Insurance Education Part 2 Health Plan Options Health


- Slides: 84
Insurance Education Part #2 Health Plan Options

Health Plan Options Choices • State Health Plan Standard Plan § Savings Plan § • HMOs Blue. Choice Health. Plan* (available statewide) § CIGNA HMO* § *Must live or work in service area
Insurance Education Part #2 Health Plan Options Standard Plan and Savings Plan (Features the Plans have in Common)
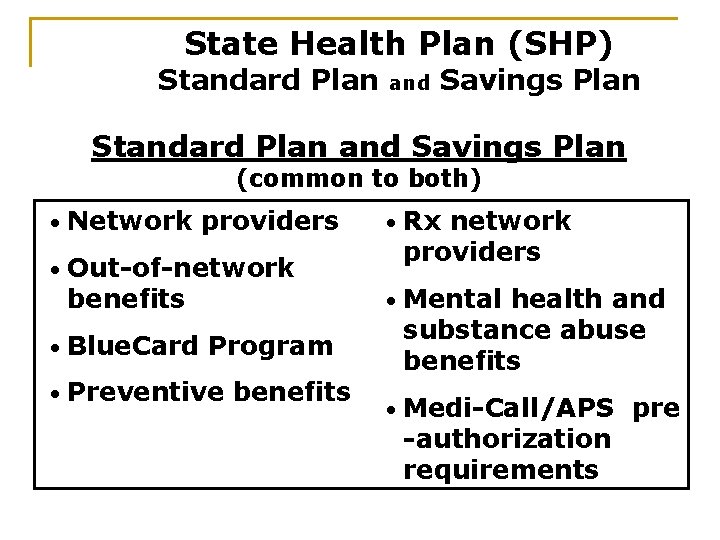
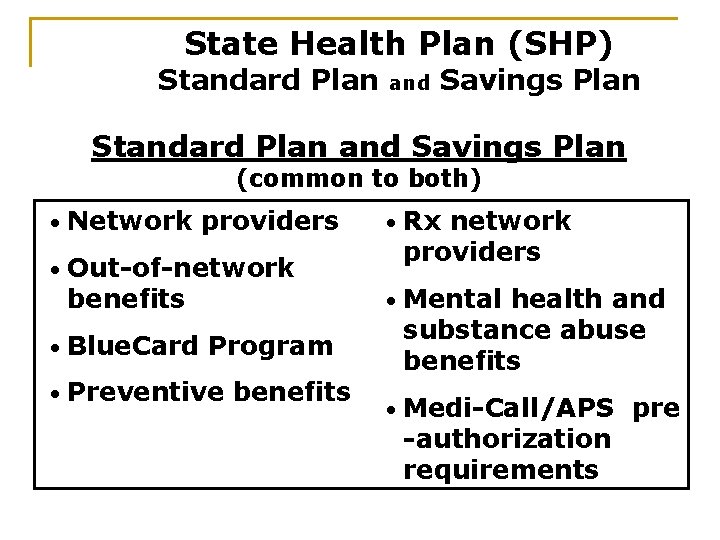
State Health Plan (SHP) Standard Plan and Savings Plan (common to both) • Network providers • • Out-of-network benefits Rx network providers • Mental health and substance abuse benefits • Medi-Call/APS pre -authorization requirements • Blue. Card Program • Preventive benefits
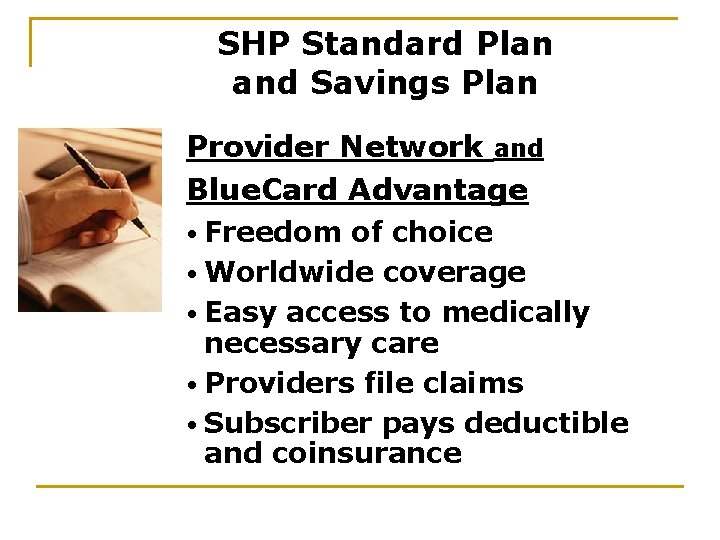
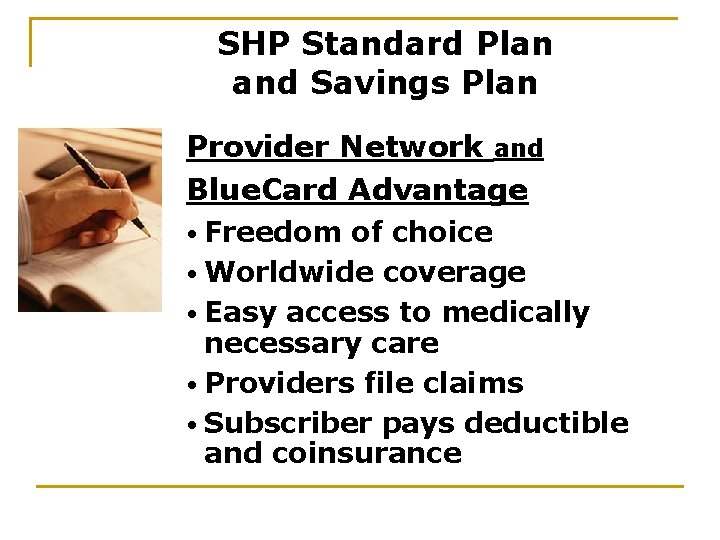
SHP Standard Plan and Savings Plan Provider Network and Blue. Card Advantage • Freedom of choice • Worldwide coverage • Easy access to medically necessary care • Providers file claims • Subscriber pays deductible and coinsurance

SHP Standard Plan and Savings Plan (cont. ) • Subscribers not balance-billed for charges over allowed amount (negotiated pricing) • SHP ID card (Preferred Provider Organization, or PPO, logo located in bottom corner of ID card) • National PPO organization coverage • Worldwide coverage • Call 800 -810 -BLUE
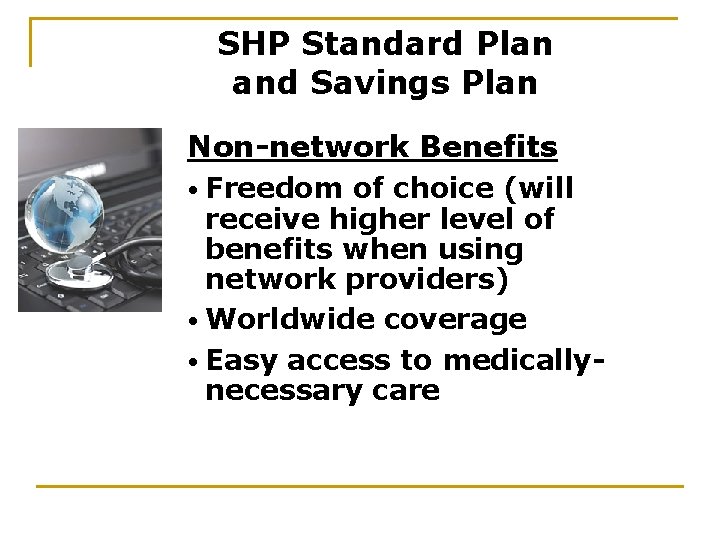
SHP Standard Plan and Savings Plan Non-network Benefits • Freedom of choice (will receive higher level of benefits when using network providers) • Worldwide coverage • Easy access to medicallynecessary care
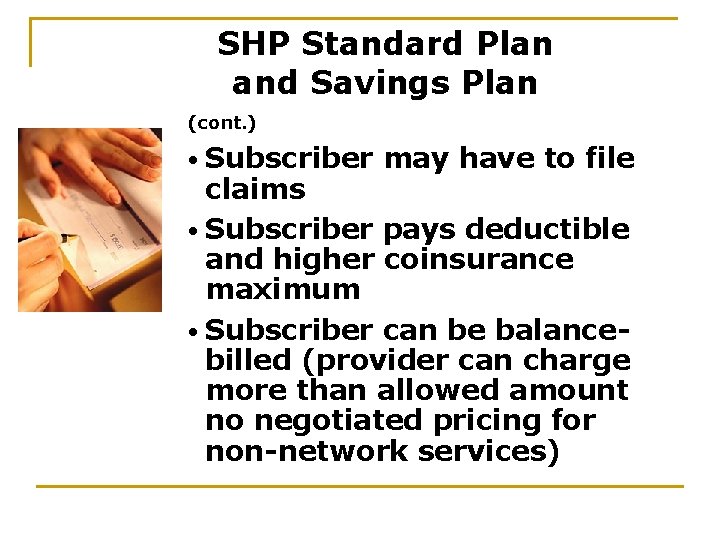
SHP Standard Plan and Savings Plan (cont. ) • Subscriber may have to file claims • Subscriber pays deductible and higher coinsurance maximum • Subscriber can be balancebilled (provider can charge more than allowed amount no negotiated pricing for non-network services)
SHP Standard Plan and Savings Plan Preventive Benefits (must follow Plan guidelines) • Mammography • Pap testing Test • Well-child care • Routine colonoscopy • Worksite health screening (available to HMO subscribers as well)
SHP Standard Plan and Savings Plan Mammography Testing • 100 percent coverage for routine, four-view mammograms, according to Plan guidelines • Performed at participating mammography facilities
SHP Standard Plan and Savings Plan (cont. ) • Ages 35 -39 (one routine mammogram during those years) • Ages 40 -74 (one routine mammogram every 12 months) • Deductible and coinsurance apply to diagnostic mammograms
SHP Standard Plan and Savings Plan Pap Test • No deductible or coinsurance • Subscriber free to choose provider • One Pap Test each year for covered females, ages 18 through 65 • For routine and diagnostic Pap Tests • Pays lab costs only - routine office visit NOT covered
SHP Standard Plan and Savings Plan Well-child Care Benefits • Well-child checkups Five visits for children younger than 1 year old § Three visits for children 1 year and older § One visit per year for children age 2 through 18 §
SHP Standard Plan and Savings Plan (cont. ) • 100 percent benefit for regular check-ups provided by network providers • 100 percent benefit for covered immunizations, according to recommended schedule (catch-up provision for delayed or missed immunizations through age 18)
SHP Standard Plan and Savings Plan (cont. ) • Covered immunizations Diphtheria-Tetanus-Pertussis (DTP) § Polio § Hepatitis A and B § Haemophilus (Hib) §
SHP Standard Plan and Savings Plan (cont. ) • Additional § § § covered immunizations Measles-Mumps-Rubella Chicken pox Pneumoccocal vaccine (Prevnar) HPV (Human Papilomavirus) Influenza Meningococcal
SHP Standard Plan and Savings Plan Routine Colonoscopies • One routine colonoscopy every 10 years for subscribers age 50 and older • Subject to deductible and coinsurance • Diagnostic colonoscopy subject to deductible and coinsurance
SHP Standard Plan and Savings Plan Prevention Partners (State Employee Wellness Program) • Worksite screening available to employees and spouses covered by State Health Plan or HMO/POS § Subscriber/spouse pays $15 for screening
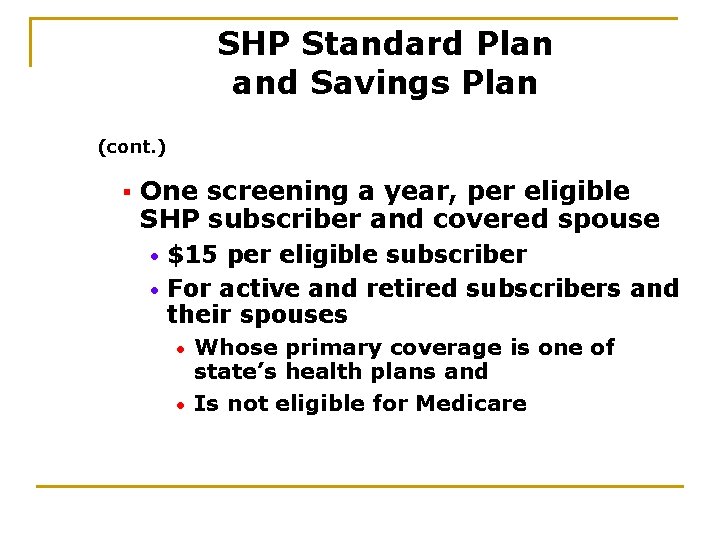
SHP Standard Plan and Savings Plan (cont. ) § One screening a year, per eligible SHP subscriber and covered spouse $15 per eligible subscriber • For active and retired subscribers and their spouses • Whose primary coverage is one of state’s health plans and • Is not eligible for Medicare •
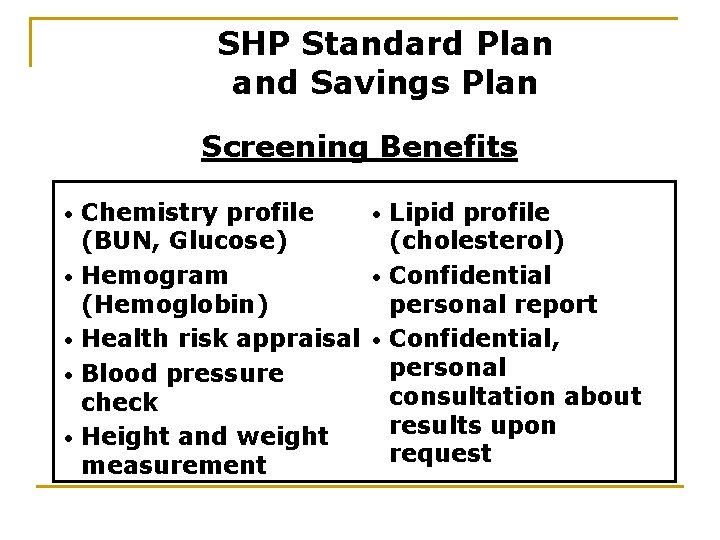
SHP Standard Plan and Savings Plan Screening Benefits • • • Lipid profile Chemistry profile (cholesterol) (BUN, Glucose) • Confidential Hemogram personal report (Hemoglobin) Health risk appraisal • Confidential, personal Blood pressure consultation about check results upon Height and weight request measurement
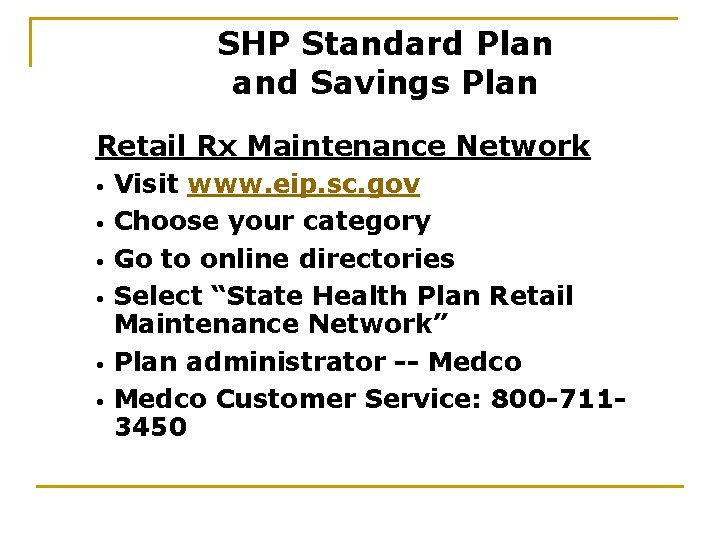
SHP Standard Plan and Savings Plan Retail Rx Maintenance Network • • • Visit www. eip. sc. gov Choose your category Go to online directories Select “State Health Plan Retail Maintenance Network” Plan administrator -- Medco Customer Service: 800 -7113450
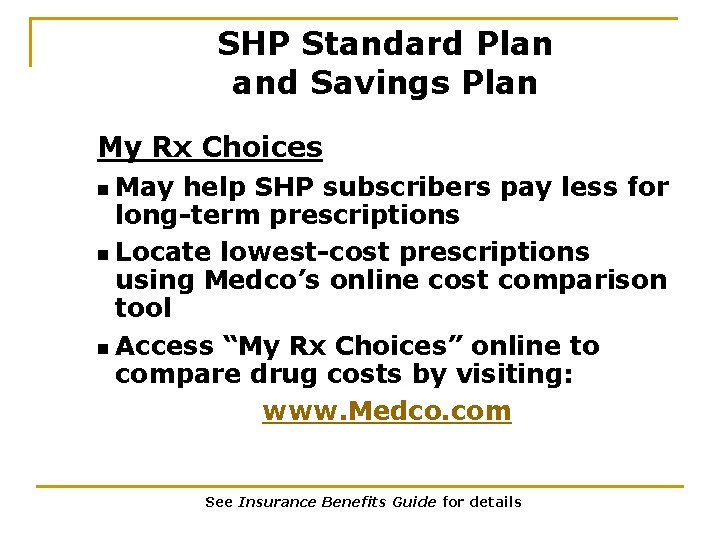
SHP Standard Plan and Savings Plan My Rx Choices n May help SHP subscribers pay less for long-term prescriptions n Locate lowest-cost prescriptions using Medco’s online cost comparison tool n Access “My Rx Choices” online to compare drug costs by visiting: www. Medco. com See Insurance Benefits Guide for details
SHP Standard Plan and Savings Plan Medi-Call (state managed care) • State Health Plan’s utilization review program for medical/ surgical benefits • Ensures subscriber and covered family members receive appropriate medical care in most beneficial, cost-effective manner
SHP Standard Plan and Savings Plan (cont. ) • Some Call § services requiring a Medi- Provider may call for subscriber; however, subscriber has responsibility for calling Medi-Call for pre-authorization
SHP Standard Plan and Savings Plan (cont. ) • Some § § § services include All inpatient admissions Emergency admissions within 48 hours or next business day All outpatient surgery in hospital or ambulatory surgical center Hospice services Home health care services
SHP Standard Plan and Savings Plan (cont. ) Skilled nursing service § In-vitro fertilization procedures § Call during first trimester of pregnancy § MRI, MRA, CT or PET scan § • Consult Insurance Benefits Guide for complete listing of services requiring a Medi-Call
SHP Standard Plan and Savings Plan (cont. ) • Penalties if Medi-Call not contacted $200 penalty (penalty does not apply to coinsurance maximum) § Charges for services not preauthorized by Medi-Call do not apply toward deductible or coinsurance maximum §
SHP Standard Plan and Savings Plan Medi-Call Columbia: 803 -699 -3337 SC, nationwide and Canada: 800 -925 -9724
SHP Standard Plan and Savings Plan Mental Health/Substance Abuse • Administered by APS • Coverage for medically necessary treatment of mental health and substance abuse conditions • Same coinsurance, deductible and out-of-pocket amounts as for physical conditions
SHP Standard Plan and Savings Plan (cont. ) • Must use participating provider or no benefits paid • Can nominate provider for network
SHP Standard Plan and Savings Plan (cont. ) • Inpatient/outpatient care Pre-authorization required before receiving care § Call APS: 800 -221 -8699 § • Outpatient treatment beyond 10 visits must be reviewed for medical necessity
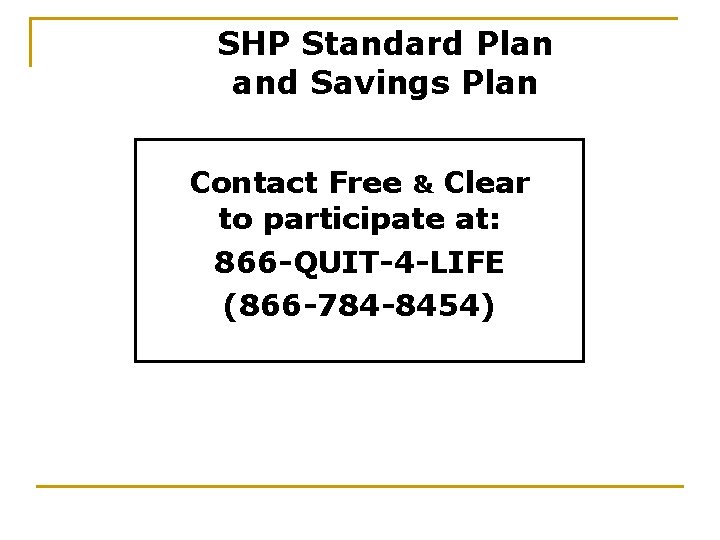
SHP Standard Plan and Savings Plan Tobacco Cessation Benefits • Free & Clear Program, administered by APS • Free for subscribers and covered dependents
SHP Standard Plan and Savings Plan Contact Free & Clear to participate at: 866 -QUIT-4 -LIFE (866 -784 -8454)
Insurance Education Part #2 SHP Standard Plan
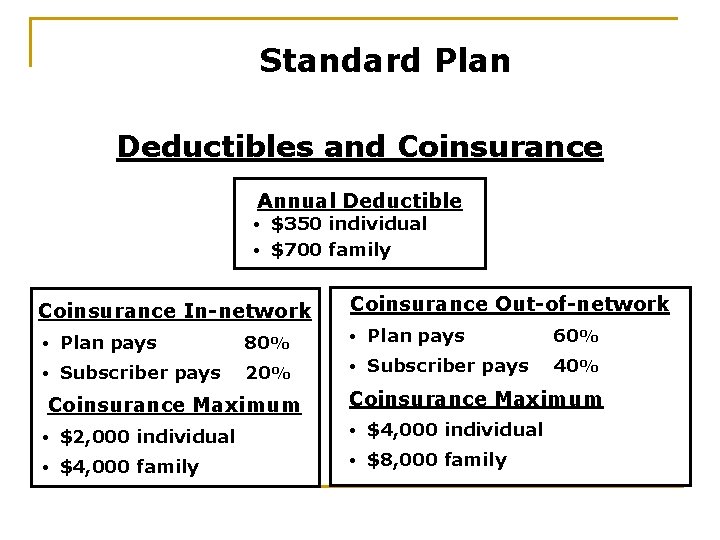
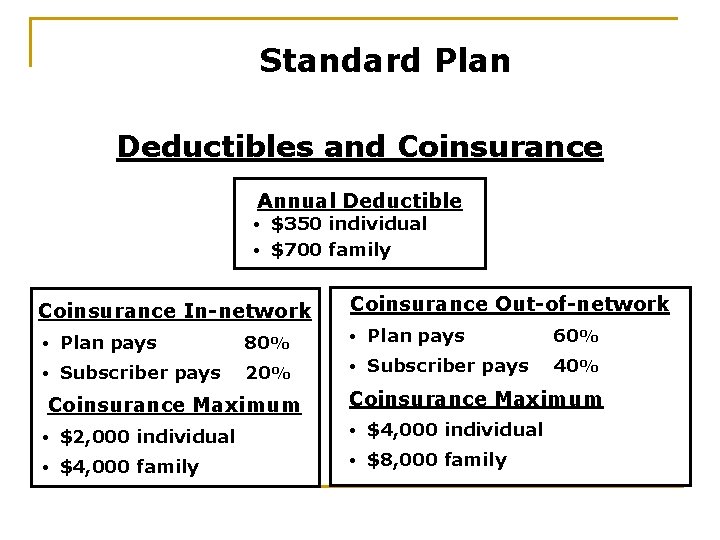
Standard Plan Deductibles and Coinsurance Annual Deductible $350 individual • $700 family • Coinsurance In-network Coinsurance Out-of-network • Plan pays 80% • Plan pays 60% • Subscriber pays 20% • Subscriber pays 40% Coinsurance Maximum • $2, 000 individual • $4, 000 family • $8, 000 family
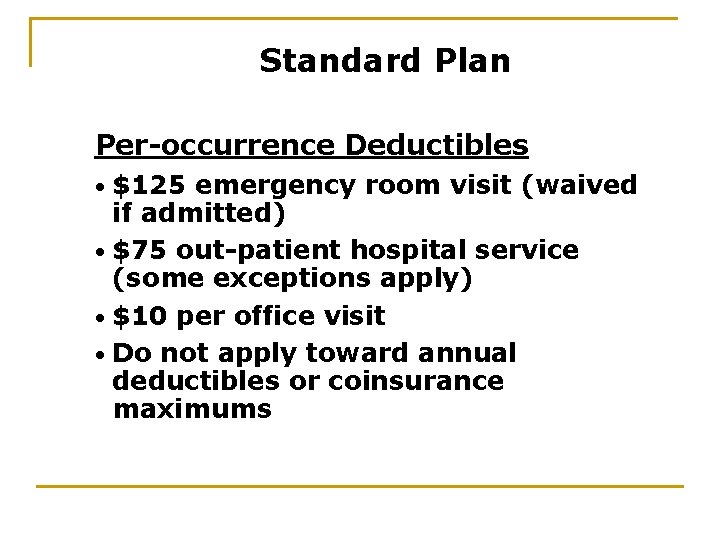
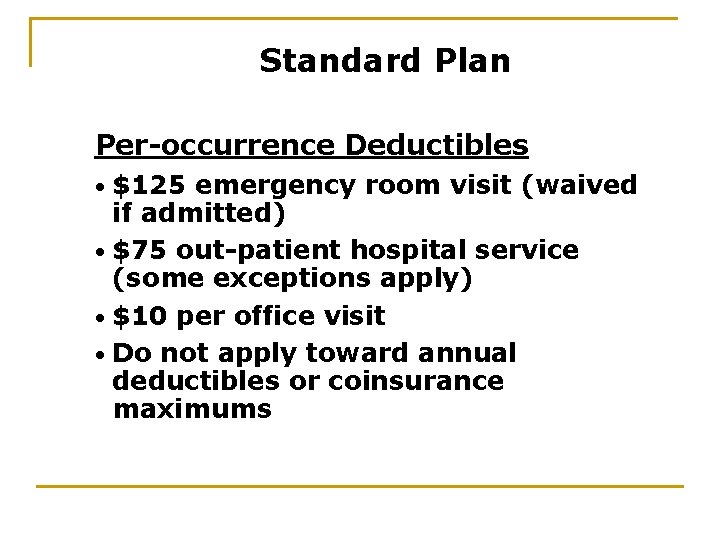
Standard Plan Per-occurrence Deductibles $125 emergency room visit (waived if admitted) • $75 out-patient hospital service (some exceptions apply) • $10 per office visit • Do not apply toward annual deductibles or coinsurance maximums •
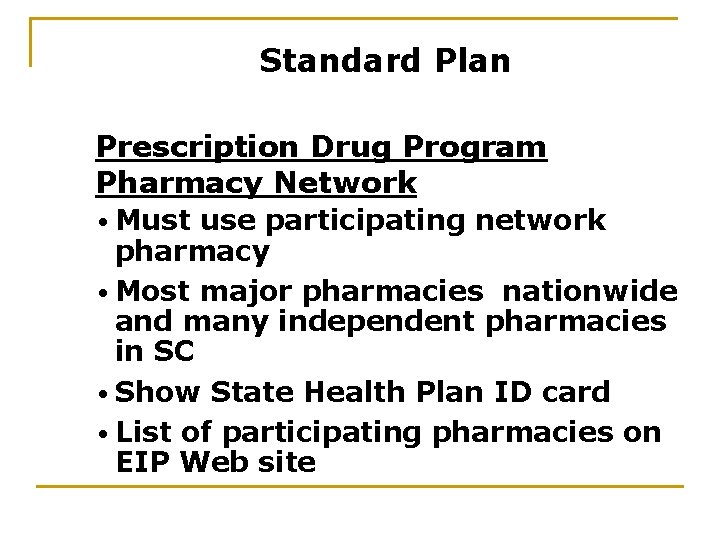
Standard Plan Prescription Drug Program Pharmacy Network • Must use participating network pharmacy • Most major pharmacies nationwide and many independent pharmacies in SC • Show State Health Plan ID card • List of participating pharmacies on EIP Web site
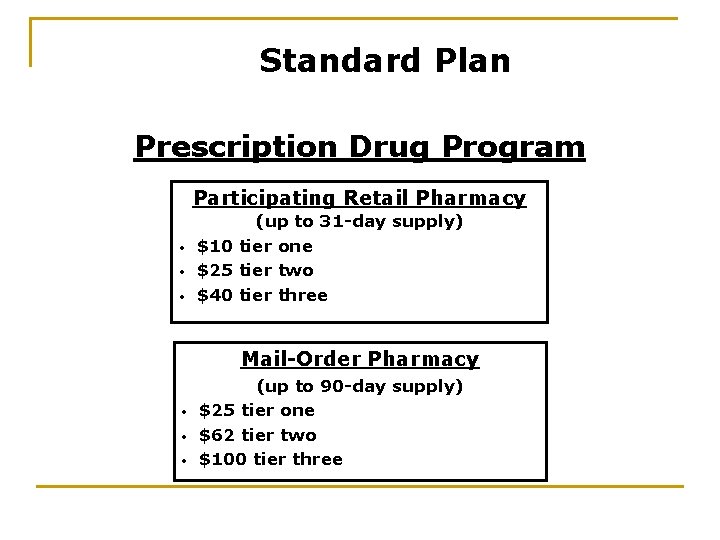
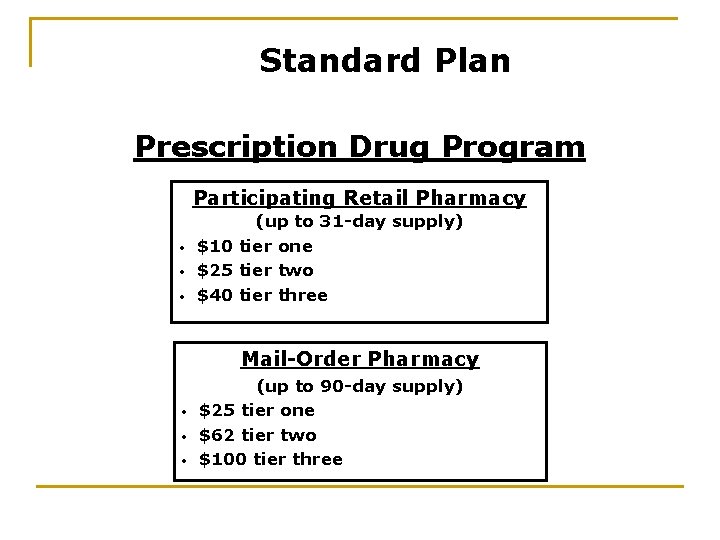
Standard Plan Prescription Drug Program Participating Retail Pharmacy • • • (up to 31 -day supply) $10 tier one $25 tier two $40 tier three Mail-Order Pharmacy • • • (up to 90 -day supply) $25 tier one $62 tier two $100 tier three
Standard Plan Prescription Drug Program Facts • Annual copayment maximum of $2, 500 person • Coordination of benefits
Standard Plan (cont. ) • “Pay § the Difference” If generic brand drug is available and subscriber or doctor chooses brand name, subscriber responsible for difference in price between the allowable charge for name brand generic brand, plus generic brand copayment
Standard Plan (cont. ) “Pay the difference” does not apply to $2, 500 out-of-pocket maximum § Generic copayment does apply to out-of-pocket maximum §
Insurance Education Part #2 Savings Plan Health Savings Accounts (HSA) and Limited-use Medical Spending Accounts
Savings Plan Choice for Subscribers Who: n Want lower premiums n Are willing to take more responsibility for their healthcare n Want to save for major medical expenses through Health Savings Account
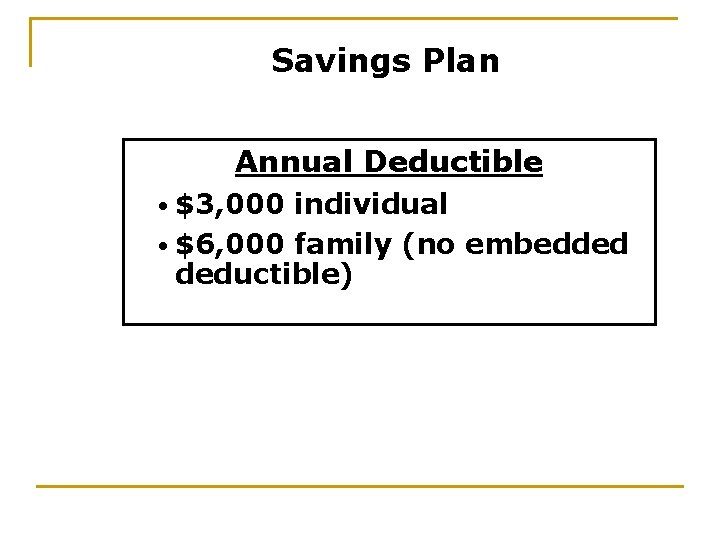
Savings Plan Annual Deductible • $3, 000 individual • $6, 000 family (no embedded deductible)
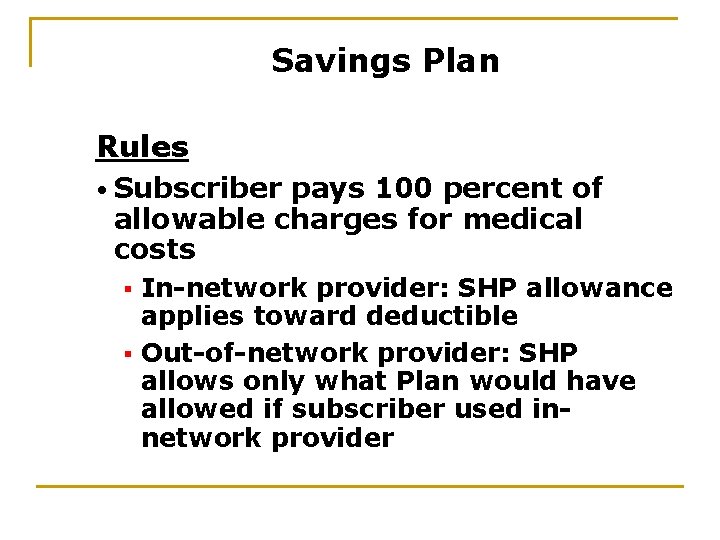
Savings Plan Rules • Subscriber pays 100 percent of allowable charges for medical costs In-network provider: SHP allowance applies toward deductible § Out-of-network provider: SHP allows only what Plan would have allowed if subscriber used innetwork provider §
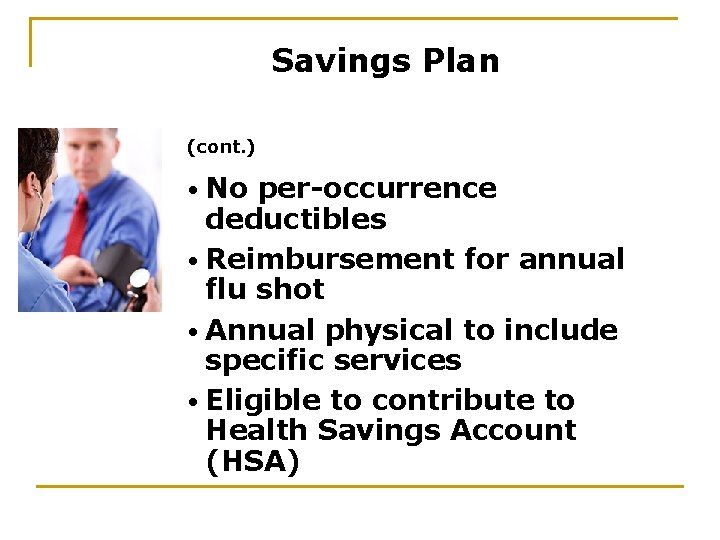
Savings Plan (cont. ) • No per-occurrence deductibles • Reimbursement for annual flu shot • Annual physical to include specific services • Eligible to contribute to Health Savings Account (HSA)
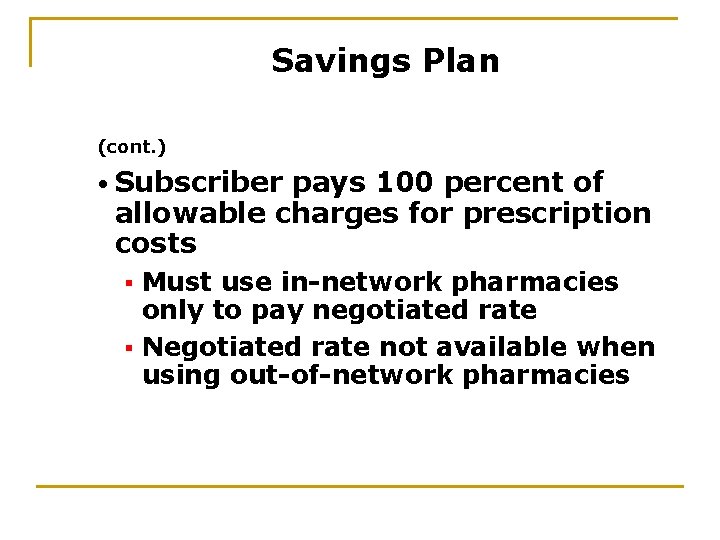
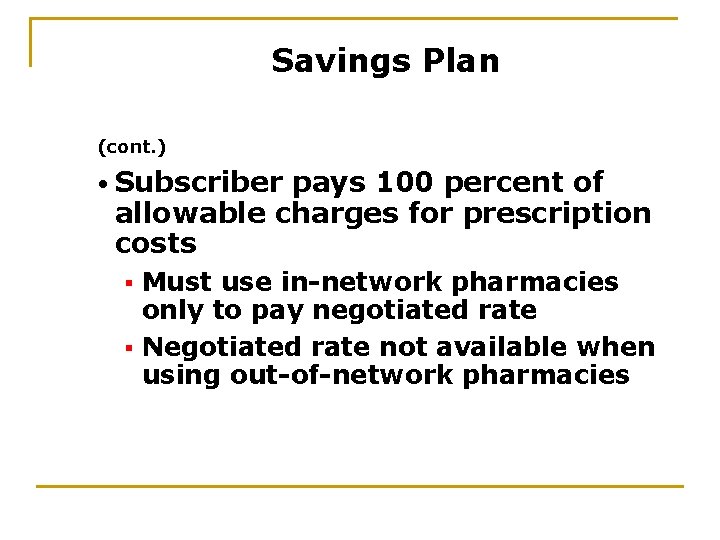
Savings Plan (cont. ) • Subscriber pays 100 percent of allowable charges for prescription costs Must use in-network pharmacies only to pay negotiated rate § Negotiated rate not available when using out-of-network pharmacies §
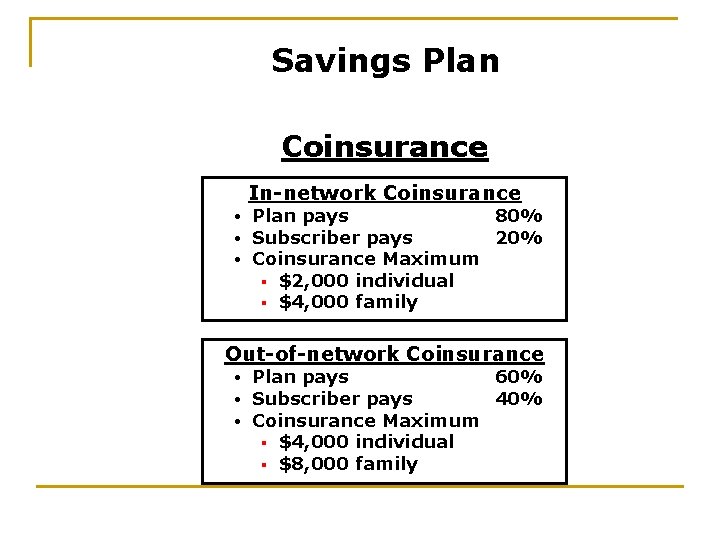
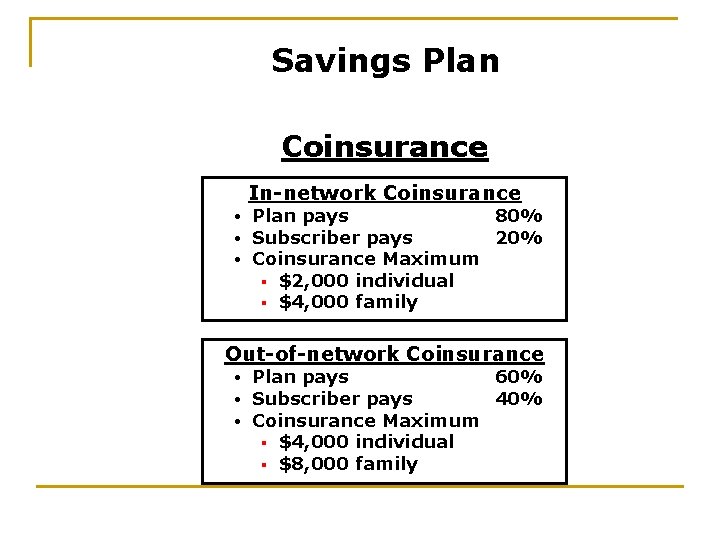
Savings Plan Coinsurance In-network Coinsurance • • • Plan pays 80% Subscriber pays 20% Coinsurance Maximum § $2, 000 individual § $4, 000 family Out-of-network Coinsurance • • • Plan pays 60% Subscriber pays 40% Coinsurance Maximum § $4, 000 individual § $8, 000 family
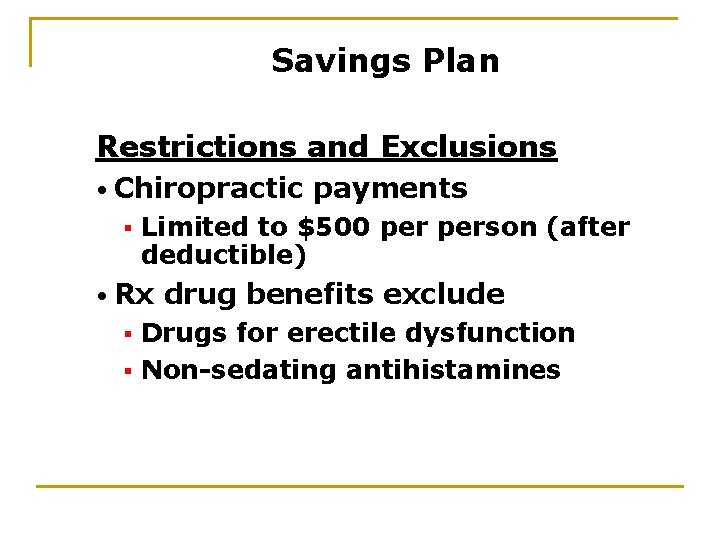
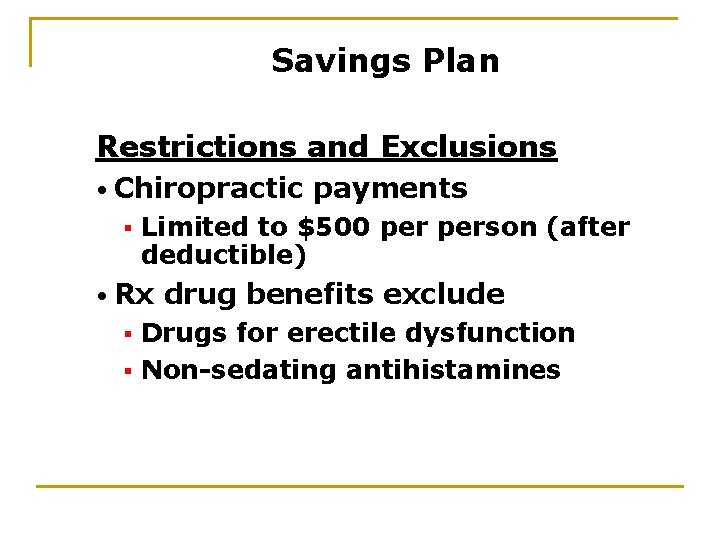
Savings Plan Restrictions and Exclusions • Chiropractic § payments Limited to $500 person (after deductible) • Rx drug benefits exclude Drugs for erectile dysfunction § Non-sedating antihistamines §
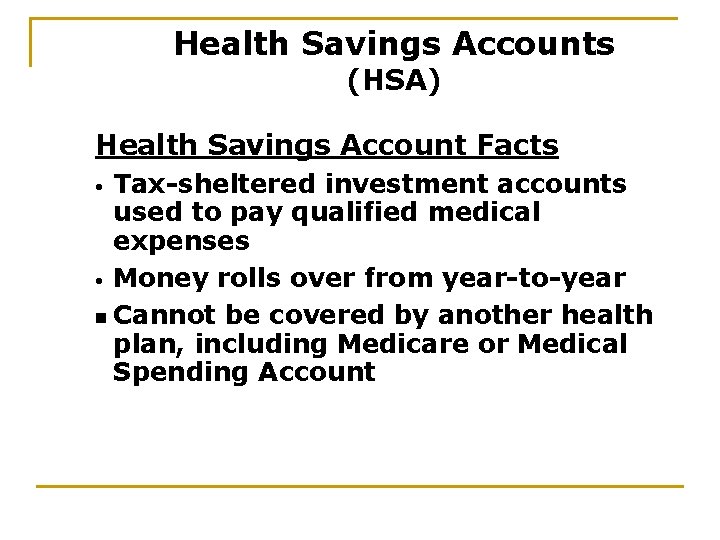
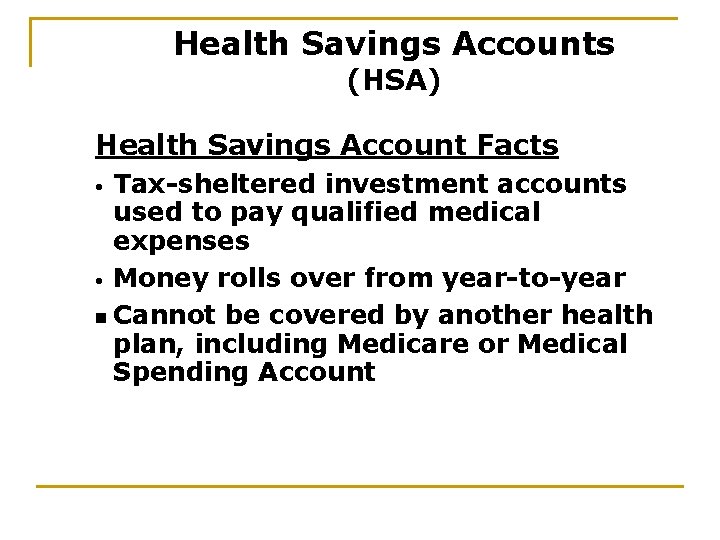
Health Savings Accounts (HSA) Health Savings Account Facts Tax-sheltered investment accounts used to pay qualified medical expenses • Money rolls over from year-to-year n Cannot be covered by another health plan, including Medicare or Medical Spending Account •
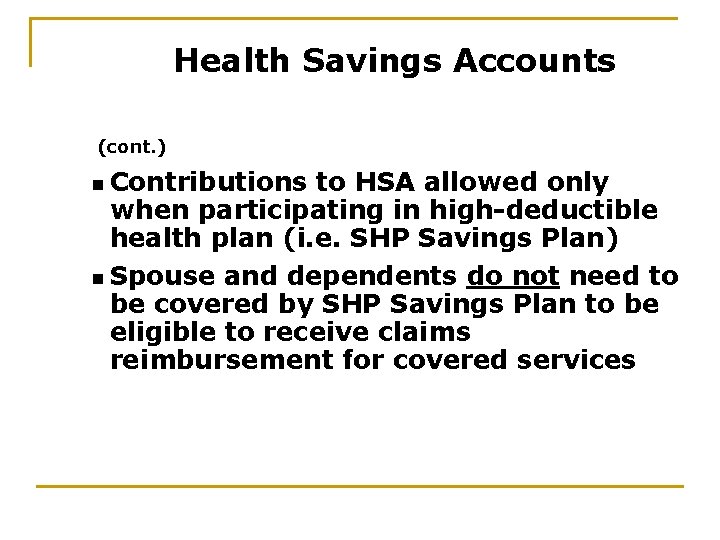
Health Savings Accounts (cont. ) n Contributions to HSA allowed only when participating in high-deductible health plan (i. e. SHP Savings Plan) n Spouse and dependents do not need to be covered by SHP Savings Plan to be eligible to receive claims reimbursement for covered services
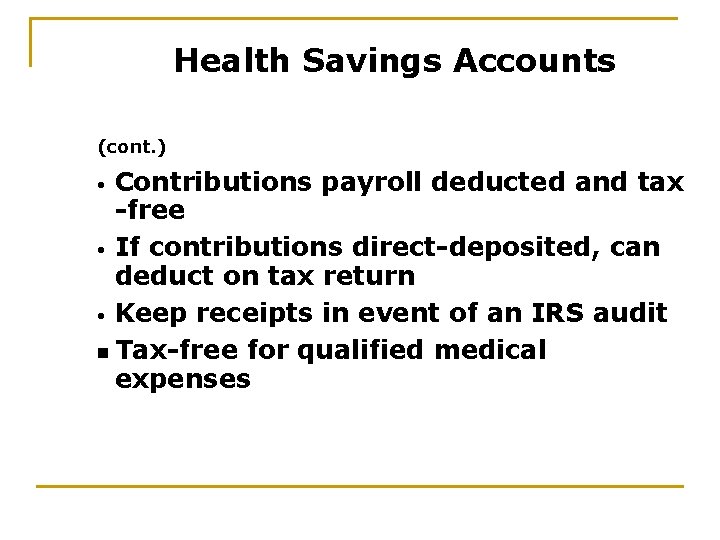
Health Savings Accounts (cont. ) Contributions payroll deducted and tax -free • If contributions direct-deposited, can deduct on tax return • Keep receipts in event of an IRS audit n Tax-free for qualified medical expenses •
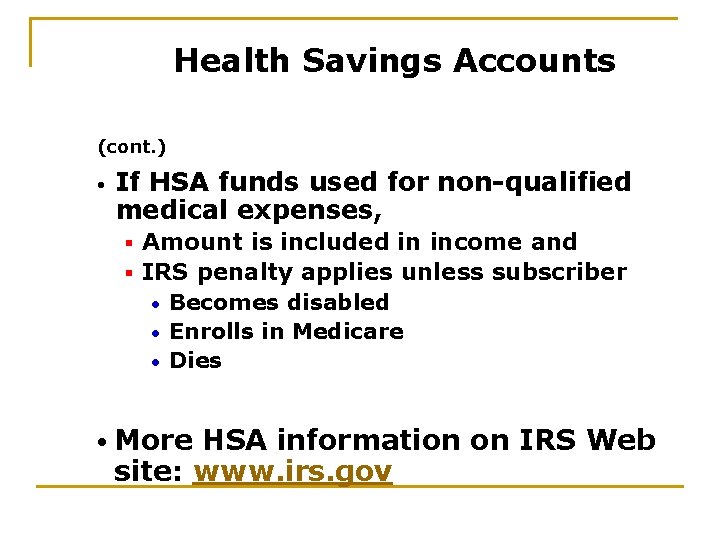
Health Savings Accounts (cont. ) • If HSA funds used for non-qualified medical expenses, Amount is included in income and § IRS penalty applies unless subscriber • Becomes disabled • Enrolls in Medicare • Dies § • More HSA information on IRS Web site: www. irs. gov
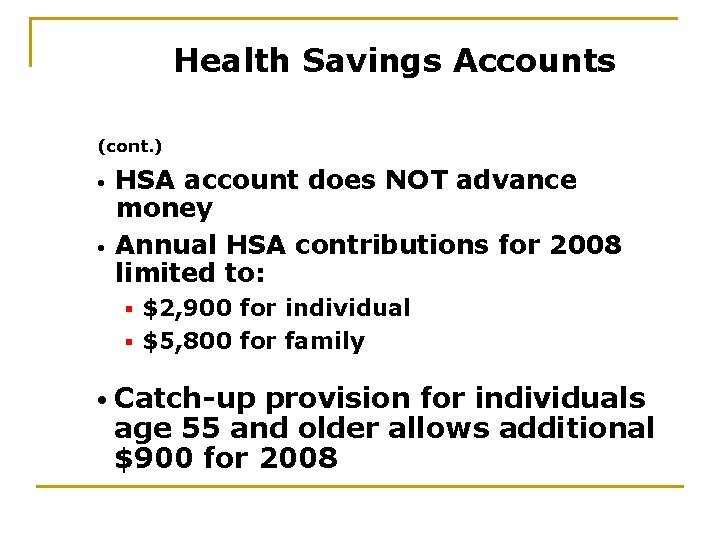
Health Savings Accounts (cont. ) • • HSA account does NOT advance money Annual HSA contributions for 2008 limited to: $2, 900 for individual § $5, 800 for family § • Catch-up provision for individuals age 55 and older allows additional $900 for 2008
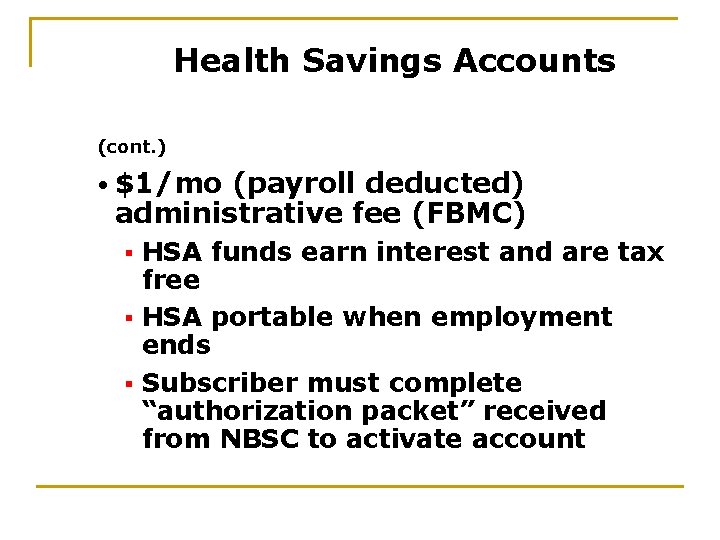
Health Savings Accounts (cont. ) • $1/mo (payroll deducted) administrative fee (FBMC) HSA funds earn interest and are tax free § HSA portable when employment ends § Subscriber must complete “authorization packet” received from NBSC to activate account §
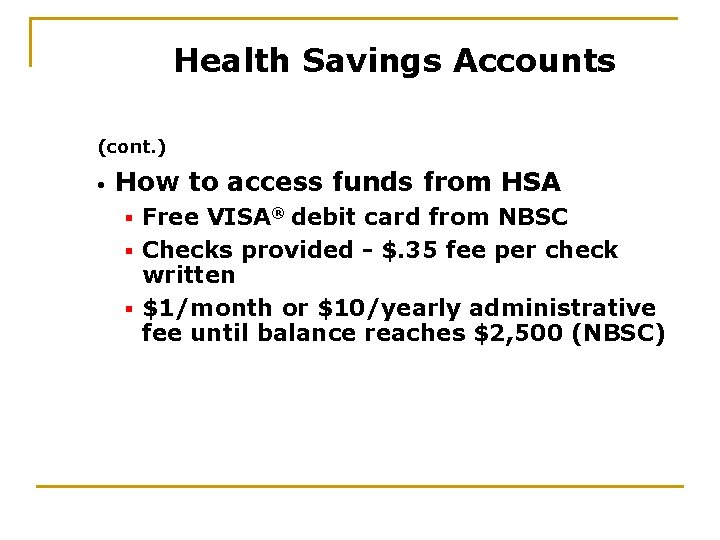
Health Savings Accounts (cont. ) • How to access funds from HSA Free VISA® debit card from NBSC § Checks provided - $. 35 fee per check written § $1/month or $10/yearly administrative fee until balance reaches $2, 500 (NBSC) §
“Limited Use” Medical Spending Accounts (MSA) “Limited Use” MSA Facts n Can use for vision and dental expenses only (maximum $5, 000) $3. 50 per month administrative fee applies § Must be continuously employed for one year to enroll §
“Limited Use” Medical Spending Accounts (MSA) (cont. ) • “Use it or lose it” (funds do not roll over as with HSA) • Claims must be incurred by March 15 th grace period and submitted by March 31 st • Not eligible for EZ REIMBURSE® Card
Insurance Education Part #2 My Insurance Manager BCBS of South Carolina www. southcarolinablues. com
My Insurance Manager BCBS of South Carolina (www. southcarolinablues. com) My Insurance Manager’s Features • Review claims via BCBS Web site • View and print Explanation of Benefits (EOB) • See amount paid toward deductible and coinsurance maximum • Secure E-mail customer service questions • View up-to-date provider directory • Request new ID card
Insurance Education Part #2 Health Insurance Options Health Maintenance Organizations (HMOs)
Health Maintenance Organizations (HMOs) Rules • • • Subscribers must choose primary care physician (PCP) Referral required for most specialty care You must live or work in HMO service area
Health Maintenance Organizations (HMOs) (cont. ) • • • Provide qualified emergency service out-of-network No non-emergency out-of-network benefits Read HMO materials carefully before making health plan selection
Insurance Education Part #2 Blue. Choice Health. Plan
Blue. Choice Health. Plan (available in all South Carolina counties) Features • Annual deductible Amount subscriber pays before HMO begins paying (deductible does not apply to PCP charges) § $250 individual § $500 family §
Blue. Choice Health. Plan (available in all South Carolina counties) (cont. ) • After subscriber pays annual deductible and copayment, plan pays 90 percent of allowable charges subscriber pays 10 percent, which applies to coinsurance maximum
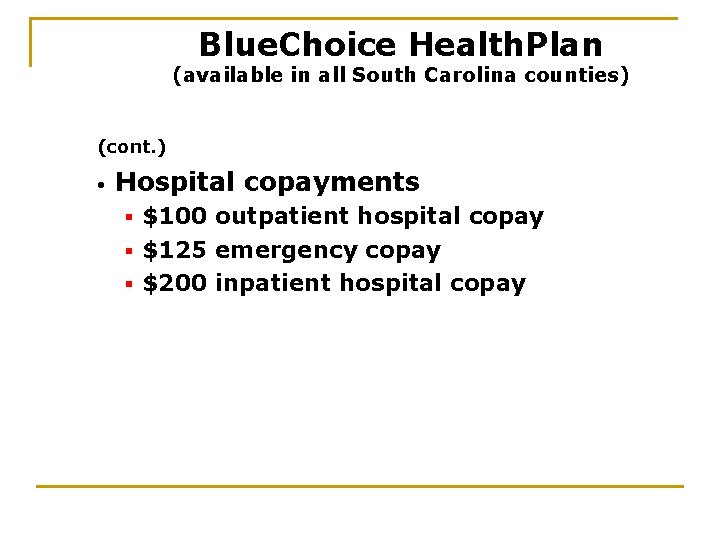
Blue. Choice Health. Plan (available in all South Carolina counties) (cont. ) • Hospital copayments $100 outpatient hospital copay § $125 emergency copay § $200 inpatient hospital copay §
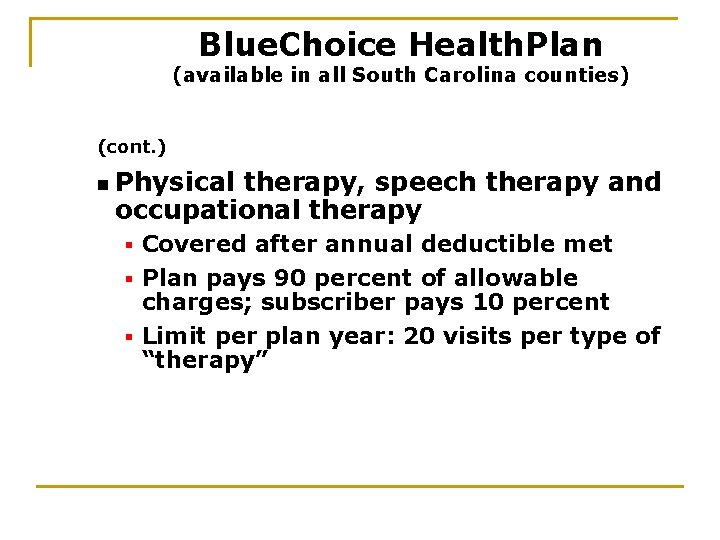
Blue. Choice Health. Plan (available in all South Carolina counties) (cont. ) n Physical therapy, speech therapy and occupational therapy Covered after annual deductible met § Plan pays 90 percent of allowable charges; subscriber pays 10 percent § Limit per plan year: 20 visits per type of “therapy” §
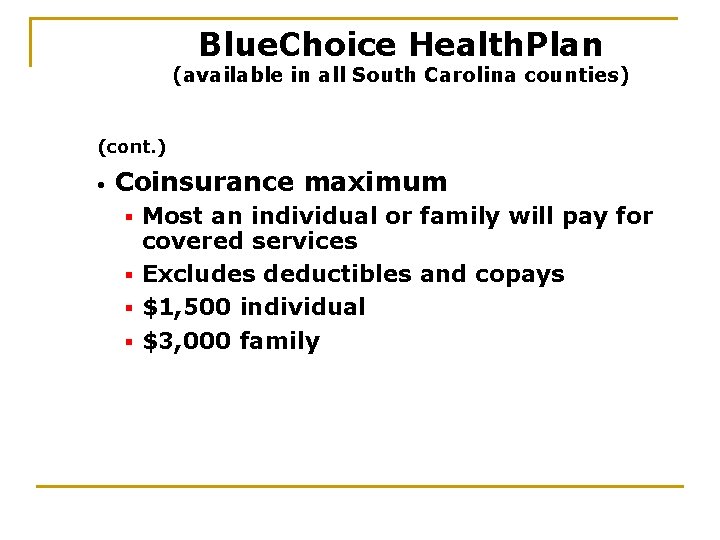
Blue. Choice Health. Plan (available in all South Carolina counties) (cont. ) • Coinsurance maximum Most an individual or family will pay for covered services § Excludes deductibles and copays § $1, 500 individual § $3, 000 family §
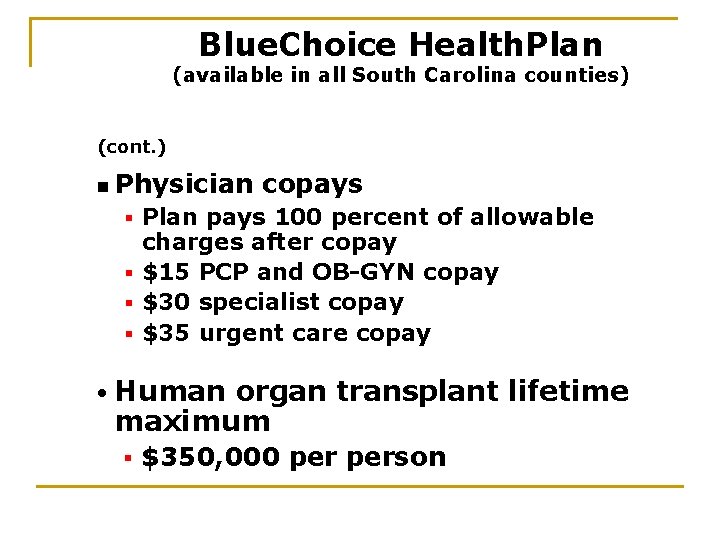
Blue. Choice Health. Plan (available in all South Carolina counties) (cont. ) n Physician copays Plan pays 100 percent of allowable charges after copay § $15 PCP and OB-GYN copay § $30 specialist copay § $35 urgent care copay § • Human organ transplant lifetime maximum § $350, 000 person
Blue. Choice Health. Plan (available in all South Carolina counties) (cont. ) • Tobacco cessation benefits available Free for subscribers and covered dependents, age 18 and older § Contact Free & Clear at: § 866 -Quit-4 -Life (866 -784 -8454)
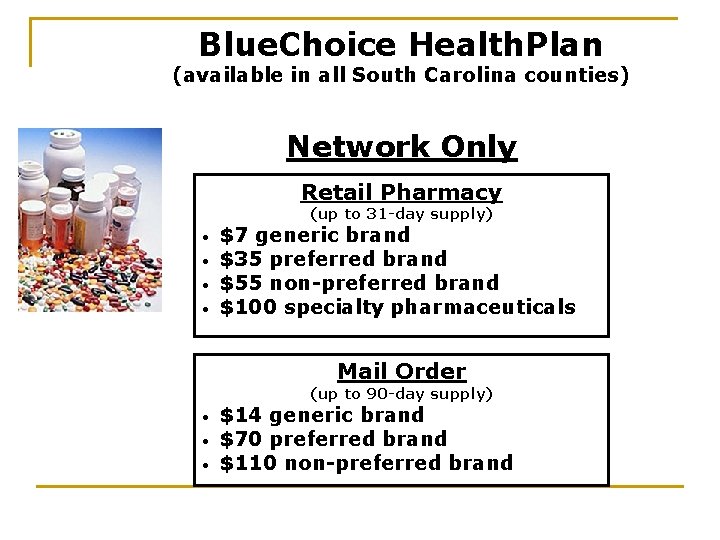
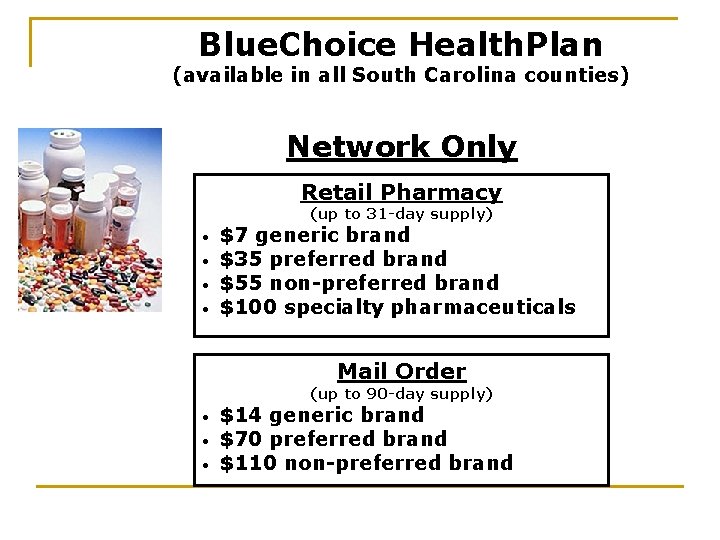
Blue. Choice Health. Plan (available in all South Carolina counties) Network Only Retail Pharmacy (up to 31 -day supply) • • $7 generic brand $35 preferred brand $55 non-preferred brand $100 specialty pharmaceuticals Mail Order (up to 90 -day supply) • • • $14 generic brand $70 preferred brand $110 non-preferred brand
Insurance Education Part #2 CIGNA HMO
CIGNA HMO (available in all South Carolina counties except: Abbeville, Aiken, Barnwell, Edgefield, Greenwood, Laurens, Mc. Cormick and Saluda) Features • Annual deductible: none • HMO pays 80 percent of allowable charges • Subscriber pays 20 percent -applies toward coinsurance maximum
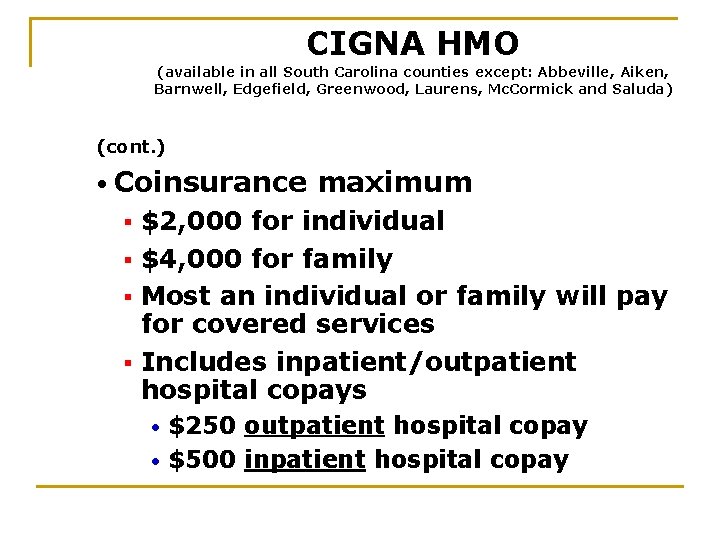
CIGNA HMO (available in all South Carolina counties except: Abbeville, Aiken, Barnwell, Edgefield, Greenwood, Laurens, Mc. Cormick and Saluda) (cont. ) • Coinsurance maximum $2, 000 for individual § $4, 000 for family § Most an individual or family will pay for covered services § Includes inpatient/outpatient hospital copays § $250 outpatient hospital copay • $500 inpatient hospital copay •
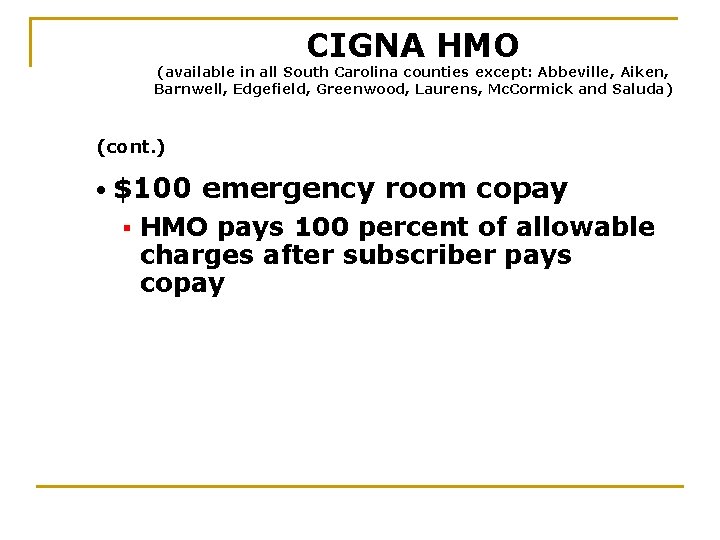
CIGNA HMO (available in all South Carolina counties except: Abbeville, Aiken, Barnwell, Edgefield, Greenwood, Laurens, Mc. Cormick and Saluda) (cont. ) • $100 § emergency room copay HMO pays 100 percent of allowable charges after subscriber pays copay
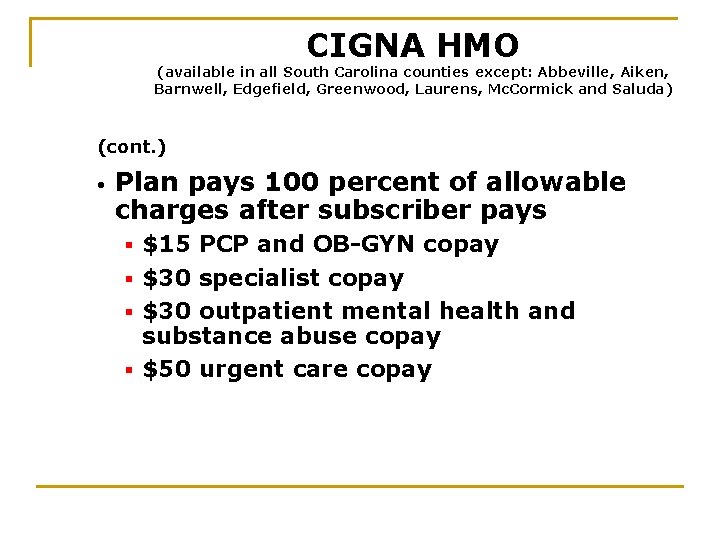
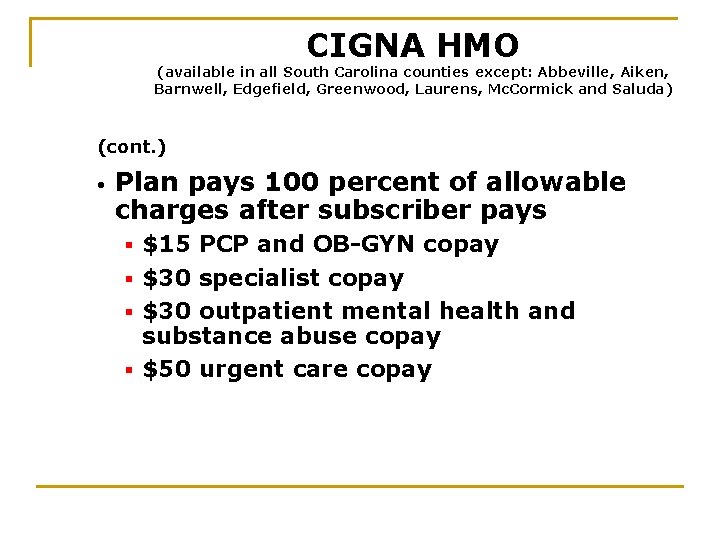
CIGNA HMO (available in all South Carolina counties except: Abbeville, Aiken, Barnwell, Edgefield, Greenwood, Laurens, Mc. Cormick and Saluda) (cont. ) • Plan pays 100 percent of allowable charges after subscriber pays $15 PCP and OB-GYN copay § $30 specialist copay § $30 outpatient mental health and substance abuse copay § $50 urgent care copay §
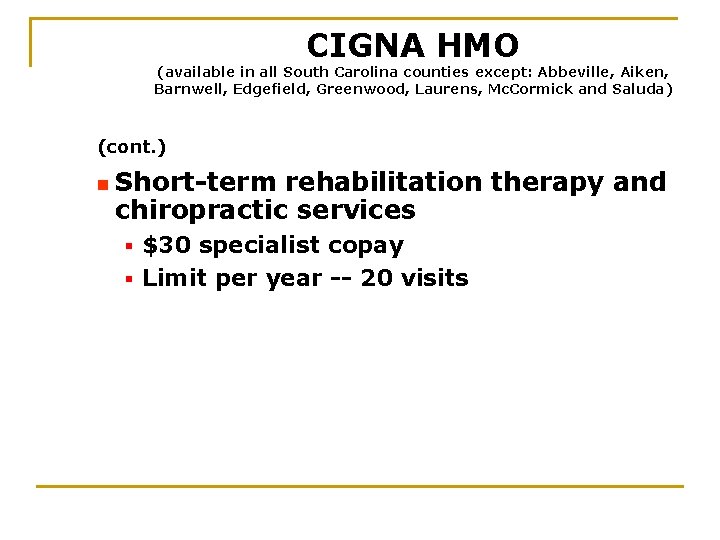
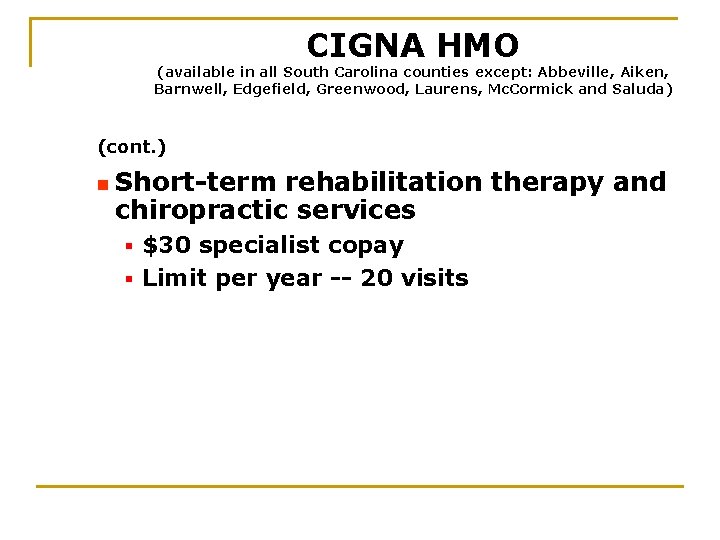
CIGNA HMO (available in all South Carolina counties except: Abbeville, Aiken, Barnwell, Edgefield, Greenwood, Laurens, Mc. Cormick and Saluda) (cont. ) n Short-term rehabilitation therapy and chiropractic services $30 specialist copay § Limit per year -- 20 visits §
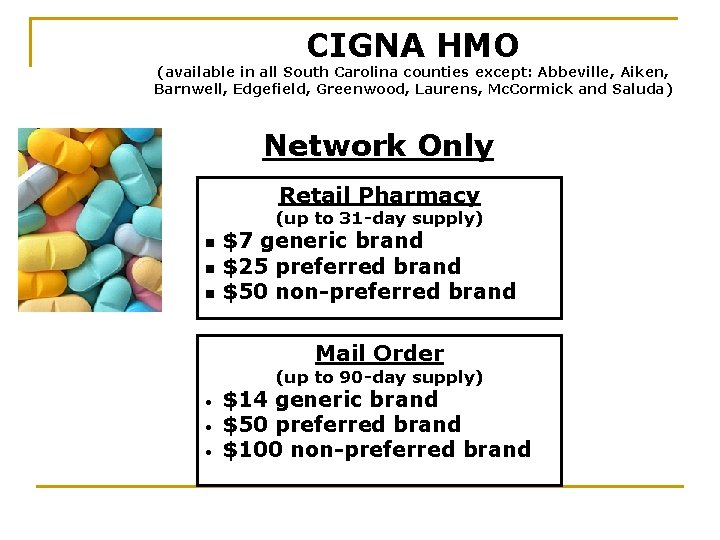
CIGNA HMO (available in all South Carolina counties except: Abbeville, Aiken, Barnwell, Edgefield, Greenwood, Laurens, Mc. Cormick and Saluda) Network Only Retail Pharmacy (up to 31 -day supply) n n n $7 generic brand $25 preferred brand $50 non-preferred brand Mail Order (up to 90 -day supply) • • • $14 generic brand $50 preferred brand $100 non-preferred brand
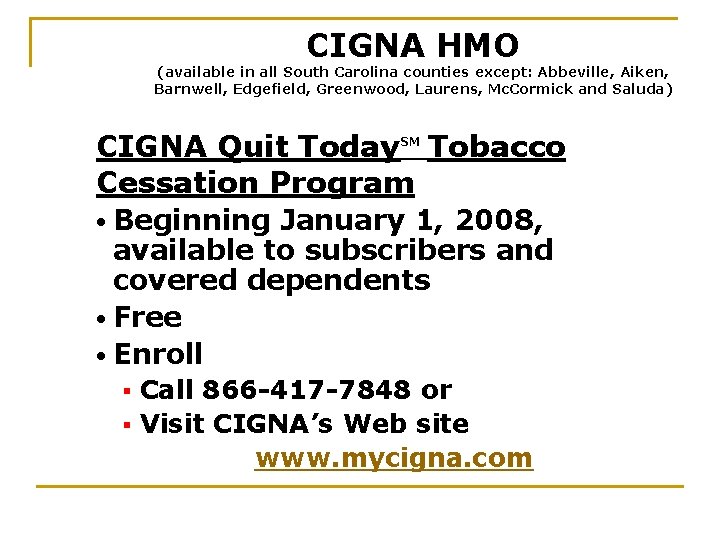
CIGNA HMO (available in all South Carolina counties except: Abbeville, Aiken, Barnwell, Edgefield, Greenwood, Laurens, Mc. Cormick and Saluda) CIGNA Quit Today Tobacco Cessation Program SM • Beginning January 1, 2008, available to subscribers and covered dependents • Free • Enroll Call 866 -417 -7848 or § Visit CIGNA’s Web site www. mycigna. com §
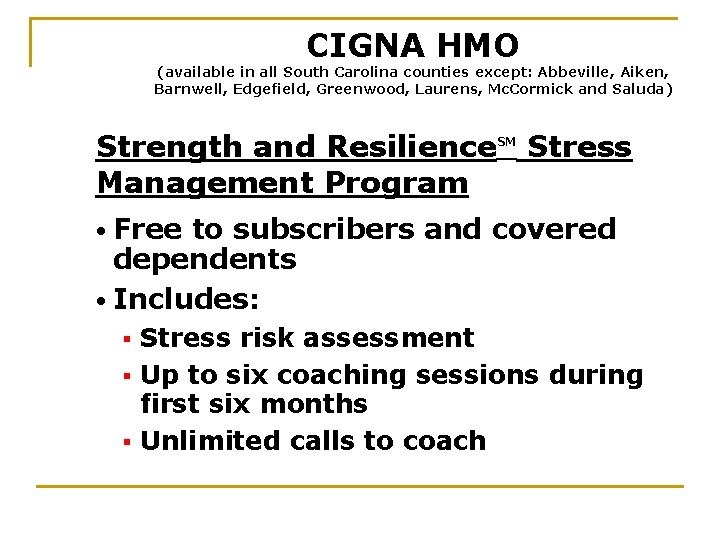
CIGNA HMO (available in all South Carolina counties except: Abbeville, Aiken, Barnwell, Edgefield, Greenwood, Laurens, Mc. Cormick and Saluda) Strength and Resilience Management Program SM Stress • Free to subscribers and covered dependents • Includes: Stress risk assessment § Up to six coaching sessions during first six months § Unlimited calls to coach §
CIGNA HMO (available in all South Carolina counties except: Abbeville, Aiken, Barnwell, Edgefield, Greenwood, Laurens, Mc. Cormick and Saluda) (cont. ) • To enroll Call 866 -417 -7848 or § Visit CIGNA’s Web site: www. mycigna. com §
Insurance Education Part #2 Active Employee Health Plan Premiums
Active Employee Monthly Health Premiums
 Uw madison student health insurance
Uw madison student health insurance Nature of fire insurance
Nature of fire insurance Postsecondary education options
Postsecondary education options Difference between health promotion and health education
Difference between health promotion and health education Types of instructional materials
Types of instructional materials Health education and propaganda
Health education and propaganda 877-804-1679
877-804-1679 Part whole model subtraction
Part whole model subtraction Unit ratio definition
Unit ratio definition Part part whole
Part part whole Define technical description
Define technical description Dispense bar layout
Dispense bar layout The part of a shadow surrounding the darkest part
The part of a shadow surrounding the darkest part 미니탭 gage r&r 해석
미니탭 gage r&r 해석 Ttuhsc sakai
Ttuhsc sakai Fau health insurance
Fau health insurance Umms employee benefits
Umms employee benefits Blue cross tonik plan
Blue cross tonik plan Ouhsc student health
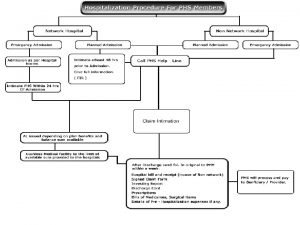
Ouhsc student health Raksha tpa claim
Raksha tpa claim Myfrs.com investment plan
Myfrs.com investment plan Health insurance market segmentation
Health insurance market segmentation Deloitte health insurance
Deloitte health insurance What is deductible in health insurance
What is deductible in health insurance Hipp program ny
Hipp program ny Commonwealth health insurance connector
Commonwealth health insurance connector Chapter 14 health disability and life insurance
Chapter 14 health disability and life insurance Aditya birla nuvo health insurance
Aditya birla nuvo health insurance Statewide health insurance benefits advisors
Statewide health insurance benefits advisors Paramounttpa
Paramounttpa Ceww health insurance consortium
Ceww health insurance consortium Religare health insurance franchise
Religare health insurance franchise Missouri state health insurance assistance program
Missouri state health insurance assistance program Ira b wilson
Ira b wilson Healthscope benefits whirlpool
Healthscope benefits whirlpool Pace university health insurance
Pace university health insurance Cm health insurance belgium
Cm health insurance belgium Chickasaw nation health insurance
Chickasaw nation health insurance Panabridge advantage plan reviews
Panabridge advantage plan reviews Keller isd health insurance
Keller isd health insurance Whirlpool health insurance
Whirlpool health insurance Early arrival student health insurance asu
Early arrival student health insurance asu Small business health insurance delaware
Small business health insurance delaware Small business health insurance delaware
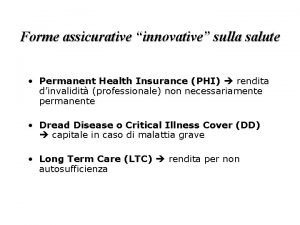
Small business health insurance delaware Phi permanent health insurance
Phi permanent health insurance Uib health insurance
Uib health insurance Characteristics of health insurance
Characteristics of health insurance Allianz cern mpa
Allianz cern mpa Travel health insurance association annual conference
Travel health insurance association annual conference Unl student health insurance
Unl student health insurance Paramount tpa hospital list
Paramount tpa hospital list Free health insurance
Free health insurance Predictive analytics in health insurance
Predictive analytics in health insurance Wsu health insurance
Wsu health insurance Etsu health insurance
Etsu health insurance Ouhsc health club
Ouhsc health club New mexico health insurance pool
New mexico health insurance pool Dchr health insurance
Dchr health insurance Colorado health insurance cooperative
Colorado health insurance cooperative Chapman university financial services
Chapman university financial services Unit 2 lesson 3 health insurance and financial planning
Unit 2 lesson 3 health insurance and financial planning Unit 2 lesson 3 health insurance and financial planning
Unit 2 lesson 3 health insurance and financial planning Chip adultbasic health insurance
Chip adultbasic health insurance Ace health insurance
Ace health insurance What was the union's three part plan
What was the union's three part plan Part plan
Part plan What was the third part of james k. polk's war plan?
What was the third part of james k. polk's war plan? Difference between education and literacy
Difference between education and literacy Types of extension education
Types of extension education What options did an accused witch have in salem?
What options did an accused witch have in salem? Systems analysis and design in an age of options
Systems analysis and design in an age of options Policyrules
Policyrules Putcall parity
Putcall parity Standard deviation options
Standard deviation options Steadyoptions review
Steadyoptions review Options for formulating a digital transformation strategy.
Options for formulating a digital transformation strategy. Options appraisal template
Options appraisal template Global operations strategy
Global operations strategy Molina medicare washington
Molina medicare washington Wan concepts
Wan concepts Tug of war visible thinking
Tug of war visible thinking Macro instruction arguments
Macro instruction arguments Linkage loader and linkage editor
Linkage loader and linkage editor Atm wan technology
Atm wan technology Ramya ullagaddimath
Ramya ullagaddimath