks gestation in a woman with previously normal blood pressure Diagnosis of Preeclampsia AND Greater than 300 mg of protein in a 24 hour urine or P/C ratio of. 3 Dipstick reading of 1+ (used only if other quantitative methods are available)
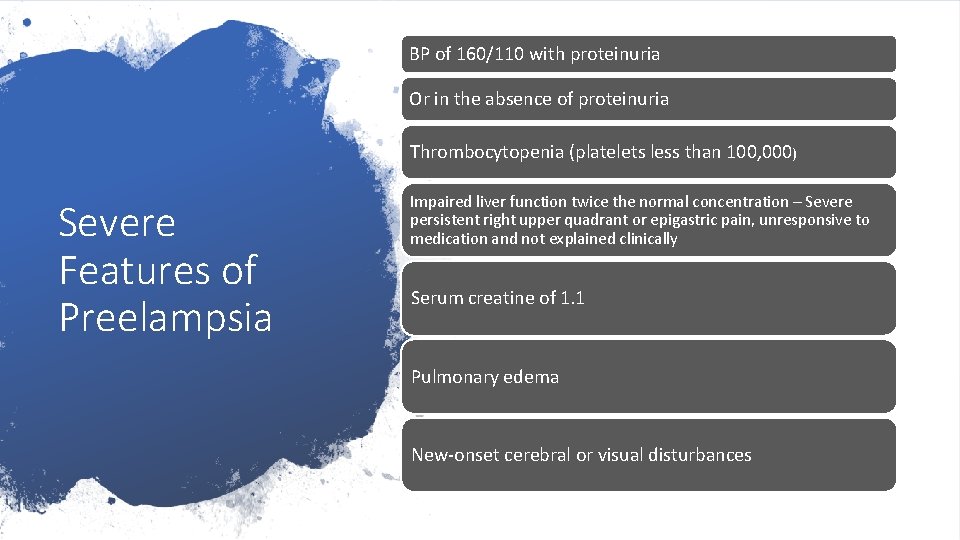
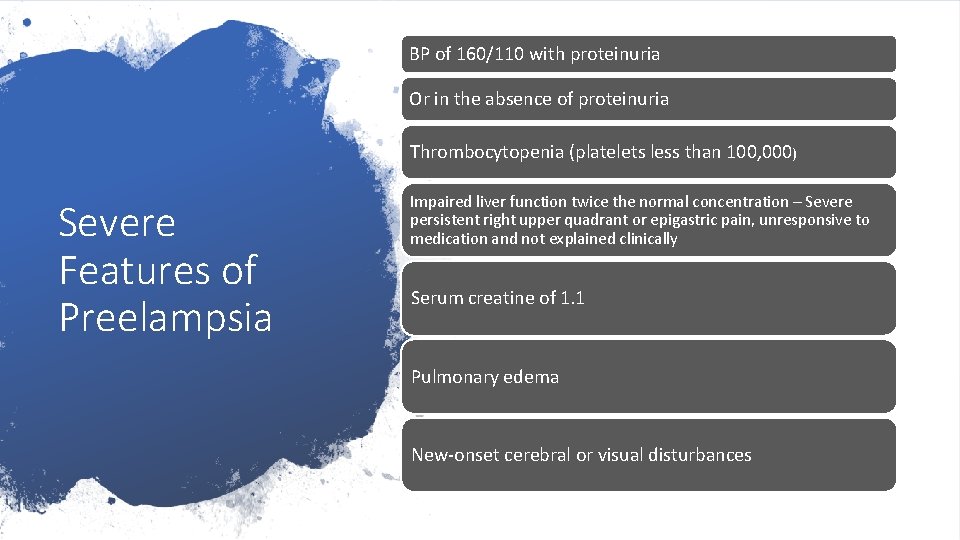
BP of 160/110 with proteinuria Or in the absence of proteinuria Thrombocytopenia (platelets less than 100, 000) Severe Features of Preelampsia Impaired liver function twice the normal concentration – Severe persistent right upper quadrant or epigastric pain, unresponsive to medication and not explained clinically Serum creatine of 1. 1 Pulmonary edema New-onset cerebral or visual disturbances
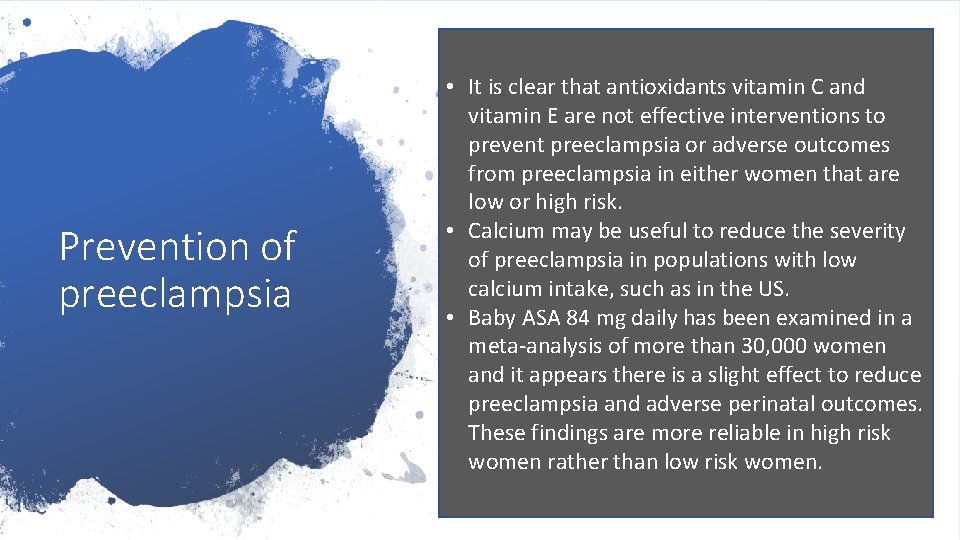
Prevention of preeclampsia • It is clear that antioxidants vitamin C and vitamin E are not effective interventions to prevent preeclampsia or adverse outcomes from preeclampsia in either women that are low or high risk. • Calcium may be useful to reduce the severity of preeclampsia in populations with low calcium intake, such as in the US. • Baby ASA 84 mg daily has been examined in a meta-analysis of more than 30, 000 women and it appears there is a slight effect to reduce preeclampsia and adverse perinatal outcomes. These findings are more reliable in high risk women rather than low risk women.
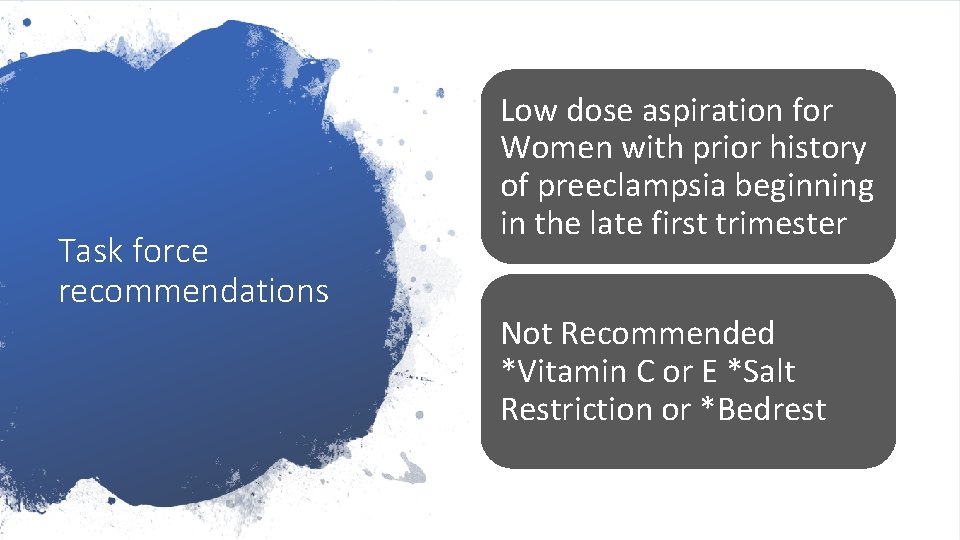
Task force recommendations Low dose aspiration for Women with prior history of preeclampsia beginning in the late first trimester Not Recommended *Vitamin C or E *Salt Restriction or *Bedrest
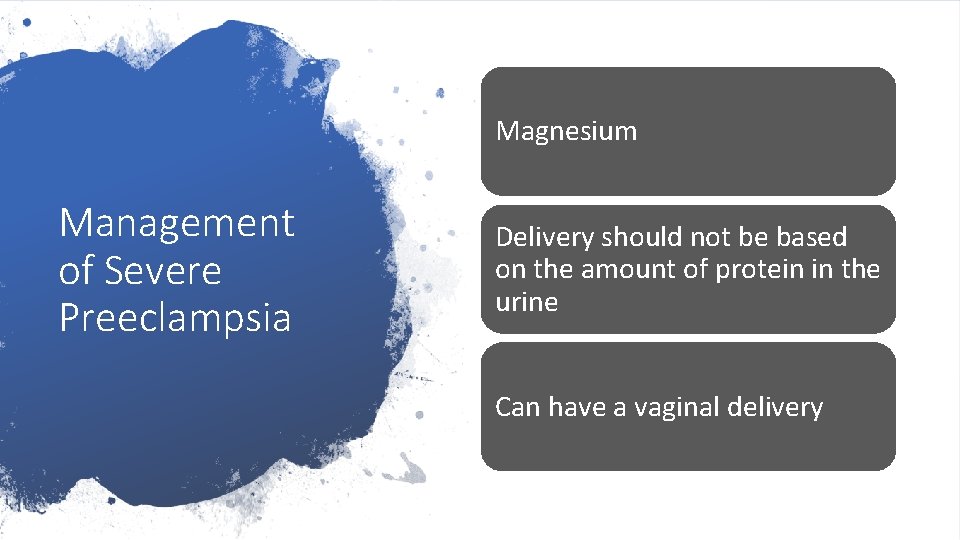
Proteinuria • Review of maternal mortality data revels that Deaths can be avoided if providers remain alert to the likelihood that preeclampsia will progress. • The same reviews identified that invervention in acutely ill women has been delayed because of the abscense of proteinuria. • Furthermore accumulating information indicates that the amount of proteinuria does not predict maternal or fetal outcome.
BP Medications Home BP monitoring Chronic HTN Management Baby ASA late first trimester Growth scans monthly weekly BPPs/NSTs 36 weeks Delivery after 38 weeks

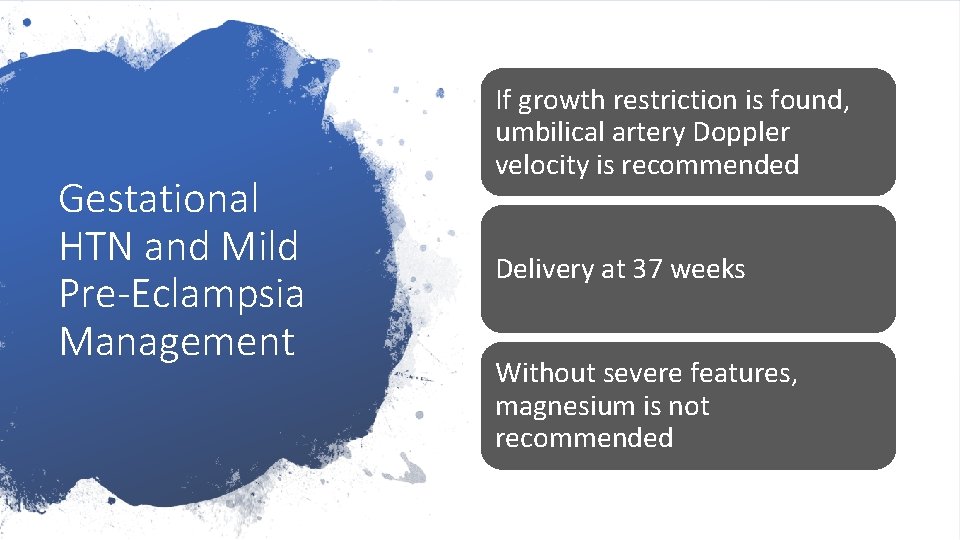
Serial assessment of maternal symptoms and fetal movement (by the mother) Gestational HTN and Mild Pre-Eclampsia Management Serial measures of BP twice weekly with once occurring in the office – The other BP can be done at home Serial assessment of maternal symptoms and fetal movement weekly and assessment of platelets, liver enzymes and proteinuria Ultrasound for Fetal Growth Do no administer antihypertensives or put on bedrest
Gestational HTN and Mild Pre-Eclampsia Management If growth restriction is found, umbilical artery Doppler velocity is recommended Delivery at 37 weeks Without severe features, magnesium is not recommended
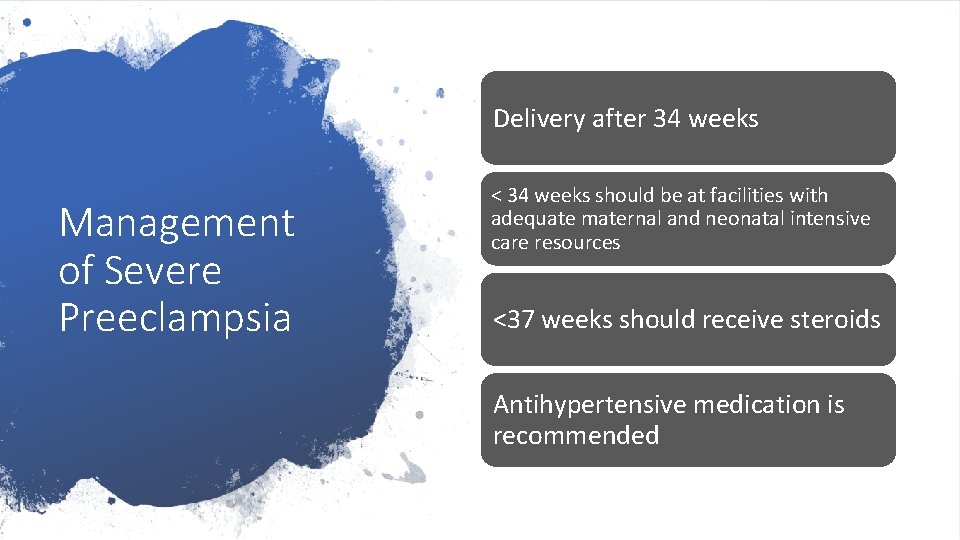
Delivery after 34 weeks Management of Severe Preeclampsia < 34 weeks should be at facilities with adequate maternal and neonatal intensive care resources <37 weeks should receive steroids Antihypertensive medication is recommended
Magnesium Management of Severe Preeclampsia Delivery should not be based on the amount of protein in the urine Can have a vaginal delivery
New onset granmal seizures Eclampsia Magnesium Sulfate
Hemolysis, abnormal liver function, Thrombocytopenia HELLP Characterized by progressive and sometimes sudden maternal and fetal deterioration Associated with increased rates of maternal orbidity and mortality Usually immediate delivery
Can first develop in the postpartum period Postpartum Hypertension Can be missed because of early discharge Onset at any time Sometimes last up to 6 mos postpartum requiring BP medications
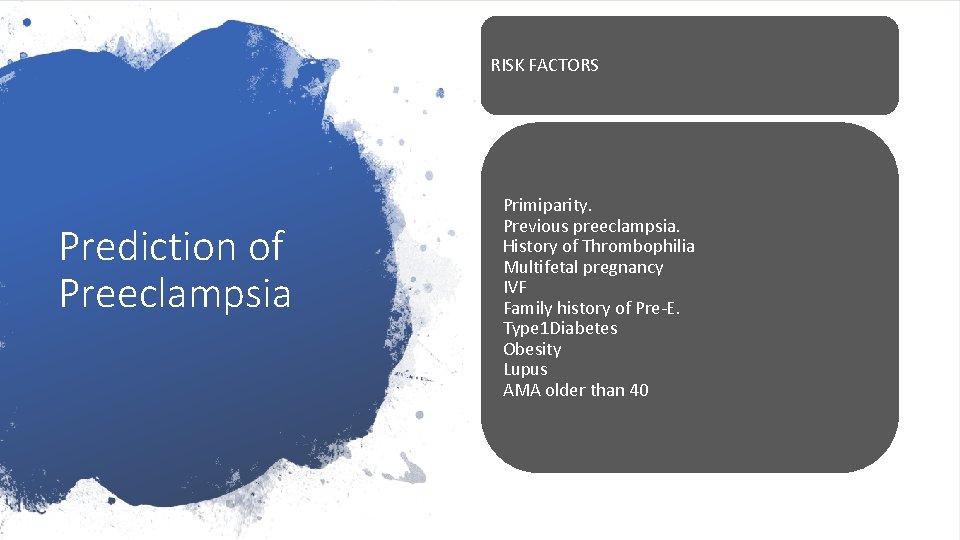
RISK FACTORS Prediction of Preeclampsia Primiparity. Previous preeclampsia. History of Thrombophilia Multifetal pregnancy IVF Family history of Pre-E. Type 1 Diabetes Obesity Lupus AMA older than 40
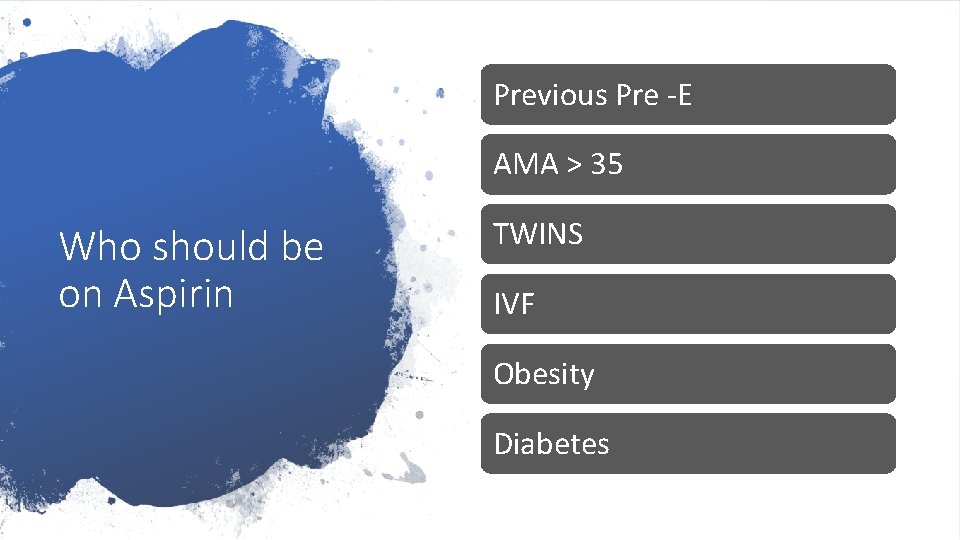
Previous Pre -E AMA > 35 Who should be on Aspirin TWINS IVF Obesity Diabetes
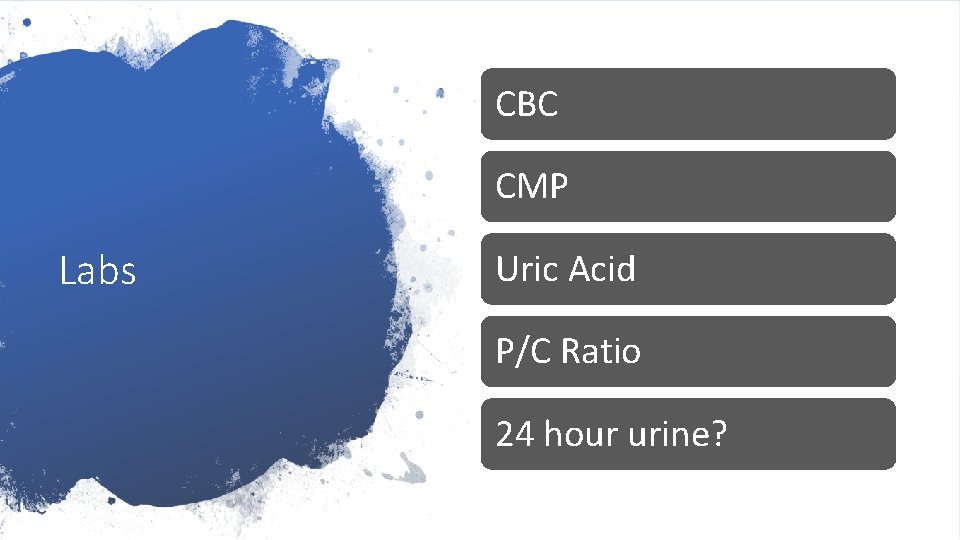
CBC CMP Labs Uric Acid P/C Ratio 24 hour urine?
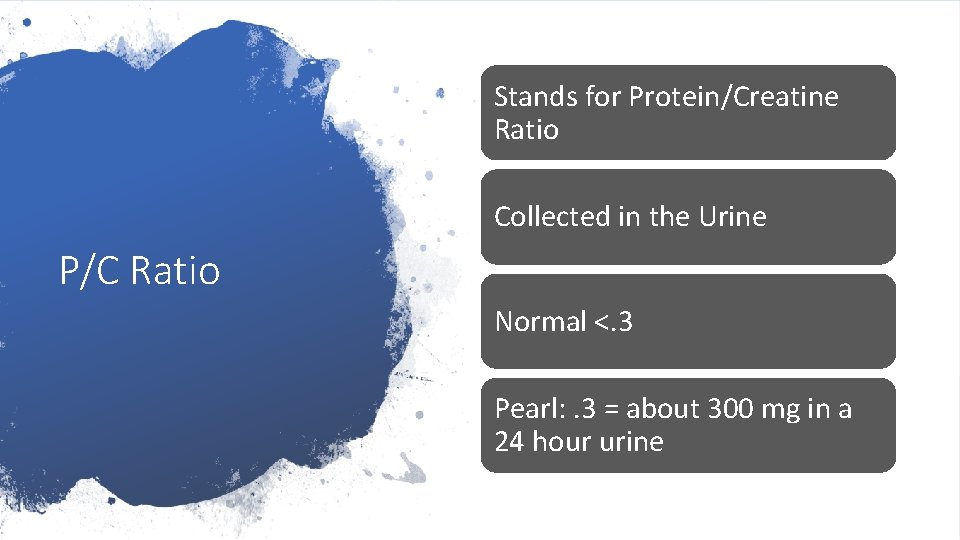
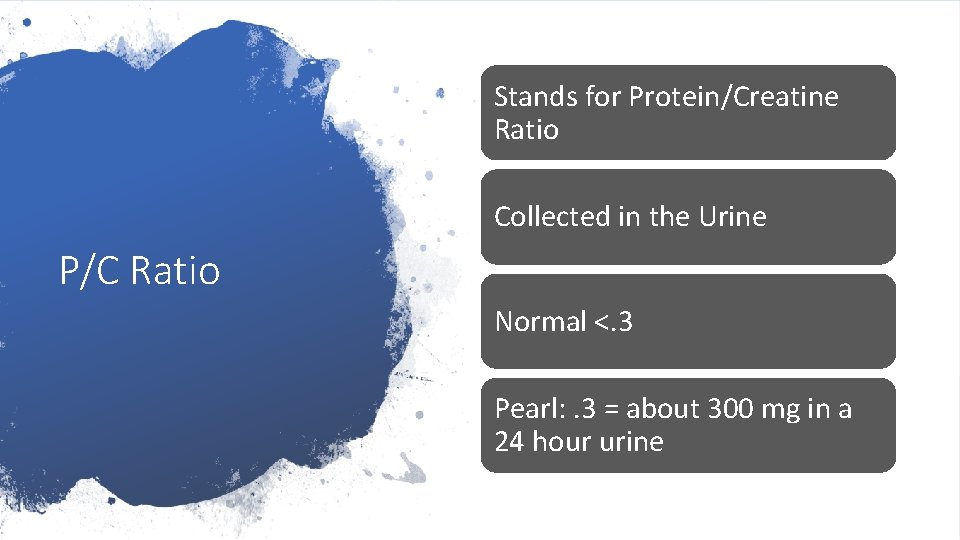
Stands for Protein/Creatine Ratio Collected in the Urine P/C Ratio Normal <. 3 Pearl: . 3 = about 300 mg in a 24 hour urine
Still Gold Standard 24 Hour Urine Normal below 300

Take through history OOH Elevated Blood Pressure Guidelines Clients at Risk should be started on baby ASA – Fish Oil is an alternative Normal BP is 140/90 or below
Be sure BP is taken correctly OOH Elevated Blood Pressure Guidelines U-dip not evidenced based without indication If BP is elevated < 20 weeks, have client take home BPs If you get a very high reading prior to 20 weeks, may need to go to ER
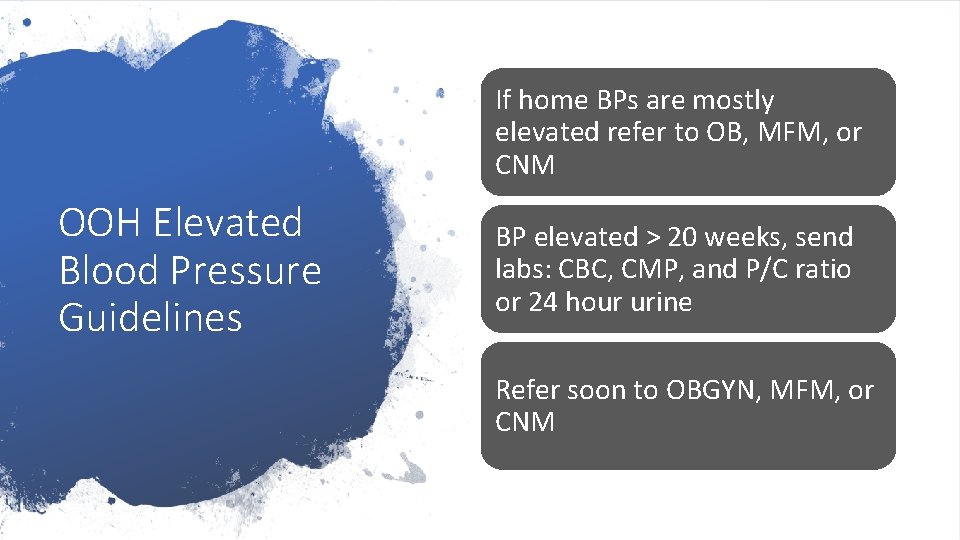
If home BPs are mostly elevated refer to OB, MFM, or CNM OOH Elevated Blood Pressure Guidelines BP elevated > 20 weeks, send labs: CBC, CMP, and P/C ratio or 24 hour urine Refer soon to OBGYN, MFM, or CNM
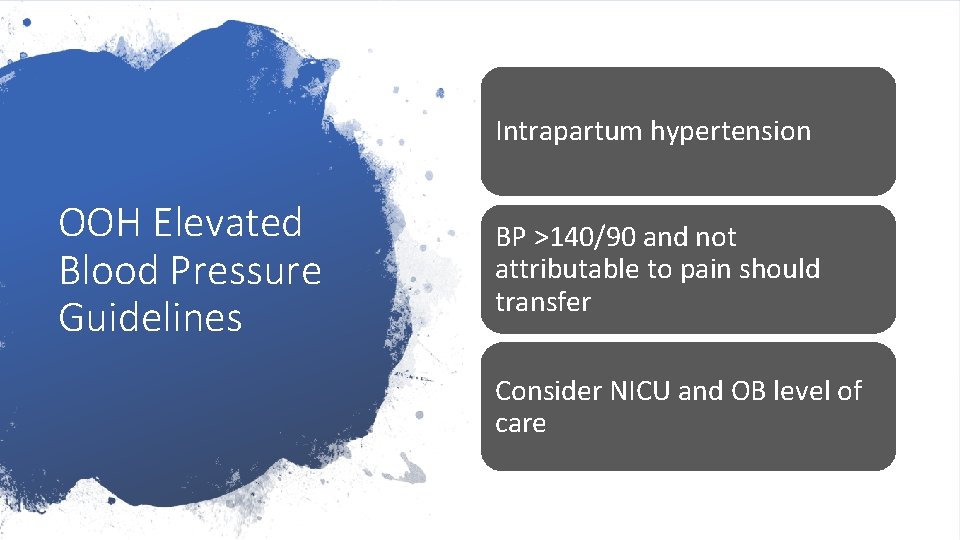
Intrapartum hypertension OOH Elevated Blood Pressure Guidelines BP >140/90 and not attributable to pain should transfer Consider NICU and OB level of care
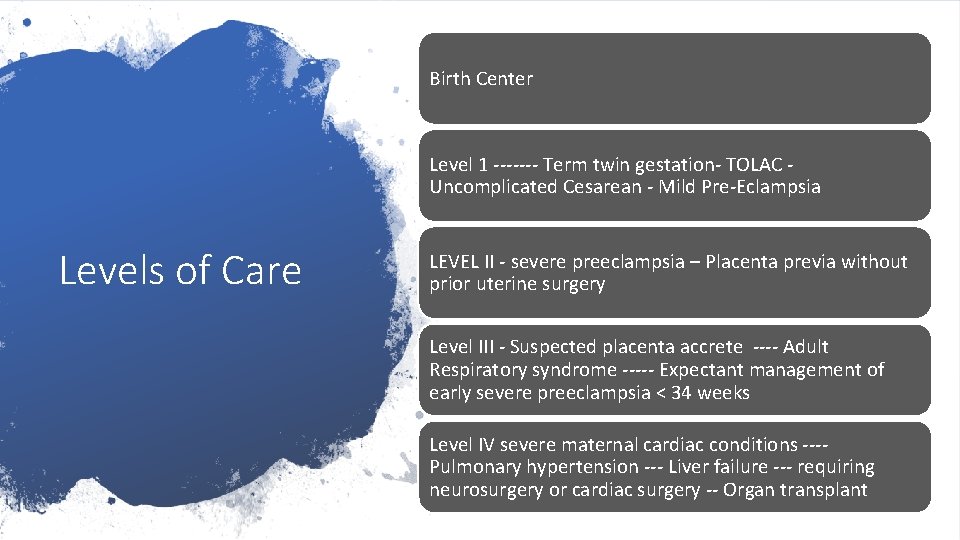
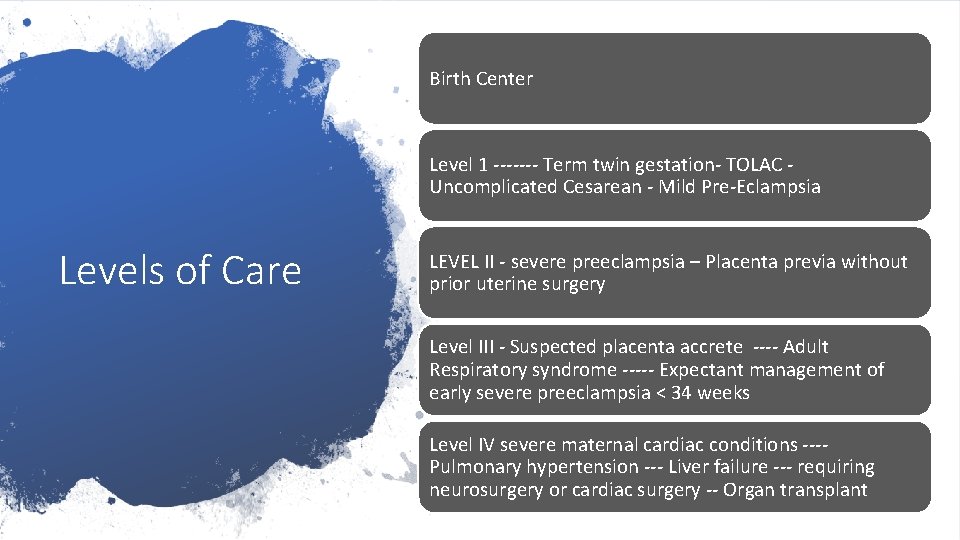
Birth Center Level 1 ------- Term twin gestation- TOLAC Uncomplicated Cesarean - Mild Pre-Eclampsia Levels of Care LEVEL II - severe preeclampsia – Placenta previa without prior uterine surgery Level III - Suspected placenta accrete ---- Adult Respiratory syndrome ----- Expectant management of early severe preeclampsia < 34 weeks Level IV severe maternal cardiac conditions ---Pulmonary hypertension --- Liver failure --- requiring neurosurgery or cardiac surgery -- Organ transplant
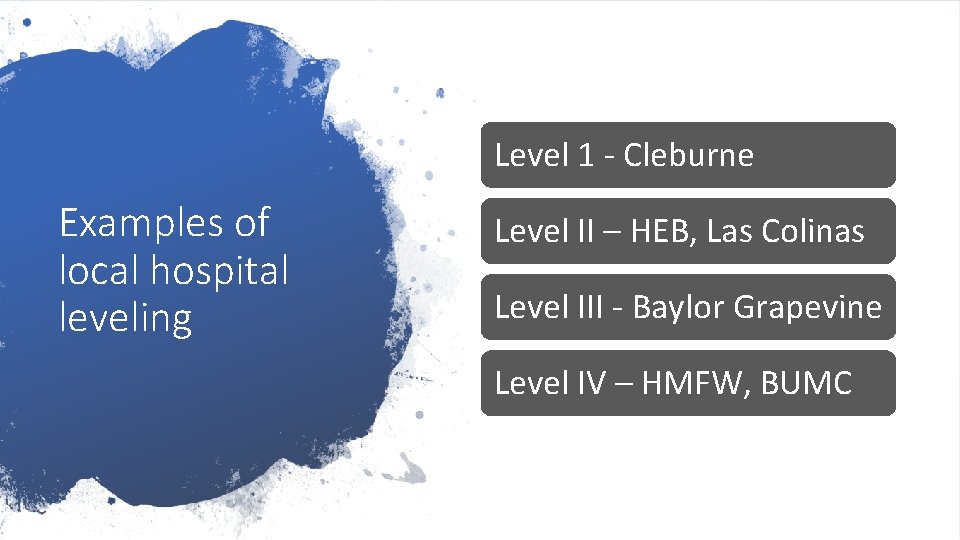
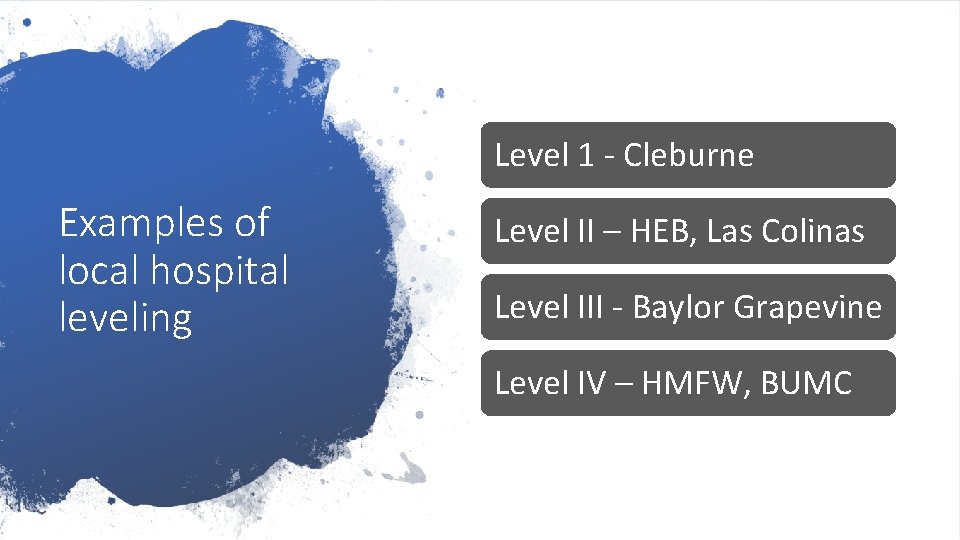
Level 1 - Cleburne Examples of local hospital leveling Level II – HEB, Las Colinas Level III - Baylor Grapevine Level IV – HMFW, BUMC
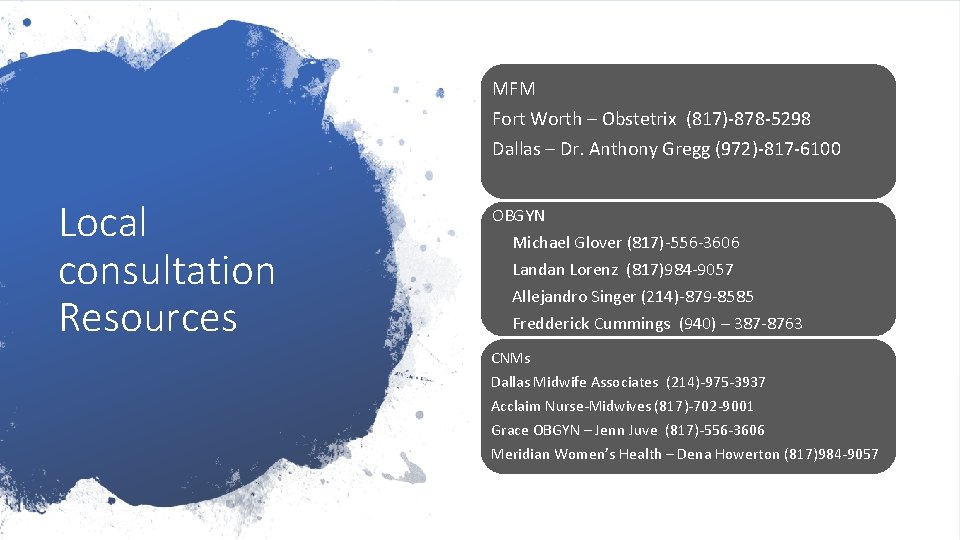
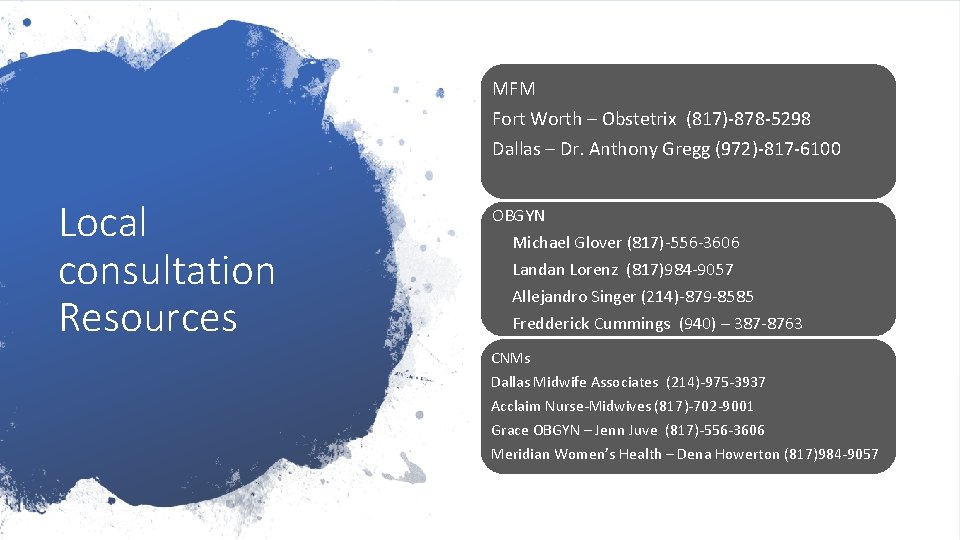
MFM Fort Worth – Obstetrix (817)-878 -5298 Dallas – Dr. Anthony Gregg (972)-817 -6100 Local consultation Resources OBGYN Michael Glover (817)-556 -3606 Landan Lorenz (817)984 -9057 Allejandro Singer (214)-879 -8585 Fredderick Cummings (940) – 387 -8763 CNMs Dallas Midwife Associates (214)-975 -3937 Acclaim Nurse-Midwives (817)-702 -9001 Grace OBGYN – Jenn Juve (817)-556 -3606 Meridian Women’s Health – Dena Howerton (817)984 -9057
 Dallas midwife associates
Dallas midwife associates Carla morrow midwife
Carla morrow midwife Cindy morrow midwife
Cindy morrow midwife Cnm 190
Cnm 190 Nmcid
Nmcid Chamberlain fnp practicum
Chamberlain fnp practicum Uca dnp
Uca dnp Spi dnp
Spi dnp Sicodis histórico
Sicodis histórico Norma 017 epidemiologia
Norma 017 epidemiologia Preeclampsia teaching
Preeclampsia teaching Prof sandra lowe
Prof sandra lowe Management
Management Superimposed preeclampsia
Superimposed preeclampsia Superimposed preeclampsia
Superimposed preeclampsia Diagnosticos de enfermeria para preeclampsia
Diagnosticos de enfermeria para preeclampsia Eclampsia
Eclampsia Magnesium sulfate toxicity level
Magnesium sulfate toxicity level Pregnancy trimester breakdown
Pregnancy trimester breakdown Diagnostic criteria of preeclampsia
Diagnostic criteria of preeclampsia Superimposed preeclampsia
Superimposed preeclampsia Superimposed preeclampsia
Superimposed preeclampsia Acute fulminating preeclampsia
Acute fulminating preeclampsia Mgso4 mechanism of action in eclampsia
Mgso4 mechanism of action in eclampsia Bestwood and sherwood midwifery
Bestwood and sherwood midwifery Nysalm
Nysalm Kepanjangan sst
Kepanjangan sst Future nurse future midwife
Future nurse future midwife Dirty jobs dairy cow midwife worksheet answer key
Dirty jobs dairy cow midwife worksheet answer key Stefan morrow
Stefan morrow Rosemary morrow legos
Rosemary morrow legos Aimee rises from the sea apush
Aimee rises from the sea apush Melanie morrow
Melanie morrow Whatever dies was not mixed equally
Whatever dies was not mixed equally